SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING
THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
JANUARY 2019
The Steering Committee for the ABA Services Workgroup (representatives of the organizations shown above
and their CPT consultant) prepared this article to assist providers, billers, and payers in using the Category I
and modied Category III CPT codes for adaptive behavior services that go into effect January 1, 2019. This
document is meant to supplement the essential information about the new codes that is published in the 2019 CPT
Code book (available from the American Medical Association [AMA] Store) and an article in the November 2018
issue of the CPT Assistant newsletter, which can be purchased by calling 1-800-621-8335, selecting option 2 in
the recorded menu, and asking for item BI506118.
In this article, we provide the descriptor for each code and the typical patient
1
vignette that the AMA CPT
®
Editorial Panel approved, followed by a clinical example illustrating the use of that code. Importantly, the
examples for the codes representing services provided directly to patients or caregivers specify indirect services
that occur prior to and after an assessment or treatment session conducted with a patient of caregiver, as well
as services provided face-to-face with the patient or caregiver during the session. Only the face-to-face time is
reported for billing purposes with CPT codes (with the exception of CPT code 97151). There is no CPT code for
reporting the indirect services separately, so they must be bundled with direct services for payment unless the
contract with the payer includes a HCPCS or other code for reporting indirect services. As used here, bundled
payment refers to payment for the work done prior to face-to-face time with the patient or caregiver (e.g.,
reviewing records), the work done with the patient or caregiver (e.g., delivering the treatment), and the work done
after the face-to-face time with the patient or caregiver (e.g., writing a progress note). When payment is bundled,
the face-to-face time is reported, but the work done prior to and after the face-to-face time is factored into the
reimbursement rate. For CPT codes where the face-to-face service is delivered by a technician, the work related to
that service that is completed by the technician and/or the QHP prior to and after the face-to-face time is factored
into the reimbursement rate for that code.
97151
Behavior identification assessment, administered by a physician or other qualified health care
professional, each 15 minutes of the physician’s or other qualified health care professional’s
time face-to-face with patient and/or guardian(s)/caregiver(s) administering assessments and
discussing findings and recommendations, and non-face-to-face analyzing past data, scoring/
interpreting the assessment, and preparing the report/treatment plan
TYPICAL PATIENT: A 3-year-old male is brought in by his parents for an assessment. The patient has
nonfunctional speech, poor eye contact, repetitive motor movements, tantrums with unexpected changes in
routines, and ritualistic play. He does not respond to gestures or his name and has almost no imitative behavior.
1 The term “patient” is used throughout to be consistent with the code descriptors.
Stefanie Koehler Designs_BACB_113011 BACB LOGO VECTOR MASTER FILE
CONTACT :: Stefanie Koehler • [email protected] • 604-563-9412 • Vancouver, BC, Canada
Association of
Professional
Behavior Analysts

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 2 -
CLINICAL EXAMPLE:
Prior to the appointment, the qualied health care professional (QHP) reviews the child’s medical records,
previous assessments, and records of any previous or current treatments. Just before the assessment
session, the QHP gathers all materials required for that session.
During the session (face-to-face), the QHP conducts a structured interview with the parents to solicit their
observations about the child’s decient adaptive behaviors (e.g., social, communication, or self-care skills),
maladaptive behaviors, and other concerns. The QHP conducts a series of indirect and direct assessments to
identify potential skills to be strengthened and maladaptive behaviors to be reduced by treatment.
Indirect assessments include standardized and non-standardized scales and checklists completed by the
parents and other caregivers to evaluate the patient’s adaptive skills in several domains. Direct assessments
of adaptive skills include direct observation and recording of the child’s performance of skills in typical
everyday situations, including information about the type and amount of assistance (cues, prompts) the child
requires to perform each skill successfully and the types of reinforcers for which the child responds. Direct
assessments of maladaptive behaviors include a functional behavior assessment comprising an interview with
the parents about environmental events that may precede and follow occurrences of maladaptive behaviors,
and observations of the child in several everyday settings to record occurrences of tantrums, repetitive
movements, and other maladaptive behaviors as well as environmental events that precede and follow those
occurrences. Information from the functional behavior assessment is used to design functional analyses of
tantrums and ritualistic behaviors. These assessments may be conducted over several days of service.
After: The data from all assessments are used to develop a treatment plan with goals and objectives, including
social, communication, play and leisure, self-care, and other skills to be developed and maladaptive
behaviors to be reduced, all dened in observable, measurable terms. The plan also species for each
treatment target: (a) the current (baseline) level; (b) procedures for direct observation and measurement; (c)
conditions under which the behavior is to occur; (d) a written protocol with instructions for implementing
procedures (e.g., materials needed, instructions, prompting and prompt-fading, consequences for correct
and incorrect responses, etc.) to change the behavior and promote generalization of behavior changes; and
(e) criteria for mastery or attainment of the treatment goal.
Q: Is 97151 intended to be used for day-to-day assessment and treatment planning?
A: No. This code is intended for reporting initial assessment and treatment plan development and reassessment
and progress reporting by the QHP (timeframes for reassessments are determined by payer policy or medical
necessity). 97151 includes face-to-face time with the patient and/or caregivers to conduct assessments as well as
non-face-to-face time for reviewing records, scoring and interpreting assessments, and writing the treatment plan
or progress report. The QHP must have conducted both the face-to-face and non-face-to-face activities to report
this service. Day-to-day assessment and treatment planning by the QHP are bundled into the treatment codes
below (i.e., 97153-97158 and 0373T); therefore, 97151 cannot be used to report those indirect services because
they do not meet all requirements of the code descriptor.
Q: Why does 97151 include non-face-to-face work and the other codes in the 2019 set do not?
A: Assessments and reassessments require extensive non-face-to-face time for the QHP to score assessments,
review records and data, and write or update the treatment plan. That can take several hours, and in many cases
occurs across multiple dates of service. That is why only this code allows for reporting of non-face-to-face time.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 3 -
97152
Behavior identification supporting assessment, administered by one technician under the
direction of a physician or other qualified health care professional, face-to-face with the
patient, each 15 minutes
TYPICAL PATIENT: A 10-year-old female requires an additional assessment for severe stereotypic behavior
that interferes with acquisition of adaptive skills.
CLINICAL EXAMPLE:
Prior: Once the QHP has determined from the initial assessment that the stereotypic behavior is a treatment
target and that more information is needed to develop appropriate treatment protocols, the QHP directs the
technician to directly observe and record occurrences of the behavior in everyday situations. The technician
and the QHP review information about the patient’s stereotypic behavior from the behavior identication
assessment, the denition of that behavior, and procedures for directly observing and measuring occurrences
of the behavior and environmental events that precede and follow occurrences. The technician practices
observing and recording occurrences of the behavior from a live or recorded sample that is also scored by
the QHP. The QHP compares his/her data to the data recorded by the technician and provides feedback to the
technician regarding the accuracy and completeness of the technician’s data recording until the technician
demonstrates prociency. Prior to the assessment session the technician gathers all materials required
for that session. The technician also reviews the data and session notes from the most recent treatment
sessions, if applicable.
During the session (face-to-face), the behavior technician, under the direction of the QHP, observes and records
occurrences of the patient’s stereotypic behavior and environmental events that precede and follow those
occurrences several times in a variety of situations.
After the session, the technician graphs the resulting data, indicating on the graph the date, time, and context for
each of the data samples. The QHP reviews and analyzes the graphed data from the technician’s observations
of the patient’s stereotypic behavior and writes a progress note with a plan of action.
Q: Does the descriptor for 97152 indicate that technicians can perform assessments independently?
A: No. This code is for reporting supplemental assessments conducted by the technician that the QHP determines
are needed to develop the treatment plan or progress report (see code 97151). Additionally, as indicated in the
clinical example, the QHP reviews the assessment procedures with the technician and has the technician practice
recording data. That may occur on the day of an assessment session with a patient or several days leading up to
the session(s). That work by the QHP is bundled into the value of code 97152 and is not reported separately.
0362T
Behavior identification supporting assessment, each 15 minutes of technicians’ time
face-to-face with a patient, requiring the following components:
• administered by the physician or other qualified health care professional who is on site,
• with the assistance of two or more technicians,
• for a patient who exhibits destructive behavior,
• completed in an environment that is customized to the patient’s behavior.
TYPICAL PATIENT: A 26-year-old male requires additional assessment of a behavior – hitting his head with his
sts – that is at risk of becoming self-injurious. Initial direct observation and measurement shows that the behavior
occurs more than 50 times per hour on average.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 4 -
CLINICAL EXAMPLE:
Prior: The QHP reviews prior records and all prior functional behavior assessments and functional analyses and
attempts to treat SIB, including behavioral and pharmacologic interventions. He completes a risk assessment
to determine safeguards needed to conduct a functional analysis safely, prepares materials, and briefs the
technicians regarding idiosyncratic aspects of the patient’s behavior.
During the session (face-to-face), three technicians work with the patient in a safe environment according to a
QHP-designed protocol. During each of the functional analysis sessions, one technician collects continuous
real-time data on the patient’s SIB and communication responses, a second technician stands closely behind
the patient and gently blocks his attempts at SIB directed toward the eyes, and the third technician carries out
the QHP-designed functional analysis procedures. The QHP is on site and closely monitors the technicians’
implementation of the procedures, providing corrective feedback when needed.
After: Technicians record all results and provide data to the QHP following each session. The QHP analyzes the
graphed data on an ongoing basis and, if needed, modies the assessment protocol appropriately.
Q: What is meant by “on site”?
A: On site is dened as the QHP being “immediately available and interruptible.” This means that the QHP is
at the same site and can join the session if needed.
Q: Can 0362T be reported when additional technicians are needed for safety, but on an impromptu basis
(e.g., if a destructive behavior occurs unexpectedly and a second or third technician steps in to help)?
A: No. These services should be preauthorized for cases where all four of the criteria in the code descriptor are met.
Q: What is meant by a “customized environment”?
A: For codes 0362T and 0373T, the term “customized” means that the environment is congured to safely
conduct a functional analysis of destructive behavior (0362T) or treatment for that behavior (0373T). For
some patients, this can be accomplished in the home. For example, in the case of a patient who displays
aggression using objects, those objects that the patient might use as dangerous weapons (e.g., a wooden
baseball bat) would be removed and replaced with soft items (e.g., a foam baseball bat). Other patients may
require treatment in a padded treatment room. For example, a patient with severe head banging may require
functional analysis and initial treatment in a padded treatment room because the behavior causes tissue
damage and places the patient at risk for detached retinas.
97153
Adaptive behavior treatment by protocol, administered by technician under the direction
of a physician or other qualified health care professional, face-to-face with one patient, each
15 minutes
TYPICAL PATIENT: A 4-year-old female presents with decits in language and social skills. She engages in
perseverative speech on one or two preferred topics and displays strong emotional outbursts in response to small
changes in routines or when preferred items are unavailable.
CLINICAL EXAMPLE:
Prior to the rst implementation of any treatment protocols, the QHP and technician review the denitions of
treatment targets in the areas of language, social skills, responding to changes in routines, and responding
to the unavailability of preferred items in the patient’s treatment plan as well as the written protocols
for addressing each of those targets. Prior to each treatment session, the technician gathers all materials
required for that session. The technician also reviews the data and session notes from the most recent
treatment sessions.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 5 -
During each session (face-to-face), the technician implements the treatment protocols and data collection
procedures with the patient in the family home and selected community settings. Sessions are designed
to provide multiple planned opportunities for the patient to practice each target skill.
After the session, the technician records notes summarizing what occurred and any aspects of the behavioral
denitions or treatment protocols that may need to be scrutinized by the QHP. The QHP reviews technician-
recorded graphed data and notes from all treatment sessions weekly to assess the child’s progress and
determine if any treatment targets or protocols need to be revised.
Q: How do I report a typical direct treatment session that is rendered by a QHP?
A: If no protocols have been modied and a QHP is simply acting in place of the technician, report 97153 with
a modier to indicate the higher-level service provider.
Q: Can I report 97153 and 97155 concurrently?
A: Yes, as long as the criteria in the descriptors of both codes are met. A single QHP may not report 97153 and
97155 concurrently. See the Concurrent Billing Overview table in the Other Frequently Asked Questions section.
97154
Group adaptive behavior treatment by protocol, administered by technician under the direction
of a physician or other qualified health care professional, face-to-face with two or more patients,
each 15 minutes
TYPICAL PATIENT: A 7-year-old female exhibits decits in social skills. The patient is verbal and has emerging
social skills as a result of one-to-one therapy designed to teach basic communication and social interactions. Peer
social skills training in a small group is recommended.
CLINICAL EXAMPLE:
Prior to the treatment session, the QHP and technician review the data and notes from the most recent treatment
session, the treatment protocol, and the data collection procedures. Prior to each treatment session, the
technician gathers all materials required for that session. The technician also reviews the data and session
notes from the most recent treatment sessions.
During the session (face-to-face), the QHP directs a technician in the implementation of the patient’s treatment
protocol and data collection procedures in small-group activities conducted by the technician. The
technician implements the treatment protocols and data collection procedures with the patient(s). Sessions
are designed to provide multiple planned opportunities for the patient(s) to practice each target skill.
After the session, the QHP reviews technician-recorded graphed data to assess the patient’s progress and determine
if the treatment protocol needs to be adjusted. The QHP writes a progress note with a plan of action.
Q: Can I report 97154 and 97158 concurrently?
A: No. 97158 is intended to be reported for QHP-led group sessions only.
Q: Can I report 97154 and 97155 concurrently?
A: Yes, as long as the criteria in the descriptors for both codes are met. A single QHP may not report 97154 and
97155 concurrently.
Q: What constitutes a “group”?
A: A group includes at least 2 patients but no more than 8.
Q: Do I report 97154 for each patient in the group session?
A: Yes. Report this code for each patient attending the group session.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 6 -
97155
Adaptive behavior treatment with protocol modification administered by physician or other
qualified health care professional, which may include simultaneous direction of technician,
face-to-face with one patient, each 15 minutes
TYPICAL PATIENT: A 5-year-old male previously showed steady improvements in language and social skills
at home as a result of one-to-one intensive applied behavior analysis intervention, but skill development seems to
have reached a plateau recently.
CLINICAL EXAMPLE:
Prior to the treatment session, the QHP reviews data and notes from previous sessions. To promote generalization
of treatment gains across situations, the QHP modies the written protocols used previously to incorporate
procedures designed to build the individual’s language and social skills into daily home routines (e.g., play,
dressing, mealtimes). Just before the session, the QHP gathers all materials required for that session.
During the session (face-to-face), the QHP demonstrates the modied treatment procedures with the patient while
the technician observes. The technician then implements the modied treatment protocol with the individual
while the QHP observes and provides feedback. The QHP records data on the technician’s performance.
After the session, the QHP modies the protocols if indicated by the QHP’s observations during the session. The
QHP writes a progress note with a plan of action.
Q: When do I report 97155?
A: In two cases: (1) When a QHP conducts 1:1 direct treatment with the patient to observe changes in behavior or
troubleshoot treatment protocols; or (2) when the QHP joins the patient and the technician during a treatment session
to direct the technician in implementing a new or modied treatment protocol. In the second case, 97153 should be
reported concurrently (see Concurrent Billing Overview in the Other Frequently Asked Questions section).
Q: What is an adaptive-behavior service protocol?
A: An adaptive behavior service protocol encompasses (a) a written description of procedures for implementing
a specied service to address a patient’s assessment or treatment goal(s) and (b) implementation of the
procedures with the patient.
Q: What is adaptive-behavior service protocol modication?
A: Adaptive behavior service protocol modication involves changes made by a qualied health care provider
(QHP) to the procedures for implementing an adaptive behavior service. Protocol modication includes but
is not limited to (a) adjustments to specic components of a protocol (e.g., treatment targets, treatment goals,
observation and measurement, reinforcers, reinforcer delivery, prompts, instructions, materials, discriminative
stimuli, contextual variables); (b) observations to determine if the protocol components are functioning
effectively for the patient or require adjustments; (c) active direction of a technician while the technician
delivers a service to a patient to ensure that the procedures are being implemented correctly, to correct errors
in implementation, or to train the technician to implement a modied protocol; and (d) QHP implementation
of the protocol with the patient to determine if changes are needed to improve patient progress or to test a
modied protocol. Any protocol-modication services that are delivered during face-to-face sessions with
patients or caregivers are billable. Modifying written protocols is an indirect service that is not reported
separately, but is bundled with 97155 for payment.
SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 7 -
97156
Family adaptive behavior treatment guidance, administered by physician or other qualified
health care professional (with or without the patient present), face-to-face with guardian(s)/
caregiver(s), each 15 minutes
TYPICAL PATIENT: Parents of a 6-year-old male seek training on procedures for helping the child
communicate using picture cards (skills he previously developed in ABA therapy sessions with technicians)
during typical family routines.
CLINICAL EXAMPLE:
Prior to the appointment, the QHP reviews data, notes, and treatment protocols regarding the individual’s picture
communication skills. Just before the session, the QHP gathers all materials required for that session.
During the session (face-to-face), the QHP reviews the treatment protocol with the parents, which involves the use
of prompting and reinforcement to promote the individual’s use of picture cards and gestures to indicate his
desire to stop an activity and to request help. The QHP demonstrates those procedures with the individual
while the parents observe, then has each parent in turn implement the procedures with the individual while
the QHP observes, provides feedback, and records data on the individual’s performance. The QHP gives
the parents a copy of the treatment protocol and data sheets with instructions for implementing the protocol
during typical family routines.
After the session, the QHP graphs and reviews data recorded during the session and writes a progress note and
plan of action.
Q: Can I report 97156 for services delivered to parents while the patient is receiving direct treatment
elsewhere (e.g., when the patient is in a treatment session with a technician and the parents are meeting
with the QHP in another room for a family training)?
A: Yes. Those are separate and distinct services delivered to different family members by different providers.
Q: Who constitutes a “caregiver”?
A: This is determined by payer policy. Immediate family members are almost always covered, but some payers
may have a broader denition and include others such as babysitters, teachers, day care providers, etc.
97157
Multiple-family group adaptive behavior treatment guidance, administered by physician or
other qualified health care professional (without the patient present), face-to-face with multiple
sets of guardians/caregivers, each 15 minutes
TYPICAL PATIENT: The parents of a 3-year-old male who has pervasive hyperactivity and no functional play,
social, or communication skills seek training on how to manage his hyperactive and disruptive behavior and help
him develop appropriate play, social, and communication skills.
CLINICAL EXAMPLE:
Prior: The QHP invites the parents to attend a training session with several other sets of parents. Prior to the session
the QHP reviews data, notes, and treatment protocols regarding the individual’s hyperactive and disruptive
behavior as well as his play, social, and communication skills.
During the session (face-to-face), the QHP asks each set of parents to identify one skill to be increased or one
problem behavior to be decreased in their own child. The QHP describes how behavior-analytic principles
and procedures could be applied to the behavior identied by the parents of this 3-year-old patient. S/he

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 8 -
demonstrates a procedure (e.g., prompting the child to speak instead of whining when he wants something,
and not giving him preferred items when he whines). The parents then role-play implementing that
procedure. Other group participants and the QHP provide feedback and make constructive suggestions. That
process is repeated for skills/behaviors identied by other sets of parents. The QHP ends the group session by
summarizing the main points, answering questions, and giving each set of parents a homework assignment to
practice the skills they worked on during the session.
After the session the QHP writes a progress note and plan of action.
Q: Do I report 97157 for every attendee in the group session?
A: No. Report this code for each set of caregivers for a given patient who attend the group session. For example,
if ve sets of parents attend the group session, report the code once for each set.
97158
Group adaptive behavior treatment with protocol modification, administered by physician or
other qualified health care professional face-to-face with multiple patients, each 15 minutes
TYPICAL PATIENT: A 13-year-old female is reported to be isolated from peers due to poor social skills and
odd behavior. She has difculty recognizing emotions in others and often annoys her peers because she tells the
same joke over and over and talks incessantly about comic-book heroes.
CLINICAL EXAMPLE:
Prior: The QHP includes participation in group treatment sessions that focus on peer social skills in the
patient’s treatment plan. Prior to the treatment session, the QHP reviews data, notes, and treatment
protocols regarding the patient’s social and communication skills and modies the treatment protocol to
be implemented in group treatment sessions. Just before the session, the technician and QHP gather all
materials required for that session.
During the session (face-to-face), the QHP begins the group session by asking each patient to briey describe
two of their recent social encounters with peers, one that went well and one that did not. The QHP uses
that information to develop a group activity in which the patient has the opportunity to practice the skills
she used in the encounters that went well and to problem solve the interactions that did not go well.
The QHP helps the patient identify social cues that were interpreted correctly and incorrectly and what
she could have done differently, and provides prompts and feedback. The QHP also records data on the
patient’s performance. The QHP ends the session by summarizing the discussion and skills that were
practiced, answering questions, and giving the patient an assignment to practice a particular peer social
skill and record her own performance of that skill.
After the session, the QHP graphs and reviews data recorded during the session and writes a progress note and
plan of action.
Q: Can I report 97154 and 97158 concurrently?
A: No. 97158 is intended to be reported for QHP-led group sessions only.
Q: What constitutes a “group”?
A: A group includes at least 2 patients but no more than 8.
Q: Do I report 97158 for each patient in the group session?
A: Yes. Report this code for each patient attending the group session.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 9 -
Q: What is an adaptive-behavior service protocol?
A: An adaptive behavior service protocol encompasses (a) a written description of procedures for implementing a
specied service to address a patient’s assessment or treatment goal(s) and (b) implementation of the procedures
with the patient.
Q: What is adaptive-behavior service protocol modication?
A: Adaptive behavior service protocol modication involves changes made by a qualied health care provider
(QHP) to the procedures for implementing an adaptive behavior service. Protocol modication includes but
is not limited to (a) adjustments to specic components of a protocol (e.g., treatment targets, treatment goals,
observation and measurement, reinforcers, reinforcer delivery, prompts, instructions, materials, discriminative
stimuli, contextual variables); (b) observations to determine if the protocol components are functioning effec-
tively for the patient or require adjustments; (c) active direction of a technician while the technician delivers
a service to a patient to ensure that the procedures are being implemented correctly, to correct errors in im-
plementation, or to train the technician to implement a modied protocol; and (d) QHP implementation of the
protocol with the patient to determine if changes are needed to improve patient progress or to test a modied
protocol. Any protocol-modication services that are delivered during face-to-face sessions with patients or
caregivers are billable. Modifying written protocols is an indirect service that is not reported separately, but is
bundled with 97158 for payment.
0373T
Adaptive behavior treatment with protocol modification, each 15 minutes of technicians’ time
face-to-face with a patient, requiring the following components:
• administered by the physician or other qualified health care professional who is on site,
• with the assistance of two or more technicians,
• for a patient who exhibits destructive behavior,
• completed in an environment that is customized to the patient’s behavior.
TYPICAL PATIENT: A 16-year-old male has had two surgeries to relieve esophageal blockages due to pica
involving repeated ingestion of small metal objects (e.g., paper clips, push pins). The patient’s pica has not
responded to previous treatment.
CLINICAL EXAMPLE:
Prior: The QHP has modied previously developed written protocols for reducing the patient’s pica based on a
recent medical evaluation and a functional analysis of pica. Just before the session, the QHP gathers all
materials required for that session. One technician carefully inspects the treatment room before the session
to make sure there are no potential pica items on the oor.
During the session (face-to-face), the QHP demonstrates the modied treatment procedures with the patient
while the technicians observe. The modied procedures involve one technician presenting the patient with
one small preferred food item and one item that resembles a pica item but is not dangerous if ingested on
each of a series of trials. On each trial the two items are placed on a table in front of the patient. The second
technician is positioned directly behind the patient to provide the patient with a gentle physical prompt to pick
up and eat the food item. If the patient tries to pick up the pica item, the second technician gently blocks that
response and removes the pica item from the patient’s line of sight. The third technician records the patient’s
appropriate and maladaptive responses on each trial (e.g., consuming the food item and/or attempting to pick
up the pica item). The technicians then implement the modied treatment protocol with the patient while the
QHP observes and provides feedback. The QHP records data on the technicians’ performances.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 10 -
After the session, the QHP reviews technician-recorded graphed data to assess the patient’s progress and
determine if the treatment protocol needs to be adjusted further. The QHP writes a progress note with
a plan of action.
Q: For 0373T, do I report each technician’s time separately?
A: No. Report only the total time of one technician. Example: if three technicians are needed for a 3-hour
session, report 12 units of 0373T (15 minutes x 12 units = 180 minutes, or 3 hours).
Q: For 0373T, what is meant by “on site”?
A: On site is dened as the QHP being “immediately available and interruptible.” This means that the QHP is at
the same site and can join the session if needed.
Q: Can 0373T be billed concurrently with 97155 if the QHP directs the technician during the session?
A: No. That and other indirect services must be bundled with this code.
Q: What is meant by a “customized environment”?
A: For codes 0362T and 0373T, the term “customized” means that the environment is congured to safely
conduct a functional analysis of destructive behavior (0362T) or treatment for that behavior (0373T). For
some patients, this can be accomplished in the home. For example, in the case of a patient who displays
aggression using objects, those objects that the patient might use as dangerous weapons (e.g., a wooden
baseball bat) would be removed and replaced with soft items (e.g., a foam baseball bat). Other patients may
require treatment in a padded treatment room. For example, a patient with severe head banging may require
functional analysis and initial treatment in a padded treatment room because the behavior causes tissue
damage and places the patient at risk for detached retinas.
Q: What is an adaptive-behavior service protocol?
A: An adaptive behavior service protocol encompasses (a) a written description of procedures for implementing
a specied service to address a patient’s assessment or treatment goal(s) and (b) implementation of the
procedures with the patient.
Q: What is adaptive-behavior service protocol modication?
A: Adaptive behavior service protocol modication involves changes made by a qualied health care provider
(QHP) to the procedures for implementing an adaptive behavior service. Protocol modication includes but
is not limited to (a) adjustments to specic components of a protocol (e.g., treatment targets, treatment goals,
observation and measurement, reinforcers, reinforcer delivery, prompts, instructions, materials, discriminative
stimuli, contextual variables); (b) observations to determine if the protocol components are functioning
effectively for the patient or require adjustments; (c) active direction of a technician while the technician
delivers a service to a patient to ensure that the procedures are being implemented correctly, to correct errors
in implementation, or to train the technician to implement a modied protocol; and (d) QHP implementation
of the protocol with the patient to determine if changes are needed to improve patient progress or to test a
modied protocol. Any protocol-modication services that are delivered during face-to-face sessions with
patients or caregivers are billable. Modifying written protocols is an indirect service that is not reported
separately, but is bundled with 0373T for payment.
SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 11 -
OTHER FREQUENTLY ASKED QUESTIONS
Q: Do all payers have to adopt the 2019 CPT codes?
A: Yes. Under HIPAA, if a payer accepts electronic claims submissions, they must utilize Category I CPT codes.
Q: Are all payers required to implement the new CPT codes as of January 1, 2019 or by some
other deadline?
A: No. Payers have their own procedures and timelines for implementing new codes, so providers must obtain
that information from each payer with whom they work.
Q: Are there established values (relative value units) for the new CPT codes in 2019?
A: No. The new codes will be carrier priced for 2019. That means that payers will establish reimbursement rates
for each code with providers via the contract negotiation process.
Q: Please clarify and summarize the conditions under which 97155 can be billed concurrently with codes
for direct treatment of the patient.
A: See the table below.
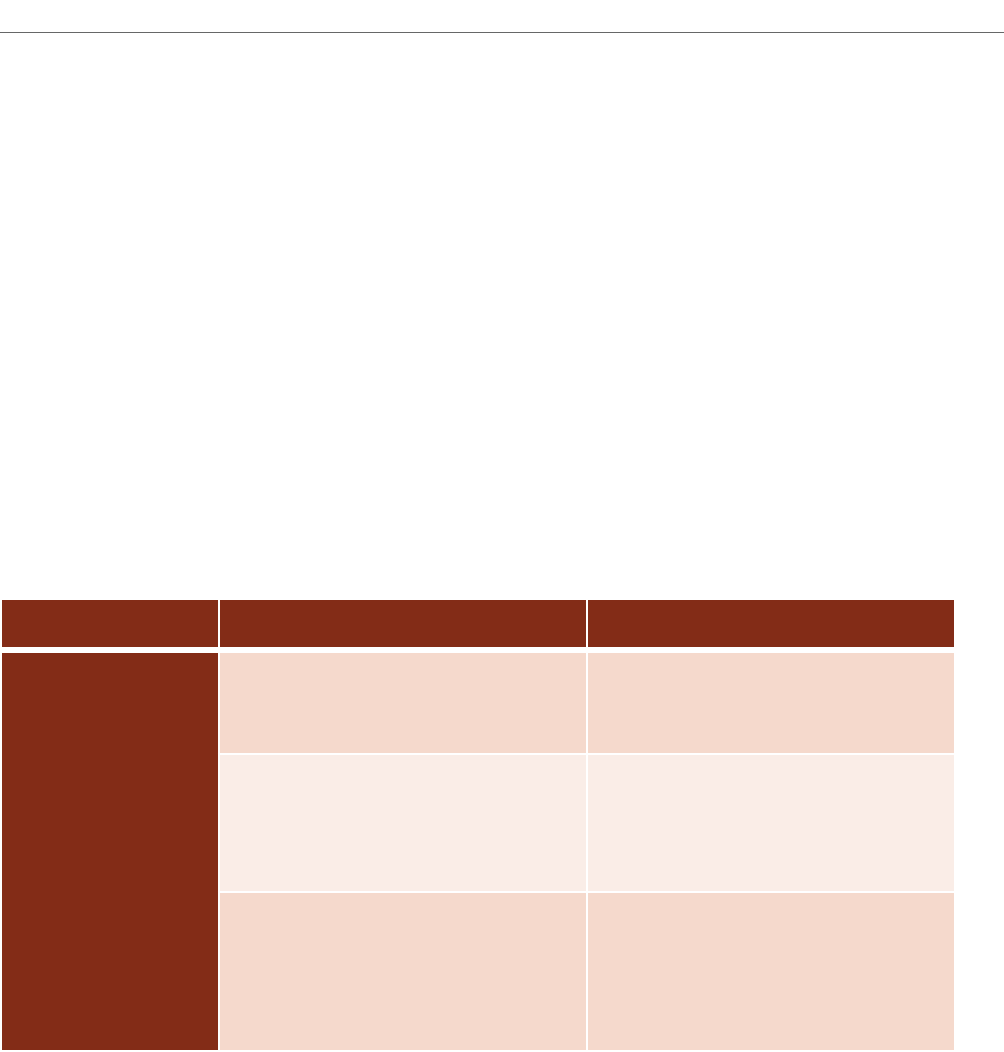
Concurrent Billing Overview
Direct Treatment Codes Direction of Technician Code
Code pairs for
Direction of
Technician
97153 individual treatment –
by technician or QHP
97155 –
by QHP (not the same as
QHP delivering 97153)
97154 group treatment –
by technician or QHP
97155 –
by QHP (not the same as
QHP delivering 97154)
0373T individual treatment –
by two or more technicians or two
or more QHPs
NO ADDITIONAL CODE FOR
DIRECTION OF TECHNICIAN;
BUNDLED INTO 0373T BASED
ON “ON SITE” REQUIREMENTS
Q: How is time for the QHP’s day-to-day review of data and treatment planning captured?
A: There is no separate code for those indirect services in the new CPT code set (nor was there in the Category III
CPT code set). Some payers may supplement the adaptive behavior services code set with a HCPCS or other
CPT code (e.g., H0032, G9012, H2019) to report indirect activities. In the event payers do not, the activities
that occur prior to and after the face-to-face time should be bundled so that reimbursement for those codes
captures both face-to-face and non-face-to-face time.
Q: Can I report 97155 for treatment planning conducted by the QHP while the technician implements
treatment with the patient?
A: No. Code 97155 should be reported only for services where the QHP is either engaged directly with the
patient or is directing a technician in implementing a modied protocol with the patient.

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 12 -
Q: Can I bill for supervision of technicians without the patient present?
A: No. That is an indirect service for which CPT does not allow stand-alone codes. Some payers may allow the
use of HCPCS or other CPT codes to report that work.
Q: Do payers allow use of the codes to report telehealth delivery of ABA assessment or treatment services?
A: This varies based on state law and payer policy. Review your contracts and provider manuals for guidance on
whether telehealth is approved by your individual payers.
Q: My payers currently pay for treatment planning under a HCPCS code. Am I now limited to only the
2019 CPT codes?
A: No. Payers may supplement the 2019 CPT codes with HCPCS or other CPT codes for indirect services or other
activities, which would be specied in your modied 2019 contracts.
Q: Why do I need resources on the 2019 CPT code set other than code descriptors I’ve seen on some slides or
the code conversion table that was distributed by the Steering Committee?
A: The 2019 CPT
®
Code Book and the CPT® Assistant article both contain information that is essential for a full
understanding of the code set and how it should be reported. Those materials are copyrighted by the AMA, so
we cannot distribute them without express permission from the AMA.
Q: What is “direction” as that term is used in code 97155 and how does it differ from “supervision”?
A: “Direction” in the context of code 97155 refers to the QHP directly monitoring the delivery of treatment to a
patient by a behavior technician. The focus is on ensuring that treatment protocols are implemented correctly
in order to maximize benet to that patient. Direction of a technician includes, but is not limited to, the QHP
frequently observing the technician implementing the patient’s protocols with the patient, providing instructions
and conrming or corrective feedback as needed, and/or demonstrating correct implementation of a new
or modied treatment protocol with the patient while the technician observes, followed by the technician
implementing the protocol with the patient while the QHP observes and provides feedback. That service should
be reported and billed using code 97155 (adaptive behavior treatment with protocol modication administered
by physician or other qualied health care professional). The technician’s time is separately reportable under
97153 (adaptive behavior treatment by protocol administered by technician under the direction of a physician or
other qualied health care professional). Time reported and billed must be face-to-face time with the patient.
“Supervision” of a technician or other employee by a QHP generally refers to processes through which the
QHP ensures that the supervisee (a) practices in a competent, professional, and ethical manner in accordance
with the standards of the profession; (b) engages with and follows the employer’s policies and procedures; (c)
continues to develop their knowledge and skills; and (d) receives the personal support needed to cope with
the stressors and demands of their position. “Supervision” may also involve activities to enable the supervisor
and supervisee to comply with specic requirements for obtaining or maintaining a paraprofessional or
professional credential, such as a certication or license, or to fulll ethical responsibilities. Supervision
activities that do not involve delivery of services directly to patients are generally not reportable or billable to
health plans using CPT codes, though some payers may allow them to be billed using HCPCS or other codes.
Those that do involve direct delivery of services to maximize benets to individual patients may be reportable
and billable to a health plan and fulll some supervision requirements for certication or licensure purposes,
but only the former should be reported to the health plan.
Note: The Applied Behavior Analysis Treatment of Autism Spectrum Disorder: Practice Guidelines for
Healthcare Funders and Managers (2nd ed.) use the terms “case supervision” and “clinical direction”
to refer to the work conducted by the QHP to develop, deliver, and oversee implementation of a patient’s
treatment plan. Those terms encompass both direct contact with the patient or caregivers and indirect services.
Direct adaptive behavior services by the QHP include delivering assessment or treatment face-to-face with

SUPPLEMENTAL GUIDANCE ON INTERPRETING AND APPLYING THE 2019 CPT CODES FOR ADAPTIVE BEHAVIOR SERVICES
- 13 -
the patient (reported with codes 97151, 97153 with modier, 97155, 0362T, 0373T, 97158) or caregiver(s)
(reported with codes 97156, 97157). Only code 97151 allows non-face-to-face activities (reviewing records,
scoring assessments, and preparing a treatment plan or progress report) to also be reported and billed. Indirect
services by the QHP include activities involved in ongoing monitoring of patient progress and revising
protocols, preparing for assessment or treatment sessions by the QHP and/or technicians, reviewing data, and
writing progress notes – that is, activities like those described in the “prior” and “after” sections of the clinical
examples in this document. As indicated in the introduction, there is no stand-alone CPT code for those
indirect services, so they must be bundled with direct services for payment unless the payer allows them to be
reported and billed with a HCPCS or other code.
