Gender Dysphoria Treatment
Page 1 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
UnitedHealthcare
®
Community Plan
Medical
Policy
Gender Dysphoria Treatment
Policy Number: CS145.O
Effective Date: May 1, 2024
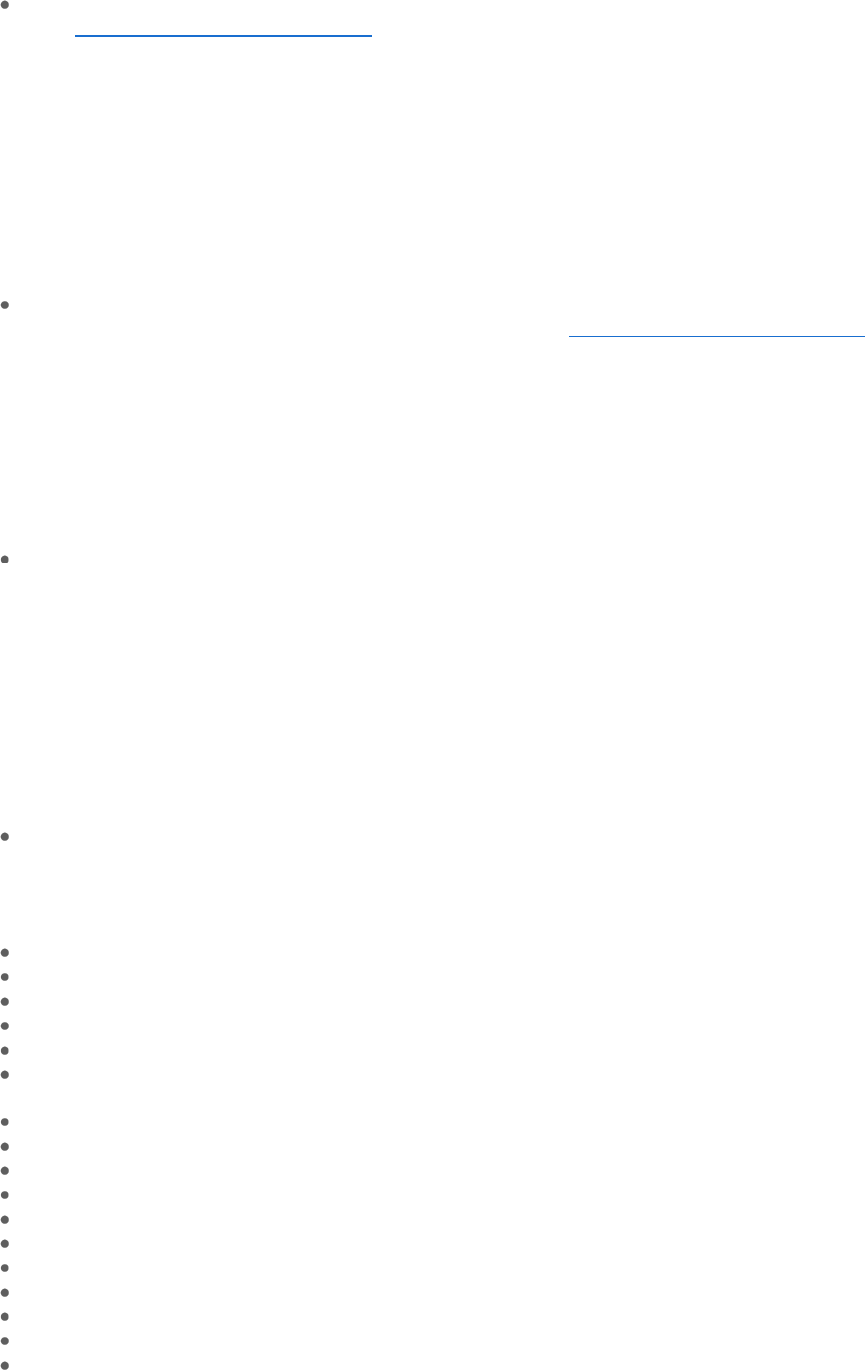
Instructions for Use
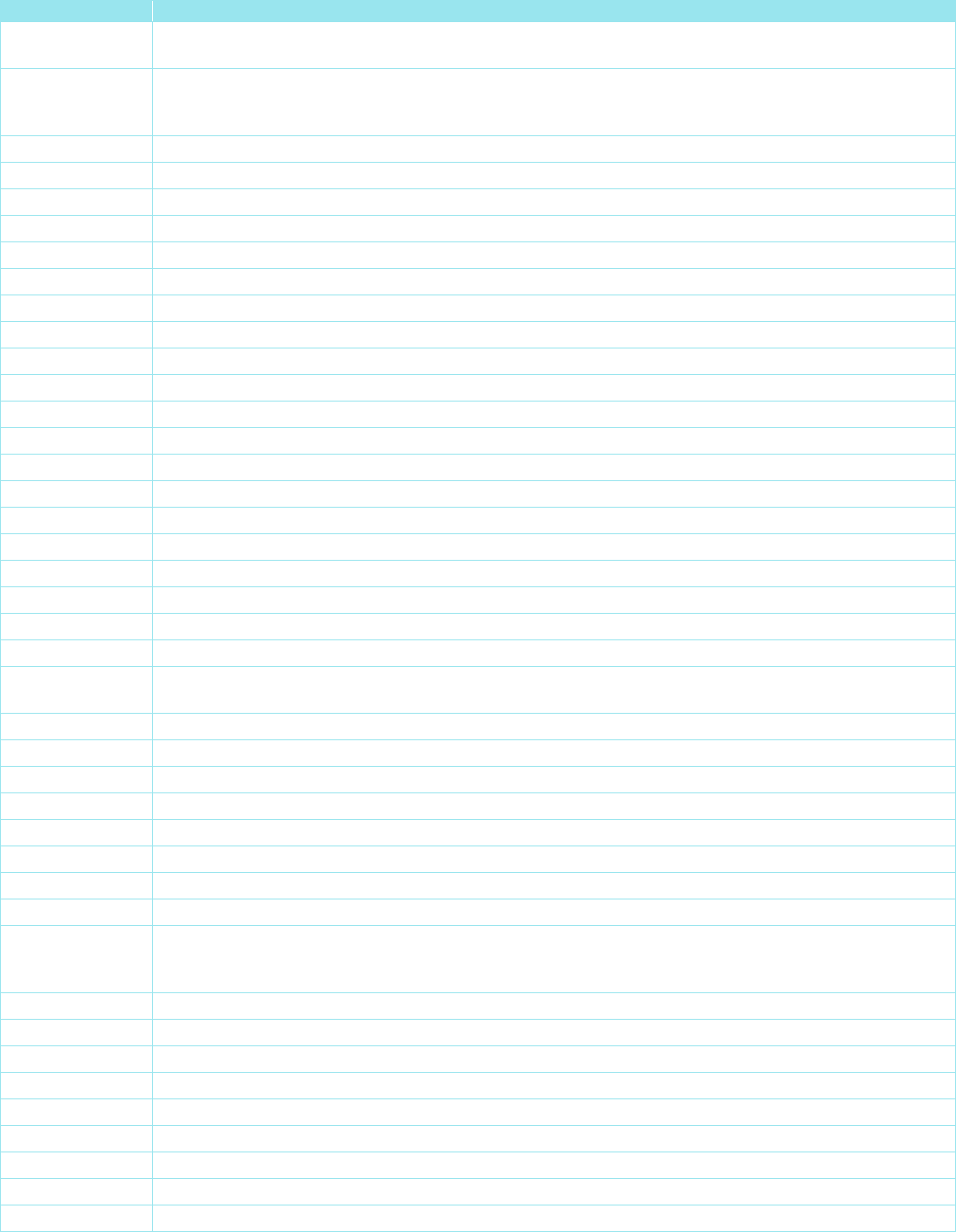
Table of Contents Page
Application ............................................................................. 1
Coverage Rationale .............................................................. 1
Definitions .............................................................................. 3
Applicable Codes .................................................................. 4
Description of Services ......................................................... 8
Benefit Considerations .......................................................... 8
Clinical Evidence ................................................................... 9
U.S. Food and Drug Administration .................................... 15
References .......................................................................... 15
Policy History/Revision Information .................................... 17
Instructions for Use ............................................................. 18
Application
This Medical Policy does not apply to the states listed below; refer to the state-specific policy/guideline, if noted:
State
Policy/Guideline
Indiana
Gender Dysphoria Treatment (for Indiana Only)
Kentucky
None
Louisiana
Gender Dysphoria Treatment (for Louisiana Only)
Nebraska
None
New Jersey
Gender Dysphoria Treatment (for New Jersey Only)
New Mexico
Gender Dysphoria Treatment (for New Mexico Only)
North Carolina
None
Ohio
Gender Dysphoria Treatment (for Ohio Only)
Pennsylvania
Gender Dysphoria Treatment (for Pennsylvania Only)
Tennessee
None
Virginia
Virginia Medicaid Department of Medical Assistance Services: Bulletin > Coverage of Gender
Dysphoria Services
Coverage Rationale
See Benefit Considerations
Note: This Medical Policy does not apply to individuals with ambiguous genitalia or disorders of sexual development.
Surgical treatment for Gender Dysphoria may be indicated for individuals who provide the following
documentation:
Related Community Plan Policies
• Botulinum Toxins A and B
• Breast Reconstruction
• Breast Reduction Surgery
• Brow Ptosis and Eyelid Repair
• Cosmetic and Reconstructive Procedures
• Gonadotropin Releasing Hormone Analogs
• Habilitation and Rehabilitation Therapy
(Occupational, Physical, and Speech)
• Panniculectomy and Body Contouring Procedures
•
Rhinoplasty and Other Nasal Procedures
Commercial Policy
• Gender Dysphoria Treatment
Gender Dysphoria Treatment
Page 2 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
For breast surgery (mastectomy, breast reduction, or breast augmentation), a written clinical assessment from at least
one
Qualified Healthcare Professional experienced in treating Gender Dysphoria* is required. The assessment must
document that an individual meets all of the following criteria:
o Persistent, well-documented Gender Dysphoria; and
o Capacity to make a fully informed decision and to consent for treatment; and
o Must be at least 18 years of age for breast augmentation; and
o For mastectomy or breast reduction, individuals must be at least 18 years of age; however, individuals within one
calendar year of turning 18 can be considered on a case-by-case basis; and
o Favorable psychosocial-behavioral evaluation to provide screening and identification of risk factors or potential
postoperative challenges; and
o For breast augmentation, continued Gender Dysphoria following the completion of 12 months of continuous
hormone therapy prior to the breast procedure is required
For thyroid cartilage reduction and/or voice modification surgery (e.g., laryngoplasty, glottoplasty or shortening of the
vocal cords), a written clinical assessment from at least one
Qualified Healthcare Professional experienced in treating
Gender Dysphoria is required. The assessment must document that an individual meets all of the following criteria:
o Persistent, well-documented Gender Dysphoria; and
o Capacity to make a fully informed decision and to consent for treatment; and
o Must be at least 18 years of age; and
o Favorable psychosocial-behavioral evaluation to provide screening and identification of risk factors or potential
postoperative challenges; and
o Completion of 6 months of continuous hormone therapy prior to surgery is required for voice masculinization; and
o For voice modification surgery, documentation of presurgical voice lessons and/or therapy
For genital surgery, a written clinical assessment from at least two Qualified Healthcare Professionals experienced in
treating Gender Dysphoria, who have independently assessed the individual, is required. The assessment must
document that an individual meets all of the following criteria:
o Persistent, well-documented Gender Dysphoria; and
o Capacity to make a fully informed decision and to consent for treatment; and
o Must be at least 18 years of age; and
o Favorable psychosocial-behavioral evaluation to provide screening and identification of risk factors or potential
postoperative challenges; and
o Complete at least 12 months of successful continuous full-time real-life involvement in the identified gender; and
o Complete 12 months of continuous hormone therapy appropriate for the experienced gender (unless medically
contraindicated or not indicated for gender)
and
Treatment plan that includes ongoing follow-up and care by a Qualified Healthcare Professional experienced in
treating Gender Dysphoria
When the above criteria are met, the following surgical procedures and/or therapies to treat Gender Dysphoria
are medically necessary and covered as a proven benefit:
Bilateral mastectomy or breast reduction
Breast augmentation with breast implants or fat transfer
Clitoroplasty (creation of clitoris)
Hysterectomy (removal of uterus)
Labiaplasty (creation of labia)
Laser or electrolysis hair removal in advance of genital reconstruction prescribed by a physician for the treatment of
Gender Dysphoria
Metoidioplasty (creation of penis, using clitoris)
Orchiectomy (removal of testicles)
Penectomy (removal of penis)
Penile prosthesis
Phalloplasty (creation of penis)
Salpingo-oophorectomy (removal of fallopian tubes and ovaries)
Scrotoplasty (creation of scrotum)
Testicular prostheses
Thyroid cartilage reduction/reduction thyroid chondroplasty/tracheal shave (removal or reduction of the Adam’s apple)
Urethroplasty (reconstruction of female urethra)
Urethroplasty (reconstruction of male urethra)
Gender Dysphoria Treatment
Page 3 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Vaginectomy (removal of vagina)
Vaginoplasty (creation of vagina)
Voice lessons and/or voice therapy (with or without surgery)
Voice modification surgery (e.g., laryngoplasty, glottoplasty or shortening of the vocal cords)
Vulvectomy (removal of vulva)
Gender affirming surgery is considered an irreversible intervention. Although infrequent, reversal of prior gender
affirming surgery may be covered when the medical necessity criteria for the requested treatment above are met.
Certain ancillary procedures, including but not limited to the following, are considered cosmetic and not
medically necessary, when performed as part of surgical treatment for Gender Dysphoria (check the federal, state
or contractual requirements for benefit coverage*):
Refer to the Benefit Considerations section as member specific benefit plan language may vary.
Abdominoplasty (also refer to the Medical Policy titled Panniculectomy and Body Contouring Procedures)
Blepharoplasty (also refer to the Medical Policy titled Brow Ptosis and Eyelid Repair)
Body contouring (e.g., fat transfer, lipoplasty, panniculectomy) (also refer to the Medical Policy titled Panniculectomy
and Body Contouring Procedures)
Brow lift
Calf implants
Cheek, chin and nose implants
Face/forehead lift and/or neck tightening
Facial bone remodeling for facial feminization
Hair transplantation
Injection of fillers or neurotoxins (also refer to the Medical Benefit Drug Policy titled Botulinum Toxins A and B)
Laser or electrolysis hair removal not related to genital reconstruction
Lip augmentation
Lip reduction
Liposuction (suction-assisted lipectomy) (also refer to the Medical Policy titled Panniculectomy and Body Contouring
Procedures)
Mastopexy
Pectoral implants for chest masculinization
Rhinoplasty (also refer to the Medical Policy titled Rhinoplasty and Other Nasal Procedures)
Skin resurfacing (e.g., dermabrasion, chemical peels, laser)
*Note: For New York plans, refer to the Benefit Considerations section for more information.
Definitions
Gender Dysphoria in Adolescents and Adults: A disorder characterized by the following diagnostic criteria [Diagnostic
and Statistical Manual of Mental Disorders, 5
th
edition, Text Revision (DSM-5-TR
™
)]:
A marked incongruence between one’s experienced/expressed gender and assigned gender, of at least 6 months’
duration, as manifested by at least two of the following:
o A marked incongruence between one’s experienced/expressed gender and primary and/or secondary sex
characteristics (or in young adolescents, the anticipated secondary sex characteristics)
o A strong desire to be rid of one’s primary and/or secondary sex characteristics because of a marked
incongruence with one’s experienced/expressed gender (or in young adolescents, a desire to prevent the
development of the anticipated secondary sex characteristics)
o A strong desire for the primary and/or secondary sex characteristics of the other gender
o A strong desire to be of the other gender (or some alternative gender different from one’s assigned gender)
o A strong desire to be treated as the other gender (or some alternative gender different from one’s assigned
gender)
o A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender
different from one’s assigned gender)
The condition is associated with clinically significant distress or impairment in social, occupational, or other important
areas of functioning
Gender Dysphoria Treatment
Page 4 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Gender Dysphoria in Children: A disorder characterized by the following diagnostic criteria [Diagnostic and Statistical
Manual of Mental Disorders, 5
th
edition, Text Revision (DSM-5-TR
™
)]:
A. A marked incongruence between one’s experienced/expressed gender and assigned gender, of at least 6 months’
duration, as manifested by at least six of the following (one of which must be criterion A1):
1. A strong desire to be of the other gender or an insistence that one is the other gender (or some alternative gender
different from one’s assigned gender)
2. In boys (assigned gender), a strong preference for cross-dressing or simulating female attire; or in girls (assigned
gender), a strong preference for wearing only typical masculine clothing and a strong resistance to the wearing of
typical feminine clothing
3. A strong preference for cross-gender roles in make-believe play or fantasy play
4. A strong preference for the toys, games, or activities stereotypically used or engaged in by the other gender
5. A strong preference for playmates of the other gender
6. In boys (assigned gender), a strong rejection of typically masculine toys, games, and activities and a strong
avoidance of rough-and-tumble play; or in girls (assigned gender), a strong rejection of typically feminine toys,
games, and activities
7. A strong dislike of ones’ sexual anatomy
8. A strong desire for the primary and/or secondary sex characteristics that match one’s experienced gender
B. The condition is associated with clinically significant distress or impairment in social, school or other important areas
of functioning
Qualified Healthcare Professional:
Documented credentials from a relevant licensing board
A minimum of a master’s degree or equivalent training in a clinical field relevant to the assessment and treatment of
Gender Dysphoria
Knowledge and experience in treating Gender Dysphoria
(Coleman et al., 2022; Hembree et al., 2017)
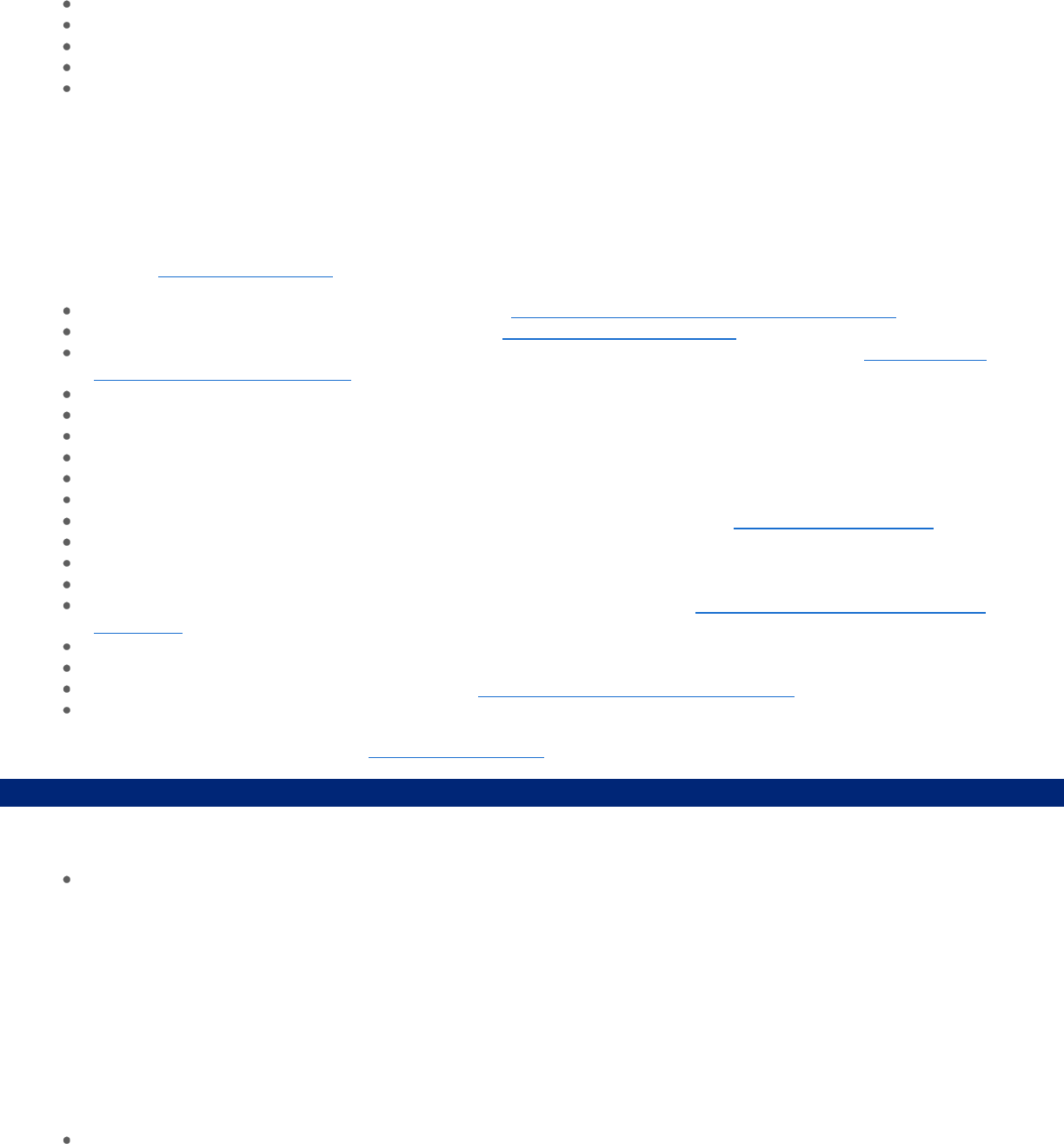
Applicable Codes
The following list(s) of procedure and/or diagnosis codes is provided for reference purposes only and may not be all
inclusive. Listing of a code in this policy does not imply that the service described by the code is a covered or non-covered
health service. Benefit coverage for health services is determined by federal, state, or contractual requirements and
applicable laws that may require coverage for a specific service. The inclusion of a code does not imply any right to
reimbursement or guarantee claim payment. Other Policies and Guidelines may apply.
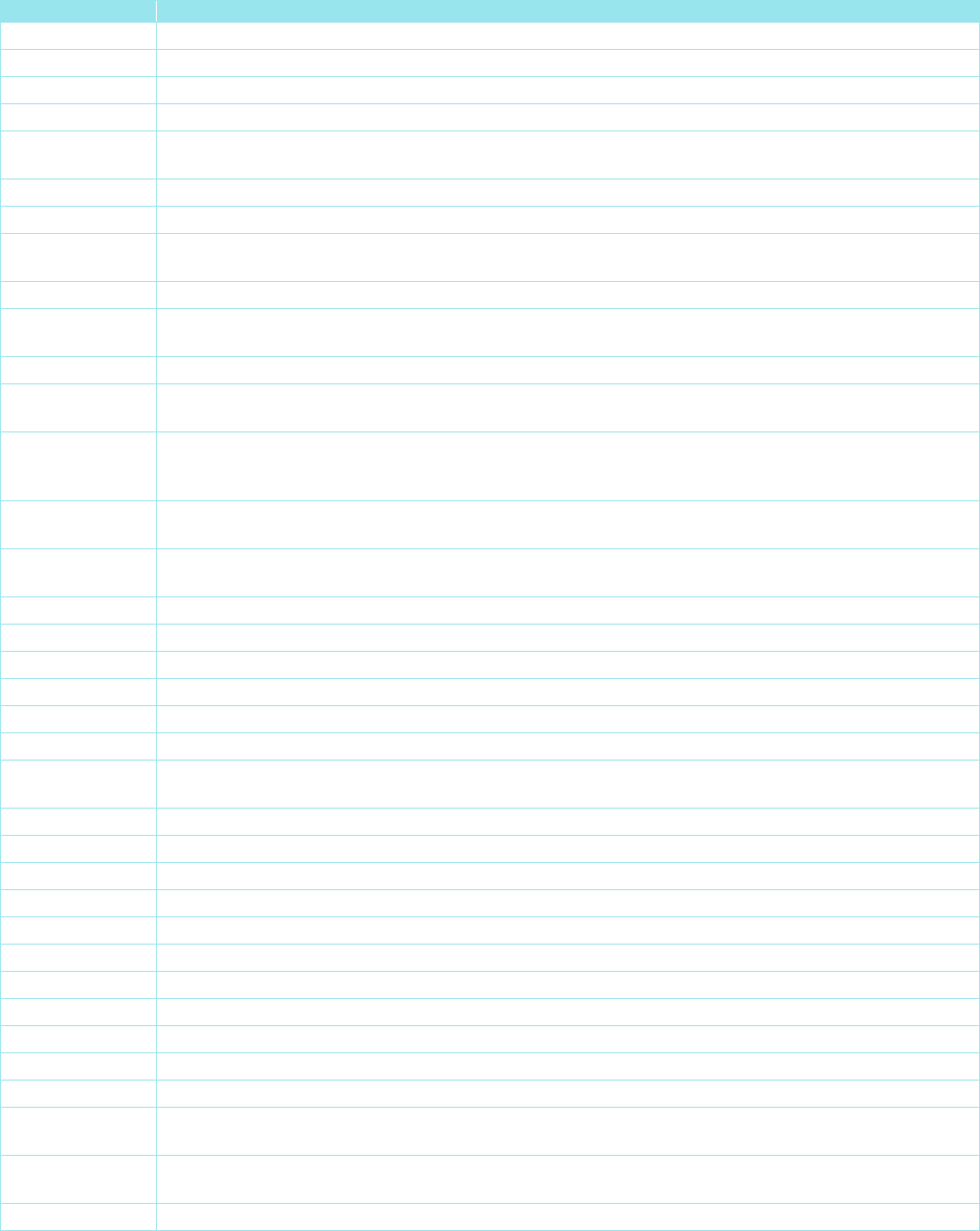
CPT Code
Description
11950
Subcutaneous injection of filling material (e.g., collagen); 1 cc or less
11951
Subcutaneous injection of filling material (e.g., collagen); 1.1 to 5.0 cc
11952
Subcutaneous injection of filling material (e.g., collagen); 5.1 to 10.0 cc
11954
Subcutaneous injection of filling material (e.g., collagen); over 10.0 cc
14000
Adjacent tissue transfer or rearrangement, trunk; defect 10 sq cm or less
14001
Adjacent tissue transfer or rearrangement, trunk; defect 10.1 sq cm to 30.0 sq cm
14041
Adjacent tissue transfer or rearrangement, forehead, cheeks, chin, mouth, neck, axillae, genitalia,
hands and/or feet; defect 10.1 sq cm to 30.0 sq cm
15734
Muscle, myocutaneous, or fasciocutaneous flap; trunk
15738
Muscle, myocutaneous, or fasciocutaneous flap; lower extremity
15750
Flap; neurovascular pedicle
15757
Free skin flap with microvascular anastomosis
15758
Free fascial flap with microvascular anastomosis
15769
Grafting of autologous soft tissue, other, harvested by direct excision (e.g., fat, dermis, fascia)
15771
Grafting of autologous fat harvested by liposuction technique to trunk, breasts, scalp, arms, and/or
legs; 50 cc or less injectate
15772
Grafting of autologous fat harvested by liposuction technique to trunk, breasts, scalp, arms, and/or
legs; each additional 50 cc injectate, or part thereof (List separately in addition to code for primary
procedure)
Gender Dysphoria Treatment
Page 5 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
CPT Code
Description
15773
Grafting of autologous fat harvested by liposuction technique to face, eyelids, mouth, neck, ears,
orbits, genitalia, hands, and/or feet; 25 cc or less injectate
15774 Grafting of autologous fat harvested by liposuction technique to face, eyelids, mouth, neck, ears,
orbits, genitalia, hands, and/or feet; each additional 25 cc injectate, or part thereof (List separately in
addition to code for primary procedure)
15775
Punch graft for hair transplant; 1 to 15 punch grafts
15776
Punch graft for hair transplant; more than 15 punch grafts
15780
Dermabrasion; total face (e.g., for acne scarring, fine wrinkling, rhytids, general keratosis)
15781
Dermabrasion; segmental, face
15782
Dermabrasion; regional, other than face
15783
Dermabrasion; superficial, any site (e.g., tattoo removal)
15788
Chemical peel, facial; epidermal
15789
Chemical peel, facial; dermal
15792
Chemical peel, nonfacial; epidermal
15793
Chemical peel, nonfacial; dermal
15819
Cervicoplasty
15820
Blepharoplasty, lower eyelid
15821
Blepharoplasty, lower eyelid; with extensive herniated fat pad
15822
Blepharoplasty, upper eyelid
15823
Blepharoplasty, upper eyelid; with excessive skin weighting down lid
15824
Rhytidectomy; forehead
15825
Rhytidectomy; neck with platysmal tightening (platysmal flap, P-flap)
15826
Rhytidectomy; glabellar frown lines
15828
Rhytidectomy; cheek, chin, and neck
15829
Rhytidectomy; superficial musculoaponeurotic system (SMAS) flap
15830 Excision, excessive skin and subcutaneous tissue (includes lipectomy); abdomen, infraumbilical
panniculectomy
15832
Excision, excessive skin and subcutaneous tissue (includes lipectomy); thigh
15833
Excision, excessive skin and subcutaneous tissue (includes lipectomy); leg
15834
Excision, excessive skin and subcutaneous tissue (includes lipectomy); hip
15835
Excision, excessive skin and subcutaneous tissue (includes lipectomy); buttock
15836
Excision, excessive skin and subcutaneous tissue (includes lipectomy); arm
15837
Excision, excessive skin and subcutaneous tissue (includes lipectomy); forearm or hand
15838
Excision, excessive skin and subcutaneous tissue (includes lipectomy); submental fat pad
15839
Excision, excessive skin and subcutaneous tissue (includes lipectomy); other area
15847
Excision, excessive skin and subcutaneous tissue (includes lipectomy), abdomen (e.g.,
abdominoplasty) (includes umbilical transposition and fascial plication) (List separately in addition to
code for primary procedure)
15876
Suction assisted lipectomy; head and neck
15877
Suction assisted lipectomy; trunk
15878
Suction assisted lipectomy; upper extremity
15879
Suction assisted lipectomy; lower extremity
17380
Electrolysis epilation, each 30 minutes
17999
Unlisted procedure, skin, mucous membrane and subcutaneous tissue
19303
Mastectomy, simple, complete
19316
Mastopexy
19318
Breast reduction
Gender Dysphoria Treatment
Page 6 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
CPT Code
Description
19325
Breast augmentation with implant
19350
Nipple/areola reconstruction
21120
Genioplasty; augmentation (autograft, allograft, prosthetic material)
21121
Genioplasty; sliding osteotomy, single piece
21122
Genioplasty; sliding osteotomies, 2 or more osteotomies (e.g., wedge excision or bone wedge
reversal for asymmetrical chin)
21123
Genioplasty; sliding, augmentation with interpositional bone grafts (includes obtaining autografts)
21125
Augmentation, mandibular body or angle; prosthetic material
21127 Augmentation, mandibular body or angle; with bone graft, onlay or interpositional (includes
obtaining autograft)
21137
Reduction forehead; contouring only
21138
Reduction forehead; contouring and application of prosthetic material or bone graft (includes
obtaining autograft)
21139
Reduction forehead; contouring and setback of anterior frontal sinus wall
21172 Reconstruction superior-lateral orbital rim and lower forehead, advancement or alteration, with or
without grafts (includes obtaining autografts)
21175
Reconstruction, bifrontal, superior-lateral orbital rims and lower forehead, advancement or alteration
(e.g., plagiocephaly, trigonocephaly, brachycephaly), with or without grafts (includes obtaining
autografts)
21179
Reconstruction, entire or majority of forehead and/or supraorbital rims; with grafts (allograft or
prosthetic material)
21180
Reconstruction, entire or majority of forehead and/or supraorbital rims; with autograft (includes
obtaining grafts)
21208
Osteoplasty, facial bones; augmentation (autograft, allograft, or prosthetic implant)
21209
Osteoplasty, facial bones; reduction
21210
Graft, bone; nasal, maxillary or malar areas (includes obtaining graft)
21270
Malar augmentation, prosthetic material
21899
Unlisted procedure, neck or thorax
30400
Rhinoplasty, primary; lateral and alar cartilages and/or elevation of nasal tip
30410
Rhinoplasty, primary; complete, external parts including bony pyramid, lateral and alar cartilages,
and/or elevation of nasal tip
30420
Rhinoplasty, primary; including major septal repair
30430
Rhinoplasty, secondary; minor revision (small amount of nasal tip work)
30435
Rhinoplasty, secondary; intermediate revision (bony work with osteotomies)
30450
Rhinoplasty, secondary; major revision (nasal tip work and osteotomies)
31599
Unlisted procedure, larynx
31899
Unlisted procedure, trachea, bronchi
53410
Urethroplasty, 1-stage reconstruction of male anterior urethra
53430
Urethroplasty, reconstruction of female urethra
54125
Amputation of penis; complete
54400
Insertion of penile prosthesis; non-inflatable (semi-rigid)
54401
Insertion of penile prosthesis; inflatable (self-contained)
54405
Insertion of multi-component, inflatable penile prosthesis, including placement of pump, cylinders,
and reservoir
54406
Removal of all components of a multi-component, inflatable penile prosthesis without replacement
of prosthesis
54408
Repair of component(s) of a multi-component, inflatable penile prosthesis
Gender Dysphoria Treatment
Page 7 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
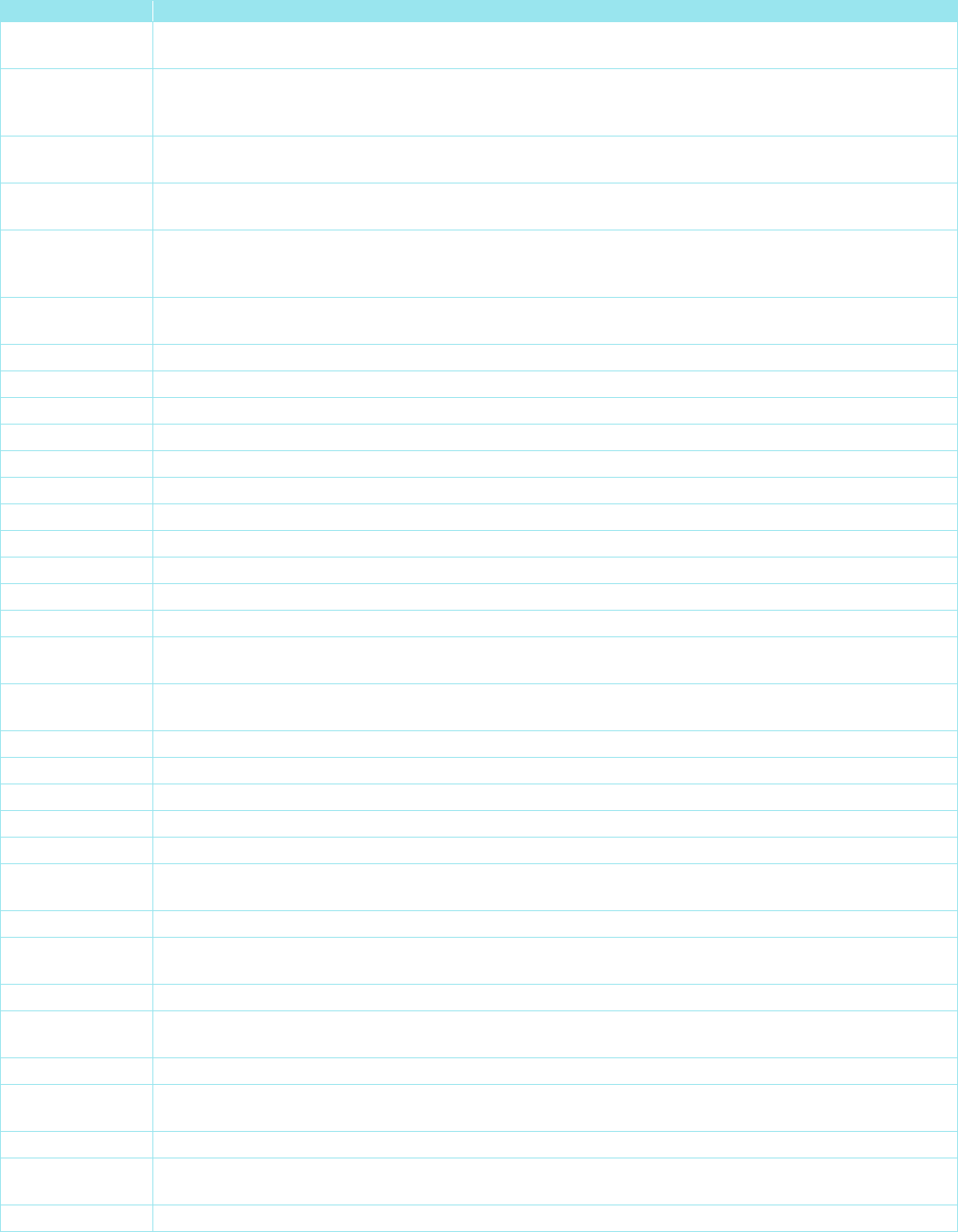
CPT Code
Description
54410
Removal and replacement of all component(s) of a multi-component, inflatable penile prosthesis at
the same operative session
54411 Removal and replacement of all components of a multi-component inflatable penile prosthesis
through an infected field at the same operative session, including irrigation and debridement of
infected tissue
54415 Removal of non-inflatable (semi-rigid) or inflatable (self-contained) penile prosthesis, without
replacement of prosthesis
54416
Removal and replacement of non-inflatable (semi-rigid) or inflatable (self-contained) penile
prosthesis at the same operative session
54417
Removal and replacement of non-inflatable (semi-rigid) or inflatable (self-contained) penile
prosthesis through an infected field at the same operative session, including irrigation and
debridement of infected tissue
54520
Orchiectomy, simple (including subcapsular), with or without testicular prosthesis, scrotal or inguinal
approach
54660
Insertion of testicular prosthesis (separate procedure)
54690
Laparoscopy, surgical; orchiectomy
55175
Scrotoplasty; simple
55180
Scrotoplasty; complicated
55970
Intersex surgery; male to female
55980
Intersex surgery; female to male
56625
Vulvectomy simple; complete
56800
Plastic repair of introitus
56805
Clitoroplasty for intersex state
57110
Vaginectomy, complete removal of vaginal wall
57335
Vaginoplasty for intersex state
58150
Total abdominal hysterectomy (corpus and cervix), with or without removal of tube(s), with or
without removal of ovary(s)
58180 Supracervical abdominal hysterectomy (subtotal hysterectomy), with or without removal of tube(s),
with or without removal of ovary(s)
58260
Vaginal hysterectomy, for uterus 250 g or less
58262
Vaginal hysterectomy, for uterus 250 g or less; with removal of tube(s), and/or ovary(s)
58290
Vaginal hysterectomy, for uterus greater than 250 g
58291
Vaginal hysterectomy, for uterus greater than 250 g; with removal of tube(s) and/or ovary(s)
58541
Laparoscopy, surgical, supracervical hysterectomy, for uterus 250 g or less
58542
Laparoscopy, surgical, supracervical hysterectomy, for uterus 250 g or less; with removal of tube(s)
and/or ovary(s)
58543
Laparoscopy, surgical, supracervical hysterectomy, for uterus greater than 250 g
58544 Laparoscopy, surgical, supracervical hysterectomy, for uterus greater than 250 g; with removal of
tube(s) and/or ovary(s)
58550
Laparoscopy, surgical, with vaginal hysterectomy, for uterus 250 g or less
58552
Laparoscopy, surgical, with vaginal hysterectomy, for uterus 250 g or less; with removal of tube(s)
and/or ovary(s)
58553
Laparoscopy, surgical, with vaginal hysterectomy, for uterus greater than 250 g
58554 Laparoscopy, surgical, with vaginal hysterectomy, for uterus greater than 250 g; with removal of
tube(s) and/or ovary(s)
58570
Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less
58571
Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less; with removal of tube(s)
and/or ovary(s)
58572
Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g
Gender Dysphoria Treatment
Page 8 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
CPT Code
Description
58573
Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g; with removal of
tube(s) and/or ovary(s)
58661 Laparoscopy, surgical; with removal of adnexal structures (partial or total oophorectomy and/or
salpingectomy)
58720
Salpingo-oophorectomy, complete or partial, unilateral or bilateral (separate procedure)
58940
Oophorectomy, partial or total, unilateral or bilateral
64856
Suture of major peripheral nerve, arm or leg, except sciatic; including transposition
64892
Nerve graft (includes obtaining graft), single strand, arm or leg; up to 4 cm length
64896
Nerve graft (includes obtaining graft), multiple strands (cable), hand or foot; more than 4 cm length
67900
Repair of brow ptosis (supraciliary, mid-forehead or coronal approach)
92507
Treatment of speech, language, voice, communication, and/or auditory processing disorder;
individual
92508 Treatment of speech, language, voice, communication, and/or auditory processing disorder; group,
2 or more individuals
CPT
®
is a registered trademark of the American Medical Association
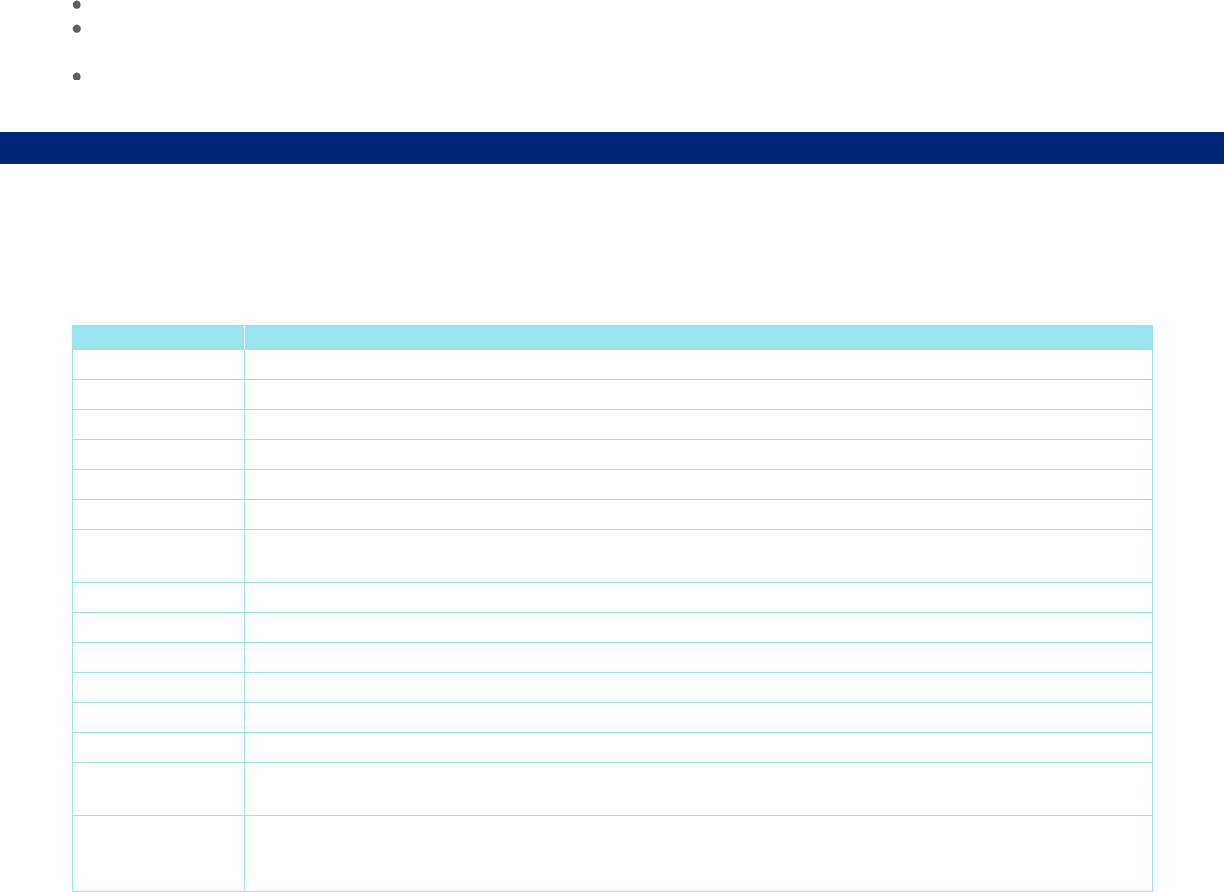
Diagnosis Code
Description
F64.0 Transsexualism
F64.1 Dual role transvestism
F64.2 Gender identity disorder of childhood
F64.8 Other gender identity disorders
F64.9 Gender identity disorder, unspecified
Z87.890 Personal history of sex reassignment
Description of Services
Gender Dysphoria is a condition in which there is a marked incongruence between an individual’s experienced/expressed/
alternative gender and assigned gender (DSM-5-TR). Gender-affirming care encompasses a range of social,
psychological, behavioral, and medical interventions to support an individual’s gender identity. Treatment options include
behavioral therapy, psychotherapy, hormone therapy, and surgery for gender transformation. Surgical treatments for
Gender Dysphoria may include the following: clitoroplasty, hysterectomy, labiaplasty, mastectomy, orchiectomy,
penectomy, phalloplasty or metoidioplasty (alternative to phalloplasty), placement of testicular and/or penile prostheses,
salpingo-oophorectomy, scrotoplasty, urethroplasty, urethroplasty, vaginectomy, vaginoplasty, and vulvectomy.
Other terms used to describe surgery for Gender Dysphoria include gender affirming surgery, sex transformation surgery,
sex change, sex reversal, gender change, transsexual surgery, transgender surgery, and sex reassignment.
Benefit Considerations
Coverage Information
Benefit coverage for health services is determined by the federal, state or contractual requirements that may require
coverage for a specific service.
Unless otherwise specified, if a plan covers treatment for Gender Dysphoria, coverage includes psychotherapy, gender-
affirming hormone therapy, puberty suppressing medications, laboratory testing to monitor the safety of hormone therapy,
and certain surgical treatments listed in the Coverage Rationale section. Certain plans may not cover all of the listed
surgical treatments in the Coverage Rationale section above. Refer to the federal, state, or contractual requirements for
details. Also, for hormone therapy, refer to the Medical Benefit Drug Policy titled Gonadotropin Releasing Hormone
Analogs.
Limitations and Exclusions
Certain treatments and services are not covered. Examples include, but are not limited to:
Gender Dysphoria Treatment
Page 9 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Treatments and procedures that are specifically excluded, or otherwise do not meet the requirements of a Covered
Health Care Service, in the federal, state, or contractual requirements
Treatment received outside of the United States
Reproduction services, including, but not limited to, sperm preservation in advance of hormone treatment or Gender
Dysphoria surgery, cryopreservation of fertilized embryos, oocyte preservation, surrogate parenting, donor eggs,
donor sperm and host uterus (refer to the federal, state or contractual requirements for benefit coverage)
Transportation, meals, lodging, or similar expenses
Cosmetic procedures (refer to the Medical Policy titled Cosmetic and Reconstructive Procedures and the Coverage
Rationale section). Refer to the section below for additional information on New York plans
Coverage does not apply to members who do not meet the indications listed in the Coverage Rationale section above.
For New York Plans Only
Certain ancillary procedures may be considered cosmetic and not medically necessary when performed as part of surgical
treatment for Gender Dysphoria. Clinical review for medical necessity of ancillary procedures is conducted on a case-by-
case basis.
Clinical Evidence
In a 2023a evolving evidence review, Hayes evaluated combination facial feminization surgery in patients with gender
dysphoria. There were eleven very poor- to poor-quality studies with 10 being retrospective designs, five systematic
reviews, and four guidelines identified. The overall conclusion is that facial feminization surgery has the potential to safely
improve satisfaction and quality of life; however, data are lacking for mental health outcomes, patient and third-party
perception of femininity, and longer-term follow-up. The quality of the evidence creates difficulty evaluating interventions
and is unlikely to improve.
Hayes (2023b) conducted an evidence review for female-to-male gender-affirming surgical (GAS) procedures for
adolescents with gender dysphoria. There were three clinical studies included in the review that were of poor to very poor
quality, no systematic reviews were identified, and three evidence-based guidelines with expert opinion. Evidence
suggests that masculinizing chest GAS may provide psychological and social benefits for transgender adolescent boys,
however, uncertainty remains for this age group due to lack of long-term follow-up, lack of validated structure outcome
assessments, no studies evaluating efficacy and safety of genital GAS, and no studies evaluating reversal rates after
GAS. The overall conclusion is that there is unclear to minimal support for female-to-male GAS in adolescents.
Additionally, because randomization of treatment is inappropriate in this patient population, it is unlikely that there will be
higher-quality studies forthcoming.
A Hayes (2023c) evolving evidence review evaluated gender-affirming hair removal for patients with gender dysphoria.
There were two very poor- to poor-quality prospective studies identified, no systematic reviews, and three guidelines
identified of which 1 performed a systematic review of the literature. The two low-quality studies suggest clearance of hair
is at least moderately effective and highly satisfactory when modality is properly selected but not guaranteed to be 100%
permanent for any modality. Better laser hair removal results may be attained if no mechanical epilation is done prior and
no adverse events were reported. The overall conclusion is that there is minimal support for gender-affirming hair removal
based on clinical studies as data is lacking or nonexistent for efficacy of hair removal treatment before versus after
starting hormone therapy, adverse events/effects, pain, quality of life, and long-term follow-up.
Hayes (2023d) conducted an evidence review for male-to-female GAS procedures for adolescents with gender dysphoria.
There were no clinical studies or systematic reviews identified for this population and only three evidence-based
guidelines with expert opinion were identified. It was determined that the evidence for efficacy and safety of vaginoplasty
gender-affirming surgery is unclear in this population. Additionally, given that there are no current or ongoing studies
specifically aimed at this population, high-quality studies are unlikely to be forthcoming as randomization of treatment is
inappropriate in this population.
In a 2023e evolving evidence review, Hayes evaluated Wendler glottoplasty (WG) surgery for voice feminization in
patients with gender dysphoria. Six poor- to very poor-quality studies were identified along with one systematic review
with meta-analysis of 13 poor quality studies, and one guideline. The conclusion is that WG may achieve improvement in
vocal qualities when combined with voice therapy, however, due to heterogeneity in surgical techniques and lack of
organizational support for a recommended surgical modality, no recommendation can be made of a single approach.
Gender Dysphoria Treatment
Page 10 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Schwarz et al. (2023) performed a systematic review and meta-analysis evaluating speech therapy and phonosurgery for
transgender women. There were 16 studies included in the review. The relationship between therapy time and post-
treatment frequency gain was not significant. The authors found that the type of sample collected significantly influenced
the voice frequency gain. The authors also noted that both phonosurgery and voice feminization therapy showed an
increase in voice frequency with phonosurgery having significantly more fundamental frequency gain compared to speech
therapy alone. Limitations of the review include a low quality of evidence based on the lack of randomized controlled trials,
small sample sizes, and various methods of collecting voice frequency.
A panel of facial gender surgeons presented guidelines for screening, management, and surgical technique for patients
undergoing facial gender surgery (Coon et al., 2022). The specific recommendations and position statements presented
represent the panel’s expert opinion based on collective experience and review of current evidence. Of the 21 studies
included in the systematic review, 16 included some form of patient-centered outcomes. Thirteen studies included upper
face procedures, primarily forehead; 14 studies described midface procedures, including rhinoplasty; 11 studies described
lower face procedures, primarily genioplasty and mandibular osteotomy; and two studies did not specify. Most studies
pointed to high rates of satisfaction and improved quality of life in patients who have undergone facial gender surgery;
however, many cases were small cohorts or lacked effective instruments for assessing patient-reported outcomes. The
panel also noted that nearly all articles originated from the same few experienced high-volume authors. Larger,
multicenter, prospective studies with sufficient sample size are needed to advance the science further and to identify
which patients would benefit the most from these procedures. Research priorities include better procedural outcomes
data, more quality-of-life studies, and insight into variation in both patient and procedural subgroups.
Hayes (2022a) performed an evidence review for feminizing voice and communication therapy for gender dysphoria and
identified one poor- and four very poor-quality clinical studies, one systematic review that only included 2 clinical studies,
and two expert-opinion guidelines. All clinical studies had a small sample size, lacked comparison groups and did not
report clear benefits or advantages in patient-oriented outcomes. There are two RCTs underway examining feminizing
voice therapy.
Hayes (2022b) performed an evidence review for masculinizing voice and communication therapy for gender dysphoria
and identified one poor-quality clinical study, no systematic reviews, and two expert opinion-based guidelines. The clinical
study identified appeared to suggest that masculinizing voice therapy is associated with improvement in patient
satisfaction; however, evidence is extremely sparse and low in quality. There is one randomized controlled trial that is
underway examining voice therapy.
Wang et al. (2022) performed a systematic review and meta-analysis to evaluate the outcomes for different phalloplasty
surgical techniques. There were 39 articles included in the analysis which consisted of 19 case series, 3 cross-sectional
studies, and 17 retrospective cohort studies for a total of 1,731 patients. The most common type of reconstruction was
radial forearm free flap (75.1%). The overall complication rate for phalloplasty was 76.5% with urethral complications
being common (fistula 34.1% and stricture 25.4%). Only 14 of the 39 studies reported on functional outcomes. Of those
studies, most patients (93.9%) reported having tactile sensation and ability to void while standing (92.2%) and 59.93%
reported erogenous sensation/sexual function. Aesthetic outcomes were reported in 6.3% of patients with mean length
achieved of 12.26 cm and mean circumference of 10.18 cm. The authors conclude that the evidence available for
phalloplasty surgical techniques and expected outcomes is weak and lacking. Future research is needed to develop
standardized core outcomes and improve clinical decision making.
Oles et al. (2022) performed a systematic review of gender-affirming surgery publications to assess outcomes and
outcome assessment tools. Part 1 of the review encompasses non-genital procedures such as chest feminization, chest
masculinization and voice surgery. Patient-centered outcomes included survival, function, symptoms and health-related
quality of life. Outcome data was pooled to assess reported complications, satisfaction and other outcome rates. A total of
406 cohort publications were included. The lack of consistent use of the same outcome measures and validated gender-
affirming surgery-specific instruments represent the two primary barriers to high-quality research. The authors address
current methodologic limitations in the literature and what dimensions must be included in assessing surgical success.
Addressing gaps in the literature will promote evidence-based practices and lead to improved surgical techniques.
Siringo, et al. (2022) performed a systematic review designed to critically appraise the literature, identify knowledge gaps,
and inform future advancements in facial feminization surgical practice. Potential components of facial feminization
surgery included frontal sinus setback, burring of the supraorbital ridge, hairline lowering, rhinoplasty, malar
augmentation, genioplasty, mandibular angle reduction or alternative jaw contouring, and tracheal shave. A total of 23
articles were included in the review, including primary data pertaining to 3,554 patients who underwent 8,506 total
procedures. Participants ranged in age from 18 to 73. Data on procedures, outcomes, patient age, follow-up time,
complications, and patient satisfaction were collected. Information was categorized by facial thirds and then further
Gender Dysphoria Treatment
Page 11 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
stratified by facial feature. Most of the procedures addressed the upper facial third (hairline, forehead, and brow),
comprising 49.1% of total procedures performed. Further categorization by facial feature revealed that the most commonly
addressed feature was the forehead (34.6% of procedures), followed by the nose (12.8%) and the chin (12.2%). The
authors reported that facial feminization surgery was found to be safe, whether conducted in a single stage or as a staged
procedure. Patients reported high satisfaction and better gender congruency after facial feminization procedures. The use
of validated and specific patient-reported outcome measures and standardization of follow-up would better inform patients'
postoperative quality of life. Future investigations focused on the timing and coordination of procedures, as well as the
development of patient-reported outcome measures, might better guide these surgeries moving forward. Author noted
limitations include potential for bias in data interpretation and variations in the extent of information regarding surgical
techniques and features addressed. Further research is needed to establish best surgical practice and gauge patient
satisfaction beyond the length of average follow-up.
Bustos et al. (2021) conducted a systematic review and meta-analysis of the complications and patient-reported outcomes
in transfemale vaginoplasty. This was an updated systematic review and included data compiled from the previous
systematic review by Manrique et al. (2018). There were 57 studies included in the review and 52 studies included in the
meta-analysis with a total of 4,680 cases. Results including any surgical technique showed a complication rate of 1% for
fistula, 11% for stenosis and/or strictures, 4% for tissue necrosis, and 3% for prolapse. The patient-reported satisfaction
rate was 91% for overall, functional, and aesthetic outcomes with 76% of patients reporting the ability to achieve orgasm.
There was a regret rate of 2%. The average neovaginal depth was 9.4 cm for the penile skin inversion and 15.3 cm for the
intestinal vaginoplasty. The authors noted that in general, the quality of the studies was either low or moderate with the
majority being retrospective with no control group. They conclude that transfemale vaginoplasty is an important
component of a comprehensive surgical treatment for transfemale patients with gender dysphoria and there will likely be
an increase in demand for these procedures, therefore, continued surgical training, clinical/surgical experience, and
research outcomes are necessary to provide the best care possible for this population. (Publications by Bouman 2016,
Buncamper 2016, Gaither 2018, and Manrique 2018, which were previously cited in this policy, are included in this
systematic review).
Sijben et al. (2021) analyzed complications, surgical trends and long-term follow-up of breast augmentations in 527
transgender women and nonbinary individuals. A total of nine studies were included, most were of retrospective design.
Reoperations due to short-term complications were infrequent. Reoperations due to long-term complications included
implant rupture (5.7%), capsular contracture (4.9%), aesthetic problems (3.8%), low-grade infection (0.4%) or seroma
(0.6%). Follow-up time ranged from 30 days to 5.5 years.
Almazan et al. (2021) conducted a secondary analysis of the 2015 United States Transgender Survey (USTS) that
included 27,715 transgender and gender diverse (TGD) people to evaluate whether gender-affirming surgeries were
associated with better mental health outcomes including psychological distress, substance use and suicide risk when
compared to TGD people who do not undergo gender-affirming surgeries. The survey was conducted across all 50 states,
Washington, DC, U.S. territories and U.S. military bases abroad. The exposure group included respondents who indicated
they had undergone 1 or more gender-affirming surgeries at least 2 years prior to submitting survey responses. This
group was compared to respondents who indicated a desire to undergo 1 or more types of gender-affirming surgeries but
denied having had any gender-affirming surgeries. Of the 27,715 respondents, 3,559 (12.8%) indicated they had
undergone 1 or more gender-affirming surgeries at least 2 years prior to the survey while 59.2% (n = 16,401) indicated a
desire to undergo a gender-affirming surgery but had not done so as of the time they responded to the survey.
Demographics of the respondents to the survey showed that 81.1% (n = 16,182) were between the ages of 18 and 44
years, 82.1% (n = 16,386) identified as white, 38.8% (n = 7,751) identified as transgender women, 32.5% (n = 6,489)
identified as transgender men and 26,6% (n = 5,300) identified as nonbinary. After adjusting for sociodemographic
factors, the authors concluded that the analysis showed TGD people with a history of gender-affirming surgery had
significantly lower odds of past-month psychological distress, past-year tobacco smoking, and past-year suicidal ideation
compared with TGD people who did not have any gender-affirming surgery. Limitations noted by the authors included the
nonprobability sampling of the database, the self-reporting structure of the measures, and the risk of confounding. The
authors concluded that the study showed a positive association between gender-affirming surgery and improved mental
health outcomes for TGD people who seek gender affirming surgical interventions.
Gray and Courey (2019) reported that many male to female (MtF) patients require initial or sustained voice therapy with or
without phonosurgery to achieve voice goals. A study comparing voice outcomes after Wendler glottoplasty with and
without voice therapy found that voice therapy was associated with higher pitch, improved self-evaluation and increased
perception of feminine voice. The authors also noted that hormone therapy is recommended for at least six months prior
to further voice intervention.

Gender Dysphoria Treatment
Page 12 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Scandurra et al. (2019) performed a systematic review assessing the health of nonbinary and genderqueer (NBGQ)
individuals compared to binary transgender (BT) and cisgender individuals. Eleven studies were included in the review.
Results related to the difference in health between NBGQ and BT were mixed, with some finding a better health status
while others a worse one. Results related to the differences in health between NBGQ and cisgender individuals
highlighted higher health needs in NBGQ individuals compared with cisgender counterparts. The authors noted the need
for research expansion in terms of both methodology and research contents.
Wernick et al. (2019) conducted a systematic review of the psychological benefits of gender-affirming surgery. Thirty-three
studies were included in the analysis. Overall, most of the studies comparing pre- and post-operative data on quality of
life, body image/satisfaction, and overall psychological functioning among individuals with gender dysphoria suggested
that gender-affirming surgery leads to multiple, significant psychological benefits. Of the studies comparing psychological
well-being between individuals who did or did not undergo surgery, most demonstrated a trend of better mental health
among individuals who underwent surgery compared with those who did not. The authors encouraged future research to
focus on standardizing the assessment of psychological functioning pre- and post-gender-affirming surgery to gather
longitudinal data that will allow for more definitive conclusions to be made about factors that contribute to the
psychological benefits of surgery.
Cohen et al. (2019) conducted a systematic review of surgical options and associated outcomes for transmasculine top
surgery. Twenty-two studies were included (n = 2,447). The authors reported that future research is needed to improve
patient selection, surgical decision making, and patient-reported outcomes for different chest contouring techniques.
Mahfouda et al. (2019) conducted a systematic review of the available published evidence on gender-affirming hormone
and surgical interventions in transgender children and adolescents, amalgamating findings on mental health outcomes,
cognitive and physical effects, side-effects, and safety variables. The small amount of available data suggests that when
clearly indicated in accordance with international guidelines, gender-affirming hormone therapy and chest wall
masculinization in transgender males are associated with improvements in mental health and quality of life. Evidence
regarding surgical vaginoplasty in transgender females younger than age 18 years remains extremely scarce and
conclusions cannot yet be drawn regarding its risks and benefits in this age group. Further research on an international
scale is urgently warranted to clarify long-term outcomes on psychological functioning and safety.
A Hayes report on sex reassignment surgery (2018; updated 2022) for the treatment of gender dysphoria made the
following conclusions:
Studies suggest that following sex reassignment surgery, patients reported decreased gender dysphoria and
improved body image satisfaction. However, results were mixed regarding effects of sex reassignment surgery on
quality of life and psychological symptoms
Few studies compare outcomes in patients who received sex reassignment surgery with stand-alone hormone
therapy. The results of these studies suggest that sex reassignment surgery may improve gender dysphoria, quality of
life, body image and psychological symptoms to a greater extent than hormone therapy alone. However, the results
were conflicting
Few studies compared outcomes in patients who received different components of sex reassignment surgery. For
most outcome measures, there was only a single study available. This evidence is therefore insufficient to support
definitive conclusions regarding the comparative effectiveness of different components of sex reassignment surgery
for treating gender dysphoria
Not all studies reported all outcomes; the following findings therefore do not inform overall incidence of complications.
Following sex reassignment surgery, there were very low rates of regret of surgery (0% to 6% per study) and suicide
(2% to 3% per study). Complications following sex reassignment surgery were common, and some were serious
Dreher et al. (2018) conducted a systematic review and meta-analysis to evaluate the epidemiology, presentation,
management, and outcomes of neovaginal complications in the MtF transgender reassignment surgery patients. Selected
studies reported on 1,684 patients with an overall complication rate of 32.5% and a reoperation rate of 21.7% for non-
esthetic reasons. The most common complication was stenosis of the neo-meatus (14.4%). Wound infection was
associated with an increased risk of all tissue-healing complications. Use of sacrospinous ligament fixation (SSL) was
associated with a significantly decreased risk of prolapse of the neovagina. The authors concluded that gender-affirmation
surgery is important in the treatment of gender dysphoric patients, but there is a high complication rate in the reported
literature. Variability in technique and complication reporting standards makes it difficult to assess the accurately the
current state of MtF gender reassignment surgery. Further research and implementation of standards is necessary to
improve patient outcomes.
Van Damme et al. (2017) conducted a systematic review of the effectiveness of pitch-raising surgery performed in MtF
transsexuals. Twenty studies were included: eight using cricothyroid approximation, six using anterior glottal web
Gender Dysphoria Treatment
Page 13 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
formation and six using other surgery types or a combination of surgical techniques. A substantial rise in postoperative
frequency was identified. The majority of patients seemed satisfied with the outcome. However, none of the studies used
a control group and randomization process. Further investigation regarding long-term results using a stronger study
design is necessary.
An ECRI special report systematically reviewed the clinical literature to assess the efficacy of treatments for gender
dysphoria. The authors identified limited evidence from mostly low-quality retrospective studies. Evidence on gender
reassignment surgery was mostly limited to evaluations of MtF individuals undergoing vaginoplasty, facial feminization
surgery and breast augmentation. Outcomes included mortality, patient satisfaction, physical well-being, psychological-
related outcomes, quality of life, sexual-related outcomes, suicide and adverse events. Concluding remarks included the
need for standardized protocols and prospective studies using standardized measures for correct interpretation and
comparability of data (ECRI, 2016).
Morrison et al. (2016) conducted a systematic review of the facial feminization surgery literature. Fifteen studies were
included, all of which were either retrospective or case series/reports. The studies covered a variety of facial feminization
procedures. A total of 1,121 patients underwent facial feminization surgery, with seven complications reported, although
many studies did not explicitly comment on complications. Satisfaction was high, although most studies did not use
validated or quantified approaches to address satisfaction. The authors noted that further studies are needed to better
compare different techniques to more robustly establish best practices. Prospective studies and patient-reported
outcomes are needed to establish quality of life outcomes for patients.
Frey et al. (2016) conducted a systematic review of metoidioplasty and radial forearm flap phalloplasty (RFFP) in female
to male (FtM) transgender genital reconstruction. Eighteen studies were included: 7 for metoidioplasty and 11 for RFFP.
The quality of evidence was low to very low for all included studies. In studies examining metoidioplasty, the average
study size and length of follow-up were 54 patients and 4.6 years, respectively [1 study did not report (NR)]. Eighty-eight
percent underwent a single-stage reconstruction, 87% reported an aesthetic neophallus (3 NR) and 100% reported
erogenous sensation (2 NR). Fifty-one percent of patients reported successful intercourse (3 NR) and 89% of patients
achieved standing micturition (3 NR). In studies examining RFFP, the average study size and follow-up were 60.4 patients
and 6.23 years, respectively (6 NR). No patients underwent single-stage reconstructions (8 NR). Seventy percent of
patients reported a satisfactorily aesthetic neophallus (4 NR) and 69% reported erogenous sensation (6 NR). Forty-three
percent reported successful penetration of partner during intercourse (6 NR) and 89% achieved standing micturition (6
NR). Compared with RFFP, metoidioplasty was significantly more likely to be completed in a single stage, have an
aesthetic result, maintain erogenous sensation, achieve standing micturition and have a lower overall complication rate.
The authors reported that, although the current literature suggests that metoidioplasty is more likely to yield an “ideal”
neophallus compared with RFFP, any conclusion is severely limited by the low quality of available evidence.
Despite the significant increase in genital gender affirming surgery (GAS) within the past 50 years, there is limited data
regarding hair removal practices in preparation for genital GAS. Genital GAS involves reconstruction of the genitals to
match a patient's identified sex. The use of hair-bearing flaps in this procedure may result in postoperative intra-vaginal
and intra-urethral hair growth and associated complications, including lower satisfaction with genital GAS. In 2016, Zhang
et al. conducted a literature review, recommendations from experience, and a practical laser hair removal (LHR) approach
to hair removal prior to genital GAS.
Horbach et al. (2015) conducted a systematic review of vaginoplasty techniques in MtF individuals with gender dysphoria.
Twenty-six studies were included (mostly retrospective case series of low to intermediate quality). Outcome of the penile
skin inversion technique was reported in 1,461 patients and bowel vaginoplasty in 102 patients. Neovaginal stenosis was
the most frequent complication in both techniques. Sexual function and patient satisfaction were overall acceptable, but
many different outcome measures were used. Quality of life was only reported in one study. Comparison between
techniques was difficult due to the lack of standardization. The authors concluded that the penile skin inversion technique
is the most researched surgical procedure. Outcome of bowel vaginoplasty has been reported less frequently but does not
seem to be inferior. The available literature is heterogeneous in patient groups, surgical procedure, outcome
measurement tools and follow-up. There is a need for prospective studies with standardized surgical procedures, larger
patient groups and longer follow-up periods. Uniformity in outcome measurement tools such as validated questionnaires
and scores for sexual function and quality of life is mandatory for correct interpretation and comparability of data.
Bouman et al. (2014) conducted a systematic review of surgical techniques and clinical outcomes of intestinal
vaginoplasty. Twenty-one studies were included (n = 894). All studies had a retrospective design and were of low quality.
Prevalence and severity of procedure-related complications were low. The main postoperative complication was introital
stenosis, necessitating surgical correction in 4.1% of sigmoid-derived and 1.2% of ileum-derived vaginoplasties. Neither
diversion colitis nor cancer was reported. Sexual satisfaction rate was high, but standardized questionnaires were rarely
Gender Dysphoria Treatment
Page 14 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
used. Quality of life was not reported. The authors concluded that prospective studies, using standardized measures and
questionnaires, are warranted to assess functional outcomes and quality of life.
Djordjevic et al. (2013) evaluated 207 patients who underwent single-stage metoidioplasty, comparing two different
surgical techniques of urethral lengthening. The procedure included lengthening and straightening of the clitoris, urethral
reconstruction and scrotoplasty with implantation of testicular prostheses. Buccal mucosa graft was used in all cases for
dorsal urethral plate formation and joined with one of the two different flaps: longitudinal dorsal clitoral skin flap (n = 49)
(group 1) and labia minora flap (n = 158) (group 2). The median follow-up was 39 months. The total length of
reconstructed urethra ranged from 9.1 to 12.3 cm in group 1 and from 9.4 to 14.2 cm in group 2. Voiding while standing
was significantly better in group 2 (93%) than in group 1 (87.82%). Urethral fistula occurred in 16 patients in both groups.
Overall satisfaction was noted in 193 patients. The authors concluded that combined buccal mucosa graft and labia
minora flap was the method of choice for urethroplasty in metoidioplasty, minimizing postoperative complications.
In a non-randomized study, Dhejne et al. (2011) evaluated mortality, morbidity and criminal rates after gender
reassignment surgery in 324 individuals (MtF n = 191; FtM n = 133). Random population controls (10:1) were matched by
birth year and birth sex or reassigned final sex. The authors reported substantially higher rates of overall mortality, death
from cardiovascular disease and suicide, suicide attempts and psychiatric hospitalizations in sex-reassigned individuals
(both MtF/FtM) compared to a healthy control population. FtMs had a higher risk for criminal convictions.
Murad et al. (2010) conducted a systematic review to evaluate the effects of hormone therapy on patients undergoing
gender reassignment surgery. The authors identified 28 eligible studies, all of which were observational and most lacked
controls. These studies enrolled 1,833 participants with gender dysphoria (1,093 MtF; 801 FtM). After gender
reassignment surgery, individuals reported improvement in gender dysphoria (80%), psychological symptoms (78%),
sexual function (72%) and quality of life (80%). The authors concluded that very low quality evidence suggests that
gender reassignment, which includes hormonal interventions, is likely to improve gender dysphoria, psychological
functioning and comorbidities, sexual function and overall quality of life.
Sutcliffe et al. (2009) systematically reviewed five individual procedures for MtF gender reassignment surgery:
clitoroplasty, labiaplasty, orchiectomy, penectomy and vaginoplasty. Further evaluations were made of eight surgical
procedures for FtM gender reassignment surgery: hysterectomy, mastectomy, metoidioplasty, phalloplasty, salpingo-
oophorectomy, scrotoplasty/placement of testicular prostheses, urethroplasty and vaginectomy. Eighty-two published
studies (38 MtF; 44 FtM) were included in the review. For MtF procedures, the authors found no evidence that met the
inclusion criteria concerning labiaplasty, penectomy or orchiectomy. A large amount of evidence was available concerning
vaginoplasty and clitoroplasty procedures. The authors reported that the evidence concerning gender reassignment
surgery in both MtF and FtM individuals with gender dysphoria has several limitations including lack of controlled studies,
lack of prospective data, high loss to follow- up and lack of validated assessment measures. Some satisfactory outcomes
were reported, but the magnitude of benefit and harm for individual surgical procedures cannot be estimated accurately
using the current available evidence.
World Professional Association for Transgender Health (WPATH)
In Standards of Care version 8, WPATH offers standards for promoting optimal healthcare and guidance for the treatment
of transgender and gender diverse individuals. Recommendation statements were developed based on data derived from
independent systematic literature reviews, where available, background reviews and expert opinions (Coleman et al.,
2022).
Clinical Practice Guidelines
American Academy of Pediatrics (AAP)
In a 2018 policy statement entitled Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse
Children and Adolescents, the AAP states the following regarding surgery: Surgical approaches may be used to feminize
or masculinize features, such as hair distribution, chest, or genitalia, and may include removal of internal organs, such as
ovaries or the uterus (affecting fertility). These changes are irreversible. Although current protocols typically reserve
surgical interventions for adults, they are occasionally pursued during adolescence on a case-by case basis, considering
the necessity and benefit to the adolescent’s overall health and often including multidisciplinary input from medical, mental
health, and surgical providers as well as from the adolescent and family (Rafferty et al, 2018).
American College of Obstetrics and Gynecology (ACOG)
An ACOG committee opinion (2021) provides guidance on health care for transgender and gender diverse individuals.
The document does not make specific recommendations regarding surgery but does provide an overview of surgical
procedures and education for clinicians who care for transgender patients before and after surgery.

Gender Dysphoria Treatment
Page 15 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Endocrine Society
Endocrine Society practice guidelines (Hembree et al., 2017) addressing endocrine treatment of gender-
dysphoric/gender-incongruent persons makes the following recommendations regarding surgery for sex reassignment and
gender confirmation:
Suggest that clinicians delay gender-affirming genital surgery involving gonadectomy and/or hysterectomy until the
patient is at least 18 years old or legal age of majority in his or her country (Recommendation based on low quality
evidence)
A patient pursue genital gender-affirming surgery only after the mental health practitioner (MHP) and the clinician
responsible for endocrine transition therapy both agree that surgery is medically necessary and would benefit the
patient’s overall health and/or well-being (Strong recommendation based on low quality evidence)
Surgery is recommended only after completion of at least one year of consistent and compliant hormone treatment
unless hormone therapy is not desired or medically contraindicated (Ungraded Good Practice Statement)
The physician responsible for endocrine treatment medically clears individual for surgery and collaborates with the
surgeon regarding hormone use during and after surgery (Ungraded Good Practice Statement)
Recommend that clinicians refer hormone treated transgender individuals for genital surgery when (Strong
recommendation based on very low quality evidence):
o The individual has had a satisfactory social role change
o The individual is satisfied about the hormonal effects
o The individual desires definitive surgical changes
Suggest that clinicians determine the timing of breast surgery for transgender males based upon the physical and
mental health status of the individual. There is insufficient evidence to recommend a specific age requirement
(Recommendation based on very low quality evidence)
U.S. Food and Drug Administration (FDA)
This section is to be used for informational purposes only. FDA approval alone is not a basis for coverage.
Gender transformation surgeries are procedures, and therefore, not subject to FDA regulation. However, medical devices,
drugs, biologics, or tests used as a part of these procedures may be subject to FDA regulation. Refer to the following
website to search by product name. Available at: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm.
(Accessed August 16. 2023)
References
Almazan AN, Keuroghlian AS. Association between gender-affirming surgeries and mental health outcomes. JAMA Surg.
2021 Jul 1;156(7):611-618.
American College of Obstetricians and Gynecologists (ACOG). Committee Opinion #823. Health care for transgender and
gender diverse individuals. Obstet Gynecol. 2021 Mar 1;137(3):e75-e88.
Bouman MB, van der Sluis WB, Buncamper ME, et al. Primary total laparoscopic sigmoid vaginoplasty in transgender
women with penoscrotal hypoplasia: a prospective cohort study of surgical outcomes and follow-up of 42 patients. Plast
Reconstr Surg. 2016 Oct;138(4):614e-23e.
Bouman MB, van Zeijl MC, Buncamper ME, et al. Intestinal vaginoplasty revisited: a review of surgical techniques,
complications, and sexual function. J Sex Med. 2014 Jul;11(7):1835-47.
Buncamper ME, van der Sluis WB, van der Pas RS, et al. Surgical outcome after penile inversion vaginoplasty: a
retrospective study of 475 transgender women. Plast Reconstr Surg. 2016 Nov;138(5):999-1007.
Bustos SS, Bustos VP, Mascaro A, et al. Complications and patient-reported outcomes in transfemale vaginoplasty: An
updated systematic review and meta-analysis. Plast Reconstr Surg Glob Open. 2021 Mar 19;9(3):e3510.
Cohen WA, Shah NR, Iwanicki M, et al. Female-to-male transgender chest contouring: a systematic review of outcomes
and knowledge gaps. Ann Plast Surg. 2019 Nov;83(5):589-593.
Coleman E, Radix AE, Bouman WP, et al. World Professional Association for Transgender Health (WPATH). Standards of
Care for the Health of Transgender and Gender Diverse People, Version 8. Int J Transgend Health. 2022 Sep 6;23(Suppl
1):S1-S259.
Coon D, Berli J, Oles N, et al. Facial gender surgery: Systematic review and evidence-based consensus guidelines from
the international facial gender symposium. Plast Reconstr Surg. 2022 Jan 1;149(1):212-224.

Gender Dysphoria Treatment
Page 16 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Dhejne C, Lichtenstein P, Boman M, et al. Long-term follow-up of transsexual persons undergoing sex reassignment
surgery: cohort study in Sweden. PLoS One. 2011 Feb 22;6(2):e16885.
Djordjevic ML, Bizic MR. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty)
surgery. J Sex Med. 2013 May;10(5):1431-8.
Diagnostic and statistical manual of mental disorders (5
th
ed., Text Revision). 2022. Washington, DC: American
Psychiatric Association.
Dreher PC, Edwards D, Hager S, et al. Complications of the neovagina in male-to-female transgender surgery: A
systematic review and meta-analysis with discussion of management. Clin Anat. 2018 Mar;31(2):191-199.
ECRI Institute. Special Report. Gender dysphoria. January 2016.
Frey JD, Poudrier G, Chiodo MV, Hazen A. A systematic review of metoidioplasty and radial forearm flap phalloplasty in
female-to-male transgender genital reconstruction: is the “ideal” neophallus an achievable goal? Plast Reconstr Surg Glob
Open. 2016 Dec 23;4(12):e1131.
Gaither TW, Awad MA, Osterberg EC, et al. Postoperative Complications following Primary Penile Inversion Vaginoplasty
among 330 Male-to-Female Transgender Patients. J Urol. 2018;199(3):760-765.
Gray ML and Courey MS. Transgender voice and communication. Otolaryngol Clin North Am. 2019 Aug;52(4):713-722.
Hayes, Inc. Evolving Evidence Review. Combination facial feminization surgery in patients with gender dysphoria. Hayes,
Inc.; May 5, 2023a.
Hayes, Inc. Evolving Evidence Review. Feminizing voice and communication therapy for gender dysphoria. Hayes, Inc.;
September 6, 2022a.
Hayes, Inc. Evolving Evidence Review. Female-to-Male gender-affirming surgical procedures for adolescents with gender
dysphoria. Hayes, Inc.; May 23, 2023b.
Hayes, Inc. Evolving Evidence Review. Gender-affirming hair removal for patients with gender dysphoria. Hayes, Inc.;
June 15, 2023c.
Hayes, Inc. Evolving Evidence Review. Male-to-Female gender-affirming surgical procedures for adolescents with gender
dysphoria. Hayes, Inc.; May 12, 2023d.
Hayes, Inc. Evolving Evidence Review. Masculinizing voice and communication therapy for gender dysphoria. Hayes,
Inc.; September 8, 2022b.
Hayes, Inc. Evolving Evidence Review. Wendler glottoplasty surgery for voice feminization in patients with gender
dysphoria. Hayes, Inc.; February 9, 2023e.
Hayes, Inc. Hayes Directory Report. Sex reassignment surgery for the treatment of gender dysphoria. Hayes, Inc.; August
2018; updated July 2022.
Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent
Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017 Nov 1;102(11):3869-3903.
https://academic.oup.com/jcem/article/102/11/3869/4157558. Accessed August 6, 2023.
Horbach SE, Bouman MB, Smit JM, et al. Outcome of vaginoplasty in male-to-female transgenders: a systematic review
of surgical techniques. J Sex Med. 2015 Jun;12(6):1499-512.
Mahfouda S, Moore JK, Siafarikas A, Hewitt T, Ganti U, Lin A, Zepf FD. Gender-affirming hormones and surgery in
transgender children and adolescents. Lancet Diabetes Endocrinol. 2019 Jun;7(6):484-498.
Manrique OJ, Adabi K, Martinez-Jorge J, et al. Complications and Patient-Reported Outcomes in Male-to-Female
Vaginoplasty -Where We Are Today: A Systematic Review and Meta-Analysis. Ann Plast Surg. 2018 Jun;80(6):684-691.
Morrison SD, Vyas KS, Motakef S, et al. Facial feminization: systematic review of the literature. Plast Reconstr Surg. 2016
Jun;137(6):1759-70.
Murad MH, Elamin MB, Garcia MZ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis
of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
Nondiscrimination in Health Programs and Activities, 81 Fed. Reg. 31376 (May 18, 2016) (codified at 45 C.F.R. pt. 92).
Oles N, Darrach H, Landford W, et al. Gender affirming surgery: a comprehensive, systematic review of all peer-reviewed
literature and methods of assessing patient-centered outcomes (part 1: breast/chest, face, and voice). Ann Surg. 2022
Jan 1;275(1):e52-e66.
Gender Dysphoria Treatment
Page 17 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Rafferty J; Committee on Psychosocial Aspects of Child and Family Health; Committee on Adolescence; Section on
Lesbian, Gay, Bisexual and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender
and gender-diverse children and adolescents. Pediatrics. 2018 Oct;142(4):e20182162.
Scandurra C, Mezza F, Maldonato NM, et al. Health of non-binary and genderqueer people: a systematic review. Front
Psychol. 2019 Jun 25;10:1453.
Schwarz K, Cielo CA, Spritzer PM, et al. A speech therapy for transgender women: an updated systematic review and
meta-analysis. Syst Rev. 2023 Jul 23;12(1):128.
Sijben I, Timmermans FW, Lapid O, et al. Long-term follow-up and trends in breast augmentation in 527 transgender
women and nonbinary individuals: a 30-year experience in Amsterdam. J Plast Reconstr Aesthet Surg. 2021
Nov;74(11):3158-3167.
Siringo NV, Berman ZP, Boczar D, et al. Techniques and trends of facial feminization surgery: A systematic review and
representative case report. Ann Plast Surg. 2022 Jun 1;88(6):704-711.
Sutcliffe PA, Dixon S, Akehurst RL, et al. Evaluation of surgical procedures for sex reassignment: a systematic review. J
Plast Reconstr Aesthet Surg. 2009 Mar;62(3):294-306; discussion 306-8.
Van Damme S, Cosyns M, Deman S, et al. The effectiveness of pitch-raising surgery in male-to-female transsexuals: a
systematic review. J Voice. 2017 Mar;31(2):244.e1-244.e5.
Wang AMQ, Tsang V, Mankowski P, et al. Outcomes following gender affirming phalloplasty: A systematic review and
meta-analysis. Sex Med Rev. 2022 Oct;10(4):499-512.
Wernick JA, Busa S, Matouk K, et al. A systematic review of the psychological benefits of gender-affirming surgery. Urol
Clin North Am. 2019 Nov;46(4):475-486.
Zhang WR, Garrett GL, Arron ST, Garcia MM. Laser hair removal for genital gender affirming surgery. Transl Androl Urol.
2016 Jun;5(3):381-7.
Policy History/Revision Information
Date
Summary of Changes
07/01/2024
Application
New Mexico
Added language to indicate this policy does not apply to the state of New Mexico; refer to the
state-specific policy version
05/01/2024
Related Policies
Added reference link to the Medical Policy titled:
o Breast Reconstruction
o Breast Reduction Surgery
Coverage Rationale
Added language to indicate gender affirming surgery is considered an irreversible intervention;
although infrequent, reversal of prior gender affirming surgery may be covered when the
medical necessity criteria for the requested treatment are met
Breast Surgery
Revised list of criteria that must be met and documented in the written clinical assessment:
o Replaced criterion requiring “[the individual] must be 18 years of age” with “[the individual]
must be 18 years of age for breast augmentation”
o Added language to indicate individuals must be at least 18 years of age for mastectomy or
breast reduction; however, individuals within one calendar year of turning 18 can be
considered on a case-by-case basis
Medically Necessary and Covered as a Proven Benefit
Revised list of procedures and/or therapies that are medically necessary and covered as a
proven benefit; replaced “voice lessons and/or voice therapy” with “voice lessons and/or voice
therapy (with or without surgery)”
Benefit Considerations
Coverage Information
Replaced language indicating “all plans may not cover all of the listed surgical treatments” with
“certain plans may not cover all of the listed surgical treatments in the Coverage Rationale
section [of the policy]; refer to the federal, state, or contractual requirements for details”
Gender Dysphoria Treatment
Page 18 of 18
UnitedHealthcare Community Plan Medical Policy
Effective 05/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Instructions for Use
This Medical Policy provides assistance in interpreting UnitedHealthcare standard benefit plans. When deciding coverage,
the federal, state or contractual requirements for benefit plan coverage must be referenced as the terms of the federal,
state or contractual requirements for benefit plan coverage may differ from the standard benefit plan. In the event of a
conflict, the federal, state or contractual requirements for benefit plan coverage govern. Before using this policy, please
check the federal, state or contractual requirements for benefit plan coverage. UnitedHealthcare reserves the right to
modify its Policies and Guidelines as necessary. This Medical Policy is provided for informational purposes. It does not
constitute medical advice.
UnitedHealthcare may also use tools developed by third parties, such as the InterQual
®
criteria, to assist us in
administering health benefits. The UnitedHealthcare Medical Policies are intended to be used in connection with the
independent professional medical judgment of a qualified health care provider and do not constitute the practice of
medicine or medical advice.
Date
Summary of Changes
Limitations and Exclusions
Revised list of examples of non-covered treatments and services:
o Added “treatments and procedures that are specifically excluded or otherwise do not meet
the requirements of a covered health care service in the federal, state, or contractual
requirements”
o Removed “reversal of genital surgery or reversal of surgery to revise secondary sex
characteristics”
Supporting Information
Updated Clinical Evidence and References sections to reflect the most current information
Archived previous policy version CS145.N
