
I
n 2010 Congress enacted the Affordable Care Act, a historic and vigorously debated law designed
to dramatically overhaul the health system. Included in the Affordable Care Act are comprehensive
prevention provisions consistent with those called for by the American Public Health Association
(APHA) in its health reform agenda and supported by other leading experts in population health
and prevention.
12
The Affordable Care Act, if it is adequately funded, effectively implemented, and creatively
leveraged through public and private-sector partnerships, will mark the turning point in the fundamental
nature of our health system, initiating the transformation of our health system from one that treats sickness
to one that promotes health and wellness. This issue brief begins (Section III) by summarizing the state of
public health in the United States, including some measures of the growth of preventable diseases. Section
IV describes the major provisions of the Affordable Care Act that address prevention through: (1) investing
in public health; (2) educating the public; (3) expanding insurance coverage and requiring that health insur-
ance include recommended preventive benefits; and (4) building capacity for better prevention in the future
through demonstrations, research and evaluation.
American Public Health Association
OCTOBER 2010
Prevention Provisions
in the Affordable
Care Act
Gail Shearer, MPP
800 I Street, NW • Washington, DC 20001-3710 • 202-777-APHA • fax: 202-777-2534 • www.apha.org
Executive Summary
2
Section V identifies key implementation
issues. Federal, state and local policy makers
charged with implementing the Affordable
Care Act face challenging issues in the near
future such as: (1) deciding how to allocate
new prevention funds and protect exist-
ing funds; (2) allocating grants (federal) and
applying for grants (state and local) so that
prevention efforts are coordinated effi-
ciently; (3) learning the best ways to ensure
the accessibility of available information
about the benefits of prevention to both the
general population and hard-to-reach popu-
lations; and (4) learning how best to com-
municate with consumers and patients so
that they act on that information to prevent
disease and disability and improve health.
Successful implementation of the preven-
tion provisions of the Affordable Care Act
will require the devoted efforts of staff at all
levels of government, of all members of the
healthcare and public health professional
workforce, and of health plans and insurance
companies. It also will demand the engage-
ment of citizens, who will need to be more
educated about choices in the health system.
Section VI includes recommendations for
policymakers to: (1) leverage health reform
funding and other existing funding to ex-
pand total funds for prevention and maxi-
mize progress; (2) conduct research about
how to communicate prevention messages
most effectively to traditionally under-
served populations; and (3) improve public
health by making comparative effectiveness
research on prevention a priority and by ex-
panding successful prevention pilot projects.
This issue brief does not cover workforce
issues such as the expansion of primary care
and community health centers. These im-
portant areas will be addressed in a separate
forthcoming issue brief.
I. Introduction and
Overview
[Health reform’s] aim is to transform
America’s current sick care system into
a genuine health care system, one that is
focused on keeping us healthy and out of
the hospital in the first place.—Senator Tom
Harkin
3
Senator Harkin, a long-time leader on
preventive health care, captures in his quote
the hope that the landmark health reform
legislation enacted in 2010 will make
fundamental changes in our system so that
it prevents disease and promotes wellness.
The Affordable Care Act, signed into law on
March 23, 2010
4
, included comprehensive
initiatives that elevate the nation’s commit-
ment to preventing disease and promoting
wellness. Its provisions cut across a range of
needs that have been articulated by ex-
perts.
5
These include the establishment of a
large Prevention and Public Health Fund,
creation of a National Prevention, Health
Promotion and Public Health Council to
coordinate federal prevention initiatives,
development of new grant programs to
fund state and local initiatives at the com-
munity level, a new requirement that health
insurance policies cover recommended
preventive services, and development and
implementation of a goal-driven strategy
for prevention that will include a timeline
for measurable actions. The law also requires
that changes to insurance coverage and poli-
cy must be guided by scientific evidence,
and calls for evaluations and reports that
provide an opportunity to learn from expe-
rience and make improvements over time.
The American Public Health Association
(APHA) and the public health community
have long supported health reform that ex-
pands health insurance coverage to the mil-
lions of uninsured Americans and provides
The American Public Health Association (APHA) and the public health community have long supported
health reform that expands health insurance coverage to the millions of uninsured Americans and provides
access to care for all residents. APHA also has supported the creation of a dedicated funding stream for
prevention, wellness and public health.
6
H
ealth reform’s aim
is to transform
America’s current
sick care system into a genu-
ine health care system, one
that is focused on keeping us
healthy and out of the hospital
in the first place.
—Senator Tom Harkin
3
3
access to care for all residents. APHA also
has supported the creation of a dedicated
funding stream for prevention, wellness
and public health.
6
APHA’s 2009 Agenda
for Health Reform describes the population-
based services needed to help communities
and individuals be healthy.
4
A number of
organizations and coalitions that promote
improved public health have taken similar
positions.
7
The Affordable Care Act addresses many
of these recommendations from the public
health community and represents a bold
step for the nation in creating a system that
promotes wellness.
This issue brief addresses the provisions in
health reform that directly relate to preven-
tion. It does not deal with the many indirect
ways that health reform promotes health
and prevents disease, most notably by reduc-
ing the ranks of the uninsured who have
faced financial and access barriers to both
acute and preventive care. Nor does it cover
workforce issues, such as those related to the
expansion of primary care, the public health
workforce, medical homes, and community
health centers, all of which will play a cru-
cial role in supporting the transformation of
our health care culture to one that embraces
prevention.
At this time, there is ambiguity in the
law about the extent to which funds are
authorized and/or appropriated, creating
uncertainty about the precise amounts of
funding that will actually be available. The
law often uses language such as “there are
authorized to be appropriated such sums as
may be necessary to carry out this section”
(Section 4004), and “out of any funds in the
Treasury not otherwise appropriated, there
are appropriated $1,000,000 for fiscal year
2010 to carry out this subsection” (Section
4203). Many sections do not include any
language about funding, creating uncer-
tainty about future funding. The Congres-
sional Budget Office has published a table
of authorizations subject to appropriation
in order to clarify which provisions have
specific dollar amounts authorized (by year)
and which provisions do not yet have a
specified budget.
8
The success of the Afford-
able Care Act’s prevention and public health
initiatives will depend not only on whether
the authorized funds are appropriated, but
also on the ability to achieve changes across
many non-health care aspects of our society
through healthy environments, education, a
more nutritious food supply, and modifica-
tion of individual behaviors.
After a brief overview of the problem
of inadequate focus on prevention in the
past, this issue brief describes the major
prevention provisions in health reform
and identifies some of the key policy and
implementation issues that lie ahead. For
an implementation timeline of the public
health, prevention and wellness provisions in
the Affordable Care Act, see Appendix 1.
II. The Problem
Rising rates of preventable disease and
death, as well as international comparisons
of health outcome measures, reveal that
Americans are not as healthy as they could
be, and that they are becoming increasingly
unhealthy over time. The relatively un-
healthy population stems from many factors,
including but not limited to the health sys-
tem. Lack of access to a high-quality educa-
tion, nutritious food, adequate exercise,
and a healthy and safe environment are key
factors driving the diminishing health of the
T
he Affordable Care Act addresses recommendations from the public
health community and represents a bold step for the nation in creat-
ing a system that promotes wellness.
4
nation. In the absence of other changes, even
a complete transformation of the health sys-
tem is not sufficient to significantly alter the
growing problems of heart disease, obesity
and cancers that affect our nation’s health.
Preventable disease and death: Prevent-
able disease and death impose a large burden
in the United States. In 2009, an alarming
26.6 percent of the U.S. population was
obese,
9
8.2 percent of the adult U.S. popu-
lation had diabetes,
10
and 27.8 percent of
the adult population had high blood pres-
sure.
11
Lifestyle behaviors and choices, such
as tobacco use, poor diet, physical inactivity,
and alcohol consumption are primary deter-
minants of disease and death in the United
States, yet these have historically received
little attention from our health system with
respect to preventing them in the first place.
This lack of attention has resulted in an
estimated 60 percent of deaths in America
being attributed to “social or behavioral cir-
cumstances.”
12
In many cases, the unhealthy
choices that lead to poor health outcomes
are not in fact lifestyle “choices,” but rather
the consequences of economic and geo-
graphic factors that restrict or prevent access
to healthy food and safe environments in
which to exercise.
Research has shown that coronary artery
disease can be reversed with lifestyle changes
including diet, stress reduction, psychosocial
support and exercise.
13
Recent growth in the
self-reported obesity rate, a 1.1 percentage
point increase (2.4 million additional people)
between 2007 and 2009, is another indica-
tor of the growth of preventable disease
and the need for an aggressive public health
focus.
14
The World Cancer Research Fund
and American Institute for Cancer Research
found that cancers are principally caused by
environmental factors, the most important of
which are tobacco, diet, physical activity and
exposures in the workplace. Two-thirds of all
cancers can be eliminated through changes
to diet, physical activity and tobacco use.
15
It is widely recognized that as a country we
need to take steps to prevent obesity, and that
problems with “the availability of healthy
and affordable food options, eating patterns,
levels of physical activity, quality of the built
environment, social and cultural attitudes
around body weight, and reduced access to
primary care” all contribute to the preva-
lence of obesity.
16
International comparisons of health:
The United States lags far behind other
countries in key health measures, yet we
manage to spend far more per capita each
year on health care than other countries,
$7,680 per person, for a national total of
$2.3 trillion in 2008.
17
Male life expectancy
(at birth) in the United States in 2006 was
75, compared with 79 in Australia, 77 in
Austria, and 79 in Japan.
18
“Healthy life ex-
pectancy,” a measure of the number of years
a newborn can be expected to live a produc-
tive and healthy life, is 70 years in the United
The World Cancer Research Fund and American Institute for Cancer Research found that cancers are
principally caused by environmental factors, the most important of which are tobacco, diet, physical
activity and exposures in the workplace. Two-thirds of all cancers can be eliminated through changes to
diet, physical activity and tobacco use.
16
R
esearch has shown that coronary artery disease can be reversed
with lifestyle changes including diet, stress reduction, psychosocial
support and exercise.
13

5
States, less favorable than 30 other countries
such as the United Kingdom, Spain, and
Japan, which has the highest life expectancy
of 76.
19
Infant mortality in the United States
was seven per 1,000 live births in 2009, with
36 countries (out of 193 rated) having lower
infant mortality rates.
20
A Commonwealth
Fund international comparison of health
systems placed the United States as worst in
an analysis that considered measures such as
quality, access, efficiency, equity and cost.
21
Health System Failures: Primary Care
Shortages. A central challenge to the health
system is the short supply of primary care
providers and public health professionals, and
their maldistribution across the nation. Sev-
enty percent of health leaders surveyed by
the Commonwealth Fund said that address-
ing the shortage of trained health care work-
ers was an essential, urgent part of health
reform.
22
The Institute of Medicine has
documented how demands for the health-
care workforce will grow because of the
aging of the Baby Boomers.
23
The current
shortage of primary care providers, especially
in rural areas, before Baby Boomers turn 65
and before the enactment of the Affordable
Care Act, undoubtedly means that short-
ages will intensify over the coming years
as Boomers need more health services, and
implementation of the law removes financial
barriers to seeking health care. Additionally,
the recession, the high unemployment rate,
and continued financial pressures has led to a
long-lasting crisis affecting state budgets, and
resulted in severe cuts in the workforce that
provides basic health, public health and other
services at the state and local levels.
Health System Failures: Financial Incen-
tives. Another factor contributing to the
declining population health is the health care
financing system, which is largely fee-for-
service. The U.S. health system is riddled
with financial incentives to provide medical
care to treat disease (e.g., coronary bypass
and bariatric surgery) rather than offer
primary care and guidance to address health
through basic lifestyle changes before the
disease process begins.
Focus on Children as a Proxy. The health
of the nation’s children best exemplifies our
lack of attention to prevention. The follow-
ing measures indicate how poorly our nation
is doing with respect to raising healthy
children.
Only 70 percent of pregnant women have
access to adequate prenatal care.
24
Seventy-eight percent of children be-
tween the age of 19 months and 35
months received complete immuniza-
tions in 2009 (a 42 percent increase in 10
years).
25
In 2007-2008, 19 percent of children six
to 17 years old were obese.
26
Nine percent of children have asthma,
with 400,000 of these having mild to se-
vere asthma.
27
In 2008, 25 percent of 12th graders re-
ported having five or more alcoholic bev-
erages in a row in the last two weeks.
28
An estimated 17 percent of children have
“some type of developmental disorder,”
and 21 percent have a “diagnosable mental
or addictive disorder”;
29
About 1.2 million children drop out of
high school every year, with only 70 per-
cent of freshmen ultimately graduating
from high school.
30
The Surgeon General reported a suicide
incidence of 9.5 per 100,000 for 15- to
19- year-olds in 1996.
31
There is increasing awareness that early
environmental factors before birth and in
early childhood influence health over the
long term. These disturbing measures of
the health status of children are troubling
harbingers of health status of the population
of the future.
Making the Case for Prevention: Another
way to consider the value of prevention is
to examine the “return on investment” for
prevention dollars. A report by Trust for
America’s Health estimated that investments
in community-based programs in initiatives
that encourage physical activity, good nutri-
tion and tobacco cessation can yield very
favorable returns on investment, returning an
overall $5.60 in health cost savings for every
$1 spent.
32
Health outcomes reflect the physical,
social, and demographic environments and
communities in which people live, work,
play, learn, pray and seek healthcare. Each
plays a critical role in determining the health
A
Commonwealth
Fund international
comparison of health
systems placed the United
States as worst in an analysis
that considered measures such
as quality, access, efficiency,
equity and cost.
22
6
of a population. Healthy People
33
creates a
roadmap for achieving population health
goals through interventions in a variety of
non-health and health arenas. Achieving
the goal of reducing childhood obesity, for
example, will require changes outside the
health system, such as removing junk food
from schools and taxing sodas. The Commis-
sion to Build a Healthier America, convened
by the Robert Wood Johnson Founda-
tion, recently concluded that achieving the
goal of a healthy nation will require broad
changes “in every aspect of society and daily
life.” The Commission recommendations
focused on improving early childhood health
and development, encouraging good nutri-
tion and promoting healthy communities.
34
APHA’s work to improve the health of the
nation supports changes in the workplace, in
schools and in the environment, in addition
to changes in the health system. For example,
APHA has outlined five general goals and 27
specific goals across non-health and health
sectors to reduce childhood obesity. The Pre-
vention Institute has documented the impact
of community violence on healthy eating
and activity.
35
Each of these efforts supports the intent of
addressing poor health outcomes by reaching
beyond the traditional “health care system”
of doctors, nurses and hospitals; instead, they
involve coaching (from parents and educa-
tors) about a range of things including nutri-
tion, exercise, activities; and systemic changes
to our environments.
III. Preventive Health
Provisions in the
Affordable Care Act
The Affordable Care Act addresses poor
health outcomes in a number of ways, such
as improving access to care, making care
and coverage more affordable, encouraging
preventive care, and increasing the supply of
primary care providers. Congress recognized
the need to address population health com-
prehensively, both within the health system
and through initiatives that extend to other
sectors, such as the school system.
The Affordable Care Act includes a broad
range of initiatives designed to promote
wellness and prevent disease. The prevention
provisions in the Affordable Care Act require
large implementation roles for federal, state
and local governments and the private sector.
While phased in over time, implementation
timelines are tight. Many involve multiple
divisions within the U.S. Department of
Health and Human Services. Stakeholders in
the health care system—patients, consumers,
doctors, nurses, insurance companies, hospi-
tals, employers, and government employees
at the federal, state and local levels—will
all face major changes in how they interact
with the health system. For example, the
Affordable Care Act provides grants to state
and local health departments to educate
targeted populations, build the public health
infrastructure, prevent chronic disease, and
foster healthy and safe communities through
policy, systems, and environmental changes.
A second category of initiatives—public
education campaigns—are designed to pro-
mote healthy behaviors (e.g., good nutrition,
adequate exercise) and discourage unhealthy
behaviors (e.g., tobacco use). A third cat-
egory tests new approaches to improving
health, evaluates the effectiveness of these
approaches, and expands successful efforts
over time to promote healthy behavior and
healthy outcomes. Finally, a fourth category
of initiatives involves insurance coverage
requirements that are designed to assure that
various populations (e.g., Medicare benefi-
ciaries, people with private insurance cover-
age) do not face financial barriers to access-
ing evidence-based preventive care such as
cancer screenings.
In this issue brief the provisions of the
Affordable Care Act are grouped into four
categories:
investing in public health through grant
programs, contracts, support and infra-
structure that will develop a national
prevention, health promotion and pub-
lic health strategy, and coordinate federal
programs;
educating the public through educational
campaigns aimed at improving health;
learning from experience through re-
search and demonstrations; and
requiring that evidence-based preventive
health care services be covered in both
T
he Affordable Care
Act addresses this
fragmentation and
lack of coordination through
two initiatives: (1) the National
Prevention, Health Promotion
and Public Health Council,
which will coordinate and
execute a comprehensive
strategy; and (2) the Preven-
tion and Public Health Fund,
which will invest in prevention
and public health programs
to improve health and restrain
health costs.
7
public and private health coverage, with-
out cost-sharing.
A. Investments In PublIc HeAltH
The United States dedicates a mere 3
percent of its healthcare budget to disease
prevention and public health.
36
These funds
are administered across multiple federal, state
and local agencies, with no loci of coordina-
tion and review.
The Affordable Care Act addresses this
fragmentation and lack of coordination
through two initiatives: (1) the National
Prevention, Health Promotion and Public
Health Council, which will coordinate and
execute a comprehensive strategy; and (2)
the Prevention and Public Health Fund,
which will invest in prevention and pub-
lic health programs to improve health and
restrain health costs.
National Prevention, Health Promotion
and Public Health Council
38
(Section 4001,
10401): The law creates a new Council,
within HHS, to coordinate and lead the
federal government’s efforts on prevention,
wellness and health promotion, and estab-
lishes a locus of control, multi-sector coor-
dination, and accountability for advancing a
national prevention agenda. The Council is
to be chaired by the U.S. Surgeon General
and will consist of Secretaries of appropri-
ate federal departments (e.g., Health and
Human Services, Agriculture, Education,
Homeland Security, Transportation, Labor),
the Chairman of the Federal Trade Com-
mission, the Director of the Domestic Policy
Council, several other senior administration
appointees, and other members as deter-
mined appropriate.
38
The Council is charged
with making policy recommendations to the
President and Congress to advance public
health goals. It is to consider and propose
“evidence-based models, policies, and in-
novative approaches for the promotion of
transformative models of prevention, integra-
tive health, and public health on individual
and community levels across the United
States.”
A key function of the Chairperson (in
consultation with the Council) is to “de-
velop and make public a national prevention,
health promotion, public health strategy,”
within one year of enactment. The strategy
must articulate specific goals and objectives
for improving the health status of Ameri-
cans through federal health promotion and
prevention programs. It is to include “spe-
cific and measurable actions and timelines”
to implement the strategy. An annual report
to the President and relevant committees
of Congress will provide a forum for the
Council to describe activities on preven-
tion, health promotion and public health,
report on progress in meeting the goals of
Healthy People 2020, and report on the status
of federal coordination of programs. The
first report was issued on July 1, 2010. (See
Section V.)
Prevention and Public Health Fund (Sec-
tions 4002, 10401): While the National
Prevention, Health Promotion and Public
Health Council provides a mechanism to
coordinate federal programs, the new Pre-
vention and Public Health Fund provides
the resources to fund prevention and public
health initiatives. The Fund is intended “to
provide for expanded and sustained national
investment in prevention and public health
programs to improve health and help restrain
the rate of growth in private and public
health care costs.” The law provides $500
million for the Fund in FY2010, and annual
A
ffordable Care Act provides grants to state and local health depart-
ments to educate targeted populations, build the public health
infrastructure, prevent chronic disease, and foster healthy and safe
communities through policy, systems, and environmental changes.
8
Table 1: Grant Programs to Promote Prevention
41
School-based Health Centers (Section 4101)
The Secretary of HHS will establish a grant program “to support the operation of school-based Health Centers”
grants for schools, preference to those with large number of children eligible for Medicaid
funds to support facilities and equipment, not to support personnel or pay for health services
Secretary is to develop evaluation plan and monitor quality performance of grants
appropriates $50 million per year for FY2010 to FY2013
Incentives for Prevention of Chronic Disease in Medicaid (Section 4108)
The Secretary of the Department of Health and Human Services (HHS) will award grants to states to carry out comprehensive, evidence-based, accessible programs
to lower health risks of Medicaid beneficiaries
funds can be used, for example, for programs to cease use of tobacco products, control or reduce weight, lower cholesterol, lower blood pressure, avoid
onset of diabetes
requires various reports from states receiving grants, independent evaluation of initiatives, reports from Secretary to Congress
appropriates $100,000,000 for the five-year period beginning January 1, 2011
Community Transformation Grants (Section 4201)*
The Secretary of HHS, through the Director of the Centers for Disease Control and Prevention (CDC), to award grants “for the implementation, evaluation, and
dissemination of evidence-based community preventive health activities in order to reduce chronic disease rates, prevent the development of secondary conditions,
address health disparities, and develop a stronger evidence-base of effective prevention programming”
competitive grants to state and local governmental agencies, community-based organizations, non-profit organizations, and Indian tribes for implementation,
evaluation and dissemination of evidence-based community preventive health care activities
grant recipients to provide detailed plan for the policy, environmental, programmatic and (as appropriate) infrastructure changes needed to promote healthy
living and reduce disparities
activities could include: creating healthier school environments, creating infrastructure to support active living, access to nutritious food, and tobacco
cessation
grant recipients are to evaluate impact by measuring the changes in prevalence of chronic disease risk factors of community members participating in
preventive health activities
grantees will meet at least annually to discuss challenges, best practices, and lessons learned
does not specify an amount to be appropriated (authorizes “sums as may be necessary”)
Health Aging, Living Well (Section 4202)
42
*
Secretary of HHS (through the Director of the CDC) will award grants to states, local health departments and Indian tribes:
to carry out 5-year pilot programs to provide public health community interventions, screenings, and where necessary clinical referrals for individuals who
are between 55 and 64;
interventions include efforts to improve nutrition, increase physical activity, reduce tobacco use and substance abuse, improve mental health, and promote
healthy lifestyle
grant applicants to design a strategy to improve the health of individuals between ages 55 and 64 through community-based public health interventions;
does not specific an amount to be appropriated (authorizes “sums as may be necessary”)
Epidemiology and Laboratory Capacity Grant Program (Section 4304)*
The Secretary of HHS (through the CDC Director) to establish a grant program to provide:
grants to state health departments, local health departments, tribal jurisdictions, and academic centers
funding for assisting public health agencies in improving surveillance for, and response to, infectious diseases and other important public health conditions
authorizes $190,000,000 for each year between FY2010 and FY2013
Maternal, Infant and Early Childhood Home Visiting Programs (Section 2951)
The Secretary of HHS will award grants to states, Indian tribes, and (in certain circumstances) non-profit organizations:
to fund early childhood home visitation programs;
each grantee is to measure benchmarks including maternal and newborn health, prevention of child injuries, improvement in school readiness, reduction
in crime or domestic violence;
Appropriates $100 million in FY2010, increasing steadily until FY2014 when appropriations are $400,000.
*Funds have not been appropriated for these grant programs, and they will not be implemented in the absence of future appropriations.
9
T
he prevalence of
largely preventable
diseases such as
heart disease, cancer and
diabetes has increased in
the United States. Congress
recognized the potential to
improve population health by
addressing these preventable
diseases through broad-based
public education campaigns,
and included them as a corner-
stone of reform.
authorizations increase, with total authoriza-
tions of $15 billion for FY2010 to FY2019.
The Fund is administered by the Secretary
of the Department of Health and Human
Services (HHS).
Table 1 summarizes the five major preven-
tion programs to be funded by the health
reform law, to be administered by the Secre-
tary of the HHS. The programs include:
support for the operation and expansion
of school-based health centers;
state programs to help lower health risks
of Medicaid beneficiaries;
state, local, and other organization proj-
ects to fund implementation, evaluation
and dissemination of preventive health
activities through enhancing infrastructure
and capacity (community transformation
grants);
state, local and Indian tribe pilot programs
to provide public health community in-
terventions for individuals between ages
55 and 64 (e.g., increasing physical activity
of 64-year-olds);
grants to state, local and tribal health
departments and academic centers to in-
crease surveillance and response to emerg-
ing public health issues, including infec-
tious disease (epidemiology and laboratory
capacity grant program); and
grants to state and tribal organizations, and
under certain circumstances non-profit
organizations, to provide early childhood
home visitation programs, with a require-
ment that at least 75% of the funding be
used for programs using evidence-based
models.
Each of these grant programs provides
an opportunity to address health disparities
that result in disproportionate adverse health
conditions for specific groups in the United
States.
39
The health reform law also provides
support at a more modest funding level
for important but smaller-scale preventive
programs. It provides for technical assis-
tance, through the Director of the Centers
for Disease Control and Prevention, for
employer-based wellness programs (Sec-
tion 4303). For example, it provides tools
for measuring participation in workplace
wellness programs, methods for increasing
participation, and assistance for determining
the impact on participants’ health status.
41
The Act authorizes $500 million to fund the
public education campaigns of the Secretary
(described below in the next section). It au-
thorizes the Secretary of HHS to negotiate
contracts with manufacturers for vaccines,
and supports a demonstration program to
improve immunization coverage and grants
to states to increase rates for recommended
immunizations for children, adolescents and
adults (Section 4204).
b. PublIc educAtIon cAmPAIgns
As described above (Section II), the
prevalence of largely preventable diseases
such as heart disease, cancer and diabetes
has increased in the United States. Congress
recognized the potential to improve popula-
tion health by addressing these preventable
diseases through broad-based public edu-
cation campaigns, and included them as a
cornerstone of reform. The Act establishes
a well-funded “education and outreach
campaign” on preventive services that will
be included in health coverage for most
people. The public education campaigns aim
to dramatically alter behaviors that result in
60 percent of deaths attributed to “social or
behavioral circumstances” as described in the
Problem section above.
43
The Secretary of HHS is charged with
planning and implementing a national
public-private partnership that will focus on
educating the nation’s diverse population
about disease prevention and health promo-
tion. The campaign will provide information
about the importance of using evidence-
Restaurants will be required to include the nutrient content and the number of calories in food selections
on their menus, and must make additional nutritional information available upon request. In addition,
vending machine operators who own more than 20 machines are required to post signs disclosing the
number of calories in each item sold

10
based preventive services “to promote well-
ness, reduce health disparities and mitigate
chronic disease.”
44
The campaign may use
TV, radio, a Web site, and other venues to
address lifestyle choice related to appropri-
ate and adequate nutrition, exercise, tobacco
cessation and obesity reduction. The five
leading disease killers in the United States
(heart disease, cancer, stroke, respiratory
disease and Alzheimer’s disease in 2007) will
also be targeted in a public education cam-
paign, and will include an educational Web
site that includes information for health care
providers and for consumers.
A second public education campaign is to
be carried out by a non-traditional source
of health information: restaurants that are
part of a chain with 20 or more locations.
Restaurants will be required to include the
nutrient content and the number of calories
in food selections on their menus, and must
make additional nutritional information
available upon request. In addition, vending
machine operators who own more than 20
machines are required to post signs disclos-
ing the number of calories in each item sold.
The third education initiative establishes a
five-year, national public educational cam-
paign on oral health care and the prevention
of oral disease. This campaign will target
activities to children, pregnant women, the
elderly, individuals with disabilities, and
ethnic and racial minority populations. It
will convey oral health prevention messages,
including education about the importance
of community water fluoridation and dental
sealants to encourage broader provision and
use of routine dental services. This campaign
is authorized, and will be implemented only
if funds are appropriated. Section 1302 of the
Affordable Care Act specifies that oral health
services are to be included in the basic ben-
efits for children (but not adults).
c. coverIng recommended
PreventIve servIces As A HeAltH
benefIt
There are several reasons that preventive
services have not been included in health
insurance policies until recently. The relative
predictability of the cost of recommended
preventive services makes them different
(from an insurance perspective) from low-
probability illnesses and injuries that health
insurance was initially designed to cover.
Health insurance was originally designed to
be more “catastrophic” rather than “first-
dollar coverage”. Insurers would argue
that including preventive benefits simply
increased premiums to cover the expected
cost of the benefits. Additionally, health plans
and employers have little incentive to cover
preventive services that are more likely to
have an impact on a member’s or employee’s
long-term health and well-being, because
the employee might have left the employer
by the time the preventive services pay off.
However, increased employer and con-
sumer demand for coverage of services
which prevent disease and disability over the
long term, in conjunction with the evidence
of value and effectiveness, led to the change
in insurance coverage in recent years. The
scientific understanding of which preventive
services are appropriate at different stages
of life increased, with the help of the U.S.
Preventive Services Task Force. Insurers have
responded to employers’ and consumers’ de-
mand for coverage of preventive services in
otherwise high deductible health insurance
policies: 92 percent of high deductible plans
offered by employers included preventive
care without any deductible in 2009.
45
A
PHA recommended first-dollar coverage for evidence-based
clinical preventive services in its Agenda for Health Reform.47 And
in fact, the new health reform law requires that health benefits in-
clude selected preventive services with no cost-sharing both for individual and
group plans and for Medicare.
11
At the same time, there is growing aware-
ness that cost-sharing (e.g., co-payments,
deductibles) presents a financial barrier that
deters people from getting the screenings
and preventive services that are recommend-
ed for them. The continuing recession has
resulted in cutting back on routine care such
as preventive services, most likely because
of the large out-of-pocket costs involved.
46
While most employer plans include preven-
tive care without cost-sharing, individual
policies (under competitive pressure to keep
premiums low) are unlikely to do so in the
absence of a legal requirement.
Recognizing the importance of elimi-
nating financial barriers to receiving
evidence-based preventive services, APHA
recommended first-dollar coverage for
evidence-based clinical preventive services
in its Agenda for Health Reform.
47
And in
fact, the new health reform law requires
that health benefits include selected preven-
tive services with no cost-sharing both for
individual and group plans and for Medicare.
These new benefits will be required by late
2010 (six months after enactment) for indi-
viduals with new private coverage, and by
January 1, 2011, for Medicare beneficiaries.
States are encouraged to extend preventive
health services in their Medicaid programs,
paid for in large part by increased federal
payments for Medicaid.
The U.S. Preventive Services Task Force,
an independent panel of experts in primary
care and prevention, is based at the Agency
for Healthcare Research and Quality. Its rec-
ommendations provide the basis for preven-
tive services coverage. Specific recommenda-
tions vary by age and other factors, and the
U.S. Preventive Services Task Force recom-
mends that clinicians discuss the recom-
mended preventive services with patients as
appropriate. Examples of the services recom-
mended for adult women include screening
for breast cancer, cervical cancer, colorectal
cancer, depression, high blood pressure and
obesity.
48
Private plans: For private plans, cover-
age will be required in new plans for all
evidence-based preventive services that are
rated “A” or “B” by the U.S. Preventive
Services Task Force (Section 1001). Cost-
Table 2: Preventive Care and Public Health Research Projects
53
Individualized Wellness Plans (Sec. 4206)
Goal: Test impact of providing at-risk populations an individualized wellness plan designed to reduce risk of preventable conditions. Wellness plans would
include plans for nutritional counseling, physical activity, alcohol and tobacco cessation counseling, stress management.
Target population: At-risk individuals who use community health centers.
Implementation: Secretary of HHS to identify 10 community health centers to conduct evaluation.
Delivery of Public Health Services (Sec. 4301)
Goal: Evaluate (and report to Congress) the effectiveness of evidence-based practices relating to prevention and community-based public health interventions,
and identify effective strategies for state and local systems to organize, finance and deliver public health services.
Target population: Communities and populations that would benefit from prevention priorities identified by the National Prevention Strategy and Health
People 2020.
Implementation: The Secretary of HHS, working with the CDC, Community Preventive Services Task Force, and various private and public partners, will analyze
and report annually to Congress.
Evaluation of Community-based Prevention and Wellness Programs (Sec. 4202)
Goal: Evaluate the ability of community health interventions to improve the health of people nearing Medicare eligibility and the effectiveness of community-based
prevention and wellness programs for Medicare beneficiaries.
Target Population: People nearing Medicare eligibility (55 to 64 years old) and Medicare beneficiaries.
Implementation: The Secretary of HHS, working with the CDC and the Administration on Aging, will provide grants for the pilot study of people nearing
Medicare eligibility. The Secretary of HHS will evaluate the programs for Medicare beneficiaries.
12
sharing (i.e., deductibles and co-payments)
is explicitly prohibited. Similarly, immuniza-
tions that are recommended by the Advisory
Committee on Immunization Practices and
“evidence-informed preventive care and
screenings” for infants, children and adoles-
cents, and breast cancer screening mammog-
raphy are covered (Section 1001).
Medicare: Cost-sharing will be elimi-
nated for Medicare beneficiaries for preven-
tive services (including colorectal cancer
screening) that are rated “A” or “B” by the
Task Force.
49
Medicare beneficiaries will be
covered for an annual wellness visit. Before
the visit, beneficiaries will receive support to
help them complete a health risk assessment.
Each beneficiary will be provided with a
personalized prevention plan that includes a
health risk assessment, the establishment or
update of an individual medical and fam-
ily history, personalized health advice, and,
when appropriate, referral to health educa-
tion or preventive counseling services. Even
if recommended, health education services
are generally not covered by Medicare, with
the exception of medical nutrition therapy
for people with diabetes or kidney disease,
and diabetes education for those with diabe-
tes; outpatient mental health counseling will
continue to be covered with a 45 percent
coinsurance rate in 2010–2014.
50
Medicaid: The health reform law encour-
ages, but does not require, states to expand
preventive coverage for Medicaid ben-
eficiaries. It adds preventive services rated
“A” or “B” by the U.S. Preventive Services
Task Force and vaccines recommended by
the Advisory Committee on Immuniza-
tion Practices to the list of services that state
Medicaid programs can cover, and encour-
ages states to do so by increasing the federal
financial contribution (federal medical assis-
tance percentage, or FMAP) by 1 percent for
any states that cover these services without
any cost-sharing (Section 4106). Pregnant
women covered by Medicaid will have cov-
erage for counseling and prescription drugs
for cessation of tobacco use (Section 4107).
d. demonstrAtIon ProgrAms And
reseArcH Projects
The health reform law uses evidence of
effectiveness to make decisions and fund
educational programs. New programs will
be evaluated and adjusted based on effective-
ness evidence. The law includes a number
of research and demonstration programs
designed to improve capacity to promote
prevention and public health in the future.
There are three major prevention-oriented
research projects in the health reform law:
(1) a demonstration project for individual-
ized wellness plans developed for individu-
als at risk of preventable conditions; (2) a
comparative analysis of effectiveness and
cost of public health interventions; and (3)
an analysis of community-based prevention
and wellness programs for the population
nearing Medicare eligibility and for Medi-
care beneficiaries. These three programs are
summarized in Table 2.
In addition, the health reform law has a
number of provisions aimed at improving
the understanding of prevention-related ac-
tivities, in concert with the needs of various
population groups. Other evaluation-orient-
ed provisions of the law include:
1. a requirement that all federal surveys col-
lect data on race, ethnicity, sex, primary
language and disability status (Section
4302);
2. the convening of a conference, through
the Institute of Medicine, that explores
many facets of pain management, includ-
ing how specific races, genders and ages
are affected, and reports to Congress (Sec-
tion 4305);
3. appropriation of funds for a previously
authorized Childhood Obesity Demon-
stration project52 (Section 4306);
4. development of methodologies for esti-
mating the budget impact of prevention
and wellness programs (since benefits of-
ten accrue beyond a 10-year budget win-
dow) by the Congressional Budget Office
(Section 4401);
5. an analysis of the impact of health and
wellness initiatives on the health status
(e.g., absenteeism, productivity) of the
federal workforce (Section 4402);
6. review of the scientific evidence of
effectiveness, appropriateness, and cost-
effectiveness of clinical preventive services
by the U.S. Preventive Services Task Force,
and publication of the findings in the
S
hortages in the
primary care health
workforce, espe-
cially in underserved areas,
will grow more intense as
the number of insured adults
grows. This will require early
and aggressive attention so
that the expanded access to
care does not result in long
waiting lines at doctors’ of-
fices and clinics.

13
Guide to Clinical Preventive Services (Sec-
tion 4003);
523
and
7. review of the effectiveness, appropriate-
ness and cost-effectiveness of community
preventive interventions (including health
impact assessments and population health
modeling) and publication of recommen-
dations in the Guide to Preventive Services
by the independent Community Preven-
tive Services Task Force (Section 4003)
IV. Some Key Issues
Transforming our nation’s health system
to one that promotes health and wellness in
the first place is an iterative process, one that
requires routine assessment, evaluation and
adjustments over time. The scope of prob-
lems addressed by the legislation is ambitious
and broad, and cuts across many sectors of
the economy and across disciplines/sectors.
The ambiguity about authorizations and
appropriations ensures that there will be
scrutiny by Congress with input from many
stakeholders, and that there will be uncer-
tainty on the part of implementing agencies
about precise funding streams. Early imple-
mentation efforts are occurring at a time of
fiscal crisis in virtually all states, making it
especially difficult for state and local gov-
ernments to continue to provide existing
services at the same time that they ramp up
comprehensive health reform implementa-
tion activities. Shortages in the primary care
health workforce, especially in underserved
areas, will grow more intense as the number
of insured adults grows. This will require
early and aggressive attention so that the ex-
panded access to care does not result in long
waiting lines at doctors’ offices and clinics.
There are a number of factors that will
influence the ultimate impact of the preven-
tive provisions. First and foremost is the state
of the economy and pace of the recovery.
This directly influences the ability of state
and local governments to fund a depleted
public health workforce. Without a signifi-
cant improvement, state and local govern-
ments will be able to do little more than
hold steady, perhaps even facing further ero-
sion of their public health infrastructure and
programs. A second key factor is the need for
prevention and public health advocates to
coordinate their efforts in order to maximize
their influence in bringing about change.
More significantly, success in altering the
course of the public’s health and its grow-
ing prevalence of obesity requires substantial
lifestyle changes by individuals, communi-
ties, businesses and governments. This is a
long and arduous road, and while the United
States has made advances in many areas, we
will need comprehensive policies to support
environmental change.
The following section summarizes some
of the implementation challenges facing the
federal, state and local governments as they
implement the Affordable Care Act.
Deployment of the Prevention and
Public Health Fund: Never before has the
government invested such a large amount
of money—$15 billion over the next 10
years—in prevention through a single fund-
ing stream. The harsh reality is, however, that
the amount of money authorized is not as
large as the need. Tough choices lay ahead
to ensure that the investment successfully
“[transforms] our health system into one
that truly promotes health, not just disease
treatment.”
54
It will have a greater chance
of success if the funding represents a new
investment rather than supplants existing
prevention and public health funding.
55
One implementation issue that arose early,
with the Administration’s announcement of
how to deploy the $500 million appropriat-
ed for Fiscal Year 2010, is whether funds tar-
geted for prevention and public health could
be diverted to fund other priorities. On June
18, 2010, the Department of Health and
Human Services announced that it would
spend $250 million (half of the appropriated
funding for the year) on a one-time invest-
ment in the primary care workforce. The
other $250 million was spent on community
and clinical prevention ($126 million), the
public health infrastructure ($70 million),
research and tracking ($31 million) and
public health training ($23 million).
56
APHA
was part of a group of 90 organizations that
urged the Administration to allocate the
entire $500 million, not just $250 million,
to public health issues, not the primary
care workforce.
57
The allocation process for
the Prevention and Public Health Funds is
expected to receive increased scrutiny by
Definition
of Health
Disparities
70
“
…the difference in the
incidence, prevalence,
mortality and burden
of disease and other adverse
health conditions that exist
among specific groups in the
United States.”
14
congressional appropriations committees in
future years.
58
Assuming future Fund allocations are
entirely devoted to prevention and public
health workforce training, there will still be
difficult decisions about how to allocate the
funds among different public health initia-
tives (e.g., tobacco cessation, nutrition, physi-
cal activity), the public health infrastructure,
research and tracking, and public health
workforce training. Transparent reporting of
funding allocations, evaluation and strategic
planning is required by both the National
Health Prevention, Health Promotion and
Public Health Council and the Secretary of
the Department of Health and Human Ser-
vices. Ideally, the investment will be lever-
aged through careful coordination with state,
local and private resources and reflect the
best evidence on efficacy to have maximum
impact.
59
An amendment (to the Small Business Jobs
and Credit Act) by Senator Mike Johanns
in late summer of 2010 was the first official
congressional threat to the Prevention and
Public Health Fund. This amendment would
have repealed a provision of the Affordable
Care Act designed to raise new revenue by
decreasing non-compliance with tax laws. It
would have been funded by eliminating the
Prevention and Public Health Fund from fis-
cal year 2010 to fiscal year 2017. APHA and
other organizations opposed the amendment
and it was defeated.
60
Increased pressure to
reduce the federal deficit during the 112th
Congress is likely to result in legislative pro-
posals to cut the Fund. Preserving the Fund
as created by the Affordable Care Act will
require vigilance and coordinated strate-
gic efforts by public health and prevention
advocates. It will be important to remind
lawmakers of the economic case for preven-
tion, with an estimated $5.60 of health cost
savings for every $1 spent on certain preven-
tion initiatives.
61
Role of the National Prevention, Health
Promotion, and Public Health Council. The
White House released an Executive Order
on June 10, 2010, officially establishing the
National Prevention, Health Promotion, and
Public Health Council.
62
On July 1, 2010,
the Surgeon General released the Council’s
first annual status report.
63
The Council
is charged with coordinating and leading
the work on the federal level with respect
to prevention, wellness, health promotion,
public health system, and integrative health
care. In addition, it is to develop a broad-
ranging “national prevention, health pro-
motion, public and integrative health-care
strategy,” and make recommendations to the
President and Congress regarding tobacco
use, sedentary behavior and poor nutrition.
The Council is well-positioned to build
on the work of Healthy People 2010 and
Healthy People 2020, and has the authority
to coordinate the work of various federal
agencies in a way that is more transparent
and accountable to the public, the Adminis-
tration and Congress. The first annual report
acknowledges the importance of leading and
coordinating federal efforts on prevention.
That role will continue into the future even
after the strategy is completed and released
to the public early in 2011.
The Council’s first status report notes
the significance of its taking “a community
health approach to prevention and wellness”
and of the requirement that its recommen-
dations be grounded in science-based pre-
vention recommendations and guidelines.
64
The Council’s report reflects an understand-
ing of the need for actions, interventions and
policies that go beyond the health system
to address problems in schools, transporta-
tion and education. The report expands on
how it will determine whether interventions
are effective, listing five major strategies for
public health interventions. They are:
65
Policy: supporting policies that promote
prevention, create healthy environments,
and foster healthy behaviors (e.g., remov-
ing barriers to safe and convenient walk-
ing and bicycling).
Systems change: establishing policies
that support healthy behaviors (e.g., es-
tablish patient registries, appointment and
medication reminder systems, and incen-
tives to help monitor and control high
blood pressure and high cholesterol).
Environment: creating social and physi-
cal environments that support healthy lives
and choices (e.g., improve access to fresh
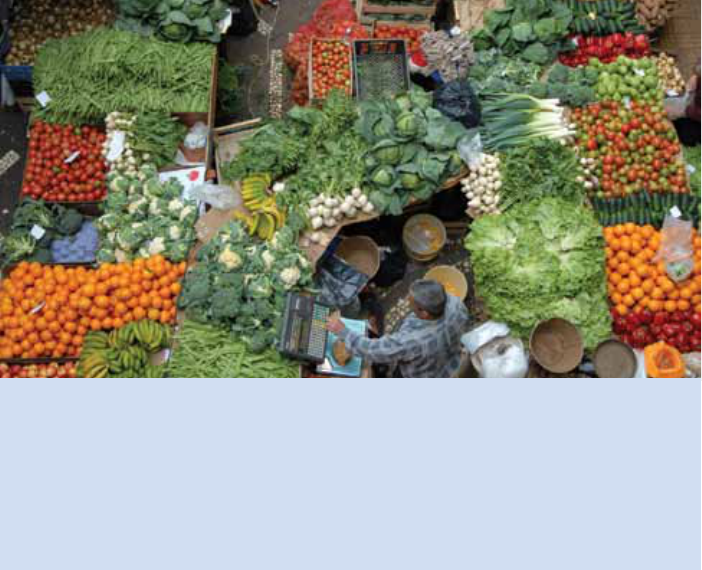
fruits and vegetables in at-risk urban and
underserved communities).
N
ational Prevention,
Health Promotion,
and Public Health
Council is to develop a broad-
ranging “national prevention,
health promotion, public and
integrative health-care strat-
egy,” and make recommen-
dations to the President and
Congress regarding tobacco
use, sedentary behavior and
poor nutrition.

15
Communications and media: Sup-
porting healthy choices and raising
health awareness, especially among
those who experience health dis-
parities, through interactive, social and
mass media (e.g., inform consumers
about options for accessing and pre-
paring healthy and affordable foods).
Program and Service Delivery:
Designing prevention programs and
services to contribute to wellness (e.g.,
provide safe and affordable opportuni-
ties for physical activity in schools).
Implementation Issues at Various
Government Entities: As noted above,
the National Prevention, Health Pro-
motion and Public Health Council will
coordinate federal prevention and public
health initiatives. The Secretary of HHS,
and agencies such as CDC, HRSA, and
AHRQ are responsible for specific initia-
tives of varying scope and complexity,
including hundreds of reports, and strate-
gic decisions on a myriad of issues such
as what criteria to use in awarding grants
to state and local governments for various
programs.
66
Each entity will face a set of
implementation challenges in balancing
research, grant-making, public education
and congressional reporting deadlines.
For example, the timing of the funding
will impact implementation. Further-
more, specific awards will receive media
scrutiny and pushback from stakeholders
who may disagree. These pressures make
it crucial that the leaders of the imple-
mentation effort, both in the Office of
the Secretary and at each implementing
agency, build highly skilled staff to lead
the implementation efforts, including staff
with proven project management skills
and expertise in the communication of
findings, recommendations and programs
to the public in an accessible and trans-
parent manner.
Efficient Use of State and Local
Resources: Implementation of the health
reform law is beginning at a time of
strains and restrictions on the budgets of
state and local governments. According
to the National Association of County
and City Health Officials, the recession
has forced state and local governments
to reduce their overall workforces by 15
percent, cutting 23,000 staff, many of
whom protect health and provide safety.
It would take tens of billions of dollars
to replace the lost staff, and the money
provided in the Affordable Care Act will
not be sufficient to restore the services
that these employees provided.
67
So while
state and local governments will mobilize
to respond to the many new grant op-
portunities, they will do so in the context
of a depleted health and public health
workforce. This will make it difficult to
create and sustain efficiencies around the
new prevention and public health op-
portunities. It will be especially difficult
for implementation efforts to reach their
full potential at the state and local levels
during the prolonged weak economy.
The states have major implementation
responsibilities, including administering
expanded Medicaid programs, revising
state high-risk pool programs, establishing
and regulating health insurance ex-
changes, and regulating and policing the
health insurance marketplace. In addition,
they are eligible to apply for grants, for
example, to help them monitor premium
increases, participate in personal respon-
P
ublic Health Council’s intervention is creating social and physical
environments that support healthy lives and choices (e.g., improve
access to fresh fruits and vegetables in at-risk urban and under-
served communities).

16
sibility education programs, and establish
insurance exchanges.
States already have established the State
Consortium on Health Care Reform, con-
sisting of the National Governors Associa-
tion, the National Association of Insurance
Commissioners, the National Association of
State Medicaid Directors, and the National
Academy for State Health Policy. Individual
states have set up organizational structures.
For example, California has established
the Health Care Reform Task Force, and
Colorado has appointed a Director of Health
Reform Implementation and an Interagency
Health Reform Implementing Board.
68
Additionally, 13 states have jointly filed
a lawsuit contending that the individual
mandate provision violates the Constitution.
The outcome of this lawsuit, and its impact
on implementation actions of these states,
threatens to delay or even derail the abil-
ity of the Affordable Care Act to meet its
potential.
69
Lessons learned from the American
Recovery and Reinvestment Act of 2009
(ARRA). The implementation experience
with the ARRA offers some lessons for
consideration as the Affordable Care Act
is implemented. Dr. Paul Jarris, Executive
Director of the Association of State and Ter-
ritorial Health Officials (ASTHO), contends
that that the ARRA prevention funds, which
were distributed as two-year grants, were
disseminated to high-capacity proven entities
with “ready-to-go” programs. They were
allocated, in large part, to big, sophisticated
organizations, with the hope that positive
results could be demonstrated more clearly.
But to reach underserved and rural popula-
tions, the prevention funds would need to
be distributed in a way that disseminates
benefits more broadly, even though this may
divert some funds to building infrastructure
and may produce a more diffuse (and less
measurable) impact. In the long-term, mak-
ing an investment to communities where
there is the greatest need but the weakest
infrastructure is likely to have a large impact
on the improvement of public health.
Using Investment in Prevention to
Address Health Disparities: The Agency for
Healthcare Research and Quality has issued
reports for the past seven years that measure
and document the extent to which dispari-
ties exist in our health system. The reports
document the level of quality (e.g., safety,
timeliness) and access to care (e.g., barriers
to care) for various racial, ethnic, income
groups, as well as priority populations such
as children and older adults. This year’s report
found that significant disparities continue to
pervade our health care system.
71
The Affordable Care Act has several
provisions that address health disparities as
a priority in awarding various grants (e.g.,
community transformation grants) (Section
4201), developing research priorities (Sec-
tion 6301), gathering accurate data (Section
4302), and evaluating community preventive
services (Section 4003). In addition, the Pre-
vention Education Campaign must address
health disparities. The challenge of reaching
individuals and groups that have tradition-
ally been least well served by our health
care system is large, and it is important that
attention be paid during implementation
to developing effective strategies that reach
underserved populations with the informa-
tion they need.
Preventive Care Benefits: The require-
ment that private group and individual
health plans include preventive care ben-
efits (recommended by the U.S. Preventive
Services Task Force) without cost-sharing
could face some implementation challenges.
First, large employers that do not currently
cover preventive services (a small percent-
age of health plans)
72
could argue that the
requirement to cover preventive services will
increase premiums. Some might argue that
the requirements to cover preventive services
will increase total health care costs, notwith-
standing research that estimates an average
return of over $5 for each dollar invested in
The Council is well-positioned to build on the work of Healthy People 2010 and Healthy People 2020, and
has the authority to coordinate the work of various federal agencies in a way that is more transparent and
accountable to the public, the Administration and Congress.

17
prevention.
73
While premiums could increase
for the small percentage of plans that do not
already include preventive care benefits, the
increase in premium will offset out-of-pock-
et costs to cover such benefits, all of which
are to be covered because they are recom-
mended based on scientific evidence.
Another implementation issue concerning
the preventive benefits in private and public
health plans is the potential controversy that
could arise over certain recommendations
offered by the U.S. Preventive Services Task
Force and the Task Force on Community
Preventive Services. The controversy over
the recommendations on mammography
provided lessons about wording recommen-
dations carefully to reflect the nuances of the
evidence, and about the need for discussing
an individual’s personal circumstances with
health care providers.
74
A third implementation issue is timing:
When will health plans incorporate the new
preventive benefits? The grandfather provi-
sion (and Administration rule) affects the
timing. Grandfather status refers to the abil-
ity of a plan to continue to be offered “as is”
to current enrollees so that people can truly
“keep the plan” they are in.
75
In general, new
private policies issued after Sept. 23, 2010,
must include the new preventive benefits.
Employer Wellness Plans: Before the en-
actment of the health reform law, 58 percent
of companies that offered health benefits
covered at least one wellness program—such
as gym membership discounts, weight-loss
programs or nutrition classes—with larger
firms more likely than smaller firms to do so.
Few firms provided financial incentives for
employers to participate in these programs.
The most common forms of incentive, used
by 10 percent of firms, were gift cards, travel,
merchandise or cash. Only 1 percent of firms
offered a lower deductible for participating
in these programs, while 4 percent offered
a discount on the employer share of pre-
mium.
76
The Health Insurance Portability and Ac-
countability Act (HIPAA), enacted in 1996,
established requirements for employer well-
ness programs that guard against employer
health plans using minimum health standards
(e.g., blood pressure levels or tobacco ces-
sation) to discriminate against people who
have existing health conditions.
77
The provisions in the health reform law
that encourage and support employer well-
ness plans have the potential to raise con-
cerns that some employees may be penalized
because they do not meet certain health sta-
tus standards. The health reform law (section
4303) provides support to employers that of-
fer wellness programs. For example, technical
assistance will be provided to help employers
increase participation and evaluate the im-
pact. In addition, the law provides grants to
employers with fewer than 100 employees to
establish wellness programs.
78
While the law
prohibits the use of assessments to require
workplace wellness programs, some ques-
tions could arise when another provision is
implemented. Section 2705 of Title I, which
prohibits discrimination against individuals
based on health status (i.e., higher premiums
or denial of coverage), allows employers to
provide financial rewards to employees who
meet certain health standards. The financial
incentive can be as high as 30 percent of
the total employee premium initially, and
can increase to 50 percent eventually, if the
Secretary of the Department of Health and
T
he Agency for Healthcare Research and Quality has issued reports
for the past seven years that measure and document the extent to
which disparities exist in our health system. The reports document
the level of quality (e.g., safety, timeliness) and access to care (e.g., barriers to
care) for various racial, ethnic, income groups, as well as priority populations
such as children and older adults.
18
Human Services allows this increase. Today
the potential reward for employees is limited
to 20 percent.
79
There are a number of re-
strictions that provide an opportunity for an
employee to improve his or her performance
on a health measure, but the bottom line is
that some employees might feel that they
are financially penalized for a poor blood
pressure or cholesterol test result which
they may consider to be more genetic than
controllable through good nutrition, exercise
and modified lifestyle habits.
The Affordable Care Act (Section 4303)
requires employers to build capacity to
evaluate the affect of these programs, and the
Director of the Centers for Disease Control
and Prevention to assess, analyze and moni-
tor the impact of the programs, and report
findings and recommendations to Congress.
Earlier research about disease management
programs, which share many elements of
employer wellness programs, should provide
lessons for employers and the CDC to help
shape evaluation of these programs.
80
Healthcare and Public Health Workforce:
Millions of people will be newly covered
under health reform by expanded benefits
that include preventive care. This will place
increased demands on primary care provid-
ers who focus on prevention. Massachusetts
experienced shortages in primary care doc-
tors after implementation of its health re-
form law.
81
Title V of the Affordable Care Act
calls for a Healthcare Workforce Commis-
sion that will issue reports with recommen-
dations every year, beginning April 1, 2011.
Even before health reform was enacted, the
Association of American Medical Colleges
projected that there would be a shortage of
46,000 primary care doctors in 2025.
82
The workforce issues that must be ad-
dressed go beyond the pipeline issue of train-
ing more primary care providers. Expanding
access to high-quality, high-value care—and
matching that care to a workforce with the
requisite skills to provide it—is a long-term
endeavor. Reaching that goal will require us
to consider new team practice approaches to
increase the accountability of health organi-
zations, medical homes and other models of
care, integration of electronic health records
and interactive systems, and review of medi-
cal licensing restrictions, among many other
things.
83
Patient-Centered Outcomes Research In-
stitute (Institute): The Affordable Care Act
establishes a new Institute that will establish
and carry out a clinical outcomes research
agenda to help patients, providers and poli-
cymakers make better informed decisions to
advance health care quality. While the law
refers to preventing illness as one of the areas
for research, much depends on the extent to
which the Institute makes prevention-
focused research a priority. Close coordina-
tion with the U.S. Preventive Services Task
Force and the Task Force on Community
Preventive Services will be critical.
V. Conclusion and
Recommendations
The health reform law includes language and
funding that significantly expand the country’s
commitment to promoting health and preventing
disease. The Affordable Care Act:
establishes a high-level Council, with substan-
tial funding for programs to improve popula-
tion health, to coordinate federal programs and
develop and implement a national strategy;
seeks to reduce the large number of pre-
ventable deaths and illness by improving the
environment and policies which in turn will
increase positive health behavior; for example,
by educating the public about nutrition, exer-
cise, and tobacco cessation;
builds evidence-based preventive services into
private and public health coverage, without
cost-sharing; and
conducts pilot projects and research in com-
munities nationwide that will increase our
ability to further improve preventive and
public health services and population health in
the future.
The implementation challenges ahead are sub-
stantial, and legal and political challenges to the
law create additional uncertainty. Coordination
and cooperation across all levels of government
and the private health industry will be needed
to achieve the law’s potential. The following
recommendations, many drawn from the work
of experts in the prevention arena, are offered
to help guide the work of policymakers at the
federal, state and local levels who are implement-
ing reform:
E
xpanding access to
high-quality, high-
value care—and
matching that care to a work-
force with the requisite skills
to provide it—is a long-term
endeavor. Reaching that goal
will require us to consider new
team practice approaches to
increase the accountability of
health organizations, medical
homes and other models of
care, integration of electronic
health records and interactive
systems, and review of medical
licensing restrictions, among
many other things.
83

19
Policymakers should take steps to ensure that
Prevention and Public Health Fund dollars
provide a net incremental investment rather
than displace existing spending,
84
and find cre-
ative ways to alleviate the severe budget pres-
sure at state and local government agencies.
New efforts should build on the theme em-
phasized throughout the health reform law
that bases policy on good science. Com-
municate with target populations, healthcare
providers, public health professionals and indi-
viduals, with evidence-based information that
can improve health.
Programs to improve population health should
be designed with sensitivity to patient prefer-
ences, culture, needs and well-being, and with
the goal of addressing the health disparities
which severely limit the quality of care and
health of millions of people;
The Patient-Centered Outcomes Research
Institute and other entities establishing re-
search priorities should make research about
effectiveness of techniques to prevent disease
and disability a high priority, enabling new
research that substantially improves population
health.
Notwithstanding the health reform law’s focus
on “clinical effectiveness” and not “cost-effec-
tiveness,” policymakers should explore how re-
imbursement policy (for Medicare, Medicaid,
the Department of Veterans Affairs, the Federal
Employees Health Benefits Program, and the
private marketplace) can further encourage
promotion of health and prevention of disease.
Pilot projects (such as individual wellness plans
for at-risk populations and interventions tar-
geted at the pre-Medicare population) should
be evaluated, and those that prove successful
should be expanded nationwide.
Acknowledgments
I would like to thank Susan Abramson, Donald
Hoppert, and Susan Polan of the APHA for
their guidance and thoughtful review of earlier
drafts of this issue brief. Thanks to Larry Cohen,
Sana Chehimi, and Dalila Butler of Prevention
Institute and Donna Brown of the National As-
sociation of County and City Health Officials
for their helpful comments. I would also like to
express my appreciation for the insights provided
in interviews with Dr. Paul Jarris, Executive
Director of the Association of State and Territo-
rial Health Organizations, Robert M. (Bobby)
Pestronk, Executive Director of the National
Association of County and City Health Officials,
and Caroline Fichtenberg, staff member of the
Senate HELP Committee.
Endnotes
1 APHA 2009 Agenda for Health Reform. Washington, DC:
American Public Health Association, 2009. Available online
at: http://www.apha.org/NR/rdonlyres/681AD0D2-
7DD0-48DD-8D59-E425E271156D/0/HlthRe-
form09C6.pdf. To see how provisions of health reform
compare with the APHA Agenda for Health Reform,
see APHA Agenda for Health Reform and Relevant
Provisions in the Patient Protection and Affordable Care
Act as Amended by the Health Care and Education Afford-
ability Reconciliation Act. Online at: http://www.apha.
org/NR/rdonlyres/00CA506E-4B96-4487-9937-
07F3F4C7470F/0/EnactedPatientProtectionandAfforda-
bleCareActandAPHAAgendaforHealthReform.pdf. S
2 See also Blueprint for a Healthier America, Trust for America’s
Health, October 2008. Online at: http://healthyamericans.
org/report/55/blueprint-for-healthier-america.
3 National Journal Expert Blogs: Health Care, Senator Tom
Harking, May 21, 2010. Available at http://healthcare.
nationaljournal.com/contributors/sen-tom-harkin-d-
iowalth Care and Education Reconciliation Aa.php (June
14, 2010)
4 The prevention provisions were included in the first of
the two health reform bills enacted, the Patient Protection
and Affordable Care Act, P.L. 111-148 (signed into law
on March 23, 2010) and The Health Care and Education
Reconciliation Act of 2010, P.L. 111-152 (signed into law
on March 30, 2010). P.L. 111-152 contained primarily
funding and payment provisions, not prevention provisions.
5 See for example, Blueprint for a Healthier America, Washing-
ton, DC: Trust for America’s Health 2008. Available at: http://
healthyamericans.org/report/55/blueprint-for-healthier-
america. Accessed June 10, 2010. See, for example, the
T
he Affordable Care Act seeks to reduce the large number of prevent-
able deaths and illness by improving the environment and policies
which in turn will increase positive health behavior; for example, by
educating the public about nutrition, exercise, and tobacco cessation.
20
letter from Dr. Georges C. Benjamin, Executive Director,
APHA, to Senator Harry Reid, Senator Max Baucus, and
Senator Tom Harkin, November 20, 2009.
6 The prevention provisions were included in the first of
the two health reform bills enacted, the Patient Protection
and Affordable Care Act, P.L. 111-148 (signed into law
on March 23, 2010) and The Health Care and Education
Reconciliation Act of 2010, P.L. 111-152 (signed into law
on March 30, 2010). P.L. 111-152 contained primarily
funding and payment provisions, not prevention provisions.
7 The National Priorities Partnership, consisting of experts
in quality health care from a broad range of public and
private organizations recommended transformation of
our health care system including creation of “communi-
ties that foster health and wellness as well as national, state,
and local systems of care fully invested in the prevention
of disease, injury, and disability.” See: National Priori-
ties Partnership. National Priorities and Goals: Aligning Our
Efforts to Transform America’s Healthcare, Washington, DC:
National Quality Forum, 2008. Available at: http://www.
nationalprioritiespartnership.org/uploadedFiles/NPP/
About_NPP/ExecSum_no_ticks.pdf. Accessed October
18, 2010. The Partnership for Prevention, a nonpartisan
group of business, nonprofit, and government leaders
called for making prevention a high priority in health re-
form, publishing a report Real Reform Starts with Prevention.
Available at: http://www.prevent.org/data/files/initiatives/
fullreport-rhrstartswithprevention.pdf Accessed October
18, 2010. The Trust for America’s Health (Trust) released
its Blueprint for a Healthier America: Modernizing the Federal
Public Health System to Focus on Prevention and Preparedness,
calling for the establishment of short and long-term health
goals, investing in disease prevention “as a cornerstone of
health care reform,” and implementation of a “national
health and prevention strategy focused on lowering disease
rates,” among other things. See Trust for America’s Health,
Blueprint for a Healthier America, Washington, DC: Trust for
America’s Health, 2008. Available at: http://healthyameri-
cans.org/report/55/blueprint-for-healthier-america. Ac-
cessed June 10, 2010. The Prevention Institute, joined by
PolicyLink, called for investing in community prevention
“as a core component of health reform” and “promot[ing]
collaboration across fields and sectors encouraging healthy
people and healthy places.” See: Prevention Institute and
PolicyLink, Strengthening What Works: Critical Provisions for
Prevention in Public Health in Health Reform Legislation, Oak-
land, CA: Prevention Institute 2009. Available online at:
http://www.preventioninstitute.org/component/jlibrary/
article/id-110/127.html. Accessed October 18, 2010.
8 The Congressional Budget Office has estimates of Autho-
rizations for Spending Subject to Appropriations for the
PPACA (by section) Letter of May 11, 2010 from Douglas
W. Elmendorf, Director, Congressional Budget Office to
Honorable Jerry Lewis, Ranking Member, Committee on
Appropriations, U.S. House of Representatives, Available
at: http://www.cbo.gov/ftpdocs/114xx/doc11490/Lewis-
Ltr_HR3590.pdf.
9 America’s Health Rankings. Minnetonka, MN: United
Health Foundation, 2009. Available at: http://www.
americashealthrankings.org/2009/report/AHR2009%20
Final%20Report.pdf
10 Ibid.
11 Ibid.
12 Kindig DA, Asada Y, Booske B, A population health frame-
work for setting national and state health goals, JAMA;
299: 2081-2083, 2008.
13 Ornish, D. Intensive Lifestyle Changes for Reversal of Coronary
Heart Disease, JAMA. 280:2001-2007, 1998. Available at:
http://jama.ama-assn.org/cgi/content/full/280/23/2001.
Accessed October 18, 2010.
14 Adult Obesity: Obesity Rises Among Adults, U.S. Center
for Disease Control and Prevention, August 3, 2010. On-
line at: http://cdc.gov/vitalsigns/AdultObesity/.
15 Food, Nutrition, Physical Activity and the Prevention of Cancer:
A Global Perspective. Washington, D.C. World Cancer Re-
search Fund and American Institute for Cancer Research,
2007.
16 Whelan, EM, Sekhar, S. Tackling the Obesity Epidemic: How
Health Reform Helps Address the Childhood Obesity Epidemic,
Washington, DC: Center for American Progress, 2010.
17 Hartman, M., Martin, A., Nuccio, O., et al. Health Spending
Growth At A Historic Low In 2008, Health Affairs, 29147-
155, 2010.
18 Life Expectancy at Birth and Age 65, by Sex—Select Countries,
Washington, DC: U.S. Census Bureau, 2010. Available at:
http://www.census.gov/compendia/statab/cats/interna-
tional_statistics.html. Accessed October 18, 2010.
19 America’s Health Rankings. Minnetonka, MN: United
Health Foundation, 2009. Available at: http://www.
americashealthrankings.org/2009/report/AHR2009%20
Final%20Report.pdf Accessed on June 13, 2010.
20 American’s Health Rankings. Minnetonka, MN: United
Health Foundation, 2009. Available at: http://www.
americashealthrankings.org/Measure/2009/List%20All/
Infant%20Mortality.aspx. Accessed on June 13, 2010.
21 The countries performing better than the United States
were Australia, Canada, Germany, the Netherlands, New
Zealand and the United Kingdom. Davis, K, Schoen, C.,
Stremikis, K. How the Performance of the U.S. Health Care
System Compares Internationally 2010 Update, New York:
The Commonwealth Fund, 2010. Available at: http://
www.commonwealthfund.org/Content/Publications/
Fund-Reports/2010/Jun/Mirror-Mirror-Update.aspx.
Accessed October 18, 2010.
22 The Commonwealth Fund Opinion Leaders Survey, January
2007. Available at: http://www.commonwealthfund.org/
Maps-and-Data/ChartCart/View-All.aspx?charttopic=He
alth+Care+Workforce. Accessed October 18, 2010.
23 Committee on the Future Health Care Workforce for
Older Americans, Retooling for an Aging America: Build-
ing the Health Care Workforce, Washington, DC: Institute
of Medicine. Available at: http://books.nap.edu/catalog.
php?record_id=12089. Accessed October 18, 2010.
24 American’s Health Rankings. Minnetonka, MN: United
Health Foundation, 2009. Available at: http://www.
americashealthrankings.org/2009/report/AHR2009%20
Final%20Report.pdf Accessed on June 13, 2010.
25 Ibid.
26 America’s Children in Brief: Key National Indicators of Well-
being, Federal Interagency Forum on child and Family
Statistics, 2010. Available at: http://childstats.gov. Accessed
October 18, 2010.
27 Ibid. AHRQ, p. 6.
28 Ibid. p. 20. 1.4 million children between 12 and 17 years
old needed treatment for an alcohol problem in 2006.
Office of Applied Studies. 2007. Results from the 2006
National Survey on Drug Use and Health: National Find-
ings. Rockville, MD: Substance Abuse and Mental Health
Services Administration. Cited at: http://www.alcohol-
freechildren.org/files/pubs/html/stat.htm#health.
29 Ibid. AHRQ, p. 8.
21
30 March 1, 2010l, Announcement from the White House.
Online at: http://www.whitehouse.gov/the-press-office/
president-obama-announces-steps-reduce-dropout-rate-
and-prepare-students-college-an
31 U.S Surgeon General. Mental Health: A Report of the Surgeon
General. Washington, DC: U.S. Public Health Service.
Available at: http://www.surgeongeneral.gov/library/men-
talhealth/chapter3/sec5.html. Accessed October 18, 2010.
32 Trust for America’s Health. Prevention for a Healthier America:
Investments in Disease Prevention Yield Significant Savings,
Stronger Communities, Washington, DC: Trust for America’s
Health, 2008. Available at: www.healthyamericans.org. Ac-
cessed June 10, 2010.
33 Healthy People 2010 and Healthy People 2020 (still under
development) are initiatives based in the Office of Disease
Prevention and Health Promotion. They establish preven-
tion goals for the nation, and build on the 1979 Surgeon
General’s Report, Healthy People, and Healthy People 2000:
National Health Promotion and Disease Prevention Objectives.
34 Williams DR, McClellan MB, Rivlin SM, Beyond The
Affordable Care Act: Achieving Real Improvements in Americans’
Health, Health Affairs, 29: 1481-1488, 2010.
35 Prevention Institute, Addressing the Intersection: Prevent-
ing Violence and Promoting Healthy Eating and Active
Living, May 2010. Online at: http://www.preventioninsti-
tute.org/component/jlibrary/article/id-267/127.html.
36 Hartman M, Martin A, Nuccio O, et al. Health Spending
Growth At A Historic Low in 2008. Health Affairs, January,
Exhibit 1.
37 This was established by an Executive Order of the Presi-
dent on June 10, 2010.
38 Also included by the law on the Council: Administrator
of the Environmental Protection Agency, Director of the
Office of National Drug Control Policy, Assistant Secretary
for Indian Affairs, Chairman of the Corporation for
National and Community Service, and head of any other
Federal agency that the chairman considers appropriate.
Additional members currently serving are the Secretar-
ies of Defense, Veterans Affairs and Housing and Urban
Development, as well as a representative of the Office of
Management and Budget. See: http://www.healthcare.
gov/center/councils/nphpphc/about/index.html#ovr.
39 For a description of local programs that can benefit popu-
lations that have often been marginalized and underserved,
see A Time of Opportunity: Local Solutions to Reduce Inequities
in Health and Safety, Prevention Institute, May 2009. On-
line at: http://www.preventioninstitute.org/component/
jlibrary/article/id-81/288.html.
40 In addition, Title I, section 2705 allows employers to
provide financial incentives to employees to meet certain
health standards, as discussed in Employer Wellness Plan
section in implementation and policy section below.
41 These provisions (and the sections) are from the Patient
Protection and Affordable Care Act, P.L. 111-148.
42 See Table 2 for information about evaluating interventions
regarding the Medicare population. This section of Table 1
includes the grants for programs targeted to the 55 to 64
year old population.
43 Op. cit. National Priorities Partnership.
44 Section 4004, Public Law 111-148.
45 Exhibit 7-16. Employer Health Benefits: 2009 Annual Sur-
vey, The Kaiser Family Foundation and Health Research
& Educational Trust. Available at: http://ehbs.kff.org/
pdf/2009/7936.pdf Accessed October 18, 2010.
46 Pear, R. Economy Led Americans to Limit Use of Routine
Health Services, Study Says, New York Times, August 17,
2010, p. A14. The article describes the study that compared
routine care provided in five countries, and found that cut-
backs in care corresponded to the level of out-of-pocket
costs. Article reports on The Economic Crisis and Medical
Care Usage, National Bureau of Economic Research
Working Paper No. 15842, March 2010. Co-authors An-
namaria Lusardi, Daniel Schneider and Peter Tufano.
47 APHA Agenda for Health Reform and Relevant Provi-
sions in the Patient Protection and Affordable Care Act as
Amended by the Health Care and Education Affordability
Reconciliation Act. Washington, DC: American Pub-
lic Health Association. Available at: http://www.apha.
org/NR/rdonlyres/00CA506E-4B96-4487-9937-
07F3F4C7470F/0/EnactedPatientProtectionandAf-
fordableCareActandAPHAAgendaforHealthReform.pdf.
Accessed October 18, 2010.
48 U.S Preventive Services Task Force. The Guide to Clinical
Preventive Services: Recommendations of the U.S. Preventive
Services Task Force, Washington, DC: Agency for Healthcare
Research and Quality, 2009. Available at: http://www.ahrq.
gov/clinic/pocketgd09/pocketgd09.pdf Accessed June 8,
2010. The Affordable Care Act (Section 4003) also requires
enhanced dissemination of the recommendations for best
practices.
49 The Secretary of HHS is given authority in the health
reform law to expand the coverage beyond that recom-
mended by the U.S. Preventive Services Task Force.
50 Center for Medicare and Medicaid Services, Your Medicare
Benefits. Washington, DC: Department of Health and
Human Services. Available at: http://www.medicare.gov/
publications/pubs/pdf/10116.pdf. Accessed October 18,
2010.
51 Amends section (8) of the Social Security Act (42 U.S.C.
132b-9a(e)(8).
52 This provision also calls for review of each recommenda-
tion every 5 years.
53 The section numbers refer to the Patient Protection and
Affordability Act, P.L. 111-148.
54 Trust for America’s Health, Letter to Secretary Sebelius,
April 20, 2010.
55 Ibid.
56 Sebelius Announces New $250 Million Investment
to Lay Foundation for Prevention and Public Health,
News Release, June 18, 2010, and Fact Sheet: Afford-
able Care Act: Laying the Foundation for Prevention, June
18, 2010. Available at: http://www.hhs.gov/news/
press/2010pres/06/20100618g.html and http://www.
healthreform.gov/newsroom/acaprevention.html.
57 Press Release: Prevention and Public Health Fund to Jumpstart
Community-Based Prevention Programs, Trust for America’s
Health (TFAH), June 18, 2010. Available at: http://
healthyamericans.org/newsroom/releases/?releaseid=215.
58 Conversation with Caroline Fichtenberg, staff of U.S.
Senate Health, Education, Labor and Pensions Committee,
June 30, 2010.
59 Ibid.
60 Letter from Georges C. Benjamin, MD, FACP, FACEP,
Executive Director, APHA, to the United States Senate,
August 3, 2010. Edwin Park and Chuck Marr, Johanns
Amendment to Small Business Bill Would Raise Health
Insurance Premiums, Increase the Ranks of the Uninsured, and
Eliminate Preventive Health Funding, Center on Budget and
Policy Priorities, September 13, 2010.
22
61 See Section II above and Prevention for a Healthier America:
Investments in Disease Prevention Yield Significant Savings,
Stronger Communities, Trust for America’s Health, July 2008.
(Above in note 33).
62 White House Executive Order Executive Order-- Estab-
lishing the National Prevention, Health Promotion, and
Public Health Council, June 10, 2010. Available at: http://
www.whitehouse.gov/the-press-office/executive-order-
establishing-national-prevention-health-promotion-and-
public-health. Accessed October 18, 2010.
63 2010 Annual Status Report. Washington, DC: National
Prevention, Health Promotion and Public Health Council,
2010.
64 Ibid
65 Ibid. The language below is a condensed form of the list
of strategies in the report, in some cases shortening the
descriptions.
66 Health reform implementation materials for the Depart-
ment of Health and Human Services are posted at www.
healthcare.gov.
67 Conversation with Bobby Pestronk, Executive Director,
National Association of City and County Health Officials,
July 1, 2010.
68 50 Ways to Implement Health Reform: State Challenges and
Federal Assistance, Alliance for Health Reform, August 2,
2010. Available at: http://allhealth.org/briefing_detail.
asp?bi=190. Accessed October 18, 2010.
69 Legal Challenges to Health Reform: An Alliance for Health
Reform Toolkit, May 18, 2010. Available at: http://www.
allhealth.org/publications/Uninsured/Legal_Challenges_
to_New_Health_Reform_Law_97.pdf.
70 National Institute of Health Working Group on Health
Disparities, Draft Trans-NIH Strategic Research Plan on Health
Disparities, Bethesda, MD: National Institute of Health,
2000.
71 Agency for Healthcare Research and Quality. 2009 Nation-
al Healthcare Disparities Report, Washington, DC: Department
of Health and Human Services, 2010. Available at: www.ahrq.
gov/qual/qrdr09.htm. Accessed October 18, 2010.
72 90 percent of workers with employer coverage in health
maintenance organizations, preferred provider organiza-
tions, point-of-service plans and high deductible health
plans had preventive services coverage, without having to
meet a deductible, in 2009. The Henry J. Kaiser Family
Foundation and Health Research & Educational Trust,
Employer Health Benefits: 2009 Annual Survey, Washington,
DC: Kaiser Family Foundation, 2009. Available at: http://
ehbs.kff.org/pdf/2009/7936.pdf. Accessed on June 10,
2010.
73 Trust for America’s Health, Prevention for a Healthier America:
Investments in Disease Prevention Yield Significant Savings,
Stronger Communities, July 2008. Available at: http://
healthyamericans.org/reports/prevention08. Accessed on
June 10, 2010.
74 See also: Wilensky, GR. The Mammography Guidelines
and Evidence-Based Medicine. Health Affairs Blog, January
12, 2010. Available online at: http://healthaffairs.org/
blog/2010/01/12/the-mammograpy-guidelines-and-
evidence-based-medicine/ Accessed June 14, 2010.
75 Julian Pecquet, Insurers seek more flexibility to avoid health
reform mandates, The Hill, August 11, 2010; Mike Lillis, U.S.
Chamber lodges complaints with new rules for grandfa-
thered health plans,” The Hill, August 16, 2010.
76 Section 12, Kaiser and HRET, Employer Health Benefits
2009 Annual Survey, p. 170.
77 Employer Wellness Programs, Posted by Health Reform GPS,
August 16, 2010. Available at: http://healthreformgps.org/
resources/employer-wellness-programs/
78 Section 10408 authorizes $200 million for FY2011-
FY2015.
79 Darling H., Health Care Reform: Perspective from large Em-
ployers, Health Affairs (Millwood) 29: 1220-1224, 2010.
80 See, e.g., Congressional Budget Office, An Evaluation of
the Literature of Disease Management Programs, October
13, 2004. Online at: http://www.cbo.gov/ftpdocs/59xx/
doc5909/10-13-DiseaseMngmnt.pdf and Mattke S., Seid
M., Ma S., Evidence for the Effect of Disease Manage-
ment: Is $1 Billion a Year a Good Investment? American
Journal of Managed Care, 13: 670-676, 2007. Available
at: http://www.ajmc.com/media/pdf/AJMC_07dec_
Mattke_670to76.pdf. Accessed October 18, 2010.
81 Long SK., Masi PB. Access And Affordability: An Update
On Health Reform In Massachusetts, Fall 2008, Health Af-
fairs, Web Exclusive, May 28, 2009. W578.
82 Center for Workforce Studies, The Complexities of Physician
Supply and Demand: Projections Through 2025, Washington,
DC: Association of American Medical Colleges, 2008.
Available at: https://services.aamc.org/publications/
showfile.cfm?file=version122.pdf&prd_id=244&prv_
id=299&pdf_id=122. Accessed October 18, 2010.
83 See Margolis M, and Bodenheimer T, Transforming Primary
Care: From Past Practice to the Practice of the Future, Health
Affairs. 29: 779-783, 2010.
84 Trust for America’s Health, Letter to Secretary Sebelius,
April 20, 2010.
85 See: http://www.healthypeople.gov/.
86 See: http://www.thecommunityguide.org/index.html.
87 Available at http://www.ahrq.gov/clinic/pocketgd.htm.
23
Appendix 2
Terms Used in Preventive Health and in the Issue Brief
Agency for Healthcare Quality and Research (AHRQ)—The agency within the U.S. Department of Health
and Human Services that is charged with improving the quality, safety, efficiency, and effectiveness of health care
for all Americans.
Centers for Disease Control and Prevention (CDC)—This is an agency within HHS responsible for
increasing access to health care services to the uninsured and others who are medically vulnerable.
Department of Health and Human Services (HHS)—This is the federal department that is responsible for
federal programs that involve the health and human services of Americans. It is the focal point for the nearly all
health reform implementation. Key agencies are housed within HHS – the Agency for Health care Research and
Quality, the Center for Disease Control and Prevention, the Health Resources Administration.
Health Resources and Services Administration (HRSA)—The Health Resources and Services
Administration (HRSA), an agency of the U.S. Department of Health and Human Services, is the primary Federal
agency for improving access to health care services for people who are uninsured, isolated or medically vulnerable.
Affordable Care Act—Congress enacted two laws in 2010 that reform the health care system in many ways.
The Patient Protection and Affordable Care Act (P.L. 111-148) is the law that includes the provisions described
in this issue brief. The Health Care and Education Reconciliation Act of 2010 (P.L. 111-152) included provisions
primarily related to funding and payment issues. The “Affordable Care Act” encompasses both laws.
Healthy People—A project by federal agencies, working with State and Territorial health departments and
hundreds of consortium members, to establish a framework for disease prevention and health promotion. The
overarching goals are to increase quality and years of healthy life and to reduce health disparities. Healthy People
2010 had a comprehensive list objectives for disease prevention and health promotion, covering 28 focus areas
(e.g., diabetes).
85
Task Force on Community Preventive Services—This independent task force, newly authorized by the
health reform law and housed at the CDC, consists of experts in prevention and public health experts. It is charged
with overseeing the analyses of public health interventions. It makes recommendations for interventions that
advance population health. Its recommendations are available for free online; they are published in the Guide to
Community Preventive Services.
86
U.S Preventive Services Task Force—An independent panel of experts in prevention and primary care. First
established in 1984, it is now housed at the Agency for Healthcare Research and Quality. Its recommendations
for preventive care are available for free online to everyone and are published in the Guide to Clinical Preventive
Services.
87
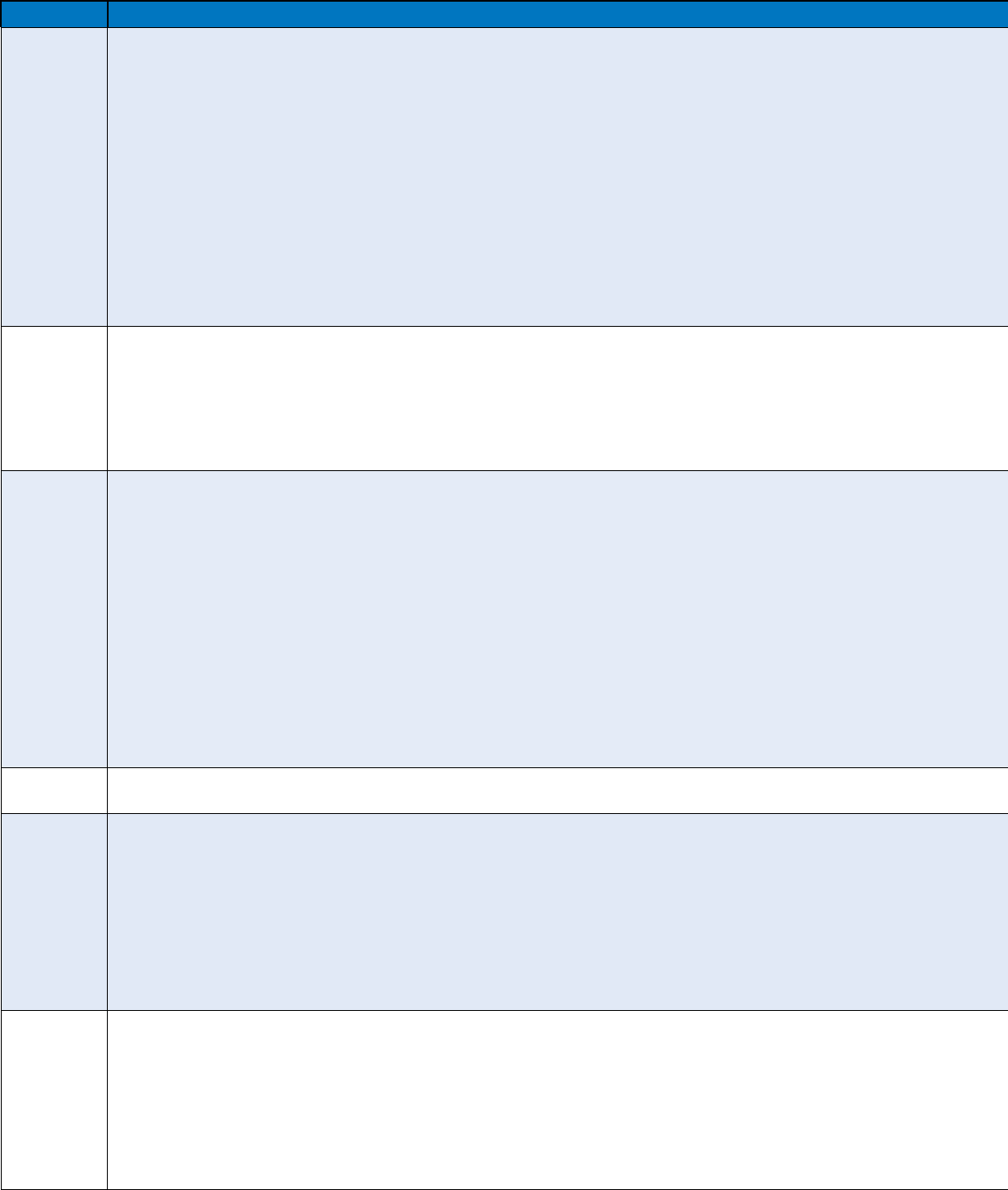
24
Appendix 1:
APHA’s Health Reform Implementation Timeline—Beyond coverage: Public health, prevention and wellness provisions
2010 2011 2012 2013
Prevention
and
Wellness
• Prevention and Public Health Investment Fund: Provides expanded and sustained national investment increasing from $500 million in FY2010 to $2 billion in FY2015 and each fiscal
year thereafter.
•
National Health Promotion and Prevention Strategy: Directs an interagency council, chaired by the U.S. Surgeon General, to develop a national prevention and health promotion strategy.
• Healthy Aging, Living Well Program: Creates a pilot program to help control chronic disease and reduce Medicare costs of the pre-Medicare-eligible population.
•
Pregnancy Assistance Fund: Awards competitive grants to states to assist pregnant and parenting teens and women, and victims or domestic violence and sexual assault. Authorizes $25
million each year for FY2010-2019.
•
Commission on Key National Indicators: Establishes “Commission on Key National Indicators” to develop and oversee a “Key National Indicators” system. Authorizes but does not
appropriate $10 million for FY2010 ; $7.5 million from FY2011-2018.
• Community Transformation Grants: Grants to implement, evaluate and disseminate proven evidence-based community preventive health activities.
•
Increased Funding for Immunizations: State grants to increase recommended immunizations in high-risk populations. Allows states to purchase adult vaccines directly from
manufacturers at HHS-negotiated price. Reauthorizes section 317 program; Authorizes but does not appropriate $1 million for FY2010.
•
Maternal, Infant and Early Child Home Visitation Programs: Funding to states, tribes and territories to develop and implement one or more evidence-based Maternal, Infant, and Early
Childhood Visitation model(s). Authorizes $1.5 billion in total funding FY2010-2015.
•
Personal Responsibility Education Grants: Funding to states to educate adolescents on abstinence and contraception for prevention of teenage pregnancy and sexually transmitted
infections, including HIV/AIDS. Authorizes but does not appropriate $75 million/year FY2010-2014.
• National Improvement Strategy: Develops a national quality improvement strategy
that includes priorities to improve the delivery of health care services, patient health
outcomes, and population health.
• Nutrition Labeling Requirements: Requires nutrition labeling on standard menu items
at chain restaurants and on of food sold from vending machines.
• Education and Outreach Campaign on Preventive Benefits: Requires HHS to convene
a national public/private partnership to conduct a national prevention and health
promotion outreach and education campaign; funding not to exceed $500 million.
• Oral Health Campaign:
Establishes 5-year
national public education
campaign on oral
healthcare prevention.
Demonstration grants
to demonstrate
the effectiveness
of research-based
dental caries disease
management activities.
Public Health
• Federally Qualified Health Center (FQHC): Authorizes but does not appropriate funding for FQHCs that increases from $2.98 billion in FY2010 to $8.33 billion in FY2015.
• Address Access to Care Issues: Authorizes but does not appropriate $100 million to be available through September 20, 2011 to fund infrastructure projects to expand access to care.
• School-Based Health Clinics: Creates a grant program for the operation and development of school-based health clinics. Authorizes $50 million each year for FY2010-2013 for facilities
and equipment expenditures.
•
Nurse-Managed Health Clinics: Grant program, administered by HRSA, to support nurse-managed health clinics. Authorizes but does not appropriate $50 million for FY2010.
• Surveillance and Lab Capacity: Establishes a CDC grant program to improve surveillance for and responses to infectious diseases and other conditions of public health importance.
Authorizes but does not appropriate $190 million each year for FY2010-2013.
• Expansion of National Health Service Corps: Establishes Community Health Center
Fund to increase investment in National Health Service Corps. Authorizes a total of
$1.5 billion in funding increasing from $290 million in FY2011 to $310 million in
FY2015.
• Increasing Community Health Center Funding: Authorizes additional funding for
community health centers, increasing from $1 billion in FY2011 to $3.6 billion in
FY2015. Provides an additional $1.5 billion for renovation and construction.
Public Health
Workforce
• National Health Care Workforce Commission: Creates a commission charged with disseminating information on current and projected health care workforce supply and demand,
education and training capacity, retention programs, and fiscal sustainability.
• National Health Service Corps: Increases and extends funding authorization for the scholarship and loan repayment program for FY2010-2015.
• Public Health Professional Training: Training program for mid-career public health professionals. Authorizes but does not appropriate $30 million for FY2010.
•
Healthcare Workforce Development: Grant program to support state and regional partnerships to complete comprehensive workforce planning and development. Authorizes but does not
appropriate $8 million in FY2010 for planning grants (entities must match at least 15% of funding) and $150 million for FY2010 for implementation grants (entities must match at least
25% of funding).
•
National Emergency Corps: Establishes Ready Reserve Corps within the Commissioned Corps for service in times of national emergency. Authorizes but does not appropriate $50 million
each year for FY2010-2014.
•
Allied Health Professional Loan Repayment: Loan repayment to allied health professionals employed at public health agencies or in settings providing health care to patients in
underserved areas. Authorizes but does not appropriate $30 million for FY2010.
•
Pediatric Loan Repayment: Loan repayment program for pediatric subspecialists who are or will be working in underserved areas. Authorizes but does not appropriate $30 million each
year for FY2010-2014.
•
Primary Care Training: Authorizes but does not appropriate $125 million for FY2010 for primary care training grants. Authorizes but does not appropriate $750,000 for each year FY2010-
2014 for integrating academic units of primary care.
• Payments for Teaching Residency Positions: Requires HHS to redistribute certain
unfilled residency positions for training of primary care physicians.
• Public Health Workforce Loan Repayment: Creates a Public Health Workforce Loan
Repayment Program, authorizing but not appropriating $195 million for FY2010 and
such sums as may be necessary for FY2011-2015. Participants eligible to receive up
to $35,000 for loan repayment for each year of service.
Insurance
• Elimination of Cost-Sharing for Preventive Care in Private plans: Eliminates co-payments, co-insurance, and deductibles for preventive care for plans purchased after September 23,
2010; provides 100% coverage for preventive services.
Medicaid
• Coverage for Family Planning Services: Creates a state option to provide Medicaid coverage for family planning services to certain low-income individuals.
•
Coverage for Tobacco Cessation Programs: Requires states to provide Medicaid coverage for tobacco cessation services for pregnant women and eliminates cost sharing for these
services.
• Behavior Modification Incentives: State grants for behavior modification incentive
programs to lower chronic disease risk factors among Medicaid beneficiaries.
Authorizes $100 million in FY2011-2015.
• Primary Care Payment Increase: Increases
Medicaid payments for primary care services
provided by primary care doctors for FY2013-
2014 with 100% federal funding.
• Elimination of Cost-Sharing for Preventive Care in
Medicaid: Eliminates co-payments, co-insurance
and deductibles for preventive care; provides
100% coverage for preventive services. Increases
FMAP allocation to states for these services by
1%.
Medicare
• Elimination of Cost-Sharing for Preventive Care in Medicare: Eliminates co-payments,
co-insurance and deductibles for preventive care; provides 100% coverage for
preventive services.
• Prevention Plans and Behavior Modification: Medicare coverage of an annual wellness
visit and personalized prevention plan, which include a comprehensive health risk
assessment. Provides incentives to complete behavior modification programs.
• Heath Profession Shortage Area (HPSAs) Bonuses: Provides primary care practitioners
and general surgeons practicing in HPSAs, with a 10% Medicare payment bonus for
five years.
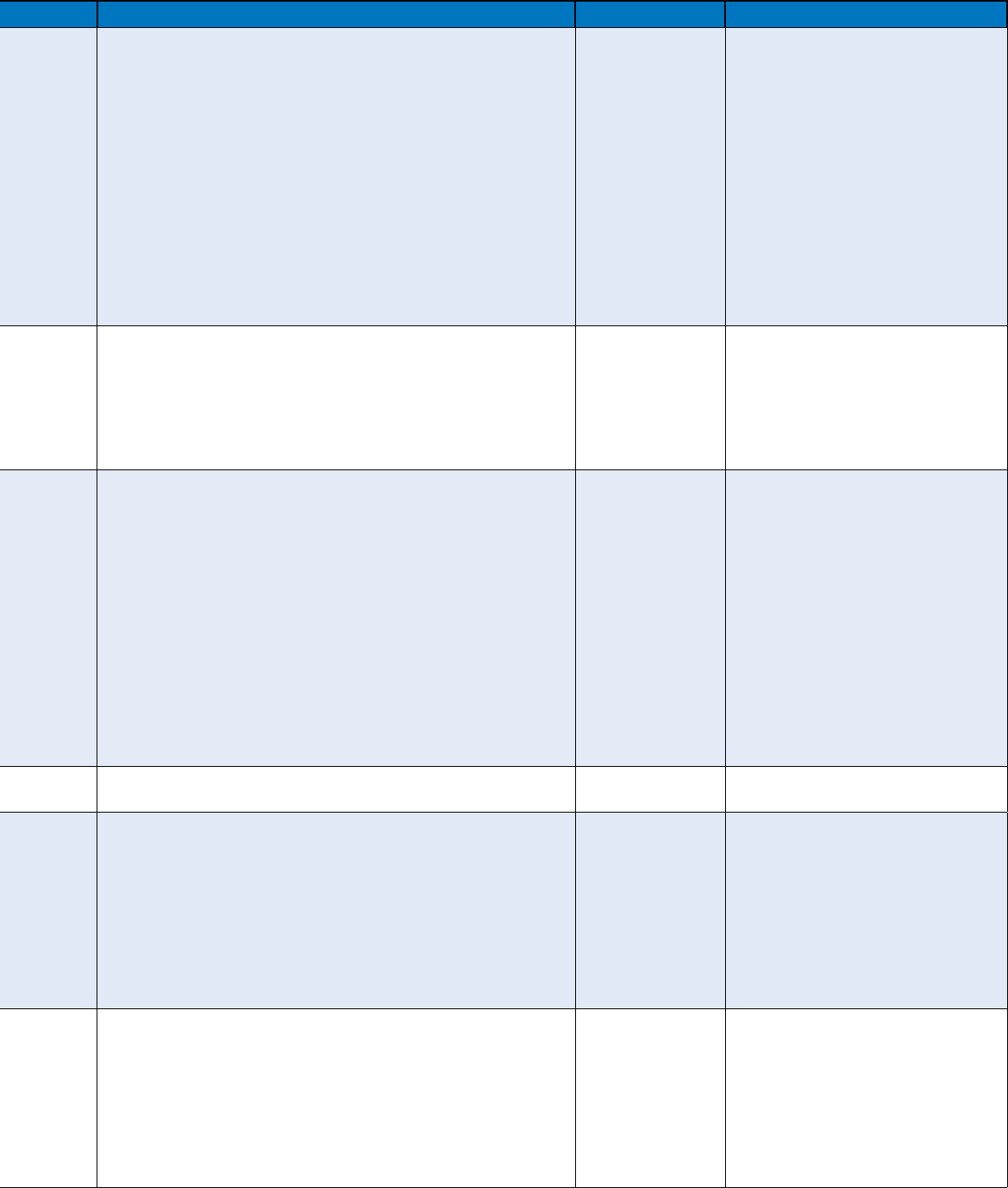
25
Appendix 1:
APHA’s Health Reform Implementation Timeline—Beyond coverage: Public health, prevention and wellness provisions
2010 2011 2012 2013
Prevention
and
Wellness
• Prevention and Public Health Investment Fund: Provides expanded and sustained national investment increasing from $500 million in FY2010 to $2 billion in FY2015 and each fiscal
year thereafter.
• National Health Promotion and Prevention Strategy: Directs an interagency council, chaired by the U.S. Surgeon General, to develop a national prevention and health promotion strategy.
• Healthy Aging, Living Well Program: Creates a pilot program to help control chronic disease and reduce Medicare costs of the pre-Medicare-eligible population.
• Pregnancy Assistance Fund: Awards competitive grants to states to assist pregnant and parenting teens and women, and victims or domestic violence and sexual assault. Authorizes $25
million each year for FY2010-2019.
• Commission on Key National Indicators: Establishes “Commission on Key National Indicators” to develop and oversee a “Key National Indicators” system. Authorizes but does not
appropriate $10 million for FY2010 ; $7.5 million from FY2011-2018.
• Community Transformation Grants: Grants to implement, evaluate and disseminate proven evidence-based community preventive health activities.
• Increased Funding for Immunizations: State grants to increase recommended immunizations in high-risk populations. Allows states to purchase adult vaccines directly from
manufacturers at HHS-negotiated price. Reauthorizes section 317 program; Authorizes but does not appropriate $1 million for FY2010.
• Maternal, Infant and Early Child Home Visitation Programs: Funding to states, tribes and territories to develop and implement one or more evidence-based Maternal, Infant, and Early
Childhood Visitation model(s). Authorizes $1.5 billion in total funding FY2010-2015.
• Personal Responsibility Education Grants: Funding to states to educate adolescents on abstinence and contraception for prevention of teenage pregnancy and sexually transmitted
infections, including HIV/AIDS. Authorizes but does not appropriate $75 million/year FY2010-2014.
• National Improvement Strategy: Develops a national quality improvement strategy
that includes priorities to improve the delivery of health care services, patient health
outcomes, and population health.
• Nutrition Labeling Requirements: Requires nutrition labeling on standard menu items
at chain restaurants and on of food sold from vending machines.
• Education and Outreach Campaign on Preventive Benefits: Requires HHS to convene
a national public/private partnership to conduct a national prevention and health
promotion outreach and education campaign; funding not to exceed $500 million.
• Oral Health Campaign:
Establishes 5-year
national public education
campaign on oral
healthcare prevention.
Demonstration grants
to demonstrate
the effectiveness
of research-based
dental caries disease
management activities.
Public Health
• Federally Qualified Health Center (FQHC): Authorizes but does not appropriate funding for FQHCs that increases from $2.98 billion in FY2010 to $8.33 billion in FY2015.
• Address Access to Care Issues: Authorizes but does not appropriate $100 million to be available through September 20, 2011 to fund infrastructure projects to expand access to care.
• School-Based Health Clinics: Creates a grant program for the operation and development of school-based health clinics. Authorizes $50 million each year for FY2010-2013 for facilities
and equipment expenditures.
• Nurse-Managed Health Clinics: Grant program, administered by HRSA, to support nurse-managed health clinics. Authorizes but does not appropriate $50 million for FY2010.
• Surveillance and Lab Capacity: Establishes a CDC grant program to improve surveillance for and responses to infectious diseases and other conditions of public health importance.
Authorizes but does not appropriate $190 million each year for FY2010-2013.
• Expansion of National Health Service Corps: Establishes Community Health Center
Fund to increase investment in National Health Service Corps. Authorizes a total of
$1.5 billion in funding increasing from $290 million in FY2011 to $310 million in
FY2015.
• Increasing Community Health Center Funding: Authorizes additional funding for
community health centers, increasing from $1 billion in FY2011 to $3.6 billion in
FY2015. Provides an additional $1.5 billion for renovation and construction.
Public Health
Workforce
• National Health Care Workforce Commission: Creates a commission charged with disseminating information on current and projected health care workforce supply and demand,
education and training capacity, retention programs, and fiscal sustainability.
• National Health Service Corps: Increases and extends funding authorization for the scholarship and loan repayment program for FY2010-2015.
• Public Health Professional Training: Training program for mid-career public health professionals. Authorizes but does not appropriate $30 million for FY2010.
• Healthcare Workforce Development: Grant program to support state and regional partnerships to complete comprehensive workforce planning and development. Authorizes but does not
appropriate $8 million in FY2010 for planning grants (entities must match at least 15% of funding) and $150 million for FY2010 for implementation grants (entities must match at least
25% of funding).
• National Emergency Corps: Establishes Ready Reserve Corps within the Commissioned Corps for service in times of national emergency. Authorizes but does not appropriate $50 million
each year for FY2010-2014.
• Allied Health Professional Loan Repayment: Loan repayment to allied health professionals employed at public health agencies or in settings providing health care to patients in
underserved areas. Authorizes but does not appropriate $30 million for FY2010.
• Pediatric Loan Repayment: Loan repayment program for pediatric subspecialists who are or will be working in underserved areas. Authorizes but does not appropriate $30 million each
year for FY2010-2014.
• Primary Care Training: Authorizes but does not appropriate $125 million for FY2010 for primary care training grants. Authorizes but does not appropriate $750,000 for each year FY2010-
2014 for integrating academic units of primary care.
• Payments for Teaching Residency Positions: Requires HHS to redistribute certain
unfilled residency positions for training of primary care physicians.
• Public Health Workforce Loan Repayment: Creates a Public Health Workforce Loan
Repayment Program, authorizing but not appropriating $195 million for FY2010 and
such sums as may be necessary for FY2011-2015. Participants eligible to receive up
to $35,000 for loan repayment for each year of service.
Insurance
• Elimination of Cost-Sharing for Preventive Care in Private plans: Eliminates co-payments, co-insurance, and deductibles for preventive care for plans purchased after September 23,
2010; provides 100% coverage for preventive services.
Medicaid
• Coverage for Family Planning Services: Creates a state option to provide Medicaid coverage for family planning services to certain low-income individuals.
• Coverage for Tobacco Cessation Programs: Requires states to provide Medicaid coverage for tobacco cessation services for pregnant women and eliminates cost sharing for these
services.
• Behavior Modification Incentives: State grants for behavior modification incentive
programs to lower chronic disease risk factors among Medicaid beneficiaries.
Authorizes $100 million in FY2011-2015.
• Primary Care Payment Increase: Increases
Medicaid payments for primary care services
provided by primary care doctors for FY2013-
2014 with 100% federal funding.
• Elimination of Cost-Sharing for Preventive Care in
Medicaid: Eliminates co-payments, co-insurance
and deductibles for preventive care; provides
100% coverage for preventive services. Increases
FMAP allocation to states for these services by
1%.
Medicare
• Elimination of Cost-Sharing for Preventive Care in Medicare: Eliminates co-payments,
co-insurance and deductibles for preventive care; provides 100% coverage for
preventive services.
• Prevention Plans and Behavior Modification: Medicare coverage of an annual wellness
visit and personalized prevention plan, which include a comprehensive health risk
assessment. Provides incentives to complete behavior modification programs.
• Heath Profession Shortage Area (HPSAs) Bonuses: Provides primary care practitioners
and general surgeons practicing in HPSAs, with a 10% Medicare payment bonus for
five years.

800 I Street, NW • Washington, DC 20001-3710 • 202-777-APHA • fax: 202-777-2534 • www.apha.org
Printed on paper containing 50% recycled content including 25% post consumer waste.
FSC logo here
A total of 126 lbs of paper containing 25% post consumer recycled fiber was used to print this brochure saving:
• 109 lbs wood - A total of 1 tree that supplies enough oxygen for 1 individual annually.
• 138 gal water - Enough water to take 8 eight-minute showers.
• 1 mln BTUs energy - Enough energy to power an average American household for 1 day.
• 33 lbs emissions - Carbon sequestered by 1 tree seedling grown for 10 years.
• 18 lbs solid waste - A total of 1 thirty-two gallon garbage can of waste.
