Engility Corporation - Full-time
Summary of Long-Term Disability (LTD) Benefits
Your Group Long-Term Disability Benefits
Steady income for longer-lasting disabilities
Coverage Effective Date: 01/01/2019
Coverage Basics
Am I eligible for
coverage?
When does coverage
become effective?
Do I have to provide proof
of good health known as
Evidence of Insurability
(EOI) to enroll?
When will coverage that
requires proof of good
health (EOI) begin?*
How much Voluntary
Long-Term Disability can
I buy through my
employer?
Are all types of illnesses
and injuries covered?
You qualify if you are an active full-time hourly or salaried employee working at least 30
hours per week.
Your Long-Term Disability coverage will begin on 01/01/2019, if you are actively at work.
New Hire/Newly Eligible: EOI is not required to enroll during your 31 - day period of initial
eligibility. If you choose not to enroll, you will be considered a "late applicant."
Annual Enrollment: EOI is required to enroll if you are a late applicant (did not enroll during
your initial eligibility period.) You will be required to submit an EOI Form (medical questionnaire)
and be approved by Aetna.
Coverage will begin after Aetna approves your EOI.
*You must be actively-at-work for coverage to begin.
You have a choice of plans that pay a monthly benefit based on a percentage of your
Pre-Disability Earnings* for a covered disability. You must submit a claim and be approved by
Aetna to receive benefits:
*Generally, Pre-Disability Earnings include your total income before taxes and any deductions for pre-tax contributions. Please
consult your Policy Documents available through your employer for additional information, including def inition of Pre-Disability
Earnings.
*
Long-Term Disability (LTD) covers injuries and illnesses that are both work-related and
non-work-related.
Disability insurance plans/policies are offered and/or underwritten by Aetna Life Insurance Company (Aetna). We are located at 151 Farmington
Avenue, Hartford, CT 06156.
26.06.305.1_(8/2016)
Page 1 of 4
©2016 Aetna Inc.
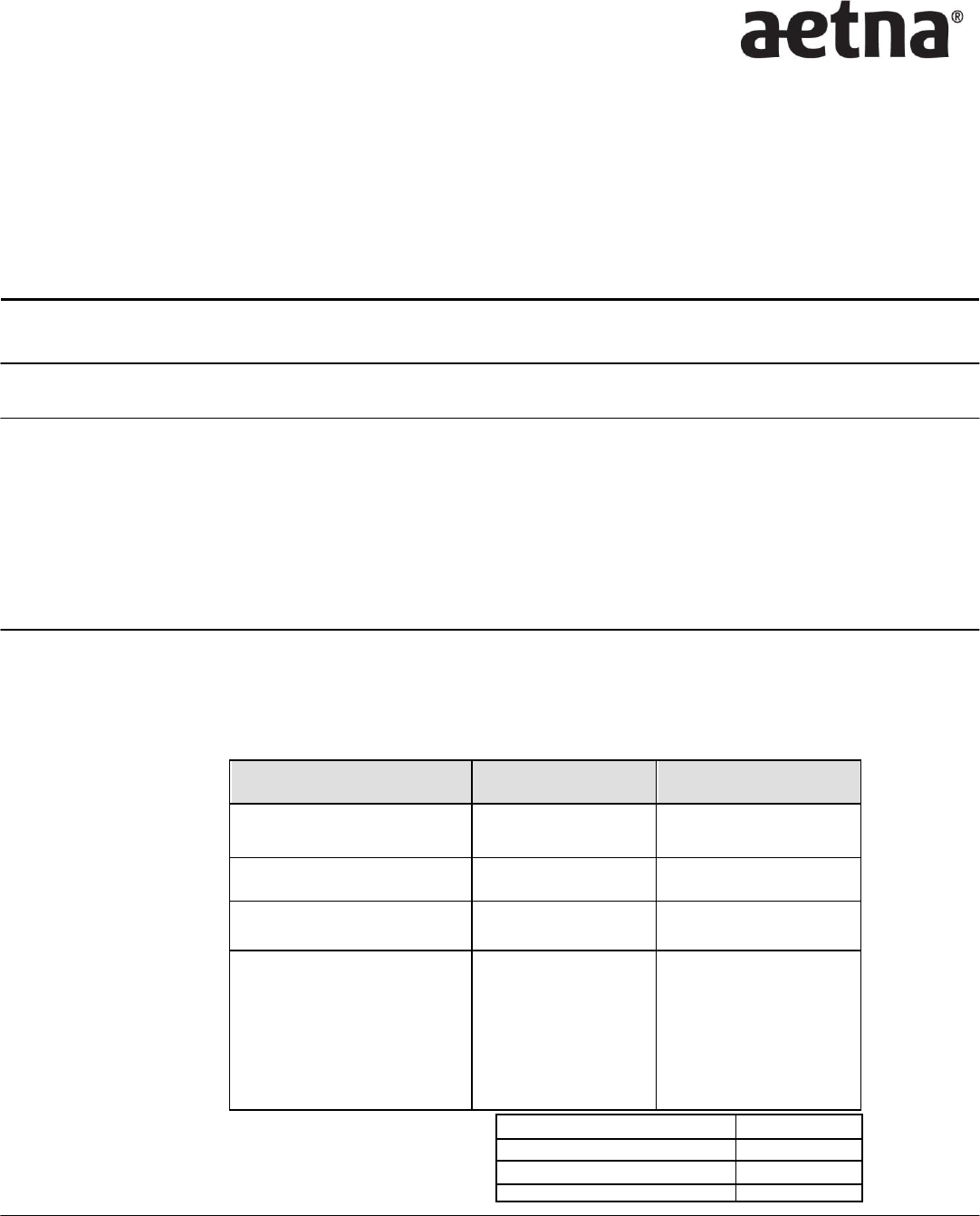
Voluntary Long-Term Disability
Option 1
Option 2
Percentage of monthly income
replacement:
50%
66
⅔
%
Maximum monthly benefit:
$10,000
$20,000
Benefits begin after a covered
Injury or Illness:
180 days
180 days
Benefits end at recovery
or:
whichever comes
first*
For disabilities starting
before age 62,
benefits
continue to age 65
.
For disabilities starting
after age
62,
benefits will
follow
a pre-deter mi ne d
sche dul e. *
For disabilities starting
before age 62,
benefits
continue to age 65
.
For disabilities starting
after age
62,
benefits will
follow
a pre-deter mi ne d
sche dul e. *
Age 62,but less than age 65
36 months
Age 65,but less than age 67
24 months
Age 67,but less than age 69
18 months
Age 69 and over
12 months
Engility Corporation - Full-time
Your Summary of Long-Term Disability (LTD) Benefits
Page 2 of 4
When am I considered to
be Disabled?
You will be considered disabled for 24 months from the date you last worked if:
After a significant mental or physical change resulting from an illness or injury, you can't
perform the material duties of your own occupation.
Your earnings are 80%, or less, of your adjusted Pre-Disability earnings.
After the first 24 months of your disability that monthly benefits are payable, you will be considered
disabled on any day that you can't perform the materials duties of any reasonable occupation*
due to illness and injury, and your earnings are 60%, or less, of your adjusted Pre-Disability
Earnings.
If your occupation requires a professional license or certification, you will not be considered
disabled solely because you lose your license or certification.
*Any "reasonable occupation" means a job you could be expected to perform satisfactorily in light of your age, education,
training, experience, station in life and physical and mental capacity.
Are there any offsets that
may reduce Long-Term
Disability?
Offsets
Your benefits may be reduced if you are receiving income from other sources. See your plan
documents for a complete listing. Examples include:
Employer sources: Government sources:
Any disability or retirement benefit
received under a retirement plan
Disability benefits received from any
statutory disability plan
Payments received from accumulated
sick time or salary continuation program
related to your current employer
Temporary disability benefits received under any
state or federal workers' compensation law
Benefits from Social Security or similar plan or
act
Income from a Governmental retirement system
earned as a result of working for your current
employer
Are there any exclusions
that apply to Long-Term
Disability?
Exclusions
You will not receive benefits under certain circumstances. Examples include:
Your disability results from an intentional self-inflicted injury; or you became injured while
committing a criminal act or driving under the influence of alcohol/drugs.
You are not under the regular care of a doctor when requesting disability benefits.
You are receiving payment under a salary continuance or retirement plan sponsored by your
employer.
Pre-existing Conditions
Pre-existing Conditions may affect the benefits paid by your Long-Term Disability policy:
A pre-existing condition is an illness, injury or pregnancy-related condition for which you were
diagnosed, received medical treatment, or prescribed medications during the 3 month period
before your coverage effective date.
No benefit will be paid for a disability that occurs during the first 12 months after your
coverage effective date that is caused by, or related to, a pre-existing condition.
Benefits will be paid for covered disabilities not related to a pre-existing condition.
Please refer to your policy documents for a complete list of income sources that will reduce your
benefits, as well as a complete list of exclusions and limitations.
Engility Corporation - Full-time
Your Summary of Long-Term Disability (LTD) Benefits
Page 3 of 4
Are there any limitations
that apply to Long-Term
Disability?
Limitations
You can receive benefit payments for Long-Term Disabilities resulting from mental illness,
alcoholism and substance abuse for a total of 24 months per occurrence. This time period may be
extended if you are confined to a hospital.
Is there anything else I
should know about my
plan?
Recurring disabilities
If you return to work and become disabled again from the same illness or injury, it may be
considered the same disability. If it is, you will only have to satisfy one elimination period and may
be eligible to begin receiving benefits immediately if:
The disability recurs during the elimination period and within 30 consecutive days of work or the
disability recurs after the elimination period and within 6 consecutive months of work.
Partial disabilities
Partial disability benefits allow you to work, earn income and continue receiving benefits so you
can receive up to 100% of your income during the first 12 months of your disability. You are
considered partially disabled if, due to an injury or illness:
You are performing some of the material duties of your own occupation
And you are earning 80% or less than your Pre-Disability Earnings
After the first 12 months, partial disability benefits can continue based on a formula that you will
find in your policy documents.
Vocational Rehabilitation and Return to Work
Our goal is to help you return to gainful employment. Consultants will review each claim to
determine if rehabilitation services would be appropriate and effective. We will work with your
employer to provide reasonable accommodations to help you return to work. You may even
qualify for an increase in your benefits by participating in a rehabilitation program.
What additional features should I know about?
Survivor Benefit If you die during a period when you qualify for disability benefits we will pay your eligible survivor a
lump sum equal to 6 months of your gross disability benefit.
Conversion If your employment ends, you may be eligible to convert to a disability conversion contract as a
temporary policy until you become insured under another group plan. This conversion plan can
provide $4,000 of LTD coverage.
How much does Voluntary Long-Term Disability cost?
Monthly Rates per $100 of Covered Monthly Payroll:
Option 1
Option 2
Rate
$0.277
$0.498
Engility Corporation - Full-time
Your Summary of Long-Term Disability (LTD) Benefits
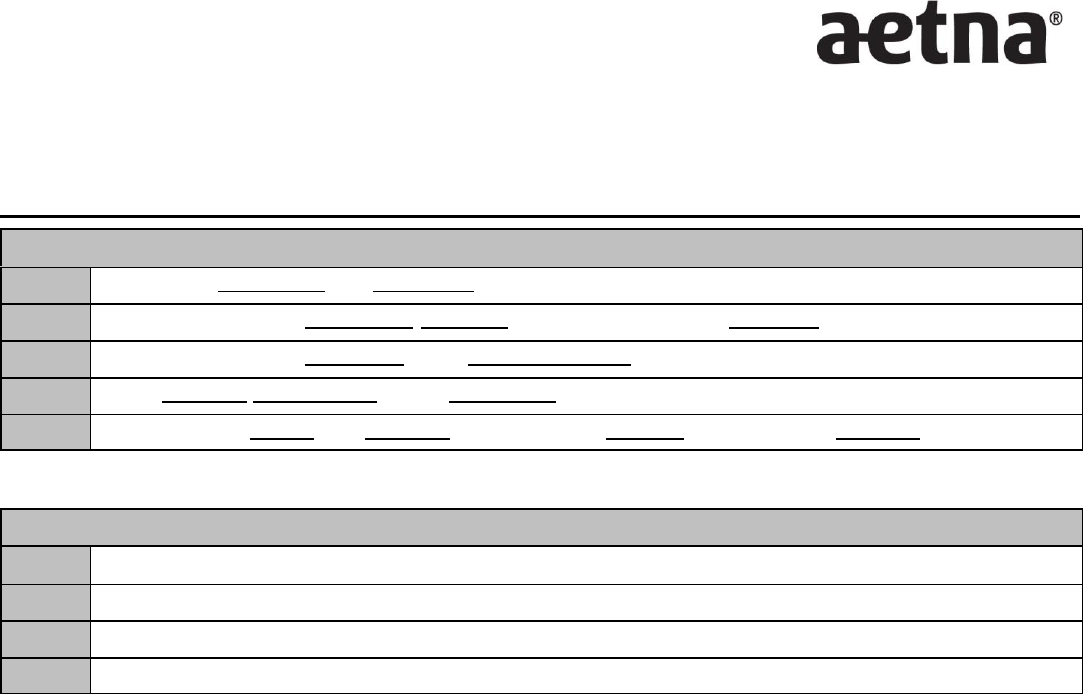
Premium calculation
Calculation:
Step 1:
Annual Salary / 12 = Covered Monthly Payroll
Step 2:
Covered Monthly Payroll x % Percentage of Benefit = Monthly Benefit*
Step 3:
Covered Monthly Payroll / 100 = # Units
Step 4:
# Units x Rate = $ Premium Per Month
Step 5:
Monthly Premium x 12 = Annual Premium / # Pay Periods = $ Payroll Deduction
*Please note: Step 2 calculates monthly benefit and is not necessary for premium calculation. Subject to $10,000.000
maximum monthly benefit.
Example: Option 1, $45,000 annual salary
Step 1:
$45,000 / 12 = $3,750.000 Covered Monthly Payroll
Step 2:
$3,750.000 x .50 = $1,875.000 Monthly Benefit
Step 3:
$3,750.000 / 100 = 37.500 # Units
Step 4:
37.500 x 0.277 (Rate) = $10.39 Premium Per Month
This material is for information only. Insurance plans contain exclusions and limitations. See plan documents for a complete description of benefits, exclusions, limitations and
conditions of coverage. Policies may not be available in all states, and rates and benefits may vary by location. Policies are subject to United States economic and trade
sanctions. Not all services are available in all states. Policy form numbers issued in Idaho and Oklahoma include: GR-9/GR-9N and/or GR-29/GR-29N.
26.06.305.1_(8/2016)
Page 4 of 4
©2016 Aetna Inc.
