
Aetna® update on Change
Healthcare service interruption
Updated July 10, 2024
On February 21, Change Healthcare took several of their services offline in response to a cyber security incident they
experienced. On June 21, UnitedHealth Group notified us that Aetna member information was included in the PHI or PII
We do not currently know which Aetna businesses or Aetna members were impacted and are waiting for additional
information from Change Healthcare regarding their plans to provide notice to impacted individuals.
Nothing is more central to us than protecting the privacy and security of our members' information. CVS Health’s
systems, including Aetna’s systems, were not compromised by the cyberattack against Change Healthcare.
More information is available at changecybersupport.com and call center support is being provided by UHG at
1-866-262-5342.
Here is a summary of the current state of Aetna support for Electronic Data Interchange transactions.
• As of April 10, we restored our connection to the Change Healthcare Electronic Remittance Advice distribution
service. See the FAQ below for additional information about accessing ERA files.
• On April 3, we restored our connection to the Change Healthcare claim intake service.
• Payment of Commercial, Individual & Family Plan, Medicare and Medicaid claims are going out on our normal
schedule.
• We have not established a timeline for reconnecting to any other Change Healthcare EDI transaction systems,
including member eligibility and benefits checks, and prior authorization submission. We will provide updates as that
changes.
For First Health: There is no disruption in EDI service between First Health clients that have a direct EDI connection with
First Health. Clients who use Change Healthcare to route claims to First Health, and are experiencing a disruption in
claims transmission, can manually key claims into our First Health online web portal.
For Aetna Signature Administrators: There is no disruption in EDI service between Aetna Signature Administrators
clients and Aetna Signature Administrators. Clients can continue to send electronic claims via normal processes. The
small percentage of paper claims sent from providers directly to Change Healthcare is under review.
This bulletin provides the latest to our network providers about how we are moving forward following the Change
Healthcare service interruption. Below is a set of Frequently Asked Questions that address the mitigation plans in place
for providers to complete transactions with Aetna. We will continue to share additional information as it becomes
available.
©2024 Aetna Inc.
3222355-02-01 (04/24)

How do providers access ERA files from Aetna?
For Commercial and Medicare claims, here is guidance on how to access ERA files:
• Providers that have not switched ERA vendors and are still using Change Healthcare can get historical ERA files
from CHC. Providers should contact CHC if they are experiencing any issues accessing their ERA files. Contact
information is provided below – providers should use the contact information for the solution they are using.
o Revenue Performance Advisor (RPA) Support: Please enter a ticket here: Customer Care Hub
o Assurance Reimbursement Manager Support: Please email [email protected] or call
1-800-457-1209.
o Clearance Patient Access Suite Support: Please email [email protected]
• For providers that have switched to a new ERA vendor, the files will be sent to that new vendor on a go forward
basis. Note, enrollment with a new vendor is not complete until the provider receives an email from Aetna
confirming the completion and effective date of the vendor change.
o
Providers that have switched to a new vendor can still access historical ERA files from CHC. The contact
information listed above can be used to contact CHC to receive those files. Providers can also ask their new
vendor to reach out to CHC to get their historical ERAs.
o Providers need all ERAs to rectify their payment postings.
o Provider must enroll with the new ERA vendor FIRST before sending their ERA enrollment form to Aetna.
o Providers may also access historical Explanation of Benefit statements on the Availity portal.
• Providers that are in the process of enrolling with a new ERA vendor or planning to do so in the future should
note the following:
o
Enrollment with a new vendor is not complete until the provider receives an email from Aetna confirming the
completion and effective of the vendor change.
o Due to volume of ERA enrollment requests, it is currently taking approximately two months to complete
processing of new enrollment forms. Please be patient.
o Provider ERA files will continue to be sent to the existing (previous) vendor until the provider receives a
confirmation from Aetna of the request to switch vendors.
o Please note that the provider must also enroll with the new ERA vendor FIRST before sending their
enrollment form to Aetna.
For Aetna Better Health (Medicaid) plan claims, here is guidance on how providers can access ERA files:
• Providers can access ECHO Health generated ERA files from the clearinghouse they have on file with ECHO Health,
via the ECHO Health portal or through the Availity Remit Viewer screen. Providers that want to update their
payment/ERA distribution preferences with ECHO Health for Medicaid claims payment may do so here.
• Access to Change Healthcare generated remits is still limited. Providers can access CHC remits back to Jan 11, 2024
through the Availity Remit Viewer screen.
• Access to other historical CHC remittances are still impacted. We are continuing to work closely with CHC to
understand their recovery timeline.
©2024 Aetna Inc.
3222355-02-01 (04/24)

What options do providers have for submitting their claims going forward?
For Aetna Commercial, Individual & Family Plan, Medicare, Dental and plans administered by Meritain Health:
With the Aetna connection to the Change Healthcare claims submission system restored, providers that want to submit
claims via CHC should work with their direct claims vendor to validate they are ready to do so. Providers may also
continue to use the other approved clearinghouse vendors, as well as our medical provider portal hosted on Availity or
dental provider portal hosted on Dental Exchange.
For Aetna Better Health (Medicaid) plans: We have restored our direct 837 claim submission capability with CHC, so
providers now have the option of submitting Medicaid claims through CHC or Office Ally.
For First Health: There is no disruption in EDI service between First Health clients that have a direct EDI connection
with First Health. Clients who use Change Healthcare to route claims to First Health, and are experiencing a disruption
in claims transmission, can manually key claims into our First Health online web portal.
For Aetna Signature Administrators: There is no disruption in EDI service between Aetna Signature Administrators
clients and Aetna Signature Administrators. Clients can continue to send electronic claims via normal processes. The
small percentage of paper claims sent from providers directly to Change Healthcare is under review.
I am a provider who submits claims to Aetna through CHC and did not select a different EDI
clearinghouse vendor to send my claims to Aetna during the service interruption. What
should I do?
Now that a portion of the CHC claim intake services are available and Aetna has reconnected to their system, you will
want to work with your direct claims vendor to validate you are ready to submit claims to Aetna. If you have claims that
you submitted around the time of the outage that were not acknowledged by Aetna, please resubmit them, including
any attachments.
What should providers do about claims submitted prior to the Change Healthcare service
interruption that are still pending or outstanding?
Providers that have claims that were submitted prior to the Change Healthcare service interruption on Feb. 21 but have
not been not acknowledged by Aetna should resubmit those claims and any correlating electronic attachments.
• For Commercial, IFP and Medicare medical claims, providers can submit through CHC once they have validated
they are ready to do so with their direct claims vendor, as well as any of the other approved clearinghouse
vendors or use our medical provider portal hosted on Availity.
• For Medicaid medical claims, providers may use CHC once they validated they are ready to do so with their direct
claims vendor or continue to use Office Ally.
• For Dental claims, providers may use CHC once they have validated they are ready to do so with their direct claims
vendor, or they may continue using NEA/Vyne or Dental Exchange.
What options do providers have for submitting “member eligibility and benefits” checks
going forward?
We have not established a timeline to reconnect to the Change Healthcare system for submitting member eligibility and
benefits checks.
For Aetna Commercial, Individual & Family Plan and Medicare: Providers may use another approved EDI
clearinghouse vendor, medical provider portal hosted by Availity or our dental provider portal hosted by Dental
Exchange for member eligibility and benefits checks.
©2024 Aetna Inc.
3222355-02-01 (04/24)
If providers work through a billing partner, practice management system or other vendor partner, they likely can
advise on an alternate connection method for electronic transactions with Aetna.
Finally, when digital submission isn’t possible, providers can utilize the Aetna Voice Advantage system. A list of
phone numbers is available for providers to select from based on the specific transaction they are calling about.
For Aetna Better Health (Medicaid) plans: Providers need to use Availity to submit electronic member eligibility and
benefits checks.
For First Health & Aetna Signature Administrators: Providers would need to work directly with the payor to
determine alternative methods.
How is Aetna paying providers?
For Aetna Better Health (Medicaid) plans: We’ve moved to national payment solutions vendor ECHO Health, to
process and distribute Medicaid claims payments to providers. Medicaid claims payments are now going out on our
normal schedule.
For Aetna Commercial, Individual & Family Plan and Medicare: Claims payment is going out on our normal
schedule for all payment methods.
How do providers utilize ECHO Health to receive payments for Medicaid claims?
Providers do not need to take additional action at this time to receive claims payment or remittance files through
ECHO Health for Medicaid claims they have submitted.
Providers that want to update their payment/Electronic Remittance Advice (ERA) distribution preferences for Aetna
Medicaid claims payment on the dedicated Aetna Better Health/ECHO portal. No fees apply when using this
dedicated portal, which is identified by the “Aetna Better Health” name in the top left of the page.
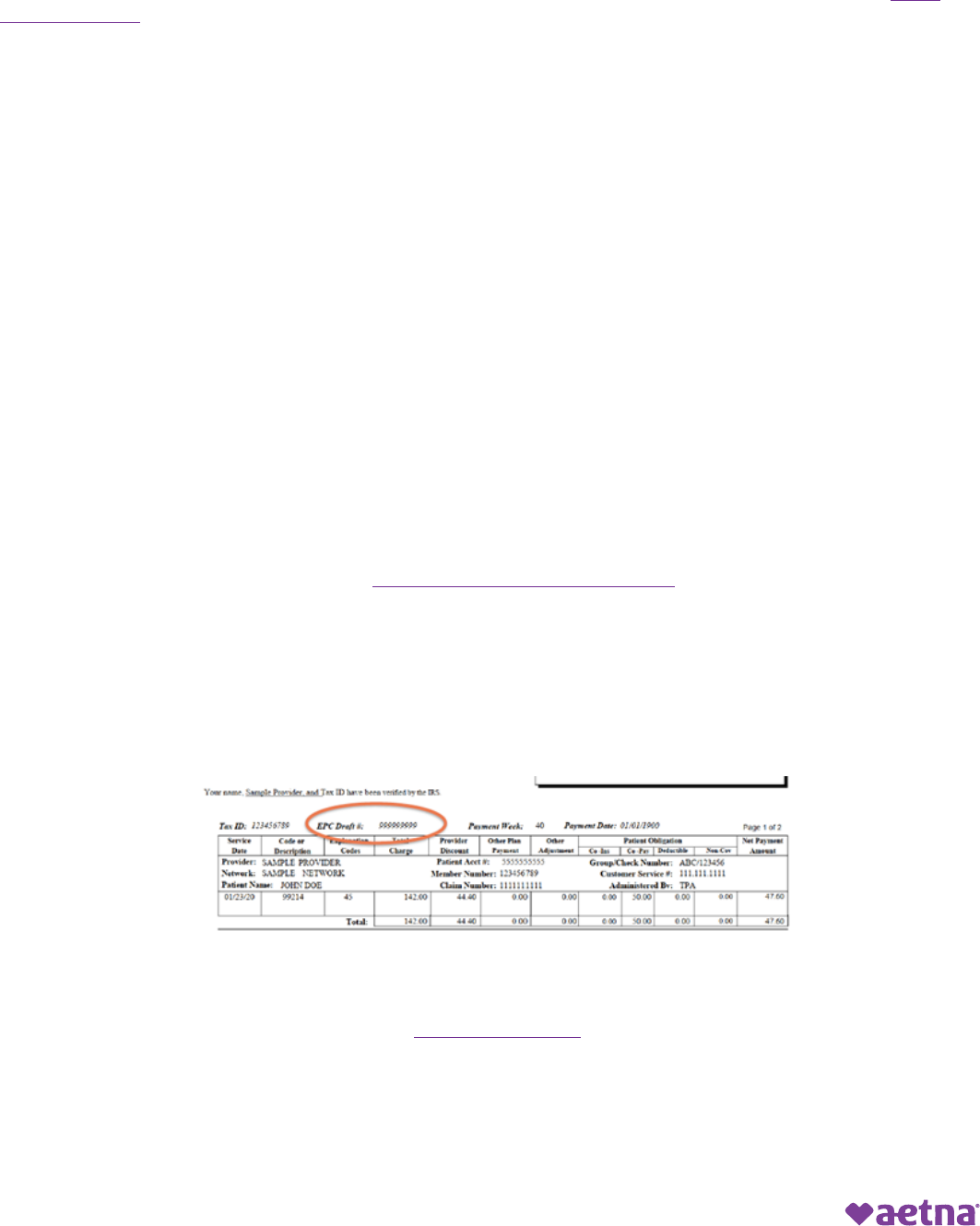
To sign up for electronic funds transfer, providers will need to provide an ECHO payment draft number and payment
amount for security reasons as part of the enrollment authentication. The ECHO draft number can be found on all
provider Explanation of Provider Payments (EPP), typically above your first claim on the EPP. If you have not received
a payment from ECHO previously, you will receive a paper check with a draft number you can use to register after
receiving your first payment.
Providers that choose to enroll in ECHO’s ACH all payer program will be charged fees, so be sure to use the Aetna ECHO
portal for no-fee processing.
To opt out of the virtual credit card option, visit our Aetna ECHO portal to manage your payments. You can also
contact ECHO directly at 1.800.830.5831. If you are not enrolled with us to receive payments via EFT and you opt out of
virtual card and have enrolled for ECHO’s Medical Payment Exchange (MPX) with another payer, you will receive your
payments in your MPX portal account. Otherwise, you will receive a paper check via print and mail.
Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life
Insurance Company and its affiliates (Aetna).
©2024 Aetna Inc.
3222355-02-01 (04/24)
