1
UNITED STATES DISTRICT COURT FOR THE SOUTHERN DISTRICT OF IOWA
Monitoring Team Report
Dates of Onsite: August 15-18, 2023
Date of Report: October 18, 2023
Submitted By: James M. Bailey, MCD-CCC-SLP
Court Appointed Lead Monitor
Teri Towe, B.S.
Alan Harchik, Ph.D., BCBA-D
Assistant Lead Monitors
Monitoring Team: Wayne Zwick, M.D
Daphne Glindmeyer, M.D.
Teka Harris, M.A., BCBA
Melanie Reeves-Miller, B.S.
Bonnie Wallington, RN, CCM
Jane Wiemerslage, B.A.
Scott Umbreit M.S
2
Table of Contents
Methodology 3
Organization of Report 3
Executive Summary 3
Summary of Compliance 4
Status of Compliance with Settlement Agreement
Section A 5
Section B 6
Section C 10
Section D 55
Section E 64
Section F 73
Section G 74
Section H 84
Section I 101
Section J 102
Section K 104
3
Methodology
undertook several activities.
a. Selection of individuals: The Monitoring Team requested various types of information
about the individuals who lived at the Center and those who had transitioned to the
community. From this information, the Monitoring Team then chose the individuals to be
included in the monitoring review. This non-random selection process is necessary for the
th all provisions of the Consent
Decree.
b. Onsite review: The Monitoring Team was present onsite at the Center.
c. Review of documents: Prior to the onsite review, the Monitoring Team requested several
documents regarding the individuals selected for review, as well as some Center-wide
documents. During the week of the review, the Monitoring Team requested and reviewed
additional documents.
d. Observations: The Monitoring Team observed individuals in their homes, day/work sites,
and other locations at GRC during regularly occurring activities. Specific activities were
also scheduled and observed, such as administration of medication, implementation of skill
acquisition plans, and mealtimes.
e. Interviews: The Monitoring Team interviewed several staff, individuals, clinicians, and
managers.
f. Monitoring Report: The monitoring report details each of the various outcomes and
indicators that comprise each section of the Settlement Agreement. A summary paragraph
is provided for each section. In this paragraph, the Monitor provides some details about the
provisions that comprise the section.
Organization of Report
relates to the Consent Decree. Specifically, for each of the lettered sections of the Consent Decree,
the report includes the following sub-sections:
a. The Moni
lettered section.
b. Indicators were developed as part of the monitoring plan and tool listed under paragraph
248. These indicators break down the Consent Decree paragraphs into measurable actions
and components.
c. Paragraphs and their related indicators were determined to be in:
a. compliance if 80% or greater consistency or presence was noted.
b. partial compliance if between 50%-80% consistency or presence was noted.
c. noncompliance if <50% consistency or presence was noted.
d. Throughout this report, reference is made to specific individuals by using a numbering
methodology that identified the individuals according to their assigned numbers.
Executive Summary
The Monitoring Team wishes to acknowledge and thank the individuals, staff, clinicians, managers,
and administrators at Glenwood Resource Center for their openness and responsiveness to the
many requests made and the extra activities of the Monitoring Team during the review. The
Center Superintendent supported the work of the Monitoring Team and was available and
responsive to all questions and concerns. Many other staff were involved in the production of
documents and graciously worked with the Monitoring Team; their time and efforts are much
appreciated.

4
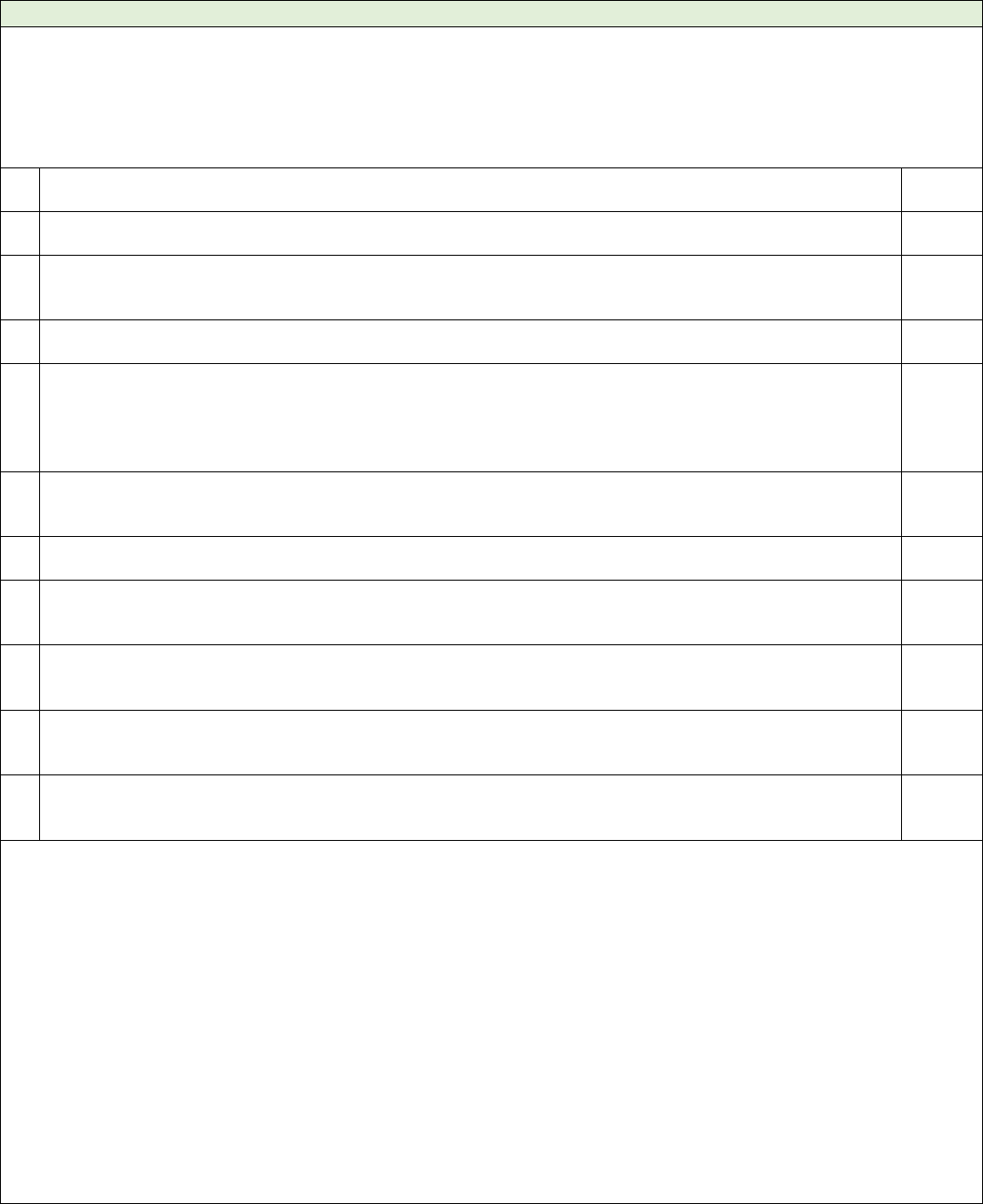
The following sections below were identified as being either in substantial, partial or
noncompliance with the Consent Decree. Sections that are in substantial compliance may no
longer be actively monitored.
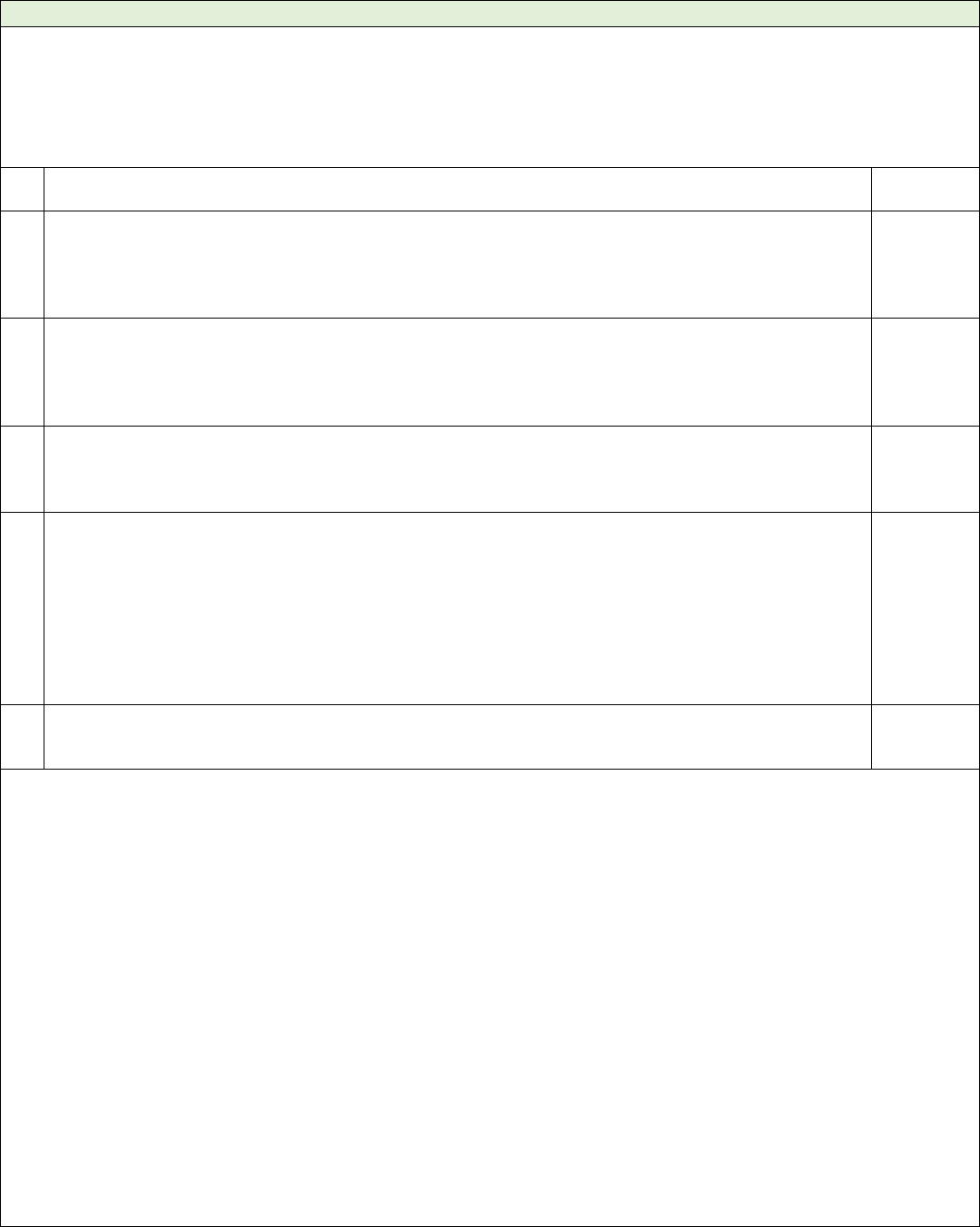
Section
Substantial Compliance
Partial Compliance
Non-Compliance
A
41-47
B
53,54,55
49
48,50,51,52,56,57
C
59,60,61,68,69,70,73,92,100,108
, 109,110,112,116,118
74,75,77,79,87,88,89,90,93,96,
102,105,107,121,122
58,62,63,64,65,66,67,
71,72,76,78,80,81,82,
83,84,85,86,91,94,95,
97,98,99,101,103,104,
106,111,113,114,115,
117,119,120
D
128,131,138,141,142,144,
145,146,147,148,149,150,151,
152
123,126,127,129,130,
124,125,132,133,134,
135,136,137,139,140,
143,153,154
E
156,157,159
155,158,160,161,162,
163
F
166
164,165
G
167,168,169
170,171,172,173,174,
175,176
H
179,180,190,
198
177, 178, 183, 197, 200,
201,202,206,207,209, 211
181,181,184,185,186,
187,188,189,191,192,
193,194,195,196,199,203
204,205,208
I
213
212,214,215
J
216,218,219,220,227,228
217, 221,223,225,226
224
K
233
229,230,231

5
Section A: Research (41-47)
Summary: A Research policy existed that would ensure informed consent by the individual and/or guardian and
guide the center in ensuring all levels of safety were in place. Per interview, there was no research currently
taking place at GRC nor was there an intent to have any in the future. Additionally, all staff of all levels had been
provided with training regarding the Research policy.
Substantial Compliance: Paragraph 41-Paragraph 47
#
Indicator
Overall
Score
1
If an individual participates in research, the
a. a. resident or guardian has provided written Informed Consent for such research.
b. Research has been independently reviewed.
(par. 41, 47)
SC
2
GRC with confirmation by the IRB will ensure any risks associated with the research are minimized and
reasonable (par. 42)
SC
3
Residents involved in research will be monitored by a staff with experience in research to ensure safety.
(par. 43)
SC
4
All residents subject to Research were free to cease participation in such Research at any time and for any
reason without perceived or actual repercussion or other negative impact to the resident. (par. 41)
N/A
5
Only trained staff conduct research. (par. 45)
SC
6
Policies and Procedures regarding Research are consistent with the provisions of this Section and with
current, generally accepted professional standards regarding the conduct of research. (par. 45)
SC
7
State shall conduct effective oversight throughout the implementation of this Agreement to detect
noncompliance with the requirements of Section IV. A
SC
Comments:
1. Individuals were not subjected to any form of research based upon the review of policies,
procedures, documentation, and interview. Per interview with the GRC Director and HHS,
research of any kind will not occur at GRC.
2. Indicators 2-7 were based on what was included in the Research policy as no individuals
were involved in any form of research. The Policy dated 5/23/22 stated that for an
individual to participate in research there must be clear informed consent and the
identified research must be reviewed to ensure risks are reviewed and all methods of
mitigation are implemented. If the individual was unable to provide such consent, then
the legal guardian may provide consent on their behalf. Any research-related proposals
were to be presented to and approved by the Human Rights Committee.
The Office of Research Integrity within HHS appeared to monitor annually for research
misconduct as noted on 1/4/22 and 1/9/23. Policies, certification, and any related
research activities were part of this review.
A list was provided showing that all staff continue to be trained in the Research Policy.
This training dated back to April 2023 and included the months of May and June 2023.
Training was provided to all levels of staffing. As of the 6/5/23, report, 91.14% of all staff
had been trained,

6
Section B: Integrated Interdisciplinary Care and Services (48-57)
Summary: ISPs generally included services, supports, and treatments. As identified in Section C, those
assessments were not always adequate for identifying needed support and treatment. An important component
of person-centered planning missing from the ISP was the determination of what skills the individual wanted to
learn and what supports were needed to participate fully in day and residential services in the most integrated
setting.
Substantial Compliance: Paragraph 53, Paragraph 54, & Paragraph 55.
Partial Compliance: Paragraph 49
#
Indicator
Overall
Score
1
Every GRC resident shall receive, consistent with current, generally accepted professional standards of
care: person-centered planning, and individualized protections, services, supports, and treatments. (par.
48)
NC
2
Every protections, planning, services, supports, and treatments are documented in the ISP.
(49,51,183)
NC
3
The ISP was updated annually, and when the service needs and preferences change (par.
49,51,179)
SC
4
a. Each resident and their LAR had the opportunity to participate in service planning meetings about their
services and had the opportunity to provide input to each of their service plans and/or revision of that
plan. (par. 49,51,183b)
SC
5
A reason for non-participation in the documentation, when applicable. (par. 49,51,183b)
NC
6
The ISP includes goals and objectives that align with and support the wishes and preferences
regarding developing skills, working, daily routines, and engagement with their community, including
community-based living options. (par. 50)
NC
7
Protections, planning, services, supports, and treatments are based on reliable comprehensive
assessments, conducted routinely and in response to significant changes in the life. (par. 52)
NC
8
The individual and/or guardian provided informed consent confirmed in writing following disclosure and
understanding of all benefits and risks of supports and services and appropriate strategies, if any, to
mitigate the risks. (par. 53)
SC
9
IDT members are knowledgeable regarding ISP outcomes, supports and services for individuals. (par. 54)
SC
10
Individuals and their guardians are informed of changes in treatment, supports and services. (par. 55)
SC
11
The responsible IDT member(s) for each program or support included in the ISP reviewed and analyzed
the data and other information necessary to assess the physical and behavioral health status
progress and the effectiveness of current interventions at least monthly but more often if needed. (par 56)
SC
12
Monthly reviews include reviewing data for any emerging risks. When emerging risks are identified, an
At-Risk Plan shall be developed and implemented (par. 56a, 78, 79)
NC
13
There was reliable and valid data to determine if the individual met, or is making progress towards
achieving, his/her overall personal goals. (par. 56c)
NC
14
The individual met or is making progress towards achieving his/her overall personal outcomes.
(par. 56d)
NC
15
If personal outcomes were met, the IDT met and updated or made new personal outcomes (par. 56e)
N/A
16
If the individual was not making progress, activity and/or revisions were made (par. 56f)
N/A
17
If there was disagreement among team members, the issue was resolved through the State resolution
process including external clinical consultations, when appropriate. (par. 57)
N/A
Comments:
1. The Center attempted to involve individuals and their guardians in the ISP process by
inviting them to attend annual ISP meetings, other IDT meetings, and monthly review
meetings. The ISP did not document how individuals participated in the meetings or
what support, education, and training was offered to individuals to support meaningful
participation and self-advocacy.
Facility staff recently completed person-centered planning training. The sample of ISPs
reviewed pre-dated the recent training, so the Monitoring Team was unable to determine
if person-centered planning principles were used to guide ISP development. It was

7
positive to see that a person-centered preference assessment was completed for each
individual in the review group.
To review this section of the Consent Decree, a set of ISPs was reviewed. Individuals and
their guardians routinely participated in the development of the ISP.
Person centered planning should be used as part of a discovery process to identify
as such as recreation, relationship, housing, vocational
preferences, and/or other meaningful day activities. That discovery process should drive
the development of an ISP that outlines supports, services, and training focused on
helping the individual achieve their vision for what their life might look like in a less
restrictive setting. GRCs ISP process was centered around activities available at the
facility and identification of living options that might be available to support the
individual
2. The ISP documented various assessment findings and recommendations, including
supports needed, but that information was not integrated into one comprehensive plan
that was bas, including preferences
for living options, working, daily routines, opportunities for community integration, and
building relationships.
For all individuals, many assessments were not submitted at least five days prior to the
annual ISP meeting, so those support needs and recommendations could not be
integrated into the ISP. When available, they were oftentimes pasted into the ISP
document with no evidence of discussion.
3. Each individual had an ISP that was updated at least annually. Changes were made
throughout the ISP year when warranted within the monthly integrated review process.
4. For five of seven individuals, the individual and their LAR had the opportunity to
participate in service planning meetings about their services and had the opportunity to
provide input to each of their service plans and/or revision of that plan. Individual #30
and Individual #s did not attend their annual ISP meetings. Other
opportunities for participation/input were not documented.
5. For the two guardians that did not attend annual ISP meetings, a reason for non-
participation was not found in the documentation provided.
6. ISPs did not provide opportunities for individuals to explore new activities, particularly
related to work and day programming. None of the ISPs included goals and objectives
related to work and day programming other than to increase attendance. Some
individuals spend most of the day in their homes with limited opportunities for
engagement or exposure to new activities. All individuals had opportunities to go on
excursions into the community. IDTs were documenting data related to where the
individual went,
the outing. Documenting this detail might have led to recommendations for day and
vocational supports to include in discharge/transition planning.
• Individual #39 had attended day programming three days in the past six months. He
had been on three community outings in the same period.
• Individual #29 attended day programming eight times in the past six months (three
or fewer days per month). He had been on 10 community outings over six months.
• Individual #30 consistently attended work daily. He was scheduled for various jobs
including at the greenhouse and recycling center. He had been on 23 community
outings over the past six months.
• According to data provided to the Monitoring Team, Individual #42 had attended
day programming one time over the past six months. He had been on 12 community
outings over the past six months.

8
• Individual #31 was scheduled to work delivering mail less than two hours per day.
He worked between six and 18 days per month over the past six months. There was
no other evidence provided of routine participation in day programming. He had
been on eight community outings over the past six months.
• Individual #78 had participated in day programming six times over the past six
months. He had been on 15 community outings.
• Individual #79 chose to work at the recycling center part-time and attend day
programming at the building 102-day program. She worked 47 days over a four-
month period and attended the building 102-day program from four to nine times
per month over the same period.
None of the action plans offered opportunities to explore community-based activities or
engage in integrated activities in the community, such as banking, going to church,
participating in retirement programs, joining community groups, attending classes,
volunteering, etc. so that individuals were better able to make informed choices
regarding what they wanted to do during the day and where they wanted to live.
7. Relevant assessments were missing for all individuals prior to ISP development, so it was
unlikely that protections, planning, services, support, and treatments could be based on
reliable comprehensive assessments that were conducted routinely and in response to
significant changes in the individuallife. See H.1.8 for more detail on late and missing
assessments prior to ISP development. Comments on the quality of assessments are
included in Section C.
8. IDTs met often to review changes in services and support, individuals and their
guardians were invited to participate in discussions. There was evidence that guardians
were routinely contacted when supports were added or changed. Consent was
documented for most changes, however, there were instances where documentation was
not found to confirm that individuals and their guardians had provided informed consent
regarding the benefits and risks of all treatments and supports. For example,
• Individual #79 was started on a new prescription for Depakote in May of 2023.
There was no evidence that the benefits and risks were discussed with the individual
or guardian or that they signed consent for this treatment. On 5/11/23, the IDT met
to discuss Botox injections for hip pain. The guardian was not present at the meeting.
The IDT approved treatment without documenting discussion with the guardian.
9. IDT members were knowledgeable regarding ISP outcomes, supports, and services for
individuals. Multiple QIDPs and direct support staff were interviewed throughout the
10. Individuals and their guardians were informed of changes in treatment, supports, and
services through communication with the QIDP and monthly integrated reviews.
Additionally, IDT meetings were held when there was an immediate need for discussion.
Individuals and guardians were invited to participate in all IDT meetings, as well.
11. The monthly integrated review process was the process in place to review the status of
all services and supports at least monthly.
• For Individual #42, the MIR did not document a review or data related to each
recommended supports and services. Missing were behavioral,
psychiatric, and program data.
• For Individual #30, Individual #29, Individual #29, Individual #78, Individual #79,
and Individual #31, there was no data or evidence of IDT review related to most
services and supports.
12. Monthly reviews for all individuals included a process for reviewing data for any
emerging risks. When emerging risks were identified, a plan was to be developed and
tracked for implementation. However, they were not shared with the IDT, so that plans
were revised when needed. See details regarding the assessment of risks and data
collection in section C.iv.3

9
13. -16. Missing from all monthly integrated reviews were data related to personal goal
achievement, so progress could not be determined. IDTs were not developing
measurable action steps for achieving personal goals and QIDPs were not commenting
on whether progress towards goals had been made. See additional comments for H.i.6
regarding personal goals.
17. There was no documented evidence of disagreement among team members to review.

10
Section C: Clinical Care (58-67)
Summary: Overall, GRC residents did not receive quality integrated preventative, chronic, and acute clinical care,
and services, including psychiatric, psychological, medical, nursing, pharmaceutical, pain management, seizure
management, and habilitation therapy services, consistent with current, generally accepted professional
standards of care.
Substantial Compliance: Paragraph 60
#
Indicator
Overall
Score
1
GRC residents shall receive quality integrated preventative, chronic, and acute clinical care, and services,
including psychiatric, psychological, medical, nursing, pharmaceutical, pain management, seizure
management, and habilitation therapy services, consistent with current, generally accepted professional
standards of care. (To meet criteria with this indicator, all the indicators for Section C must be met.)
NC
2
Assessments shall be performed on a regular basis and in response to developments or changes in a
medical, behavioral, or functional status to ensure the timely detection of and response to
needs. (par. 59,74,82)
NC
0%
0/14
3
Diagnoses shall be clinically appropriate and consistent with the current Diagnostic and Statistical Manual
of Mental Disorders and the International Statistical Classification of Diseases and Related Health Problems.
(par. 60)
SC
100%
14/14
4
Treatments, supports, and interventions shall be timely and clinically appropriate based upon assessments
and diagnoses. Clinicians shall conduct direct assessments consistent with current, generally accepted
professional standards of care. (par. 61,74,76,106,111)
NC
44%
4/9
5
Clinical indicators of the effectiveness of treatments, supports, and interventions shall be determined in a
clinically justified manner. (par, 62,84,96)
NC
44%
4/9
6
Clinical indicators of the effectiveness of treatments, supports, and interventions shall be effectively
monitored. (par. 63,84,97)
NC
44%
4/9
7
Treatments, supports, and interventions shall be modified in response to the results of monitoring of clinical
indicators. (par. 64)
NC
44%
4/9
8
GRC shall routinely collect, analyze, and act on valid and reliable data sufficient to ensure that the clinical
care and services provided to GRC residents are consistent with current, generally accepted professional
standards and implemented in an appropriate manner. Where such data show that clinical care and
services, or their implementation, do not meet such standards, GRC clinical staff shall appropriately address
the deficiency. (par, 65)
NC
9
quality management system shall include processes to ensure that the provision of clinical care and
services at GRC are consistent with current, generally accepted professional standards and implemented in
an appropriate manner. The State shall ensure data related to the provision of clinical care and services is
shared with Quality Management program and that the data is valid, analyzed, and utilized for
quality improvement, pursuant to the processes set forth in Section IV.K. (par.66)
NC
10
Whenever problems are identified under the processes set forth in Paragraphs 65-66, GRC shall develop and
implement plans to remediate the problems. (par. 67)
NC
Comments:
1. Examples of current challenges included gaps in preventive care, specifically, not
following current immunization guidelines for several of the reviewed individuals. Other
examples included documentation gaps concerning progress notes with the required
components when reviewing consultations, post hospital progress notes until resolution
of the illness and stabilization of the individual, and lack of interval medical reviews.
2. Assessments were only performed on a regular basis at the time of the annual review.
There was no evidence of a 90-day review, which is recommended for this population of
individuals with complex medical and psychiatric challenges.

11
3. All diagnoses were clinically appropriate and consistent with the current Diagnostic and
Statistical Manual of Mental Disorders and the International Statistical Classification of
Diseases and Related Health Problems.
4. For four of nine (44%), there was lack of ongoing monitoring for those individuals
hospitalized and discharged back to the facility. Two synchronous days of follow-up with
documentation of assessment is expected for all hospitalizations. For the following
individuals, two daily PCP post hospital follow-up notes were lacking: Individual #78
hospitalization on 5/12/23-5/19/23, and hospitalization 4/29/23-5/2/23, Individual
#42 hospitalization on 4/4/23-5/5/23, Individual #39 hospitalization on 1/29/23-
1/31/23, and Individual #29 hospitalization on 5/19/23-5/22/23. A transfer note by the
PCP for ED visits and hospitalizations that reviewed the events leading up the transfer
was not always completed (Individual#39, transfer to ED 1/29/23).
5. For indicators 5-7, treatments, supports, and interventions needed improved
documentation when returning from a hospitalization (Individual#78, Individual #42,
Individual #39, and Individual #29). There was no daily close monitoring post
hospitalization until stabilization of condition was documented by the PCP. Without
sufficient monitoring, effectiveness of treatment could not be determined. Whether
modification of clinical treatment was needed likewise was not documented. The medical
record was often lacking when an acute illness was resolved, as there was no closure note
confirming resolution of the acute problem.
8. GRC submitted documentation that included a Monthly Quality Indicator Report for the
months of January 2023-June 2023. This included data on lacerations requiring sutures or
Dermabond, fractures, ER visits, hospitalizations, infirmary/quarantine, bowel
obstruction, dehydration, and medication variance.
Information was not analyzed to target areas needing improvement, and there were no
action steps and responsible parties with timelines to resolve the concern.
9. GRC submitted documentation minutes of the Medical Quality Council dated 4/11/23,
5/9/23, 6/13/23, and 7/11/23. Analysis of the most recent 12 months of data was
reviewed for any trend in multiple health care indicators. Indicators reviewed each month
included aspiration pneumonia, dehydration, bowel obstruction/ileus, respiratory
infections, urinary tract infections, health care related infections, ER visits/on campus
transfers/hospitalizations, skin breakdown, lacerations requiring closure with sutures or
Dermabond, underweight status, obese status, and unplanned significant weight change.
These Quality Council Meeting minutes provided evidence that the medical department
data were shared with the GRC Quality Management program. Also see Indicator 10
below.
10. Trends were identified in the most recent rolling 12 months of data, but there was no
discussion about which trends were significant and needed an action plan and responsible
department for the minutes of 4/11/23-6/13/23. That is, whenever problems were
identified, there was no information as to the creation and implementation of corrective
steps involving one or more of the healthcare departments. For the 7/11/23 meeting, the
minutes indicated two recommendations with assigned party and follow-up date. The
recommendations were specific to individual events. It was a positive step that the
medical director was acting on the rich database accumulated. There was no systemic
recommendation identified leading to an action step. A separate Interdisciplinary QI data
form was submitted that provided a summary of data per areas of risk, listed as a total per
month for each of the defined risks.
12
Section C.i – Supervision and Management of Clinical Services (68-72)
Summary: GRC provided appropriate and competent supervision of clinical services and employed sufficient
medical staff. Areas to focus included the ability to update Face sheets to ensure appropriate and relevant data
as well as the development of action steps with assignment of responsible party and follow-up date to resolution
for any medical concern.
Substantial Compliance: Paragraph 68, Paragraph 69, & Paragraph 70.
#
Indicator
Overall
Score
1
Appropriate and competent supervision and management of clinical services by individuals with
appropriate training and credentials. (par. 68)
SC
2
GRC shall employ adequate numbers of clinical staff with appropriate training, credentials, competence, and
expertise to provide the clinical services identified herein to a reasonable caseload of individuals with IDD
consistent with generally accepted professional standards of care (par. 69)
SC
3
Clinical staff shall demonstrate maintenance of the requisite training, credentials, competence, and expertise
throughout their period of employment. (par. 70)
SC
4
The State shall regularly have board-certified clinicians, who do not have a professional or personal
relationship with GRC clinicians or GRC Leadership, assess the adequacy of clinical services in the clinical
areas for which they are board-certified, including, at a minimum, all medical staff. The assessment findings
shall be written and shared with the clinician whose work was the subject of the review and the
supervisor. (par. 71)
NC
5
Action steps to remediate identified issues shall be developed, as necessary. The findings, action steps, and
rationale for not acting steps shall be provided to and reviewed by the Superintendent and HHS Central
Office as part of a comprehensive oversight process. (par. 71)
NC
6
Clinical services shall engage in and be subject to Quality Management, including appropriate peer review
and appropriate mortality reviews. (par. 72)
NC
7
For an individual who has died, the clinical death review is completed within 21 days of the death unless the
Facility Director approves an extension with justification, and the administrative death review is completed
within 14 days of the clinical death review. Pre Clinical peer review, then post peer review. (par. 72)
NC
0%
0/1
8
Based on the findings of the death review(s), necessary clinical recommendations identify areas across
disciplines that require improvement. (par. 72)
SC
100%
1/1
9
Based on the findings of the death review(s), necessary training/education/in-service recommendations
identify areas across disciplines that require improvement. (par. 72)
SC
100%
1/1
10
Based on the findings of the death review(s), necessary administrative/documentation recommendations
identify areas across disciplines that require improvement. (par 72)
N/A
Comments:
1. The medical director was an MD who provided appropriate oversight. Examples of quality
oversight included the morning medical meeting minutes as well as the periodic reviews
completed by the medical director of medically complex challenging individuals (located
in the electronic record as physician progress notes).
2. There were two APNs assigned to a census of 71, which was a manageable caseload.
3. Training documents indicate ongoing continuing education for the medical director and
two APNs.
4. There were no external medical peer review reports for any clinical cases at GRC
(excluding a mortality review). There was a one-time review by external medical peers
concerning individuals on specific medications as listed in the Consent Decree. However,
there was no evidence of a regularly scheduled external peer review of a challenging case
or grand rounds equivalent involving ongoing clinical care of an individual at GRC.

13
5. Several policies were in place at the time of the Monitoring Team visit on 8/15/23, with
further revision since the last Monitoring Team visit (March 2023) These included an
Antibiotic Stewardship Program Procedure with Revised McGeer Criteria for Infection
Surveillance Checklist, with an effective date of 4/4/23 and revision date of 4/24/23. Skin
Integrity Breakdown Monitoring Procedure with an effective date of 4/13/23 and revised
4/23/23.
An area of concern was the inability to update the Face sheet with current new diagnoses,
as well as update the MAR with newly identified allergies. Currently, the medical team did
not have access to this process, despite placing orders for these changes in the electronic
medical record. Discharge planning would use the MAR and face sheet in planning. This is
an area of critical importance, as new diagnoses need to have a care plan at the time of
discharge. More critically, allergy information should be updated without any delay in the
EMR to be available for discharge planning. This is an area needing resolution, especially
with adding critical information, such as allergies in a timely manner to MARs. This is an
example of a systemic issue identified, but without resolution.
6. The Medical Quality Council met on 4/11/23, 5/11/23, 6/13/23, and 7/11/23. Data were
reviewed in the areas of infection control, falls, nursing/ medical quality indicators, and
medication variance. The facility-wide Quality Council meetings listed health care data in
their meeting minutes of February 2023 (the date of the meeting was not recorded in the
minutes/report), March 2023 (the date of the meeting was not recorded in the
minutes/report). April 2023 (the date of the meeting was not recorded in the
minutes/report), May 2023 (the date of the meeting was not recorded in the
minutes/report), and 7/18/23.
Topics that had data provided monthly included aspiration pneumonia, dehydration,
bowel obstruction/ileus, respiratory infection, urinary tract infections, healthcare related
infections, ER visits/on campus transfers/ hospitalizations, skin breakdown lacerations
requiring closure with sutures or Dermabond, underweight persons, obese persons, and
persons with an unplanned significant weight change. Although there was considerable
data collection, there were no action steps with assignment of responsible party and
follow-up date to resolution for any medical concern. This was of concern due to the
relatively high number of respiratory-related hospitalizations.
For the one mortality in the time period reviewed during this Monitoring Team visit, there
were two external peer reviews completed.
7. For Indicators 7-9, Individual #9s DOD was 3/29/23, and the PCP review was completed
on 4/10/23. An autopsy report was completed 4/2/23 and received by GRC 4/24/23. The
first committee meeting 4/24/23 reviewed whether death was expected. There was a
Mortality Review Committee Report dated 4/25/23 with signature 5/12/23 by the
Director of Quality Management with recommendations: 1. Train all Area 1 and Area 2
direct support staff and supervisors on the Code blue Protocol. 2. Retrain all nursing staff
on NEWscore findings and how to report the information in real time when making
notifications to the provider. 3. Train all medical providers in requesting NEWscore
findings if not reported by nursing during notification of sudden change in health status.
There was a Type 1 Incident Investigation Report (final facility administration report)
dated 5/17/23 with no recommendations. These were beyond the benchmark timelines
for this section. For recommendation 1., training occurred 3/29/23-6/1/23. For
recommendation 2. Training occurred: 4/5/23-4/21/23. For recommendation 3, training
occurred 6/6/23 for two medical department staff.
Additional questions to be answered may include defining the main cause of death (which was
determined by the autopsy in this case), potential contributing factors/comorbid conditions that
led to the death, whether there was appropriate management for chronic medical conditions
that may have impacted the death, a review of preventive care (were immunizations up to date,
preventive cancer/health maintenance screens up to date, documentation of appropriate acute

14
care in the 3 to 6 months prior to death, and whether additional supports or services would have
changed the outcome of the final illness. The final statement that should be documented is
whether the mortality review committee determined the death was preventable or not.
Additionally, what was striking is that only nursing and medical services reviewed the death.
Input from habilitation services, psychiatry services, and behavioral health services would be
appropriate to review the death from their perspective. The contract clinical PharmD should also
review the medications leading up to the time of death for any comments concerning
polypharmacy, dosage concerns, drug interactions, etc.

15
Section C.ii. Medical Services (73-76)
Summary: Individuals received a timely annual medical assessment as well as prior to hospitalization. Lacking
was timely follow-up care upon return from the hospital and timely preventive care. Other issues noted, but
were not limited to timely labs and proper review and acceptance of consultations.
Substantial Compliance: Paragraph 61, & Paragraph 73.
Partial Compliance: Paragraph 74, & Paragraph 75.
#
Indicator
Overall
Score
1
Medical Director at GRC is board certified and has the expertise to lead the Center forward. (par. 73)
SC
2
Individual has an annual medical assessment (AMA) that is: (par. 61)
i. Completed within 365 days of prior annual assessment; and
ii. No older than 365 days
SC
100%
7/7
3
The Individual has timely periodic medical reviews, based on their individualized needs, but no less than
every three months or within 30 days of planned discharge. For individuals with all areas of defined risk
that are considered stable for the prior year, the medical director may determine a periodic review of every
6 months is clinically appropriate. This decision should be recorded in the AMA POC at the beginning of the
POC section. If an area of risk changes and requires a change of medications, non-routine consultations,
change of supervision level, etc., then the periodic review reverts to every 3 months. (par. 61)
NC
0%
0/14
4
Individual receives quality AMA, including:
i. Prenatal history
ii. Family history
iii. Social/Smoking/Alcohol/Drug use
iv. Childhood illness
v. Past medical history
vi. Interval history
vii. Allergies
viii. List of meds
ix. Physical exam with vitals
x. Laboratory information
xi. Active Problem List
xii. Plan of Care for each medical issues (as appropriate)
xiii. Plan for monitoring
(par. 58-64)
NC
0%
0/7
5
Individual receives timely preventative care including:
i. Immunizations
ii. Colorectal screening
iii. Breast cancer
iv. Hearing and Vision
v. Osteoporosis
vi. Cervical caner
(par. 61,74)
NC
29%
2/7
6
If the individual experiences an acute medical issue that is addressed at the Facility, the PCP or other
provider assesses it according to accepted clinical practice, including:
i. Timely assessment based upon the clinical needs.
ii. Review of the history of the problem.
iii. Source of the information
iv. Focused PE including documentation of all positive and relevant negative findings.
v. Review/summary of most recent diagnostic or lab tests/results, including documentation of
relevant normal or negative results.
vi. A definitive or differential diagnosis that clinically fits the corresponding evaluation or assessment,
vii. Plan for further evaluation and monitoring by PCP and related staff.
(par. 58-64, 74)
PC
67%
4/6

16
7
If the individual receives treatment for the acute medical issue at the Facility, there is evidence the PCP
conducted follow-up assessments and documentation at a frequency consistent with the status
and the presenting problem until the acute problem resolves or stabilizes. (par. 58-64, 74)
PC
75%
3/ 4
8
If the individual requires hospitalization, an ED visit, then, the individual receives timely evaluation by the
PCP or a provider prior to the transfer, or if unable to assess prior to transfer, within one business day, the
PCP or a provider provides an IPN with a summary of events leading up to the acute event and the
disposition. (par. 74)
SC
89%
8/9
9
As appropriate, prior to the hospitalization, ED visit, or Infirmary admission, the individual has a quality
assessment documented in the PCP progress note, including:
i. Vitals
ii. Review of most recent s/s (up to 5 days)
iii. Assessment including pertinent history, physical findings, lab tests, and pending consults/tests.
iv. Working diagnosis
v. At time of transfer, reason for sending person to ED.
(par 74)
SC
100%
5/5
10
Prior to the transfer to the hospital or ED, the individual receives timely treatment and/or interventions for
the acute illness. (par. 74)
SC
100%
9/9
1
11
If individual is transferred to the hospital, PCP or nurse communicates necessary clinical information with
hospital staff. (par. 74)
SC
89%
8/9
12
The individual has a post-hospital IDT mtg that addresses follow-up medical, and healthcare supports to
reduce risks and early recognition, as appropriate. (par. 74)
SC
86%
6/7
13
Upon the return to the Facility, there is evidence the PCP conducted follow-up assessments and
documentation at a frequency consistent with the status and the presenting problem with
documentation of resolution of acute illness. (par. 74)
NC
44%
4/9
14
If the Individual needs a consultation, one is ordered in a timely manner. (par. 75a)
SC
100%
14/14
15
The consultant is provided with the needed background and history to provide an informed assessment and
the desired question to be answered. (par. 75b,75c)
S C
93%
13/14
16
If the individual has non-Facility consultations that impact medical care, the PCP indicates agreement or
disagreement with recommendations. (par. 75d)
NC
8%
1/13
17
PCP completes review within five business days, or sooner if clinically indicated. (par. 75e)
SC
85%
11/13
18
The PCP writes an IPN that explains the reason for the consultation, the significance of the results,
agreement, or disagreement with the recommendation(s), and whether there is a need for referral to the
IDT. (par. 75e)
NC
0%
0/13
19
If PCP agrees with consultation recommendation(s), there is evidence it was ordered. (par. 75e)
SC
100%
13/13
20
The PCP, in consultation with appropriate IDT members, documents the basis for agreeing or
disagreeing with the
obt1aining a second opinion), or the basis for taking no action. (par. 75f)
NC
0%
0/13
21
GRC will ensure:
i. Timely initiation of laboratory and diagnostic testing.
ii. Urgent notification of critical results
iii.
circumstances,
(par. 76a,76b,76c)
NC
43%
3/7
17
Comments:
1. The Medical Director was Board Certified in Internal Medicine (1988). His curriculum
vitae indicated extensive clinical leadership role in diverse clinical settings for more than
25 years.
2. All annual medical assessments were completed within the last 365 days and were
completed within 365 days of the prior annual medical assessment.
3. None of the individuals had timely periodic medical reviews, based on their individualized
needs. Except for the annual history and physical, the facility did not have a system in
place requiring routine interval medical reviews at 90-day intervals or any other time
interval (180 days if clinically stable without any changes in medical history or
medications). There were no interval medical reviews submitted.
4. Zero of seven individuals received a quality AMA. The AMA had deficits in the following
areas:
• Individual #78, Individual #42, Individual #30, Individual #39, Individual #79, and
Individual #29 were missing information regarding family history and
social/smoking history. Lack of family history may impact the scheduling of future
preventative tests and deter early identification.
• Individual #31 was missing social/smoking history.
5. Two of the seven individuals (29%) received timely preventative care. Gaps in preventive
care included:
• Individual #78 immunizations (lack of Prevnar 20 and Shingrix), #42 immunizations
(lack of Prevnar 20 and Shingrix).
• Individual #39 immunizations (lack of Prevnar 20 and Shingrix).
• Individual #79 lack of follow-up to an incomplete colonoscopy 3/31/22.
• Individual #30 immunizations (lack of COVID 19 booster, Prevnar 20, and Shingrix).
From the submitted documentation, one was unable to distinguish if a guardian or other
legal representative refused consent for a vaccine.
The above information was based on the time period reviewed. There was information
provided by the medical director of awareness of the need for updating vaccinations, and
consents were in the process of being obtained for vaccinations, The immunization record
was also confusing for Tdap. It appeared to record DTaP (a pediatric immunization) when
Tdap was administered.
6. Four of six (67%) individuals that experienced an acute medical issue that was addressed
at GRC, the PCP or other provider assessed it according to accepted clinical practice Acute
illness events reviewed included:
• Individual #78 on 2/16/23 presented with lethargy with mild fever.
• Individual #79 on 3/6/23 presented with pain in left inner thigh.
• Individual #79 on 5/16/23 presented with left thigh and hip pain.
• Individual #30 6/22/23 presented with skin discoloration to wrist.
• Individual #29 on 2/15/23 presented with seizures.
• Individual #31 on 6/16/23 had an insect bite.
7. For the acute illness event for Individual #78 on 2/16/23 lethargy and mild fever, the
event was s/p full mouth extraction, and was placed on Levaquin. PCP notation indicated
that follow-up was not indicated, but clinical description indicated a follow-up until
closure was indicated. Individual #30 on 6/22/23 had skin discoloration to wrist, and
Individual #31 on 6/16/23 had an insect bite, but the source of the information was not
included in the progress note.
8. For eight of nine (89%) individuals that required hospitalization or an ED visit, the
individual received timely evaluation by the PCP or a provider prior to the transfer, or if
18
unable to assess prior to transfer, within one business day, the PCP or a provider provided
an IPN with a summary of events leading up to the acute event and the disposition. Acute
events reviewed included:
• Individual #78, 5/12-19/23 hospital for pneumonia and UTI.
• Individual #78, 4/29-/2/23 hospital for pancreatitis.
• Individual #42, 4/4-5/5/23 hospital for sepsis, aspiration pneumonia and g-tube
placement.
• Individual #39, 5/23/23 ED for respiratory distress.
• Individual #39, 1/29-31/23 hospital of laceration to forehead requiring staples.
• Individual #79, 1/21/23 ED for left thigh contusion.
• Individual #29, 5/19-22/23 hospital for seizures.
• Individual #29, 6/15-20/23 for seizures.
• Individual #3,1 12/7/22 ingestion of wrong medication.
For Individual #39, 1/29/23-1/31/23 hospital for laceration to forehead with staples,
there was lack of a PCP transfer note on first business day (1/30/23). There was a PCP
progress note on 1/29/23, which gave an update at the hospital, but it did not describe
events leading to the decision to transfer to the ED.
9. As appropriate, prior to the hospitalization, ED visit, or infirmary admission, all
individuals had a quality assessment documented in the PCP progress note.
10. Prior to the transfer to the hospital or ED, all individuals received timely treatment
and/or interventions for the acute illness.
11. For eight of nine (89%) individuals transferred to the hospital, the PCP or nurse
communicated necessary clinical information with hospital staff. Though requested, there
was no documentation for this indicator submitted for Individual #78 who on 4/29/23-
5/2/23 had a hospitalization for pancreatitis.
12. Six of seven (86%) individuals had a post-hospital IDT meeting that addressed the follow-
up medical, and healthcare supports to reduce risks and early recognition, as appropriate.
There was a lack of evidence submitted by GRC for Individual #78 who on 5/12/23-
5/19/23 had a hospitalization for pneumonia and UTI. While there was an IDT meeting
during the individualn on 5/14/23, there was no evidence of a post
hospital IDT meeting.
13. -
up assessments and documentation at a frequency consistent with the in
and the presenting problem with documentation of resolution of acute illness on four of
nine occasions (44%). There was a lack of PCP follow-up for:
• Individual #78 was hospitalized on 5/12-/19/23 for pneumonia and UTI.
• Individual #42 was hospitalized for sepsis, aspiration pneumonia and g-tube
placement.
• Individual #39 had a hospitalization for laceration to the forehead.
• Individual #29 was hospitalized on 6/15-20/23 for seizures.
14. All consultations were completed in a timely manner.
15. On 93% of the occasions, the consult referral form provided adequate information,
including information as to current health at GRC. The exception was for Individual #78
nephrology consult completed on 3/27/23. The consultant documented a lack of follow-
up of recommendations from prior visit, with no information provided to the consultant
concerning the rationale for not following the recommendations.
16. If the individual had non-Facility consultations that impacted medical care, the PCP
indicated agreement or disagreement with recommendations. This determination was not
evident in consultation follow-up notes by the PCP. Examples included Individual #78
19
cardiology and nephrology, Individual #42 GI 7/13/23 and surgery 7/5/23, Individual
#39 ENT 1/11/23 and ENT 6/30/23, Individual #79 dermatology 7/7/23, Individual#30
oncology 6/21/23, Individual#29 neurology 2/28/23, hepatology 5/30/23, and
Individual #31 dermatology 12/20/22 and neurology 4/14/23.
17. The PCP completed a review within five business days, or sooner if clinically indicated on
11/13 occasions (85%). PCP progress notes beyond five days of consultation included.
• Individual #78 who had a cardiology consult on 1/12/23, with the date of the PCP
progress note completed on 1/30/23.
• Individual #42 had a surgery consult dated 7/5/23, with the PCP progress note dated
7/14/23.
18. For zero of 13 opportunities, the PCP wrote an IPN that explained the reason for the
consultation, the significance of the results, agreement, or disagreement with the
recommendation(s), and whether there was a need for referral to the IDT.
PCP progress notes did not include all components of information required:
• Individual #78 cardiology 1/12/23 and nephrology 3/27/23.
• Individual #42 Gastroenterology 7/13/23, and surgery 7/5/23.
• Individual #39 ENT 1/11/23, ENT 6/30/23.
• Individual #79 movement disorder 6/6/23, and dermatology 7/7/23.
• Individual #30 oncology 6/21/23.
• Individual #29 neurology 2/28/23, and hepatology 5/30/23.
• Individual #31 dermatology 12/20/22, and neurology 4/13/23.
All components listed in Indicator #18 are required for compliance for each consult
reviewed.
19. If PCP agreed with consultation recommendation(s), there was evidence it was ordered
for all occasions (13/13 100%).
20. Based on lack of information in the PCP progress notes (indicator #18), it was not possible
to determine whether the PCP referred any consultation recommendations to the IDT for
review, agreement or disagreement, and action plan.
21. Labs and diagnostic testing were ordered timely on 7/7 occasions. There were no critical
results for labs ordered during the monitoring review period for Individual #78,
Individual#42, Individual #39, Individual #30, Individual #79, Individual #29, and
Individual #31.
• For Individual #78, several labs in February 2023-April 2023 with abnormalities did
not have any PCP progress note. There was an occasional handwritten notation on the
lab test report with interpretation rather than a PCP progress note.
• For Individual #42, several lab results were submitted, with initial and date of review,
but only one of numerous lab draws had a progress note reviewing results. The
medical record progress note section did not reflect the frequent lab monitoring.
• For Individual #39, Individual #31, and Individual #79, all labs had PCP progress note
reviewing results.
• For Individual # 30, labs of 1/9/23 and 5/22/23 were not referenced in any PCP
progress note.
• For Individual #29, there were numerous labs, but with no PCP progress note
documenting a review of the results.
20
Section C.iii Residents at Risk of Harm (77-81)
Summary: Individuals were not consistently provided with accurate risks scores with those risks being
adequately reviewed when there was a change in status or new plan of care. The at-risk plans were inconsistent
in their ability to meet the needs of the individual and there was no clear evidence that the at-risk plan was
reviewed and approved by the IDT.
Partial Compliance: Paragraph 77, & Paragraph 79.
#
Indicator
Overall
Score
1
The individuals risk rating is accurate.
i. IDT uses clinical data.
ii. Any risk guidelines are used.
iii. Justification provided when variance occurs.
(par. 77)
PC
57%
4/7
2
Risks are identified timely, including:
i. Risks are reviewed and updated min annually.
ii. No more than 5 days post CoS
(par. 78,56)
NC
0%
0/7
3
Risks are responded to in a timely manner.
i. IDT mtg within 5 days to revise POC.
ii. Assessments as indicated.
(par. 78,56)
NC
0%
0/7
4
-Risk Plan sufficiently addresses the chronic or at-risk condition in accordance with
applicable guidelines, or other current standards of practice consistent with risk-benefit considerations.
i. include preventative interventions to minimize the chronic/at-risk condition.
ii. incorporates measurable objectives to address the chronic/at-risk condition to allow the team to
iii. action steps support the goal/objective.
iv. identifies and supports the specific clinical indicators to be monitored (e.g., oxygen saturation
measurements).
(par. 79)
PC
43%
3/7
5
The At-Risk Plan should be reviewed and approved by the IDT. (par. 80,81)
NC
O%
0/7
Comments:
1. (Indicators 1-4). Individual #29 was transferred from the hospital to Hospice at a skilled
facility 7/5/23, therefore, did not review for risk updates or his Transition Plan. Three of
six Transition Plans had nursing section completed (individual #39 in February 2023 and
Individual #360 in March 2022), however, those nursing assessments were not updated
to be current.
The nursing sections in the Transition plans were not being completed early enough in the
process, so that potential providers could fully review risk plans and supports needed and
ask questions of GRC RN and PNMT professionals earlier in the process to ensure the
provider could
• Individual #78 was a PNM Critical risk level for aspiration and was NPO. Their
transfer and positioning were being monitored by HAB. The Nursing UTI risk
assessment dated 7/5/23 was blank and had no comments or check off as to which of
the risk factors impacted his risk level (as per the instructions on the form). Risk
screenings for Constipation, DVT, and Diabetes was accurate. Osteoporosis screening
notes dated 7/5/23 by the nurse did not identify risk factors, but did identify lack of
justification for exceptions as he was prescribed Prolia injections every six
months for osteoporosis, without an active corresponding diagnosis and did
not note plan for resolving this (i.e., communications with the prescriber).
There was no nursing data in the Transition Plan. Per the Event Log on 5/19/23 -

21
12:19 PM, a note from the Social Worker indicated that they (Q, Nurse, Amerigroup,
SW, and the guardian) set up a meeting with a provider to talk to the team about him
since he was hospitalized, and they cannot meet him. They had not realized in his
information that he required a tube, and was not fed orally. They were not able to
support individuals with those needs, so they gracefully exited and allowed the team
to continue chatting about him to the newer guardian so she could learn more about
his needs.
• For Individual #42 his annual risk screenings appeared accurate, including high risk
for aspiration. Upon hospitalization for aspiration pneumonitis and sepsis with
discharge back to GRC on 5/5/23, nursing and PNMT reviewed his risks and PNM
increased his risk level to Critical from High on 5/14/23. The enteral tube was also
increased from At Risk to High, and Fluid imbalance from Not at Risk to High. There
was no nursing data in the transition plan to update upon clinical changes.
• For Individual #39, upon the individual returning from the community to GRC, the
SLP/PNMT completed an aspiration risk screen, noting that he had a g-tube placed
when living in the community and reassessed him as at HIGH risk (same as prior to
transition). The Braden scale was dated 12/7/22 with a score of 13 (moderate risk),
therefore, it appeared that Nursing did not complete a new Braden scale despite the
individual change of condition with a pressure injury.
• Individual #79 was a PNM Critical risk level for aspiration. They had a detailed plan in
place by the SLP for safe PO intake. The individual had a Braden scale score 9/3/22
(19 = not at risk), however, the Activity score of 4 (walks frequently) was
questionable after observing the current challenges for her to ambulate, the need for
staff assistance, and recent episode of lowering self to floor. When changes occur with
mobility, the nurse should review the Braden scale score to ensure accuracy.
• For Individual #30, risk screenings were completed on 2/27/23, Braden scale not at
risk for skin breakdown. Morse Fall Scale at 25, low risk, DVT/PE score of 5 (high
risk) due to age and history of cancer. Cardiac at risk due to age and HDL of 38,
Diabetes at risk due to new generation antipsychotic medication and age over 40. The
UTI risk screening and the Constipation risk screening tool were both incomplete
(blank) without a score. No clinical changes to update and the transition plan did not
have the nursing sections completed.
• Individual #29 had a PNM High risk level for aspiration due to dysphagia (and
seizures), positioning, and special approaches required for safe oral intake that were
documented on the PNMP. Nursing Risk screenings for Circulatory, Diabetes,
Osteoporosis, and Constipation risk lacked details of qualifying factors that were to
be identified on the forms. The result caused conflicting results. For example, the
cardiac assessment was LOW (not at risk), however, in the GRC Nursing report it
stated at high risk for cardiac due to his HTN and high cholesterol. For constipation, it
stated at risk, but did not identify the supporting clinical risk factors. Individual had a
seizure log / high risk, PNMP last updated April 2023 with training of staff
documented.
• For Individual #31, risk screenings for skin (Braden scale) and Diabetes screenings
were completed. The other risk screening tools submitted with the annual nursing
assessment for ISP 11/18/22 were not filled out completely, were blank, or stated no
changes to risks with no clarifying information offered.
5. -Risk Plan was not clearly reviewed and approved by the IDT. Each of
the HSSPs/Risk Plans noted the developers of the at-risk plan to be nursing, QIDP, RTS,
therapist, etc. (by name), but there was no evidence of a review/discussion of the at-risk
plan.

22
Section C.iv – Nursing (82-87)
Summary: The annual record review format currently utilized for nursing was referred to as the GRC Nursing
Report, which was a
of family medical history, social/smoking/substance abuse history, allergies, or medication side effects.
Information found in the ISP, Medical history and active problem list, MAR, Immunization record, and Monthly
Integrated Review (MIR) documentation was included, however, none of the annual nursing assessments were
considered to have all the needed components to be considered as comprehensive assessments.
#
Indicator
Overall
Score
1
Individual receives a quality annual nursing record review, including:
i. Diagnosis/Active problem list
ii. Procedure History
iii. Family medical history
iv. Social/Smoking/Substance abuse history
v. Allergies or medication side effects
vi. List of current medications
vii. Pain
viii. Immunizations
ix. Tertiary Care
x. Consultation summary
xi. Lab and Diagnostic testing results
(par. 52,58,59,61,64,81,82,83,84)
PC
0%
0/7
54%
36/66
2
Individual receives quality annual nursing physical assessment, including, as applicable to the individual:
i. Functional status
ii. Review of each body system.
iii. Vital signs; including oxygen saturation level, lung sounds,
iv. Height and Weight
v. Pain scale and score
vi. elimination pattern/status
vii. Braden scale score; skin condition
viii. Fall risk score and supporting details.
ix. Follow up for any abnormalities found during the physical assessment.
(par. 52,58,59,61,64,82,83,86)
PC
14%
1/7
56%
35/63
3
For the annual ISP, nursing -risk conditions are
sufficient to assist the team in developing a plan responsive to the level of risk, including:
i. status updates of the current medical and behavioral/mental health risks.
ii. an analysis of the chronic conditions, including high/medium health risks as compared to the
previous quarter or year, progression, or regression.
iii. a nursing review of effectiveness of current health care plan supports/interventions, to identify
updates/revisions indicated.
iv. Recommendations to the IDT to individualize and enhance the new health support plan, with
preventative, individualized interventions as appropriate to address the chronic conditions and
promote amelioration of the at-risk condition to the extent possible.
(par. 52,58-64,81,82,84)
NC
29%
2/7
4
Individual receives a quality quarterly nursing record review, including:
i. Diagnosis/Active problem list
ii. Procedure History
iii. Family medical history
iv. Social/Smoking/Substance abuse history
v. Allergies or medication side effects
vi. List of current medications
vii. Pain
viii. Immunizations
ix. Tertiary Care
x. Consultation summary
xi. Lab and Diagnostic testing results
(par. 52,58,59,64,84)
N/A

23
5
Individual receives quality quarterly nursing physical assessment, including, as applicable to the individual:
i. Functional status
ii. Review of each body system.
iii. Vital signs; including oxygen saturation level, lung sounds,
iv. Height and Weight
v. Pain scale and score
vi. elimination pattern/status
vii. Braden scale score; skin condition
viii. Fall risk score and supporting details.
ix. Follow-up for any abnormalities found during the physical assessment.
(par. 52,58,59,64,82,83,86)
PC
60%
3/5
6
-risk conditions are
sufficient to assist the team in maintaining a plan responsive to the level of risk, including:
i. status updates of the current medical and behavioral/mental health risks.
ii. an analysis of the chronic conditions, including high/medium health risks as compared to the
previous quarter or year, progression, or regression.
iii. a nursing review of effectiveness of current health care plan supports/interventions, to identify
updates/revisions indicated.
iv. Recommendations to the IDT to individualize and enhance the new health support plan, with
preventative, individualized interventions as appropriate to address the chronic conditions and
promote amelioration of the at-risk condition to the extent possible
(par. 52,58-64,81,82,84)
NC
17%
1/6
33%
8/24
7
If the individual has a change in status that requires a nursing assessment, a nursing assessment is
completed in accordance with nursing protocols or current standards of practice. This includes active
communication with the PCP regarding health status and changes. (par. 59,78,79,81-84)
PC
50%
4/5
8
Nurses shall routinely assess residents for symptoms of pain, in response to changes in client condition
when one would reasonably expect pain to result, and when other relevant staff communicate the suspicion
of resident pain in the event the resident is not able to verbalize pain. The nurse shall attend to and treat
-call provider as needed.
(par. 59,78,79,81-84)
PC
71%
5/7
9
Ensure residents are appropriately protected from infection. GRC shall establish and maintain an effective
infection control committee and ensure ongoing access to and consultation with experts in infection control
and infectious diseases. (par. 82,85)
SC
86%
6/7
10
Ensure residents maintain maximum skin integrity. (par. 82,86)
SC
100%
7/7
11
Ensure residents receive medications and treatments as prescribed. (par. 87)
NC
17%
1/6
Comments:
1. Individuals did not receive a quality annual nursing record review.
•
•
•

24
•
•
•
•
2. The annual nursing physical assessments showed partial presence of including the needed
quality indicators.
•
•
•

25
•
•
•
•
3. The annual nursing assessments were not sufficient in addressing th-risk
conditions to assist the team in developing a responsive plan.
•
•
•
•

26
•
•
•
The quarterly nursing physical assessments showed partial presence of quality indicators.
•
•
•

27
•
•
•
•
6. Status updates, risk review, data analysis and nursing recommendations were partially
present by nursing in the monthly integrated reviews (MIR).
•
•
•
•
•

28
•
7. Individuals were assessed by nursing upon a change of status, but did not all include
thorough evidence of communications with the PCP regarding the changes.
•
•
29
•
•
•
•
•
Individuals were assessed for pain routinely as part of the annual and quarterly nursing
assessments. In response to changes in condition when one would reasonably expect pain
to result, there was an identified gap in addressing pain for one individual.
•

30
•
•
•
•
•
•
9. . A dedicated nurse
provided surveillance of all infections and coordination of preventative immunizations.
•
•
•
•
•
•
•
10. The individuals had monitoring and treatment for problems with skin integrity, including
an appointed wound care nurse.
•
31
•
•
•
•
•
•
For indicator #11, please refer to Medication details (indicators 31-36) under the Medication
Variance section.

32
Section C.v Psychiatric Services (88-91)
Summary: Positives included a status a treatment document being completed consistently for all individuals
within the past 12 months. Medications were also not given in a manner to induce sedation or as a punishment.
Additionally, multiple medications were not used during chemical restraint unless there is proper justification.
Areas to focus on included CPE content, active participation, documentation to the ISP, and involvement in
transition planning.
Partial Compliance: Paragraph 88, Paragraph 89 & Paragraph 90.
#
Indicator
Overall
Score
1
GRC psychiatrists are board certified or eligible. (par. 88)
PC
50%
1/2
2
The individual has a CPE. (par. 88)
PC
60%
3/5
3
CPE content is comprehensive.
i. Identifying information
ii. History of present illness
iii. Past psychiatric history
iv. Substance Use History
v. Family History
vi. Medical history
vii. Developmental history
viii. Social history
ix. Physical exam
x. Labs
xi. Mental Status
xii. Diagnostic assessment
xiii. Bio-psychosocial formulation
xiv. Recommendations
(par. 58-64, 88)
NC
0%
0/5
4
Status and treatment document was updated within past 12 months. (par. 88)
SC
100%
5/5
5
Documentation prepared by psychiatry for the annual ISP was complete and includes:
i. Demographic
ii. Psychiatric diagnosis
iii. Symptoms of Diagnosis
iv. Target symptoms monitored.
v. Derivation of symptoms
vi. Psychological assessment or BH assessment
vii. Combined BH review /formulation
viii. Psychoactive medication
ix. Each psych med prescribed has an identified diagnosis /symptoms.
x. Each med corresponds with the diagnosis.
xi. Risk of meds
xii. Risk of illness
xiii. Non-pharmacological treatment
xiv. Risk/Benefit. Analysis
xv. Past Pharmacotherapy
xvi. Future plans
xvii. This should include other consultations performed over the course of the year.
(par. 52,88-90)
NC
0%
0/5
6
Psychiatry documentation for annual /transition plan was submitted to the ISP team at least 10 days prior
to the ISP and was no older than three months. (par. 61,88)
NC
0%
0/5

33
7
The psychiatrist or member of the psychiatric team (par. 88, 89)
NC
0%
0/5
8
Psychiatric documentation references the behavioral health target behaviors, and the functional behavior
assessment discusses the role of the psychiatric disorder upon the presentation of the target behaviors.
(par. 58,59,89)
NC
0%
0/5
9
The psychiatrist participated in the development of the PBSP. (par. 89)
NC
0%
0/5
10
Daily medications indicate dosages not so excessive as to suggest goal of sedation. (par. 89)
SC
100%
5/5
11
There is no indication of medication being used as a punishment, for staff convenience, or as a substitute
for treatment. (par. 89)
SC
100%
5/5
12
There is a treatment program in the record of individual who receives psychiatric medication. (par. 89)
SC
100%
5/5
13
Documentation of Chemical Restraint: Consult and Review was completed within 10 days post restraint.
(par. 90)
NC
0%
0/1
14
Multiple medications were not used during chemical restraint unless there is proper justification. (par.
90)
SC
100%
1/1
15
Psychiatry follow-up occurred following chemical restraint. (par. 90)
NC
0%
0/1
16
The final ISP/Transition document included the following essential elements and showed evidence of the
i. The rationale for determining that the proposed psychiatric treatments represented the least
intrusive and most positive interventions.
ii. Integration of behavioral and psychiatric approaches.
iii. The signs and symptoms monitored to ensure that the interventions are effective, and the
incorporation of data into the discussion would support the conclusions of these discussions.
iv. A discussion of both the potential and realized side effects of the medication, in addition to the
benefits (i.e., risk benefit analysis).
(par. 91)
NC
0%
0/5
Comments:
1. One of the two psychiatrists providing contracted psychiatric services at the facility was
board certified. The second psychiatrist, although residency trained, was not board
certified. Given the time that has lapsed since he completed his residency, he was no
longer eligible to take the board examinations.
During the monitoring visit, psychiatry clinic was observed with both psychiatrists for a
total of eight individuals, none of whom were in the review group. Psychiatry clinics were
well attended by the IDT members, but there was a paucity of communication by the team
members. Typically, one or two staff, generally the QIDPs, were the most informative. The
data presented was anecdotal, and the behavioral health data was not reliable. As such,
the psychiatrists were making decisions regarding psychotropic medications in the
absence of data.
2. Two individuals in the review group, Individual #39 and Individual #29, were not
receiving psychiatric services. As such, they were scored N/A for this indicator, having an
initial Comprehensive Psychiatric Evaluation (CPE). As the CPE documents were not
provided with the initial document request, these were requested again on-site. The
information revealed that two individuals, Individual #42 and Individual #79, were
receiving psychiatric services and prescribed psychotropic medications, but never had an

34
initial CPE. In summary, three of the five individuals in the review group receiving
psychiatric services had a completed initial CPE in the record.
3. The three completed initial CPE documents, for Individual #78, Individual #79, and
Individual #30, did not include the required elements.
• The CPE regarding Individual #78 was missing the family history, physical
examination, laboratory examinations, bio-psycho-social formulation, and treatment
recommendations.
• The CPE regarding Individual #79 was missing the physical examination, mental
status examination, and bio-psycho-social formulation.
• The CPE regarding Individual #30 was missing the physical examination, laboratory
examinations, bio-psycho-social formulation, and treatment recommendations.
4. All individuals in the review group who required an annual CPE had one completed within
the previous 12 months.
5. None of the annual CPE documents included all the required elements. The annual CPEs
were missing 10 to 11 essential elements.
• The annual CPE regarding Individual #78 was missing the symptoms of the diagnosis,
the derivation of symptoms, the psychological assessment or behavioral health
assessment, the combined behavioral health review/formulation, the identified
diagnosis or symptoms for each medication, risk of medication, risk of illness, non-
pharmacological treatment, risk/benefit analysis, past pharmacotherapy, and review
of other consultations performed over the year.
• The annual CPE regarding Individual #42 was missing the symptoms of the diagnosis,
the derivation of symptoms, the psychological assessment or behavioral health
assessment, the combined behavioral health review/formulation, the identified
diagnosis or symptoms for each medication, risk of medication, risk of illness, non-
pharmacological treatment, risk/benefit analysis, past pharmacotherapy, and review
of other consultations performed over the year.
• The annual CPE regarding Individual #79 was missing the symptoms of the diagnosis,
the derivation of symptoms, the psychological assessment or behavioral health
assessment, the combined behavioral health review/formulation, the identified
diagnosis or symptoms for each medication, risk of medication, risk of illness, non-
pharmacological treatment, risk/benefit analysis, past pharmacotherapy, and review
of other consultations performed over the year.
• The annual CPE regarding Individual #30 was missing the symptoms of the diagnosis,
the derivation of symptoms, the psychological assessment or behavioral health
assessment, the combined behavioral health review/formulation, the identified
diagnosis or symptoms for each medication, risk of medication, risk of illness, non-
pharmacological treatment, risk/benefit analysis, past pharmacotherapy, review of
other consultations performed over the year.
• The annual CPE regarding Individual #79 was missing the symptoms of the diagnosis,
the derivation of symptoms, the psychological assessment or behavioral health
assessment, the combined behavioral health review/formulation, the identified
diagnosis or symptoms for each medication, risk of medication, risk of illness, non-
pharmacological treatment, risk/benefit analysis, and past pharmacotherapy.
6. A review of the annual Individual Support Plan (ISP) documentation in the context of the
presentation of psychiatric information revealed that for all five individuals in the review
group receiving psychiatric services, the annual psychiatric evaluation was not submitted
for review within the required time frame.
• For Individual #78, the annual ISP was dated 8/15/22. The annual psychiatric
evaluation was dated after the ISP, on 8/31/22.

35
• For Individual #42, the annual ISP was dated 2/7/23. The annual psychiatric
evaluation was dated after the ISP, on 3/29/23.
• For Individual #79, the annual ISP was dated 10/3/22. The annual psychiatric
evaluation was dated after the ISP, on 10/26/22.
• For Individual #30, the annual ISP was dated 3/1/23. The annual psychiatric
evaluation was dated after the ISP, on 5/9/23.
• For Individual #79, the annual ISP was dated 11/18/22. The annual psychiatric
evaluation was dated two days prior to the ISP, on 11/16/22, so it could not have
been submitted to the Interdisciplinary Team within the required timeframe. Please
note, in the documents, the annual psychiatric evaluation for Individual #79 was
dated 11/16/23. This was an apparent typographical error, and the date was
corrected for the purposes of this report to 11/16/22.
7. Per a review of the ISP documentation and interviews with the facility psychiatrists,
psychiatrists did not participate in the ISP meetings at the facility. If the psychiatrist did
not participate in the ISP meeting, there needs to be some evidence that the psychiatrist
participated in the decision to not be required to attend the ISP meeting. The presence of
the psychiatrist always allows for richer discussion during the ISP regarding the
integration/inclusion of psychiatric data (e.g., diagnoses, symptom presentation,
psychotropic medication, related medical concerns).
8. The psychiatric documentation generally referenced the behavioral health target
behaviors via listing the indicators. There was no detailed evidence of a review of the
associated data. Given the lack of reliable data, this was not surprising. When reviewing
the behavioral health documentation, the Functional Behavioral Assessment did not
This, when
documented, was included in the Behavioral Health Assessment. Overall, this indicator is
attempting to address the documentation of integrated care between psychiatry and
behavioral health. Based on document review, staff interviews, and observation of
psychiatry clinical encounters, the disciplines are not integrated and the psychiatric
diagnoses inclusive of autism spectrum disorders and the symptoms thereof were not
9. Per staff interviews and document review, the psychiatric clinicians did not participate in
the development of the Behavior Support Plans.
10. Based on a review of the psychiatric documentation and the medication administration
record for the five individuals in the review group receiving psychiatric services, daily
medication dosages were not excessive as to suggest the goal of sedating individuals.
11. There is no indication of medication being used as a punishment, for staff convenience, or
as a substitute for treatment.
12. Each of the five individuals in the review group had a Behavior Support Plan in effect.
13. Indicators 13-15 are regarding a chemical restraint for Individual #46 that occurred
2/8/23 at 10:44 pm. The Documentation of Chemical Restraint: Consult and Review was
not submitted. Further, there was no documentation regarding psychiatric follow-up after
the restraint episode. One medication, Zyprexa, was utilized in the chemical restraint.
16. As psychiatry did not participate in the Individual Support Plan or Transition Planning
meetings, the documents generated because of these meetings did not include evidence of
psychiatric participation nor did the documents include the integration of psychiatric
clinical information. As each psychiatrist is contracted for one day per week, it was not
surprising that they were not at the table for transition planning, but this needs to be
accomplished. Psychiatrists had a great deal of historical information about individuals
and knew them well. They knew what had been trialed and what had failed. They could
write a brief, but detailed transition plan/summary for the next treatment provider. This

36
would be incredibly helpful in the transition process. Further, a transition conference call
between the current psychiatrist and the community psychiatrist would be important.

37
Section C.vi: Medications (92-102)
Summary: All individuals had a diagnosis supporting the use of the prescribed medications and if an
intervention was required, the pharmacist notified the prescribing practitioner. The IDY reviewed instances that
would have placed the individual on the monthly review. An external review process existed for identified
individuals. Regarding administration, The Monitoring Team and RN Supervisor observed medication
administrations and no medication errors were observed. For only one staff was additional training/follow-up
needed. It was for ensuring placement of g-tube prior to administering the medications.
Substantial Compliance: Paragraph 92, & Paragraph 100.
Partial Compliance: Paragraph 87, Paragraph 93, Paragraph 96, and Paragraph 102.
#
Indicator
Overall
Score
1
medications have a justifying diagnosis. (par. 92)
SC
100%
14/14
2
If the individual has new medications, the pharmacy completes a new order review prior to dispensing the
medication. This includes:
i. Interactions, side effects, allergies, adverse reactions
ii. Review of clinically relevant lab
iii. Need for additional lab work.
iv. Potential to use alternate medications.
v. Need to consider dose adjustments.
(par. 93)
NC
0 %
0/5
3
If an intervention is necessary, the pharmacy notifies the prescribing practitioner. (par. 93)
SC
100%
1/1
4
QDRRs are completed quarterly by the pharmacist. (par. 94)
NC
46%
6/13
5
The pharmacist addresses laboratory results, and other issues in the QDRRs, noting any irregularities, the
significance of the irregularities, and makes recommendations to the prescribers in relation to:
i. Laboratory results, including sub-therapeutic medication values.
ii. Benzodiazepine use.
iii. Medication polypharmacy.
iv. New generation antipsychotic use; and Anticholinergic burden.
(par. 94)
PC
69%
9/13
6
The PCP and/or psychiatrist document agreement/disagreement with the recommendations of the
pharmacist with clinical justification for disagreement:
i. The PCP reviews and signs QDRRs within 28 days, or sooner depending on clinical need.
ii. When the individual receives psychotropic medications, the psychiatrist reviews and signs QDRRs
within 28 days, or sooner depending on clinical need.
(par. 61,95)
NC
0%
0/13
7
Records document that prescribers implement the recommendations agreed upon from QDRRs. (par. 95)
NC
33%
3/9
8
If a review of a new order by pharmacy indicates the need for a change in order and the prescriber agrees,
then a follow-up order shows that the prescriber made the change in a timely manner. (par. 95)
NA
9
Monitoring of any first-generation antipsychotic medication, two or more psychiatric or neurological
medications from the same general class (e.g., two antipsychotics) to the same resident, and the
prescription of three or more psychiatric or neurological medications, regardless of class, to the same
resident, to ensure that the use of such medications is clinically justified and that medications that are not
clinically justified are eliminated. (par. 96)
PC
75%
9/12
10
Monitoring shall be conducted by the Pharmacy and Therapeutics Committee, which shall include: the
Medical Director; the Pharmacy Director or PharmD (clinical pharmacist); one PCP, if available, who is not
the treating physician; and other appropriate staff. (par. 96)
PC
3 of 4
mtg

38
11
Before a prescriber initiates treatment with a medication that would render a person subject to the
monthly review described above (e.g., by prescribing a third psychiatric or neurological medication to a
resident already prescribed two such medications), the IDT shall meet to consider the
recommended medication and alternative nonpharmacological interventions and shall document the
rationale for the selected decision. (par. 96)
SC
100%
1/1
12
GRC residents receiving psychiatric or neurologic medications shall be monitored accordingly. (par. 97)
NC
0 of 4
mtg
13
Clinically significant DUEs are completed in a timely manner based on the determined frequency but no
less than quarterly. (par. 98,99)
NC
14
There is evidence of follow-up to closure of any recommendations generated by the DUE. (par. 98,99)
NC
15
GRC shall identify all medications prescribed for dual purposes, and for all medications so identified,
ensure ongoing collaboration between relevant disciplines (e.g., psychiatry, neurology) regarding their
continued use. Collaboration among necessary disciplines regarding use of the dual-use medication shall
be coordinated by the PCP. (par 100)
NC
16
Within three months of the Effective Date of this agreement, GRC shall conduct an external clinical review
to verify the continuing propriety of th
into the following categories, and shall then implement the recommendation arising from that review:
A. Residents who are prescribed Dilantin, Valproic Acid, Thorazine, Loxapine, Fluphenazine,
Perphenazine, Haloperidol, Primidone, and Phenobarbital.
B. Residents who are prescribed oral bisphosphonates and have esophageal motility disorders, have
GERD, are at increased risk of aspiration, or who are unable to stand or sit upright for at least 30
minutes after dose administration.
(par. 100)
SC
100%
5/5
17
ADRs are reported immediately. (par. 101)
N/A
18
Clinical follow-up action is completed, as necessary, with the individual. (par. 101)
N/A
19
The Pharmacy and Therapeutics Committee thoroughly discusses the ADR. (par. 101)
N/A
20
Individual receives prescribed medications in accordance with applicable standards of care.
(par. 87,102a)
SC
80%
4/5
21
Medications that are not administered or the individual does not accept are explained. (par. 102a)
SC
100%
2/2
22
The individual receives medications in accordance with the eight (8) rights (right patient (individual),
right medication, right dosage, right route, right time, right documentation, right reason, and right
response), and their PNMP as applicable. (par. 87, 102a)
SC
100%
5/5
23
To ensure nurses and CMAs administer medications safely: For individuals who exhibit signs and
symptoms of respiratory issues and /or aspiration during medication administration, the nurse or CMA
will immediately stop the medication administration and notify nurse to/or complete an assessment
which will include lung sounds and may include a full set of vital signs, pulse oximetry, etc. as indicated at
the time of the assessment. (par. 102a)
SC
100%
1/1
24
If the individual receives pro re nata (PRN, or as needed)/STAT medication or one time dose,
documentation reflects adherence to GRC policy as to nurse assessment prior to, reason for and
(par. 102a)
NC
33%
1/3
25
(par. 102a)
SC
80%
4/5
26
Instructions are provided to the individual and staff regarding new orders or when orders change. (par.
102a)
N/A
27
Nurses and CMAs administering medications are knowledgeable of the individuals needs and preferences
and are competent to follow the facility medication administration policies and procedures (par. 102b)
SC
80%
4/5
28
When a new medication is initiated, when there is a change in dosage, and after discontinuing a
medication, documentation shows the individual is monitored for possible adverse drug reactions. (par.
102a)
N/A
29
If an ADR occurs, the (par. 102c)
N/A

39
30
If an ADR occurs, documentation shows that orders/instructions are followed, and any untoward change
in status is immediately reported to the practitioner /physician. (par. 102c)
N/A
31
If the individual is subject to a medication variance, there is proper reporting of the variance (par. 102c)
NC
33%
2/6
32
If a medication variance occurs, documentation shows that orders/instructions are followed, and any
untoward change in status is immediately reported to the practitioner/physician. (par. 102c)
SC
100%
1/1
33
Actual medication variances (Level 3 - 9) and potential medication variances (Level 1-2) are documented
per the Medication Variance Policy. (par. 102c)
NC
16%
1/6
34
Variance and potential variance data are reviewed monthly to aid in identifying systemic issues. (par.
102c)
NC
0%
0/6
35
Corrective actions are planned to address any identified issues or predisposing factors. (par. 102c)
NC
0%
0/6
36
Corrective action items are followed-up to closure. (par. 102c)
NC
0%
0/6
Comments:
1. All the i The QDRR reviewed the
diagnoses and ICD-10 codes on the Facesheet to ensure there were appropriate diagnoses
listed for each prescribed medication.
2. No new order medication reviews, including all the listed requirements, were completed
prior to dispensing the medication. The contract pharmacy that filled the prescriptions
and delivered the medication used a software drug database with a template for each
patient that included allergies and description of reaction/symptoms, medical conditions,
and age. Since this is a pharmacy that is off site, it did not have access to clinical
information, such as lab data.
The patient profile report was provided for Individual #29, Individual #42, and Individual
#79 indicating review of medication and food allergies, including symptoms of the
allergies. It did not include any review of lab data. Drug interactions for new prescriptions
were found by the pharmacy for Individual#78 (Iron supplement and Esomeprazole),
Individual #42 (Diazepam rectal and Metoprolol tartrate), Individual #39
(Acetaminophen and Scopolamine), Individual #29 (Montelukast and Gemfibrozil), and
Individual #29 (Nayzilam and Fycompa). Medications that were not new medication
orders were excluded from this review. During a telephone conversation with pharmacy
staff, if a dosage change was recommended or consideration of alternate medications,
communication with the PCP occurred and was documented in the pharmacy database.
These occurrences were infrequent. This section did not meet criteria due to lack of
ability to review lab data.
3. The pharmacy software filtered all new orders (and all orders) for drug -drug
interactions, with information concerning severity of the interaction. Communication was
made with the PCP for questions the pharmacy may have that concerned this information.
4. QDRRs were generally not completed every quarter (every three months). The dates of
the three most recent QDRRs and the scores are as follows:
• Individual #78: QDRR1 7/7/22 and 3/31/23, QDRR2 3/31/23 and 6/26/23.
• Individual #42: QDRR1 11/22/22 and 2/7/23 or 3/1/23, QDRR2 2/7/23 or 3/1/23
and 5/5/23.
• Individual #39: QDRR1 7/22/22 and 1/6/23 and QDRR2 discharge to community and
readmitted 5/19/23 (score NA).
• Individual #79: QDRR1 10/20/22 and 3/31/23 and QDRR2 3/31/23 and 6/30/23.
• Individual #30: QDRR1 9/22/22 and 3/3/23, and QDRR2 3/3/23 and 6/1/23.

40
• Individual #29: QDRR1 9/22/22 and 1/19/23, and QDRR#2 1/19/23 and 6/30/23.
• Individual #31: QDRR1 3/31/23 and no prior QDRR, and QDRR2 3/31/23 and
6/20/23.
5. On nine of 13 occasions, the pharmacist addressed laboratory results and other issues in
the QDRRs, noting any irregularities, the significance of the irregularities, and making
recommendations to the prescribers. The following were concerns for reviewed QDRRs:
• For Individual #42, the QDRR1 did not discuss the current risk factors of metabolic
syndrome as he was on Risperidone.
• For Individual #39, the QDRR1 stated there was no anticholinergic burden despite
being prescribed atropine drops indicating a high anticholinergic burden.
• For Individual #30, the QDRR1 did not discuss whether any of the metabolic
syndrome risks were present despite being prescribed a new generation
antipsychotic.
• For Individual #29, there was no QDRR for the one due approximately in March 2023.
6. The psychiatrists did not review the QDRRs if there were psychotropic medications
prescribed. Currently, there was no tracking system to determine the date the QDRR was
reviewed by the PCP to determine if the QDRR was reviewed within 28 days of being
made available to the facility. Currently, the QDRR completion was subcontracted to
another State facility pharmacy department.
7. Three of seven records documented that prescribers implemented the recommendations
agreed upon from QDRRs. The pharmacy that completed the QDRRs was not involved in a
separate pharmacy contract administered by a pharmacy out of Omaha, NE that processed
and delivered medications. Consequently, the pharmacist that completed the QDRRs was
not able to follow-up on recommendations to determine which recommendations may
have been completed and which were not completed. Currently, the PCP did not document
in the electronic record if a recommendation was not followed due to disagreement with
the recommendation and did not document the reason for the disagreement.
The pharmacist completing the QDRRs had no access to this information until the next
QDRR review. Examples of lack of follow-up of QDRR recommendations or lack of
documentation of disagreement with the recommendation by the PCP included:
• , but there was no
documentation of this and, therefore, no closure to the recommendation. Despite the
recommendation to update the Face sheet with current diagnoses, the medical team
did not have access to complete this task for Individual #42, Individual #39,
Individual #30, and Individual #31. Additionally, for Individual #39, the PCP
disagreed with a recommendation, but this was not documented.
8. From the submitted document by the contract pharmacy filling new medication orders,
there was no order that needed a change by the PCP.
9. Monitoring for this area was included in the quarterly drug regimen review. Gaps in
information were noted for:
• .
• Individual #30 QDDR 3/3/23.
• Individual #29 had no QDRR for the quarter January to March 2023.
10. P&T Committee meetings
Attendance
3/28/23
4/11/23
5/9/23
6/21/23
Medi Dir
present
Present
present
present
Pharm Dir or
Pharm D
present
Present
present
present
PCP
two
None
one
two
Psychiatrist
present
Present
present
present

41
Psych med
monitoring
No
No
yes
yes
Neurological
meds
monitoring
No
No
No
No
Psychotropic
use
NR
NR
82/88 93%
70/87
80%
Intraclass
polypharmacy
NR
NR
4/88
4.5%
3/87
4%
Interclass
polypharmacy
NR
NR
26/88 29.5%
22/87
31%
Mixed class
NR
NR
NR
5/87
7%
Atypical
antipsychotics
NR
NR
NR
49/87
70%
First
generation
antipsychotics
NR
NR
7
10
>3 or =3
psychotropics
NR
NR
31/88 (35.2%)
28/87 (29%)
Haldol
NR
NR
NR
4
11. For one occasion, the individualIDT met to consider the recommended medication and
alternative nonpharmacological interventions and documented the rationale for the
selected decision.
12. The GRC individuals receiving psychiatric or neurologic medications were not monitored
accordingly. The P&T Committee chart indicated psychotropic medications that were
currently monitored at the P&T Committee meetings (as of 5/9/23), but not neurological
medications.
13. No DUEs were submitted.
14. No DUEs were submitted.
15. There were no dates in which psychiatry and neurology met to discuss dual purpose
medications since the last monitoring team visit.
16. Within three months of the Effective Date of this agreement, GRC conducted an external
clinical review to verify the continuing propriety of the prescriptions with
respect to every resident who fell into the following categories (listed in indicator 16), and
implemented the recommendation arising from that review.
17. For indicators 17-19, the only ADR occurred on 2/26/23 and as followed to resolution on
6/22/23. It did not involve any of the seven individuals chosen for this review.
18. See #17 above.
19. See #17 above.
20. For indicators 20-30, overall medication administration consisted of safe practices for
health and safety. Individual #91 was added due to a few individuals in the review group
not being able to be seen.
• For Individual #78, the observed medication administration (via GT) displayed no
deficiencies. The primary nurse in the home had 17 years of service, knew the
individual well, and displayed competency with administration of his medications,
including a special approach to reduce his reluctance to cooperate, which was
successful. The individual had a slight cough upon checking his GT for placement, the

42
nurse stopped everything and completed a respiratory assessment/lung sounds,
which were clear. There was verification/validation in the form of tracing logs that
reflected the nurses competency required observation/check internally.
• For Individual #42, the observed medication administration (oral, crushed) displayed
no deficiencies. There was documentation submitted of the nurses competency
required observation/check internally.
• For Individual #42, the observed medication administration (oral, crushed) displayed
no deficiencies. The nurse had a question regarding the dosing on atropine as the
product brand in use had changed. Before administering it, she contacted and
received clarification from the ordering provider. The primary nurse had 20+ years of
service, was very knowledgeable about the individual, and displayed competency
with positioning and accommodating his need for small spoon/slow and careful
administration. There was evidence submitted of the nurses competency check off.
• For Individual #30, the observed medication administration (oral, whole pills)
displayed no deficiencies. The nurse was a contract nurse that appeared competent
and though she had only recently been assigned to the home/individual, she included
him in conversation during the brief interaction. She referenced the PNMP. The
internal nurse auditor reminded her to ensure the use of hand gel was 20 seconds.
PRNs given included MOM on 6/1/23, 6/4/23, and 6/17/23, however, no
results/effectiveness was documented on the back of the MAR.
• For Individual #91, the nurse was familiar with the individual, accommodated his
needs, referenced PNMP for positioning, and administered the right medication at the
right time. The nurse checked bowel sounds with a stethoscope prior to the use of the
g-tube, but was not observed to follow standards of care for verifying placement of
the g-tube/checking residual. The nurse also was given feedback by the internal
nurse auditor as to using hand sanitizer between glove changes, and although she did
not touch anything in between, it was a potential issue.
Additionally, there was evidence
observation/check internally.
31. If the individual was subject to a medication variance, there was proper reporting of the
variance for 33% of the opportunities.
• For Individual #78, review of the MAR showed that on 5/31/23, his 8:00 pm
medications were not signed for. No medication variance form was found.
• For Individual #42, review of the MAR for dates (5/31/23-6/27/23 showed that
metoprolol was not initialed for the 8:00 pm doses on 6/2/23, 6/3/23, and 6/19/23.
Famotidine was missing initials on 6/15/23 at 8:00 pm and Risperidone 6/19/23 pm.
Additionally, valproic acid was missing on 6/4/23 and 6/22/23 (pm doses). No
medication variance form was found.
• For Individual #79, review of the MAR for dates 5/17/23-6/13/23 showed gaps in
documentation of medication administration of zinc oxide topical on 5/25/23 missing
an 8:00 pm dose of olanzapine and MiraLAX signatures for 8:00 pm doses on 5/24/23
and 5/25/23. No medication variance was found.
• For Individual #30, review of MAR for dates 5/31/23-6/27/23 did not find gaps with
routine meds. PRNs given included MOM on 6/1/23, 6/4/23, and 6/17/23, however,
no results/effectiveness was documented on the back of the MAR.
• For Individual #29, review of MAR for dates 6/14/23-6/30/23 indicated gaps in
properly documenting medications not given (possibly while hospitalized) on
6/29/23 and 6/30/23. Weekly allergy injection on 6/28/23 left blank with no note

43
on back of MAR as to why. On MAR 5/17/23-6/13/23, missing initials for Gemfibrozil
600 mg 6/7/23 at 8:00 am. Record review of MAR indicated Individual received PRN
MOM on 6/15/23 for no BM x day 3, and Tylenol on 6/22/23, however, results /
effectiveness was not documented.
• For Individual #31, review of MAR for dates 5/31/23-6/27/23 showed gaps in
documenting administration of atropine, calcium, and divalproex on 6/9/23 at 8:00
pm. No medication variance form was found. PRNs received were MOM on 6/19/23
for bowel; results were documented as effective on back of MAR. On 5/21/23, the
8:00 am meds were missing initials/circled. 5/26/23 omission was documented per
the medication variance policy. The individual did not receive his am meds at the
ordered time of 5:00 am on 5/26/23 before he traveled to a special event; PCP was
notified.
The 3/30/23 Medication Variance committee action plans included that as of 4/1/23 the
RN Supervisors would be completing monthly rounds in the med rooms and the
assignments were made. They were to be checking med carts ensuring that no
discontinued or expired meds were present, that meds were being stored in the
appropriate places and checking to see that the MAR was being signed off correctly. The
weekly meeting minutes for April, May and June 2023 did not include any follow-up on
this initiative.
32. If a medication variance occurred, evidence showed that orders/instructions were
followed, and any untoward change in status was immediately reported to the
practitioner/physician for the single occurrence.
33. For Indicators 33-36, based upon a review of the May/June 2023 MARs submitted for the
seven individuals six of seven (86%) showed gaps/issues in documentation and could not
find variance data /documentation for potential variances Level 1-2.

44
Section C.vii: Psychological Services (103-122)
Summary: The functional behavioral assessment was a component of the Comprehensive Psychological
Assessment and included current clinical and behavioral data, as well as graphs that displayed behavioral
trends. The assessments also documented modifications to behavioral programming and a detailed summary of
previous treatment. While behavioral functions were determined by a variety of indirect assessment method, it
was not evident that functional hypotheses were supported by direct observations of behavior.
Behavior plans offered guidance for responding to maladaptive behaviors. As written, they did not include
information about functionally equivalent alternatives to maladaptive behaviors. Behavior plans also did not
describe prosocial behaviors and skills, and staff were not adequately supported to recognize, teach, or reinforce
desired behaviors.
Behavioral health staff were credentialed and had the training and expertise to meet the behavioral needs of the
individuals at GRC. Behavioral health staff included two master-level psychologists, three full-time BCBAs, and
the Director who was a doctoral-level BCBA. The behavioral health team worked together to provide
individualized services and supports to the residents of GRC. Issues were noted regarding the
comprehensiveness of BSPs and consistent ongoing reviews.
The Monitoring Team was unable to find evidence of a policy or formal system outlining the expectations for
data collection. Behavioral and skill-acquisition data were collected on each shift. Data were compiled monthly
and annually by behavioral health staff. Although data were reviewed by other members of the IDT, they had not
showed that data were used to inform
decisions about services and supports.
Staff at GRC were required to complete annual trainings on a variety of relevant topics. Individualized training
on behavior plans and skill-acquisition programs occurred onsite and was delivered by the psychology assistant
clear whether training formats were standardized or that staff were developing consistent competencies
implement programs. While it was good to see that staff were provided with on-the-spot feedback and direction,
it was not clear that staff across shifts were implementing plans and programs consistently and reliably.
Substantial Compliance: Paragraph 59, Paragraph 108, Paragraph 109, Paragraph 110, Paragraph 112,
Paragraph 116 & Paragraph 118.
Partial Compliance: Paragraph 105, Paragraph 107, Paragraph 121, & Paragraph 122
#
Indicator
Overall
Score
1
GRC shall review its psychological assessment protocols to ensure they are consistent with current,
generally accepted professional standards of care, and revise them as warranted. The assessment protocols
shall:
i. Include protocols for a functional behavioral assessment to identify target behaviors and the
function of each target behavior.
ii. Identify medical, psychiatric, environmental, diagnostic, or other reasons for target behaviors; and
iii. Identify other psychological and mental health needs that may require intervention, including
history of trauma.
iv. (par. 58-64,103)
SC
2
GRC shall ensure that its suicide assessment protocol is consistent with current, generally accepted
professional standards of care and shall revise it as needed. (par. 104)
N/A
3
staff members responsible for administering suicide assessments have training in assessing suicide risk for
people with IDD and are demonstrably competent to assess such risk. (par. 104)
PC
4
thereafter as often as needed, the State shall ensure that a GRC Behavioral Health Professional completes a
PC
71%

45
psychological assessment of each GRC resident, which shall include a functional behavioral assessment for
at least those residents with behavioral needs. (par. 58-64, 105, 122)
5/7
5
The functional assessment is current (within the past 12 months). Those residents needing psychological
services other than BSPs shall receive such services in a documented manner enabling progress to be
measured in a reliable manner to determine the effectiveness of treatment. (par. 105,122_
SC
100%
5/5
6
The functional assessment is complete.
a. an acceptable direct assessment
b. an acceptable indirect assessment
c. identified antecedents of the target behaviors
d. identified consequences of the target behaviors
e. The findings are summarized based on the hypothesized antecedent and consequent conditions
that affect the target behavior
f. ensure individuals receive the needed counseling and other therapeutic interventions
recommended from these assessments.
(par. 52,106,122)
NC
0%
0/5
7
If the individual exhibits behaviors that constitute a risk to the health or safety of the individual/others,
and/or engages in behaviors that impede his or her growth and development, the individual has a BSP.
(par. 107)
SC
100%
5/5
8
The individual has goals/objectives related to psychological/behavioral health services, such as regarding
the reduction of problem behaviors, and an increase in replacement/alternative behaviors.
• The goals are measurable.
• The goals are based upon the assessment.
• Reliable data is available that supports/summarizes status/progress.
(par. 107)
NC
0%
0/5
9
The individual is making expected progress. (par. 107)
NC
0%
0/5
10
Progress/lack of progress is responded to appropriately. (par. 107)
NC
0%
0/5
11
There was documentation that the BSP was implemented within 14 days of attaining all the necessary
consents/approval. (par. 61,107)
NC
%
0/5
12
The BSP was current (within the past 12 months). (par. 59,107)
SC
100%
5/5
13
The BSP was complete.
i. acceptable operational definitions of target behaviors
ii. acceptable operational definitions of replacement behaviors
iii. the use of positive reinforcement in a manner that is likely to be effective.
iv. antecedent strategies for weakening undesired behaviors.
v. consequent strategies for weakening undesired behaviors.
vi. the training/reinforcement of replacement behaviors
vii. sufficient opportunities for replacement behaviors to occur/be trained.
viii. If the replacement behaviors require the acquisition of new skills, they are in a skill acquisition plan
format.
ix. the replacement behaviors should be functional, when possible
x. treatment objectives clear, precise, interventions based on the results of the functional assessment
(par. 58,107)
NC
0%
0/5
14
Each resident with behavioral health needs as determined by the assessment process set forth in
Paragraphs 103-106 shall be assigned a Behavioral Health Professional whose caseload and expertise are
Any resident with severe behavioral health needs
that present risk to health and safety shall be assigned a Behavioral Health Professional who is a Board-
Certified Behavior Analyst. (par. 108)
SC
15
Caseloads and assigned BH progressions will be commensurate with the variety of needs of the residents
on their caseload. (par. 109)
SC
16
GRC shall retain enough Behavioral Health Professionals who are Board Certified Behavioral Analysts to
(par. 68,110)
SC

46
17
GRC shall provide residents requiring a BSP with individualized services and comprehensive programs.
(par 68,111)
NC
18
GRC shall employ a qualified Director of Psychology who is responsible for maintaining a consistent level of
psychological care throughout the GRC, (par. 68,112)
SC
19
GRC shall conduct reliable reviews to assess the quality of behavioral assessments and BSPs of each
Behavioral Health Professional at least semi-annually. (par. 113)
NC
20
behavior support plans. (par. 114)
NC
21
frequency and variability of behavioral incidents, as well as the effectiveness of treatment. (par. 114,115)
NC
0%
0/5
22
Behavioral Graphs are:
i. Simple and easy to interpret.
ii. Graphed at intervals that best demonstrate response to treatment.
iii. Include phase change lines, with axes labeled appropriately.
(par. 114,115)
PC
0/1
23
make appropriate treatment decisions. (par. 114,115)
NC
0%
0/5
24
If the individual has been presented in peer review, there is evidence of documentation of follow-up
and/or implementation of recommendations made in peer review. (par. 114,115)
NC
0%
0/5
25
If the individual has a BSP, the data collection system adequately measures his/her target behaviors across
all treatment sites. (par. 115)
NC
0%
0/5
26
If the individual has a BSP, the data collection system adequately measures his/her replacement behaviors
across all treatment sites. (par. 115)
NC
0%
0/5
27
If the individual has a BSP, there are established acceptable measures of:
a. data collection timeliness
b. IOA
c. treatment integrity.
(par. 115)
NC
0%
0/5
28
If the individual has a BSP, there are established goal frequencies (how often it is measured) and levels
(how high it should be) of:
a. data collection timeliness
b. IOA
c. treatment integrity.
(par. 115)
NC
0%
0/5
29
If the individual has a BSP, goal frequencies and levels are achieved of
a. data collection timeliness
b. IOA
c. treatment integrity.
(par. 115)
NC
0%
0/5
30
If the Individual has a BSP, it is written so that it can be easily understood and implemented by Direct Care
Staff. (par. 116)
SC
100%
5/5
31
BSPs are consistently implemented by staff. Any significant deviations in implementation are immediately
reported to the assigned Behavioral Health Professional or psychology assistant, and to the GRC
administration so that appropriate action can be taken. (par. 117)
NC
0%
0/5
32
All Behavioral Health Professionals and psychology assistants shall successfully complete annual
competency-based training in providing trauma-informed behavioral services to individuals who have IDD
and challenging behaviors. (par. 118)
SC
33
Staff monitoring the implementation of behavioral programming has been deemed competent to
implement programming and shall be monitored by Behavioral Health Professionals. (par. 119)
NC
34
All direct contact staff and their supervisors shall successfully complete competency-based training on
severe behavioral needs, the co-occurrence of mental health needs and IDD, and the principles of applied
behavioral analysis at least annually. (par. 120)
NC

47
35
GRC has a monitoring schedule developed that ensures ongoing review of BSP implementation. (par. 121)
PC
60%
3/5
36
hology Department shall routinely collect, analyze, and act on valid and reliable data sufficient
to ensure that the use of restrictive procedures at GRC is consistent with current, generally accepted
professional standards and implemented in an appropriate manner. (par. 125)
NC
Comments:
1. Comprehensive Psychological Assessments were required to include a functional
challenging behaviors. Assessments were also required to include information about
medical, psychiatric, environmental, diagnostic, or other reasons for target behaviors, as
well as supports that were trauma-
and mental health needs.
2. Following a suicide threat or suicide attempt made by an individual, the assigned
psychologist or a registered nurse completed a suicide risk screen to determine the level
of risk and next steps. The suicide risk screen determined if a suicide watch order that
consisted of increased supervision, environmental modifications, and other safety
precautions and restrictions was necessary.
The suicide watch protocol identified points of contact for reporting and documentation
purposes. The suicide risk screen provided multiple-
comments.
reason for making the suicide threat or attempt. During the previous monitoring visit, the
Center informed the Monitoring Team of a plan to revise the suicide assessment protocol
and suicide risk screen to include more evidence-based guidance on response to action
steps. Revisions to the protocol and risk screen were still ongoing and will be evaluated
once completed. This provision of the Consent Decree was not applicable to the
individuals in the review group because none of the individuals had exhibited suicidal
ideation or made a threat or attempt that required a suicide assessment or risk screening.
3. All staff who had routine interactions with individuals received training on the suicide
watch protocol. Suicide assessments were completed by a psychologist or nurse.
There was no evidence of competency-based training on the assessment of suicide risks.
This provision of the Consent Decree was not applicable to the individuals in the review
group because none of the individuals had exhibited suicidal ideation or made a threat or
attempt that required a suicide assessment or risk screening.
4. For five of the seven individuals in the review group, Comprehensive Psychological
Assessments were current and had been updated within the past twelve months.
• For Individual #29, the assessment was not completed according to required
timelines.
• For Individual #39, it was not evident that he had had an assessment completed prior
to the current assessment and his current assessment was not in compliance. The
assessment lacked required components as per policy, including information about
his history, strengths, and communication abilities. It was also not clear when the
assessment had been written because the document was not dated.
5. The functional assessment was a component of the Comprehensive Psychological
Assessment and included current clinical and behavioral data as well as graphs that
depicted behavioral trends. Modificati
were tracked in a detailed and thorough summary of previous treatment.
For five of five individuals, the assessments contained the required components. The two
remaining individuals, Individual #29 and Individual #39, did not exhibit challenging
48
behaviors that required a BSP, and their assessments were not required to describe target
behaviors or include behavioral data.
Regarding trauma and mental health needs, the individuals in the review group did not
require specialized supports beyond what their current behavioral programming and
psychiatric supports provided. There was nothing in their histories that indicated the
need for trauma-based interventions or supports.
It was positive to learn that the social work division at GRC had used information
contained within the psychological assessment to explain the behavioral presentations of
two individuals whose referrals to community providers had been denied based on
behavioral concerns and support needs. According to the social work team, medication
adjustments, changes to behavioral programming, and environmental factors found
within the assessment were shared with the providers who then reconsidered the
referrals and agreed to visit GRC to assess the individuals onsite.
6. Although multiple assessment tools were used to determine behavioral functions for the
five individuals who required behavior supports, the tools were indirect and functional
hypotheses were generally derived from staff interviews.
Functional hypotheses were not supported by direct observations of behavior.
Assessments did identify antecedents and consequences that were hypothesized to
provoke or maintain target behaviors based on their functions. The assessments did not
recommend counseling and other therapeutic interventions, though it was not evident
that the individuals in the review group required interventions beyond what their current
behavioral and psychiatric programming provided.
7 Five of five (100%) individuals who engaged in behaviors that impeded growth and
development had a BSP.
8 Behavior plans provided guidance and support to prevent and respond to instances of
problematic behaviors. The plans did not identify or define replacement behaviors or
describe how replacement behaviors were trained or reinforced. Training of replacement
behaviors was found in Individual Implementation Programs (IIPs). In general,
replacement behaviors were not function-based or based on assessments, and they did
not typically teach functional skills. Replacement behaviors were mostly objectives that
taught the individual to comply with a demand or tolerate an aversive situation. For
example:
• Individual #31 engaged in aggression, property destruction, teasing and provoking
others, self-injury, and elopement. The behaviors were maintained by access to
attention, escape, and preferred stimuli. His behavior plan and skill acquisition
programs did not identify or train functionally equivalent replacement behaviors. The
replacement behavior training outlined in his IIP taught him to sit with his hands in
his lap when prompted.
• Individual #78 exhibited signs of agitation that included grinding his teeth if he
perceived others to be too close to him. As a replacement behavior, he was taught to
tolerate staff sitting next to and touching him.
• Despite not being included in behavior plans as functionally equivalent replacements,
it was good to see that Individual #42 and Individual #79 were being taught to use
communication devices to express their desires to delay or escape nonpreferred
activities. Individual #79 was also learning to request assistance using her device.
• For Individual #30, who engaged in inappropriate sexualized behavior, his
replacement behaviors were verbal responses to questions about ways to
appropriately greet females, how to keep his hands to himself, and how to engage in
appropriate conversation. It was not clear that he was learning to exhibit appropriate

49
and/or alternative responses in natural settings or situations, or that he had the
opportunity to practice his skills during naturally occurring opportunities.
Some behavior plans described how and how often an individual was reinforced for
desired behaviors, while others provided vague guidance to staff and did not offer specific
examples of desired behaviors to be reinforced. For Individual #30, Individual #42, and
Individual #78, their behavior plans guided staff to reinforce appropriate social
interactions with others. It was not clear what appropriate social interactions were for
each of the individuals, or which specific behaviors staff were to reward.
As written, behavior plans did not promote growth, development, or independence
because they did not teach functionally equivalent alternatives to problematic behaviors.
Behavior plans also did not describe prosocial behaviors and skills, and staff were not
adequately supported to recognize, teach, or reinforce desired behaviors.
9 Regarding behaviors targeted for decrease, partial interval measures were typically used
to determine behavioral levels from month to month. In general, individuals were not
making progress towards achievement of behavioral objectives. Some data remained
steady over time, while other data showed increasing trends. GRC had not established a
system to assess data reliability. Reliability of data was, therefore, questionable and did
not accurately display the indi
10 Even though because
the data could not be deemed to be reliable (see indicator #9), it was also not evident that
IDTs were responding to an
manner. For example:
• Individual #31 had engaged in higher levels of aggression and property destruction
over the course of three months. There was no evidence of a discussion or plan to
address the increasing trend.
• Individual #79 was diagnosed with pica. According to her data, she had not engaged
in pica for at least 12 months. It was not clear that the IDT had discussed or
developed a plan for next steps. Pica was considered a barrier to her community
transition, although the data showed that the behavior was no longer occurring. The
data, however, were questionable because according to information shared with the
Monitoring Team, staff had verbally reported at least one instance of the behavior
that had not been documented during the year. The Monitoring Team informed GRC
11. Following review by the Internal Peer Review Committee, behavior plans were reviewed
by the Human Rights Committee. Behavior plans were required to be implemented within
14 days of HRC approval. This paragraph of the Consent Decree was not applicable to two
of the seven individuals who did not exhibit behavioral challenges that required behavior
plans. For two of the other five individuals, their behavior plans were implemented within
the 14-day timeline. For the three remaining individuals, behavior plans were not
implemented on time. Findings included:
Individual
#
Date of
Psychological
Assessment
Behavior
Support
Plan
Written
Human
Rights
Approval
Obtained
Behavior Support Plan
Implemented
29
10/27/22
N/A
8/9/22
N/A
30
2/15/23
2/17/23
3/20/23
3/21/23
31
11/16/22
11/15/22
12/29/22
12/21/22
39
Not dated
N/A
8/30/22
N/A
42
2/1/23
2/1/23
2/27/23
3/2/23
78
8/8/22
8/11/22
9/20/22
9/2/22
79
9/26/22
9/27/22
12/29/22
10/17/22

50
• Individual #29 did not exhibit challenging behaviors that warranted a behavior plan.
•
timelines.
•
been developed and the behavior plan was implemented prior to HRC approval.
• Individual #39 did not exhibit challenging behaviors that warranted a behavior plan.
His psychological assessment was not dated.
•
timelines.
• o HRC approval.
•
12. Five of five individuals who engaged in behaviors requiring behavior plans had current
behavior plans.
13. Behavior plans used objective, clear, and concise language to describe precursor
behaviors, target behaviors of concern, and strategies for avoiding and addressing target
behaviors. The plans also provided guidance on data collection. As discussed in comments
for indicator #8, behavior plans did not include replacement behaviors. Replacement
behavior training was outlined in Individual Implementation Programs (IIPs). In general,
replacement behaviors were not functionally-equivalent to respective maladaptive
behaviors and antecedent and consequent strategies did not correspond to behavioral
functions. Positive reinforcement was not always used to reward target behaviors or
skills. For example:
• Individual #31 engaged in aggression, property destruction, leaving the assigned
area, and provoking others. According to his behavioral assessment, the behaviors
functioned to gain access to attention. His behavior plan included strategies to reward
appropriate escape. Reinforcement was not provided for prosocial attention seeking
behaviors.
• Individual #78 had a behavior plan because he was prescribed psychotropic
medications to address symptoms of agitation. The symptoms included loud
vocalizations, swatting in the air, and pushing others away. He engaged in the
behaviors in attempts to escape aversive situations. His behavior plan included a
strategy to reward positive social interactions. The plan did not include strategies to
reward prosocial escape.
Transition BSPs had been developed for individuals with higher-level support needs for
challenging behaviors. Transition BSPs were developed after the BCBA visited the
prospective residential site and determined what the individual would specifically need
for behavioral supports. The plans were supposed to provide community providers with
specialized information needed to support the individual effectively in the community.
Transition BSPs were clear and easy to understand. While they did provide valuable
i
address behavioral challenges, they did not offer information and guidance beyond what
the traditional behavior plans provided. Transition BSPs had the potential to equip
community provider staff with the proper tools to prevent and address behavioral
challenges exhibited in the community. Transition BSPs also had the potential to teach
relevant community-based replacement behaviors and behavioral strategies. For
example:
Crowded spaces were aversive to Individual #42 and Individual #78. Both individuals
were learning to tolerate staff being in their personal spaces. Given their impending
transitions to the community and the likelihood that they would visit highly populated
community venues such as restaurants, shopping malls and sporting events, their

51
transition BSPs could have included training, desensitization techniques and coping skill
strategies to better support them to engage in community-based activities.
14. (Indicators 14-16). There were three full-time BCBAs and two master-level psychologists
who worked to oversee the behavioral programming of the individuals who remained at
the Center. Two of the three BCBAs were contracted to develop community-based
transition behavior plans for individuals with significant behavioral challenges and needs.
One BCBA was assigned to support individuals who had behavioral health needs that did
not pose a significant risk to health and safety. All five behavioral health professionals
reported directly to the Director of Psychology who was a doctoral level BCBA.
During the last monitoring visit, the Center shared a plan to ensure that all behavior plans
were reviewed and approved by BCBA. It was not evident that the Center had fully
accomplished this, however, functional behavioral assessments and behavior support
plans were written by staff who had been trained in Applied Behavior Analysis.
17. GRC provided individuals with individualized services and programs. Programs, however, did
not address many of the individuals
not functional, or function based (see comments for indicators #8 and #13).
18. The Director of Psycholo
psychology. The Director actively participated in meetings and was involved in the overall
care of the individuals at GRC.
19. The Monitoring Team was unable to find evidence of reliability measures to assess the quality
of behavioral assessments and BSPs or for collection of valid and reliable data. There was also
no evidence of a process for assessing interrater agreement of behavioral instances as they
occurred. Data was not reviewed and discussed by the IDT and data were not used to inform
decisions about behavioral programming. For individuals who were not making progress,
their assessments and interventions were not revised to promote behavioral goal
achievement.
20. The Monitoring Team was unable to find evidence of a policy or system outlining the
acquisition and analysis of behavioral data. This was not included in their behavioral health
policy.
21.
assessment and offered a comprehensive timeline of supports and behavioral programming
that included psychiatric consults, medication regimen adjustments, and new or modified
behavioral interventions. In conjunction with behavioral data and graphs, the timeline could
have permitted ongoing clinical review of previous and current treatment and supports, and
the monitoring of progress and effectiveness of treatment. It was not clear, however, that
behavioral data and graphs were shared with the IDT and used to make decisions about
behavioral programming.
22. Behavioral graphs were simple, easy to interpret, and displayed variability and progress
overall. Graphs most often displayed the number of behavioral incidents per month. Graphs
did not include phase change lines to highlight the impact of interventions and modifications
to behavioral, psychological, and/or psychiatric treatment of target behaviors. For example:
•
environmental modifications to his bedroom and to add a program for staff to prompt him
to identify his emotions and communicate his feeling using words instead of problematic
behaviors. The modifications were not reflected in his graphs.
• 3 after he was started on psychotropic
medications for agitation. The graph displaying a decreasing trend in the levels of
agitation each month did not reflect the BSP or the new medication regime.
52
23. The IDTs met monthly for an integrated review (MIR) of behavioral programming and other
therapeutic and habilitative supports. The meetings were a forum for discussion about
habilitative progress and supports, behavioral incidents, trends, and ongoing needs and
concerns. When a risk or concern was identified, the IDT typically developed a plan to address
it. Anecdotal information as well as behavioral and skill-acquisition data were presented for
IDT review, and treatment recommendations and decisions were generally based on that
information and data. There were times, however, when information presented to the IDT did
not lead to robust discussions about a problem behavior or result in appropriate treatment
decisions. For example:
•
the SIB he exhibited, most of which resulted in bruising to his body. The IDT had
not fully discussed the frequency or severity of the SIB, and data were not
presented for review. It was also not clear that the IDT had discussed appropriate
interventions to address the behavior.
24. Peer review meetings occurred days following the development of psychological assessments
and BSPs, and annually thereafter. Peer review meetings were a forum for the Director of
Psychology, along with a team of BCBAs and psychologists, to assess the overall quality of
behavioral programming and supports and ensure assessments and plans aligned with GRC
policies. Recommendations made by the team were considered and sometimes incorporated
into assessments and/or plans. Evidence of follow-up and response to peer review
recommendations was not always clear.
• For Individual #31 and Individual #78, the peer review clinical feedback form
indicated that follow-up to address recommendations had been completed. For the
other individuals, follow-up had not been documented.
25. (Indicators 25-26). It was not evident that behavioral and skill-acquisition data were
measured across all treatment settings. Behavioral data measured the number of intervals
during which problematic behaviors were exhibited per month. Replacement behavior data
measured the number of teaching trials completed per month. For all individuals in the review
group, behavioral data that were compiled each month did not identify the setting where
target behaviors were exhibited. IIPs also did not describe treatment settings and it was not
possible to determine if teaching trials were conducted at home or at vocational or day
programs. Awareness of the setting could have been helpful in assessing antecedents and
motivation with respect to problematic behaviors.
27. (Indicators 27-28). Behavioral data were generally collected using 30-minute partial intervals.
At the end of each shift, staff recorded the number of intervals during which the problematic
behavior occurred. Data collection instructions were included on accountability sheets and the
IIP document that staff were able to access. There was no system for measuring reliability or
inter-observer agreement, and treatment integrity measures did not adequately or accurately
show staff competencies in all aspects of behavioral programming (see indicator #31). Data
collection instructions also did not identify expectations for behavioral levels (how high they
should be). Accountability sheets provided staff with the information and guidance needed to
collect behavioral and skill-acquisition data each shift. The documents included examples of
problematic behaviors and what to look for when evaluating whether the individual
completed an objective or task. Accountability sheets did not indicate the goal level of
behavior or the skill-acquisition criterion the individual was working to achieve. For example:
•
exposing himself to others, and sexual statements. The document also included a

53
place to document the number of times he engaged in those behaviors during the
morning and event shifts. The document did not indicate performance goals, and it
was not clear what he was working to achieve.
•
destruction, and agitation. The document did not include behavioral expectations or
goals.
29. This indicator was not met, because the reliability and fidelity measures were not adequate
(see indicators #2728 and #31).
30. Behavior plans used clear and concise language to describe precursor behaviors, target
behaviors of concern, and strategies for avoiding and addressing target behaviors. The plans
also provided guidance on data collection. The plans were written in a way that could be easily
understood and implemented by direct care staff.
31. Program Implementation and Monitoring (PIM) forms were fidelity measures used to assess
staff knowledge and ability to implement behavior plans and skill-acquisition plans. Regarding
plan along with a
their knowledge of that section of the plan. Behavioral PIM forms were not individualized, or
competency based. They did not identify specific skills for staff to describe or demonstrate. If
the staff did not accurately describe or demonstrate their knowledge of a particular section of
the behavior plan, then the evaluator used the comments section of the PIM form to document
the type of retraining provided to the staff. If there were significant deviations in
specific skills or knowledge the staff was lacking. It was also not evident that deviations in
implementation were reported to the assigned psychologist, BCBA, or administrator.
32. -34. All staff were required to complete Applied Behavior Analysis training in addition to a
two-day training on the following topics:
• Building healthy relationships.
• Healthy communication
• Healthy conflict resolution.
• Trauma-informed services.
• Positive Behavioral Supports.
• Intervention and restraint during emotionally escalated situations.
It was not evident that staff had received training in the areas of severe behavioral needs or
the co-occurrence of mental health needs and IDD. When asked about training methods, staff
reported that they had been trained by psychology assistants and QIDPs who provided
overviews of behavioral programs, skill-acquisition programs, and data collection systems.
Trainings did not appear to be standardized (i.e., trainees were not receiving the same
information and developing a consistent set of competencies). Training rosters included
printed names and signatures of staff who had received training on individual behavior plans.
It was not clear what had been trained or what the training format was.
35. Although the IIP Monitoring Procedure protocol required Program Implementation
Monitoring (PIM) to be completed monthly for each individual, monitoring of behavior plans
did not occur consistently for all individuals in the review group. For example:
• For Individual #30, Individual #31, and Individual #79 PIM documents were
completed monthly.
• For Individual #42, PIM documents were completed three months apart.
• For Individual #78, PIM documents were completed two months apart.
Restrictive procedures other than psychotropic medications were listed as an environmental
need in some behavior plans. Staff knowledge of restrictive procedures was assessed via the
54
Program Implementation and Monitoring (PIM) process, using a form that indicated whether
staff were able to describe or demonstrate their knowledge of a particular section of an
of the plan the staff were expected to describe or demonstrate. PIM forms also did not
evaluate or demonstrate reliability. It was not evident that reliability checks were occurring or
that the GRC had implemented a system to routinely collect, analyze, and act on data regarding
the use of restrictive interventions. Restrictive procedures were included in Monthly
Integrated Review (MIR) minutes, however, there was no evidence of a robust discussion or
analysis of the procedures. Especially lacking was the impact of the community on the
ind
36. See indicator 35.

55
Section D Restrictive Interventions (123-127)
Summary: There were policies and procedures directing Facility practices. For the most part, policies appeared
to be appropriate and comprehensive. Restrictive interventions were not always consistent with current,
generally accepted professional standards of care.
Partial Compliance: Paragraph 123, Paragraph 126, & Paragraph 127.
#
Indicator
Overall
Score
1
GRC shall provide residents with a safe and humane environment and ensure they are protected from
harm, including the unnecessary use of restrictive interventions, consistent with current, generally
accepted professional standards of care. (par. 123)
PC
2
monthly integrated reviews, to ensure that: a plan to implement the alternative interventions is being
implemented, and to update or revise the plan to implement the alternative interventions as warranted.
(par. 124)
NC
3
Psychology Department shall routinely collect, analyze, and act on valid and reliable data sufficient
to ensure that the use of restrictive procedures at GRC is consistent with current, generally accepted
professional standards and implemented in an appropriate manner. (par. 125) (par. 126)
NC
4
quality management system shall include processes to ensure that the use of restrictive procedures
at GRC is consistent with current, generally accepted professional standards and implemented in an
appropriate manner. The State shall ensure that the Psychology Department shares restrictive
intervention data with Quality Management program, and that the data is valid, analyzed, and
utilized for quality improvement, pursuant to the processes set forth in Section IV.K
PC
5
Whenever problems are identified under the processes set forth in Paragraphs 125-126, GRC shall
develop and implement plans to remediate the problems. (par. 127)
PC
Comments:
1. Resident homes appeared to be a safe and humane environment, however restrictive
interventions were not always consistent with current, generally accepted professional
standards of care. For example, for Individual #29 and Individual #78, there were
cameras installed in the common areas of the homes. Although the cameras had been
approved by the Human Rights Committee, HRC documentation did not reflect a thorough
review or discussion about the cameras, and it was not clear why the cameras were
necessary. The purpose of the camera must be clearly indicated so that rights may be fully
reviewed within the right context. It was also not clear that there had been a discussion
about less-intrusive monitoring options.
Individual #29 and Individual #78 also required automatic external defibrillators (AEDs)
that were life saving devices, however, they were considered restrictive because the boxes
they were secured in were equipped with alarms. The devices were also included in HRC
documentation and related meetings that did not reflect a thorough discussion or
review. Individual #31 required several restrictive interventions to prevent and address
challenging behaviors, including: 1:1 supervision to prevent and address aggression,
property destruction and SIB; window blocks to prevent unauthorized departure; and
enclosed televisions, secured electronics, and curtains that were secured to the window
frame with Velcro all to prevent property destruction. Restrictive interventions
for Individual #31 were included in his behavior plan and had been approved by the
Human Rights Committee. The Monitoring Team was unable to find evidence of a
thorough discussion or review of the restrictions, or any consideration of alternative and
less-restrictive options.
2. Program Implementation and Monitoring Process (PIM) forms did not evaluate or
demonstrate reliability. It was not evident that reliability checks were occurring or that
the GRC had implemented a system to routinely collect, analyze, and act on data regarding
the use of restrictive interventions. Restrictive procedures were included in Monthly
56
Integrated Review (MIR) minutes, however, there was no evidence of a robust discussion
or analysis of the procedures.
3. Restrictive procedures other than psychotropic medications were listed as a
programmatic restraint in some behavior plans. Staff knowledge of restrictive procedures
was assessed via the Program Implementation and Monitoring (PIM) process, using a
form that indicated whether staff were able to describe or demonstrate their knowledge
of a particular section of an behavior plan. PIM forms did not clearly identify
specific elements or subsections of the plan the staff were expected to describe or
demonstrate. PIM forms also did not evaluate or demonstrate reliability. It was not
evident that reliability checks were occurring or that the GRC had implemented a system
to routinely collect, analyze, and act on data regarding the use of restrictive interventions.
Restrictive procedures were included in Monthly Integrated Review (MIR) minutes,
however, there was no evidence of a robust discussion or analysis of the procedures.
4. Restrictive interventions, including the number of individuals with any type of restrictive
intervention and the number of individuals with restrictive intervention(s) based on a
peer's identified needs, were included on the monthly Quality Council Meeting report. It
was clearly documented that the data on restrictive interventions was the responsibility
of the QIDPs. This change occurred in July 2020. Prior to that, the house psychologist was
responsible for providing these data. Recommended action for the 4/18/23 Quality
Council meeting included having psychologist review pica diagnosis and how data was
collected. This suggested that a psychologist may not routinely be involved in verifying
the validity of data and analyzing it. Also included in the monthly Quality Report was data
on the number of programs with restrictive interventions that were submitted and that
were approved by the Human Rights Committee each month. In addition, each month's
report contains a detailed analysis of restraint use. Also lacking was the impact of the
community on the restrictions and how these would change or be presented
in the community.
5. Examples of remediation actions were noted in an untitled document that included
recommended follow-up to the Quality Council meetings. For the months of March and
April 2023, the number of restrictive interventions decreased by 7, from 67 in March to
60 in April. In May, there was an increase of 20, from 60 to 80. In June that number
decreased by 7 to 73. Since there was a decrease in April and again in June, remediation
action was likely not required. However, no evidence of remediation following the May
increase in the number of restrictive interventions was noted. This practice of a second
document for noting remediation actions started for the meeting that occurred on
3/21/23 and going forward. For the meeting dated 4/18/23, there was a month-to-month
increase of six individuals with restrictive interventions from February 2023 (61) to
March 2023 (67). On the tracking document for remediation, there were two
recommended actions for the 4/18/23 meeting. However, both actions were for the same
individual (Individual #7). No action was noted for the other five additional individuals
who required restrictive interventions for the month of March 2023. Further, a review of
minutes from the Quality Council meeting that occurred on 2/21/23, action needed was
to be noted in the meeting minutes document itself. There was an increase of two
individuals who required restrictive intervention from December (61) to January (63),
but action needed was not documented on the minutes for the 2/21/23 Quality Council
meeting that included a review of these data.

57
Section D.i Restraints (128-143)
Summary: For the six-month pre-visit data collection period the Facility reported 14 incidents of restraint
involving 11 Individuals. From these data, it appeared that three of the 14 were medical restraint (a hold
necessary to allow for a medication injection or blood draw) leaving 11 restraints for nine individuals that were
related to behavior that was presented as an imminent danger to self or others.
Four restraints episodes were selected for this review. Two were brief arm holds of the same Individual
(Individual # 11) to allow for a blood draw necessary to monitor drug levels. The other two were in response to
a behavior incident. Documentation, for the most part, was in order and easy to follow.
Substantial Compliance: Paragraph 128, Paragraph 131, Paragraph 138, Paragraph 141, & Paragraph 142
Partial Compliance: Paragraph 129, & Paragraph 130.
#
Indicator
Overall
Score
1
permitted restraints by level of restriction. (par. 128)
SC
2
The resident posed an immediate and serious risk of harm to him- or herself or others. (par. 129)
PC
50%
1/2
3
The restraint was the least restrictive intervention necessary. (par. 129)
PC
50%
2/4
4
The restraint was used as a last resort and after a graduated range of less restrictive measures were
exhausted or considered in a clinically justifiable manner. (par. 129)
PC
50%
2/4
5
The restraint was applied in the least restrictive form and duration of restraint necessary and appropriate
for the circumstances. (par. 129)
PC
50%
2/4
6
The restraint was applied in accordance with applicable written policies, procedures, and plans governing
restraint use. (par. 129)
NC
0%
0/4
7
The restraint was not used for punishment, for convenience of staff, or in the absence of, or as an alternative
to, treatment. (par. 130)
PC
50%
2/4
8
Prone restraint was not used. (par. 131)
SC
100%
4/4
9
The restraint was terminated as soon as the resident was no longer a danger to him/herself or others. (par.
132)
PC
75%
3/4
10
(par. 133)
NC
0%
0/4
11
If a medical restraint (for routine medical or dental care) the ISP included treatments or strategies to
minimize or eliminate the need for restraint. (par. 133)
NC
0%
0/2
12
Within 30 minutes after initiation of restraint, a physician, physician's assistant, nurse practitioner, or a
Registered Nurse with training in application and assessment of restraint, conducted and documented a
face-to-face examination of the resident, including a check for restraint-related injury. (par. 134)
PC
50%
2/4
13
Staff (who meet criteria) checked the resident as soon as possible but, in exceptional circumstances where
restraints exceed 15 minutes, no later than 15 minutes from the start of the restraint, to review the
application and consequence of restraint. (par. 135)
NC
25%
1/4
14
A registered nurse shall monitor and document vital signs and mental status of a resident in restraints at
NC
0%
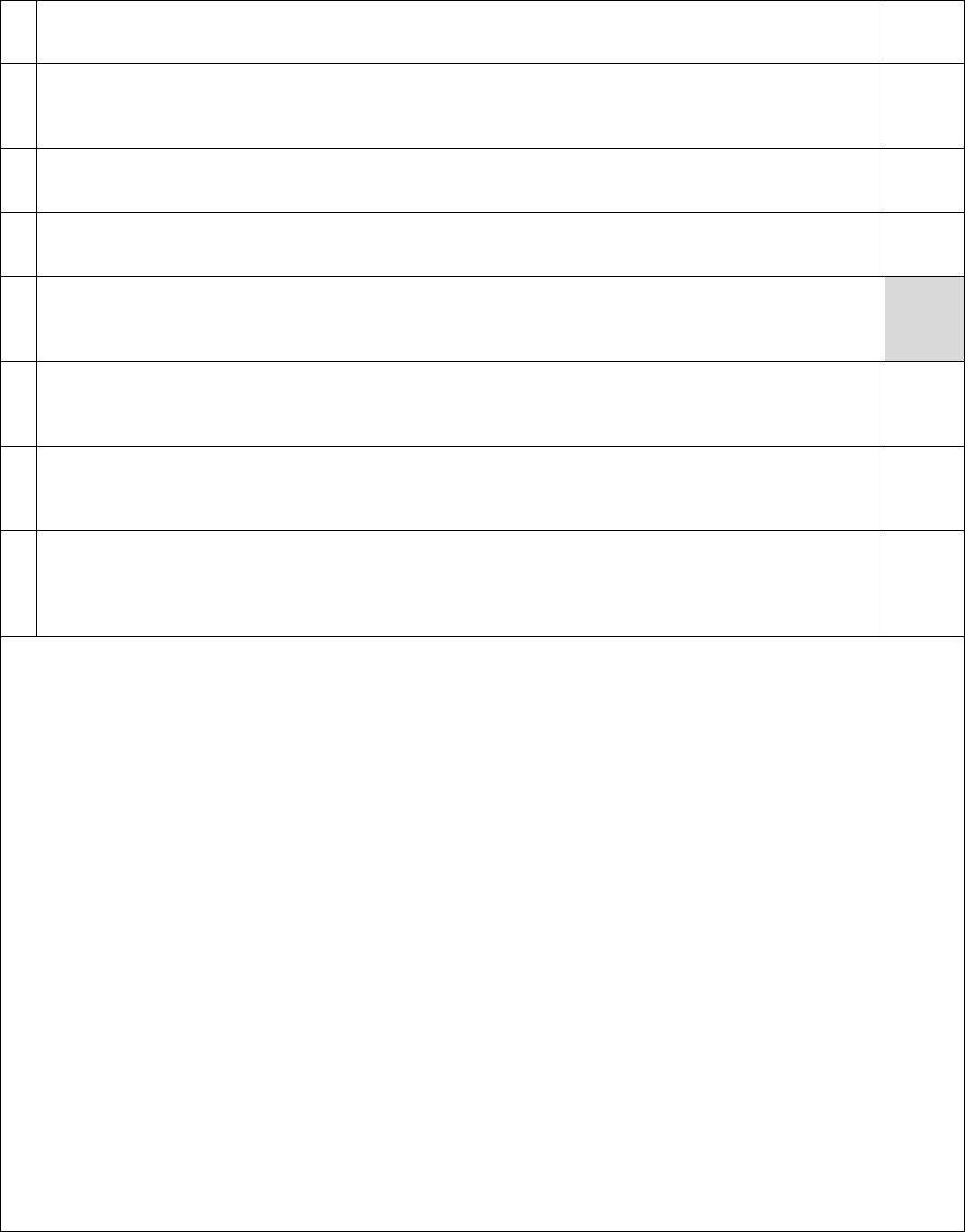
58
restraint pursuant
the schedule and type of monitoring required). (par. 136)
0/4
15
Every resident in physical or medical mechanical restraint shall receive opportunities to exercise restrained
limbs, to eat as near mealtimes as possible, to drink fluids, and to use a toilet or bed pan, consistent with
generally accepted professional standards of care; and shall be under continuous one-to-one supervision.
(par. 137)
NC
0%
0/4
16
Mechanical restraints were not used (other than as prescribed for necessary medical care). (par. 138)
SC
100%
4/4
17
The restraint was documented consistent with generally accepted professional standards of care. (par. 139)
NC
0%
0/4
18
NA
19
GRC staff responsible for applying restraints have successfully completed competency-based training on
applicable BSPs and safety plans; approved verbal intervention and redirection techniques; approved
restraint techniques; and adequate supervision of any resident in restraint. (par. 141)
SC
100%
4/4
20
GRC Behavioral Health Professionals shall be involved in the selection of any crisis management system used
by GRC. All Behavioral Health Professionals at GRC shall have a high degree of expertise with the crisis
management system. Training shall be conducted by certified trainers. (par. 142)
SC
21
leads to use of the restraint and alternative, positive adaptive behaviors to be taught to the resident to
replace the behavior that initiates the use of restraint, as well as other programs, where possible, to reduce
or eliminate the use of such restraint. (par. 143)
PC
50%
2/4
Comments:
1.
and shall categorize permitted restraints by level of restriction. This policy was
revised/updated 1/25/23 but should be reviewed to determine if the findings in this
report suggest a need for policy changes or refinement.
2. The individual posed an immediate and serious risk of harm to him- or herself or others.
• For the restraint of Individual #46, the RRC minutes noted staff could have stepped
back and deescalated (making the restraint unnecessary).
• For restraint of Individual #11, these were both medical restraints (arm hold) to
allow for med procedure (2/1/23 Covid test, 6/8/23 blood draw)
3. The restraint was not consistently the least restrictive intervention necessary.
• For Individual #46, refer to the comment in #2 above.
• For Individual #48, an Incident Investigation was conducted post restraint. It
implementing the restraint.
4. The restraint was not always used as a last resort and after a graduated range of less
restrictive measures were exhausted or considered in a clinically justifiable manner.
• For Individual #46, refer to the comment in Indicator 2 above.
• For Individual #48, refer to the comment in Indicator 3 above.
5. The restraint was not consistently applied in the least restrictive form and duration of
restraint necessary and appropriate for the circumstances.
• For Individual #46, refer to the comment in Indicator 2 above.
• For Individual #48, refer to the comment in Indicator 3 above.

59
6. The restraint was not applied in accordance with applicable written policies, procedures,
and plans governing restraint use.
• For Individual #46, Restraint Reduction Committee review concluded this was an
unauthorized restraint as it was performed in a sitting position.
• For Individual #11, the 2/1/23 Type 1 report (investigation) concluded these
restraints failed to meet criterion for medical stabilization. The 6/8 /23 Type 1 report
(investigation) showed there was no guardian permission for this type of restraint.
• For Individual #48, the post restraint investigation determined restraint was not the
least restrictive intervention.
7. For two of four restraints, the restraint was not used for punishment, for convenience of
staff, or in the absence of, or as an alternative to, treatment. For Individual #46, and
Individual #48, the issues described in Indicators 2-6, the Monitoring Team cannot rule
out these two restraints may have been done for the convenience of staff.
8. Prone restraint was not used for 4/4 restraints reviewed. The Monitoring Team did not
find any evidence of the use of prone restraint.
9. On three of four occasions, the restraint was not terminated as soon as the resident was
no longer a danger to him/herself or others. For Individual #46, the restraint was not
effective, and he was given a chemical restraint.
10.
• For Individual #46, this was unclear. The ISP addresses this topic, but the medical
assessment did not.
• For Individual #11, this was unclear. The ISP did not address this topic, but there
were specific directions in the medical assessment.
• For Individual #48, there was nothing in either document.
11. If a medical restraint (for routine medical or dental care), the ISP did not include
treatments or strategies to minimize or eliminate the need for restraint.
• For Individual #11, the Monitoring Team did not find anything in the ISP or the BSP
addressing this topic.
12. On two of four occasions, within 30 minutes after initiation of restraint, a physician,
physician's assistant, nurse practitioner, or a Registered Nurse with training in
application and assessment of restraint, conducted and documented a face-to-face
examination of the resident, including a check for restraint-related injury.
• For Individual #46 and Individual #48, there were no entries in the nurses section of
Restraint Documentation and Initial Debriefing Report (RDIDR). The RDIDR is the
record of relevant data regarding the application of the restraint.
• For Individual #11, there was a nurse present (covid test and blood draw).
13. On one of four occasions, staff (who meet criteria) checked the resident as soon as
possible, but in exceptional circumstances where restraints exceed 15 minutes, no later
than 15 minutes from the start of the restraint, to review the application and consequence
of restraint. The Facility referred to the staff conducting these activities as observers. The
Monitoring Team reviewed the training records for the observers of the four restraints in
the review group. All had completed MANDT training. MANDT was described as the core
training staff received for restraint use.
• For Individual #46, the RDIDR showed a 15-minute check at 10:59 which was more
than 22 minutes from the start of the restraint.
• For Individual #11, there was a Nurse present (covid test and blood draw), but there
was no evidence that a 15-minute post restraint assessment occurred by either a
nurse or any other staff designated as the observer.
14. On zero of four opportunities, a registered nurse did not monitor and document vital signs
and mental status of a resident in restraints at least every 30 minutes from the start of the

60
In each instance of a medical restraint, the physician shall specify the
schedule and type of monitoring required).
• For Individual #46 the time vitals were taken (from the Chemical Restraint Report)
showed 1/2 hour and one hour. This was not adequate. The actual time should be
noted.
• For Individual #11, there was a nurse present to administer a covid test and a blood
draw. There was nothing in the documentation that showed the nurse did any follow-
up check (e.g., at 15 or 30 minutes).
• For Individual #48, there was no data recorded on the documentation and debriefing
report.
15. The RIDDR did not record data the level of supervision and to show that every resident in
physical or medical mechanical restraint shall receive opportunities to exercise restrained
limbs, to eat as near mealtimes as possible, to drink fluids, and to use a toilet or bed pan,
consistent with generally accepted professional standards of care; and shall be under
continuous one-to-one supervision.
16. Mechanical restraints were not used (other than as prescribed for necessary medical
care).
17. The restraint was not documented consistent with generally accepted professional
standards of care. Instances of missing, incomplete, or confusing documentation are noted
in comments in Indicators 1-16 above.
18. There were no occurrences of three instances of restraint in 30 days.
19. GRC staff responsible for applying restraints successfully completed competency-based
training on applicable BSPs and safety plans, approved verbal intervention and
redirection techniques, approved restraint techniques, and adequate supervision of any
resident in restraint.
The Monitoring Team reviewed the training records for staff applying restraint to
Individual #46 (three staff) and Individual #8 (four staff). All staff had MANDT training.
It was not evident that staff had received training in the areas of severe behavioral needs
or the co-occurrence of mental health needs and IDD. When asked about training
methods, staff reported that they had been trained by psychology assistants and QIDPs
who provided overviews of behavioral programs, skill-acquisition programs, and data
collection systems.
Trainings did not appear to be standardized (i.e., trainees were not receiving the same
information and developing a consistent set of competencies). Training rosters included
printed names and signatures of staff who had received training on individual behavior
plans. It was not clear what had been trained or what the training format was.
20. Training records were in place showing behavioral health staff received training by
certified trainers (MANDT). QAD reported that behavioral health staff had been involved
in selecting MANDT as an appropriate training curriculum for use at GRC.
21. On two of four occasions, the IDT reviewed the individualBSP and ensured that it
contained the objectively defined behavior that led to use of the restraint and alternative,
positive adaptive behaviors to be taught to the resident to replace the behavior that
initiates the use of restraint, as well as other programs, where possible, to reduce or
eliminate the use of such restraint.
• For Individual #46, the BSP presented important information well and was likely
understandable to DSPs.
• For Individual #11, the BSP did not address medical restraint. Ordinarily there is an
expectation of a separate individualized plan that discusses and sets out specific
protocols for medical restraint, that is, a Medical Restraint Plan. The Facility did not

61
do anything that could be construed as a medical restraint plan, although the
restraints for Individual #11 were viewed as a physical restraint (in the view of the
Monitoring Team this was an incorrect categorization).

62
Section D.ii: Seclusion (144-149)
Summary: The Facility reported it did not use seclusion and facility policy confirmed this. The Monitoring Team
did not observe the use of seclusion.
Substantial Compliance: Paragraph 144 Paragraph 149.
#
Indicator
Overall
Score
1
GRC shall eliminate, to the extent practicable, the use of seclusion. (par. 144)
SC
2
If seclusion was used,
• the resident posed an immediate and serious risk of harm to him/herself or others.
• only as a last resort and after a graduated range of less restrictive measures has been exhausted or
considered in a clinically justifiable manner.
• only for reasons other than as punishment, for convenience of staff, or in the absence of or as an
alternative to treatment; and only in accordance with applicable written policies, procedures, and
plans governing seclusion.
(par. 145)
NA
3
of, and precursors to, the behaviors leading to seclusion and a documented exhaustion of less restrictive
interventions. Seclusion shall not be implemented for any resident without approval by the Human Rights
Committee. (par. 146)
NA
4
•
•
•
(par. 147)
NA
5
•
•
•
(par. 148)
NA
6
No resident experiencing seclusion shall be denied access to typical items that a resident at GRC has access
to, absent a well-
access t
a plan is implemented. (par. 149)
NA
Comments:
1. GRC shall eliminate, to the extent practicable, the use of seclusion. The QAD reported seclusion was not
authorized or used at GRC. No evidence to the contrary was identified.
Indicators 2-6 are marked as not applicable.

63
Section D.iii: Other Restrictive Interventions (150-154)
Summary: No inappropriate restrictive techniques were identified for the three individuals in the restraint
review group. There may be issues related to this subject matter (other restrictive interventions) noted by the
Monitoring Team in other sections of this report.
Substantial Compliance: Paragraph 150, Paragraph 151, & Paragraph 152.
#
Indicator
Overall
Score
1
•
•
•
• GRC shall ensure that any restrictive interventions are used only consistent with current, generally
accepted professional standards of care.
(par. 150)
SC
2
In the event of an imminent safety risk, brief restrictive interventions may be used for up to 15 minutes and
may continue for up to 12 hours with the advance approval of the Administrator on Duty. (par. 151)
SC
100%
1/1
3
(par. 152)
SC
100%
4/4
4
After three instances of a restrictive intervention of a resident in 30 days (or an increasing trend in
restrictive intervention data over the course of three months of a resident), the IDT shall examine and refine
the resident's behavioral programming as set forth in Paragraph 140. (par. 153)
NA
5
(par. 154)
NC
Comments:
1. No other restrictive interventions were identified by the Monitoring Team, however, the
Monitoring Team reviewed four specific restraints involving three individuals.
2. In the event of an imminent safety risk, brief restrictive interventions may be used for up
to 15 minutes and may continue for up to 12 hours with the advance approval of the
Administrator on Duty. The 5-minute restraint of Individual #48 included, as required, an
advance approval from the AOD.
3. No other restrictive interventions were identified by the Monitoring Team.
4. There were no instances of three restrictive interventions being provided within 30 days.
5. Based on the document review, restrictive interventions were approved in an individual
Behavioral Health Professional, the Director of
From document review, there was no evidence that the requirements of this indicator
were met.

64
Section E: Engagement and Skill Acquisition (155-163)
Summary: Assessments were crucial prerequisites to skill-acquisition plans that had potential to support the
preferences. Assessments, while thorough, did not always offer recommendations for meaningful and functional
supports to improve behavior and teach functional skills. Assessments were also not informed by other
disciplines to ensure supports were comprehensive and integrated. Assessments did not offer supports for
future planning for individuals who planned to transition to the community. Assessments instead focused on the
needs of individuals as they pertained to their lives at the Center.
SAPs were in place for all individuals in the review group. SAPs had potential to teach meaningful and functional
skills. Many of the SAPs, however, were compliance objectives for individuals to complete household chores or to
engage in or tolerate nonpreferred activities. SAPs were not reflective of assessment results and progress could
not be confirmed because SAP data were not reliable.
While engagement was still a challenge due to low staffing levels, it was good to see that more individuals were
engaged in meaningful activities as compared to the previous Monitoring Team visit. It was also good to see that
there was a monitoring procedure in place to assess engagement at random times. The procedure was mostly
subjective, and it was not clear how staff had been trained to assess and determine if activities individuals
engaged in met criterion. Nevertheless, it was good to see that regular observations were occurring and that
administrators were involved in the process.
It was positive to see that strengths and deficits in a variety of areas had been evaluated by respective
disciplines. It was not evident that evaluation results and data had been shared with the GRC Quality
Management team or that data were used to assist the Quality Management team to identify and address trends.
For individuals who exhibited behaviors that were barriers to community transition, IDTs did not develop plans
or strategies to minimize or overcome the barriers, and there was no evidence of a formal community
integration plan to minimize and/or overcome behavioral barriers. Staff training was an area that needed
attention as it was not evident that trainings were standardized and that trainees were receiving consistent
information and developing a consistent set of competencies.
Partial Compliance: Paragraph 156, Paragraph 157, & Paragraph 159
#
Indicator
Overall
Score
1
An individual receives assessments in time for the annual ISP, or when based on change of healthcare status,
as appropriate, an assessment is completed in accordance with the needs. (par. 155)
NC
0%
0/7
2
Individual receives a quality assessment including the following components:
i. Discussion of pertinent history
ii. Preferences and strengths
iii. Pertinent health risks
iv. Discussion of medications
v. Functional description
vi. Use and rationale for supportive equipment.
vii. Comparative analysis to previous assessments
viii. Effectiveness of supports
ix. Recommendations for services
(par. 156)
PC
57%
12/21
3
There is evidence that the measurable strategies and action plans included in the ISPs/ISPAs related to Hab
supports are implemented. (par. 156)
SC
100%
2/2
4
Assistive/adaptive equipment identified in the PNMP is clean. (par. 156)
SC
100%
5/5

65
5
Assistive/adaptive equipment identified in the PNMP is in proper working condition. (par. 156)
SC
100%
5/5
6
Assistive/adaptive equipment identified in the PNMP appears to be the proper fit for the
individual. (par. 156)
SC
100%
5/5
7
The individual has skill acquisition plans. (par. 157,159)
SC
100%
7/7
8
The SAPs are measurable. (par. 157,159)
SC
100%
7/7
9
The SAPs were based on assessment results. (par. 157,159)
NC
0%
0/7
10
SAPs are practical, functional, and meaningful. (par. 157,159)
NC
0%
0/7
11
Reliable and valid data are available that report/summarize the status and progress. (par.
157,161)
NC
0%
0/7
12
The individual is progressing on his/her SAP. (par. 159)
NC
0%
0/7
13
If the goal/objective was met, a new or updated goal/objective was introduced. (par. 159)
NC
0%
0/7
14
If the individual was not making progress, actions were taken. (par. 159)
NC
0%
0/7
15
The individual is meaningfully engaged in residential and treatment sites (par. 157)
PC
67%
4/6
16
The facility regularly measures engagement in all (par. 157)
NC
0%
0/7
17
The day and treatment sites of the individual have goal engagement level scores. (par. 157)
NC
0%
0/6
18
The goal levels of engagement in the day and treatment sites are achieved. (par. 157)
NC
0%
0/6
19
For the individual, goal frequencies of community recreational activities are (a) established and (b)
achieved. (par. 157)
NC
0%
0/7
20
For the individual, goal frequencies of SAP training in the community are (a) established and (b) achieved.
(par. 157)
NC
0%
0/7
21
GRC shall conduct annual assessments, with quarterly reviews, of preferences, strengths, skills,
needs, and barriers to community integration, in the areas of living, working, and engaging in leisure
activities. For residents with behavioral barriers to community integration, the Behavioral Health
Professional shall assist with developing a Community Integration Plan to minimize the existence of
behavioral barriers. (par. 158)
NC
0%
0/4
22
GRC shall use the information gained from the assessment and review process to develop, integrate, and
revise programs of training, education, and skill acquisition to address each needs. (par. 159)
NC
23
The State shall ensure that all GRC direct care staff have successfully completed competency-based training
on the implementation of the habilitation programs, including training, education, and skill acquisition
NC

66
programs, of the residents they work with, annually and every time a new habilitation program is
implemented. (par. 160)
24
quality management system shall include processes to ensure that the habilitation, training,
education, and skill acquisition programs provided to GRC residents are consistent with current, generally
accepted professional standards and implemented in an appropriate manner. (par. 162)
NC
25
Whenever problems are identified under the processes set forth in Paragraphs 161-162, GRC shall develop
and implement plans to remediate the problems. (par. 163)
NC
Comments:
1. For the individuals in the review group, discipline assessments were required to be
developed and submitted within 10 days prior to the ISP meeting. This portion of the
indicator was not met for any of the individuals in the review group because relevant
assessments had not been submitted on time. Findings included:
• Individual #29: the OT assessment was last updated 10/26/21 and the PT assessment
was completed on the day of the ISP meeting, 9/22/22. The nutrition assessment was
submitted late.
• Individual #30: the SLP report and OT assessment dated 2/27/23 was not completed
five days prior to the ISP meeting on 3/1/23. The PT assessment was not completed
until April 2023. The psychiatry, nursing, and vocational assessments were submitted
after the deadline.
• Individual #31: the OT assessment was dated 11/16/22 and the PT assessment was
dated 11/18/22. Both were not completed five days prior to the 11/18/22 ISP
meeting. The behavioral, psychiatry, and nutrition assessments were submitted late.
• Individual #39: The nursing assessment was submitted after the deadline.
• Individual #42: The OT, SLP, and PT assessments were not completed at least five
days prior to the ISP meeting on 2/7/23. The psychiatry, pharmacy, nutrition, and
day/vocational assessments were submitted late.
• Individual #78: the PT assessment dated 8/17/23 was not completed until after the
ISP meeting on 8/15/22. The medical, nursing, behavioral, psychiatry, and nutrition
assessments were submitted after the deadline.
• Individual #79: the OT assessment was completed on 10/4/2 and the PT assessment
on 10/3/22, not completed five days prior to the ISP meeting on 10/3/22. The
nursing, nutrition, and psychiatry assessments were submitted after the deadline.
It was good to see that assessments were consistently updated following a change in
assessment recommendations were reviewed every 90 days as required by the Consent
Decree.
2. Assessments generally focused on a particular life area and did not integrate much, if any,
information from other disciplines. Assessments also tended to focus on the
immediate needs at GRC and not the supports the individual might need following a
transition to the community. For example, vocational assessments for four individuals
offered the same boilerplate set of recommendations for future planning:
• Continually monitor assessment results, data, and anecdotal feedback from support
professionals to guide the development of behavioral supports and the acquisition of
skills that will enable this individual to be successful in community-based settings
and are consistent with standards in the field of applied behavior analysis.
• Continually work with the support team, guardian, and psychiatrist to identify
whether the benefits of psychotropic medication outweigh the risks and, if so, the
most effective medications and dosages.
• Continue to explore community-based residences.

67
• -based providers
that the Glenwood Resource Center behavioral services are available to help them
make a smooth transition into a less restrictive environment.
• Also, further behavioral supports are offered through the Money Follows the Person
-
TABS) program for individuals moving from the Resource Center into a community-
based residential home.
Although preference assessments were conducted, supports and SAPs were not based on
the results. Supports and SAPs, therefore, were not based on the preferences of the
individuals. It was not evident that assessments were informed by IDT review or
discussion, or that the IDTs had discussed how the assessment results impacted the
functional performance. Assessments generally did not present or involve an
analysis of clinical data to support treatment efficacy, and data were not used to assess an
Regarding habilitative supports (OT, PT, and SLP combined), 48 percent of the
assessments contained the necessary components to meet the needs of the individual.
Few assessments included recommendations for direct or indirect supports and/or SAPs.
Pervasive issues noted across all assessments included a lack of a clear focus on what was
needed to be successful in the community. Also lacking were recommendations developed
to address identified areas of deficit, and a discussion about the effectiveness of the
supports provided. Findings included:
• For Individual #29, two of the three assessments were considered comprehensive.
The SLP report stated that the communication plan was reviewed and revised, but did
not state what was revised. Also, the SLP noted that the ADL objectives remained in
place and were the most appropriate AAC, but then did not discuss possible
expansion.
• For Individual #30, one of three assessments were considered comprehensive. The
SLP report noted decreased receptive language and support needed for more complex
information, but offered no clear justification as to why they would not benefit from
direct or indirect services. The OT assessment identified many issues within the
assessment, but stated that ambition and desire were the primary barriers without
offering collaboration with BHS to address and possibly improve.
• For Individual #31, two of the three assessments were considered comprehensive.
The SLP report stated that expressive communication had improved due to him
learning new words, but then did not state what these words were and if they were
used appropriately. There was no discussion on how to continue to improve the
expansion of his vocabulary. It stated that he was seen by ST during the year to
develop scripts, but did not offer any additional information on what these were.
• For Individual #78, none of the assessments were considered comprehensive. The
SLP report contained some of the needed components. Missing from the assessment
was a comparative analysis of current versus previous status outside of the staff
interview, expansion of the use of object cues (outside of intake), and clear
recommendations on what was needed to enjoy community success. The OT
assessment lacked clear discussion of the effectiveness of provided OT supports and
equipment. The PT assessment did not identify what, if any, supports would be
needed in the therapy environment to mitigate risks or issues requiring PT supports.
• For Individual #79, one of three assessments were considered comprehensive. The
OT assessment lacked discussion of the effectiveness of supports. For example,
increased tone to the trapezius was noted. Cortisone shots were identified as being
provided on two occasions, but there was no discussion as to effectiveness. The PT
assessment lacked effectiveness of PT related supports identified as part of the PNMP.

68
3. Three of the individuals had skill-development programs that were based on habilitative
support recommendations. The SAPs for all three individuals were implemented. Findings
included:
•
cards as a form of AAC to alert others to his readiness to participate in activities
throughout the day. The support was developed into an SAP to promote
communication.
• During an IDT meeting held on 3/8/23, the team decided to develop a plan to teach
Individual #42 to use an AAC device to express his desire to be left alone. The plan
was implemented, and data was being collected.
• to address her unsteady gait and
communication deficits. Corresponding IIPs had been implemented that taught her to
use an AAC device to request assistance and to request a delay after receiving a
prompt to complete a nonpreferred task. There was also an IIP that prompted her to
slow down while ambulating. All three IIPs were implemented, and data were being
collected.
4.
PNMP was clean.
5. For five of five individuals, as
PNMP was in proper working condition.
6.
PNMP looked to be the proper fit for the individual.
7. SAPs were developed and implemented for seven of seven individuals.
8. For all seven individuals, SAPs and teaching strategies used observable and measurable
terms to describe what the individual was expected to do.
9. Most SAPs were not reflective of assessment results and generally did not teach functional
or meaningful skills. Implementation Programs (IIPs) did not generally teach skills that
promoted growth, development, integration, and independence. Some IIPs were
behavioral expectations that an individual did not engage in more than a designated
number of behavioral incidents per month. Other IIPs were compliance objectives that
prompted individuals to complete tasks and respond to demands instead of teaching
functional skills. For example:
• Individual #30 had an IIP for cleaning his room. After prompting from staff, he was
expected to place his soiled clothing into a hamper. If he refused, then the staff
reminded him about the importance of being responsible and keeping his room clean.
It was clear that Individual #30 already possessed the skills necessary to complete
the task. The IIP served to prompt his compliance with the task.
• Individual #30 had an IIP for exercise. Staff prompted and encouraged him to walk or
access the wellness center. The IIP did not include teaching steps for exercise. The
individual appeared to already possess the necessary skills. The IIP served to prompt
his compliance with the task.
• Individual #39 had an IIP for keeping his eyeglasses on. The teaching plan listed steps
for staff to apply his glasses once he was assisted to his wheelchair and to remove
them once he was positioned in bed. Individual #39 was not actively involved in the
program and the steps did not lead to the development of functional skills.
Implementation of IIPs for three individuals were observed by the Monitoring Team
during the review week. It was positive that the SAPs were based on recommendations
found in their OT/PT and communication assessments.

69
• Individual #30 had an IIP that taught him to complete a budgeting sheet and choose
items he wanted to purchase with his weekly paycheck. The Monitoring Team
observed the QIDP who used a Program Implementation and Monitoring form to
follow along and provide feedback as the direct support staff supported the individual
to complete the budgeting sheet. It was also good to see Individual #30 learning to
budget his money and make choices and develop a meaningful skill that he would
likely need after transitioning to the community.
• Individual #78 was not able to communicate verbally. Overall, his expressive
communication skills were limited. He had an IIP that prompted him to choose a
leisure activity by looking at it. During the observation, staff stood next to the
ing up a radio and prompted the individual to make
a choice between the two leisure activities by looking at the desired item. When he
did not respond, the staff provided a second and third prompt. When the individual
still did not respond, the staff returned the radio to the shelf and walked away. It was
not clear that Individual #78 was adequately supported to learn to choose desired
items given his communication deficits. It was also not clear that staff had been
adequately supported to teach the skill.
• Individual #79 had one IIP that taught her to use a communication device to request
help, and another IIP that taught her to use the same communication device to
request a break or delay after a demand had been placed on her. It was good to see
that she was supported to communicate her preferences.
10. See indicator #9 above.
11. The Monitoring Team was unable to find that the Center assessed the quality of skill-
acquisition programs or of the collection of reliable individual performance data.
12.
• Individual #30 was learning to describe appropriate social responses. He was asked
to describe how to appropriately greet females, how he needs to keep his hands to
himself, and examples of appropriate things he can say to staff and peers. Monthly
data documented if he met criterion overall. Data were not analyzed and did not show
his progress on each step.
• Individual #31 was learning to put his clean clothes away in the dresser or closet. The
steps included opening the dresser drawer, taking his clothes out of the laundry
basket, putting his clothes in drawers, or hanging clothes in the closet, and closing the
drawer or closet. Monthly data documented whether he successfully completed the
overall task with no more than a verbal prompt. Data were not analyzed to show
which areas of the task where he was successful or where he needed more support.
13. Indicators #13 and #14 were not met because data did not accurately demonstrate the
-acquisition objectives. (Also see
indicator 12 above.)
14. See indicator #13 above.
15. During the review week, it was good to see that several of the individuals had attended the
state fair and other community venues for recreational outings. It was also good to see an
increase in the number of individuals who accessed day services in building #102 since
the last monitoring review. Building #102 continued to offer a wide array of options for
meaningful engagement, learning, and skill-development.

70
During three separate visits to the program, the Monitoring Team observed six individuals
in attendance each time. Although the program could have accommodated more
individuals, the Center continued to struggle with staffing shortages, and staff from the
homes were often unable to accompany and support individuals at the program. The
Monitoring Team observed some individuals who were actively engaged in meaningful
activities while others were not. During one visit, the Monitoring Team observed four
individuals who were engaged in a painting activity. They were actively participating and
appeared to enjoy the activity. Another group of individuals, who had significant
expressive language deficits, sat on a sofa facing a television. It was not clear that they
were actively engaged in watching the television. Regarding individuals in the review
group, visits to their homes, jobs, and day programs showed varying levels of engagement.
Findings included:
• Individual #30: was attending the state fair during one visit to his home. During a
second visit, he was asleep in his bedroom. During a third visit to the home, the
Monitoring Team observed him completing an IIP for budgeting his money.
• Individual #31: During one visit to his home, he was seated in his bedroom and not
engaged in an activity. During a second visit to his home, he was out walking the
grounds with staff. During a third visit, he was attending work.
• Individual #39: During one visit to his home, he was seated in front of a television and
did not appear to be engaged.
• Individual #42: During one visit to his home, he was on an outing with staff in the
community. During a visit to the day program, he was seated at a table with peers and
was manipulating a peg board.
• Individual #78: During two visits to his home, he was seated in a recliner in his room
and did not appear to be engaged. During a third visit, he was in the community at a
dental appointment.
• Individual #79: During one visit to the home, she was seated at the kitchen table and
working to complete a puzzle. During a second visit to the home, the Monitoring Team
observed her completing two IIPs. During a visit to her job, she was observed
shredding paper with staff support.
16. GRC had an Observation Procedure that required weekly assessments to ensure
individuals were engaged. According to the policy, the Residential Treatment Specialist,
QIDP and Treatment Program Administrator were responsible for tracking the date,
location, number of individuals present, and the activity individuals were engaged in. The
observation form also listed expectations for engagement and staff support, along with a
place for the observer to respond positively or negatively indicating whether the
expectations were met. Even so, individuals were being assessed for preferred leisure
activities and offered opportunities to engage in those activities.
Although the definition of engagement was subjective, and it was not clear how staff had
been trained to assess and determine if activities individuals engaged in enhanced their
physical, emotional, social, intellectual, and vocational development as indicated on the
form, it was still good to see that regular observations were occurring and that
administrators were involved in the process.
17. It was not evident that GRC had established goal levels for engagement or that evaluators
had been trained to recognize and respond to low levels of engagement and active
treatment.
18. See indicator #17.

71
19. Habilitation, vocational, and skill-acquisition programs did not tend to focus on the
development of functional skills or promote personal growth or independence.
Individuals were not supported with skill development programs to teach the skills
necessary to work successfully in the community. Programs did not teach skills to prepare
individuals to transition to the community. Skill acquisition programs were implemented
in the homes and individuals were not offered opportunities to learn and practice skills in
community settings. This lack of carry-over and immersion into the community impacts
skill development and may pose as an additional barrier to transitioning to the
community.
20. See indicator #19.
21. Strengths and deficits in the areas of self-help, domestics, eating, hygiene, communication,
and social skills, as well as barriers to community integration were reviewed annually at
t were barriers
to community transition, IDTs did not develop plans or strategies to minimize or
overcome the barriers, and there was no evidence of a formal community integration plan
to minimize and/or overcome behavioral barriers as required by the Consent Decree.
Individual #30 engaged in inappropriate sexualized behaviors during catheter irrigation
procedures. The behavior was a barrier to his community transition. Although he was
redirected whenever he engaged in the behavior and he was learning to describe
appropriate social interactions, the IDT had not discussed ways to overcome the barrier
and proceed with a plan to transition him to the community.
22. It was positive to see that supports recommended in communication and OT/PT
assessments had been implemented, and training and skill-acquisition programs had been
developed based on the recommendations. For example:
• Individual #30: The communication assessment recommended that he engage in
activities that involved reading, writing, and comprehension. An IIP was developed
that taught him to complete a budgeting worksheet while reviewing store
advertisements to determine how much money would need to make purchases each
week.
• Individual #78: The communication assessment recommended the use of a Go Talk
4+ to make requests and express other needs. An IIP was developed that taught her to
use the device to request assistance and to request a delay after a demand was
presented.
• Individual #78: The PT assessment recommended a gait belt ambulation strategy. An
IIP was developed to encourage safe walking using the recommended strategy.
23. When asked about training methods, staff reported that they had received on-the-spot
training by psychology assistants and QIDPs who provided overviews of behavioral
programs, skill-acquisition programs, and data collection systems. It was not evident that
trainings were standardized and that trainees were receiving the same information and
developing a consistent set of competencies. Training rosters included printed names and
signatures of staff who had received training. It was not clear what had been trained or
what the training format was.
24. GRC Quality Management team did not participate in the review and analysis of behavioral
and skill-acquisition data, or regarding whether data were used to assist the team to
identify and address trends. According to GRC policy, quality management involved
routine collection and analysis of performance data to ensure data were reliable and that
procedures were implemented with integrity. Without proper analysis of data and review
of trends, the GRC Quality Management program could not effectively remediate problems
and initiate quality improvement processes.
25. See indicator #23
72

73
Section F: Record Keeping (164-166)
Summary: Records were not consistently updated when a change in event occurred or when a medical or
behavioral plan of care was implemented. Additionally, SAPs were often not clearly documented within the
record. It was noted that any changes to the record or plan of care did have evidence of the individual making
such changes and the reason for the changes being made. Time and date were consistently noted in the record.
This practice was supported by a policy titled Late entry, Addendum, and Amendment of Documentation that
was dated September 2022.
Substantial Compliance: Paragraph 166
Partial Compliance: Paragraph 164, and Paragraph 165
#
Indicator
Overall
Score
1
GRC will maintain complete and accurate records. (par. 164)
PC
2
GRC shall ensure pertinent information about assessment, treatment, and diagnosis, including information
integrated electronic health record. (par. 165)
PC
3
GRC shall maintain and produce records in a manner that clearly demonstrates:
a. The time and date when a particular record or entry was created or entered.
b. The identity and job title of the person creating or entering the record or entry.
c. The time and date to which the record or entry pertains.
d. Whether the record or entry was created or entered timely according to State policy; and
e. If a record or entry is subsequently changed:
-The time and date the change is made.
- The identity and job title of the person making the change.
-The reason for the change.
-The nature of the change; and
-A version of the record or entry as it existed before it was changed.
(par. 166)
SC
Comments:
1. ISPs, MIRs, and transition plans were inconsistent in the amount and quality of
information they included. Multiple assessments were not signed and/or dated. Other
areas that were lacking in clearly documenting clinical findings, assessments, or plans of
care included nursing.
There were no periodic (90 day) interval medical reviews. Except for the annual exam,
there was no methodical review of events, labs, or consults on a regular basis.
The annual and quarterly nursing assessments did not meet standards as the primary
documentation entitled Nursing Report was missing components.
2. See indicator 1 above.
3. Any records that were created or modified contained evidence of the individual who was
making such revisions to the record. Addendums were used when paper was involved,
and signature was stamped when electronic records were utilized.

74
Section G. Incident Management (167-176)
Summary: In the six-month period February 2023 through July 2023, the Facility reported it conducted 68 Type
1 Investigations (Type 1 Investigations include ANE and Serious Injuries). Seventeen of these were for
Allegations of abuse, seven were for Allegations of Neglect, and three were for serious Injuries.
During this same time the Facility reported it had conducted 76 Type 2 Investigations. Type 2 Investigations are
Investigations of Injuries of unknown origin (not witnessed or self-reported by Individuals considered to be
reliable self-reporters). Staffing may impact overall the ability to witness incidents, but this could not be clearly
linked at this time in causative manner.
GRC policies were generally in order, but were described as undergoing continual review and revision. They did
not cover all components of the Consent Decree. They cannot be considered final at this time and, further, there
were some implementation issues as noted elsewhere in this report that should be addressed in future revisions.
GRC procedures and administrative practices associated with incident reporting, investigating, post
investigation review, and administrative follow-up were generally in order, however, several specific areas were
noted as needing immediate attention. These are described in the following comments.
Posters displayed on recognizing ANE and how to report was a problem. Monitoring Team members while in the
t really posters, but a written statement requiring a
lot of reading, with the 800 number not displayed prominently.
Facility practices for alleged perpetrator (AP) removal after an allegation was problematic. Facility practice, as
reported, was to assess the circumstances associated with each allegation and decide a course of action
regarding AP removal, reassignment, or something else. It was reported that usually the AP was not 100%
removed from contact with individuals, pending the outcome of the investigation. And, in many circumstances
the AP as allowed to continue to work in the home and even with the alleged victim named in the allegation. This
practice leaves room for too much discretion, which might not always be applied in a manner that maximizes
client protection and can potentially place an alleged victim, and other individuals in the home, or other homes
where the AP is assigned to work while the investigation is ongoing, at risk.
Procedures for anonymous reporting of ANE were problematic. It was reported that people can report
anonymously to the Department of Inspections and Appeals (DIA), which is the part of the State government
responsible for the Medicaid rules governing facilities like GRC. GRC reported that anonymous reporting to DIA
was permissible, but not necessarily encouraged.
Type 1 investigations were, for the most part, well done, however only two of the nine were completed within
the required 10 days. The investigations were thorough, with a well-organized report, and good documentation
with one consistent exception as follows. The Type 1 investigation report includes a data item: Immediate
Protections Implemented. The response on all nine investigation reports was supervisor and nurse notified. This
iate
protections.
The timeliness of investigations completion is an issue that needs to be addressed immediately. Some non-timely
investigations may be easy to explain (e.g., having to wait until DIA completed their investigation). For the nine
investigations, seven were not completed within 10 days. There was no explanation (or evidence) of what may
have represented the extraordinary circumstances for a delay in completion. The Facility should consider
developing a form that documents each request for an extension that clearly shows the extraordinary
circumstances, and approval by the appropriate administrator.

75
Administrative review of investigations was very thorough (with the obvious exception related to 10-day
completion).
Partial Compliance: Paragraph 167, Paragraph 168, & Paragraph 169.
#
Indicator
Overall
Score
1
GRC shall implement and maintain policies, procedures and practices that include a commitment that GRC
shall Not tolerate abuse or Neglect of Individuals and that staff are required to report abuse or Neglect of
Individuals. (par. 167)
PC
2
GRC policy Includes all the components of 168 a-j. (par. 168)
PC
3
GRC policy Includes all the Components of 169 a-k. (par. 169)
PC
4
For deaths, abuse, Neglect, and Exploitation: report was made to the Superintendent (or that
designee) and such other officials and agencies as warranted, consistent with Iowa law. (par. 168a)
SC
5
For serious injuries and other serious Incidents, a report should be made to the Superintendent (or that
designee). Staff shall report these and all other Unusual Incidents, using standardized reporting.
(par. 168b)
SC
6
After the allegation or injury, the Center took immediate and appropriate action to protect the residents
involved, including removing alleged perpetrators, if any, from direct contact with residents. (par. 168b)
NC
7
Staff received competency-based training on recognizing and reporting potential signs and symptoms of
abuse, neglect, and exploitation. (par. 168c)
SC
8
All staff persons who are mandatory reporters of abuse or neglect shall sign a statement that shall be kept
at Glenwood evidencing their recognition of their reporting obligations. (par. 168d)
SC
9
Glenwood shall take appropriate personnel action in response to any mandatory failure to report
abuse or neglect. (par 168d)
NC
10
The facility had taken steps to educate the Individual and primary correspondent (e.g., guardian) with
respect to abuse/Neglect identifications and reporting.
1. Material provided to Individual and PC.
2. ISP review and discussion occurred.
3. 3. responses during Interview
4 Poster present in living area
(par, 168e, 168f)
NC
11
GRC had mechanisms for residents, visitors, and other persons to report anonymously allegations of abuse,
neglect, exploitation, other possible violations of rights, or other unusual incidents. (par. 168g)
NC
12
GRC had procedures for referring, as appropriate, allegations of abuse and/or Neglect to law enforcement.
(par. 168h)
SC
13
If the Individual, any staff member, family member, or visitor was subject to or expressed concerns regarding
retaliation, the facility took appropriate administrative action. (par. 168i)
NC
14
The facility conducted audit activity to ensure that all significant injuries for this Individual were reported for
Investigation. (par. 168j)
NC
15
The Investigation was conducted by a qualified investigator. (par. 169a)
SC
100%
9/9
16
Facility staff cooperated with the Investigation. (par. 169b, 169c)
SC
17
The conclusions drawn from the investigation were not compromised due to improper safeguarding of
evidence. (par. 169d)
SC
18
The investigation commenced within 24 hours of being reported. (par. 169e)
SC
19
The investigation was completed within 10 calendar days of when the incident was reported (unless a
written extension documenting extraordinary circumstances was approved in writing). (par. 169f)
NC
2/9
22%
20
HHS Central Office shall track and trend the number of extensions requested and take appropriate remedial
action. (par. 169f)
NC
0/9
0%
21
Required specific elements for the conduct of a complete and thorough investigation were present. A
standardized format was utilized that set forth explicitly:
SC
8/9

76
(par. 169g)
89%
22
There was evidence that the investigation supervisor conducted a review of the investigation report to
determine whether (1) the investigation was thorough and complete and (2) the report was accurate,
complete, and coherent. (par. 169h)
NC
2/9
22%
23
The supervisor review indicator above was also applied to any Investigation that was not deemed a serious
Incident. (par. 169j)
SC
9/9
100%
24
The Investigation included recommendations for corrective action that were related to the findings and
addressed any concerns noted in the case. (par. 169j)
SC
8/9
89%
25
If the investigation recommended disciplinary actions or other employee related actions, they occurred and
they were taken timely. (par. 169j)
SC
8/9
89%
26
If the investigation recommended programmatic and other actions, they occurred and they occurred timely.
(par. 169j)
SC
9/9
100%
27
The format of the completed investigation was maintained in a manner that permits investigators and other
appropriate personnel to easily access every investigation involving a particular staff member or Individual.
(par. 169k)
SC
9/9
100%
28
If the incident met criteria for sentinel event: GRC conducted an effective root cause analysis of the Incident.
•
•
(par. 170)
NA
29
If the investigation was deemed a preliminary assessment of an allegation, the following was in place: re:
chronic callers.
• Within the previous six months, the resident made four or more allegations of abuse, Neglect, or
exploitation, all of which were determined to be unfounded.
•
unfounded and was made within 30 days of such a previous allegation.
• An initial assessment shows No evidence (other than the resid
occurred.
• The resident has a BSP with components listed in the interpretive guidelines for this indicator.
(par. 171)
NA
30
If the investigation was deemed a preliminary assessment of an allegation, the following was in place:
Alleged perpetrator(s) were removed from contact with residents.
• until the full investigation is completed.
OR
Central Office determines that the risk to residents from contact with the alleged perpetrator(s) on the
been sufficiently minimized, at which time the Superintendent may allow the
alleged perpetrator(s) to have continued on-campus client contact, but only with ongoing supervision
perpetrator(s) by a supervisor.
(par, 172)
NA

77
31
alleged perpetrator(s) did not have off-grounds contact with
residents. (par. 173)
NA
32
If the Investigation was deemed a preliminary assessment of an allegation, the preliminary assessment:
• Did Not conflict or interfere with the concurrent full investigation conducted by GRC or State
Investigators.
• Focused exclusively on determining the appropriate action to take regarding the work duty
assignment of the alleged perpetrator(s).
• Where the preliminary assessment recommends allowing the alleged perpetrator to work in a resident
contact position, provided the rationale for doing so; and
• Required the prior review and approval of the Superintendent or the Administrator on Duty.
(par. 174)
NA
33
For all categories of unusual incidents and investigations, the facility had a system that allowed tracking and
trending by:
a. Type of incident.
b. Staff alleged to have caused the incident.
c. individuals directly involved.
d. Location of incident.
e. Date and time of Incident.
f. Cause(s) of Incident; and
g. Outcome of Investigation.
(par. 175)
NC
34
Staff assigned to work with the Individual passed criminal background checks. (par. 176)
NC
Comments:
1. The QAD reported that many policies and procedures were under review and were being
revised as needed and updated. The current policy included the requirements of this
provision. The QAD agreed that policy updates were a work in progress.
2. Refer to the above comment. Additionally, the Facility did not maintain a crosswalk
between Consent Decree requirements and GRC policy provisions. Without this, it will be
difficult to ensure its policies include all components of 168 a-k.
3. Refer to the above comment.
4. The Facility Quality Assurance Director (QAD) said that State law required reporting
within 24 hours, thus, the GRC two-hour policy complied with Iowa law. Standard practice
in most states is one hour and one hour notification is generally viewed as necessary to
demonstrate commitment to a zero-tolerance policy (which GRC had). GRC should
consider moving to a one-hour reporting requirement to demonstrate commitment to its
zero-tolerance policy.
5. The Monitoring Team verified there was a standardized process for reporting.
6. Regarding alleged perpetrators, the QAD described a process that assessed the
circumstances associated with each allegation that resulted in a determination regarding
AP removal or some other course of action. The QAD reported that usually the AP was not
100% removed from contact with individuals pending the outcome of the investigation.
And, in many circumstances, the AP may continue to work in the home and even with the
alleged victim named in the allegation. This practice leaves room for considerable
discretion that might not always result in decisions in the best interest of client
protection. The Monitoring Team recommends this process be revised with clear written
guidelines that direct decision-making in this regard.
7. Facility reported the ANE component for staff training had been updated and staff trained
in June 2023. Training transcripts reviewed by the Monitoring Team confirmed this.
However, the Full Compliance rating only validates that the training occurred, not that
staff were necessarily following the substantive content of the training. That that point,
the Facility reported five instances of failure to report during this review period. Refer to
Indicator 9 below.

78
8. The QAD reported this practice was just instituted a week or so prior to this review. This
was confirmed by document review by the Monitoring Team. The Monitoring Team
expectation was that these signed statements will be updated annually.
9. The QAD reported four instances where allegations of abuse were not reported and one
instance where an allegation of neglect was not reported at all. It is commendable that the
Facility had a process that made such discoveries, but it was alarming that there were
many instances in a short period of time (2/4/23 to 7/17/23) for a Facility with less than
100 individuals with 71 at the time of the review. In each case, the employee who did not
report was retrained. Failure to report is a serious offense and more significant personnel
action was needed to deter future instances of not reporting. In other words, appropriate
personnel action was not taken.
10. The Monitoring Team found that the Facility had not provided ANE information to
individuals and guardians (Individual #39 and Individual #58). No relevant information
regarding ANE was included in ISPs and there was no evidence of any material being
provided to individuals or their guardian (Individual #96). Monitoring Team members
while on the homes often found it difficult to locate posters, which really posters,
but a written statement (a lot of reading) with the 800 number (but not displayed
prominently). This would not likely be useful to individuals, guardians, and family
members. Individuals were not interviewed.
11. As described by the QAD, reporting to the GRC Facility Director/designee was encouraged,
but direct reporting to DIA (State Regulatory) was not. This was also true for staff. Anyone
can report anonymously to DIA, but DIA may or may not investigate. If an allegation is
reported directly to DIA (and not to the Facility Director/designee), GRC is unaware of
this allegation unless DIA investigates. GRC, therefore, cannot initiate client protection
measures including removal of an identified alleged perpetrator. If DIA does investigate it
is not usually done immediately. GRC will only learn of the substance of the allegation if
they can figure out from surveyor activity what the investigation is about. If there is a
regulatory citation, then GRC will get all the details. If there is no citation, GRC gets
nothing official and is left to guess and hypothesize as to the substance of the allegation.
This is a significant issue that should be addressed at the State Office level.
12. The QAD described the process and the Monitoring Team saw evidence of it in one of the
investigations reviewed.
13. The QAD was unaware of retaliation ever being an issue at GRC. The Facility had not taken
any specific proactive measures to address staff fear of retaliation for reporting ANE
and/or cooperating in an investigation. This was concerning as this was inconsistent with
previous DOJ findings and the QAD was employed at the time of these issues so being
also did not seem consistent. The Monitoring Team did not see any reference
to retaliation in any of the nine investigations reviewed, but should ensure that the proper
education is provided to staff and opportunities for reminders (such as posters with
contact information and directions) provided.
14. The QAD reported it conducted no specific activity or procedures that would represent
audit activity.

79
•
•
•
•
20. The QAD was unaware if State Office tracked and trended the number of extensions
requested and took appropriate remedial action. The assumption is that if Central Office
was engaged in this activity, the QAD would likely be aware. A tracking log was requested
but not provided to validate the evidence of tracking.
•

80
i. Type of incident
ii. Staff alleged to have caused the incident.
iii. individuals directly involved.
iv. Location of incident.
v. Date and time of Incident.
vi. Cause(s) of Incident; and
vii. Outcome of Investigation.
34. Data regarding staff assigned to work with the Individual having passed a criminal background check was
incomplete and compliance could not be determined.

81
Section H. Individual Support Planning, Discharge Planning, and Transition from Resource
Center (177-178)
Summary: GRC continued to develop their process for ISP development, discharge planning, and transition. The
facility was committed to ensuring that transitions were appropriate and went smoothly, however, there were
still issues with identifying all needed supports and ensuring that all supports were in place prior to discharge.
QIDPs had recently completed training on person-centered planning practices and were starting to implement
some of the procedures. It was good to see that individuals were included in all planning meetings and IDTs
attempted to determine their preferences, however, limited exposure to living and day options in the community
was a barrier to individuals making an informed choice about where they wanted to live.
Partial Compliance: Paragraph 177, Paragraph 178
#
Indicator
Overall
Score
1
The State shall develop and implement individual support planning, discharge planning, and transition
processes at Glenwood. (par 177)
PC
2
The individual participated in their individual support planning, discharge planning, and transition planning
to the maximum extent practicable, unless the individual chose not to participate. (par. 178,49)
SC
86%
6/7
3
Individuals were supported to meaningfully participate in their annual ISP meeting. (par. 178)
SC
86%
6/7
Comments:
1. The State had developed and implemented individual support planning, discharge
planning, and transition processes. While these processes were documented for everyone,
the thoroughness in planning and documentation varied among individuals as did the
implementation. Most individuals lacked measurable action plans to ensure that
processes were in place and monitored throughout the transition process. ISPs/transition
plans should include measurable action plans to address identified barriers and supports
needed to live successfully in the community.
2. Six of the seven individuals participated in their annual ISP meeting. Discharge planning
and transition were discussed at each annual meeting. Individuals were encouraged to
attend and participate in all meetings including annual ISP meetings and monthly review
of service meetings.
3. As noted, all individuals were encouraged to attend their meetings, and some had
rudimentary communication strategies to facilitate communication and their ability to
make choices. This was a good first step to meaningful participation, however, many
lacked opportunities for exposure to new things so they could make informed choices.
ISPs did not document how individuals participated in their meetings or whether
accommodations were offered to ensure optimal input into discussions/decision making.
As noted, beyond initial steps, the extent of participation could not be evaluated for all
individuals. IDTs should document specific support offered to enhance participation and
decision-making efforts. For meetings observed, the IDT encouraged input from
individuals present.

82
Section H.i : Individual Support and Discharge Planning (179-188)
strengths, and
support needs. The IDTs stopped short of developing a vision that included where they want to live, as well as
what types of activities they wanted to participate in during the day (i.e., work, retirement activities,
volunteering recreational activities), and who they wanted to spend time with. ISPs did not include measurable
goals and offered few opportunities for exposure to new things and training opportunities to facilitate skill
development.
Substantial Compliance: Paragraph 179
Partial Compliance: Paragraph 183
#
Indicator
Overall
Score
1
The individual has an ISP that was developed within 30 days of admission and revised at least annually or
change in status that includes a discharge plan. (par. 179, 49)
SC
100%
7/7
2
All relevant IDT members (including the resident) participated in the planning process and attended the
annual meeting. (par. 49,51,183)
NC
29%
2/7
3
The ISP include
was determined by the IDT (e.g., communication style, responsiveness to educational activities). The
determination was based on a thorough discussion of living options and informed consent by the
individual and their guardians. (par. 180)
NC
100%
0/7
4
objections to community placement. (par. 188)
NC
17%
1/6
5
IDTs created individualized, measurable, and comprehensive action plans to address any identified
obstacles to referral or, if the individual was currently referred, to transition. (par. 180,186,50)
NC
14%
1/7
6
The ISP defined individualized personal goals (such as community living, activities, employment,
education, recreation, healthcare, and relationships). (par. 181,183)
NC
43%
3/7
7
Personal goals are measurable. (par. 183)
NC
43%
3/7
8
Assessments for all relevant disciplines submitted for the annual ISP were timely for IDT review prior to
the annual meeting (par. 52, 183)
NC
0%
0/7
9
Assessments for all relevant disciplines submitted for the annual ISP included recommendations for
supports and services. (par. 52, 183)
NC
43%
3/7
10
Assessments for all relevant disciplines submitted for the annual ISP were updated if there was a change
in status identified. (par. 52, 183)
SC
100%
5/5
11
The ISP integrated information from the behavior support plan; crisis plan; physical and nutritional
management plan; clinical, medical, and nursing plans; skill acquisition programs; and other evaluations
and assessments. (par. 49,182)
PC
4/7
12
The ISP identified the indivi. (par. 183)
SC
100%
7/7
13
(par.
183)
SC
86%
6/7
14
Action plans identify the amount, duration, and scope of all necessary services and supports to ensure
consistent implementation, review, and monitoring including timeframes and responsible person. (par.
183)
NC
0%
0/7

83
15
ISP action plans were written to be practical and functional both at the facility and in the community. (par.
181)
NC
0%
0/7
Comments:
To review this section of the Consent Decree, a set of ISPs was requested, along with sign-in
sheets, assessments, PNMPs, PBSPs, Integrated Health Care Plans and/or risk action plans,
individuals, QIDPs and direct support were interviewed, and observations were made in both
residences and day programs.
1. All individuals had an ISP that was developed annually. ISPs were revised when status
changed through the monthly integrated review process.
2. For the most part, IDT participation at meetings was good. Seven ISP signatures were
reviewed to determine if relevant staff attended the meetings. As noted at the previous
review, there was little participation by psychiatry even though five of the seven
individuals received psychiatry services. The following is a summary of that review.
IDT members not in attendance at the annual IDT meeting:
Individual #78
All relevant team members attended.
Individual #42
PCP, psychiatry, dental
Individual #29
PCP, psychiatry, dental
Individual #30
Guardian, PCP
Individual #31
QIDP, Psychiatry
Individual #39
All relevant team members attended.
Individual #79
QIDP, guardian
3. All ISPs included a determination of where the individual would like to live based on
known preferences. A more detailed description was included in the transition plans.
However, as noted throughout this report, individuals had limited exposure to a range of
living and day program options in the community, so were unable to make an informed
choice regarding where they would like to live. Individuals and their guardians had
limited opportunities to speak with providers, visit community placements (including
where feasible, overnight visits) and programs, and facilitate conversations and meetings
with individuals currently living in the community and their families prior to a
determination being made.
4. For one of six individuals (Individual #31), IDTs created individualized measurable action
5. None of the IDTs created individualized, measurable action plans to address barriers
support needed for catheter care and inappropriate sexual behaviors. There were no
measurable action plans to address these barriers.
6. Although all ISPs included a section labeled personal goals, listed goals were not
individualized and did not address all major life areas, such as community living,
employment/day activities, or recreational activities. For the most part, personal goals
were broad statements that did not include enough detail to determine what the
individual would need to do to accomplish the goal (i.e., stay healthy). ISPs should include
ion/
leisure, relationships, independence, work/day/retirement, and living options based on
the vision for what they want their life to look like. Examples of goals that did not meet
criteria included:
• to continue to stay healthy, learn new skills to
be as independent as possible, make better relationships with staff that are not
preferred, and fine tune skills that he had at one time and may have forgotten.

84
• to communicate with others, be healthy, and improve
hygiene independence.
• to maintain health and attend family gatherings.
• to move on placement and have more recreational
outings.
• ude personal goals.
• to have an endless supply of new hats, eat regular food
again, and wear his glasses more.
7. None of the personal goals were measurable, thus, the IDT would not be able to determine
when the goal was met. Goals should be worded in a way that the IDT can determine what
specifically the individual wants to do using measurable terms, so that the IDT will know
when the goal has been accomplished.
8. None of the individuals had all the relevant assessments completed within five days of the
annual ISP meeting as directed by GRC policy. Psychiatry assessments were not submitted
timely when relevant for any of the individuals. Two of five individuals receiving
psychiatric support did not have an annual assessment (Individual #42 and Individual
#31). For the three others, the assessment was not timely for IDT review. This indicator
evaluates the submission and timeliness of assessments. Section C of this report evaluates
the quality of assessments.
Assessments were often brief and did not include data or a comparative analysis of the
9. Most discipline assessment included some general recommendations for support. Some
were generic statements that were repeated for other individuals in the review group. For
example, behavioral assessments for Individual #31, Individual #78, and Individual #42
all included the following identical recommendations.
• Continually monitor assessment results, data, and anecdotal feedback from support
professionals to guide the development of behavior supports and the acquisition of
skills.
• Continually work with the support team, guardian, and psychiatrist to identify
whether the benefits of psychotropic medication outweigh the risks and, if so, the
most effective dosages.
• Continue to explore community-based residences.
-term goals might be, recommendations
GRC. Day and vocational assessments did not include recommendations for day or
vocational activities in the community. For example,
assessment recommended that he continue with his current employment at the
Greenhouse while living at GRC. The assessment did not consider employment options
sment also
recommended that he should continue with his current work if he enjoyed the job.
Relevant assessments not submitted prior to the annual ISP meeting:
Individual #78
Medical, nursing, behavioral, PT, nutrition, psychiatry, and day/vocational
Individual #42
OT, PT, dietician, psychiatry, vocational and pharmacy
Individual #29
OT, PT, dietician, day/vocational
Individual #30
PT, dietician, pharmacy, day/vocational, psychiatry, nursing
Individual #31
behavioral, OT, PT, nutrition, and psychiatry
Individual #39
nursing
Individual #79
OT, dietician, nursing (no date) and psychiatry

85
Recommendations rarely considered what new skills the individual might learn to live and
work in a less restrictive environment.
10. Relevant disciplines updated assessments when there was a change of status. Examples
where this occurred included:
•
hospitalization in May 2023. New recommendations were made and his PNMP was
revised.
• Assessments were updated for Individual #78 following a hospitalization in
December 2022.
• Individual #79 was reassessed by PT on 6/9/23 after repeated fall.
• Individual #29 was reassessed in June 2023 to determine support needs following a
hospitalization and failed community placement.
11. ISPs included some information from the behavior support plan; crisis plan; physical and
nutritional management plan; clinical, medical, and nursing plans; skill acquisition
programs; and other evaluations and assessments. Often information was cut and pasted
into the ISP document without evidence of integrated discussion. As noted above, some
assessments and recommendations were not submitted timely for consideration. Findings
included:
• e.g., medical and OT/PT) cut and
pasted into the ISP, while others were not included at all (e.g., behavior and
psychiatry). There was no documented integrated discussion regarding support
needs.
• All as
included in his list of what was most important to him, however, the IDT did not
discuss or develop integrated action plans or training based on recommendations.
• For Individual #79, the ISP included integrated supports needed in various areas of
her life.
• s included some integrated
discussion regarding supports that they needed throughout his day.
• For Individual #30, most of his assessments and recommendations were attached to
the ISP and there were some integrated strategies to address risk areas, but did not
carry over to the discussion of supporting him to achieve his goals and action plans.
12.
IDT. As noted throughout this report, however, the identification of preferences was
limited due to the lack of exposure to options, particularly the range of options available
in the community. GRC had recently begun using a new person-centered assessment that
should broaden the scope of preferences listed in the ISP. Regarding the determination of
needs, this was also limited by the quality of assessments and recommendations from
those assessments. This is further addressed in other indicators throughout this report.
13. Six of seven ISPs minimally included training of the individuals to support greater
independence and acquisition of skills
related to training. It was not evident that training had been prioritized or based on
preferences.
14. Expectations for goal achievement were not clear. Action plans were not developed to
support goal achievement in most cases. ISPs included a list of action plans/training
objectives; however, it was not clear how they supported personal goals achievement.
Training strategies were included for most, however, they did not include mastery

86
criteria, so that the IDT could determine when a skill had been mastered. Findings
included:
•
•
example, he had a goal to increase dining participation. Strategies included before
each meal; he will feel the transition card (spoon) with hand under wrist assistance. It
was not clear how many times he would need to complete this task before it was
considered mastered.
• Individual #78 had goals to increase his domestic skills, increase his personal skills,
and social skills, but none included mastery criteria, so that the IDT could determine
when a new skill had been mastered.
• Individual #30, Individual #39, Individual
not include mastery criteria except for behavioral goals.
15. Outcomes tended to focus on training to address skills identified through the assessment
process and were generally basic skills that would be needed in the community; however,
they were not prioritized based on long term outcomes that the individual wanted to
achieve, and specific training strategies were not developed for training in the community.
It should be noted that with good planning, the acquisition of skills should not be a
deterrent or barrier to the transition process.

87
Section H.ii: In-reach and Community Engagement (189-192)
Summary: Individuals did not consistently receive community living option information every six months and
were not offered integrated opportunities for community integration.
Substantial Compliance: Paragraph 190
#
Indicator
Overall
Score
1
a. Individuals receive information regarding community living options at least every six months.
b. had opportunities to visit community-based residential and vocational settings and meet with other
individuals with IDD receiving services in integrated settings at least quarterly. (par. 189)
NC
2
All staff responsible for directing, managing, or coordinating discharge planning and other informational
activities regarding community options have sufficient knowledge about community services and supports
to propose appropriate options about how an individual's needs could be met in a more integrated setting.
(par. 190)
SC
3
ISP action plans integrated opportunities for community participation and integration. (par. 192)
NC
Comments:
1.
documentation that they received information regarding living options at least every six
months. None of the individuals had visited residential or day programs in the community
or had opportunities to meet with other individuals with IDD receiving services in an
integrated setting. IDTs sent information about individuals to various agencies providing
services in the community and if accepted for services, individuals had opportunities to
visit those providers, however, they did not routinely have opportunities to visit other
residential and day providers prior to choosing a provider, so that they could make an
informed decision about options available.
2. Staff responsible for directing, managing, or coordinating discharge planning and other
informational activities regarding community options had sufficient knowledge about
community services and supports to propose appropriate options about how an
individual's needs could be met in a more integrated setting. Based on interviews and
observations, the social work team was knowledgeable regarding living options available
in the community. They met as a group weekly and reviewed transition status for all
individuals and available community options. Social workers were an integral part of the
IDT and met monthly with the IDT. Additionally, the CIM was very knowledgeable
regarding supports available in the community and provided additional information and
support when needed. This question is about knowledge regarding what's available in
the community only. Whether or not the IDT determined support needs for each
individual or whether plans were in place is addressed in H.iii Transition Planning
3. All ISPs included some general activities/outings that the individual enjoyed in the
community, however, there were no outcomes developed to ensure that individuals had
regular opportunities to participate in community activities based on their preferences or
to receive supports and services in the community. There were few options for
integration prior to discharge from the facility.
None of the individuals had action plans that offered opportunities to explore a wide
range of community-based activities or engage in integrated activities in the community
such as banking, going to church, participating in retirement programs, joining
community groups, attending classes, volunteering, etc. so that individuals were better
able to make informed choices regarding what they wanted to do during the day and
where they wanted to live.

88
Section H.iii: Transition Planning (193-200)
Summary:
Because of the lack of pre- and post-transition supports, post-move monitoring was broad, generic, and not
based on assessing the adequacy of supports and services or the success of the transition. Post-Move Monitoring
meetings observed by the Monitoring Team were not tailored to assess specific expected outcomes for the
individual.
Substantial Compliance: Paragraph 198.
Partial Compliance: Paragraph 197, & Paragraph 200.
#
Indicator
Overall
Score
1
The individual is offered a meaningful choice of community providers consistent with identified needs and
preferences. (par. 193)
NC
0%
0/6
2
The IDT assisted the individual, and their authorized representative (where applicable) in choosing a
provider. (par. 194)
NC
0%
0/6
3
participated in development of the transition plan. The individual had opportunities for meaningful
experiences and visits that enabled the individual to become familiar and comfortable with the home. (par.
195)
NC
0%
0/6
4
If requested, the individual has a right to return the agreement. (par. 196)
NC
0%
0/6
5
If the individual requested to return to GRC:
a. GRC identified barriers to community placement.
b. GRC implemented strategies to resolve barriers.
c. GRC documented steps taken to resolve barriers to community placement.
(par. 196)
N/A
6
The transition occurred no longer than six weeks after the provider agreed to serve the individual. (par.
197)
SC
100%
6/6
7
If transition did not occur within the planned timeframe,
a. the reasons it did not occur was documented, and
b. a new time frame for discharge was developed by the IDT.
(par. 197)
N/A
8
The individual has a current transition plan, updated within 30 days prior to the discharge. (par. 198)
SC
100%
6/6
9
supports, protections, and services (including amount, duration, and scope)
NC
0%
0/6
10
The transition plan identified training for the provider staff. (par. 199)
NC
0%
0/6
11
The transition plan identified assistance to be provided by GRC staff to the receiving agency. (par. 199)
NC
0%
0/6

89
12
The transition plan identified by name who would take specific action and when to deliver (or ensure
delivery) all needed supports, protections, and services. (par. 199)
SC
100%
6/6
13
All essential supports needed for transition were identified. (par. 200)
NC
0%
0/6
14
All identified supports (including behavioral supports, crisis plan, provision for physical and mental health,
etc.) were documented as in place prior to discharge. (par. 200)
NC
0%
0/6
15
All non-essential supports were in place within 60 days of discharge. (par. 200)
SC
100%
6/6
Comments:
1. Based on a review of transition plans for six individuals, none had a transition plan that
clearly identified individual preferences and no evidence
type of setting most likely to ensure a successful transition (e.g., number of roommates,
urban or rural, preferred geographic location, proximity to family) based on the
Further, none of the individuals had a transition plan that reflected meaningful choice of
community providers or facilitated support by their IDTs. It seemed that the social
workers at GRC submitted transition profiles to community providers for consideration as
potential referrals. Therefore, the choice rested with the provider who responded with an
acceptance of the individual and then they and their guardians could proceed from that
point forward. For example:
• to the Court Monitor as requested.
However, a document titled Partnership for Community Integration Transition and
Service Plan, developed by the MFP case manager, indicated he had a dream to live on
the Winnebago Reservation in Nebraska, so he would be able to attend cultural
events and celebrations. Northwest Iowa was identified on his transition referral
form as the preferred geographic location. They transitioned to a group home right in
Glenwood, which was the southwest area of the state. Documentation from Iowa
Target Case Management notes and Money Follows the Person case management
notes reflected a less than adequate process for communicating with the individual
and his guardian about their options to make an informed decision as to community
living. This lack of communication and coordination prompted intervention from the
Community Integration Manager (CIM) just weeks prior to transition from GRC.
The CIM intervened and stated that transitions were to be a cooperative effort with
MFP, case management, and the GRC social workers as a team toward a common goal,
but the scenario in this case was anything but that
West Virginia and was against his transition from GRC. The guardian (his foster
sister) expressed that she did not want him to go back to the reservation, but would
like for him to be close to the Sioux city area, so he could be near family.
Documentation reflected that the guardian did not generally participate in his IDT
, but had contact with his
social worker.
The guardian agreed for Target Case Management to assist with community living
referrals in July 2022 as she understood he could no longer stay at GRC. Eight
referrals had been made by the time the guardian agreed to proceed. It was unclear if
any of these referrals were made with guardian consent. Of those referrals, four
provider agencies did not respond, one responded with a denial, two showed
interested but did not provide a formal decision, one provider agency accepted
Individual #8 on a wait list, and one provider agency (Community Options) accepted
his referral. The guardian completed a virtual tour for a home operated by REM near
Sioux City, but this tour was from a realtor web site and not directly with the provider
agency. Additionally, GRC did not take the individual to tour the home in person.

90
In March 2023, the guardian chose Community Options and indicated she would be
happy if they would be living in the Glenwood area with other individuals he knew
from the Center. His first transition meeting was held 4/13/23. The individual
participated in several visits to his new home prior to the transition and documents
reflected he was happy and satisfied with the selection.
Information regarding informed choice was less than comprehensive for the other 5
individuals reviewed by the Monitoring Team:
• that she wanted to live in a small town in a
house with two to four other women around her age and quiet. Here interests and
preferences were defined as bowling, sports, movies, eating out, music, museums,
shopping, art, swimming, and exercising. The transition plan indicated her
parents/guardians were provided information on different provider opportunities.
•
would like to reside, but it was believed he would like a home with structure and
routine and as his family was very involved in his life, to reside closer to them. His
parents toured potential homes with AmeriServe and various day hab programs.
• that he visited the house and attended
meetings. The transition plan also indicated that different providers had shown
interest in him, but through visits and conversations, his guardian chose Nishna.
•
choice was offered. The plan stated she was going to a HCBS home in Red Oak with
three other roommates, two of whom were GRC residents. The plan also indicated she
was invited to her meetings. She went to visit the home and really enjoyed it. Her
guardians also attended meetings and visited the prospective home.
• hat transition to a community-based
setting was a personal goal he had worked toward. His plan indicated he wanted to
live with housemates who were active and shared his interest and live close to his
parents who lived in Amana. He ended up moving to a home in Glenwood
approximately 3½ hours from his parents, but his plan indicated he was excited to be
moving to a home where a friend already lived. The transition plan indicated that
viders as
they made their decision to accept support through the GRC Waiver program. The
individual was especially happy about this transition as he would be living with a
long-time friend.
2. See indicator 1 above.
3. The selected provider was actively engag
and actively participated in development of the transition plan. For the six individuals, the
selected provider was involved in communication and planning for their transition.
However, one of the six transitions, for Individual #110, appeared rushed. For example,
the provider was first involved at the time of transition plan development (just a few days
prior to her move from GRC).
For the six individuals, there was evidence that reflected all had engaged to varying
degrees in visits to their prospective home prior to the actual move. However, these visits
were either one time or lacked specificity as to their reaction to the visit. According to
available documentation:
• Individual #8 visited his new home and had supper with his housemates on 4/20/23.
• Individual #110 had been on several visits to the new waiver home and that she got
to meet her peers and staff.
• Individual #118 visited his new home on 11/20/22 and 11/28/22 and visited the day
hab program on 11/17/22.

91
• Individual #103 visited the house.
• Individual #107 visited her home and really enjoyed it.
• Individual #126 visited the house and men who would be living with him.
4. For the six individuals who had transitioned from the Center between August 2022 and
May 2023, two had a transition plan that reflected a Return Agreement had been
requested:
• -move support that a return agreement
had been completed, signed, and placed in folder completed 5/17/23.
• For Individual #107, the transition plan had a pre-move support that a return
agreement had been completed, signed, and placed in folder (but had a target
completion date of 4/6/24).
There was a provision in the Glenwood Resource Center Discharge and Transition
Planning policy (dated 5/24/21, reviewed 4/25/22, revised 6/26/23) for a six-month
return agreement. This provision indicated:
All individuals who transition from GRC to a more integrated setting shall have the
right to a return agreement, which will guarantee a right to return to either State
Resource Center [until such time as GRC does not have the capacity, then the return
will be to Woodward Resource Center (WRC)], if the request is made within six
months after the date of transition. Upon receiving a request to return GRC shall
ensure:
• The identification of barriers regarding community placement.
• Implementation of individualized strategies to resolve those barriers (including,
as appropriate, strategies to support the community service provider's ability to
care for and support the individual, and to thoroughly search for other
community service options); and
• Documentation of steps taken to resolve the barriers regarding community
placement.
• If after two (2) months from the receipt of a request to return, the individual, or
where applicable their guardian determines that the issues cannot be resolved,
the individual will be permitted to return to either State Resource Center (until
such time as GRC does not have the capacity, then the return will be to WRC).
It was unclear as to how individuals and guardians were presented with information
about their right to request a return agreement and there was nothing within the
transition plan for Individual #103 or Individual #107 to reflect the parameters for this
agreement to be enacted if requested.
5. None of the six individuals had requested a return to GRC.
6. For all six individuals, the transition occurred within six weeks after the provider agreed
to serve the individual. According to the transition plan document, development of the
transition plan was to begin at the time of referral for community transition with the
completion of the profile and continue past the transition date. However, transition
planning did not occur until a provider had accepted an individual from a referral.
• Individual #8: per the MFP case management plan, transition planning was initiated
4/13/23 and he moved 5/9/23.
• Individual #110: the profile was dated 10/16/22. The transition plan did not include
dates of meetings or the date of transition. Other documents reflected her transition
occurred 11/7/22. Additionally, Social Worker and Case Manger notes reflected
difficulty and a rush of time for scheduling a transition meeting. Some documentation
reflected that a transition meeting was held 10/27/22; other documentation reflected
a meeting date of 11/4/22.

92
• Individual #118: was accepted by AmeriServe on 10/25/22. Profile was dated
11/1/22, transition meetings were held 11/15/22 and 11/29/22, and he transitioned
on 12/5/22.
• Individual #103: the profile was dated 4/1/23. Transition meetings were held
4/6/23, 5/5/23, and 5/15/23, and he transitioned 5/17/23.
• Individual #107: the profile was dated 2/23/23. Transition meetings were held
3/3/23, 3/20/23, and 4/4/23, and she transitioned 4/6/23.
• Individual #126: the profile was dated 7/8/22. Transition meetings were held
8/9/22, and 8/16/22, and he transitioned 8/16/22.
7. N/A.
Transition planning did not appear to occur until a provider had accepted an individual
from a referral.
8. All six individuals had a current transition plan, updated within 30 days prior to the
discharge.
9. None of the six individuals had a transition plan that fully r
preferences and desired outcomes, supports, protections, and services (including amount,
duration, and scope). Goals and habilitation training that was in place at GRC was not
carried into the transition plans to continue after the move. Transition plans indicated
that outcomes and goals would be developed at the 30-day meeting. Therefore, IDTs did
not sufficiently identify desired outcomes for incorporation into transition plans to ensure
consistency for a successful transition. This was a systemic issue. This was discussed with
the CIM and at the exit meeting. Individuals working at the GRC workshop or enclaves
were required to quit their jobs at transition. Referrals to Vocational Rehabilitation were
not timely or VR was not responsive in scheduling work assessments. Individuals were
therefore relegated to workshops or day hab programs in lieu of work. For example:
• . These were to
learn to read and follow a recipe and to access recreational swimming opportunities.
Yet no strategies were developed to ensure these outcomes were supported.
Additionally, work was identified as important, but no supports were developed to
link him with vocational agencies in the community that could help him find
employment. His job at the GRC workshop that he had held for two years ended after
he moved.
10. None of the six individuals had a transition plan the identified the required competency
training the provider staff should receive prior to transition and none of the assessments
incorporated into the transition plans provided expectations for competency training.
This was noted as well for those individuals included as part of the mortality review.
The transition plan for Individual #118 reflected that training was provided to the
receiving agency on his GoTalk 4 device on 12/7/22 at 3:00 pm and that GRC trained staff
on his BSP, ISP and PNMP on 11/28/22 during a visit to the agency. For Individual #108,
the transition plan indicated training had been completed for the new provider by GRC on
5/17/23 and to see summary reports for further details, but those were not incorporated
into his transition plan.
11. None of the individuals had a transition plan that identified the specific assistance to be
provided by GRC staff to the receiving agency. Transition plans were formatted with
prompts to describe facility collaboration with community clinicians, clinician assessment
of settings, and facility and provider staff activities, such as spending time at the provider
or the receiving staff at GRC. However, the narrative provided for these prompts was most
often generic statements, such as that clinicians assisted in providing reports for the
transition plan, along with training when needed, or that facility clinicians did
assessments of the new home and current supports.

93
12. The transition plan identified by name who would take specific action and when to deliver
(or ensure delivery) all needed supports, protections, and services.
13. Essential supports needed for transition were identified, but did not include measurable
identifiers for ensuring coordination and implementation. Therefore, post-move
monitoring documentation did not provide substantive commentary on implementation
of identified support needs for the transition.
14. Identified supports (e.g., behavioral supports, crisis plans, provision for physical and
mental health, etc.) were not always documented as in place prior to discharge. For the
most part, transition plans identified the primary care provider, psychiatrist, pharmacy,
hospital, and other medical providers. However, transition plans did not always ensure
adequate carry-over of necessary supports such as behavior services, communication
services, etc. Nor did transition plans include recommendations with timeframes to obtain
assessments or consultations with community-based providers, such as behavior services,
OT, SLP, etc. For individuals who had identified support needs in these areas, it was
reported during interviews with the providers, MFP, and MCO case managers during the
ty case
management if needed.
15. Non-essential supports were in place within 60 days of discharge per documentation
within the transition plans.
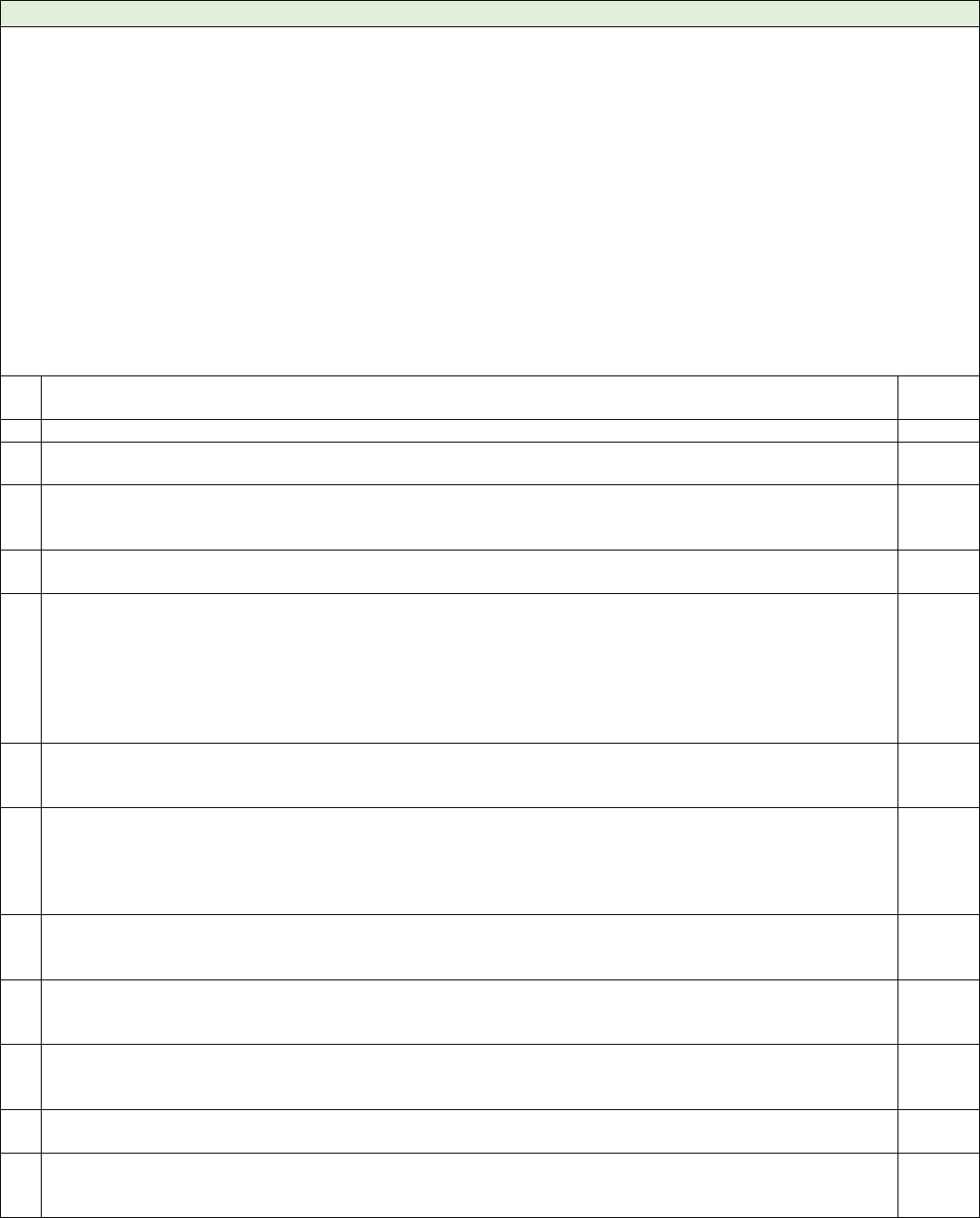
94
Section H.iv: Community Integration Management (201-211)
Summary: The Community Integration Manager was a strong asset to support GRC in moving forward with
transitions and facility closure. The CIM had requested regional CIM positions to share the workload, but this
was just in the initial stages at the time of the monitoring visit. While GRC staff were meeting regularly to discuss
barriers to transition, there were few actions developed to meaningfully address barriers, such as the lack of
providers and the lack of available ICF options for guardians who wanted that type of placement (or working
with ICF providers to remedy the perception that individuals over age 65 could not be supported in an ICF
environment and would require long-term care placement). For individuals whose guardians had chosen WRC,
there was no documentation to reflect they were offered a meaningful choice of alternate providers. The post-
transition monitoring required extensive revision for development of individualized and measurable pre- and
post-move supports to ensure timely and successful implementation of supports and services that were
Case management services to monitor services, progress, and
general wellbeing was a critical component of the transition process that needed immediate correction.
Partial Compliance: Paragraph 201, Paragraph 202, Paragraph 206, Paragraph 207, Paragraph 209, & Paragraph
211
#
Indicator
Overall
Score
1
The Community Integration Manager provides oversight of transition activities. (par. 201)
PC
2
The Community Integration Manager is engaged in addressing barriers to placement, if applicable. (par.
202)
PC
3
If an IDT recommended maintaining a placement at GRC or placement in a congregate setting with five or
more individuals, the barriers to placement in a more integrated setting, and the steps the team will take to
address the barriers were documented. (par. 203,204)
NC
4
If Woodward was the chosen provider, the individual was offered a meaningful choice of providers
consistent with their identified needs and preferences. (par, 205)
NC
5
The State maintains public reports that identify monthly data regarding:
b. number of residents in each stage of transition planning
c. number of transitions
d. types of placements
e. number of individuals recommended to remain at GRC.
(par. 206)
PC
6
collected from GRC and is aggregated and analyzed for ongoing quality improvement, discharge planning,
and development of community-based services. (par. 207)
PC
7
The State shall develop and implement quality assurance processes to ensure that ISPs, discharge plans, and
transition plans are developed and implemented, in a documented manner, consistent with the terms of this
Agreement. These quality assurance processes shall be sufficient to show whether the objectives of this
Agreement are being advanced. Whenever problems are identified, the State shall develop and implement
plans to remedy the problems.
NC
8
GRC staff conducted monitoring visits seven, 30-, 60- and 90-days following transition. (par. 209)
NC
0%
0/6
9
For each visit, a checklist was completed that included all areas of the transition plan to ensure all supports
and services were in place. (par. 209)
NC
0%
0/6
10
Individuals who had transitioned to the community had a current ISP in place. (par. 209)
SC
100%
6/6
11
Staff conducting post transition monitoring received adequate training and have been assessed for
reliability of the process. (par. 209)
CND
12
The individual has received ongoing community case management services at the frequency required based
. (par. 210)
NC
0%
0/6

95
13
The case manager met with the individual face to face at least every 30 days; at least one such visit every 2
. (par. 210)
NC
14
The case manager:
a. observed the individual.
b. assessed the environment.
c. assessed the status of identified risks, injuries, needs or other changes in status.
d. assessed implementation of the ISP.
e. assessed appropriateness of the ISP.
f. assessed the implementation of all supports and services.
(par. 210)
NC
0%
0/6
15
The case manager documented any issues/concerns noted from monitoring visits, convened the IDT to
address noted issues/concerns, and documented resolution. (par. 210)
NC
0%
0/6
16
The case manager followed any identified issues to resolution. (par. 210)
NC
0%
0/6
17
The State implemented a system to identify and monitor individuals in the Target Population who transition
from Glenwood Resource Center (for at least 365 days following transition) to another placement. (par.
211)
PC
Comments:
1. A Community Integration Manager (CIM) position was created as required under H.iv.201
of the Consent Decree. The CIM had been refining her role of transition activity oversight
and was actively involved in identification of needed actions to address shortcomings of
the discharge and transition planning process at Glenwood Resource Center as well as
systemic community barriers. The CIM was regularly meeting with the transition
facilitators and social workers in discussing the barriers report and status of transition
planning for individuals. The CIM reported that she had been working with the MCO and
MFP case managers to identify what was needed for each individual transition. The MFP
program expanded by adding eight transition specialists and the CIM had been meeting
with them bi-weekly on issues she had noted that needed action. Another MCO was
added, which made a total of three for the state. The CIM had met with the team of case
managers and management who would be assigned to the individuals from GRC and had
expressed the need for consistency and had provided information on trainings for new
case managers in the areas of motivational interviewing skills and person-centered
thinking. The CIM had met with the Social Security Department several times to try and
initiate a process to expedite the transfer of representative payee to the receiving
agencies, so that individuals were not waiting extended periods of time for their disability
income. Additionally, the CIM reported that the Iowa HHS would be hiring regional
Community Integration Managers to support transition and integration efforts.
2. See indicator 1 above.
3. Individual support and discharge plans did not reflect whether IDTs had recommended
maintaining placement at GRC or other congregate setting and did not include clear
justification for the decision, the barriers to placement in a more integrated setting, and
actions the IDT would take to address the barriers.
4. There was no prohibition in the Consent Decree for individuals to transfer to Woodward
Resource Center unless an informed decision was documented for the individual to
continue to receive services in a Resource Center. None of the individuals transferred to
WRC made an informed decision that it was the most integrated, most appropriate
setting. According to the transition tracking report provided to the Monitoring Team in
preparation for the visit, since September 2022, 18 individuals had transferred to
Woodward Resource Center (one of whom was discharged to a Hospice setting and died
7/9/23).
The Monitoring Team visited six individuals who all transferred to Woodward Resource
Center in August 2022. None of the individuals had an individual support and discharge
plan from GRC that reflected how the individuals and guardians were offered options of

96
community providers that could provide supports and services consistent with their
identified needs and preferences and how an informed choice for WRC was made.
There was no process in place to identify how many of the individuals remaining at GRC
and their authorized representatives were contemplating such a transfer. The Barriers
Report included a column titled Reality and Next Step which noted Woodward Resource
Center as the most likely possible placement for several individuals for reasons being they
(a) were denied by all ICFs from referral, (b) had complicated medical and/or behavioral
needs, and/or (c) had 1:1 supervision requirements. For other individuals, long-term care
was noted as the most likely scenario. It was evident that there was no robust
development of resources and incentives for HCBS providers to accept individuals with
high support needs. See Indicator 6 below for additional information.
Two individuals returned to GRC after transition. One individual transitioned to a HCBS
group home on 7/25/22 and had five assault arrests between September 2022 and
January 2023. The individual returned to GRC on 1/11/23. One individual transitioned to
a HCBS group home on 3/15/23 and was hospitalized on 3/30/23. An allegation was
submitted to Dependent Adult Abuse for investigation after community group home staff
j-tube. The individual returned to GRC on 5/18/23. There
was no clear summary of events that led to the individuals return to GRC nor was there
evidence to reflect that the IDT had fully assessed the transition to identify shortcomings
in the planning or identified actions to ensure necessary provision of support that would
have reduced the negative event occurring.
5. The State developed a dashboard for reporting data to the public on the census by facility,
number of individuals per transition stage category, among other data points.
(https://hhs.iowa.gov/dashboard_facilities). The public dashboard did not, however,
accomplished, whether the State was on track to accomplish the timeframes set forth in
the Consent Decree, the types of placements where individuals transitioned (e.g., HCBS
waiver group homes and size of homes, ICF/IID homes and size of homes, preferred
geographic location), recommendations that individuals remain at Glenwood, or
recommendations that individuals be transferred to Woodward Resource Center.
6. According to the Barriers to Community Placement report dated 8/14/23, there were 22
individuals with identified barriers to community transition. This report tracked, among
other things, provider agencies to whom the individuals were referred, which agencies
denied the referral, guardian preference, IDT identified barriers, and MCO/MFP
engagement and action to address identified barriers. Notably, the column on this report
titled Reality and Next Step indicated a systemic issue regarding ICF/IID as an available
option for choice of community providers. Several guardians had expressed a choice for
ICF providers, but during the barriers meeting observed by the Monitoring Team, it was
ed into acceptance by an ICF provider. That is, that
for individuals aged 65 whose guardians requested ICF as their preferred type of service,
ICF providers determined that the level of treatment required under regulations could not
be provided and that those individuals were more suitable for long-term care placement.
Individuals and guardian should be provided with a choice among all available options for
IDTs had determined that a community based ICF/IID was the most appropriate service,
the State should ensure that option is available without constraint. This was discussed
during the onsite review. The CIM was present in the meetings and identified it as an item
needing investigation.
This spreadsheet of individuals and identified barriers did not include an analysis for
ongoing quality improvement, discharge planning, and development of community-based
services as contemplated in the Consent Decree.
According to the Acceptance Timeline Status report provided during the review week,
eight individuals were identified as accepted by a provider with target move dates for

97
August 2023 (including one who was being transferred to Woodward Resource Center).
Of the remaining five individuals, one was waiting on the agency to hire staff, one was
waiting on home modifications, and three were waiting on the provider agency to build
the home. So, while these individuals may be classified as having a tentative move date,
the actual projected date of transition could not be determined for the majority.
This report also reflected nine individuals who had been accepted by a provider, but their
status was noted as being with movement which was not clearly defined but appeared to
reflect those individuals that had providers linked to the individual. The first transition
meeting for four of these individuals was held in August 2023. One individual was
awaiting a Supports Intensity Scale (SIS) assessment before transition meetings could be
scheduled. One individual had an initial transition meeting on July 7/20/23, but was
awaiting modifications and it was documented that the provider was having a difficult
time obtaining quotes from contractors for the renovations. Therefore, further transition
planning for that individual was technically on hold. Similarly, another individual was
awaiting renovation to the home but had a status of scheduling meetings noted along with
another individual whose status also indicated scheduling meetings.
The remaining 30 individuals in this report were classified as Provider Accepted with the
following status:
Status
# of Individuals
Awaiting purchase/build of home
11
Awaiting new build/ICF only choice
1
Guardian exploring options; awaiting guardian decision
4
Awaiting open bed
3
Awaiting Home Renovations
3
Guardian chose host home, awaiting process
2
Individual recovering from illness
1
waitlisted
3
Newly accepted
2
A transition report was provided to the Monitoring Team that showed tracking of 82
individuals who had been discharged or transitioned from GRC since September 2022. As
noted above, 18 individuals had been transferred to WRC. Two individuals returned to
GRC after transition. One individual transitioned to a HCBS group home on 7/25/22 and
experienced five assault arrests between September 2022 and January 2023. The
individual returned to GRC on 1/11/23. One individual transitioned to a HCBS group
home on 3/15/23 and was hospitalized on 3/30/23. An allegation was submitted to
Dependent Adult Abuse for investigation after community group home staff put solid food
j-tube. The individual returned to GRC on 5/18/23. Documentation did
not include a clear summary of events that led to the individuals return to GRC nor was
there evidence to reflect that the IDT had fully assessed the transition to identify
shortcomings in the planning or identified actions to ensure necessary provision of
support that would have reduced the negative event occurring.
Three individuals were discharged from GRC between March 2023 and July 2023 to either
nursing homes or to Hospice care in nursing homes.
7. Quality assurance processes were not in place to ensure that ISPs, discharge plans, and
transition plans were developed and implemented, in a documented manner, consistent
with the terms of this Agreement. See section K.
8. The Center provided policy Post-Transition Follow-up Protocol (effective 6/2/23) that
outlined the expected implementation of post-transition monitoring at 7, 14, 30, and 60
days to be completed by the GRC social work department. Additional monthly follow-up
monitoring was identified through 365 days post transition. Expectations for onsite
monitoring were identified for the 30-day or 60-day visits and at least one additional visit
98
during the 365 days of monitoring. Evidence of these visits was to be captured on a
standard checklist that encompassed all areas of the transition plan and addressed
whether all supports and services were in place, including that the new provider had a
current person-centered individual support plan in place, as contemplated in the Consent
Decree. There was no indication whether the CIM or other State representative would
assess a sample of monitoring visits to ensure that the process occurred and that it was
done correctly.
For the six individuals, GRC social work staff had conducted monitoring visits following
transition via TEAMs or Zoom which did not meet the criteria for a face-to-face visit.
Additionally, the standardized checklist developed for post-transition monitoring
(Transition Provider Follow-up Questions) was comprised of general domains of medical,
behavioral, health, and environmental. Within these domains were several broad
questions that were not tailored to the specific pre- and post-move supports
and services identified in each transition plan.
Therefore, monitoring of transitions was not individualized and did not measure the
timely and successful implementation of supports and services that were recommended
d, in turn, did not guide the monitoring to identify
potential events that could be disruptive to a successful transition or prompt the social
worker and case managers to develop corrective measures.
The Monitoring Team observed post-move monitoring visits for two individuals during
the review week. For both, the MFP case manager and the MCO case manager were
present along with the GRC social worker/transition specialist. The post-move monitoring
visits were structured, so that the GRC social worker/transition specialist asked questions
from the Transition Provider Follow-up Questions, followed by questions asked by the
MFP and then the MCO case managers. This was an improvement over previous PMM
visits where this framework did not exist. The Monitoring Team did not observe that the
GRC staff or the case managers ask to review data related to implementation of the ISP
goals, medication administration records, incident reports, daily staff notes, etc. to fully
assess implementation of the indi
9. See Indicator 8.
10. For all six individuals who had transitioned to the community, each had a current
Individual Support Plan. These plans varied in format and content. None of their ISPs
included meaningful goals or action plans that, if implemented, would lead toward
achievement of their personal goals. For example, none of the individuals had goals
designed to support community participation and integration, work, or volunteer
opportunities, or gaining skills to increase their independence in daily life activities.
11. Staff conducting post transition monitoring did not appear to have received adequate
training and were assessed for reliability of the process as each PMM visit was run a little
differently with no clear agenda. Training records were not requested by the Monitoring
Team, so this was unable to be verified. Documentation will be requested during the next
review to support. See Indicator 10.
12. (Indicators 12-16) The individual received ongoing community case management
services at the frequency required based on the
For the six individuals, each received Money Follows the Person (MFP) as the primary
case management service for the first year after transition. Individuals also had an
assigned Targeted Case Manager through the Managed Care Organization who
participated in the transition and attended meetings and provided support to the MFP
case manager as needed. At the end of the MFP year, the MCO case manager would
become the primary service.

99
The Monitoring Team reviewed visit, contact, and monitoring notes from the assigned
MFP and MCO case managers. MFP and MCO case managers were meeting with the
individuals monthly and some of the meetings were virtual.
Case management activity did not reflect that case managers were reviewing data and
documentation to assess ISP implementation, stability of the transition, and
implementation of all supports and services. Case management notes reflected visits with
the individuals and broadly stated observations of seemed happy or having a good
relationship with housemates. Or notes were solely correspondence with provider
representatives about appointments. The case note format did not provide comprehensive
prompts to gather substantive information based on review of documents and interview
of provider staff and the individual to identify potential or emerging problems with the
transition or to identify areas of needed follow up with development of adequate
correction actions.
ervices to monitor
services, progress, and general well-being was a critical component of the transition
process that needed immediate correction. This was also noted in the Department of
Justice Investigation of Glenwood and Woodward Resource Centers report issued
12/8/21: A lack of role clarity regarding key aspects of transition planning further
impedes the process. Social workers, MCO case managers, and, in some instances, MFP
staff share responsibility for engaging with residents and guardians about community
services, identifying options, and planning for transition. State officials acknowledge that
the responsibilities of each remain unclear. The lack of coordination contributed to
deficient information sharing and support planning.
17. As noted in indicators 8-9 above, the State had implemented a system to identify and
monitor individuals who transition from Glenwood Resource Center (for at least 365 days
following transition), but the system lacked substance.
It should also be noted that eight individuals had passed away after discharge from GRC:
• One individual was discharged on 5/31/22 to a HCBS waiver group home and died
approximately six months later.
• One individual was discharged on 9/12/22 and died in a skilled nursing facility
approximately four months later 1/5/23.
• One individual was discharged on 11/18/22 and died 11 days later in a hospice
facility.
• One individual was discharged on/12/7/22 to a HCBS group home and died 1/15/23.
• One individual was discharged on 3/16/23 to a nursing home and died eight days
later in hospice services.
• Another individual was discharged to this same facility on 7/15/23 and died seven
days later in Hospice services.
• One individual was discharged 4/11/23 to a nursing facility and died 13 days later.
• Another individual was discharged to this same facility on 4/12/23 and died 26 days
later.
A Community Mortality Review was completed with the following results.
An additional four individuals that died in the period reviewed by the Monitoring Team
were chosen for a mortality review (Individual #9, Individual #57, Individual #88, and
Individual #120.)
Three of these had transitioned to the community (Individual #57, Individual #88,
Individual #120). Review of Individual #88 and Individual #120 suggested a significant
need for improvement in the transition process.
• The medical team should be reviewing deaths for GRC individuals even if they had
transitioned to the community within the past rolling one year period. However, this

100
was not done. Consequently, there was no way to learn what happened and how the
likelihood of death can be minimized, and the transition process improved. The
medical department needs access to the community documents (nurses notes, death
certificate, PCP notes, lab results, orders, etc.) to review deaths. Access to documents
may be an inter-agency challenge, but the transition process should include a
requirement that record availability is complete and timely from any community
agency receiving an individual.
• There was no or very little quality training that ensured an adequate knowledge
based for the agency staff receiving the two individuals. Training needs to include
shadowing, with components of agency staff being at GRC and observing the GRC staff
interactions with the individual. Moreover, GRC staff need to follow the individual
into the community at the time of transfer, and observe the agency staff doing ADLs,
etc. to ensure there is proper food texture, the PNMP is followed for eating,
positioning, bathing, cueing properly, etc. The shadowing should continue until the
new staff demonstrate competency in all areas of care. This would take at a minimum
of 48 continuous hours, but could take much longer.
• There was the need to ensure there was a follow-up technical assistance team that
was readily available for a year after the transition date, 24/7, to answer questions
and make an urgent visit if needed. Threshold markers of when technical assistance is
mandated need to be developed, such as, rapid weight loss of more than two pounds
per week, two falls within a week, or development of skin breakdown. The member of
the technical assistance team involved in that area (e.g., speech therapy for dysphagia
issues) would be the member of the team that would interact and visit the home
promptly with follow-up until resolution of the concern.
• In the future, for nonverbal individuals, there should be a heightened need for a
gradual transition process. Being blind or deaf (or both) requires additional steps, so
that the transition process can meet their needs. For instance, if an individual were
deaf and knew sign language and later developed blindness, the staff would be able to
continue to
be taught to the receiving staff and they would need to know enough symbols.
However, this can take months of planning and learning on the part of the agency staff
prior to the final move. Another example is the recording of familiar staff and family
voices to encourage meal intake and increase comfort with their unfamiliar
environment and new staff. In such cases, having GRC staff jointly participate with the
receiving agency staff may allow the individual to be more accepting of the unfamiliar
environment.

101
Section I: State Staff (212-215)
Summary: Staffing continued to be a barrier in meeting the needs of the individual. GRC continued to actively
recruit and had some success since the previous review by expanding their external contracting with vendors.
While a policy did not exist regarding the staff complaint process, based upon the documentation provided,
there did appear to be some method to accumulate the data.
Substantial Compliance: Paragraph 213
Partial Compliance: Paragraph 212, Paragraph 214, & Paragraph 215.
#
Indicator
Overall
Score
1
GRC shall maintain appropriate and adequate staffing by ensuring:
i. Retention of sufficient residential treatment workers per resident to safely staff GRC always.
ii. Retention of an adequate number of supervisory staff, and GRC leadership
iii. Retention of demonstrably competent, appropriately trained, and credentialed, staff and facility
leadership
iv. Responsibilities and workloads are appropriate.
v. Any hiring or firing of leadership is approved by HHS Central Office.
(par. 212,215)
PC
2
GRC will have a performance evaluation process for all GRC staff.
i. Will occur annually.
ii. Be conducted by someone of the same specialty.
(par. 213)
SC
3
GRC will have a system in place to ensure complaints regarding GRC staff are investigated to ensure needed
actions are completed. (par. 214,221)
PC
Comments:
1. GRC was facing multiple challenges in recruiting and maintaining staffing. The issue of
closure further complicated the challenge for individuals living at GRC.
As of this review, GRC had 216 filled Resident Treatment Workers and 31 Resident
Treatment Supervisors. The current RTW relief factor was 1.677, including the temporary
RTWs. This fell short of the 1.8 relief factor identified in the Consent Decree. A relief factor
multiplier formula of 1.8 (meaning there will be 1.8 residential treatment workers filled
and budgeted for every residential treatment worker needed on shift) or more if
necessary to account for staff vacancies and leave.
2. A Performance Planning and Evaluation policy guided the ongoing review of staff to
ensure continued competency. The policy provided information regarding the purpose of
the evaluation and the responsibilities and tasks. The accompanying administrative rule
Chapter 62-Performance review included the minimum requirements of the performance
evaluation and the sharing of information. The training log provided contained the
individual trained as well as the manager who provided the training with date completed.
3. The Center was asked to provide a policy for the training of staff on how to report
concerns as well as the methods in which staff can report such concerns, but no
documentation was provided. A document was provided that contained a list of staff
complaints dating back to 11/23/22. The list identified the issue, the staff name, date, and
outcome of the event, such as training etc.

102
Section J: Organizational Accountability (216-228)
Summary: Glenwood Resource Center had a full leadership team that consisted of the below professionals. In
addition, GRC was supported by Kelly Garcia-Director of Iowa Health and Human Services and Cory Turner-
Division Administrator of Iowa Human Services. Most complaints were responded to in a timely manner. As part
of the HHS website, there was access to multiple Consent Decree pages that explain the case and the process for
GRC to close.
Substantial Compliance: Paragraph 216, Paragraph 218, Paragraph 219, Paragraph 220, Paragraph 227, and
Paragraph 228
Partial Compliance: Paragraph 217, Paragraph 221, Paragraph 223, Paragraph 225, & Paragraph 226
#
Indicator
Overall
Score
1
b. HHS Staff has been identified to oversee operations at GRC. They will have oversight to ensure
compliance with SA provisions. (par. 216,217)
PC
2
The State shall engage with Stakeholders to ID concerns, goals, and recommendations regarding the CD.
(par. 218)
SC
3
HHS Central Office conducts regular in person visit at GRC. (par. 219)
SC
4
The State developed and trained staff in methods to report complaints with one method being
anonymous. (par. 220)
SC
5
State shall implement timely and effective investigations into reported concern. (par 221)
PC
75%
3/4
6
The State shall provide reporting GRC staff with a substantive response concerning the outcome of the
investigation. (par. 222)
N/A
7
GRC and HHS Central Office develop and implement effective mechanisms for identifying, tracking, and
addressing trends regarding resident care and health outcomes. (par. 223)
PC
8
well-being, and shall ensure regular reporting, analysis and, when necessary, corrective actions by GRC
and HHS Central Office. (par. 217, 225)
PC
9
The State shall establish a Resident Council to enable GRC residents to make recommendations and
provide information to the GRC Superintendent (par. 225)
NC
10
State shall establish a reliable method of public reporting that includes QM reporting (Section K) (par.
226)
PC
11
HHS Central Office shall review and approve all policies, and amendments to them. (par 226)
SC
Comments:
1. Glenwood Resource Center had a full leadership team that consisted of the below
professionals. In addition, GRC was supported by Kelly Garcia-Director of Iowa Health and
Human Services and Cory Turner-Division Administrator of Iowa Human Services.
Cory Turner was currently serving as the Director for all State-Operated Facilities and
reported directly to the HHS Director. Per his position description, he was directly
responsible for the oversight of the six HHS 24/7 facilities. His role was to ensure the
superintendent in charge of GRC developed and implemented strategic and effective
operational plans. He along with other State leadership were routinely on site and
involved as evidence of presence in meetings via signature sheet.
NAME
TITLE
Angel, Jose
CHIEF MEDICAL OFFICER
Baggett, Karen
TREATMENT PROGRAM ADMINISTRATOR - AREA 2
Darrow, Charles
PSYCHOLOGY ADMINISTRATOR
Edgington, Marsha
SUPERINTENDENT
Heiman, Cara
ADMINISTRATOR OF NURSING
Hunter, Daniel
DAY SERVICES DIRECTOR

103
Iversen, Cade
ASSISTANT SUPERINTENDENT OF INTEGRATED SERVICES
Konfrst, Scott
INFORMATION TECHNOLOGY ADMINISTRATOR
Landeen, Dax
ASSISTANT SUPERINTENDENT OF TREATMENT SUPPORT
SERVICES
Lovato, Darlene
QUALITY MANAGEMENT DIRECTOR
Mayhew, Diane
TREATMENT THERAPY SERVICES DIRECTOR
Robinson, Kelly
SOCIAL WORK ADMINISTRATOR
Sayers, Heath
ASSISTANT SUPERINTENDENT TREATMENT PROGRAM SVCS.
Wade, John
TREATMENT PROGRAM ADMINISTRATOR - AREA 1
2. Per report, the State currently engaged with stakeholders (including staff, parents,
guardians, non-governmental entities with oversight responsibilities for GRC, and other
stakeholders) to identify their goals, concerns, and recommendations regarding
implementation of this Agreement. Additionally, the meetings were no longer combined
with the other State Resource Center.
3. See indicator 1.
4. Documentation provided by GRC showed active training of the Center Complaint process,
including methods to report anonymously.
5. Three of the four complaints were followed for resolution in a timely manner.
• For one staff, a complaint was filed on 3/5/23 regarding possible inappropriate
interactions with a nurse and another on 3/23/23. An interview was not conducted
until 4/6/23 regarding the incident on 3/23/23.
• For the three other staff, investigations were completed in a timely manner.
6. Not applicable for this review.
7. See QM indicator 3.
8. See QM indicator 3.
9. There was no Resident Council in place that enabled GRC individuals to make
recommendations regarding topics of interest to the Superintendent and HHS Central
Office.
10. As part of the HHS website, there was access to multiple Consent Decree pages that
explained the case and the process for GRC to close.
11. GRC policies had been, and continued to be, updated, and reviewed, but lacked evidence of
review and approval by HHS prior to implementation.

104
Section K: Effective Quality Management (229-235)
Summary: Data need to be added to the Quality Management program. This included engagement and skill
acquisition, choice/self-determination, staff capacity, compliance with policies and procedures
eferrals/transitions to other providers.The QM program should include evidence of HHS central office review
of quality data in Quality Council meeting minutes (or however quality data review is typically documented).
Substantial Compliance: Paragraph 233.
Partial Compliance: Paragraph 229, Paragraph 230, & Paragraph 231
#
Indicator
Overall
Score
1
services at GRC are consistent with current, generally accepted professional standards and implemented in
an appropriate manner. The State shall ensure data related to the provision of clinical care and services is
dependable, analyzed, and
(par. 66)
NC
2
Quality Management process and procedures are consistent with current, generally accepted professional
standards of care. These processes timely and effectively detect problems and ensure appropriate
corrective steps are implemented. (par. 229)
PC
3
data pertaining to the domains and topics listed below, sufficient to implement an effective continuous
quality improvement cycle.
quality management program shall use this data in a continuous quality improvement cycle to
develop sufficient reliable measures relating to the following domains, with corresponding goals and
timelines for expected positive outcomes, and triggers for negative outcomes.
A Quality Management program shall collect, report on, and analyze valid and reliable data regarding GRC
sufficient to identify overall trends in the following domains:
i. Safety and freedom from harm
ii. Physical health and well-being
iii. Beh health and well-being
iv. Engagement and skill acquisition
v. Choice/self-determination
vi. Risk management
vii. Staff capacity
viii. Compliance with policies and procedures
ix. Referrals/transitions to other providers
(par. 66,102,211,223,230,231)
PC
4
The IDT utilizes the data provided through the QM process to drive the decision-making process. (par. 232)
NC
5
HHS reviews the routine QM reporting (par. 233)
SC
6
program and take action to improve the Quality Management program when necessary.
The State shall effectively identify the need for and shall direct and monitor the implementation and
effectiveness of needed corrective actions and performance improvement initiatives at GRC.
(par. 234,235)
NC
7
i.
ii.
(par. 102c i,ii)
PC
8
at GRC is consistent with current, generally accepted professional standards and implemented in an
appropriate manner. The State shall ensure that the Psychology Department shares restrictive intervention
PC

105
quality improvement, pursuant to the processes set forth in Section IV.K. (par. 126)
9
uality management system shall include processes to ensure that the habilitation, training,
education, and skill acquisition programs provided to GRC residents are consistent with current, generally
accepted professional standards and implemented in an appropriate manner. The State shall ensure that
.
(par. 162)
NC
10
The State shall develop and implement quality assurance processes to ensure that ISPs, discharge plans,
and transition plans are developed and implemented, in a documented manner, consistent with the terms
of this Agreement. These quality assurance processes shall be sufficient to show whether the objectives of
this Agreement are being advanced. Whenever problems are identified, the State shall develop and
implement plans to remedy the problems. (par. 208)
NC
Comments:
1. GRC submitted documentation of the Medical Quality Council dated 4/11/23, 5/9/23,
6/13/23, and 7/11/23. Health care indicators reviewed each month included aspiration
pneumonia, dehydration, bowel obstruction/ileus, respiratory infections, urinary tract
infections, health care related infections, ER visits/on campus transfers/hospitalizations,
skin breakdown, lacerations requiring closure with sutures or Dermabond, underweight
status, obese status, and unplanned significant weight change. The Quality Council
Meeting report and minutes provided evidence the medical department data were shared
with the GRC Quality Management program.
Trends were identified in the most recent rolling 12 months of data, but for the minutes of
4/11/23 6/13/23, there was no discussion about which trends were significant and
needed an action plan and responsible department. Hence, whenever problems were
identified, there was no information as to the creation and implementation of corrective
steps involving one or more of the healthcare departments. For the 7/11/23 meeting, the
minutes indicated two recommendations with assigned party and follow-up date. The
recommendations were specific to individual events. There was no systemic
recommendation identified leading to an action step. A separate Interdisciplinary QI data
form was submitted, which provided a summary of data per areas of risk, listed as a total
per month for each of the defined risks.
2. The quality management process and procedures were minimally consistent with current,
generally accepted professional standards of care. ell short of industry
benchmarks or best practices in the following areas:
• Data Reporting: Data were reported on a frequency (count) basis, which made it
challenging to assess whether changes in the data required action or if they were
simply a result of fluctuations in census (the number of people being tracked).
Reporting data as a count may not provide sufficient context for meaningful analysis.
• Timely Problem Detection: The inability to accurately compare data over time made it
difficult to determine if problems were being detected in a timely manner. This
implied that GRC may struggle to identify issues promptly and take appropriate
corrective actions.
It is recommended that GRC enhance its quality management processes and data
reporting practices to facilitate better analysis and decision-making by implementing a
methodology for normalizing the data, reporting it as a rate rather than a count.
Normalization allows for meaningful comparisons over time and across different contexts,
potentially improving the accuracy of data analysis.
Alternatively, the summary of individuals with 5+ incident reports completed for Area 1
in March and April 2023 and for Area 2 in March 2023 (no incidents met the trigger
threshold for Area 2 in April 2023) included corrective steps, implementation, and results.
With this threshold identified per individual, it is possible to compare data over time and
to identify issues and corrective action for an individual.

106
3. ed data and maintained a process for
reviewing its monthly. The monthly Glenwood Resource Center Quality Indicator Report
included data for over 250 outcome and performance measures that had been defined.
However, there was no indication that all this data sets were reviewed and acted upon
regularly. A subset of the quality indicator data was evaluated in greater detail in each
meetings. There remained domains that were required under the consent decree that
were not reported within the quality management structure. See bullets below.
Minutes were generated that summarized discussions during the Quality Council
meetings. According to the Quality Management policy, last revised on 5/22/23, the
minutes from the Quality Council meetings shall include the following information:
corrective actions identified, the person responsible for implementation, and the due date.
However, this was not the case. Instead, a separate, untitled document for recording
remediation actions was initiated with the 3/21/23 meeting and was maintained through
the meeting on 8/15/23. Although, it appeared that tasks that were determined to be
completed (closed) during previous meetings were removed from the document dated
8/28/23 for the 8/15/23 meeting. It is recommended that GRC develop a system for
documenting corrective actions, person responsible, and due date that can be tied to each
At minimum, all identified actions and their status
should be maintained.
A review of minutes from the Quality Council meetings dated 3/21/23, 4/18/23, 5/16/23,
and 8/15/23 and the untitled list of remediation actions resulted in the following
observations. The document review included meetings through May and the Monitor
observed the August production. The July report was requested, but not provided.
• Data for each indicator was shown as compared to the previous month, but no
indication of trends over time.
• Pharmacy data was made available and reviewed during the 8/15/23 Quality Council
meeting. Prior to that meeting, this information and data were not provided.
• Extensive analysis of medication variances was included in all the referenced
minutes, along with remediation actions planned and/or implemented.
• Information about types of community outings completed by recreation staff was
included in the minutes for the 8/15/23 Quality Council meeting. This detail had
previously not been included.
For the domains specified in the Consent Decree, the Quality Management data did not
include the following:
• Engagement and skill acquisition
• Choice and self determination
• Staff capacity
• Compliance with policies and procedures
• Referrals / transitions to other providers
Data and information on these topics may be included in other reports (e.g., employee
vacancy and staff assignment reports, Glenwood Resource Center Transition and
Discharge Monitoring Report, Glenwood Resource Center Transition Barrier, and
Guardian Preference Report) or compiled through other processes (e.g., Individual
Implementation Program Monitoring Procedure and ISP reviews), but these data were not
included in the Quality Management data.
4. There was no documented or reported indication that quality management data were
used by the IDTs to drive decision making.
5. Evidence of review of Quality Council data was observed in email exchanges between the
State-Operated Facilities Division Director and GRC staff. The email exchanges occurred
prior to the 8/15/23 Quality Council Meeting minutes, but they were not initially included

107
in the analysis of the Quality Council Report. This indicated that the exchange was not
formally part of the quality management program at that time.
The evidence of oversight of quality data was eventually included in the minutes for the
meeting held on 8/15/23. However, it was placed in a section titled, HHS Oversight
Questions/Concerns at the end of the minutes, rather than being associated with specific
topics discussed during the meeting. It is recommended that the comments and
discussions related to the oversight of quality data be associated with each specific topic
discussed during the Quality Council Meeting. This would ensure clarity and transparency,
making it evident that these discussions were based on relevant data and were acted upon
as appropriate. This may improve the organization and accessibility of information for
future reference and decision-making.
6. Other than cited in the previous item, there was no indication that the Quality
Management program was specifically monitored by HHS Central Office staff. During an
interview with the State-Operated Facilities Division Director, it was mentioned that there
were plans to hire someone skilled in data management who would support quality
management, but this had not been accomplished at the time of the monitoring visit. It
was also mentioned in an interview with central office staff that HHS Central Office
Management Analyst had responsibilities for monitoring Consent Decree compliance.
Specific details of these duties were not relayed. It is recommended that a formal schedule
and procedure be developed and implemented to clearly outline HHS responsibilities for
this oversight, the frequency of review, and expected actions.
7. Accurate reporting of medication variances was not consistently observed. Based upon a
review of the May/June 2023 MARS for seven individuals, six of the seven showed
gaps/issues with documentation and could not find variance data/documentation for
potential variances 1-2.
The Quality Management Director chaired the Medication Variance Committee. Evidence
of training in Quality Management for all Medication Variance Committee members was
not found.
The Monitoring Team Nurse was present to observe the Medication Variance Committee
meeting 8/17/23 and, afterwards, interviewed the AON who chaired the committee.
The Medication Variance Committee meeting was well organized, with a brief but
thorough discussion about the best course of corrective action for reported medication
variances reviewed. The focus was on variances level 3-9 (that reached the individuals)
from their agenda list. Present were QA, Residential, Medical, and AON.
The facility took steps to reduce medication variances. The Nursing Administrator
provided information that the reported rate of variances is trending downward over the
past three months, and that the process changes implemented included:
• A policy for the Medication Variance Committee was implemented since the
February 2023 monitoring review, and the format for action plans modified.
• The Medication Variance Committee meets weekly, allowing for timely responses
to occur, including planning, and tracking corrective actions (retraining, if
indicated, formal counseling and HR/administrative actions if indicated).
• Actual administration of medications and treatments are now completed
primarily by licensed nurses (LPNs, RNs). The use of Certified Medication Aides
• Upon exchange dates with pharmacy, RNs are now reviewing the orders, bubble
packs, labels, and MARs to catch any potential error before it reaches an
individual.
Minutes from the Quality Council meetings on 3/21/23, 4/18/23, 5/16/23, and 8/15/23
included an analysis of types of actual and potential variances. Minutes from the 4/18/23

108
meeting included a list of remediation actions. One item in the list was that QIDPs would
also start doing weekly compliance checks. The Monitoring Team interviewed five QIDPs
during the visit and all confirmed that this activity was completed at least weekly.
8. The monthly Quality Council Meeting report included data on restrictive interventions,
both the number of individuals subjected to any form of restrictive intervention and the
number of individuals with restrictive intervention(s) based on a peer's identified needs.
However, it was noted in the minutes for the Quality Council meetings that these data
were not provided by the Psychology Department. Specifically, the note indicated the
responsibility for these data shifted from the house psychologist to the QIDPs in July
2020. It was further observed that recommended action for the 4/18/23 Quality Council
meeting included having the psychologist review pica diagnosis and how data were
collected. This suggests that a psychologist was not routinely involved in verifying the
validity and reliability of these data and analyzing it.
The Quality Report also contained information about programs with approved restrictive
interventions by the Human Rights Committee, as well as a detailed analysis of restraint
use.
It is not possible to determine if remediation plans were developed and executed for
issues that arose and if the plans were consistently completed. The Quality Council
meetings now maintained a separate, untitled document for recording remediation
actions, starting from the 3/21/23 meeting. An example from the 4/18/23 meeting
demonstrated a month-to-month increase of six individuals with restrictive interventions
(from 61 in February 2023 to 67 in March 2023). However, the tracking document for
remediation showed two recommended actions for the same individual (Individual #7),
overlooking the other five new cases that required restrictive interventions in March
2023.
Additionally, a review of minutes from the 2/21/23 Quality Council meeting indicated a
discrepancy. That is, actions needed should have been noted for the increase of two
individuals requiring restrictive intervention from December 2022 to January 2023, but
this documentation was absent.
9. GRC engaged in several processes designed to evaluate habilitation, training, education,
and skill acquisition programs. During an interview with the QIDP supervisor and five
QIDPs, it was shared that they completed monitoring activities for engagement,
medication administration, and Individual Implementation Programs. The supervisor was
responsible for managing these activities completed by the QIDPs and to complete them
personally. The supervisor also completed the Unannounced Rounds Tool at least weekly
at each program. A review of the documents for two weeks prior to the onsite monitoring
visit revealed these checklists were completed for each program on 7/28/23, 8/3/23 or
8/4/23, 8/6/23, and 8/10/23 or 8/11/23. The day of the week and time of observations
and checklist completion varied.
A newly appointed Quality Management Coordinator completed reviews of individual
service plans using the ISP Performance Measures for Compliance2023 Format
document. It included the minimum standard and the best practice standard for many
areas. This was a recent practice that lapsed when a previous Quality Management
Coordinator terminated employment. As of the time of the monitoring visit, the current
QM Coordinator had completed two reviews. These reviews appeared very thorough and
provided guidance for developing a more complete, detailed ISP.
The documentation maintained for the above processes was on a case-by-case basis.
There was no mention of aggregate data analysis validation or utilization of data as part of
the Quality Management program. It is recommended to include this aggregated data or
other data on habilitation, training, education, and skill acquisition programs to gain
insights, identify trends, and make informed decisions.

109
Additionally, the observation form may need improvement. Some items on the checklist
were subjective and lacked observable, measurable criteria. Consider reviewing and
updating the form to include specific, objective assessment criteria or provide clear
definitions for terms presently on the form. For example, the phrase activity enhances
social development was subjective and should be clarified. Reviewing and updating
assessment forms to make them more objective will lead to more consistent and reliable
evaluations.
Data on length of stay at GRC was not available. Admission date was recorded on each
individualFace sheet, but data were not aggregated for the GRC population.
10. GRC maintained a monthly report titled Glenwood Resource Center Transition and
Discharge Monitoring. This report included a listing of individuals who discharged from
GRC and narrative of any follow-up since discharge. A spreadsheet listing all individuals,
discharge date, provider, and follow-up activity was also maintained. However, there was
no indication that the State had a formal process to assess that ISPs, discharge plans, and
transition plans were developed and implemented and no evidence of problem
identification or plans to remedy any problems.
