Evidence-Based Clinical Guidelines for
Multidisciplinary Spine Care:
Diagnosis & Treatment of Low Back Pain
7075 Veterans Blvd
Burr Ridge, IL 60527
630-230-3600
www.spine.org
© 2020 North American Spine Society
978-1-929988-65-5
Diagnosis & Treatment of Low Back Pain | Preface
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
2
Authors & Contributors
Evidence-Based Guideline Development
Committee Co-Chairs
D. Scott Kreiner, MD
Paul Matz, MD
Diagnosis Section
Section Chair:
Daniel K. Resnick, MD, MS
Authors:
Norman B. Chutkan, MD, FACS
Adam C. Lipson, MD
Anthony J. Lisi, DC
Tom E. Reinsel, MD
Robert L. Rich Jr, MD, FAAFP; Stakeholder
Representative, American Academy of Family
Physicians (AAFP)
Contributor:
Robert C. Nucci, MD
Imaging Section
Section Co-Chairs:
Charles H. Cho, MD, MBA
Gary Ghiselli, MD
Authors:
Sean D. Christie, MD
Bernard A. Cohen, PhD
S. Raymond Golish, MD, PhD, MBA
Murat Pekmezci, MD
Walter S. Bartynski, MD; Stakeholder Representative,
American Society of Spine Radiology (ASSR)
Medical & Psychological Treatment Section
Section Chair:
Christopher M. Bono, MD
Authors:
Paul Dougherty, DC
Gazanfar Rahmathulla, MD, MBBS
Christopher K. Taleghani, MD
Terry Trammell, MD
Randall P. Brewer, MD; Stakeholder Representative,
American Academy of Pain Medicine (AAPM)
Ravi Prasad, PhD; Stakeholder Representative, American
Academy of Pain Medicine (AAPM)
Contributor:
John P. Birkedal, MD
Physical Medicine & Rehabilitation Section
Section Chair:
Charles A. Reitman, MD
Authors:
R. Carter Cassidy, MD
Dennis E. Enix, DC, MBA
Daniel S. Robbins, MD
Alison A. Stout, DO
Ryan A. Tauzell, PT, MA, MDT
Contributor:
William L. Tontz, Jr., MD
Interventional Treatment Section
Section Chair:
John E. Easa, MD, FIPP
Authors:
Jamie Baisden, MD, FACS
Shay Bess, MD
David S. Cheng, MD
David A. Provenzano, MD; Stakeholder Representative,
American Society of Regional Anesthesia and Pain
Medicine (ASRA)
Yakov Vorobeychik, MD, PhD; Stakeholder
Representative, Spine Intervention Society (SIS)
Contributors:
Michael P. Dohm, MD
Thomas J. Gilbert, MD
Joseph Gjolaj, MD
Matthew Smuck, MD, Stakeholder Representative,
American Academy of Physical Medicine and
Rehabilitation (AAPM&R)

Diagnosis & Treatment of Low Back Pain | Preface
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
3
Surgical Treatment Section
Section Chair:
William C. Watters III, MD, MS
Authors:
Thiru M. Annaswamy, MD
Steven W. Hwang, MD
Cumhur Kilincer, MD, PhD
RJ Meagher, MD
Anil K. Sharma, MD
Kris E. Radcli, MD; Stakeholder Representative,
American Academy of Orthopaedic Surgeons (AAOS)
Contributor:
Jordan Gliedt, DC
Cost-Utility Section
Section Chair:
Zoher Ghogawala, MD, FACS
Authors:
Simon Dagenais, PhD, MSc, DC
Jerey A. King, DC, MS
Paul Park, MD
Daniel R. Perry, MPT, MDT
Jonathan N. Sembrano, MD
John E. O’Toole, MD, MS; Stakeholder Representative,
American Association of Neurological Surgeons
(AANS)
Padma Gulur, MD; Stakeholder Representative, Ameri-
can Society of Anesthesiologists (ASA)
Contributors:
Darren R. Lebl, MD (Cost-Utility Section)
Alex Seldomridge, MD, MBA (Cost-Utility Section)
Participating Societies
(does not necessarily imply endorsement)
American Academy of Family Physicians (AAFP)
American Academy of Orthopaedic Surgeons
(AAOS)
American Academy of Pain Medicine (AAPM)
American Association of Neurological Surgeons
(AANS)/Congress of Neurological Surgeons (CNS)
American Society of Anesthesiologists (ASA)
American Society of Regional Anesthesia and Pain
Medicine (ASRA)
American Society of Spine Radiology (ASSR)
Spine Intervention Society (SIS)
Contributing Societies
(does not necessarily imply endorsement)
American Academy of Physical Medicine and
Rehabilitation (AAPM&R)
American Physical Therapy Association (APTA)

Diagnosis & Treatment of Low Back Pain | Preface
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
4
Financial Statement/
Disclosures
This clinical guideline was developed and funded
in its entirety by the North American Spine Society
(NASS) with the exception that stakeholder societies
provided representatives and paid for the travel
and accommodation of their representatives to
recommendation meetings. All participating
authors have disclosed potential conicts of interest
consistent with NASS’ disclosure policy (http://
www.spine.org/DisclosurePolicy). Disclosures of all
authors and contributors are listed in the Technical
Report associated with this document.
Comments
Comments regarding this guideline may be submitted
to the North American Spine Society at guidelines@
spine.org and will be considered in development of
future revisions of the work.
Endorsements
Letters of endorsement from external societies can
be found in the Technical Report associated with this
document.

Diagnosis & Treatment of Low Back Pain | Preface
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
5
Table of Contents
I. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
II. Guideline Development Methodology and Process ..................................8
III. Glossary and Acronyms .............................................................12
IV. GuidelineDenitionandInclusion/ExclusionCriteria ...............................16
V. Summary of Recommendations ..................................................... 17
VI. Recommendations for Diagnosis and Treatment of Low Back Pain ..................40
A. Diagnosis .......................................................................40
B. Imaging .........................................................................60
C. Medical and Psychological Treatment ...........................................69
D. Physical Medicine & Rehabilitation .............................................101
E. Interventional Treatment .......................................................158
F. Surgical Treatment .............................................................190
G. Cost-Utility ....................................................................198
VII. Appendices ........................................................................213
A full bibliography and technical report, including the literature search parameters and evidentiary tables
developed by the authors, can be accessed at https://www.spine.org/Research-Clinical-Care/Quality-
Improvement/Clinical-Guidelines.

Diagnosis & Treatment of Low Back Pain | Introduction
6
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Objective
The objective of the North American Spine Society
(NASS) Clinical Guideline for the Diagnosis and Treat-
ment of Low Back Pain is to provide evidence-based
recommendations to address key clinical questions
surrounding the diagnosis and treatment of adult
patients with nonspecic low back pain. This guide-
line is based upon a systematic review of the evidence
and reects contemporary treatment concepts for
low back pain as reected in the highest quality clin-
ical literature available on this subject as of February
2016. The goals of the guideline recommendations are
to assist in delivering optimum, ecacious treatment
and functional recovery from nonspecic low back
pain.
Scope, Purpose and Intended User
This document was developed by the North American
Spine Society Evidence-Based Guideline Development
Committee with representation from stakeholder or-
ganizations as an educational tool to assist practi-
tioners who treat adult patients with nonspecic low
back pain. The goal is to provide a tool that assists
practitioners in improving the quality and eciency
of care delivered to these patients. The NASS Clinical
Guideline for the Diagnosis and Treatment of Low Back
Pain outlines a reasonable evaluation of patients with
nonspecic low back pain and outlines treatment op-
tions for adult patients with this condition.
THIS GUIDELINE DOES NOT REPRESENT A
“STANDARD OF CARE,” nor is it intended as a xed
treatment protocol. It is anticipated that there will be
patients who will require less or more treatment than
the average. It is also acknowledged that in atypical
cases, treatment falling outside this guideline will
sometimes be necessary. This guideline should not
be seen as prescribing the type, frequency or duration
of intervention. Treatment should be based on the
individual patient’s need and doctor’s professional
judgment and experience. This document is designed
to function as a guideline and should not be used as
the sole reason for denial of treatment and services.
This guideline is not intended to expand or restrict a
health care provider’s scope of practice or to supersede
applicable ethical standards or provisions of law.
Patient Population
The patient population for this guideline encompass-
es adults (18 years or older) with low back pain dened
as pain of musculoskeletal origin extending from the
lowest rib to the gluteal fold that may at times extend
as somatic referred pain into the thigh (above the
knee).
Considerations:WhyThisGuidelineIsDierent
andHowExclusionofLegPainImpactsthe
Recommendations
NASS typically writes clinical guidelines based on di-
agnosis. Due to demand and the expertise of NASS
spine care specialists, NASS, in this single instance,
has opted to address low back pain as a generalized
topic rather than a specic diagnosis or code. As a
multidisciplinary organization for spine care provid-
ers, NASS was uniquely positioned to provide specialty
expertise and a real-world perspective on multidisci-
plinary spine care. It is important to keep in mind that
“low back pain” is no more a diagnosis in the spine
eld than “chest pain” is for cardiology, but rather a
generalized patient complaint that can encompass a
variety of diagnoses.
Recommendations were developed based on a specic
denition, inclusion/exclusion criteria, and the re-
sulting literature which excluded leg pain below the
knee. Leg pain was excluded in order to address treat-
ment of nonspecic low back pain. For many sections,
the inclusion of leg pain in the literature search would
have included many specic causes of back pain, in-
cluding disc herniation and spondylolisthesis, that
would have made the focus on nonspecic low back
pain more dicult and less clear.
Without the inclusion of leg pain, these guideline rec-
ommendations address only a subset of low back pain
and its care. The inclusion and exclusion criteria used
resulted in the removal of multiple articles that may
have inuenced overall recommendations for a par-
ticular treatment or procedure. Evaluation of a par-
ticular treatment or procedure under dierent clinical
circumstances would necessitate a separate evalua-
tion of the evidence.

Diagnosis & Treatment of Low Back Pain | Introduction
7
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Due to the time needed to develop a guideline of this
size and breadth, some explanation is needed as to the
why or why not certain items can be found in the con-
tent.
Although opioids are addressed, it is in a limited
fashion. The opioid crisis as we know it today was
a phenomenon that reached crisis proportions af-
ter the guideline was already in development. In
the future, more substantial attention to this is-
sue will be merited.
This is the largest clinical guideline NASS has
ever undertaken and four years in the making.
There were 82 clinical questions and the literature
search resulted in more than 45,000 articles. Due
to the high volume of literature and the labor-
intensive nature of the review, literature search
dates are spread out in some instances (although
most were within the same month). In addition,
consideration should be given to the fact that
newer research has been published since the
literature searches have taken place.
This document is based on the evidence known at
the time of the literature review. However, evi-
dence can be incomplete or immature and recom-
mendations can change in the future where the
current evidence is thin, weak, or evolving. NASS’
future recommendations for research are a valu-
able tool when considering these areas.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Development Methodology and Process
8
Guideline Development
Methodology
Through objective evaluation of the evidence
and transparency in the process of making
recommendations, it is NASS’ goal to develop
evidence-based clinical practice guidelines for the
diagnosis and treatment of adult patients with various
spinal conditions. These guidelines are developed for
educational purposes to assist practitioners in their
clinical decision-making processes.
Multidisciplinary and Multi-Stakeholder
Collaboration
With the goal of ensuring the best possible care for
adult patients suering with spinal disorders, NASS
is committed to multidisciplinary involvement in the
process of guideline development. To this end, NASS
has ensured that representatives from research, both
operative and non-operative, medical, interventional
and surgical spine specialties have participated in the
development and review of NASS guidelines. To en-
sure broad-based representation on this topic, NASS
invited representatives from organizations whose
members are involved in the care of patients with low
back pain to serve on guideline work groups. A more
detailed description of stakeholder involvement is
included under the “Guideline Development Process”
on page 9.
Evidence Analysis Training of all Guideline
Developers
As a condition of participation, all developers com-
pleted NASS’ Fundamentals of Evidence-Based Med-
icine Training prior to participating in guideline de-
velopment. The training includes a series of readings
and exercises to prepare guideline developers for
systematically evaluating literature and developing
evidence-based guidelines. Participants are awarded
CME credit upon completion of the course.
DisclosureofPotentialConictsofInterest
All participants involved in guideline development
have disclosed potential conicts of interest to their
colleagues in accordance with NASS’ Disclosure Pol-
icy (https://www.spine.org/DisclosurePolicy) and
their potential conicts have been documented in the
Technical Report associated with this guideline. NASS
does not restrict involvement in guidelines based on
conicts as long as members provide full disclosure.
Individuals with a conict relevant to the subject
matter were asked to recuse themselves from delib-
eration. Participants have been asked to update their
disclosures regularly throughout the guideline devel-
opment process.
Levels of Evidence and Grades of
Recommendation
NASS has adopted standardized levels of evidence
(Appendix A) and grades of recommendation (Appen-
dix B) to assist practitioners in easily understanding
the strength of the evidence and recommendations
within the guidelines. The levels of evidence range
from Level I (high quality randomized controlled tri-
al) to Level V (expert consensus). Grades of recom-
mendation indicate the strength of the recommenda-
tions made in the guideline based on the quality of the
literature.
Grades of Recommendation:
A: Good evidence (Level I studies with consistent
ndings) for or against recommending interven-
tion.
B: Fair evidence (Level II or III studies with con-
sistent ndings) for or against recommending
intervention.
C: Poor quality evidence (Level IV or V studies) for
or against recommending intervention.
I: Insucient or conicting evidence not allowing
a recommendation for or against intervention.
Levels of evidence have very specic criteria and are
assigned to studies prior to developing recommenda-
tions. Recommendations are then graded based upon
the level of evidence. To better understand how levels
of evidence inform the grades of recommendation and
the standard nomenclature used within the recom-
mendations see Appendix C.
Guideline recommendations are written utilizing a
standard language that indicates the strength of the
recommendation. “A” recommendations indicate a
test or intervention is “recommended”; “B” recom-
mendations “suggest” a test or intervention and “C”
recommendations indicate a test or intervention “may
be considered” or “is an option.” “I” or “Insucient
Evidence” statements clearly indicate that “there is
insucient evidence to make a recommendation for
or against” a test or intervention. Work group con-
sensus statements clearly state that “in the absence of
reliable evidence, it is the work group’s opinion that”
a test or intervention may be appropriate.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Development Methodology and Process
9
In evaluating studies as to levels of evidence for this
guideline, the study design was interpreted as estab-
lishing only a potential level of evidence. As an ex-
ample, a therapeutic study designed as a randomized
controlled trial would be considered a potential Level
I study. The study would then be further analyzed as
to how well the study design was implemented and
signicant shortcomings in the execution of the study
would be used to downgrade the levels of evidence for
the study’s conclusions. In the example cited previ-
ously, reasons to downgrade the results of a potential
Level I randomized controlled trial to a Level II study
II would include, among other possibilities: an un-
derpowered study (patient sample too small, variance
too high), inadequate randomization or masking of
the group assignments and lack of validated outcome
measures.
In addition, a number of studies were reviewed sev-
eral times in answering dierent questions within
this guideline. How a given question was asked might
inuence how a study was evaluated and interpreted
as to its level of evidence in answering that particular
question. For example, a randomized controlled trial
reviewed to evaluate the dierences between the out-
comes of surgically treated versus untreated patients
with lumbar disc herniation with radiculopathy might
be a well-designed and implemented Level I ther-
apeutic study. This same study, however, might be
classied as providing Level II prognostic evidence if
the data for the untreated controls were extracted and
evaluated prognostically.
Guideline Development Process
Step 1: Recruitment of Guideline Members and
Involvement of Stakeholder Representatives
NASS Evidence-Based Guideline Development Com-
mittee members were solicited to participate in the
guideline development process. NASS also invited
stakeholder organizations who participate in the Spine
Summit, a multi-stakeholder meeting convened to
discuss and collaborate on projects that advance the
eld of spine care, to nominate representatives from
their respective organization to serve on the guideline
panel. Additional specialties not represented at the
Spine Summit were also solicited to participate in the
guideline to ensure broad representation of all spe-
cialties directly involved in the care of patients with
low back pain. In total, 62 volunteers participated in
this eort, including 11 stakeholder societies. Names
of guideline panelists are listed on page 2 and dis-
closures are listed in the Technical Report associated
with this document. The stakeholder groups can also
be found on page 3.
NASS spearheaded this guideline eort by providing
sta support and nancial support, including liter-
ature searches, full text articles, webinar/conference
capabilities and food and beverage and facility fees
for the in-person recommendation meetings. Stake-
holder organizations were asked to cover travel and
accommodation related expenses for their represen-
tative to attend any in-person meetings.
Step 2: Identication of Work Groups
The guideline panel consists of seven sections: Diag-
nosis, Imaging, Medical and Psychological Treatment,
Interventional Treatment, Physical Medicine and Re-
habilitation, Surgical Treatment and Cost-Utility.
Stakeholder societies were asked to rank their interest
in participating in each section and their representa-
tive was placed in their rst or second choice. Senior
and newer NASS Evidence-Based Guideline Develop-
ment members were equally placed in work groups to
ensure that groups with newer members were bal-
anced with members who have more guideline de-
velopment experience. Each work group consisted
of 7 to 11 members representing multi-disciplinary
backgrounds. The guideline panel includes represen-
tation from the elds of primary care, psychology,
neurosurgery, orthopedic surgery, physical medicine
and rehabilitation, physiatry, chiropractic care, phys-
ical therapy, anesthesiology, research, and radiology.
NASS believes that having multidisciplinary teams
involved in the guideline development process helps
to minimize inadvertent biases in evaluating the lit-
erature and formulating recommendations.
Step 3: Surveying Patients
To seek patient input to help inform the development
of clinical questions, NASS circulated an informal
Survey Monkey poll to better understand patients’
experiences with low back pain treatment. The sur-
vey link was circulated through various websites and
social media sites, including NASS’ Facebook and
Twitter pages; spine-health.com’s website, Face-
book group and blog; Low-Back Pain Patient Support
Group on Facebook; Lower Back Pain Management
Support Group on Facebook; and numerous Facebook
shares (of the survey link) on consumer and physician
proles. A total of 415 people opened the survey link,
including 413 who consented to participate in the sur-
vey and 2 who did not participate. The survey included
the following questions that allowed for check the box
and open-ended responses:

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Development Methodology and Process
10
1. What symptoms made you seek medical attention
for your current and/or any past episodes of low-
back pain?
2. Please identify the treatment(s) you received for
your current and/or any past episodes of low back
pain.
3. Based on your treatment experiences for your
current and any previous episodes of low back
pain, is there anything that you wish your health-
care provider shared with you before making your
decision to receive treatment?
4. What questions do you recommend that other pa-
tients with low back pain ask their providers when
seeking a diagnosis and treatment options for low
back pain?
Step 4: Identication of Clinical Questions
Framing questions to ask in the guideline is critical to
the guideline development process. Guideline partici-
pants were asked to submit a list of clinical questions
pertaining to their assigned section with the patient
survey as reference. Members were asked to use the
acronym “PICO” when drafting questions. “PICO”
serves to guide the development of clinical questions
that include all of the necessary components to build a
literature search: “P” for the patient/problem; “I” for
the intervention or indicator of interest (procedures,
therapies, diagnostic tests, exposure, etc.); “C” for
comparison and “O” for outcome of interest. The pro-
posed questions were compiled into a master list and
circulated to each member for review and comment.
Step 5: External Review of Clinical Question
Protocol
The draft list of clinical questions was made public-
ly available on the NASS website for a 4-week public
comment period from June 16, 2015 to July 14, 2015.
Additionally, stakeholders were invited through email
solicitations to comment on the draft questions. In
response, 27 individuals and organizations submit-
ted comment letters. Based on feedback, several re-
visions were incorporated in the guideline denition
and clinical question list. After the comment period,
an updated clinical question list with summarized
changes was posted to the NASS website and circulat-
ed to all public comment period reviewers.
Step 6: Identication of Search Terms and
Parameters
One of the most crucial elements of evidence analy-
sis is the comprehensive literature search. Thorough
assessment of the literature is the basis for the re-
view of existing evidence and the formulation of ev-
idence-based recommendations. In order to ensure
a thorough literature search, NASS has instituted a
Literature Search Protocol (Appendix D) which has
been followed to identify literature for evaluation in
guideline development. In keeping with the Literature
Search Protocol, work group members have identied
appropriate search terms and parameters to direct the
literature search. Specic search strategies, including
search terms, parameters and databases searched, are
documented in the Technical Report associated with
this document. The guideline denition and inclu-
sion/exclusion criteria are outlined on page 16.
Step 7: Completion of the Literature Search
Once each work group identied search terms/pa-
rameters, the literature search was implemented by
a medical/research librarian at InfoNOW at the Uni-
versity of Minnesota, consistent with the Literature
Search Protocol. Following these protocols ensures
that NASS recommendations (1) are based on a thor-
ough review of relevant literature; (2) are truly based
on a uniform, comprehensive search strategy; and (3)
represent the current best research evidence avail-
able. NASS maintains a search history in Endnote, for
future use or reference.
Step 8: Review of Search Results/Identication
of Literature to Review
Work group members reviewed all abstracts yielded
from the literature search and identied the litera-
ture they would review in order to address the clinical
questions, in accordance with the Literature Search
Protocol (Appendix D).
Step 9: Evidence Analysis
Members independently developed evidentiary ta-
bles summarizing study conclusions, identifying
strengths and weaknesses and assigning levels of ev-
idence. In order to systematically control for poten-
tial biases, two or more work group members have
reviewed each article selected and independently as-
signed levels of evidence to the literature using the
NASS levels of evidence. Any discrepancies in scoring
have been addressed by two or more reviewers. Final
ratings are completed at a nal meeting or web con-
ference of section workgroup members including the
section chair and a guideline co-chair. As a nal step
in the evidence analysis process, members have iden-
tied and documented gaps in the evidence to educate
guideline readers about where evidence is lacking and
help guide further needed research.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Development Methodology and Process
11
Step 10: Formulation of Evidence-Based
Recommendations and Incorporation of Expert
Consensus
Work groups held web-conferences and face-to-face
meetings to discuss the evidence-based answers to
the clinical questions, the grades of recommenda-
tions and the incorporation of expert consensus. Ex-
pert consensus was incorporated only where Level
I-IV evidence is insucient and the work group has
deemed that a recommendation is warranted. Trans-
parency in the incorporation of consensus is crucial
and all consensus-based recommendations made in
this guideline very clearly indicate that Level I-IV ev-
idence is insucient to support a recommendation
and that the recommendation is based only on expert
consensus.
Consensus Development Process
For recommendations with a consensus grading,
voting was conducted using a modication of the
nominal group technique in which each work group
member independently and anonymously ranked
a recommendation on a scale ranging from 1 (“ex-
tremely inappropriate”) to 9 (“extremely appropri-
ate”). Consensus was obtained when at least 80% of
work group members ranked the recommendation as
7, 8 or 9. When the 80% threshold was not attained,
up to three rounds of discussion and voting were held
to resolve disagreements. If disagreements were not
resolved after these rounds, no recommendation was
adopted. After the recommendations were estab-
lished, work group members developed the guideline
content, addressing the literature supporting the rec-
ommendations.
Step 11: Internal Review of Draft Guideline
Guideline sections were reviewed by the section work
groups that developed them. The full guideline draft
was submitted to the guideline co-chairs and NASS
Research Council for review and comment. Revisions
to recommendations were considered only when sub-
stantiated by a preponderance of appropriate level ev-
idence.
Step 12: External Review of Draft Guideline
Stakeholder societies were invited to comment on
the draft guideline during an external review period
June-August 2019. Nine of 11 stakeholder societies
provided comments. Revisions to recommendations
were considered only when substantiated by a pre-
ponderance of appropriate level evidence. Responses
to external comments are available in the technical
report associated with this guideline. Prior to publi-
cation, external stakeholders were invited to be listed
as participating or contributing societies.
Step 13: Submission for Board Approval
Once any evidence-based revisions were incorporat-
ed, the drafts were prepared for NASS Board of Di-
rectors review and approval. Edits and revisions to
recommendations and any other content were con-
sidered for incorporation only when substantiated by
a preponderance of appropriate level evidence.
Step 14: Submission for Publication
Following NASS Board approval, the guidelines were
slated for publication. No revisions were made after
submission for publication, but comments have been
and will be saved for the next iteration.
Step 15: Review and Revision Process
The guideline recommendations will be reviewed ev-
ery ve years by an EBM-trained multidisciplinary
team and revised as appropriate after review and as-
sessment of relevant literature published since the
development of this version of the guideline or the
guideline will be rescinded if it will not be updated.
Use of Acronyms
Throughout the guideline, readers will see many ac-
ronyms with which they may not be familiar. A glos-
sary of acronyms is available on page 14.
NomenclatureforMedical/Interventional
Treatment
Throughout the guideline, readers will see that what
has traditionally been referred to as “nonoperative,”
“nonsurgical,” or “conservative” care is now referred
to as “medical/interventional care.” The term medi-
cal/interventional is meant to encompass pharmaco-
logical treatment, physical therapy, exercise therapy,
manipulative therapy, modalities, various types of
external stimulators and injections.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Glossary & Acronyms
12
Glossary
Acute low back pain: Within rst 6 weeks of person’s
current LBP episode.
1
Chronic low back pain: Symptoms for current LBP
episode present for greater than 12 weeks.
2
General tness program: Exercise program not fo-
cused on specic muscle groups; by denition the goal
is to improve the overall general tness of the patient
by using a combination of aerobic conditioning with
stretching/strengthening of all major muscle groups.
Lumbar stabilization exercises: Focused on facilitat-
ing and strengthening specic muscles that directly
or indirectly control spinal joint function, especially
the abdominal, gluteal and spinal extensor muscle
groups.
Medical/interventional treatment: The term medi-
cal/interventional treatment is used in place of “non-
operative,” “conservative,” or “nonsurgical” treat-
ment. It encompasses pharmacological treatment,
physical therapy, exercise therapy, manipulative
therapy, modalities, various types of external stimu-
lators and injections.
Nonspecic low back pain: Pain in which no specic
cause or structure can be identied to account for the
patient’s perceived symptoms.
3
Radiculopathy: Dysfunction of a nerve root associated
with pain, sensory impairment, weakness, or dimin-
ished deep tendon reexes in a nerve root distribu-
tion.
4
Recurrent low back pain: Symptoms less than ½ the
days in a year occurring in multiple episodes.
5
Sciatica: Pain radiating down the leg below the knee in
the distribution of the sciatic nerve, suggesting nerve
root compromise due to mechanical pressure or in-
ammation. Sciatica is the most common symptom
of lumbar radiculopathy.
4
Specic low back pain: Pain that can be linked to a
disorder, disease, infection, injury, trauma, or struc-
tural deformity. A potential causal relationship can be
found between the diagnosis and the pain.
3
Spinal manipulative therapy (SMT): SMT is dened
as spinal manipulative therapy, manual therapy, mo-
bilization and high velocity thrusts.
Subacute low back pain: Symptoms for current LBP
episode present for 6-12 weeks.
1
Visceral diseases resulting in back pain: Pain second-
ary to diseases of the viscera. Examples: endometrio-
sis, prostatitis, aortic aneurysm.
5
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Glossary & Acronyms
13
Red Flag Conditions
4,6-7
History
Cancer
Unexplained weight loss
Immunosuppression
Intravenous drug use
Urinary tract infection
Fever
Signicant trauma relative to age
Bladder or bowel incontinence
Urinary retention (with overow incontinence)
PhysicalExamination
Saddle anesthesia
Loss of anal sphincter tone
Major motor weakness in lower extremities
Fever
Neurologic ndings persisting beyond one month
or progressively worsening
References
1. Frymoyer JW. Back pain and sciatica. N Engl J Med.
1988;318(5):291-300.
2. Von Kor M. Studying the natural history of back
pain. Spine. 1994;19(18 Suppl):2041S-6S.
3. Nordin M, Weiser S, van Doorn JW, Hiebert R. Non-
specic low back pain. In: Rom.W.N., editor. Envi-
ronmental and Occupational Medicine. 3rd ed. Phila-
delphia, PA: Lippincott-Raven Publishers; 1998. p.
947-56.
4. Chou R, Qaseem A, Snow V, et al. Diagnosis and
treatment of low back pain: a joint clinical practice
guideline from the American College of Physicians
and the American Pain Society. Ann Intern Med.
2007;147(7):478-491.
5. Deyo RA. Early diagnostic evaluation of low back
pain. J Gen Int Med. 1986;1(5):328-38.
6. Bigos SJ, Bowyer OR, Braen GR, Brown K, Deyo R,
Haldeman S, et al. Acute low back problems in adults.
Clinical practice guideline no. 14 (AHCPR publication
no. 95-0642). Rockville, Md.: U.S. Department of
Health and Human Services, Public Health Service,
Agency for Health Care Policy and Research, De-
cember 1994.
7. Forseen S, Corey A. Clinical decision support and
acute low back pain: evidence-based order sets. J
Am Coll Radiol. 2012;9(10):704-12

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Glossary & Acronyms
14
Acronyms
AAQ-II Acceptance and Action Questionnaire
ADS Allgemeine Depressions-Skala
ALIF Anterior lumbar interbody fusion
AM Active management
BDI Beck Depression Inventory
BDI-II Beck Depression inventory-II
BMI Body mass index
BMP Bone morphogenetic protein
BPI Brief Pain Inventory
CBA Cognitive behavioral approach
CBT Cognitive behavioral therapy
CCBT Contextual cognitive-behavioral
therapy
CEQ Cognitive Error Questionnaire
CLBP Chronic low back pain
CMDQ Common Mental Disorders
Questionnaire
COX-2 Cyclooxygenase-2
CPAQ Chronic Pain Acceptance
Questionnaire
CPR Clinical Prediction Rule
CT Computed tomography
DPQ Dallas Pain Questionnaire
DD Disc degeneration
DDS Descriptor Dierential Scale
DIS Diagnostic Interview Schedule Version
III-R
DSN Disc space narrowing
ED Emergency department
EEG Electroencephalogram
ESC End plate signal change
EMG Electromyography
ESI Epidural steroid injection
FABQ Fear Avoidance Beliefs Questionnaire
FD End of First Dose
FJ Facet joint
FJOA Facet joint osteoarthrosis
FJP Facet joint pain
FRI Function Rating Index
HADS Hospital Anxiety and Depression Scale
HADS-D Anxiety Hospital Anxiety and
Depression Scale
HILT High-intensity laser therapy
HIZ High intensity zone
HRQOL Health related quality of life
IAS Illness Attitude Scale
IDD Internal disc disruption
IDD Intervertebral Dierential Dynamics
IPQ-R Revised Illness Perception
Questionnaire
IDET Intradiscal electrothermal therapy
IDETA Intradiscal electrothermal anuloplasty
IV Intravenous
K-ODI Korean Oswestry Disability Index
K-SF-36 Korean Short Form-36
LBP Low back pain
MDR Multidisciplinary rehabilitation
MDT Mechanical diagnosis and therapy
MMPI Minnesota Multiphasic Personality
Inventory
MPQ McGill Pain Questionnaire
MR Magnetic resonance
MRI Magnetic resonance imaging
MSPQ Modied Somatic Perception
Questionnaire
MVK Modied Von Kor Scale
NPRS Numeric Pain Rating Scale
NRS Numerical rating scale
NSAIDS Nonsteroidal anti-inammatory drugs
ODI Oswestry Disability Index
ODQ Oswestry Low Back Pain Disability
Questionnaire
OLBPQ Oswestry Low Back Pain Disability
Questionnaire
PCS Pain Catastrophizing Scale
PDI Pain Disability Index
PGADS Patient Global Assessment of Disease
Status
PGAP Progressive Goal Attainment Program
PGI-I Patient’s Global Impressions of
Improvement
PHIC Modied Patient Global Impression of
Change
PLF Posterolateral fusion
PLIF Posterior lumbar interbody fusion
PRI Pain Rating Index
PRP Platelet-rich plasma
PSQI Pittsburgh Sleep Quality Index
PTSD Post-traumatic stress disorder
QALYs Quality-adjusted life years
QOL Quality of life
PENS Percutaneous electrical nerve
stimulation
RCT Randomized controlled trial
RMDQ Roland Morris Disability
Questionnaire
ROAD Research on Osteoarthritis/
Osteoporosis against Disability
RTW Return to work
SCL-90-R Symptom Checklist
SEBT Star excursion balance test
SF-36 Medical Outcome Study Short Form-
36
SFMPQ Short-Form McGill Pain Questionnaire

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Glossary & Acronyms
15
SI Sacroiliac
SIJ Sacroiliac joint
SIJI Sacroiliac joint injection
SIJP Sacroiliac joint pain
SIP Sickness Impact Prole
SJD Sacroiliac joint dysfunction
SMT Spinal manipulative therapy
SN Schmorl’s nodes
SPECT Single photon emission computerized
tomography
STAXI State-Trait Anger Expression
Inventory
TDR Total disc replacement
TENS Transcutaneous electrical nerve
stimulation
TLIF Transforaminal lumbar interbody
fusion
TSE Transcutaneous spinal
electroanalgesia
TSK Tampa Scale for Kinesiophobia
TTM Transtheoretical Model
UK BEAM UK Back pain Exercise And
Manipulation (UK BEAM)
VAS Visual analog scale
VNS Visual Numeric Pain Scale
VO Vertebral osteophytes
VRS Verbal rating scale
ZDS Zung Depression Scale

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain |
16
Denition & Inclusion/Exclusion Criteria
Denition
Low back pain is dened as pain of musculoskeletal
origin extending from the lowest rib to the gluteal
fold that may at times extend as somatic referred pain
into the thigh (above the knee).
Inclusion Criteria
1. Adult patients aged 18 and older
2. Patients with low back pain limited to somatic re-
ferred pain/non-radicular pain limited to above
the knee only
Exclusion Criteria
1. Patients less than 18 years of age
2. Low back pain due to:
a. Tumor
b. Infection
c. Metabolic disease
d. Inammatory arthritis
e. Fracture
3. Patients with a diagnosed deformity, including
spondylolisthesis, spondylolysis and scoliosis
4. Pain experienced below the knee
5. Extra-spinal conditions (ie, visceral, vascular,
genito-urinary)
6. Patients who have undergone prior lumbar sur-
gery
7. Presence of neurological decit
8. Back pain that is associated with widespread
multi-site pain (>2 sites)
9. Pregnancy
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
17
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
Clinical Question Guideline Recommendation
See recommendation sections for supporting text
A=Recommended; B=Suggested; C=May be considered; I=Insucient or
Conicting Evidence
Diagnosis
Diagnosis Question 1. In patients
with low back pain, are there spe-
cic history or physical examina-
tion ndings that would indicate
the structure causing pain and,
therefore, guide treatment?
a. Vertebral body
b. Intervertebral disc
c. Zygapophyseal joint
d. Posterior elements
e. Sacroiliac joint
f. Muscle/tendon
g. Central sensitization
There is insucient evidence to make a recommendation for or against the
use of innominate kinematics for the assessment of sacroiliac joint pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of pain localization in predicting response to a diagnostic injection.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
assessment of centralization or peripheralization for the prediction of discog-
raphy results.
Grade of Recommendation: I
Diagnosis Question 2. In patients
with low back pain, are there histo-
ry or physical examination ndings
that would serve as predictors for
the recurrence of low back pain?
There is insucient evidence to indicate that body mass index (BMI) is a po-
tential predictor of a recurrence of low back pain.
Grade of Recommendation: I
It is suggested that history of low back pain is a potential predictor of a recur-
rence of low back pain.
Grade of Recommendation: B

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
18
Diagnosis Question 3. In patients
with acute low back pain, are there
history or physical examination
ndings that would predict that
an episode will resolve within one
month?
Diagnosis Question 6. What are
the patient characteristics that
increase or decrease the risk of
developing chronic low back pain
after an acute episode?
Diagnosis Question 9. Does a psy-
chological evaluation assist with
identifying patients with low back
pain who are at risk for developing
chronic pain or disability?
The work group considered these
questions together as the vast ma-
jority of the literature evaluating the
conversion from acute to chronic
pain combined various demograph-
ic, social, psychological and physical
examination ndings in predictive
models.
It is recommended that psychosocial factors and workplace factors be as-
sessed when counseling patients regarding the risk of conversion from acute
to chronic low back pain.
Grade of Recommendation: A
It is recommended that psychosocial factors be used as prognostic factors
for return to work following an episode of acute low back pain.
Grade of Recommendation: A
It is recommended that pain severity and functional impairment be used to
stratify risk of conversion from acute to chronic low back pain.
Grade of Recommendation: A
It is suggested that prior episodes of low back pain be considered a prognos-
tic factor for the conversion from acute to chronic low back pain.
Grade of Recommendation: B
There is insucient evidence to assess sleep quality as a prognostic variable
to predict recovery from acute low back pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of smoking and/or obesity as prognostic factors for the conversion from
acute to chronic low back pain.
Grade of Recommendation: I
Diagnosis Question 4. In patients
with low back pain, what histo-
ry and/or physical examination
ndings are useful in determining
if the cause is nonstructural in
nature and, therefore, guide treat-
ment?
A nonstructural cause of low back pain may be considered in patients with
diuse low back pain and tenderness.
Grade of Recommendation: C
There is insucient evidence to make a recommendation for or against the
use of fear avoidance behavior to determine the likelihood of a structural
cause of low back pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
presence of diuse back tenderness for the prediction of the presence of
disc degeneration on radiographs.
Grade of Recommendation: I
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
19
Diagnosis Question 5. In patients
with low back pain, what elements
of the patient’s history and nd-
ings from the physical examination
would suggest the need for diag-
nostic laboratory studies?
There is insucient evidence to make a recommendation for or against
obtaining laboratory tests to assess for inammatory disease in patients with
sacroiliac joint pain.
Grade of Recommendation: I
Diagnosis Question 7. In patients
with low back pain, are there
specic ndings on a pain diagram
that help dierentiate the struc-
ture which is causing pain?
Diagnosis Question 8. Are there
assessment tools or question-
naires that can help identify the
cause of acute, subacute or chron-
ic low back pain?
A systematic review of the literature yielded no studies to adequately ad-
dress these questions.
Diagnosis Question 10. Are there
history and physical examination
ndings that would warrant ob-
taining advanced imaging studies?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Work Group Consensus Statement:
In the absence of reliable evidence supporting an absolute indication for
advanced imaging based upon history and physical examination in the specif-
ically-dened patient population, it is the work group’s opinion that, in pa-
tients with severe and intractable pain syndromes who have failed medical/
interventional treatment, advanced imaging may be indicated. Subgroups of
patients have been shown to have a higher or lower incidence of radiograph-
ic abnormalities based upon acuity of low back pain, tenderness to palpation
and provocation maneuvers; however, the utility of these ndings in guiding
treatment is not clear.
Imaging
Imaging Question 1. What is the
association between low back pain
and spondylosis on routine radiog-
raphy?
There is insucient evidence to make a recommendation for or against an
association between low back pain and spondylosis using routine radiogra-
phy.
Grade of Recommendation: I
Imaging Question 2. Is there evi-
dence to support the use of com-
puted tomography (CT) or mag-
netic resonance imaging (MRI) for
the evaluation of low back pain in
the absence of x-ray/radiographic
abnormality?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Imaging Question 3. In patients
with low back pain, does duration
of symptoms correlate with abnor-
mal ndings on imaging?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
20
Imaging Question 4. What is the
optimal imaging protocol that
should be used in the setting of
low back pain?
4a. Are unique MRI sequences con-
sidered preferential or optimal?
There is insucient evidence that unique magnetic resonance imaging (MRI)
sequences can be considered preferential or optimal.
Grade of Recommendation: I
4b. What is the history and clinical
presentation that suggests the use
of contrast enhanced imaging in
patients with low back pain?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
4c. Is there evidence to support im-
aging the lumbar spine in an oblique
plane?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
4d. What is the value of exion/
extension lms in evaluating lower
back pain?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Imaging Question 5. In the ab-
sence of red ags, what are the
imaging (x-ray, CT or MRI) recom-
mendations for patients with acute
or chronic low back pain?
There is insucient evidence to make a recommendation for or against ob-
taining imaging in the absence of red ags.
Grade of Recommendation: I
Imaging Question 6. Are there im-
aging ndings that correlate with
the presence of low back pain?
There is insucient evidence for or against imaging ndings correlating with
the presence of low back pain.
Grade of Recommendation: I
Imaging Question 7. Are there
imaging ndings that contribute
to decision-making by health care
providers to guide treatment?
There is insucient evidence to determine whether imaging ndings contrib-
ute to decision-making by health care providers to guide treatment.
Grade of Recommendation: I
Medical and Psychological Treatment
Med/Psych Question 1. Is smoking
cessation eective in decreasing
the frequency of low back pain
episodes?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
21
Med/Psych Question 2. In patients
with low back pain, is pharmaco-
logical treatment eective in de-
creasing duration of pain, decreas-
ing intensity of pain, increasing
functional outcomes of treatment
and improving the return-to-work
rate?
Versus:
a. No treatment
i. Risks
ii. Complications
b. Cognitive behavioral therapy
(CBT) and/or psychosocial inter-
vention alone
c. Patient education alone
There is insucient evidence to make a recommendation for or against the
use of anticonvulsants for the treatment of low back pain.
Grade of Recommendation: I
Antidepressants are not recommended for the treatment of low back pain.
Grade of Recommendation: A
There is insucient evidence to make a recommendation for or against the
use of Vitamin D for the treatment of low back pain.
Grade of Recommendation: I
Non-selective NSAIDs are suggested for the treatment of low back pain.
Grade of Recommendation: B
There is insucient evidence to make a recommendation for or against the
use of selective NSAIDs for the treatment of low back pain.
Grade of Recommendation: I
It is suggested that the use of oral or IV steroids is not eective for the treat-
ment of low back pain.
Grade of Recommendation: B
It is suggested that the use of opioid pain medications should be cautiously
limited and restricted to short duration for the treatment of low back pain.
Grade of Recommendation: B
Med/Psych Question 3. In pa-
tients with low back pain, is topical
treatment (eg, cream or gel) ef-
fective in decreasing duration of
pain, decreasing intensity of pain,
increasing functional outcomes
of treatment and improving the
return-to-work rate?
There is insucient evidence to make a recommendation for or against the
use of lidocaine patch for the treatment of low back pain.
Grade of Recommendation: I
Topical capsicum is recommended as an eective treatment for low back
pain on a short-term basis (3 months or less).
Grade of Recommendation: A
Med/Psych Question 4. Following
treatment for low back pain, do
patients with healthy sleep habits
experience decreased duration of
pain, decreased intensity of pain,
increased functional outcomes
and improved return-to-work rates
compared to patients with poor
sleeping habits?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
22
Med/Psych Question 5. In patients
with low back pain, is cognitive
behavioral therapy (CBT) and/or
psychosocial intervention and/or
neuroscience education eective
in decreasing duration of pain, de-
creasing intensity of pain, increas-
ing functional outcomes, decreas-
ing anxiety and/or depression and
improving return-to-work rate?
Cognitive behavioral therapy is recommended in combination with physical
therapy, as compared with physical therapy alone, to improve pain levels in
patients with low back pain over 12 months.
Grade of Recommendation: A
Cognitive behavioral therapy in combination with physical therapy, compared
to physical therapy alone, is suggested to improve functional outcomes (dis-
ability) and return to work in patients with low back pain.
Grade of Recommendation: B
There is conicting evidence to make a recommendation for or against cogni-
tive behavioral therapy for improving depression or anxiety in patients with
low back pain.
Grade of Recommendation: I
Med/Psych Question 6. In pa-
tients with low back pain, does
the timing of cognitive behavioral
therapy (CBT) and/ or psychosocial
intervention and/or neuroscience
education aect duration of pain,
intensity of pain, functional out-
comes, anxiety, depression and
return-to-work status?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Med/Psych Question 7. In pa-
tients undergoing interventional
or surgical treatment for low back
pain, does the addition of cogni-
tive behavioral therapy (CBT) and/
or psychosocial intervention add
incremental benet?
There is insucient evidence to make a recommendation for or against the
addition of cognitive behavioral therapy or psychosocial intervention for pa-
tients undergoing interventional or surgical treatment for low back pain and
whether it would provide incremental benet.
Grade of Recommendation: I
Med/Psych Question 8. Does
educating a patient about low back
pain improve treatment compli-
ance and outcomes, including
duration of pain, intensity of pain,
functional outcomes, anxiety,
depression and return-to-work
status?
There is conicting evidence to make a recommendation for or against the
use of patient education to improve treatment compliance and outcomes,
including duration of pain, intensity of pain, functional outcomes, anxiety,
depression and return to work status.
Grade of Recommendation: I
Med/Psych Question 9. In patients
undergoing treatment for low
back pain, what is the eective-
ness of interventions that address
fear-avoidance behaviors?
Treatments targeting fear avoidance combined with physical therapy are
recommended compared to physical therapy alone to improve low back pain
in the rst six months.
Grade of Recommendation: A
Med/Psych Question 10. Is active
treatment (pharmacological or
psychotherapeutic) of anxiety and
depression eective in decreasing
low back pain?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
23
Med/Psych Question 11. What are
the psychological factors inuenc-
ing outcomes, including duration
of pain, intensity of pain, function-
al outcomes and return-to-work
status, of low back pain treatment?
It is suggested that kinesiophobia is a negative prognostic factor for predict-
ing response to low back pain treatment.
Grade of Recommendation: B
Med/Psych Question 12. In pa-
tients with low back pain, what
psychosocial/cognitive/emotional
or other assessments should be
utilized to establish an accurate
diagnosis?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Med/Psych Question 13. Does
nutrition (other than weight reduc-
tion) inuence the frequency of
low back pain episodes?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Physical Medicine and Rehabilitation
PM&R Question 1. In patients
undergoing treatment for low back
pain, what is the eectiveness of
the following in decreasing the
duration of pain, decreasing inten-
sity of pain, increasing functional
outcomes and improving return-
to-work status, as compared with
natural history plus or minus
medication:
a. Acute vs subacute vs chronic
i. Patient education and self-
directed exercise program
Back school is recommended to provide improvements in pain and function
when compared with general medical care, modality care or a simple hand-
out at 6-12 months’ follow-up for chronic low back pain.
Grade of Recommendation: A
There is insucient evidence that outcomes from a home-based exercise pro-
gram are dierent than no care.
Grade of Recommendation: I
There is insucient evidence that a self-directed McKenzie exercise program for
acute low back pain results in dierent outcomes compared to usual medical
care.
Grade of Recommendation: I
There is insucient evidence that a monitored pedometer-based exercise
program with web-based feedback provides any improvement over pedome-
ter instruction alone.
Grade of Recommendation: I
ii. Physical agents
a. (eg, heat, cold)
It is suggested that the use of heat for acute low back pain results in short-
term improvements in pain.
Grade of Recommendation: B
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
24
b. (eg, ultrasound)
It is suggested that ultrasound does not improve functional outcomes in
patients with chronic low back pain.
Grade of Recommendation: B
There is conflicting evidence that ultrasound provides immediate pain relief
in patients with chronic low back pain.
Grade of Recommendation: I
c. (eg, TENS)
There is conicng evidence that transcutaneous electrical nerve smulaon
(TENS) results in improvement in pain or funcon at short- to medium-term
follow-up.
Grade of Recommendation: I
d. (eg, laser- cutaneous
stimulation for pur-
pose of pain modula-
tion)
Laser acupuncture provides no short-term or medium-term benet over
sham treatment for patients with chronic low back pain.
Grade or Recommendation: A
It is suggested that the combination of laser therapy (low-level or high level)
with exercise provides better short-term relief of pain than either exercise or
laser therapy alone.
Grade of Recommendation: B
There is conicting evidence that the combination of laser therapy with
exercise provides better short-term improvement in function compared to
exercise or laser therapy alone.
Grade of Recommendation: I
It is suggested that there is no short-term benet of laser therapy (low-level
or high level) when compared with exercise alone.
Grade of Recommendation: B
e. (eg, traction) In patients with subacute or chronic low back pain, traction is not recom-
mended to provide clinically signicant improvements in pain or function.
Grade of Recommendation: A
f. (eg, dry needling) There is insucient evidence for or against the use of dry needling as a treat-
ment option for patients with chronic low back pain.
Grade of Recommendation: I
g. (eg, electrical stimula-
tion)
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
25
iii. Acupuncture In patients with low back pain, there is conicting evidence that acupuncture
provides improvements in pain and function as compared to sham acupunc-
ture.
Grade of Recommendation: I
In patients with chronic low back pain, addition of acupuncture to usual care
is recommended for short-term improvement of pain and function com-
pared to usual care alone.
Grade of Recommendation: A
There is insucient evidence to draw conclusions regarding the comparative
eectiveness of acupuncture techniques.
Grade of Recommendation: I
iv. Bracing
— Lumbosacral brace
— Sacroiliac brace
There is conicting evidence that bracing results in improvements in pain
and function in patients with subacute low back pain.
Grade of Recommendation: I
v. SMT For patients with acute or chronic low back pain, spinal manipulative therapy
(SMT) is an option to improve pain and function.
Grade of Recommendation: C
For patients with acute low back pain, spinal manipulative therapy (SMT) re-
sults in similar outcomes to no treatment, medication or modalities. Periodi-
cally, short-term improvement is statistically better, but clinical signicance is
uncertain.
Grade of Recommendation: A
For patients with chronic low back pain, there is conicting evidence that
outcomes for spinal manipulative therapy (SMT) are clinically dierent than
no treatment, medication or modalities.
Grade of Recommendation: I
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
26
vi. Exercise/physical therapy ver-
sus or plus massage
There is insucient evidence to determine the ecacy of acupressure com-
pared to a standardized multimodal physical therapy.
Grade of Recommendation: I
In the long term, it is suggested that the addition of massage to an exercise
program provides no benet when compared to an exercise program alone.
Grade of Recommendation: B
There is insucient evidence that the addition of massage to an exercise
program provides short-term relief of pain.
Grade of Recommendation: I
vii. Active stabilization exercise There is insucient evidence to make a recommendation for or against lum-
bar stabilization in patients with chronic low back pain.
Grade of Recommendation: I
viii. McKenzie exercise [includes
directional preference, centraliza-
tion and mechanical diagnosis and
therapy (MDT)]
McKenzie method is an option for the treatment of chronic low back pain.
Grade of Recommendation: C
There is insucient evidence that McKenzie method results in dierent out-
comes when compared to a dynamic strengthening program for the treat-
ment of chronic low back pain.
Grade of Recommendation: I
There is insucient evidence that McKenzie method is better or worse than
back school for the treatment of chronic low back pain.
Grade of Recommendation: I
ix. Yoga It is suggested that, in patients with mild chronic low back pain, yoga may
oer medium-term improvements in pain and function compared to usual
care, although these improvements are not clinically meaningful due to low
baseline pain/disability.
Grade of Recommendation: B
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
27
x. Aerobic exercise Aerobic exercise is recommended to improve pain, disability and mental
health in patients with nonspecic low back pain at short-term follow-up.
Grade of Recommendation: A
There is insucient evidence that aerobic exercise improves pain, disability
and mental health in patients with nonspecic low back pain at long-term
follow-up.
Grade of Recommendation: I
xi. Work hardening or conditioning In patients with low back pain, work hardening may be considered to im-
prove return to work.
Grade of Recommendation: C
There is insucient evidence that work hardening is dierent than an active
therapeutic exercise program or guideline-based physical therapy.
Grade of Recommendation: I
PM&R Question 2. In patients
undergoing treatment for low
back pain, what is the appropriate
timing, frequency and duration of
treatment with:
Acute vs. subacute vs. chronic
i. Patient education and self- di-
rected exercise program
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
ii. Physical agents
a. (eg, heat, cold)
b. (eg, ultrasound)
c. (eg, TENS)
d. (eg, laser- cutane-
ous stimulation
for purpose of pain
modulation)
e. (eg, traction)
f. (eg, dry needling)
g. (eg, electrical stimula-
tion)
iii. Acupuncture
iv. Bracing
— Lumbosacral brace
— Sacroiliac brace
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
28
v. SMT There is insucient evidence to determine whether 12 to 18 visits of spinal
manipulative therapy (SMT) results in better outcomes than 6 visits for the
treatment of low back pain.
Grade of Recommendation: I
vi. Exercise/Physical Therapy ver-
sus or plus massage
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
vii. Active stabilization exercise
viii. McKenzie exercise [includes
directional preference, centraliza-
tion and mechanical diagnosis and
therapy (MDT)]
ix. Yoga
x. Aerobic exercise
xi. Work hardening or conditioning
PM&R Question 3. Are there spe-
cic patient or treatment char-
acteristics that predict improved
duration of pain, intensity of pain,
functional outcomes and return-
to-work status with SMT following
an episode of low back pain?
There is conicting evidence that symptoms above the knee, low fear avoid-
ance questionnaire score, at least one hypo-mobile segment, and greater
than 35° of internal rotation of the hip are predictive of responding to spinal
manipulative therapy (SMT) for patients with acute low back pain.
Grade of Recommendation: I
There is insucient evidence that hyper- or hypo-mobility, patient age,
strains and sprains, instability, severe aective distress, relationship with
healthcare provider, use of thrust vs nonthrust techniques, pretreatment
psychological or socioeconomic status, or number of visits are predictive
factors of response to spinal manipulative therapy (SMT).
Grade of Recommendation: I
PM&R Question 4. In patients
undergoing treatment for low back
pain, what are outcomes, includ-
ing duration of pain, intensity of
pain, functional outcomes and
return-to-work status, for exercise
therapy alone versus exercise with
cognitive behavioral therapy (CBT)?
There is conicting evidence that addition of cognitive behavioral therapy
(CBT) to an exercise program results in signicant improvement in pain and
function compared to exercise alone in patients with chronic low back pain.
Grade of Recommendation: I
PM&R Question 5. In patients
undergoing treatment for low back
pain, what are outcomes, including
duration of pain, intensity of pain,
functional outcomes and return-
to-work status, for a lumbar stabi-
lization exercise program versus a
general tness program?
It is suggested that a specic stabilization exercise program is equivalent to a
general exercise program.
Grade of Recommendation: B

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
29
PM&R Question 6. In patients
undergoing treatment for low back
pain, what are outcomes, including
duration of pain, intensity of pain,
functional outcomes and return-
to-work status, for SMT versus
SMT plus active exercise?
It is suggested that the addition of exercise to spinal manipulative therapy
(SMT) results in similar outcomes to SMT alone.
Grade of Recommendation: B
PM&R Question 7. In patients
undergoing treatment for low back
pain, what are the outcomes, in-
cluding duration of pain, intensity
of pain, functional outcomes and
return-to-work status, for bed rest
versus active exercise?
It is suggested that, for patients with acute low back pain, those that exercise
more at baseline and use exercise to facilitate recovery are predicted to have
better functional outcomes over time than patients who do not exercise or
use bed rest to help with recovery.
Grade of Recommendation: B
For patients with acute low back pain, it is suggested that advice to remain
active within limits of pain compared to short periods of bed rest from 3 to 7
days all result in similar outcomes in pain and function at short- and medi-
um-term follow-up.
Grade of Recommendation: B
Work Group Consensus Statement: In the absence of reliable evidence for
patients with nonspecic back pain, based on abundant data for other spinal
disorders that result in back pain, it is the work group’s opinion that remain-
ing active is preferred and likely results in better short-term outcomes than
does bed rest.
PM&R Question 8. In patients
with low back pain, does a regular
exercise program (or presurgical
intervention with exercise, PT,
education) prior to lumbar surgery
decrease the duration of pain,
decrease the intensity of pain, in-
crease the functional outcomes of
treatment and improve the return-
to-work rate compared to those
who don’t exercise?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
PM&R Question 9. In patients with
low back pain, does exercise treat-
ment after epidural steroid injec-
tions/spinal interventions decrease
the duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate
compared to injections alone?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
30
PM&R Question 10. Following
surgery for low back pain, are out-
comes, including duration of pain,
intensity of pain, functional out-
comes and return-to-work status,
improved with a formal exercise/
rehabilitation program versus
home instruction plus or minus
self-directed exercise program
alone?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
PM&R Question 11. Can a clinical
prediction rule determine appro-
priate indications and predict out-
comes, including duration of pain,
intensity of pain, functional out-
comes and return-to-work status,
for exercise for low back pain?
There is insucient evidence to provide any reliable predictors of outcomes
to an exercise program for the treatment of either acute or chronic low back
pain.
Grade of Recommendation: I
Interventional Treatment
Interventional Question 1. In
patients with low back pain, do
uoroscopically-guided epidural
steroid injections decrease the
duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the
use of caudal epidural steroid injections in patients with low back pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of interlaminar epidural steroid injections in patients with low back pain.
Grade of Recommendation: I
Interventional Question 2.
When evaluating uoroscopically-
guided intra-articular lumbar facet
joint injections in patients with
acute or chronic low back pain:
a. What is the diagnostic utility of
this procedure?
b. From a therapeutic standpoint,
does this procedure decrease the
duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the
use of patient-reported reproduction of pain during a zygapophyseal joint
injection as a predictor of response to dual diagnostic blocks.
Grade of Recommendation: I
In patients selected for facet joint procedures using diagnostic criteria of
physical exam and a response to a single diagnostic intra-articular injection
with 50% relief, it is suggested that intra-articular injection of steroids pro-
vides no clinically meaningful improvement at 6 months.
Grade of Recommendation: B
In patients selected for facet joint procedures using diagnostic criteria of physical
exam and a response to a single diagnostic intra-articular injection with 50% re-
lief, there is insucient evidence to make a recommendation for or against the
use of radiofrequency neurotomy or periarticular phenol injections.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of steroid injections into the zygapophyseal joint in patients with chronic
back pain and a physical exam suggestive of facet-mediated pain.
Grade of Recommendation: I
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
31
Interventional Question 3. In
patients with low back pain, do
medial branch blocks have a role
in dening treatment for low back
pain?
a. Does duration of pain, intensity
of pain, functional outcomes and
return-to-work status vary when
candidates for neurotomy are de-
termined by single vs comparative
medial branch blocks?
b. Is there a threshold for the
magnitude of relief from diagnos-
tic facet nerve blocks that predict
outcomes to neurotomy?
c. Does duration of pain, intensity
of pain, functional outcomes and
return-to-work status vary when
candidates for neurotomy are de-
termined by diagnostic facet nerve
blocks vs. intra-articular facet joint
injections?
d. Is there a therapeutic utility of
medial branch blocks?
e. Does technical accuracy of
medial branch blocks (eg, contrast
use) aects its validity and eec-
tiveness of subsequent neuroto-
my?
There is insucient evidence to make a recommendation for or against the
use of SPECT imaging in the diagnosis of zygapophyseal joint pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of uncontrolled medial branch blocks vs. pericapsular blocks for the di-
agnosis of zygapophyseal joint pain based on the outcomes of medial branch
nerves cryoablation.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of cryodenervation for the treatment of zygapophyseal joint pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of a 50% reduction in pain following medial branch blockade for the diag-
nosis of zygapophyseal joint pain.
Grade of Recommendation: I
Thermal radiofrequency ablation is suggested as a treatment for patients
with low back pain from the zygapophyseal joints. The outcomes of this
procedure become more reliable when more stringent diagnostic criteria are
used. The relief from these ablations is durable for at least six months follow-
ing the procedure.
Grade of Recommendation: B
Interventional Question 4. In
patients with low back pain due
to lumbar facet joint arthropa-
thy, does uoroscopically-guided
neurotomy decrease the duration
of pain, decrease the intensity of
pain, increase the functional out-
comes of treatment and improve
the return-to-work rate?
Thermal radiofrequency ablation is suggested as a treatment for patients
with low back pain from the zygapophyseal joints. The outcomes of this
procedure become more reliable when more stringent diagnostic criteria are
used. The relief from these ablations is durable for at least six months follow-
ing the procedure.
Grade of Recommendation: B
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
32
Interventional Question 5. In
patients with low back pain, do
uoroscopically-guided sacroiliac
joint injections (SIJI) decrease the
duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
a. Does duration of pain, intensity
of pain, functional outcomes and
return-to-work status vary when
candidates for neurotomy are
determined by single vs compara-
tive SIJI?
b. Is there a benet to performing
lateral branch blocks as compared
with intra-articular diagnostic in-
jections as a predictor to response
to lateral branch neurotomy?
c. Is there a threshold for the
magnitude of relief from diagnos-
tic SIJI that predict improvement in
duration of pain, intensity of pain,
functional outcomes and return-to-
work status from SIJ neurotomy?
Intra-articular steroid joint injections may be considered in patients with
suspected SI joint pain
Grade of Recommendation: C
Interventional Question 6. In pa-
tients with pelvic posterior girdle
pain relieved temporarily by image
guided SIJ injections or lateral
branch blocks, does lateral branch
neurotomy decrease the duration
of pain, decrease the intensity of
pain, increase the functional out-
comes of treatment and improve
the return-to-work rate?
Cooled radiofrequency ablation of the sacral lateral branch nerves and
dorsal ramus of L5 may be considered in patients with sacroiliac joint pain
diagnosed with dual diagnostic blocks.
Grade of Recommendation: C
Interventional Question 7. In
patients with low back pain, does
spinal cord stimulation decrease
the duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the
use of spinal cord stimulation as a treatment for low back pain.
Grade of Recommendation: I
Interventional Question 8. In
patients with low back pain, does
continuous delivery of intrathecal
opioids decrease the duration of
pain, decrease the intensity of
pain, increase the functional out-
comes of treatment and improve
the return-to-work rate and are
there risks associated with its use?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
33
Interventional Question 9. In
patients with low back pain, is
provocative lumbar discography
more accurate than other diag-
nostic modalities in identifying the
disc as a source of pain?
There is high-level evidence that provocative discography without mano-
metric measurements correlates with pain reproduction in the presence of
moderate to severe disc degeneration on MRI/CT discography.
Grade of Recommendation: A
There is high-level evidence that provocative discography without manomet-
ric pressure measurements correlates with the presence of endplate abnor-
malities on MRI imaging.
Grade of Recommendation: A
Bony vibration provocation may be considered to correlate with the presence
of pain in patients who have pain on provocation discography without mano-
metric pressure measurements. There is no correlation with the segmental
level of pain.
Grade of Recommendation: C
There is insucient evidence to make a recommendation for or against the
use of axial loaded magnetic resonance imaging (MRI) for the diagnosis of
low back pain.
Grade of Recommendation: I
There is conicting evidence that pressure controlled provocative discogra-
phy correlates with nuclear T2 signal intensity on magnetic resonance imag-
ing (MRI) in patients with low back pain.
Grade of Recommendation: I
There is conicting evidence that provocative discography without manomet-
ric pressure measurements correlates with the presence of a high-intensity
zone (HIZ) on MRI imaging.
Grade of Recommendation: I
Interventional Question 10. In
patients with low back pain, is an-
esthetic lumbar discography more
accurate than other diagnostic
modalities in identifying the disc as
a source of pain?
There is insucient evidence to make a recommendation for or against the
use of anesthetic discography.
Grade of Recommendation: I

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
34
Interventional Question 11. In
patients with low back pain, does
intradiscal injection decrease the
duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
Intradiscal steroids are suggested to provide short-term improvements in
pain and function in patients with Modic changes.
Grade of Recommendation: B
There is insucient evidence that intradiscal steroids provide improvements
in pain or function in patients with discogenic low back pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of intradiscal bone marrow concentrate in patients with discogenic low
back pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of intradiscal platelet rich plasma in patients with discogenic low back
pain.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the
use of intradiscal Methylene Blue in patients with discogenic low back pain.
Grade of Recommendation: I
Interventional Question 12. In
patients with low back pain, does
intradiscal electrothermal ther-
apy or biacuplasty decrease the
duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
Intradiscal electrothermal annuloplasty is suggested to provide improve-
ments in pain and function at up to two years. This treatment is limited in its
eectiveness with roughly 40-50% of patients receiving a 50% reduction in
pain.
Grade of Recommendation: B
Biacuplasty is an option to produce clinically and statistically signicant im-
provements in pain at 6 months in patients with discogenic low back pain.
Grade of Recommendation: C
There is insucient evidence to make a recommendation for or against the
use of percutaneous intradiscal radiofrequency thermocoagulation.
Grade of Recommendation: I
Interventional Question 13. In
patients with low back pain, do
trigger point injections decrease
the duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the
use of trigger point injections in the treatment of low back pain. The type of
injectate does not inuence outcomes.
Grade of Recommendation: I
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
35
Surgical Treatment
Surgical Question 1. In patients
with low back pain, does surgical
treatment vs medical/interven-
tional treatment alone decrease
the duration of pain, decrease the
intensity of pain, increase the func-
tional outcomes of treatment and
improve the return-to-work rate?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 2. In patients
with low back pain, are there
predictive factors which determine
the benet of initial treatment with
surgical intervention versus initial
medical/interventional treatment?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 3. In patients
undergoing fusion surgery for low
back pain, which fusion technique
results in the best outcomes for
the following: decreased duration
of pain, decreased intensity of
pain, increased functional out-
comes of treatment and improved
return-to-work rate?
a. Posterolateral fusion without
internal xation vs
b. Posterolateral transverse fusion
with internal xation vs
c. Stand-alone (anterior) interbody
fusion vs
d. Transforaminal lumbar inter-
body fusion (TLIF) or posterior
lumbar interbody fusion (PLIF) vs
e. Circumferential fusion (anterior
interbody, lateral techniques)
There is insucient evidence to make a recommendation for or against a
particular fusion technique for the treatment of low back pain.
Grade of Recommendation: I
Surgical Question 4. In patients
undergoing fusion surgery for low
back pain, are clinical outcomes,
including duration of pain, inten-
sity of pain, functional outcomes
and return-to-work status, dier-
ent for multi-level fusions vs single
level fusions?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 5. In patients
undergoing fusion surgery for
low back pain, does radiograph-
ic evidence of fusion correlate
with decreased duration of pain,
decreased intensity of pain, in-
creased functional outcomes of
treatment and improved return-to-
work rate?
There is insucient evidence to make a recommendation regarding whether
radiographic evidence of fusion correlates with better clinical outcomes in
patients with low back pain.
Grade of Recommendation: I
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
36
Surgical Question 6. In patients
undergoing fusion surgery for low
back pain, does the use of bone
growth stimulators (vs fusion
alone) decrease the duration of
pain, decrease the intensity of
pain, increase the functional out-
comes of treatment and improve
the return-to-work rate?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 7. In patients
undergoing fusion surgery for low
back pain, does the use of BMP (vs
fusion alone) decrease the dura-
tion of pain, decrease the intensity
of pain, increase the functional
outcomes of treatment and im-
prove the return-to-work rate?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 8. In patients
undergoing fusion surgery for
low back pain, does the use of
minimally invasive techniques
decrease the duration of pain,
decrease the intensity of pain, in-
crease the functional outcomes of
treatment and improve the return-
to-work rate compared to open
fusion techniques?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 9. In patients
undergoing surgery for low back
pain, do motion preserving sys-
tems (disc prosthesis and dynamic
stabilization systems treatment)
decrease the duration of pain,
decrease the intensity of pain, in-
crease the functional outcomes of
treatment and improve the return-
to-work rate compared to fusion
surgery?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 10. In patients
undergoing surgery for low back
pain, do motion preserving sys-
tems (disc prosthesis and dynamic
stabilization systems) result in
lower incidence of symptomatic
adjacent segment disease?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
37
Surgical Question 11. In patients
with low back pain, does fusion
treatment decrease the duration
of pain, decrease the intensity of
pain, increase the functional out-
comes of treatment and improve
the return-to-work rate compared
to treatment with:
a. Discectomy
b. Discectomy plus rhizotomy
c. Decompression alone
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Surgical Question 12. In patients
with low back pain due to sacro-
iliac joint dysfunction, does sac-
roiliac joint fusion compared with
medical/interventional treatment
decrease the duration of pain,
decrease the intensity of pain, in-
crease the functional outcomes of
treatment and improve the return-
to-work rate?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility
Cost-Utility Question 1. Who is
the most cost-eective spinal care
provider for evaluating patients
with low back pain:
a. Chiropractor vs
b. Physical Therapist vs
c. Primary Care Provider
(including nonphysician providers)
vs
d. Neurologist vs
e. Physiatrist vs
f. Spine Surgeon vs
g. Anesthesiologists/Pain
Medicine Physician vs
h. Radiologist
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
38
Cost-Utility Question 2. What
is the cost-utility of diagnostic
imaging studies/workup in the
evaluation of low back pain (acute,
subacute and chronic), in terms of
inuencing/altering treatment or
in terms of leading to pain reduc-
tion and functional improvement?
a. X-rays (lumbar standing, lumbar
exion-extension, entire spine)
b. CT scan / CT myelogram
c. MRI (conventional or dynamic/
upright/weight bearing)
There is insucient evidence to make a recommendation for or against the
cost-eectiveness of the use of routine ordering of lumbar spine radiographs
for low back pain lasting greater than 6 weeks in the absence of red ags.
Grade of Recommendation: I
Cost-Utility Question 3. Does the
use of ordering physician-owned
diagnostic and treatment facilities
aect the cost of low back pain
related healthcare services?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility Question 4. Are epi-
dural steroid injections (including
interlaminar, transforaminal and
caudal injections and selective
nerve root blocks) more cost-ef-
fective in the management of
patients with low back pain than
other medical/interventional treat-
ments?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility Question 5. Is spinal
cord stimulation more cost-ef-
fective in the management of
patients with low back pain than
other medical/interventional treat-
ments?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility Question 6. Is physical
therapy in the management of
patients with low back pain more
cost-eective than other medical/
interventional treatments?
There is insucient evidence to make a recommendation for or against the
cost-utility of physical therapy in the management of low back pain versus
other medical/interventional treatments.
Grade of Recommendation: I
Cost-Utility Question 7. Is phar-
macological management (over-
the-counter + prescription medi-
cations) for patients with low back
pain more or less cost-eective
than interventional treatments
including physical therapy and
injection therapies?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility Question 8. Is spi-
nal manipulative therapy in the
management of patients with
low back pain more cost-eective
than other medical/interventional
treatments?
There is insucient evidence to make a recommendation for or against the
cost-utility of spinal manipulative therapy for the treatment of low back pain.
Grade of Recommendation: I
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Summary of Recommendations
39
Cost-Utility Question 9. Is acu-
puncture-based therapy in the
management of patients with
low back pain more cost-eective
than other medical/interventional
treatments?
Acupuncture-based therapy in the management of patients with low back
pain is suggested to be cost-eective when compared with other medical/
interventional treatments.
Grade of Recommendation: B
Cost-Utility Question 10. Are
over-the-counter medications only
without other medical interven-
tions more cost-eective in the
management of patients with low
back pain than other medical/in-
terventional treatments?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility Question 11. Is
cognitive or psychological-based
therapy in the management of
patients with low back pain more
cost-eective than other medical/
interventional treatments?
There is conicting evidence regarding the cost-utility of cognitive or psycho-
logical-based therapy in the management of low back pain.
Grade of Recommendation: I
Cost-Utility Question 12. In
patients with low back pain, is
a symptom guided treatment
approach using directional prefer-
ence/centralization matched exer-
cise more cost-eective than usual
care (home care vs medication
vs. nonspecic physical therapy
exercise vs nonspecic physical
therapy modalities) long-term at
12 months, 36 months?
There is insucient evidence to make a recommendation for or against the
cost-utility of directional preference based therapy versus alternatives.
Grade of Recommendation: I
Cost-Utility Question 13. Is the
surgical management (including
fusion and lumbar disc replace-
ment and spinal cord stimulators)
of patients with low back pain
more cost-eective than medical/
interventional treatments?
There is insucient evidence to make a recommendation for or against the
cost-utility of surgical therapies versus medical/interventional therapies for
low back pain.
Grade of Recommendation: I
Cost-Utility Question 14. Is cogni-
tive or psychological-based thera-
py in the management of patients
with low back pain more cost-ef-
fective than surgical therapies?
There is insucient evidence to make a recommendation for or against the
cost-utility of cognitive or psychological-based therapies versus surgical ther-
apies in the treatment of low back pain.
Grade of Recommendation: I
Cost-Utility Question 15. Are
minimally invasive surgical proce-
dures more cost-eective in the
management of patients with low
back pain than conventional open
surgical procedures?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Cost-Utility Question 16. Is in-
strumented lumbar fusion more
cost-eective compared to non-in-
strumented fusion for the treat-
ment of patients with low back
pain?
A systematic review of the literature yielded no studies to adequately ad-
dress this question.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
40
Section Authors
Guideline Co-Chair
D. Scott Kreiner, MD
Diagnosis Section Chair
Daniel K. Resnick, MD, MS
Members
Norman B. Chutkan, MD
Adam C. Lipson, MD
Anthony J. Lisi, DC
Tom E. Reinsel, MD
Robert L. Rich Jr., MD, FAAFP Stakeholder
Representative: American Academy of Family Physicians
(AAFP)
Introduction
This section of the guideline deals with the diagno-
sis of low back pain (LBP) as dened specically for
this project. As the questions were developed, there
were two main focuses. The authors were interested
in determining if there were specic patient charac-
teristics that would be useful in identifying structural
abnormalities of the spine. The rationale behind this
strategy was that structural abnormalities would have
specic treatments and the ability to identify such
patients early in the process may allow for expedited
specic treatment for subgroups of patients. The sec-
ond emphasis related to identication of patient char-
acteristics that could predict the time course of an ep-
isode of back pain. Again, the rationale was to attempt
to identify patients at high risk for conversion from
an acute episode to a more chronic condition in order
to rationally allocate aggressive treatment strategies.
Because back pain is so prevalent, there is an abun-
dance of literature from multiple sources and the
panel reviewed thousands of references. Eventual-
ly, the references were pruned down to slightly more
than 600 selected manuscripts. As the literature was
reviewed, several issues arose that require comment.
First of all, it is recognized that many assessments of
LBP are not necessarily focused on structural abnor-
malities but may be focused on functional or dynamic
characteristics of the pain syndrome. These assess-
ments were not adequately addressed in this section
because of the a priori link between assessment and
structural abnormality in our question set.
Second, dening the gold standard for a “structural
abnormality” as a cause of LBP was extremely prob-
lematic. References reporting correlations between
dierent assessment methods, assessment methods
and injections, assessment methods and surgery and
assessment methods and specic noninvasive thera-
pies were identied. When such studies were well-do-
ne, the results were reported as providing high-qual-
ity evidence regarding the correlation between the
assessment method and the test or treatment em-
ployed as a comparator. For example, a study of pa-
tients with tenderness over the sacroiliac joint may
correlate well with a positive response to a sacroiliac
joint injection. However, with regard to the primary
question, the panel could not agree that a “gold stan-
dard” exists for the diagnosis of LBP due to the wide
range of treatment ecacy when patients are selected
for therapies based on a purported “gold standard.”
There was uncertainty as to whether the “gold stan-
dard” was therefore inaccurate or if the treatment
methods based on that standard were simply vari-
ably eective. Therefore, with regard to the diagnosis
of LBP, the evidence derived from these studies was
downgraded.
Third, the majority of the literature dealing with the
assessment of patients with LBP includes patients
with radicular complaints. Studies were considered
for inclusion only if patients with leg pain were ex-
cluded or if a subgroup analysis was provided allow-
ing for assessment of only patients without radicular
pain/radiculopathy. If, however, patients with radic-
ular complaints were included in a study and a sub-
group analysis was not provided, the study did not
meet the population targeted by this guideline eort
and was discarded. Unfortunately, many well-known
and highly-cited papers fall into this latter category.
Fourth, many of the best-designed and best-performed
prognosis papers looking at recovery from an acute
episode of LBP used return to work (RTW) as their
primary outcome measure without an assessment of
LBP during the follow-up period. The author panel
felt that the use of RTW represented a potentially false
endpoint as it relates to the resolution or persistence
of LBP. It is recognized that patients may return to

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
41
QQ
work despite persistent pain and that patients whose
pain has resolved may choose not to return to work. For
this reason, references that used RTW as the outcome
measure without a concomitant assessment of relevant
patient-reported outcomes were downgraded with
respect to the level of evidence.
Finally, some observations consistently reported by
numerous authors were not specically addressed by
the initial question set. The author group felt it ap-
propriate to include statements reecting such ob-
servations where applicable.
Diagnosis Question 1. In patients with low back pain, are there specic history or
physical examination ndings that would indicate the structure causing pain and,
therefore, guide treatment?
a. Vertebral body
b. Intervertebral disc
c. Zygapophyseal joint
d. Posterior elements
e. Sacroiliac joint
f. Muscle/tendon
g. Central sensitization
There is insucient evidence to make a recommendation for or against the use of innominate
kinematics for the assessment of sacroiliac joint pain.
Grade of Recommendation: I
Adhia et al
1
conducted a single-blinded cross-sectional
case-control study to compare the innominate
kinematic measures (movement pattern, range of
motion and trends of rotation) of participants with
LBP of sacroiliac joint (SIJ) origin versus participants
with LBP of non-SIJ origin. Participants with LBP ≥
3 months (n=122) underwent a clinical examination
with valid and reliable noninvasive SIJ symptom
provocation tests to be classied as SIJ-positive (≥
3 familiar symptom reproduction pain provocation
tests) or SIJ-negative. The clinical evaluation was
followed by innominate kinematic testing by a
blinded tester using an electromagnetic palpation-
digitization technique. Disability (Modied Oswestry
Low Back Pain Disability Questionnaire), level
of physical activity, duration of pain and current
intensity of pain per the visual analog scale (VAS) were
recorded. Innominate range of motion, movement
patterns and trend of rotation were recorded and
compared between SIJ-positive and SIJ-negative
participants. Results demonstrated that SIJ-positive
participants had signicantly dierent innominate
movement patterns and trends of rotation, but not
innominate ranges of motion. The authors concluded
that there was an association between SI joint pain
and altered innominate kinematics. This study
provides Level III evidence that altered innominate
kinematics is associated with 3 out of 5 positive
sacroiliac provocation tests and may be considered for
the diagnosis of SI joint pain.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
42
There is insucient evidence to make a recommendation for or against the use of pain localization in
predicting response to a diagnostic injection.
Grade of Recommendation: I
There is insucient evidence to make a recommendation for or against the assessment of centralization
or peripheralization for the prediction of discography results.
Grade of Recommendation: I
In a retrospective chart review, Depalma et al
2
aimed
to estimate the sensitivity, specicity, positive and
negative predictive values, diagnostic accuracy and
likelihood ratios of positive and negative tests for
diagnosing internal disc disruption (IDD), facet
joint pain (FJP) or sacroiliac joint pain (SIJP) by use
of presence of midline and paramidline LBP. During
the clinical evaluation, patients pointed to the most
painful LBP with one nger, which was documented
as midline (by the spinous processes) or paramid-
line (more than one ngerbreadth lateral to the mid-
line). Charts of patients with a denitive diagnosis for
source of LBP were reviewed and classied as IDD,
FJP, or SIJP. In cases of IDD, signicantly great per-
centages of patients reported midline LBP compared
to FJP or SIJP and signicantly lower percentages of
patients reported paramidline pain compared to FJP
or SIJP. The diagnostic accuracy of midline LBP was
83.5% for IDD, 24.1% for FJP and 31.8% for SIJP. The
authors concluded that the spine specialist can pre-
dict the likely source of the patient’s LBP by evaluat-
ing the location of LBP as the presence of midline LBP
increases the probability of lumbar IDD and reduces
the probability of symptomatic FJ and SIJ dysfunction.
This study provides Level I evidence that location of
pain can predict response to the injection and Level III
evidence that the presence of midline LBP increases
the probability of lumbar IDD and reduces the prob-
ability of symptomatic FJ and SIJ dysfunction. The
presence of isolated paramidline LBP increases the
probability of symptomatic FJ or SIJ but mildly reduc-
es the likelihood of lumbar IDD.
Donelson el al
3
investigated the relationship between
responses of centralization and peripheralization with
discographic ndings in a prospective blinded study
of patients with chronic LBP greater than 3 months.
Patients who were scheduled for discography were
enrolled in the study (n=63). Participants underwent
an initial McKenzie mechanical assessment by a ther-
apist blinded to medical records and were classied
as centralizers, peripheralizers, or no change. During
discography that immediately followed the assess-
ment, pain response was assessed to disc injection
and axial CT was performed on all painful discs. Exact
pain reproduction and an abnormal image were cri-
teria for a positive discogram. Of the 31 centralizers,
23 (74%) had a positive discogram; 21 (91%) of those
had a competent annular wall of the positive disc. Of
the 16 peripheralizers, 11 (69%) had a positive discog-
ram; 6 (54%) of those had a competent annular wall.
Of the 16 with no change upon initial assessment, only
2 (12.5%) had a positive discogram, both with com-
petent annular walls. The authors concluded that the
McKenzie assessment process reliably dierentiated
discogenic versus nondiscogenic pain as well as com-
petent versus incompetent annulus in symptomat-
ic discs. This study provides Level III evidence that
patients who centralize or peripheralize pain with
McKenzie exercises have a higher incidence of posi-
tive discogram than those with no change. Those who
centralize have a higher incidence of an intact annu-
lus as compared to those whose pain peripheralized.
Future Directions for Research
It is recognized that the vast majority of LBP does not have an identiable struc-
tural cause. The term “nonspecic low back pain” provides no biologic basis
for LBP nor assistance in clinical decision-making. Therefore, future research
should focus on reliably identifying clusters of history and physical examination
ndings which can classify patients into subgroups to be validated by identifying
predictably eective treatments. Further studies of nonspecic LBP are unwar-
ranted.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
43
References
1. Adhia DB, Milosavljevic S, Tumilty S, Bussey MD. In-
nominate movement patterns, rotation trends and
range of motion in individuals with low back pain of
sacroiliac joint origin. Man Ther. 2016;21:100-108.
2. Depalma MJ, Ketchum JM, Trussell BS, Saullo TR, Slip-
man CW. Does the location of low back pain predict its
source? Pm R. 2011;3(1):33-39.
3. Donelson R, Aprill C, Medcalf R, Grant W. A prospective
study of centralization of lumbar and referred pain: a
predictor of symptomatic discs and anular competence.
Spine. 1997;22(10):1115-1122.
QQ
Diagnosis Question 2. In patients with low back pain, are there history or physical
examination ndings that would serve as predictors for the recurrence of low
back pain?
There is insucient evidence to indicate that body mass index (BMI) is a potential predictor of a
recurrence of low back pain.
Grade of Recommendation: I
Heuch et al
1
conducted a prospective cohort study to
evaluate the relationship between an elevated body
mass index (BMI) and probability of experiencing
chronic LBP in individuals with and without LBP at
baseline. Participants in the Norwegian HUNT 2 study
were included for analysis (n=25,450). Participants
included those with LBP at baseline (2,669 men and
3,899 women) and without LBP at baseline (8,733 men
and 10,149 women). Subjects indicated presence of
LBP >3 months at baseline and after 11 years. Results
revealed a signicant positive association between
BMI and risk of LBP among individuals without LBP
at baseline. There was a signicant positive associa-
tion between BMI and LBP recurrence among women.
The authors concluded that elevated BMI might pre-
dispose to chronic LBP over 11 years. This study pro-
vides Level II evidence that increasing BMI is associ-
ated with higher reporting of back pain in long-term
follow-up in women.
It is suggested that history of low back pain is a potential predictor of a recurrence of low back
pain.
Grade of Recommendation: B
Kääriä et al
2
evaluated symptoms, chronic disorders,
low back clinical ndings and work absenteeism and
their relationship to inpatient hospitalization in a pro-
spective cohort study. Employees of a manufacturing
facility in Finland who agreed to participate (n=902)
underwent a health examination and completed a
questionnaire. Personal data and clinical information,
including low back diagnoses, were available through
a Finnish Register. Hazard rate ratios of hospitaliza-
tion due to a low back disorder were analyzed. The au-
thors concluded that predictors of inpatient hospital
care for low back disorders included frequent or radi-
ating low back symptoms, chronic low back disorders,
back-related work absenteeism and clinical ndings
in the low back. This study provides Level I evidence
that the occurrence of previous episodes of LBP pre-
dicts future episodes of LBP.
Heuch et al
1
conducted a prospective cohort study to
evaluate the relationship between an elevated BMI
and probability of experiencing chronic LBP in indi-
viduals with and without LBP at baseline. Participants
in the Norwegian HUNT 2 study were included for
analysis (n=25,450). Participants included those with
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
44
LBP at baseline (2,669 men and 3,899 women) and
without LBP at baseline (8,733 men and 10,149 wom-
en). Subjects indicated presence of LBP >3 months at
baseline and after 11 years. Results revealed a signi-
cant positive association between BMI and risk of LBP
among individuals without LBP at baseline. There was
a signicant positive association between BMI and
LBP recurrence among women. The authors conclud-
ed that elevated BMI might predispose to chronic LBP
over 11 years. This study provides Level II evidence
that the occurrence of previous episodes of chron-
ic LBP results in greater risk of recurrence of chronic
LBP.
Future Directions for Research
The work group encountered numerous high quality prognostic studies with
heterogeneous study populations including patients with leg pain. In order to
make useful recommendations, it is recommended that subgroups (ie with or
without leg pain) be identied and analyzed separately.
References:
1. Heuch I, Heuch I, Hagen K, Zwart JA. Body mass index
as a risk factor for developing chronic low back pain: a
follow-up in the Nord-Trondelag Health Study. Spine.
2013;38(2):133-139.
2. Kääriä S, Kaila-Kangas L, Kirjonen J, Riihimäki H, Luuk-
QQ
Diagnosis Question 3. In patients with acute low back pain, are there history or
physical examination ndings that would predict that an episode will resolve
within one month?
Diagnosis Question 6. What are the patient characteristics that increase or
decrease the risk of developing chronic low back pain after an acute episode?
Diagnosis Question 9. Does a psychological evaluation assist with identifying
patients with low back pain who are at risk for developing chronic pain or disability?
The work group considered these questions together as the vast majority of the literature evaluat-
ing the conversion from acute to chronic pain combined various demographic, social, psychologi-
cal and physical examination ndings in predictive models.
konen R, Leino-Arjas P. Low back pain, work absenteeism,
chronic back disorders and clinical ndings in the low back
as predictors of hospitalization due to low back disor-
ders: a 28-year follow-up of industrial employees. Spine.
2005;30(10):1211-1218.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
45
It is recommended that psychosocial factors and workplace factors be assessed when
counseling patients regarding the risk of conversion from acute to chronic low back pain.
Grade of Recommendation: A
Matsudaira et al
1
studied prospective cohort data from
the Japan epidemiological research of Occupation-
related Back pain (JOB) study to assess the association
between aggravated LBP and psychosocial factors.
Participating Japanese workers completed a
questionnaire at baseline (n=5,310) and at one-year
follow-up (n=3,811) which included information
regarding LBP. Of the 1,675 individuals with mild
LBP, 43 (2.6%) developed persistent LBP. Using
logistic regression, interpersonal stress at work, job
satisfaction, depression, somatic symptoms, support
from supervisors, previous sick leave due to LBP and
family history of LBP with disability were associated
with the conversion of mild LBP to persistent LBP.
The authors concluded that psychosocial factors
are important risk factors for persistent LBP in
urban Japanese workers. This study provides Level
I evidence that low job satisfaction, lack of support
from supervisors, interpersonal stress at home,
depression, somatic symptoms and family history
of LBP with disability predicted development of
persistent LBP related disability. Other risk factors for
persistent disability included ergonomic factors such
as bending, twisting, lifting and pushing.
Bakker et al
2
evaluated the use of spinal mechanical
load as a prognostic factor for the conversion of acute
nonspecic LBP to persistent (dened as recurrent
and/or chronic) LBP in a prospective cohort study.
Subjects with acute LBP <6 weeks were enrolled and
underwent a baseline assessment (n=97). A trained
evaluator asked each participant to describe dai-
ly activities and subsequently recorded posture and
spinal load applied (“no load applied”, “loaded”, or
“loaded with movement”) on the standardized 24-
hour schedule (24HS) form. Participants completed
a 6-month follow-up telephone call (n=88) to assess
changes in characteristics, mechanical load per the
24HS, and LBP. Sixty percent of the follow-up partic-
ipants reported persistent LBP. Mechanical load was
not a prognostic factor for persistent LBP, but smok-
ing and advanced age were associated with persistent
LBP. The authors concluded that mechanical loading
of the spine is not predictive for chronicity or recur-
rent episodes of LBP. This study provides Level I evi-
dence that smoking and advanced age are predictors
of conversion of acute to chronic LBP.
Alsaadi et al
3
aimed to evaluate the association be-
tween sleep quality and pain intensity in patients
with acute LBP using data from an existing random-
ized controlled trial. Participants from the PACE study
received paracetamol or placebo until “recovery from
back pain” for up to 4 weeks and recorded outcome
data in a weekly diary for 12 weeks. Sleep quality over
the past 7 days was assessed using the Pittsburgh
Sleep Quality Index (PSQI) and average pain over the
last 24 hours was rated using a 10-point numerical
rating scale (NRS). A generalized estimating equation
model was used with the participants with adequate
follow-up data (n=1246). Sleep quality and pain in-
tensity both improved over the 12-week follow-up
period; for every 1-point decrease in sleep quality,
pain intensity increased by 2.08 points. The authors
concluded that sleep quality is related to subsequent
pain intensity in patients with acute LBP. This study
provides Level I evidence that poor sleep quality as-
sociated with acute LBP is a positive predictor for lack
of recovery.
Coste et al
4
evaluated the associations between vari-
ous risk factors and the natural history of acute LBP
as well as the impact of LBP on health-related quali-
ty of life (HRQOL). Patients with LBP < 72 hours who
self-referred to a general practitioner for LBP (n=113)
completed a baseline assessment which included a
questionnaire on job satisfaction, pain intensity (on
a 100-mm VAS), functional disability (Roland Morris
Disability Questionnaire) and HRQOL (SF-36). Partic-
ipants recorded pain intensity and functional disabil-
ity and had follow-up visits as needed over a 3-month
period. Independent associations with delayed recov-
ery included prior low back surgery, higher initial
disability, lower SF-36 and temporary compensation
status. The authors concluded that work-related fac-
tors and initial HRQOL can contribute to the prognosis
of LBP. This study provides Level I evidence that pri-
or back disability, high scores on disability question-
naire, temporary disability status and SF-36 general
health measure were strong determinants of conver-
sion of acute to chronic LBP.
Foster et al
5
conducted a multicenter prospective co-
hort study to describe illness perceptions and their
associations with clinical outcomes at 6 months in
patients with nonspecic LBP. Patients who consulted

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
46
a general practice for LBP completed questionnaires
that included RMDQ and Revised Illness Perception
Questionnaire (IPQ-R) at enrollment (n=1,591) and
6 months (n=810). Patients who expected their back
problem to last a long time, who perceived serious
consequences and who held weak beliefs in the con-
trollability of their back problem were more likely to
have poor clinical outcomes after 6 months. The au-
thors concluded that patient perceptions about their
back pain predict clinical outcomes 6 months after
consulting their doctor. This study provides Level II
evidence that patient expectations at baseline, fear of
adverse consequences and perception of lack of con-
trol predicted 6-month outcomes.
In a longitudinal cohort study, Fritz et al
6
aimed to
determine cut-o values to maximize the predictive
ability of nonorganic signs and symptoms in patients
with acute LBP and their ability to predict return to
work. Patients with work-related LBP < 3 weeks re-
ferred for physical therapy completed a question-
naire and underwent a physical examination upon
enrollment. A physical therapist gave each participant
a score from 0 to 5 based on nonorganic signs pres-
ent during examination. That number was added to
the nonorganic symptom score based on participant
questionnaire (0-7) to calculate a nonorganic index.
Participants completed the recommended physical
therapy, were reevaluated after 4 weeks and were di-
chotomously categorized as returned to work without
restrictions or not. The presence of 2 or more signs,
3 or more symptoms and an index score of 3 or more
were the best cut-o values. The areas under the
curve ranged from 0.60 to 0.63 which indicate only
slightly greater predictive ability than that expected
by chance. The authors concluded that the nonorgan-
ic tests were not eective screening tools, even with
optimal cut-o values. This study provides Level III
evidence that nonorganic signs are not a predictor of
acute LBP resolution.
Hancock et al
7
prospectively studied data from a ran-
domized controlled trial to develop a simple prognos-
tic rule to help clinicians identify patients with acute
LBP. Patients who presented to a general practitioner
in Australia with LBP < 6 weeks were enrolled in a ran-
domized controlled trial in which they received place-
bo versus active spinal manipulative therapy and pla-
cebo versus active diclofenac. Prognostic factors were
recorded such as average pain over 24 hours, disabili-
ty, function, gender, age, duration of current episode,
number of previous episodes, area of symptoms,
segmental mobility, hip internal rotation range, fear
of pain (fear avoidance beliefs questionnaire), cata-
strophizing, coping and physiotherapist’s prediction
score. Recovery was dened as a pain score of 0 or 1 on
a 0-10 scale for 7 consecutive days per individual pain
diaries. In the eligible sample (n=239), lower than av-
erage initial pain intensity, shorter duration of symp-
toms and fewer episodes were found to be prognostic
factors to predict patients who recover quickly. The
authors concluded that, although it needs external
validation before recommending for clinical use, the
simple clinical prediction rule (CPR) can help primary
care clinicians identify prognosis better than clinician
judgement in terms of days to recovery for patients
with acute LBP. In critique of the methodology, the
work group downgraded this potential Level I study
due to inclusion of patients with radiculopathy; how-
ever, an appropriate subgroup multivariate analysis
was completed. This study provides Level II evidence
that patients with acute LBP who report more severe
pain (>7 out of 10), have longer than 5 days duration
of pain and who have previous episodes of acute LBP
are less likely to recover rapidly from the episode.
Shaw et al
8
aimed to determine if disability risk fac-
tors could predict one-month clinical outcomes of
functional limitation and return to work in patients
with work-related LBP. Enrolled participants (n=568)
completed a questionnaire at baseline and after one
month that included physical health risks, workplace
factors, pain, mood and expectations for recovery.
Outcome measures included functional limitation
(RMDQ) and return to work. Employer factors and
self-ratings of pain and mood better predicted func-
tional improvement and return to work compared to
health history or physical examination. The authors
concluded that identication and intervention fo-
cused on job factors, pain coping strategies and ex-
pectations for recovery may improve outcomes. The
work group downgraded this potential Level I study
due to uncertainty regarding the patient population,
specically regarding radiculopathy. This study pro-
vides Level II evidence that risk factors for prolonged
disability and the converse of recovery from LBP at 30
days include job circumstances, pain coping strate-
gies and poor expectation for recovery.
In a prospective cohort, Shaw et al
9
assessed the re-
lationship between BMI and pain and function out-
comes in work-related LBP. Participants with LBP ≤
14 days (n=607) reported height, weight, pain, func-
tional limitation and work status at baseline and af-
ter one and 3 months. Participants were categorized
as normal, overweight or obese based on BMI for data
analysis. There were no signicant dierences in out-
comes of pain, functional limitation (RMDQ) or return

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
47
to work based on categorization of BMI. The authors
concluded that BMI is not a useful prognostic factor
for work-related acute or subacute LBP. This study
provides Level II evidence that BMI is not predictive
of transition to chronicity in the workers compensa-
tion population.
Gatchel et al
10
assessed the relationship between psy-
chological characteristics and conversion of acute to
chronic LBP. A total of 324 participants with acute
LBP ≤ 6 weeks completed assessments at baseline
including pain and disability (Million VAS), psycho-
pathology (Structured Clinical Interview for DSM-
III-R) and Minnesota Multiphasic Personality In-
ventory (MMPI). After 6 months, patients completed
a telephone questionnaire and were categorized as
currently working or in training/school (n=274), not
currently working due to original back injury (n=36)
or not currently working due to factors other than
original back injury (n=14; not analyzed in this study).
The disabled group had higher self-reported pain and
disability, more individuals with a personality disor-
der and higher scores on Scale 3 of the MMPI. The au-
thors concluded that the presence of these psychoso-
cial variables is associated with injured workers who
are likely to convert from acute to chronic LBP. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to the inclusion of
workers with a history of “chronic back pain” in the
original cohort. This study provides Level II evidence
that workers with more severe LBP, increased psy-
chological distress and/or personality disorders are
more likely to remain o work 6 months after acute
episode.
Gatchel et al
11
evaluated the eectiveness of a psycho-
social and personality assessment in predicting the
transition of acute LBP to chronic pain disability. Par-
ticipants (n=421) with LBP for less than 6 weeks com-
pleted assessments including the DSM-III-R Diag-
nosis, Minnesota Multiphasic Personality Inventory
and Million Visual Pain Analog Scale. Return-to-work
status was collected at 6- and 12-month follow-up
telephone calls. Participants were categorized as cur-
rently working or in training/school (n=365), not
currently working due to original back injury (n=29),
or not currently working due to factors other than
original back injury (n=27; not analyzed in this study).
Compared to the nondisabled group, the participants
not currently working due to the original back injury
had higher pain and disability analog scores, higher
MMPI Scale 3 scores and proportionately more in-
dividuals with workers compensation and person-
al injury cases. Major psychopathology (depression
and substance abuse) did not precede or cause devel-
opment of chronic pain disability. The authors con-
cluded that their statistical algorithm to determine a
“psychosocial disability factor” can predict patients
with acute LBP that will likely develop into chronic
disability. The work group downgraded this poten-
tial Level I study due to the inclusion of some work-
ers with preexisting chronic LBP in the cohort. This
study provides Level II evidence that initial pain and
disability MMPI score, female gender and insurance
status can predict return to work one year following
acute LBP episode.
Reme et al
12
conducted a study to identify clusters
of self-reported concerns and expectations in
individuals with LBP who would benet from early
intervention. Participants with acute LBP related
to work (n=496) completed a questionnaire with
11 possible risk factors upon enrollment and a
follow-up questionnaire assessing pain, functional
limitation and work status after 3 months. Eight of
the risk factors had signicant associations with the
outcomes and were used to create 4 clusters: minimal
risk (best functional outcomes), workplace concerns,
activity limitations and emotional distress (poorest
functional outcomes). The authors concluded that
questionnaires that contain pain-related concerns
and expectations can be useful to identify patients
with LBP who could benet from early intervention.
This study provides Level II evidence that recovery
expectations, life impact of pain, organizational
support, kinesiophobia, functional limitation,
pain catastrophizing, depressive symptoms and
pain intensity showed signicant associations
with functional recovery and return to work. These
measures were entered into the cluster analysis. A
4-cluster solution met criteria for cluster separation
and interpretability and the 4 clusters were labeled:
(a) minimal risk (29 %), (b) workplace concerns (26
%), (c) activity limitations (27%) and (d) emotional
distress (19 %). Functional outcomes were best in the
minimal risk group, poorest in the emotional distress
group and intermediate in the other two groups.
Rolli Salathe et al
13
aimed to identify work-related
resources to predict sickness absence in individuals
with LBP. Employed individuals with acute (<6
weeks) or subacute (<12 weeks) LBP (n=279)
completed a questionnaire at baseline and after one
year which included the work-related section of
the Fear-Avoidance Beliefs Questionnaire (FABQ),
life satisfaction, job satisfaction, participation in
sports and social support at work. The outcome
measure, sickness absence, was self-reported on the

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
48
questionnaire as days missed from work due to LBP.
Multiple linear regression analysis revealed that life
satisfaction, work-related FABQ and sickness absence
at baseline were predictors of sickness absence after
one year. The authors concluded that life satisfaction
was a predictor of sickness absence after one year. This
study provides Level III evidence that life satisfaction,
job satisfaction and social support decreased sickness
absence at baseline and one-year follow-up.
In a prospective cohort study, Shaw et al
14
evaluated
the eect of psychiatric diagnoses on the likelihood
of transitioning from subacute to chronic LBP. Men
presenting to their provider with LBP for 6-10 weeks
completed an assessment at baseline (n=140) and after
6 months (n=120) which included a standardized or-
thopedic evaluation, structured psychodiagnostic in-
terview (Diagnostic Interview Schedule Version III-R
[DIS]) and details on pain intensity (Descriptor Dif-
ferential Scale [DDS]) and Disability (Sickness Impact
Prole [SIP]). The outcome of transition to chronic
pain was dened as SIP score >10 and DDS score for
pain intensity >10 at 6-month follow-up. Men with a
diagnosis of major depressive disorder, generalized
anxiety, post-traumatic stress disorder (PTSD), or
current nicotine dependence had greater risk of tran-
sitioning to chronic LBP. The authors concluded that
screening for depressive disorder or anxiety disorder
may identify individuals with greater risk of transi-
tion to chronic LBP. Due to the subacute patient popu-
lation, the work group determined this study provid-
ed Level II evidence that risk of conversion to chronic
pain in male patients was signicantly elevated in the
presence of a lifetime diagnosis of major depression,
PTSD and generalized anxiety or a diagnosis of nico-
tine dependence in the past 6 months.
Turner et al
15
assessed the predictive value of work-
er demographic, pain, disability and psychosocial
variables on 6-month work disability in individ-
uals with work-related LBP. Individuals who sub-
mitted a workers’ compensation back pain disabili-
ty claim (n=1,068) completed a telephone interview
that addressed pain intensity (on a scale from 0 to
10), disability (RMDQ), catastrophizing (Pain Cata-
strophizing Scale), recovery expectations, coworker
relations, and blame. The outcome measure of work
disability was wage replacement compensation for
total disability after initially submitting the claim. At
6 months, predictors of disability included age, race,
education and baseline pain and disability. High levels
of fear-avoidance and low expectations of recovery
were independent predictors of 6-month disability.
The authors concluded that in the studied population,
risk factors for chronic work disability include high
pain and disability, low recovery expectations and
fears that work may increase pain or cause harm. The
work group initially rated this study as a Level II due
to uncertainty regarding the duration of enrollment,
but downgraded the level of evidence to a Level III due
to the outcome of “not being paid” for return to work.
This was felt to introduce an additional false endpoint
that may not have been completely dependent upon
the resolution of back pain. Therefore, this study pro-
vides Level III evidence that workers with lower re-
covery expectations and greater work fear avoidance
at baseline were signicantly (P < 0.05) more likely to
be receiving work disability wage replacement com-
pensation at 6 months.
Melloh et al
16
investigated factors that inuence the
progression of acute LBP to persistent LBP in an in-
ception cohort study of patients presenting to a health
practitioner for acute LBP. Enrolled participants
(n=62) completed a questionnaire at baseline and were
invited to complete follow-up questionnaires after 3,
6, 12 weeks and 6 months. Predictor variables were
combined into three indices: “working conditions,”
“depression and maladaptive cognitions” and “pain
and quality of life.” Persistent LBP was dened as an
Oswestry Disability Index (ODI) score >10 points after
6 weeks. In the participants who followed up after 6
months (n=53), the index “depression and maladap-
tive cognitions” (depression, somatization, resigned
attitude towards the job, fear-avoidance, rumination,
helplessness, catastrophizing and negative expecta-
tions on return to work) at baseline was a signicant
predictor for transition of acute to persistent LBP. The
authors concluded that psychological factors at base-
line correlated with progression from acute to per-
sistent LBP at 6 months and may be benecial to add
into screening tools. In critique of the methodology,
the work group downgraded this potential Level I ar-
ticle due to concerns of select patient population and
sample size. This study provides Level II evidence that
depression and maladaptive cognitions are a signi-
cant risk factor for conversion from acute to chronic
LBP at 6 months.
Sewitch et al
17
conducted a secondary analysis of data
from a randomized controlled trial on the eective-
ness of a back school program in order to nd the re-
lationship between psychological factors and recovery
from rst episode of LBP. Participants (n=134) with a
rst occurrence of LBP receiving workers’ compensa-
tion with the inability to work due to LBP completed
baseline assessments. Demographics, lifestyle hab-
its, job-related variables, mental health status (per

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
49
Psychiatric Symptom Index and General Well Being
Scale), functional status (RMDQ) and pain (VAS) were
recorded. The outcome of late return to work was de-
ned as return to work > 31 days after enrollment in
study; the outcome of compensated recurrence was
dened as a subsequent compensated disability due to
LBP after initial return to work. Multivariate analysis
revealed that lower psychological distress predicted
late return to work while higher general well-being,
greater control over emotions, higher aggressiveness
and lower anxiety predicted compensated recurrence.
The authors concluded that psychological factors do
not impact clients with all types of LBP the same way.
The work group downgraded this potential Level II
study due to nonconsecutive patients and the return-
to-work outcome measure. This study provides Level
III evidence that history of back pain and psychologi-
cal level of functioning inuences return to work in a
workers’ compensation population.
It is recommended that psychosocial factors be used as prognostic factors for return to work
following an episode of acute low back pain.
Grade of Recommendation: A
Gatchel et al
10
assessed the relationship between psy-
chological characteristics and conversion of acute to
chronic LBP. A total of 324 participants with acute
LBP ≤ 6 weeks completed assessments at baseline
including pain and disability (Million VAS), psycho-
pathology (Structured Clinical Interview for DSM-
III-R) and Minnesota Multiphasic Personality In-
ventory (MMPI). After 6 months, patients completed
a telephone questionnaire and were categorized as
currently working or in training/school (n=274), not
currently working due to original back injury (n=36)
or not currently working due to factors other than
original back injury (n=14; not analyzed in this study).
The disabled group had higher self-reported pain and
disability, more individuals with a personality disor-
der and higher scores on Scale 3 of the MMPI. The au-
thors concluded that the presence of these psychoso-
cial variables is associated with injured workers who
are likely to convert from acute to chronic LBP. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to the inclusion of
workers with a history of “chronic back pain” in the
original cohort. This study provides Level II evidence
that workers with more severe LBP, increased psy-
chological distress and/or personality disorders are
more likely to remain o work 6 months after acute
episode.
Gatchel et al
11
evaluated the eectiveness of a psycho-
social and personality assessment in predicting the
transition of acute LBP to chronic pain disability. Par-
ticipants (n=421) with LBP for less than 6 weeks com-
pleted assessments including the DSM-III-R Diagno-
sis, Minnesota Multiphasic Personality Inventory and
Million Visual Pain Analog Scale. Return-to-work sta-
tus was collected at 6- and 12-month follow-up tele-
phone calls. Participants were categorized as currently
working or in training/school (n=365), not current-
ly working due to original back injury (n=29), or not
currently working due to factors other than original
back injury (n=27; not analyzed in this study). Com-
pared to the nondisabled group, the participants not
currently working due to the original back injury had
higher pain and disability analog scores, higher MMPI
Scale 3 scores and proportionately more individu-
als with workers compensation and personal injury
cases. Major psychopathology (depression and sub-
stance abuse) did not precede or cause development
of chronic pain disability. The authors concluded that
their statistical algorithm to determine a “psychoso-
cial disability factor” can predict patients with acute
LBP that will likely develop into chronic disability. The
work group downgraded this potential Level I study
due to the inclusion of some workers with preexisting
chronic LBP in the cohort. This study provides Level II
evidence that initial pain and disability MMPI score,
female gender and insurance status can predict return
to work one year following acute LBP episode.
Rolli Salathe et al
13
aimed to identify work-related re-
sources to predict sickness absence in individuals with
LBP. Employed individuals with acute (< 6 weeks) or
subacute (< 12 weeks) LBP (n=279) completed a ques-
tionnaire at baseline and after one year which includ-
ed the work-related section of the Fear-Avoidance
Beliefs Questionnaire (FABQ), life satisfaction, job
satisfaction, participation in sports and social support
at work. The outcome measure, sickness absence, was
self-reported on the questionnaire as days missed
from work due to LBP. Multiple linear regression
analysis revealed that life satisfaction, work-related
FABQ and sickness absence at baseline were predic-

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
50
tors of sickness absence after one year. The authors
concluded that life satisfaction was a predictor of
sickness absence after one year. This study provides
Level III evidence that life satisfaction, job satisfac-
tion and social support decreased sickness absence at
baseline and one-year follow-up.
Turner et al
15
assessed the predictive value of work-
er demographic, pain, disability and psychosocial
variables on 6-month work disability in individuals
with work-related LBP. Individuals who submitted
a workers’ compensation back pain disability claim
(n=1,068) completed a telephone interview that ad-
dressed pain intensity (on a scale from 0 to 10), dis-
ability (RMDQ), catastrophizing (Pain Catastrophiz-
ing Scale), recovery expectations, coworker relations,
and blame. The outcome measure of work disability
was wage replacement compensation for total disabil-
ity after initially submitting the claim. At 6 months,
predictors of disability included age, race, educa-
tion and baseline pain and disability. High levels of
fear-avoidance and low expectations of recovery were
independent predictors of 6-month disability. The
authors concluded that in the studied population, risk
factors for chronic work disability include high pain
and disability, low recovery expectations and fears
that work may increase pain or cause harm. The work
group initially assigned this study as a Level II due to
uncertainty regarding the duration of enrollment, but
downgraded the level of evidence to a Level III due to
the outcome of “not being paid” for return to work.
This was felt to introduce an additional false endpoint
that may not have been completely dependent upon
the resolution of back pain. Therefore, this study pro-
vides Level III evidence that workers with lower re-
covery expectations and greater work fear avoidance
at baseline were signicantly (P < 0.05) more likely to
be receiving work disability wage replacement com-
pensation at 6 months.
Sewitch et al
17
conducted a secondary analysis of data
from a randomized controlled trial of the eective-
ness of a back school program in order to nd the re-
lationship between psychological factors and recovery
from rst episode of LBP. Participants (n=134) with a
rst occurrence of LBP receiving workers’ compensa-
tion with the inability to work due to LBP completed
baseline assessments. Demographics, lifestyle hab-
its, job-related variables, mental health status (per
Psychiatric Symptom Index and General Well Being
Scale), functional status (RMDQ) and pain (VAS) were
recorded. The outcome of late return to work was de-
ned as return to work >31 days after enrollment in
study; the outcome of compensated recurrence was
dened as a subsequent compensated disability due to
LBP after initial return to work. Multivariate analysis
revealed that lower psychological distress predicted
late return to work while higher general well-being,
greater control over emotions, higher aggressiveness
and lower anxiety predicted compensated recurrence.
The authors concluded that psychological factors do
not impact clients with all types of LBP the same way.
This study provides Level III evidence that history of
back pain and psychological level of functioning in-
uences return to work in a workers’ compensation
population.
It is recommended that pain severity and functional impairment be used to stratify risk of con-
version from acute to chronic low back pain.
Grade of Recommendation: A
Coste et al
4
evaluated the associations between vari-
ous risk factors and the natural history of acute LBP
as well as the impact of LBP on health-related quali-
ty of life (HRQOL). Patients with LBP < 72 hours who
self-referred to a general practitioner for LBP (n=113)
completed a baseline assessment which included a
questionnaire on job satisfaction, pain intensity (on
a 100-mm VAS), functional disability (RMDQ) and
HRQOL (SF-36). Participants recorded pain intensity
and functional disability and had follow-up visits as
needed over a 3-month period. Independent associ-
ations with delayed recovery included prior low back
surgery, higher initial disability, lower SF-36 and
temporary compensation status. The authors con-
cluded that work-related factors and initial HRQOL
can contribute to the prognosis of LBP. This study
provides Level I evidence that prior back disability,
high scores on disability questionnaire, temporary
disability status and SF-36 general health measure
were strong determinants of conversion of acute to
chronic pain.
Gatchel et al
10
assessed the relationship between psy-
chological characteristics and conversion of acute to
chronic LBP. A total of 324 participants with acute LBP
≤ 6 weeks completed assessments at baseline includ-
ing pain and disability (Million VAS), psychopathol-
ogy (Structured Clinical Interview for DSM-III-R)

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
51
and Minnesota Multiphasic Personality Inventory
(MMPI). After 6 months, patients completed a tele-
phone questionnaire and were categorized as cur-
rently working or in training/school (n=274), not
currently working due to original back injury (n=36),
or not currently working due to factors other than
original back injury (n=14; not analyzed in this study).
The disabled group had higher self-reported pain and
disability, more individuals with a personality disor-
der and higher scores on Scale 3 of the MMPI. The au-
thors concluded that the presence of these psychoso-
cial variables is associated with injured workers who
are likely to convert from acute to chronic LBP. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to the inclusion of
workers with a history of “chronic back pain” in the
original cohort. This study provides Level II evidence
that workers with more severe LBP, increased psy-
chological distress and/or personality disorders are
more likely to remain o work 6 months after acute
episode.
Gatchel et al
11
evaluated the eectiveness of a psycho-
social and personality assessment in predicting the
transition of acute LBP to chronic pain disability. Par-
ticipants (n=421) with LBP for less than 6 weeks com-
pleted assessments including the DSM-III-R Diag-
nosis, Minnesota Multiphasic Personality Inventory
and Million Visual Pain Analog Scale. Return-to-work
status was collected at 6- and 12-month follow-up
telephone calls. Participants were categorized as cur-
rently working or in training/school (n=365), not
currently working due to original back injury (n=29),
or not currently working due to factors other than
original back injury (n=27; not analyzed in this study).
Compared to the non-disabled group, the participants
not currently working due to the original back injury
had higher pain and disability analog scores, higher
MMPI Scale 3 scores and proportionately more in-
dividuals with workers compensation and person-
al injury cases. Major psychopathology (depression
and substance abuse) did not precede or cause devel-
opment of chronic pain disability. The authors con-
cluded that their statistical algorithm to determine a
“psychosocial disability factor” can predict patients
with acute LBP that will likely develop into chronic
disability. The work group downgraded this poten-
tial Level I study due to the inclusion of some work-
ers with preexisting chronic LBP in the cohort. This
study provides Level II evidence that initial pain and
disability MMPI score, female gender and insurance
status can predict return to work one year following
acute LBP episode.
Costa et al
18
investigated prognostic markers to iden-
tify the transition from acute to chronic LBP in an
inception cohort study with one-year follow-up in
Australia. Patients who initially presented to primary
care with acute (<2 weeks) LBP which transitioned to
chronic (>3 months) LBP were included in this study
(n=406). A telephone interview was conducted at on-
set of chronic LBP and after 9 and 12 months to as-
sess potential prognostic factors as well as intensity
of pain, disability and work status. Participants were
considered to be completely recovered when they
reported they were pain free, had no disability from
back pain and returned to work for 30 consecutive
days. Delayed recovery was associated with previous
sick leave due to low LBP, high disability levels or pain
intensity at onset of chronic LBP, low levels of edu-
cation, greater perceived risk of persistent pain and
birthplace outside of Australia. The authors conclud-
ed that the prognosis for individuals with chronic LBP
is moderately optimistic; they identied prognostic
factors that may make prognosis less favorable. This
study provides Level II evidence that patients who do
not rapidly recover from acute LBP who are at risk for
developing chronic symptoms have: lower educa-
tion; workers compensation claims; the use of med-
ications; increased disability at acute presentation;
previous sick leave for LBP; feelings of depression,
tension or anxiety; high pain intensity; morning back
stiness and perception of having a high risk of per-
sistent pain.
Hancock et al
7
prospectively studied data from a ran-
domized controlled trial to develop a simple prognos-
tic rule to help clinicians identify patients with acute
LBP. Patients who presented to a general practitioner
in Australia with LBP <6 weeks were enrolled in a ran-
domized controlled trial in which they received pla-
cebo versus active spinal manipulative therapy and
placebo versus active diclofenac. Prognostic factors
were recorded such as average pain over 24 hours,
disability, function, gender, age, duration of cur-
rent episode, number of previous episodes, area of
symptoms, segmental mobility, hip internal rotation
range, fear of pain (fear avoidance beliefs question-
naire), catastrophizing, coping and physiotherapist’s
prediction score. Recovery was dened as a pain score
of 0 or 1 on a 0-10 scale for 7 consecutive days per in-
dividual pain diaries. In the eligible sample (n=239),
lower than average initial pain intensity, shorter du-
ration of symptoms and fewer episodes were found to
be prognostic factors to predict patients who recover
quickly. The authors concluded that, although it needs
external validation before recommending for clinical

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
52
use, the simple CPR can help primary care clinicians
identify prognosis better than clinician judgement in
terms of days to recovery for patients with acute LBP.
In critique of the methodology, the work group down-
graded this potential Level I study due to inclusion of
patients with radiculopathy; however, an appropriate
subgroup multivariate analysis was completed. This
study provides Level II evidence that patients with
acute LBP who report more severe pain (>7 out of 10),
have longer than 5 days duration of pain and who have
previous episodes of acute LBP are less likely to re-
cover rapidly from episode.
Friedman et al
19
investigated whether 5 high-risk
variables predict poor functional outcomes in patients
presenting to the emergency department (ED) for
nontraumatic LBP classied as musculoskeletal.
The high-risk variables included baseline functional
disability related to LBP, radicular signs, depression,
work-related injury or history of chronic or recurrent
LBP. In this prospective observational cohort study
at a single ED, enrolled participants (n=556) were
interviewed prior to ED discharge which included
information regarding demographics, duration
and symptoms of LBP and the RMDQ. Patients’ LBP
was categorized as chronic, episodic or rare/never.
Participants were contacted at one week (97% follow-
up) and three months (92% follow-up) post-discharge
to assess the outcome measure of functional limitation
per the RMDQ score (score >0 indicating LBP-related
functional impairment). A higher baseline RMDQ
score and chronic LBP were each associated with LBP-
related functional disability at 7-day and 3-month
follow-up. Depression, radicular signs and work-
injury did not predict functional outcome at either
time point. The authors concluded that, in patients
presenting to the ED with nontraumatic LBP, those
with worse baseline functional impairments and
history of chronic LBP are more likely to have worse
short- and long-term functional outcomes. In critique
of the methodology, the work group downgraded this
potential Level I study due to the short follow-up
period. This study provides Level II evidence that high
initial disability (RMDQ ≥ 17) and a history of previous
LBP for 30 straight days predicted lack of recovery at
3 months.
Neubauer et al
20
conducted a prospective cohort study
with the objective to develop a short and reliable in-
strument to predict the chronicity of LBP. Patients
presenting to an orthopedic specialist for acute LBP
<6 months were invited to participate. Participants
completed a questionnaire at enrollment (n=235)
and again by mail after 6 months (n=192, 82%) af-
ter receiving standard treatment for LBP. Question-
naires covered 167 items including LBP history and
pain (VAS), cognitive strategies of pain management,
psychosomatic comorbidities, subjective well-being,
depressive symptoms (Zung Depression Index), work
satisfaction and socio-demographic data. The main
outcome measure was chronicity of LBP, dened as
presence of LBP after 6 months. Results revealed that
pain intensity, tolerance and duration, as well as edu-
cational level, pain experienced elsewhere in the body,
depression, female gender, catastrophizing thoughts,
and feelings of helplessness were strong predictors
for the development of chronic LBP. The authors con-
cluded that a questionnaire with these items can pre-
dict a patient’s risk of developing chronic LBP with a
probability of 78%. This study provides Level II evi-
dence that pain intensity and acceptance, response
to massage therapy, duration of pain, patient educa-
tional level, pain elsewhere in body, depression, fe-
male gender, catastrophizing thoughts, and feelings
of helplessness predicted conversion to chronic LBP
at 6 months.
It is suggested that prior episodes of low back pain be considered a prognostic factor for the
conversion from acute to chronic low back pain.
Grade of Recommendation: B
Coste et al
4
evaluated the associations between vari-
ous risk factors and the natural history of acute LBP
as well as the impact of LBP on health-related qual-
ity of life (HRQOL). Patients with LBP <72 hours who
self-referred to a general practitioner for LBP (n=113)
completed a baseline assessment which included a
questionnaire on job satisfaction, pain intensity (on
a 100-mm VAS), functional disability (RMDQ) and
HRQOL (SF-36). Participants recorded pain intensity
and functional disability and had follow-up visits as
needed over a 3-month period. Independent associ-
ations with delayed recovery included prior low back
surgery, higher initial disability, lower SF-36 and
temporary compensation status. The authors con-
cluded that work-related factors and initial HRQOL
can contribute to the prognosis of LBP. This study

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
53
provides Level I evidence that prior back disability,
high scores on disability questionnaire, temporary
disability status and SF-36 general health measure
were strong determinants of conversion of acute to
chronic pain.
Costa et al
18
investigated prognostic markers to iden-
tify the transition from acute to chronic LBP in an
inception cohort study with one-year follow-up in
Australia. Patients who initially presented to primary
care with acute (<2 weeks) LBP which transitioned to
chronic (>3 months) LBP were included in this study
(n=406). A telephone interview was conducted at on-
set of chronic LBP and after 9 and 12 months to as-
sess potential prognostic factors as well as intensity
of pain, disability and work status. Participants were
considered to be completely recovered when they
reported they were pain free, had no disability from
back pain and returned to work for 30 consecutive
days. Delayed recovery was associated with previous
sick leave due to low LBP, high disability levels or pain
intensity at onset of chronic LBP, low levels of edu-
cation, greater perceived risk of persistent pain and
birthplace outside of Australia. The authors conclud-
ed that the prognosis for individuals with chronic LBP
is moderately optimistic; they identied prognostic
factors that may make prognosis less favorable. This
study provides Level II evidence that patients who do
not rapidly recover from acute LBP who are at risk for
developing chronic symptoms have: lower educa-
tion; workers compensation claims; the use of med-
ications; increased disability at acute presentation;
previous sick leave for LBP; feelings of depression,
tension or anxiety; high pain intensity; morning back
stiness and perception of having a high risk of per-
sistent pain.
Sewitch et al
17
conducted a secondary analysis of data
from a randomized controlled trial of the eective-
ness of a back school program in order to nd the re-
lationship between psychological factors and recovery
from rst episode of LBP. Participants (n=134) with a
rst occurrence of LBP receiving workers’ compensa-
tion with the inability to work due to LBP completed
baseline assessments. Demographics, lifestyle hab-
its, job-related variables, mental health status (per
Psychiatric Symptom Index and General Well Being
Scale), functional status (RMDQ) and pain (VAS) were
recorded. The outcome of late return to work was de-
ned as return to work >31 days after enrollment in
study; the outcome of compensated recurrence was
dened as a subsequent compensated disability due to
LBP after initial return to work. Multivariate analysis
revealed that lower psychological distress predicted
late return to work while higher general well-being,
greater control over emotions, higher aggressiveness
and lower anxiety predicted compensated recurrence.
The authors concluded that psychological factors do
not impact clients with all types of LBP the same way.
This study provides Level III evidence that history of
back pain and psychological level of functioning in-
uences return to work in a workers’ compensation
population.
There is insucient evidence to assess sleep quality as a prognostic variable to predict recov-
ery from acute low back pain.
Grade of Recommendation: I
Alsaadi et al
3
aimed to evaluate the association be-
tween sleep quality and pain intensity in patients with
acute LBP using data from an existing randomized
controlled trial. Participants from the PACE study re-
ceived paracetamol or placebo until “recovery from
back pain” for up to 4 weeks and recorded outcome
data in a weekly diary for 12 weeks. Sleep quality over
the past 7 days was assessed using the Pittsburgh
Sleep Quality Index (PSQI) and average pain over the
last 24 hours was rated using a 10-point numerical
rating scale (NRS). A generalized estimating equation
model was used with the participants with adequate
follow-up data (n=1246). Sleep quality and pain in-
tensity both improved over the 12-week follow-up
period; for every 1-point decrease in sleep quality,
pain intensity increased by 2.08 points. The authors
concluded that sleep quality is related to subsequent
pain intensity in patients with acute LBP. This study
provides Level I evidence that poor sleep quality as-
sociated with acute LBP is a positive predictor for lack
of recovery.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
54
There is insucient evidence to make a recommendation for or against the use of smoking
and/or obesity as prognostic factors for the conversion from acute to chronic low back pain.
Grade of Recommendation: I
Bakker et al
2
evaluated the use of spinal mechanical
load as a prognostic factor for the conversion of acute
nonspecic LBP to persistent (dened as recurrent
and/or chronic) LBP in a prospective cohort study.
Subjects with acute LBP <6 weeks were enrolled and
underwent a baseline assessment (n=97). Spinal me-
chanical load was calculated using the 24HS measure-
ment. Participants completed a 6-month follow-up
telephone call (n=88) to assess changes in character-
istics, mechanical load per the 24HS and LBP. Sixty
percent of the follow-up participants reported per-
sistent LBP. Mechanical load was not a prognostic
factor for persistent LBP, but smoking and advanced
age were associated with persistent LBP. The authors
concluded that mechanical loading of the spine is not
predictive for chronicity or recurrent episodes of LBP.
This study provides Level I evidence that smoking and
advanced age are predictors of conversion of acute to
chronic LBP.
In a prospective cohort, Shaw et al
9
assessed the rela-
tionship between BMI on pain and function outcomes
in work-related LBP. Participants with LBP ≤14 days
(n=607) reported height, weight, pain, functional
limitation and work status at baseline and after one
and 3 months. Participants were categorized as nor-
mal, overweight or obese based on BMI for data anal-
ysis. There were no signicant dierences in out-
comes of pain, functional limitation (RMDQ) or return
to work based on categorization of BMI. The authors
concluded that BMI is not a useful prognostic factor
for work-related acute or subacute LBP. This study
provides Level II evidence that BMI is not predictive
of transition to chronicity in the workers compensa-
tion population.
In a prospective cohort study, Shaw et al
14
evaluated
the eect of psychiatric diagnoses on the likelihood
of transitioning from subacute to chronic LBP. Men
presenting to their provider with LBP for 6-10 weeks
completed an assessment at baseline (n=140) and after
6 months (n=120) which included a standardized or-
thopedic evaluation, structured psychodiagnostic in-
terview (Diagnostic Interview Schedule Version III-R
[DIS]) and details on pain intensity (DDS) and Dis-
ability (Sickness Impact Prole [SIP]). The outcome
of transition to chronic pain was dened as SIP score
>10 and DDS score for pain intensity >10 at 6-month
follow-up. Men with a diagnosis of major depressive
disorder, generalized anxiety, post-traumatic stress
disorder (PTSD) or current nicotine dependence had
greater risk of transitioning to chronic LBP. The au-
thors concluded that screening for depressive disor-
der or anxiety disorder may identify individuals with
greater risk of transition to chronic LBP. Due to the
subacute patient population, the work group deter-
mined this study provided Level II evidence that risk
of conversion to chronic pain in male patients was
signicantly elevated in the presence of a lifetime di-
agnosis of major depression, PTSD and generalized
anxiety, or a diagnosis of nicotine dependence in the
past 6 months.
Future Directions for Research
The work group encountered numerous high quality prognostic studies with
heterogeneous study populations including patients with leg pain. In order to
make useful recommendations, it is recommended that subgroups (ie with or
without leg pain) be identied and analyzed separately.
The work group recommends further research on interventions addressing the
prognostic factors above and the eect of those interventions on the conver-
sion from acute to chronic LBP.
References
1. Matsudaira K, Konishi H, Miyoshi K, Isomura T, Inuzu-
ka K. Potential risk factors of persistent low back pain
developing from mild low back pain in urban Japanese
workers. PLoS ONE. 2014;9(4):e93924.
2. Bakker EWP, Verhagen AP, Lucas C, Koning HJCMF,
Koes BW. Spinal mechanical load: A predictor of per-
sistent low back pain? A prospective cohort study. Eur
Spine J. 2007;16(7):933-941.
3. Alsaadi SM, McAuley JH, Hush JM, et al. Poor sleep qual-
ity is strongly associated with subsequent pain intensity

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
55
in patients with acute low back pain. Arthritis Rheumatol.
2014;66(5):1388-1394.
4. Coste J, Lefrancois G, Guillemin F, Pouchot J. Prognosis
and Quality of life in patients with acute low back pain:
insights from a comprehensive inception cohort study.
Arthritis Care Res. 2004;51(2):168-176.
5. Foster NE, Bishop A, Thomas E, et al. Illness perceptions
of low back pain patients in primary care: what are they,
do they change and are they associated with outcome?
Pain. 2008;136(1-2):177-187.
6. Fritz JM, Wainner RS, Hicks GE. The use of nonorgan-
ic signs and symptoms as a screening tool for return-
to-work in patients with acute low back pain. Spine.
2000;25(15):1925-1931.
7. Hancock MJ, Maher CG, Latimer J, Herbert RD, McAu-
ley JH. Can rate of recovery be predicted in patients with
acute low back pain? Development of a clinical predic-
tion rule. Eur J Pain. 2009;13(1):51-55.
8. Shaw WS, Pransky G, Patterson W, Winters T. Early dis-
ability risk factors for low back pain assessed at outpa-
tient occupational health clinics. Spine. 2005;30(0):572-
580.
9. Shaw WS, Tveito TH, Woiszwillo MJ, Pransky G. The ef-
fect of body mass index on recovery and return to work
after onset of work-related low back pain. J Occup Envi-
ron Med. 2012;54(2):192-197.
10. Gatchel RJ, Polatin PB, Kinney RK. Predicting outcome
of chronic back pain using clinical predictors of psy-
chopathology: a prospective analysis. Health Psychol.
1995;14(5):415-420.
11. Gatchel RJ, Polatin PB, Mayer TG. The dominant role of
psychosocial risk factors in the development of chronic
low back pain disability. Spine. 1995;20(24):2702-2709.
12. Reme SE, Shaw WS, Steenstra IA, Woiszwillo MJ, Pransky
G, Linton SJ. Distressed, immobilized, or lacking em-
ployer support? A sub-classication of acute work-re-
lated low back pain. J Occup Rehabil. 2012;22(4):541-552.
13. Rolli Salathe C, Melloh M, Mannion AF, et al. Resourc-
es for preventing sickness absence due to low back pain.
Occup Med. 2012;62(4):273-280.
14. Shaw WS, Means-Christensen AJ, Slater MA, et al.
Psychiatric disorders and risk of transition to chro-
nicity in men with rst onset low back pain. Pain Med.
2010;11(9):1391-1400.
15. Turner JA, Franklin G, Fulton-Kehoe D, et al. Worker
recovery expectations and fear-avoidance predict work
disability in a population-based workers’ compensa-
tion back pain sample. Spine. 2006;31(6):682-689.
16. Melloh M, Elfering A, Egli Presland C, et al. Predicting
the transition from acute to persistent low back pain.
Occup Med. 2011;61(2):127-131.
17. Sewitch MJ, Rossignol M, Bellavance F, et al. First life-
time back pain and psychiatry treatment: psychological
factors and recovery in compensated workers. AAOHN J.
2000;48(5):234-242.
18. Costa Lda C, Maher CG, McAuley JH, et al. Prognosis for
patients with chronic low back pain: inception cohort
study. BMJ. 2009;339:b3829.
19. Friedman BW, Mulvey L, Davitt M, et al. Predicting
7-day and 3-month functional outcomes after an ED
visit for acute nontraumatic low back pain. Am J Emerg
Med. 2012;30(9):1852-1859 1858p.
20. Neubauer E, Junge A, Pirron P, Seemann H, Schilten-
wolf M. HKF-R 10 - screening for predicting chronicity
in acute low back pain (LBP): a prospective clinical trial.
Eur J Pain. 2006;10(6):559-566.
QQ
Diagnosis Question 4. In patients with low back pain, what history and/or physical
examination ndings are useful in determining if the cause is nonstructural in nature
and, therefore, guide treatment?
A nonstructural cause of low back pain may be considered in patients with diuse low back pain
and tenderness.
Grade of Recommendation: C
Jensen et al
1
assessed the associations between the
number of tender points and spinal structural chang-
es as well as psycho-social factors in a cross-sec-
tional study of patients who were sick-listed due to
LBP for 3-16 weeks. Participants completed a ques-
tionnaire that included information on LBP and the
Common Mental Disorders Questionnaire (CMDQ)
and underwent a clinical examination that includ-
ed a standardized assessment of tender points. Pa-
tients were classied as nonspecic LBP without leg
pain (n=96), nonspecic radiating pain (n=119), or
veried nerve root aection with relevant structur-
al lesion on MRI (n=111). A disc degeneration score
was computed based on x-ray ndings of disc height

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
56
reductions and patients were classied as “moder-
ate or severe degeneration at minimum one level”
or “no or slight degeneration at any level.” Results
revealed that many tender points on exam were as-
sociated with female sex, psychological distress and
widespread pain. Multiple tender points were neg-
atively associated with disc degeneration (DD) and
veried root involvement. The authors concluded that
the presence of multiple tender points indicates that
the pain syndrome is widespread and unlikely due to a
specic spinal cause. This study provides Level III ev-
idence that diuse back tenderness tends to indicate a
nonstructural cause.
Coste et al
2
conducted a descriptive cross-sectional
study with the aim of developing a clinical and psy-
chological classication of LBP to dene treatment
protocols. Patients presenting to an outpatient clinic
with chief complaint of LBP of any time duration were
included. Participants (n=330) completed a clinical
interview (including information on LBP and DSM-
III classication) and underwent physical and radio-
graphic examinations. Per DSM-III classication, 136
patients (41.2%) had at least one psychiatric disorder.
Diuse spinal pain, impossibility to assess intensity of
pain on a pain scale and pain increased by changing
climate, domestic activities or psychological factors
were related to the presence of a psychiatric disorder.
The authors concluded that LBP should be assessed
both physically and psychologically so that an appro-
priate management may be initiated, which may in-
clude psychiatric therapy. This study provides Level II
evidence that psychological disorders are common in
patients with nonspecic LBP. A combination of dif-
fuse spinal pain, impossibility to assess pain inten-
sity, pain increased by psychological factors, or with
changing climate and dysesthesias in the back, indi-
cates a nonorganic syndrome.
There is insucient evidence to make a recommendation for or against the use of fear avoid-
ance behavior to determine the likelihood of a structural cause of low back pain.
Grade of Recommendation: I
In a prospective cross-sectional study, Lundberg et
al
3
aimed to describe the occurrence and association
of fear-avoidance variables (pain intensity, kinesi-
ophobia, depression and disability) in patients with
specic or nonspecic chronic LBP. Participants
with LBP (n=147) were diagnosed as specic (attrib-
utable to a specic pathology such as disc hernia-
tion, isthmic spondylolisthesis and spinal stenosis)
or nonspecic (pain not able to be attributed to a
recognizable specic pathology). Upon enrollment,
participants completed questionnaires that includ-
ed information on demographics, pain duration, in-
tensity (VAS), disability (Oswestry Disability Index),
kinesiophobia (Tampa Scale of Kinesiophobia) and
depressed mood (Zung Self-Rating Depression Scale).
Both groups of patients, with either specic or non-
specic chronic LBP, had elevated fear-avoidance val-
ues. All fear-avoidance variables predicted disability
in all patients with chronic LBP with the exception of
kinesiophobia in those with nonspecic chronic LBP.
The authors concluded that pain must be analyzed and
treated, in addition to searching for the cause of pain.
This study provides Level IV evidence that the pres-
ence of fear avoidance behavior does not indicate the
absence of a specic structural cause of LBP.
There is insucient evidence to make a recommendation for or against the presence of diuse
back tenderness for the prediction of the presence of disc degeneration on radiographs.
Grade of Recommendation: I
Jensen et al
1
assessed the associations between the
number of tender points and spinal structural chang-
es as well as psycho-social factors in a cross-section-
al study of patients who were sick-listed due to LBP
for 3-16 weeks. Participants completed a question-
naire that included information on LBP and the CMDQ
and underwent a clinical examination that included
a standardized assessment of tender points. Patients
were classied as nonspecic LBP without leg pain
(n=96), nonspecic radiating pain (n=119), or veried
nerve root aection with relevant structural lesion on
MRI (n=111). A disc degeneration score was comput-
ed based on x-ray ndings of disc height reductions
and patients were classied as “moderate or severe
degeneration at minimum one level” or “no or slight
degeneration at any level.” Results revealed that many

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
57
tender points on exam were associated with female
sex, psychological distress and widespread pain. Mul-
tiple tender points were negatively associated with DD
and veried root involvement. The authors concluded
that the presence of multiple tender points indicates
that the pain syndrome is widespread and unlike-
ly due to a specic spinal cause. This study provides
Level III evidence that diuse back tenderness tends
to indicate a nonstructural cause.
Future Directions for Research
The work group recommends further prospective research evaluating the associ-
ation between psychological distress and structural abnormalities of the lumbar
spine.
References:
1. Jensen OK, Nielsen CV, Stengaard-Pedersen K. Low
back pain may be caused by disturbed pain regulation:
a cross-sectional study in low back pain patients using
tender point examination. Eur J Pain. 2010;14(5):514-
522 519p.
2. Coste J, Paolaggi JB, Spira A. Classication of nonspe-
cic low back pain. I. Psychological involvement in
low back pain: A clinical, descriptive approach. Spine.
1992;17(9):1028-1037.
3. Lundberg M, Frennered K, Hagg O, Styf J. The impact of
fear-avoidance model variables on disability in patients
with specic or nonspecic chronic low back pain. Spine.
2011;36(19):1547-1553.
QQ
Diagnosis Question 5. In patients with low back pain, what elements of the
patient’s history and ndings from the physical examination would suggest the
need for diagnostic laboratory studies?
There is insucient evidence to make a recommendation for or against obtaining laboratory
tests to assess for inammatory disease in patients with SI joint pain.
Grade of Recommendation: I
Gupta et al
1
retrospectively reviewed pain history,
clinical examination including SIJ provocative tests,
laboratory investigations and skeletal imaging to de-
scribe the clinical spectrum and propose a diagnos-
tic scheme in patients with LBP due to sacroiliac joint
(SIJ) involvement. Of the 61 patients with suspected
SIJ problems, 52 had specic SIJ pathology diagnoses;
40 of which had rheumatic conditions and 12 of which
had nonrheumatic conditions. The authors concluded
that sacroiliac joint pathology diagnosis was support-
ed by medical history, clinical examination including
sacroiliac joint tests, plain radiography and labora-
tory investigations and that a diagnostic scheme of
dividing SIJ pathologies into rheumatic and nonrheu-
matic conditions in these patients was helpful. This
study provides Level IV evidence that, in patients with
SI joint pain, laboratory tests should be considered to
assess for inammatory disease.
Future Directions for Research:
The work group recommends prospective studies of patients with sacroiliac joint
pain to dene the role of laboratory investigation in the absence of other signs of
inammatory disease.
References:
1. Gupta AD. Sacroiliac joint pathologies in low back pain.
Journ Back Musculoskel Rehabil. 2009;22(2):91-97.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
58
QQ
Diagnosis Question 7. In patients with low back pain, are there specic ndings
on a pain diagram that help dierentiate the structure which is causing pain?
Diagnosis Question 8. Are there assessment tools or questionnaires that can
help identify the cause of acute, subacute or chronic low back pain?
A systematic review of the literature yielded no studies to adequately address these questions
in this patient population.
Future Directions for Research:
Based upon a review of the available literature, the work group feels that, in the
specically-dened patient population, it is unlikely that pain diagrams are going
to elucidate the cause of LBP.
QQ
Diagnosis Question 10. Are there history and physical examination ndings that
would warrant obtaining advanced imaging studies?
A systematic review of the literature yielded no studies to adequately address this question.
Work Group Consensus Statement:
In the absence of reliable evidence supporting an absolute indication for advanced imaging based
upon history and physical examination in the specically-dened patient population, it is the work
group’s opinion that, in patients with severe and intractable pain syndromes who have failed med-
ical/interventional treatment, advanced imaging may be indicated. Subgroups of patients have
been shown to have a higher or lower incidence of radiographic abnormalities based upon acuity
of low back pain, tenderness to palpation and provocation maneuvers; however, the utility of these
ndings in guiding treatment is not clear.
Future Directions for Research:
The work group does not have any recommendations for future research on this
topic.

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Diagnosis
59
References:
1. Berg L, Hellum C, Gjertsen O, et al. Do more MRI nd-
ings imply worse disability or more intense low back
pain? A cross-sectional study of candidates for lumbar
disc prosthesis. Skelet Radiol. 2013;42(11):1593-1602.
2. Elgafy H, Semaan HB, Ebraheim NA, Coombs RJ. Com-
puted tomography ndings in patients with sacroiliac
pain. Clin Orthop. 2001(382):112-118.
3. Graves JM, Fulton-Kehoe D, Jarvik JG, Franklin GM. Ear-
ly imaging for acute low back pain: one-year health and
disability outcomes among Washington State workers.
Spine. 2012;37(18):1617-1627.
4. Kumar N, Wijerathne SI, Lim WWJ, Barry TWL, Nath C,
Liang S. Resistive straight leg raise test, resistive for-
ward bend test and heel compression test: Novel tech-
niques in identifying secondary gain motives in low
back pain cases. Eur Spine J. 2012;21(11):2280-2286.
5. Mainka T, Lemburg SP, Heyer CM, Altenscheidt J, Nico-
las V, Maier C. Association between clinical signs as-
sessed by manual segmental examination and ndings
of the lumbar facet joints on magnetic resonance scans
in subjects with and without current low back pain: a
prospective, single-blind study. Pain. 2013;154(9):1886-
1895.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
60
Section Authors
Guideline Co-Chair
Paul G. Matz, MD
Imaging Section Co-Chairs
Charles H. Cho, MD, MBA
Gary Ghiselli, MD
Members
Sean D. Christie, MD
Bernard Cohen, PhD
S. Raymond Golish, MD
Murat Pekmezci, MD
Walter Bartynski, MD, Stakeholder Representative:
American Society of Spine Radiology (ASSR)
QQ
Imaging Question 1. What is the association between low back pain and
spondylosis on routine radiography?
There is insucient evidence to make a recommendation for or against an association be-
tween low back pain and spondylosis using routine radiography.
Grade of Recommendation: I
Nemoto et al
1
conducted a longitudinal study to in-
vestigate the development of low back pain (LBP) and
lumbar degenerative changes. In 1984, 45 Japanese
male parachutists, aged 18-19 years, in the Japanese
Self Defense Forces were enrolled. None of the partic-
ipants had a history of LBP, sciatica, neurogenic clau-
dication, or abnormal lumbar spine radiographs at the
time of enrollment. In 2009, repeat radiographs were
obtained for 40 of the original subjects who then com-
pleted an updated questionnaire related to LBP (de-
ned as ≥7 consecutive days experienced during the
year prior to this study), lifestyle habits and number
of parachute descents. A single trained observer as-
sessed the radiographs and assigned summary grades
to each lumbar spine based on presence and severity
of vertebral osteophytes (VOs), disc space narrowing
(DSN) and facet joint osteoarthrosis (FJOA). The inci-
dence of VOs, DSN, or FJOA was 70%, 48% and 57%,
respectively. Mild LBP pain was reported by 60% of
subjects. Multivariate analysis demonstrated that an
increased risk of VOs was associated with number of
parachute descents (p=0.025) and DSN (p=0.014). No
signicant association was found between LBP and
various factors. However, VO development showed a
greater (nonsignicant) odds ratio (OR 3.80, 95% CI
0.95-15.20). The authors concluded that, in young
and radiologically normal parachutists, frequent
parachuting descent and newly developed DSN were
predictors of VO formation. In critique of the meth-
odology, the work group downgraded the level of evi-
dence of this potential Level III study due to the small
sample size. This study provides Level IV evidence that
there is an association between vertebral osteophyte
formation and incidence of LBP.
Nemoto et al
2
conducted a longitudinal study to inves-
tigate the association between LBP and the incidence
of newly developed lumbar degenerative changes at
middle age. In 1990, 84 Japanese infantry servicemen
in the Japanese Self Defense Forces, aged 18 years,
were enrolled after conrming normal anteroposte-
rior, lateral and bilateral oblique lumbar spine radio-
graphs. None of the enrolled participants had a his-
tory of LBP, sciatica or neurogenic claudication. In
2010, repeat radiographs were obtained for each of the
original 84 participants who then also completed an
updated questionnaire related to LBP (dened as ≥7
consecutive days experienced during the year prior to
this study) and lifestyle factors. A single trained ob-
server assessed the radiographs and assigned sum-
mary grades to each lumbar spine based on presence
and severity of vertebral osteophytes (VOs) and DSN.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
61
Mild LBP was reported by 44 subjects (52%). No as-
sociation between LBP and lifestyle factors such as
smoking, sports, alcohol intake or weight gain was
demonstrated. Lumbar degenerative changes were
found in 52% of the subjects, with DSN and VOs found
in 30% and 46% of subjects, respectively. More lum-
bar spine degeneration was found in subjects with LBP
compared to those without LBP. There was a signi-
cant correlation between VOs and LBP (OR 3.00, 95%
CI 1.23-7.33; p=0.013). There was not a signicant
association between DSN and LBP. The authors con-
cluded that, in young men without initial radiologi-
cal abnormalities, there was a signicant association
between VOs and incidence of mild LBP. In critique
of the methodology, the work group downgraded the
level of evidence of this potential Level III study due
to the small sample size. This study provides Level IV
evidence that there is an association between verte-
bral osteophyte formation and incidence of LBP.
Future Directions for Research
The work group recommends the development of studies that incorporate a
reference standard in patients without other confounding factors such as spon-
dylolisthesis or radiculopathy.
References
1. Nemoto O, Kitada A, Tsuda Y, Yokobe J, Matsukawa K,
Ukegawa Y. A longitudinal study of radiological changes
in the lumbar spine in asymptomatic Japanese military
young adults. Eur Orthop Traumatol. 2012;3(2):135-139.
2. Nemoto O, Kitada A, Naitou S, Tsuda Y, Matsukawa K,
Ukegawa Y. A longitudinal study for incidence of low
back pain and radiological changes of lumbar spine in
asymptomatic Japanese military young adults. Eur Spine
J. 2013;22(2):453-458.
QQ
Imaging Question 2. In patients with low back pain, what elements of the patient’s
history and ndings from the physical examination would suggest the need for
diagnostic laboratory studies?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends development of studies investigating the use of
MRI or CT scans for the evaluation of LBP in the absence of radiographic abnor-
mality.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
62
QQ
Imaging Question 3. In patients with low back pain, does duration of symptoms
correlate with abnormal ndings on imaging?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends development of longitudinal studies that include
both clinical and imaging ndings.
QQ
Imaging Question 4. What is the optimal imaging protocol that should be used in
the setting of low back pain?
a. Are unique MRI sequences considered preferential or optimal?
There is insucient evidence that unique magnetic resonance imaging (MRI) sequences can be
considered preferential or optimal.
Grade of Recommendation: I
Lakadamyali et al
1
conducted a retrospective case
control study to investigate the relationship between
degenerative changes in posterior spinal elements
and LBP, as well as to explore the age- and sex-re-
lated distribution of those changes on STIR sequence
magnetic resonance (MR) images. In the rst stage of
this two-stage study, the MR images of 372 patients
(231 women, 141 men) with LBP without radiculopa-
thy were evaluated after being referred to a radiology
department between the years 2000-2004. During the
second stage, 249 additional volunteers (123 women,
126 men) without LBP who were referred to the same
department for other MRI examinations, formed a
control group. Conventional and sagittal STIR se-
quences were obtained for all subjects. Two experi-
enced radiologists evaluated the lumbar MR images
and recorded presence of intervertebral disc degen-
eration (DD), disc herniation, interspinous ligament
degeneration or rupture, facet joint eusion, neocyst
formation, intrinsic spinal muscular degeneration
and/or subcutaneous edema. Compared to patients
without LBP, patients with LBP had higher incidenc-
es of facet joint eusion (p=0.0001), interspinous
ligament edema (p=0.001 for T12-L1; p=0.0001 for
all lumbar levels), neocyst formation (p=0.0001) and
intrinsic muscle degeneration (p=0.0001). The inci-
dences of intervertebral DD, disc herniation, subcuta-
neous edema and muscle edema were similar in sub-
jects with and without LBP, but increased with age in
both groups. Relevant posterior paraspinal changes
were better visualized with STIR imaging than rou-
tine MRI. The authors concluded that the percentage
of posterior paraspinal degenerative change ndings
was higher in subjects with LBP compared to those
without LBP and that the use of the STIR sequence im-
proved the visualization of those changes. This study
provides Level III evidence that patients with LBP had
signicantly higher rates of facet joint eusion, in-
terspinous ligament edema, neocyst formation and
paraspinal muscle edema. The incidence of interver-
tebral DD, disc herniation and subcutaneous edema in
persons with and without LBP were similar.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
63
QQ
b. What is the history and clinical presentation that suggests the use of contrast
enhanced imaging in patients with low back pain?
A systematic review of the literature yielded no studies to adequately address this question.
A systematic review of the literature yielded no studies to adequately address this question.
A systematic review of the literature yielded no studies to adequately address this question.
QQ
c. Is there evidence to support imaging the lumbar spine in an oblique plane?
QQ
d. What is the value of exion/extension lms in evaluating lower back pain?
Future directions for Research
The work group recommends that future imaging studies relative to LBP include
subgrouping of relevant populations. In order to assess a specic imaging pro-
tocol, the work group recommends a prospective study evaluating patients with
and without nonspecic low back pain.
Reference
1. Lakadamyali H, Tarhan NC, Ergun T, Cakir B, Agildere
AM. STIR sequence for depiction of degenerative chang-
es in posterior stabilizing elements in patients with
lower back pain. AJR Am J Roentgenol. 2008;191(4):973-
979.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
64
QQ
Imaging Question 5. In the absence of red ags, what are the imaging (x-ray, CT
or MRI) recommendations for patients with acute or chronic low back pain?
There is insucient evidence to make a recommendation for or against obtaining imaging
in the absence of red ags.
Grade of Recommendation: I
One Level II study shows that in the absence of red
ags, x-ray does not provide additional benet at
initial consultation. Kerry et al
1
performed a random-
ized controlled trial (RCT) with an observational arm
across 94 general practices in South London and the
South Thames region in order to compare outcomes of
patients with LBP who were immediately referred for
lumbar spine x-ray with those who were not. Over the
course of 26 months, patients with LBP, aged 16-64
years, were allocated into a RCT (n=153) or an obser-
vational arm (n=506) at the time they consulted their
general practitioners. Allocation into these groups
was determined by sealed envelope or per the discre-
tion of the individual practitioner. The patients in the
RCT group were then randomized into an immediate
x-ray referral group (n=73) or no immediate x-ray
referral (control) group (n=80). Subjects were includ-
ed in the nal analysis if they completed a question-
naire which included the back-pain specic Roland
Morris Disability Questionnaire (RMDQ), the Hospital
Anxiety and Depression Scale (HADS) and the short
form health survey SF-36 at the time of enrollment,
6 weeks and one year later (response rate at one year
was 67%). In the RCT, those who had been immedi-
ately referred for radiography had no dierences in
physical functioning, pain, or disability compared to
the control group. However, the subjects in the im-
mediate radiography group scored higher on psycho-
logical wellbeing at 6 weeks and one year compared to
the control group. Similar ndings were observed in
the observational study in which, after adjusting for
length of back pain episode at presentation, there were
no dierences in physical outcomes between groups.
Those referred for x-ray had lower depression scores
at six weeks and one year. The authors concluded that,
unless patient anxiety is a major factor, it is not rec-
ommended to routinely refer for early x-ray for LBP
as it is not associated with improvement of physical
functioning, pain or disability. The work group down-
graded this potential Level I study due to poor fol-
low-up, signicant crossover and potential bias. This
study provides Level II evidence that, in the absence of
red ags, x-ray does not provide additional benet at
initial consultation.
Future directions for Research
The work group recommends studies to evaluate the value of imaging (x-ray, CT
or MRI) for patients with acute or chronic LBP in the absence of red ags.
Reference
1. Kerry S, Hilton S, Dundas D, Rink E, Oakeshott P. Radi-
ography for low back pain: a randomised controlled trial
and observational study in primary care. Br J Gen Pract.
2002;52(479):469-474.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
65
QQ
Imaging Question 6. Are there imaging ndings that correlate with the presence of
low back pain?
There is insucient evidence for or against imaging ndings correlating with the presence of
low back pain.
Grade of Recommendation: I
Carragee et al
1
investigated the association between
new and serious LBP episodes with MRI ndings of
200 subjects in a 5-year prospective observational
study. Working subjects with risk factors for degener-
ative lumbar disc disease but without a history of clin-
ical LBP episodes underwent a physical examination
with plain radiographs, lumbar spine MRI and a de-
tailed interview at enrollment, 6 months and 5 years.
The detailed interview included using a visual analog
scale (VAS) for LBP intensity, Modied Oswestry Low
Back Disability Questionnaire for subjective function-
al assessment and modied psychometric studies. If a
new serious LBP episode with a rating scale intensity
≥6 for ≥1 week was reported, MR imaging taken within
6-12 weeks of the episode was compared with base-
line images. MR images were assessed by 2 indepen-
dent blinded examiners. Outcome measures includ-
ed MR ndings (DD, annular disruption, herniation,
moderate-severe endplate changes, spinal stenosis or
neurologic compression, serious back pain episodes
and occupation compensation or disability claims due
to LBP. A total of 51 subjects had repeat scans avail-
able. The most common progressive ndings were
disc signal loss, facet arthrosis and endplate changes.
Subjects having another MR were more likely to have
had baseline psychological distress (OR 2.27, 95%
CI 1.15-4.49). Radicular symptoms were the primary
reason for three of the repeat scans. Only 2 subjects
with primary radicular complaints had new ndings
of probable clinical signicance. The authors con-
cluded that it was highly unlikely that new ndings on
MRI within 12 weeks of serious LBP represent any new
structural change as many of the changes were relat-
ed to progressive age changes. The work group noted
that although there was a subgroup analysis, the mix
of back and radicular pain resulted in a small patient
population with only LBP. Therefore, the work group
downgraded this potential Level II study. This study
provides Level III evidence that, in the setting of new
back pain, MRI is highly unlikely to detect new struc-
tural disease and instead represents existing struc-
tural disease.
Cho et al
2
conducted a cross-sectional study to eval-
uate the prevalence and risk factors of LBP in mid-
dle-age and elderly residents of a rural community in
South Korea. All participants were a part of the Korean
Health and Genome cohort (aged 40-79 years). A total
of 1,772 subjects had lumbar spine radiographs avail-
able. A single rheumatologist reviewed the radio-
graphs and graded the presence and severity of an-
terior osteophytes, endplate sclerosis and joint space
narrowing using a reference atlas. Each vertebral
level was graded using the Kellgren-Lawrence (K-L)
grading system. Each subject completed a question-
naire that included information on lifestyle habits and
self-report of LBP (current, past 6 months and life-
time) using the 7-item Guttman scale to classify pain
intensity. Based on the results, the authors conclud-
ed that risk factors associated with either current or
lifetime LBP included advanced age, female sex, time
spent squatting, presence of osteophytes, joint space
narrowing and advanced K-L grading; there was no
association between presence of endplate sclerosis
and LBP. This study provides Level III evidence that
presence of disc space narrowing and osteophytes,
but not presence of endplate sclerosis, correlates with
LBP.
Lakadamyali et al
3
conducted a retrospective case
control study to investigate the relationship between
degenerative changes in posterior spinal elements
and LBP, as well as to explore the age- and sex-re-
lated distribution of those changes on STIR sequence
magnetic resonance (MR) images. In the rst stage
of this 2-stage study, the MR images of 372 patients
(231 women, 141 men) with LBP without radiculopa-
thy were evaluated after being referred to a radiology
department between the years 2000-2004. During the
second stage, 249 additional volunteers (123 women,
126 men) without LBP who were referred to the same
department for other MRI examinations, formed a
control group. Conventional and sagittal STIR se-
quences were obtained for all subjects. Two experi-
enced radiologists evaluated the lumbar MR images

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
66
and recorded presence of intervertebral DD, disc her-
niation, interspinous ligament degeneration or rup-
ture, facet joint eusion, neocyst formation, intrinsic
spinal muscular degeneration and/or subcutaneous
edema. Compared to patients without LBP, patients
with LBP had higher incidences of facet joint eusion
(p=0.0001), interspinous ligament edema (p=0.001
for T12-L1; p=0.0001 for all lumbar levels), neocyst
formation (p=0.0001) and intrinsic muscle degen-
eration (p=0.0001). The incidences of intervertebral
DD, disc herniation, subcutaneous edema and muscle
edema were similar in subjects with and without LBP,
but increased with age in both groups. Relevant pos-
terior paraspinal changes were better visualized with
STIR imaging than routine MRI. The authors conclud-
ed that the percentage of posterior paraspinal degen-
erative change ndings was higher in subjects with
LBP compared to those without LBP and that the use
of the STIR sequence improved the visualization of
those changes. This study provides Level III evidence
that patients with LBP had signicantly higher rates
of facet joint eusion, interspinous ligament edema,
neocyst formation and paraspinal muscle edema. The
incidence of intervertebral DD, disc herniation and
subcutaneous edema in persons with and without LBP
were similar.
Liu et al
4
conducted a prospective comparative and
reliability study in order to develop and evaluate a
quantitative assessment of the high-intensity zone
(HIZ) on magnetic resonance imaging (MRI) in pa-
tients with LBP compared to those without LBP. A to-
tal of 72 patients (40 males, 32 females, aged 24-59
years) with LBP for ≥ 6 months were enrolled into the
symptomatic group (group A). All subjects underwent
MRI scanning to conrm absence of potential non-
discogenic LBP sources. A total of 79 patients without
LBP who presented to the hospital for routine health
examinations or minor extremity injuries (44 males,
35 females, aged 23-59 years) were enrolled into an
asymptomatic control group (group B). All subjects
underwent MR imaging. HIZ was recorded using Pic-
ture Archiving and Communication System (Jin YeX-
iang, Beijing, China). Blinded, experienced radiol-
ogists evaluated the images. The incidence of HIZ in
symptomatic group A (45.8%) was signicantly high-
er than asymptomatic group B (20.2%) (p=0.001). The
intensity of the HIZ signal was signicantly brighter
in symptomatic group A (57.55 ± 14.04%) compared
to asymptomatic group B (45.61 ±- 7.22%) (p=0.000).
There were no signicant dierences in area of disc
and HIZ nor the area ratio between group A and group
B. The authors concluded that HIZ intensity is greater
in subjects with LBP compared to those without LBP.
In critique of the methodology, the work group down-
graded this potential Level II study as the study arm
was retrospective rather than prospective. This study
provides Level III evidence that HIZ intensity is great-
er in patients with LBP compared to controls.
Maatta et al
5
examined the relationship between Mod-
ic change (MC) and severe, disabling LBP along with
features of DD in a longitudinal cohort study of twins.
All subjects completed a comprehensive nurse-led
questionnaire related to LBP and underwent lumbar
MRI at baseline (n=823, 95.7% female) and after 10
years (n=429, 98.1% female). A single blinded observ-
er evaluated all MR images to assess for MC and DD.
A second reader evaluated a select subset of images
to conrm acceptable inter-rater reliability. Subjects
with severe and disabling LBP ≥ 1 month were more
likely to have MC at baseline (subjects with MC: 35.0%
vs. subjects without MC: 16.4%, p<0.001) and at fol-
low-up (subjects with MC: 35.1% vs subjects without
MC: 20.0%, p<0.001). After adjusting for age, BMI,
DD and Schmorl’s nodes (SN) at baseline, there was
a signicant association between severe, disabling
LBP and MC (OR 1.58, 95% CI 1.04-2.41). The authors
concluded that MC is an independent risk factor for
episodes of severe and disabling LBP in middle-aged
women. In critique of the methodology, the work-
group downgraded this potential Level III study due
to poor follow-up. This study provides Level IV evi-
dence that Modic changes are associated with severe
disabling back pain.
Riihimaki et al
6
studied the relationship between LBP
and lumbar spinal degeneration in concrete workers
(n=216) and house painters (n=201). Each participant
completed a self-administered questionnaire (related
to occupation history, back accidents and smoking)
and a physiotherapist-administered interview relat-
ed to back symptoms. Demographic information and
lumbar radiographs were obtained. A radiologist re-
viewed the radiographs and recorded the presence of
disc space narrowing, vertebral osteophytes (spondy-
lophytes) and endplate sclerosis for each of the lumbar
intervertebral spaces using a graded system. Although
there was a trend of increasing LBP with increased se-
verity of degeneration, there was no statistical signif-
icance. The authors concluded that there was an as-
sociation between moderate to severe degenerative
changes and increased risk of sciatic pain. However,
there were no signicant correlations between these
changes and occurrence of back pain. This study pro-
vides Level III evidence that degenerative changes on
imaging were not associated with increased risk of the
occurrence of nonspecic LBP.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
67
Teraguchi et al
7
examined the associations between
LBP and combinations of DD, endplate signal change
(ESC) and Schmorl node (SN) in a cross-sectional
study of 975 patients (324 men, 651 women, aged 21-
97 years) in Japan. Participants were recruited from
the Research on Osteoarthritis/Osteoporosis against
Disability (ROAD) cohort and included in this study af-
ter agreeing to a whole-spine MRI. T2-weighted im-
ages were obtained for all subjects used to assess DD,
ESC and SN from L1-L2 to L5-S1. A board-certied or-
thopedic surgeon, who was blinded to the background
of the participants, classied the degree of DD and the
presence of ESC and/or SN. Kappa analysis to describe
intraobserver and interobserver variability was com-
pleted for scoring of two orthopedic surgeons for DD,
ESC and SN. LBP was diagnosed based on a standard-
ized question asked by board-certied orthopedic
surgeons. The overall prevalence of DD alone (30.4%)
was highest compared to ESC alone (0.8%), SN alone
(1.5%), DD and ESC (26.6%), DD and SN (12.3%), SN
and ESC (0.6%) and DD, ESC and SN (19.1%). A combi-
nation of DD, ESC and SN was signicantly associated
with LBP (OR 2.17, 95% CI 1.2-3.9; p<0.01). Addition-
ally, signicant associations with LBP were found in
a combination of DD, ESC and SN at L1-L2 (OR 6.00,
95% CI 1.9-26.6; p<0.005), L4-L5 (OR 2.56, 95% CI
1.4-4.9; p<0.005) and L5-S1 (OR 2.85, 95% CI 1.1-2.3;
p<0.05) as well as a combination of DD and ESC at L3-
L4 (OR 2.43, 95% CI 1.5-4.0; p<0.05), L4-L5 (OR 1.82,
95% CI 1.2-2.8; p<0.01) and L5-S1 (OR 1.60, 95% CI
1.1-2.3; p<0.05). The authors concluded that although
DD alone is not associated with LBP, a combination
of DD and ESC, with or without SN, was signicantly
associated with LBP. Although there were some lim-
itations to the methodology as only T2 images were
available, the work group did not nd this sucient
reason to downgrade the study. This study provides
Level II evidence that a combination of degenerative
changes shows high correlation to LBP.
Wiikeri et al
8
studied the relationship between lum-
bar DD and LBP in 295 Finnish concrete workers aged
19-64 years. After each participant was radiological-
ly examined, a radiologist and an orthopedic surgeon
evaluated each participant’s radiograph and graded
lumbar DD as none, slight (12%), moderate (23%) or
severe (9%). After adjusting for age, there was a weak
association between history of LBP and DD (p<0.01).
There was also a weak association between history of
sciatica and DD (p<0.001). The authors concluded that
there is a weak association between lumbar DD and
LBP or sciatica, independent of age. This study pro-
vides Level IV evidence that lumbar degeneration has
a weak correlation with LBP.
Future directions for Research
The work group recommends separation between radicular pain and LBP
groups, inclusion of an asymptomatic reference group and inclusion of a refer-
ence standard in a well-powered study.
References
1. Carragee E, Alamin T, Cheng I, Franklin T, van den Haak
E, Hurwitz E. Are rst-time episodes of serious LBP as-
sociated with new MRI ndings? Spine J. 2006;6(6):624-
635.
2. Cho, N.H., Jung, Y.O., Lim, S.H., Chung, C.K., Kim, H.A.
The prevalence and risk factors of low back pain in ru-
ral community residents of Korea. Spine. 2012;37:2001–
2010.
3. Lakadamyali H, Tarhan NC, Ergun T, Cakir B, Agildere
AM. STIR sequence for depiction of degenerative chang-
es in posterior stabilizing elements in patients with
lower back pain. AJR Am J Roentgenol. 2008;191(4):973-
979.
4. Liu C, Cai HX, Zhang JF, Ma JJ, Lu YJ, Fan SW. Quantita-
tive estimation of the high-intensity zone in the lum-
bar spine: comparison between the symptomatic and
asymptomatic population. Spine J. 2014;14(3):391-396
396p.
5. Maatta JH, Wadge S, MacGregor A, Karppinen J, Wil-
liams FMK. ISSLS prize winner: Vertebral endplate
(Modic) change is an independent risk factor for ep-
isodes of severe and disabling low back pain. Spine.
2015;40(15):1187-1193.
6. Riihimaki H, Wickstrom G, Hanninen K, Mattsson T,
Waris P, Zitting A. Radiographically detectable lumbar
degenerative changes as risk indicators of back pain. A
cross-sectional epidemiologic study of concrete rein-
forcement workers and house painters. Scand J Work En-
viron Health. 1989;15:280–285.
7. Teraguchi M, Yoshimura N, Hashizume H, et al. The as-

Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
Diagnosis & Treatment of Low Back Pain | Recommendations | Imaging
68
sociation of combination of disc degeneration, end plate
signal change, and Schmorl node with low back pain in
a large population study: the Wakayama Spine Study.
Spine J. 2015;15(4):622-628.
8. Wiikeri, M., Nummi, J., Riihimaki, H., Wickstrom. Ra-
diologically detectable lumbar disc degeneration in
concrete reinforcement workers. Scand J Work Environ
Health. 1978;4:47–53
QQ
Imaging Question 7. Are there imaging ndings that contribute to decision-making
by health care providers to guide treatment?
There is insucient evidence to determine whether imaging ndings contribute to decision-
making by health care providers to guide treatment.
Grade of Recommendation: I
Pneumaticos et al
1
conducted a prospective random-
ized controlled trial to evaluate the use of bone scin-
tigraphy with single photon emission computed to-
mography (SPECT) in 47 adult patients (23 men and
24 women) with low back pain who were referred
for facet joint injection. The patients were random-
ized into group A or group B (with a ratio of 2:1 for
patients in group A to group B). Bone scanning with
SPECT was used for group A. If abnormalities were
found, these patients were further categorized into
group A1 (n=15) and injections were given at the lev-
el of the spine in which facet joint abnormalities were
found on the scan. If no abnormalities were found, the
patients were categorized into group A2 (n=16) and
injections were given at the level originally indicated
by the referring physician. Group B (n=16) underwent
injections at the level originally indicated by the re-
ferring physician, without SPECT bone scanning. All
participants completed a validated pain and function
questionnaire before the injection and after 1, 3, and
6 months. There was no signicant dierence be-
tween groups in average pain score at baseline. At one
month, 87%, 13%, and 31% of patients in group A1,
group A2, and group B, respectively, reported positive
improvement in pain. The change in pain score was
signicantly higher in group A1 than group A2 and
group B after one month and 3 months, but there was
no dierence after 6 months. The authors concluded
that bone scintigraphy with SPECT can help identi-
fy patients with LBP who have been referred for facet
joint injections. In critique of the methodology, the
work group downgraded this potential Level I study
due to a small sample size. Therefore, this study pro-
vides Level II evidence that bone scintigraphy with
SPECT can help identify patients with LBP.
Future directions for Research
The work group recommends designing studies focused on the role of imaging
in health care decision-making related specically to LBP.
Reference
1. Pneumaticos SG, Chatziioannou SN, Hipp JA, Moore
WH, Esses SI. Low back pain: prediction of short-term
outcome of facet joint injection with bone scintigraphy.
Radiology. 2006 Feb;238(2):693-8.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
69
Section Authors
Guideline Co-Chair
Paul G. Matz, MD
Medical and Psychological Treatment Section
Chair
Christopher M. Bono, MD
Members
Paul Dougherty, DC
Gazanfar Rahmathulla, MD
Christopher K. Taleghani, MD
Terry R. Trammell, MD
Randall Brewer, MD, Stakeholder Representative:
American Academy of Pain Medicine (AAPM)
Ravi Prasad, PhD, Stakeholder Representative: American
Academy of Pain Medicine (AAPM)
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
QQ
Med/Psych Question 1. Is smoking cessation eective in decreasing the
frequency of low back pain episodes?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends further population-based observational studies
that investigate the association between low back pain (LBP) and smoking. Spe-
cically, a study comparing the frequency of LBP episodes between patients who
have quit smoking and those who continue to smoke would be useful.
QQ
Med/Psych Question 2. In patients with low back pain, is pharmacological
treatment eective in decreasing duration of pain, decreasing intensity of pain,
increasing functional outcomes of treatment and improving the return-to-work
rate?
versus:
a. No treatment
i. Risks
ii. Complications
b. Cognitive behavioral therapy (CBT) and/or psychosocial intervention alone
c. Patient education alone

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
70
Antidepressants are not recommended for the treatment of low back pain
Grade of Recommendation: A
Atkinson et al
2
conducted a double-blind random-
ized controlled trial with head-to-head comparison
to evaluate the relative ecacy of noradrenergic and
serotonergic antidepressants to treat chronic LBP in
patients without depression. Participants aged 21-
65 years with chronic LBP ≥6 months who met study
inclusion criteria were enrolled and randomized into
groups using a stratied allocation scheme based on
presence of radicular pain. Participants in the mapro-
tiline (n=33), paroxetine (n=34) and diphenhydr-
amine hydrochloride active placebo (n=36) groups
were instructed to take a single capsule at the same
time each day. Each drug dosage was increased ev-
ery 3 days as tolerated to the maximum range that is
used for antidepressant dosage. Participants were in-
terviewed weekly to determine side eects. Pain in-
tensity using the Descriptor Dierential Scale (DDS)
and mood measures were obtained at enrollment and
exit of the study. A total of 20, 22 and 32 participants
in the maprotiline, paroxetine and placebo groups,
respectively, completed the trial. Based on analyses
of participants who completed the trial, the partici-
pants had an average pain intensity decrease of 45%,
26% and 27% on maprotiline, paroxetine and place-
bo, respectively. The participants in the maprotiline
group had signicantly greater reduction in pain in-
tensity compared to paroxetine (p=0.013) and placebo
(p=0.023). There was no dierence in pain intensity
reduction from paroxetine compared to placebo. Us-
ing an intent-to-treat analysis, pain intensity re-
duction was greater with maprotiline compared to
paroxetine (p=0.028) but not compared to placebo
(p=0.275). The most frequent adverse events reported
were dry mouth, insomnia and sedation. The authors
concluded that noradrenergic agents may be more
eective analgesic agents than selective serotoner-
gic reuptake inhibitors. In critique of the methodol-
ogy, the work group downgraded this potential Level
I study due to the rapid dose escalation and less than
80% follow-up. This study provides Level II evidence
that noradrenergic agents such as maprotiline are
associated with greater reductions in LBP compared
with selective serotonin reuptake inhibitors in non-
depressed patients with chronic LBP.
Dickens et al
3
conducted a randomized controlled trial
to determine if paroxetine is more eective at reducing
depression and pain than placebo. Patients with LBP
(aged 18-65 years) were included in this study, given
a placebo for 7 days and then randomized to receive
either 20 mg paroxetine (n=44) or placebo (n=48) for
the remainder of the study. Assessments were com-
pleted after 14, 28 and 56 days (±3 days each). At each
assessment, measurements obtained included sever-
ity of depressive symptoms using MADRS, diagnosis
of depression per DSM-III-R, pain intensity using a
Muehlbacher et al
1
studied the ecacy of topira-
mate for the treatment of chronic LBP in a random-
ized, double-blind, placebo-controlled study. Par-
ticipants with chronic LBP were recruited through
advertisements and randomized into the topiramate
group (n=48) or placebo group (n=48). Each partici-
pant completed the McGill pain Questionnaire (MPQ),
State-Trait Anger Expression Inventory (STAXI), Os-
westry Low Back Pain Disability Questionnaire (OLB-
PQ) and and SF-36 Health Survey (SF-36) during a
face-to-face interview at the time of enrollment and
weekly for the duration of the study. After a one-week
period in which participants were asked not to use an
analgesic or anti-inammatory medication, they re-
ceived daily study medication for 10 weeks. The par-
ticipants in the topiramate group received 50 mg of
topiramate per day which was titrated at 50 mg/week
to 300 mg/d by week 6 through week 10. Using an in-
tent-to-treat analysis, the participants in the topira-
mate group had signicantly greater improvements
in MPQ (p<0.001), STAXI (p<0.001), OLBPQ (p<0.001)
and and SF-36 (p<0.001) compared to the partici-
pants in the placebo group. Adverse events such as
severe somnolence, vision problems, psychomotor
slowing, memory problems, dizziness, headache and
paresthesia were reported, but there were no serious
side eects reported. The authors concluded that the
study drug is safe and eective in treating chronic
LBP. This study provides Level I evidence that topira-
mate is more eective than placebo for the treatment
of chronic LBP over 10 weeks.
There is insucient evidence to make a recommendation for or against the use of anticon-
vulsants for the treatment of low back pain.
Grade of Recommendation: I
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
71
100-mm Visual Analog Scale (VAS) and short-form of
the McGill Pain Questionnaire (MPQ), disability using
the Oswestry Low Back Pain Disability Questionnaire
(ODQ) and health cognitions using the Illness Attitude
Scale (IAS). In an intention-to-treat analysis, there
were no signicant dierences in depression symp-
toms (MADRS), pain intensity (VAS) or disability per
Owestry Disability Index (ODI). However, subjects in
the paroxetine group were more likely to reduce their
intake of analgesia (n=4) compared to subjects in the
placebo group (n=1). In an analysis of patients who
took all pills as prescribed and attended all appoint-
ments, there were no signicant dierences between
the placebo group (n=34) or paroxetine group (n=27)
regarding depression, pain or disability. The authors
concluded that paroxetine showed no eects on pain
or depression compared to placebo. This study pro-
vides Level I evidence that treatment with paroxetine
is no better than placebo at 56 days follow-up.
Goodkin et al
4
assessed the ecacy of trazadone
hydrochloride for the relief of LBP in a multicenter,
randomized controlled trial. Adults with current LBP
≥2 weeks which had either been continuous ≥1 year
or with at least 2 prior LBP episodes ≥2 weeks were
randomized to receive 50 mg trazadone (n=22) or
placebo (n=20) tablets. Participants were instructed
to start with one tablet per day and increase at inter-
vals of 3 days as tolerated to a maximum of 4 tablets 3
times a day was reached. A 10-point VAS was used to
rate pain every 12 hours at baseline; results were col-
lected at biweekly visits. Additionally, the Beck De-
pression Inventory (BDI) and Sickness Impact Prole
(SIP) were used to assess depressed mood and daily
life function, respectively. There were no signicant
dierences in VAS scores between groups. Side ef-
fects of constipation, orthostatic hypotension, light-
headedness/dizziness, sedation/lethargy, dry mouth
and confusion were reported more frequently in the
trazadone group than placebo. The authors conclud-
ed that trazadone did not have any signicant treat-
ment eects in patients with LBP. This study provides
Level II evidence that trazadone HCL is not more ef-
fective than placebo/no treatment for chronic LBP in
the short-term study.
Skljarevski et al
5
assessed the ecacy of duloxetine
for the treatment of chronic LBP in a multicenter,
double-blind, randomized controlled trial. Patients
with LBP ≥6 months who met inclusion criteria were
enrolled in a one-week screening phase. Eligible
participants were then randomized, stratied by
reported regular analgesic/NSAID usage, to receive
a placebo (n=117) or duloxetine at 20 mg (n=59), 60
mg (n=116), or 120 mg (n=112). During this 13-week
treatment phase, participants recorded average 24-
hour pain ratings in a daily diary. A total of 267 (66.1%)
of participants completed the study. The patients
taking 60 mg duloxetine had signicantly improved
weekly pain from weeks 3 through 11, but not at weeks
12 and 13. The patients receiving duloxetine 60 mg had
signicantly improved Patient’s Global Impressions
of Improvement (PGI-I), 24-item Roland-Morris
Disability Questionnaire (RMDQ), Brief Pain Inventory
(BPI) average pain and BPI average interference.
There were no signicant dierences between groups
in occurrence of serious adverse events. Treatment-
emergent adverse events included nausea, insomnia,
dry mouth, constipation, headache, diarrhea,
dizziness, somnolence and fatigue. There were
signicantly more treatment-emergent adverse
events in the 120 mg duloxetine group compared to
the placebo. The authors concluded that duloxetine
was superior to placebo for pain relief only from weeks
3-11, but was superior to placebo for other secondary
measures. In critique of the methodology, the work
group downgraded the Level of evidence due to less
than 80% follow-up. This study provides Level II
evidence that duloxetine has no statistical benet on
pain or function in chronic LBP patients at 12 weeks.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
72
There is insucient evidence to make a recommendation for or against the use of Vitamin D for
the treatment of low back pain
Grade of Recommendation: I
In a double-blind randomized clinical trial, Sandoughi
et al
6
studied the eect of vitamin D on LBP. Patients
aged 18-40 years with chronic LBP >3 months were
recruited from a rheumatology clinic and randomized
to receive either 50,000 IU vitamin D (n=26) or pla-
cebo (n=27) once a week for 8 weeks. All participants
were encouraged to exercise at home and were given
celecoxib to use as needed (up to 200 mg per day) for
back pain. Severity of pain was assessed at baseline
and after the 8-week trial using a VAS. At trial com-
pletion, both groups had signicant improvements in
mean VAS scores and chronic pain with no signicant
dierences between groups. There was no signicant
dierence between groups for usage of celecoxib. The
authors concluded that there were no signicant dif-
ferences between vitamin D3 and placebo groups as
both improved chronic LBP. This study provides Lev-
el II evidence that vitamin D is no more eective than
placebo for treatment of chronic LBP.
Non-selective NSAIDs are suggested for the treatment of low back pain.
Grade of Recommendation: B
There is insucient evidence to make a recommendation for or against the use of selective
NSAIDs for the treatment of low back pain
Grade of Recommendation: I
Birbara et al
7
conducted a double-blind, randomized,
placebo-controlled trial across 46 centers in the
United States. Adults with LBP for ≥3 months who
regularly used an NSAID or acetaminophen for 30
days prior to enrollment were included in this study.
They were classied into two groups: LBP without
radiation to the extremities or LBP with radiation
to extremities but not below the knee and without
neurological signs. At enrollment, each participant
underwent a physical exam and completed the LBP
intensity scale, low back pain bothersomeness scale,
Patient Global Assessment of Disease Status (PGADS),
Roland-Morris Disability Questionnaire (RMDQ), 27
Hospital Anxiety and Depression Scale (HADS) and
the Patient Health Survey (MOS Short Form [SF]-
12). If, after a 4-15 day washout period abstaining
from their previous use of NSAID or acetaminophen,
the patients had a LBP intensity scale score ≥40 mm
which increased by at least 10 mm from baseline
and a worsened PGADS score by at least 1 point,
they remained enrolled. Patients were randomized
into one of three groups: 90 mg dose of etoricoxib
(n=107), 60 mg dose of etoricoxib (n=103), or placebo
(n=109). They were instructed to take the study pill
once daily and return after 1, 2, 4, 8 and 12 weeks to
measure vital signs and undergo physical and safety
assessments. The completion rates for the placebo,
60 mg etoricoxib and 90 mg etoricoxib groups were
59.6%, 72.8% and 67.3%, respectively. There were no
signicant dierences in results between intent-to-
treat and per-protocol analyses. Compared to placebo,
both etoricoxib groups had signicant improvements
in back pain intensity after 4 weeks (p≤0.001) and 12
weeks (p≤0.05). Signicantly dierent improvements
in RMDQ, LBP bothersomeness scale, PGADS and
patient and investigator-global assessment of
response to therapy were also observed in both
etoricoxib doses compared to placebo after 4 and 12
weeks. There were no signicant dierences between
reported clinical adverse events between the placebo
(46.8%), 60 mg etoricoxib (58.3%) and 90 mg
etoricoxib (52.3%) treatment groups. Compared to
placebo group, the incidence of adverse events that the
investigator judged as drug-related was high in the 90
mg etoricoxib group, but not in the 60 mg etoricoxib
group. The authors concluded that compared to
placebo, etoricoxib once daily provided signicant
improvement in chronic LBP-related symptoms and

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
73
disability after one week, with a maximal eect at 4
weeks, for up to 3 months. This study provides Level I
evidence that COX-2 inhibitors at two dierent doses
have a mild eect on chronic LBP. However, this eect
did not reach clinical signicance as dened as 20 mm
improvement on VAS.
Pallay et al
8
evaluated the ecacy and safety of
etoricoxib for LBP in a randomized multicenter,
double-blind, placebo-controlled trial. Adults aged
18-75 years with LBP >3 months and regularly treated
with NSAID or paracetamol for ≥30 days who met
inclusion criteria were enrolled in this 12-week study
across 46 outpatient centers. After a 4-25 day washout
period of analgesic discontinuation, participants were
randomized to take once-daily etoricoxib 60 mg
(n=109), etoricoxib 90 mg (n=106), or placebo (n=110)
using a double-dummy approach. Patients were
evaluated and completed questionnaires at baseline
and 1, 2, 4, 8 and 12 weeks postrandomization.
Outcomes measured included LBP intensity
using a 0-100 mm VAS, Roland-Morris Disability
Questionnaire (RMDQ), LBP bothersomeness, patient
global assessment of disease status and the Patient
Health Survey (MOS Short Form [SF]-12). A total
of 231 participants completed the study (77 in each
group) with over 95% compliance in each group. An
intention-to-treat analysis found the etoricoxib 60
mg and 90 mg groups had signicantly improved
RMDQ scores at 12 weeks and decreased LBP intensity
at 4 and 12 weeks compared to the control group. The
per-protocol analysis was not signicantly dierent.
There were no signicant dierences in adverse
events between groups. The authors concluded that
etoricoxib provided relief in LBP symptoms and
disability at 1 week, 4 weeks and 3 months. The work
group downgraded this potential Level I study due
to low follow-up rate, potential bias to responders
to NSAIDS and no active comparator in this trial to
compare against other NSAIDs. This study provides
Level II evidence that etoricoxib can reduce chronic
LBP better than placebo for up to three months.
Dreiser et al
9
conducted a multicenter, double-blind,
double-dummy, randomized controlled trial to assess
the safety and ecacy of diclofenac-K (12.5 mg tab-
let) compared to placebo and ibuprofen (200 mg) for
acute LBP. Patients aged 18-60 years with acute LBP
≥50 mm on a 100 mm VAS were randomized into a
12.5 mg diclofenac-K group (n=124), 200 mg ibupro-
fen group (n=122), or placebo group (n=126). All par-
ticipants were instructed to follow a exible multiple
dosing regimen by taking 2 tablets initially, then 1-2
tablets every 4-6 hours, not to exceed 6 tablets per
day, while recording frequency of each dosage in a di-
ary. They were given the option to take a rescue med-
ication, paracetamol, which would terminate par-
ticipation in the trial. Each participant recorded pain
(4-point scale) and pain relief (5-point scale) at 30
minutes after initial trial drug and after each hour for
6 hours. The End of First Dose (FD) global assessment
of ecacy (5-point scale) was used to assess eca-
cy after 6 hours, time of rescue medication, or time of
remedication. Participants completed a 100-mm VAS
and the Eifel algofunctional questionnaire at base-
line and at the end of the 7-day trial. Compliance was
measured using the diary entries and counting the
medication left at the end of the trial. Intent-to-treat
analysis was completed. Compared to patients in the
placebo group, patients in the diclofenac-K group had
signicantly greater improvements in total pain relief
over the rst 3 and 6 hours as well as greater sum of
pain intensity dierences over 6 hours. Patients in the
diclofenac-K group experiences greater pain intensi-
ty dierences over the rst 3 hours compared to both
placebo and ibuprofen. Adverse events were similar in
the diclofenac-K and ibuprofen groups, but higher in
the placebo group. The most frequent adverse events
were digestive reports; there were no serious adverse
outcomes or deaths. The authors concluded that the
exible multiple dosing regimen of diclofenac-K 12.5
mg is an eective and safe treatment for acute LBP.
This paper provides Level I evidence that use of di-
clofenac in the treatment of acute LBP in the short-
term (one week) is safe and eective in the treatment
of acute LBP for both pain and disability.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
74
It is suggested that the use of oral or IV steroids is not eective for the treatment of low back
pain.
Grade of Recommendation: B
Eskin et al
10
evaluated the ecacy of oral corticoste-
roids for the treatment of acute musculoskeletal LBP
in the emergency department (ED) in a double-blind
randomized controlled trial. Adults in the ED aged 18-
55 years with LBP with an intensity ≥5 out of 10 on a
VAS were enrolled. Participants were randomly allo-
cated into the treatment group of 50 mg of prednisone
(n=39) or placebo (n=40). Pain was reported using the
10-cm VAS upon ED arrival and discharge. Each pa-
tient was discharged home with 4 doses of the study
medication (one dose per day). Five to 7 days after
discharge, a phone interview was conducted to assess
pain on a 3-point verbal rating scale (VRS). At 5 days,
there was no statistically-signicant dierence in the
3-point VRS for pain between groups. No signicant
side eects were reported during the follow-up tele-
phone call for either groups. The authors conclud-
ed that oral corticosteroids did not provide a benet
to ED patients with musculoskeletal LBP. This study
provides Level II evidence that oral steroid (predni-
sone) is not more eective than placebo for acute LBP
presenting to an emergency department.
Friedman et al
11
conducted a double-blind randomized
controlled trial to test the ecacy of intramuscular
methylprednisolone acetate to treat nonradicular LBP
one month after discharge from the emergency de-
partment (ED). Adults 21-50 years of age with a chief
complaint of nontraumatic LBP upon presentation to
the ED were enrolled if inclusion criteria were met af-
ter eligibility screening and interview. Only patents
with a LBP etiology of twisting or lifting and who had
a negative straight leg raise test were included. Par-
ticipants were randomized into the 160 mg methyl-
prednisolone acetate group (n=44) or placebo (n=43).
After the attending physician completed individual-
ized treatment and back pain was controlled to a level
acceptable for patient discharge, the subject received
an injection of the study drug or placebo. Each par-
ticipant was discharged with a one-week supply of
naproxen (500 mg), oxycodone 5 mg/acetamino-
phen 325 tablets, a detailed standardized instruction
sheet. Subjects were called one week and one month
after ED discharge and provided pain rating on an
11-point numerical rating scale (NRS) and a 4-point
descriptive scale. A total of 44 and 42 patients in the
methylprednisolone and placebo groups were includ-
ed in nal analysis. There were no dierences in NRS
scores between groups at one week or one month. The
authors concluded that parenteral corticosteroids did
not provide any benet for treatment of nonradicular
LBP in patients in the ED. This study provides Level
II evidence that intravenous steroids are not more ef-
fective than placebo for acute LBP presenting to the
emergency department.
It is suggested that the use of opioid pain medications should be cautiously limited and restrict-
ed to short duration for the treatment of low back pain.
Grade of Recommendation: B
Work Group Narrative: There are limited data that support the short-term eectiveness of opioid pain medication for
low back pain. There remain concerns in study design including the role of enriched enrollment and high dropout rates
in these trials. The trials also report high rates of adverse events, which may factor into the high dropout rates. As there
are few studies evaluating the ecacy and safety of opioids for low back pain beyond 12 weeks and given the con-
cerns associated with the use of opioids with the availability of other eective pharmacologic and nonpharmacologic
treatment options, we recommend the cautious use of opioid pain medication in those with low back pain and, when
utilized, that a short duration is recommended.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
75
Buynak et al
12
conducted a multicenter, double-blind,
randomized controlled trial to evaluate the ecacy
and safety of tapentadol extended relief (ER) for the
treatment of moderate to severe chronic LBP. Adults
with LBP ≥ 3 months with a pain intensity ≥ 5 out of
11 on a numerical rating scale (NRS) were enrolled
in this study. Participants were randomized into
the 100-250 mg BID tapentadol ER group (n=321),
20-50 mg BID oxycodone HCl controlled release
(CR) group (n=334), or BID placebo group (n=326)
and underwent a screening and washout period.
During a 3-week double-blind titration period, doses
were increased every 3 days, as tolerated, with the
assistance of a physician to reach optimal pain relief.
Participants were instructed to maintain a steady
dose for the duration of the 12-week maintenance
trial period if possible. The mean pain intensity was
measured using an 11-point NRS throughout the
maintenance period and at week 12. A total of 52.2%,
40.5% and 47.6%, of participants completed the
study in the tapentadol ER, oxycodone CR and placebo
groups, respectively. An intent-to-treat analysis was
completed on participants who received at least one
dose of their assigned medication in the tapentadol
(n=315), oxycodone HCl (n=326), or placebo (n=317)
groups. There was a signicant reduction in mean
pain intensity with tapentadol compared to placebo
(least square mean dierence vs placebo [95%
condence interval {CI}] -0.8, [-1.22 to -0.47]) at
week 12. There was also a signicant reduction in
mean pain intensity with oxycodone CR compared
to placebo (least square mean dierence vs. placebo
[95%CI], -0.9 [-1.24 to -0.49]) at week 12. Mean pain
intensity was signicantly reduced throughout the
overall maintenance period for both tapentadol ER
compared to placebo and oxycodone HCl compared
to placebo. The most common adverse events
reported in the treatment groups included nausea,
constipation, headache, vomiting, dizziness, pruritus
and somnolence. Compared to the tapentadol group,
the oxycodone HCl group had approximately double
the incidence of vomiting, constipation and pruritus
as well as higher odds of experiencing constipation
or nausea and/or vomiting (p<0.001). Serious adverse
events were reported in the placebo group (0.9%),
tapentadol ER group (2.2%) and oxycodone CR
group (3.4%). Serious adverse events likely related to
either of the study drugs included decreased level of
consciousness, mental confusion, atrial brillation,
dizziness and dehydration.The authors concluded
that tapentadol ER was eective for relief of moderate
to severe chronic LBP over 15 weeks. In critique of
the methodology, the work group downgraded this
potential Level I article due to less than 80% follow-up.
This study provides Level II evidence that tapentadol
improved pain, sleep and physical functioning (BPI
scores in patients with chronic LBP compared to
placebo and similar to oxycodone CR with improved
tolerability [gastrointestinal side eects]).
Cloutier et al
13
conducted a double-blind randomized
controlled trial to study the ecacy and safety of con-
trolled release (CR) oxycodone/CR naloxone for the
treatment of chronic LBP. Adults with chronic LBP ≥
3 months with a pain intensity of ≥2 out of a 5-point
ordinal scale were enrolled in this study and com-
pleted a 2-7 day washout period from period opioid
analgesics. Participants were randomly assigned to
the study treatment group to receive CR oxycodone/
CR naloxone (n=39) or placebo (n=44). Patients at-
tended weekly clinic visits in which the dosage was
titrated to the maximum eect with acceptable side
eects and maintained that dosage for 4 weeks. After
4 weeks, they received the initial dose again and re-
peated the same titration period. The 5-point ordinal
scale and 100 mm VAS were used to measure pain two
times a day in a daily diary. A per-protocol analysis
was completed for patients who completed at least 2
weeks in each phase while following protocol (n=54,
65%). Per the per-protocol analysis, the CR oxyco-
done/CR naloxone group had a signicantly greater
reduction in mean VAS (p=0.0296) and ordinal pain
scores (p=0.0415) compared to placebo. An intent-to-
treat analysis was conducted for participants who had
at least one dose and at least one post-randomization
data point (n=83). Compared to the placebo group,
the CR oxycodone/CR naloxone group had lower, but
with no statistical signicance, VAS and 5-point ordi-
nal pain scale. There were four serious adverse events
during the trail, which were all deemed “not related
to study medication.” Other adverse events report-
ed included nausea, constipation, diarrhea, fatigue,
somnolence, vomiting, dizziness, dry mouth, upper
respiratory tract infection and abdominal pain. There
was no dierence in the incidence of adverse events
between groups. The authors concluded that CR oxy-
codone/CR naloxone was eective for treatment of
moderate to severe chronic LBP in patients who com-
plied with the protocol. In critique of the methodol-
ogy, the work group downgraded this potential Level
I article due to small sample size and less than 80%
follow-up. This study provides Level II evidence that
opioids help pain control for chronic LBP versus pla-
cebo.
Hale et al
14
conducted a multicenter, double-blind,
randomized controlled trial to evaluate the ecacy
and safety of osmotic-controlled release oral deliv-

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
76
ery system (OROS) hydromorphone extended release
(ER) in the treatment of moderate to severe chronic
LBP in opioid-tolerant patients. After a screening pe-
riod of <2 weeks, 459 patients with chronic LBP un-
derwent a 2-4 week conversion and titration phase in
which they received a dose of hydromorphone ER that
was approximately 75% of their previous total daily
opioid dose. If they met inclusion criteria, they were
then randomized into the hydromorphone ER group
(n=134) or placebo group (n=134) and entered the 12-
week double-blind treatment phase. The hydromor-
phone ER group continued to take a xed dose for the
duration of the treatment phase. The placebo group
received gradually-reduced doses of hydromorphone
ER over 14 days and received placebo only for the du-
ration of the treatment phase. Patients recorded their
pain rating using a 10-point numerical rating system
(NRS) in a daily diary. Patients were asked to bring
their diaries to each follow-up visit. Sta also called
patients to monitor safety and compliance in between
visits. A total of 49.6% and 33.1% of participants in the
hydromorphone ER and placebo group, respectively,
completed the 12-week treatment trial. A total of 266
patients were included in the intent-to-treat analy-
sis of the hydromorphone group (n=133) and placebo
group (n=133). Over the 12-week treatment phase, the
hydromorphone ER group had signicantly reduced
pain intensity (p<0.001), change in weekly patient di-
ary NRS scores (p<0.001) and change in oce visit NRS
scores (p<0.05) compared to placebo. The hydromor-
phone group had a signicantly higher proportion of
participants (60.6%) who reported at least 30% pain
reduction compared to placebo (42.9%). A total of 43
(32.1%) in the placebo group and 36 (26.9%) in the
hydromorphone ER group of the double-blind phase
reported adverse events that were considered likely to
be related to the study medication in the double-blind
phase. Adverse events including constipation, sinus-
itis and arthralgia were reported at a higher rate in the
hydromorphone ER group compared to placebo. The
authors concluded that hydromorphone ER was safe
and eective in opioid-tolerant patients with mod-
erate to severe LBP. In critique of the methodology,
the workgroup downgraded the level of evidence of
this potential Level I study due to the high drop-out
rate, less than 80% follow-up and no validated out-
come measures. This study provides Level II evidence
that once daily oral hydromorphone ER is more eec-
tive than placebo in opioid-experienced patients with
chronic lower back pain for up to three months in a
randomized withdrawal protocol which tapered both
long acting and short acting (rescue opioids) in the
placebo group. Functional improvements were noted
in the treatment arm per RMDQ.
Lasko et al
15
conducted a double-blind, multicenter,
randomized controlled trial to assess the safety and
ecacy of an extended-release combination for-
mulation of 75mg tramadol and 650mg paracetamol
(DDS-06C) compared to placebo for treatment of LBP.
Patients aged 18-80 years with LBP rated as at least
2 out of 4 and 2 out of 11 on intensity rating scales
were included in this phase III study. Patients were
randomized into DDS-06C (n=141) or placebo group
(n=136) and instructed to take 1-2 tablets of the study
pill every 10-12 hours for 2.5 hours. They rated their
pain intensity (4-point scale) and pain relief (5-point
scale) at 0.5 h, 1 h, 1.5 h, 2 h, 4 h, 6 h (±30 min), 26 h
(±30 min), 30 h (±30 min), 34 h (±30 min) and 50 h
(±30 min). If patients required ongoing treatment at
the day 3 follow-up visit, they continued to receive the
open-label DDS-06C for 2.5 more days (n=219). Com-
pared to the subjects in the placebo group, the sub-
jects in the DDS-06C group had a signicantly greater
decrease in pain intensity (p=0.038) and greater pain
relief (p=0.026) during the 50 hour observation peri-
od. Adverse events were reported by both the placebo
(2.2%) and DDS-06C group (12.1%). Most of the ad-
verse events were mild-to-moderate and considered
to be at least possibly related to the treatment. There
was one serious adverse event (hospitalization due to
exacerbation of back pain) but it was deemed not re-
lated to the study medication. The authors concluded
that the study drug was superior to placebo for relief
of LBP and intensity. This paper provides Level I evi-
dence that tramadol/paracetamol ER can reduce acute
LBP better than placebo in the short-term (50 hours).
Lee et al
16
studied the ecacy and safety of trama-
dol hydrochloride 75-mg/acetaminophen 650-mg
extended release tablets (TA-ER) for the treatment
of chronic LBP. Adults aged 25-75 years with mod-
erate to severe chronic LBP who met inclusion crite-
ria were enrolled in this multicenter, double-blind,
randomized controlled trial. After a 7-day screening
period, participants were randomized into the TA-ER
group (n=125) or placebo group (n=120) and began a
4-week trial which included a 7-day dose-titration
phase. Patients attended regularly-scheduled fol-
low-up visits and rated their average pain intensity
using a 6-point VAS, quality of life using the Korean
Short Form-36 (K-SF-36) and functionality using
the Korean Oswestry Disability Index (K-ODI). A to-
tal of 104 and 92 patients in the placebo and TA-ER
group, respectively, completed this study. In the full
analysis set and the per-protocol analysis, the TA-ER
group had a signicantly higher percentage of patents
with a pain intensity change rate ≥30% compared to
the placebo group (p<0.05). The patients in the TA-ER

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
77
group also had signicantly higher pain relief at days
8 and 15, improved general health and higher func-
tional improvements compared to the placebo group.
Adverse events were reported more frequently in the
TA-ER group compared to the placebo group. No se-
rious adverse events that were believed to be related
to the study drug occurred. The authors concluded
that TA-ER was safe and eective in treating chronic
LBP. In critique of the methodology, the work group
downgraded the level of evidence of this potential
Level I article due to the short follow-up period and
non-stratication of the patients. This paper provides
Level II evidence that short-term relief is better with
ER tramadol/acetaminophen than no treatment in
patients with chronic LBP.
Peloso et al
17
conducted a multicenter, double-blind,
randomized, placebo-controlled trial to study the ef-
cacy of tramadol 37.5 mg/acetaminophen 325 mg
(tramadol/APAP) for the treatment of LBP. Adults
with LBP requiring daily medication > 3 months but
otherwise generally healthy were enrolled, complet-
ed a washout phase of all pain medication for up to
21 days, were randomized to receive tramadol/APA
(n=167) or placebo (n=169) and completed a titration
phase. Patients were evaluated and reported pain us-
ing a 100 mm VAS, Short-Form McGill Pain Question-
naire (SFMPQ), Roland Morris Disability Question-
naire (RMDQ), Medical Outcome Study Short Form-36
(SF-36) Health Survey and overall medication assess-
ments on days 1, 14, 28, 56 and 91. Patients were given
instructions regarding the use of rescue medications
and were allowed to maintain physiotherapy if it was
started prior to the double-blind portion of the study.
A total of 86 and 61 participants completed the study
in the tramadol/APAP and placebo groups, respec-
tively. Intention-to-treat analysis found that the par-
ticipants in the tramadol/APA group had signicantly
better mean pain VAS, pain relief, RMDQ and SF-36
scores compared to the placebo group. Common ad-
verse events included nausea, dizziness, constipation
and somnolence, but there were no serious adverse
events thought to be related to the study medication.
The authors concluded that the study drug had similar
tolerability as other opioids and was eective in pain
reduction, physical functioning and quality of life for
the treatment of LBP. The work group downgraded
the level of evidence due to less than 80% follow-up
and other critique of the methodology such as un-
certainty regarding blinding, patients may have had
other interventions, and pain patients were a selected
group with various exclusion criteria. Therefore, this
study provides Level II evidence that tramadol/acet-
aminophen provides better pain relief and functional
improvement than placebo for up to three months.
Ruo et al
18
assessed the ecacy and safety of tra-
madol 37.5 mg/acetaminophen 325 mg (tramadol/
APAP) for the treatment of LBP in a multicenter, ran-
domized, double-blind, placebo-controlled trial. Pa-
tients aged 25-75 years with chronic LBP requiring
daily pain medication≥3 months who met inclusion
criteria were enrolled. Eligible patients completed a
3-week screening and washout period and were then
randomized to receive tramadol/APA or placebo. Af-
ter a 10-day titration period, participants received up
to 8 tablets per day. Patients reported their pain us-
ing a 100 mm and completed the Pain Relief Rating
Scale (PRRS), Short-Form McGill Pain Questionnaire
(SF-MPQ), Roland Morris Disability Questionnaire
(RMDQ), 36-Item Short-Form Health Survey (SF-36)
and overall medication assessment at various time
points from day 1-91. A total of 161 and 157 partici-
pants were included in the intention-to-treat analy-
sis in the tramadol/APAP and placebo groups, respec-
tively. A total of 91 and 74 participants completed the
treatment in its entirety in the tramadol/APAP and
placebo groups, respectively. Compared to the place-
bo group, the tramadol/APAP group had signicant-
ly favorable nal mean PVA scores (p=0.015), PRRS
scores (p<0.001), SF-MPQ improvements (p=0.021),
RMDQ score improvements (p<0.027) and SF-36 sub-
category improvements. Adverse events thought to
be related to treatment medication included nausea,
somnolence and constipation; there were no treat-
ment-related serious adverse events. The authors
concluded that tramadol/APAP was eective for the
treatment of chronic LBP and had a favorable safe-
ty prole. This study provides Level II evidence that
tramadol/acetaminophen is better than placebo for
chronic LBP for up to 3 months.
Schiphorst et al
19
conducted a randomized controlled
trial to evaluate the ecacy of tramadol/acetamino-
phen in patients with chronic LBP. Adult patients with
chronic LBP >3 months on a wait list for a rehabili-
tation program were randomized to receive tramadol
37.5 mg/acetaminophen 325 mg capsules (n=25) or
placebo (n=25). All participants conducted a wash-out
period up to 7 days before beginning a one-week ti-
tration phase followed by a steady dose for at least one
week. Functional capacity, pain intensity and self-re-
ported disability per the Roland Morris Disability
Questionnaire (RMDQ) were measured at baseline and
at completion of the two-week trial. One patient in the
treatment group was lost to follow-up; a total of 49
patients were included in nal analysis. There were no
signicant dierences in outcome measures between
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
78
groups. One subgroup (n=10) reported improvements
in RMDQ and global pain relief. Side eects such as
dizziness, nausea, tiredness, diarrhea and skin rash
were reported in both the placebo group (24%) and
treatment group (88%). The authors concluded that
there were only small nonsignicant treatment ef-
fects with tramadol/acetaminophen. The workgroup
downgraded the level of evidence from Level I to Level
II due to the small sample study, no power analysis,
short follow-up and limited generalizability of this
exploratory study. This study provides Level II evi-
dence that tramadol/acetaminophen provided simi-
lar outcomes to placebo in measures of function in a
2-week study.
Schnitzer et al
20
evaluated the ecacy and safety of
tramadol for treatment of moderate chronic LBP in a
two-part trial at 26 centers in the United States. Eligi-
ble patients aged 25-75 with LBP requiring daily med-
ication ≥3 months who met inclusion criteria were
enrolled in a screening and washout phase for up to
3 weeks. Patients with at least moderate LBP (n=380)
then entered a 3-week open-label phase in which they
initially received 50 mg tramadol/day which increased
to at least 200 mg/day (maximum 400 mg/day) by
day 14. If patients tolerated and perceived benet
during the open-label phase, they were enrolled in
the 4-week randomized, double-blind, placebo-con-
trolled phase. These participants were randomized to
receive tramadol 200-400 mg/day (n=127) or placebo
(n=127) with no rescue medication. Patients were in-
structed to continue their current level of exercise but
not to initiate any new physiotherapy during the trial.
Participants recorded pain according to a 10-cm VAS,
pain relief per the pain relief rating scale, LBP details
per the short form McGill Pain Questionnaire (SF-
MPQ), quality of life per the Roland Morris Disability
Questionnaire (RMDQ). Patients were considered to
have “therapeutic failure” if they did not experience
pain relief for any 24-hour period. A total of 91 and
55 patients completed the entire trial in the tramadol
and placebo group, respectively. The time to ther-
apeutic failure was signicantly dierent between
groups. The participants in the tramadol group also
experienced signicantly lower mean pain VAS scores
and signicantly better SF-MPQ and RMDQ scores.
Common adverse events included nausea, dizziness,
somnolence and headache. Seventy-eight of the 380
participants in the open-label period discontinued
treatment due to adverse events, but <10% experi-
enced each adverse event in the double-blind phase.
Four participants in the tramadol group experienced
serious adverse events that were deemed possibly or
unlikely related to the treatment drug (ie, myocardial
infarction, myocardial ischemia, prostate cancer and
depression). The authors concluded tramadol was ef-
fective for the treatment of chronic LBP in patients
who tolerate it well. This study provides Level II ev-
idence that tramadol is better than no treatment at
reducing chronic LBP up to 45 days in tramadol re-
sponders.
Future Directions for Research
The work group recommends development of studies that identify specic
groups of patients who respond to a particular opioid medication with minimal
dependence risk.
References
1. Muehlbacher M, Nickel MK, Kettler C, et al. Topiramate
in treatment of patients with chronic low back pain: a
randomized, double-blind, placebo-controlled study.
Clin J Pain. 2006;22(6):526-531.
2. Atkinson JH, Slater MA, Wahlgren DR, et al. Eects of
noradrenergic and serotonergic antidepressants on
chronic low back pain intensity. Pain. 1999;83(2):137-
145.
3. Dickens C, Jayson M, Sutton C, Creed F. The relationship
between pain and depression in a trial using paroxetine
in suerers of chronic low back pain. Psychosomatics.
2000;41(6):490-499.
4. Goodkin K, Gullion CM, Agras WS. A randomized,
double-blind, placebo-controlled trial of trazodone
hydrochloride in chronic low back pain syndrome. J Clin
Psychopharmacol. 1990;10(4):269-278.
5. Skljarevski V, Ossanna M, Liu-Seifert H, et al. A dou-
ble-blind, randomized trial of duloxetine versus place-
bo in the management of chronic low back pain. Eur J
Neurol. 2009;16(9):1041-1048.
6. Sandoughi M, Zakeri Z, Mirhosainee Z, Mohammadi M,
Shahbakhsh S. The eect of vitamin D on nonspecic
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
79
low back pain. Int J Rheum Dis. 2015;18(8):854-858.
7. Birbara CA, Puopolo AD, Munoz DR, et al. Treatment of
chronic low back pain with etoricoxib, a new cyclo-ox-
ygenase-2 selective inhibitor: improvement in pain
and disability--a randomized, placebo-controlled,
3-month trial. J Pain. 2003;4(6):307-315.
8. Pallay RM, Seger W, Adler JL, et al. Etoricoxib reduced
pain and disability and improved quality of life in pa-
tients with chronic low back pain: a 3 month, random-
ized, controlled trial. Scand J Rheumatol. 2004;33(4):257-
266.
9. Dreiser RL, Marty M, Ionescu E, Gold M, Liu JH. Relief of
acute low back pain with diclofenac-K 12.5 mg tablets: a
exible dose, ibuprofen 200 mg and placebo-controlled
clinical trial. Int J Clin Pharmacol Ther. 2003;41(9):375-
385.
10. Eskin B, Shih RD, Fiesseler FW, et al. Prednisone for
emergency department low back pain: A randomized
controlled trial. J Emerg Med. 2014;47(1):65-70.
11. Friedman BW, Holden L, Esses D, et al. Parenter-
al corticosteroids for Emergency Department pa-
tients with non-radicular low back pain. J Emerg Med.
2006;31(4):365-370.
12. Buynak R, Shapiro DY, Okamoto A, et al. Ecacy and
safety of tapentadol extended release for the manage-
ment of chronic low back pain: results of a prospective,
randomized, double-blind, placebo- and active-con-
trolled Phase III study.[Erratum appears in Expert Opin
Pharmacother. 2010 Nov;11(16):2773]. Expert Opin Phar-
macother. 2010;11(11):1787-1804.
13. Cloutier C, Taliano J, O’Mahony W, et al. Controlled-re-
lease oxycodone and naloxone in the treatment of
chronic low back pain: A placebo-controlled, random-
ized study. Pain Res Manag. 2013;18(2):75-82.
14. Hale M, Khan A, Kutch M, Li S. Once-daily OROS hydro-
morphone ER compared with placebo in opioid-toler-
ant patients with chronic low back pain.[Erratum ap-
pears in Curr Med Res Opin. 2010 Aug;26(8):1904]. Curr
Med Res Opin. 2010;26(6):1505-1518.
15. Lasko B, Levitt RJ, Rainsford KD, Bouchard S, Rozova A,
Robertson S. Extended-release tramadol/paracetamol
in moderate-to-severe pain: a randomized, place-
bo-controlled study in patients with acute low back
pain. Curr Med Res Opin. 2012;28(5):847-857.
16. Lee JH, Lee CS, Ultracet ERSG. A randomized, dou-
ble-blind, placebo-controlled, parallel-group study to
evaluate the ecacy and safety of the extended-release
tramadol hydrochloride/acetaminophen xed-dose
combination tablet for the treatment of chronic low
back pain. Clin Ther. 2013;35(11):1830-1840.
17. Peloso PM, Fortin L, Beaulieu A, Kamin M, Rosenthal
N, Protocol TRPCANSG. Analgesic ecacy and safety
of tramadol/ acetaminophen combination tablets (Ul-
tracet) in treatment of chronic low back pain: a multi-
center, outpatient, randomized, double blind, placebo
controlled trial. J Rheumatol. 2004;31(12):2454-2463.
18. Ruo GE, Rosenthal N, Jordan D, Karim R, Kamin M,
Protocol C-SG. Tramadol/acetaminophen combination
tablets for the treatment of chronic lower back pain: a
multicenter, randomized, double-blind, placebo-con-
trolled outpatient study. Clin Ther. 2003;25(4):1123-
1141.
19. Schiphorst Preuper HR, Geertzen JHB, Van Wijhe M, et
al. Do analgesics improve functioning in patients with
chronic low back pain? An explorative triple-blinded
RCT. Eur Spine J. 2014;23(4):800-806.
20. Schnitzer TJ, Gray WL, Paster RZ, Kamin M. Ecacy of
tramadol in treatment of chronic low back pain. J Rheu-
matol. 2000;27(3):772-778.
QQ
Med/Psych Question 3. In patients with low back pain, is topical treatment (eg,
cream or gel) eective in decreasing duration of pain, decreasing intensity of pain,
increasing functional outcomes of treatment and improving the return-to-work
rate?
There is insucient evidence to make a recommendation for or against the use of lidocaine
patch for the treatment of low back pain.
Grade of Recommendation: I
Gimbel et al
1
assessed the eectiveness and safe-
ty of 5% lidocaine patch for the treatment of LBP in
an open-label pilot study. Patients with LBP from 5
dierent centers in the United States were catego-
rized into groups upon enrollment based on duration
of LBP: acute/subacute (3 months), n=21; short-term
chronic (3-12 months), n=33; or long-term chron-
ic (12 months), n=77. Participants applied the lido-
caine patch to the area of LBP up to 4 times daily for
6 weeks. After 2 weeks, patients were allowed to taper
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
80
headache. There were no drug-related serious adverse
events reported. The authors concluded that the lido-
caine patch 5% resulted in signicant improvements
in pain intensity and QOL and randomized controlled
trials are warranted to further investigate its ecacy
and safety for the treatment of LBP. This study pro-
vides Level III evidence that treatment with lidocaine
patch 5% provided a signicant improvement in pain
intensity and QOL.
Topical capsicum is recommended as an eective treatment for low back pain on a short-term
basis (3 months or less).
Grade of Recommendation: A
Frerick et al
2
conducted a double-blind, randomized,
placebo-controlled multicenter study to assess the ef-
cacy and tolerance of capsicum plaster for the treat-
ment of LBP. A total of 320 patients were random-
ized to the treatment group which received a 12 x 18
cm capsicum plaster (n=160) or placebo group which
received a similar plaster with no active medication
(n=160). All participants were instructed to apply the
plaster to the site of pain for 4-8 hours once daily for
21 days. The Arhus Low Back Rating Scale was used to
record patient-reported pain, disability and physical
impairment at baseline and days 7 and 21. The glob-
al assessments of ecacy by patient and investiga-
tor were also recorded at baseline and days 7 and 21.
An intent-to-treat analysis included 319 participants
(159 in the treatment group and 160 in the placebo
group). The treatment group experienced signicant-
ly greater reduction in pain (42%) compared to the
placebo group (31%). The responder rate (≥30% pain
reduction) was greater in the treatment group (67%)
compared to the placebo group (49%). A total of 120
and 129 participants completed the study in the treat-
ment group and placebo group, respectively and were
included in the per-protocol analysis. Per-protocol
analysis supported the intention-to-treat analysis.
Adverse events likely related to capsicum included
excessively severe sensation of heat or erythema. The
authors concluded that capsicum plasters may oer
an alternative treatment for LBP. This study provides
Level I evidence that capsicum plaster applied topi-
cally may have short-term benet for patients with
back pain persisting for more than 3 months.
Keitel et al
3
studied the ecacy of capsicum plaster for
the treatment of LBP in a double-blind randomized
controlled study. A total of 154 participants were
randomized to receive a capsicum plaster or placebo
plaster. Participants placed the plaster at the site of
pain for 4-12 hours once daily for 21 days. The Arhus
Low Back Rating Scale was used to measure pain and
impairment of movement. The global assessments of
ecacy and tolerance by participant and physician
were recorded at baseline and follow-up. A total of
76 participants in the placebo group and 74 patients
in the capsicum group were included in intention-
to-treat analysis. The responder rate (≥30% pain
reduction) was signicantly greater in the capsicum
group (60.8%) compared to the control group (42.1%).
The participants in the capsicum group experienced
signicantly greater reduction in the sum of 3 separate
pain scores compared to the placebo group. Common
adverse events included local sensation of warmth
and itching; more adverse reactions were reported in
the treatment group compared to the placebo group.
The authors concluded that capsicum plaster can be
used in chronic nonspecic LBP. This study provides
Level I evidence that capsicum plaster provided more
analgesia than placebo in a 3-week trial of patients
with nonspecic LBP.
o existing analgesic drugs and increase daily lido-
caine patches if pain was unacceptable during the ta-
per period. Patients completed the BPI to report pain
and quality of life (QOL) at baseline, 2 weeks and 6
weeks. At 2 and 6 weeks, each group had signicantly
improved pain scores compared to baseline (p≤0.001).
Improvements in QOL were observed in each group
from baseline to 2 and 6 weeks. Adverse events re-
ported included skin reactions, lightheadedness and
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
81
References
1. Gimbel J, Linn R, Hale M, Nicholson B. Lidocaine patch
treatment in patients with low back pain: results of
an open-label, nonrandomized pilot study. Am J Ther.
2005;12(4):311-319.
2. Frerick H, Keitel W, Kuhn U, Schmidt S, Bredehorst A,
Kuhlmann M. Topical treatment of chronic low back
pain with a capsicum plaster. Pain. 2003;106(1-2):59-
64.
3. Keitel W, Frerick H, Kuhn U, Schmidt U, Kuhlmann
M, Bredehorst A. Capsicum pain plaster in chron-
ic non-specic low back pain. Arzneimittelforschung.
2001;51(11):896-903.
QQ
Med/Psych Question 4. Following treatment for low back pain, do patients with
healthy sleep habits experience decreased duration of pain, decreased intensity of
pain, increased functional outcomes and improved return-to-work rates compared
to patients with poor sleeping habits?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends high quality, prospective studies that utilize sleep
logs or other tracking methodologies to evaluate low back treatment outcomes
in patients with and without healthy sleep habits.
QQ
Med/Psych Question 5. In patients with low back pain, is cognitive behavioral
therapy (CBT) and/or psychosocial intervention and/or neuroscience education
eective in decreasing duration of pain, decreasing intensity of pain, increasing
functional outcomes, decreasing anxiety and/or depression and improving return-
to-work rate?
Cognitive behavioral therapy is recommended in combination with physical therapy, as com-
pared with physical therapy alone, to improve pain levels in patients with low back pain over 12
months.
Grade of Recommendation: A
Cognitive behavioral therapy in combination with physical therapy, compared to physical thera-
py alone, is suggested to improve functional outcomes (disability) and return to work in patients
with low back pain.
Grade of Recommendation: B
There is conicting evidence to make a recommendation for or against cognitive behavioral
therapy for improving depression or anxiety in patients with low back pain.
Grade of Recommendation: I

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
82
Bendix et al
1
compared the rehabilitation outcomes
from 3 dierent therapy approaches to treat LBP in
prospective randomized study. A total of 132 patients
were randomized into one of 3 groups. Group 1 (n=46)
received an intensive multidisciplinary rehabilita-
tion program 39 hours per week for 3 weeks plus an
additional 6-hour follow-up session once a week for
the following 3 weeks (total of 135 hours). Group 2
(n=43) received active physical training of aerobics,
weight training and back education twice weekly for
6 weeks (total of 24 hours). Group 3 (n=43) received
a combined psychological and physical therapy pro-
gram twice weekly for 6 weeks (total of 24 hours). Re-
habilitation outcomes such as return-to-work rate,
days of sick leave, health-care contacts, pain and dis-
ability score and staying physically active were mea-
sured at baseline and 4 months after therapy. After 4
months, 40, 31 and 35 patients in Group 1, Group 2 and
Group 3, respectively, were available for follow-up.
Compared to the participants in Group 2 and Group
3, the participants in Group 1 had signicantly im-
proved work-readiness (p=0.01), health care contacts
(p=0.05), pain (p≤0.001), disability (p=0.002) and
self-reported physical activity (p=0.005). The authors
concluded that the multidisciplinary program may be
more expensive than a less-intensive program, but is
overall economically worthwhile due to savings in sick
pay, health care contacts and early retirement pen-
sions. Of note, when psychological interventions were
combined with physical training there was an im-
provement in outcomes related to LBP but the nature
of this question did not address physical and psych
training together. The work group determined that
this study provides Level I evidence that psychological
training programs in addition to physical training do
not improve functional outcomes compared to physi-
cal training alone with regard to LBP.
Dufour et al
2
studied the ecacies of a group-based
multidisciplinary biopsychosocial rehabilitation pro-
gram and an individual intensive therapist-assisted
back muscle exercise program. In this randomized
controlled trial, patients with chronic LBP >12 weeks
were stratied and randomly allocated into the mul-
tidisciplinary biopsychosocial rehabilitation program
(group A) or the individual exercise program (group
B). Each group program ran for 12 weeks. Group A
(n=129) received biweekly education from a phys-
iotherapist and occupational therapist along with a
total of 75 hours of moderate muscle training exer-
cise which included warm up, stretching, aerobic ex-
ercises, strengthening exercises, playing ball games,
training in hot water and ball stick training. Group B
(n=143) received intensive muscle training exercises,
without stretching or abdominal exercises, guided by
a therapist for a total of 22 hours of exercise. Through-
out the program, each patient received a total of 12
and 24 hours of therapist assistance in Group A and
Group B, respectively. Outcomes were measured at
baseline, after 3 months of treatment and at 6, 12 and
24 months. Pain per the VAS, disability per the Ro-
land-Morris Disability Questionnaire (RMDQ), most
of the MOS Short-Form Health Survey results and
ability to work signicantly improved in both groups
after treatment using an intent-to-treat analysis as
well as an analysis of actual data. There were some
minor statistically-signicant (but not clinically sig-
nicant) dierences in improvement between groups.
A total of 11 patients in each group dropped out due
to adverse events such as requirement of surgery,
concussion, leg pain, delayed onset muscle sore-
ness, or other reasons unrelated to treatment. The
authors concluded that both groups had signicantly
improved long-term pain and disability scores. This
study provides Level I evidence that a biopsychosocial
program plus physical training is as eective as an in-
tensive physical exercise program for chronic LBP.
Lamb et al
3
conducted a multicenter randomized con-
trolled trial to compare the clinical and cost-eec-
tiveness of active management with a cognitive-be-
havioral approach (CBA) versus active management
alone (AM) in patients with LBP. Patients with sub-
acute or chronic LBP from 56 dierent clinical prac-
tices in English regions were randomized into either
the CBA (n=468) or AM (n=233) group. Both groups
received a 15-minute standard best-practice inter-
vention, which included distribution of an education-
al back book. The CBA group additionally attended 6
professionally led group sessions that covered goal
setting, pacing, challenging beliefs, managing pain
and improving communication with health profes-
sionals. Patients were asked to provide demograph-
ic, LBP-associated disability information per the
Roland Morris Disability Questionnaire (RMDQ) and
pain and disability information per the Modied Von
Kor Scale (MVK) through postal questionnaires or
telephone surveys (85% follow-up at 12 months).
The CBA group experienced signicantly greater im-
provements in mean RMDQ scores at 3 (1.1; 95% CI 0.4
to 1.7), 6 (1.4; 95% CI, 0.7 to 2.1) and 12 months (1.3;
95% CI 0.6 to 2.1). Signicantly greater improvements
in the CBA group compared to the AM group were also
seen in pain per the MVK at 3 (6.8; 95% CI 3.5 to 10.2),
6 (8.0; 95% CI 4.3 to 11.7) and 12 months (7.0; 95% CI
3.2 to 10.7) as well as disability per the MVK at 3 (4.3;
95% CI 0.4 to 12.4), 6 (8.1; 95% CI 4,1 to 12.0) and 12
months (8.4; 95% CO 4.4 to 12.4). The authors con-

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
83
cluded that CBA showed long-term eectiveness in
treating patients with subacute and chronic LBP. This
study provides Level I evidence that cognitive behav-
ioral therapy (CBT) plus active management is better
than active management alone in terms of pain and
function.
Linden et al
4
assessed the ecacy of CBT for improv-
ing pain tolerance compared to a multimodal inpatient
orthopedic rehabilitation program alone in patients
with LBP in a randomized controlled trial. Patients
with LBP >6 months were randomly allocated into
an intervention (n=53) or control (n=50) group. All
patients received 21 days of inpatient treatment in-
cluding various therapies, occupational therapy and
general patient education sessions on coping. The pa-
tients in the intervention group additionally received
3 90-minute CBT group sessions per week focused
on stress reduction, problem solving, self-moni-
toring, pain management, change in dysfunction-
al cognitions, reduction of avoidance behavior and
well-being therapy. Before and after treatment, pa-
tients reported fear and avoidance per the Fear Avoid-
ance Beliefs Questionnaire (FABQ), subjective pain
per the VAS Pain (VAS-pain), pain-related disability
per the Pain Disability Index (PDI) and psychologi-
cal and psychosomatic complaints per the Symptom
Checklist (SCL-90-R). The intervention group expe-
rienced signicantly greater improvements in VAS-
pain (p=0.002) and FABQ (p<0.001). There were no
dierences between groups in changes in PDI and SCL
scores. The authors concluded that the results of this
study support the recommendation that CBT should
be a part of the treatment of chronic LBP. This study
provides Level I evidence that CBT plus usual care im-
proves short-term pain and disability (over 3 weeks)
in chronic LBP patients.
Sullivan et al
5
investigated the physical and psycho-
social changes that occur throughout physiotherapy
with psychotherapy compared to physiotherapy alone
in a retrospective study of 2 matched cohorts. A da-
tabase of individuals receiving treatment for mus-
culoskeletal conditions was used to systematically
identify participants with LBP who were enrolled in
the subacute phase of recovery at various clinics. The
patients who received physiotherapy plus a Progres-
sive Goal Attainment Program (PGAP) psychothera-
py program (n=24) were matched for age, education,
duration of sick leave and initial pain severity with
patients who received only physiotherapy (n=24).
Due to the retrospective design of this study, the pa-
tients received therapy per the clinical discretion of
each individual therapist; no specic techniques were
described. Participants recorded severity of pain per
the McGill Pain Questionnaire (MPQ), pain experience
per the Pain Rating Index (PRI) within the MPQ and
the severity of their pain per an 11-point numerical
rating scale. Function was assessed using a 5-min-
ute walk and nger-to-oor test. Self-perceived
disability per the Pain Disability Index (PDI), cata-
strophic thinking per the Pain Catastrophizing Scale
(PCS), fear of re-injury per the Tampa Scale for Ki-
nesiophobia (TSK) and depression per the Beck De-
pression inventory-II (BDI-II) were also recorded.
Twelve months after treatment termination, partic-
ipants were contacted by telephone. There were no
post-treatment dierences in pain intensity, number
of pain sites, nger-to-oor test, 5-minute walk dis-
tance or self-reported disability. The participants in
the physiotherapy + PGAP group had lower MPQ-PRI
scores (F(1,45)=4.5, p<0.05), measures of pain cata-
strophizing (F(1,45=5.2, p<0.05), fear of movement
(F(1,45)=5.0, p<0.05) and depression (F(1,45)=23.8,
p<0.001). The authors concluded that the psycho-
social treatment in addition to physiotherapy alone
may contribute to more positive outcomes including
reductions in psychosocial risk factors for pain and
disability in people with LBP. The work group down-
graded the level of evidence due to small sample size.
This study provides Level II evidence that psychoso-
cial treatment augments the outcomes of physiother-
apy in terms of reduction of depression, anxiety and
improved return to work.
Turner et al
6
compared the ecacy of cognitive ther-
apy techniques with behavioral treatment in patients
with chronic LBP in a randomized controlled study. A
total of 102 patients met inclusion criteria and were
randomized into a relaxation training (R) group
(n=24), cognitive therapy (C) group (n=23), cogni-
tive therapy/relaxation training (CR) group (n=25), or
waiting list (WL) group (n=30). Patients in the R group
were instructed to use systematic progressive muscle
relaxation and imagery. Patients in the C group were
trained to identify and counter negative emotions re-
lated to pain and stress. The CR group combined the
aspects of the R and C group. All training programs
were led by psychologists. Measurements including
pain intensity using a VAS, pain-related physical and
psychosocial dysfunction using the Sickness Impact
Prole (SIP), depression using the Beck Depression
Inventory (BDI), standardized coding of observer
ratings of pain behaviors, and maladaptive cogni-
tions using the Cognitive Error Questionnaire (CEQ)
were obtained before treatment and immediately, 6
months and 12 months after treatment. A total of 17,
16, 21 and 18 participants completed the treatment

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
84
and post-treatment in the R, C, CR and WL groups, re-
spectively. Pain intensity decreased in all 3 treatment
groups and remained improved at 6- and 12-month
follow-up. Depressive symptoms and disability im-
proved signicantly in all groups, including the WL
group. There were no dierences in results between
treatment groups. The authors concluded that cogni-
tive therapy may be as eective as relaxation train-
ing in reducing self-reported LBP; however, neither
relaxation training nor cognitive therapy, alone or in
combination with each other, is more eective in re-
ducing cognitive errors, depression, disability or pain
behavior than a waiting list group. This study pro-
vides Level I evidence that CBT, relaxation training
alone or in combination improve LBP compared to no
treatment; however these modalities compared to no
treatment did not improve disability and depression
over 12 months as compared to no treatment.
Hampel et al
7
investigated the eects of a multi-
disciplinary inpatient rehabilitation program with
cognitive-behavioral management training for pa-
tients with chronic LBP and depressive symptoms.
Patients from two dierent inpatient orthopedic re-
habilitation clinics with LBP >6 months and moder-
ate to severe depressive symptoms were assigned to
a control group or intervention group. The control
group (n=80) received a standard 3-4 week biopsy-
chosocial multidisciplinary rehabilitation program
that included medication, physiotherapy, physical
applications and group sessions with a psychologist
focusing on cognitive-behavioral pain management
and muscle relaxation. The intervention group (n=85)
received the same rehabilitation program plus ad-
ditional group therapy sessions focusing on behav-
ioral activation, cognitive restructuring and social
skills training from a psychologist. Rehabilitation
outcome measures such as days of sick leave, depres-
sive symptoms per the Allgemeine Depressions-Skala
(ADS), anxiety per the Hospital Anxiety and Depres-
sion Scale (HADS-D Anxiety) and somatization per
the Symptom Checklist (SCL-90-R) were assessed
at baseline, immediately after rehabilitation and 6,
12 and 24 months after rehabilitation. A total of 40
and 44 participants in the control group and inter-
vention group, respectively, completed the program
and were included in the per-protocol analysis. Per
both the intention-to-treat and per-protocol anal-
yses, both groups initially showed improvement in
depressive symptoms and anxiety, but only the inter-
vention group showed persistent improvement over
24 months. The intervention group had signicant-
ly lower depression and anxiety scores at 6 months
compared to the control group. The authors concluded
that the intervention rehabilitation program was su-
perior to the standard rehabilitation alone. In critique
of the methodology, the workgroup downgraded this
potential Level I study due to the small sample size.
Therefore, this study provides Level II evidence that
adding psychological treatment in people who are
depressed with LBP improves their depressive symp-
toms over the course of a year and improves anxiety at
6 months, but not at 2 years.
Monticone et al
8
conducted a randomized controlled
trial pilot study to evaluate the ecacy of a
multidisciplinary rehabilitation program with exercise
and CBT compared to exercise alone in patients with
chronic LBP. Ten patients were randomized into a
multidisciplinary treatment program group with
physiatrists, physiotherapists, a psychologist and an
occupational therapist in which they received usual-
care rehabilitation, spinal stabilizing exercises,
and individualized CBT aimed at addressing fear of
movement beliefs, catastrophizing, and negative
feelings. The control group (n=10) received only usual-
care rehabilitation which involved passive spinal
mobilization, stretching, muscle strengthening and
postural control. Disability per the Oswestry Disability
Index (ODI), kinesiophobia per the Italian Tampa
Scale of Kinesiophobia (TSK), catastrophizing per the
Italian Pain Catastrophizing Scale (PCS), pain rating
using a numerical rating scale (NRS), quality of life
using the Italian Short Form Health Survey (SF-36),
a 6-minute walking test and treatment satisfaction
using the global perceived eect (GPE) were assessed
at baseline, after the 8-week treatment period and
3 months after the treatment ended. The patients in
the treatment group had signicant improvements in
disability, kinesiophobia, catastrophizing and quality
of life in group, time and time-by-group interactions.
The authors concluded that this superiority trial
revealed that the multidisciplinary rehabilitation
program with CBT was superior to exercise alone
in patients with chronic LBP. In critique of the
methodology, the work group downgraded the level of
evidence of this potential Level I study due to the small
sample size. Therefore, this paper provides Level II
evidence that CBT is better than usual care alone in
reducing pain and disability from chronic LBP.
In a multicenter randomized controlled trial, Pincus
et al
9
studied the feasibility of contextual cognitive-
behavioral therapy (CCBT) compared to physiotherapy
alone in patients classied as “avoidant” with LBP.
Participants were randomly allocated to the CCBT
group (n=45) in which they received up to 8 individual
50-minute sessions with a trained psychologist or the

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
85
physiotherapy group (n=44) in which they received up
to 8 exercise sessions. Questionnaires were completed
at baseline and 3 and 6 months after randomization
and included Tampa Scale for Kinesiophobia (TSK),
BPI, Chronic Pain Acceptance Questionnaire (CPAQ),
Acceptance and Action Questionnaire (AAQ-II), Roland
Morris Disability Questionnaire (RMDQ), Hospital
Anxiety and Depression Scale (HADS), EuroQol-5D,
Modied Patient Global Impression of Change (PHIC)
and expectations and satisfaction with treatment. At
6-month follow-up, most outcomes improved for
both groups. The CCBT group experienced signicantly
greater improvements in disability per the RMDQ and
pain per the CPAQ. The authors concluded that CCBT
is credible and acceptable for patients with LBP and
psychological obstacles. In critique, the work group
downgraded the level of evidence for this study due to
less than 80% follow-up. This study provides Level II
evidence that CBT is better than physiotherapy alone
in terms of pain and disability at 6 months.
Schiltenwolf et al
10
studied the ecacy of biopsy-
chosocial treatment compared to biomedical therapy
alone in patients with subacute LBP in a randomized
controlled clinical trial. Participants were random-
ized into either the conventional biomedical therapy
(MT) group (n=31) or the biopsychosocial treatment
(BT) group (n=33). All participants received 6 hours of
treatment per day for 15 days over the course of 3 weeks.
The MT group received physiotherapy, group therapy
in water, workout, passive interventions such as mas-
sage and physical therapy and education on stretch-
ing, strengthening and improving mobility and body
control. The BT group received the same biomedical
therapy as the MT group, but additionally received
additional psychotherapy and relaxation therapy 3
and 4 times per week, respectively. Questionnaires
were completed at baseline, immediately after the
3-week therapy program and at 6-month follow-up.
At each time point, pain was assessed using a numeric
rating scale (NRS), mobility per the nger-oor-test,
torque of abdominal muscles, functional capacity per
the Hannover Functional Status Questionnaire-Back
(FFbH-R), depressive dysfunction (CES-D) and sick
leave data according to the patient’s insurance com-
pany. A total of 32 (97%) and 29 (94%) participants
completed the post-treatment evaluation at 3 weeks
in the BT and MT groups, respectively. Both groups
experienced improvement in pain intensity and func-
tional capacity of the back (FFbH-R) after 3 weeks, but
the BT group experienced signicantly greater im-
provements at 6 months compared to the MT group.
The BT group required signicantly less sick leave
(912 days of leave) with 13 out of 22 (59%) not requir-
ing further sick leave due to LBP compared to the MT
group (2,228 days of leave) with 2 out of 20 (10%) not
requiring further sick leave due to LBP. The authors
concluded that a biopsychosocial treatment program
for patients with LBP is benecial in improving pain,
functional status and work performance compared
to conventional biomedical therapy alone. The work
group downgraded this potential Level I article due to
small sample size and less than 80% follow-up. This
study provides Level II evidence that CBT can decrease
sick leave (improve return to work) as well as pain and
depression compared to control treatment.
Smeets et al
11
conducted a randomized controlled tri-
al to compare active physical, cognitive-behavioral
therapy (CBT) and a combined treatment for chronic
LBP compared to a wait list control group. Participants
with LBP >3 months from three dierent rehabilita-
tion centers were randomized into the Active Physical
Treatment group (APT), CBT group, Combined Treat-
ment group, or Waitlist group (WL). The APT group
(n=53) received aerobic training, individually adjust-
ed based on heart rate and perceived exertion, along
with strengthening exercises. The participants in the
CBT group (n=58) did not receive strength or aerobic
exercises but gradually increased daily activity lev-
el using operant behavioral graded activity training
and participated problem solving training (PST) with
a trained psychologist or social worker to help reach
their goals and modify dysfunctional believes relat-
ed to LBP. The Combined Treatment group (n=61)
received the same training as the APT group and the
PST portion of the CBT group. Each treatment group
received 10 weeks of treatment. The WL group (n=51)
was oered individual treatment after 10 weeks. Each
participant completed a questionnaire at baseline,
immediately after treatment and 6 and 12 months
after treatment to measure functional limitation per
the Roland Morris Disability Questionnaire (RMDQ),
pain and severity of complaints using a 100-mm VAS,
depression per the Beck Depression Inventory, glob-
al assessment of overall results using an ordinal scale
and treatment satisfaction using a 100-mm VAS. A
total of 52, 55, 55 and 50 participants were available
for analysis immediately after the 10-week treatment
period in the APT, CBT, Combined Treatment and WL
groups, respectively. For various reasons such as re-
jection of treatment or non-LBP-associated medical
or psychological problems, some of those participants
did not complete sucient training. A total of 83%
completed the appropriate APT sessions, 78% and
76% had sucient GA and PST sessions (respective-
ly) in the CBT group and 72% and 62% had sucient
physical training and GA/PST (respectively). Using an
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
86
intention-to-treat analysis, RMDQ, pain and severity
of complaints signicantly improved in all three treat-
ment groups compared to the WL group. The authors
concluded that all 3 treatment groups were more ef-
fective than the wait list group, but were not statisti-
cally signicantly dierent from each other. The work
group downgraded this potential Level I study due to
a follow-up rate less than 80%. This study provides
Level II evidence that CBT is better than control (no
treatment), but not better than physical treatment
alone in terms of pain and disability at 10 weeks.
Future Directions for Research
The work group recommends future studies that clearly identify what types of
psychosocial interventions (eg, CBT, neuroscience education), in what frequency
and what combination is most eective for the treatment of LBP.
References
1. Bendix AF, Bendix T, Ostenfeld S, Bush E, Andersen n.
Active treatment programs for patients with chronic low
back pain: a prospective, randomized, observer-blinded
study. Eur Spine J. 1995;4(3):148-152.
2. Dufour N, Thamsborg G, Oefeldt A, Lundsgaard C,
Stender S. Treatment of chronic low back pain: A ran-
domized, clinical trial comparing group-based mul-
tidisciplinary biopsychosocial rehabilitation and in-
tensive individual therapist-assisted back muscle
strengthening exercises. Spine. 2010;35(5):469-476.
3. Lamb SE, Lall R, Hansen Z, et al. A multicentred ran-
domised controlled trial of a primary care-based cog-
nitive behavioural programme for low back pain. The
Back Skills Training (BeST) trial. Health Technol Assess.
2010;14(41):1-253, iii-iv.
4. Linden M, Scherbe S, Cicholas B. Randomized controlled
trial on the eectiveness of cognitive behavior group
therapy in chronic back pain patients. J Back Musculo-
skeletal Rehabil. 2014;27(4):563-568.
5. Sullivan MJ, Adams H. Psychosocial treatment tech-
niques to augment the impact of physiothera-
py interventions for low back pain. Physiother Can.
2010;62(3):180-189.
6. Turner JA, Jensen MP. Ecacy of cognitive therapy for
chronic low back pain. Pain. 1993;52(2):169-177.
7. Hampel P, Tlach L. Cognitive-behavioral management
training of depressive symptoms among inpatient or-
thopedic patients with chronic low back pain and de-
pressive symptoms: A 2-year longitudinal study. J Back
Musculoskeletal Rehabil. 2015;28(1):49-60.
8. Monticone M, Ambrosini E, Rocca B, Magni S, Brivio
F, Ferrante S. A multidisciplinary rehabilitation pro-
gramme improves disability, kinesiophobia and walk-
ing ability in subjects with chronic low back pain: re-
sults of a randomised controlled pilot study. Eur Spine J.
2014;23(10):2105-2113.
9. Pincus T, Anwar S, McCracken LM, et al. Delivering an
Optimised Behavioural Intervention (OBI) to people
with low back pain with high psychological risk; results
and lessons learnt from a feasibility randomised con-
trolled trial of Contextual Cognitive Behavioural Ther-
apy (CCBT) vs. Physiotherapy. BMC Musculoskelet Disord.
2015;16 (1) (no pagination)(147).
10. Schiltenwolf M, Buchner M, Heindl B, Von Reumont
J, Muller A, Eich W. Comparison of a biopsychosocial
therapy (BT) with a conventional biomedical therapy
(MT) of subacute low back pain in the rst episode of
sick leave: A randomized controlled trial. Eur Spine J.
2006;15(7):1083-1092.
11. Smeets RJ, Vlaeyen JW, Hidding A, et al. Active rehabil-
itation for chronic low back pain: cognitive-behavioral,
physical, or both? First direct post-treatment results
from a randomized controlled trial [ISRCTN22714229].
BMC Musculoskelet Disord. 2006;7:5.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
87
QQ
Med/Psych Question 6. In patients with low back pain, does the timing of cognitive
behavioral therapy (CBT) and/ or psychosocial intervention and/or neuroscience
education aect duration of pain, intensity of pain, functional outcomes, anxiety,
depression and return-to-work status?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that future studies of cognitive behavioral therapy
should also include timing and duration of this treatment.
QQ
Med/Psych Question 7. In patients undergoing interventional or surgical treatment
for low back pain, does the addition of cognitive behavioral therapy (CBT) and/or
psychosocial intervention add incremental benet?
There is insucient evidence to make a recommendation for or against the addition of cognitive
behavioral therapy or psychosocial intervention for patients undergoing interventional or surgi-
cal treatment for low back pain and whether it would provide incremental benet.
Grade of Recommendation: I
Rolving et al
1
conducted a randomized clinical trial to
evaluate the cost-eectiveness of a CBT intervention
compared to usual care in patients undergoing lum-
bar spinal fusion surgery (LSF). Patients with chron-
ic LBP scheduled for LSF who met inclusion criteria
were randomly allocated into a control group (n=31)
or CBT group (n=59). All participants received usual
care of the LSF operation and rehabilitation 3 months
post-surgery. The CBT group received additional pre-
operative CBT intervention to address pain-coping
strategies. Quality-adjusted life years (QALYs) were
calculated based on EQ-5D scores; a societal view-
point was adapted to calculate costs. There was no
dierence in the overall cost between groups, but the
CBT group had a statistically-signicantly more fa-
vorable QALY than the control group at one-year fol-
low-up (0.071 QALY, 95% CI: 0.001-0.139, p=0.045).
Compared to the control group, the CBT group experi-
enced greater reductions in disability per the Oswestry
disability index (ODI) at 3 months (p=0.003) and 6
months (p=0.047) but not at one year (p=0.082). The
authors concluded that preoperative CBT was more
eective and cost-neutral in the treatment of LSF sur-
gery. This study provides Level I evidence that, in pa-
tients undergoing lumbar fusion, the addition of CBT
improves function at 3 and 6 months but not at one
year.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
88
Future Directions for Research
The work group recommends future studies to evaluate whether the addition of
cognitive behavioral therapy or psychosocial intervention add incremental ben-
et in patients undergoing interventional or surgical treatment for LBP.
References
1. Rolving N, Sogaard R, Nielsen CV, Christensen FB, Bung-
er C, Oestergaard LG. Preoperative cognitive-behavioral
patient education versus standard care for lumbar spi-
nal fusion patients: Economic evaluation alongside a
randomized controlled trial. Spine. 2016;41(1):18-25.
QQ
Med/Psych Question 8. Does educating a patient about low back pain improve
treatment compliance and outcomes, including duration of pain, intensity of pain,
functional outcomes, anxiety, depression and return-to-work status?
There is conicting evidence to make a recommendation for or against the use of patient edu-
cation to improve treatment compliance and outcomes, including duration of pain, intensity of
pain, functional outcomes, anxiety, depression and return-to-work status.
Grade of Recommendation: I
Cherkin et al
1
evaluated the relative eectiveness
of physical therapy, chiropractic manipulation and
an educational booklet for the treatment of LBP in a
randomized controlled trial. Adults with LBP (n=321)
were randomized to receive one of the three treat-
ments for one month and recorded bothersomeness of
symptoms on an 11-point scale along with a 24-point
Roland Disability Scale. There were no signicant dif-
ferences in outcomes between the chiropractic and
physical therapy group; both groups reported slight
and insignicantly less severe symptoms than the
educational booklet group after treatment. The au-
thors concluded that the eects of physical therapy
and chiropractic manipulation had similar eects and
costs and were marginally better than the eects of
the educational booklet. This study provides Level I
evidence that patient education did not improve out-
comes compared to standard care.
In a randomized controlled trial, Basler et al
2
evaluated the eect of counseling based on the
Transtheoretical Model (TTM) in elderly patients with
LBP. Elderly participants with LBP (n=170) received
10 20-minute physiotherapy sessions. Prior to each
session, the experimental group (n=86) received an
additional 10 minutes of TTM-based counseling while
the placebo group (n=84) received an ultrasound
treatment with an inactivated device. There were no
signicant dierences in outcomes such as duration
of physical activity, functional capacity, or range of
motion between groups after treatment. The authors
concluded that a TTM-based motivation program is
not superior to placebo in the treatment of LBP. This
study provides Level II evidence that, in older adults
with chronic LBP, education combined with physical
therapy did not improve outcomes at 6 months when
compared to physical therapy alone.
Berwick et al
3
conducted a randomized prospective
trial to compare the eects of an educational pam-
phlet against a single 4-hour back school psychoed-
ucational session with or without a one-year program
encouraging self-management for the treatment of
LBP. A total of 222 participants were randomized into
one of the 3 treatment groups. There were no signi-
cant dierences between groups in pain or functional

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
89
status at 3, 6, or 12 months after enrollment. The au-
thors concluded that a short version of back school,
with or without follow-up reinforcement, is not likely
to aect pain and disability in patients with LBP. This
study provides Level II evidence that the addition of
back school does not improve pain reduction as com-
pared to usual care for acute LBP.
Cecchi et al
4
conducted a randomized trial to com-
pare treatments for LBP. Patients with LBP (n=210)
were randomized to receive spinal manipulation (4-6
20-minute sessions once-a-week), back school with
group exercise and education/ergonomics (15 one-
hour sessions for 3 weeks), or individual physiothera-
py with exercise, passive mobilization and soft-tissue
treatment (4-6 20-minute sessions once per week).
Pain and function were assessed by Pain Rating Scale
and Roland Morris Disability Questionnaire, respec-
tively, at 3, 6 and 12 months. The authors concluded
that spinal manipulation provided functional im-
provement and more pain relief compared to back
school or individual physiotherapy. This study pro-
vides Level II evidence that spinal manipulation ther-
apy has greater treatment eect than either physical
therapy or back school in improving disability.
In order to assess the eectiveness of routine phys-
iotherapy compared with advice on remaining active,
Frost et al
5
conducted a randomized controlled trial of
286 patients with LBP. Although the patients in the
physiotherapy group reported greater perceived ben-
et, there were no signicant dierences in scores of
the Oswestry disability index, Roland and Morris dis-
ability questionnaire, or SF-36 12 months after en-
rollment. The authors concluded that routine phys-
iotherapy was no more eective than one session of
assessment and advice from a physiotherapist. This
study provides Level II evidence that routine physio-
therapy for mild to moderate LBP is no more eective
than a session with a physiotherapist that includes
advice.
Hsieh et al
6
conducted a randomized trial to compare
the eectiveness of back school, joint manipulation,
myofascial therapy and combined joint manipulation
and myofascial therapy with 200 patients with LBP.
Participants received the assigned treatment for 3
weeks. Pain per a visual analog pain scale and activity
per the Roland-Morris activity scale were recorded at
baseline, immediately after treatment and 6 months.
There were no statistically signicant dierences
found between groups at either time point. The au-
thors concluded that back school was as eective as
joint manipulation, myofascial therapy or a combi-
nation of the two for treatment of subacute LBP. This
study provides Level II evidence that back school was
no more eective than standard treatment.
In a multicenter randomized controlled trial, John-
son et al
7
evaluated the eect of a group exercise and
education program for the treatment of LBP. All par-
ticipants (n=234) received an educational booklet and
audio-cassette with advice on self-management of
LBP. Participants were randomized into a 6-week in-
terventional program (n=116) consisting of 8 2-hour
group sessions with exercise and education delivered
using a CBT approach or a control group (n=118) which
did not receive any additional intervention. The inter-
vention group showed only a small but nonsignicant
eect at reducing pain and disability compared to the
control group at 12-month follow-up. The authors
concluded that the intervention program produc-
es only modest eects in reducing LBP and disability
over a one-year period. This study provides Level II
evidence (moderate) that exercise with CBT approach
is no more eective than education with booklets
alone.
Karjalainen et al
8
conducted a multicenter random-
ized controlled trial to study the eectiveness of a
mini-intervention with or without an additional
worksite visit compared to usual care for treatment
of LBP. The patients in the mini-intervention group
(n=56) received consultations with a physician and
physiotherapist which included education, encour-
agement of physical activity and exercise planning.
The worksite visit group (n=51) received the same
treatment, but had an additional visit with a physio-
therapist, nurse and physician at each participant’s
workplace to ensure and encourage proper adoption
of the previous instructions. The patients in the usu-
al care group (n=57) received a leaet on back pain
and were treated by their general practitioners. There
were no signicant dierences in pain intensity, per-
ceived disability or health-related quality of life be-
tween groups at 3, 6, 12 or 24 months. The authors
concluded that the mini-intervention is an eective
treatment for subacute LBP. This study provides Level
II evidence that mini-intervention does not appear to
be more eective than worksite visit or usual care.
Leclaire et al
9
evaluated the ecacy of a back school
program compared to physiotherapy alone for
the treatment of LBP in a randomized controlled
trial. Participants were randomized to receive daily
physiotherapy (n=86) or back school with daily
physiotherapy plus 3 90-minute education sessions
at weeks 0, 1 and 8 (n=82). There were no dierences

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
90
between groups in terms of time o work for LBP,
duration of recurrences in the year after enrollment,
level of pain, spinal mobility, active straight-leg
raising, or functional disability per the Oswestry or
Roland-Morris scales at post-treatment, 6-month,
or 12-month follow-up. The authors concluded that
back school did not reduce time to return to work or
the number or duration of recurrences of LBP after one
year. This study provides Level II evidence that back
school does not improve outcomes of physiotherapy
for treatment of acute LBP in workers.
In a randomized controlled trial, Magalhaes et al
10
compared the eectiveness of graded activity and
physiotherapy for the treatment of LBP. Participants
were randomly assigned to groups and received
individual sessions twice a week for 6 weeks. The
graded activity group (n=33) included moderate
intensity treadmill walking, brief education and
strength exercises. The physiotherapy group (n=33)
included strengthening, stretching and motor control.
There were no signicant dierences in pain (Pain
Numerical Rating Scale) or disability (Rolland-Morris
Disability Questionnaire) between groups after 6
weeks. The authors concluded that graded activity and
physiotherapy have similar eects for patients with
chronic LBP. This study provides Level II evidence
that graded activity and physiotherapy exercises have
similar benecial eects in patients with chronic LBP.
Ribeiro et al
11
conducted a randomized controlled trial
to evaluate the eectiveness of a 4-week back school
program for the treatment of LBP. Patients random-
ized into the intervention group (n=29) received 5
one-hour group sessions of back school which in-
cluded education, exercise and relaxation. Partici-
pants in the control group (n=31) had weekly medical
visits without education. There were no signicant
dierences between the groups in pain (pain visual
analogical scale), functional status (Roland-Morris
Disability Questionnaire), anxiety or depression at
30, 60 or 120 days after enrollment. The authors con-
cluded that the back school program was ineective
in improving quality of life domains, pain, function-
al status, anxiety and depression. This study provides
Level II (weak) evidence that back school is no more
eective than meeting with the provider to talk about
their pain.
Sparkes et al
12
conducted a randomized controlled
trial to assess the eectiveness of an evidence-based
booklet, The Back Book, for the treatment of LBP. Af-
ter referral from a general practitioner to a spinal pain
clinic, participants were randomized into an inter-
vention group who received The Back Book (n=33) or a
control group who did not receive the booklet (n=29).
At the time of the initial appointment at the spinal
pain clinic, there were no signicant dierences be-
tween groups in pain (VAS) or disability (Roland Mor-
ris Disability questionnaire). The authors concluded
that The Back Book may not be suitable if used alone
for the treatment of LBP. In critique of the methodol-
ogy, the work group downgraded this potential Level
I study due to the small sample size without a power
analysis reported. Therefore, this study provides Lev-
el II (weak) evidence that The Back Book is not eec-
tive when given in isolation.
Göhner et al
13
studied the eects of a cognitive-
behavioral training program for the treatment of
patients with LBP. Patients were enrolled in an
exercise plus a CBT program (n=25) or exercise only
program (n=22) for 6-8 weeks. Although there were
signicant dierences in self-ecacy, perceptions
and frequency of exercise, there were no dierences
regarding pain intensity between groups immediately
after the program or 3 or 6 months post-treatment.
The authors concluded that the CBT program is an
eective tool to enable patients with LBP to follow
treatment recommendations. This study provides
Level III evidence that the addition of CBT enhances
treatment compliance but does not improve pain
outcomes with exercise therapy for LBP.
In a randomized controlled trial, Cherkin et al
14
eval-
uated the eects of two educational interventions for
the treatment of LBP compared to a control group.
Patients received usual care (n=98) or an educational
booklet with (n=103) or without (n=98) a 15-minute
session with a clinic nurse who reviewed the booklet,
answered questions, provided encouragement and
assisted with goal development related to exercise.
Outcomes of satisfaction with care, perceived knowl-
edge, participation in exercise, functional status,
symptom relief and health care use were assessed at
1, 3, 7 and 52 weeks after the intervention. Although
the participants in the nurse intervention group re-
ported greater satisfaction and perceived knowledge,
there were no signicant dierences between groups
in terms of functional status, health care use or worry.
The authors concluded that the educational interven-
tions had no impact on symptoms, function, disabili-
ty, or health care use. In critique of the methodology,
the work group downgraded the Level of evidence due
to nonmasked reviewers and patients. This study pro-
vides Level II evidence that patient education did not
improve outcomes compared to standard care.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
91
DuBois et al
15
studied the ecacy of a rehabilitation-
oriented coaching intervention compared to a usual
care control group for the treatment of LBP. In a
randomized controlled trial, patients allocated to the
intervention group (n=252) received medical advice
during a disability evaluation during the rst, second
and third month of sick leave. Patients randomized to
the control group (n=257) received a brief disability
evaluation during the third month of sick leave without
medical advice. Results revealed that the patients in
the intervention group had a statistically signicantly
higher return-to-work rate at one year. The authors
concluded that a disability evaluation should include
reassurance and advice about LBP. This study provides
Level I evidence that combined counseling and
disability evaluation by a medical adviser results in a
higher return-to-work rate due to a lower sick leave
recurrence than disability evaluation alone.
Durmus et al
16
evaluated the eectiveness of an ex-
ercise program with or without back school for the
treatment of LBP in a randomized controlled trial.
Subjects (all female) participated in 60 minutes of
exercise therapy 3 times a week for 3 months. The
intervention group (n=61) received back school edu-
cation in addition to exercise therapy while the con-
trol group (n=60) only participated in the exercises.
Both groups showed improvements in outcomes after
therapy. Compared to the control group, the interven-
tion group had signicantly greater improvements for
pain (per the VAS and pain disability index), pain and
disability according to the Oswestry Disability Ques-
tionnaire, trunk and knee muscle strength, endurance
and walking performance. The authors concluded
that back school increases the eectiveness of exer-
cise programs for the treatment of LBP. This paper
provides Level I evidence that, in females, back school
in combination with specic exercise programs was
more eective than specic exercise therapy alone in
patients with chronic LBP.
Van den Hout et al
17
aimed to evaluate the supplemen-
tal value of problem-solving therapy when added to
behavioral graded activity for the treatment of LBP in
a randomized controlled trial. The participants in the
intervention group (n=45) received behavioral graded
therapy, group education and CBT focusing on prob-
lem solving for application in daily life. The control
group (n=39) received behavioral graded activity and
group education without problem-solving therapy.
The participants in the intervention group had fewer
days of sick leave in the second half-year after inter-
vention. The authors concluded that there was value in
adding problem-solving therapy to behavioral graded
activity for the treatment of LBP. This study provides
Level I evidence that the addition of problem-solving
therapy to behavioral graded activity had supplemen-
tal value in employees with non-specic LBP.
In a cluster randomized trial, Albaladego et al
18
inves-
tigated the ecacy of a short education and physio-
therapy program for the treatment of LBP. All partic-
ipants received advice, drug treatment and potential
diagnostic procedures as part of usual care for LBP. The
control group (n=109) additionally received a booklet
and group education session on healthy nutrition hab-
its. The Education Group (n=139) was given The Back
Book with a corresponding education session. The Ed-
ucation + Physiotherapy Group (n=100) received the
same education as the Education Group in addition to
an additional booklet and education session on pos-
tural hygiene and 4 one-hour group sessions focusing
on relaxation techniques, stretching, active exercises
and encouragement to continue those movements at
home. Compared to the control group, participants in
both intervention groups had signicantly greater im-
provements in disability per the Roland Morris Ques-
tionnaire and pain per the VAS. The authors concluded
that the short education program added to usual care
of patients with LBP leads to small improvements in
disability, pain and quality of life. This study provides
Level II evidence that physical therapy plus a short
education program improves outcomes compared to
physical therapy alone at 6 months.
Friedrich et al
19
conducted a randomized controlled
trial to evaluate the eect of an exercise and motiva-
tional program in the treatment of LBP. Participants
were randomly assigned to the control group (n=49)
with standard exercise or the motivational interven-
tion group (n=44) with exercise combined with ex-
tensive counseling, information and reinforcement
techniques. Pain (according to a 101-point numerical
scale), disability (per a 13-question questionnaire)
and working ability were measured at 3.5 weeks, 4
months, 12 months and 5 years. The intervention
group had greater improvements in disability at all
time points and greater decrease in pain at 5 years.
Improvement in working ability was only found in the
intervention group. The authors concluded that the
combined exercise and motivation group was superior
to the standard exercise program. This study provides
Level II evidence that a motivational program (ie, ed-
ucational program) improves the outcome of exercise
treatment for LBP in terms of function, pain and var-
ious other factors included in the cumulative eects
at 5 years.
Heymans et al
20
conducted a randomized controlled

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
92
trial to assess the eectiveness of a low-intensity and
high-intensity back school compared to usual care for
workers who were sick-listed due to LBP. The partic-
ipants in the usual care group (n=103) received advice
to continue normal activities as much as possible. The
participants in the low-intensity group (n=98) par-
ticipated in 4 sessions of exercise (90 minutes) plus
education (30 minutes) each week for 4 weeks. The
participants in the high-intensity group (n=98) par-
ticipated in 2 one-hour exercise sessions per week
for 8 weeks. Sick leave was recorded throughout the
study along with pain intensity (VAS) and function-
al status (Roland Morris Disability Questionnaire) at
baseline and 3 and 6 months. The authors concluded
that the low-intensity back school was most eec-
tive in reducing work absence, functional disability
and kinesiophobia. This study provides Level II evi-
dence of the positive eects on work absence for a
low-intensity back school compared with the eects
of a high-intensity back school and usual care during
six months follow-up, in workers sick-listed for sub-
acute nonspecic LBP. Treatment eects on the sec-
ondary outcomes functional status, kinesiophobia
and perceived recovery were borderline signicant
at 3 and 6 months, also in favor of the low-intensity
back school. Dierences between groups concerning
pain relief were small and not statistically signicant.
Indahl et al
21
studied the long-term eects of an edu-
cation program for treating LBP in a controlled clin-
ical trial. Subjects in the intervention group (n=245)
participated in a “mini back school” which focused
on an explanation of back pain and encouragement
to decrease fear about LBP. Subjects in the control
group (n=244) were not called in for an examination
and were treated in the conventional medical system.
There were fewer recurrences of sick days for the pa-
tients in the intervention group compared to control
group. The authors concluded information designed
to reduce fear and increase light activity may help re-
duce long-term disability in patients with LBP. This
study provides Level II evidence (moderate) that ed-
ucation to reduce fear may improve return-to-work
status.
Pengel et al
22
compared the eectiveness of a
physiotherapist-directed exercise program, advice
or both for the treatment of LBP in a randomized
controlled trial. Participants (n=259) were randomized
into one of 4 groups: exercise (individualized
progressive therapy guided by a physiotherapist) and
advice (graded return to normal activity encouraged
by a physiotherapist), exercise and sham advice,
sham exercise and advice, or sham exercise and
sham advice. Pain (scale, 0-10), function (Patient-
Specic Functional Scale), global perceived eect
(11-point scale), disability (Roland-Morris Disability
Questionnaire), number of health care contacts and
depression (Depression Anxiety Stress Scales-21)
were measured at 6 weeks and 12 months. When
combined, exercise and advice had greater eects
at 6 weeks for all outcomes, but had greater eects
only on function at 12 months. The authors concluded
that exercise and advice were more eective for the
treatment of LBP compared to placebo at 6 weeks,
with greater eects observed when the two were
combined. This study provides Level II evidence that
exercise and advice were slightly better than exercise
alone at 12 months follow-up in terms of function for
treatment of subacute LBP.
Tavaan et al
23
conducted a randomized controlled
trial to assess the eect of a health education pro-
gram, “Back School Programme,” on quality of life
in patients with LBP. Female participants with LBP
were randomized into the intervention group (n=50)
to receive a physician evaluation followed by a 4-day,
5-session health education program or a control
group (n=52) to receive only the initial physician eval-
uation and standard care. Quality of life was measured
using the Short Form Health Survey (SF-36) at base-
line and at three months follow-up. The intervention
group had signicantly better outcomes. The authors
concluded that the “Back School Programme” might
improve the quality of life over 3 months in patients
who experience chronic LBP (CLBP). In critique of the
methodology, the work group downgraded this po-
tential Level I study due to lack of generalizability.
This study provides Level II evidence that Back School
was more eective than a control nonintervention
population of female patients with CLBP in this short-
term study.
Zhang et al
24
conducted a randomized controlled tri-
al to compare the eects of a 12-week exercise pro-
gram with health education on active management
and postural hygiene compared to exercise alone for
the treatment of LBP. Participants were randomized
to receive education plus exercise (n=25) or exercise
along (n=24) and recorded pain, disability (Oswestry
Disability Index), muscle endurance and quality of life
(SF-36) at baseline and immediately after treatment.
Pain, disability and SF-36 results were signicant-
ly better in the health education group compared to
the exercise-only group. This study was downgrad-
ed from Level I due to small sample size and provides
Level II evidence that health education provides addi-
tional benets over and above lumbar exercise alone

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
93
for improving the pain, disability and health-related
quality-of-life of young patients (aged 18–30 years)
with chronic LBP.
In a randomized controlled trial, Basler et al
25
assessed
the eects of medical treatment plus cognitive-
behavioral treatment in the treatment of LBP.
The participants in the intervention group (n=36)
received usual medical treatment plus 12 weekly
2.5-hour cognitive-behavioral treatment sessions
focusing on education, relaxation, modied thoughts
and feelings, enhancement of pleasant activities
and training of good postural habits. The control
group (n=40) received medical treatment only. The
intervention group experienced less pain, better pain
control, more pleasurable activities, less avoidance,
less catastrophizing and reduced disability compared
to the medical treatment only group. The authors
concluded that the cognitive-behavioral treatment
added to medical care resulted in better outcomes
compared to medical treatment alone. This study
provides Level III evidence that a treatment package
of cognitive-behavioral and standard care is more
eective than standard care alone.
Castagnoli et al
26
compared the eects of global pos-
tural reeducation (GPR) to standard physical therapy
(PT) for the treatment of LBP. All subjects received
educational booklets and a home exercise program.
The PT group (n=45) received an individualized
treatment guided by a physiotherapist while the GPR
group (n=45) were subjected to a postural assessment
in which postures were selected to correct identi-
ed muscle imbalances. Both groups received 15 six-
ty-minute sessions twice weekly. Both groups experi-
ences improvement in pain and function at discharge
(15 working days after enrollment), but only the GPR
group sustained those improvements at 12 months af-
ter discharge. The authors concluded that GPR and PT
both result in short-term improvements in function
and pain; GPR may have longer lasting eects com-
pared to PT. This study provides Level III evidence
that patients who received global postural reeduca-
tion still reported statistically signicant pain relief
compared to baseline and a lower frequency of pain.
Gremeaux et al
27
conducted a randomized study to
evaluate the eect of education workshops added to
spa therapy for the treatment of LBP. Participants
were randomized into the intervention group (n=188)
to receive 3 90-minute education sessions in ad-
dition to thermal therapy for 3 weeks or the control
group (n=172) to receive usual thermal therapy and
non-standardized verbal information. Both groups
had signicant reductions in physical fear-avoidance
beliefs (FABQ), disability and pain, with a signicant-
ly greater reduction in FABQ in the intervention group
only. The authors concluded that standardized educa-
tion workshops during spa therapy reduce the eect
of fear-avoidance beliefs and relieve pain in patients
with LBP. The work group downgraded the Level of
evidence for this study in critique of the methodology
due to nonmasked reviewers and patients. This study
provides Level II evidence that the addition of patient
education improves the outcomes of spa therapy for
LBP.
Iles et al
28
compared the eects of telephone coaching
in addition to physiotherapy with physiotherapy
alone for the treatment of LBP in a randomized trial.
Participants were randomized into the intervention
group (n=15) to receive 5 sessions of telephone
coaching or the control group (n=15) to receive
physiotherapy alone. The coaching group had
signicantly greater scores for function (Patient
Specic Functional Scale) and recovery expectation.
The authors concluded that the addition of telephone
coaching to physiotherapy improved activity and
recovery expectation. This study provides Level III
evidence (weak) that telephone coaching may improve
patient-specic functional outcomes in patients with
chronic LBP.
Jaromi et al
29
hypothesized that nurses with LBP
would have signicantly decreased pain intensity lev-
els and improved body posture after completing a pro-
gram with ergonomics training and education (Back
School) once a week for 6 weeks compared to a control
group receiving passive physiotherapy once a week
for 6 weeks. Although both groups showed improve-
ment in pain intensity immediately after therapy, the
Back School group (n=56) had signicantly better
improvements at 6 months and one year compared to
the control group (n=55). The authors concluded that
Back School results in signicant improvements in
pain intensity and posture in nurses who are experi-
encing chronic lower back pain. This study provides
Level III evidence that, in working nurses with chron-
ic LBP, the addition of back school to passive physical
therapy results in a signicantly better result at one
year than physical therapy alone.
Paolucci et al
30
conducted a randomized controlled
trial to evaluate the eect of a Back School program in
the treatment of LBP. The intervention group (n=29)
participated in a 4-week multidisciplinary Back
School program with education and exercise while
the control group (n=21) received medical assistance
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
94
only. Signicant improvements in quality of life (SF-
36), disability (Waddell Disability Index and Oswestry
Disability Index) and pain (VAS) were observed in the
intervention group. Additional mental component
improvements in the SF-36 were observed in the pa-
tients in the intervention group who had at least one
scale elevation in Minnesota Multiphasic Personality
Inventory-II (MMPI-II) scores. The authors conclud-
ed that Back School has positive eects in patients
with at least one scale elevation of MMPI-II. The work
group downgraded the level of evidence of this study
due to small sample size. This study provides Level II
evidence for the eectiveness of back school.
Burton et al
31
conducted a randomized controlled
trial to study the eects of a novel educational
booklet on patients’ beliefs on LBP and functional
outcomes. Patients with LBP received The Back Book
with evidence-based information and advice (n=53)
compared to a traditional booklet control group
(n=50). The participants who received The Back
Book had signicant improvements in beliefs about
physical activity at 2 weeks, 3 months and one year.
There were no statistically signicant dierences
between groups in pain or disability. The authors
concluded that carefully selected information and
advice on LBP can have a positive eect on outcomes
for individuals with LBP. This study provides Level II
evidence that patient education can improve function
but not pain up to 3 months following usual treatment
for LBP.
Future Directions for Research
The work group recommends future studies to evaluate whether the inclusion of
patient education impacts LBP treatment compliance and outcomes.
References
1. Cherkin DC, Deyo RA, Battié M, Street J, Barlow W. A
comparison of physical therapy, chiropractic manipu-
lation, and provision of an educational booklet for the
treatment of patients with low back pain. N Engl J Med.
1998;339(15):1021-1029.
2. Basler HD, Bertalany H, Quint S, Wilke A, Wolf U. TTM-
based counselling in physiotherapy does not contribute
to an increase of adherence to activity recommenda-
tions in older adults with chronic low back pain - A ran-
domised controlled trial. Eur J Pain. 2007;11(1):31-37.
3. Berwick DM, Budman S, Feldstein M. No clinical eect
of back schools in an HMO. A randomized prospective
trial. Spine. 1989;14(3):338-344.
4. Cecchi F, Molino-Lova R, Chiti M, et al. Spinal manipu-
lation compared with back school and with individually
delivered physiotherapy for the treatment of chronic
low back pain: a randomized trial with one-year fol-
low-up. Clin Rehabil. 2010;24(1):26-36 11p.
5. Frost H, Lamb SE, Doll HA, Carver PT, Stewart-Brown S.
Randomised controlled trial of physiotherapy compared
with advice for low back pain. Bmj. 2004;329(7468):708.
6. Hsieh CY, Adams AH, Tobis J, et al. Eectiveness of four
conservative treatments for subacute low back pain: a
randomized clinical trial. Spine. 2002;27(11):1142-1148.
7. Johnson RE, Jones GT, Wiles NJ, et al. Active exercise,
education, and cognitive behavioral therapy for per-
sistent disabling low back pain: a randomized con-
trolled trial. Spine. 2007;32(15):1578-1585.
8. Karjalainen K, Malmivaara A, Mutanen P, Roine R, Hur-
ri H, Pohjolainen T. Mini-intervention for subacute low
back pain: two-year follow-up and modiers of eec-
tiveness. Spine. 2004;29(10):1069-1076.
9. Leclaire R, Esdaile JM, Suissa S, Rossignol M, Proulx R,
Dupuis M. Back school in a rst episode of compensated
acute low back pain: a clinical trial to assess ecacy and
prevent relapse. Arch Phys Med Rehabil. 1996;77(7):673-
679.
10. Magalhaes MO, Muzi LH, Comachio J, et al. The short-
term eects of graded activity versus physiotherapy in
patients with chronic low back pain: A randomized con-
trolled trial. Manual Therapy. 2015;20(4):603-609.
11. Ribeiro LH, Jennings MF, Jones A, Furtado R, Natour J.
Eectiveness of a back school program in low back pain.
Clin Exp Rheumatol. 2008;26(1):81-88.
12. Sparkes V, Chidwick N, Coales P. Eect of The Back
Book on fear-avoidance beliefs, disability, and pain
levels in subjects with low back pain. Int J Ther Rehabil.
2012;19(2):79-86 78p.
13. Göhner W, Schlicht W. Preventing chronic back pain:
evaluation of a theory-based cognitive-behavioural
training programme for patients with subacute back
pain. Patient Educ Couns. 2006;64(1-3):87-95.
14. Cherkin DC, Deyo RA, Street JH, Hunt M, Barlow W. Pit-
falls of patient education. Limited success of a program
for back pain in primary care. Spine. 1996;21(3):345-
355.
15. Du Bois M, Donceel P. Guiding low back claim-
ants to work: a randomized controlled trial. Spine.
2012;37(17):142
16. Durmus D, Unal M, Kuru O. How eective is a modi-
ed exercise program on its own or with back school in
chronic low back pain? A randomized-controlled clin-
ical trial. J Back Musculoskelet Rehabil. 2014;27(4):553-
561. 5-1431.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
95
17. Van Den Hout J, Vlaeyen J, Heuts P, Zijlema J, Wijen
JA. Secondary prevention of work-related disabili-
ty in nonspecic low back pain: does problem-solving
therapy help? A randomized clinical trial. Clin J Pain.
2003;19(2):87-96.
18. Albaladejo C, Kovacs FM, Royuela A, Pino R, Zamo-
ra J. The ecacy of a short education program and a
short physiotherapy program for treating low back
pain in primary care: a cluster randomized trial. Spine.
2010;35(5):483-496.
19. Friedrich M, Gittler G, Arendasy M, Friedrich KM.
Long-term eect of a combined exercise and motiva-
tional program on the level of disability of patients with
chronic low back pain. Spine. 2005;30(9):995-1000
1006p.
20. Heymans MW, de Vet HCW, Bongers PM, Knol DL, Koes
BW, van Mechelen W. The eectiveness of high-inten-
sity versus low-intensity back schools in an occupa-
tional setting: a pragmatic randomized controlled trial.
Spine. 2006;31(10):1075-1082 1078p.
21. Indahl A, Haldorsen EH, Holm S, Reikerås O, Ursin H.
Five-year follow-up study of a controlled clinical trial
using light mobilization and an informative approach to
low back pain. Spine. 1998;23(23):2625-2630.
22. Pengel LHM, Refshauge KM, Maher CG, Nicholas MK,
Herbert RD, McNair P. Physiotherapist-directed exer-
cise, advice, or both for subacute low back pain: a ran-
domized trial. Ann Intern Med. 2007;146(11):787-756
710p.
23. Tavaan SS, Jamshidi A, Mohammad K, Montazeri A.
Low back pain education and short term quality of life: a
randomized trial. BMC Musculoskelet Disord. 2007;8:21.
24. Zhang Y, Wan L, Wang X. The eect of health education
in patients with chronic low back pain. J Int Med Res.
2014;42(3):815-820.
25. Basler HD, Jäkle C, Kröner-Herwig B. Incorporation of
cognitive-behavioral treatment into the medical care
of chronic low back patients: a controlled randomized
study in German pain treatment centers. Patient Educ
Couns. 1997;31(2):113-124.
26. Castagnoli C, Cecchi F, Del Canto A, et al. Eects in
Short and Long Term of Global Postural Reeducation
(GPR) on Chronic Low Back Pain: A Controlled Study
with One-Year Follow-Up. Scientic World Journal.
2015;2015:271436.
27. Gremeaux V, Benaïm C, Poiraudeau S, Hérisson C,
Dupeyron A, Coudeyre E. Evaluation of the benets of
low back pain patients’ education workshops during spa
therapy. Joint Bone Spine. 2013;80(1):82-87.
28. Iles R, Taylor NF, Davidson M, O’Halloran P. Telephone
coaching can increase activity levels for people with
non-chronic low back pain: a randomised trial. J Phys-
iother. 2011;57(4):231-238.
29. Jaromi M, Nemeth A, Kranicz J, Laczko T, Betlehem J.
Treatment and ergonomics training of work-related
lower back pain and body posture problems for nurses. J
Clin Nurs. 2012;21(11/12):1776-1784 1779p.
30. Paolucci T, Morone G, Iosa M, et al. Psychological fea-
tures and outcomes of the Back School treatment in
patients with chronic non-specic low back pain. A
randomized controlled study. Eur J Phys Rehabil Med.
2012;48(2):245-253.
31. Burton AK, Waddell G, Tillotson KM, Summerton N.
Information and advice to patients with back pain can
have a positive eect. A randomized controlled trial
of a novel educational booklet in primary care. Spine.
1999;24(23):2484-2491.
QQ
Med/Psych Question 9. In patients undergoing treatment for low back pain, what
is the eectiveness of interventions that address fear-avoidance behaviors?
Treatments targeting fear avoidance combined with physical therapy are recommended com-
pared to physical therapy alone to improve low back pain in the rst 6 months.
Grade of Recommendation: A
George et al
1
conducted a multicenter randomized
controlled trial to compare physical therapy to fear-
avoidance-based physical therapy in patients with
acute LBP. Eligible patients were randomized into one
of 2 groups to receive either standard physical ther-
apy (n=32) or fear-avoidance-based physical ther-
apy (n=34). All participants received education and
a one-hour individualized treatment with exercise
prescriptions and progressions while recording home
participation in a diary. The participants in the fear-
avoidance-based physical therapy group additionally
received specic education with fear-avoidance mod-
el principles and a graded exercise program with pos-
itive reinforcement. At baseline, 4 weeks after treat-

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
96
ment and 6 months after treatment, each participant
completed a questionnaire that addressed disability
per the Oswestry Disability Questionnaire (ODQ), pain
intensity on a scale from 0 to 10 and fear-avoidance
beliefs per the Fear-Avoidance Beliefs Questionnaire
(FABQ). Using an intention to treat analysis, disabil-
ity and pain intensity improved in both groups. The
fear-avoidance beliefs signicantly improved in the
fear-avoidance therapy group and were signicantly
lower than the standard therapy group at both fol-
low-up time points. The authors concluded that pa-
tients with elevated fear-avoidance beliefs at base-
line experienced less disability with fear-avoidance
treatment compared to standard treatment; however,
those with reduced fear-avoidance fared worse with
an increase in fear-avoidance with the fear-avoid-
ance-based physical therapy. The work group down-
graded this potential Level I study due to recruitment
and small sample size. This study provides Level II
evidence that fear avoidance-based physical therapy
can improve outcomes more than standard physical
therapy for treatment of acute LBP in patients with
elevated fear-avoidance on screening questionnaire.
Screening would be indicated as a blanket approach
and would not work well without screening for fear
avoidance.
George et al
2
later conducted another multicenter
randomized controlled trial to compare physical ther-
apy to physical therapy combined with graded exer-
cise or graded exposure in patients with acute and
subacute LBP. Eligible patients were randomized into
a treatment-based classication (TBC) physical ther-
apy group (n=36), TBC plus graded activity/exercise
(GA) group (n=37), or TBC with graded exposure (GX)
group (n=35). The participants in the TBC group re-
ceived education and an individualized treatment.
The participants in the GA group received treatment
similar to the TBC group but augmented with grad-
ually increased activity according to pain tolerance.
The participants in the GA group rst completed a
questionnaire to indicate existing fear (such as lift-
ing more than 20 pounds) which the therapist used
to guide gradually-progressing activities to improve
movements related to that goal. Questionnaires were
administered at baseline, 4 weeks and 6 months which
collected demographic information, disability per the
Oswestry Disability Questionnaire (ODQ), fear-avoid-
ance beliefs per the Fear-Avoidance Beliefs Question-
naire (FABQ) and pain catastrophizing per the Pain
Catastrophizing Scale (PCS). Additionally, a blinded
physical therapist used the physical impairment scale
(PIS) at baseline and 4 weeks to quantify physical im-
pairment. A total of 26, 22 and 24 participants com-
pleted the 6-month follow-up in the TBC, GA and GX
groups, respectively. All groups experienced improve-
ment in ODQ scores; however, there were no signi-
cant dierences in improvements between groups. All
groups had an improvement in FABQ scores; both TBC
and GX showed signicant decreases in pain-relat-
ed fear (p<0.01). Intention to treat analyses showed
similar results as the completers-only analyses. The
authors concluded that in patients with LBP, add-
ing GA or GX to TBC was not eective for improving
outcomes. This study provides Level I evidence that
treatment-based classication physical therapy sup-
plemented with graded activity or graded exposure
was not eective for improving outcomes related to
the development of chronic LBP
Monticone et al
3
conducted a randomized, parallel-
group, superiority-controlled trial to evaluate the
ecacy of a CBT-based multidisciplinary program
on perceived disability, kinesiophobia, pain and
QoL in patients with nonspecic chronic LBP.
Patients with LBP for >3 months were randomized
to receive a program with exercise and CBT (n=45)
or an exercise-only program (n=45). All participants
received training on a 60-minute exercise program
that involved active and passive spine mobilization,
muscle strengthening and stretching and postural
control twice a week for a 5-week instructive phase
and were instructed to continue twice-weekly sessions
independently for a year. The participants in the
exercise and CBT (experimental) group additionally
received a 60-minute CBT session under the
supervision of a clinical psychologist once a week for
5 weeks followed by one session per month for a year.
All participants completed questionnaires at baseline,
after the 5-week instructive phase and then at 12
and 24 months. Questionnaires measured disability
per the Roland-Morris Disability Questionnaire
(RMDQ), fear-avoidance behaviors per the Tampa
Scale for Kinesiophobia (TSK), pain using an 11-point
numerical rating scale (NRS) and QoL per the Short-
Form (36) Health Survey (SF-36). No patients dropped
out during this study. The patients in the experimental
group experienced signicant improvements in
RMDQ, TSK, NRS and SF-36 scores (p<0.001 for all).
The authors concluded that the CBT and exercise
program was superior to the program with exercise
alone in reducing disability, fear-avoidance beliefs
and pain and enhancing the quality of life of patients
with chronic LBP. This study provides Level I evidence
that cognitive behavior therapy specically targeting
FAB can improve outcomes of treatment for chronic
LBP better than exercise alone for the rst year.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
97
Woods et al
4
conducted a randomized controlled trial to
evaluate the eectiveness of a graded in vivo exposure
(GivE) therapy program on improving self-ecacy
and reducing fear, avoidance, emotional distress,
perceived pain and perceived disability in patients with
LBP. A total of 85 participants met inclusion criteria
after recruitment through advertisement, had a score
≥38 on the Tampa Scale for Kinesiophobia (TSK) and
were randomized into one of 3 groups: GivE (n=36),
graded activity (n=25) and wait-list control (n=22). At
baseline, each participant completed a questionnaire
which included functional ability per the Pain Disability
Index (PDI), ratings of pain and psychological factors
per the Hospital Anxiety and Depression Scale
(HADS), McGill Pain Questionnaire-Short Form (SF-
MPQ), Pain Self-Ecacy Questionnaire (PSEQ), TSK,
Fear Avoidance Belief Questionnaire (FABQ), short
form of Pain Anxiety Symptoms Scale (PASS-20),
Pain Catastrophising Scale (PCS) and the Working
Alliance Inventory – Client Form (WAI). Participants
in both treatment groups received 8 individualized
45-minute therapy sessions over the course of four
weeks. The participants in the graded activity group
received therapy from a Registered Physiotherapist
along with positive reinforcement.
The participants in the GivE group received education
about the cognitive-behavioral perspective on fear-
avoidance and its consequences in addition to the
same treatment as the graded activity group. The
wait-list control group was oered participation
at a later time. A total of 15, 13 and 16 participants
completed the GivE, graded activity and wait-list
control therapy programs, respectively. Per an
intention-to-treat analysis, there were no signicant
dierences in outcomes between GivE and graded
activity. However, participants in the GivE group had
signicant improvements on the TSK (p = .011), FABQ
(p = .020), PCS (p = .010), HADS (p = .010) and SF-MPQ
(p = .030) compared to the wait-list control group.
With a complete case analysis, participants in the GivE
group had signicantly greater improvement in PSEQ
(p=0.028), TSK (p=0.008), FABQ (p=0.027) and PASS-
20 (p=0.027) compared to the graded activity group.
The work group determined this study provides Level
I evidence that graded activity exposure, targeted
towards decreasing fear avoidance behavior compared
to standard treatment or no treatment, can improve
outcomes in patients with chronic LBP.
Future Directions for Research
The work group recommends longer-term follow-up studies (one year or great-
er) to determine longitudinal benets of treatments targeting fear avoidance.
References
1. George SZ, Fritz JM, Bialosky JE, Donald DA. The eect
of a fear-avoidance-based physical therapy interven-
tion for patients with acute low back pain: results of
a randomized clinical trial. Spine. 2003;28(23):2551-
2560.
2. George SZ, Zeppieri Jr G, Cere AL, et al. A randomized
trial of behavioral physical therapy interventions for
acute and sub-acute low back pain (NCT00373867).
Pain. 2008;140(1):145-157.
3. Monticone M, Ferrante S, Rocca B, Baiardi P, Farra FD,
Foti C. Eect of a long-lasting multidisciplinary pro-
gram on disability and fear-avoidance behaviors in pa-
tients with chronic low back pain: results of a random-
ized controlled trial. Clin J Pain. 2013;29(11):929-938.
4. Woods MP, Asmundson GJG. Evaluating the ecacy of
graded in vivo exposure for the treatment of fear in pa-
tients with chronic back pain: A randomized controlled
clinical trial. Pain. 2008;136(3):271-280.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
98
QQ
Med/Psych Question 10. Is active treatment (pharmacological or
psychotherapeutic) of anxiety and depression eective in decreasing low back
pain?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends consideration of a clinical trial to assess whether
active treatment of depression or anxiety can improve back pain.
QQ
Med/Psych Question 11. What are the psychological factors inuencing
outcomes, including duration of pain, intensity of pain, functional outcomes and
return-to-work status, of low back pain treatment?
It is suggested that kinesiophobia is a negative prognostic factor for predicting response to low
back pain treatment.
Grade of Recommendation: B
Foster et al
1
conducted a prospective cohort study
across 8 general practices to evaluate the association
between psychological factors at the time of presen-
tation of LBP as well as the psychological factors that
predict clinical outcomes after 6 months. A total of
1,591 patients with LBP completed a questionnaire at
baseline which included the Roland and Morris Dis-
ability Questionnaire (RMDQ) and questions related
to sociodemographics and psychological factors. After
6 months, 810 patients completed the same question-
naire. At baseline, there were associations between
RMDQ scores and 18 out of 20 of the psychological
factors; the strongest correlations were found in per-
ceptions of consequences (IPQ-R), depression (HADS)
and pain self-ecacy (PSEQ). At 6 months, acute/
chronic timeline, illness identity, perceptions of per-
sonal control and pain self-ecacy were signicantly
predictive of LBP outcomes (RMDQ) using a reduced
multivariate model (n=761). The authors concluded
that patients who experience these four psychological
factors are more likely to have poor clinical outcomes.
The work group determined that this study provides
Level III evidence that perception of personal con-
trol, illness identity and pain self-ecacy were psy-
chological factors that were predictive of outcomes of
LBP treatment.
Helmhout et al
2
evaluated relationship of improve-
ment of chronic LBP and baseline individual factors,
pain-related factors, work-related psychosocial fac-
tors and psychological factors in a prospective cohort
study of data from three randomized controlled tri-
als. A total of 273 military employees, predominant-
ly male, were recruited by a general practitioner or
military advertisements. Each participant completed
a questionnaire at baseline which included functional
disability per the Roland-Morris Disability Question-
naire (RMDQ), details of LBP complaints (duration
and pain radiation), fear of movement per the Tam-
pa Scale for Kinesiophobia (TSK), psychological dis-
tress per the General Health Questionnaire (GHQ),
perceived social and coworker support and degree of
physical activity. Six months after treatment, partic-
ipants completed the same questionnaire again along
with perceived improvement (0-100%) or the Global
Perceived Eect (GPE). Improvement was dened by
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
99
improvement of ≥30% on the RMDQ and an improve-
ment of ≥20% of self-perceived improvement or a
GPE score of “completely recovered” or “much im-
proved.” Signicant associations were found between
long-term LBP improvement and RMDQ score of 4-7
(OR 2.29), RMDQ score ≥11 (OR 2.53) and TSK score
(OR 0.97) at baseline. The authors concluded that in-
dividuals with a high level of baseline disability and
fear avoidance behavior are at risk for poor long-term
recovery from LBP and may need additional cogni-
tive behavioral treatment. This study provides Level II
evidence that kinesiophobia can negatively inuence
the outcomes of LBP treatment.
Keeley et al
3
conducted a prospective cohort study to
assess the predictive relationship between both so-
cial and psychological factors at baseline with phys-
ical health-related quality of life (HRQoL) and health
service utilization in patients with mechanical LBP.
At baseline, each participant (n=108) completed a
questionnaire that included demographic informa-
tion, details of back pain, anxiety and depression
symptoms per the Hospital Anxiety and Depression
Scale (HADS), beliefs about the relationship between
physical activity and LBP per the Fear-Avoidance Be-
liefs Questionnaire (FABQ) and social stress per the
Life Events and Diculties Schedule (LEDS). Phys-
ical HRQoL was measured at baseline and 6 months
after initial assessment using the UK version of the
36-item Short-Form Health Survey (SF-36) Phys-
ical Component Score (PCS). Health care utilization
was measured for 6 months after initial assessment
using the Client Socio-Demographic and Service
Receipt Inventory (CSSRI). At 6-month follow-up,
baseline variables found to have a statistical signi-
cant prediction of physical HRQoL included duration
of pain (standardized regression coecient β=0.18,
p=0.04), HADS score (β=0.27,p=0.003) and back pain
related social diculties (β=0.42, p<0.0005). Fear
Avoidance Beliefs about work (Incident Rate Ratio
[IRR]=1.02,p=0.009), back pain related social di-
culties (IRR=1.16, p=0.03) and perceived cause of pain
(IRR=1.46, p=0.03) were independent predictors of
number of health care contacts. The authors conclud-
ed that anxiety, depression, fear avoidance beliefs re-
lating to work and back pain-related stresses are pre-
dictors of physical HRQoL and number of health care
utilization contacts. This study provides Level III evi-
dence that SF-36 scores improved in patients without
fear avoidance behavior before treatment.
Future Directions for Research
The work group recommends development of registries that collect information
regarding psychological factors that can inuence low back pain and quantita-
tive analysis of this information.
References
1. Foster NE, Thomas E, Bishop A, Dunn KM, Main CJ.
Distinctiveness of psychological obstacles to recov-
ery in low back pain patients in primary care. Pain.
2010;148(3):398-406.
2. Helmhout PH, Staal JB, Heymans MW, Harts CC, Hen-
driks EJ, Bie RA. Prognostic factors for perceived recov-
ery or functional improvement in non-specic low back
pain: secondary analyses of three randomized clinical
trials. Eur Spine J. 2010;19(4):650-659.
3. Keeley P, Creed F, Tomenson B, Todd C, Borglin G, Dick-
ens C. Psychosocial predictors of health-related quali-
ty of life and health service utilisation in people with
chronic low back pain. Pain. 2008;135(1-2):142-150.
Diagnosis & Treatment of Low Back Pain |
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
100
QQ
Med/Psych Question 12. In patients with low back pain, what psychosocial/
cognitive/emotional or other assessments should be utilized to establish an
accurate diagnosis?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that future studies on the evaluation and man-
agement of LBP specically identify psychological assessment that facilitate di-
agnostic accuracy.
QQ
Med/Psych Question 13. Does nutrition (other than weight reduction) inuence
the frequency of low back pain episodes?
* This question focuses on healthy eating, nutrition/diet and not weight reduction.
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends systematic evaluation of the role of nutrition and
nutraceuticals in the management of LBP.
Recommendations | Medical & Psychological Treatment

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
101
Section Authors
Guideline Co-Chair
D. Scott Kreiner, MD
Physical Medicine & Rehabilitatoin Section
Chair
Charles A. Reitman, MD
Members
R. Carter Cassidy, MD
Dennis Enix, DC, MBA
Daniel S. Robbins, MD
Alison A. Stout, DO
Ryan Tauzell, PT, MA, MDT
Follow-up rule for evidentiary review: Follow-up must be at least 6 weeks after active treatment for study to be
included unless otherwise noted
QQ
PM&R Question 1. In patients undergoing treatment for low back pain, what is
the eectiveness of the following in decreasing the duration of pain, decreasing
intensity of pain, increasing functional outcomes and improving return-to-work
status, as compared with natural history plus or minus medication:
PM&R Question 2. In patients undergoing treatment for low back pain, what is
the appropriate timing, frequency and duration of treatment with:
a. Acute versus subacute versus chronic
Q1 Recommendations:
Back school is recommended to provide improvements in pain and function when com-
pared with general medical care, modality care or a simple handout at 6-12 months’ fol-
low-up for chronic low back pain.
Grade of Recommendation: A
i. patient education and self-directed exercise program
Q1 Evidence Summary:
In a randomized controlled trial of patients with
chronic low back pain (LBP), Durmus et al
1
evaluat-
ed the eectiveness of the addition of back school to
a modied exercise program. Participants were ran-
domized to receive an exercise program with back
school (n=61) or exercise alone (n=60) 3 days a week
for 3 months. Pain (Visual Analog Scale, VAS) and dis-
ability (Oswestry Disability Questionnaire) were re-
corded at baseline, immediately after treatment and
at 6-month follow-up. The participants who received
back school in addition to exercise had signicantly
greater improvements in pain and disability. The au-
thors concluded that modied exercise programs can
be used to treat chronic LBP and that the addition of
back school can further increase the eect. This study
provides Level I therapeutic evidence that the addition
of low back school to an exercise program improves
pain and function at 6 months.
Hurri et al
2
evaluated the eect of a Swedish-type back
school in patients with chronic LBP in a randomized
controlled trial. Female patients with LBP for at least

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
102
12 months were invited to participate and random-
ized into a treatment group (n=95) or control group
(n=93). Patients in the treatment group completed 6
60-minute exercise and education sessions over three
weeks plus 2 additional 60-minute review classes af-
ter 6 months. The control group received written ma-
terials and otherwise continued regular follow-up
healthcare services. Pain (VAS and low back pain in-
dex), disability (Oswestry Disability Questionnaire),
spinal mobility and strength, and length of sick leave
were recorded at baseline and at 6- and 12-month
follow-up. The treatment group experienced signi-
cantly greater improvements in pain, disability and
mobility compared to the control group at 12-month
follow-up. The authors concluded that patients with
chronic or recurrent LBP may get relief of subjective
symptoms from back school. This study oers Level
I therapeutic evidence that for women with nonspe-
cic chronic LBP, a back school regimen of education
and exercise 6 times in 3 weeks and reviewed with 2
sessions at 6 months improves pain and disabili-
ty at 6 months compared to education booklet con-
trols. Though clinically meaningful improvements
were only seen for pain at 6 months; the intervention
group did not have improvements in sick leave or oth-
er medical treatment.
Jaromi et al
3
conducted a randomized controlled trial
to assess the eectiveness of a spine training program
(Back School) in nurses with chronic LBP. Partici-
pants randomized to the control group (n=55) re-
ceived passive physiotherapy once a week for 6 weeks.
The intervention group (n=56) received ergonomics
training and an educational Back School program.
Pain intensity (VAS) and body posture (Zebris biome-
chanical motion analysis) were recorded at baseline,
immediately after treatment and at 6- and 12-month
follow-up. The participants in the intervention group
had signicantly greater improvements in back pain
intensity at both follow-up points and signicant-
ly greater improvement in back posture. The authors
concluded that back school, including active physi-
cal therapy methods, can signicantly improve pain
intensity and body posture in nurses with LBP. This
study provides Level I therapeutic evidence that for
health care workers with nonspecic chronic LBP,
back school one time per week for 6 weeks is eec-
tive at decreasing pain at the end of treatment, 6-and
12-month follow-up. Passive PT in the same study
showed improvement in pain only at the end of treat-
ment. The results retained clinically meaningful lev-
els at 6 and 12 months for the treatment group as
compared to the control group.
In a randomized controlled trial, Morone et al
4
evaluated the eects of a multidisciplinary back
school program in patients with chronic LBP. Patients
with LBP for at least 3 months were randomized to
participate in 4 weeks of either a multidisciplinary
Back School program with education and exercises
(n=44) or a control group with medical assistance
(n=29). Quality of life (Short Form 36), disability
(Waddell Disability Index and Oswestry Disability
Index) and pain perceptions (VAS) were recorded at
baseline, after treatment completion and at 3- and
6-month follow-up. The Back School participants had
signicantly greater improvements in quality of life,
disability and pain perception. The authors concluded
that the Back School program investigated can be an
eective treatment in people with chronic nonspecic
LBP. This study provides Level I therapeutic evidence
that a back school program can improve quality of
life, disability and pain in nonspecic chronic LBP
compared to supportive medical care control.
There is insucient evidence that outcomes from a home-based exercise program are dierent
than no care.
Grade of Recommendation: I
Kuukkanen et al
5
conducted a randomized controlled
trial and 5-year follow-up to evaluate the long-term
eectiveness of a home exercise program in relieving
pain and improving function in patients with chron-
ic LBP. Participants with LBP for at least 3 years were
randomized into a home exercise group (n=29) or
control group with no exercise (n=28). LBP intensity
(Borg CR-10 scale) and function (Oswestry Disability
Index) were recorded at baseline and at 5-year fol-
low-up. LBP intensity and function improved in both
groups after 3 months; pain intensity remained sig-
nicantly lower in the home exercise group compared
to the control group at 5-year follow-up. The authors
concluded that supervised, controlled home exercises
can reduce LBP over 5 years. This study was down-
graded to Level II due its small sample and provides

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
103
therapeutic evidence that, in patients with low-level
baseline pain and disability, a home exercise program
provides pain improvements at 5-year follow-up.
There was no statistically signicant dierence in
function as compared with no treatment.
In a multicenter, randomized controlled trial, Shirado
et al
6
evaluated the eectiveness of home-based
exercise on pain, dysfunction and quality of life (QOL)
in Japanese individuals with chronic LBP. Participants
were randomized to a treatment group to complete
trunk muscle strengthening and stretching exercises
(n=103) or a control group to be treated with nonste-
roidal anti-inammatory drugs (n=98). Pain intensi-
ty (VAS) and dysfunction (Japan Low back pain Eval-
uation Questionnaire and Roland-Morris Disability
Questionnaire, RMDQ) were recorded at baseline, af-
ter treatment and at 6- and 12-month follow-up. Both
groups experienced improvement in pain and dys-
function; however, the exercise treatment group had
a statistically signicantly greater improvement in
function (95% condence interval for the dierence
of median of change ratio was from -0.33 to 0.00). The
authors concluded that the home-based exercise pro-
gram was more eective than nonsteroidal anti-in-
ammatory drugs in Japanese patients with chronic
LBP. This study oers Level I therapeutic evidence
that a home-based program with frequent physician
oversight resulted in signicantly better function and
similar pain outcomes at one year compared to non-
steroidal anti-inammatory drugs.
There is insucient evidence that a self-directed McKenzie exercise program for acute low
back pain results in dierent outcomes compared to usual medical care.
Grade of Recommendation: I
In a randomized controlled trial, Underwood et al
7
examined the eectiveness of teaching back exer-
cises based on the McKenzie approach in addition to
usual care for acute LBP. Patients with acute LBP for
less than 28 days were randomized to attend a group
back class (n=35) or receive conventional manage-
ment (n=40). Disability (Oswestry disability score)
and pain (VAS) were recorded at baseline and 4, 8, 12
and 52 weeks after study enrollment. There were no
dierences in the primary outcome measures for pain
or disability between groups. The authors conclud-
ed that the back class was not eective compared to
conventional care. The sample size was small and the
study was underpowered. This study provides Lev-
el II therapeutic evidence that there is no dierence
in pain or disability scores in patients with acute LBP
treated with a McKenzie exercise program compared
to usual care.
There is insucient evidence that a monitored pedometer-based exercise program with web-
based feedback provides any improvement over pedometer instruction alone.
Grade of Recommendation: I
Krein et al
8
conducted a randomized controlled trial
to determine whether a pedometer-based internet-
mediated program can reduce disability due to chronic
back pain. After trial enrollment, veterans with
nonspecic chronic back pain received a pedometer.
The intervention group (n=111) also received access to
a website with walking goals, feedback, motivational
messages and social support, while the control group
(n=118) did not. Disability (Roland Morris Disability
Questionnaire) was recorded at baseline and at 6-
and 12-month follow-up. The results showed slight
improvement in the intervention group. This was
statistically signicant at 6 months but not at one
year and in neither case was the dierence clinically
meaningful. This study provides Level I evidence that
a walking program resulted in improved function,
but the addition of internet based instruction and
motivation did not make a clinically meaningful
dierence in improvement.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
104
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends development of additional studies to corroborate
or dispute the existing evidence base. Opportunities exist for technology-
assisted exercise monitoring.
s
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
a. heat/cold
Note: 6-week follow-up rule does not apply
Q1 Recommendation:
It is suggested that the use of heat for acute low back pain results in short-term improve-
ments in pain.
Grade of Recommendation: B
Q1 Evidence Summary:
Dehghan and Farahbod
9
studied the ecacy of ther-
motherapy and cryotherapy added to pharmacologic
treatment in a randomized trial of patients with LBP.
Patients with LBP for less than one month received
500 mg naproxen twice daily and were randomized
to receive additional thermotherapy (hot water bag),
cryotherapy (ice), or naproxen only (n=29 in each
group) for one week. Pain (McGill Pain Questionnaire)
was recorded at baseline and on the 3rd, 8th and 15th
day after enrollment. Pain signicantly reduced in the
thermotherapy and cryotherapy groups by the sec-
ond visit; the thermotherapy group had signicantly
greater reductions than the cryotherapy group. The
authors concluded that thermotherapy and cryother-
apy are eective in the short-term to help reduce pain
in patients with acute LBP. This study provides Level
II evidence that addition of heat or cold to an NSAID
results in improved outcomes for pain compared to
NSAID alone for acute back patients at 3 weeks.
Kettenman
10
et al conducted a randomized controlled
trial to determine the ecacy of heat therapy in
patients with LBP. Patients with LBP for less than 3
months were randomized to the intervention group
with heat-wrap therapy for at least 4 hours a day for 4
consecutive days (n=15) or control group without heat
therapy (n=15). Both groups received nonsteroidal
anti-inammatory drugs (NSAIDs) to use as needed.
Subjective reports of sleep, well-being and pain
intensity (Pain, Sleep and Stress Questionnaire) were
recorded in a patient diary and the power of frequency
bands in the spontaneous electroencephalogram
(EEG) were recorded on days 2 and 4. The patients
in the heat therapy group reported signicantly
improved pain, less stressful everyday situations and
sleep. EEG-recordings in the heat group indicated
reduced arousal as evidenced by decreased power in
frequency bands. The authors concluded that heat
therapy resulted in improved pain, psychophysical
measures and objective measures that suggest acute
therapeutic relaxation. This study provides Level
II evidence that addition of heat therapy to NSAIDs
results in better pain scores than NSAIDs alone in
patients with acute back pain at 4-week follow-up.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
105
In a randomized controlled trial, Mayer
11
et al inves-
tigated the eect of combining continuous low-level
heat wrap therapy with directional preference-based
exercises on functional outcomes in patients with
acute LBP. Patients with LBP for less than 3 months
were randomized to receive 5 consecutive days of heat
wrap therapy alone (n=25), exercise alone (n=25),
heat wrap plus exercise (n=24) or a control group
booklet (n=26). Functional improvement (0-200 Rat-
ing of Perceived Capacity-Spine), disability (Roland
Morris Disability Questionnaire) and pain (6-point
verbal rating scale) were recorded at baseline and
day 2, 3 and 7 follow-ups. The combination of heat
wrap plus exercise resulted in signicantly greater
improvements in function, disability and pain relief
compared to each individual treatment or control. The
authors concluded that a combination of heat wrap
therapy with directional preference-based exercise is
more eective for the treatment of LBP compared to
either intervention alone or control treatment (book-
let). This study provides Level II evidence that heat
and exercise together result in better pain scores than
heat or exercise alone in patients with acute back pain
at 7-day follow-up.
Nadler et al
12
aimed to determine the ecacy of con-
tinuous low-level heat wrap therapy for the treatment
of acute nonspecic LBP in a randomized, parallel,
single-blind, placebo-controlled, multicenter clinical
trial. Patients with acute LBP for less than 3 months
were randomized to receive 3 consecutive days of heat
wrap therapy for 8 consecutive hours per day (n=95),
oral placebo (n=96), oral ibuprofen (n=12) or unheat-
ed back wrap (n=16) after being stratied by baseline
pain and gender. Pain (0-5-point verbal response
scale), muscle stiness (numeric rating scale), lateral
trunk exibility and disability (Roland-Morris Dis-
ability Questionnaire) were recorded over the course
of the 3-day treatment and 2 days of follow-up. The
patients in the heat wrap group had signicantly
greater pain relief, less muscle stiness, increased
exibility and reduced disability. The authors con-
cluded that continuous low-level heat wrap therapy
was eective for the treatment of acute, nonspecic
LBP. This study provides Level II evidence that heat
wrap results in better pain and disability scores as
compared to oral placebo in patients with acute back
pain. Heat wrap results in better pain scores than pla-
cebo heat wrap or NSAIDs.
Nadler et al
13
studied the safety and ecacy of eight
hours of continuous overnight low-level heat wrap
therapy for the treatment of LBP in a randomized,
single-blind, placebo-controlled, multicenter clin-
ical trial. Patients with LBP for less than 3 months
were randomized to receive 3 consecutive days of heat
wrap therapy (n=33), oral placebo (n=34), unheated
wrap (n=5) or oral ibuprofen (n=4) after being strati-
ed for baseline pain and gender. Morning pain relief
(0-5-point verbal response scale), daytime pain relief,
extended pain relief, muscle stiness, lateral trunk
exibility, and disability (Roland-Morris Disability
Questionnaire) were recorded on days 2 through 4.
All outcomes were signicantly improved in the heat
wrap group. The authors concluded that use of a heat
wrap overnight resulted in improved pain relief, less
muscle stiness and disability and improved exi-
bility sustained more than 48 hours after treatment
completion. This study provides Level II evidence that
overnight heat wrap results in better pain and disabil-
ity scores as compared to oral placebo in patients with
acute back pain.
Shakoor et al
14
investigated the eects of deep heat
therapy for the treatment of patients with chronic
LBP. Patients with LBP for more than 3 months
were randomized to receive nonsteroidal anti-
inammatory drugs (NSAIDs) and short-wave
diathermy (n=50) or NSAIDs and placebo short-
wave diathermy (n=52). Pain intensity, disability
and physical impairment were assessed using
the Lettinen Test Scores and VAS. Both groups
experienced improvements, with signicantly greater
improvements in the short wave diathermy group
compared to the placebo group at weeks 3 and 6. The
authors concluded that although both interventions
may be benecial for the treatment of LBP, treatment
with short wave diathermy added to NSAID use may
be more benecial than NSAID use alone. This study
provides Level II evidence that diathermy, exercise
and NSAIDs results in nonsignicant improvement in
VAS scores at 6 weeks relative to sham, exercise and
NSAIDs for treatment of chronic LBP.
Tao et al
15
conducted a randomized controlled trial
to study the eects of an education program with or
without heat wrap therapy in patients with acute LBP.
Patients with work-related LBP for less than 3 months
were randomized to receive back therapy education
and pain management (n=18) or back therapy edu-
cation, pain management and 3 consecutive days of
8-hour heat therapy (n=25). Pain intensity, pain relief
and disability were recorded at baseline, 4 times per
day for the 3-day treatment period and 4 and 14 days
after enrollment. The patients in the heat wrap group
had signicantly reduced pain intensity, increased
pain relief and improved disability scores during and
after treatment. In critique, the work group down-
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
106
graded this potential Level I study due to small sample
size. This study provides Level II evidence that heat
wrap signicantly reduced pain intensity, increased
pain relief and improved disability scores compared
to placebo.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
b. ultrasound
Q1 Recommendations:
It is suggested that ultrasound does not improve functional outcomes in patients with chronic
low back pain
Grade of Recommendation: B
There is conflicting evidence that ultrasound provides immediate pain relief in patients
with chronic low back pain.
Grade of Recommendation: I
Q1 Evidence Summary:
Durmus et al
16
investigated the eects of phonopho-
resis and ultrasound therapy in patients with chron-
ic LBP. Patients with LBP for at least 3 months were
randomized to the control group to receive exercise
only (n=20), ultrasound plus exercise (n=20), or pho-
nophoresis plus exercise (n=20), 3 days a week for
6 weeks. Pain (VAS), disability (Oswestry Disabili-
ty Questionnaire and pain disability index), walking
performance, depression (Beck Depression Inventory
scores), quality of life (SF-36), and muscle strength
and endurance were recorded before and after treat-
ment. All groups had improvements in outcomes. The
ultrasound and phonophoresis groups had statistical-
ly signicant greater improvements in pain, walking
performance and extensor muscle strength compared
to the control group, although not necessarily clini-
cally important improvement. The authors concluded
that both ultrasound and phonophoresis were eec-
tive treatments for patients with chronic LBP. Base-
line impairment was mild and sample size was small.
This study provides Level II therapeutic evidence that,
in patients with LBP, addition of ultrasound therapy
to exercise program provides questionable immediate
clinically-important reduction in pain, but not dis-
ability compared to exercise alone.
Ebadi et al
17
compared the eect of exercise plus con-
tinuous versus placebo ultrasound in patients with
chronic LBP in a randomized controlled trial. Patients
with nonspecic chronic LBP were randomized to
receive 10 treatment sessions, 3 times per week (ev-
ery other day) for 4 weeks of continuous ultrasound
updated 1/27/2021
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
107
(n=25) or placebo ultrasound (n=25). All participants
were instructed to perform a semi-supervised exer-
cise program consisting of stretching and strengthen-
ing exercises daily during the trial and for one month
after treatment. Functional disability (Functional
Rating Index) and global pain (VAS) were among the
outcomes measured upon enrollment, after treatment
and after one-month follow-up. Intention-to-treat
analysis found that both groups experienced im-
proved function and pain. The Time x Group inter-
actions for pain and function were not statistically
signicant. The main eect of Group on Functional
Rating Index was signicant. The authors concluded
that continuous ultrasound added to an exercise pro-
gram improved function, lumbar range of motion and
endurance time. This study provides Level I therapeu-
tic evidence that, in patients with LBP, there is no dif-
ference in pain and function between ultrasound plus
exercise compared to placebo ultrasound.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
c. Transcutaneous Electrical Nerve Stimulation (TENS)
Q1 Recommendation:
There is conicting evidence that transcutaneous electrical nerve stimulation (TENS) re-
sults in improvement in pain or function at short- to medium-term follow-up.
Grade of Recommendation: I
Q1 Evidence Summary:
Herman et al
18
conducted a randomized controlled
trial to evaluate the eectiveness of a standard ex-
ercise program with or without transcutaneous elec-
trical nerve stimulation (TENS) in patients with in-
dustry-related acute LBP. Patients with LBP from a
work-related injury with a duration of 3-10 weeks
were randomized to receive TENS (n=29) or placebo
stimulation (n=29) in addition to an exercise pro-
gram. Disability (Roland-Morris disability question-
naire) and pain (VAS) were recorded before and after
each treatment session and 4 weeks after enrollment.
Return to work was assessed at 5 weeks and 6 months
after enrollment. There were no signicant dier-
ences in outcomes between groups. The authors con-
cluded that there were no additional benets of TENS
when added to an exercise program. This study was
limited by signicant number of dropouts. This study
provides Level II evidence that there are no additional
benets from TENS when added to exercise treatment
for industrial-related LBP.
In a randomized controlled trial, Weiner et al
19
stud-
ied the eectiveness of percutaneous electrical nerve
stimulation (PENS) for the treatment of chronic LBP.
Patients with LBP for at least 3 months were random-
ized to receive twice-weekly PENS (n=17) or sham
PENS (n=17) in addition to physical therapy for 6
weeks. Pain intensity (McGill Pain Questionnaire) and
disability (Roland-Morris Back Pain Disability Ques-
tionnaire) were assessed at baseline, immediately af-
ter the 6-week treatment period and after 3 months.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
108
The patients who received PENS had statistically sig-
nicant reductions in pain intensity and disability at
both follow-up points, while the sham PENS group
did not. The study was limited by a small sample size.
This study provides Level II evidence that percutane-
ous electrical nerve stimulation added to an exercise
program resulted in signicant improvement in pain
and function at 3 months in geriatric patients with
chronic LBP.
Weiner et al
20
investigated the eectiveness of per-
cutaneous electrical nerve stimulation (PENS) for the
treatment of chronic LBP in a randomized controlled
trial. Patients with chronic LBP were randomized to
receive one of 4 treatments twice weekly for 6 weeks:
PENS (n=50), control-PENS (n=50), PENS plus gen-
eral conditioning and aerobic exercise (n=50), or
control-PENS plus general conditioning and aerobic
exercise (n=50). Control-PENS consisted of brief elec-
trical stimulation. Pain (McGill Pain Questionnaire)
and disability (Roland Morris Questionnaire) were
recorded at baseline, within one week of completing
the intervention and 6 months after completing the
intervention. All groups experienced improved pain
and disability at 6 months. The authors concluded
that the exact dose of electrical stimulation required
for analgesia cannot be determined. This study pro-
vides Level I evidence that PENS and a modied PENS
as the sham resulted in signicant improvements in
pain and function that did not improve with exercise
in a geriatric population with chronic LBP at 6 months
follow-up, although the addition of exercise did seem
to improve fear avoidance in particular.
Deyo et al
21
compared the eect of transcutaneous
electrical nerve stimulation (TENS), a program of
stretching exercises, or a combination of both for the
treatment of chronic LBP. Patients with LBP for at least
3 months were randomized to receive TENS (n=36),
sham TENS (n=36), TENS plus exercises (n=37), or
sham TENS plus exercises (n=36). Patients assigned
to TENS received instructions for home-use of at least
3 45-minute TENS sessions per day. Patients allocat-
ed to receive exercise received instructions for a daily
structured exercise sequence, adding one new exer-
cise each day. Functional status (modied Sickness
Impact Prole), self-reported activity level, pain (or-
dinal and VAS for pain, improvement and frequency)
pain scale) and physical measures were recorded at
baseline, after 2 and 4 weeks of therapy and 2-month
follow-up after completion of the trial. There were
no signicant dierences in outcomes in those who
received TENS and no interactive eect of TENS with
exercise. The authors concluded that TENS is no more
eective than placebo and adds no additional benet
to exercise alone. This study provides Level I thera-
peutic evidence that TENS does not provide improve-
ment in pain in patients with chronic LBP.
In a randomized double-blind crossover study,
Jarzem et al
22
compared transcutaneous electrical
nerve stimulation (TENS) to sham therapy in pa-
tients with chronic LBP. Patients with LBP for at least
3 months were randomized to receive TENS followed
by 2 treatments of sham TENS (n=25) or sham treat-
ment followed by 2 treatments of conventional TENS
(n=25). Pain tolerance (VAS) and physical measure-
ments were recorded upon enrollment and within an
hour after each treatment. There were signicant im-
provements in pain and physical measurements after
TENS compared to sham treatment. These measure-
ments were usually done within an hour of treatment.
Durable eects from treatment were not evaluated.
The authors concluded that TENS signicantly re-
duces pain and improves physical performance on the
studied measurements and should be considered for
short-term pain relief. This study oers Level I ther-
apeutic evidence that TENS provides immediate relief
in patients with chronic LBP.
Marchand et al
23
aimed to compare the eect of
transcutaneous electrical nerve stimulation (TENS),
placebo-TENS and no treatment in patients with
chronic LBP. Patients with LBP for more than 6 months
were allocated into one of 3 groups using a pseudo-
random assignment to control for sex, weight,
diagnosis and pain severity. Patients presented
to the clinic twice weekly for ten weeks to receive
TENS (n=14), placebo-TENS (n=12), or no treatment
(n=16). Pain intensity and unpleasantness (VAS) were
recorded before and after each treatment, as well as
every two hours at home during 3-day periods before
treatment, 1 week after treatment and 3 and 6 months
after treatment. Both TENS and placebo-TENS reduced
pain intensity and unpleasantness. TENS reduced
pain intensity signicantly more than placebo-TENS
immediately after treatment sessions and one week
after sessions, but not 3 months or 6 months after.
The authors concluded that TENS should be used as
a short-term treatment as part of a multidisciplinary
program for LBP. In critique of the methodology, this
potential Level I study was downgraded due to small
sample size. This study provides Level II therapeutic
evidence that TENS provides immediate term pain
relief in patients with chronic LBP.
Thompson et al
24
conducted a double-blind random-
ized controlled trial to study the eect of transcuta-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
109
neous spinal electroanalgesia (TSE) in patients with
LBP. Patients with LBP for greater than one year were
randomized to blindly receive a single 20-minute
treatment of TSE (n=29) or sham treatment (n=29).
Pain (VAS) was recorded every day of the week pri-
or to and following treatment as well as immediate-
ly before and after the treatment session. There were
no signicant dierences in pain scores between TSE
and sham after treatment. The authors concluded that
a single 20-minute treatment of TSE does not signi-
cantly impact pain in patients with LBP. This tech-
nique has some similarity to TENS, but can be run at
higher frequencies. This study is limited by the fact
that patients received only one dose. This study pro-
vides Level I therapeutic evidence that a single dose
of transcutaneous spinal electroanalgesia did result in
short-term pain relief when compared to placebo in
patients with chronic LBP.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends randomized clinical trials with long-term follow-up
looking at the benets of TENS compared to exercise/physical therapy, or the
addition of TENS to usual care of LBP.
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
d. Laser (Cutaneous stimulation for purpose of pain modulation)
Q1 Recommendations:
Laser acupuncture provides no short-term or medium-term benet over sham treatment for
patients with chronic low back pain.
Grade or Recommendation: A
Q1 Evidence Summary:
Glazov et al
25
studied the eect of laser acupuncture
for the treatment of chronic LBP in a double blind ran-
domized controlled trial. Patients with LBP for at least
three months were randomized to receive 5-10 treat-
ments (0.2 Joules/point) of laser acupuncture (n=50)
or sham control (n=50). All treatments were provided
by a single blinded investigator. Pain (VAS) and dis-
ability were recorded at baseline and at the end of the
6-week treatment period and pain was also evaluated
at 6 months follow-up after completion along with a
global assessment. Baseline pain (5.2 to 6.2) and dis-
ability scores (25 to 35) were moderate. Forty-ve out
of 50 patients in each group were evaluated at the -
nal follow-up. All participants experienced improve-
ments in outcomes, but there were no signicant dif-
ferences between groups. Improvements were modest
and not clinically important for functional scores. The
authors concluded that laser acupuncture does not
have a specic eect for the treatment of chronic LBP.
This study oers Level I therapeutic evidence that for
patients with chronic and moderately severe LBP, la-
ser acupuncture provides no benet over sham treat-
ment at short-term follow-up.
Glazov et al
26
later conducted another double-blind
controlled trial to investigate the eect of dierent
doses of laser acupuncture in reducing pain and dis-
ability in patients with chronic LBP. Patients with LBP
for at least 3 months were randomized to receive one
session per week for 8 weeks of high-dose (0.8 Joules/

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
110
point) laser acupuncture (n=48), low-dose (0.2 Joules/
point) laser acupuncture (n=48) or sham (0 Joules/
point) laser acupuncture (n=48). Treatment was pro-
vided by experienced general practitioners at six dif-
ferent general practices. Pain (Numerical Pain Rating
Scale) and disability (Oswestry Disability Inventory)
were recorded at baseline, one and 6 weeks into the
treatment period and 6 months post-treatment. Pain
was also recorded 12 months post treatment. Baseline
pain (means 4.9 to 5.3) and function (mean ODI 26 to
27) scores were moderate. Final analysis was done for
42, 40 and 45 patients respectively. All groups experi-
enced improvements in pain and disability, but there
were no dierences in outcomes between groups. Im-
provements in function were statistically signicant,
but not clinically important. This study oers Level I
therapeutic evidence that laser acupuncture provides
no short- or medium-term benet over sham treat-
ment in patients with moderately severe chronic LBP.
It is suggested that the combination of laser therapy (low-level or high-level) with exercise pro-
vides better short-term relief of pain than either exercise or laser therapy alone.
Grade of Recommendation: B
There is conicting evidence that the combination of laser therapy with exercise provides bet-
ter short-term improvement in function compared to exercise or laser therapy alone.
Grade of Recommendation: I
It is suggested that there is no short-term benet of laser therapy (low-level or high-level) when
compared with exercise alone.
Grade of Recommendation: B
Alayat et al
27
compared the eect of high-intensity la-
ser therapy (HILT) in patients with chronic LBP in a
randomized controlled trial. Patients in the male sec-
tion of a single rehabilitation department with LBP for
at least one year were randomized to receive twelve
15-minute sessions over 4 weeks of HILT plus a home
exercise program to be completed twice daily for 4
weeks (n=28), placebo laser plus exercise (n=24),
or HILT alone (n=20). Range of motion, pain (VAS),
functional disability (Roland Morris Disability Ques-
tionnaire and Modied Oswestry Disability Question-
naire) were recorded at baseline, after the 4-week
treatment period and at 12-week follow-up from the
start of treatment. All groups experienced improved
pain and disability, with no signicant dierences
in disability between groups. The HILT plus exercise
group experienced a clinically meaningful and statis-
tically signicantly greater decrease in pain compared
to the HILT only group. The authors concluded that
HILT combined with exercise is more eective than
HILT or exercise alone for the treatment of chron-
ic LBP. The study is limited by potential problems
with compliance with home exercise program and its
short duration of follow-up (8 weeks after conclusion
of treatment). This study oers Level I therapeutic
evidence that combination of high-intensity laser
therapy (HILT) plus exercise provides short-term in-
creased pain relief and function as compared to HILT
or home exercise alone. Home exercise alone provides
increased pain relief but no dierence in function over
HILT alone.
Djavid et al
28
conducted a randomized trial to investi-
gate the eect of low-level laser therapy for the treat-
ment of chronic LBP. Patients referred to a single oc-
cupational medicine department with LBP for at least
12 weeks were randomized to receive laser therapy
(n=20), laser therapy plus exercise (n=21) or placebo
laser therapy plus exercise (n=20). The exercise pro-
gram consisted of a home program of strengthening,
stretching, mobilizing and stabilization exercises. La-
ser therapy was performed twice weekly for 6 weeks.
Pain severity (VAS), range of motion and disability
(Oswestry Disability Index) was recorded at baseline,
immediately following the 6-week treatment peri-
od and 6 weeks after completion of the trial. Baseline
disability was moderate (ODI low 30s). There were 8
dropouts and no power analysis was done for sample
size. There were no signicant dierences in out-
comes between laser therapy alone and exercise plus
sham. At 12 weeks (6 weeks following conclusion of
treatment), the laser therapy plus exercise group had
signicantly improved pain, range of motion and dis-
ability compared to the exercise plus sham group. The
authors concluded that low-level laser therapy plus
exercise is more benecial than exercise plus sham.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
111
The study was downgraded for small eect size and
small sample size. This study provides Level II ther-
apeutic evidence that, at short-term follow-up, laser
plus exercise provided more pain relief and improved
disability compared to exercise plus sham laser. There
is no short-term benet of low-level laser alone as
compared to exercise plus sham laser.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends that current studies be supported by larger
sample sizes with longer follow-up.
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
e. Traction
Q1 Recommendation:
In patients with subacute or chronic low back pain, traction is not recommended to provide
clinically signicant improvements in pain or function.
Grade of Recommendation: A
Q1 Evidence Summary:
Borman, et al
29
conducted a randomized controlled
study to determine the ecacy of traction in the
treatment of LBP. Patients with LBP for at least 6
weeks were randomized to receive ten sessions of
standard physical therapy of heat, ultrasound and
active exercise (n=21) or standard physical therapy
with conventional lumbar traction (n=21). Disability
(Oswestry Disability Index) and pain (VAS) were
recorded at baseline, at the end of the intervention
and 3-month follow-up. Both groups experienced
improvement in pain and disability after treatment,
with no signicant dierences between groups.
The authors concluded that traction has no specic
eect on standard physical therapy. The work group
downgraded this potential Level I study during
critique of the methodology due to small sample
size and for 35% of participants receiving another
treatment during the 3-month follow-up period.
This study provides Level II evidence that there was
no ecacy in adding traction to a standard physical
therapy protocol of passive and active intervention.
Diab et al
30
investigated the eect of lumbar ex-
tension traction on pain, function and whole spine
sagittal balance in patients with chronic LBP. Pa-
tients with LBP for greater than three months were
randomly allocated to a control group (n=40) to re-
ceive stretching exercises and infrared radiation or a
traction group (n=40) to receive 3 sessions a week of
lumbar extension traction for 10 weeks in addition to
the same stretching exercises and infrared radiation.
Pain (Back Pain Rating Scale), disability (Oswestry
Disability Index) and radiological spine sagittal bal-
ance parameters were recorded at baseline, after the
10-week treatment period and 6-month follow-up.
Their primary measure was radiographic outcomes.
There were signicant dierences in pain and dis-
ability at 6-month follow-up, but not immediately
after the 10-week treatment period. However, the ac-
tual change in lordosis was 4° and sacral slope 1° with
substantial overlap in standard deviations. Mean ODI
scores (32 and 31) and pain scores (6 and 5.5) revealed
moderate severity. There were improvements in both
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
112
groups and while statistically dierent, the dier-
ences do not appear to be clinically important. The
authors concluded that the addition of lumbar ex-
tension to stretching exercises and infrared radiation
resulted in improvements in spine sagittal balance
parameters, pain and disability. This study provides
Level I evidence that extension traction added to an
exercise program and infrared heat to treat patients
with chronic LBP with moderate pain and disability
results in statistically better but clinically insigni-
cant improvement in pain and disability at 6-month
follow-up.
Schimmel et al
31
conducted a randomized controlled
trial to study the eect of adding Intervertebral Dif-
ferential Dynamics (IDD) therapy to standard grad-
ed activity program for the treatment of chronic LBP.
Patients with LBP for more than 3 months were ran-
domized to receive sham therapy (n=29) or IDD Ther-
apy which included intermittent traction sessions in
the AccuSPINA device (n=31). During the rst 6 weeks,
all participants received 20 sessions of their assigned
sham or IDD Therapy. A standard graded activity pro-
gram was added after two weeks for both groups and
consisted of one-hour sessions twice weekly for 12
weeks. Pain (100-mm VAS), disability (Oswestry Dis-
ability Index), quality of life (SF-36) and fear of move-
ment (Tampa Scale for Kinesiophobia) were recorded
upon enrollment and 2, 6 and 14 weeks after initiation
of the treatment. Improvements in outcomes were
seen in both groups. The authors concluded that the
addition of intermittent, mechanical traction added
to standard graded activity is not eective. This study
provides Level I evidence that the addition of inter-
mittent traction with the AccuSPINA device versus
sham when coupled with graded activity does not re-
sult in improved pain or disability scores in patients
with chronic LBP at short-term follow-up.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
f. Dry needling
Q1 Recommendation:
There is insucient evidence for or against the use of dry needling as a treatment option for
patients with chronic low back pain.
Grade of Recommendation: I
Q1 Evidence Summary:
Gunn et al
32
conducted a clinical trial to evaluate the
eect of dry needling in patients with chronic LBP.
Patients (men only) with LBP for at least 12 weeks
were randomized to receive standard therapy plus dry
needling 1-2 times per week at muscle motor points
(n=29) or standard therapy alone (n=27). Standard
therapy included physiotherapy, exercise and occu-
pational therapy. Pain and work status were classied
as 0 (no improvement), + (some improvement), ++
(good improvement) or +++ (total improvement). The
patient’s status was recorded at baseline, at time of
discharge, 12 weeks post-discharge and again when
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
113
contacted at the time of writing the report (12-61
weeks, average 27.3 weeks). The group that received
dry needling in addition to standard therapy signi-
cantly improved compared to standard therapy alone
at time of discharge and both follow-up points. The
authors concluded that the addition of dry needling
to standard care seems justied for the treatment of
chronic LBP in patients with myofascial pain. In cri-
tique, study outcome measures are poorly dened and
not validated. Sample size was small without pow-
er analysis. This was a mix of subacute patients with
symptoms present for as little as 12 weeks combined
with patients that had symptoms for years, with a
mean of 27 weeks. Lastly the randomization was con-
strained to randomization in blocks of 2. Due to aws
in randomization methodology, the study started as a
Level II design and was downgraded to Level III. This
study oers Level III therapeutic evidence that, in pa-
tients with LBP, addition of dry needling to a compre-
hensive exercise program results in greater improve-
ment than exercise alone.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends undertaking high quality studies evaluating eec-
tiveness of dry needling.
QQ
PM&R Questions 1 & 2.
ii. Physical agents (eg, heat, cold, ultrasound, electrical stimulation, laser, dry
needling, traction, TENS)
g. Electrical Stimulation
Q1 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this ques-
tion.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this ques-
tion.
Q1&2 Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
114
QQ
PM&R Questions 1 & 2.
iii. Acupuncture
Q1 Recommendations (sham acupuncture):
In patients with low back pain, there is conicting evidence that acupuncture provides improve-
ments in pain and function as compared to sham acupuncture.
Grade of Recommendation: I
Q1 Evidence Summary (sham acupuncture):
Carlsson et al
33
conducted a blinded placebo-controlled
study to investigate the eect of needle acupuncture
on long-term relief of chronic LBP. Patients with
LBP for at least 6 months were randomized to receive
needle acupuncture (n=34) or placebo stimulation
using a disconnected transcutaneous electrical nerve
stimulation stimulator (n=16) once weekly for 8 weeks
plus 2 additional treatments over a 6-month follow-
up. Pain intensity (VAS), analgesic intake, quality of
sleep and activity level were recorded in a diary. An
independent blinded observer completed a global
assessment at 1, 3 and 6 months after treatment. A
signicantly greater proportion of the patients in the
acupuncture group had improved global assessments
at 1- and 6-month follow-up. There were signicant
improvements in mean weekly pain scores, return
to work, quality of sleep and analgesic intake in the
acupuncture group compared to the placebo group.
The authors concluded that needle acupuncture
provides long-term pain-relieving eect in some
patients with chronic nociceptive LBP. Due to the small
sample size of the study, the level of evidence was
downgraded. This potential Level I study oers Level
II therapeutic evidence that, in patients with chronic
LBP, acupuncture was associated with improvement
in return to work, quality of sleep and analgesic
intake at 6 months compared to placebo; acupuncture
was associated with statistically signicant, but
not clinically meaningful, improvement in pain at 6
months compared to placebo.
Kerr et al
34
investigated the eect of acupuncture
for the treatment of chronic LBP in a randomized
controlled trial. Patients with LBP for more than 6
months were randomized to receive acupuncture
therapy (n=30) or placebo transcutaneous electrical
nerve stimulation (n=30) for 6 weeks. Pain (McGill
Pain Questionnaire and VAS), quality of life (SF-36)
and range of motion were recorded at baseline, after
completion of the 6-week treatment and 6 months
after treatment. Both groups had improvements in all
outcomes (with the exception of McGill Pain Ques-
tionnaire in the placebo group). The authors conclud-
ed that there were no signicant dierences between
acupuncture therapy and placebo. In critique, less
than 80% of patients completed follow-up and there
was concern for Type II error due to small sample size.
Due to these reasons, the work group downgraded the
level of evidence for this study. This potential Level I
study provides Level II therapeutic evidence that, in
patients with chronic LBP, there were no dierences
in pain and function between acupuncture and place-
bo at 6 months.
Vas et al
35
conducted a multicenter randomized
controlled trial to investigate the ecacy of
acupuncture in patients with acute nonspecic
LBP. Patients with their rst episode of LBP, with
a duration of less than 2 weeks, were randomized
into one of 4 groups: conventional treatment alone
(n=70), conventional treatment plus acupuncture
(n=68), conventional treatment plus sham
acupuncture (n=68), or conventional treatment
plus placebo acupuncture (n=69). Conventional
treatment consisted of posture recommendations,
analgesics, nonsteroidal anti-inammatory drugs
and myorelaxant drugs). Each acupuncture group
received 5 20-minute sessions over a 2-week period.
Disability (Roland Morris Disability Questionnaire),
pain intensity (VAS), occupational disability, LBP
persistence, appearance of LBP and patient-perceived
improvement were recorded at baseline and at 3, 12 and
48 weeks. All 3 acupuncture groups (true acupuncture,
sham and placebo) improved signicantly more
than conventional treatment alone; but there were
no signicant dierences between the acupuncture
groups. The authors concluded that acupuncture is not

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
115
better than sham or placebo acupuncture. This study
oers Level I therapeutic evidence that, in patients
with acute LBP, acupuncture, sham acupuncture,
placebo acupuncture and conventional treatment
provide similar functional outcomes at 48 weeks
follow-up.
Cho et al
36
conducted a randomized sham-controlled
clinical trial to study the eect of individualized acu-
puncture for the treatment of chronic LBP. Patients
with LBP for at least three months were randomized
to receive twice-weekly sessions of individualized
acupuncture (n=65) or sham acupuncture (n=65). LBP
bothersomeness (VAS), pain intensity (VAS), disabil-
ity (Oswestry Disability Index), general health status
(Short-Form-36) and depression (Beck Depression
Inventory) were recorded at baseline and at 3- and
6-month follow-ups. Disability, depression and gen-
eral health status improved in both groups with no
dierences between groups. LBP intensity and both-
ersomeness improved signicantly more in the indi-
vidualized acupuncture group than the sham group.
The authors concluded that acupuncture is more ef-
fective in reducing LBP bothersomeness and inten-
sity compared to sham acupuncture in patients with
chronic LBP. This study provides Level I therapeutic
evidence that, in patients with LBP, acupuncture is
more eective than sham acupuncture for pain relief
at 6 months with no dierence for function or depres-
sion.
Cherkin et al
37
compared the eectiveness of individ-
ualized acupuncture, standardized acupuncture, sim-
ulated acupuncture and usual care for the treatment
of chronic LBP. Patients with LBP for at least 3 months
were randomized to receive 10 15-20 minute sessions
over 7 weeks of individualized acupuncture with no
limits on number of needs, depth of insertion or nee-
dle manipulation (n=157), standardized acupuncture
(n=158), simulated acupuncture using a toothpick in a
needle guide tube (n=162), or usual care per the discre-
tion of their physician (n=161). Back-related dysfunc-
tion (Roland-Morris Disability Questionnaire) and
symptom bothersomeness were recorded at baseline
and after 8, 26 and 52 weeks. All 3 acupuncture groups
had signicantly greater improvement in mean dys-
function scores at 8 weeks compared to usual care.
The authors concluded that individualizing acupunc-
ture does not aect therapeutic benets. This study
provides Level I therapeutic evidence that, in patients
with LBP, acupuncture and sham acupuncture provide
statistically signicant, but not clinically meaningful,
improvement in function.
In a randomized controlled trial, Haake et al
38
studied
the eect of acupuncture for reducing chronic
LBP compared to conventional therapy or sham
acupuncture. Patients with LBP for at least six months
were randomized to receive 10 30-minute sessions
of verum acupuncture (n=387), sham acupuncture
avoiding all verum points or medians (n=387) or
guideline-based conventional therapy including
exercise or physiotherapy sessions with a physician
or physiotherapist (n=388). Pain (Von Kor Chronic
Pain Grade Scale) and functional status (Hanover
Functional Ability Questionnaire) were assessed at
baseline and 1.5, 3 and 6 months after start of treatment.
Both the verum and sham acupuncture groups had
greater improvements than the conventional therapy,
with no dierences between verum and sham
acupuncture. The authors concluded that verum and
sham acupuncture improved LBP for at least 6 months
with greater eectiveness than conventional therapy.
This study provides Level I therapeutic evidence
that, in patients with LBP, acupuncture and sham
acupuncture result in improved pain and function at
6 months compared to guideline-based conventional
therapy (physical therapy).

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
116
Q1 Recommendations (usual care):
In patients with chronic low back pain, addition of acupuncture to usual care is recommended
for short-term improvement of pain and function compared to usual care alone.
Grade of Recommendation: A
Q1 Evidence Summary (usual care):
In a randomized controlled trial, Haake et al
38
stud-
ied the eect of acupuncture for reducing chronic LBP
compared to conventional therapy or sham acupunc-
ture. Patients with LBP for at least 6 months were ran-
domized to receive 10 30-minute sessions of verum
acupuncture (n=387), sham acupuncture avoiding all
verum points or medians (n=387), or guideline-based
conventional therapy including exercise or physio-
therapy sessions with a physician or physiotherapist
(n=388). Pain (Von Kor Chronic Pain Grade Scale)
and functional status (Hanover Functional Ability
Questionnaire) were assessed at baseline and 1.5, 3
and 6 months after start of treatment. Both the verum
and sham acupuncture groups had greater improve-
ments than the conventional therapy, with no dif-
ferences between verum and sham acupuncture. The
authors concluded that verum and sham acupuncture
improved LBP for at least 6 months with greater ef-
fectiveness than conventional therapy. This study
provides Level I therapeutic evidence that, in patients
with LBP, acupuncture and sham acupuncture result
in improved pain and function at 6 months compared
to guideline-based conventional therapy (physical
therapy).
Witt et al
39
compared the eectiveness and cost of
acupuncture in addition to routine care for chronic LBP
in a randomized controlled trial and nonrandomized
cohort. Patients with LBP for more than 6 months
were randomized to receive up to 15 sessions of
acupuncture in addition to routine medical care
(n=1,549) or routine medical care alone (n=1,544).
Patients who did not agree to participate in the RCT
were enrolled in a nonrandomized acupuncture group
(n=8,537). Back function (Hannover Functional
Ability Questionnaire), pain (Low Back Pain Rating
Scale) and quality of life (SF-36) were assessed at
baseline and after 3 and 6 months. Back function,
back pain and quality of life improved signicantly
more in the acupuncture group compared to the
control group at 3-month follow-up. The cost-
eectiveness analysis revealed that acupuncture was
relatively cost-eective. The authors concluded that
acupuncture added to routine care was associated
with clinical improvements. This study provides Level
I therapeutic evidence that, at 3 months, acupuncture
shows improvement in pain and function compared to
routine care (routine care not dened); these results
were not sustained at 6 months.
Yeung et al
40
conducted a randomized controlled trial
to investigate the eect of electro-acupuncture added
to exercise for the treatment of chronic LBP. Patients
with LBP for at least 6 months were randomized to
receive one hour per week of a standard group exercise
program (n=26) or the same exercise program plus 12
sessions of electro-acupuncture (n=26) for 4 weeks.
Pain (Numerical Rating Scale), disability (Aberdeen
LBP scale), range of motions and isokinetic strength
were assessed at baseline, immediately after treatment
and at one- and 3-month follow-up. The patients
who received the additional electro-acupuncture
had signicantly better pain and disability scores
compared to those who had exercise only. The authors
concluded that the addition of electro-acupuncture to
exercise might be an eective treatment for chronic
LBP. This study provides Level I therapeutic evidence
that, at 3 months, in patients with LBP, electro-
acupuncture added to an exercise program improves
pain and function better than an exercise program
alone.
Yun et al
41
aimed to determine if Hegu acupuncture
is more eective than standard acupuncture and if
both forms of acupuncture are more eective than
medical care alone for the treatment of chronic LBP.
Patients with back pain for at least three months
were randomized to receive 18 treatments of Hegu
acupuncture (n=64), standard acupuncture (n=60), or
usual care only (n=63) over 7 weeks. Hegu acupuncture
involved inserting and drawing back the needle in
dierent directions before inserting straight to the de
qi point compared to standard acupuncture in which
the acupuncturist inserted the needle straight to the
de qi point. The participants in the usual care did not
receive any treatment but were allowed to continue
any care recommended by their own physicians.
Back-related dysfunction (Roland-Morris Disability
Questionnaire) and pain (VAS) were recorded at
baseline and at 8 and 48 weeks after enrollment. The

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
117
Hegu acupuncture group had greater improvements
in dysfunction and pain scores compared to the
standard acupuncture group at both follow-up points.
Both acupuncture groups had greater improvements
in dysfunction and pain compared to the usual care
group at both follow-up points. This study provides
Level I therapeutic evidence that, at 48 weeks, Hegu
acupuncture is associated with statistically signicant
improvements in pain and disability compared
to standard acupuncture and provide statistically
signicant improvements in pain and disability
compared to usual care. These improvements are
small and may not be clinically signicant.
Q1 Recommendation (acupuncture technique):
There is insucient evidence to draw conclusions regarding the comparative eectiveness of
acupuncture techniques.
Grade of Recommendation: I
Q1 Evidence Summary (acupuncture technique):
Ceccherelli et al
42
compared the eect of supercial
and in-depth insertion of acupuncture needs in
treatment of chronic LBP in a randomized double-
blind study. Patients with lumbar myofascial pain for
more than three months were randomized to receive
8 sessions of acupuncture using either a 2 mm depth
(n=21) or deep placement into the muscular tissue
(n=21). Pain intensity (McGill Pain Questionnaire)
was recorded at baseline, after the 6-week treatment
period and at 3-month follow-up. The patients who
received deep acupuncture had signicantly greater
pain reduction compared to the supercial insertion at
3-month follow-up. The authors concluded that deep
stimulation has better pain relief eects compared
to supercial stimulation. This study oers Level I
therapeutic evidence that, in patients with LBP, deep
acupuncture provided more pain relief at 3 months
compared to supercial acupuncture.
Pach et al
43
conducted a randomized controlled trial
to compare the eectiveness of standardized and in-
dividualized acupuncture for the treatment of chronic
LBP. Patients with LBP for at least 3 months were ran-
domized to receive 10-15 sessions of standardized acu-
puncture (n=78) or individualized acupuncture based
on diagnosis (n=72) over 8 weeks. Pain (VAS) was re-
corded in a daily diary. Both groups had improvement
in pain severity over 8 weeks, with no dierences in
the area under the curve for pain severity from base-
line to end of week 8. The authors concluded that in-
dividualized acupuncture was not superior to standard
acupuncture. This study oers Level I therapeutic ev-
idence that, in patients with LBP, outcomes for stan-
dard and individualized acupuncture are equivalent.
This study oers Level IV therapeutic evidence that
acupuncture results in signicant pain relief.
Shin et al
44
compared the eect of bee venom acu-
puncture and sham control for the treatment of
chronic LBP. Patients with LBP for at least 3 months
were randomized to receive twice-weekly treatments
of bee venom acupuncture (n=30) or sham control of
normal saline injection (n=30) for four weeks. Pain
intensity (VAS), disability (Oswestry Disability Ques-
tionnaire) and quality of life (SF-36) were record-
ed at baseline, at each treatment session and 4- and
12-month follow-up after completion of treatment.
Both groups had signicant improvement in pain in-
tensity, disability and quality of life at all follow-up
points with no signicant dierences between groups
in disability or quality of life. At the 7th and 8th treat-
ment sessions, the participants in the bee venom acu-
puncture group had signicantly greater pain relief
compared to the control group, but there were no dif-
ferences at 4- or 12-month follow-up. Adverse events
such as pruritus and other skin reactions occurred but
resolved without medical intervention. The authors
concluded that bee venom acupuncture is eective in
treating chronic LBP. This study provides Level I ther-
apeutic evidence that, in patients with LBP, bee ven-
om acupuncture and saline acupuncture are equally
eective in pain relief similar at 3 months’ follow-up.
Yun et al
41
aimed to determine is Hegu acupuncture is
more eective than standard acupuncture and if both
forms of acupuncture are more eective than medical
care alone for the treatment of chronic LBP. Patients
with back pain for at least three months were random-
ized to receive 18 treatments of Hegu acupuncture,
standard acupuncture, or usual care only over sev-
en weeks. Hegu acupuncture involved inserting and
drawing back the needle in dierent directions before
inserting straight to the de qi point compared to stan-
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
118
dard acupuncture in which the acupuncturist inserted
the needle straight to the de qi point. The participants
in the usual care did not receive any treatment but
were allowed to continue any care recommended by
their own physicians. Back-related dysfunction (Ro-
land-Morris Disability Questionnaire) and pain (VAS)
were recorded at baseline and at 8 and 48 weeks after
enrollment. The Hegu acupuncture group had greater
improvements in dysfunction and pain scores com-
pared to the standard acupuncture group at both fol-
low-up points. Both acupuncture groups had greater
improvements in dysfunction and pain compared to
the usual care group at both follow-up points. This
study provides Level I therapeutic evidence that, at 48
weeks, Hegu acupuncture is associated with statisti-
cally signicant, but not clinically meaningful, im-
provements in pain and disability compared to stan-
dard acupuncture; both types of acupuncture provide
statistically signicant, but not clinically meaning-
ful improvements in pain and disability compared to
usual care.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group does not recommend the undertaking of additional studies. It
appears that additional high-level studies will not change recommendations.
QQ
PM&R Questions 1 & 2.
iv. Bracing
Lumbosacral brace
Sacroiliac brace
Q1 Recommendation:
There is conicting evidence that bracing results in improvements in pain and function in pa-
tients with subacute low back pain
Grade of Recommendation: I
Q1 Evidence Summary:
Calmels et al
45
investigated the eects of an elastic
lumbar belt for the treatment of LBP in a multicenter,
randomized controlled trial. Patients with a current
LBP episode lasting 1-3 months were randomly as-
signed to receive a lumbar belt (n=102) or to a con-
trol group instructed not to wear any type of lumbar
belt (n=95). Participants who received the lumbar
belt were instructed to wear the belt every day for
the duration of the 3-month trial. Pain (VAS), func-
tional capacity (EIFEL scale, French version of the
Roland-Morris scale) and number of days of medical
consumption were recorded at baseline and on day
30, 60 and 90. The lumbar belt group had statistically
signicant improvements in pain, functional capacity
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
119
and medication consumption. The authors conclud-
ed that the addition of a lumbar belt can improve the
functional status, pain level and pharmacologic con-
sumption in patients with subacute LBP. Although the
dierences between groups were statistically signif-
icant, in critique, the work group deemed the results
clinically insignicant. This study oers Level I ther-
apeutic evidence that, in patients with subacute LBP,
there does not appear to be a clinically signicant
dierence in pain and function at 3 months between
wearing a nonrigid lumbar corset and medication.
Oleske et al
46
conducted a multicenter randomized
clinical trial to compare the eectiveness of a back
support lumbar corset plus education versus education
alone in patients with LBP. Patients with work-
related LBP were randomized to receive education
plus the back support corset (n=222) or education
alone (n=211). LBP frequency and bothersomeness
(numerical rating scale), disability (Oswestry Back
Pain Disability Questionnaire), physical health (SF-
12), mental health and work time were recorded
at follow-up and after 1, 2, 6 and 12 months. Both
groups experienced improvements in pain, disability,
neurogenic symptoms and physical health over 12
months. The back support plus education group had
a lower likelihood of LBP recurrence, but otherwise
there were no dierences in outcomes between
groups. The authors concluded that the back support
may prevent recurrence of work-related LBP when
added to education. This study provides Level I
therapeutic evidence that, in patients with subacute
LBP, the addition of lumbar corset to education does
not result in decreased pain and disability compared
to education alone at one year.
Doran and Newell
47
investigated the eectiveness of
four dierent treatment options in patients with LBP.
Participants were randomly assigned to receive at
least 2 sessions of manipulation per week (n=98), at
least 2 sessions of physiotherapy per week (n=104),
corset applied on the rst day of the trial (n=93), or
2 paracetamol tablets every 4 hours (n=100). Patients
completed questionnaires to report whether their
pain was worse, unchanged, improved or completely
relieved at the end of the 3-week trial, 3 weeks after
the conclusion of the trial, 3 months after enrollment
and one year after enrollment. The authors conclud-
ed that there were no signicant dierences between
any of the 4 studied interventions. In critique, no val-
idated outcomes were included in this study and out-
come data is limited. Due to these reasons, the work
group downgraded this study. This potential Level I
study provides Level II therapeutic evidence that, in
patients with acute LBP, SMT, physiotherapy, medi-
cation and corset resulted in similar improvements up
to 3 months.
Q2 Recommendation:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends comparative eectiveness studies using bracing in
patients with chronic LBP.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
120
QQ
PM&R Questions 1 & 2.
v. Spinal manipulative therapy (SMT)
Work Group Narrative: The majority of SMT literature involves the centralization phenomenon which is
commonly seen in patients with leg pain. This review examined only evidence in the sub-set of patients
without radiating pain. Additional literature discussing clinical benets from SMT for the treatment of
LBP including radiating pain were not included in our systematic review. Therefore, a denitive state-
ment of SMT in all patients with LBP cannot be made.
Q1 Recommendations:
For patients with acute or chronic low back pain, spinal manipulative therapy (SMT) is an option
to improve pain and function.
Grade of Recommendation: C
For patients with acute low back pain, spinal manipulative therapy (SMT) results in similar out-
comes to no treatment, medication or modalities. Periodically, short-term improvement is sta-
tistically better, but clinical signicance is uncertain.
Grade of Recommendation: A
For patients with chronic low back pain, there is conicting evidence that outcomes for spinal
manipulative therapy (SMT) are clinically dierent than no treatment, medication or modalities.
Grade of Recommendation: I
Q1 Evidence Summary:
In a randomized control trial, Dougherty et al
48
evalu-
ated the eectiveness of spinal manipulative therapy
(SMT) in older veterans with chronic LBP compared to
a sham intervention. Veterans at least 65 years of age
with LBP for at least 3 months were randomly allo-
cated to groups to receive SMT (n=69) or sham inter-
vention (n=67) twice weekly for 4 weeks. Pain (VAS,
SF-36 pain subscale), disability (Oswestry Disability
Index) and physical function (SF-36 subscale, Timed
Up and Go) were recorded at baseline and after 5 and
12 weeks. Both groups experienced improvements in
pain and disability at 5 and 12 weeks. Disability im-
proved signicantly more in the SMT group compared
to the control group. The authors concluded that SMT
resulted in greater improvement in disability but not
pain at 12 weeks. This study oers Level I therapeu-
tic evidence that, in patients with chronic LBP, there
were similar improvements in pain when comparing
SMT to sham. There was statistically signicant im-
provement in function in the SMT group. However, it
is uncertain as to whether these functional improve-
ments were clinically signicant.
Haas et al
49
conducted a randomized controlled trial
in patients with chronic LBP to identify the dose-re-
sponse relationship between visits to a chiroprac-
tor for SMT and treatment outcomes and to compare
treatment outcomes of manipulation versus light
massage. Four hundred patients with non-specic
LBP for at least 3 months were prescribed 18 sessions
with a chiropractor (three times a week for six weeks).
Participants were randomized to receive either 0, 6,
12 or 18 sessions of SMT (n=100 in each group). The
chiropractor provided light massage for the remain-
ing sessions that did not include SMT. Pain and dis-
ability (modied Von Kor pain and disability scales)
were recorded at baseline and throughout a 52-week
follow-up period. Pain and disability improved in all

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
121
groups and was sustained for 52 weeks. The greatest
treatment eects were found from 12 sessions of SMT.
The authors concluded that 12 SMT visits had mod-
est eects on chronic LBP outcomes compared to the
other dose levels, but the dierence was not well dis-
tinguished. This study oers Level I therapeutic evi-
dence that, in patients with LBP, spinal manipulative
therapy is associated with statistically signicant im-
provement in pain compared to light massage. How-
ever, it is uncertain whether this was clinically sig-
nicant. Regarding frequency, this study oers Level
I therapeutic evidence that 12-18 visits of SMT were
statistically better than 6 visits at 12-week follow-up;
no dierence between doses at one-year follow-up.
Again, the dierences were small and the clinical sig-
nicance was uncertain.
In a placebo controlled randomized trial, Hancock et
al
50
evaluated the eectiveness of nonsteroidal anti-
inammatory drugs (NSAIDS), spinal manipulative
therapy (SMT), or combination of NSAIDs and SMT
for the treatment of acute LBP. Patients presenting to
their general practitioner with LBP were randomized
into one of 4 groups: diclofenac 50 mg twice daily and
placebo SMT (n=60); SMT and placebo drug (n=60);
diclofenac 50 mg twice daily and SMT (n=60); or
double placebo (n=60) until recovery or up to 4 weeks.
The primary outcome of “days to recovery” was
recorded as the rst pain-free day and the rst of 7
consecutive days with a pain score of 0 or 1. There were
no signicant dierences in days to recovery between
groups. The authors concluded that the addition of
diclofenac or spinal manipulative therapy do not
improve recovery in patients with acute LBP already
receiving rst-line care. This study oers Level I
therapeutic evidence that, in patients with acute LBP,
there was no dierence in resolution of pain between
spinal manipulative therapy, NSAIDS and placebo.
Hoiriis et al
51
compared chiropractic adjustments
and muscle relaxants to sham treatment and place-
bo in a randomized controlled trial of patients with
subacute LBP. Patients with LBP for 2-6 weeks were
randomly allocated into one of 3 groups: chiropractic
adjustments with placebo medicine (n=50), muscle
relaxants with sham adjustments (n=53) or place-
bo medicine with sham adjustments (n=53). Primary
outcomes of pain (VAS), disability (Oswestry Disabili-
ty Questionnaire) and depression (Modied Zung De-
pression Scale) were assessed at baseline, 2 weeks and
4 weeks. Patients at baseline had mild pain and dis-
ability. The chiropractic group had greater pain im-
provement compared to the control group and greater
improvement in a secondary outcome of Global Im-
pression of Severity compared to all groups. There
were no signicant dierences between groups in
other outcomes. The authors concluded that chiro-
practic treatment was more benecial than placebo
in reducing pain. This study oers Level I therapeu-
tic evidence that, in patients with acute LBP and mild
baseline disability, there was statistically better im-
provement in pain with SMT, while improvements in
function were otherwise similar relative to medica-
tion and sham groups at 4 weeks. However, the dif-
ferences across groups were small and it is uncertain
whether these improvements in pain were clinically
signicant.
Juni et al
52
conducted a randomized controlled trial
in patients with subacute LBP to evaluate the ecacy
of SMT as an addition to standard care compared to
standard care alone. Patients with acute LBP for less
than four weeks were randomized to receive standard
care of general advice and paracetamol, diclofenac or
dihydrocodeine as required (n=52) or standard care
plus SMT (n=52). Pain (11-point box scale) and anal-
gesic use were recorded throughout the 2-week trial
and at 6-month follow-up. There were no signicant
dierences in pain or analgesic use between groups.
The authors concluded that SMT is not likely to reduce
pain in patients with acute LBP. This study provides
Level I therapeutic evidence that, in patients with
acute LBP, there were no dierences in pain and func-
tion between SMT and medication at up to 6 months
follow-up.
Schneider et al
53
conducted a randomized controlled
trial in patients with acute or subacute LBP to
evaluate manual thrust manipulation compared to
mechanical-assisted manipulation and manipulation
compared to usual medical care. Patients with LBP
of less than 12 weeks duration were randomized
into one of three groups for 4 weeks: twice-weekly
manual-thrust manipulation (n=37), twice-weekly
mechanical-assisted manipulation (n=35), or 3 visits
of usual medical care (n=35). Disability (Oswestry LBP
Disability Index) and pain (numeric pain rating scale)
were recorded at baseline, after 4 weeks of treatment
and at 3- and 6-month follow-up. The participants
who received manual-thrust manipulation had
signicantly greater improvements in disability and
pain compared to the machine-assisted manipulation
and usual medical care at 4 weeks. There was a
greater proportion of responders (30-50% reduction
in Oswestry LBP Disability Index score) in the
manual-thrust manipulation compared to machine-
assisted manipulation or usual medical care. The
authors concluded that manual-thrust manipulation

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
122
provides greater short-term improvements in pain
and disability compared to usual medical care or
machine-assisted manipulation. This study oers
Level I therapeutic evidence that, in patients with
acute LBP, manual based SMT had signicantly
greater improvement in pain and function compared
to mechanical assisted manipulation or usual care at
4 weeks follow-up, but not at 3 months.
In patients with chronic LBP, Senna et al
54
conduct-
ed a randomized controlled trial to compare SMT to
sham SMT. Patients with LBP for at least 6 months
were randomized to one of 3 groups: 12 treatments of
sham SMT over one month (n=40), 12 treatments of
SMT over one-month followed by no treatment for
9 months (n=27) or 12 treatments of SMT over one
month with “maintenance spinal manipulation” ev-
ery 2 weeks for the following 9 months (n=26). Pain
(VAS), disability (Oswestry disability questionnaire),
generic health status (SF-36) and back-specic pa-
tient satisfaction were recorded at baseline and after
one, 4, 7 and 10 months. After one month, both of the
SMT groups had signicantly lower pain and disabil-
ity compared to the sham SMT group. At 10 months,
only the maintenance SMT group had improvements
in pain and disability. The authors concluded that
SMT is eective for the treatment of LBP and suggest-
ed maintenance manipulation for long-term benets.
In critique, less than 80% of patients completed fol-
low-up. Due to this potentially confounding factor,
the work group downgraded the level of evidence for
this study. This potential Level I study provides Level
II therapeutic evidence that, in patients with chron-
ic LBP, pain and function showed more improvement
in group with maintained SMT than in the group with
nonmaintained SMT or sham SMT at all time frames
after one month.
In a placebo and sham randomized controlled trial,
Von Heymann et al
55
evaluated the eectiveness of
spinal high-velocity low-amplitude manipulation
compared to treatment with a nonsteroidal anti-
inammatory drug. Patients with LBP for less
than 48 hours were randomized to receive spinal
manipulation therapy (SMT) and placebo drug
(n=37), sham SMT and 50 mg tablets diclofenac three
times a day (n=38), or sham SMT and placebo drug
(n=25). Physical disability (Roland Morris Disability
Questionnaire), function (SF-12), pain (VAS) o-
work time and rescue medication usage were recorded
at baseline, 7-9 days after randomization and 12-
week follow-up. Both intervention groups had better
outcomes than the placebo group. The manipulation
group experienced faster and more distinct reduction
in pain and disability compared to the diclofenac
group. There were no adverse eects, harm or
unexpected untoward events in either group. The
authors concluded that SMT was signicantly better
than diclofenac and placebo in the treatment of LBP.
This study oers Level I therapeutic evidence that, in
patients with acute LBP, SMT resulted in statistically
signicant short-term (9 days) improvement in pain
compared to medication. The clinical signicance was
uncertain. The two groups were similar at medium-
term follow-up.
In a randomized control trial, Grunnesjo et al
56
eval-
uated muscle stretching, manual therapy and steroid
injections in addition to staying active in patients
with acute and subacute LBP. Participants were ran-
domized into one of 4 groups: “stay active” care only
(n=35), “stay active” and muscle stretching (n=36),
“stay active, muscle stretching and manual therapy
(n=42), or “stay active,” muscle stretching, manual
therapy and steroid injections (n=47). The “stay ac-
tive” care included some active physical therapies in
addition to encouragement to stay physically active.
Quality of life measurements (The Gothenburg Qual-
ity of Life instruments) were recorded at baseline, af-
ter 5 weeks of treatment and at the end of the 10-week
trial. There was a signicant trend for increasing
well-being as additional modalities were added. The
authors concluded that additional eects were seen
as additional treatment modalities were added. This
study oers Level I therapeutic evidence that, in pa-
tients with LBP, addition of manual therapy to staying
active and stretching had similar eects on quality of
life compared to staying active and stretching alone at
10 weeks.
Licciardone et al
57
conducted a randomized controlled
study to determine the ecacy of osteopathic ma-
nipulative treatment for the treatment of LBP. Pa-
tients with LBP for at least 3 months were random-
ized to receive 7 visits over 5 months of osteopathic
manipulative treatment (n=46), sham manipulation
(n=23), or usual care only (n=20). Pain (VAS), self-re-
ported health status (SF-36 Health Survey), disability
(Roland-Morris Disability Questionnaire), lost work/
school days and satisfaction of care were recorded.
Follow-up was completed after one month (n=82), 3
months (n=71) and 6 months (n=66). There were no
signicant dierences in outcomes between osteo-
pathic manipulative treatment compared to sham
manipulation; both manipulation groups experienced
benets compared to no intervention. The authors
concluded that both osteopathic manipulative treat-
ment and sham manipulation provide benets com-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
123
pared to usual care alone in patients with chronic LBP.
In critique, the work group downgraded this study
from Level I to Level II due to less than 80% follow-up.
This study provides Level II therapeutic evidence that,
in patients with subacute LBP, osteopathic manipu-
lation provides no benet in pain or disability com-
pared with sham manipulation and that both provide
statistically signicant, but not clinically meaningful,
improvements when compared with no care.
Cambron et al
58
compared pain and disability
outcomes in patients with chronic LBP who received
exion distraction chiropractic care or physical
therapy in a randomized clinical trial. Patients with
LBP > 3 months were randomly assigned to receive
exion distraction chiropractic care using exion
distraction (n=123) or a physical therapy program
of strength, exibility and cardiovascular exercises
with the goal of strengthening the trunk muscles
(n=112). Both treatment programs were 4 weeks with
2-4 sessions per week. Patients reported pain (VAS)
and dysfunction (Roland Morris) at baseline and
one-month follow-up questionnaire. Both groups
experienced improvements in pain and disability;
however, the pain scores were signicantly lower
in the chiropractic group compared to the physical
therapy group. The authors concluded that exion
distraction was more eective in reducing pain than
the studied physical therapy program. This study
oers Level I therapeutic evidence that, in patients
with chronic LBP, SMT provides similar improvement
in pain and function compared to an exercise program
at one year follow-up. It oers Level IV evidence that
SMT results in improved pain and function.
Cecchi et al
59
compared the eect of spinal manipu-
lation, back school and individual physiotherapy on
pain and disability outcomes in a randomized trial of
patients with chronic LBP. Patients were randomized
to receive 15 one-hour sessions of back school (group
exercise, education/ergonomics) over the course of
3 weeks (n=70), 15 one-hour sessions of individu-
al physiotherapy (exercise, passive mobilization and
soft-tissue treatment) over the course of 3 weeks
(n=70), or 4-6 20-minute sessions of spinal manip-
ulation per week for 4-6 weeks (n=70). Participants
recorded pain (Pain Rating Scale) and disability (Ro-
land Morris Disability Questionnaire) at baseline, dis-
charge and follow-up at 3, 6 and 12 months. All pa-
tients experienced improvement in pain and disability
at discharge and 12-month follow-up. Function, pain
recurrences and drug intake were signicantly re-
duced compared to back school or physiotherapy. The
authors concluded that spinal manipulation resulted
in better improvements in pain and function com-
pared to back school or individual physiotherapy. This
study provides Level I therapeutic evidence that, in
patients with LBP, SMT results in statistically signif-
icant improvement in pain and functional compared
to multimodal physical therapy (baseline scores indi-
cate mild pain). However, it is uncertain if these im-
provements are of clinical signicance. It oers Lev-
el IV evidence that SMT results in improved pain and
function.
Cherkin et al
60
evaluated the dierent outcomes after
patients with acute LBP received the McKenzie meth-
od of physical therapy, chiropractic manipulation or
an educational booklet. Patients who still had LBP 7
days after an initial visit to the primary care practi-
tioner were randomized to receive up to 8 sessions in
a one-month period of McKenzie method of physical
therapy (n=133), up to 8 sessions in a one-month pe-
riod of chiropractic manipulation (n=122), or an ed-
ucational booklet only (n=66). Patients reported LBP
bothersomeness (11-point scale) and dysfunction
(Roland Disability Scale). There were no statistically
and clinically signicant dierences between groups.
The authors concluded that the McKenzie method of
physical therapy and chiropractic manipulation re-
sulted in similar outcomes in patients with LBP and
were only marginally better than the educational
booklet intervention. This study oers Level I thera-
peutic evidence that, in patients with LBP, there were
no statistical dierences in functional outcomes be-
tween educational booklet, SMT and McKenzie exer-
cise at 12 weeks. It oers Level IV evidence that SMT
results in improved pain and function.
Doran and Newell
47
investigated the eectiveness
of four dierent treatment options in patients with
acute LBP. Participants were randomly assigned to
receive at least 2 sessions of manipulation per week
(n=98), at least 2 sessions of physiotherapy per week
(n=104), corset applied on the rst day of the tri-
al (n=93) or two paracetamol tablets every 4 hours
(n=100). Patients completed questionnaires to report
whether their pain was worse, unchanged, improved,
or completely relieved at the end of the 3-week trial,
3 weeks after the conclusion of the trial, 3 months af-
ter enrollment and one year after enrollment. The au-
thors concluded that there were no signicant dier-
ences between any of the four studied interventions.
In critique, no validated outcomes were included in
this study and outcome data is limited. Due to these
reasons, the work group downgraded this study. This
potential Level I study provides Level II therapeutic
evidence that, in patients with acute LBP, SMT, phys-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
124
iotherapy, medication and corset resulted in similar
improvements up to 3 months.
In a randomized controlled trial, Enix et al
61
aimed
to compare chiropractic care and physical therapy
as treatments for chronic LBP in geriatric patients.
Participants aged 60-85 years with LBP were ran-
domized to receive 6 weeks (12-18 sessions) of either
chiropractic care (n=61) or physical therapy (n=57).
Patients completed pain questionnaires at baseline,
at the end of the 6-week trial and 6 weeks after trial
completion (week 12). Both groups experienced sig-
nicant improvements in pain. The authors conclud-
ed that there were no dierences in pain outcomes
between groups at 6- or 12-week follow-up. This
study oers Level I therapeutic evidence that, in geri-
atric patients with chronic LBP, physical therapy and
SMT resulted in similar improvement in pain relief
at 6 weeks’ follow-up (baseline scores indicate mild
pain). It oers Level IV evidence that SMT results in
improved pain and function.
Hemmila et al
62
conducted a randomized controlled
trial to compare the eectiveness of bone-setting,
light exercise therapy and physiotherapy in patients
with LBP greater than 7 weeks. Patients were ran-
domly allocated into groups to receive up to 10 ses-
sions of bone-setting (n=45), light exercise therapy
(n=35) or physiotherapy (n=34) over 6 weeks. Dis-
ability (Oswestry Disability Questionnaire) was re-
corded at baseline and one-year after treatment. Dis-
ability improved more in the bone-setting group. The
authors concluded that traditional bone-setting was
more eective than exercise or physiotherapy for pain
and disability related to LBP. However, baseline dis-
ability was low and the bone setting group had slight-
ly worse baseline scores on average than the compar-
ison groups. Overall improvements were small across
all groups and although the net improvement in the
bonesetting group was statistically greater, it is un-
certain whether this had clinical signicance. In addi-
tion, inclusion criteria included pain beyond 7 weeks,
but the duration of pretreatment pain beyond that
is unknown as is the balance of pain duration across
patients in each group. If there is substantial het-
erogeneity in pain duration across groups, this could
bias the outcomes as well. This study provides Level
I therapeutic evidence that, in patients with subacute
or chronic LBP and mild baseline disability, SMT,
physiotherapy and exercise result in similar improve-
ments in function at one year. It oers Level IV evi-
dence that SMT results in improved pain and function.
Hurwitz et al
63
compared outcomes related to LBP in
patients who received medical or chiropractic care
with or without physical modalities or physical ther-
apy in a multicenter randomized controlled trial.
Participants had back pain ranging from 3 weeks to
greater than one year. Distribution based on chronic-
ity was reasonably similar. In general, about 40% had
pain for less than 3 months at onset of treatment and
the other 60% had pain greater than 3 months, with
45 to 49% of the total having pain for greater than a
year. Patients were randomly assigned to receive chi-
ropractic care with physical modalities (n=172), chi-
ropractic care without physical modalities (n=169),
medical care with physical therapy (n=170), or med-
ical care without physical therapy (n=170). Physical
modalities included heat or cold therapy, ultrasound
and/or electrical muscle stimulation. Physical thera-
py included heat or cold therapy, ultrasound, electri-
cal muscle stimulation, soft tissue and joint mobili-
zation, traction, supervised therapeutic exercise and/
or strengthening and exibility exercises. Disability
(Roland-Morris Low-Back Disability Questionnaire)
and pain (numerical rating scale) were recorded at
baseline and 2, 6, 26, 52 and 78 weeks after enroll-
ment. A total of 610 (90%) completed follow-up after
18 months. Results revealed small, clinically insig-
nicant dierences in pain and disability outcomes.
The authors concluded that there were no clinically
meaningful dierences in outcomes between medi-
cal and chiropractic care without physical therapy or
modalities, besides a dierence in patient perception.
This study provides Level I therapeutic evidence that,
in patients with LBP of variable duration, SMT, SMT
with modalities, routine medical care and medical
care with physical therapy produced similar improve-
ments in pain and function at 18 months follow-up.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
125
Question 2 Evidence Summary:
Haas et al
49
conducted a randomized controlled trial
in patients with chronic LBP to identify the dose-
response relationship between visits to a chiropractor
for spinal manipulative therapy (SMT) and treatment
outcomes and to compare treatment outcomes of
manipulation versus light massage. Four hundred
patients with nonspecic LBP for at least 3 months
were prescribed 18 sessions with a chiropractor
(three times a week for six weeks). Participants were
randomized to receive either 0, 6, 12 or 18 sessions of
SMT (n=100 in each group). The chiropractor provided
light massage for the remaining sessions that did not
include SMT. Pain and disability (modied Von Kor
pain and disability scales) were recorded at baseline
and throughout a 52-week follow-up period. Pain and
disability improved in all groups and was sustained for
Question 2 Recommendation:
There is insucient evidence to determine whether 12 to 18 visits of spinal manipulative thera-
py (SMT) results in better outcomes than 6 visits for the treatment of low back pain.
Grade of Recommendation: Grade I
52 weeks. The greatest treatment eects were found
from 12 sessions of SMT. The authors concluded that 12
SMT visits had modest eects on chronic LBP outcomes
compared to the other dose levels, but the dierence
was not well distinguished. This study oers Level I
therapeutic evidence that, in patients with LBP, spinal
manipulative therapy is associated with statistically
signicant improvement in pain compared to light
massage. However, it is uncertain whether this was
clinically signicant. Regarding frequency, this study
oers Level I therapeutic evidence that 12-18 visits of
SMT were statistically better than 6 visits at 12-week
follow-up; no dierence between doses at 1-year
follow-up. Again, the dierences were small and the
clinical signicance was uncertain.
Q1&2 Future Directions for Research
Despite multiple studies, there is still uncertainty regarding the benets of SMT
for both acute and chronic LBP. There is signicant heterogeneity across stud-
ies that contribute to uncertainty as well. There are opportunities for further
well-designed studies to determine the ecacy of SMT in the treatment of LBP.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
126
QQ
PM&R Questions 1 & 2.
vi. Exercise/PT Exercise/Physical Therapy vs or plus Massage
Q1 Recommendations:
There is insucient evidence to determine the ecacy of acupressure compared to a standard-
ized multimodal physical therapy.
Grade of Recommendation: I
In the long term, it is suggested that the addition of massage to an exercise program provides
no benet when compared to an exercise program alone.
Grade of Recommendation: B
There is insucient evidence that the addition of massage to an exercise program provides
short-term relief of pain.
Grade of Recommendation: I
Q1 Evidence Summary:
Hsieh et al
64
compared ecacy of acupressure with
that of usual care hospital based physical therapy for
treating patients with chronic LBP. Patients received
treatment for 4 weeks in both groups. Pain scores were
evaluated in 56 and 65 patients studied at 6 months
with 82% follow-up. This was a randomized study
with one provider for the acupressure. At 6-month
follow-up, there was signicant reduction in pain in
the acupressure group compared to physical therapy.
This study provides Level I evidence that acupressure
results in signicantly greater relief of pain than usual
care hospital based physical therapy at medium-term
follow-up in patients with chronic LBP.
Hsieh et al
65
compared ecacy of acupressure with
that of standardized out patient physical therapy for
treating patients with chronic LBP. This was a ran-
domized study with one provider for the acupressure.
At 6 months, with 84% follow-up, there was signi-
cant improvement in pain and disability scores in the
acupressure group compared to physical therapy. This
study provides Level I evidence that acupressure re-
sults in signicantly greater improvement in pain and
function than standardized outpatient physical thera-
py at medium-term follow-up in patients with chron-
ic LBP.
These two studies by Hseih et al provided high quality
evidence favoring acupressure over physical therapy.
However, the acupressure was administered by one
provider in both studies and concerns for external va-
lidity demand corroborating results by other provid-
ers to verify ecacy.
Kankaanpa et al
66
conducted a randomized trial to
compare ecacy of active rehabilitation to a passive
control group consisting of heat and massage. There
were 54 patients total with 91% follow-up at one year.
These patients had mild disability at baseline. At one
year, the active group showed more improvement in
pain and disability scores. This study was downgrad-
ed for small sample size, inability to mask groups and
the relatively low baseline disability scores. It pro-
vides Level II evidence that active rehabilitation re-
sults in greater improvement in LBP relative to heat
and massage at one year.
Little et al
67
compared the eectiveness of Alexander
technique lessons, massage therapy and exercise ad-
vice with behavioral counseling for the treatment of
chronic or recurrent back pain. Patients with LBP for
at least 3 months were randomized to receive normal
care (n=144), massage (n=147), 6 Alexander tech-
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
127
nique lessons (n=144) or 24 Alexander technique les-
sons (n=144). Half of each group randomly received
an exercise prescription with behavioral counseling.
Disability (Roland Morris disability score) and num-
ber of days in pain were recorded at baseline, three
months and one year. Disability in the group that
received exercise and lessons in the Alexander tech-
nique decreased while those who received massage
had no eect on disability. This study provides Level
II evidence that massage produced no long-term clin-
ically meaningful eects compared to usual care.
In a prospective study, Zhang et al
68
aimed to deter-
mine the eectiveness of Chinese massage added to
core stability exercises for the treatment of LBP. The
inclusion criteria are not clearly stated in terms of
acuity. It is implied that these were probably acute or
subacute episodes, but this is uncertain. These pa-
tients were randomized to receive Chinese massage
combined with core stability exercises (n=46) or Chi-
nese massage alone (n=46). Pain (VAS) and disability
(Oswestry disability index) were assessed at baseline
and after 2 and 8 weeks. Recurrence of LBP was eval-
uated after one year, but denition of recurrence was
not clearly stated. Both groups experienced improve-
ments in pain and disability with no dierences be-
tween groups after 2 weeks. After 8 weeks, pain and
disability were signicantly lower in the exercise and
massage group compared to the massage-only group.
The massage-only group had a signicantly higher
recurrence rate compared to the massage and exercise
group based on phone interview one year later. This
study provides Level II evidence that exercise is more
eective than massage.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends high-level studies on acupressure versus exercise
across multiple centers.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
128
QQ
PM&R Questions 1 & 2.
vii. Active stabilization exercise
Q1 Recommendation:
There is insucient evidence to make a recommendation for or against lumbar stabilization in
patients with chronic low back pain.
Grade of Recommendation: I
Q1 Evidence Summary:
Moussouli et al
69
investigated the eects of an iso-
metric and isotonic stabilization exercise program on
health-related quality of life in a study of women with
chronic LBP. Women with LBP for at least 6 months
were randomized to receive 4 60-minute sessions
per week of isometric stabilization exercises (n=13),
isotonic stabilization exercises (n=13), or no exercise
(n=13). Health-related quality of life (SF=36) was as-
sessed upon enrollment, immediately after the four-
week treatment period and 9-months after treatment
termination. The patients in the isometric stabiliza-
tion group had signicant improvements in pain and
vitality at treatment-termination that was maintained
for 9 months. The authors concluded that isometric
stabilization exercises reduce pain and enhance vital-
ity for at least 9 months in women with chronic LBP.
The study’s small sample size was the primary factor
in downgrading the level of evidence. This potential
Level I study oers Level II therapeutic evidence that
use of an isometric stabilization program improves
functional outcomes in women with chronic LBP at
9 months relative to a dynamic stabilization exercise
program or no exercise at all.
Lomond et al
70
compared the eects of trunk stabili-
zation versus a movement system impairment exer-
cise strategy to treat patients with chronic LBP. Their
premise is that LBP arises at least in part due to im-
paired postural coordination. Patients with LBP for at
least 6 months were randomized to a 10-week physi-
cal therapy program consisting of either stabilization
(n=29) or movement system impairment exercises
(n=29). Pain (Numeric Pain Index) and function (Os-
westry Disability Index) were assessed 11 weeks and
6 months after treatment initiation along with EMG
function to assess postural reeducation. Both groups
experienced improvements in pain and function at
6-month follow-up. The detailed data reporting fo-
cused on EMG and muscle reeducation changes. There
is one sentence that mentions comparable improve-
ment in pain and disability scores although it suggests
these improvements are modest and maybe not clin-
ically meaningful. The authors concluded that sta-
bilization treatment does not preferentially improve
treatment outcomes in patients with LBP. The study
had no power calculation and the sample size was
small. They also did not report the details of the pain
and disability scores. This study oers Level IV thera-
peutic evidence exercise improves pain and disability
in patients with LBP and Level II evidence that trunk
stabilization and movement system impairment exer-
cises result in similar outcomes for pain and disability
with no improvement voluntary postural adjustment
mechanisms in patients with LBP.
Ganesh et al
71
investigated the eectiveness of the
star excursion balance test (SEBT) grid training for
the treatment of chronic LBP. Patients with mechan-
ical LBP for at least three months were randomized
to receive 5 sessions per week for 4 weeks of diagno-
sis-specic interventions, core muscles strengthen-
ing and muscle training using the SEBT grid (n=30)
or diagnosis-specic interventions, core muscle
strengthening and stationary cycling (n=30). Disabil-
ity (Oswestry Disability Index), strength and endur-
ance (pressure-biofeedback unit) were assessed at
baseline and at 4 and 16 weeks. Both groups had im-
provement in disability, strength and endurance with
better improvement in the SEBT group compared to
the conventional exercises. Although both programs
resulted in improvement, the authors concluded that
core muscle strengthening using a SEBT grid is more
eective than conventional exercise programs. This
study provides Level I therapeutic evidence that the
addition of star excursion balance test and training
to a diagnosis-specic intervention and core mus-
cle strengthening improves functional outcomes at
short-term follow-up when compared with a cycling
program using the same exercise program. Baseline
disability for this study was modest (low 20 scores on
Oswestry Disability prior to treatment).
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
129
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends undertaking randomized controlled trials with
long-term follow-up evaluating the benets of stabilization exercise in patients
with LBP.
QQ
PM&R Questions 1 & 2.
viii. McKenzie exercise (includes directional preference, centralization and
mechanical diagnosis and therapy [MDT])
Work Group Narrative: The majority of McKenzie literature involves the centralization phenomenon
which is commonly seen in patients with leg pain. This review examined only evidence in the subset
of patients without radiating pain. Additional literature discussing clinical benets from McKenzie for
the treatment of LBP including radiating pain were not included in our systematic review. Therefore, a
denitive statement of McKenzie in all patients with LBP cannot be made.
Q1 Recommendations:
McKenzie method is an option for the treatment of chronic low back pain.
Grade of Recommendation: C
There is insucient evidence that McKenzie method results in dierent outcomes when com-
pared to a dynamic strengthening program for the treatment of chronic low back pain.
Grade of Recommendation: I
There is insucient evidence that McKenzie method is better or worse than back school for the
treatment of chronic low back pain.
Grade of Recommendation: I
Q1 Evidence Summary:
Petersen et al
72
conducted a randomized controlled
trial to compare the eect of a McKenzie-based ex-
ercise program versus a strengthening exercise pro-
gram in patients with subacute or chronic LBP. Pa-
tients with LBP for at least 8 weeks were randomized
to be treated with the McKenzie method (n=132) or
with a dynamic strength training program (n=128) for
8 weeks in a clinic followed by 2 weeks at home. A total
of 260 patients were randomized. Follow-up was 71%
(90/132) in the McKenzie group and 67% (86/128) in
the dynamic exercise group. Pain (Manniche’s Low
Back Pain Rating Scale) and disability (15-item dis-
ability scale) were recorded at baseline, after comple-
tion of the treatment program and 2 and 8 months af-
ter termination of the treatment. The participants in
the McKenzie group had signicantly greater reduc-
tion of disability compared to the strengthening pro-
gram at 2-month follow-up. At 8-month follow-up,
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
130
there were no dierences in pain or disability between
groups. The authors concluded that the McKenzie
method and intensive dynamic strengthening train-
ing are equally eective for the treatment of subacute
or chronic LBP. This Level I study was downgraded
because a substantial percent of patients were lost to
follow-up. This provides Level II evidence that, at 8
months, there is no dierence between pain and dis-
ability scores between strength training and a McK-
enzie based exercise program in patients with CLBP.
This also provides Level IV evidence that an exercise
program results in signicant improvement in pain
and disability for patients with chronic LBP.
In a one-year follow-up to the Petersen et al
72
ran-
domized controlled trial, Petersen et al
73
reported the
long-term outcomes of the McKenzie-based exercise
program and strengthening exercise program. This is
the same study as above, but slightly longer follow-up
and with evaluation of prognostic factors. They were
able to retrieve additional patients with data on
93% at 14 months, versus the 70% follow-up at the
8-month mark. There were no dierences in func-
tional status, pain level, work status or use of health
care services at 14-month follow-up between the 2
groups. Again there was signicant improvement in
pain and disability scores that was of questionable
clinical importance. In the McKenzie group, there was
a 7-point improvement in the ODI from 36 to 29 and a
9 point improvement in the other group from 39 to 30.
A total of 665 reported poor outcomes on reduction of
disability and 75% poor reduction of pain. There were
similar modest improvements in pain scores. Out-
comes were most correlated with low expectations
for future work ability, lack of compliance with ex-
ercise program and lower initial baseline scores. The
authors concluded that poor long-term outcomes can
be explained by various patient-related factors which
seemed to be stronger determinants of outcomes than
the exercise programs studied. This study oers Level
I therapeutic evidence that, at 14 months, there is no
dierence between pain and disability scores between
strength training and a McKenzie based exercise pro-
gram in patients with chronic LBP.
Garcia et al
74
aimed to compare the eectiveness of
Back School and the McKenzie method for patients
with chronic nonspecic LBP. Patients with LBP for
at least 3 months were randomized to receive one
session per week for 4 weeks of either a group-based
Back School (n=74) or individual McKenzie treatment
(n=74). All participants were also instructed to com-
plete exercises at home daily. The care provider of
both groups was certied by the McKenzie Institute of
Brazil and the outcome assessor received two months
of McKenzie training from the McKenzie-certied
therapist. Pain intensity (numerical rating scale) and
disability (Roland-Morris Disability Questionnaire)
were assessed at baseline and 1, 3 and 6 months after
randomization. Participants in the McKenzie group
had statistically greater improvements in disability
at one month but not 6 months compared to the Back
School group. The authors concluded that the McK-
enzie method was slightly more eective than Back
School for disability, but not for pain intensity in par-
ticipants with chronic LBP. This study provides Level I
therapeutic evidence that, at 6-month follow-up, the
McKenzie method provides slight disability benet as
compared to the back school method though pain im-
provements are similar and modest at this time point.
Both result in improvement, although clinical impor-
tance is debatable.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends high-level studies on McKenzie/MDT for axial back
pain utilizing certied MDT clinicians.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
131
QQ
PM&R Questions 1 & 2.
ix. Yoga
Q1 Recommendation:
It is suggested that, in patients with mild chronic low back pain, yoga may oer medium-term
improvements in pain and function compared to usual care, although these improvements are
not clinically meaningful due to low baseline pain/disability.
Grade of Recommendation: B
Q1 Evidence Summary:
In a randomized controlled trial. Aboagye et al
75
compared the cost-eectiveness of medical yoga
versus evidence-based exercise therapy and self-care
advice for nonspecic LBP. In a 6-week treatment
period, participants were randomly assigned to
participate in group medical yoga twice a week (n=52),
individual standardized strength exercise therapy
twice weekly (n=52), or a booklet of self-care advice
and advice to stay active (n=55). Health-related
quality of life (EQ-5D) was assessed at baseline, 6
weeks, 6 and 12 months. Follow-up response rates
were 89% for yoga, 69% for exercise and 63% for
self-care advice. At 12-month follow-up, participants
in the yoga group who adhered to the recommended
protocol had statistically signicantly better HRQOL
(0.79 ± 0.14) compared to self-care advice (0.75 ±
0.23), but there was no dierence when comparing to
exercise therapy. The authors concluded that 6 weeks
of adherence to uninterrupted medical yoga therapy is
cost-eective for early treatment of nonspecic LBP.
During critical appraisal, the work group downgraded
the level of evidence of this study due to less than 80%
follow-up. In addition, the authors did not clearly
dene the nature of the inclusion criteria. These
appear to be patients with nonspecic back pain, but
acuity is not stated and baseline severity appears to
be mild. Implication would be that these were patients
with relatively acute back pain. This potential Level
I study oers Level II therapeutic evidence that
there was no dierence in health outcomes between
treatment groups for patients receiving yoga relative
to an alternative exercise program, although both
were better than self-care in patients with uncertain
acuity of LBP.
Tilbrook et al
76
conducted a multicenter randomized
controlled trial to examine the eectiveness of yoga
for treatment of chronic or recurrent LBP. Patients
with LBP received a back pain education booklet and
were randomized to participate in 12 yoga classes over
3 months (n=156) or usual care (n=157). Back func-
tion (Roland-Morris Disability Questionnaire), pain
(Aberdeen Back Pain Scale), pain self-ecacy (Pain
Self-Ecacy Questionnaire) and general health mea-
sures were recorded at baseline and after 3, 6 and 12
months. These patients had mild disability at base-
line. The yoga group had better back function at all 3
follow-up points. Pain and general health scores were
similar between groups. The authors concluded that a
12-week yoga program had greater improvements in
back function compared to usual care in adults with
chronic or recurrent LBP. This study provides Level I
therapeutic evidence that, in patients with LBP of mild
severity, yoga is associated with greater improve-
ments in disability at one year compared to usual care.
Williams et al
77
compared the eects of Iyengar yoga
therapy versus education in a randomized controlled
trial of patients with nonspecic chronic LBP. Patients
with LBP for more than 3 months were randomized to
receive a 16-week period of Iyengar yoga (n=30) or
education (n=30). Functional disability (Pain Disabil-
ity Index), pain intensity (Short Form-McGill Pain
Questionnaire), pain medication usage, pain-related
attitudes and behaviors, and spinal range of motion
were assessed before and after the interventions and
at 3-month follow-up. Of the 60 participants en-
rolled, 42 (70%) completed the study. The yoga group
had signicant reduced pain intensity, function-
al disability and pain medication usage at 3-month
follow-up. The authors concluded that Iyengar yoga
therapy results in improvement in medical and func-
tional LBP-related outcomes in patients with mild
chronic LBP. In critique, small sample size and less
than 80% follow-up were factors in downgrading the
level of evidence for this study. In addition, it is not-
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
132
ed that this group of patients had chronic LBP that
was mild in severity at baseline. This potential Level I
study oers Level II therapeutic evidence that, in pa-
tients with LBP of mild severity, yoga may decrease
disability at 3 months compared to self-directed
standard medical care. It also resulted in signicant
improvement in pain, although these improvements
were clinically very small, at least in part due to the
relatively low starting scores at baseline.
Williams et al
78
conducted a randomized controlled
trial to compare the eects of yoga and standard
medical care in patients with chronic LBP. Patients
with LBP for greater than 3 months were randomized
to a yoga group (n=43) or control group of standard
medical care (n=47). Yoga participants completed a
24-week program of biweekly yoga classes. Disability
(Oswestry Disability Questionnaire), pain (VAS), de-
pression (Beck Depression Inventory) and pain med-
ication usage were recorded upon enrollment, after 12
weeks, upon completion of the program (24 weeks)
and 6-month follow-up. The yoga group experienced
signicantly greater functional disability, pain inten-
sity and depression improvements compared to the
usual care group at 24 weeks. The authors concluded
that yoga results in improved functional disability,
pain intensity and depression in adults with chronic
LBP. Patient follow-up was less than 80%; therefore,
the work group downgraded this study from Level I to
Level II. Again, it is noted that this group of patients
had chronic LBP that was mild in severity at baseline.
This study provides Level II therapeutic evidence that
yoga provides signicant improvements in pain and
disability at 6 months compared to standard care.
Again, at least in part due to low starting scores at
baseline, the magnitude of these improvements were
small.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
There is an opportunity to look at the ecacy of yoga in populations with higher
baseline pain and disability.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
133
QQ
PM&R Questions 1 & 2.
x. Aerobic exercise
Q1 Recommendations:
Aerobic exercise is recommended to improve pain, disability and mental health in patients with
nonspecic low back pain at short-term follow-up.
Grade of Recommendation: A
There is insucient evidence that aerobic exercise improves pain, disability and mental health
in patients with non-specic low back pain at long-term follow-up.
Grade of Recommendation: I
Q1 Evidence Summary:
Murtezani et al
79
conducted a randomized controlled
trial to study the eectiveness of high-intensity aer-
obic exercise for the treatment of chronic LBP. Pa-
tients with LBP for at least 3 months were randomized
to receive 3 30- to 45-minute sessions per week of
supervised aerobic exercise based on individual heart
rate zones (n=50) or passive modalities such as in-
terferential current, transcutaneous electrical nerve
stimulation, ultrasound and heat without any form
of physical activity (n=51) for 12 weeks. LBP intensity
(VAS), disability (Oswestry Low Back Pain Disability
Questionnaire), ngertip-to-oor distance and psy-
chosocial factors were assessed upon enrollment and
after 12 weeks. The exercise group had signicant im-
provements in pain intensity, disability and anxiety/
depression at 12 weeks. The authors concluded that
high-intensity aerobic exercise reduces pain, disabil-
ity and psychological strain in patients with chronic
LBP. This study oers Level I therapeutic evidence
that, in patients with LBP, aerobic exercise resulted
in better pain and functional outcomes compared to
passive modalities at short-term follow-up.
In a randomized controlled trial, Cuesta-Vargas et al
80
evaluated the eect of the addition of deep water run-
ning to standard general practice compared to general
practice alone for the treatment of LBP. Patients with
LBP for at least three months were randomized to re-
ceive general practice plus three 30-minute sessions
of deep water running per week (n=29) or general
practice alone (n=29) for 15 weeks. General practice
involved a physician’s consultation and educational
booklet. Disability (Spanish version of Roland Mor-
ris Disability Questionnaire), pain (VAS) and general
health (SF-12) were recorded at baseline and at 4, 6
and 12 months. Both groups had improvements. The
deep-water running group had signicantly great-
er improvements in pain and disability compare to
general practice alone. The authors concluded that
the addition of deep water running to general prac-
tice was more eective than general practice alone
in patients with nonspecic chronic LBP. This study
provides Level I therapeutic evidence that, in patients
with LBP, the addition of aerobic exercise to an ed-
ucation program compared to an education program
alone resulted in signicant improvement in pain,
disability and mental health at 12-month follow-up.
Chatzitheodorou et al
81
aimed to evaluate the ef-
fects of high-intensity aerobic exercise in patients
with chronic musculoskeletal LBP. Patients with LBP
for at least 6 months were randomized to receive a
high-intensity aerobic exercise program 3 times per
week (n=10) or passive modalities without physi-
cal activity (n=10) for 12 weeks. Pain (McGill Pain
Questionnaire), disability (Roland-Morris Disability
Questionnaire), psychological strain (Hospital anxi-
ety and Depression Scale) and cortisol concentrations
(ng/mL) were recorded before and after the 12-week
treatment period. Participants in the exercise group
had signicant reductions in pain, disability and
psychological strain while the subjects who received
passive modalities did not experience any changes.
The authors concluded that high-intensity exercise
improved pain, disability and psychological strain in
subjects with chronic LBP, but did not improve serum
cortisol concentrations. Although the sample size
was small, statistically signicant dierences were
found between patient groups. This study oers Lev-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
134
el I therapeutic evidence that, at 12-week follow-up,
high intensity aerobic exercise decreases pain, dis-
ability and anxiety/depression compared to passive
modalities in patients with chronic LBP.
Tritilanunt et al
82
evaluated the ecacy of an aerobic
exercise and health education program for the treat-
ment of chronic LBP. Patients with LBP for at least
three months were randomly assigned to participate
in an aerobic exercise program (n=36) or a lumbar
exion exercise program (n=36). Health education
was included in both programs. Pain (VAS), anthro-
pometric and biochemical characteristics were re-
corded before and after the 12-week treatment period.
The aerobic exercise group had signicantly greater
improvements in pain compared to the lumbar ex-
ion group. The authors concluded that the aerobic ex-
ercise and education program is useful and can be a
treatment option for patients with chronic LBP. This
study provides Level I therapeutic evidence that, in
patients with chronic LBP, aerobic exercise decreases
pain more than lumbar exion exercise and both ex-
ercise treatments resulted in signicant reduction in
pain.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends randomized controlled trials with long-term
follow-up looking at the benets of aerobic exercise.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
135
QQ
PM&R Questions 1 & 2.
xi. Work hardening or conditioning
Q1 Recommendations:
In patients with low back pain, work hardening may be considered to improve return to work.
Grade of Recommendation: C
There is insucient evidence that work hardening is dierent than an active therapeutic ex-
ercise program or guideline-based physical therapy.
Grade of Recommendation: I
Q1 Evidence Summary:
Bendix et al
83
conducted a randomized controlled tri-
al to investigate the eectiveness of a comprehensive
functional restoration program versus an intensive
outpatient physical training program for the treat-
ment of chronic LBP. Patients with chronic LBP were
randomized to receive functional restoration (n=64)
or outpatient intensive physical training (n=74). The
functional restoration program involved physical
training, ergonomic training and behavioral support
for 39 hours per week for 3 weeks. The outpatient in-
tensive physical training program consisted of 1.5
hours of training 3 times per week for 8 weeks. Pa-
tients were assessed at baseline and at one-year fol-
low-up. There were no statistically signicant dif-
ferences in work capability, sick leave, health care
contacts, back pain, leg pain or self-reported activi-
ties of daily living outcomes between groups. The au-
thors concluded that functional restoration program
was superior to the physical training program only in
terms of overall assessment, but no other outcomes.
This study provides Level I therapeutic evidence that,
in patients with LBP, functional restoration and out-
patient intensive training provide equivalent results
for sick leave, back pain and function at one year.
Sang et al
84
evaluated the eectiveness of a work hard-
ening program for the treatment of LBP. Patients with
a work-related back injury who were unable to work
and referred to the occupational therapy department
were enrolled in a 12-week work hardening program
(n=32). The program consisted of muscle stretching,
lifting capacity training, carrying capacity training
and work tolerance training based on the overload
training principle. Participants completed two to three
90-minute sessions per week for 12 weeks. Return to
work was recorded during a 3-month follow-up via
telephone. Seventy-ve percent of the participants
who completed the program had returned to work by
3-month follow-up. The authors concluded that since
this rate was similar to other studies, the overload-
ing principle should be used to design work hardening
programs. This study oers Level IV therapeutic evi-
dence that work hardening is associated with return
to sedentary-to-medium work in 75% patients with
LBP.
Casso et al
85
conducted a prospective study to investi-
gate the return-to-work status one year after a phys-
ical reconditioning program in manual laborers with
chronic LBP. Patients with LBP and absent from work
for at least 3 months (n=125) completed a 3-week in-
patient program consisting of 6 hours of group treat-
ment per day, 5 days a week. Participants and their
physicians were sent a follow-up questionnaire one
year after completion of the program. Of the 109 pa-
tients who had a job available to them at the time of
completion of the program, 90 (81.6%) were consid-
ered capable of returning to work full- or part-time.
After one year, 57 (52.3%) patients were working and
52 patients were on disability leave (47.7%). The au-
thors concluded that the reconditioning program had
positive eects on return-to-work status after one
year. This study oers Level IV therapeutic evidence
that an intensive recondition program results in re-
turn to part-time or full-time work in about 80% at
the end of training program and about 50% at one-
year follow-up.
Beaudreuill et al
86
evaluated the eectiveness of a
functional restoration program for patients with
chronic LBP in a prospective study with one-year
follow-up. Patients absent from work due to LBP for at

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
136
least three months (n=39) were enrolled in a functional
restoration program. The program consisted of
physician counseling, physical exercises, aerobic
activity, manual handling and lifting techniques,
muscle strengthening on machines, stretching and
relaxation for a total of 5.5 hours per day, 5 days a
week, for 5 weeks. One year after completion of the
program, 25 (64%) patients had returned to work and
the number of sick leave days signicantly decreased
compared to the year before the program. The authors
concluded that the functional restoration program
was eective. This study oers Level IV therapeutic
evidence that, in patients with LBP, work hardening
improves return-to-work rate.
Luk et al
87
aimed to study the eectiveness of a mul-
tidisciplinary rehabilitation program for patients
with chronic LBP. Patients with LBP for at least three
months (n=65) were enrolled in a 14-week multidis-
ciplinary rehabilitation program consisting of phys-
ical conditioning, work conditioning and work read-
iness. LBP intensity (VAS), self-perceived disability
(Oswestry Disability Questionnaire Index), range of
motion, isoinertial performance of the trunk mus-
cles and depression were recorded at baseline, week
7 and 14 and month 6. Twenty-eight (51.8%) of the
54 patients who completed the 6-month follow-up
assessments returned to work. Pain signicantly im-
proved in both groups at 6-month follow-up. Disabil-
ity improved signicantly more in those who returned
to work compared to those who did not. The authors
concluded that this rehabilitation program improved
physical functioning and ability to return to work.
This study provides Level IV therapeutic evidence that
14-week work hardening program resulted in about
50% return-to-work (RTW) rate, improved function-
al scores only in those that RTW and improved pain
scores regardless of RTW. RTW was predicted 74% of
the time. All patients that returned to work were on
sick leave at entry.
Roche et al
88
performed a multicenter prospective ran-
domized controlled study to compare the short-term
eectiveness of active individual therapy and a func-
tional restoration program for the treatment of LBP.
All patients were unable to work at the time of enroll-
ment. Patients with chronic LBP were randomized to
receive 5 weeks of either a functional restoration pro-
gram (n=68) or active individual therapy (n=64). The
functional restoration program consisted of 25 hours
per week of isotonic muscular-strengthening exer-
cises and endurance exercises increasing progressive-
ly throughout the program, referral to a psychologist
and dietary advice. The active individual therapy con-
sisted of 3 hours per week of exibility training, pain
management, stretching and proprioception exercis-
es plus instructions to complete exercises at home for
50 minutes twice a week. Trunk exibility, endurance,
pain severity (VAS) and impact of pain on quality of
life (Dallas Pain Questionnaire, DPQ) such as dai-
ly activities, work and leisure activities, anxiety and
depression and social interest were recorded at base-
line and upon completion of the 5-week program. All
outcomes improved in both groups with the exception
of endurance in the active individual therapy group.
Pain intensity and DPQ scores for daily activities and
work and leisure were similar between groups. Other
outcomes improved signicantly greater in the func-
tional restoration program compared to the active
individual therapy group. The authors concluded that
low-cost ambulatory active individual therapy is ef-
fective and the main advantage of a functional resto-
ration program is improved endurance. This study of-
fers Level I therapeutic evidence that work hardening
may be slightly better than active exercise program
in improving quality of life and RTW in patients with
CLBP currently unable to work. This study also pro-
vides Level IV therapeutic evidence that an active to
intensive exercise program results in improvement in
quality of life and RTW.
Sivan et al
89
investigated the eect of a 3-week func-
tional restoration program on functional and voca-
tional outcomes in patients with chronic LBP. Pa-
tients with LBP for at least 6 months were enrolled in
an intense rehabilitation program 5 days a week for
3 weeks totaling 100 hours. The program consisted of
physical training (aerobics, hydrotherapy, back ex-
ercises) and psychological and occupational training
(education, CBT, relaxation techniques, recreational
activities, group counseling). Functional status (Os-
westry Disability Index, ODI and Roland Morris Dis-
ability Questionnaire, RM) and impact on work status
were assessed at baseline and at least one year after
completion of the program (n=118). Functional status
(ODI and RM) and work status signicantly improved.
The authors concluded that this functional restoration
program improves the functional and vocational sta-
tus of patients with chronic LBP Approximately 1/3
of patients were lost to follow-up. This study oers
Level IV therapeutic evidence that, for patients with
CLBP and impaired ability to work, an intensive exer-
cise program results in improved RTW and functional
outcome scores after 2 years.
Van der Roer et al
90
conducted a multicenter prag-
matic randomized controlled trial to study the e-
cacy of an intensive group training protocol for the
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
137
treatment of nonspecic chronic LBP. Patients with
LBP for less than 12 weeks from 49 dierent primary
care practices were randomly assigned to an intensive
group training protocol (n=60) or physiotherapy ac-
cording to the Dutch guidelines for LBP (n=54). The
intensive group training protocol included 10 individ-
ual sessions and 20 group sessions of exercise thera-
py, back school and operant-conditioning behavioral
principles with a goal to return to normal daily activ-
ities. Functional disability (Roland Morris disabili-
ty questionnaire), pain intensity (numerical rating
scale), perceived recovery and sick leave due to LBP
were recorded at baseline and after 6, 13, 26 and 52
weeks. Intention-to-treat and per-protocol analyses
revealed no signicant dierences between groups at
one-year follow-up. The authors concluded that the
intensive group training protocol was not more eec-
tive than usual physiotherapy for chronic LBP. In cri-
tique, the study’s sample size was small and less than
80% of patients completed follow-up. Due to these
reasons, the work group downgraded the study from
Level I to Level II. This is also a less chronic popula-
tion than other studies with symptoms present less
than 12 weeks. This study provides Level II therapeu-
tic evidence that an intensive group training protocol
involving exercise, education and behavioral princi-
ples was no more eective than PT done per the Dutch
guidelines at one-year follow-up of patients with
chronic LBP. This was true for functional outcomes
(RM), pain and fear avoidance.
Q2 Evidence Summary:
A systematic review of the literature yielded no studies to adequately address this question.
Q1&2 Future Directions for Research
The work group recommends undertaking high quality clinical and cost-
eectiveness studies comparing work hardening to other forms of occupational
rehabilitation.
References
1. Durmus D, Unal M, Kuru O. How eective is a modi-
ed exercise program on its own or with back school in
chronic low back pain? A randomized-controlled clini-
cal trial. J Back Musculoskel Rehabil. 2014;27(4):553-561.
2. Hurri H. The Swedish back school in chronic low back
pain. Part I. Benets. Scand J Rehabil Med. 1989;21(1):33-
40.
3. Jaromi M, Nemeth A, Kranicz J, Laczko T, Betlehem J.
Treatment and ergonomics training of work-related
lower back pain and body posture problems for nurses. J
Clin Nurs. 2012;21(11/12):1776-1784.
4. Morone G, Paolucci T, Alcuri MR, et al. Quality of life
improved by multidisciplinary back school program in
patients with chronic non-specic low back pain: a sin-
gle blind randomized controlled trial. Eur J Phys Rehabil
Med. 2011;47(4):533-541.
5. Kuukkanen T, Mälkiä E, Kautiainen H, Pohjolainen T.
Eectiveness of a home exercise programme in low
back pain: a randomized ve-year follow-up study.
Physiother Res Int. 2007;12(4):213-224.
6. Shirado O, Doi T, Akai M, et al. Multicenter random-
ized controlled trial to evaluate the eect of home-
based exercise on patients with chronic low back pain:
the Japan low back pain exercise therapy study. Spine.
2010;35(17):E811-819.
7. Underwood MR, Morgan J. The use of a back class teach-
ing extension exercises in the treatment of acute low
back pain in primary care. Fam Pract. 1998;15(1):9-15.
8. Krein SL, Kadri R, Hughes M, et al. Pedometer-based
internet-mediated intervention for adults with chronic
low back pain: randomized controlled trial. J Med Inter-
net Res. 2013;15(8):e181-e181 181p.
9. Dehghan M, Farahbod F. The ecacy of thermother-
apy and cryotherapy on pain relief in patients with
acute low back pain, a clinical trial study. J Clin Diag Res.
2014;8(9):LC01-LC04.
10. Kettenmann B, Wille C, Lurie-Luke E, Walter D, Kobal
G. Impact of continuous low level heatwrap therapy in
acute low back pain patients: subjective and objective
measurements. Clin J Pain. 2007;23(8):663-668.
11. Mayer JM, Ralph L, Look M, et al. Treating acute low
back pain with continuous low-level heat wrap therapy
and/or exercise: a randomized controlled trial. Spine J.
2005;5(4):395-403.
12. Nadler SF, Steiner DJ, Erasala GN, Hengehold DA, Abeln
SB, Weingand KW. Continuous low-level heatwrap
therapy for treating acute nonspecic low back pain.
Arch Phys Med Rehabil. 2003;84(3):329-334 326p.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
138
13. Nadler SF, Steiner DJ, Petty SR, Erasala GN, Henge-
hold DA, Weingand KW. Overnight use of continuous
low-level heatwrap therapy for relief of low back pain.
Arch Phys Med Rehabil. 2003;84(3):335-342 338p
14. Shakoor MA, Rahman MS, Moyeenuzzaman M. Effects
of deep heat therapy on the patients with chronic low
back pain. Mymensingh Med J. 2008;17(2 Suppl):S32-38.
15. Tao X, Bernacki EJ. A randomized clinical trial of con-
tinuous low-level heat therapy for acute muscular
low back pain in the workplace. J Occup Environ Med.
2005;47(12):1298-1306 1299p.
16. Durmus D, Alayli G, Goktepe AS, Taskaynatan MA, Bilgi-
ci A, Kuru O. Is phonophoresis effective in the treatment
of chronic low back pain? A single-blind randomized
controlled trial. Rheumatol Int. 2013;33(7):1737-1744.
17. Ebadi S, Ansari NN, Naghdi S, et al. The effect of
continuous ultrasound on chronic non-specific low
back pain: a single blind placebo-controlled
randomized trial. BMC Musculoskelet Disord.
2012;13:192.
18. Herman E, Williams R, Stratford P, Fargas-Babjak A,
Trott M. A randomized controlled trial of transcutane-
ous electrical nerve stimulation (CODETRON) to deter-
mine its benefits in a rehabilitation program for acute
occupational low back pain. Spine. 1994;19(5):561-568.
19. Weiner DK, Rudy TE, Glick RM, et al. Efficacy of percu-
taneous electrical nerve stimulation for the treatment
of chronic low back pain in older adults. J Am Geriatr Soc.
2003;51(5):599-608.
20. Weiner DK, Perera S, Rudy TE, Glick RM, Shenoy S,
Delitto A. Efficacy of percutaneous electrical nerve
stimulation and therapeutic exercise for older adults
with chronic low back pain: a randomized controlled
trial. Pain. 2008;140(2):344-357.
21. Deyo RA, Walsh NE, Martin DC, Schoenfeld LS, Rama-
murthy S. A controlled trial of transcutaneous electrical
nerve stimulation (TENS) and exercise for chronic low
back pain. N Engl J Med. 1990;322(23):1627-1634.
22. Jarzem PF, Harvey EJ, Arcaro N, Kaczorowski J. Trans-
cutaneous electrical nerve stimulation [TENS] for
short-term treatment of low back pain - Randomized
double blind crossover study of sham versus conven-
tional TENS. J Musculoskel Pain. 2005;13(2):11-17.
23. Marchand S, Charest J, Li J, Chenard JR, Lavignol-
le B, Laurencelle L. Is TENS purely a placebo effect?
A controlled study on chronic low back pain. Pain.
1993;54(1):99-106.
24. Thompson JW, Bower S, Tyrer SP. A double blind ran-
domised controlled clinical trial on the effect of trans-
cutaneous spinal electroanalgesia (TSE) on low back
pain. Eur J Pain. 2008;12(3):371-377.
25. Glazov G, Schattner P, Lopez D, Shandley K. Laser acu-
puncture for chronic non-specific low back pain: a con-
trolled clinical trial. Acupunct Med. 2009;27(3):94-100.
26. Glazov G, Yelland M, Emery J. Low-dose laser acupunc-
ture for non-specific chronic low back pain: a dou-
ble-blind randomised controlled trial. Acupunct Med.
2014;32(2):116-123.
27. Alayat MS, Atya AM, Ali MM, Shosha TM. Long-term
effect of high-intensity laser therapy in the treatment
of patients with chronic low back pain: a random-
ized blinded placebo-controlled trial. Lasers Med Sci.
2014;29(3):1065-1073.
28. Djavid GE, Mehrdad R, Ghasemi M, Hasan-Zadeh H, So-
toodeh-Manesh A, Pouryaghoub G. In chronic low back
pain, low level laser therapy combined with exercise is
more benecial than exercise alone in the long term: A
randomised trial. Aust J Physiother. 2007;53(3):155-160.
29. Borman P, Keskin D, Bodur H. The ecacy of lumbar
traction in the management of patients with low back
pain. Rheumatol Int. 2003;23(2):82-86.
30. Diab AA, Moustafa IM. The ecacy of lumbar extension
traction for sagittal alignment in mechanical low back
pain: a randomized trial. J Back Musculoskeletal Rehabil.
2013;26(2):213-220.
31. Schimmel JJ, de Kleuver M, Horsting PP, Spruit M, Ja-
cobs WC, van Limbeek J. No eect of traction in patients
with low back pain: a single centre, single blind, ran-
domized controlled trial of Intervertebral Dierential
Dynamics Therapy. Eur Spine J. 2009;18(12):1843-1850.
32. Gunn CC, Milbrandt WE, Little AS, Mason KE. Dry nee-
dling of muscle motor points for chronic low-back pain:
a randomized clinical trial with long-term follow-up.
Spine. 1980;5(3):279-291.
33. Carlsson CP, Sjolund BH. Acupuncture for chronic low
back pain: a randomized placebo-controlled study with
long-term follow-up. Clin J Pain. 2001;17(4):296-305.
34. Kerr DP, Walsh DM, Baxter D. Acupuncture in the man-
agement of chronic low back pain: a blinded random-
ized controlled trial. Clin J Pain. 2003;19(6):364-370.
35. Vas J, Aranda JM, Modesto M, et al. Acupuncture in
patients with acute low back pain: a multicentre ran-
domised controlled clinical trial. Pain. 2012;153(9):1883-
1889.
36. Cho YJ, Song YK, Cha YY, et al. Acupuncture for chronic
low back pain: a multicenter, randomized, patient-as-
sessor blind, sham-controlled clinical trial. Spine.
2013;38(7):549-557 549p.
37. Cherkin DC, Sherman KJ, Avins AL, et al. A randomized
trial comparing acupuncture, simulated acupuncture,
and usual care for chronic low back pain. Arch Intern
Med. 2009;169(9):858-866 859p.
38. Haake M, Muller HH, Schade-Brittinger C, et al. Ger-
man Acupuncture Trials (GERAC) for chronic low
back pain: randomized, multicenter, blinded, paral-
lel-group trial with 3 groups.[Erratum appears in Arch
Intern Med. 2007 Oct 22;167(19):2072]. Arch Intern Med.
2007;167(17):1892-1898.
39. Witt CM, Jena S, Selim D, et al. Pragmatic randomized
trial evaluating the clinical and economic eectiveness
of acupuncture for chronic low back pain. Am J Epidemi-
ol. 2006;164(5):487-496.
40. Yeung CK, Leung MC, Chow DH. The use of electro-acu-
puncture in conjunction with exercise for the treatment
of chronic low-back pain. J Altern Complement Med.
2003;9(4):479-490.
41. Yun M, Shao Y, Zhang Y, et al. Hegu Acupuncture for
Chronic Low-Back Pain: A Randomized Controlled Tri-
al. J Altern Complement Med. 2012;18(2):130-136.
42. Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L.
Comparison of supercial and deep acupuncture in
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
139
the treatment of lumbar myofascial pain: A dou-
ble-blind randomized controlled study. Clin J Pain.
2002;18(3):149-153.
43. Pach D, Yang-Strobel X, Ludtke R, et al. Standardized
versus individualized acupuncture for chronic low back
pain: A randomized controlled trial. Evid Based Comple-
ment Altern Med. 2013;2013 (no pagination)(125937).
44. Shin BC, Kong JC, Park TY, Yang CY, Kang KW, Choi SM.
Bee venom acupuncture for chronic low back pain: A
randomised, sham-controlled, triple-blind clinical tri-
al. Eur J Integ Med. 2012;4(3):e271-e280.
45. Calmels P, Queneau P, Hamonet C, et al. Eectiveness
of a lumbar belt in subacute low back pain: an open,
multicentric, and randomized clinical study. Spine.
2009;34(3):215-220.
46. Oleske DM, Lavender SA, Andersson GB, Kwasny MM.
Are back supports plus education more eective than
education alone in promoting recovery from low back
pain?: Results from a randomized clinical trial. Spine.
2007;32(19):2050-2057.
47. Doran DM, Newell DJ. Manipulation in treatment
of low back pain: a multicentre study. Br Med J.
1975;2(5964):161-164.
48. Dougherty PE, Karuza J, Dunn AS, Savino D, Katz P.
Spinal Manipulative Therapy for Chronic Lower Back
Pain in Older Veterans: A Prospective, Randomized,
Placebo-Controlled Trial. Geriatr Orthop Surg Rehabil.
2014;5(4):154-164.
49. Haas M, Vavrek D, Peterson D, Polissar N, Neradilek MB.
Dose-response and ecacy of spinal manipulation for
care of chronic low back pain: a randomized controlled
trial. Spine J. 2014;14(7):1106-1116.
50. Hancock MJ, Maher CG, Latimer J, et al. Assessment of
diclofenac or spinal manipulative therapy, or both, in
addition to recommended rst-line treatment for acute
low back pain: a randomised controlled trial. Lancet.
2007;370(9599):1638-1643.
51. Hoiriis KT, Peger B, McDue FC, et al. A random-
ized clinical trial comparing chiropractic adjustments
to muscle relaxants for subacute low back pain. J Manip
Physiol Therap. 2004;27(6):388-398.
52. Juni P, Battaglia M, Nuesch E, et al. A randomised con-
trolled trial of spinal manipulative therapy in acute low
back pain. Ann Rheum Dis. 2009;68(9):1420-1427.
53. Schneider M, Haas M, Glick R, Stevans J, Landsittel D.
Comparison of spinal manipulation methods and usu-
al medical care for acute and subacute low back pain: a
randomized clinical trial. Spine. 2015;40(4):209-217.
54. Senna MK, Machaly SA. Does maintained spinal ma-
nipulation therapy for chronic nonspecic low back
pain result in better long-term outcome? Spine.
2011;36(18):1427-1437.
55. von Heymann WJ, Schloemer P, Timm J, Muehlbauer
B. Spinal high-velocity low amplitude manipulation in
acute nonspecic low back pain: a double-blinded ran-
domized controlled trial in comparison with diclofenac
and placebo. Spine. 2013;38(7):540-548.
56. Grunnesjo MI, Bogefeldt JP, Blomberg SI, Strender LE,
Svardsudd KF. A randomized controlled trial of the ef-
fects of muscle stretching, manual therapy and steroid
injections in addition to ‘stay active’ care on health-re-
lated quality of life in acute or subacute low back pain.
Clin Rehabil. 2011;25(11):999-1010.
57. Licciardone JC, Stoll ST, Fulda KG, et al. Osteopathic
manipulative treatment for chronic low back pain: A
randomized controlled trial. Spine. 2003;28(13):1355-
1362.
58. Cambron JA, Gudavalli MR, Hedeker D, et al. One-
year follow-up of a randomized clinical trial com-
paring exion distraction with an exercise program
for chronic low-back pain. J Altern Complement Med.
2006;12(7):659-668.
59. Cecchi F, Molino-Lova R, Chiti M, et al. Spinal manipu-
lation compared with back school and with individually
delivered physiotherapy for the treatment of chronic
low back pain: a randomized trial with one-year fol-
low-up. Clin Rehabil. 2010;24(1):26-36.
60. Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A
comparison of physical therapy, chiropractic manipu-
lation, and provision of an educational booklet for the
treatment of patients with low back pain. N Engl J Med.
1998;339(15):1021-1029.
61. Enix DE, Sudkamp K, Malmstrom TK, Flaherty JH. A
randomized controlled trial of chiropractic compared to
physical therapy for chronic low back pain in commu-
nity swelling geriatric patients. Top Integr Health Care.
2015;6(1):1-17.
62. Hemmila HM, Keinanen-Kiukaanniemi SM, Levoska
S, Puska P. Long-term eectiveness of bone-setting,
light exercise therapy, and physiotherapy for prolonged
back pain: a randomized controlled trial. J Manipulative
Physiol Ther. 2002;25(2):99-104.
63. Hurwitz EL, Morgenstern H, Kominski GF, Yu F, Chiang
LM. A randomized trial of chiropractic and medical care
for patients with low back pain: Eighteen-month fol-
low-up outcomes from the UCLA low back pain study.
Spine. 2006;31(6):611-621.
64. Hsieh LLC, Kuo CH, Yen MF, Chen THH. A random-
ized controlled clinical trial for low back pain treat-
ed by acupressure and physical therapy. Prevent Med.
2004;39(1):168-176.
65. Hsieh LLC, Kuo CH, Lee LH, Yen AMF, Chien KL, Chen
THH. Treatment of low back pain by acupressure and
physical therapy: Randomised controlled trial. Br Med J.
2006;332(7543):696-698.
66. Kankaanpaa M, Taimela S, Airaksinen O, Hanninen O.
The ecacy of active rehabilitation in chronic low back
pain. Eect on pain intensity, self-experienced disabil-
ity and lumbar fatigability. Spine. 1999;24(10):1034-
1042.
67. Little P, Lewith G, Webley F, et al. Randomised con-
trolled trial of Alexander technique lessons, exercise,
and massage (ATEAM) for chronic and recurrent back
pain. Br Med J. 2008;337:a884.
68. Zhang Y, Tang S, Chen G, Liu Y. Chinese massage com-
bined with core stability exercises for nonspecic low
back pain: a randomized controlled trial. Complement
Ther Med. 2015;23(1):1-6.
69. Moussouli M, Vlachopoulos SP, Kofotolis ND, Theodor-
akis Y, Malliou P, Kellis E. Eects of stabilization ex-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
140
ercises on health-related quality of life in women with
chronic low back pain. J Phys Act Health. 2014;11(7):1295-
1303.
70. Lomond KV, Henry SM, Hitt JR, DeSarno MJ, Bunn JY.
Altered postural responses persist following physical
therapy of general versus specic trunk exercises in
people with low back pain. Manual Ther. 2014;19(5):425-
432.
71. Ganesh GS, Chhabra D, Pattnaik M, Mohanty P, Patel R,
Mrityunjay K. Eect of trunk muscles training using a
star excursion balance test grid on strength, endurance
and disability in persons with chronic low back pain. J
Back Musculoskel Rehabil. 2015;28(3):521-530.
72. Petersen T, Kryger P, Ekdahl C, Olsen S, Jacobsen S. The
eect of McKenzie therapy as compared with that of
intensive strengthening training for the treatment of
patients with subacute or chronic low back pain: A ran-
domized controlled trial. Spine. 2002;27(16):1702-1708.
73. Petersen T, Larsen K, Jacobsen S. One-year follow-up
comparison of the eectiveness of McKenzie treatment
and strengthening training for patients with chronic
low back pain: outcome and prognostic factors. Spine.
2007;32(26):2948-2956.
74. Garcia AN, Costa Lda C, da Silva TM, et al. Eectiveness
of back school versus McKenzie exercises in patients
with chronic nonspecic low back pain: a randomized
controlled trial. Phys Ther. 2013;93(6):729-747.
75. Aboagye E, Karlsson ML, Hagberg J, Jensen I. Cost-ef-
fectiveness of early interventions for non-specic low
back pain: a randomized controlled study investigating
medical yoga, exercise therapy and self-care advice. J
Rehabil Med. 2015;47(2):167-173.
76. Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chron-
ic low back pain: a randomized trial. Ann Intern Med.
2011;155(9):569-578.
77. Williams KA, Petronis J, Smith D, et al. Eect of Iyengar
yoga therapy for chronic low back pain. Pain. 2005;115(1-
2):107-117.
78. Williams K, Abildso C, Steinberg L, et al. Evaluation of
the eectiveness and ecacy of Iyengar yoga therapy
on chronic low back pain. Spine. 2009;34(19):2066-
2076.
79. Murtezani A, Hundozi H, Orovcanec N, Sllamniku S,
Osmani T. A comparison of high intensity aerobic exer-
cise and passive modalities for the treatment of workers
with chronic low back pain: a randomized, controlled
trial. Eur J Phys Rehabil Med. 2011;47(3):359-366.
80. Cuesta-Vargas AI, Adams N, Salazar JA, Belles A, Haz-
anas S, Arroyo-Morales M. Deep water running and
general practice in primary care for non-specic low
back pain versus general practice alone: randomized
controlled trial. Clin Rheumatol. 2012;31(7):1073-1078.
81. Chatzitheodorou D, Kabitsis C, Malliou P, Mougios V. A
pilot study of the eects of high-intensity aerobic ex-
ercise versus passive interventions on pain, disability,
psychological strain, and serum cortisol concentra-
tions in people with chronic low back pain. Phys Ther.
2007;87(3):304-312.
82. Tritilanunt T, Wajanavisit W. The ecacy of an aerobic
exercise and health education program for treatment of
chronic low back pain. Chotmaihet Thangphaet. 2001;84
Suppl 2:S528-533.
83. Bendix T, Bendix A, Labriola M, Haestrup C, Ebbehoj
N. Functional restoration versus outpatient physical
training in chronic low back pain: a randomized com-
parative study. Spine. 2000;25(19):2494-2500.
84. Sang LS, Eria LPY. Outcome evaluation of work hard-
ening program for manual workers with work-related
back injury. Work. 2005;25(4):297-305.
85. Casso G, Cachin C, Van Melle G, Gerster JC. Return-to-
work status 1 year after muscle reconditioning in chronic
low back pain patients. Joint Bone Spine. 2004;71(2):136-
139.
86. Beaudreuil J, Kone H, Lasbleiz S, et al. Ecacy of
a functional restoration program for chronic low
back pain: Prospective 1-year study. Joint Bone Spine.
2010;77(5):435-439.
87. Luk KD, Wan TW, Wong YW, et al. A multidisciplinary
rehabilitation programme for patients with chron-
ic low back pain: a prospective study. J Orthop Surg.
2010;18(2):131-138.
88. Roche G, Ponthieux A, Parot-Shinkel E, et al. Compari-
son of a functional restoration program with active in-
dividual physical therapy for patients with chronic low
back pain: a randomized controlled trial. Arch Phys Med
Rehabil. 2007;88(10):1229-1235.
89. Sivan M, Sell B, Sell P. The outcome of a functional res-
toration programme for chronic low back pain. Ir J Med
Sci. 2009;178(4):461-467.
90. van der Roer N, van Tulder M, Barendse J, Knol D, van
Mechelen W, de Vet H. Intensive group training pro-
tocol versus guideline physiotherapy for patients with
chronic low back pain: a randomised controlled trial.
Eur Spine J. 2008;17(9):1193-1200.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
141
QQ
PM&R Question 3. Are there specic patient or treatment characteristics that
predict improved duration of pain, intensity of pain, functional outcomes and
return-to-work status with SMT following an episode of low back pain?
Denition: SMT dened as spinal manipulative therapy, manual therapy, mobilization, and high
velocity thrusts
Recommendations:
There is conicting evidence that symptoms above the knee, low fear avoidance question-
naire score, at least one hypomobile segment, and greater than 35° of internal rotation of
the hip are predictive of responding to spinal manipulative therapy (SMT) for patients with
acute low back pain.
Grade of Recommendation: I
Flynn et al
1
prospectively studied a cohort of patients
with LBP in order to develop a clinical prediction rule
(CPR) to identify patients with LBP who are like-
ly to improve with spinal manipulation. Patients re-
ferred to physical therapy for LBP (n=71) underwent
an initial standardized examination and reported
pain (11-point scale), disability (Modied Oswestry
Disability Questionnaire) and beliefs about activity
(Fear-Avoidance Beliefs Questionnaire). A therapist
performed spinal manipulation on all patients during
an initial session. Participants reported disability and
attended a second treatment session 2-4 days af-
ter the initial session. If disability improvement was
>50%, the study participant was ended due to success
in treatment. If disability improvement was<50%, the
participant attended one nal treatment session after
2-4 days. Patients were also instructed to complete
pelvic tilt range of motion exercise and maintain usual
activity levels within pain limits. Statistical analyses
aimed to determine the association between individ-
ual variables from the initial examination and catego-
rization of successful treatment. Thirty-two patients
were classied as having successful treatment. A CPR
was developed using 5 variables: <16-day duration of
symptoms, at least one hip with >35° of internal rota-
tion, hypomobility with lumbar spring testing, FABQ
work subscale score <19 and no symptoms distal to
the knee. The authors concluded that patients with
LBP who are likely to respond to spinal manipulation
can be identied before treatment. This study oers
Level II prognostic evidence that, in patients with
LBP receiving SMT and exercise, the following clini-
cal predictors are associated with 50% improvement
for function within one week: symptoms less than 16
days, symptoms above the knee, low fear avoidance
questionnaire score, at least one hypomobile seg-
ment, greater than 35° of internal rotation of the hip;
presence of more predictors associated with increased
likelihood of responding to treatment.
Childs et al
2
aimed to validate the spinal manipulation
CPR developed by Flynn et al
1
in a multicenter ran-
domized controlled trial. Patients who were referred
to physical therapy for LBP were randomly assigned
to receive exercise alone (n=61) or exercise plus ma-
nipulation (n=70). All participants completed ques-
tionnaires to measure pain (11-point pain-rating
scale), Fear-Avoidance Beliefs Questionnaire (FABQ)
and Oswestry Disability Questionnaire (ODQ) and
were assessed by a physical therapist using the CPR.
To be considered positive on the CPR, patients had to
have at least 4 out of 5 of the following: duration of
current episode of LBP <16 days, no symptoms distal
to the knee, FABQ work subscale score <19 points, ≥1
hypomobile segment in the lumbar spine, ≥ one hip
with >35° of internal rotation range of motion. Par-
ticipants were invited for follow-up after one week, 4
weeks and 6 months. Patients who received manip-
ulation had greater improvements in disability and
pain than those who received exercise alone. The pa-
tients who were positive on the rule and received ma-
nipulation had greater improvement in disability and
pain at all follow-up points compared to patients who
were negative on the rule and received manipulation.
The authors concluded that the CPR could be used to
assist with decision-making in patients with LBP.
This study oers Level II prognostic evidence that,
in patients with LBP receiving SMT and exercise, the
following clinical predictors are associated with 50%
improvement for function within one week: symp-
toms less than 16 days, symptoms above the knee, low
fear avoidance questionnaire score, at least one hy-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
142
pomobile segment, greater than 35° of internal rota-
tion of the hip; presence of more predictors associated
with increased likelihood of responding to treatment.
Dougherty et al
3
conducted a randomized controlled
trial to evaluate a modied CPR for spinal manipula-
tive therapy (SMT) in patients with chronic LBP. Pa-
tients with chronic LBP were screened using a modi-
ed version of Flynn et al’s
1
CPR and were categorized
as positive or negative. They were then randomized to
receive SMT (n=92) or active exercise therapy (n=89)
twice weekly for 4 weeks. Active exercise therapy in-
cluded directional preference exercises, lumbar stabi-
lization, general exibility and specic training exer-
cises. To be considered positive on the modied CPR,
patients had to have at least 3 out of the following: pain
proximal to the knee, internal hip rotation of greater
than 35°, hypomobility of one or greater lumbar seg-
ments and FABQ work subscale score of less than 19.
Participants completed questionnaires at baseline
and after 5, 12 and 24 weeks which included pain in-
tensity (VAS), SF-36, disability (Oswestry Disability
Index), patient satisfaction and patient expectation.
Both groups experienced improvements in pain and
disability after treatment. There were no signicant
dierences in outcomes between therapy groups or
based on classication on the modied CPR. The au-
thors concluded that the modied CPR cannot be used
to determine which patients would benet more from
SMT. This study oers Level I prognostic evidence
that, in patients with chronic LBP receiving SMT, the
following clinical predictors are not associated with a
substantially dierent pain and functional outcome:
symptoms above the knee, low fear avoidance ques-
tionnaire score, at least one hypomobile segment and
greater than 35° of internal rotation of the hip.
Hancock et al
4
conducted a multicenter randomized
controlled trial in Sydney, Australia to investigate the
use of the CPR developed by Flynn et al
1
in patients with
LBP presenting to outpatient general practice clinics.
Patients who presented to a general practitioner with
LBP <6 weeks received usual care (reassurance, advice
to remain active and avoid bed rest and prescription
of paracetamol) and were randomized into one of four
treatment arms. Patients were randomized to receive
either diclofenac or placebo and further randomized
to receive SMT or placebo. Since neither SMT nor di-
clofenac were found to signicantly reduce time to
recovery from pain, both placebo SMT groups were
considered the control group and both active SMT
groups were considered the intervention group for the
purpose of this study. During initial evaluation, each
patient was classied using the CPR; at least 4 out of
5 criteria were necessary to be classied as positive.
The participants in the intervention group (n=120)
received up to 12 treatments of SMT over 4 weeks. The
participants in the intervention group (n=120) re-
ceived sham ultrasound for the same duration of time.
Pain (11-point scale) and disability (24-point Roland
Morris disability questionnaire) were recorded at 1, 2,
4 and 12 weeks. Patients who were classied as po-
sition on the CPR had greater improvements in pain
and disability regardless of treatment. There were no
signicant interaction eects in pain or disability be-
tween treatment groups and prediction rule classi-
cation. The authors concluded that the CPR validated
by Childs et al
2
was not generalizable to patients in
the primary care setting. This study provides Level II
prognostic evidence that, in patients with acute LBP
receiving SMT, the following clinical predictors were
not found to be associated with improvements for pain
and function: symptoms less than 16 days, symptoms
above the knee, low fear avoidance questionnaire
score, at least one hypomobile segment, greater than
35° of internal rotation of the hip; presence of more
predictors associated with increased likelihood of re-
sponding to treatment
Hallegrae et al
5
assessed the ecacy of manipula-
tive therapy in a multicenter randomized controlled
trial. Patients with acute nonspecic LBP who met
three factors of the CPR (duration of symptoms <16
days, no pain distal of the knee, age >35 years)
1
were
randomized into one of 2 treatment arms. The in-
tervention group (n=31) received 4 sessions of ma-
nipulative therapy along with physical therapy (low
intensity endurance exercises). The control group
(n=33) received physical therapy alone. Pain (VAS),
disability (Oswestry Disability Low Back Pain Ques-
tionnaire) and mobility (Sit-and-Reach Test) were
recorded at baseline and after 2.5 weeks of treatment.
The patients who received manipulation therapy had
a greater improvement in disability compared to the
control group, but there were no signicant dier-
ences in pain or mobility. The authors concluded that
although there were statistically signicant interac-
tion eects for disability and sex, these had low eect
size and there were no signicant eects for pain or
mobility. This study provides Level I prognostic evi-
dence that the addition of manipulative therapy added
benet over physical therapy alone for improving dis-
ability. However, it did not support that the two-factor
CPR was predictive of responders (predictive variables
include: duration of symptoms less than 16 days, no
pain distal to the knee and age greater than 35 years).

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
143
There is insucient evidence that hyper- or hypo-mobility, patient age, strains and sprains, in-
stability, severe aective distress, relationship with healthcare provider, use of thrust vs. non-
thrust techniques, pretreatment psychological or socioeconomic status, or number of visits are
predictive factors of response to spinal manipulative therapy (SMT).
Grade of Recommendation: I
Cook et al
6
aimed to evaluate the predictive value of
prognostic variables in outcomes in patients with
LBP in a secondary analysis of a multicenter random-
ized controlled trial (RCT). All participants received
manual therapy for 2 visits, either thrust (n=76) or
non-thrust (n=73). The results of the RCT found no
dierences between thrust or nonthrust techniques.
Outcome measures included disability per the Os-
westry Disability Index (ODI), Numeric Pain Rating
Scale (NPRS), total visits and report of rate of re-
covery. Predictive values included body mass index
(BMI), NPRS at baseline, ODI at baseline, Fear-Avoid-
ance Beliefs Questionnaire (FABQ) work subscale at
baseline, CPR for spinal manipulation (presence of at
least 4 of the following: no pain below knee, symp-
tom duration <16 days, FABQ-W score <19, 1+ hips
with internal rotation range of motion >35° and 1+
hypomobile lumbar segment), duration of symptoms
(weeks), age, irritability, diagnosis and allocation to
thrust versus nonthrust technique. Logistic and linear
regression modeling were used to create predictive
models and nd signicant explanatory power for
the outcome variables. A positive CPR at baseline was
present in all 4 models. The authors concluded that
the CPR was prognostic for all outcome measures.
This study oers Level II prognostic evidence that,
in preselected patients with LBP, CPR is a predictor
of success for treatment with SMT; factors included
meeting the CPR, age, strains and sprains, instability,
irritability, ODI score on rst visit, duration of symp-
toms and met numerical pain rating scale score on
rst visit.
In a retrospective analysis of data from a random-
ized controlled trial, Cecchi et al
7
aimed to identify
predictors of response to various interventions for
chronic LBP. Patients with chronic LBP were random-
ly assigned to receive back school (n=68), individual
physiotherapy (n=68) or spinal manipulation (n=69).
Participants were classied as nonresponders to ther-
apy if their changes in Roland Morris Disability score
improved by less than <2.5 after treatment. Poten-
tial predictors of response, including demographics,
baseline disability and pain intensity and life satis-
faction, were analyzed using multivariable backward
logistic regression to predict the probability of non-
response to treatment. The authors concluded that a
lower baseline Roland Morris Disability score predict-
ed nonresponse for physiotherapy, but not for spinal
manipulation. This study provides Level II prognostic
evidence that there are no predictive factors for suc-
cess with SMT.
Cook et al
8
analyzed data from a multicenter ran-
domized clinical trial to determine if changes in pain
during or between sessions of manual therapy were
associated with outcomes in patients treated for LBP.
Participants (n=100) had been randomized to receive
thrust or nonthrust manipulation, along with a home
exercise program. Patients reported pain (Numeri-
cal Pain Rating Scale), disability (Oswestry Disability
Questionnaire) and rate of recovery (0-100%) at base-
line, after two sessions and at discharge. Functional
recovery was dened as ≥50% reduction in Oswestry
Disability Index (ODI). The authors concluded that a
change of ≥2 points on the 11-point scale is associat-
ed with functional recovery at discharge. This study
oers Level II prognostic evidence that, in preselect-
ed patients with LBP treated with SMT, a 2-point re-
duction in pain score after the second visit predicts a
higher likelihood of functional improvement.
In a secondary analysis of data from a prospective,
multicenter, randomized controlled trial (RCT), Don-
aldson et al
9
studied outcomes in patients with LBP
who were matched, unmatched, or indierent to their
preference of thrust versus nonthrust manual thera-
py intervention. Prior to randomization, patients in-
dicated their preference of an exercise program plus
two sessions of either thrust or nonthrust manual
therapy. As part of the RCT, 77 participants were al-
located to thrust manipulation and 77 participants
were allocated to nonthrust manipulation. Outcomes
of disability (Oswestry Disability Index), pain per-
ception (11-point Numerical Pain Rating Scale), care
intensity, fear-avoidance behaviors (FABQ) and per-
ception of extent of recovery were measured. There
were no statistically signicant dierences in any
of the outcomes between patient preference groups.
The authors concluded that there were no statistical
dierences in disability or pain in patients who were
matched, unmatched, or indierent to their assigned
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
144
intervention. This study provides Level II prognostic
evidence that, in patients with LBP, patient prefer-
ence for specic manipulation technique did not af-
fect outcomes.
Fritz et al
10
investigated the value of posterior-anterior
mobility testing for predicting disability outcomes
in patients with LBP in a randomized controlled
trial. Participants underwent an initial assessment
with posterior-anterior mobility testing and were
classied as presence or absence of hypomobility
and hypermobility. Participants were randomized to
receive an intervention of manipulation (n=70) or
stabilization exercise (n=61) for 4 weeks. Disability
(Oswestry Disability Questionnaire) was recorded
upon study enrollment and after the 4-week
treatment. Three-way repeated measures analyses of
variance were performed to assess interaction eects
of mobility categorization and intervention on change
in disability. The authors concluded that patients
with LBP and hypomobility had better outcomes with
manipulation while those with hypermobility were
more likely to benet from stabilization exercise. This
study oers Level I prognostic evidence that patients
with hypomobility had better functional outcomes
when receiving SMT and those with hypermobility had
better functional outcomes when receiving exercise.
Haas et al
11
conducted a randomized controlled trial to
evaluate the eect of number of spinal manipulation
treatment visits with or without physical modalities
on pain and disability outcomes in patients with LBP.
Patients were randomized to a treatment interven-
tion of spinal manipulation only or spinal manipula-
tion plus physical modalities (soft tissue therapy, hot
packs, electrotherapy, or ultrasound). Patients were
randomly assigned number of visits per week (1, 2, 3,
or 4) for 3 weeks. Pain intensity and disability (Mod-
ied Von Kor Scales) were recorded. There were no
signicant eects of treatment intervention type.
There were signicant eects of number of treatment
sessions per week (3-4 sessions per week) on pain and
disability at 4 weeks. The authors concluded that relief
was substantial for patients receiving 3 to 4 sessions
per week for 3 weeks. This study oers Level II prog-
nostic evidence that, in patients with LBP who receive
SMT, the optimal number of treatments is 3 to 4 times
a week for 3 weeks.
Hoehler et al
12
investigated the predictive value of a
modied Minnesota Multiphasic Personality Inven-
tory (MMPI) for response to spinal manipulation in
patients with acute or chronic LBP. Patients referred
for spinal manipulative therapy (n=90) complet-
ed questionnaires and a modied version of MMPI.
They reported improvement in pain immediately af-
ter treatment and again several days later (reported as
much better, somewhat better, no change, somewhat
worse or much worse). Other variables such as age,
sex and duration of pain were also included in analy-
sis to study predictive value. Immediately after treat-
ment, there were no signicant correlations between
psychological measures and extent of relief. Several
days after treatment, the percentage of patients re-
porting improvement was lower; lack of improvement
was associated with hypochondriasis, hysteria and
functional LBP. The authors concluded that underly-
ing psychosomatic factors may predispose the condi-
tion to recur. This study provides Level III prognostic
evidence that MMPI scores indicating hysteria, hypo-
chondriasis or higher LBP scores are associated with
recurrence of pain after manipulation and not associ-
ated with immediate response to SMT.
In an analysis of data from a randomized controlled
trial, Niemisto et al
13
investigated the predictive value
of sociodemographic data for response to treatment
for chronic (>3 months) LBP. Patients were random-
ized to receive spinal manipulation therapy (SMT),
exercise and physician consultation (n=102) or phy-
sician consultation only (n=102). Questionnaires were
completed to record potential risk factors such as so-
ciodemographics, characteristics of LBP, disability,
quality of life, work ability, psychological variables
(Modied Somatic Perception Questionnaire) and
physical activity at work. Patients were clustered into
groups based on improvement in pain intensity (VAS)
and disability (Oswestry Questionnaire) at one-year
follow-up. Results indicated that severe aective dis-
tress was a risk factor for poor response to SMT. Risk
factors for poor response to the physician consulta-
tion approach included >25-day sick leave during
the previous year, poor life control and generalized
somatic symptoms. The authors concluded that psy-
chosocial dierences are important determinants for
treatment outcomes. This study oers Level II prog-
nostic evidence that, in patients with LBP, severe af-
fective distress is associated with a poor response to
treatment outcome with SMT.
Underwood et al
14
conducted an analysis of the UK
Back Pain Exercise And Manipulation (UK BEAM) Tri-
al to identify characteristics predictive of response
to treatment of LBP. The UK BEAM Trial (n=1334)
found that compared treatment packages of spinal
manipulation (up to 8 sessions over 12 weeks), ma-
nipulation plus exercise (6 weeks manipulation and 6
weeks of exercise) and exercise alone (9 group class-
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
145
es over 12 weeks) against usual care, including The
Back Book. Disability (Roland Morris Disability Ques-
tionnaire), back pain beliefs (Fear Avoidance Beliefs
Questionnaire), psychological state (Distress and
Risk Assessment Method), treatment expectations
and other demographic characteristics were obtained
before randomization and at 3-month and one-year
follow-up. None of the studied baseline characteris-
tics predicted response (disability per Roland Morris
Disability Questionnaire) to treatment. The authors
concluded that there were no characteristics that pre-
dicted response to the UK BEAM treatment packages.
This study oers Level II prognostic evidence that, in
patients with subacute LBP receiving SMT, there were
no predictors (including pain duration) for response
to treatment.
Future Directions for Research
1. There has been a lot of work done to look at the CPR for response to acute LBP
developed by Flynn et al
1
, with conicting results. It is possible that a large ran-
domized controlled trial with specic attention to subgroups may identify cer-
tain populations that are responders, as there have been conicting outcomes
to date.
2. There is very little work done for clinical predictors in chronic LBP. In addition,
there have been several well conducted studies looking at response to thrust
versus nonthrust, mobility versus stability, socioeconomic and psychological fac-
tors and number of visits. Repeated high quality studies looking at these ques-
tions could be useful for generating higher levels of recommendations either for
or against.
References
1. Flynn T, Fritz J, Whitman J, et al. A clinical prediction
rule for classifying patients with low back pain who
demonstrate short-term improvement with spinal ma-
nipulation. Spine. 2002;27(24):2835-2843.
2. Childs JD, Fritz JM, Flynn TW, et al. A clinical predic-
tion rule to identify patients with low back pain most
likely to benet from spinal manipulation: a validation
study.[Summary for patients in Ann Intern Med. 2004
Dec 21;141(12):I39; PMID: 15611484]. Ann Intern Med.
2004;141(12):920-928.
3. Dougherty PE, Karuza J, Savino D, Katz P. Evaluation
of a modied clinical prediction rule for use with spi-
nal manipulative therapy in patients with chronic low
back pain: A randomized clinical trial. Chiro Man Therap.
2014;22 (1) (no pagination).
4. Hancock MJ, Maher CG, Latimer J, Herbert RD, McAuley
JH. Independent evaluation of a clinical prediction rule
for spinal manipulative therapy: a randomised con-
trolled trial. Eur Spine J. 2008;17(7):936-943 938p.
5. Hallegrae JM, de Greef M, Winters JC, Lucas C. Manip-
ulative therapy and clinical prediction criteria in treat-
ment of acute nonspecic low back pain. Percept Mot
Skills. 2009;108(1): 196-208.
6. Cook CE, Learman KE, O’Halloran BJ, et al. Which prog-
nostic factors for low back pain are generic predictors of
outcome across a range of recovery domains? Phys Ther.
2013;93(1): 32-40.
7. Cecchi F, Negrini S, Pasquini G, et al. Predictors of
functional outcome in patients with chronic low back
pain undergoing back school, individual physiother-
apy or spinal manipulation. Eur J Phys Rehabil Med.
2012;48(3):371-378.
8. Cook CE, Showalter C, Kabbaz V, O’Halloran B. Can a
within/between-session change in pain during reas-
sessment predict outcome using a manual therapy in-
tervention in patients with mechanical low back pain?
Man Ther. 2012;17(4):325-329.
9. Donaldson M, Learman K, O’Halloran B, Showalter C,
Cook C. The role of patients’ expectation of appropri-
ate initial manual therapy treatment in outcomes for
patients with low back pain. J Manipulative Physiol Ther.
2013;36(5):276-283.
10. Fritz JM, Whitman JM, Childs JD. Lumbar spine seg-
mental mobility assessment: an examination of validity
for determining intervention strategies in patients with
low back pain. Arch Phys Med Rehabil. 2005;86(9):1745-
1752.
11. Haas M, Kraemer DF. Dose-response for chiropractic
care of chronic low back pain. Spine J. 2004;4(5):574-
583.
12. Hoehler FK, Tobis JS. Psychological factors in the treat-
ment of back pain by spinal manipulation. Br J Rheuma-
tol. 1983;22(4):206-212.
13. Niemisto L, Sarna S, Lahtinen-Suopanki T, Lindgren
KA, Hurri H. Predictive factors for 1-year outcome of
chronic low back pain following manipulation, stabiliz-
ing exercises, and physician consultation or physician
consultation alone. J Rehabil Med. 2004;36(3):104-109.
14. Underwood MR, Morton V, Farrin A, Team UBT. Do
baseline characteristics predict response to treat-
ment for low back pain? Secondary analysis of the
UK BEAM dataset [ISRCTN32683578]. Rheumatology.
2007;46(8):1297-1302.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
146
QQ
PM&R Question 4. In patients undergoing treatment for low back pain, what are
outcomes, including duration of pain, intensity of pain, functional outcomes and
return-to-work status, for exercise therapy alone versus exercise with cognitive
behavioral therapy (CBT)?
Recommendation:
There is conicting evidence that addition of cognitive behavioral therapy (CBT) to an exer-
cise program results in signicant improvement in pain and function compared to exercise
alone in patients with chronic low back pain.
Grade of Recommendation: I
Steenstra et al
1
conducted a randomized controlled
trial to assess the eectiveness of graded activity as
part of a return-to-work (RTW) program for patients
with LBP. Patients enrolled in a multistage RTW
program who were absent from work greater than 8
weeks due to LBP were randomized to receive graded
activity (n=55) or usual care treatment according
to Dutch occupational physician guidelines for LBP
(n=57). All these patients were treated initially from
2 to 6 weeks following injury in a pain management
program and failed. The graded activity used an
operant-conditioning behavioral approach in 2 one-
hour sessions per week for a maximum of 26 sessions
and ended when the participant fully returned to
work. Outcome measures included severity of pain,
functional status, total number of days on sick leave
during follow-up and the number of days o work
until rst RTW for more than 28 days. Graded activity
prolonged RTW and did not improve pain or functional
status. The authors concluded that graded activity was
not eective for any of the outcome measures. This
study oers Level I evidence that, in patients with
LBP, graded activity is not eective for improving
return to work, disability, or pain compared to usual
care according to Dutch guideline care.
Lindstrom et al
2
studied the eectiveness of graded
activity to restore occupational function in patients
with LBP. Blue-collar workers with subacute,
nonspecic, mechanical LBP, absent from work
for at least 8 weeks due to LBP were randomized
to the graded activity group (n=51) or control
group (n=52). The graded activity program used an
operant-conditional behavioral approach based on
measurements of functional capacity and a work-
place visit while the control group continued to be
traditionally treated by their regular physicians. The
patients in the graded activity group returned to
work signicantly earlier than those in the control
group. The authors concluded that the patients with
subacute, nonspecic, mechanical LBP in the graded
activity group had faster restoration of occupational
function and reduced long-term sick leave compared
to those who received traditional care. This study
provides Level I therapeutic evidence that, in patients
with subacute LBP, a graded activity program is
associated with decreased health care utilization,
increased return to work and decreased sick leave at 2
years as compared to usual care.
Johnson et al
3
conducted a multicenter randomized
controlled trial to study the eect of a group exercise and
education program on pain and disability in patients
with persistent LBP, as well as its cost-eectiveness
and whether patient preference inuences outcomes.
Patients who had LBP persisting 3 months after initial
consultation to one of 9 family medical practices in the
United Kingdom were randomized into an intervention
or control group. The control group (n=118) received
an educational booklet and audio-cassette along with
usual care. The intervention group (n=116), in addition
to the same resources as the control group, received
8 2-hour group sessions over 6 weeks that included
exercise and education from a physiotherapist using
a cognitive behavioral therapy (CBT) approach. All
participants were sent a questionnaire that measured
pain severity (100-mm VAS), disability (Roland-
Morris Disability Questionnaire) and general health
(EQ-5D) at 3, 9 and 15 months postrandomization and
at 6 and 12 months post-treatment. Twelve months
post-treatment, 196 subjects (84%) completed
follow-up. Both groups had signicant improvements
in pain and disability, but there were no signicant
dierences between groups. The incremental cost-
eectiveness ratio was $8,650 per quality adjusted
life year. Patients in the intervention group who had
expressed a preference for the intervention before
randomization had signicant improvements in pain

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
147
and disability compared to those in the intervention
group who had initially expressed a preference for
the control group. The authors concluded that the
intervention with exercise and education with CBT
had only a small eect in reducing LBP and disability
over a one-year period. However, they recommended
further investigation regarding the impact of patient
preference for treatment on outcomes. This study
oers Level I therapeutic evidence that, in patients
with LBP, addition of group-exercise-based CBT
produces no meaningful improvement at 15 months
compared to educational pack alone unless patients
had preference for treatment.
In a parallel-group, randomized, superiority
controlled study, Monticone et al
4
investigated the
eect of a CBT-based multidisciplinary intervention
program targeted against fear-avoidance beliefs
in patients with chronic (>3 months) LBP. Patients
referred to a specialized rehabilitation institute in
Italy for chronic LBP were randomized to receive
the intervention treatment with exercise or exercise
alone. Both groups participated in 2 60-minute
exercise sessions per week for 5 weeks and were
encouraged to continue home exercise twice weekly
for a year. The intervention group (n=45) additionally
received a 60-minute CBT session each week for 5
weeks plus a 60-minute session with a psychologist
once per month for a year. The control group (n=45)
did not receive any resources in addition to the
exercise program alone. Participants were asked to
complete questionnaires pretreatment, immediately
post-treatment and 12- and 24-months post-
treatment that measured disability (Roland-Morris
Disability Questionnaire), fear-avoidance behaviors
(Tampa Scale for Kinesiophobia), pain (numerical
rating scale) and the Short-Form Health Survey.
All participants completed the follow-up. Results
revealed signicant improvements in all outcomes
in the intervention group while the control group
experienced no signicant changes. The authors
concluded that the multidisciplinary program was
superior to the exercise program in reducing disability,
fear-avoidance beliefs and pain and enhancing the
quality of life of patients with chronic LBP for at least
one year after the conclusion of the intervention. This
study oers Level I therapeutic evidence that CBT
via a psychologist with exercise results in signicant
improvement in pain, function and fear-avoidance
behaviors at one year versus exercise alone.
Vibe Fersum et al
5
aimed to compare the eect of
classication-based cognitive functional therapy
versus traditional manual therapy and exercise on
pain and disability outcomes in patients with LBP.
Participating patients with chronic LBP (>3 months)
in outpatient practices in a Norwegian university
town were randomized into an intervention group or
control group. The participants in the intervention
group (n=62) received 12 weeks of individualized
sessions that included a cognitive component, specic
movement exercises to normalize maladaptive
movement behaviors identied, integration of
daily functional activities that the patient had
been avoiding and a physical activity program. The
participants in the control group (n=59) underwent
joint mobilization or manipulation per best current
practice and were instructed to complete general
exercises or motor control exercises at home. Follow-
up questionnaires included perceived function
(Oswestry Disability Index), pain (Pain Intensity
Numerical Rating Scale), anxiety and depression
(Hopkins Symptoms Checklist), fear-avoidance
beliefs (Fear-Avoidance Beliefs Questionnaire), total
lumbar spine range of motion, patient satisfaction,
sick-leave days and care-seeking. A total of 51 and
43 participants completed follow-up assessments in
the intervention and control groups, respectively. The
patients in the intervention group had clinically- and
statistically-signicantly greater improvements in
disability and pain intensity compared to the control
group. The authors concluded that the classication-
based cognitive functional therapy resulted in superior
outcomes compared to traditional manual therapy
and exercise in patients with chronic LBP. In critique,
less than 80% of study patients completed follow-up.
Due to this reason, the work group downgraded the
level of evidence for this study. This potential Level
I study provides Level II therapeutic evidence that
physical therapy based cognitive functional therapy
provides improvements in pain, function and fear-
avoidance behaviors at 1 year compared to standard
physical therapy.
Friedrich et al
6
conducted a randomized controlled
trial to investigate the long-term eect of a com-
bined exercise and motivation program versus ex-
ercise alone on disability outcomes in patients with
chronic (>4 months) LBP in Austria. All participants
completed a questionnaire at baseline to measure dis-
ability (13-item questionnaire by Greenough and Fra-
ser), pain intensity (101-point numerical rating scale)
and working ability. The participants randomized
to the control group (n=49) were prescribed ten 25-
min exercise sessions with follow-up assessments
at 3.5 weeks (73.5%), 4 months (83.7%), 12 months
(71.4%) and 5 years (61.2%). In addition to the same
exercise prescription, the participants randomized
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
148
to the intervention group (n=44) also received ex-
tensive counseling, reinforcement techniques from
the therapist and encouragement to post a treatment
contract and complete an exercise diary. The inter-
vention group had follow-up at 3.5 weeks (86.4%),
4 months (97.7%), 12 months (77.3%) and 5 years
(59.1%). Disability scores improved in both groups
at all follow-up points, but the cumulative eect in
the intervention group was more than twice than the
control group. The patients in the intervention group
experienced a steady decrease in pain intensity from
baseline to 5-year follow-up while the control group
only had a decrease in pain intensity from baseline
to 4-month follow-up. The authors concluded that
the combined exercise and motivation program was
superior to exercise alone. In critique, follow-up of
less than 80% was a factor in downgrading the lev-
el of evidence for this study from Level I to Level II.
This study provides Level II therapeutic evidence that
the addition of a motivational program to an exercise
program provides improvements in pain and working
ability at one year compared to exercise alone.
Monticone et al
7
investigated the eect of a multidis-
ciplinary rehabilitation program compared to usu-
al care on outcomes in patients with chronic LBP in
a randomized controlled pilot study. Patients with
chronic LBP (>3 months) were randomly assigned to
the intervention group or a control group to receive
usual care. The control group (n=10) participated
in rehabilitation with passive spinal mobilization,
stretching, muscle strengthening and postural con-
trol. The participants in the intervention group (n=10)
participated in a multidisciplinary program includ-
ing spinal stabilizing exercises and CBT in addition
to usual care. Participants completed a questionnaire
to measure disability (Oswestry Disability Index), ki-
nesiophobia (Tampa Scale for Kinesiophobia), cata-
strophizing (Pain Catastrophizing Scale), pain (Pain
Numerical Rating Scale) and quality of life (Short-
Form Health Survey) at baseline, immediately after
the 8-week trial and 3-months post-treatment. The
authors concluded that the multidisciplinary program
with CBT and exercise was superior to exercise alone
in reducing disability, kinesiophobia, catastrophizing
and enhancing quality of life in patients with chron-
ic LBP. Due to the small sample size, the work group
downgraded this potential Level I study. This study
provides Level II evidence that CBT plus stabilization
exercise plus usual care is better than usual care alone
at 3 months’ follow-up for patients with chronic LBP.
Sahin et al
8
conducted a randomized controlled trial
to compare outcomes in patients with chronic LBP
who participated in a program with exercise, physi-
cal therapy and back school (n=75) compared to ex-
ercise and physical therapy alone (n=75). The back
school program, taught by a physiatrist, included
education on the function of the back, life skills and
discussion of problems and problem-solving skills.
All participants completed questionnaires to measure
pain (VAS) and functional status (Oswestry Low Back
Pain Disability Questionnaire) at baseline, immedi-
ately after the 2-week trial and 3 months after treat-
ment. Both groups experienced improvements in pain
and functional status immediately after treatment.
At 3-month follow-up, the participants who partic-
ipated in back school had signicantly greater im-
provements in pain and functional status compared to
those who participants in exercise and physical thera-
py alone. The authors concluded that, in patients with
chronic LBP, the addition of back school was more
eective than exercise and physical treatment alone.
This study provides Level I evidence that, in patients
with chronic LBP, pain and disability scores improved
for both PT plus exercise group as well as PT plus ex-
ercise combined with CBT. At 3-month follow-up, the
addition of CBT resulted in statistically signicant but
not clinically signicant improvement compared to
the group without CBT.
Future Directions for Research
There were several high-quality studies with heterogeneity across outcome
measures, cohorts of patients and types of interventions. It is clear that in some
cases, CBT oered a distinct benet. Future research will need to focus on de-
tails of comparative eectiveness study design to identify the specic variables
that contribute to success.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
149
References
1. Steenstra IA, Anema JR, Bongers PM, de Vet HCW, Knol
DL, van Mechelen W. The eectiveness of graded activ-
ity for low back pain in occupational healthcare. Occup
Environ Med. 2006;63(11):718-725.
2. Lindstrom I, Ohlund C, Eek C, et al. The eect of grad-
ed activity on patients with subacute low back pain: a
randomized prospective clinical study with an op-
erant-conditioning behavioral approach. Phys Ther.
1992;72(4):279-290; discussion 291-273.
3. Johnson RE, Jones GT, Wiles NJ, et al. Active exercise,
education, and cognitive behavioral therapy for per-
sistent disabling low back pain: a randomized con-
trolled trial. Spine. 2007;32(15):1578-1585.
4. Monticone M, Ferrante S, Rocca B, Baiardi P, Farra FD,
Foti C. Eect of a long-lasting multidisciplinary pro-
gram on disability and fear-avoidance behaviors in pa-
tients with chronic low back pain: results of a random-
ized controlled trial. Clin J Pain. 2013;29(11):929-938.
5. Vibe Fersum K, O’Sullivan P, Skouen JS, Smith A, Kvale
A. Ecacy of classication-based cognitive function-
al therapy in patients with non-specic chronic low
back pain: A randomized controlled trial. Eur J Pain.
2013;17(6):916-928.
6. Friedrich M, Gittler G, Arendasy M, Friedrich KM.
Long-term eect of a combined exercise and motiva-
tional program on the level of disability of patients with
chronic low back pain. Spine 2005;30, 995-1000.
7. Monticone M, Ambrosini E, Rocca B, Magni S, Brivio
F, Ferrante S. A multidisciplinary rehabilitation pro-
gramme improves disability, kinesiophobia and walk-
ing ability in subjects with chronic low back pain: re-
sults of a randomised controlled pilot study. Eur Spine J.
2014;23(10):2105-2113.
8. Sahin N, Albayrak I, Durmus B, Ugurlu H. Eectiveness
of back school for treatment of pain and functional dis-
ability in patients with chronic low back pain: a ran-
domized controlled trial. J Rehabil Med. 2011;43(3):224-
229.
QQ
PM&R Question 5. In patients undergoing treatment for low back pain, what are
outcomes, including duration of pain, intensity of pain, functional outcomes and
return-to-work status, for a lumbar stabilization exercise program versus a general
tness program?
Denition: Lumbar stabilization exercises are focused on facilitating and strengthening specic mus-
cles that directly or indirectly control spinal joint function, especially the abdominal, gluteal and spinal
extensor muscle groups. General tness programs are not focused on specic muscle groups; by de-
nition the goal is to improve the overall general tness of the patient by using a combination of aerobic
conditioning with stretching/strengthening of all major muscle groups.
Recommendation:
It is suggested that a specic stabilization exercise program is equivalent to a general exercise
program.
Grade of Recommendation: B
Aluko et al
1
conducted a preliminary randomized con-
trolled trial to compare outcomes in patients with LBP
completing regular trunk exercises with or without
additional core stability exercises. Thirty-three pa-
tients with LBP for ≤6 weeks were randomized to re-
ceive regular core stability exercises (n=17) or regular
exercise plus 8 specic stabilization exercises (n=16)
for 6 weeks. Trunk sagittal acceleration (Lumbar Mo-
tion Monitor), pain (pain VAS) and disability (Roland
Morris Disability Questionnaire) were measured at
baseline, 3 weeks, 6 weeks and 3 months. Outcomes
improved in both groups, but there were no statis-
tical dierences between groups. The authors con-
cluded that the addition of specic core stability ex-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
150
ercises does not provide additional benets for acute
LBP compared with exercise alone at short-term fol-
low-up. Due to the small sample size, the work group
downgraded this study. This potential Level I study
oers Level II therapeutic evidence that, compared to
general exercise program, stabilization adds no bene-
t in terms of pain or disability.
Koumantakis et al
2
compared outcomes in patients
with subacute or chronic back pain after completing
an exercise program with versus without addition-
al stabilization exercises in a randomized controlled
trial. Patients with recurrent nonspecic back pain
were randomized into an exercise-only group (n=26)
or stabilization-enhanced exercise group (n=29). All
participants received The Back Book along with twice
weekly 45-60 minute sessions and encouraged to re-
peat the assigned exercises at home for 30 minutes 3
times per week. Outcomes of pain (Short-Form Mc-
Gill Pain Questionnaire), disability (Roland-Morris
Disability Questionnaire) and cognitive status (Pain
Self-Ecacy Questionnaire, Tampa Scale of Kinesi-
ophobia, Pain Locus of Control Scale) were record-
ed at baseline, immediately after intervention and
3-months after intervention. All outcomes improved
with times in both groups. Disability improved sig-
nicantly more in the general exercise group com-
pared to the stabilization-enhanced group. Otherwise,
there were no statistically signicant dierences in
outcomes between groups. The authors conclud-
ed that the addition of stabilization exercises do not
appear to provide additional benet to patients with
subacute or chronic LBP without spinal instability. In
critique, the sample size is small and less than 80%
of patients completed follow-up. In addition these
are a mixture of subacute and chronic patients that
are not subgrouped and the distribution across inter-
ventions is uncertain. Due to these reasons, the work
group downgraded the study from Level I to Level II.
This study provides Level II therapeutic evidence that
a general exercise and stabilization program results
in similar pain relief and functional improvement in
patients with low baseline disability.
Unsgaard-Tondel et al
3
compared outcomes of motor
control exercises, sling exercises and general exercis-
es for the treatment of LBP in a randomized controlled
trial. Patients with chronic nonspecic LBP (n=109)
were randomized to one of 3 intervention groups:
low-load ultrasound-guided motor control exercises
(n=36), high-load sling exercises (n=36), or general
exercises (n=37). All participants received an educa-
tional booklet on LBP, were encouraged to stay active
in their daily lives and participated in their assigned
therapy once a week for 8 weeks. Outcomes included
pain (Numeric Pain Rating Scale), self-reported ac-
tivity limitation (Oswestry Disability Index), function
(Fingertip-to-Floor Test) and fear-avoidance beliefs
and were recorded at baseline, after treatment and at
one-year follow-up. There were no signicant dif-
ferences in outcomes between groups. The authors
concluded that there is no evidence of benets of the
studied motor control exercises or sling exercises
compared to general exercises for chronic LBP. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to the small sample
size without power analysis and overall mild disability
at baseline. This study provides Level II evidence that
Pilates as a form of stabilization exercise are equal to
general exercise program for patients with chronic
LBP and relatively low-level baseline disability.
Mostagi et al
4
aimed to compare pain and function-
ality outcomes of Pilates versus general exercise in
patients with chronic LBP in a randomized controlled
trial. Patients with non-specic chronic LBP were
randomized to participate in Pilates (n=11) or gener-
al exercise (n=11) twice weekly for 8 weeks. Outcome
measures of pain (VAS), functionality (Quebec Back
Pain Questionnaire) and exibility (kinematic anal-
ysis measuring the hip joint angle) were measured
at baseline, immediately after treatment and after
three-month follow-up. Follow-up rate was 91%;
77% of patients were included in analysis. The par-
ticipants in the general exercise group had improved
functionality at both follow-up time points com-
pared to baseline. There were no signicant pain or
functionality dierences between groups otherwise.
The authors concluded that there were no dierences
in pain and functionality after patients with chronic
LBP completed general exercise versus Pilates, but
the subjects in the Pilates group had increased func-
tionality and exibility. The work group downgraded
this study due to small sample size and less than 80%
follow-up. This study provides Level II evidence that
Pilates is equivalent to general exercise program for
patients with chronic LBP.
Rasmussen-Barr et al
5
tested the hypothesis that
stabilizing treatment has more long-term eective-
ness than manual treatment for patients with LBP in
a randomized trial. Patients with LBP greater than 6
weeks were randomized to receive 6 weeks of either
stabilizing training (n=22) or manual therapy (n=20).
Stabilizing training consisted of training on how to
activate and control deep abdominal and lumbar mul-
tidus muscles. Manual therapy included a combina-
tion of muscle stretching, traction, soft tissue mobili-

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
151
zation and mobilization of thoracic and upper lumbar
segments if needed. Pain (VAS), general health (VAS),
functional disability (Oswestry Low-Back Pain Ques-
tionnaire) and perceived diculty (Disability Rating
Index) were measured at baseline (n=42), after treat-
ment (n=41) and at 3-month follow-up (n=33) and
12-month follow-up (n=31). Pain and disability im-
proved in both groups. While there was a small dier-
ence favoring stabilization, this was not clinically sig-
nicant. In critique, this study had a small sample size
and less than 80% follow-up. Due to these reasons,
the work group downgraded this study. This potential
Level I study provides Level II therapeutic evidence
that, in patients with subacute and chronic LBP, SMT
and stabilization exercise provide similar improve-
ments in pain and function at one year.
Future Directions for Research
There were several high quality studies with heterogeneity across outcome mea-
sures, cohorts of patients and types of interventions. Future research will need
to focus on details of comparative eectiveness study design to identify the spe-
cic variables that contribute to success.
References
1. Aluko A, DeSouza L, Peacock J. The eect of core sta-
bility exercises on variations in acceleration of trunk
movement, pain, and disability during an episode of
acute nonspecic low back pain: a pilot clinical trial. J
Manip Physiol Ther. 2013;36(8):497-504.e491-493.
2. Koumantakis GA, Watson PJ, Oldham JA. Trunk mus-
cle stabilization training plus general exercise ver-
sus general exercise only: randomized controlled tri-
al of patients with recurrent low back pain. Phys Ther.
2005;85(3):209-225.
3. Unsgaard-Tondel M, Fladmark AM, Salvesen O, Vassel-
jen O. Motor control exercises, sling exercises, and gen-
eral exercises for patients with chronic low back pain: a
randomized controlled trial with 1-year follow-up. Phys
Ther. 2010;90(10):1426-1440.
4. Mostagi FQRC, Dias JM, Pereira LM, et al. Pilates versus
general exercise eectiveness on pain and functionality
in non-specic chronic low back pain subjects. J Body-
work Move Ther. 2015;19(4):636-645.
5. Rasmussen-Barr E, Nilsson-Wikma L, Arvidsson I.
Stabilizing training compared with manual treatment
in sub-acute and chronic low-back pain. Man Ther.
2003;8(4):233-241.
QQ
PM&R Question 6. In patients undergoing treatment for low back pain, what are
outcomes, including duration of pain, intensity of pain, functional outcomes and
return-to-work status, for SMT versus SMT plus active exercise?
Recommendation:
It is suggested that the addition of exercise to SMT results in similar outcomes to SMT alone.
Grade of Recommendation: B
Researchers for the UK BEAM Trial
1
compared out-
comes in patients with LBP who received treatment of
“best care” alone or with additional exercise classes,
spinal manipulation, or manipulation followed by ex-
ercises. Patients had back pain for at least 4 weeks. In
this multicenter pragmatic randomized trial, partici-
pants (n=1334) were randomized into four groups: the
“best care” group (n=338) to receive active manage-
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
152
ment and The Back Book, the exercise program group
(n=310) with up to nine community classes over 12
weeks in addition to “best care,” the spinal manip-
ulation group (n=353) with 8 sessions over 12 weeks
in addition to “best care,” or the combined group
(n=333) which included 6 weeks of manipulation and 6
weeks of exercise in addition to “best care.” Disability
(Roland Morris disability questionnaire) was record-
ed at baseline and at 3- and 12-month follow-up. All
groups experienced improvement in disability scores
at all time-points. The authors concluded that “rel-
ative to ‘best care’ in general practice, manipulation
followed by exercise achieved a moderate benet at
three months and a small benet at 12 months; spinal
manipulation achieved a small to moderate benet at
3 months and a small benet at 12 months; and exer-
cise achieved a small benet at 3 months but not 12
months.” Due to less than 80% follow-up, the work
group downgraded this study from Level I to Lev-
el II. Length of symptoms prior to treatment beyond
4 weeks was unknown. Therefore the nal results
were evaluated over an unknown duration of baseline
chronicity. This study oers Level II therapeutic evi-
dence that, in patients with LBP, educational booklet,
educational booklet plus exercise, educational book-
let plus manipulation alone, and educational booklet
plus manipulation and exercise provide similar im-
provements in pain and function at one year (baseline
scores indicate mild disability).
In a randomized controlled trial, Hsieh et al
2
assessed
the eectiveness of back school, joint manipulation,
myofascial therapy and combined joint manipulation
and myofascial therapy in patients with subacute
LBP. Patients with LBP for more than 3 weeks but
less than 6 months were randomly allocated into one
of four treatment groups for 3 weeks: back school
(n=48), joint manipulation (n=49), myofascial
therapy (n=51), or combined joint manipulation and
myofascial therapy (n=52). Pain (VAS) and Roland-
Morris activity scales were assessed at baseline,
immediately after the 3-week treatment period and
6 months after completion of treatment. All groups
had improvements in outcomes immediately after
treatment – with no dierences between groups. The
authors concluded that back school or combined joint
manipulation and myofascial therapy were as eective
as joint manipulation or myofascial therapy alone for
the treatment of subacute LBP. The inclusion criteria
are a weakness in this study, as the outcomes of
patients with pain ranging from 3 weeks to 6 months
can be substantially variable, although in this case it
did not seem to make any dierence. This study oers
Level I therapeutic evidence that, in patients with LBP
from 3 weeks to 6 months, myofascial therapy, joint
manipulation, combination therapy (myofascial and
joint manipulation) and back school provided similar
improvement in pain and function at 6 months.
Future Directions for Research
There is a need for well-conducted studies to evaluate the benet of SMT alone
compared to SMT and exercise in the treatment of LBP.
References
1. Team UBT. United Kingdom back pain exercise and ma-
nipulation (UK BEAM) randomised trial: eectiveness
of physical treatments for back pain in primary care. Br
Med J. 2004;329(7479):1377.
2. Hsieh CY, Adams AH, Tobis J, et al. Eectiveness of four
conservative treatments for subacute low back pain: a
randomized clinical trial. Spine. 2002;27(11):1142-1148.

Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
153
QQ
PM&R Question 7. In patients undergoing treatment for low back pain, what are
the outcomes, including duration of pain, intensity of pain, functional outcomes
and return-to-work status, for bed rest versus active exercise?
Recommendations:
It is suggested that, for patients with acute low back pain, those that exercise more at base-
line and use exercise to facilitate recovery are predicted to have better functional outcomes
over time than patients who do not exercise or use bed rest to help with recovery.
Grade of Recommendation: B
For patients with acute low back pain, it is suggested that advice to remain active within limits
of pain compared to short periods of bed rest from 3 to 7 days all result in similar outcomes in
pain and function at short- and medium-term follow-up.
Grade of Recommendation: B
Work Group Consensus Statement:
In the absence of reliable evidence for patients with nonspecic back pain, based on abundant
data for other spinal disorders that result in back pain, it is the work group’s opinion that remaining
active is preferred and likely results in better short-term outcomes than does bed rest.
Oleske et al
1
evaluated the eect of personal, med-
ical and job factors on recovery from work-related
low back disorders in an observational longitudinal
study. Active employees at 2 automotive plants with
a work-related low back disorder were included in the
study (n=352). Participants completed a structured
interview related to LBP, health habits, job factors and
medical interventions at enrollment and at 1, 2, 6 and
12 months afterwards. From the interview, 106 items
were selected as independent variables and compared
with the dependent variable of recovery from LBP
(Oswestry Disability Questionnaire). Better recovery
was associated with lower stress levels and exercise
outside of work. Cigarette smoking and bedrest were
associated with higher disability levels. The authors
concluded that personal modiable factors are ma-
jor inuences in the recovery from work-related, low
back disorders. This study provides Level II evidence
that more exercise at baseline is a prognostic factor
for better improvement than bedrest to help recovery.
Hagen et al
2
conducted a randomized controlled study
to evaluate the eect of a light mobilization program
on the duration of sick leave. Patients who were on
sick leave 8-12 weeks due to LBP were randomized to
a control group (n=220) to receive conventional pri-
mary health care or an intervention group (n=237).
The intervention group was invited to a spine clinic
for an approximately 3-hour visit with a physician
and physiotherapist. Participants in the intervention
group were encouraged to remain active and were giv-
en additional information about LBP and radiographs.
All participants completed questionnaires at 3, 6 and
12 months. At all 3 time points, a greater percentage
of the intervention group had returned to full-du-
ty work compared to the control group. The authors
concluded that early intervention, information and
recommendations to stay active signicantly reduced
sick leave for patients with LBP. This study provides
Level II evidence that, in subacute LBP patients (8 to
12 weeks LBP), one visit oering reassurance and en-
couragement to increase activity level versus a reg-
ular primary care visit resulted in signicantly more
patients who returned to work at one year.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
154
Rozenberg et al
3
conducted a randomized controlled
trial to compare LBP outcomes after 4 days of bed
rest versus normal daily activity. Patients with acute
LBP or an acute-on-chronic episode of LBP with
current symptoms for <72 hours were randomized
into two treatment groups. Patients in the bed rest
group (n=137) were encouraged to stay in bed for at
least 16 hours of a 24-hour day for 4 days. Patients in
the normal activity group (n=140) were instructed to
continue normal daily activity as able and to spend no
more than 12 hours per 24-hour day in bed. Medical
treatment was otherwise the same across groups;
physical therapy, bracing and chiropractic care were
not allowed in either group for 3 months during the
trial. Outcomes were measured with the VAS and Eifel
index (French version of Roland Morris) plus a global
assessment score. A total of 277 out of 281 patients
were analyzed with intention-to-treat analysis,
which satised power calculation. Compliance rates
were 72% and 90% in the bed rest and usual activity
groups, respectively. At one week and 3 months, both
groups improved, with no signicant dierence in
pain or function scores. The authors concluded that
normal activity is at least equivalent to bed rest. This
study provides Level I evidence that, for patients
with acute LBP of less than 3 days in duration,
implementation of bed rest for 4 days versus usual
care results in similar outcomes for pain and function
at short- and medium-term follow-up.
Wiesel et al
4
aimed to objectively analyze the roles of
bedrest and medication for the treatment of LBP. Two
hundred male basic combat trainees (average age 23
years) were randomly allocated to an experimental
group or control group in a 3-section study. The rst
part of the study focused on bedrest (n=80); the sec-
ond and third parts focused on medication treatment
(n=45 and n=75). During the rst section of the study,
all participants described their pain at baseline and
were given a quantiable score each day. The experi-
mental group was admitted to the hospital for bedrest
treatment until their LBP subsided. The control group
was assigned restricted-duty without exercise, but
entailed standing on their feet. The primary outcome
was return to full duty which occurred when pain was
resolved and physical exam had returned to normal.
The bed rest group returned to duty signicantly fast-
er than the ambulatory group (6.6 days in the bed rest
group compared to 11.8 days in the light duty group).
The authors concluded that bedrest, as compared with
ambulation, will decrease the amount of time lost
from work by 40% to 50%; decrease discomfort by
60%; and, in combination with analgesic medication,
will further decrease the amount of pain. In critique
of the methodology, the workgroup downgraded this
potential Level I study due to the use of non-validat-
ed outcome measures and an unrealistic form of bed
rest used (hospitalization). This study provides Level
II evidence that bed rest, in the form of hospitaliza-
tion, results in sooner return to full duty than treat-
ment with light duty in young male combat trainees.
Outcomes by 2 weeks appeared to be the same.
Future Directions for Research
The work group recommends future randomized controlled trials to evaluate
the eect of bed rest on LBP
References
1. Oleske DM, Neelakantan J, Andersson GB, et al. Fac-
tors aecting recovery from work-related, low back
disorders in autoworkers. Arch Phys Med Rehabil.
2004;85(8):1362-1364.
2. Hagen EM, Eriksen HR, Ursin H. Does early intervention
with a light mobilization program reduce long-term
sick leave for low back pain. Spine. 2000;25(15):1973-
1976.
3. Rozenberg S, Delval C, Rezvani Y, et al. Bed rest or nor-
mal activity for patients with acute low back pain. Spine.
2002;27(14):1487-1493.
4. Wiesel SW, Cuckler JM, Deluca F, Jones F, Zeide MS,
Rothman RH. Acute low-back pain an objective analysis
of conservative therapy. Spine. 1980;5(4):324-330.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
155
QQ
PM&R Question 8. In patients with low back pain, does a regular exercise
program (or presurgical intervention with exercise, PT, education) prior to lumbar
surgery decrease the duration of pain, decrease the intensity of pain, increase
the functional outcomes of treatment and improve the return-to-work rate
compared to those who don’t exercise?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends future randomized controlled trials to assess if
prehabilitation compared to usual activity aects outcomes of lumbar spine sur-
gery.
QQ
PM&R Question 9. In patients with low back pain, does exercise treatment after
epidural steroid injections/spinal interventions decrease the duration of pain,
decrease the intensity of pain, increase the functional outcomes of treatment and
improve the return-to-work rate compared to injections alone?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that high-level studies be performed evaluating
the outcomes of interventional spine procedures alone versus interventional
spine procedures in combination with physical therapy/exercise.
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
156
QQ
PM&R Question 10. Following surgery for low back pain, are outcomes, including
duration of pain, intensity of pain, functional outcomes and return-to-work status,
improved with a formal exercise/rehabilitation program versus home instruction
plus or minus self-directed exercise program alone?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends comparative eectiveness research, preferably
prospective, but even retrospective, to dene value of post-op rehab for LBP.
QQ
PM&R Question 11. Can a clinical prediction rule determine appropriate indications
and predict outcomes, including duration of pain, intensity of pain, functional
outcomes and return-to-work status, for exercise for low back pain?
Recommendation:
There is insucient evidence to provide any reliable predictors of outcomes to an exercise
program for the treatment of either acute or chronic low back pain.
Grade of Recommendation: I
Underwood et al
1
conducted an analysis of the UK
Back pain Exercise And Manipulation (UK BEAM) Tri-
al to identify characteristics predictive of response to
treatment of LBP. The UK BEAM Trial (n=1334) found
that compared treatment packages of spinal manipu-
lation (up to 8 sessions over 12 weeks), manipulation
plus exercise (6 weeks manipulation and 6 weeks of
exercise) and exercise alone (9 group classes over 12
weeks) against usual care, including The Back Book.
Disability (Roland Morris Disability Questionnaire),
back pain beliefs (Fear Avoidance Beliefs Question-
naire), psychological state (Distress and Risk As-
sessment Method), treatment expectations and oth-
er demographic characteristics were obtained before
randomization and at 3-month and one-year fol-
low-up. None of the studied baseline characteris-
tics predicted response (disability per Roland Morris
Disability Questionnaire) to treatment. The authors
concluded that there were no characteristics that pre-
dicted response to the UK BEAM treatment packages.
This study oers Level II prognostic evidence that, in
patients with subacute LBP receiving SMT, there were
no predictors (including pain duration) for response
to treatment.
Cecchi et al
2
prospectively enrolled patients with
chronic LBP to be treated with an exercise program
devised by a physical therapist based on the individual
assessment of each patient. Six sessions were provid-
ed along with education and the patients were encour-
aged to continue with a home exercise program. At one
year, 211 of 225 patients were contacted for follow-up
and evaluated for predictors of improvement. The only
predictive factor of functional outcome at discharge
was less intense pain at baseline assessment. At one-
year follow-up, younger age, better baseline mental
Diagnosis & Treatment of Low Back Pain | Recommendations | Physical Medicine & Rehabilitation
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
157
health, no history of prior treatment and low drug use
predicted higher long-term response rates. This is a
Level I prognostic study to indicate that in patients
with chronic LBP, short-term favorable response to
an exercise program is predicted by less intense pain
at baseline. Younger age, better mental health, no
prior history of treatment and lower drug use predict
better long-term functional outcomes at one year.
Future Directions for Research
Establishing clinical predictors to exercise for the treatment of LBP would be
very practical and useful for both the patient and provider. Prospective trials or
post hoc reviews of registry data could be used to improve our understanding
of these predictors. Great care will need to be taken in study design to ensure
that LBP is dened in a consistent, measurable and evaluable manner and that
homogeneous exercise programs are developed and applied across studies to
improve the strength of the evidence.
References
1. Underwood MR, UK BEAM Trial Team. (2007). Do baseline
characteristics predict response to treatment for low
back pain? Secondary analysis of the UK BEAM data-
set [ISRCTN32683578]. Rheumatology. 46(8):1297-302.
Epub 2007 May 23.
2. Cecchi F, Pasquini G, Paperini A, et al. Predictors of re-
sponse to exercise therapy for chronic low back pain: re-
sult of a prospective study with one year follow-up. Eur J
Phys Rehabil Med. 2014;50(2):143-151.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
158
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
158
Section Authors
Guideline Co-Chair
D. Scott Kreiner, MD
Interventional Treatment Section Chair
John Easa, MD, FIPP
Members
Jamie Baisden, MD, FACS
Robert Shay Bess, MD
David Cheng, MD
David Provenzano, MD, Stakeholder Representative:
American Society of Regional Anesthesia and Pain
Medicine
Yakov Vorobeychik, MD, PhD,
Stakeholder Representative: Spine Intervention Society
With Contributions from:
Joseph Gjolaj, MD
Thomas Gilbert, MD
QQ
Interventional Question 1. In patients with low back pain, do uoroscopically-
guided epidural steroid injections decrease the duration of pain, decrease the
intensity of pain, increase the functional outcomes of treatment and improve the
return-to-work rate?
There is insucient evidence to make a recommendation for or against the use of caudal
epidural steroid injections in patients with low back pain.
Grade of Recommendation: I
Southern et al
1
investigated the ecacy of uoro-
scopic caudal epidural steroid injections for the treat-
ment of chronic lumbar discogenic pain. Patients with
chronic low back pain (LBP) with evidence of disc pa-
thology without stenosis (n=97) received at least one
uoroscopically-guided caudal epidural injection
with 12 mg of betamethasone and 8 cc of 0.5% lido-
caine. Disability (Roland Morris Disability Question-
naire, RMDQ), pain (Visual Numeric Pain Scale, VNS)
and patient satisfaction (North American Spine So-
ciety, NASS, patient satisfaction questionnaire) were
assessed before and after the injection. Eighty-four
patients were included in follow-up analysis. Patients
were classied as procedure failure (if a discography
and/or surgery was needed after injection) or success
(score of 1-2 on NASS patient satisfaction, >50% re-
duction in VNS and >2-point change in RMDQ score).
After at least one year, 19 patients were classied as
successes and 65 as failures. Patient satisfaction was
45%. The patients classied as successes had signi-
cantly lower baseline pain scores. The authors con-
cluded that patient satisfaction exceeds reported rate
of ecacy of uoroscopically-guided caudal epidur-
al steroid injections in patients with chronic lumbar
discogenic pain. This study provides Level IV evidence
that roughly 20% of patients with chronic discogen-
ic LBP will experience at least 50% reduction in pain
following caudal epidural steroid injections.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
159
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
159
There is insucient evidence to make a recommendation for or against the use of interlaminar
epidural steroid injections in patients with low back pain.
Grade of Recommendation: I
Lee et al
2
conducted an observational study to deter-
mine the eect of a uoroscopic interlaminar epidur-
al steroid injection (ESI) for axial LBP. Patients with
LBP (n=81) at a single facility received an interlaminar
ESI and followed-up within the rst month and again
1-2 years later via telephone interview. The proce-
dure was classied as eective if the patient’s report-
ed pain score was reduced by >50%. Sixty-three of 81
procedures were considered eective at short-term
follow-up. Thirty-seven (37%) reported greater than
6 months’ symptom relief. There were no signicant
outcome predictors. The authors concluded that the
therapeutic trial of a uoroscopic interlaminar ESI
was eective for axial LBP. This study provides Level
IV evidence that interlaminar epidural steroid injec-
tions in patients with LBP can be expected to provide
patient-reported pain relief in roughly 40% of pa-
tients at 6 months or greater. Ninety percent of these
patients received one or two ESI.
Future Directions for Research
The work group had no additional recommendations for future research on this
topic.
References
1. Southern D, Lutz GE, Cooper G, Barre L. Are uoroscop-
ic caudal epidural steroid injections eective for man-
aging chronic low back pain? Pain Phys. 2003;6(2):167-
172.
2. Lee JW, Shin HI, Park SY, Lee GY, Kang HS. Therapeutic
trial of uoroscopic interlaminar epidural steroid injec-
tion for axial low back pain: eectiveness and outcome
predictors. AJNR Am J Neuroradiol. 2010 Nov;31(10):1817-
23.
QQ
Interventional Question 2. When evaluating uoroscopically-guided intra-articular
lumbar facet joint injections in patients with acute or chronic low back pain:
a. What is the diagnostic utility of this procedure?
b. From a therapeutic standpoint, does this procedure decrease the duration of
pain, decrease the intensity of pain, increase the functional outcomes of treatment
and improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the use of patient-
reported reproduction of pain during a zygapophyseal joint injection as a predictor of
response to dual diagnostic blocks.
Grade of Recommendation: I

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
160
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
160
Schwarzer et al
1
investigated the relationship between
pain provocation and the analgesic response in lum-
bar zygapophyseal joint blocks. Patients with LBP for
greater than 3 months underwent at least one intraar-
ticular, uoroscopically-guided injection of lidocaine
into the zygapophyseal joints. Ten minutes after in-
jection, each patient was asked to perform previously
painful movements and rate the pain as “worse,” “no
change,” “partial,” “denite” or “complete” relief. If
the pain relief was less than complete, the same pro-
cedure was completed using the next segmental level.
Two weeks later, conrmatory blocks using 0.5% bu-
pivacaine were completed for each patient and classi-
ed as a positive response if the patient experienced
>50% improvement in pain (VAS). Analysis of the 203
joints revealed that reproduction of pain correlated
with either denite or complete relief of pain after a
single analgesic block, only with liberal criteria. The
authors concluded that the validity of pain provoca-
tion alone as a criterion standard in patients under-
going diagnostic lumbar zygapophyseal joint blocks
should be questioned. This study provides Level I evi-
dence that pain reproduction during a zygapophyseal
joint injection is not predictive of the zygapophyse-
al joint as the pain generator. The positive predictive
value was 16%.
In patients selected for facet joint procedures using diagnostic criteria of physical exam and
a response to a single diagnostic intra-articular injection with 50% relief, it is suggested that
intra-articular injection of steroids provides no clinically meaningful improvement at 6 months
Grade of Recommendation: B
Carette et al
2
conducted a randomized controlled
study to investigate the eectiveness of corticosteroid
injections into the facet joints to treat chronic LBP.
Patients with LBP for at least 6 months who report-
ed immediate pain relief after a diagnostic injection of
local anesthetic into the facet joints were randomized
to receive 20 mg methylprednisolone acetate (n=49)
or isotonic saline (n=48) under uoroscopic guidance.
Pain severity (Visual Analog Scale [VAS] and McGill
pain questionnaire), back mobility and limitation
of function (modied Sickness Impact Prole) were
recorded one, 3 and 6 months after injection. There
were no statistically signicant dierences between
groups after one and three months. The methylpred-
nisolone group had greater improvements in pain and
disability after 6 months, but the dierences were re-
duced when concurrent interventions were taken into
account. The authors concluded that injecting meth-
ylprednisolone acetate into the facet joints is of little
value in the treatment of patients with chronic LBP.
This study provides Level II evidence that, in patients
selected for facet joint injections with steroid using a
single diagnostic intra-articular block with 50% re-
lief, the outcome of pain relief is similar in the steroid
group to the saline group.
In a double-blind randomized controlled trial,
Lakemeier et al
3
compared the eectiveness of
intra-articular facet joint steroid injections and
radiofrequency denervation for the treatment
of chronic LBP. Patients with LBP for at least 24
months who had hypertrophy of the facet joints
L3/L4-5/S1 on magnetic resonance imaging and
experienced at least 50% pain reduction after a test
injection of local anesthetics were included in this
study. Participants were randomized to receive
radiofrequency denervation (n=27) or intra-articular
steroid inltration (n=29). Participants completed the
RMDQ, VAS and Oswestry Disability Index at baseline
and after 6 months. Both groups had improvements
with no signicant dierences between groups. This
study provides Level II evidence that, in patients who
receive a 50% reduction in pain with a single intra-
articular facet joint injection of local anesthetic,
intra-articular steroids provide similar results to a
radiofrequency ablation. Neither provides clinically
meaningful improvements at 6 months.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
161
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
161
In patients selected for facet joint procedures using diagnostic criteria of physical exam and
a response to a single diagnostic intra-articular injection with 50% relief, there is insucient
evidence to make a recommendation for or against the use of radiofrequency neurotomy or
periarticular phenol injections.
Grade of Recommendation: I
In a double-blind randomized controlled trial,
Lakemeier et al
3
compared the eectiveness of
intra-articular facet joint steroid injections and
radiofrequency denervation for the treatment
of chronic LBP. Patients with LBP for at least 24
months who had hypertrophy of the facet joints
L3/L4-5/S1 on magnetic resonance imaging and
experienced at least 50% pain reduction after a test
injection of local anesthetics were included in this
study. Participants were randomized to receive
radiofrequency denervation (n=27) or intra-articular
steroid inltration (n=29). Participants completed the
RMDQ, VAS and Oswestry Disability Index at baseline
and after 6 months. Both groups had improvements
with no signicant dierences between groups. This
study provides Level II evidence that, in patients who
receive a 50% reduction in pain with a single intra-
articular facet joint injection of local anesthetic,
intra-articular steroids provide similar results to a
radiofrequency ablation. Neither provides clinically
meaningful improvements at 6 months.
Schulte et al
4
aimed to investigate the clinical im-
provement after a standard facet joint injection ther-
apy protocol and determine the best time for repet-
itive injection therapy. Patients with chronic LBP
diagnosed with lumbar facet joint syndrome (n=39)
were treated with a standardized protocol of uo-
roscopically-guided injection therapy. Patients who
reported at least 50% reduction of pain after initial
injection of 1 ml crystalline prednisolone acetate (50
mg) mixed with 2 ml lidocaine (1%) received an in-
jection using only lidocaine and phenol solution (5%,
1 ml each joint) the next day. Participants completed
questionnaires that contained the pain disability in-
dex, Macnab criteria (excellent, good, fair or poor)
and VAS for pain at baseline and after 6 months. Pain
was reduced up to 6 months. Patients reported as ex-
cellent or good by 62% of patients after 1 month, 41%
of patients after three months and 36% of patients af-
ter six months. The authors concluded that facet joint
injection therapy using a standardized protocol is
safe, eective and easy to perform and recommended
repetitive injection after 3 months. This study pro-
vides Level IV evidence that, in patients who receive a
50% reduction in pain with a single periarticular facet
joint injection of local anesthetic and steroids, periar-
ticular injection of phenol produced excellent to good
response using Macnab criteria and roughly half of
patients reported a poor outcome at 6 months.
There is insucient evidence to make a recommendation for or against the use of steroid in-
jections into the zygapophyseal joint in patients with chronic back pain and a physical exam
suggestive of facet-mediated pain.
Grade of Recommendation: I
Chaturvedi et al
5
evaluated the ecacy of facet joint
inltrations for the treatment of chronic LBP. Patients
with LBP for greater than 3 months (n=44) received
facet joint injections under uoroscopic guidance
(n=39) or CT guidance (n=5). Pain was assessed one
hour after the procedure and at 1, 4, 12 and 24 weeks.
Signicant pain relief was reported after one hour
(81.8%), one week (86.3%), 4 weeks (93.3%), 12 weeks
(85.7%) and 24 weeks (62.5%). The authors conclud-
ed that the minimally invasive facet nerve block was
safe, resulted in long-term success rates over 60%
and should be considered an alternative treatment for
non-radicular back pain. This study provides Level IV
evidence that, in patients with greater than 3 months
of LBP and symptoms and physical exam suggestive
of facet-mediated pain, intra-articular steroid injec-
tions into the facet joints produces signicant pain re-
lief in 90% of patients at 12 weeks and 2/3 of patients
at 24 weeks. Roughly 15% of patients required more
than one injection.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
162
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
162
Future Directions for Research
1. The work group recommends future randomized controlled trials of various
facet joint interventions including therapeutic injections and radiofrequency
neurotomy in patients diagnosed with facet joint pain using dual diagnostic
blocks with 80% relief.
2. The work group recommends, in patients with suspected facet mediated pain,
more than one comparison trial between outcomes of patients undergoing dual
diagnostic blocks with a single local anesthetic versus dual diagnostic blocks
with local anesthetics with dierent durations of action and pain relief commen-
surate with the local anesthetic used.
References
1. Schwarzer AC, Derby R, Aprill CN, Fortin J, Kine G,
Bogduk N. The value of the provocation response in
lumbar zygapophyseal joint injections. Clin J Pain.
1994;10(4):309-313.
2. Carette S, Marcoux S, Truchon R, et al. A controlled trial
of corticosteroid injections into facet joints for chronic
low back pain. N Engl J Med. 1991;325(14):1002-1007.
3. Lakemeier S, Lind M, Schultz W, et al. A comparison of
intraarticular lumbar facet joint steroid injections and
lumbar facet joint radiofrequency denervation in the
treatment of low back pain: a randomized, controlled,
double-blind trial. Anesth Analg. 2013;117(1):228-235.
4. Schulte TL, Pietila TA, Heidenreich J, Brock M, Stendel R.
Injection therapy of lumbar facet syndrome: a prospec-
tive study. Acta Neurochir (Wien). 2006;148(11):1165-
1172; discussion 1172.
5. Chaturvedi A, Chaturvedi S, Sivasankar R. Image-guid-
ed lumbar facet joint inltration in nonradicular low
back pain. Indian J Radiol Imaging. 2009;19(1):29-34.
QQ
Interventional Question 3. In patients with low back pain, do medial branch
blocks have a role in dening treatment for low back pain?
a. Does duration of pain, intensity of pain, functional outcomes and return-to-
work status vary when candidates for neurotomy are determined by single vs
comparative medial branch blocks?
b. Is there a threshold for the magnitude of relief from diagnostic facet nerve
blocks that predict outcomes to neurotomy?
c. Does duration of pain, intensity of pain, functional outcomes and return-to-
work status vary when candidates for neurotomy are determined by diagnostic
facet nerve blocks vs intra-articular facet joint injections?
d. Is there a therapeutic utility of medial branch blocks?
e. Does technical accuracy of medial branch blocks (eg, contrast use) aects its
validity and eectiveness of subsequent neurotomy?
There is insucient evidence to make a recommendation for or against the use of SPECT imag-
ing in the diagnosis of zygapophyseal joint pain.
Grade of Recommendation: I
Ackerman et al
1
compared the eectiveness of intra-
articular and medial branch nerve blocks in patients
with LBP with single-photon emission computed
tomography (SPECT)-positive lumbar facet joints.
Patients with nonradicular LBP who were lumbar
facet joint SPECT-positive were randomized to

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
163
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
163
receive intra-articular (n=23) or medial branch nerve
blocks (n=23) with lidocaine and triamcinolone.
Pain (Numeric Pain Intensity Score) and disability
(Oswestry Disability Index Score) were measured after
the injection and after 12 weeks. The intra-articular
group experienced signicantly greater improvements
in pain and disability. The authors concluded that
intra-articular lumbar facet joint injections are more
eective than medial branch nerve blocks in SPECT-
positive patients. In critique of the methodology, the
work group downgraded this potential Level I study as
the diagnostic utility of SPECT imaging was negated
by injecting bilateral joints and/or bilateral medial
branch blocks in every patient. This study provides
Level II evidence that, in patients with LBP and positive
SPECT imaging showing uptake in the facet joint,
intra-articular injection of steroid provides at least
a 50% reduction in pain in roughly 60% of patients
and steroid injection around the medial branch nerves
provides at least a 50% reduction in pain in roughly
25% of patients.
There is insucient evidence to make a recommendation for or against the use of uncontrolled
medial branch blocks vs. pericapsular blocks for the diagnosis of zygapophyseal joint pain
based on the outcomes of medial branch nerves cryoablation.
Grade of Recommendation: I
Birkenmaier et al
2
aimed to compare the predictive
value of uncontrolled medial branch blocks versus
pericapsular blocks for predicting successful out-
comes of cryodenervation. Patients with LBP for at
least 3 months were randomized to receive medial
branch blocks or pericapsular blocks. The patients
who had a positive response (≥50% improvement in
LBP for at least 3 hours) were enrolled in the study
(n=13 in each group). Percutaneous medial branch
cryodenervation was performed, under uoroscopic
guidance, with local anesthesia and 1% mepivacaine
by use of a Lloyd Neurostat 2000. Pain (VAS), limita-
tion of activity (Macnab) and overall satisfaction were
recorded at baseline and after 2 and 6 weeks as well as
3 and 6 months. Patients who received diagnostic me-
dial branch blocks had statistically signicantly bet-
ter pain relief at 6 weeks and 3 months compared to
those who received pericapsular blocks. The authors
concluded that, although both blocks worked, uncon-
trolled medial branch blocks are superior to pericap-
sular blocks in selecting patients for facet joint cryo-
denervation. From a diagnostic perspective, this study
provides Level III evidence that a single medial branch
block is a better predictor of an outcome of pain re-
lief following cryodenervation of the medial branch
nerves than a pericapsular local anesthetic injection.
There is insucient evidence to make a recommendation for or against the use of cryodenerva-
tion for the treatment of zygapophyseal joint pain.
Grade of Recommendation: I
Birkenmaier et al
2
aimed to compare the predictive
value of uncontrolled medial branch blocks versus
pericapsular blocks for predicting successful out-
comes of cryodenervation. Patients with LBP for at
least 3 months were randomized to receive medial
branch blocks or pericapsular blocks. The patients
who had a positive response (≥50% improvement in
LBP for at least three hours) were enrolled in the study
(n=13 in each group). Percutaneous medial branch
cryodenervation was performed, under uoroscopic
guidance, with local anesthesia and 1% mepivacaine
by use of a Lloyd Neurostat 2000. Pain (VAS), limita-
tion of activity (Macnab) and overall satisfaction were
recorded at baseline and after 2 and 6 weeks as well
as 3 and 6 months. Patients who received diagnostic
medial branch blocks had statistically signicantly
better pain relief at 6 weeks and 3 months compared
to those who received pericapsular blocks. The au-
thors concluded that, although both blocks worked,
uncontrolled medial branch blocks are superior to
pericapsular blocks in selecting patients for facet joint
cryodenervation. From a therapeutic perspective, this
study provides Level IV evidence that cryodenerva-
tion of the medial branch nerves in patients with LBP
selected using a single medial branch block patients
noted a 66% reduction in pain at 6 months.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
164
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
164
There is insucient evidence to make a recommendation for or against the use of a 50% reduc-
tion in pain following medial branch blockade for the diagnosis of zygapophyseal joint pain.
Grade of Recommendation: I
Kaplan et al
3
conducted a randomized controlled trial
to investigate the eectiveness of conventional medial
branch blocks for zygapophysial joint pain. In the rst
phase, healthy, asymptomatic adults with no history
of lumbar pain (n=18) received a uoroscopically-
guided intra-articular zygapophysial joint injection of
contrast until pain was elicited. Participants recorded
pain (VAS) immediately after pain was elicited, every
hour for the rst 6 hours and every day for 7 days.
In the second phase of this study, the participants
who incurred pain provocation that lasted less than
48 hours were randomly allocated to receive medial
branch nerve injections with 2.0% lidocaine (n=10)
or saline (n=5). Thirty minutes after injection, the
participants underwent the same joint injection that
elicited pain the previous week and recorded pain in
the same manner. All patients who received saline
medial branch injections experienced pain on repeat
capsular distention. Of the individuals who received
2% lidocaine medial branch blocks, eight felt no pain.
The authors concluded that the 2% lidocaine was
signicantly more eective on anesthetization of the
zygapophysial joint when uptake was avoided during
these injections. The workgroup felt that this type
of study was not adequately described in the dened
Levels of Evidence Table and, as a consensus, rated
this as Level I. This study provides Level I evidence
that medial branch blockade with local anesthetic
eectively anesthetizes the zygapophyseal joint.
Venous uptake may negatively aect the response to
medical branch blockade.
Rocha et al
4
studied the prevalence of LBP after con-
trolled medial branch blocks in a prospective, con-
trolled, diagnostic study. Patients with chronic LBP
for at least 3 months underwent a saline injection fol-
lowed by a controlled medial branch block (0.5 ml of
lidocaine at 2%, without epinephrine). Pain (VAS) was
recorded before and after the injection. Patients who
reported >50% improvement of pain after the block-
ade (n=54) were included in follow-up after one day,
one week and one, 2 and 3 months. After 3 months, 18
participants (33%) experienced return of lumbar pain.
The authors concluded that patient diagnosis with a
controlled medial branch block was eective but not
associated with any demographic variables. This study
provides Level IV evidence that, in patients undergo-
ing medial branch blocks, using a cuto of a 50% pain
reduction, 2/3 of the patients who responded to this
block will have continued reduction in pain 3 months
after the block.
Thermal radiofrequency ablation is suggested as a treatment for patients with low back pain
from the zygapophyseal joints. The outcomes of this procedure become more reliable when
more stringent diagnostic criteria are used. The relief from these ablations is durable for at least
6 months following the procedure.
Grade of Recommendation: B
Kaplan et al
3
conducted a randomized controlled trial
to investigate the eectiveness of conventional me-
dial branch blocks for zygapophysial joint pain. In
the rst phase, healthy, asymptomatic adults with
no history of lumbar pain (n=18) received a uoro-
scopically-guided intra-articular zygapophysial joint
injection of contrast until pain was elicited. Partici-
pants recorded pain (VAS) immediately after pain was
elicited, every hour for the rst 6 hours and every day
for 7 days. In the second phase of this study, the par-
ticipants who incurred pain provocation that lasted
less than 48 hours were randomly allocated to receive
medial branch nerve injections with 2.0% lidocaine
(n=10) or saline (n=5). Thirty minutes after injection,
the participants underwent the same joint injection
that elicited pain the previous week and recorded pain
in the same manner. All patients who received saline
medial branch injections experienced pain on repeat
capsular distention. Of the individuals who received
2% lidocaine medial branch blocks, 8 felt no pain. The
authors concluded that the 2% lidocaine was signi-
cantly more eective on anesthetization of the zyga-
pophysial joint when uptake was avoided during these
injections. The workgroup felt that this type of study
was not adequately described in the dened Levels
of Evidence Table and, as a consensus, rated this as

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
165
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
165
Level I. This study provides Level I evidence that me-
dial branch blockade with local anesthetic eectively
anesthetizes the zygapophyseal joint. Venous uptake
may negatively aect the response to medical branch
blockade.
Nath et al
5
conducted a randomized controlled study
to determine the eectiveness of percutaneous ra-
diofrequency zygapophysial joint neurotomy in pa-
tients with lumbar zygapophysial joint pain. Patients
with LBP for at least 2 years who had at least 80%
pain relief after controlled medial branch blocks were
randomized to receive an active treatment with 2 mL
of bupivacaine (n=20) or sham with the same pro-
cedure without radiofrequency (n=20). The degree
and duration of pain (VAS) was recorded every hour
for 6 hours after the injection, the following day and
6-month follow-up. The active treatment group had
signicantly greater improvements in pain, quality
of life, analgesic consumption and global perception
of improvement compared to the sham group. The
authors concluded that radiofrequency facet dener-
vation can be used as a treatment for chronic LBP in
carefully-selected patients. This study provides Level
I evidence that, in patients undergoing dual diagnos-
tic comparative medial branch blocks with 80% relief,
radiofrequency ablation of the medial branch nerves
provides clinically and statistically signicant im-
provements in pain, quality of life variables and an-
algesic consumption compared to sham at 6 months.
Van Kleef et al
6
investigated the eectiveness of per-
cutaneous radiofrequency denervation of the lumbar
zygapophysial joints in the treatment of LBP origi-
nating from the lumbar zygapophysial joints. Patients
with LBP for at least one year who had a positive re-
sponse to a diagnostic nerve blockade were random-
ized to receive a 60-second 80°C radiofrequency le-
sion of the dorsal ramus of the segmental nerve roots
L3-L5 (n=15) or a control group of the same proce-
dure without radiofrequency current (n=16). Physical
impairment, global perceived eect, pain (VAS) and
disability (Oswestry disability scale) were recorded
before the treatment and 8 weeks after treatment.
Success was dened as ≥50% pain reduction on global
perceived eect and ≥2-points reduction on the VAS
scale. The radiofrequency group experiences statis-
tically signicantly greater improvements in pain,
global perceived eect and disability. There were
more successes in the radiofrequency group at 3, 6 and
12 months compared to the sham group. The authors
concluded that radiofrequency lumbar zygapophysial
joint denervation signicantly reduces pain and func-
tional disability on a short-term and long-term basis
in a select group of patients with chronic LBP. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to poor inclusion
criteria and no concealment prior to randomization.
This study provides Level II evidence that, in patients
who have at least a 50% reduction in pain from diag-
nostic medial branch blocks, radiofrequency ablation
provides better improvements in pain and functional
outcomes than sham.
Civelek et al
7
compared the eectiveness of facet joint
injections and facet joint radiofrequency denervation
in patients with chronic LBP. Patients with LBP who
did not respond to conservative treatment and diag-
nosed with lumbar facet syndrome were randomized
to receive a facet joint injection (n=50) or facet joint
radiofrequency denervation at 80°C temperature for
120 seconds (n=50). The facet joint injection consist-
ed of a medial branch block of the posterior primary
ramus with 1 cc of methyl-prednisolone acetate (40
mg) (diluted with 1 cc SF) combined with 2 cc bupiva-
caine hydrochloride (diluted with 2 cc SF). Pain (NVS),
patient satisfaction (NASS) and general health status
(EQ-5D) were recorded at baseline as well as 3, 6 and
12 months. The patients who received facet joint ra-
diofrequency denervation experienced statistically
signicantly greater improvements in pain at one, 6
and 12 months. The authors concluded radiofrequen-
cy denervation should be used for the treatment of
chronic LBP if pain recurs or if pain relief is not expe-
rienced after the rst line facet joint injection. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to poor selection
criteria for facet joint pain. This study provides Level
II evidence that, in patients without diagnostic blocks
with suspected facet pain, radiofrequency ablation
shows better improvements in pain at 6 months and
1 year when compared with a medial branch steroid
injection.
Kroll et al
8
conducted a prospective, randomize,
double-blind study to compare the ecacy of
continuous radiofrequency thermocoagulation
with pulsed radiofrequency in the treatment of
lumbar facet syndrome. Patients were randomly
allocated to receive continuous radiofrequency
thermocoagulation at 80°C for 75 seconds (n=13) or
pulsed radiofrequency at 42°C with a pulse duration
of 20 ms and pulse rate of 2 Hz for 120 seconds
(n=13). Pain (VAS) and disability (Oswestry Low Back
Pain and Disability Questionnaire) were assessed at
baseline and after 3 months. There were no signicant
dierences between groups in relative percentage of
improvement in pain or disability. The patients in the

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
166
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
166
continuous radiofrequency thermocoagulation group
experienced signicant improvement in pain and
disability over time while the pulsed radiofrequency
group did not experience any signicant changes
over time. The authors concluded that continuous
radiofrequency resulted in greater improvement over
time compared to pulsed radiofrequency. In critique,
the work group downgraded this potential Level I
study due to lack of follow-up and small sample size.
This study provides Level II evidence that thermal
radiofrequency ablation produces clinically and
statistically signicant improvements in pain and
function at 3 months when compared with pulse
radiofrequency.
Tekin et al
9
compared the eectiveness of conven-
tional radiofrequency and pulsed radiofrequency de-
nervation to medial branches of dorsal rami in the
treatment of facet joint pain. Patients with chronic
LBP for more than six months who responded to a di-
agnostic medial branch block (0.3 mL lidocaine 2%)
with greater than 50% pain reduction on VAS were
enrolled. Participants were randomly allocated into
a control group to receive local anesthetic (n=20), or
treatment groups to receive 80°C conventional radiof-
requency group (n=20), or 2 Hz pulsed radiofrequency
(n=20). Pain (VAS) and disability (Oswestry Disability
Index) were recorded before and after the procedure
as well as 6 months and one year after the procedure.
Pain and disability improved immediately after the
procedure in all groups, with lower scores in both
treatment groups compared to the control group. The
decrease in pain was maintained at 6- and 12-month
follow-ups in the conventional radiofrequency group,
but not the pulsed radiofrequency denervation group.
The authors concluded that both treatments were
safe and eective, but conventional radiofrequency
resulted in long-lasting facet joint pain relief. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to poor inclusion
criteria. This study provides Level II evidence that, in
patients diagnosed with facet pain using a single me-
dial branch block and 50% relief, thermal radiofre-
quency ablation provides statistically signicant im-
provements in pain and function when compared to
pulsed radiofrequency ablation and sham.
In a double-blind randomized controlled trial,
Lakemeier et al
10
compared the eectiveness of
intra-articular facet joint steroid injections and
radiofrequency denervation for the treatment
of chronic LBP. Patients with LBP for at least 24
months who had hypertrophy of the facet joints
L3/L4-5/S1 on magnetic resonance imaging and
experienced at least 50% pain reduction after a
test injection of local anesthetics were included in
this study. Participants were randomized to receive
radiofrequency denervation (n=27) or intra-articular
steroid inltration (n=29). Participants completed the
RMDQ, VAS and Oswestry Disability Index at baseline
and after 6 months. Both groups had improvements
with no signicant dierences between groups. This
study provides Level II evidence that, in patients who
receive a 50% reduction in pain with a single intra-
articular facet joint injection of local anesthetic,
intra-articular steroids provide similar results to a
radiofrequency ablation. Neither provides clinically
meaningful improvements at 6 months.
In a double-blind randomized controlled trial,
Leclaire et al
11
evaluated the ecacy of percutaneous
radiofrequency articular facet denervation for the
treatment of LBP. Patients with LBP for more than 3
months and positive response after uoroscopically-
guided intra-articular facet injections were enrolled.
Participants were randomized into a treatment group
to receive uoroscopically-guided percutaneous
radiofrequency articular facet denervation (n=36) or
control group to receive sham therapy of the same
procedure without denervation (n=34). Pain (VAS) and
disability (Oswestry and RMDQ scales) were recorded
at baseline and after 4 and 12 weeks. The treatment
group had signicantly greater improvement in
RMDQ scores compared to the control group at 4
weeks, with no dierences in Oswestry or VAS. There
were no dierences between groups at 12 weeks in any
outcomes. The authors concluded that radiofrequency
facet joint denervation may provide short-term
improvement in functional disability in patients
with chronic LBP, but the ecacy has not been
established. In critique of the methodology, the work
group downgraded this potential Level I study due
to poor inclusion criteria. This study provides Level
II evidence that patients who reported relief from
their back pain within one week of an intra-articular
steroid injection and undergo radiofrequency ablation
with the active tip of the needle placed perpendicular
to the nerve, report no improvement in pain at 3 and
12 months when compared with sham RF.
MacVicar et al
12
investigated the eectiveness of lum-
bar medial branch radiofrequency neurotomy for the
treatment of chronic LBP. Patients who experienced
complete relief of pain after controlled diagnostic me-
dial branch blocks (n=106) were treated with radiof-
requency neurotomy performed by 2 trained practi-
tioners. Pain relief of 80-100% for at least 6 months
with complete return to work and return to activities
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
167
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
167
of daily living without need for further health care
was classied as a successful outcome. Successful
outcomes were achieved in 58% and 53% of patients
at two dierent practices. The authors concluded that
lumbar radiofrequency neurotomy can be an eective
treatment for chronic back pain when performed in a
rigorous manner in appropriately-selected patients.
The study provides Level IV evidence that the major-
ity of patients selected by comparative lumbar facet
nerve blocks for radiofrequency neurotomies have
80–100% relief from their LBP with the restoration of
activities and no other health care for a median dura-
tion of 15 months. Further, patients that experienced
successful relief from their LBP after the rst radiof-
requency neurotomies will likely experience a similar
response to repeat radiofrequency neurotomies for
the same condition.
Future Directions for Research
The work group recommends randomized controlled trials comparing the re-
sponse to medial branch radiofrequency ablation outcomes to various diagnos-
tic methods of diagnosing zygapophyseal joint pain, including intra-articular fac-
et joint injections and medial branch blocks with varying response rates using
dierent local anesthetics.
References
1. Ackerman WE, 3rd, Ahmad M. Pain relief with intraar-
ticular or medial branch nerve blocks in patients with
positive lumbar facet joint SPECT imaging: a 12-week
outcome study. South Med J. 2008;101(9):931-934.
2. Birkenmaier C, Veihelmann A, Trouillier H, Hausdorf J,
von Schulze Pellengahr C. Medial branch blocks versus
pericapsular blocks in selecting patients for percutane-
ous cryodenervation of lumbar facet joints. Reg Anesth
Pain Med. 2007;32(1):27-33 27p.
3. Kaplan M, Dreyfuss P, Halbrook B, Bogduk N. The abil-
ity of lumbar medial branch blocks to anesthetize the
zygapophysial joint. A physiologic challenge. Spine.
1998;23(17):1847-1852.
4. Rocha ID, Cristante AF, Marcon RM, Oliveira RP, Le-
taif OB, Barros Filho TE. Controlled medial branch an-
esthetic block in the diagnosis of chronic lumbar facet
joint pain: the value of a three-month follow-up. Clinics.
2014;69(8):529-534.
5. Nath S, Nath CA, Pettersson K. Percutaneous lum-
bar zygapophysial (Facet) joint neurotomy using ra-
diofrequency current, in the management of chronic
low back pain: a randomized double-blind trial. Spine.
2008;33(12):1291-1297; discussion 1298.
6. Van Kleef M, Barendse GA, Kessels A, Voets HM, We-
ber WE, de Lange S. Randomized trial of radiofrequen-
cy lumbar facet denervation for chronic low back pain.
Spine (Phila Pa 1976). 1999;24(18):1937-1942.
7. Civelek E, Cansever T, Kabatas S, et al. Comparison of
eectiveness of facet joint injection and radiofrequen-
cy denervation in chronic low back pain. Turk Neurosurg.
2012;22(2):200-206.
8. Kroll HR, Kim D, Danic MJ, Sankey SS, Gariwala M,
Brown M. A randomized double blind prospective study
comparing the ecacy of continuous versus pulsed
radiofrequency in the treatment of lumbar facet syn-
drome. J Clin Anesth. 2008;20(7):534-537.
9. Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A
comparison of conventional and pulsed radiofrequency
denervation in the treatment of chronic facet joint pain.
Clin J Pain. 2007;23(6):524-529.
10. Lakemeier S, Lind M, Schultz W, et al. A comparison of
intraarticular lumbar facet joint steroid injections and
lumbar facet joint radiofrequency denervation in the
treatment of low back pain: a randomized, controlled,
double-blind trial. Anesth Analg. 2013;117(1):228-235.
11. Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol
M. Radiofrequency facet joint denervation in the treat-
ment of low back pain: a placebo-controlled clinical trial
to assess ecacy. Spine. 2001;26(13):1411-1416; discus-
sion 1417.
12. MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM,
Bogduk N. Lumbar medial branch radiofrequency neu-
rotomy in New Zealand. Pain Med. 2013;14(5): 639-645.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
168
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
168
QQ
Interventional Question 4. In patients with low back pain due to lumbar facet joint
arthropathy, does uoroscopically-guided neurotomy decrease the duration of
pain, decrease the intensity of pain, increase the functional outcomes of treatment
and improve the return-to-work rate?
Thermal radiofrequency ablation is suggested as a treatment for patients with low back pain
from the zygapophyseal joints. The outcomes of this procedure become more reliable when
more stringent diagnostic criteria are used. The relief from these ablations is durable for at
least 6 months following the procedure.
Grade of Recommendation: B
Nath et al
1
conducted a randomized controlled study
to determine the eectiveness of percutaneous ra-
diofrequency zygapophysial joint neurotomy in pa-
tients with lumbar zygapophysial joint pain. Patients
with LBP for at least 2 years who had at least 80%
pain relief after controlled medial branch blocks were
randomized to receive an active treatment with 2 mL
of bupivacaine (n=20) or sham with the same pro-
cedure without radiofrequency (n=20). The degree
and duration of pain (VAS) was recorded every hour
for 6 hours after the injection, the following day and
6-month follow-up. The active treatment group had
signicantly greater improvements in pain, quality
of life, analgesic consumption and global perception
of improvement compared to the sham group. The
authors concluded that radiofrequency facet dener-
vation can be used as a treatment for chronic LBP in
carefully-selected patients. This study provides Level
I evidence that, in patients undergoing dual diagnos-
tic comparative medial branch blocks with 80% relief,
radiofrequency ablation of the medial branch nerves
provides clinically and statistically signicant im-
provements in pain, quality of life variables and an-
algesic consumption compared to sham at 6 months.
Van Kleef et al
2
investigated the eectiveness of per-
cutaneous radiofrequency denervation of the lumbar
zygapophysial joints in the treatment of LBP origi-
nating from the lumbar zygapophysial joints. Patients
with LBP for at least one year who had a positive re-
sponse to a diagnostic nerve blockade were random-
ized to receive a 60-second 80°C radiofrequency le-
sion of the dorsal ramus of the segmental nerve roots
L3-L5 (n=15) or a control group of the same proce-
dure without radiofrequency current (n=16). Physical
impairment, global perceived eect, pain (VAS) and
disability (Oswestry disability scale) were record-
ed before the treatment and eight weeks after treat-
ment. Success was dened as ≥50% pain reduction on
global perceived eect and ≥2-points reduction on
the VAS scale. The radiofrequency group experienc-
es statistically signicantly greater improvements
in pain, global perceived eect and disability. There
were more successes in the radiofrequency group at
3, 6 and 12 months compared to the sham group. The
authors concluded that radiofrequency lumbar zyga-
pophysial joint denervation signicantly reduces pain
and functional disability on a short- and long-term
basis in a select group of patients with chronic LBP. In
critique of the methodology, the work group down-
graded this potential Level I study due to poor inclu-
sion criteria and no concealment prior to random-
ization. This study provides Level II evidence that,
in patients who have at least a 50% reduction in pain
from diagnostic medial branch blocks, radiofrequen-
cy ablation provides better improvements in pain and
functional outcomes than sham.
Civelek et al
3
compared the eectiveness of facet joint
injections and facet joint radiofrequency denervation
in patients with chronic LBP. Patients with LBP who
did not respond to conservative treatment and diag-
nosed with lumbar facet syndrome were randomized
to receive a facet joint injection (n=50) or facet joint
radiofrequency denervation at 80°C temperature for
120 seconds (n=50). The facet joint injection consist-
ed of a medial branch block of the posterior primary
ramus with 1 cc of methyl-prednisolone acetate (40
mg) (diluted with 1 cc SF) combined with 2 cc bupiv-
acaine hydrochloride (diluted with 2 cc SF). Pain (Vi-
sual Numeric Pain Scale), patient satisfaction (NASS)
and general health status (EQ-5D) were recorded at
baseline as well as 3, 6 and 12 months. The patients
who received facet joint radiofrequency denervation
experienced statistically signicantly greater im-
provements in pain at 1, 6 and 12 months. The au-
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
169
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
169
thors concluded radiofrequency denervation should
be used for the treatment of chronic LBP if pain re-
curs or if pain relief is not experienced after the rst
line facet joint injection. In critique of the methodol-
ogy, the work group downgraded this potential Level I
study due to poor selection criteria for facet joint pain.
This study provides Level II evidence that, in patients
without diagnostic blocks with suspected facet pain,
radiofrequency ablation shows better improvements
in pain at 6 months and one year when compared with
a medial branch steroid injection.
Kroll et al
4
conducted a prospective, randomize,
double-blind study to compare the ecacy of
continuous radiofrequency thermocoagulation
with pulsed radiofrequency in the treatment of
lumbar facet syndrome. Patients were randomly
allocated to receive continuous radiofrequency
thermocoagulation at 80°C for 75 seconds (n=13) or
pulsed radiofrequency at 42°C with a pulse duration
of 20 ms and pulse rate of 2 Hz for 120 seconds
(n=13). Pain (VAS) and disability (Oswestry Low Back
Pain and Disability Questionnaire) were assessed at
baseline and after 3 months. There were no signicant
dierences between groups in relative percentage of
improvement in pain or disability. The patients in the
continuous radiofrequency thermocoagulation group
experienced signicant improvement in pain and
disability over time while the pulsed radiofrequency
group did not experience any signicant changes
over time. The authors concluded that continuous
radiofrequency resulted in greater improvement over
time compared to pulsed radiofrequency. In critique,
the work group downgraded this potential Level I
study due to lack of follow-up and small sample size.
This study provides Level II evidence that thermal
radiofrequency ablation produces clinically and
statistically signicant improvements in pain and
function at 3 months when compared with pulse
radiofrequency.
Tekin et al
5
compared the eectiveness of conven-
tional radiofrequency and pulsed radiofrequency de-
nervation to medial branches of dorsal rami in the
treatment of facet joint pain. Patients with chronic
LBP for more than 6 months who responded to a di-
agnostic medial branch block (0.3 mL lidocaine 2%)
with greater than 50% pain reduction on VAS were
enrolled. Participants were randomly allocated into
a control group to receive local anesthetic (n=20), or
treatment groups to receive 80°C conventional radiof-
requency group (n=20), or 2 Hz pulsed radiofrequency
(n=20). Pain (VAS) and disability (Oswestry Disability
Index) were recorded before and after the procedure
as well as 6 months and one year after the procedure.
Pain and disability improved immediately after the
procedure in all groups, with lower scores in both
treatment groups compared to the control group. The
decrease in pain was maintained at 6- and 12-month
follow-ups in the conventional radiofrequency group,
but not the pulsed radiofrequency denervation group.
The authors concluded that both treatments were
safe and eective, but conventional radiofrequency
resulted in long-lasting facet joint pain relief. In cri-
tique of the methodology, the work group downgrad-
ed this potential Level I study due to poor inclusion
criteria. This study provides Level II evidence that, in
patients diagnosed with facet pain using a single me-
dial branch block and 50% relief, thermal radiofre-
quency ablation provides statistically signicant im-
provements in pain and function when compared to
pulsed radiofrequency ablation and sham.
In a double-blind randomized controlled trial,
Lakemeier et al
6
compared the eectiveness of
intra-articular facet joint steroid injections and
radiofrequency denervation for the treatment
of chronic LBP. Patients with LBP for at least 24
months who had hypertrophy of the facet joints
L3-4, L4-5, L5-S1 on magnetic resonance imaging
and experienced at least 50% pain reduction after
a test injection of local anesthetics were included in
this study. Participants were randomized to receive
radiofrequency denervation (n=27) or intra-articular
steroid inltration (n=29). Participants completed the
RMDQ, VAS and Oswestry Disability Index at baseline
and after 6 months. Both groups had improvements
with no signicant dierences between groups. This
study provides Level II evidence that, in patients who
receive a 50% reduction in pain with a single intra-
articular facet joint injection of local anesthetic,
intra-articular steroids provide similar results to a
radiofrequency ablation. Neither provides clinically
meaningful improvements at 6 months.
In a double-blind randomized controlled trial,
Leclaire et al
7
evaluated the ecacy of percutaneous
radiofrequency articular facet denervation for the
treatment of LBP. Patients with LBP for more than 3
months and positive response after uoroscopically-
guided intra-articular facet injections were enrolled.
Participants were randomized into a treatment group
to receive uoroscopically-guided percutaneous
radiofrequency articular facet denervation (n=36) or
control group to receive sham therapy of the same
procedure without denervation (n=34). Pain (VAS) and
disability (Oswestry and RMDQ scales) were recorded
at baseline and after 4 and 12 weeks. The treatment

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
170
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
170
group had signicantly greater improvement in
Roland-Morris scores compared to the control group
at 4 weeks, with no dierences in Oswestry or VAS.
There were no dierences between groups at 12
weeks in any outcomes. The authors concluded that
radiofrequency facet joint denervation may provide
short-term improvement in functional disability in
patients with chronic LBP, but the ecacy has not
been established. In critique of the methodology, the
work group downgraded this potential Level I study
due to poor inclusion criteria. This study provides
Level II evidence that patients who reported relief from
their back pain within one week of an intra-articular
steroid injection and undergo radiofrequency ablation
with the active tip of the needle placed perpendicular
to the nerve, report no improvement in pain at 3 and
12 months when compared with sham radiofrequency
denervation.
MacVicar et al
8
investigated the eectiveness of lum-
bar medial branch radiofrequency neurotomy for the
treatment of chronic LBP. Patients who experienced
complete relief of pain after controlled diagnostic me-
dial branch blocks (n=106) were treated with radiof-
requency neurotomy performed by 2 trained practi-
tioners. Pain relief of 80-100% for at least 6 months
with complete return to work and return to activities
of daily living without need for further health care
was classied as a successful outcome. Successful
outcomes were achieved in 58% and 53% of patients
at 2 dierent practices. The authors concluded that
lumbar radiofrequency neurotomy can be an eective
treatment for chronic back pain when performed in a
rigorous manner in appropriately-selected patients.
The study provides Level IV evidence that the major-
ity of patients selected by comparative lumbar facet
nerve blocks for radiofrequency neurotomies have
80–100% relief from their LBP with the restoration of
activities and no other health care for a median dura-
tion of 15 months. Further, patients that experienced
successful relief from their LBP after the rst radiof-
requency neurotomies will likely experience a similar
response to repeat radiofrequency neurotomies for
the same condition.
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
References
1. Nath S, Nath CA, Pettersson K. Percutaneous lum-
bar zygapophysial (Facet) joint neurotomy using ra-
diofrequency current, in the management of chronic
low back pain: a randomized double-blind trial. Spine.
2008;33(12):1291-1297; discussion 1298.
2. Van Kleef M, Barendse GA, Kessels A, Voets HM, We-
ber WE, de Lange S. Randomized trial of radiofrequen-
cy lumbar facet denervation for chronic low back pain.
Spine. 1999;24(18):1937-1942.
3. Civelek E, Cansever T, Kabatas S, et al. Comparison of
eectiveness of facet joint injection and radiofrequen-
cy denervation in chronic low back pain. Turk Neurosurg.
2012;22(2):200-206.
4. Kroll HR, Kim D, Danic MJ, Sankey SS, Gariwala M,
Brown M. A randomized double blind prospective study
comparing the ecacy of continuous versus pulsed
radiofrequency in the treatment of lumbar facet syn-
drome. J Clin Anesth. 2008;20(7):534-537.
5. Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A
comparison of conventional and pulsed radiofrequency
denervation in the treatment of chronic facet joint pain.
Clin J Pain. 2007;23(6):524-529
6. Lakemeier S, Lind M, Schultz W, et al. A comparison of
intraarticular lumbar facet joint steroid injections and
lumbar facet joint radiofrequency denervation in the
treatment of low back pain: a randomized, controlled,
double-blind trial. Anesth Analg. 2013;117(1):228-235.
7. Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol
M. Radiofrequency facet joint denervation in the treat-
ment of low back pain: a placebo-controlled clinical tri-
al to assess ecacy. Spine. 2001;26(13):1411-1416; dis-
cussion 1417.
8. MacVicar J, Borowczyk JM, MacVicar AM, Loughnan
BM, Bogduk N. Lumbar medial branch radiofrequency
neurotomy in New Zealand. Pain Med. 2013;14(5): 639-
645.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
171
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
171
QQ
Interventional Question 5. In patients with low back pain, do uoroscopically-
guided sacroiliac joint injections (SIJI) decrease the duration of pain, decrease the
intensity of pain, increase the functional outcomes of treatment and improve the
return-to-work rate?
a. Does duration of pain, intensity of pain, functional outcomes and return-to-
work status vary when candidates for neurotomy are determined by single vs.
comparative SIJI?
b. Is there a benet to performing lateral branch blocks as compared with
intra-articular diagnostic injections as a predictor to response to lateral branch
neurotomy?
c. Is there a threshold for the magnitude of relief from diagnostic SIJI that predict
improvement in duration of pain, intensity of pain, functional outcomes and return-
to-work status from SIJ neurotomy?
Intra-articular steroid joint injections may be considered in patients with suspected SI joint pain
Grade of Recommendation: C
Chakraverty et al
1
reported hospital audit results on
the outcomes of patients who underwent spinal in-
jection and interventional procedures for presumed
facet joint or sacroiliac joint pain. Retrospective chart
audits were performed of patients with chronic LBP
from 7 dierent hospitals. Patients were diagnosed
with either intra-articular facet joint injections, me-
dial branch blocks, or intra-articular sacroiliac joint
injections. Pain was recorded using a VAS; pain relief of
at least 50% indicated response to the diagnostic pro-
cedure. Patients were treated with lumbar facet injec-
tion (n=42), medial branch block (n=10), intra-artic-
ular sacroiliac injection with local anesthesia (n=52),
intra-articular facet injection with corticosteroid
(n=34), radiofrequency denervation of medial branch
(n=38), intra-articular sacroiliac injection with cor-
ticosteroid (n=33), or sacroiliac ligament prolother-
apy (n=19). Thirty percent of patients who received
an intra-articular corticosteroid injection reported
greater than 50% pain relief at 6-month follow-up.
The authors concluded that both radiofrequency de-
nervation and sacroiliac prolotherapy showed good
long-term outcomes at one year. There appears to be
a continuing role for intra-articular corticosteroid in-
jections. Sacroiliac ligament prolotherapy is worthy of
further study. This study provides Level IV evidence
that patients with mechanical LBP who receive a 50%
reduction in pain following a diagnostic sacroiliac
joint injection may experience up to 6 months of at
least 50% improvement from their LBP following SIJI
of local anesthetic and corticosteroid.
Cusi et al
2
investigated the eectiveness of prolother-
apy in the treatment of decient load transfer of the
sacroiliac (SI) joint. Patients diagnosed with persistent
suboptimal stability of the SI joint with LBP for at
least 6 months were enrolled (n=25). Participants un-
derwent three injections of prolotherapy with 6 weeks
between each injection. Disability (Roland-Morris)
and pain (Quebec Back Pain Disability Scale) were re-
ported 24 hours before each injection and one week
after each injection as well as at follow-up after 3, 12
and 24 months. Results revealed improvements at 3-,
12- and 24-month follow-up. The authors conclud-
ed that prolotherapy resulted in positive outcomes for
a majority of the patients who attended the 3-month
follow-up visit. This study provides Level IV evidence
that, in patients with sacroiliac joint pain diagnosed
using clinical criteria who undergo three prolothera-
py injections, 76% of patients will receive improve-
ments in pain and function at 12 months, though this
declines to 1/3 of patients at 24 months.
Slipman et al
3
evaluated the eectiveness of

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
172
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
172
uoroscopically-guided therapeutic SI joint injections
for sacroiliac joint syndrome in a retrospective study.
Patients with LBP who failed to improve after at least
4 weeks of physical therapy and who had a positive
response to a uoroscopically-guided diagnostic SI
joint injection were included. Participants received
up to four total therapeutic uoroscopically-guided
SI joint injections of 2.0 ml of betamethasone sodium
phosphate and acetate suspension, 6 mg/ml and 0.5
ml 2% lidocaine hydrochloride. Pain (VAS), disability
(Oswestry), work status and medication usage were
recorded at baseline and an average of 94.4 weeks after
the last injection. There were statistically signicant
improvements in disability, pain and work status over
time. The authors concluded that uoroscopically-
guided SI joint injections are clinically eective for the
treatment of SI joint syndrome. This study provides
Level IV evidence that patients with LBP and reduced
function due to sacroiliac joint dysfunction having an
80% improvement from a diagnostic sacroiliac joint
injection followed by an intra-articular steroid joint
injection experienced a clinically and statistically
signicant reduction in pain and disability scores. The
average number of injections was 2.1.
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
References
1. Chakraverty R, Dias R. Audit of conservative manage-
ment of chronic low back pain in a secondary care set-
ting -- part I: facet joint and sacroiliac joint interven-
tions. Acupunct Med. 2004;22(4):207-213.
2. Cusi M, Saunders J, Hungerford B, Wisbey-Roth T, Lu-
cas P, Wilson S. The use of prolotherapy in the sacroiliac
joint. Br J Sports Med. 2010;44(2):100-104.
3. Slipman CW, Lipetz JS, Plastaras CT, et al. Fluoroscop-
ically guided therapeutic sacroiliac joint injections
for sacroiliac joint syndrome. Am J Phys Med Rehabil.
2001;80(6):425-432.
QQ
Interventional Question 6. In patients with pelvic posterior girdle pain relieved
temporarily by image guided SIJ injections or lateral branch blocks, does lateral
branch neurotomy decrease the duration of pain, decrease the intensity of pain,
increase the functional outcomes of treatment and improve the return-to-work
rate?
Work Group Narrative: There are other studies in the literature that show clinical benets from
cooled lateral branch radiofrequency neurotomies for the treatment of sacroiliac joint pain that
were not included in our systematic review. These studies were omitted from our review because
they either did not fulll our initial denition or inclusion criteria, or were published after our litera-
ture search closed.
Cooled radiofrequency ablation of the sacral lateral branch nerves and dorsal ramus of
L5 may be considered in patients with sacroiliac joint pain diagnosed with dual diagnostic
blocks.
Grade of Recommendation: C
Kapural et al
1
retrospectively reviewed the eect of
cooled radiofrequency denervation on pain, function
and global patient satisfaction. Patients with chron-
ic LBP (n=27) who had >50% pain relief after 2 diag-
nostic sacroiliac joint (SI) joint blocks and underwent
cooled radiofrequency were included in this case se-
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
173
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
173
ries. Pain relief (VAS), function (pain disability in-
dex) and global patient satisfaction were analyzed.
Three to 4 months after the procedure, function and
pain scores signicantly improved functional capac-
ity and patient satisfaction. This study provides Lev-
el IV evidence that, in patients who experience a 50%
reduction in LBP with dual diagnostic intra-articular
injections, cooled radiofrequency ablation of the lat-
eral branch nerves and L5 dorsal ramus reduces pain
by approximately 50% in half the patients.
Karaman et al
2
evaluated the safety and ecacy
of cooled radiofrequency for sacral lateral-branch
denervation. Patients with chronic sacroiliac pain who
reported at least 75% pain relief from two diagnostic
joint blockages were included in this observational
study. Participants (n=15) received uoroscopically-
guided cooled radiofrequency denervation on the
dorsal ramus and the S1-3 lateral branches. Pain (VAS)
and physical function (Oswestry Disability Index) were
recorded after one, 3 and 6 months. Eighty percent of
the participants reported at least 50% reduction in
pain scores at 6 months. The authors concluded that
cooled radiofrequency for sacroiliac denervation was
eective and safe in the short to intermediate term.
This study provides Level IV evidence that, in patients
who reported a 75% reduction in pain with dual
diagnostic intra-articular SI joint injections, cooled
radiofrequency neurotomy of the lateral branch
nerves and L5 dorsal ramus produced a least a 50%
improvement in pain in roughly 80% of patients.
Future Directions for Research
1. The work group recommends future research on comparative studies be-
tween lateral branch blocks and intraarticular sacroiliac joint injections for the
diagnosis of sacroiliac joint pain versus pain from the posterior sacroiliac com-
plex.
2. The work group recommends randomized controlled trials of radiofrequency
denervation of the lateral branch nerves following lateral branch blocks.
3. The work group recommends randomized controlled trials comparing the var-
ious nerve ablation techniques of the lateral branch nerves for SI joint pain.
References
1. Kapural L, Nageeb F, Kapural M, Cata JP, Narouze S,
Mekhail N. Cooled radiofrequency system for the treat-
ment of chronic pain from sacroiliitis: the rst case-se-
ries. Pain Practice. 2008;8(5):348-354 347p.
2. Karaman H, Kavak GO, Tufek A, et al. Cooled radiof-
requency application for treatment of sacroiliac joint
pain. Acta Neurochir (Wien). 2011;153(7):1461-1468.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
174
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
174
QQ
Interventional Question 7. In patients with low back pain, does spinal cord
stimulation decrease the duration of pain, decrease the intensity of pain, increase
the functional outcomes of treatment and improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the use of spinal
cord stimulation as a treatment for low back pain.
Grade of Recommendation: I
Vallejo et al
1
investigated the eectiveness of spinal
cord stimulation for relieving discogenic pain in a
prospective observational study. Patients with intrac-
table discogenic LBP were enrolled. A control group
was formed of patients with insurance denial, medical
reasons, or failed trial (n=4) while the remaining par-
ticipants underwent spinal cord stimulation implan-
tation (n=9). Pain (Numerical Rating Scale), disability
(Oswestry Disability Index) and opioid use were re-
corded at intervals for twelve months. At 12 months,
there was no change in pain in the control group, but
signicant improvements were observed in the spi-
nal cord stimulation group. Disability decreased, but
there were no dierences in average disability be-
tween groups at 12 months. There was a 69% reduc-
tion in opioid consumption in the spinal cord stimu-
lation group and 54% increase in opioid consumption
in the control group. The authors concluded that spi-
nal cord stimulation may eectively improve pain and
disability and reduce opioid usage in patients with
discogenic pain. In critique of the methodology, the
work group downgraded this potential Level II article
to Level III due to the small sample size. This study
provides Level III evidence that, in patients with dis-
cogenic LBP diagnosed with provocative discography,
spinal cord stimulation produces clinically and statis-
tically signicant improvements in pain and function.
Future Directions for Research
The work group recommends randomized controlled trials utilizing spinal cord
stimulation in patients with LBP.
Reference
1. Vallejo R, Manuel Zevallos L, Lowe J, Benyamin R. Is
Spinal Cord Stimulation an Eective Treatment Option
for Discogenic Pain? Pain Pract. 2012;12(3):194-201.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
175
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
175
QQ
Interventional Question 8. In patients with low back pain, does continuous delivery
of intrathecal opioids decrease the duration of pain, decrease the intensity of pain,
increase the functional outcomes of treatment and improve the return-to-work
rate and are there risks associated with its use?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
QQ
Interventional Question 9. In patients with low back pain, is provocative lumbar
discography more accurate than other diagnostic modalities in identifying the disc
as a source of pain?
There is high-level evidence that provocative discography without manometric measure-
ments correlates with pain reproduction in the presence of moderate to severe disc degen-
eration on MRI/CT discography.
Grade of Recommendation: A
Chen et al
1
retrospectively investigated the relation-
ship between magnetic resonance (MR) ndings and
pain response during discography. Patients with LBP
for at least a year who underwent MRI and provoca-
tion discography were included (n=93). The MR im-
ages were interpreted by two experienced radiologists
and included the grading of disc degeneration (DD)
per Pearce grade I-V, the presence of high-intensity
zone (HIZ) and the presence of endplate abnormali-
ties (Modic changes). Discography was reviewed by
2 experienced radiologists who classied disc mor-
phology as Type I cotton ball; Type II, lobular; Type
III, irregular; Type IV, ssured; or Type V, ruptured.
Concordant pain (numeric rating scale) reported by
the patient during discography was considered pos-
itive. There were statistically signicant correlations
between concordant pain and Type IV-V discs on
discography, Grade IV-V DD on MR imaging, pres-
ence of HIZ and endplate abnormalities. The authors
concluded that DD grades on MR imaging were asso-
ciated with discographic grades. This study provides
Level I evidence that provocative discography without
manometric pressure measurements correlates with
grade IV-V DD, the presence of HIZ and endplate ab-
normalities on MRI.
Weishaupt et al
2
aimed to determine the eectiveness
of MR imaging abnormalities in predicting symptom-
atic disc derangement by investigating the relation-
ship with discography as the standard. Fifty patients
with chronic LBP underwent MR imaging followed by
lumbar discography with pain provocation test. MR
images were evaluated for DD, high-signal-intensity
zone and endplate abnormalities. Standard discogra-
phy was conducted and pain provocation was rated as
concordant, noncordant or painless. The abnormali-
ties on MR images were compared with disc morpho-
logic characteristics and pain response on discogra-

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
176
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
176
phy. When comparing abnormalities and considering
only moderate and severe type I and type II endplate
abnormalities, all injected discs caused concordant
pain with provocation (sensitivity, 38%; specicity,
100%; PPV, 100%). The authors concluded that DD
and presence of HIZ may not correlate to painful DD,
but moderate and severe endplate type I and type II
abnormalities on MR imaging may predict painful
disc derangement in patients with LBP. This study
provides Level I evidence that provocative discogra-
phy without manometry correlates with pain in the
presence of moderate to severe endplate abnormali-
ties on MRI. It did not correlate with HIZ and DD.
Vanharanta et al
3
investigated the relationship be-
tween radiographic ndings on CT and pain provoca-
tion discography. Patients with LBP (n=91) underwent
discography and CT/discography. Disc deterioration
on discogram was classied as normal, slight, mod-
erate or severe. Pain on provocation discography was
classied as no pain, dissimilar, similar or exact re-
production of clinical pain. The authors conclud-
ed that as disc deterioration increased, discography
was more likely to be painful and that CT/Discogra-
phy is a reasonable tool to demonstrate why injection
into a disc is provoking a patient’s clinical pain. This
study provides Level I evidence that provocative dis-
cography without manometry correlates with pain in
the presence of DD on CT scan post discography. The
absence of pain on provocative discography without
manometry correlates with a normal disc on CT scan
post discography.
Collins et al
4
compared magnetic resonance imaging
(MRI) ndings and lumbar provocative discogra-
phy in order to more precisely dene the role in each
pain diagnosis due to degenerative disc disease. Pa-
tients being considered for surgical treatment due to
spinal pain for more than 4 months that was not re-
lieved with conservative therapy were enrolled. After
patients were examined by MRI, they underwent dis-
cography and reported pain provoked. Seventy-three
levels were studied by discography in 29 subjects; 13 of
which reproduced the patient’s symptoms. The dis-
cography ndings correlated with MRI in 65 (89.5%)
subjects. The authors concluded that, of the patients
who underwent surgery, an annular bulge was present
in the majority. There were no specic features found
on the MR images to dierentiate symptomatic from
asymptomatic damaged discs. This study provides
Level III evidence that provocative discography with-
out manometric pressure measurements correlated
with DD on MRI scan 90% of the time. Seventy-ve
percent of patients who had a positive discography
did well with surgical fusion.
Lim et al
5
investigated the relationship between mag-
netic resonance (MR) and CT discography ndings
with pain response on provocative discography. Pa-
tients with discogenic back pain (n=47) were enrolled
in the study and underwent MR imaging followed by
CT discography. MR images were evaluated for DD,
endplate abnormalities, facet joint osteoarthritis and
high intensity zone. Pain during discography was re-
corded as concordant or discordant. In a total of 97
discs analyzed, there was a signicant correlation be-
tween concordant pain and grade 4 or 5 DD, high in-
tensity zone, combination of the above two ndings,
ssured and ruptured disc at discogram and contrast
beyond inner annulus on CT discogram. The authors
concluded that these ndings are typical with concor-
dant pain at discography. This study provides Level III
evidence that provocative discography without ma-
nometry correlates with concordant pain in the pres-
ence of grade 4-5 DD on MRI. The presence of annular
tearing on discography and postdiscography CT scan
also correlates with painful disc.
There is high-level evidence that provocative discography without manometric pressure mea-
surements correlates with the presence of endplate abnormalities on MRI imaging.
Grade of Recommendation: A
Chen et al
1
retrospectively investigated the relation-
ship between magnetic resonance (MR) ndings and
pain response during discography. Patients with LBP
for at least a year who underwent MRI and provoca-
tion discography were included (n=93). The MR im-
ages were interpreted by two experienced radiologists
and included the grading of DD (Pearce grade I-V), the
presence of high-intensity zone (HIZ) and the pres-
ence of endplate abnormalities (Modic changes). Dis-
cography was reviewed by two experienced radiolo-
gists who classied disc morphology as Type I cotton
ball; Type II, lobular; Type III, irregular; Type IV, s-

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
177
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
177
sured; or Type V, ruptured. Concordant pain (numeric
rating scale) reported by the patient during discogra-
phy was considered positive. There were statistical-
ly signicant correlations between concordant pain
and Type IV-V discs on discography, Grade IV-V DD
on MR imaging, presence of HIZ and endplate abnor-
malities. The authors concluded that DD grades on MR
imaging were associated with discographic grades.
This study provides Level I evidence that provocative
discography without manometric pressure measure-
ments correlates with grade IV-V DD, the presence of
HIZ and endplate abnormalities on MRI.
Weishaupt et al
2
aimed to determine the eectiveness
of MR imaging abnormalities in predicting symptom-
atic disc derangement by investigating the relation-
ship with discography as the standard. Fifty patients
with chronic LBP underwent MR imaging followed by
lumbar discography with pain provocation test. MR
images were evaluated for DD, high-signal-inten-
sity zone and endplate abnormalities. Standard dis-
cography was conducted and pain provocation was
rated as concordant, nonconcordant or painless. The
abnormalities on MR images were compared with
disc morphologic characteristics and pain response
on discography. When comparing abnormalities and
considering only moderate and severe type I and type
II endplate abnormalities, all injected discs caused
concordant pain with provocation (sensitivity, 38%;
specicity, 100%; PPV, 100%). The authors conclud-
ed that DD and presence of HIZ may not correlate to
painful DD, but moderate and severe endplate type I
and type II abnormalities on MR imaging may predict
painful disc derangement in patients with LBP. This
study provides Level I evidence that provocative dis-
cography without manometry correlates with pain in
the presence of moderate to severe endplate abnor-
malities on MRI. It did not correlate with HIZ and DD.
Bony vibration provocation may be considered to correlate with the presence of pain in patients
who have pain on provocation discography without manometric pressure measurements. There
is no correlation with the segmental level of pain.
Grade of Recommendation: C
Yrjama and Vanharanta
6
aimed to nd a noninvasive
tool for examining the intradiscal source of pain in pa-
tients with low back disorders. Patients with LBP un-
derwent an evaluation using an electrical tool to pro-
duce bony vibration to the lumbar spinal processes.
Participants indicated when pain was induced when
the vibrator, a standard electric toothbrush shaft with
a blunt head instead of a brush, compressed the lum-
bar spinal processes. Immediately following the eval-
uation, participants underwent discography evalua-
tion under uoroscopy with local anesthesia. Results
of pain provocation were compared between methods.
The sensitivity and specicity of the vibration test
was 0.71 and 0.63, respectively. The authors conclud-
ed that this non-invasive bony-vibration stimulation
test is easy, quick, inexpensive and reliable for ex-
amining intradiscal pain. In critique of the method-
ology, the work group noted that the bony vibration
provocation test was not used to identify a segmental
level of pain. For that reason, along with nonconsec-
utive patients and small sample size, the work group
downgraded the level of evidence for this potential
Level III study. This study provides Level IV evidence
that bony vibration provocation test may correlate
with the presence of pain on provocative discography
without manometry, although does not identify the
segmental level of pain.
With the same purpose of identifying a non-invasive
method for spine diagnostics, Yrjama et al
7
aimed to
compare ndings on ultrasound, bony vibration stim-
ulation and discography. Patients with LBP were en-
rolled in the study (n=38). Participants were evaluated
with ultrasound (discs were classied as Grade 0, 1, 2,
or 3 based on annular ruptures), bony vibration stim-
ulation (induced pain was recorded after compression
with a commercial electric toothbrush) and discogra-
phy (induced pain was recorded after standard uo-
roscopically-guided injections). The sensitivity and
specicity of the vibration provocation test in cases
of intradiscal ultrasound ndings was 0.90 and 0.75,
respectively; however, the sensitivity and specicity
was only 0.50 and 0.50 in ultrasound ndings of total
annular ruptures. The authors concluded that a com-
bination of ultrasound and the bony vibration test are
useful screening tests when evaluating LBP. In cri-
tique of the methodology, the work group downgraded
the level of evidence for this potential Level III study
as the quality of evoked pain was not dened, there
was no correlation between the segment of pain and
discography ndings, a poor reference standard was
used and due to nonconsecutive patients and small

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
178
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
178
sample size. This study provides Level IV evidence
that ultrasound and vibration screening may possibly
indicate that the spine is the source non-specic LBP.
Yrjama et al
8
later compared magnetic resonance im-
aging (MRI) and bony vibration test with discographic
pain provocation ndings in patients with LBP. Partic-
ipants (n=33) underwent evaluation by MRI, bony vi-
bration test and uoroscopically-guided discography.
The sensitivity and specicity of the bony vibration
test was 0.88 and 0.50, respectively. The authors con-
cluded that the addition of bony vibration stimulation
to MRI evaluation can provide more information on
the origin of LBP compared to MRI alone. In critique
of the methodology, the work group downgraded the
level of evidence for this potential Level III study due
to lack of a denition for evoked pain, poor reference
standard, nonconsecutive patients and a small sample
size. This study provides Level IV evidence that bony
vibration provocation test may correlate with the
presence of pain on provocative discography without
manometry, although does not identify the segmental
level of pain.
There is insucient evidence to make a recommendation for or against the use of axial loaded
magnetic resonance imaging (MRI) for the diagnosis of low back pain.
Grade of Recommendation: I
Hanna and Tommy
9
investigated the relationship be-
tween high-intensity zones (HIZ) and pressure-con-
trolled discography and aimed to determine if detec-
tion of HIZ was aected by axial load. Patients with
chronic LBP were enrolled (n=41) and underwent
pressure-controlled discography, CT, magnetic reso-
nance imaging (MRI) and axial loaded MRI. Presence
of HIZ was compared between MRI methods and pro-
voked pain was recorded as none, unfamiliar, simi-
lar, or exact, on discography. There were no signi-
cant correlations between HIZ and the pain response
at discography. The sensitivity, specicity, positive
predictive value and negative predictive value of HIZ
in detecting discs with “exact pain” on discography
was 0.49, 0.69, 0.39 and 0.76, respectively. The au-
thors concluded that HIZ was not inuenced by axial
load. This study provides Level I evidence that pres-
sure-controlled provocative discography does not
correlate with the presence of abnormal ndings on
axial loaded MRI.
There is conicting evidence that pressure controlled provocative discography correlates with
nuclear T2 signal intensity on magnetic resonance imaging (MRI) in patients with low back pain.
Grade of Recommendation: I
O’Neill et al
10
aimed to determine the accuracy of
magnetic resonance imaging (MRI) for the diagno-
sis of discogenic pain in an observational report of
patients with chronic LBP. Participants (n=143) un-
derwent MRI which were evaluated for high intensity
zone (HIZ), nuclear signal, disc height, disc contour
and bony marrow intensity change. Participants were
then evaluated using uoroscopically-guided dis-
cography using a syringe with an integrated pressure
transducer; pain provocation was classied as posi-
tive or negative at each disc. Moderate loss of nucle-
ar signal combined with disc bulge has a sensitivity
of 79.8% and specicity of 79.3% for the diagnosis
of discogenic pain. The authors concluded that MRI
parameters are correlated with each other and with
discography ndings. This study provides Level I evi-
dence that pressure-controlled provocative discogra-
phy correlates with pain in the loss of nuclear T2 sig-
nal intensity on MRI.
Scuderi et al
11
prospectively studied patients with
symptomatic lumbar degenerative disc disease to
investigate the relationship between magnetic reso-
nance imaging (MRI) grade, biochemical inamma-

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
179
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
179
tory markers and concordant pain on discography.
Participants (n=48) underwent MRI, discography
and biochemical analysis for inammatory markers.
Prrmann grading of MRI, concordant pain (VAS) on
discography and levels of biochemical inammatory
markers were compared. The authors concluded that
there are only weak correlations between demograph-
ic, discogram and radiographic variables. This study
provides Level I evidence that pressure-controlled
provocative discography does not correlate with Pr-
rmann scores on MRI.
There is conicting evidence that provocative discography without manometric pressure mea-
surements correlates with the presence of a high-intensity zone (HIZ) on MRI imaging.
Grade of Recommendation: I
Chen et al
1
retrospectively investigated the relation-
ship between magnetic resonance (MR) ndings and
pain response during discography. Patients with LBP
for at least a year who underwent MRI and provoca-
tion discography were included (n=93). The MR im-
ages were interpreted by 2 experienced radiologists
and included the grading of DD (Pearce grade I-V), the
presence of high-intensity zone (HIZ) and the pres-
ence of endplate abnormalities (Modic changes). Dis-
cography was reviewed by 2 experienced radiologists
who classied disc morphology as Type I cotton ball;
Type II, lobular; Type III, irregular; Type IV, ssured;
or Type V, ruptured. Concordant pain (numeric rating
scale) reported by the patient during discography was
considered positive. There were statistically signi-
cant correlations between concordant pain and Type
IV-V discs on discography, Grade IV-V DD on MR im-
aging, presence of HIZ and endplate abnormalities.
The authors concluded that DD grades on MR imaging
were associated with discographic grades. This study
provides Level I evidence that provocative discog-
raphy without manometric pressure measurements
correlates with grade IV-V DD, the presence of HIZ
and endplate abnormalities on MRI.
Weishaupt et al
2
aimed to determine the eectiveness
of MR imaging abnormalities in predicting symptom-
atic disc derangement by investigating the relation-
ship with discography as the standard. Fifty patients
with chronic LBP underwent MR imaging followed by
lumbar discography with pain provocation test. MR
images were evaluated for DD, high-signal-inten-
sity zone and endplate abnormalities. Standard dis-
cography was conducted and pain provocation was
rated as concordant, nonconcordant or painless. The
abnormalities on MR images were compared with
disc morphologic characteristics and pain response
on discography. When comparing abnormalities and
considering only moderate and severe type I and type
II endplate abnormalities, all injected discs caused
concordant pain with provocation (sensitivity, 38%;
specicity, 100%; PPV, 100%). The authors conclud-
ed that DD and presence of HIZ may not correlate to
painful DD, but moderate and severe endplate type I
and type II abnormalities on MR imaging may predict
painful disc derangement in patients with LBP. This
study provides Level I evidence that provocative dis-
cography without manometry correlates with pain in
the presence of moderate to severe endplate abnor-
malities on MRI. It did not correlate with HIZ and DD.
Saifuddin et al
12
retrospectively studied the relation-
ship between magnetic resonance imaging (MRI)
and discography ndings to determine the sensitiv-
ity of MRI in detecting painful annular tears mani-
fested by the high-intensity zone (HIZ). Patients
with LBP underwent MRI followed by discography
(n=58). MR images were evaluated for annular tears
based on presence of HIZ. Presence and site of dis-
rupted annulus and concordant pain reproduction on
discography were classied as a positive MRI. A HIZ
observed on MRI with normal discography was clas-
sied as a false-positive. Of the 152 discs examined
by discography, 27 HIZ were identied on MRI; 24
were associated with pain reproduction on discogra-
phy. The authors concluded that the high-intensity
zone is a marker of a painful posterior annular tear,
but its usefulness is limited by low sensitivity. This
study provides Level I evidence that provocative dis-
cography without manometry correlates with pain in
the presence of an HIZ on MRI. Provocative discogra-
phy without manometry also identied painful discs
without an HIZ.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
180
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
180
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
References
1. Chen JY, Ding Y, Lv RY, et al. Correlation between MR
imaging and discography with provocative concordant
pain in patients with low back pain. Clinical Journal of
Pain. 2011;27(2):125-130.
2. Weishaupt D, Zanetti M, Hodler J, et al. Painful lumbar
disk derangement: Relevance of endplate abnormalities
at MR imaging. Radiology. 2001;218(2):420-427.
3. Vanharanta H, Sachs BL, Spivey MA, et al. The relation-
ship of pain provocation to lumbar disc deterioration as
seen by CT/discography. Spine. 1987;12:295-298.
4. Collins CD, Stack JP, O’Connell DJ, et al. The role of dis-
cography in lumbar disc disease: a comparative study of
magnetic resonance imaging and discography. Clin Ra-
diol. 1990;42(4):252-257.
5. Lim CH, Jee WH, Son BC, Kim DH, Ha KY, Park CK. Dis-
cogenic lumbar pain: association with MR imaging and
CT discography. Eur J Radiol. 2005;54(3):431-437.
6. Yrjama M, Vanharanta H. Bony vibration stimulation:
A new, non-invasive method for examining intradiscal
pain. Eur Spine J. 1994;3(4):233-235.
7. Yrjama M, Tervonen O, Vanharanta H. Ultrasonic im-
aging of lumbar discs combined with vibration pain
provocation compared with discography in the diagno-
sis of internal anular ssures of the lumbar spine. Spine.
1996;21(5):571-575.
8. Yrjama M, Tervonen O, Kurunlahti M, Vanharanta H.
Bony vibration stimulation test combined with mag-
netic resonance imaging: Can discography be replaced?
Spine. 1997;22(7):808-813.
9. Hanna H, Tommy H. HIZ’s relation to axial load and low
back pain: Investigated with axial loaded MRI and pres-
sure controlled discography. Eur Spine J. 2013;22(4):734-
739.
10. O’Neill, C., et al. Accuracy of MRI for diagnosis of dis-
cogenic pain. Pain Phys. 2008;11(3): 311-326.
11. Scuderi GJ, Brusovanik GV, Golish SR, et al. A critical
evaluation of discography in patients with lumbar in-
tervertebral disc disease. Spine J. 2008;8(4):624-629.
12. Saifuddin A, Braithwaite I, White J, Taylor BA, Rent-
on P. The value of lumbar spine magnetic resonance
imaging in the demonstration of anular tears. Spine.
1998;23(4):453-457.
QQ
Interventional Question 10. In patients with low back pain, is anesthetic lumbar
discography more accurate than other diagnostic modalities in identifying the
disc as a source of pain?
There is insucient evidence to make a recommendation for or against the use of anesthetic
discography.
Grade of Recommendation: I
Alamin et al
1
prospectively compared the ndings
from standard pressure-controlled provocative dis-
cography and functional anesthetic discogram in pa-
tients with chronic LBP. Patients with chronic LBP in
consideration for surgery (n=52) underwent mag-
netic resonance imaging (MRI) followed by standard
pressure-controlled provocative discography. Pain
(VAS) and concordancy were reported. If the disc was
assessed as positive (greater than 5/10 on VAS and
“similar” or “exact” pain reproduction), functional
anesthetic discogram was performed. The functional
anesthetic discogram evaluation involved two sepa-
rate uoroscopically-guided injections of 4% lido-
caine and placebo (normal saline) into one or more
discs of the lumbar spine while the patient was in a
position or activity that typically caused pain. Pain
scores were compared at baseline and after each in-
jection. Forty-six percent of the patients had discor-
dant results of the pressure-controlled provocative
discography and functional anesthetic discogram. The
authors concluded that the ndings from the func-
tional anesthetic discogram diered from those of
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
181
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
181
standard pressure-controlled provocative discogra-
phy in 46% of the cases reported. This study provides
Level III evidence that there is a poor correlation be-
tween the ndings on provocation discography with
manometry and functional anesthetic discography.
Putzier et al
2
compared the results of provocative dis-
cography, discoblock (disc analgesia) and magnetic
resonance (MR) imaging ndings. Patients with LBP
for at least 6 months who had MR imaging with de-
generative disc disease Prrmann grade III or IV, with
or without Modic changes and with or without high in-
tensity zones (HIZ) were included (n=26). Participants
underwent MR discogram without an MRI-pressure
measurement syringe and reported pain (Numerical
Rating Scale, Dallas Discogram Scale) immediately
after injection. If there was no concordant pain (pain
endpoint) or fast/markedly manually-registered
elastic resistance (pressure endpoint) after 2.0 ml
contrast was applied, patients were categorized as the
contrast agent leak out through the annulus was reg-
istered in discogram (anatomic endpoint) or not (vol-
ume endpoint). Concordant pain was evoked in 35% of
the idiopathic degenerated discs and discoblock was
positive in 64%. Discoblock correlated with concor-
dant pain and Modic changes/discography endpoint.
The authors concluded that discoblock correlates
with concordant pain on provocative discography as
well as presence of Modic changes and can be added to
surgery decision-making in patients with idiopathic
degenerated discs. This study provides Level III ev-
idence that single injection anesthetic discography
correlates with a concordant response on provocative
discography without manometry.
Derby et al
3
compared data from a multicenter
prospective review against published results of
pain relief following injection of local anesthetic
into lumbar discs that caused concordant pain
during provocation testing. Patients who underwent
stand-alone analgesic discography (n=33), routine
provocative discography followed by injection of
local anesthetic (n=120), or provocation discography
followed by injection of local anesthetic through a
catheter (n=28) were included in the prospective data
review from 3 separate facilities. Two cohorts were
drawn from a previously published study of patients
who underwent conventional, pressure-controlled
provocation discography without anesthetic (n=23) or
provocative discography using an equal combination
of local anesthetic and contrast (n=47) were also
included. Subjective pain relief was compared for
each protocol. None of the patients who received
pressure-controlled provocation discography
without anesthetic had pain relief. Less than 10% of
the patients who underwent provocative discography
using an equal combination of local anesthetic and
contrast had pain relief. The authors concluded that
the stand-alone analgesic discography, provocative
discography followed by injection of local anesthetic
and provocative discography with injection of local
anesthetic through a catheter have similar results
in conrming painful annular tears by concordant
pain provocation and 80% or greater pain relief after
injection of local anesthetic to the lumbar disc. This
study provides Level IV evidence that local anesthetic
plus contrast produces similar results to contrast
alone in the performance of pressure-controlled
provocative discography. The addition of local
anesthetic reduces postdiscogram pain.
Ohtori et al
4
conducted a randomized controlled study
to compare discography and discoblock for the diag-
nosis of discogenic LBP. Patients with LBP and evi-
dence of DD on MRI were randomized to be evaluated
by discography or discoblock. Surgery was performed
if the procedure response was positive (n=15 in each
group). Pain (VAS, Japanese Orthopedic Association
Score) and disability (Oswestry Disability Index) were
recorded before and 3 years after surgery. The patients
who were evaluated with discoblock had signicantly
greater improvements in outcomes compared to those
evaluated with discography. The authors concluded
that discoblock with bupivacaine into the painful disc
was useful for the diagnosis of discogenic LBP com-
pared with discography. This study provides Level IV
evidence that pain and functional outcomes after sur-
gical fusion are improved more in patients who had
a single positive anesthetic discogram compared to
provocation discography without manometry.
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
182
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
182
References
1. Alamin TF, Kim MJ, Agarwal V. Provocative lumbar
discography versus functional anesthetic discography:
a comparison of the results of two dierent diagnostic
techniques in 52 patients with chronic low back pain.
Spine J. 2011;11(8):756-765.
2. Putzier M, Streitparth F, Hartwig T, Perka CF, Ho EK,
Strube P. Can discoblock replace discography for iden-
tifying painful degenerated discs? Eur J Radiol. 2013;
82(9): 1463-1470.
3. Derby R, Lee JE, Lee SH. Analgesic discography: Eect of
adding a local anesthetic to routine lumbar provocation
discography. Pain Med. 2010; 11:1335- 1342.
4. Ohtori S, Kinoshita T, Yamashita M, et al. Results of
surgery for discogenic low back pain: a randomized
study using discography versus discoblock for diagno-
sis. Spine. 2009;34(13): 1345-1348.
QQ
Interventional Question 11. In patients with low back pain, does intradiscal
injection decrease the duration of pain, decrease the intensity of pain, increase
the functional outcomes of treatment and improve the return-to-work rate?
Intradiscal steroids are suggested to provide short-term improvements in pain and func-
tion in patients with Modic changes.
Grade of Recommendation: B
Cao et al
1
conducted a double-blind, randomized,
controlled, prospective clinical study to evaluate the
eectiveness of intradiscal injection regimens for the
treatment of LBP. Patients with degenerative chronic
discogenic LBP and endplate Modic changes on mag-
netic resonance imaging (MRI) who received discog-
raphy but did not accept surgical operation were cat-
egorized into Group A (Modic change Type I and Type
I-predominated mixed Type I/II) or Group B (Mod-
ic change Type II and Type II-predominated mixed
Type I/II). Each group was randomized into one of
3 subgroups: (A1/B1) intradiscal injection of normal
saline, (A2/B2) intradiscal injection of diprospan, or
(A3/B3) intradiscal injection of diprospan mixed with
songmeile (cervus and cucumis polypeptide). Pain
(VAS) and disability (Oswestry Disability Index) were
recorded 3 and 6 months after the procedure. There
were no signicant dierences in outcomes between
Group A and Group B. There were no signicant
changes in pain or disability in subgroups 1 after 3 or 6
months. Subgroups 2 and 3 had signicant improve-
ments in pain and disability at both follow-up points,
with no signicant dierences between groups. The
authors concluded that intradiscal injection of corti-
costeroid could be a short-term ecient alternative
for discogenic LBP in patients with endplate Mod-
ic changes on MRI unwilling to accept surgery. This
study provides Level I evidence that intradiscal ste-
roid injections can provide pain relief in patients with
single level Modic changes and positive provocative
discography with contrast contained within the disc
space for up to 6 months.
Fayad et al
2
investigated the relationship between the
severity of Modic changes on magnetic resonance im-
aging (MRI) and clinical response to intradiscal cor-
ticosteroid injections in patients with chronic LBP.
Patients with chronic LBP with inammatory Modic
changes on MRI who had no response to conservative
treatment for 3 months were included. Patients were
classied as Modic type I with pure edema endplate
changes (n=37), Modic I-2 with mixture of Modic
type I and type II changes but predominantly edema
changes (n=25) and Modic II-1 with predominantly
fatty changes (n=12). All participants received a lum-
bar intradiscal injection of corticosteroids and report-
ed pain intensity (VAS) before and one, three and six
months after injection. Modic I and Modic I-2 groups

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
183
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
183
had signicantly greater reductions in pain scores
after one month compared to the Modic II-1 group.
The authors concluded that intradiscal injection of
corticosteroids can provide short-term treatment for
patients with chronic LBP and predominantly inam-
matory endplate changes. This study provides Level
III evidence that intradiscal steroid injections provide
short-term pain relief in patients with Modic changes.
There is insucient evidence that intradiscal steroids provide improvements in pain or function
in patients with discogenic low back pain.
Grade of Recommendation: I
Khot et al
3
conducted a randomized trial of patients
with chronic discogenic LBP to determine the ef-
fect of intradiscal steroid injections in clinical out-
comes after one year. Patients with concordant pain
on discography were randomized to receive an in-
jection into the disc space of normal saline (n=60) or
methylprednisolone (n=60). Patients reported pain
(VAS) and disability (Oswestry Disability Index) for 12
months post-injection (46 of 60 in the steroid group
and 52 of 60 in the saline group). There were no sig-
nicant dierences in percent change in disability or
change in pain score between the groups. The authors
concluded that intradiscal steroid injections do not
improve clinical outcomes in patients with discogenic
back pain. The work group downgraded this potential
Level I study due to low follow-up. This study pro-
vides Level II evidence that intradiscal steroids pro-
vide no benet over intradiscal saline in patients with
discogenic LBP.
Yavuz et al
4
investigated the eectiveness of intra-
discal steroid injections in patients with chronic LBP.
Patients with chronic LBP due to degenerative disc
disease (n=18) underwent provocative discography
to identify the discogenic pain level followed by in-
jection of 1 cc betamethasone. Patients reported pain
(VAS) and disability related to LBP (Quebec Back Pain
Disability Scale scores) before as well as 2 weeks and
3 months after injection. There was a signicant re-
duction in pain intensity and signicant improvement
in disability at 2 weeks and 3 months compared to
baseline. The authors concluded that intradiscal ste-
roid injection may provide short- and mid-term ef-
fectiveness in reducing pain intensity and improving
LBP-related disability. This study provides Level IV
evidence that intradiscal steroids result in improved
pain and function in patients with chronic LBP and
MRI ndings of dark disc, an HIZ or annular tearing
on discography.
There is insucient evidence to make a recommendation for or against the use of intradiscal
bone marrow concentrate in patients with discogenic low back pain.
Grade of Recommendation: I
Pettine et al
5
evaluated the safety and feasibility
of intradiscal bone marrow concentrate injections
for the treatment of discogenic LBP. Candidates
for surgery (failed conservative treatment) with
discogenic LBP for at least 6 months and evidence of
degenerative disc pathology on magnetic resonance
imaging (MRI) with modied Prmann grade of
IV-VII were included (n=26). Participants received
a uoroscopically-guided injection of intradiscal
bone marrow concentrate into the nucleus pulposus
of the symptomatic disc(s). Patients were clinically
evaluated and reported disability (Oswestry Disability
Index) and pain (VAS) prior to injection and 3, 6, 12
and 24 months after treatment. Twenty-four patients
avoided surgery for 12 months; 21 avoided surgery
throughout the 24-month follow-up period. Pain
and disability improved in the patients who avoided
surgery. The authors concluded that autologous
bone marrow concentrate is a safe and feasible non-
surgical treatment option for discogenic pain through
two years. This study provides Level IV evidence that
intradiscal injection of autologous bone marrow
concentrate may provide reductions in back pain and
disability at 2 years in patients with discogenic back
pain.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
184
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
184
There is insucient evidence to make a recommendation for or against the use of intradiscal
platelet rich plasma in patients with discogenic low back pain.
Grade of Recommendation: I
In a double-blind, randomized controlled study,
Tuakli-Wosornu et al
6
evaluated the eect of a
single injection of autologous platelet-rich plasma
(PRP) on pain and function. Patients with chronic
lumbar discogenic pain for at least 6 months who
were unresponsive to conservative treatment were
randomized to receive intradiscal PRP (n=36) or
contrast (n=22) after provocative discography. Pain
(Numeric Rating Scale, NRS) and physical function
(Functional Rating Index, FRI) were recorded after
one, 4 and 8 weeks, 6 months and one year. The
authors concluded that patients who received PRP had
signicant improvements in FRI and NRS Best Pain at
8 weeks compared to control; the FRI improvements
remained signicant at one year. This study provides
Level II evidence that intradiscal platelet-rich plasma
may provide improvements in pain and function as
compared with intradiscal contrast.
There is insucient evidence to make a recommendation for or against the use of intradiscal
Methylene Blue in patients with discogenic low back pain.
Grade of Recommendation: I
Peng et al
7
conducted a randomized placebo-
controlled trial to evaluate the eectiveness of
intradiscal methylene blue for the treatment of
chronic discogenic LBP. Patients with discogenic LBP
longer than 6 months who underwent discography
were randomized to receive injection of intradiscal
methylene blue (n=36) or placebo (n=36). Pain
(Numerical Rating Scale) and functional recovery
(Oswestry Disability Index) were recorded 6, 12 and
24 months after randomization. The participants who
received methylene blue had signicantly greater
improvements in pain and disability at 24-month
follow-up compared to the placebo group. There were
no adverse eects or complications in the methylene
blue group. The authors concluded that methylene
blue injections into painful discs is a safe, eective
and minimally-invasive method for the treatment
of intractable and incapacitating discogenic LBP.
This study provides Level I evidence that Intradiscal
Methylene Blue provides improvements in pain and
function when compared with intradiscal normal
saline in patients with chronic discogenic LBP.
Future Directions for Research
The work group recommends:
• High-level randomized controlled trials using platelet rich plasma and stem
cells in patients with disc degeneration
• Another RCT of intradiscal steroids in patients with Modic changes
• High-level randomized controlled trials Methylene Blue in patients with disc
degeneration
References
1. Cao P, Jiang L, Zhuang C, et al. Intradiscal injection ther-
apy for degenerative chronic discogenic low back pain
with end plate Modic changes. Spine J. 2011;11(2):100-
106.
2. Fayad F, Lefevre-Colau MM, Rannou F, et al. Relation
of inammatory modic changes to intradiscal steroid
injection outcome in chronic low back pain. Eur Spine J.
2007;16(7):925-931.
3. Khot A, Bowditch M, Powell J, Sharp D. The use of intra-
discal steroid therapy for lumbar spinal discogenic pain:
a randomized controlled trial. Spine. 2004;29(8):833-
836; discussion 837.
4. Yavuz F, Taskaynatan MA, Aydemir K, Ozgul A, Tan AK.
The ecacy of intradiscal steroid injections in degener-
ative lumbar disc disease. Turkiye Fiziksel Tip ve Rehabil-
itasyon Dergisi. 2012;58(2):88-92.
5. Pettine K, Suzuki R, Sand T, Murphy M. Treatment of
discogenic back pain with autologous bone marrow

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
185
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
185
concentrate injection with minimum two year fol-
low-up. Int Orthop. 2016;40(1):135-140.
6. Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, et al.
Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injec-
tions: A Prospective, Double-Blind, Randomized Con-
trolled Study. PM and R. 2016;8(1):1-10.
7. Peng B, Pang X, Wu Y, Zhao C, Song X. A randomized
placebo-controlled trial of intradiscal methylene blue
injection for the treatment of chronic discogenic low
back pain. Pain. 2010;149(1):124-129.
QQ
Interventional Question 12. In patients with low back pain, does intradiscal
electrothermal therapy or biacuplasty decrease the duration of pain, decrease the
intensity of pain, increase the functional outcomes of treatment and improve the
return-to-work rate?
Intradiscal electrothermal annuloplasty is suggested to provide improvements in pain and
function at up to two years. This treatment is limited in its eectiveness with roughly 40-50% of
patients receiving a 50% reduction in pain.
Grade of Recommendation: B
Pauza et al
1
conducted a randomized controlled trial
to investigate the eectiveness of intradiscal elec-
trothermal therapy (IDET) for the treatment of dis-
cogenic LBP. Patients with discogenic LBP greater
than 6 months were randomized after provocation
discography to receive IDET (n=37) or sham treat-
ment of introducing a needle onto the disc in the same
environment as the real procedure (n=27). IDET was
performed using a standard protocol, in which a exi-
ble electrode was navigated into the posterior annulus
of the painful disc and heated to 90°C. After heating
and removing the electrode, 1 cc of bupivacaine 0.75%
mixed with antibiotic was injected into the disc. Pain
and disability (VAS, Oswestry Disability Scale and
Short Form-36) were recorded before treatment and
six months after treatment. Eighty-ve percent and
89% of participants were included in follow-up anal-
ysis in the IDET group and sham group, respective-
ly. Both groups experienced improvements, but the
treatment group had signicantly greater improve-
ments compared to the sham group. The authors con-
cluded that the ecacy of IDET cannot be completely
attributed to a placebo eect. This study provides Lev-
el I evidence that IDET provides signicant improve-
ments in pain and function as compared with sham
at 6 months. Forty percent of treatment patients re-
ceived at least a 50% reduction in pain.
Bogduk et al
2
prospectively evaluated the ecacy of
intradiscal electrothermal anuloplasty (IDETA) for the
treatment of LBP. Patients with LBP related to inter-
nal disc disruption who underwent discography and
met inclusion criteria were allocated to a treatment
group to receive IDETA (n=36) or comparison group if
their insurer did not approve IDETA (n=17). The treat-
ment group underwent IDETA following standard
procedure in which an electrode was placed within
one to 3 electrode diameters from the outer surface of
the annulus brous and heater to 80-90°C. Cefalozin
was prophylactically administered intravenously be-
fore the procedure and intrasdiscally after the proce-
dure. The comparison group completed a 36-month
physical therapy program. Pain (VAS), return to work
and opioid consumption were assessed at baseline, 3
months, 12 months and 2 years after treatment. The
comparison group did not experience signicant im-
provement in their pain at any follow-up point. The
treatment group experienced signicant improve-
ments in median pain scores which was sustained at
all follow-up points. The authors concluded that IDE-
TA results in long-term results, 54% of patients can
reduce their pain by half and one in ve patients can
expect to achieve complete relief of pain. This study
provides Level II evidence that, in patients who had
IDETA, pain and functional outcomes remained im-
proved at 2 years.
In a randomized, double-blind, placebo-controlled
trial, Freeman et al
3
evaluated the safety and eca-
cy of intradiscal electrothermal therapy (IDET) for
the treatment of chronic discogenic LBP. Patients
with chronic discogenic LBP with evidence of one- or

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
186
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
186
2-level symptomatic DD with posterior or posterolat-
eral annular tears per provocative discography with
CT were included. Participants were randomized to
a treatment group to receive IDET (n=38) or place-
bo group to receive sham treatment (n=19). After the
IDET catheter was positioned to cover at least 75% of
the annular tear, the treatment group received elec-
trothermal energy while the placebo group did not.
Low Back Outcome Scores, Oswestry Disability Index,
Short Form-36, Zung Depression Index and Modied
Somatic Perceptions Questionnaire were measured
before treatment and after 6 months. There were no
signicant improvements in either group. The au-
thors concluded that IDET provides no signicant
benet over placebo but the procedure itself appeared
safe. The work group downgraded this potential Lev-
el II study due to the small sample size that does not
meet the power statement. This study provides Level
III evidence that IDET provides no improvements in
pain and function as compared with sham.
Biacuplasty is an option to produce clinically and statistically signicant improvements in pain
at 6 months in patients with discogenic low back pain.
Grade of Recommendation: C
Desai et al
4
aimed to investigate the eectiveness
of intradiscal biacuplasty compared to convention-
al medical management for the treatment of lumbar
discogenic pain in a multicenter randomized con-
trolled trial. Patients who underwent provocation dis-
cography and diagnosed with lumbar discogenic pain
were randomized to receive intradiscal biacuplasty
plus conventional medical management (n=29) or
individualized conventional medical management in-
cluding physical therapy, pharmacological manage-
ment, interventional procedures and lifestyle chang-
es (n=34). Pain (VAS), disability (Oswestry Disability
Index), physical functioning (Short Form-36), de-
pression (Beck Depression Inventory), Patient Global
Impression of Change, EQ-5D and back pain-related
medication usage were assessed at baseline and af-
ter 6 months. Patients were classied as responders
if they experienced a 2-point or 30% decrease in VAS
scores. The intradiscal biacuplasty group experienced
signicantly greater pain reduction compared to con-
ventional medical management alone. Dierences
in other outcomes favored intradiscal biacuplasty.
The authors concluded that intradiscal biacuplasty
is more eective for discogenic pain treatment than
conventional medical management alone. This study
provides Level I evidence that biaculoplasty provides
statistically signicant improvements in pain, but
no statistically signicant improvement in function
as compared with conservative management at 6
months.
Kapural et al
5
investigated the eectiveness of intra-
discal biacuplasty, a bipolar cooled radiofrequency
system, for the treatment of degenerative disc disease.
Patients with chronic LBP for more than 6 months
and concordant pain on provocative discography un-
derwent intradiscal biacuplasty (n=15). Biacuplasty
was performed under uoroscopy using 2 radiofre-
quency probes. Pain disability (Oswestry and Short
Form-36) and pain (VAS) were assessed at baseline
and after one, 3 and 6 months. There were no com-
plications related to the procedure. Pain and disability
improved at one month and remained improved af-
ter 6 months. The authors concluded that intradiscal
biacuplasty improves pain measures in patients with
discogenic pain. This study provides Level IV evidence
that biacuplasty produces clinically and statistical-
ly signicant improvements in pain in patients with
discogenic LBP.
Fukui and Rohof
6
aimed to study the eect of biannular
pulsed radiofrequency disc method in patients with
discogenic LBP. Patients with chronic discogenic LBP
that did not respond to conservative nonoperative
care (n=15) underwent the pulsed radiofrequency
technique involving 2 electrodes placed bilaterally
in the annulus in the disc to apply a radiofrequency
current for 12 minutes. Pain intensity (Numeric
Rating Scale) and disability (Roland-Morris Disability
Questionnaire) were measured at baseline and after
one week and one, 3 and 6 months after treatment.
Pain and disability improved signicantly at the
6-month follow-up compared to baseline. The authors
concluded that the biannular pulsed radiofrequency
technique using Diskit needles is a safe and minimally
invasive treatment option for patients with chronic
discogenic LBP. This study provides Level IV evidence
that biacuplasty produces clinically and statistically
signicant improvements in pain and function in
patients with discogenic LBP.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
187
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
187
In a prospective observational study, Karaman et al
7
evaluated the ecacy and safety of TransDiscal Bi-
acuplasty. Patients with chronic discogenic LBP for
at least 6 months, DD or internal disc disruption and
positive discography who did not respond to conser-
vative treatment were included. Participants (n=15)
underwent the procedure in which 2 radiofrequency
probes were passed through introducers and tted
into the disc with the probe tip in the posterior annu-
lus. TransDiscal Biacuplasty was applied for 15 min-
utes with the software set at a temperature of 45°C
and Ramp Rate of 2.0°C/min. Patients were recom-
mended to wear lumbar braces for 6-8 weeks after the
intervention. Physical function (Oswestry Disability
Index), pain (VAS) and patient satisfaction were re-
corded at baseline and one, 3 and 6 months after treat-
ment. At 6-month follow-up, 57.1% of patients had
at least 50% reduction in pain at 6-month follow-up
and 78.6% reported reduction of at least 2 points in
VAS. A total of 78.6% reported 10-point improvement
in physical function. There were no reported compli-
cations related to treatment. The authors concluded
that TransDiscal Biacuplasty is eective and safe. This
study provides Level IV evidence that biacuplasty pro-
duces clinically and statistically signicant improve-
ments in pain and function in patients with discogen-
ic LBP.
There is insucient evidence to make a recommendation for or against the use of percutane-
ous intradiscal radiofrequency thermocoagulation.
Grade of Recommendation: I
Kvarstein et al
8
conducted a randomized double-blind
controlled trial to evaluate the long-term safety and
ecacy of percutaneous intradiscal radiofrequen-
cy thermocoagulation with the discTRODE probe.
Patients with chronic LBP, evidence of moderate
structural DD on MRI and concordant pain on pres-
sure-controlled provocation discography were ran-
domized to receive intra-annular percutaneous in-
tradiscal radiofrequency thermocoagulation (n=10) or
sham (n=10). Pain intensity (Numeric Rating Scale),
Oswestry Disability Index and SF-36 were recorded
at baseline and after 6 and 12 months There were no
signicant dierences between groups at either fol-
low-up point. The authors concluded that there is no
evidence of percutaneous intradiscal radiofrequen-
cy thermocoagulation. The work group downgraded
this potential Level I study due to the small sample
size; the study was discontinued due to no benecial
eects shown. This study provides Level II evidence
that percutaneous intradiscal radiofrequency ther-
mocoagulation provides no improvements in pain and
function as compared with sham.
Future Directions for Research
The work group recommends a randomized controlled trial for biacuplasty.
References
1. Pauza KJ, Howell S, Dreyfuss P, Peloza JH, Dawson K,
Bogduk N. A randomized, placebo-controlled trial of
intradiscal electrothermal therapy for the treatment of
discogenic low back pain. Spine J. 2004;4(1):27-35.
2. Bogduk N, Karasek M. Two-year follow-up of a con-
trolled trial of intradiscal electrothermal anuloplasty
for chronic low back pain resulting from internal disc
disruption. Spine J. 2002 Sep-Oct;2(5):343-50.
3. Freeman BJ, Fraser RD, Cain CM, Hall DJ, Chapple DC.
A randomized, double-blind, controlled trial: intra-
discal electrothermal therapy versus placebo for the
treatment of chronic discogenic low back pain. Spine.
2005;30(21):2369-2377; discussion 2378.
4. Desai MJ, Kapural L, Petersohn JD, Vallejo R, Menzies
R, Creamer M, Gofeld M. A Prospective, Randomized,
Multicenter, Open-label Clinical Trial Comparing In-
tradiscal Biacuplasty to Conventional Medical Manage-
ment for Discogenic Lumbar Back Pain. Spine. 2016 Jul
1;41(13):1065-74.
5. Kapural L, Ng A, Dalton J, Mascha E, Kapural M, de la
Garza M, Mekhail N. Intervertebral disc biacuplasty for
the treatment of lumbar discogenic pain: results of a

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
188
Diagnosis & Treatment of Low Back Pain | Recommendations | Interventional Treatment
188
six-month follow-up. Pain Med. 2008 Jan Feb;9(1):60-
7.
6. Fukui S, Rohof O. Results of pulsed radiofrequency
technique with two laterally placed electrodes in the
annulus in patients with chronic lumbar discogenic Pain
J. 2012;26(4):606-609.
7. Karaman H, Tufek A, Kavak GO, et al. 6-month results
of TransDiscal Biacuplasty on patients with discogen-
ic low back pain: Preliminary ndings. Int J Med Sci.
2011;8(1):1-8.
8. Kvarstein G, Måwe L, Indahl A, Hol PK, Tennøe B, Di-
gernes R, Stubhaug A, Tønnessen TI, Beivik H. A ran-
domized double-blind controlled trial of intra-annular
radiofrequency thermal disc therapy--a 12-month fol-
low-up. Pain. 2009 Oct;145(3):279-86.
QQ
Interventional Question 13. In patients with low back pain, do trigger point
injections decrease the duration of pain, decrease the intensity of pain, increase
the functional outcomes of treatment and improve the return-to-work rate?
There is insucient evidence to make a recommendation for or against the use of trigger
point injections in the treatment of low back pain. The type of injectate does not inuence
outcomes.
Grade of Recommendation: I
In a randomized, double-blind study, Garvey et al
1
investigated the ecacy of trigger-point injection
therapy for the treatment of LBP. Patients who failed
four weeks of conservative treatment were included
in this study LBP (n=63). Patients were randomized
to receive an injection of lidocaine (n=13), lidocaine
combined with a steroid (n=14), a single dry-needle
stick (n=20), or vapocoolant spray with acupressure
(n=16). Patients rated their level of pain on a scale of
1 to 10, with 10 being the worst pain experienced, 2
weeks after injection. Patients reported improvement
in pain in the lidocaine injection group (40%), lido-
caine plus steroid group (45%), acupuncture group
(61%) and vapocoolant and acupressure (66%). The
authors concluded that trigger-point therapy is a use-
ful adjunct in treatment of low-back strain, but the
injected substance is not the critical factor. The work
group downgraded this potential Level I study due to
the short follow-up. This article provides Level II ev-
idence that trigger point therapies reduce pain in 40-
60% of patients at 2 weeks. The type of medication
used for injection does not aect the outcome.
De Andrés et al
2
conducted a double-blind randomized
controlled trial to evaluate the ecacy of type-A bot-
ulinum toxin for LBP relief. Patients with LBP due to
myofascial pain syndrome were enrolled (n=27). Each
patient received a uoroscopically-guided injection of
type-A botulinum toxin to a randomly-selected side
of the back and a control drug (NaCl 0.8% or bupiv-
acaine 0.25%) injected to the opposite side. Patients
completed questionnaires at baseline and after 15, 30
and 90 days to record pain (VAS), disability (Oswestry
Disability Index) and other lifestyle and psychologi-
cal characteristics. There were no signicant changes
in pain, daily life activities, or psychologic status be-
tween injections. The authors concluded that type-A
botulinum toxin can provide post-intervention pain
relief, but only with small dierences compared to
control treatments. The work group downgraded this
potential Level I study due to the small sample size.
This article provides Level II evidence that trigger
point injections with either botulinum toxin A or bu-
pivacaine or normal saline provide similar results;
none provide clinically meaningful improvements in
pain or function.
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
189
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
References
1. Garvey TA, Marks MR, Wiesel SW. A prospec-
tive, randomized, double-blind evaluation of trig-
ger-point injection therapy for low-back pain. Spine.
1989;14(9):962-964.
2. De Andres J, Adsuara VM, Palmisani S, Villanueva V,
Lopez-Alarcon MD. A double-blind, controlled, ran-
domized trial to evaluate the ecacy of botulinum tox-
in for the treatment of lumbar myofascial pain in hu-
mans. Reg Anesth Pain Med. 2010;35(3):255-260.
Recommendations | Interventional Treatment
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
190
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
190
Section Authors
Guideline Co-Chair
Paul G. Matz, MD
Surgical Treatment Section Chair
William C. Watters III, MD, MS
Members
Thiru M. Annaswamy, MD, MA
Steven W. Hwang, MD
Cumhur Kilincer, MD, PhD
RJ Meagher, MD
Anil K. Sharma, MD
Kris E. Radcli, MD, Stakeholder Representative:
American Academy of Orthopaedic Surgeons
QQ
Surgical Question 1. In patients with low back pain, does surgical treatment vs.
medical/interventional treatment alone decrease the duration of pain, decrease
the intensity of pain, increase the functional outcomes of treatment and improve
the return-to-work rate?
A systematic review of the literature yielded no studies to adequately address this question.
A systematic review of the literature yielded no studies to adequately address this question.
Work Group Narrative: Several frequently-referenced studies evaluating surgical treatment com-
pared to medical/interventional treatment were excluded because they did not meet inclusion cri-
teria. Patient populations with prior surgical treatment or pain below the knee without subgroup
analysis were primary factors for eliminating these studies.
Future Directions for Research
The work group recommends undertaking additional randomized controlled
trials comparing surgical treatment to medical/interventional treatment in pa-
tients with low back pain (LBP) only without history of prior lumbar surgery.
QQ
Surgical Question 2. In patients with low back pain, are there predictive factors
which determine the benet of initial treatment with surgical intervention versus
initial medical/interventional treatment?
Future Directions for Research
The work group recommends undertaking large database observational studies,
such as multi-center registry studies, examining the clinical characteristics asso-
ciated with clinical predictors for treatment options in patients with LBP only.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
191
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
191
QQ
Surgical Question 3. In patients undergoing fusion surgery for low back pain,
which fusion technique results in the best outcomes for the following: decreased
duration of pain, decreased intensity of pain, increased functional outcomes of
treatment and improved return-to-work rate?
a. Posterolateral fusion without internal xation versus
b. Posterolateral transverse fusion with internal xation versus
c. Stand-alone (anterior) interbody fusion versus
d. Transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody
fusion (PLIF) versus
e. Circumferential fusion (anterior interbody, lateral techniques)
There is insucient evidence to make a recommendation for or against a particular fusion
technique for the treatment of low back pain.
Grade of Recommendation: I
Madan et al
1
described a comparative study of 74 LBP
patients who received either instrumented circumfer-
ential fusion through a posterior approach (PLIF and
posterolateral fusion, n=35) or instrumented anteri-
or lumbar interbody fusion (ALIF) using the Hartshill
horseshoe cage (n=39). Although the article states
that study data was collected prospectively, it is un-
clear whether the study was carried out in this man-
ner. Therefore, the work group evaluated this study as
a retrospective analysis. Outcomes were assessed us-
ing the Oswestry Disability Index (ODI), quality of life
questionnaire (subjective), pain drawing, visual ana-
log scale (VAS), disability benet, compensation sta-
tus and psychological prole using the Modied So-
matic Perception Questionnaire (MSPQ) and the Zung
Depression Scale (ZDS). At follow-up, 74% of patients
in the circumferential fusion group and 72% in ALIF
group reported a satisfactory outcome (p <0.05) and
80% of patients in both groups reported satisfactory
outcomes according to ODI criteria. Return to work,
compensation and disability rates were also similar
between groups. Authors reported 4 complications
in the circumferential fusion group, including 3 in-
fections and 1 patient with persistent iliac crest do-
nor site pain for 4 months. Rates of complications in
the ALIF group were similar with infections in 2 pa-
tients and severe sciatica due to impingement from
the screw necessitating another operation in 1 patient.
The authors concluded that ALIF with the Hartshill
horseshoe cage and circumferential fusion using in-
strumented PLIF are both acceptable in the treatment
of discogenic back pain. This study provides Level III
therapeutic evidence that there were no dierences in
outcomes between circumferential fusion and ALIF
using Hartshill xation at 2 years follow-up.
Vamvanij et al
2
performed a retrospective analysis of
various fusion techniques in 56 patients with chron-
ic LBP. Patients received either posterolateral fusion
(PLF) with iliac crest autograft and translaminar fac-
et screw augmentation (Group 1, n=16), anterior ret-
roperitoneal interbody fusion (ALIF) with allograft
(Group 2, n=11), PLF with iliac crest autograft sup-
plemented with pedicle screw rod xation (Group 3,
n=13), or ALIF with threaded fusion cages and poste-
rior facet fusion with iliac crest autograft (Group 4,
n=16) and followed for a mean of 4.2 years. Pain in-
tensity, medication required, activity tolerance and
work status were evaluated on a 4-point scale (excel-
lent, good, fair, poor). The Dallas Pain Questionnaire
(DPQ) was used to evaluate the degree of pain inten-
sity on daily activities. At follow-up, solid fusion was
achieved in 50% of patients in Group 1, 60% in Group
2, 69% in Group 3 and 88% in Group 4. In Groups 1-4,
a satisfactory result was achieved in 38%, 36%, 46%
and 63%, respectively. Group 4 had signicantly low-
er DPQ scores compared to Groups 1 and 2 (p<0.05) at
follow-up. Thirty-one percent of patients in Groups
1 and 2 returned to work and 38% in Groups 3 and 4
returned to work by follow-up. There were no dif-
ferences in compensation status and disability peri-
ods between patients who were able and those unable
to go back to work in any group. Complications rates
were not discussed. The authors concluded that ALIF
using cages with posterior facet fusion oered the
highest fusion rate, pain relief and clinical success.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
192
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
192
In critique, this study had limited statistical analysis
and subgroup populations were small. Due to these
limitations, the work group downgraded the study
from Level III to Level IV. This study provides Level
IV therapeutic evidence that circumferential fusion is
correlated with better outcomes compared to both in-
strumented PLF and ALIF with allograft, but similar
in outcomes to PLF with autograft supplemented by
pedicle screw rod xation.
Future Directions for Research
The work group recommends the undertaking of:
1. Large database observational studies, such as multi-center registry studies,
examining various fusion techniques in patients with LBP only.
2. Randomized controlled trials examining various fusion techniques in patients
with LBP only.
3. Economic studies evaluating the cost-eectiveness of various fusion tech-
niques in patients with LBP only. Given the dearth of literature supporting supe-
riority of fusion technique in LBP patients, economic analysis studies are needed
to further investigate the costs associated with various techniques.
References
1. Madan SS, Boeree NR. Comparison of instrumented an-
terior interbody fusion with instrumented circumfer-
ential lumbar fusion. Eur Spine J. Dec 2003;12(6):567-
575.
2. Vamvanij V, Fredrickson BE, Thorpe JM, Stadnick ME,
Yuan HA. Surgical treatment of internal disc disruption:
an outcome study of four fusion techniques. J Spinal Dis-
ord. Oct 1998;11(5):375-382.
QQ
Surgical Question 4. In patients undergoing fusion surgery for low back pain,
are clinical outcomes, including duration of pain, intensity of pain, functional
outcomes and return-to-work status, dierent for multilevel fusions versus
single-level fusions?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends the undertaking of:
1. Large database observational studies, such as multicenter registry studies,
examining various fusion techniques, including single and multi-level fusions, in
patients with LBP only.
2. Randomized controlled trials examining various fusion techniques, including
single and multi-level fusion, in patients with LBP only.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
193
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
193
QQ
Surgical Question 5. In patients undergoing fusion surgery for low back pain, does
radiographic evidence of fusion correlate with decreased duration of pain, decreased
intensity of pain, increased functional outcomes of treatment and improved returnto
work rate?
There is insucient evidence to make a recommendation regarding whether radiographic evi-
dence of fusion correlates with better clinical outcomes in patients with low back pain.
Grade of Recommendation: I
Vamvanij et al
1
performed a retrospective analysis of
various fusion techniques in 56 patients with chron-
ic LBP. Patients received either posterolateral fusion
(PLF) with iliac crest autograft and translaminar fac-
et screw augmentation (Group 1, n=16), anterior ret-
roperitoneal interbody fusion (ALIF) with allograft
(Group 2, n=11), PLF with iliac crest autograft (Group
3, n=13), or ALIF with threaded fusion cages and pos-
terior facet fusion with iliac crest autograft (Group
4, n=16) and followed for a mean 4.2 years. Pain in-
tensity, medication required, activity tolerance and
work status were evaluated on a 4-point scale (excel-
lent, good, fair, poor). The Dallas Pain Questionnaire
(DPQ) was used to evaluate the degree of pain inten-
sity on daily activities. At follow-up, solid fusion was
achieved in 50% of patients in Group 1, 60% in Group
2, 69% in Group 3 and 88% in Group 4. Fifty percent
of patients who achieved solid fusion had satisfactory
results compared to only 28% of patients with pseu-
darthorisis (p <0.05). Return to work was also signi-
cantly higher in patients with successful fusion com-
pared to those without, 43% versus 17% (p<0.05). In
Groups 1-4, a satisfactory result was achieved in 38%,
36%, 46% and 63%, respectively. Group 4 had signi-
cantly lower DPQ scores compared to Groups 1 and 2
(p<0.05) at follow-up. Thirty-one percent of patients
in Groups 1 and 2 returned to work and 38% in Groups
3 and 4 returned to work at follow-up. There were no
dierences in compensation status and disability pe-
riods between patients who were able and those un-
able to go back to work in any group. Complications
rates were not discussed. The authors concluded that
ALIF using cages with posterior facet fusion oered
the highest fusion rate, pain relief and clinical suc-
cess. In critique, this study had limited statistical
analysis and subgroup populations were small. Due
to these weaknesses, the work group downgraded the
study from Level III to Level IV. This study provides
Level IV therapeutic evidence that there is a correla-
tion between solid fusion and functional outcomes.
Future Directions for Research
The work group recommends the undertaking of:
1. Large database observational studies, such as multi-center registry studies,
examining the correlation between radiographic evidence and functional and
clinical outcomes in patients with LBP only.
2. Randomized controlled trials examining the correlation between radiographic
evidence and functional and clinical outcomes in patients with LBP only.
Reference
1. Vamvanij V, Fredrickson BE, Thorpe JM, Stadnick ME,
Yuan HA. Surgical treatment of internal disc disruption:
an outcome study of four fusion techniques. J Spinal Dis-
ord. Oct 1998;11(5):375-382.
updated 8/10/2020
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
194
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
194
QQ
Surgical Question 6. In patients undergoing fusion surgery for low back pain,
does the use of bone growth stimulators (versus fusion alone) decrease the
duration of pain, decrease the intensity of pain, increase the functional outcomes
of treatment and improve the return-to-work rate?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends the undertaking of:
1.Large database observational studies, such as multi-center registry studies
examining the use of bone growth stimulators with fusion in patients with LBP
only.
2. Randomized controlled trials examining the use of bone growth stimulators
with fusion in patients with LBP only.
QQ
Surgical Question 7. In patients undergoing fusion surgery for low back pain, does
the use of BMP (versus fusion alone) decrease the duration of pain, decrease the
intensity of pain, increase the functional outcomes of treatment and improve the
return-to-work rate?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends the undertaking of:
1. Large database observational studies, such as multicenter registry studies ex-
amining the use of BMP with fusion in patients with LBP only.
2. Randomized controlled trials examining the use of BMP with fusion in patients
with LBP only.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
195
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
195
QQ
Surgical Question 8. In patients undergoing fusion surgery for low back pain, does
the use of minimally invasive techniques decrease the duration of pain, decrease
the intensity of pain, increase the functional outcomes of treatment and improve
the return-to work-rate compared to open fusion techniques?
A systematic review of the literature yielded no studies to adequately address this question.
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends the undertaking of:
1. Large database observational studies, such as multi-center registry studies
examining the use of various minimally invasive fusion techniques in patients
with LBP only.
2. Randomized controlled trials examining the use of various minimally invasive
fusion techniques in patients with LBP only.
QQ
Surgical Question 9. Inpatients undergoing surgery for low back pain, do motion
preserving systems (disc prosthesis and dynamic stabilization systems treatment)
decrease the duration of pain, decrease the intensity of pain, increase the functional
outcomes of treatment and improve the return-to-work rate compared to fusion
surgery?
Work Group Narrative: Several frequently referenced studies comparing motion preserving sys-
tems to fusion surgery were excluded because they did not meet inclusion criteria. Patient popula-
tions with prior surgical treatment or pain below the knee without subgroup analysis were primary
factors for eliminating these studies.
Future Directions for Research
The work group does not have any recommendations for future research on this
topic.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
196
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
196
A systematic review of the literature yielded no studies to adequately address this question.
QQ
Surgical Question 10. In patients undergoing surgery for low back pain, do motion
preserving systems (disc prosthesis and dynamic stabilization systems) result in
lower incidence of symptomatic adjacent segment disease?
Future Directions for Research
The work group recommends the undertaking of randomized controlled trials
evaluating the ecacy of motion preserving systems for the prevention of symp-
tomatic adjacent segment disease in patients with LBP only.
QQ
Surgical Question 11. In patients with low back pain, does fusion treatment
decrease the duration of pain, decrease the intensity of pain, increase the
functional outcomes of treatment and improve the return-to-work rate compared
to treatment with:
a. Discectomy
b. Discectomy plus rhizotomy
c. Decompression alone
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends the undertaking of:
1. Large database observational studies, such as multi-center registry studies,
examining discectomy with additional pain management techniques in patients
with LBP only.
2. Randomized controlled trials examining discectomy with additional pain man-
agement techniques in patients with LBP only.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
197
Diagnosis & Treatment of Low Back Pain | Recommendations | Surgical Treatment
197
QQ
Surgical Question 12. In patients with low back pain due to sacroiliac joint
dysfunction, does sacroiliac joint fusion compared with medical/interventional
treatment decrease the duration of pain, decrease the intensity of pain, increase
the functional outcomes of treatment and improve the return-to-work rate?
A systematic review of the literature yielded no studies to adequately address this question.
Work Group Narrative: The majority of literature evaluating sacroiliac joint dysfunction includes
patients with prior lumbar surgery (which is a frequently recognized predisposing factor for the
development of sacroiliac dysfunction) and/or lower limb pain (which is a common clinical nd-
ing in patients with sacroiliac dysfunction). This review examined only evidence in the subset
of patients without prior lumbar surgery and without pain below the knee. Additional literature
comparing surgical treatment to medical/interventional treatment including patients with prior
lumbar surgery or pain below the knee were not included in our systematic review. Therefore, a
denitive statement favoring sacroiliac fusion over medical/interventional treatment in patients
suering with LBP from an SI source cannot be made.
Future Directions for Research
The work group recommends additional randomized controlled trials (non-
industry funded) to conrm the superiority of surgical treatment for SJD in
patients failing medical/interventional treatment.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
198
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
198
Section Authors
Guideline Co-Chair
Paul G. Matz, MD
Cost-Utility Section Chair
Zoher Ghogawala, MD
Members
Simon Dagenais, DC, PhD, MSc
Jerey A. King, DC, MS
Paul Park, MD
Daniel R. Perry, PT
Jonathan N. Sembrano, MD
Padma Gulur, MD, Stakeholder Representative,
American Society of Anesthesiologists (ASA)
John E. O’Toole, MD, MS, Stakeholder Representative,
American Association of Neurological Surgeons/Congress
of Neurological Surgeons Joint Section on Spine and
Peripheral Nerves (AANS/CNS)
Introduction
The cost of low back pain (LBP) in our society has
reached staggering proportions. Some studies esti-
mate that LBP costs as much as all cancer care in the
United States.
1
Overall cost of LBP might be as much
as 100 billion dollars per year including indirect costs
such as lost productivity.
2
There is enormous practice
variation as it relates to the management of LBP. Uti-
lization of advanced imaging diers widely and uti-
lization of interventional treatments and surgery are
also sources of variation.
3-5
Cost-eectiveness and
cost-utility research permits valid comparison of dif-
ferent approaches to managing LBP. The purpose of
this section of the guideline is to summarize the evi-
dence on cost-utility analysis as it relates to the man-
agement of LBP.
A cost-utility analysis is a specic type of cost-
eectiveness evaluation that compares 2 or more
alternative treatment strategies in terms of both
cost and outcome. Outcomes are measured in terms
of quality-adjusted life years (QALYs) gained using
a preference-based health-related quality of life
(HR-QOL) outcome tool, such as the EQ-5D (EuroQol
Group).
6-7
An alternative , the SF-6D, which consists
of 11 items from the short form 36 item Health Survey
(SF-36)
8
, is also used in some studies.
9
Preference-
based HR-QOL is reported as a number from 0 (death)
to 1 (perfect health). QALYs gained are determined by
multiplying the number of years in a given health state
by the preference-based HR-QOL score. For example,
a single year spent in perfect health would be 1 QALY.
10
In order to compare the cost-utility of two interven-
tions, A and B, it is important to calculate the incre-
mental cost-utility ratio: Cost of B – Cost of A/ (QALYs
gained from B-QALYs gained from A).
10
In general,
a treatment is considered to be cost-eective in our
society when a treatment costs less than $100,000/
QALY gained.
11
Calculating costs is often challenging. Costs are not
the same as charges. Direct costs are health costs that
involve physician time/expertise, facility cost and
material costs (eg, implant costs). Indirect costs re-
fer to loss of productivity or costs associated with a
patient’s inability to function (need for home health
aide or nurse).
10
In general, a comprehensive eco-
nomic analysis should include both direct (inpatient
and outpatient) health costs along with indirect costs,
which can sometimes be much greater over time than
direct costs alone.
In this section of the guideline, we have included only
papers that provided valid cost-utility analyses. In
some of the sections, there were no papers that sat-
ised the criteria of a true cost-utility analysis and
therefore no recommendation could be issued. It is
important to note that cost-utility is largely depen-
dent upon the country and health system in which the
research was performed.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
199
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
199
References:
1. Martin BI, Deyo RA, Mirza SK, et al. Expenditures and
health status among adults with back and neck prob-
lems. JAMA. 2008;299(6):656-664.
2. Katz JN. Lumbar disc disorders and low-back pain: so-
cioeconomic factors and consequences. J Bone Joint Surg
Am. 2006;88 Suppl 2:21-24.
3. Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An
international comparison of back surgery rates. Spine.
1994;19(11):1201-1206.
4. Volinn E, Mayer J, Diehr P, Van Koevering D, Connell FA,
Loeser JD. Small area analysis of surgery for low-back
pain. Spine. 1992;17(5):575-581.
5. Chou R, Qaseem A, Snow V, et al. Diagnosis and treat-
ment of low back pain: a joint clinical practice guideline
from the American College of Physicians and the Amer-
ican Pain Society. Ann Intern Med. 2007;147(7):478-491.
6. Rabin R, de Charro F. EQ-5D: a measure of health status
from the EuroQol Group. Ann Med. 2001;33(5):337-343.
7. Suhonen R, Virtanen H, Heikkinen K, et al. Health-re-
lated quality of life of day-case surgery patients: a pre/
posttest survey using the EuroQoL-5D. Qual Life Res.
2008;17(1):169-177.
8. Brazier J, Usherwood T, Harper R, Thomas K. Deriving
a preference-based single index from the UK SF-36
Health Survey. J Clin Epidemiol. 1998;51(11):1115-1128.
9. Brazier J, Roberts J, Deverill M. The estimation of a
preference-based measure of health from the SF-36. J
Health Econ. 2002;21(2):271-292.
10. Ghogawala Z, Whitmore RG, Watters WC, 3rd, et al.
Guideline update for the performance of fusion proce-
dures for degenerative disease of the lumbar spine. Part
3: assessment of economic outcome. J Neurosurg Spine.
2014;21(1):14-22.
11. Braithwaite RS, Meltzer DO, King JT, Jr., Leslie D, Rob-
erts MS. What does the value of modern medicine say
about the $50,000 per quality-adjusted life-year deci-
sion rule? Med Care. 2008;46(4):349-356.
QQ
Cost-Utility Question 1. Who is the most cost-eective spinal care provider for
evaluating patients with low back pain:
a. Chiropractor versus
b. Physical Therapist versus
c. Primary Care Provider (including nonphysician providers) versus
d. Neurologist versus
e. Physiatrist versus
f. Spine Surgeon versus
g. Anesthesiologists/Pain Medicine Physician versus
h. Radiologist
A systematic review of the literature yielded no studies to adequately address this question.
Work Group Narrative: Dierential utilization of advanced imaging among providers would be expect-
ed to inuence cost of evaluating patients with LBP, but a thorough review of the literature did not iden-
tify any true cost-utility studies that permitted any recommendation to be made regarding the eect of
provider on the cost-utility. One study
1
found that the cost of evaluating LBP was higher for orthopedic
spine surgeons compared with general practitioners; however, there were no outcomes assessed and
therefore no conclusion could be made regarding cost-eectiveness or cost-utility.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
200
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
200
Future Directions for Research
Future studies would need to compare dierent providers by collecting all health
resource cost data including indirect costs (eg, loss of work productivity) as well
as measurement of health utility using a validated health preference quality of
life tool such as the EQ-5D in order to generate true cost-utility comparisons.
References
1. Shekelle PG, Markovich M, Louie R. Comparing the
costs between provider types of episodes of back pain
care. Spine. 1995;20(2):221-227.
QQ
Cost-Utility Question 2. What is the cost-utility of diagnostic imaging studies/
workup in the evaluation of low back pain (acute, subacute and chronic), in terms
of inuencing/altering treatment or in terms of leading to pain reduction and
functional improvement?
a. X-rays (lumbar standing, lumbar exion-extension, entire spine)
b. CT scan / CT myelogram
c. MRI (conventional or dynamic/upright/weight bearing)
There is insucient evidence to make a recommendation for or against the cost-eectiveness
of the use of routine ordering of lumbar spine radiographs for low back pain lasting greater than
6 weeks in the absence of red ags.
Grade of Recommendation: I
Kendrick et al
1
and Miller et al
2
reported on a
multicenter randomized controlled trial in the United
Kingdom with a patient preference arm to test the
hypotheses that lumbar spine radiography in primary
care patients with LBP is not associated with improved
outcomes, is not associated with changes in patient
management and is not cost-eective compared
with usual care. Patients with LBP ≥6 months were
randomized to receive general care from their general
practitioner (n=211) or a lumbar spine radiograph
with explanation from their general practitioner
(n=210). Participants completed questionnaires
and interviews at baseline, 3 and 9 months, which
included the Roland Morris Disability Questionnaire
(RMDQ) score, a VAS for pain, EuroQol-5 (EQ-5D) and
use of health services. An intention-to-treat analysis
and economic evaluation with a societal perspective
were completed. Additionally, 55 participants entered
a patient preference arm of the study and were given
the option to choose to have an x-ray (58%). Kendrick
et al
1
concluded that, in the studied population, lumbar
spine radiography is not associated with improved
functioning, severity of pain or overall health status
and is associated with an increased in workload for the
general practitioner. In critique of the methodology,
the work group downgraded this potential Level I
article due to the heterogeneous patient population.
This study provides Level II evidence that cost
per quality-adjusted life-year (QALY) gained is
redundant and no signicant dierence between the
EQ-5D scores for the groups was found. Additional
QALYs cannot be gained at any cost using lumbar
spine radiography. Lumbar spine radiographs for the
evaluation of LBP lasting >6 weeks in the absence of
red ags is not cost-eective. Miller et al
2
concluded
that lumbar spine radiography is associated with
increased patient satisfaction, but not improvement
in clinical outcomes. The work group downgraded this
potential Level I study due to the heterogeneous patient
population. This study provides Level II evidence that
radiography is likely to be cost-eective only when
satisfaction is valued relatively highly. Strategies to
enhance satisfaction for patients with LBP without
using lumbar radiography should be pursued.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
201
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
201
Work Group Narrative: A thorough review of the literature failed to yield any true cost-utility studies
that permit any recommendations to be made regarding treatment eect cost-utility of the use of MRI,
CT scan, or CT-myelogram; and the same review yielded limited evidence regarding the use of plain
radiographs. Additional literature that evaluated diagnostic imaging studies in the evaluation of low
back pain that did not meet this guideline’s inclusion criteria were not included in our systematic re-
view. Therefore, a denitive statement of the cost-utility of diagnostic imaging studies/workup for all
patients with LBP cannot be made.
Future Directions for Research
Intuitively, it would not be expected that diagnostic imaging would provide a
positive cost-utility in terms of inuencing physical treatment, pain reduction,
or functional improvement in patients with LBP. The work group recommends
prospective studies evaluating implementation of patient education programs
regarding the utility of imaging in order to align patient expectations with imag-
ing utility, improve patient satisfaction and reduce cost.
References
1. Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R,
Pringle M. The role of radiography in primary care pa-
tients with low back pain of at least 6 weeks duration: a
randomised (unblinded) controlled trial. Health Technol
Assess. 2001;5(30):1-69.
2. Miller P, Kendrick D, Bentley E, Fielding K. Cost-eec-
tiveness of lumbar spine radiography in primary care
patients with low back pain. Spine. 2002;27(20):2291-
2297.
QQ
Cost-Utility Question 3. Does the use of ordering physician-owned diagnostic and
treatment facilities aect the cost of low back pain related healthcare services?
A systematic review of the literature yielded no studies to adequately address this question.
Work Group Narrative: Although a systematic review of the literature revealed no publications directly
answering the question of whether physician ownership alters the cost-utility of diagnostic or treatment
services for patients with LBP, some publications have suggested a possible connection. Although
methodological deciencies in these publications (including the absence of rigorous cost-utility anal-
yses) excludes them from forming an evidence base for recommendations in this guideline, they serve
as a foundation for future research in this area.
Future Directions for Research
It is thought that nancial incentives may, in some cases, inuence clinical
decision-making. Physician ownership of diagnostic or treatment facilities
could theoretically increase rates of referral and utilization of those facilities by
the owning physicians or colleagues. In the case of patients with LBP, early or
frequent ordering of diagnostic imaging or of therapeutic interventions when not
clearly indicated could produce higher overall costs in the care of these patients.
The work group recommends prospective comparative studies to understand
how physician owned treatment facilities might inuence the cost-utility of the
care of patients with LBP.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
202
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
202
Cost-Utility of Medical/Interventional Treatments Questions
QQ
Cost-Utility Question 4. Are epidural steroid injections (including interlaminar,
transforaminal and caudal injections and selective nerve root blocks) more cost-
eective in the management of patients with low back pain than other medical/
interventional treatments?
A systematic review of the literature yielded no studies to adequately address this question.
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that future studies assessing epidural steroid in-
jections for LBP should consider including cost-utility analysis.
QQ
Cost-Utility Question 5. Is spinal cord stimulation more cost-eective in the
management of patients with low back pain than other medical/interventional
treatments?
Future Directions for Research
The work group recommends that future studies assessing spinal cord stimula-
tion for LBP should consider including cost-utility analysis.
QQ
Cost-Utility Question 6. Is physical therapy in the management of patients with
low back pain more cost-eective than other medical/interventional treatments?
There is insucient evidence to make a recommendation for or against the cost-utility of
physical therapy in the management of low back pain versus other medical/interventional
treatments.
Grade of Recommendation: I
The UK BEAM Trial Team
1
conducted a cost-utility
analysis with a pragmatic randomized trial to assess
the cost-eectiveness of adding spinal manipulation,
exercise classes or combined treatment to usual care
for patients with LBP. In this multicenter study in the
United Kingdom, 1,287 participants were randomized
into 4 groups: the “best care” group (n=326) to re-
ceive activ
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
203
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
203
e management and The Back Book, the exercise pro-
gram group (n=297) with up to 9 community class-
es over 12 weeks in addition to “best care,” the spi-
nal manipulation group (n=342) with 8 sessions over
12 weeks in addition to “best care,” or the combined
group (n=322) which included 6 weeks of manipula-
tion and 6 weeks of exercise in addition to “best care.”
Participants completed questionnaires which includ-
ed the EQ-5D at baseline, 3 months and 12 months.
Health care costs, quality adjusted life years (QALYs)
and cost per QALY were assessed over 12 months. All
three treatments improved the average QALY com-
pared to usual care alone. The authors concluded
that spinal manipulation is a cost-eective addition
to “best care” for back pain in general practice and
may have a better value for money alone compared to
manipulation with exercise. This study provides Lev-
el II evidence that exercise therapy alone may not be
cost-eective when compared to other therapies for
LBP.
Future Directions for Research
The work group recommends that future studies assessing physical therapy in
the management of LBP versus other medical/interventional treatments should
consider including cost-utility analysis.
Reference
1. UK BEAM Trial Team. United Kingdom back pain ex-
ercise and manipulation (UK Beam) randomised trial:
cost eectiveness of physical treatments for back pain
in primary care. BMJ. 2004 Dec 11: 329(7479): 1381. Epub
2004 Nov 19.
QQ
Cost-Utility Question 7. Is pharmacological management (over-the-counter
+ prescription medications) for patients with low back pain more or less cost-
eective than interventional treatments including physical therapy and injection
therapies?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that future studies assessing pharmacological
treatment alone for LBP should consider including cost-utility analysis.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
204
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
204
QQ
Cost-Utility Question 8. Is spinal manipulative therapy in the management of
patients with low back pain more cost-eective than other medical/interventional
treatments?
There is insucient evidence to make a recommendation for or against the cost-utility of spi-
nal manipulative therapy for the treatment of low back pain.
Grade of Recommendation: I
The UK BEAM Trial Team
1
conducted a cost-utility
analysis with a pragmatic randomized trial to assess
the cost-eectiveness of adding spinal manipulation,
exercise classes, or combined treatment to usual care
for patients with LBP. In this multicenter study in the
United Kingdom, 1287 participants were random-
ized into four groups: the “best care” group (n=326)
to receive active management and The Back Book, the
exercise program group (n=297) with up to 9 com-
munity classes over 12 weeks in addition to “best
care,” the spinal manipulation group (n=342) with 8
sessions over 12 weeks in addition to “best care,” or
the combined group (n=322) which included 6 weeks
of manipulation and 6 weeks of exercise in addition
to “best care.” Participants completed questionnaires
which included the EQ-5D at baseline, 3 months and
12 months. Healthcare costs, quality adjusted life
years (QALYs) and cost per QALY were assessed over
12 months. All three treatments improved the aver-
age QALY compared to usual care alone. The authors
concluded that spinal manipulation is a cost-eec-
tive addition to “best care” for back pain in general
practice and may have a better value for money alone
compared to manipulation with exercise. This study
provides Level II evidence that spinal manipulation
is a cost-eective treatment for LBP compared with
other medical interventional therapies.
Future Directions for Research
The work group recommends that future studies assessing spinal manipulative
therapy for LBP should consider including cost-utility analysis.
Reference
1. UK BEAM Trial Team. United Kingdom back pain ex-
ercise and manipulation (UK Beam) randomised trial:
cost eectiveness of physical treatments for back pain
in primary care. BMJ. 2004 Dec 11: 329(7479): 1381. Epub
2004 Nov 19.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
205
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
205
QQ
Cost-Utility Question 9. Is acupuncture-based therapy in the management of
patients with low back pain more cost-eective than other medical/interventional
treatments?
Acupuncture-based therapy in the management of patients with low back pain is suggested to
be cost-eective when compared with other medical/interventional treatments.
Grade of Recommendation: B
Witt et al
1
conducted a randomized controlled trial
with a nonrandomized observational cohort in or-
der to evaluate the cost-eectiveness of acupunc-
ture in addition to routine care compared to routine
care alone for patients with chronic LBP ≥6 months in
Germany. Participants who agreed to take part in the
RCT were randomized into an immediate acupunc-
ture group (n=1,309 included in analysis) or a delayed
acupuncture group to receive acupuncture 3 months
later (n=1,183 included in analysis). If patients did not
consent to randomization, they received immediate
acupuncture and were included in the nonrandom-
ized acupuncture group (n=3,846 included in analy-
sis). Trained physicians administered a maximum of
15 needle acupuncture sessions to each participant. All
participants completed a questionnaire at baseline and
after 3 months. Fifty randomly selected participants
also completed the questionnaire after 6 months. The
participants in the acupuncture group experienced
better improvements in function. No life-threatening
side eects were reported. A cost analysis evaluation
using a societal perspective (n=2,388) found that the
probability that acupuncture was cost-eective was
close to 100%. The authors concluded that acupunc-
ture added to routine care was associated with clinical
outcome improvements and was relatively cost-ef-
fective. This paper provides Level II evidence that
acupuncture plus usual care is cost-eective com-
pared to usual care.
Ratclie et al
2
conducted a randomized controlled
trial and cost-eectiveness analysis to evaluate the
cost-eectiveness of acupuncture in 241 patients
with non-specic LBP in England. Participants were
randomized at a ratio of 2:1 into an acupuncture group
(n=160) or usual care only group (n=81). Bodily pain
was reported on the SF-36 at baseline, 3, 12 and 24
months. Health care utilization details were collect-
ed from provider notes, admission documentation
and patient questionnaires. Cost-eectiveness anal-
ysis was completed on participants who completed
the questionnaire at all four time points. During the
2-year analysis, total cost was higher for the acupunc-
ture group compared to the usual care group, but the
incremental cost-eectiveness ratio was positive for
the acupuncture group. The authors concluded that
a short course of acupuncture oers a modest health
benet for a minor cost compared to usual care for the
treatment of LBP. In critique of the methodology, the
work group downgraded this potential Level II study
due to the limited sensitivity analyses performed. This
study provides Level III evidence that acupuncture is
cost-eective when compared to usual care.
In a randomized controlled trial in the United
Kingdom, Thomas et al
3
tested the hypothesis that
patients with nonspecic LBP would gain more long-
term pain relief for equal or less cost with acupuncture
added to conventional primary care, compared to
conventional care only. Participants were randomized
into an acupuncture group (n=159) or usual care group
(n=80) and completed the bodily pain dimension
of the SF-36 at baseline, 3, 12 and 24 months. Cost-
eectiveness was measured using the SF-6D (derived
from SF-36), EuroQoL 5 Dimensions (EQ-5D) and
quality-adjusted life-years (QALYs). Four patients
reported minor side eects such as pain at the site of
needling. At 24 months, the acupuncture service was
found to be cost-eective. The authors concluded that
acupuncture in a general practice environment was
associated with improvement in clinical outcomes
and was cost-eective over a 2-year period. The work
group downgraded this potential Level II study due to
the limited sensitivity analyses performed. Therefore,
this study provides Level III evidence that acupuncture
is cost-eective when compared to usual care.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
206
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
206
Future Directions for Research
The work group recommends a systematic review of existing well-designed
cost-utility studies evaluating acupuncture versus usual care.
References
1. Witt CM, Jena S, Selim D, et al. Pragmatic randomized
trial evaluating the clinical and economic eectiveness
of acupuncture for chronic low back pain. Am J Epidemi-
ol. 2006;164(5):487-496.
2. Ratclie J, Thomas KJ, MacPherson H, Brazier J. A ran-
domised controlled trial of acupuncture care for per-
sistent low back pain: Cost eectiveness analysis. BMJ.
2006;333(7569):626-628.
3. Thomas KJ, MacPherson H, Ratclie J, et al. Longer
term clinical and economic benets of oering acu-
puncture care to patients with chronic low back pain.
Health Technol Assess. 2005;9(32):68.
QQ
Cost-Utility Question 10. Are over-the-counter medications only without other
medical interventions more cost-eective in the management of patients with low
back pain than other medical/interventional treatments?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that future studies assessing over- the-counter
medications only for LBP should consider including cost-utility analysis.
QQ
Cost-Utility Question 11. Is cognitive or psychological-based therapy in the
management of patients with low back pain more cost-eective than other
medical/interventional treatments?
There is conicting evidence regarding the cost-utility of cognitive or psychological-based
therapy in the management of low back pain.
Grade of Recommendation: I
Jellema et
1
al assessed the cost-eectiveness of a
psychological-based program compared to usual
care for the treatment of LBP in the Netherlands. A
total of 314 participants from 41 general practices
were enrolled in this cluster-randomized controlled
trial with an economic evaluation. The participants
in the intervention group (n=143) participated in
a 20-minute discussion regarding psychosocial
prognostic factors related to LBP. The participants
in the control group (n=171) received usual care.
Outcomes such as functional disability (Roland-Morris
disability questionnaire), perceived recovery (Likert
scale) and health-related quality of life (EuroQol)
were collected at baseline and after 12 months. Using
cost diaries and follow-up information from general
practitioners, an economic evaluation from a societal
perspective was conducted. There were no statistically
signicant dierences in clinical outcomes between

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
207
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
207
groups. The complete case analysis and sensitivity
analyses resulted in inconsistent results regarding
cost-eectiveness of the intervention. The authors
concluded that Dutch general practitioners should
not replace usual care with this new intervention at
this time. In critique of the methodology, the work
group downgraded this potential Level II study due to
missing data and uncertainty of applying the results to
environments outside of the Netherlands. This study
provides Level III evidence that a very specic minimal
intervention strategy exploring psychological factors
was not cost-eective compared to usual care, which
was not protocolized.
Lamb et al
2,3
conducted a multicenter randomized
controlled trial and cost-eectiveness analysis
from 7 English regions to assess the clinical and
cost-eectiveness of a group cognitive behavioral
intervention program added to best practice for the
treatment of LBP. A total of 701 patients with LBP for
at least 6 weeks were randomized into a control group
(n=233) to receive usual care advice (which included
The Back Book) or an intervention group (n=468) to
receive usual care advice plus cognitive behavioral
intervention. This intervention included an individual
assessment along with 6 1.5-hour group sessions
over a 2-day course. Questionnaires were completed
at 3, 6 and 12 months. At 12 months, an intention-
to-treat analysis included 199 (85%) participants
in the control group and 399 (85%) participants
in the intervention group. The intervention group
had signicantly greater improvement in RMDQ
scores and modied Von Kor disability scores. The
additional quality-adjusted life-year (QALY) gained
from the intervention was 0.099 with an incremental
cost per QALY of £1786 and a >90% probability
of cost-eectiveness. The authors concluded that
the intervention resulted in long-term (one-year)
eectiveness and cost-eectiveness in treating
subacute and chronic LBP at a low cost to the health-
care provider. This study provides Level III evidence
that addition of cognitive behavioral approach may be
cost-eective for patients with LBP.
These results were supported by a cost-utility study
by Norton et al
4
that aimed to evaluate the cost-utility
of CBT for the treatment of LBP in the United States.
Commercial health plan members with LBP for at
least 6 weeks who independently sought care from a
general practitioner received standard education and
were subsequently randomized to a control group or
treatment group as part of the Back Skills Training
Trial (BSTT). The control group consisted of a com-
prehensive strategy of multiple approaches to LBP.
The treatment group received an individual assess-
ment and up to 6 group CBT sessions. All participants
completed questionnaires that included the EuroQol
5-dimension (EQ-5D) after one year used to estimate
quality-adjusted life-year (QALY). A Markov decision
tree model was used to estimate cost-eectiveness
of the CBT intervention at one and 10 years, using
costs from the US commercial payer perspective. The
10-year cost-eectiveness was estimated using the
probability of distribution into 3 possible health states
(improved, not improved and dead). After the rst
year, the incremental cost-utility of CBT was $7,197
per QALY and $5,855 per QALY after 10 years. The au-
thors concluded that CBT is a cost-eective approach
for treatment of chronic LBP. Although this study was
not used to develop the nal recommendation for this
question, it provides supplemental evidence by ap-
proaching the question from the perspective of the US
payers with ndings similar to those of Lamb et al.
2,3
Whitehurst et al
5
compared the cost-utility and
cost-eectiveness of a brief pain management pro-
gram (BPM) and physical therapy (PT) for the treat-
ment of LBP in the United Kingdom. All participants
received one 40-minute session plus up to 6 addition-
al 20-minute sessions of the assigned treatment from
a physiotherapist. Patients randomized to receive the
BPM (n=201) received a management plan that ad-
dressed known psychosocial risk factors for LBP and
included general exercises that were not back-specif-
ic (no physical therapy). Participants randomized into
the PT group (n= 201) received the same amount and
time of sessions from a physiotherapist that focused
on manual physiotherapy and back-specic exercis-
es. There were no signicant dierences in outcomes
or health care costs between groups. The incremen-
tal cost-per quality-adjusted life-year (QALY) was
£2,362. The authors concluded that PT is a cost-ef-
fective treatment for LBP and suggested that BPM
could be a possible additional care approach. This
study provides Level III evidence that a psychological
based program administered by physical therapists is
slightly less cost-eective compared to usual care.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
208
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
208
Future Directions for Research
The work group recommends that future studies assessing the cost-utility of
cognitive or psychological therapies should clearly dene the interventions in
order to compare them to other medical/interventional treatments.
References
1. Jellema P, van der Roer N, van der Windt DA, et al. Low
back pain in general practice: Cost-eectiveness of a
minimal psychosocial intervention versus usual care.
Eur Spine J. 2007;16(11):1812-1821.
2. Lamb SE, Lall R, Hansen Z, et al. A multicentred ran-
domised controlled trial of a primary care-based cog-
nitive behavioural programme for low back pain. The
back skills training (BeST) trial. Health Technol Assess.
2010;14(41):1-281.
3. Lamb SE, Hansen Z, Lall R, et al. Group cognitive be-
havioural treatment for low-back pain in primary care:
a randomised controlled trial and cost-eectiveness
analysis. Lancet. 2010;375(9718):916-923.
4. Norton G, McDonough CM, Cabral H, Shwartz M, Bur-
gess JF. Cost-utility of cognitive behavioral therapy for
low back pain from the commercial payer perspective.
Spine. 2015;40(10):726-733.
5. Whitehurst DG, Lewis M, Yao GL, et al. A brief pain
management program compared with physical therapy
for low back pain: Results from an economic analysis
alongside a randomized clinical trial. Arthritis Rheum.
2007;57(3):466-473.
QQ
Cost-Utility Question 12. In patients with low back pain, is a symptom guided
treatment approach using directional preference/centralization matched exercise
more cost-eective than usual care (home care vs medication vs nonspecic
physical therapy exercise vs nonspecic physical therapy modalities) long-term at
12 months, 36 months?
There is insucient evidence to make a recommendation for or against the cost-utility of direc-
tional preference based therapy versus alternatives.
Grade of Recommendation: I
Apeldoorn et al
1
compared the cost-eectiveness
of usual care physical therapy versus a modied
version of Delitto’s classication-based approach
for the treatment of LBP in the Netherlands.
Patients randomized to the control group (n=82)
received usual physical therapy such as resistive
strengthening, stretching and postural exercises.
Patients randomized into the intervention group
(n=74) were classied to receive direction-specic
exercises, spinal manipulation, or stabilization
exercises based on a standard treatment protocol.
Global perceived eect (7-point Likert scale), pain
intensity (11-point numerical rating scale), functional
status (10-item ODI) and health-related quality of
life (EuroQol) were recorded at baseline and after
one year. Quality-adjusted life-years (QALYs) were
calculated and costs were collected from a societal
perspective. The participants in the intervention
group had signicantly greater global perceived
eect, but there were no dierences between groups
in any of the other outcome measures. There was no
signicant dierence in cost between groups. The
authors concluded that the intervention was not cost-
eective compared to physical therapy. This study
provides Level III evidence that a specic directional
preference treatment approach was not cost-eective
when compared to the usual approach.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
209
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
209
Future Directions for Research
The work group recommends that any research regarding the therapeutic bene-
t of directional preference should consider the inclusion of cost-utility analysis.
Reference
1. Apeldoorn AT, Bosmans JE, Ostelo RW, de Vet HC, van
Tulder MW. Cost-eectiveness of a classication-based
system for subacute and chronic low back pain. Eur Spine
J. 2012;21(7):1290-1300
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
210
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
210
Cost-Utility of Medical/Interventional Treatment versus Surgical Treatment Questions
QQ
Cost-Utility Question 13. Is the surgical management (including fusion and lumbar
disc replacement and spinal cord stimulators) of patients with low back pain more
cost-eective than medical/interventional treatments?
There is insucient evidence to make a recommendation for or against the cost-utility of
surgical therapies versus medical/interventional therapies for low back pain.
Grade of Recommendation: I
Johnsen et al
1
assessed the cost-eectiveness of to-
tal disc replacement (TDR) compared to multidisci-
plinary rehabilitation (MDR) in a randomized clinical
trial of patients with chronic LBP >1 year in Norway.
Patients randomized to the TDR group (n=86) re-
ceived a disc prosthesis using uoroscopic guidance.
Patients randomized to the MDR group (n=87) partic-
ipated in an interdisciplinary outpatient program that
included exercise and cognitive intervention. Out-
comes recorded included EuroQol 5D (EQ-5D), Short
Form 6D (SF-6D) and costs at 6 weeks and 3, 6, 12
and 24 months. Cost analyses were conducted using a
societal perspective. The authors concluded that TDR
was cost-eective when using EQ-5D, but not with
SF-6D. This study provides Level III evidence that
total disc replacement versus multidisciplinary re-
habilitation results in conicting evidence regarding
the cost-utility of total disc replacement based on the
specic tool used to assess QALYs. The intention to
treat versus per protocol analysis also provided con-
icting results.
Rivero-Arias et al
2
conducted an economic evaluation
of a randomized controlled trial by Fairbank et al
3
to
compare the cost-eectiveness of surgical spine sta-
bilization with a rehabilitation program in patients
with chronic LBP in the United Kingdom. Participants
were randomized to receive spinal stabilization sur-
gery (n=176) or an intensive rehabilitation program
(n=173). The rehabilitation program included exer-
cise and education-based on principles of cognitive
behavior therapy for a total of 75 hours. All partici-
pants completed the EuroQoL 5D (EQ-5D), which was
used to estimate quality-adjusted life-years (QALYs).
Results revealed that spinal stabilization surgery had
higher associated mean total cost per patient com-
pared to the rehabilitation group, with no signicant
dierence between groups in mean QALYs gained.
The authors concluded that surgical stabilization of
the spine may not be a cost-eective use of scarce
health care resources, but that this could change. The
work group determined that this study provides Level
III evidence that surgical stabilization is not cost-ef-
fective when compared to an intensive rehabilitation
program.
Future Directions for Research
The work group recommends that future studies assessing the eectiveness of
surgery should consider including cost-utility analysis.
References
1. Johnsen LG, Hellum C, Storheim K, et al. Cost-eective-
ness of total disc replacement versus multidisciplinary
rehabilitation in patients with chronic low back pain: A
Norwegian multicenter RCT. Spine. 2014;39(1):23-32.
2. Rivero-Arias O, Campbell H, Gray A, Fairbank J, Frost H,
Wilson-MacDonald J. Surgical stabilisation of the spine
compared with a programme of intensive rehabilitation
for the management of patients with chronic low back
pain: Cost utility analysis based on a randomised con-
trolled trial. BMJ. 2005;330(7502):1239-1243.
3. Fairbank J, Frost H, Wilson-MacDonald J, Yu LM, Bark-
er K, Collins R. Spine Stabilisation Trial Group. BMJ.
2005 May 28;330(7502): 1233. Epub 2005. Eratum in:
BMJ (2005 Jun 25;330(7506): 1485.
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
211
Diagnosis & Treatment of Low Back Pain | Recommendations | Cost-Utility
211
QQ
Cost-Utility Question 14. Is cognitive or psychological-based therapy in the
management of patients with low back pain more cost-eective than surgical
therapies?
There is insucient evidence to make a recommendation for or against the cost-utility of
cognitive or psychological-based therapies vs surgical therapies in the treatment of low
back pain.
Grade of Recommendation: I
For the purposes of evaluating studies for this
question, the work group included studies with
treatments that incorporated the principles of
cognitive- or psychological-based therapy.
Rivero-Arias et al
1
conducted an economic evaluation
of a randomized controlled trial by Fairbank et al
2
to compare the cost-eectiveness of surgical spine
stabilization with a rehabilitation program in patients
with chronic LBP in the United Kingdom. Participants
were randomized to receive spinal stabilization
surgery (n=176) or an intensive rehabilitation
program (n=173). The rehabilitation program
included exercise and education based on principles
of cognitive behavior therapy for a total of 75 hours.
All participants completed the EuroQoL 5D (EQ-5D),
which was used to estimate quality adjusted life years
(QALYs). Results revealed that spinal stabilization
surgery had higher associated mean total cost per
patient compared to the rehabilitation group, with
no signicant dierence between groups in mean
QALYs gained. The authors concluded that surgical
stabilization of the spine may not be a cost-eective
use of scarce healthcare resources, but that this could
change. The work group determined that this study
provides Level III evidence that cognitive-based or
psychological-based rehab programs may be a cost-
eective option compared with surgical therapies.
Future Directions for Research
The work group recommends that future studies assessing the eectiveness of
cognitive or psychological-based therapies for LBP should consider including
cost-utility analysis.
References
1. Rivero-Arias O, Campbell H, Gray A, Fairbank J, Frost H,
Wilson-MacDonald J. Surgical stabilisation of the spine
compared with a programme of intensive rehabilitation
for the management of patients with chronic low back
pain: Cost utility analysis based on a randomised con-
trolled trial. BMJ. 2005;330(7502):1239-1243.
2. Fairbank J, Frost H, Wilson-MacDonald J, Yu LM, Barker
K, Collins R. Spine Stabilisation Trial Group. BMJ. 2005
May 28;330(7502): 1233. Epub 2005. Eratum in: BMJ
(2005 Jun 25;330(7506): 1485.
Diagnosis & Treatment of Low Back Pain |
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
212
Cost-Utility of Surgical Treatment Questions
QQ
Cost-Utility Question 15. Are minimally invasive surgical procedures more cost-
eective in the management of patients with low back pain than conventional
open surgical procedures?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends future studies assessing the eectiveness of mini-
mally invasive versus open surgery for LBP should consider including cost-utility
analysis.
QQ
Cost-Utility Question 16. Is instrumented lumbar fusion more cost-eective
compared to non-instrumented fusion for the treatment of patients with low back
pain?
A systematic review of the literature yielded no studies to adequately address this question.
Future Directions for Research
The work group recommends that future studies comparing instrumented ver-
sus noninstrumented fusion for LBP should consider including cost-utility anal-
ysis.
Recommendations | Cost-Utility
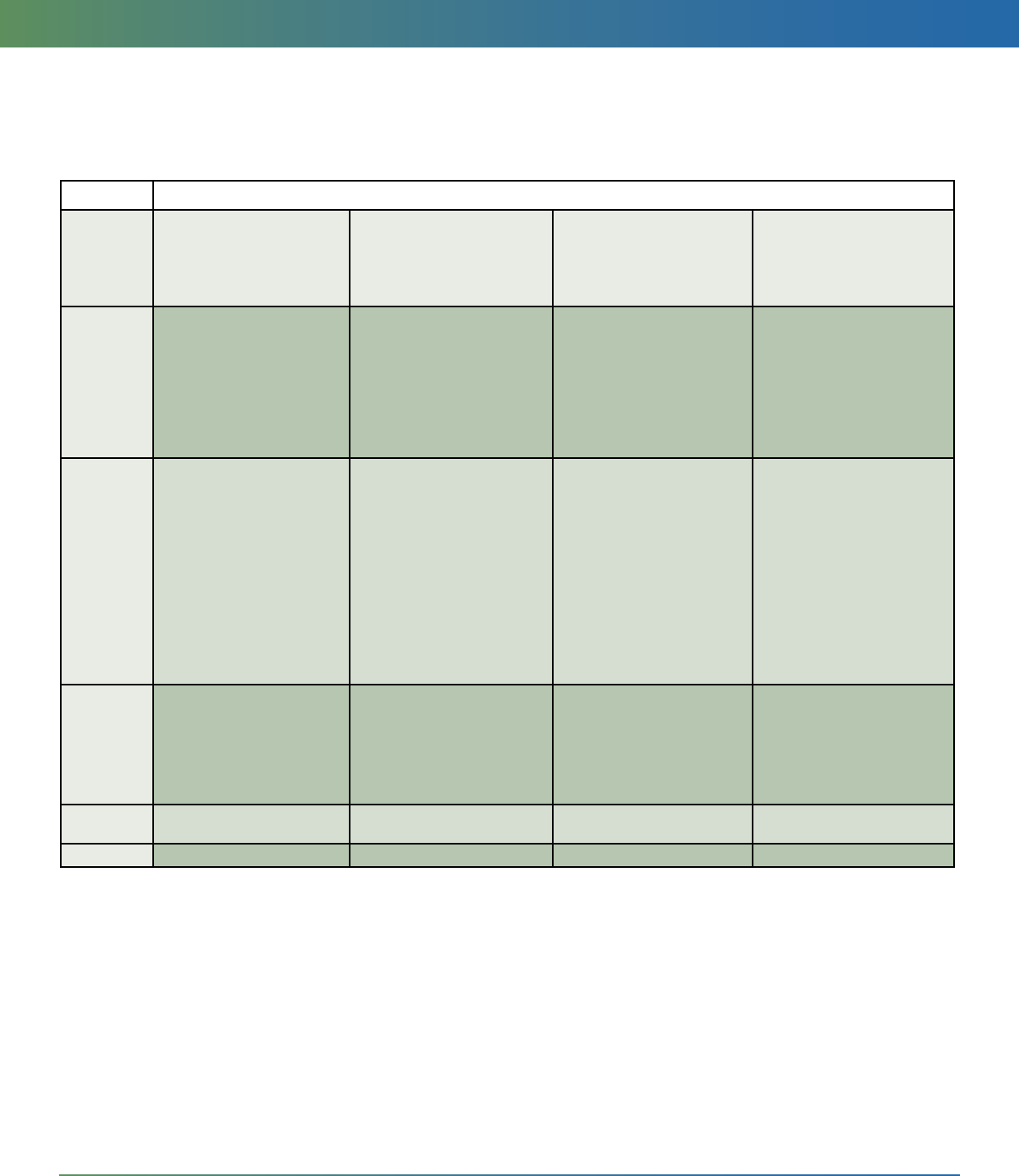
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
213
Diagnosis & Treatment of Low Back Pain | Appendices
213
Appendix A: Levels of Evidence for Primary Research Question
Levels of Evidence For Primary Research Question
1
As Adopted by the North American Spine Society January 2005
Types of Studies
Therapeutic Studies
Investigating the
results of treatment
Prognostic Studies
Investigating the eect of
a patient characteristic on
the outcome of disease
Diagnostic Studies
Investigating a
diagnostic test
Economic and
Decision Analyses
Developing an
economic or
decision model
Level I • High quality randomized
trial with statistically
signicant dierence or
no statistically signicant
dierence but narrow
condence intervals
• Systematic review
2
of Level
I RCTs (and study results
were homogenous
3
)
• High quality prospective
study
4
(all patients were
enrolled at the same point
in their disease with ≥
80% follow-up of enrolled
patients)
• Systematic review
2
of Level I
studies
• Testing of previously
developed diagnostic
criteria on consecutive
patients (with universally
applied reference “gold”
standard)
• Systematic review
2
of Level
I studies
• Sensible costs and
alternatives; values
obtained from many
studies; with multiway
sensitivity analyses
• Systematic review
2
of Level
I studies
Level II • Lesser quality RCT (eg,
< 80% follow-up, no
blinding, or improper
randomization)
• Prospective
4
comparative
study
5
• Systematic review
2
of Level
II studies or Level I studies
with inconsistent results
• Retrospective
6
study
• Untreated controls from an
RCT
• Lesser quality prospective
study (eg, patients enrolled
at dierent points in their
disease or <80% follow-up)
• Systematic review
2
of Level
II studies
• Development of diagnostic
criteria on consecutive
patients (with universally
applied reference “gold”
standard)
• Systematic review
2
of Level
II studies
• Sensible costs and
alternatives; values
obtained from limited
studies; with multiway
sensitivity analyses
• Systematic review
2
of Level
II studies
Level III • Case-control study
7
• Retrospective
6
comparative study
5
• Systematic review
2
of Level
III studies
Case-control study
7
• Study of non-consecutive
patients; without
consistently applied
reference “gold” standard
• Systematic review
2
of Level
III studies
• Analyses based on limited
alternatives and costs; and
poor estimates
• Systematic review
2
of Level
III studies
Level IV Case series
8
Case series
8
• Case-control study
7
• Poor reference standard
Analyses with no sensitivity
analyses
Level V Expert opinion Expert opinion Expert opinion Expert opinion
1. A complete assessment of quality of individual studies requires critical appraisal of all aspects of the study
design.
2. A combination of results from two or more prior studies.
3. Studies provided consistent results.
4. Study was started before the rst patient enrolled.
5. Patients treated one way (eg, cemented hip arthroplasty) compared with a group of patients treated in another
way (eg, uncemented hip arthroplasty) at the same institution.
6. The study was started after the rst patient enrolled.
7. Patients identied for the study based on their outcome, called “cases”; eg, failed total arthroplasty, are compared
to those who did not have outcome, called “controls”; eg, successful total hip arthroplasty.
8. Patients treated one way with no comparison group of patients treated in another way.
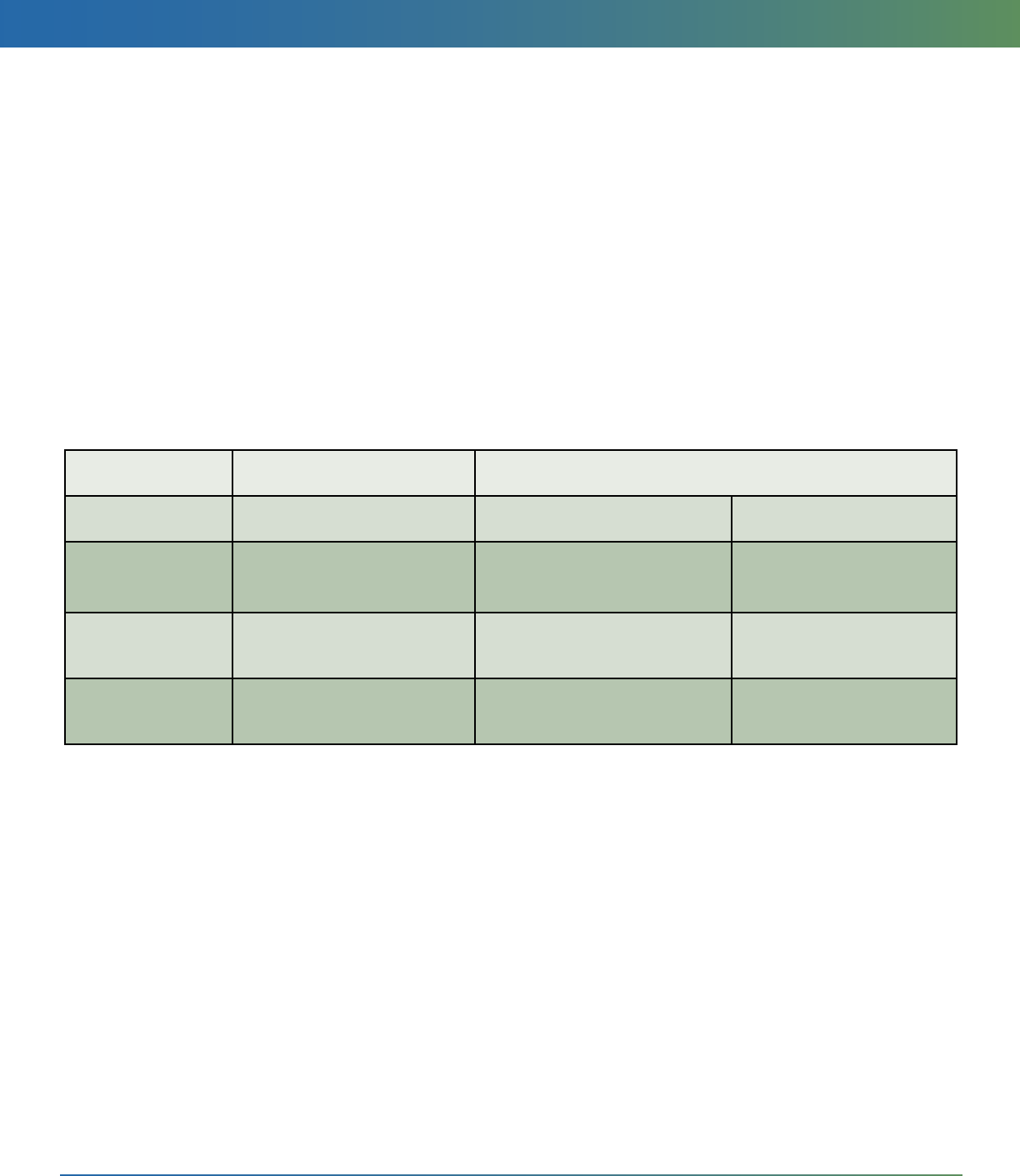
Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
214
Diagnosis & Treatment of Low Back Pain | Appendices
214
Appendix B: Grades of Recommendations for
Summaries or Reviews of Studies
Appendix C: Linking Levels of Evidence to Grades of Recommendation
Grades of Recommendation for Summaries or Reviews of Studies
As Adopted by the North American Spine Society January 2005
A: Good evidence (Level I studies with consistent ndings) for or against recommending intervention.
B: Fair evidence (Level II or III studies with consistent ndings) for or against recommending intervention.
C: Poor quality evidence (Level IV or V studies) for or against recommending intervention.
I: There is insucient or conicting evidence not allowing a recommendation for or against intervention.
Grade of
Recommendation
Standard Language Levels of Evidence
A Recommended Two or more consistent Level I
studies
B Suggested One Level I study with addi-
tional supporting Level II or III
studies
Two ore more consistent
level II or III studies
C May be considered; is an
option
One Level I, II, III or IV study
with supporting Level IV stud-
ies
Two or more consistent
Level IV studies
I Insucient evidence to make
recommendation for or
against
A single level I, II, III or IV study
without other supporting evi-
dence
More than one study with
inconsistent ndings*
* Note that in the presence of multiple consistent studies and a single outlying,
inconsistent study, the Grade of Recommendation will be based on the level of the
consistent studies.

Diagnosis & Treatment of Low Back Pain | Recommendations | Medical & Psychological Treatment
Recommendations were developed based on a specic denition, inclusion/exclusion criteria, and the resulting literature which excluded conditions
such as presence of a neurological decit or leg pain experienced below the knee, among others. Given the exclusion criteria, these guideline rec-
ommendations address a subset of low back pain care as opposed to low back pain in its entirety. This clinical guideline is not intended to be a xed
treatment protocol; it is anticipated that there will be patients who require more or less treatment than what is outlined. This clinical guideline should
not be construed as including all proper methods of care or excluding other acceptable methods of care reasonably directed to obtaining the same
results. The ultimate judgment regarding any specic procedure or treatment is to be made by the physician and patient in light of all circumstances
presented by the patient and the needs and resources particular to the locality or institution.
215
Diagnosis & Treatment of Low Back Pain | Appendices
215
Appendix D: Protocol for NASS Literature Searches
One of the most crucial elements of evidence analysis,
to support the development of recommendations for
appropriate clinical care or use of new technologies,
is the comprehensive literature search. Thorough as-
sessment of the literature is the basis for the review of
existing evidence, which will be instrumental to these
activities.
Background
Since the quality of a literature search directly aects
the quality of recommendations made NASS adheres
to a protocol to ensure that all NASS searches are con-
ducted consistently to yield the most comprehensive
results
Protocol for NASS Literature Searches
When it is determined that a literature search is need-
ed, NASS research sta will work with the requesting
parties and our contracted medical librarian to run a
comprehensive search employing at a minimum the
following search techniques:
1. A preliminary search of the evidence will be con-
ducted using the following clearly dened search
parameters (as determined by the content ex-
perts). In addition to the project goal and clinical
question(s) of interest, the following parameters
are to be provided to research sta to facilitate
this systematic literature search:
• Time frames for search
• Foreign and/or English language
• Order of results (chronological, by journal,
etc.)
• Key search terms and connectors, with or
without MeSH terms to be employed
• Age range
• Must answer the following questions:
• Should duplicates be eliminated between
searches?
• Should searches be separated by term or as
one large package?
• Should human studies, animal studies or ca-
daver studies be included?
This preliminary search should encompass a
search of the Cochrane database when access is
available.
2. Search results with abstracts will be compiled by
the medical librarian in both Endnote software
and a PubMed account, whenever possible. The
medical librarian typically responds to requests
and completes the searches within 2-5 business
days. Results will be forwarded to the Research
sta, who will share it with the appropriate NASS
sta member or requesting party(ies). (Research
sta has access to Endnote software and will
maintain a database of search results for future
use/documentation.)
3. NASS sta shares the search results with an ap-
propriate content expert (NASS Committee mem-
ber or other) to assess relevance of articles and
identify appropriate articles to review and on
which to run a “related articles” search.
4. Based on the content expert’s review, NASS Re-
search sta will then coordinate with the medical
librarian to conduct the second level searching to
identify relevant “related articles.”
5. The medical librarian will forward results to Re-
search sta to again share with appropriate NASS
sta member.
6. NASS sta shares related articles search results
with an appropriate content expert (NASS Com-
mittee member or other) to assess relevance of
this second set of articles and identify appropri-
ate articles to review and on which to run a second
“related articles” search.
7. NASS Research sta will work with the medical li-
brarian to obtain the 2nd related articles search re-
sults and any necessary full-text articles for review.
8. NASS members reviewing full-text articles should
also review the references at the end of each arti-
cle to identify additional articles which should be
reviewed, but may have been missed in the search.
Protocol for Expedited Searches
Numbers 1, 2 and 3 should minimally be followed for
any necessary expedited search. Following #3, de-
pending on the time frame allowed, deeper searching
may be conducted as described by the full protocol or
request of full-text articles may occur. If full-text ar-
ticles are requested, #8 should also be included. Use of
the expedited protocol or any deviation from the full
protocol should be documented with explanation.
Following these protocols will help ensure that NASS
recommendations are (1) based on a thorough review
of relevant literature; (2) are truly based on a uniform,
comprehensive search strategy; and (3) represent the
current best research evidence available. Research
sta will maintain a search history in Endnote, for
future use or reference.

