
#CMSQualCon21
CMS Quality Measurement
Action Plan
March 2021

Disclaimer
This presentation was prepared as a service to the public and is not intended to grant
rights or impose obligations.
This presentation may contain references or links to statutes, regulations, or other
policy materials. The information provided is only intended to be a general summary. It
is not intended to take the place of either the written law or regulation.
We encourage readers to review the specific statutes, regulations, and other
interpretive materials for a full and accurate statement of their contents.
2
Our Vision
Use impactful quality measures to improve health
outcomes and deliver value by empowering patients
to make informed care decisions while reducing
burden to clinicians.
3
Goals of the CMS Quality Measurement
Action Plan
Use Meaningful Measures to Streamline and Align Quality Measurement
Leverage Measures to Drive Outcome Improvement
Improve Quality Measures Efficiency by a Transition to Digital Measures
and Use of Advanced Data Analytics
Empower Patients to Make Best Healthcare Choices Through
Person-Centered Quality Measures and Public Transparency
Leverage Measures to Drive Improvement Through Public Reporting
and Payment Programs
Improve Quality Measures Efficiency by a Transition to Digital Measures
and Use of Advanced Data Analytics
Leverage Quality Measures to Promote Equity and Close Gaps in Care
Empower Consumers to Make Best Healthcare Choices through Patient-
Directed Quality Measures and Public Transparency
4

Meaningful Measures 1.0
5

Meaningful Measures 1.0
Accomplishments
• Since its inception in 2017, the Meaningful Measures Framework 1.0 has been utilized to review,
reduce, and align measures.
• Meaningful Measures 1.0 highlighted 6 strategic domains and 17 strategic focus areas.
• This has resulted in a 15% reduction of the overall number of measures in the CMS Medicare FFS
programs (from 534 to 460 measures).
• Overall, the measures portfolio has demonstrated a 25% increase in percentage of outcome
measures; the percentage of process measures has dropped from 52% in 2017 to 37% in 2021.
• Streamlining measures has a projected savings of an estimated $128M and a reduction of 3.3M
burden hours through 2020.*
*Seema Verma’s Speech at the 2020 CMS Quality Conference: https://www.cms.gov/newsroom/press-releases/speech-remarks-cms-administrator-seema-verma-2020-cms-quality-conference
6
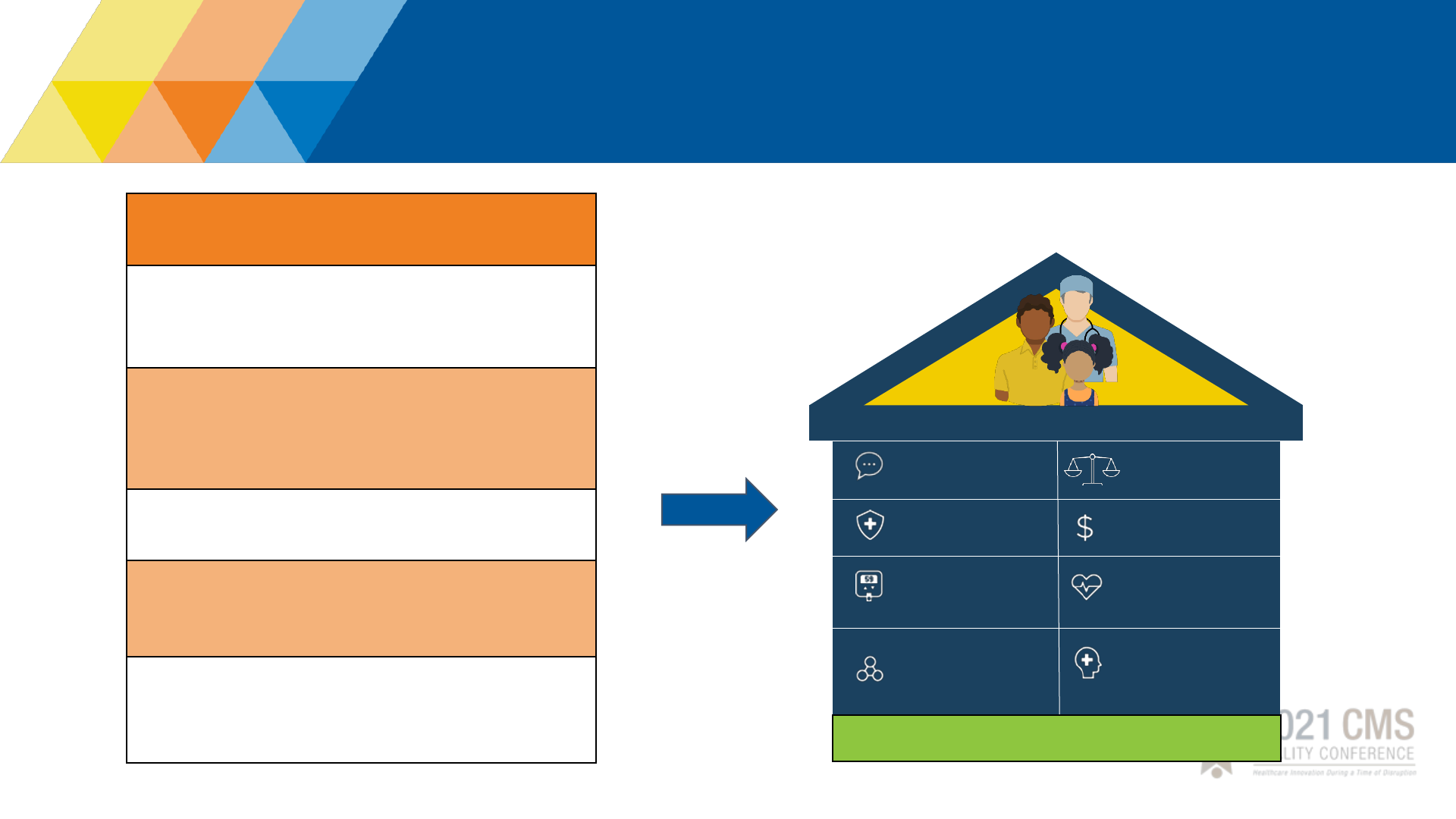
Meaningful Measures 2.0
Goals of MM 2.0
Utilize only quality measures of highest value and
impact focused on key quality domains
Align measures across value
-
based programs and
across partners, including CMS, federal, and
private entities
Prioritize outcome and patient reported measures
Transform measures to fully digital by 2025, and
incorporate all-payer data
Develop and implement measures that reflect
social and economic determinants
Person-Centered
Care
Wellness and
Prevention
Behavioral Health
Seamless Care
Coordination
Safety
Affordability and
Efficiency
Chronic
Conditions
Building Value-Based Care
Consumer and Caregiver Voice
Equity
7

Use Meaningful Measures Framework to
Streamline and Align Quality Measurement
• Leverage Meaningful Measures 2.0 framework to reduce burden and align measures
across the Agency and federal government
• Develop (as needed), prioritize, and utilize measures for high priority targeted areas,
such as socioeconomic status, maternal mortality, and kidney care and Home and
Community Based Services
• Align quality measures to quality improvement activities
• Increase the proportion of outcome measures across the CMS portfolio by 50% by
2022
• Continue the work of the Core Quality Measures Collaborative to align measures
across all payers
Objective
Align measures
across CMS, federal
programs, and private
payers
Reduce number and
burden of measures
8

Leverage Measures to Drive Improvement Through
Public Reporting and Payment Programs
Objective
Accelerate ongoing
efforts to streamline
and modernize
programs, reducing
burden and promoting
strategically important
focus areas
• Continue to examine value-based programs across CMS for modernization and
alignment, as appropriate
• Introduce 5-10 MIPS Value Pathways (MVPs)
• Incorporate robust quality measurement into all value-based payment models
• Support utilization of Adult and Child Core sets and HCBS recommended
measures
• Improve Child Core Set reporting and reduce state burden by leveraging
alternative data sources for calculation of state level rates
• Provide more timely results and feedback to help create learning systems that
support ongoing quality improvement
• Transition to all payer data
9

Improve Quality Measures Efficiency by a Transition
to Digital Measures and Use of Advanced Data
Analytics
Objective
Use data and information
as essential aspects of a
healthy, robust healthcare
infrastructure to allow for
payment and
management of
accountable, value-based
care and development of
learning health
organizations
• Transform to all digital quality measures by 2025
• Accelerate development and testing eCQMs using FHIR API technology for
transmitting and receiving quality measurement
• Transform data collection to use FHIR API technology and all CMS data (all-
payer data)
• Utilize data driven framework to assess measure priorities and performance
• Leverage centralized data analytic tools to examine programs and measures
• Evaluate new technologies for advanced machine learning and neural networks
• Expand the availability of public use files for CMS data by 2021
10

Empower Consumers to Make Best Healthcare
Choices through Patient-Directed Quality Measures
and Public Transparency
Objective
Empower patients
through transparency
of data and public
reporting, so that
patients can make the
best-informed
decisions about their
healthcare
• Expand and prioritize person and caregiver engagement during the measure
development process
• Increase Patient Reported Outcome Measures (PROMs) by 50%
• Continue to modernize Compare Sites and develop rating systems for Medicaid
and CHIP beneficiaries and their caregivers
• Advance use of FHIR API to allow patients to receive their health information
electronically
• Increase person-centered measures, such as goals of care and shared decision
making
11

Leverage Quality Measures to Promote
Equity and Close Gaps in Care
Objective
Commit to a patient-
centered approach in
quality measure and
value-based incentives
programs to ensure
that quality and safety
measures address
healthcare equity
• Expand confidential feedback reports stratified by dual eligibility in all
CMS value-based incentive programs as appropriate by the end of 2021
• Introduce plans to close equity gaps through leveraging the pay-for-
performance incentive programs by 2022
• Ensure equity by supporting development of Socioeconomic Status (SES)
measures and stratifying measures and programs by SES or dual
eligibility as appropriate. Partner with OMH regarding HESS measures
(health equity)
• Develop multi year plan to promote equity thru quality measures
12
Next Steps: Stakeholder Engagement &
Communications
• Continue collaboration and engagement with
specialty societies regarding MVPs
development, with goal of introduction of 8-10
new MVPs in 2021
• Develop strategic communications and roll out
plan
• Continue to seek input and collaboration to
advance the quality measurement action plan
through the Meaningful Measures email:
MeaningfulMeasuresQA@cms.hhs.gov
✓ Conducted multiple listening
sessions across CMS, federal
partners, and external
stakeholders
✓ Collaborated with 30 specialty
societies on the first iteration of
MVPs
✓ Developed multiple digital
measures using FHIR-based API
✓ Compare Updates rolled out
September 2020
What we’ve done so far…
13
