
Medicare Financial Management Manual
Chapter 5 - Financial Reporting
Table of Contents
(Rev. 315, 05-17-19)
Transmittals for Chapter 5
10 - Checks Paid Method - General
20 - Summary of Procedures
30 - Establishment of Special Bank Accounts
30.1 - Execution of Bank Agreement
30.2 - Collateral Requirement
30.3 - Changes in Collateral Pledged as Security for Federal Health Insurance
Accounts
30.4 - Check Format Specifications
40 - Signature of Bank Individuals Authorized to Draw on The Letter-of-Credit
40.1 - Revision of Signature Cards
40.2 - Request for Additional Cards
40.3 - Signatures of Contractor Personnel Authorized for Federal Health
Insurance Time Account
50 - Withdrawal of Federal Funds
60 - Use of Payment Vouchers
70 - Form CMS-1521, Payment Voucher on Letter-of-Credit Transmittal
70.1 - Instructions for Completion of Form CMS-1521
80 - Form CMS-1522, Monthly Contractor Financial Report
80.1 - Instructions for Completion of Form CMS-1522
80.2 - Medicare Contractor Monthly Cash Collections Worksheet
90 - Intermediary Benefit Payment Report (Form CMS-456)
90.1 - Purpose and Scope
90.2 - Due Dates and Transmittal
90.3 - Verification of Data
90.4 - Accuracy of Data Contained on Report and Reconciliation of Data
Reflected on Monthly Intermediary Financial Report (Form CMS-1522)
90.5 - General Reporting Instructions
90.6 - Instructions for Completion of the IBPR
90.7 - Form CMS-456 - Schedule R
100 - Issuance of Letter-of-Credit
100.1 - Monthly Limitation
100.2 - Amending Letter-of-Credit
100.3 - Establishment of Accounting Records
110 - Initial Federal Health Insurance Time Account Deposit
110.1 - Subsequent Time Account Deposits and Adjustments
110.2 - Bank Account Analysis
120 - Reviewing Bank Agreements
120.1 - Terminating Bank Agreements
120.2 - Terminating Federal Health Insurance Accounts
120.3 - Phase-out Period for Federal Health Insurance Bank Accounts
130 - Invitation for Bid (IFB) to Provide Banking Services Under The Checks Paid
Method of Letter-of-Credit Financing
140 - Bonding
150 - Letter-of-Credit Check List
160 - Electronic Funds Transfer (EFT)
170 - Electronic Remittance Advice (ERA)
180 - Exhibits
190 - General Information About Termination Costs
200 - General
210 - Instructions for Completing The Form CMS-750A/B, Contractor Financial Reports
220 - Due Date
230 - Certification
240 - Instructions for Completing Form CMS-751 A/B, Status of Accounts Receivable
250 - Due Date
260 - Certification
270 - Line Item Instructions Form CMS-751A/B
270.1 - Line 1, Beginning FY Balance (Principal & Interest)
270.2 - Line 2a, New Receivables (Principal)
270.3 - Line 2b, Accrued Receivables (Principal)
270.4 - Line 3, Interest Earned (Interest)
270.5 - Line 4a, Cash/Check Collections on Receivables (Principal & Interest)
270.6 - Line 4b, Offset Collections on Receivables (Principal & Interest)
270.7 - Line 4c, Collections Deposited at Another Location (Principal & Interest)
270.8 - Line 5, Adjusted/Transferred/Waived Amounts (Principal & Interest)
270.9 - Line 6, Amounts Written-off Closed (Bad Debts)/Transferred CNC
(Principal & Interest)
270.10 - Line 7, Ending Balance (Principal & Interest)
270.11 - Line 7a, Current Receivables (Principal)
270.12 - Line 7b, Non-current Receivables (Principal)
270.13 - Line 8, Allowance for Uncollectible Accounts (Principal & Interest)
270.14 - Line 9, Total Receivables Net of Allowance
270.15 - Line 10, Cash/Offsets Received for Receivables at Another Location
(Principal & Interest).
270.16 - Line 1, Total Not Delinquent (Principal & Interest)
270.17 - Line 2, Total Delinquencies (Principal & Interest)
270.18 - Line 3, Status of Delinquent Receivables, less than or equal to 180 Days
(Principal & Interest)
270.19 - Line 4, Status of Delinquent Receivables, greater than 180 Days
(Principal & Interest)
270.20 - Line 4c, Collections Deposited at Another Location (Principal &
Interest)
270.21 - Line 10, Cash/Offsets Received for Receivables at Another Location
(Principal & Interest)
270.22 - Collections on Delinquent Debt (Principal & Interest)
270.23 - Line 5c, Transfers Out to other Medicare Contractors (Principal &
Interest)
270.24 - Line 5e, Transfers Out to other CMS Locations, POR/PSOR (Principal &
Interest)
270.25 - Line 5g, Transfers Out to other CMS Locations, Not POR (Principal &
Interest)
280 - Instructions for Completing the CMS-C751A/B, Status of Debt - Currently Not
Collectible (CNC), and CMS-MC751A/B, Status of MSP Debt - Currently Not
Collectible (CNC)
290 - Due Date
300 - Certification
310 - Line Item Instructions CMS-C751A/B - Non-MSP and CMS-MC751A/B - MSP
310.1 - Line 1, Beginning FY Balance (Principal & Interest)
310.2 - Line 2, New CNC Debt (Principal & Interest)
310.3 - Line 3, Interest Earned Since CNC Approval (Interest)
310.4 - Line 4(a) through (e), Reclassified CNC Debt (Principal & Interest)
310.5 - Lines 5(a) through (f), Amounts Transferred (Principal & Interest)
310.6 - Line 6, Ending Balance (Principal & Interest)
310.7 - Line 1, Total Aged CNC Debt (Principal & Interest)
310.8 - Collections on CNC Debt (Principal & Interest)
310.9 - Status of CNC Debt over 181 Days (Principal & Interest)
400 - Exhibits
400.1 - Exhibit 1 - Statement of Financial Position and Statement of Operations -
HI/SMI
400.2 - Exhibit 2 - Statement of Financial Position and Statement of Operations -
SMI
400.3 - Exhibit 3 - Status of Accounts Receivable - HI
400.4 - Exhibit 4 - Status of Accounts Receivable - SMI
400.5 - Exhibit 5 - Status of Non-MSP Debt - CNC - HI
400.6 - Exhibit 6 - Status of Non-MSP Debt - CNC - SMI
400.7 - Exhibit 7 - Status of MSP Accounts Receivable - HI
400.8 - Exhibit 8 - Status of MSP Accounts Receivable - SMI
400.9 - Exhibit 9 - Status of MSP Debt - CNC - HI
400.10 - Exhibit 10 - Status of MSP Debt - CNC - SMI
400.11 - Exhibit 11 - Medicare Contractor Account Definitions - Data Element
Definitions
400.12 - Exhibit 12 - Accounts Payable - Protocol for Estimating Claims - Form
CMS-750A/B, Statement of Financial Position
400.13 - Exhibit 13 - Periodic Interim Payments (PIP) Protocol for Estimating
Payables/Receivables for the Form CMS-750A/B, Statement of Financial Position
(Intermediaries Only)
400.14 - Exhibit 14 - Protocol for Estimating Allowance for Uncollectible
Accounts Form CMS H/M -751A/B, Status of Accounts Receivable
400.15 - Exhibit 15 - Protocol for Prorating Intermediary Time Account Balances
Between Form CMS 750A (HI) and Form CMS 750B (SMI)
400.16 - Exhibit 16 - Electronic Certification
400.17 - Exhibit 17 - Instructions for the Transfer of Debt Between Reporting
Entities
400.18 - Exhibit 18 - Collection Reconciliation/Acknowledgement Form
400.20 - Exhibit 20 - Procedures for Reporting Currently Not Collectible (CNC)
Debt
400.21 - Exhibit 21 - CMS Policy for Recognizing Accounts Receivable
400.22 - Exhibit 22 - Accounts Receivable Trending Analysis Procedures
400.23 – Exhibit 23 – Instructions for the Benefits Payable Survey
400.24 – Exhibit 24 – Benefits Payable Trending Analysis Procedures
410 – Unsolicited Voluntary Refunds
410.1 – General Information
410.2 – Office of the Inspector General (OIG) Initiatives
410.3 – Unsolicited/Voluntary Refund Accounts
410.4 - Receiving and Processing Unsolicited/Voluntary Refund Checks When
Identify Information is Provided
410.5 – Handling Checks or Associated Correspondence with Conditional
Endorsements
410.6 - Receiving and Processing Unsolicited/Voluntary Refund Checks when
Identifying Information is not Provided
410.7 – CMS Reporting Requirements With the Exception of MSP
410.8 – Exhibit 1 Overpayment Refund
410.9 - Exhibit 2 Unsolicited/Voluntary Refund Checks – Summary Report
410.10 - Education
411 – Exhibits
411.1 – Overpayment Refund Form
411.2 – Exhibit 2 - Unsolicited/Voluntary Refund Checks – Summary Report
411.3 – OIG Law Enforcement Demand Letter
420 – Procedures for Re-issuance and Stale Dating of Medicare Checks
500 – Procedures for the Reconciliation of Total Funds Expended for Fiscal Intermediary
Shared System (FISS) Medicare Contractors Used in the Preparation of Form CMS-1522,
Monthly Contractor Financial Report
500.1 – Identification and Summarization of Detailed Claims Data Records for
Use in the Financial Reconciliation of Total Funds Expended to Fiscal
Intermediary Shared System Reports
500.2 – Using the Electronic Spreadsheet to Complete the Reconciliation of the
Detailed Claims Data File to Fiscal Intermediary Shared System Reports
500.3 – Electronic Spreadsheet Input Schedule
500.4 – Total Funds Expended (Net Disbursements and Adjustments to Net
Disbursements)
500.5 – Reconciliation of Detailed Claims Data File to FISS System Reports
500.6 – Reconciliation of Non-PIP Payments on FISS System Reports
500.7 – Reconciliation of Interest Received and Paid on FISS System Reports
500.8 – Categorization of Total Funds Expended by Category
510-Procedures for the Reconciliation of Total Funds Expended for Multi-Carrier System
(MCS) Medicare Contractors Used in the Preparation of Form CMS-1522, Monthly
Contractor Financial Report
510.1 - Reconciliation of Detailed Claims Data File to Multi-Carrier System
(MCS) Report
510.2 - List of Primary MCS Reports Used in the Reconciliation of Total Funds
Expended
510.3 - Standard MCS 1522 Reconciliation Lead Schedule
510.4 - Reconciliation of Claim Payments from the Detailed Claims Data
File/Report to the Month-to-Date Analysis of Payment (MCS Report #2002 or
HBDR2002)
510.5 - Proof of Net Disbursements and Total Issues per Detailed Claims Data
File/Report
510.6 - Proof of Net Disbursements and Total Issues Per MCS Report #2002
510.7 - Reconciliation of Net Disbursements and System Issues from the Detailed
Claims Data File/Report to the Month-to-Date Analysis of Payment (HBDR2002)
510.8 - Proof of Net Disbursement per MCS Register Summary Report
(HBDR6000) to the Month-to-Date Analysis of Payments (HBDR2002 Report,
Line G
510.9 - Input Sheet for Cash Activity Items
520 – Instructions for Completion of the Contractor’s Monthly Bank Reconciliation
Worksheet
NOTE: Throughout this chapter, reference to provider includes institutional providers,
physicians, and suppliers, i.e., all delivers of health care services that are reimbursed by
either the intermediary or the carrier.
NOTE: Revision 1, the initial release of this chapter, includes a cross reference to the
source sections in current manuals. The manual is identified by A1, A2, A3, or A4 for
Intermediary Manual Parts 1 through 4; or by B1, B2, B3 or B4 for Carriers Manual Parts
1 through 4. This indicator is followed by a dash and the related section number.
10 - Checks Paid Method - General - (Rev. 5, 08-30-02)
A1-1400, B1-4400
Certified Letter-of-Credit Defined:
A certified letter-of-credit is a legal reservation of funds on deposit in the Federal
Reserve Bank that covers payments for which the contractor has contracted to pay by
issuing checks and authorizing electronic funds transfer.
The objective of the letter-of-credit checks paid method of financing is to reduce the level
of the Federal debt and the interest costs of short-term borrowing. This method provides
cash availability to meet Medicare program requirements, while at the same time,
controls the timing of cash withdrawals so that the impact of these withdrawals on the
public debt level and related financing costs is minimized. Cash flow is controlled by:
• Postponing withdrawal of funds from the U.S. Treasury until Medicare checks are
presented to the contractor's Medicare servicing bank for payment;
• Limiting the amount withdrawn at any time; and
• Reducing the amount of Federal funds required to offset bank service charges.
The Treasury Department requires all Government agencies that make advance payments
to utilize the letter-of-credit checks paid method of financing. (See Circular No. 1075,
revised February 27, 1973, and Chapter 1000 of the Treasury Fiscal Requirements
Manual.)
20 - Summary of Procedures - (Rev. 5, 08-30-02)
A1-1401, B1-4401
A contractor shall use the following steps to implement the letter-of-credit checks paid
method of financing:
• It shall notify the RO 165 days prior to the expiration of the current three-party
bank agreement when a new bank will be secured under the checks paid method;
• It shall request the latest copy of the Invitation for Bid (IFB) from the Regional
Office (RO);
• It shall use the IFB package as a guide to prepare its IFB. The language contained
in the package cannot be materially altered except for "BID FORMS AND
CONTRACTOR'S REQUIRED MEDICARE BANKING SERVICES." (See
Attachment A, Section G, of the package.) The contractor shall obtain from its
RO the implementation package that contains examples of material required for
the bid process as follows:
o Letter to Commerce Business Daily requesting IFB advertisement; and
o Sample write-ups of contractor's specifications for bank services,
computer requirements, check specifications, and electronic funds transfer
capability;
• It shall send the completed IFB to its RO for approval prior to its release for bid.
It shall send an additional copy to:
Centers for Medicare & Medicaid Services
Office of Financial Management
7500 Security Boulevard
Baltimore MD 21244-1850
• Obtain bids from two or more banks;
• Follow the Federal Acquisition Regulations (FAR), Part 14, when securing
competitive bids;
• Evaluate the bank bids and, with the concurrence of the servicing RO, select the
commercial bank that meets all of the mandatory requirements and submits the
lowest required time account balance;
• Select a commercial bank and establish special bank accounts;
• Secure Signature Cards. Use Form SF-1194 to obtain the signatures of those
individuals authorized by the bank to draw payment vouchers against the letter-
of-credit and the signature of the bank official who has the authority to designate
the authorized individuals;
NOTE: CMS executes the three-party bank agreement between the contractor, the bank,
and the Government (the servicing RO). CMS also issues a letter-of-credit that sets forth
the monthly limitation.
• Post (Bank) collateral with the Federal Reserve Bank;
• Establish (Bank) both the Benefits Account and the Time Account;
• Submit monthly letter-of-credit transmittals (form CMS-1521) via Contractor
Administrative Financial Management (CAFM) to the Funds Control Branch,
Central Office. Distribute Medicare funds withdrawn by bank via FNS-5401
payment voucher according to type of benefits; and
• Submit the monthly form CMS-1522, TAA-1b and TAA-1C, to CMS via the
CAFM system.
30 - Establishment of Special Bank Accounts - (Rev. 5, 08-30-02)
A1-1403, B1-4403
Keep all Federal funds withdrawn under the letter-of-credit separate from all other funds.
Designate the Medicare account for deposit in a special bank account established by you
in a member bank of the Federal Reserve System. Designate the special demand deposit
checking account as follows:
(Name of Contractor)
Federal Health Insurance Benefits Account
Designate the special non-interest bearing time account as follows:
(Name of Contractor)
Federal Health Insurance Time Account
Restrict withdrawals to transfer of funds to the Federal Health Insurance Benefits
account.(FHIBA)
30.1 - Execution of Bank Agreement - (Rev. 5, 08-30-02)
A1-1403.1, B1-4403.1
The contractor shall execute the three-party bank agreement with the selected commercial
bank. The bank agreement requires that the Federal Government retain a lien on all funds
held in the special bank account. The bank abides by written instructions of the
Government with regard to the deposit and withdrawal of funds. The Government also
has the right to inspect or audit the bank's books and records that pertain to the special
accounts. (Refer to Attachment C of the IFB package.)
The contractor shall use the following guidelines when it executes a bank agreement;
• It must strictly adhere to the wording and format of the bank agreement.
• It may alter only Covenant 7. The provisions of Covenant 7 may, by agreement of
all parties, be written to require either a one or two-year period of performance
following the initial two year period;
• The RO forwards an original and three copies of the completed three-party
agreement to the bank via the contractor for execution. Each copy of the bank
agreement must contain original signatures. Facsimile signatures are not
acceptable; and
• After it is countersigned by CMS, individual copies of the agreement are
distributed to:
o The contractor;
o The bank;
o The servicing RO; and
o Centers for Medicare & Medicaid Services
Office of Financial Management
7500 Security Boulevard
Baltimore MD 21244-1850
30.2 - Collateral Requirement - (Rev. 5, 08-30-02)
A1-1403.2, B1-4403.2
Posted collateral is based on the balance to be maintained in the time account less FDIC
coverage, if applicable. The RO advises the contractor, upon notification by the Federal
Reserve Bank, when collateral is posted. (Collateral must be acceptable under the
guidelines provided to the Federal Reserve by the Department of the Treasury).
The contractor shall place the collateral with the Federal Reserve Bank or Branch of the
district where its servicing financial institution is located or with a custodian designated
by the Federal Reserve Bank or Branch. It shall include a letter with the collateral that
states that the collateral is pledged as security for public money by CMS, agency account
number 5555-4454-5 under the terms of 31 CFR, Part 202 (Treasury Circular 176).
30.3 - Changes in Collateral Pledged as Security for Federal Health
Insurance Accounts - (Rev. 5, 08-30-02)
A1-1403.3, B1-4403.3
The CMS, Division of Contractor Financial Management (DCFM), monitors collateral
requirements. DCFM continuously reviews the most recent balances maintained in the
Federal Health Insurance Bank Accounts.
If an increase in pledged collateral appears necessary, DCFM requests the bank to post
additional collateral with its Federal Reserve Bank.
If a decrease in pledged collateral appears warranted, DCFM advises the Federal Reserve
Bank of the amount of excess collateral pledged.
The contractor shall direct any request for release of excess bank collateral to the local
Federal Reserve Bank.
30.4 - Check Format Specifications - (Rev. 5, 08-30-02)
A1-1403.4, B1-4403.4, B2-5215
The following phrase must appear on all checks or drafts written for purposes of paying
benefits and related administrative costs authorized under the Medicare program:
MEDICARE PAYMENT
For Health Insurance - Social Security Act
The contractor shall use the following check format specifications:
Check Front
The contractor shall center the words "Medicare Payment" at the top of the check or draft
and print these words in at lease 1/4-inch type. Contractor name and address should
appear on the face of the check. The check may also include the contractor's emblem or a
picture of a building it occupies. The contractor may not include advertising on the face
of the check. (Advertising should not appear on the envelope in which the check is
mailed.) It is expected that the type sizes of the items placed on the check will not detract
from the required "Medicare Payment" phrase.
Check Back
The contractor shall print on the back of all Medicare checks the following statement:
"This payment is made with Federal funds. Fraud in procuring, forging a signature or
endorsement, or materially altering this check is punishable under the U. S. Criminal
Code."
For carriers, assigned claims must also include the following statement:
"As provided by the terms of the law under which this check is issued, the undersigned
payee, in accepting assignment, agreed that the charge determination by the Medicare
carrier shall be the full charge for any service which the check is payable. The patient is
responsible only for the applicable deductible and coinsurance, and for non-covered
services."
It is not necessary to show the account name on the check. If one is shown, it should read
"Federal Health Insurance Benefits Account." If both Part A and Part B are shown, it
should read, "Federal Health Insurance Benefits Account - Part A" and "Federal Health
Insurance Benefits Account - Part B."
The time limitation for cashing the check (if specified on the check) cannot be less than 6
months.
The contractor shall clear formats of checks with the servicing RO prior to printing or
contracting for printing.
40 - Signature of Bank Individuals Authorized to Draw on The Letter-
Of-Credit - (Rev. 5, 08-30-02)
A1-1405, B1-4405
Signatures of bank representatives authorized to sign payment vouchers must be on file
along with the letter-of-credit at the servicing Federal Reserve Bank or branch in order to
honor payment vouchers (FMS-5401). The contractor shall submit a signature card, Form
SF-1194, for the person(s) authorized by the bank to sign payment vouchers.
NOTE: Executed signature card(s) must be received in DCFM no later than 20 calendar
days prior to the effective date of a new letter-of-credit.
40.1 - Revision of Signature Cards - (Rev. 5, 08-30-02)
A1-1405.1, B1-4405.1
The contractor shall prepare new card(s) if more than two signatures are no longer valid.
It shall prepare two original cards for every four individuals. If more than one card is
needed, i.e., more than 4 individuals are authorized, it shall number the cards 1 of 2, 2 of
2 to ensure that all cards are received.
New signature cards must contain the signatures of all individuals who will sign payment
vouchers and be certified by an official of the bank. The contractor need not resubmit a
new signature card if change in position or title of an individual authorized to sign
payment vouchers is involved.
The contractor shall mark new signature cards "Replaces and Supersedes all Previously
Submitted Cards" on the top edge of the card.
40.2 - Request for Additional Cards - (Rev. 5, 08-30-02)
A1-1405.2, B1-4405.2
The contractor shall send requests for additional signature cards to:
Centers for Medicare & Medicaid Services
Office of Financial Management
7500 Security Boulevard
Baltimore, MD 21244-1850
40.3 - Signatures of Contractor Personnel Authorized for Federal
Health Insurance Time Account - (Rev. 5, 08-30-02)
A1-1405.3, B1-4405.3
Signatures of two or more individuals designated by the contractor to sign withdrawal
requests to transfer funds from the Federal Health Insurance Time Account to the Federal
Health Insurance Benefits Account must be on file with the designated commercial bank.
50 - Withdrawal of Federal Funds - (Rev. 5, 08-30-02)
A1-1406, B1-4406
The Federal Government assures that funds are always in the Federal Reserve Bank to
honor properly drawn payment vouchers within the limits of the letter-of-credit. This
arrangement is consistent with State banking laws since it eliminates any possibility of
intent to defraud.
60 - Use of Payment Vouchers - (Rev. 5, 08-30-02)
A1-1408, B1-4408
To obtain Federal funds, the bank prepares a daily payment voucher, Treasury Form
FMS-5401, and forwards it to the servicing Federal Reserve Bank or Branch holding the
letter-of-credit.
When the bank receives the initial letter-of-credit, the bank sequentially numbers
payment vouchers drawn beginning with the number one (1). Amendments to the letter-
of-credit do not interrupt the sequential numbering of payment vouchers.
Payment vouchers are prepared only in an amount equal to the contractor's total checks,
bank debit memos, and electronic funds transferred. These vouchers are presented for
payment each day less any balance in the benefits account representing collected other
deposits or transfers from the Federal Health Insurance Time Account.
If the bank is not located in a Federal Reserve Bank (FRB) city, CMS requests the
Treasury Department to implement a telephonic method of receiving funds for the bank.
The bank calls its FRB and requests a specific funding amount. The FRB prepares the
payment voucher and a copy is sent to the bank.
The letter-of-credit provides a ceiling on the amount that may be drawn during the month
and is purposely set high to meet peak cash needs. In no instance is a payment voucher to
be drawn for less than $5,000 or more than $5,000,000 (unless the letter-of-credit has
been annotated "Authorized to draw payment vouchers in excess of $5,000,000"). Only
one payment voucher should be drawn per day. Regardless of the factors considered in
determining when and in what amount to draw payment vouchers, banks are expected to
abide by the intent of the letter-of-credit Checks Paid Method of financing system by
assuring that the total of the daily voucher processed is the minimum required to finance
current disbursements.
NOTE: The "Name and Address of Drawer" block on the Treasury Form FMS-5401
must include the name of the bank as it appears on the letter-of-credit sent by CMS and
the annotation "agent for" (name of contractor). Due to space limitations, the contractor
does not have to show the address in this block. A supply of payment vouchers is
provided to each commercial bank. Additional supplies of payment vouchers may be
ordered from:
Centers for Medicare & Medicaid Services
Office of Budget and Administration
Distribution Liason Officer
7500 Security Boulevard
Baltimore, MD 21244-1850.
70 - Form CMS-1521, Payment Voucher on Letter-Of-Credit
Transmittal - (Rev. 5, 08-30-02)
A1-1410, B1-4410
The purpose of form CMS-1521, Payment Voucher on Letter-of-Credit Transmittal, is to
record daily voucher data that the contractor's bank submits to the Federal Reserve Bank
for payment of Hospital Insurance (HI) and Supplemental Medical Insurance (SMI)
benefit payments. Administrative costs paid through the Smartlink System are also
reported on the form. Administrative costs are allocated to current or prior fiscal years
and to special projects.
Transmit form CMS-1521 to CMS by the 15th of each month via the CAFM System.
(See operating instructions for completion that are contained in the CAFM Users Guide.)
70.1 - Instructions for Completion of Form CMS-1521 - (Rev. 5, 08-30-
02)
A1-1410.1, B1-4410.1
Data comes from Treasury Form FMS-5401 Payment Voucher.
Date drawn - Contractor enters the date funds were drawn. It shall use 2 digits.
Voucher Number - Contractor enters the payment voucher number in 3 digits beginning
with voucher number 001 to 999. It shall inform the bank to start over when number 999
is reached.
Serial Number - Contractor enters the serial number of the payment voucher.
Hospital Insurance Benefits - Contractor enters the total amount drawn for HI and SMI.
The total of HI and SMI benefits should equal the total funds drawn.
NOTE: Part B contractors enter amounts for SMI only.
PMS Smartlink Communication System for Administrative Costs –
On pages 1 and 2, the contractor shall continue to report administrative costs drawn via
the PMS Smartlink Telecommunications System in the same designated "Administrative
Cost" column 4. However, it shall show these amounts after it reports all benefit payment
amounts.
Contractor shall indicate in the "date drawn" column the date the money was deposited
into its commercial bank account and not the date it requested the money. This entry
(entries) may occur on either page 1 or 2 depending on the number of entries.
Contractor shall not make entries in the columns for Voucher Number, Serial Number,
and Voucher Totals.
Contractor shall reflect the current or prior year administrative costs drawn via Smartlink.
It shall report on page 3 any special project(s) amount(s) drawn via Smartlink.
Public reporting burden for collecting this information is estimated to average 1 hour per
response. This includes time for reviewing instructions, searching existing data sources,
gathering and maintaining data needed, and completing and reviewing the collection of
information. Contractor shall send comments regarding this estimated burden or any
other suggestions for reducing the burden to:
Office of Management and Budget
Paperwork Reduction Project (0938-0361)
Washington, D.C. 20503;
and to:
Centers for Medicare & Medicaid Services
Office of Financial Operations
7500 Security Boulevard
Baltimore, Maryland 21244-1850.
80 - Form CMS-1522, Monthly Contractor Financial Report – (Rev. 5,
08-30-02)
A1-1412, B1-4412
Form CMS-1522 is designed to provide a reconciliation of Medicare benefit dollars
between CMS, the contractor, and the bank. The contractor shall transmit this report to
CMS by the 15th of each month via the CAFM System.
80.1 - Instructions for Completion of Form CMS-1522 - (Rev. 5, 08-30-
02) - (Rev. 5, 08-30-02)
A1-1412.1, B1-4412.1
• Screen 1 - Section A - Purpose for Which Funds are Drawn:
o Contractor shall reflect the current or prior year administrative costs drawn
via Smartlink. It shall report on page 3 any special project(s) amount(s)
drawn via Smartlink.
o Funds Drawn this Month - Contractor enters the total amount of Federal
funds drawn via payment vouchers during the calendar month for use as
HI benefits, line 1-B, or SMI benefits, line 2-B. Each entry must equal the
sum of the amounts shown in this category on the Form CMS-1521 dated
during the calendar month.
o Total Funds Expended This Month - Contractor enters total funds
expended for HI benefits, line 1-D, and SMI benefits, line 2-D during the
calendar month. Totals should equal the sum of all checks drawn and
electronic funds transfer payments against the special bank account during
the calendar month. (It shall include all checks issued and electronic funds
transferred, i.e. dated during the calendar month.) Any refunds received
from beneficiaries or their assignees during the calendar month because of
prior overpayments deposited in the special bank account should serve to
reduce total funds expended.
o Funds Drawn for Fiscal Year - This is a calculated field.
o Funds on Hand End of Month - This is a calculated field.
o Line 3, Drugs and Line 4, Regular Administrative Costs - Contractor shall
not use at this time.
o Bills Paid - Lines 7 and 8 - Completed by Part A intermediaries. Part B
carriers complete only line 8.
o Retro-Adjustment - Part A contractors enter credit adjustments on
appropriate lines. Part B contractors do not use lines 9 or 10.
• Benefits Bank Account
o From Bank Statement - The contractor shall take information for lines 15
through 19 from the statement of the special bank account issued by the
bank at the end of the calendar month.
o Line 15 - Balance Beginning of Month Per Bank - Contractor enters the
balance in the special bank account as of the beginning of the calendar
month as shown on the bank statement.
o Line 16a - Payment Vouchers Drawn During Month - Contractor enters
the total amount of funds drawn on payment vouchers (FMS-5401) during
the calendar month and credited to the benefits account as shown on the
bank statement. Since all checks drawn for deposit in the Time Account
are cleared through the benefits account, a payment voucher is drawn for
this transaction and is included in line 16a. The amount shown on this line
must agree with the totals from the Form CMS-1521 corresponding to the
calendar month and also with Section A, Line 5, column (b). The only
exception is for vouchers in transit (line 20).
o Line 16b - Other Deposits - Contractor enters all other deposits credited
during the month to the special bank account as shown on the bank
statement. It shall reduce the next payment voucher by the amount of the
deposited refunds in the account in order to minimize idle funds in the
account. It shall Include any credits or adjustments made to the bank
account during the calendar month in this line.
o Line 16c - Contractor shall include funds withdrawn from the Time
Account and deposited in the Benefits Account.
o Line 16d - Miscellaneous Credit Memo - Contractor enters any
miscellaneous adjustments to the benefits bank account during the
calendar month.
o Line 17 - This is a calculated field.
o Line 18A - Contractor shall subtract: Checks and EFT Payments Honored
by Bank During Month - It enters from the bank statement the total funds
charged to the special bank account as a result of checks honored and
electronic funds transferred by the bank during the month. This total must
include all checks that were drawn for deposit in the time account and
honored by the bank during the month.
o Lines 18B and C - Miscellaneous Bank Charges - Contractor enters any
miscellaneous charges made to the special bank account that are part of
the bank statement.
o Line 19 - This is a calculated field.
o Line 20 - Add: Deposits in Transit. - Enter payment vouchers drawn and
other deposits made during the calendar month that the bank has not yet
credited to the special bank account according to the statement.
o Line 21. - This is a calculated field.
o Line 22 - Subtract: Outstanding Checks. - Enter the total of all checks
issued during the current month or any previous month that the bank has
not yet paid as of the end of the calendar month. If during the calendar
month payment is stopped on any check previously issued, or any
previously issued check is otherwise voided, subtract the amount of funds
represented by that check from this total before making an entry on this
line.
o Line 23 - This is a calculated field.
o Line 24 - Highest Balance During Month Per Bank. Contractor enters the
highest balance in the special bank account during the calendar month as
reflected on the bank statement.
• Time Account
o Line 15 - Balance Beginning of Month - Contractor enters the balance in
the time account as of the beginning of the calendar month as shown on
the bank statement.
o Line 16a - Other Deposits - Contractor enters the amount of funds drawn
from the benefits account for deposit in the time account.
o Line 17 - Total. - This is a calculated field.
o Line 18a - Contractor enters only amount of funds withdrawn from the
time account and deposited in the benefits account during the month.
o Line 18b - Contractor enters any miscellaneous items.
o Line 19 - Balance EOM Per Bank - This is a calculated field.
• Screen 4 - Completed by Part A Contractors Only
o Periodic Interim Payments - Contractor enters amounts paid during the
month by category.
o Accelerated Payments - Contractor enters the amount of accelerated
payments paid out and received during the month.
o Suspended Payments - Contractor enters the amount of payments
suspended and released during the month.
• Screen 5 - Bills Paid - Contractor enters the amount of money actually paid during
the calendar month as follows:
o Amount paid for disabled or disability (identified by Codes 1 and 3 as
contained in S trailer of query reply).
o Amount paid for chronic renal disease (identified by Code 2 as contained
in S trailer of query reply).
o Amount paid for premium paying enrollees (identified by Codes 8 and 9
as contained in S trailer of query reply).
o Amount paid for aged. Contractor shall complete entries for disabled,
chronic renal disease, and premium paying enrollees prior to completing
the entry. It shall then subtract the sum of these entries from the calculated
Total and enter that amount.
o Total - (Bills paid for the month). This is a calculated field.
NOTE: For those Part A intermediaries that transmit bills to CMS from more than one
point, each processing point should submit to the home office at the end of the calendar
month all of the data requested in screen 1. (It shall consolidate data related to amounts
paid in screen 1.)
• Only Part A Intermediaries complete retroactive adjustments.
• Only Part A Intermediaries complete adjustments between trust funds.
• Interest:
o Interest Received From Providers On Overpayments - Separate Check for
Interest Collected - When a check is received for interest on an
overpayment, the contractor shall deposit the check immediately in the
Medicare bank account. It shall report this check as an "Other Deposit"
(line 16b). Also, it shall report the check as "Interest Received" on screen
5 and use as a reduction to expenditures on screen 1, funds expended
column.
o Check Includes Both Interest Collected and Overpayment Recoupment -
Contractor shall deposit the check immediately into the Medicare bank
account. It shall report the entire amount of the check as an "Other
Deposit" (line 16b) on screen 2. It shall report the interest portion as
"Interest Recovered" on screen 5. Both the interest recovered and the
overpayment recoupment are used as a reduction to expenditures on screen
1, funds expended column.
o Interest Paid to Providers on Underpayments - Separate Check for Interest
Paid - When a check is issued for interest due to a provider on an
underpayment, the contractor shall report it as a "Check Honored" (line
18a) on screen 2. Also, it shall report this amount as "Interest Paid" on
screen 5 and as an increase to expenditures on screen 1, funds expended
column.
• Screen 6 - No entries are required at this time.
Public reporting burden for this collection of information is estimated to average 16 hours
per response. This includes time for reviewing instructions, searching existing data

sources, gathering and maintaining data needed, and completing and reviewing the
collection of information. Contractors may send comments regarding this estimated
burden or any other suggestions for reducing the burden to:
Centers for Medicare & Medicaid Service
Office of Financial Management
Baltimore, Maryland, 21244-1850;
and to:
Office of Management and Budget
Paperwork Reduction Project (0938-0361)
Washington, D.C. 20503.
80.2 - Medicare Contractor Monthly Cash Collections Worksheet
(Rev. 80, Issued: 10-21-05, Effective: 07-01-05, Implementation: 11-21-05)
The Medicare Contractor Monthly Cash Collections Worksheet is to identify cash
collections deposited in the Medicare Trust Funds related to Provider Overpayments.
The Medicare contractors are to follow the line by line instructions for completing the
collections worksheet. The instructions are to provide uniformity throughout all
contractors for the calculations of the data used to populate each line item. Medicare
contractors are required to maintain supporting documentation for the amounts reported
on the Medicare Contractor Monthly Cash Collections Worksheet.
Medicare contractors are required to submit the worksheet via email to
[email protected] on the 15
th
day of the following month end. For year-end,
Medicare contractors may be required to submit the Monthly Cash Collections
Worksheet in an accelerated time frame.
A. Total Monthly Principal Deposit (Using Forms CMS-1522, Forms CMS-751)
Line 1 - Enter the total ‘Other Deposits’ (Line 16b, Form CMS-1522) for the
reporting period (e.g., June 30, etc.).
Line 2 - Enter ‘Deposits-In-Transit’ (Line 20, Form CMS-1522) for the month
prior to the reporting period (e.g., May 31, etc.).
Line 3 - Enter ‘Deposits-In-Transit’ (Line 20, Form CMS-1522) for the reporting
period (e.g., June 30, etc.).
Line 4 – Enter the sum of Line 1 minus (-) Line 2 plus (+) Line 3 equal (=) ‘Total
Monthly Deposits.
Monthly Interest (Cash) Collections
Line 5 – Enter the total ‘Received-Provider Overpayment’ (Line 1, page 4, Form
CMS-1522) for reporting period (e.g., June 30, etc.).
Line 6 – Enter the total ‘Interest Offset’ for the reporting period. Total ‘Interest
Offset’ must equal the amount of the offset collections included in the
amount reported on Line 1, page 4/4, Form CMS-1522 and included in
the amount of the offset reported on Line 4b, Form CMS 751 for the
quarter ending June 30, 2005.
Line 7 – The sum of Line 5 minus (-) Line 6 equal (=) Monthly Interest Cash
Collections.
Line 8 – Monthly Interest Cash Collections = Line 7.
Line 9 – The sum of Line 4 (Total Monthly Deposits) minus (-) Line 8 Monthly
Interest Cash Collections) = Total Monthly Principal Cash Deposits.
B. Calculate HI/SMI Percentage Split (FI Only) – 12 month rolling average
Line 10 – Enter the sum of Line 4a (principal), Form CMS-751A (quarter ending
June 30, 2005). For example, Line 4a (principal) for the period ending
June 2005 plus (+) [Line 4a (principal), Form CMS-751A (period
ending September 2004) minus (-) Line 4a (principal), Form CMS-
751A (period ending June 2004)]. The sum of Line 4a (period ending
September 2004) minus Line 4a (period ending June 2004) must equal
Cash Collections for the period July 2004 – September 2004.
(NOTE: 12 months of most recent HI principal Cash Collections (e.g., July
2004 - June 2005))
Line 11 - Enter the sum of Line 4a (principal), Form CMS-751BA (quarter ending
June 30, 2005). For example, Line 4a (principal) for the period ending
June 2005 plus (+) [Line 4a (principal), Form CMS-751BA (period
ending September 2004) minus (-) Line 4a (principal), Form CMS-
751BA (period ending June 2004)]. The sum of Line 4a (period ending
September 2004) minus Line 4a (period ending June 2004) must equal
Cash Collections for the period July 2004 – September 2004.
(NOTE: 12 months of most recent SMI principal Cash Collections (e.g., July
2004 - June 2005))
Line 12 – Enter the sum of Line 10 plus (+) Line 11 = Total HI/SMI collections.
Line 13 – Enter the HI percentage split. The result of Line 10 divided by Line 12.
Line 14 – Enter the SMI percentage split. 1.00 minus the HI percentage split
(Line 13).
(NOTE: Line 14 must equal Line 11 divided by Line 12)
C. HI Monthly Cash Deposit = HI percentage split (Line 13) multiplied by Total
Monthly Principal Cash Deposit (Line 9).
D. SMI Monthly Cash Deposit = HI percentage split (Line 13) multiplied by Total
Monthly Principal Cash Deposit (Line 9).
E. The Chief Financial Officer (CFO) is required to certify/sign the Medicare
contractor Cash Collection Worksheet Attachment I (electronic signature is
acceptable if the email is sent by the CFO), as an indication of the
correctness/completeness of the data in accordance with applicable instructions.
(NOTE: The sum of C and D must equal Total Monthly Principal Cash Deposits
(Line 9))
90 - Intermediary Benefit Payment Report (Form CMS-456) – (Rev. 5,
08-30-02)
A1-1414
90.1 - Purpose and Scope - (Rev. 5, 08-30-02)
A1-1414.1
The Intermediary Benefit Payment Report (IBPR) is a report of current monthly
information that covers the categories of benefits the contractor paid and selected
statistical data that relates to those payments. CMS uses this data to:
Track benefit payments by type of provider to detect significant shifts in program
expenditures;
Monitor implementation of new programs, e.g., hospice benefits, and comprehensive
outpatient rehabilitation benefits; and
Identify operation problem areas for resolution by the contractor or CMS.
90.2 - Due Dates and Transmittal - (Rev. 5, 08-30-02)
A1-1414.2
Contractor shall input the reports accompanying the reconciliation between IBPR and the
Monthly Intermediary Financial Report (Form CMS-1522) into the CAFM system 20
work days following the report month.
90.3 - Verification of Data - (Rev. 5, 08-30-02)
A1-1414.3
The various subsidiary records that include the individual provider files must support the
data entered on the report.
The contractor must have the capability to trace all data entered on the report to the
individual provider files.
Where applicable, the Provider Statistical and Reimbursement Report and other provider
reports containing benefits paid data must support the data on the report.
90.4 - Accuracy of Data Contained on Report and Reconciliation of
Data Reflected on Monthly Intermediary Financial Report (Form CMS-
1522) - (Rev. 5, 08-30-02)
A1-1414.4
The contractor must ensure that all data reflected on the report is accurate.
Line 36, column (g) of the report, should equal the amount shown on the CMS-1522,
column (d), lines 1 and 2 in the aggregate. In the event that the amounts do not agree, the
contractor shall complete a reconciliation report.
90.5 - General Reporting Instructions - (Rev. 5, 08-30-02)
A1-1414.5
Where money is withheld from payments due the provider (as an offset) for monies due
the contractor, the contractor shall show the gross amount (less any deductibles,
coinsurance, interest, or sequestration) as the payment on the appropriate line and
column. It shall show the offset as a negative amount in its appropriate line and column.
For example, when the contractor reduces a PPS Periodic Interim Payment (PIP) for a
settlement amount due from the provider, it shall record the gross PIP amount (less any
deductibles, coinsurance, interest, or sequestration) on line lA in column 1 (a) or 1(b), as
appropriate. It shall record the offset on line 6B in column 1(a) or 1(b), as appropriate.
However, it shall record a claim adjustment (e.g., a PRO disallowance or subsequent
reversal) as a reduction of claims payments on line 2A for a non-PIP/PPS hospital.
Where the contractor makes an accelerated payment and the provider repays a portion of
the accelerated payment during the same reporting period, the contractor shall show the
net amount on the appropriate line and column.
For example, when an accelerated payment of $100,000 is made to a provider during the
period, and the provider repays $30,000 during the same period, the contractor shows
$70,000 as the net accelerated payment.
In situations where an accelerated payment is made during the period, and the contractor
recovers a portion of the accelerated payment through reduction of interim payments, it
shall show the gross amount (less any deductibles, coinsurance, interest, or sequestration)
of interim payments as payment on the appropriate line and column. It shall show the
offset amount as a negative amount on the appropriate line and column.
For example, when an accelerated payment is made for $100,000 and later in the month
$30,000 of the accelerated payment is recouped by offset against PPS/PIP amounts of
$150,000 paid to the provider, the contractor shows the $150,000 gross PPS/ PIP amount
on line 1A in column 1(a) or 1(b), as appropriate. It shows a net accelerated payment of
$70,000 ($100,000-$30,000) on line 7 in column 1(a) or 1(b), as appropriate.
90.6 - Instructions for Completion of the IBPR - (Rev. 5, 08-30-02)
A1-1414.6
A. Heading
The contractor enters its name and assigned number. Multi-regional intermediaries use
the number assigned to the home office for administrative budget and cost reporting
purposes. The contractor shall furnish a consolidated report for all locations.
The contractor enters the calendar month and year as a four-digit entry, e.g., 1000, 1100,
1200, 0101.
B. Column Definitions - Page 1
Column (a) - Single Facility - refers to payments to PPS hospitals that do not have
distinct part facilities, such as SNFs, HHAs, psychiatric units, or rehabilitation units.
• Column (b) - Facility With Distinct Parts - refers to payments to PPS hospitals
that include distinct parts, such as SNFs, HHAs, psychiatric units, or
rehabilitation units.
NOTE: The contractor enters non-PPS payments to the distinct part on the appropriate
line and column of page 2.
• Column (c) - Non-PPS Payment - refers to payments to the following:
o Hospitals excluded from PPS (e.g., psychiatric, children's, rehabilitation
and long term);
o Hospitals receiving payments via an alternative payment program (waiver
States);
o Hospitals yet to be phased into PPS; and
o PPS hospitals for bills or underpayments applicable to pre-PPS fiscal
years.
• Column (d) - Total - refers to the total of columns (a), (b), and (c).
C. Line Item Definitions - Page 1:
1. Hospital Inpatient (PIP) - refers to hospitals paid by the PIP method. The
contractor shall show these figures less any deductibles, coinsurance, and interest
for all items on the PIP bills and any sequestration applicable to this line with any
offsets shown on line 6A or 6B.
A. Inpatient Operating Payments - refers to the amount of the PIP that covers
items that would otherwise be paid on a per claim basis plus those items
paid on a per claim basis in addition to PIP payment. (Such as payments
for outliers and hemophilia blood clotting factor add-on.)
The contractor enters the PIP amounts paid as follows:
PPS Provider Payments - Payments related to services furnished after
conversion to PPS in columns 1(a) or 1(b), as applicable. This includes outlier
payments, hemophilia blood clotting factor add-on payments, disproportionate
share amounts, indirect medical education, ESRD payments, and phased-in
capital-related costs during the transition period. Non-PPS Provider Payments
- column (c) - Payments related to services furnished prior to conversion to
PPS. Payments to all providers listed in the definitions for column (c).
B. Pass Through Costs - Contractor enters the PIP payments, including any
withholdings, but less any sequestration amounts for items paid on a
reasonable cost basis as follows:
• Capital;
• Direct medical education which includes nursing and paramedical
health professional (allied health) programs and graduate medical
education;
• Kidney and other organ acquisitions;
• Bad debts; and
• Nonphysician anesthetists.
NOTE: This includes that part of capital-related costs not included in line
1A.
C. Indirect Medical Education - Contractor enters the PIP payments for the
indirect medical education adjustment, whether on a PIP or a claim-by-
claim basis for PIP providers, less any sequestration (already included in
line 1A).
NOTE: Contractor shall make entries on this line for memorandum purposes
only to identify the amount of indirect medical education for PIP hospitals.
2. Hospital Inpatient (Non-PIP), refers to hospitals paid based upon bills reviewed
and approved. Contractor shall show total payments less any reductions on line
6A or line 6B.
A. DRG Bills Paid/Non-DRG Bills Paid - Contractor enters the calculated
payment less any deductibles, coinsurance, and interest for all items on the
bill and any sequestration applicable to this line. It shall include payments
for outliers, disproportionate share, indirect medical education, high
percentage of end-stage renal disease beneficiary discharges, and
hemophilia blood clotting factor add-on payments on a claim-by-claim
basis. Also, it shall include phased-in capital-related costs during the
transition period.
For DRG bills, it shall use columns (a) and (b). For non-DRG bills paid, it
shall use column (c).
It shall report all retroactive adjustments pertaining to hospitals on line 6A or
6B.
B. Pass Through Costs - The contractor enters the interim payments, less any
sequestration, for items paid on a reasonable cost basis as follows:
• Capital;
• Direct medical education which includes nursing and paramedical
health professional (allied health) programs and graduate medical
education;
• Kidney and other organ acquisitions;
• Bad debts; and
• Nonphysician anesthetists. NOTE: This includes that part of the
capital-related costs that are not included in line 2A.
C. Indirect Medical Education - Contractor enters the interim payments for
the indirect medical education adjustment (already included in line 2A).
NOTE: Contractor shall make entries on this line for memorandum purposes only to
identify the amount of indirect medical education for non-PIP hospitals. It shall not
adjust these amounts for MSP or sequestration.
3. Outlier Payments - Contractor enters additional amounts paid for outlier cases.
NOTE: Contractor shall make entries on this line for memorandum purposes only to
identify the total outlier payments that are found in the UB82 billing form in Locator 46-
49 in Value Code 17. These amounts are already included in the amounts recorded on
lines lA and 2A.
A. Days - The contractor enters additional payments made as a result of the
length of stay exceeding the day outlier threshold criteria. It shall make
entries on this line for memorandum purposes only. These are non-add
items.
NOTE: After FY 1997, outlier days no longer exist.
B. Cost - The contractor enters additional payments made for claims where
extraordinary costs were approved. It shall make entries on this line for
memorandum purposes only. These are non-add items.
4. Subtotal - Contractor enters the total of the amounts on lines 1A, 1B, 2A, and 2B.
NOTE: The amounts included in lines 1C, 2C, 3A and 3B are memo entries only and
have been included in lines 1A, 1B, 2A and 2B.
5. Outpatient Payments - Contractor enters the payment, less deductibles,
coinsurance and sequestration for outpatient and Part B inpatient services. It shall
report any offset against these amounts on line 6A or 6B. See line 19 for reporting
SNF outpatient payments.
6. Retroactive Adjustments:
• PPS Provider Payments - Contractor enters on lines 6A and 6B (as
applicable), columns (a) or (b), the net amount of retroactive adjustments
paid and received as a result of interim rate adjustments, pass through cost
adjustments, and cost report settlements applicable to current or prior
provider fiscal years.
Contractor shall show interest on cost report overpayments and late-filed cost
reports on these lines. An example of a proper recording of a retroactive
adjustment would be an entry of $500,000 of cash received from the provider
as the first installment of the final settlement of $1,000,000 due the program
from the prior year's cost report.
Another example would be an entry of $500,000 offset against current PIP
payments due of $1,000,000. (The $1,000,000 would be shown on line 1A.)
• Non-PPS Provider Payments - Contractor enters on line 6A or 6B (as
applicable) in column (c) the net amount of retroactive adjustments paid
and received as a result of interim rate adjustments and cost report
settlements applicable to current or prior provider fiscal years.
It shall show interest on cost report overpayments and late-filed cost reports
on these lines.
7. Accelerated Payments - Contractor enters the net amount of accelerated payments
made to and collected from hospitals and distinct part units. (See §160.5 for an
explanation of the appropriate recording of offsets.)
8. Total - The contractor enters the total of lines 4 through 7.
D. Statistical Data-Hospitals-Page 1:
9. PIP:
A. Contractor enters the total number of bills processed for hospitals paid by
the PIP method.
B. Contractor enters the dollar amount that would have been paid if the bills
processed were not subject to PIP in accordance with the definition of line
2A.
10. Non-PIP - Contractor enters the total number of bills for hospitals paid on a
submitted-bill basis.
11. Number of Hospitals - Contractor enters the total number of hospitals
participating in the Medicare program.
12. Number of Admissions - Contractor enters the total number of admissions the
Common Working File (CWF) has approved for payment.
13. Number of Discharges - Contractor enters the number of discharge bills processed
during the reporting month.
14. Number of Readmissions - Contractor enters the total number of readmissions to a
hospital within 7 calendar days of discharge from an acute care facility.
15. Number of Transfers - Contractor enters in column (a) and column (b) the total
number of transfers to a PPS hospital. It enters in column (c) the total number of
transfers to a non-PPS hospital.
16. Outlier Bills:
A. Days - Contractor enters the total number of day outlier bills paid that
relate to the dollar amounts shown in line 3A.
NOTE: Outlier days have been obsolete since the end of FY 1997.
B. Costs - Contractor enters the total number of cost outlier bills paid that
relate to the dollar amounts shown in line 3B.
17. Outpatient - Contractor enters the total number of outpatient bills and Part B
inpatient bills paid that relate to the dollar amounts shown in line 5.
E. Column Definitions - Page 2
• Column (e) - Single Facility - Refers to all providers that are not part of a hospital
complex.
• Column (f) - Part of Hospital Complex - Refers to providers that are an integral
part of a hospital and are operated with other departments of the hospital under
common licensure and governance.
• Column (g) - Total - Refers to total of columns (e) and (f).
F. Line Item Definitions - Page 2
Skilled Nursing Facilities - Including swing bed payments for SNF care.
18. PIP - Contractor enters all PIP payments made to SNFs. It enters total payments
(less any deductibles, coinsurance, interest or sequestration) with any withholding
reductions being shown on line 20.
19. Bills Paid - Contractor enters total payments less any deductibles, coinsurance,
interest, or sequestration with any withholdings shown on line 20. It enters the
calculated payment, less any deductibles, coinsurance and interest for all items,
and any sequestration applicable to SNFs on a submitted-bill basis. It shall
include Part A and Part B services.
20. Retroactive Adjustments - Contractor enters the net amount of retroactive
adjustments paid and received as a result of cost report settlements and lump sum
interim rate adjustments made in prior or current provider fiscal years.
21. It shall show interest on cost report overpayments and late-filed cost reports on
this line. An example of a proper recording of a retroactive adjustment would be

an entry of $500,000 cash received from the provider as the first installment of the
final settlement of $1,000,000 due the program from the prior year's cost report.
22. Accelerated Payments - Contractor enters the net amount of accelerated payments
made to and collected from SNFs. (See §160.5) for an explanation for reporting
accelerated payments.)
23. Total SNF Payments - Contractor enters the total of lines 18 through 21.
Home Health Agencies:
23. PIP - Contractor enters all PIP payments made to HHAs including SNF-based.
24. It shall show total payments less any deductibles, coinsurance, interest, or
sequestration with any withholding reductions shown on line 25.
25. Bills Paid - Contractor shall show total payments (less any deductibles,
coinsurance, interest, or sequestration) with any withholdings shown on line 25. It
enters the calculated payment, less any deductibles, coinsurance, and interest, for
all items, and any sequestration applicable to HHAs on a submitted-bill basis. It
shall include Part A and Part B services and SNF-based HHAs payments.
26. Retroactive Adjustments - Contractor enters the net amount of retroactive
adjustments paid and received as a result of cost report settlements and lump sum
interim rate adjustments made in prior current provider fiscal years.
27. It shall show interest on cost report overpayments and late-filed cost reports on
this line. An example of a proper recording of a retroactive adjustment would be
an entry of $500,000 cash received from the provider as the first installment of the
final settlement of $1,000,000 due the program from the prior year's cost report.
28. Accelerated Payments - Contractor enters the net amount of accelerated payments
made to and collected from HHAs. (See §160.5) for an explanation for reporting
accelerated payments.)
29. Total HHA Payments - Contractor enters the total of lines 23 through 26.
Additional Providers:
28. ESRD - Contractor shall include in these columns payments to ESRD networks,
as applicable:
Column (e) - It enters net payments to independent facilities. Column (f) - It enters
net payments to hospital-based facilities.
29. Hospice - Contractor enters net payments made to hospices.
30. RHC - Contractor enters net payments made to rural health clinics (RHCs).
31. OPA/HL - Contractor enters net payments made to organ procurement agencies
and histocompatibility laboratories.
32. CORF - Contractor enters net payments made to comprehensive outpatient
rehabilitation facilities (CORFs).
33. Distinct Part Units - Contractor enters net payments made to exempt distinct part
rehabilitation and psychiatric units.
34. All Others - Contractor enters net payments made to other providers not listed in
lines 28 -33.
NOTE: Contractor shall make adjustments, pertaining to providers, identified on lines
28 through 34 directly to the specific line. This includes checks received and offsets or
withholdings.
35. Total - Contractor enters the total of lines 28 through 34.
36. Grand Total - Contractor enters the total of lines 8(d), 22(g), 27(g) and 35(g).
G. Statistical Data - Page 2:
37. SNF:
• Number of SNFs - Contractor enters the total number of participating
SNFs.
• Number of Admissions - Contractor enters the total number of SNF
admissions.
38. HHA:
• Number of HHAs - Contractor enters the total number of participating
HHAs.
• Number of Bills - Contractor enters the total number of bills processed.
(Audit intermediaries should not complete this line.)
39. Number of Transfers to Distinct Part Units - Contractor enters the total number of
transfers to distinct part units for which payments are shown in line 33.
It shall use edit checks to ensure completeness, arithmetical accuracy, and to discover
inconsistencies. It shall have an authorized official sign and date the report.
90.7 - Form CMS-456 - Schedule R - (Rev. 5, 08-30-02)
A1-1414.7
(Page 3 of 3 of the Monthly Intermediary Benefit Payment Report) Reconciliation
Between IBPR and CMS-1522.
A. Purpose and Scope
The contractor shall use the Schedule R to account for any variances between line 36(g),
Total on the IBPR, and the HI and SMI Benefits reported on lines 1(d) and 2(d) of the
CMS-1522 Report.
Schedule R is an integral part of the IBPR and must be completed each month whether or
not a variance exists between the IBPR and the CMS-1522 Report. If there is no variance,
the contractor shall complete line 36(g) of the IBPR and HI and SMI Benefits for lines
1(d) and 2(d) of the Form CMS-1522. If there is a variance, it shall reconcile the two
reports by completing the appropriate lines.
It must have the capability to substantiate all amounts reflected on Schedule R.
Schedule R includes line items that will facilitate the contractor's reconciliation process.
It shall input the Schedule R, along with pages 1 and 2 of the IBPR, into the Contractor
Administrative Budget and Financial Management System (CAFM) for each report
month.
B. Instructions for Completion of Schedule R:
Heading - The contractor enters the report month and year. (See §160.6A) for
intermediary name and number.) Also, it enters its current letter-of-credit number.
Line Item Definitions - Schedule R:
CMS-456 (IBPR) Column:
Line 36(g) Total - Contractor enters the amount obtained from page 2 of 3 on line 36(g)
of the IBPR.
Medicare Secondary Payer (Non-Providers Cash Recoveries) - Contractor enters the cash
receipts and offsets applied to claims payments or other refunds that are received from
attorneys, beneficiaries, insurance companies or other non-providers. These amounts
should be negative numbers since they represent cash receipts.
Other Recoveries Identify - Contractor enters recovered or offset amounts not included in
any other line item (lines 1 through 36 or lines 1 and 3 of Schedule R). These amounts
should be negative numbers since they represent cash receipts.
Other Items Identify (Lines 3A through 3E) - Contractor enters any other benefit
payments or refunds not included elsewhere on the CMS-456 or on lines 1 and 2. The
items shown here may be unique to its operation and should be identified accordingly. It
shall itemize each major category on lines 3A. through 3E. These amounts could be
positive or negative numbers.
Total - Contractor enters the sum of all line items in this column. It must take care to
subtract negative amount(s) included on the above lines. The total amount must equal the
amount in the total adjacent CMS-1522 column.
1. Remarks - Contractor enters an explanation to clarify any item or amount.
• Line Item Definitions - Schedule R:
CMS-1522
1. HI Benefits, Line 1 (d) - Contractor enters the HI benefits amount from form
CMS-1522 in line 1(d).
2. SMI Benefits, Line 2(d) - Contractor enters the SMI benefits amount from form
CMS-1522 in line 2(d).
3. Subtotal - Contractor enters the total HI and SMI benefit amounts.
4. Other Items Identify - Contractor enters any other benefit payments or refunds
that may be unique to your operation that are not included on lines 1(d) or 2(d) of
form CMS-1522. It shall itemize each major category and identify on line 1
through 6. These amounts could be positive or negative numbers.
5. Total - Contractor enters the sum of all line items in this column. It must take care
to subtract negative amounts included in items 1 through 6. The total amount must
equal the amount in the total adjacent CMS-456 column.
Public reporting burden for this collection of information is estimated to average 30 hours
per response. This includes time for reviewing instructions, searching existing data
sources, gathering and maintaining data needed, and completing and reviewing the
collection of information. Send comments regarding this estimated burden or any other
aspect of this collection of information, including suggestions for reducing the burden, to:
Centers for Medicare & Medicaid Services
Office of Financial Management
7500 Security Boulevard

Baltimore MD 21244-1850
and to:
Office of Management and Budget
Paperwork Reduction Project (0938-0361)
Washington DC 20503
100 - Issuance of Letter-Of-Credit - (Rev. 5, 08-30-02)
A1-1416, B1-4414
The Letter-of-Credit, Standard Form-1193, authorizes a Federal Reserve Bank or Branch
to advance funds to a designated commercial bank on behalf of CMS. Under the Checks
Paid Method of financing, a letter-of-credit is issued to authorize the designated
commercial bank to withdraw funds for deposit only to the contractor's Benefits Account
when a bank presents a payment voucher (FMS-5401).
Upon receipt of the properly executed signature cards and notification from the Federal
Reserve Bank that the required collateral has been posted, CMS prepares and certifies a
letter-of-credit in favor of the designated commercial bank. The certified letter-of-credit,
together with the executed signature cards, are sent to the Treasury Department for
forwarding to the servicing Federal Reserve Bank or Branch. A copy of the certified
letter-of-credit and signature cards are also sent to the contractor, the RO, and the
designated commercial bank.
100.1 - Monthly Limitation - (Rev. 5, 08-30-02)
A1-1416.1, B1-4414.1
The letter-of-credit specifies a maximum amount of funds that the bank may draw during
each month. The ceiling amount on the letter-of-credit is established at a sufficiently high
level to provide for fluctuations in monthly disbursement patterns and is based upon
benefit payments estimated by CMS and the contractor. The unused portion of the letter-
of-credit is revoked at the end of each month, and the full monthly ceiling amount is
automatically renewed at the beginning of each month. There is no carryover of any
unused ceiling amount. Each month stands by itself.
100.2 - Amending Letter-of-Credit
(Rev. 236, Issued: 06-13-14, Effective: 06-02-14, Implementation: 07-15-14)
All requests for new or amended Letters Of Credit, whether considered routine or
emergency, must be submitted no later than 6 business days prior to the calendar date of
the actual need. All requests must be sent via email to DFSE@cms.hhs.gov; the
appropriate Regional Office (RO) contacts should also be copied on the request.
Conditions requiring new LOCs include but are not limited to:

• A new MAC joins the Medicare program;
• A MAC assumes a new workload from another MAC;
• A complete or partial change in MAC’s name;
• A change in the name of the MAC’s servicing bank; or
• A change in the Federal Reserve Bank or Branch servicing the MAC’s
commercial bank.
Conditions requiring amended LOCs include but are not limited to:
• A permanent increase or decrease in the LOC funding limitation due to significant
change in Medicare workload or expenditure that is expected to affect the MAC’s
financial needs;
• A temporary increase in the LOC funding limitation to cover all Medicare checks
and Electronic Funds Transfer (EFT) payments presented to the bank for payment
within a given month.
100.3 - Establishment of Accounting Records - (Rev. 5, 08-30-02)
A1-1416.3, B1-4414.3
The contractor shall establish adequate accounting records to ensure that:
• The total monetary amount on the payment vouchers issued during the month
does not exceed the monthly limitation established by the letter-of-credit;
• Funds drawn are properly allocated between HI and SMI benefits. The contractor
shall establish memorandum accounts to separate the respective benefit payments;
• Refunds received from providers or beneficiaries resulting from prior
overpayments or retroactive adjustments are immediately deposited into the
FHIBA. The contractor shall credit all such deposits on the day following the date
of receipt in its mail room or initial point of entry. (It shall credit within 2 days if
the bank is not located in the same city as the contractor.); and
• Bank charges for services furnished are in accordance with the contractual
agreement and that the volume by types of service (e.g., checks paid and deposits)
are in agreement with the contractor's records.
110 - Initial Federal Health Insurance Time Account Deposit - (Rev. 5,
08-30-02)
A1-1418, B1-4416
To preclude excessive use of Federal funds, the contractor shall delay the initial deposit
in the Time Account until it has actually started processing checks that are cleared against
the FHIBA. It shall effect the initial deposit of Federal funds into the Federal Health
Insurance Time Account by drawing a check on the new FHIBA payable to the Time
Account.
It shall establish the amount of the initial time deposit check by re-computing the Award
Schedule (AS) (Page 2 of 2) that the selected bank submits to reflect the effective prime
rate (i.e., prime minus one percent) in effect on the date the new accounts are
implementation.
It shall make the check payable to the designated bank with the following directive
clearly printed on the reverse:
For Deposit Only In (Name of Contractor)
Federal Health Insurance Time Account
The contractor shall delay use of the Federal Health Insurance Accounts until the Federal
Reserve Bank has received authorization from the Treasury Department for the
designated commercial bank to process payment vouchers under the letter-of-credit
procedure.
110.1 - Subsequent Time Account Deposits and Adjustments – (Rev. 5,
08-30-02)
A1-1418.1, B1-4416.1
The quarterly review of bank activity in the Benefits Account may disclose the need for
an adjustment in the Time Account balance. When an adjustment is indicated, the
contractor shall make the adjustment within 15 calendar days after the close of the
quarter.
It shall follow the procedures outlined for the initial Time Account deposit as described
in §110 to increase the Time Account balance.
To decrease the Time Account balance, it shall prepare a Time Account withdrawal slip
that instructs the bank to transfer the amount of the required reduction from the Time
Account to the FHIBA.
NOTE: The contractor shall report all initial deposits and subsequent adjustments in the
Time Account balance on form CMS-1522
110.2 - Bank Account Analysis
(Rev. 158, Issued: 09-25-09, Effective: 10-26-09, Implementation: 10-26-09)
To ensure a continuing evaluation of all bank services and associated charges, the
contractor shall adhere to the following procedures:

• Arrange to receive from the bank its account analysis on a regular monthly basis
no later than the 10th of the following month. Bank analysis must include:
o Bank Processing Charges (Schedule of Itemized Bank Services Provided
Report); and
o A list of daily closing bank balances (Recap of Daily Available Balances).
• The contractor shall verify the accuracy of the data presented for the average daily
bank balance, units of service, and all other computations on the bank's account
analysis.
• The contractor shall complete and forward, within 15 calendar days after the end
of each month to CMS electronically (Excel; [email protected];), the
following schedules:
o Monthly account activity of bank processing charges (Schedule of
Itemized Bank Services Provided Report); and
o Recap of Daily Available Balances (Recap of Daily Available Balances).
120 - Reviewing Bank Agreements - (Rev. 5, 08-30-02)
A1-1420, B1-4418
The contractor shall determine if it wants to continue, renegotiate, or terminate the bank
agreement by reviewing the bank's performance and processing charges for the present
term. It shall review 165 days prior to the expiration of the three-party bank agreement.
If the bank's performance is acceptable, and the bank does not request a rate increase, the
contractor shall recommend to the RO, in writing, that it wants to continue with the bank
agreement and that it be continued for another year or two year period. It shall advise the
RO as soon as a bank's request for a rate increase is received along with its evaluation of
the bank's performance and recommendation, to continue or renegotiate the contract. The
RO develops comparative analysis of three banks' charges with similar volumes to
support the recommendation to continue the bank agreement at a higher processing
charge. If the higher processing charge is not justified, the contractor will be advised to
begin the termination process.
120.1 - Terminating Bank Agreements - (Rev. 5, 08-30-02)
A1-1420.1, B1-4418.1
The contractor, the Government, or the bank may terminate the bank agreement when the
party wishing to terminate submits written notification to the other parties 150 days prior
to the expiration of the current term. In the event of termination, the bank agrees to retain
the contractor's Federal Health Insurance Account(s) for an additional 180-day period
(phase-out) beyond the current term to allow for clearance of outstanding checks.
120.2 - Terminating Federal Health Insurance Accounts - (Rev. 5, 08-
30-02)
A1-1420.2, B1-4418.2
• Initial Adjustment to the Federal Health Insurance Time Account - Pending
receipt of the prior month's bank statement, the contractor shall reduce on the first
day of the phase-out period the current balance in the Federal Health Insurance
Time Account by seventy-five percent (75%). It shall prepare a Time Account
withdrawal slip that instructs the bank to immediately transfer the computed
amount to the FHIBA.
• Time Account Analysis - Within 7 days of the expiration of the current term, the
contractor shall complete Schedule TAA in its entirety to determine whether the
time account should remain open during the phase-out period. It shall include in
line 4 the total projected service charges for the entire phase-out period. It shall
modify the 25 percent figure on line 10 to reflect the actual length of the phase-
out period, e.g., 6-month period would show 50 percent.
o If line 13 of Schedule TAA (page 1 of 3) indicates a positive amount, the
contractor shall maintain that amount of money in the time account during
the phase-out period, and adjust the present time account balance
accordingly in lines 14-16.
o If line 9 of Schedule TAA (page 1 of 3) indicates a negative amount, the
contractor shall immediately transfer the current time account balance to
the benefits account, and the contractor should secure from the bank a
check payable to the benefits account in an amount equal to the negative
amount reflected on line 9.
• Closing Federal Health Insurance Time Accounts - At the expiration of the phase-
out period, the contractor shall transfer all funds on deposit in the Time Account,
if applicable, and FHIBA immediately to the new FHIBA.
120.3 - Phase-out Period for Federal Health Insurance Bank Accounts –
(Rev. 5, 08-30-02)
A1-1420.3, B1-4418.3
In the event of termination of the bank agreement, the bank agrees to retain the
contractor's Federal Health Insurance Account(s) for up to an additional 180-day period,
beyond the current term, to allow for clearance of outstanding checks. (See subsection C
of the IFB.) The letter-of-credit issued to the bank remains in effect to allow the bank to
draw payment vouchers to cover all outstanding checks as they are presented for
payment.
During this phase out period, the current bank agreement continues in effect with the
exception of the following:
• Letter-of-Credit - Covenant 5;
• The Term of the Bank Agreement - Covenant 7;
• Termination of Agreement - Covenants 8 and 9; and
• Renegotiation of Agreement - Covenant 10.
It is further understood that during the phase out period:
• The bank maintains collateral in an amount sufficient to cover the high balances
in the account(s) less FDIC coverage on each account;
• All bank service charges and earnings credits are consistent with those amounts
reflected in the current agreement;
• All terms and conditions of the original bid submitted by the bank, which are not
inconsistent with this additional term, remain in effect; and
• The contractor continues to complete the CMS-1521, CMS-1522 and the TAA
Schedules.
130 - Invitation For Bid (IFB) to Provide Banking Services Under The
Checks Paid Method of Letter-Of-Credit Financing - (Rev. 5, 08-30-02)
A1-1422, B1-4420
The contractor shall request the most recent copy of the IFB package from the RO to
prepare its procurement. The IFB is constantly being updated to meet CMS requirements
in the changing banking environment.
140 - Bonding - (Rev. 5, 08-30-02)
A1-1424, B1-4422
The contractor is required to have a fidelity bond on, as a minimum, each certification
and disbursement employee. Blanket bonds are an acceptable alternative.
Bonds must protect against at least the risks contained in the contractor's agreement
(specified in the article entitled "Certification and Disbursement and Indemnification").
As a general rule, the amount of the bond should equal 1/10 of the monthly limitation of
the letter of credit but not exceed $500,000.
CMS accepts a bond in excess of $500,000 and assumes an allocated share of its total
cost if the contractor determines that a larger bond is desirable.
No deductibles are permitted with respect to coverage, risks, and amounts.
150 - Letter-Of-Credit Check List
(Rev. 158, Issued: 09-25-09, Effective: 10-26-09, Implementation: 10-26-09)
FORM NAME
DUE DATE
Intermediary Benefit Payment Report,
CMS-456
Monthly - within 20 working days after the
end of the reporting month.
Payment voucher on Letter-of-Credit
Transmittal - CMS-1521
Monthly - within 15 days after the end of
the reporting month.
Monthly Intermediary Financial Report,
CMS-1522
Same as above
Banking Schedules,
Schedule of Itemized Bank Services
Provided Report and Recap of Daily
Available Balances
Monthly - within 15 days after the end of
the reporting month
160 - Electronic Funds Transfer (EFT) - (Rev. 5, 08-30-02)
A1-1430, B1-4430
The contractor shall pay claims from providers of services according to the following
criteria.
A. Requirement
The contractor may transmit payments electronically to each provider who bills
Medicare, elects to receive payments electronically, and who provides the necessary bank
account and routing data to enable the contractor to pay electronically.
B. Notification Requirement
The contractor shall provide its Regional Office (RO) with quarterly data on the number
of providers paid under EFT, the transmission protocol, such as the ANSI X12 835 used
for its EFT transmissions, and the benefit payment amount of EFT transactions. It shall
use Form CMS-588, Authorization Agreement for Electronic Funds Transfer, to maintain
a record of those physicians and suppliers that authorize Medicare payment under EFT.
C. Claims Processing Timeliness (CPT) Requirement
When transmitting electronic payments to providers, the contractor shall pay claims in a
timely manner consistent with the payment floor in effect at the time of payment. It shall
transmit the EFT authorization to its originating bank upon the expiration of claims
processing timeliness payment floor, as discussed in the Medicare Claims Processing
Manual, Chapter 1, General Billing Requirements. For example, an EFT payment in
March 2001 for an electronic claim may not be transmitted to the originating bank earlier
than 14 days after the date of receipt. An EFT payment in March 2001 for a paper claim
may not be transmitted to the originating bank earlier than 27 days after the date of
receipt. Payment settlement, i.e., the date on which funds are posted to the provider's
account, should not be earlier than 2 business days following transmission of the
electronic payment data to the originating bank. The contractor shall accomplish this by
designating an effective payment date on the electronic payment file of no earlier than 2
business days after the transmission date.
D. Electronic Transmission Standard
When making direct deposits to the accounts of providers under EFT, the contractor shall
use a transmission format that is both economical and compatible with its servicing bank
and the Automated Clearing House.
For Standard Systems Maintainers, the Medicare standard ANSI 835 health care
payment/advice can be abbreviated and used to generate an ACH-FORMATTED EFT
file that contains no beneficiary-specific data. In these cases, the bank translates the
abbreviated ANSI 835 into an ACH-COMPATIBLE payment file. The entire ANSI 835
Remittance advice record will be sent directly to the provider. In the event these
abbreviated ANSI data are not acceptable to certain banks for purposes of initiating
electronic payments through the appropriate ACH, the standard system users should
consult with their individual banks to determine which electronic payment data format is
acceptable. The contractor should refer to Part 3, Chapter 24, EDI Support Requirements
for more information on the abbreviated ANSI-835.
E. Alternatives to Electronic Payment
When EFT is not used, the contractor shall make payments to providers via hardcopy
checks drawn on the commercial bank servicing its Medicare account. It shall send the
hardcopy check by first class U.S. Postal Service only.
NOTE: The pickup, next-day delivery, express mail or the use of a courier service for
hardcopy checks is prohibited except in emergency situations, as authorized by the
contractor's RO.
F. Modification of Tri-partite Bank Agreement to Include EFT Method of Payment
The contractor shall work with its servicing bank and its RO to ensure that the Tri-partite
bank agreement is modified to include wording that allows funding of the Letter of Credit
to include electronic payments as well as hardcopy checks. The Tri-partite bank
agreement needs to clearly state that all references to checks in the original bank
agreement shall mean checks and/or electronic funds transfer (EFTs).
The contractor shall have its legal department and that of the originating bank review the
Tri-partite bank agreement to ensure that it meets contractor needs and the requirements
of the Medicare program. It shall forward any modifications to the Tri-partite bank
agreement at least 1 month prior to its effective date to the RO and the Chief, Financial
Management Unit, OCA, BPO in CO for review and approval. See §160.1, Exhibit 2 for
a sample addendum to the Tri-partite bank agreement that includes general provisions for
payment under the EFT method.
G. The Receiving Bank's Role in EFT/Electronic Remittance Advice (ERA)
While providers may wish to consider criteria such as experience with EFT and receipt of
ANSI-formatted financial data when choosing a bank, these procedures should in no way
be interpreted as requiring providers to do business with a particular financial institution
(e.g., receiving bank only).
H. Electronic Funds Transfer Transaction Costs
Prior to transmitting payments electronically, the originating bank fills in the relevant
EFT transaction costs on the Schedule AS (Schedule of Bank Processing Charges), and
submits it to the contractor. The contractor shall transmit this information to both the RO
and CO. Once electronic payments are initiated, the originating bank shall include all
payment information on the Monthly Schedule of Bank Processing Charges, (TAA 1-b),
and transmit this form to the contractor, who enters the data into the Contractor
Administrative Budget and Financial Management (CAFM) system where it is reviewed
and approved first by the RO and then CO.
NOTE: The EFT costs reported on line 8 of the AS Schedule and the Monthly Schedule
of Bank Processing Charges (TAA 1-b) shall include a breakdown of all costs associated
with EFT, including the cost per EFT transaction, set-up costs, monthly charges,
transmission costs, etc.
I. Contractor Responsibility for EFT/ERA Records Retention
The contractor shall retain records on EFT/ERA in accordance with established CMS and
Department of Justice procedures for retention of documentation associated with
electronic claims.
J - Provider Responsibility for the Accuracy of Claims Data
To minimize errors and disruptions to cash flow, providers are responsible for verifying
the accuracy of claims payment information submitted to their Medicare contractor.
170 - Electronic Remittance Advice (ERA) - (Rev. 5, 08-30-02)
A1-1431, B1-4431
The contractor shall accommodate provider requests to receive hardcopy checks or
electronic payments with ERAs. Providers have the option to receive remittance
information on paper or electronically. Providers who elect EFT are not required to
receive ERAs. The contractor shall furnish ERAs to providers using the following
criteria:
A. Standard Format Requirement
In lieu of the traditional method of sending hardcopy remittance advices and checks to
providers, effective October 1, 1992, the contractor shall transmit, over wire only, the
ANSI X12.835, Health Care Claim Payment/Advice (ANSI-835) to a requesting provider
or to a requesting provider's billing service. The ANSI-835 is the only electronic
remittance option available as of this date. If the contractor has any technical questions
on formats or electronic remittance transmission requirements, it should contact its RO.
B. Privacy Act Compliance
Unless otherwise directed by CO, the contractor shall ensure that remittance information
is transmitted to providers or their authorized billing agents either directly, through a
Value Added network, or as authorized by a provider, to a bank that is capable of
receiving ERA data and agrees to safeguard the data.
C. Reconciliation Requirement
Prior to entering into an electronic payment arrangement with a provider, the contractor
shall ensure that its providers are able to reconcile their accounting records using the
ANSI-835 remittance advice. Once this determination is made, it shall provide telephone
support during normal business hours and allow for an initial reconciliation period of up
to 30 days during which it will produce both paper and electronic remittances. After this
30-day phase-in period, it shall eliminate paper remittances for these providers.
D. Standard Format Reference
See the Claims Processing Manual, Chapter 22 - Remittance Notice to Providers, for
information and additional requirements concerning the standard remittance advice
format.
180 - Exhibits - (Rev. 5, 08-30-02)
A1-1435
Exhibit 1 - Form CMS-1521 - - See CMS Forms page.
Exhibit 2 - Form CMS-1522 - - See CMS Forms page.
Exhibit 3 - Intermediary Benefit Payment Report - - See CMS Forms page.
Exhibit 4 -Authorization Agreement for Electronic Funds Transfer
PROVIDER/PHYSICIAN
PROVIDER/PHYSICIAN
NAME____________________
ID NUMBER___________________
I hereby authorize (Insert Contractor Name), hereinafter called COMPANY, to initiate
credit entries and to initiate, if necessary, debit entries and adjustments for any credit
entries in error to my ( ) Checking ( ) Savings account (select one) indicated below and
the depository named below, hereinafter called DEPOSITORY, to credit and/or debit
the same to such account.
DEPOSITORY
NAME _____________________
BRANCH _____________________
CITY ______________________
STATE ______ ZIP ____________
TRANSIT
NUMBER ____________
ACCOUNT NUMBER ____________
This authority is to remain in full force and effect until COMPANY has received
written notification from me of its termination in such time and in such manner as to
afford COMPANY and DEPOSITORY a reasonable opportunity to act on said notice of
termination.
NAME ________________________
TITLE _____________________
(PLEASE PRINT)
SIGNED X ______________________
DATE _____________
Exhibit 5 - Addendum to Medicare Bank Agreement
The parties have executed this Agreement for the Medicare A(B) Bank Accounts using
the Checks Paid Method of Letter of Credit Financing and desire to add changes to the
existing agreement currently in force. These changes are necessitated by the
implementation by (Insert Contractor Name) of the Electronic Funds Transfer (EFT)
method of paying providers effective (Insert Date). This change in payment method is
under the direction of the Centers for Medicare and Medicaid Services (CMS) as an
initiative to increase the uniformity and efficiency of the provider payment process.
Also, item number 10 below, although not related to EFT, is incorporated into the bank
agreement to insure that no excessive earnings credits accumulate during the period of
the bank agreement.
The parties hereby agree to the following terms and conditions that shall be considered an
integral part of the bank Agreement:
1. The rates as reflected on the Schedule of Bank Processing Charges shall be in
effect for the term of this Agreement.
2. This Agreement, with all its provisions and covenants, shall continue in force
from year to year after the expiration of such term; provided, however, that
notification to terminate or renegotiate has not been given by any party as
specified in the Agreement executed on (Insert Date).
3. All references to checks in the original Agreement shall hereby mean checks
and/or Electronic Funds Transfers (EFTs).
4. The Fiscal Intermediary (Carrier) is obligated to obtain, retain, and provide copies
of provider authorizations, particularly with regard to the rights, liabilities, and
responsibilities of Medicare contractors and financial institutions under
Regulation E.
5. The nature, format and medium of entries, or entry information is to be furnished
to the originating bank in writing by the Fiscal Intermediary (Carrier) prior to
entering into an EFT arrangement.
6. The Fiscal Intermediary (Carrier) and the originating bank shall negotiate the
level of security to be established for delivering the payment data from the Fiscal
Intermediary (Carrier) to the originating bank, such as transmittals with
authorized signatures, and the method used to verify authenticity of
telecommunicated data, prior to entering into an EFT arrangement.
7. The Fiscal Intermediary (Carrier) shall specify the time when funds are to be
provided to the originating bank prior to entering into an EFT arrangement.
8. The Fiscal Intermediary (Carrier) and the originating bank shall agree to the
deadline for reversals, corrections, or changes by the Fiscal Intermediary (Carrier)
of entries or entry information furnished to the originating bank prior to entering
into an EFT arrangement.
9. In those cases where the Fiscal Intermediary's (Carrier's) Medicare bank is unable
to originate EFT transactions, the Medicare bank may subcontract certain
functions. The Medicare bank agrees that none of the functions to be performed
under the Tri-partite agreement shall be subcontracted without prior written
approval of the Fiscal Intermediary (Carrier) and the CMS. Any such approved
subcontract shall contain the language of the Examination of Records Clause
contained in the bank agreement (Covenant 3).
10. If Line 7 of Page 1 of the Quarterly Time Account Adjustment Schedule reflects
any positive balance, the contractor shall immediately forward supporting
documentation and a check made payable to CMS for that amount to:
Send a copy of the check and transmittal letter to:
Centers for Medicare & Medicaid Services
Office of Financial Management
7500 Security Boulevard
Baltimore MD 21244-1850
190 - General Information About Termination Costs - (Rev. 5, 08-30-02)
A1-1800
The contractor shall prepare a shut-down cost budget voucher based on its natural
expense line items, and submit the budget to both CMS's Central Office (CO) and to the
contractor's Regional Office (RO).
It shall include the following information on the voucher:
• All incurred shut-down expenses determined by the contractor's natural cost
items;
• The amount, and a detailed explanation, for each item it claims; and
• An attestation signed by a company official that validates the costs the contractor
is claiming are correct.
The CMS pays shut-down costs based on the contractor's voucher's information. The
contractor shall not draw administrative funds, via its letter-of-credit, after the official
date of either contract close-out or termination.
It shall submit the voucher on official company letterhead. It shall make sure the voucher
is signed by an authorized company official, and forward a copy to CMS's CO at the
following address:
Centers for Medicare & Medicaid Services
Division of Contractor Financial Management, OFO
7500 Security Boulevard
Baltimore MD 21244-1850
200 - General - (Rev. 14, 02-03-03)
A1-1900, B1-4900
The Contractor Financial Reports provide a method of reporting financial activities for
benefit payments by Medicare contractors according to the Chief Financial Officers
(CFOs) Act of 1990. The contractor is required to maintain accounting records according
to government accounting principles and applicable government laws and regulations.
This requirement complies with the Office of Management and Budget (OMB) Bulletins
about Financial Statements. These policies and procedures are developed by the Federal
Accounting Standards Advisory Board (FASAB).
The accounting principles and the auditing standards required are not substantially
different from Generally Accepted Accounting Principles (GAAP) and Generally
Accepted Auditing Standards (GAAS) as formulated by the accounting profession.
Government accounting principles which are developed by FASAB, however, require
maintaining records not only for preparing financial statements, but also to enforce
applicable laws and regulations. Accounts are maintained to provide control over
operations as well as to provide financial information.
Medicare contractors are required to use double entry bookkeeping and accrual basis
accounting. For example, if an accounts receivable is established, accounts receivable
should be debited and, most likely, operating/program expense should be credited. If an
accounts payable is established, accounts payable should be credited and, most likely,
operating/program expense should be debited. In addition, the information reported must
be supported by the contractor's books and records as of the end of the period requested
and adequate audit trails must be maintained. To ensure accurate reporting, proper cutoff
procedures must also be established in order to limit reporting to activities attributable to
the reporting period. Where actual data is not available, reasonable estimates are
acceptable. See Exhibits 12 through 15 for protocols for estimating relevant accounts.
When end of period entries are made to accrue account balances, the contractor shall
reverse the entries in the following quarter to allow normal processing of accounting
transactions.
In order to maintain consistent and accurate financial reporting, Medicare contractors
must have an internal control structure that integrates the accounting and claims
processing systems. The internal control structure must provide for the following control
procedures:
1. Independent review of proper valuation of recorded amounts and performance;
2. Segregation of duties (separate authorization, record-keeping, and custody);
3. Safeguards over access to assets and records;
4. Authorization of transactions and activities;
5. Documents and records that are adequate to ensure proper recording; and
6. Quarterly reconciliation of internal systems to the Provider Overpayment Report
(POR) system for intermediaries and the Physician Supplier Overpayment Report
(PSOR) system for carriers.
Supporting documentation must be maintained and available for review and audit. This
must include lead schedules for all amounts used for report preparation and detailed
documentation, such as demand letters for accounts receivable. A very good procedure
that CMS recommends to ensure the accuracy of reported amounts, is trending and
comparative analysis. This analysis involves comparing reported amounts to prior
amounts to identify material errors.
Hardcopy books and records used to prepare the annual financial reports should be
retained for 6 years unless microfilmed. Then, the hardcopy needs to be retained for 3
years and the microfilm retained for the balance of the 6-year period.
The Office of the Inspector General (OIG) will conduct audits of contractors according to
government auditing standards. This requirement complies with OMB Bulletin No. 98-
08, Audit Requirements for Federal Financial Statements. Applicable government laws
and regulations also supplement the government auditing standards. These standards are
similar to those contained in the Comptroller General of the United States Standards for
Audit of Governmental Organizations, Programs, Activities, and Functions (The Yellow
Book).
The OMB Bulletin No. 01-09, Form and Content of Agency Financial Statements
requires the preparation of Federal Agency interim financial statements, in addition to
accelerating the due date of the submission of year-end audited financial statements to
OMB and Congress. Because of OMB's new requirements, CMS and its Medicare
contractors must be able to prepare financial statements at the end of any month at the
request of CMS.
To meet this obligation, all shared systems must be able to produce any system reports
required by Medicare contractors utilizing those systems to prepare all the Forms CMS-
750 A/B and the Forms CMS-751 A/B on a month-end basis. These reports must be
cumulative in order to provide Medicare contractors' financial position and status of
accounts receivable activity from the beginning of the fiscal year through the month
requested.
Medicare contractors must be able to support all summary amounts reported on any of
these reports with transaction level detail, and must be able to produce this support upon
request by CMS or internal/external auditors.
210 - Instructions For Completing The Form CMS-750A/B, Contractor
Financial Reports - (Rev. 5, 08-30-02)
A1-1910, B1-4910
There are separate reports and data screens for Part A, Hospital Insurance (HI), and Part
B, Supplementary Medical Insurance (SMI) in the Contractor Administrative-Budget and
Financial Management (CAFM) system. The intermediary enters data in both HI and
SMI data screens (see Exhibits 1 and 2). The carrier enters data in the SMI data screens
(see Exhibit 2).
The data for the report is HI and SMI financial information as defined in the Medicare
Account Definitions (see Exhibit 11). In order to facilitate reconciliation, balancing and
error resolution, the contractor shall report all data in dollars and cents.
The data on the report may not equate on a one-to-one basis with data reported to CMS in
other reports, such as Draws on Letter of Credit, reported on Form CMS-1521. The
contractor must maintain records that will allow reconciliation of Form CMS-750A/B
with those other reports.
220 - Due Date - (Rev. 5, 08-30-02)
A1-1911, B1-4911
This report is due on January 21, April 21, July 21, October 21 (21 days after the end of
each quarter) via the CAFM system. If that date occurs on a holiday or a weekend, the
report is due the following Federal workday.
230 - Certification - (Rev. 5, 08-30-02)
A1-1912, B1-4912
Medicare contractor certification by the Chief Financial Officer (CFO) is required. The
CFO must input their password on the CAFM system (see Exhibit 16). Failure to record
the official's password is a serious error that will prevent acceptance of the report by the
CAFM system. The following statement appears at the end of the Form CMS-750A/B:
I hereby CERTIFY that I have examined the Statement of Financial Position prepared by
[name of contractor] for the period beginning (first day of FY) and ending (last day of
quarter), and that to the best of my knowledge and belief, it is a true, correct and
complete statement prepared from the books and records of the contractor in accordance
with applicable instructions.
NAME _______________ Date __________ Title ___________
240 - Instructions for Completing Form CMS-751 A/B, Status of
Accounts Receivable - (Rev. 5, 08-30-02)
A1-1920, A1-1940, B1-4920, B1-4960
Forms CMS-H751A/B and CMS-M751A/B are similar data entry screens used to report
the following receivables.
• Form CMS-H751A to report debt under Part A (HI) by intermediaries
• Form CMS-H751B to report debt under Part B (SMI) by intermediaries and
carriers
• Form CMS-M751A to report MSP debt under HI by intermediaries;
• Form CMS-M751B to report MSP debt under SMI by intermediaries and carriers;
MSP accounts receivable data reported on CMS-M751A/B is a subset of total accounts
receivable data reported on Form CMS-H751A/B (e.g., 751A/B includes the data
reported on the CMS M751A/B and non-MSP data.
The screen heading indicates whether the report is for the MSP subset.
Samples of the screens are shown in Exhibits 3 - 9. There are separate reports and data
screens for Part A, HI, and for Part B, SMI in the CAFM system. The intermediary enters
data in both HI and SMI data screens (Exhibits 3 and 4). The carrier enters data in only
the SMI data screens (Exhibit 4).
The intermediary or carrier reports the accounts receivable activity for fiscal year-to-date
(FYTD) for the period of the report. In order to facilitate reconciliation, balancing and
error resolution, it reports the accounts receivable in dollars and cents.
The reports require information both for the amount and the number of accounts
receivable. To provide standardization, CMS suggests that contractors use their collection
process as a guide when reporting the number of accounts receivable. For example, a
separate, stand alone accounts receivable collected would be reported as a quantity in the
number column.
EXAMPLES:
1. (Intermediaries only). A cost report is one receivable. Even though several claims
are associated with the cost report, the collection activity would be against the
entire cost report rather than each claim.
2. A demand letter issued in a Medicare Secondary Payer (MSP) case to one debtor
with several claims listed on the letter. If the collection is made and posted against
an individual claim, each claim on the demand letter would be an individual
receivable.
3. A demand letter issued to a physician based on adjustments projected from
sampling claims equals one. Even though many claims are represented by
projection of the sample.
Once the principal number is established, the contractor shall report the interest
associated with the principal amount in the same manner. There can be a difference
between the principal number and the interest number because some receivables are not
subject to interest.
250 - Due Date - (Rev. 5, 08-30-02)
A1-1921, A1-1941, B1-4921, B1-4941
This report is due on January 21, April 21, July 21, October 21 (21 days after the end of
each quarter) via the CAFM system. If that date occurs on a holiday or a weekend, the
report is due the following Federal workday.
260 - Certification - (Rev. 5, 08-30-02)
A1-1922, A1-1942, B1-4922, B1-4942
Medicare contractor certification by the CFO is required. The CFO must input their
password on the CAFM system (see Exhibit 16). Failure to record the official's password
is a serious error that will prevent acceptance of the report by the CAFM system. The
following statement appears at the end of Form CMS-H751A/B:
I hereby CERTIFY that I have examined the Status of Accounts Receivable
prepared by (name of contractor) for the period beginning (first day of FY) and
ending (last day of quarter), and that to the best of my knowledge and belief, it is
a true, correct and complete statement prepared from the books and records of the
contractor in accordance with applicable instructions.
For (Status of MSP Accounts Receivable) (Form CMS-M751) the statement includes a
reference to MSP and reads as follows:
I hereby CERTIFY that I have examined the Status of MSP Accounts Receivable
prepared by (name of contractor) for the period beginning (first day of FY) and
ending (last day of quarter), and that to the best of my knowledge and belief, it is
a true, correct and complete statement prepared from the books and records of the
contractor in accordance with applicable instructions.
The name, date and title of the person making the certification are on both certifications.
270 - Line Item Instructions Form CMS-H751A/B - (Rev. 5, 08-30-02)
A1-1923, A1-1943, B1-4923, B1-4943
Medicare contractors must develop and maintain transaction level detail (at a minimum,
this would include the provider name, provider number, date of determination,
outstanding balance, and any adjustments or recoupments) by debt to support the
amounts reported for each line outlined below.
In addition, non-MSP amounts must be reconciled to the POR (intermediary) or PSOR
(carrier) system as applicable.
Part I, Status of Receivables
For each line in Section A, below, the instruction applies to each the Form CMS-H751
and Form CMS-M751, and to the intermediary report and to the carrier report unless
otherwise noted. The instructions are applicable only to MSP amounts for the Form
CMS-M751 and are applicable to all amounts for the Form CMS-H751.
Section A - Outstanding Receivables
270.1 - Line 1, Beginning FY Balance (Principal & Interest) –
(Rev. 5, 08-30-02)
A1-1923.1, A1-1943.1, B1-4923.1, B1-4943.1
The contractor enters the number and amount for all accounts receivable outstanding as
of the beginning of the FY. These amounts will be pre-filled with the ending balances
reported on the preceding (9/30/XX) FY Contractor Financial Reports. The contractor
must make any corrections to the beginning principal and interest FY balance on Line 5a,
Adjusted Amounts, Internal Adjustments. It shall apply the offsetting entry, on the related
Form CMS-750A/B report (debit or credit) to Operating/Program Expense for
transactions that affect principal, or interest revenue if the transaction affects interest.
270.2 - Line 2a, New Receivables (Principal) - (Rev. 5, 08-30-02)
A1-1923.2, A1-1943.2, B1-4923.2, B1-4943.2
The contractor enters the number and amount for all new receivables established at its
location during the FY. New receivables for intermediaries include cost report
settlements and credit balances. For both intermediaries and carriers, overpayments and
claims accounts receivables for all claim types are included. For carriers only, beneficiary
debt and under-tolerance accounts receivable are included.
For MSP new receivables includes group health plan data-match, non-data-match,
liability (including worker's compensation, auto and no fault), etc.
The contractor does not include those receivables transferred from other Medicare
contractors, other CMS locations, Currently Not Collectible (CNC), or other transferred
locations in prior fiscal periods. It includes all of these items on Lines 5b, 5d, 5f, or 6b,
Transferred In Amounts.
NOTE: MSP accounts receivable are not established until a settlement, judgment or
award has been reached and a demand letter is sent.
270.3 - Line 2b, Accrued Receivables (Principal) - (Rev. 5, 08-30-02)
A1-1923.3, A1-1943.3, B1-4923.3, B1-4943.3
Line 2b is not applicable to carriers or to MSP.
The intermediary enters the number and amount of Periodic Interim Payment (PIP)
accrued receivables, fiscal year-to-date on this line. The only receivables a FI will accrue
are those that result from comparing PIP payments to claims submitted. For each
quarterly reporting period, a new accrual is established and the prior quarter's accrual
must be reversed or zeroed out. Both the establishment and reversal of the PIP accrual
must be reflected in this line, except for the reversal of the September's quarterly accrual,
which would be reflected in Line 5a, Adjusted Amounts, Internal Adjustments (see
Exhibit 13, Periodic Interim Payments (PIP) Protocol for Estimating
Payables/Receivables for the Form CMS-750A/B, Statement of Financial Position).
270.4 - Line 3, Interest Earned (Interest) - (Rev. 5, 08-30-02)
A1-1923.4, A1-1943.4, B1-4923.4, B1-4943.4
The contractor enters the number and amount of interest earned on: (a) existing or new
receivables established at its location during the FY; and (b) the interest earned on
receivables transferred to it, following the date the receivables are established on its
records. The contractor shall not include the amount of accrued interest earned at other
locations. It shall report the accrued interest earned at other locations as transferred in on
Line 5b, 5d, 5f or 6b, Transferred In Amounts.
270.5 - Line 4a, Cash/Check Collections on Receivables (Principal &
Interest) - (Rev. 5, 08-30-02)
A1-1923.5, A1-1943.5, B1-4923.5, B1-4943.5
The contractor enters the amount collected by cash or check on receivables during the
fiscal period.
270.6 - Line 4b, Offset Collections on Receivables (Principal & Interest)
- (Rev. 5, 08-30-02)
A1-1923.6, A1-1943.6, B1-4923.6, B1-4943.6
The contractor enters the amount collected by offset on receivables during the fiscal
period.
270.7 - Line 4c, Collections Deposited at Another Location (Principal &
Interest) - (Rev. 5, 08-30-02)
A1-1923.7, A1-1943.7, B1-4923.7, B1-4943.7
The contractor enters the amount collected or offset by CMS Central Office (CO) for
collections on accounts receivable referred under the Debt Collection Improvement Act
(DCIA). Do not transfer the case to CO where the deposit or offset of the money is made.
Upon receipt of the Collection Reconciliation/Acknowledgement form, enter the amount
collected or offset by cross servicing/TOP and received by CO in this line to reduce the
outstanding amount of the receivable being reported on Form CMS-751A/B. CO will
record the actual deposit of cash/check/offset on Line 10, Cash/Offsets Received for
Receivables at Another Location of its' Form CMS-R751.
The Medicare contractor or CO that records the actual deposit of cash/check/offset will
record this amount on Line 10, Cash/Offsets Received for Receivables at Another
Location. (See §270.15 for instructions and Exhibit 18 Collection Reconciliation/
Acknowledgement Form).
270.8 - Line 5, Adjusted/Transferred/Waived Amounts (Principal &
Interest) - (Rev. 5, 08-30-02)
A1-1923.8, A1-1943.8, B1-4923.8, B1-4943.8
The contractor enters the amount of receivables it has adjusted, transferred in from or out
to other locations, or waived. It is required to maintain supporting documentation and
records for all these receivables transferred in and out. Amounts transferred in from or
out to other CMS locations or Medicare contractors must be reconciled to the other
entity's records for the same reporting period prior to submission of the quarterly reports
to ensure that only approved transfers are being reported. Documentation of the
reconciliation must be maintained and must indicate that a supervisory review of the
reconciliation was performed. Refer to Exhibit 17 for instructions for the transfer of debt
between other reporting entities.
The contractor reports in Lines:
5.
a. Adjusted Amounts (Principal & Interest). The contractor enters the
amount for any adjustments to the beginning balance, or
corrections/adjustments of receivables previously established during the
fiscal period. These adjustments can be either positive or negative. It
separately reports adjustments resulting from Auditor/Consultant
recommendations, and those determined independently.
b. Transfers In from other Medicare Contractors (Principal & Interest). The
contractor enters the amount transferred in from other Medicare
contractors during the fiscal period.
c. Transfers Out to other Medicare Contractors (Principal & Interest). The
contractor enters the amount transferred out to other Medicare contractors
during the fiscal period.
d. Transfers In from other CMS Locations, POR/PSOR (Principal &
Interest). (Carriers report PSOR, and intermediaries report POR). The
contractor enters the amount transferred in from other CMS locations and
reported on the POR/PSOR during the fiscal period. (Applies to non-MSP
debt only.)
e. Transfers Out to other CMS Locations, POR/PSOR (Principal & Interest).
Carriers report PSOR, and intermediaries report POR). The contractor
enters the amount transferred out to other CMS locations and reported on
the POR/PSOR during the fiscal period.
f. (Applies to non-MSP debt only)
g. Transfers In from other CMS Locations, Not POR/PSOR (Principal &
Interest). The contractor enters the amount transferred in from other CMS
locations and not reported on the POR/PSOR during the fiscal period.
h. Transfers Out to other CMS Locations, Not POR/PSOR (Principal &
Interest). The contractor enters the amount transferred out to other CMS
locations and not reported on the POR/PSOR during the fiscal period.
i. Waivers (Principal & Interest). The contractor enters the amount of
accounts receivable waived based on the application of §§ 1862(b) and
1870(c) of the Social Security Act.
270.9 - Line 6, Amounts Written-off Closed (Bad Debts)/Transferred
CNC (Principal & Interest) - (Rev. 5, 08-30-02)
A1-1923.9, A1-1943.9, B1-4923.9, B1-4943.9
The contractor enters the amount which it has written-off as a bad debt, or transferred to
or from CNC.
The contractor reports in lines:
6.
a. Amounts Written-off Closed (Bad Debts)(Principal & Interest). The
contractor enters the amount for which collection efforts have been
abandoned. (This would include the remaining balance on accounts
receivable after the bankruptcy court has ruled on bankruptcy, appeals,
and other litigated cases).
b. Transfers In from CNC (Principal & Interest). The contractor enters the
amount re-established as active debt that was previously classified as CNC
during the fiscal period.
c. Transfers Out to CNC (Principal & Interest). The contractor enters the
amount removed from the ending balance and reclassified as CNC during
the fiscal period.
270.10 - Line 7, Ending Balance (Principal & Interest) - (Rev. 5, 08-30-
02)
A1-1923.10, A1-1943.10, B1-4923.10, B1-4943.10
The ending balance is a computed field reporting the number (manual entry) and amount
for receivables outstanding as of the end of the reporting period. It equals:
Principal
Interest
+
Beginning FY balance (Line 1)
+
Beginning FY balance (Line 1)
Principal
Interest
+
New Receivables (Line 2a)
+
Interest Earned (Line 3)
+/-
Accrued Receivables (Line 2b)
-
Collections on Receivables (Line 4a-
4c)
- Collections on Interest (Line 4a-c)
+/-
Adjusted/Transferred Amounts (Line
5a-5g)
+/-
Adjusted/Transferred Amounts (Line
5a-5g)
-
Waivers (line 5h)
-
Waivers (line 5h)
+/-
Amounts Written-off/Transferred
CNC(Lines 6 a - c)
Amounts Written-off/Transferred
CNC (Lines 6 a - c)
=
Ending Balance (Line 7)
=
Ending Balance (Line 7)
NOTE: Although Line 7 is a calculated amount, the contractor must be able to provide a
detailed listing of all outstanding receivable balances that support this line at any given
period of time. The ending balance must be equal to the accounts receivable and interest
receivable amounts reported on the form in Statement of Financial Position.
270.11 - Line 7a, Current Receivables (Principal and Interest) –
(Rev. 5, 08-30-02)
A1-1923.11, A1-1943.11, B1-4923.11, B1-4943.11
The contractor enters the amount of the receivables due within 12 months following the
reporting period. The definition of current and non-current does not depend on the time a
debt is outstanding but when the debt is due. A receivable for which the due date is 12
months or less from the report date is a current receivable. For example, a debt due
September 30, 2003, within 12 months from the date of a report for September 30, 2002,
is a current receivable. In addition, all delinquent receivables are to be reported as
current. The contractor shall assign between current and non-current the appropriate
amount of those receivables for which it has negotiated extended repayment schedules,
based on the installment payment dates.
270.12 - Line 7b, Non-current Receivables (Principal) - (Rev. 5, 08-30-
02)
A1-193.12, A1-1943.12, B1-4923.12, B1-4943.12
The contractor enters the amount of non-current receivables due more than 12 months
after the reporting period. The definition of non-current receivables includes those
receivables for which the due date is more than 12 months from the end of the reporting
period. For example, those receivables for which the due date is October 1, 2003, 1 year
from the date of a report for September 30, 2002, are non-current receivables.
270.13 - Line 8, Allowance for Uncollectible Accounts (Principal &
Interest) - (Rev. 5, 08-30-02)
A1-1923. 13, A1-1943.13, B1-4923.13, B1-4943.13
The contractor enters the amount of the ending balance reported in Line 7 for accounts
receivable it estimates will not be collectible. (See Exhibit 14, Allowance for
Uncollectible Accounts).
270.14 - Line 9, Total Receivables Net of Allowance - (Rev. 5, 08-30-02)
A1-1923.14, A1-1943.14, B1-4923.14, B1-4943.14
Total Receivables Net of Allowance is a computed field (Line 7 less Line 8) reporting the
contractor's estimate of the amount of accounts receivable it reasonably expects to
collect.
270.15 - Line 10, Cash/Offsets Received for Receivables at Another
Location (Principal & Interest). - (Rev. 5, 08-30-02)
A1-1923.15, A1-1943.15, B1-4923.15, B1-4943.15
This line shall be used only be used in the instances where CO receives collection from
cross servicing/TOP for DCIA debt.
The Medicare contractor who reports the receivable on Form CMS-751A/B will reduce
the outstanding balance of the receivable for the amount deposited by CO by recording
the amount of the collection in Line 4c, Collection Deposited at Another Location. (See
Exhibit 18, Collection Reconciliation/Acknowledgement Form).
Section B - Delinquent Receivables
270.16 - Line 1, Total Not Delinquent (Principal & Interest) –
(Rev. 5, 08-30-02)
A1-1923.16, A1-1943.16, B1-4923.16, B1-4943.16
The contractor enters the total number and amount of accounts receivable that are not
delinquent.
270.17 - Line 2, Total Delinquencies (Principal & Interest) - (Rev. 5, 08-
30-02)
A1-1923.17, A1-1943.17, B1-4923.17, B1-4943.17
The contractor enters the total number and amount of delinquent receivables. It enters the
amount of the past due payment unless the full amount is normally due and declared
payable. The debt becomes delinquent the day following the date that the debt is due with
all extensions recognized. Thus, for non-MSP if the debt is due 30 days after demand, the
first day of delinquency starts on day 31. For MSP, if the debt is due 60 days after
demand, the first day of delinquency starts on day 61. If any portion of a debt has been
delinquent more than 180 days, the entire amount is reported as delinquent. The
contractor enters the amount of receivables that are delinquent for the respective periods
(a through i) indicated.
270.18 - Line 3, Status of Delinquent Receivables, less than or equal to
180 Days (Principal & Interest) - (Rev. 5, 08-30-02)
A1-1923.18, A1-1943.18, B1-4923.18, B1-4943.18
The contractor enters the total number and amount of delinquent receivables 180 days
delinquent and less, which are in (a) Bankruptcy, (b) Appeal, (c) Department of Justice,
(d) Referred for Cross Servicing and/or (e) Other Status.
270.19 - Line 4, Status of Delinquent Receivables, greater than 180 Days
(Principal & Interest)
(Rev. 111; Issued: 10-27-06; Effective: 04-01-07; Implementation: 04-02-07)
The contractor enters the total number and amount of delinquent receivables 181 days
delinquent and greater, which are in one of the following categories:
(a) Referred to the Department of the Treasury for Cross Servicing. For MSP,
this means debts entered into the DCS. For Non-MSP, this means debts that have
been transmitted to DCC by CMS Central Office and the Medicare contractor has
acknowledged and verified the validity and accuracy of the debts transmitted.
(b) Not Eligible for Referral, the number and dollar amount is equal to the sum of
lines (1) through (12) of this section.
1) Bankruptcy;
2) Appeal;
3) Department of Justice/Litigation;
4) Fraud and Abuse Investigation, if the contractor has received specific
instructions from the investigating unit (i.e., Office of Inspector General or
Office of General Counsel, etc.) not to attempt collection;
5) Deceased Debtor, debts where the debtor is deceased and the estate is
closed;
6) Debts less than $25;
7) Federal Entity Debts, MSP only, where the only entity which received
the last demand letter is the employer and the employer is a Federal
agency;
8) Beneficiary Debts, Non-MSP only;
9) Pending Request for Waiver or Compromise;
10) CMS Identified Exclusions, MSP only, debts where CMS has
identified a specific debt or group of debtors as excluded from DCIA
referral.
11) Other Exclusions, must footnote.
12) In the Process of Internal Offset (Previously Under Medicare
Modernization Act, Section 935 Appeal).
(c) Eligible for Referral, debts that are eligible for referral to the Department of the
Treasury for cross servicing but not yet referred.
270.20 - Line 4c, Collections Deposited at Another Location (Principal
& Interest) - (Rev. 5, 08-30-02)
A1-1923.20, A1-1943.20, B1-4923.20, B1-4943.20
The contractor enters the distribution of collections on receivables, by location, for
amounts offset or received and deposited at another location. The total amounts listed in
this section must equal the amount reflected in Section A, Line 4c of this report.
270.21 - Line 10, Cash/Offsets Received for Receivables at Another
Location (Principal & Interest) - (Rev. 5, 08-30-02)
A1-1923.21, A1-1943.21, B1-4923.21, B1-4943.21
This will not apply to Medicare contractors.
270.22 - Collections on Delinquent Debt (Principal & Interest) –
(Rev. 5, 08-30-02)
A1-1923.22, A1-1943.22, B1-4923.22, B1-4943.22
The contractor enters the number and amount of collections on receivables that were
delinquent upon collection. The total amount should be less than total collections for the
FY.
Section D - Transferred Receivables
The contractor enters the distribution of debts transferred to Medicare contractors or other
CMS locations.
For Form CMS-H751A/B, the data in this section is also reported in Section A, Status of
Accounts Receivable Transfers Out to other Medicare contractors or other CMS
locations, and will be used by the contractor and other CMS locations to reconcile its
books and records.
For Form CMS-M751A/B, the data in this section is also reported in Section A
Outstanding Receivables, Line 5c, Transfers Out to other Medicare Contractors; Line 5e,
Transfers Out to other CMS locations on the POR/PSOR; and Line 5g, Transfers Out to
other CMS Locations, Not POR/PSOR.
270.23 - Line 5c, Transfers Out to other Medicare Contractors
(Principal & Interest) - (Rev. 5, 08-30-02)
A1-1923.23, A1-1943.23, B1-4923.23, B1-4943.23
The contractor enters the distribution to Medicare contractor locations of the debts,
entered in Line 5c, Transfers Out to other Medicare Contractors, reflected in Section A of
this report.
270.24 - Line 5e, Transfers Out to other CMS Locations, POR/PSOR
(Principal & Interest) - (Rev. 5, 08-30-02)
A1-1923.24, A1-1943.24, B1-4923.24, B1-4943.24
The contractor enters the distribution to the various regional offices (ROs) or CO of the
debts on the POR, entered in Line 5e, Transfers Out to other CMS Locations,
POR/PSOR, reflected in Section A of this report.
270.25 - Line 5g, Transfers Out to other CMS Locations, Not POR
(Principal & Interest) - (Rev. 5, 08-30-02)
A1-1923.25, A1-1943.25, B1-4923.25, B1-4943.25
The contractor enters the distribution to the various ROs or CO of the debts not reported
on the POR/PSOR, entered in Line 5g,Transfers Out to other CMS Locations, Not
POR/PSOR, reflected in Section A of this report. POR is applicable to FIs. PSOR is
applicable to carriers.
280 - Instructions for Completing the Form CMS-C751A/B, Status of
Debt - Currently Not Collectible (CNC), and Form CMS-MC751A/B,
Status of MSP Debt - Currently Not Collectible (CNC) - (Rev. 5, 08-30-
02)
A1-1930, A1-1950, B1-4930, B1-4950
Form CMS-C751A/B and Form CMS-M751A/B are similar data entry screens used to
report the following.
• Form CMS-C751A to report non-MSP debt under Part A (HI) by intermediaries;
• Form CMS-C751B to report non-MSP debt under Part B (SMI) by intermediaries
and carriers;
• Form CMS-MC751A to report MSP debt under HI by intermediaries; and
• Form CMS-MC751B to report MSP debt under SMI by intermediaries and
carriers;
Note that currently not-collectible debt reported by Forms CMS-C751 and CMS-MC751
is reported separately for non-MSP and MSP accounts receivables.
The screen heading indicates whether the CNC report is for the non-MSP or MSP subset.
Samples of the screens are shown in Exhibits 5 and 6. Note that intermediaries must
prepare separate reports for each category by trust find.
There are separate reports and data screens for Part A, HI, and for Part B, SMI in the
CAFM system. The intermediary enters data in both HI and SMI data screens (Exhibits 5
and 6). The carrier enters data in only the SMI data screens (Exhibit 6).
The data for each of these reports are essentially the same.
The contractor reports the CNC accounts receivable activity for FYTD for the period of
the report. In order to facilitate reconciliation, balancing and error resolution, it reports
the CNC accounts receivable in dollars and cents.
The reports require information both for the amount and the number of accounts
receivable. To provide standardization, CMS suggests the contractor use its collection
process as a guide when reporting the number of accounts receivable. For example, a
separate, stand alone accounts receivable collected would be reported as a quantity in the
number column.
Once the principal number is established, the contractor reports the interest associated
with the principal amount in the same manner. There can be a difference between the
principal number and the interest number because some receivables are not subject to
interest.
290 - Due Date - (Rev. 5, 08-30-02)
A1-1931, A1-1951, B1-4931, B1-4951
This report is due on January 21, April 21, July 21, October 21 (21 days after the end of
each quarter) via the CAFM system. If that date occurs on a holiday or a weekend, the
report is due the following Federal workday.
300 - Certification - (Rev. 5, 08-30-02)
A1-1932, A1-1952, B1-4932, B1-4952
Medicare contractor certification by the CFO is required. The CFO must input their
password on the CAFM system (see Exhibit 16). Failure to record the official's password
is a serious error that will prevent acceptance of the report by the CAFM system. The
following statement appears at the end of the Form CMS-C751A/B (as well as the Form
CMS-MC751A/B):
I hereby CERTIFY that I have examined the Status of Non-MSP Debt - CNC prepared by
name of contractor for the period beginning (first day of FY) and ending (last day of
quarter), and that to the best of my knowledge and belief, it is a true, correct and
complete statement prepared from the books and records of the contractor in accordance
with applicable instructions.
NAME _____________________ DATE _______ TITLE _________
NOTE: In the above statement, "MSP" replaces "Non-MSP" for the MSP report.
310 - Line Item Instructions Form CMS-C751A/B - Non-MSP and Form
CMS-MC751A/B - MSP - (Rev. 5, 08-30-02)
A1-1933, A1-1953, B1-4933, B1-4953
The following instructions are to be used by Medicare contractors to report the status of
Non-MSP or MSP, as applicable, CNC debt. Medicare contractors must develop and
maintain transaction level detail (at a minimum, this would include the provider name,
provider number, date of determination, outstanding balance, and any adjustments or
recoupments) by debt to support the amounts reported for each line outlined below (see
Exhibits 5 and 6). Medicare contractors must reclassify MSP or Non-MSP debt as CNC
in accordance with CMS policy (see Exhibit 19 and Exhibit 20).
Within this subset of instructions, the designation "MSP" or "Non-MSP" is implied,
depending on which report is being submitted, MSP or Non-MSP.
Section A - CNC Debt
310.1 - Line 1, Beginning FY Balance (Principal & Interest) –
(Rev. 5, 08-30-02)
A1-1933.1, A1-1953.1, B1-4933.1, B1-4953.1
The contractor shall report the number and amount for all CNC debts outstanding as of
the beginning of the FY. These amounts will be pre-filled with the ending balances from
the prior FY on Form CMS-C751A/B, Status of Non-MSP Debt-CNC Financial Report
or Form CMS-MC751A/B, Status of MSP Debt-CNC Financial Report. It shall make any
corrections to the beginning principal and interest FY balance only on Line 4e,
Reclassified CNC Debt - Other.
310.2 - Line 2, New CNC Debt (Principal & Interest) - (Rev. 5, 08-30-02)
A1-1933.2, A1-1953.2, B1-4933.2, B1-4953.2
The contractor enters the number and amount of all debt approved by CMS RO and CO
for CNC during the FY. This line should include the outstanding principal balance and all
outstanding interest associated with the debt that was earned up to the date the debt was
removed from Form CMS-751A/B or Form CMS-M751A/B reports, as appropriate, and
included on the current Form CMS-C751A/B report or Form CMS-MC751A/B. This
amount must equal the principal and interest amounts reported on Line 6c, Transfers Out
to CNC.
310.3 - Line 3, Interest Earned Since CNC Approval (Interest) –
(Rev. 5, 08-30-02)
A1-1933.3, A1-1953.3, B1-4933.3, B1-4953.3
The contractor enters the amount of interest earned in this fiscal year on CNC debt since
the date the debt was reclassified and included in Line 1, Beginning FY Balance and
interest earned on debts reclassified to CNC during the FY included in Line 2, New CNC
Debt on the current report.
310.4 - Line 4(a) through (e), Reclassified CNC Debt (Principal &
Interest)
(Rev. 91, Issued: 02-17-06, Effective: 03-17-06, Implementation: 03-17-06)
Reclassified CNC debt reported on Line 4a, Re-established as Active Accounts
Receivable (A/R) Due to Collection of Cash; Line 4b, Re-established as Active A/R Due
to Collection by Offset; and Line 4c, Re-established as Active A/R Due to Misstatement
or Misclassification must agree with the total amount reported on Line 6b, Transfers In
from CNC on Form CMS-H/M 751A/B. Medicare contractors must retain all
documentation supporting any reclassified amounts.
4. The contractor reports in Lines:
a. Re-established as Active Accounts Receivable (A/R) Due to Collection of
Cash (Principal & Interest). The contractor enters the amount of CNC debt
that is re-established as active debt because cash/checks have been
collected on CNC debts during the FY. Simultaneously, the amount of the
collection shall be reported on Line 6b, Transfers In from CNC and Line
4a, Cash/Check Collections on Form CMS-H/M751A/B. The effect of this
transaction will reclassify the debt from an inactive memorandum entry to
an active receivable that will be reported for financial statement purposes.
Additionally, if the outstanding balance of the CNC debt was greater than
the amount collected, the remaining balance of the debt shall remain in
CNC. Medicare contractors shall continue to accrue interest for debt that
has been reclassified as CNC.
b. Re-established as Active A/R Due to Collection by Offset (Principal and
Interest.) The contractor enters the amount of CNC debt that is re-
established as active debt because offsets have been made on CNC debt
during the FY. Simultaneously, the amount of the offset collection shall be
reported on Line 6b, Transfers In from CNC and Line 4b, Offset
Collections on Form CMS-H/M751A/B. The effect of this transaction will
reclassify the debt from an inactive memorandum entry to an active
receivable that will be reported for financial statement purposes.
Additionally, if the outstanding balance of the CNC debt was greater than
the amount collected, the remaining balance of the debt shall remain in
CNC. Medicare contractors shall continue to accrue interest for debt that
has been reclassified as CNC.
c. Re-established as Active A/R Due to Misstatement or Misclassification
(Principal & Interest). The contractor enters the amount of the CNC debt
that has been re-established to be active debt because the CNC debt is now
determined to be a misstatement or misclassification. Simultaneously, the
amount of the misstatement or misclassification shall be reported on Line
6b, Transfers In from CNC on Form CMS-H/M751A/B. The effect of this
transaction will reclassify CNC the debt from an inactive memorandum
entry to an active receivable that will be reported for financial statement
purposes.
d. Written-off Closed (Principal & Interest). The contractor enters the
number and amount of CNC debt that has been approved for written-off
closed during the FY. The receivables will be "closed" in its internal
systems. No further action will be taken on these debts. CNC debts that
are written-off as closed will not be reported on the financial statements,
and all collection activity (i.e., future offsets or interest accruals) and
servicing of the debt will be terminated. The debts will be closed within
the contractor's records, reports, and accounts receivable systems. These
debts will be written-off and closed through Form CMS-C/MC751A/B, on
line 4d. These debts shall not be reactivated on Form CMS-H/M751A/B.
e. NOTE: Medicare contractors cannot write-off debt until formal approval
has been received from the appropriate authorized official in accordance
with the existing CMS delegations of authority.
Other (Principal & Interest). The contractor shall use line 4e only to make
corrections to Form CMS-C/MC751A/B beginning principal and interest FY
balance. Medicare contractors must retain all documentation justifying any
adjustments made to the beginning balance.
310.5 - Lines 5(a) through (f), Amounts Transferred (Principal &
Interest - (Rev. 5, 08-30-02)
A1-1933.5, A1-1953.5, B1-4933.5, B1-4953.5
The contractor enters the amount of CNC debts that have been transferred in from or out
to Medicare contractors or CMS RO or CO during the FY. It shall not enter an amount on
these lines until it has received confirmation that the Medicare contractor, CMS RO or

CO, has accepted the debt. (See Exhibit 17, Transfer of Debt Between Reporting
Entities).
5. The contractor shall report in lines:
a. Transfers In from other Medicare Contractors (Principal & Interest). The
amount of CNC debt transferred in from other Medicare contractors
during the fiscal period.
b. Transfers Out to other Medicare Contractors (Principal & Interest). The
amount of CNC debt transferred out to other Medicare contractors during
the fiscal period.
c. Transfers In from CMS RO (Principal & Interest). The amount of CNC
debt transferred in from RO during the fiscal period.
d. Transfers Out to CMS RO (Principal & Interest). The amount of CNC
debt transferred out to RO during the fiscal period.
e. Transfers In from CMS CO (Principal & Interest). The amount of CNC
transferred in from CO during the fiscal period.
Transfers Out to CMS CO (Principal & Interest). The amount of CNC transferred out to
CO during the fiscal period.
Collection efforts do not cease when debt is reclassified to CNC. Medicare contractors
must recognize that all debts including CNC debt will continue to be referred (if eligible)
to the Program Support Center (PSC), Department of Health and Human Services
(DHHS) or the Treasury Offset Program (TOP).
Medicare contractors are expected to follow existing procedures for the routine referral of
delinquent debt to the Debt Collection Center (DCC) in accordance with the Debt
Collection Improvement Act (DCIA) of 1996.
Amounts transferred in from or out to other CMS locations or Medicare contractors for
the reporting period must be reconciled to the other entity's records for the same reporting
period prior to submission of the quarterly Forms CMS-750/751A/B. Medicare
contractors and other CMS locations must reconcile the transfers out lines to ensure that
only approved transfers are being reported. Documentation of the reconciliation must be
maintained and must indicate that a supervisory review of the reconciliation was
performed. See Exhibit 17 for instructions for the transfer of debt between other reporting
entities.
310.6 - Line 6, Ending Balance (Principal & Interest) - (Rev. 5, 08-30-
02)
A1-1933.6, A1-1953.6, B1-4933.6, B1-4953.6
The ending balance is a computed field, reporting the number (manual entry) and amount
of CNC debt outstanding as of the end of the reporting period. It equals:
Principal
Interest
+
Beginning FY balance (Line 1)
+
Beginning FY balance (Line 1)
+
New CNC Debt (Line 2)
+
New CNC Debt (Line 2)
+
Interest Earned (Line 3)
-
Re-established as Active A/R Due to
Collection of Cash (Line 4a)
-
Re-established as Active A/R Due to
Collection of Cash (Line 4a)
-
Re-established as Active A/R Due to
Collection by Offset (Line 4b)
-
Re-established as Active A/R Due to
Collection by Offset (Line 4b)
-
Re-established as Active A/R Due to
Bankruptcy, Fraud & Abuse Litigation
or Appeal (Line 4c)
-
Re-established as Active A/R Due to
Bankruptcy, Fraud & Abuse Litigation
or Appeal (Line 4c)
-
Written-off Closed (Line 4d)
-
Written-off Closed (Line 4d)
+/-
Other (Line 4e)
+/-
Other (Line 4e)
+
Transfers In From Medicare
Contractors/ RO/CO (Lines 5a, 5c, 5e)
+
Transfers In From Medicare
Contractors/ RO/CO (Lines 5a, 5c, 5e)
-
Transfers Out to Medicare
Contractors/ RO/CO (Lines 5b, 5d, 5f)
-
Transfers Out to Medicare
Contractors/ RO/CO (Lines 5b, 5d, 5f)
=
Ending Balance (Line 6)
=
Ending Balance (Line 6)
NOTE: Although Line 6 is a calculated amount, the contractor must be able to provide a
detailed listing of all Non-MSP (or MSP, as applicable) CNC receivable balances that
support this line at any given period of time.
Section B - Aging of MSP or Non-MSP CNC Debt
310.7 - Line 1, Total Aged CNC Debt (Principal & Interest) –
(Rev. 5, 08-30-02)
A1-1933.7, A1-1953.7, B1-4933.7, B1-4953.7
The contractor enters the number and amount of MSP or Non-MSP CNC debt, as
applicable. The total dollar amount equals the sum of lines (a) through (e), and should
also equal Line 6, Ending Balance on Form CMS-C751A/B or Form CMS-MC751AB, as
applicable.
The contractor reports on lines (a) through (e) the dollar amounts of receivables aged
from the date of determination of the debt for the respective time periods listed. For Non-
MSP, it provides an explanation in the remarks section regarding why debts in category
(d) and (e) were not recommended for written-off closed.
Section C - Collection Information
310.8 - Collections on CNC Debt (Principal & Interest) - (Rev. 5, 08-30-
02)
A1-1933.8, A1-1953.8, B1-4933.8, B1-4953.8
The contractor enters the number and amounts of cash/checks/offsets actually collected
on Non-MSP or MSP CNC debt, as applicable that is reported on Line 4a, Re-established
as Active A/R Due to Collection of Cash, and Line 4b, Re-established as Active A/R Due
to Collection by Offset.
Section D - Status CNC Debt over 181 Days
310.9 - Status of CNC Debt over 181 Days (Principal & Interest) - (Rev.
17, 05-02-03)
The contractor enters the total number and amount of delinquent receivables 181 days
delinquent and greater, which are in one of the following categories:
(a) Referred to the Department of the Treasury for Cross Servicing. For MSP,
this means debts entered into the DCS. For Non-MSP, this means debts that have
been transmitted to DCC by CMS Central Office and the Medicare contractor has
acknowledged and verified the validity and accuracy of the debts transmitted.
(b) Not Eligible for Referral, the number and dollar amount is equal to the sum of
lines (1) through (11) of this section.
1) Bankruptcy;
2) Appeal;
3) Department of Justice/Litigation;
4) Fraud and Abuse Investigation, if the contractor has received specific
instructions from the investigating unit (i.e., Office of Inspector General or
Office of General Counsel, etc.) not to attempt collection;
5) Deceased Debtor, debts where the debtor is deceased and the estate is
closed.
6) Debts less than $25;
7) Federal Entity Debts, MSP only, where the only entity which received
the last demand letter is the employer and the employer is a Federal
agency;
8) Beneficiary Debts, Non-MSP only;
9) Pending Request for Waiver or Compromise;
10) CMS Identified Exclusions, MSP only, debts where CMS has
identified a specific debt or group of debtors as excluded from DCIA
referral.
11) Other Exclusions, must footnote.
(c) Eligible for Referral, debts that are eligible for referral to the Department of
the Treasury for cross servicing but not yet referred.
400 - Exhibits - (Rev. 5, 08-30-02)
A1-1960, B1-4960
Exhibit 1
CMS-750A Contractor Financial Reports, Hospital Insurance (HI) Statement of
Financial Position/Statement of Operations
Exhibit 2
CMS-750B Contractor Financial Reports, Supplementary Medical Insurance
(SMI) Statement of Financial Position/Statement of Operations
Exhibit 3
CMS-751A Status of Accounts Receivable, Hospital Insurance (HI)
Exhibit 4
CMS-751B Status of Accounts Receivable, Supplementary Medical Insurance
(SMI)
Exhibit 5
Form CMS-C751A Status of Non-MSP Currently Not Collectible (CNC)
Accounts Receivable, Hospital Insurance (HI)
Exhibit 6
Form CMS-C751B Status of Non-MSP Currently Not Collectible (CNC)
Accounts Receivable, Supplementary Medical Insurance (SMI)
Exhibit 7
Form CMS-M751A Status of Medicare Secondary Payer (MSP) Accounts
Receivable, Hospital Insurance (HI)
Exhibit 8
Form CMS-M751B Status of Medicare Secondary Payer (MSP) Accounts
Receivable, Supplementary Medical Insurance (SMI)
Exhibit 9
Form CMS-MC751A Status of MSP Currently Not Collectible (CNC) Accounts
Receivable, Hospital Insurance (HI)
Exhibit 10
Form CMS-MC751B Status of MSP Currently Not Collectible (CNC) Accounts
Receivable, Supplementary Medical Insurance (SMI)
Exhibit 11
Medicare Contractor Account Definitions, Data Element Definitions
Exhibit 12
Accounts Payable, Protocol for Estimating Claims
Exhibit 13
Periodic Interim (PIP) Payments Protocol for Estimating Payables/Receivables on
the CMS-750A/B, Statement of Financial Position
Exhibit 14
Protocol for Estimating Allowance for Uncollectible Accounts
Exhibit 15
Protocol for Prorating Intermediary Time Account Balances Between the CMS
750A (HI) and the CMS 750B (SMI)
Exhibit 16
Electronic Certification
Exhibit 17
Transfer of Debt Between Reporting Entities
Exhibit 18
Collection Reconciliation/Acknowledgement Form
Exhibit 19
Procedures for Non-MSP Reclassification as Currently Not Collectible (CNC)
Exhibit 20
Procedures for MSP Reclassification as Currently Not Collectible (CNC)
Exhibit 21
CMS Policy for Recognizing Accounts Receivable
400.1 - Exhibit 1 - Statement of Financial Position and Statement of
Operations - HI/SMI - (Rev. 5, 08-30-02)
A1-1960 Exhibit 1, B1-4960.1
The FI submits the HI report (Form CMS-H750A). Both FI and carrier submit the SMI
report (Form CMS-H750B).
• The HI report, in applicable line item descriptions, refers to "provider" and the
SMI report refers to "physicians, provider or supplier".
• For the SMI report (Form CMS-H750B), the FI completes the items dealing with
cost reports, PIP, and credit balances; but the carrier omits them. Also, the
intermediary inserts data relating to the Provider Overpayment Report (POR),
while the carrier inserts data relating to the Physician Supplier Overpayment
Report (PSOR).
Exhibit 1 (Cont.)
Contractor Financial Reports
Statement of Financial Position
Hospital Insurance (HI)
As of __________________
Contractor Name
ID Number
_______________________
__________
Assets
Balance
Cash
Benefits Account
_______________
Time Account
_______________
Undeposited Collections
_______________
Total Cash
_______________
Accounts Receivable
Non-Medicare Secondary Payments (Non-MSP) Overpayments
Provider (Carriers Omit)
_______________
Cost Report Settlements (Carriers Omit)
_______________
Claims Accounts Receivable (Carriers Omit)
_______________
PIP Accrual (Carriers Omit)
_______________
Credit Balances (Carriers Omit)
_______________
Other (Carriers Omit)
_______________
Physician/Supplier Overpayments (Intermediaries
Omit)
_______________
Beneficiaries
_______________
Total Non-MSP
_______________
Medicare Secondary Payer (MSP)
Group Health Plan
Data Match
_______________
Non-Data Match
_______________
MSP Provider/Physician/Supplier/Beneficiary
Liability (including WC, Auto, No Fault, MSP
beneficiary and other MSP)
MSP Beneficiary
_______________
_______________
Other MSP
_______________
Total MSP
_______________
CMS-H750A/B
Exhibit 1 (Cont.)
Contractor Financial Reports
Statement of Operations
Hospital Insurance (HI)
As of _______________
Contractor Name
ID Number
_______________________
__________
Other (footnote)
_______________
Total Accounts Receivable
_______________
Advances to Others
Advance Payments
_______________
Accelerated Payments (Not applicable to carriers)
_______________
Total Advances
_______________
Interest Receivable
_______________
Other Assets (footnote)
_______________
Liabilities
Balance
Accounts Payable
Unprocessed Claims
Benefits Payable
_________________
Provider
PIP Providers A Cost Report Settlements (Carriers
Omit)
_________________
PIP Providers A Estimated Payable Accrual (Carriers
Omit)
_________________
Non-PIP Providers A Underpayments (Interim
Reviews) (Carriers Omit)
_________________
Non-PIP Providers A Underpayments (Cost
Settlements) (Carriers Omit)
_________________
Claims Withheld for Non-receipt of Cost Reports
(Carriers Omit)
_________________
Physicians/Suppliers (Intermediaries Omit)
_________________
Beneficiaries
_________________
Claims on the Payment Floor
_________________
CMS-H750A/B
Exhibit 1 (Cont.)
Contractor Financial Reports
Statement of Operations
Hospital Insurance (HI)
As of _______________
Contractor Name
ID Number
_______________________
__________
Suspended Payments
Claims
________________
Common Working File (CWF)
_________________
MR/UR Prepayment Review
_________________
Medicare Secondary Payer (MSP)
_________________
Total Accounts Payable
_______________
Accrued Interest Payable
_______________
Other Liabilities
Unapplied Receipts
_______________
Excess Recoupments
_______________
Due Medicaid
_______________
Other (footnote)
_______________
Total Other Liabilities
_______________
TOTAL LIABILITIES
_______________
Fund Account Balance
Cumulative Results of Operations
_______________
TOTAL LIABILITIES AND FUND ACCOUNT BALANCE
_______________
Revenue
Amount
Interest Revenue
Line 3
Adjustments (Interest)
Line 5a
Waivers (Interest)
Line 5h
Write-offs (Bad Debts)(Interest)
Line 6a
Transfers in from other Medicare Contractors
Line 5b
Transfers out to other Medicare Contractors
Line 5c
Transfers in from CNC (Interest)
Line 6b
Transfers out to CNC (Interest)
Line 6c
Transfers in from other CMS Locations (POR/PSOR (as
applicable)) (Interest)
Line 5d
CMS-H750A/B
Exhibit 1 (Cont.)
Contractor Financial Reports
Statement of Operations
Hospital Insurance (HI)
As of _______________
Contractor Name
ID Number
_______________________
__________
Transfers out to other CMS Locations (POR/PSOR (as
applicable)) (Interest)
Line 5e
Transfers in from other CMS Locations (Not POR/PSOR (as
applicable)) (Interest)
Line 5f
Transfers out to other CMS Locations (Not POR/PSOR (as
applicable)) (Interest)
Line 5g
Draws on Letter of Credit
________________
Other Revenue (footnote)
________________
TOTAL REVENUE
________________
Expense
Operating/Program Expense
Line 2 + Benefit Expense
Adjustments (Principal)
Line 5a (CR or DR)
Transfers In from other Medicare Contractors (Contra
Account)
Line 5b
Transfers Out to other Medicare Contractors (Principal)
Line 5c
Transfers In from CNC (Contra Account)
Line 6b
Transfers Out to CNC (Principal)
Line 6c
Transfers In from other CMS Locations (POR and Not
POR) (Contra Account)
Line 5d&5f
Transfers Out to other CMS Locations (POR and Not
POR) (Principal)
Line 5e&5g
Less: Waivers (Principal)
Line 5h
Less: Write-offs (Bad debts) (Principal)
Line 6a
CMS-H750A/B
Exhibit 1 (Cont.)
Contractor Financial Reports
Statement of Operations
Hospital Insurance (HI)
As of _______________
Contractor Name
ID Number
_______________________
__________
Total Program Expense
________________
Interest Expense
CPT Interest
________________
Other Interest
________________
Other Expense (footnote)
________________
Prior Period Adjustments (footnote)
TOTAL EXPENSE
________________
NET RESULTS OF OPERATIONS
________________
OTHER DATA (Intermediaries)
Value of 1
st
PIP Payment Cycle in ensuing quarter
________________
CMS-H750A/B
400.2 - Exhibit 2 - Statement of Financial Position and Statement of
Operations - SMI - (Rev. 5, 08-30-02)
This report is a duplicate of the above Exhibit 1, Statement of Financial Position and
Statement of Operations - HI, except:
• The HI report, in the applicable line item descriptions, refers to "provider", and
the SMI report refers to "provider, physician, and supplier".
• For the SMI report (CMS-750B), the FI completes the items dealing with cost
reports, PIP, and credit balances; but the carrier omits them. Also, the
intermediary inserts data relating to the Provider Overpayment Report (POR),
while the carrier inserts data relating to the Physician Supplier Overpayment
Report (PSOR).
400.3 - Exhibit 3 - Status of Accounts Receivable - HI
(Rev. 111; Issued: 10-27-06; Effective: 04-01-07; Implementation: 04-02-07)
This exhibit is the same as Exhibit 4, Status of Accounts Receivable – SMI, with the
following exceptions:
Section B, items 5d through 5g and Section D, items 5d and 5e refer to the POR for the
HI report and refer to the POR/PSOR for the SMI report. Only intermediaries enter POR
data on both the HI report and the SMI report. Only carriers enter the PSOR data on the
SMI report.
CMS-751A is the CMS Form Number for the HI (Part A) report.
CMS-751B is the CMS Form Number for the SMI (Part B) report.
Exhibit 3 (Cont.)
Status of Accounts Receivable
Hospital Insurance (HI)
As of _________________
Contractor Name
ID Number
_______________________
__________
Section A: Outstanding Receivables
Principal
Principal
Interest
Interest
Number
Dollars
Dollars
Number
1.
Beginning FY Balance
_________
__________
_________
_______
2a.
New Receivables
_________
__________
2b.
Accrued Receivables
_________
__________
3.
Interest Earned
_________
_______
4a.
Cash/Check Collections
__________
_________
4b.
Offset Collections
__________
_________
4c.
Collections Deposited at Another Location
__________
_________
5a.
Adjusted Amounts
__________
Internal Adjustments
__________
_________
Auditor/Consultant Adjustments
__________
_________
5b.
Transfers In from other Medicare Contractors
__________
_________
5c.
Transfers Out to other Medicare Contractors
__________
_________
5d.
Transfers In from other CMS Locations, POR/PSOR
__________
_________
5e.
Transfers Out to other CMS Locations, POR/PSOR
__________
_________
5f.
Transfers In from other CMS Locations,
not POR/PSOR
__________
_________
5g.
Transfers Out to other CMS Locations,
not POR/PSOR
__________
_________
5h.
Waivers
__________
_________
6a.
Amounts Written-off (Bad Debts)
__________
__________
_________
6b.
Transfers In from CNC
__________
__________
_________
6c.
Transfers Out to CNC
__________
__________
_________
7.
Ending Balance
_________
__________
___________
_______
a.
Current
__________
___________
b.
Non-current
__________
8.
Allowance for Uncollectible Accounts
__________
9.
Total Receivables Net of Allowance
__________
___________
10.
Cash/Offsets received for Receivables at
Another Location
__________
___________
CMS-H751A
Exhibit 3 (Cont.)
Status of Accounts Receivable
Hospital Insurance (HI)
As of _________________
Contractor Name
ID Number
_______________________
__________
Section B: Delinquent Receivables
Principal
Principal
Interest
Interest
Number
Dollars
Dollars
Number
1.
Total Not Delinquent
_________
__________
___________
_______
2.
Total Delinquent
_________
__________
___________
_______
(a)
1 - 30 days
__________
___________
(b)
31 - 60 days
__________
___________
(c)
61 - 90 days
__________
___________
(d)
91 - 180 days
__________
___________
(e)
181 - 365 days
__________
___________
(f)
1 - 2 years
__________
___________
(g)
2 - 6 years
__________
___________
(h)
6 - 10 years
__________
___________
(i)
Over 10 years
__________
___________
3.
Total Delinquent 1 - 180 days
_________
__________
_________
_______
(a)
In Bankruptcy
__________
_________
(b)
In Appeal
__________
_________
(c)
At Department of Justice
__________
_________
(d)
Referred for Cross Servicing
__________
_________
(e)
Other Status
__________
_________
(f) In the Process of Internal Offset (Previously Under
MMA Section 935 Appeal)
4.
Total Delinquent 181 days & over
_____
__________
_________
_______
A)
Referred for Cross Servicing
__________
_________
B)
1)
Not Eligible for Referral
In Bankruptcy
__________
__________
2)
In Appeal
__________
__________
3)
At Department of Justice
__________
__________
4)
Fraud and Abuse Investigation
__________
__________
5)
Deceased Debtor and Estate Closed
__________
__________
6)
Debts Less than $25
__________
__________
7)
Federal Entity Debts, MSP only, where
the only entity which received the last
demand letter is the employer and the
employer is a Federal agency;
__________
__________
8)
Beneficiary Debts, Non-MSP only;
__________
__________
9)
Pending Request for Waiver or
Compromise
__________
__________
10)
CMS Identified Exclusions, MSP only,
debts where CMS has identified a
specific debt or group of debtors as
excluded from DCIA referral.
__________
__________
11)
Other Exclusions, must footnote.
__________
__________
12)
In the Process of Internal Offset.
(Previously Under Medicare
Modernization Act (MMA) Section 935
Appeal)
__________
__________
C)
Eligible for Referral; debts that are
eligible for referral to the Department of
the Treasury for cross-servicing but not
yet referred.
__________
__________
Exhibit 3 (Cont.)
Status of Accounts Receivable
Hospital Insurance (HI)
As of _________________
Contractor Name
ID Number
_______________________
__________
Section C: Other Collections
4c.
Collections Deposited at another Location
Principal
Dollars
Interest
Dollars
Contractor/Region
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
10.
Cash Offsets Received for Receivables at another Location
Principal
Dollars
Interest
Dollars
Contractor/Region
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
Collections on Delinquent Debt _________
__________
_________
________
Section D: Transferred Receivables
5c.
Transfers Out to other Medicare Contractors
Principal
Dollars
Interest
Dollars
Contractor Number
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
____________________
__________
_________
CMS-H751A
Exhibit 3 (Cont.)
Status of Accounts Receivable
Hospital Insurance (HI)
As of _________________
Contractor Name
ID Number
_______________________
__________
5d.
Transfers Out to other CMS Locations, POR
1. Boston
__________
_________
2. New York
__________
_________
3. Philadelphia
__________
_________
4. Atlanta
__________
_________
5. Chicago
__________
_________
6. Dallas
__________
_________
7. Kansas City
__________
_________
8. Denver
__________
_________
9. San Francisco
__________
_________
10. Seattle
__________
_________
11. Central Office
__________
_________
5e.
Transfers Out to other CMS Locations, Not on POR
1. Boston
__________
_________
2. New York
__________
_________
3. Philadelphia
__________
_________
4. Atlanta
__________
_________
5. Chicago
__________
_________
6. Dallas
__________
_________
7. Kansas City
__________
_________
8. Denver
__________
_________
9. San Francisco
__________
_________
10. Seattle
__________
_________
11. Central Office
__________
_________
CMS-H751A
400.4 - Exhibit 4 - Status of Accounts Receivable - SMI - (Rev. 5, 08-30-
02)
This exhibit is the same as Exhibit 3, with the following exceptions:
• Section B, items 5d through 5g and Section D, items 5d and 5e refer to the POR
for the HI report and refer to the POR/PSOR for the SMI report.
• Only intermediaries enter POR data on both the HI report and the SMI report.
• Only carriers enter the PSOR data on the SMI report.
• Form CMS-H751A is the CMS Form Number for the HI (Part A) report.
• Form CMS-H751B is the CMS Form Number for the SMI (Part B) report.
400.5 - Exhibit 5 - Status of Non-MSP Debt - CNC - HI
(Rev. 111; Issued: 10-27-06; Effective: 04-01-07; Implementation: 04-02-07)
The screen formats in exhibits 5 and 6 are identical except 5 is for HI non-MSP and 6 is
for SMI non-MSP.
MSP debt is reported in exhibits 9 and 10.
Exhibit 5 (Cont.)
One of: Status of Non-MSP Debt - CNC; or Status of MSP Debt - CNC will be shown.
One of: Hospital Insurance (HI); or Supplementary Medical Insurance (SMI) will be shown
As of ___________________
Contractor Name
ID Number
_______________________
__________
Section A: CNC Debt
Principal
Principal
Interest
Interest
Number
Dollars
Dollars
Number
1.
Beginning FY Balance
______
__________
___________
_______
2.
New CNC Debt
______
__________
___________
_______
3.
Interest Earned Since CNC Approval
___________
4.
Reclassified CNC Debt
a.
Re-established as Active A/R due to collection of cash
______
__________
___________
____
b.
Re-established as Active A/R due to collection by offset
______
__________
___________
____
c.
Re-established as Active A/R due to bankruptcy, fraud &
abuse, litigation and appeal
______
__________
___________
____
d.
Written-off Closed
______
__________
___________
____
e.
Other
______
__________
___________
____
5.
Amounts Transferred
a.
Transfers In from Medicare Contractors
______
__________
___________
____
b.
Transfers Out to Medicare Contractors
______
__________
___________
____
c.
Transfers In from CMS RO
______
__________
___________
____
d.
Transfers Out to CMS RO
______
__________
___________
____
e.
Transfers In from CMS CO
______
__________
___________
____
f.
Transfers Out to CMS CO
______
__________
___________
____
6.
Ending Balance
______
__________
___________
_______
CMS-C751A
Exhibit 5 (Cont.)
Status of Non-MSP Debt - CNC
Hospital Insurance (HI)
As of _________________
Contractor Name
ID Number
_______________________
__________
Section B: Aging of CNC Debt (from the determination date)
1.
Total CNC Debt
______
__________
___________
_______
(a)
181 - 1 year
__________
___________
(b)
1 - 2 years
__________
___________
(c)
2 - 6 years
__________
___________
(d)
6 - 10 years *
__________
___________
(e)
Over 10 years *
__________
___________
* Provide an explanation why debts in these categories were not recommended for write-off closed
Section C: Collection Information
Collections on CNC Debt
______
__________
___________
_______
Section D: Status CNC Debt over 181 Days
Total Delinquent
A)
Referred for Cross Servicing
__________
_________
B)
1)
Not Eligible for Referral
In Bankruptcy
__________
_________
2)
In Appeal
__________
_________
3)
At Department of Justice
__________
_________
4)
Fraud and Abuse Investigation
__________
_________
5)
Deceased Debtor and Estate Closed
__________
_________
6)
Debts Less than $25
__________
_________
7)
Federal Entity Debts, MSP only, where the only entity which
received the last demand letter is the employer and the
employer is a Federal agency;
__________
_________
8)
Beneficiary Debts, Non-MSP only;
__________
_________
9)
Pending Request for Waiver or Compromise
__________
_________
10)
CMS Identified Exclusions, MSP only, debts where CMS
has identified a specific debt or group of debtors as excluded
from DCIA referral.
__________
_________
11)
Other Exclusions, must footnote.
__________
_________
12)
In the Process of Internal Offset (Previously Under MMA,
Section 935 Appeal)
__________
_________
C)
Eligible for Referral; debts that are eligible for referral to the
Department of the Treasury for cross-servicing but not yet
referred.
__________
_________
CMS-C751A
400.6 - Exhibit 6 - Status of Non-MSP Debt - CNC - SMI - (Rev. 5, 08-
30-02)
See Section 400.5, Exhibit 5 – Status of Non-MSP Debt – CNC – HI
The formats in exhibits 5 and 6 are identical except 5 is for HI non-MSP and 6 is for
SMI. non-MSP.
MSP debt is reported in exhibits 9 and 10.
400.7 - Exhibit 7 - Status of MSP Accounts Receivable - HI – (Rev. 5, 08-
30-02)
This is an exact duplicate of Exhibit 3, except that the data is limited to data involving
Medicare as secondary payer.
This exhibit, and Exhibit 8, Status of MSP Accounts Receivable - SMI, are identical with
the following exceptions:
• Section B, items 5d through 5g and Section D, items 5d and 5e refer to the POR
for HI reports and refer to the POR/PSOR for the SMI report.
• Only carriers enter the PSOR data on the SMI report.
• The CMS Form Number for this report (HI) is CMS-M751A.
• The CMS Form Number for the SMI report is CMS-M751B.
400.8 - Exhibit 8 - Status of MSP Accounts Receivable - SMI –
(Rev. 5, 08-30-02)
See Exhibit 3, above.
400.9 - Exhibit 9 - Status of MSP Debt - CNC - HI - (Rev. 5, 08-30-02)
See Exhibit 5 – Status of Non-MSP Debt – CNC – HI.
400.10 - Exhibit 10 - Status of MSP Debt - CNC - SMI - (Rev. 5, 08-30-
02)
See Exhibit 5 – Status of Non MSP Debt – CNC –SMI.
400.11 - Exhibit 11 - Medicare Contractor Account Definitions - Data
Element Definitions - (Rev. 5, 08-30-02)
Medicare Contractor Account Definitions
Data Element Definitions
Account Number
Title
1000
Assets
1100
Cash
1100.01
Part A and Part B
1100.01.01
Benefit Account
1100.01.02
Time Account
1110
Undeposited Collections
1110.01
Part A and Part B
1110.01.01
Undeposited Collections
1310
Accounts Receivable
1310.01
Part A and Part B
1310.01.01
Non-MSP Overpayments
1310.01.01.01
Provider
1310.01.01.01.01
Cost Report Settlements (FI)
1310.01.01.01.02
Claims Accounts Receivable (FI)
1310.01.01.01.03
PIP Accrual (FI)
1310.01.01.01.04
Credit Balance (FI)
1310.01.01.01.05
Other (FI)
1310.01.01.02
Beneficiaries
1310.01.01.03
Physicians/Suppliers
1310.01.04
Medicare Secondary Payer (MSP)
1310.01.04.01
Group Health Plan
1310.01.04.01.01
Data Match
1310.01.04.01.02
Non-Data Match
1310.01.04.02
Liability MSP
1310.01.04.02.01
MSP Beneficiary
1310.01.04.02.02
MSP Provider/Physician Supplier
1310.01.04.03
Other MSP
1310.01.99
Other
1311
Advances to Others
1311.01
Part A and Part B
1311.01.01
Advance Payments
1311.01.02
Accelerated Payments
Medicare Contractor Account Definitions
Data Element Definitions
Account Number
Title
1330
Interest Receivable
1330.01
Part A and Part B
1990
Other Assets
1990.01
Part A and Part B
2000
Liabilities
2110
Accounts Payable
2110.01
Part A and Part B
2110.01.01
Unprocessed Claims
2110.01.02
Benefits Payable
2110.01.02.01
Provider
2110.01.02.01.01
-PIP Provider Cost Report Settlements
2110.01.02.01.02
-PIP Provider Estimated Payable Accrual
2110.01.02.01.03
-Non-PIP Provider Underpayments Interim Rate
2110.01.02.01.04
-Non-PIP Provider Underpayments (Cost Report Settlement)
2110.01.02.01.05
Claims Withheld for Non-receipt of Cost Reports
2110.01.02.02
Beneficiaries
2110.01.02.03
Physicians/Suppliers
2110.01.02.04
Claims on the Payment Floor
2110.01.03
Suspended Payments
2110.01.03.01
Claims
2110.01.03.02
Common Working File (CWF)
2110.01.03.03
MR/UR Prepayment Review
2110.01.03.0
Medicare Secondary Payer (MSP)
2140
Accrued Interest Payable
2140.01
Part A and Part B
2990
Other Liabilities
2990.01
Part A and Part B
2990.01.01
Unapplied Receipts
2990.01.02
Excess Recoupments
2990.01.03
Due Medicaid
2990.01.04
Other
3010
Fund Account Balance
Medicare Contractor Account Definitions
Data Element Definitions
Account Number
Title
3310
Cumulative Results of Operations
3310.01
Part A and Part B
5000
Revenue
5303
Interest Revenue
5303.01
Part A and Part B
5303.01.01
Adjustments/Waivers (Contra Account)
5303.01.02
Write-off Closed/Transfers
5303.01.02.01
Bad Debt (Contra Account)
5303.01.02.02
Transfers Out to Other CMS Locations (Contra Account)
5303.01.02.02.01
Transfers In from Other CMS Locations
5303.01.02.03
Transfers Out to CNC (Contra Account)
5303.01.02.03.01
Transfers In from CNC
5303.01.02.04
Transfers Out to Other Medicare Contractors (Contra Account)
5303.01.02.04.01
Transfers In from Other Medicare Contractors
5700
Appropriated Capital Used
5700.01
Part A and Part B, Draws on Letter of Credit
5900
Other Revenue
5900.01
Part A and Part B
5900.01.01
Other
6000
Expense
6100
Operating/Program Expense
6100.01
Part A and Part B
6101
Waivers
6101.01
Part A and Part B
6101.01.02
Transfers Out to Other CMS Locations (Contra Account)
6101.01.02.01
Transfers In from Other CMS Locations
6101.01.03
Transfers Out to CNC (Contra Account)
6101.01.03.01
Transfers In from CNC
6101.01.04
Transfers Out to Other Medicare Contractors (Contra Account)
Medicare Contractor Account Definitions
Data Element Definitions
Account Number
Title
6101.01.04.01
Transfers In from Other Medicare Contractors
6106
Write Offs/Transfers
6106.01
Part A and Part B
6106.01.01
Bad Debts
6330
Interest Expense
6330.01
Part A and Part B
6330.01.01
CPT Interest
6330.01.02
Other Interest
6909
Other Expense
6909.01
Part A and Part B
7400
Prior Period Adjustments
7400.01
Part A and Part B
Medicare Contractor Account Definitions
Data Element Definitions
The account numbers used in this chart are for reference purposes only. They are not
mandated for use by Medicare contractors.
Account Number
Title
1000
Assets
The contractor reports amounts of physical items or rights to
ownership
1100
Cash
The contractor reports monetary resources on hand or on deposit
with banks or other financial institutions. Balances are the end of
quarter amounts per the contractor's books.
1100.01
Part A and Part B
The contractor reports cash allocable for Hospital Insurance (HI)
and Supplementary Medical Insurance (SMI) activities. HI data
must reconcile to Column E, Line 1, on Form CMS-
1522, Monthly
Contractor Financial Report. SMI data must reconcile to Column
E, Line 2. Prorate the Time Account by the number of checks and
electronic funds transfers (EFTs) issued for HI or SMI services.
Account Number
Title
(See Exhibit 15 Protocol for Prorating Intermediary Time Account
Balances between HI and SMI.)
1100.01.01
Benefits Account
The contractor reports the Federal Health Insurance Benefits
Account by HI and SMI
1100.01.02
Time Account
The contractor reports the balance as of the end of the quarter in
the Federal Health Insurance Time Account by HI and SMI.
1110
Undeposited Collections
1110.01
Part A and Part B
The contractor reports undeposited collections for HI and SMI
activities
1110.01.03
Undeposited Collections
The contractor reports collections on hand not deposited within the
accounting period. Undeposited collections include those items
received by the last day of the quarter that will be deposited during
the subsequent quarter. The contractor prorates undeposited
collections on the basis of Column D, Funds Expended, on Form
CMS-1522, Monthly Contractor Financial Report for Part A (HI)
and Part B (SMI). Report deposits in transit as part of the book
balance for either 1100.01.01, Benefits Account, or 1100.01.02,
Time Account. It reports amounts due from others. A receivable is
the identification of an overpayment for services rendered. CMS
will only recognize receivables related to Fraud and Abuse once
they are litigated by the Department of Justice (DOJ)
1310.01.01
Overpayments
The contractor accounts receivable for overpayments. It includes
amounts that exceed adjudicated claims processed, cost reports
settled, or other authorized payments. This includes, but is not
limited to, overpayments resulting from adjustment bills. It
reclassifies any overpayment when Medicare is deemed as
secondary payer to 1310.01.04, MSP
1310.01.01.01
Provider
The intermediary reports overpayments for institutional providers.
This includes, but is not limited to, those items listed on the
Provider Overpayment Report (POR) and the Credit Balance
Summary Report. Include periodic interim payments (PIP) in
Account Number
Title
excess of PIP bills. Include overpayments resulting from the
receipt of cost reports, tentative settlements or cost settlements
when the Notices of Provider Reimbursement (NPR) are prepared.
It includes overpayments from PRRB settlements when the Notices
of Correction (NOC) are prepared. This is not a carrier function.
1310.01.01.01.01
Cost Report Settlements
The intermediary reports the accounts receivable as a result of cost
report settlements, interim rate reviews and overpayments as a
result of accelerated payments
1310.01.01.01.02
Claims Accounts Receivable
The intermediary reports the accounts receivable as a result of
claims accounts receivable. This is not a carrier function.
1310.01.01.01.03
PIP Accrual
The intermediary reports the amount accrued for the (estimated)
accounts receivable PIP. (See Exhibit 13 Protocol for Estimating
Payables and Receivables for PIP). This is not a carrier function.
1310.01.01.01.04
Credit Balances
The intermediary reports the accounts receivable as a result of
credit balance reports This is not a carrier function.
1310.01.01.02
Beneficiaries
The contractor reports overpayments for beneficiaries. This
includes, but is not limited to, those items listed on the CMS-2174,
Carrier Beneficiary Overpayment Activity Report.
1310.01.01.03
Physicians/Suppliers
The carrier reports overpayments for physicians and suppliers. This
includes, but is not limited to, those items listed on the
Physician/Supplier Overpayment Report (PSOR) This is not an
intermediary function.
1310.01.04
Medicare Secondary Payer
The contractor reports accounts receivable for amounts due as a
result of MSP activity, and based on documented debts due
Medicare for all debtors. Debtors are employers, insurers,
providers, beneficiaries or other persons to whom a demand letter
has been issued
1310.01.04.01
Group Health Plan (GHP)
Account Number
Title
1310.01.04.01.01
Data Match (FI)
The contractor includes the amounts identified (CMS supplied
receivables via tapes with an identified report ID on MPaRTS) as a
result of MSP activity for which a demand letter has been issued
for IRS/SSA Data Match cases. Outstanding receivables are the
amount of debt that has been demanded and payment has not yet
been received
1310.01.04.01.02
Non-Data Match (FI)
The contractor includes the amounts identified (debt specific to
GHP debt, working aged, disability, End-Stage Renal Disease
(ESRD) as a result of MSP activity for which a demand letter has
been issued. Outstanding receivables are the amount of debt that
has been demanded and payment has not yet been received
1310.01.04.02
Liability MSP
The contractor includes the amounts (inclusive of all workman's
compensation, automobile/no fault and liability debt, this includes
CMS identified cases) due to MSP activity for which a settlement
has been reached related to liability cases. Outstanding receivables
are the amount of debts that have been demanded, subsequent to
settlement and/or other action, and payment has not yet been
received.
1310.01.04.02.01
MSP Beneficiaries
1310.01.04.02.02
MSP Providers/Physicians/Suppliers Outstanding receivables are
the amount of MSP initiated debts that have been demanded and
payment has not yet been received.
1310.01.04.03
Other MSP
The contractor includes the amounts due as a result of other MSP
activity for which a valid MSP debt has been recognized.
1310.01.99
Other
The contractor reports actual or estimated other accounts
receivable. It includes those receivables not otherwise classified in
the categories presented above. It provides an identifying footnote
on CAFM of the nature of this receivable
1311
Advances to Others
The contractor reports payments made to providers, physicians, or
suppliers in anticipation of claims being processed. Advances are
Account Number
Title
not to be considered as accounts receivable. It does not include
them on Form CMS-751A/B, Status of Account Receivable report
1311.01
Part A and Part B
The contractor reports advance payments and accelerated payments
attributable to HI and SMI activities
1311.01.01
Advance Payments
The contractor the outstanding balance for payments authorized by
CMS instructions for advanced payments based on actual provider
claims data. If not recovered according to CMS instructions, it
reclassifies and reports as overpayments
1311.01.02
Accelerated Payments (FI)
The intermediary reports the outstanding balance for payments
authorized by CMS instructions for accelerated payments based on
actual provider claims data. If not recovered according to CMS
instructions, it reclassifies and reports as overpayments This is not
a carrier function.
1330
Interest Receivable
The contractor reports interest receivable on accounts receivable. It
accrues interest through the last day of the reporting period.
1330.01
Part A and Part B
The contractor reports HI and SMI interest receivable on accounts
receivable, including extended repayment plans
1990
Other Assets
The contractor reports assets that are not otherwise classified. It
provides an identifying footnote in the remarks section of Form
CMS-750A/B report.
1990.01
Part A and Part B
The contractor reports HI and SMI unclassified assets.
2000
Liabilities
The contractor reports amounts owed after processing Medicare
claims and related activities
2110
Accounts Payable Report amounts owed after processing Medicare
claims or other authorized expenditures. This includes, but is not
limited to, underpayments resulting from adjustment bills
Account Number
Title
2110.01
Part A and Part B
The contractor reports accounts payable attributable to HI and SMI
activities
2110.01.01
Unprocessed Claims
The contractor reports the value of the accounts payable for
unprocessed claims received in-house that have not yet started
processing. The actual value may be developed after the reporting
period but before the required date for reporting. It uses the 30 day
rolling average for the number of claims received and not
processed to determine the number of average unprocessed claims.
2110.01.02
Benefits Payable
The contractor reports accounts payable for those claims that have
completed processing checks, but have not yet been issued nor
offsets applied. This includes, but is not limited to, underpayments
resulting from adjustment bills. It includes claims approved by the
Common Working File (CWF) and claims not approved by the
CWF, but approved by the RO for payment outside the CWF.
2110.01.02.01
Provider
The intermediary reports benefits payable to institutional providers
of Medicare services. This includes, but is not limited to the
following: accounts receivable accrual where the periodic interim
payment (PIP) bills is in excess of periodic interim payme
nts (PIP);
underpayments from receipt of accepted cost reports, tentative
settlements and final cost settlements, when Notices of Provider
Reimbursement (NPR) are prepared; and underpayments for PRRB
settlements, when Notices of Correction (NOC) are prepared, etc
This is not a carrier function.
2110.01.02.01.01
PIP Providers - Cost Report Settlements
The intermediary reports benefits payable to PIP providers as a
result of Cost Report Settlements This is not a carrier function.
2110.01.02.01.02
PIP Providers - Estimated Payable Accrued
The intermediary reports the amount accrued for the (estimated)
accounts payable PIP. (See Exhibit 13 Protocol for Estimating
Payables and Receivables for PIP). This is not a carrier function.
2110.01.02.01.03
Non-PIP Providers - Underpayments (Interim Rate)
The intermediary reports benefits payable to Non-PIP providers as
a result of Interim Rate Reviews This is not a carrier function
Account Number
Title
2110.01.02.01.04
Non-PIP Providers - Underpayments (Cost Report Settlement)
The intermediary reports benefits payable to Non-PIP providers as
a result of Cost Report Settlements This is not a carrier function.
2110.01.02.01.05
Claims Payments Withheld for Non-receipt of Cost Reports
The intermediary reports benefits payable for claims withheld for
payment for non-receipt of provider cost reports This is not a
carrier function.
2110.01.02.02
Beneficiaries
The contractor reports benefits payable to beneficiaries for
reimbursement for Medicare services.
2110.01.02.03
Physicians/Suppliers
The carrier reports benefits payable to physicians or suppliers of
Medicare services. This includes, but is not limited to,
underpayments of quarterly Health Professional Shortage Area
(HPSA) bonus amounts for which a c
heck has not been issued. Not
an intermediary function.
2110.01.02.04
Claims on the Payment Floor Adjudicated claims not yet paid
2110.01.03
Suspended Payments
The contractor reports actual or estimated benefits payable for
claims that were suspended from payment to allow for additional
processing.
2110.01.03.01
Claims
The contractor reports estimated benefits payable for claims
needing additional information or further development, including
CWF rejects and adjustments
210.01.03.02
Common Working File (CWF)
The contractor reports benefits payable for claims that are pending
submission or were submitted to the CWF for approval.
2110.01.03.03
MR/UR Prepayment Review
The contractor reports estimated benefits payable, based on a
developed rate, suspended for MR/UR before payment. The
payables after MR/UR are in 2110.01.02, Benefits Payable
2110.01.03.04
Medicare as Secondary Payer (MSP)
Account Number
Title
The contractor reports benefits payable that are suspended for
investigation of third party liability for MSP prior to payment
2140
Accrued Interest Payable
The contractor reports actual or estimated interest payable on
Medicare liabilities through the end of the reporting period
including, but not limited to, pending claims, court settlements,
claims payment timeliness (CPT), etc.
2140.01
Part A and Part B
The contractor reports HI and SMI interest payable on Medicare
liabilities
2990
Other Liabilities
The contractor reports liabilities not otherwise classified. It
provides an identifying footnote in the remarks section of Form
CMS-750A/B report.
2990.01
Part A and Part B
The contractor reports other liabilities attributable to HI and SMI
activities.
2990.01.01
Unapplied Receipts
The contractor reports amounts deposited and not yet applied to an
accounts receivable.
2990.01.02
Excess Recoupments
The contractor reports amounts recovered from overpayments or
from other sources in excess of receivables established and which
are eligible for refund. It includes those payables identified as due
to third party liability payers, e.g., excess recoupment of MSP
recoveries being returned to the third party.
2990.01.03
Due Medicaid
The contractor reports Medicare claims reimbursements withheld
based on RO instructions for payment to Medicaid.
2990.01.99
Other
The contractor reports actual or estimated amounts payable not
otherwise classified. These include, but are not limited to, claims
payments withheld to satisfy Internal Revenue Service liens, court
liens, unidentified receipts that have not been applied to an account
receivable. It provides an identifying footnote in CAFM.
Account Number
Title
3010
Fund Balance Fund balance reflects the cumulative results of
program operations and extraordinary items. It equals the
difference between assets and liabilities.
3310
Cumulative Results of Operations
These accounts track the net difference between income and
expense activity as reported on the Statement of Operations. This
account is updated with the current year-to-date net results of
operations
3310.01
Part A and Part B
The contractor reports HI and SMI interest revenue from accounts
receivable. It includes current fiscal period earned interest, and any
adjustments. It also includes accrued interest in account 1330,
Interest Receivable
5000
Revenue and Other Financing Sources
The contractor reports the amount of income from Medicare
activities. Typical sources are draws on letter of credit, interest and
recoveries of amounts expended in prior periods.
5303
Interest Revenue
The contractor reports interest earned from accounts receivable.
5303.01
Part A and Part B
The contractor reports HI and SMI interest revenue from accounts
receivable. Include current fiscal period earned interest, and any
adjustments. This will also include accrued interest in account
1330, Interest Receivable.
5303.01.01
Adjustments/Waivers (Interest)
The contractor reports the reduction of the amounts of interest
receivable based on Collections on Delinquent Debt in accordance
with §§1862(b) and 1870(c) of the Social Security Act. It
reconciles this with Form CMS-751A/B, Status of Accounts
Receivable, Line 5h, Waivers (Interest).
5303.01.02
Write-offs Closed/Transfers (Interest)
The contractor reports interest receivable for which collection
efforts have been abandoned or that have been transferred to
another Medicare contractor or other CMS location. These
accounts must be reconciled with the receiving Medicare
contractor or other CMS location.
Account Number
Title
5303.01.02.01
Amounts Written-Off Closed (Bad Debts) (Interest)
The contractor reports interest receivables for which collection is
no longer being pursued according to CMS regulations. It
reconciles this with Form CMS-751A/B, Status of Accounts
Receivable, Line 6a, Amounts Written-off Closed (Bad Debts).
5303.01.02.02
Transfers Out to other CMS Locations (POR/PSOR & Not
POR/PSOR) (Interest). POR not applicable to carriers.
The contractor reports interest receivable transferred to other CMS
locations. Reconcile with Form CMS-751A/B, Status of Accounts
Receivable, Line 5e, Transfers Out to Other CMS Locations,
POR/PSOR, (interest) and Line 5g, Transfers Out to Other CMS
Locations, Not POR/PSOR, (interest). POR not applicable to
carriers.
5303.01.02.02.01
Transfers In from other CMS Locations (POR/PSOR & Not
POR/PSOR) (Interest). POR not applicable to carriers.
The contractor reports interest receivable that has been transferred
to your location from other CMS locations in the current period. It
reconciles this with Form CMS-751 A/B, Status of Accounts
Receivable, Line 5d, Transfers In from Other CMS Locations,
POR, (interest), and Line 5f, Transfers In from Other CMS
Locations, Not POR, (interest). POR not applicable to carriers.
5303.01.02.03
Transfers Out to CNC (Interest)
The contractor reports interest receivable transferred to CNC in
accordance with CMS regulations. It transfers the full amount of
interest due on the debt. It reconciles this with Form CMS-C751,
Status of Non-MSP Debt - CNC, Line 2, New CNC A/R (interest)
and Line 6c, Transfers Out to CNC
5303.01.02.03.01
Transfers In from CNC (Interest)
The contractor reports interest receivable that has been transferred
in to its location from CNC.
5303.01.02.04
Transfers Out to other Medicare Contractors (Interest)
The contractor reports interest receivable transferred to other
Medicare contractors. Reconcile with Form CMS-751A/B, Status
of Accounts Receivable, Line 5c, Transfers Out to Other Medicare
Contractors.
5303.01.02.04.01
Transfers in from other Medicare Contractors (Interest)
Account Number
Title
The contractor reports interest receivable transferred to your
location from other Medicare contractors. It reconciles this with
Form CMS-751A/B Status of Accounts Receivable, Line 5b,
Transfers In from Other Medicare Contractors (Interest)
5700
Appropriated Capital Used
The contractor reports the amount of Medicare funds drawn to be
matched against current period expense. This amount must be
consistent with amounts reported on Form CMS-1521, Contractor
Draws on Letter of Credit, and on Form CMS-1522, Monthly
Contractor Financial Report. The contractor does not include
administrative draws through the Payment Management System
(PMS), (Smartlink)
5700.01
Part A and Part B, Draws on Letter-of-Credit
5900
Other Revenue
The contractor reports revenue not otherwise classified. It provides
identifying footnote(s) in the remarks section of Form CMS-750
A/R report
5900.01
Part A and Part B
The contractor reports HI and SMI other revenue
5900.01.01
Other
The contractor reports revenue not otherwise classified
6000
Expense
The contractor reports the outflow of assets or incurrence of
liabilities during a period resulting from rendering Medicare
services.
6100
Operating/Program Expense
The contractor reports net benefits costs incurred throughout the
FY. The expense is the adjusted benefits outlay in cash or its
equivalent and accrued liabilities incurred in carrying out the
Medicare program. This includes, but is not limited to, adjustments
for MSP recoveries, reconsiderations, and pending litigation.
6100.01
Part A and Part B
The contractor reports HI and SMI benefit program expense.
6101
Waivers (Principal)
Account Number
Title
The contractor reports HI and SMI waiver expense.
6101.01
Part A and Part B
The contractor reports the reduction of the amounts receivable
based on application of §§1862(b) and 1870(c) of the Social
Security Act. It reconciles this with Form CMS-751A/B, Status of
Accounts Receivable, Line 5h, Waivers.
6101.01.02
Transfers Out to other CMS Locations (Principal)
The contractor reports accounts receivable transferred to other
CMS locations. It reconciles this with Form CMS-751A/B, Status
of Accounts Receivable, Line 5e, Transfers Out to Other CMS
Locations, POR/PSOR and Line 5g, Transfers to Other CMS
Locations, Not POR/PSOR. POR not applicable to carriers.
6101.01.02.01
Transfers In from other CMS Locations (Principal)
The contractor reports accounts receivable amounts that have been
transferred to its location from other CMS locations in the current
period. It reconciles this with Form CMS-751 A/B, Status of
Accounts Receivable, Line 5d, Transfers In from Other CMS
Locations, POR/PSOR (principal), and Line 5f, Transfers In from
Other CMS Locations, Not POR/PSOR (principal). POR not
applicable to carriers.
6101.01.03
Transfers Out to CNC (Principal)
The contractor reports accounts receivable amounts that have been
transferred to CNC in accordance with CMS regulations. . It
reconciles this with Form CMS-C751A/B, Status of Non- MSP
Debt - CNC, Line 2, New CNC A/R, and Line 6c Transfers Out to
CNC of Form CMS-
751A/B, Status of Accounts Receivable report.
It transfers the full amount of principal due.
6101.01.03.01
Transfers In from CNC (Principal)
The contractor reports accounts receivable amounts that have been
re-established as an active accounts receivable. It reconciles this
with Form CMS-751A/B, Status of Accounts Receivable, Line 6b,
Transfers In from CNC
6101.01.04
Transfers Out to other Medicare Contractors (Principal)
The contractor reports HI and SMI accounts receivable transferred
out to a Medicare contractor for collection. It reconciles this with
Form CMS-751A/B, Status of Accounts Receivable, Line 5c,
Transfers to Other Medicare Contractors.
Account Number
Title
6101.01.04.01
Transfers In from other Medicare Contractors (Principal)
The contractor reports HI and SMI accounts receivable transferred
to your location from other Medicare contractors. It reconciles this
with Form CMS-
751 A/B, Status of Accounts Receivable, Line 5b,
Transfers In from Other Medicare Contractors.
6106
Write-offs Closed/Transfers (Principal)
The contractor reports accounts receivable for which collection
efforts have been abandoned, or that have been transferred to
another Medicare contractor or other CMS location. These
accounts must be reconciled with the receiving Medicare
contractor or other CMS location.
6106.01
Part A and Part B
The contractor reports HI and SMI accounts receivable written off
or transferred.
6106.01.01
Amounts Written-Off Closed (Bad Debts) (Principal)
The contractor reports receivables for which collection is no longer
being pursued according to CMS rules. It reconciles this with Form
CMS-751A/B, Status of Accounts Receivable, Line 6a, Amounts
Written-off Closed (Bad Debts).
6330
Interest Expense
The contractor reports interest expense incurred for claims for
Medicare benefits or accounts payable.
6330.01
Part A and Part B
The contractor reports HI and SMI interest expense.
6330.01.01
Claims Payment Timeliness (CPT) Interest
The contractor reports interest paid for claims that failed the claims
payment timeliness (CPT) requirement. It reconciles this with
Form CMS-1522, interest paid, claims timeliness.
6330.01.02
Other Interest
The contractor reports interest for other late payments. It reconciles
this with Form CMS-1522, interest paid, provider underpayments.
6909
Other Expense
The contractor reports benefit expenses not reported in named
categories or otherwise classified. It provides an identifying
footnote in the remarks section of Form CMS-750A/B report.
Account Number
Title
6909.01
Part A and Part B
The contractor reports HI and SMI unclassified benefit expenses.
7400
Prior Period Adjustments
The contractor reports adjustments for prior period activity to
restate assets, liabilities, etc. It provides an identifying footnote in
the remarks section of Form CMS-750 report.
7400.01
Part A and Part B
The contractor reports HI and SMI prior period adjustments.
400.12 - Exhibit 12 - Accounts Payable - Protocol for Estimating Claims
- Form CMS-H750A/B, Statement of Financial Position - (Rev. 5, 08-30-
02)
A1-1960.12, B1-4960.12
Accounts Payable Protocol for Estimating Claims
Form CMS-H750A/B, Statement of Financial Position
The amounts recorded in accounts payable (A/P) may be estimated based on actual
volumes and historical rates; therefore, the FI or carrier calculates and accrues a new
estimated liability each reporting period and reverses the accrual for the previous period
in full. It charges the expense accounts, rather than the A/P, as actual payments are made.
INTERMEDIARY PROCEDURES
Methodology for Calculating Average Reimbursement Amount and Average Interest for
Pricing Claim Liabilities
To assign an estimated value to claims for which the amount to be paid is unknown, the
contractor counts claims and multiplies the total by the average reimbursement amount
(net of interest) and an average interest amount (CPT), if applicable, determined as
follows:
The intermediary calculates the average reimbursement amount by taking a representative
sample of the most recent 12 months of paid claims history. It totals the reimbursement
amount minus interest and divides by the total number of claims processed. It calculates
the Claims Payment Timelines (CPT) by adding the interest from the same claims and
divides by the total number of claims (not just those bearing interest).
The intermediary performs these calculations by bill types and will be segregated
between Part A and Part B. (See Intermediary Manual, Part 3, §3894.3.)
GENERAL PROCEDURES
These methods may be used to assign an estimated value to claims in the following
categories:
1. In-house, unprocessed claims; and
MR/UR
PRO
2. Claims suspended for prepayment review
Claims
MR/UR
PRO
400.13 - Exhibit 13 - Periodic Interim Payments (PIP) Protocol for
Estimating Payables/Receivables for the Forms CMS-H750/751A/B,
Statement of Financial Position and Status of Accounts Receivable
Report (Intermediaries Only) - (Rev. 5, 08-30-02)
A1-1960.13, B1-4960.13
Periodic Interim Payments (PIP)
Protocol for Estimating Payables/Receivables for the Form CMS-H750/H751A/B,
Statement of Financial Position and Status of Accounts Receivable Reports
It is necessary to report on Form CMS-H750, a cumulative estimated accounts receivable
or payable for all fiscal periods since the provider's last accepted cost report period. To
estimate this amount, the intermediary performs the following steps:
1. It determines the total amount for PIP bills processed for the fiscal period less
outlier amounts;
2. It compares the PIP bills amount to the actual PIP cash payment and lump sum
payments (checks issued) made during the fiscal period. This does not include any
outlier payments that may have been issued on the same check with the PIP;
3. It reports the amount that PIP bills exceed the PIP cash payment as an account
payable; and
4. It reports the amount that PIP cash payment exceeds the PIP bills as an account
receivable.
For example: If the provider's FY ends on December 31, then the cost report should be
received and accepted before the June 30 reporting period. The following demonstrates
how the PIP accumulations would be reported for this provider.
Period Ending
Reporting
December 31
Assuming all prior year cost reports have been accepted,
the only entry on the books for this provider would be
the estimated accounts receivable or accounts payable
after comparing PIP payments to claims submitted since
January 1st to current.
March 31
Given the same assumption regarding prior cost reports,
the PIP estimate for this provider will include the entire
prior FY for the provider (January 1 - December 31)
unless the cost report has been filed and accepted, and
the current FY for the provider (January 1- March 31).
June 30
Given the same assumption regarding prior cost reports,
assuming the latest cost report has now been received
and accepted and the appropriate accounts receivable or
accounts payable are booked, the PIP estimated for this
provider will now include only the current FY for the
provider (January 1- June 30).
Sept 30
Given the same assumption regarding prior cost reports,
assuming the latest cost report has now been received
and accepted, the PIP estimate for this provider will now
include only the current FY for the provider (January 1-
September 30).
400.14 - Exhibit 14 - Protocol for Estimating Allowance for
Uncollectible Accounts Forms CMS-H/M751A/B, Status of Accounts
Receivable
(Rev. 115, Issued: 01-24-07; Effective Date: 04-01-07; Implementation Date: 04-02-
07)
The Federal Accounting Standards Advisory Board (FASAB) recommends through
Statement of Federal Financial Accounting Standard Number 1 (Paragraphs 44&45) that
losses on receivables should be recognized when it is more likely than not that the
receivables will not be totally collected. The phrase "more likely than not" means more
than a 50 percent chance of loss occurrence. An allowance for estimated uncollectible
amounts should be recognized to reduce the gross amount of receivables to its net
realizable value. The allowance for uncollectible amounts should be re-estimated on each
annual financial reporting date (at a minimum) and when information indicates that the
latest estimate is no longer correct. These losses should be measured through a systematic
methodology. The systematic methodology should be based on analysis of both
individual accounts and a group of accounts as a whole.
Accounts that represent significant amounts, i.e., greater that $1 million, should be
individually analyzed to determine the loss allowance. Loss estimation for individual
accounts should be based on (a) the debtor's ability to pay, (b) the debtor's payment
record and willingness to pay, and (c) the probable recovery of amounts from secondary
sources, including liens, garnishments, cross collections and other applicable collection
tools.
The entire allowance for losses generally cannot be based solely on the results of
individual account analysis. In many cases, information may not be available to make a
reliable assessment of losses on an individual account basis or the nature of the
receivables may not lend itself to individual account analysis. In these cases, potential
losses should be assessed on a group basis.
CMS has implemented FASAB's recommendations and has developed this protocol for
Medicare contractors to follow for estimating the allowance for uncollectible accounts.
The following section outlines this methodology.
Protocol for Estimating Allowance for Uncollectible Accounts
Medicare contractors must recognize on Line 8, Allowance for Uncollectible Accounts,
on Forms CMS-H/M751A/B, an estimated amount for uncollectible debt in order to
reduce the gross amount of receivables to its net realizable value. Medicare contractors
must re-estimate the allowance for uncollectible amounts on March 31 and September 30
of each FY and when information indicates that the latest estimate is no longer correct.
Medicare contractors must measure potential losses due to uncollectible amounts through
a systematic method. This systematic method must be based on an analysis. The analysis
requires that receivables be further stratified into sub-groups (i.e., Cost Report Settlement
Activity, Claims Accounts Receivable, Credit Balances, Group Health Plan (GHP) MSP,
Liability MSP and Other Accounts Receivables). The subgroups are somewhat different
for Group 1 - Fiscal Intermediaries, as compared to Group 2 - Carriers.
Group 1 (Fiscal Intermediaries)
Sub-Group 1
1. Cost Report Settlements Activity (Non MSP)
2. Claims Accounts Receivable, Credit Balances & Other Accounts
Receivables (Non-MSP)
Sub-Group 2
1. Group Health Plan (Data Match/Non Data Match) MSP
2. Liability MSP
For Group 1, Subgroup 1, fiscal intermediaries must perform the following steps to
calculate and validate the allowance for uncollectible accounts.
1. Calculate the allowance based on the historical collection percentage (see detailed
instructions below) for Non-MSP as a whole.
2. Individual Account Analyses: For cost report settlement activity only, fiscal
intermediaries will identify and total those provider debts that meet certain risk
characteristics (i.e., bankruptcy, terminations, poor collection history, no
collection activity for 6 months or more). These will be considered risk accounts,
and the fiscal intermediary should total all risk accounts identified through this
analysis.
3. Compute the total delinquencies exceeding 180 days (Section B of Forms CMS
H/M751A/B "Delinquent Receivables").
4. Compare the three estimated amounts calculated in Steps 1, 2 & 3 and identify the
amount that ensures that the net receivable is reported at its realizable value.
For Group 1, Subgroup 2, the fiscal intermediary must perform the following steps to
calculate and validate the allowance for uncollectible accounts.
1. Calculate the allowance based on the historical collection percentage (see
detailed instructions below) for MSP as a whole.
2. Compute the total delinquencies exceeding 180 days (Section B of Forms CMS-
H/M751A/B "Delinquent Receivables").
3. Compare the two estimated amounts calculated in Steps 1 & 2 and identify the
amount that ensures that the net receivable is reported at its realizable value.
Historical Collection Percentage Calculation
A - Determine Total Receivables Eligible for Collection. (Using Forms CMS
H/M751A/B)
Required Formula:
Beginning Balance
(Line 1)
Plus: New Receivables
(Line 2a)
Plus/Less: Adjusted Amounts
(Line 5a)
(plus if positive number less if negative number)
Plus: Transfers In from other Medicare Contractors
(Line 5b)
Plus: Transfers In from other CMS locations, POR &
Not POR
(Lines 5d & 5f)
Plus: Transfers In from CNC
(Lines 6b)
Less: Transfers Out to other Medicare Contractors
(Line 5c)
Less: Transfers Out to other CMS locations, POR & Not
POR
(Lines 5e & 5g)
Less: Waivers & Amounts Written Off (Bad Debts) (Lines 5h & 6a)
Less: Transfers Out to CNC
Equals: Total Receivables Available to be Collected
(Line 6c)
B - Determine Rate of Collections
Line 4a, Cash/Check Collections plus Line 4b, Offsets Collection plus Line 4c,
Collections Deposited At Another Location divided by Total Receivables Available to be
Collected (number calculated from Step A) multiplied times 100 determines the rate of
collections percentage.
C - Determine the Allowance Rate
1.00 minus the percentage determined from Step B, equals the allowance rate
D - Average the Percentage Calculated in Step C with a 5-year Historical Allowance Rate
(if available, if not available, maintain statistical data to develop historical rate, and
proceed to Step E).
E - Calculate the Allowance
Multiply the allowance rate from Step C or Step D by the sum of Line 7, Ending Balance
less Line 2b, Accrued Receivables.
Group 2 (Carriers)
Sub-Group 1
1. Claims Accounts Receivable, Credit Balances & Other Accounts
Receivables (Non-MSP)
Sub-Group 2
1. Group Health Plan (Data Match/Non Data Match) MSP
2. Liability MSP
For Group 2, Subgroup 1, the carrier must perform the following steps to calculate and
validate the allowance for uncollectible accounts.
1. Calculate the allowance based on the historical collection percentage (see detailed
instructions below) for Non-MSP as a whole.
2. Compute the total delinquencies exceeding 180 days (Section B of Forms CMS-
H/M751B "Delinquent Receivables").
3. Compare the two estimated amounts calculated in Steps 1 & 2 and identify the
amount that ensures that the net receivable is reported at its realizable value.
For Group 2, Subgroup 2, the carrier must perform the following steps to calculate and
validate the allowance for uncollectible accounts.
1. Calculate the allowance based on the historical collection percentage (see detailed
instructions below) for MSP as a whole.
2. Compute the total delinquencies exceeding 180 days (Section B of Forms CMS-
H/M751B "Delinquent Receivables").
3. Compare the two estimated amounts calculated in Steps 1 & 2 and identify the
amount that ensures that the net receivable is reported at its realizable value.
Historical Collection Percentage Calculation
A. Determine Total Receivables Eligible for Collection. (Using Forms CMS-H/M751B)
Required Formula:
Beginning Balance
(Line 1)
Plus: New Receivables
(Line 2a)
Plus/Less: Adjusted Amounts
(Line 5a)
(plus if positive number less if negative number)
Plus: Transfers In from other Medicare Contractors
(Line 5b)
Plus: Transfers In from other CMS locations, POR &
Not POR
(Lines 5d & 5f)
Plus: Transfers In from CNC
(Line 6b)
Less: Transfers Out to other Medicare Contractors
Less: Transfers Out to other CMS locations, POR & No
Less: Waivers & Amounts Written Off (Bad Debts)
(Line 5c)
(Line 5e & 5g)
(Line 5h & 6a)
Less: Transfers Out to CNC
(Line 6c)
Equals: Total Receivables Available to be Collected
B. Determine Rate of Collections
Line 4a, Cash/Check Collections plus Line 4b, Offsets Collections plus Line 4c,
Collections Deposited At Another Location divided by Total Receivables Available to be
Collected (number calculated from Step A) multiplied times 100 determines the rate of
collections percentage.
C. Determine the Allowance Rate.
1.00 minus the percentage determined from Step B, equals the allowance rate
D. Average the percentage calculated in Step C with a 5-year historical allowance rate (if
available, if not available, maintain statistical data to develop historical rate, and go
proceed to Step E).
E. Calculate the Allowance
Multiply the allowance rate from Step C or Step D (Group 2, Carriers Section) by Line 7,
Ending Balance.
Medicare contractors are required to compare the results of the estimated allowance
based on the protocol and report on Line 8, Allowance for Uncollectible Accounts, the
amount that ensures that the net receivable is reported at its realizable value. The
Medicare contactors are required to maintain supporting documentation that includes the
assumptions used to calculate the allowance amount reported on Forms CMS
H/M751A/B. The documentation must be available for review by CMS, OIG, GAO or
other parties as required.
Note: Medicare contractors may apply the same method of results of the principal
comparison (Col. D, Example 400.14.3) to estimate the interest allowance amount (Col.
E, Example 400.14.3) to be reported on Line 8, Allowance for Uncollectible Accounts, of
the Forms CMS H/M 751A/B. For example, the method of results for the Non-MSP
principal is delinquencies exceeding 180 days. The Medicare contractor has the option to
report on the allowance matrix for interest (Sub-Group 1, Col. E) the amount equal to the
delinquencies exceeding 180 days from the interest column on Form CMS 751. The
method of results for the MSP principal is the historical collection percentage. The
Medicare contractor has the option to report on the allowance matrix for interest (Sub-
Group 2, Col. E) the amount equal to the same percentage calculated for MSP principal,
multiplied by Line 7, ending balance from the interest column on Form CMS 751. The
method selected by the Medicare contractor used to estimate the interest allowance shall
ensure that the net interest receivable is reported at its realizable value.
Each Medicare contractor must complete the Allowance for Uncollectible Accounts
Matrix (Attachment I or Attachment II) for the periods ending March 31 and September
30 of each year. The accounts matrix is to be mailed to CMS CO. The March 31
Allowance for Uncollectible Accounts Matrix is due on April 21 and the September 30
Allowance for Uncollectible Accounts matrix is due on October 21. The Medicare
contractor must submit a separate Allowance for Uncollectible Accounts Matrix for each
Form CMS 751 (i.e. H751A, H751B of A, H751B and H751B-DMERC).
Please submit your matrix(s) via email to [email protected] as well as a
hard copy to the following address:
Centers for Medicare & Medicaid Services
Division of Financial Reporting and Policy
Attention: Director of DFRP
Mail Stop: N3-11-17
7500 Security Boulevard
Baltimore, Maryland 21244

Example 400.14.1
H751
Non-MSP M751
Section A: Outstanding Receivables
Principal
Principal Principal
1.
Beginning FY Balance
329,345,200
188,945,200
140,400,000
2a.
New Receivables
80,050,600
57,500,600
22,550,000
2b. Accrued Receivables 40,455,000
40,455,000
0
3.
Interest Earned
-
-
4a. Cash/Check Collections (218,697,200)
(202,697,200)
(16,000,000)
4b.
Offset Collections (424,000) (424,000)
0
4c.
Collections Deposited at another Location (50,000)
(50,000)
0
5a. Adjusted Amounts
-
Internal Adjustments (4,409,000)
(2,319,000)
(2,090,000)
Auditor/Consultant Adjustments
(5,617,400)
(5,617,400)
0
5b. Transfers In from other Medicare Contractors 10,242,000
10,242,000
0
5c. Transfers Out to other Medicare Contractors
(160,000)
-
(160,000)
5d.
Transfers In from other CMS Locations, POR
304,000
304,000
0
5e.
Transfers Out to other CMS locations, POR
(247,600)
(247,600)
0
5f. Transfers In from other CMS Locations, Not POR
126,000 126,000
0
5g.
Transfers Out to other CMS Locations, Not POR (150,000)
(150,000)
0
5h. Waivers (292,000)
-
(292,000)
6a. Amounts Written-off (Bad Debts)
(536,000)
-
(536,000)
6b.
Transfers In from CNC -
-
0
6c. Transfers Out to CNC
(106,420,000) (2,089,600)
(104,330,400)
7. Ending Balance
123,519,600
83,978,000
39,541,600
a. Current
92,639,700
62,983,500
29,656,200
b. Non-current 30,879,900
20,994,500
9,885,400
8.
Allowance for Uncollectible Accounts (49,745,910) (29,327,200)
(20,418,710)
9.
Total Receivables Net of Allowance 73,773,690
54,650,800
19,122,890
10. Cash/Offsets Received for Receivables at Another Location
-
H751 Non-MSP M751
Section B: Delinquent Receivables Principal
Principal Principal
1. Total Not Delinquent
239,000 186,000
53,000
2. Total Delinquent 123,280,600
83,792,000
39,488,600
(a) 1-30 days 6,150,302 4,182,736
1,967,566
(b) 31-60 days 20,341,299
13,825,680 6,515,619
(c) 61-90 days 23,976,069
16,346,304 7,629,765
(d) 91-180 days 29,511,844
20,110,080
9,401,764
(e) 181-365 days 12,316,710 8,371,915
3,944,795
(f) 1-2 years 30,797,413
20,940,700 9,856,713
(g) 2-6 years 86,850
7,285 79,565
(h) 6-10 years 15,113
3,200 11,913
(I) over 10 years 85,000
4,100 80,900
Status of Accounts Receivable
Hospital Insurance (HI)
As of March 31, 2003
Example 400.14.2
Historical Collection Percentage Calculation
H751A Non-MSP M751A
A. Determine Total Receivable Eligible for Collection Principal Principal Principal
1.
Beginning FY Balance
329,345,200 188,945,200 140,400,000
2a. New Receivables 80,050,600 57,500,600 22,550,000
5a. Adjusted Amounts
Internal Adjustments (4,409,000) (2,319,000) (2,090,000)
Auditor/Consultant Adjustments (5,617,400) (5,617,400) -
5b. Transfers In from other Medicare Contractors 10,242,000 10,242,000 -
5c. Transfers Out to other Medicare Contractors (160,000) - (160,000)
5d. Transfers In from other HCFA Locations, POR 304,000 304,000 -
5e. Transfers Out to other HCFA locations, POR (247,600) (247,600) -
5f. Transfers In from other HCFA Locations, Not POR 126,000 126,000 -
5g. Transfers Out to other HCFA Locations, Not POR (150,000) (150,000) -
5h. Waivers (292,000) - (292,000)
6a. Amounts Written-off (Bad Debts) (536,000) - (536,000)
6b. Transfers In from CNC - - -
6c. Transfers Out to CNC (106,420,000) (2,089,600) (104,330,400)
Total Receivables Available to be Collected 302,235,800 246,694,200 55,541,600
B. Determine Rate of Collections
4a. Cash/Check Collections 218,697,200 202,697,200 16,000,000
4b. Offset Collections 424,000 424,000 -
4c. Collections Deposited at another Location 50,000 50,000 -
Total Collections 219,171,200 203,171,200 16,000,000
Rate of Collections (Total Collections divided by Adjusted
Total Eligible for Collection) N/A 82% 29%
[ 203,171,200 / 246,694,200 = .82 or 82%]
C. Determine Allowance Rate
1.00 minus (-) the percentage determined for Step B N/A 18% 71%
[1.00 - Rate of Collections (1.00 - 0.82 = 0.18 or 18%)]
D. 5-year Average (if available)
(.50+.46+.48+.43+ Allowance Rate from Step C)/5 = N/A 41% 52%
FY 99 = 50%
FY 00 = 46%
FY 01 = 48%
FY 02 = 43%
FY 3/03 =
E. Calculate the Allowance
Multiply the ending balance less PIP accrual (Line 7 - PIP accrual) by the allowance rate
(Step C or Step D)
7. Ending Balance 123,519,600 83,978,000 39,541,600
2b. (Less) Accrued Receivables-(PIP Accrual Only) (40,455,000) (40,455,000) -
Adjusted Ending Balance 83,064,600 43,523,000 39,541,600
Allowance for Uncollectible Accounts 38,232,020 17,813,310 20,418,710
Allowance for Uncollectible Accounts
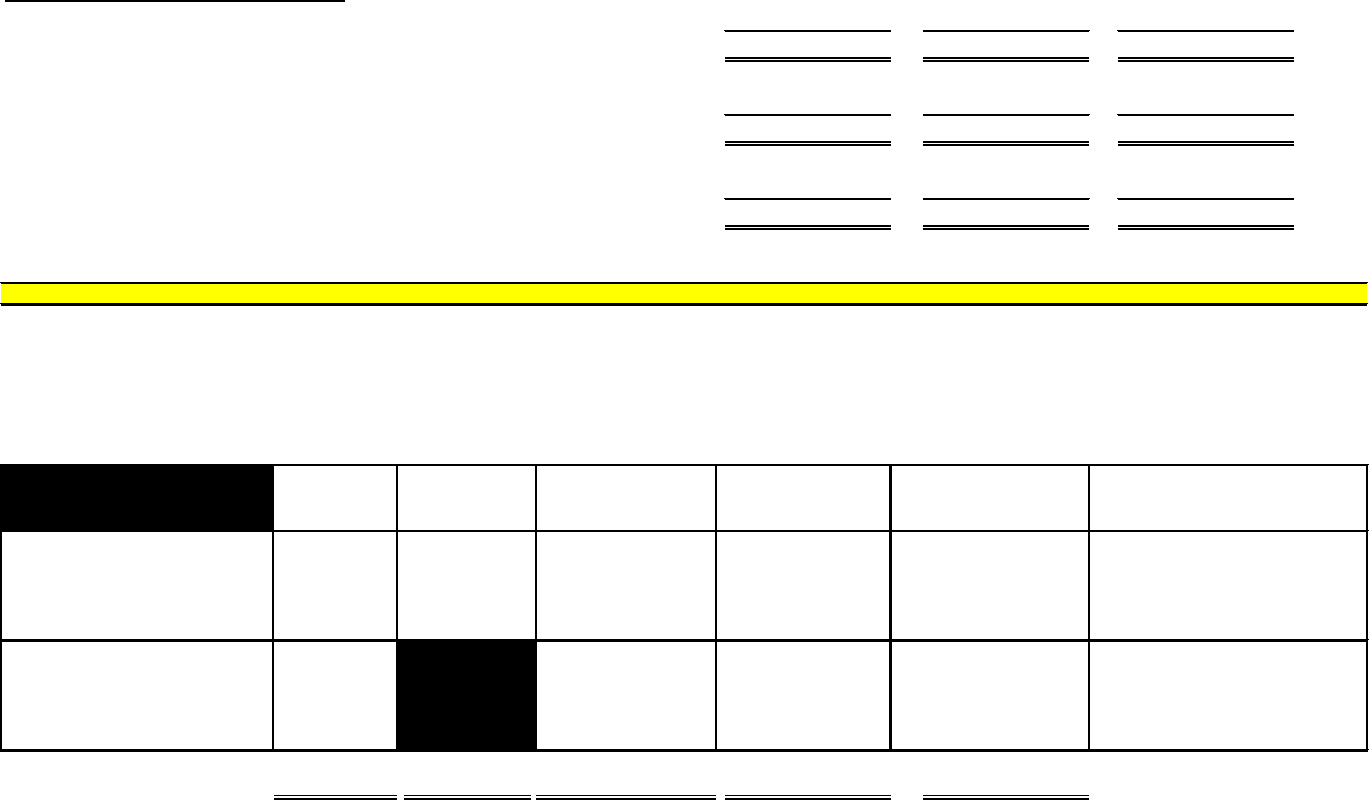
Example 400.14.3
Systematic Analysis Comparison H751A
Non-MSP MSP
Historical Collection % 38,232,020
17,813,310
20,418,710
Individual Account Analysis 15,000,800 15,000,800
-
Delinquencies Exceeding 180 days 43,301,086
29,327,200
13,973,886
400.14 - Exhibit 14 - Protocol for Estimating Allowance for Uncollectible Accounts
Attachment I - Fiscal Intermediary
Allowance for Uncollectible Accounts Matrix
Group 1 Col. A Col. B Col. C Col. D Col. E
Historical
Individual Delinquencies Estimated
Collection % Account Exceeding 180 Days Allowance for
Total Analysis Total Total Uncollectible A/R
Sub-Group 1 (Non-MSP)
Cost Report Settlements,
Claims A/R, Credit Balance &
Other Accounts Receivables
17,813,310 15,000,800 29,327,200
29,327,200 4,768,143
Sub-Group 2 (MSP)
Group Health Plan (Data-Match
& Non-Data Match),
Liability 20,418,710 13,973,886 20,418,710 3,319,762 (Amount reported on M751A/B)
Total 38,232,020 15,000,800 43,301,086 49,745,910
8,087,905
Amount Reported on H751A
Each Medicare contractor will be required to complete the allowance for uncollectible account matrix on
March 31
and
September 30 of each year.
In addition, this matrix is to be mailed to CMS CO. Supporting documentation must include assumptions used to calculate the allowance for uncollectible
accounts and should be available for review by CMS, OIG, GAO or other parties as required. The matrix must be submitted to the following address/email
(provided above) on April 21 and October 21. If these dates occur on a holiday or weekend, the matrix is due the following Federal workday.
Status of Accounts Receivable
Hospital Insurance (HI)
As of March 31, 2003
Estimated Allowance
See Attached Workpapers
See Attached Workpapers
for Uncollectible A/R
(Interest Only)
Justification for amount
reported on Line 8
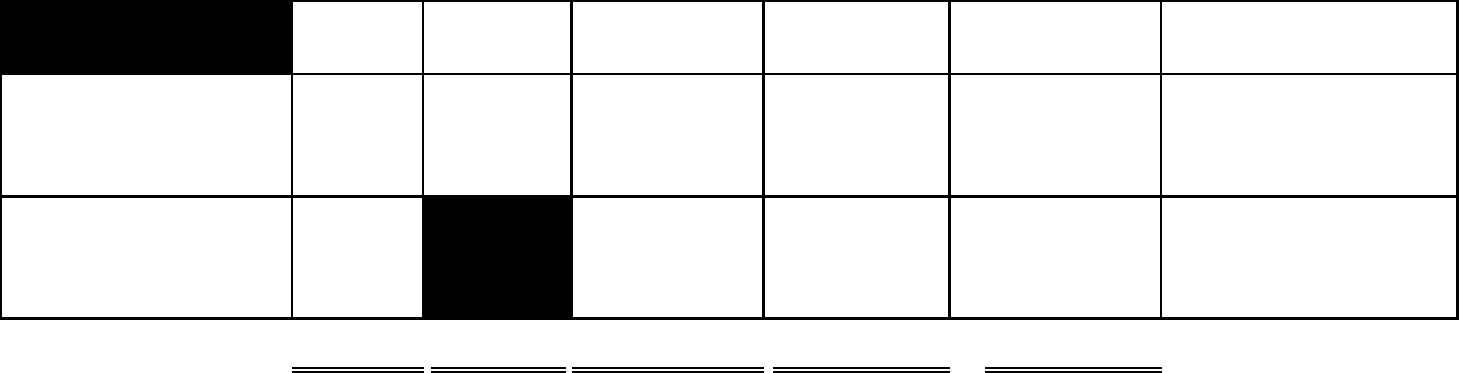
400.14 - Exhibit 14 - Protocol for Estimating Allowance for Uncollectible Accounts
Attachment I - Fiscal Intermediary
Allowance for Uncollectible Accounts Matrix
Group 1 Col. A Col. B Col. C Col. D Col. E
Historical Individual Delinquencies Estimated
Collection % Account Exceeding 180 Days Allowance for
Total Analysis Total Total Uncollectible A/R
Sub-Group 1 (Non-MSP)
Cost Report Settlements,
Claims A/R, Credit Balance &
Other Accounts Receivables
Sub-Group 2 (MSP)
Group Health Plan (Data-Match
& Non-Data Match),
Liability
(Amount reported on M751A/B)
Total
Amount Reported on H751A/B
Each Medicare contractor will be required to complete the allowance for uncollectible account matrix on March 31 and September 30 of each year.
In addition, this matrix is to be mailed to CMS CO. Supporting documentation must include assumptions used to calculate the allowance for uncollectible
accounts and should be available for review by CMS, OIG, GAO or other parties as required. The matrix must be submitted to the following address/email
(provided above) on April 21 and October 21. If these dates occur on a holiday or weekend, the matrix is due the following Federal workday.
Estimated Allowance
See Attached Workpapers
See Attached Workpapers
for Uncollectible A/R
(Interest Only)
Justification for amount
reported on Line 8
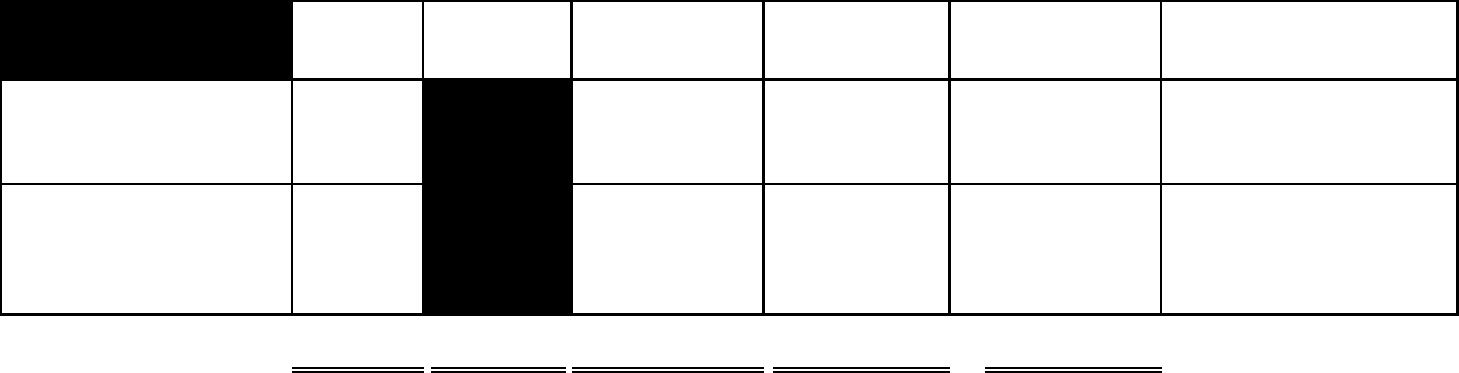
400.14 - Exhibit 14 - Protocol for Estimating Allowance for Uncollectible Accounts
Attachment II - Carrier
Allowance for Uncollectible Accounts Matrix
Group 2 Col. A Col. B Col. C Col. D Col. E
Historical Individual Delinquencies Estimated
Collection % Account Exceeding 180 Days Allowance for
Total Analysis Total Total Uncollectible A/R
Sub-Group 1 (Non-MSP)
Claims A/R, Credit Balance &
Other Accounts Receivables
Sub-Group 2 (MSP)
Group Health Plan (Data-Match
& Non-Data Match),
Liability
(Amount reported on M751A/B)
Total Amount Reported on H751B
Each Medicare contractor will be required to complete the allowance for uncollectible account matrix on March 31 and September 30 of each year.
In addition, this matrix is to be mailed to CMS CO. Supporting documentation must include assumptions used to calculate the allowance for uncollectible
accounts and should be available for review by CMS, OIG, GAO or other parties as required. The matrix must be submitted to the following address/email
(provided above) on April 21 and October 21. If these dates occur on a holiday or weekend, the matrix is due the following Federal workday.
Estimated Allowance
See Attached Workpapers
See Attached Workpapers
for Uncollectible A/R
(Interest Only)
Justification for amount
reported on Line 8
400.15 - Exhibit 15 - Protocol for Prorating Intermediary Time Account
Balances Between Form CMS-H750A (HI) and Form CMS-H750B
(SMI) - (Rev. 5, 08-30-02)
A1-1960.15, B1-4960.15
Protocol for Prorating Intermediary Time
Account Balances Between Form CMS-H750A (HI) and Form CMS-H750B (SMI)
The contractor selects a representative sample of checks and EFT payments issued and
determines the ratio of the number of HI checks/EFT payments to the number of SMI
checks/EFT payments. Checks or EFT payments for both HI and SMI will be split 50-50.
It uses this ratio to prorate the time account balance for the financial reports.
400.16 - Exhibit 16 - Electronic Certification - (Rev. 5, 08-30-02)
A1-1960.16, B1-4960.16
Electronic Certification
The Electronic Certification process requires that the Chief Financial Officer (CFO) enter
their password in the certifying official's current password field on the remarks page of
Form CMS-H750A/B and Form CMS-H751A/B. When the password is keyed in, the
CFO's name and title will appear on the document, and allow the document to be
submitted electronically through the CAFM. For security purposes, the new password
field is present to allow the certifying official to change the password assigned by CMS
to one only the CFO knows.
Two people are required to submit a certified report. The preparer may input the financial
data, but cannot certify the reports. The CFO may not input data. The preparer must
retrieve the report in order to allow certification.
1. From the CAFM Main Menu select option 2 - Data Entry
2. Select the type of report to certify
3. From the Data Entry Menu select option 5 - Update Remarks
4. Select the package (report) to certify
5. Enter the certifying official's current password
If there are no serious errors (use PF6 SHOW ERRS to show errors), the contractor may
submit the report (use PF2 SUBMIT to submit the report) and it will be accepted.
If the contractor is working in a worksheet and decides to certify and submit the report, it
may either use the function keys (PF7 PAGE- and PF8 PAGE+), enter FREM (find
remarks) on the transporter line or use the jump key (PF9 JUMP) to go to the remarks
page.
The contractor must re-enter its password if it reviews any portion of the report after
certification and prior to submission even if no changes are made. CAFM will not store
the contractor's password.
400.17 - Exhibit 17 - Instructions for the Transfer of Debt Between
Reporting Entities - (Rev. 5, 08-30-02)
A1-1960.17, B1-4960.10
Instructions for the Transfer of Debt Between Reporting Entities
CMS continues to receive criticism from the OIG and its financial statement auditors for
being inconsistent in methods of transferring accounts receivable cases to and from
Medicare contractors, and other CMS locations. This criticism is a direct result of the
lack of a formalized process and specific instructions for transferring accounts receivable
cases between reporting entities.
For financial reporting purposes, the term "referred" is used when a case is not physically
sent to the receiving entity for collection purposes. In a "referral" situation, the receiving
entity merely "advises and/or assists" the referring entity on what actions to take next
with respect to the debt. The responsibility to collect and report the accounts receivable
remains with the referring entity and must be reported as part of the ending accounts
receivable balance on their Form CMS-H751A/B, Status of Accounts Receivable report.
A "transfer" results when a copy of the up-to-date overpayment case file is physically
"transferred" to another reporting entity, i.e., the RO, CO or another Medicare contractor.
Along with the case file, the transferring entity must attach a "Transfer Request and
Notification of Acceptance" form (see Exhibit 17, Attachment I for intermediaries (parts
A and B transfers and Attachment II for carriers). This form will serve as both: 1) the
transferring entity's request to transfer the case(s), and 2) the receiving entity's
notification of acceptance of the transfer.
The transferring entity must complete the form and sign Line 1. The form summarizes the
case(s) requiring transfer approval. No entry will be made on Form CMS-751A/B at this
time. Upon receipt of the form, the entity receiving the request will sign Line 2 of the
form and forward a copy of the form back to the transferring entity. This will notify the
transferring entity of the receipt of the request. The receiving entity will process the
request within 30 days of receipt of the transfer, and will return a copy of the Transfer
Request and Notification of Acceptance form indicating the case(s) approved for transfer
by signing Line 3 of the form.
Only upon receipt of the form signed by the receiving entity, will the transferring entity
update its internal systems to reflect the transfer of the accounts receivable to the
receiving entity. The transferring entity will reflect the dollar amount of the case(s)
approved for transfer on the appropriate transfers out line of Form CMS-H751A/B (Line
5c, Transfers Out to Other Medicare Contractors; Line 5e, Transfers Out to Other CMS
Locations, POR/PSOR; Line 5g, Transfers Out to Other CMS Locations, Not on
POR/PSOR). Also upon receipt of the form, the transferring entity must sign Line 4 and
forward a copy to the receiving entity to acknowledge receipt of the formal approval for
transfer.
The receiving entity will update all internal systems, as well as the POR/PSOR to reflect
the transfer. The location or Medicare contractor number must also be updated in the
POR/PSOR system to reflect the transfer. In addition, the receiving entity will reflect the
dollar amount of the case(s) approved for transfer on the appropriate transfers in line of
Form CMS-H751A/B (Line 5b, Transfers In from Other Medicare Contractors; Line 5d,
Transfers In From Other CMS Locations, POR/PSOR; Line 5f, Transfers In from Other
CMS Locations, Not POR/PSOR).
Prior to submission of the quarterly Form CMS-H750/751A/B, reporting entities must
reconcile the transfers in and transfers out lines to ensure approved transfers are only
being reported. In addition to the requirement to maintain detailed transaction level
documentation to support these lines, reporting entities must also retain copies of the
signed Transfer Request and Notification of Acceptance forms.
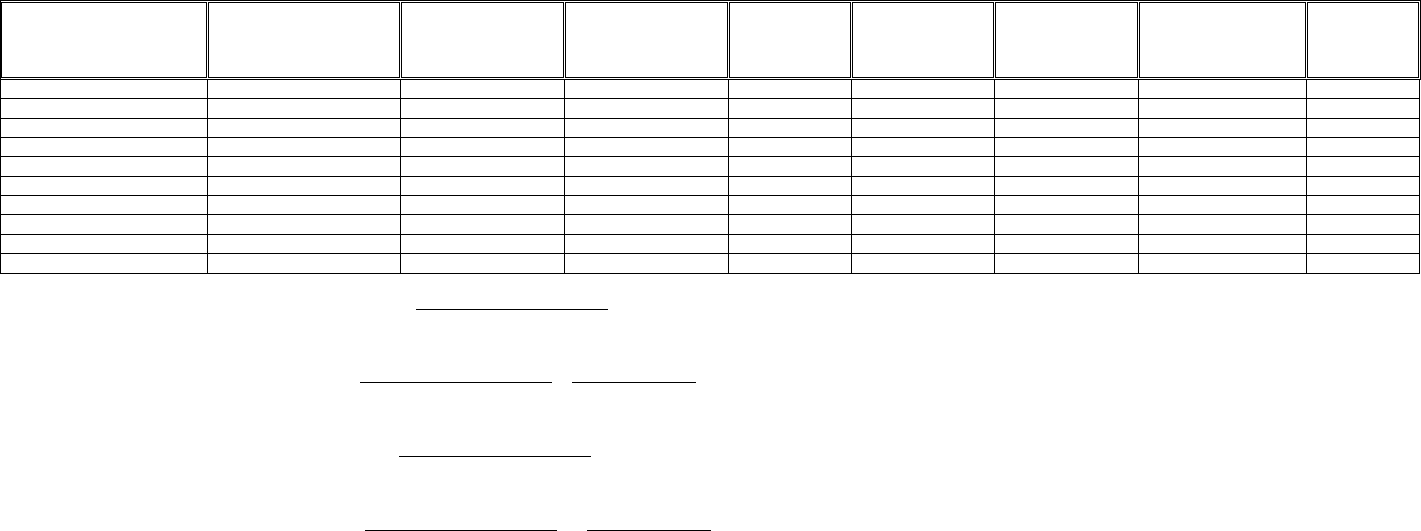
Exhibit 17, Attachment I
TRANSFER REQUEST AND NOTIFICATION OF ACCEPTANCE FORM
INTERMEDIARY PART A OR PART B - ACCOUNTS RECEIVABLE (Indicate whether HI or SMI)
Provider
Name
Provider
Number
Cost
Report
Period
Overpayment
Determination
Date
Original
Amount
Outstanding
Principal
Balance
Outstanding
Interest
Balance
Acceptance
Of Transfer
Yes/No
Reason for
Rejection
Line 1:Requesting/Transferring Entity Official: (Signature required)
Total Dollar Amount Requested for Transfer: $____________
Title:_____________________
Telephone:_________________
Date Requested:_________
Line 2: Acknowledgement of Receipt of (Signature required)__(Date received)___
Request Form
Line 3: Approving/Receiving Entity Official: (Signature required)
Total Dollar Amount Approved for Transfer: $____________
Title:_____________________
Telephone:_________________
Date Approved:_________
Line 4: Acknowledgement of Receipt of (Signature required)___(Date received)___
Approved Form
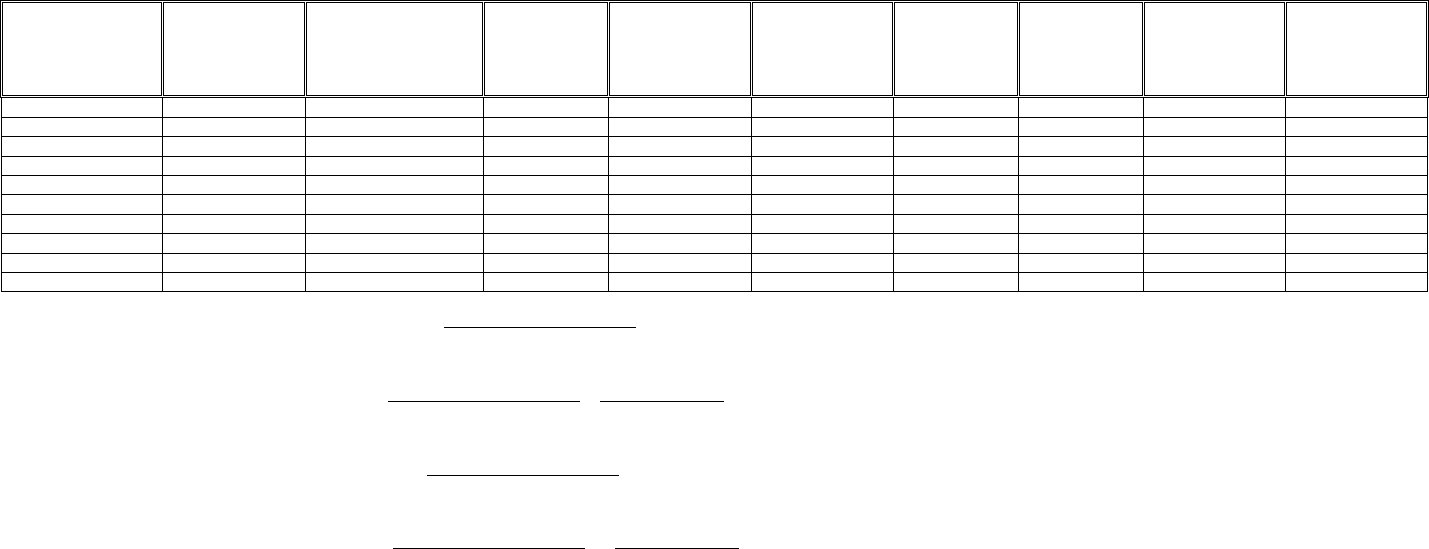
Exhibit 17 - Attachment II
TRANSFER REQUEST & NOTIFICATION OF ACCEPTANCE FORM
CARRIER ACCOUNTS RECEIVABLE
Provider
Name
Provider
Number
Claim Number
Claim Paid
Date
Overpayment
Determination
Date
Original
Amount
Outstanding
Principal
Balance
Outstanding
Interest
Balance
Acceptance
Of Transfer
Yes/No
Reason for
Rejection
Line 1:Requesting/Transferring Entity Official: (Signature required)
Total Dollar Amount Requested for Transfer: $____________
Title:_____________________
Telephone:_________________
Date Requested:_________
Line 2: Acknowledgement of Receipt of (Signature required)__(Date received)___
Request Form
Line 3: Approving/Receiving Entity Official: (Signature required)
Total Dollar Amount Approved for Transfer: $____________
Title:_____________________
Telephone:_________________
Date Approved:_________
Line 4: Acknowledgement of Receipt of (Signature required)___(Date received)___
Approved Form
400.18 - Exhibit 18 - Collection Reconciliation/Acknowledgement Form - (Rev. 5, 08-30-
02)
A1-1960.18, B1-4960.11
Collection Reconciliation/Acknowledgement Form
There are instances where one reporting entity has received and deposited cash/check/offset/electronic funds
transfers (EFTs) for a receivable that is being reported by another entity. In this situation, accounts
receivable cases will not be transferred to the location where the deposit of the money is made. To ensure
proper matching and application of the collection of monies to the outstanding receivable, the "Collection
Reconciliation/Acknowledgement" form must be completed. This form must be completed by the entity
(Medicare contractor, CMS RO or CO) receiving a collection for an accounts receivable that is currently
being reported on the financial reports (Forms CMS-H751A/B-CMS-R751A/B) of another entity.
Medicare contractors are required to ensure that internal controls are in place over the cash/check receipts
process to ensure adequate accounting, recording and custody of Medicare assets.
Treatment of Collections Made by a Medicare Contractor for an Account Receivable at Another Medicare
Contractor Location (applies to Non-Medicare Secondary Payer (MSP) accounts receivables and MSP
accounts receivables)
If a Medicare contractor collects a debt on behalf of another Medicare contractor, whether the receipt was
solicited or unsolicited, then the collection must be forwarded to the Medicare contractor that has the
accounts receivable. In these instances, the Medicare contractor receiving the collection would deposit the
collection and re-issue that amount to the Medicare contractor that is reporting the accounts receivable. The
Medicare contractor reissuing the check should ensure that proper segregation of duties exist over the check
re-issuance (e.g., that the preparer is different from the check authorizer).
The re-issued check must be made payable to "Medicare." In addition, the check must be accompanied by a
completed Collection Reconciliation/Acknowledgement Form (see MIM §1960.18 and MCM §4960.11),
any correspondence received, and a copy of the original check including the postmark date. The CFO for
Medicare Operations for the Medicare contractor reporting the accounts receivable should be contacted and
informed of the pending check. A listing of CFO contacts has been issued to each Medicare contractor CFO.
The deposit and re-issuance of the collection will only affect the CMS-H750A/B of the Medicare contractor
that received the collection. The Collection Reconciliation/Acknowledgement Form will allow for tracking
of the payment.
Upon receipt of the check and Collection Reconciliation/Acknowledgement Form, the Medicare contractor
reporting the receivable will apply its normal cash receipt procedures. However, a signed copy of the
Collection Reconciliation/Acknowledgement Form must be returned to the Medicare contractor that sent the
collection.
MSP additional information: Medicare contractors should follow the deposit and re-issue process whenever
another Medicare contractor has the account receivable or another Medicare contractor is or should be the
lead Medicare contractor. If there is no account receivable established but Medicare contractor X is the lead
and Medicare contractor Y receives payment, Medicare contractor Y should follow the deposit/re-issue
process. If there is no lead established and Medicare contractor Y receives payment, Medicare contractor Y
should do an electronic referral via the Electronic Correspondence Referral System (ECRS) and follow the
deposit/re-issue process if another Medicare contractor is assigned lead. This rule should be followed even if
the non-lead Medicare contractor has an interest and/or has paid some of the claims at issue.
Treatment of Collections Made by a Medicare Contractor for an Account Receivable at a CMS Regional
Office Location (applies to Non-MSP accounts receivables and MSP accounts receivables.)
If a Medicare contractor collects a debt on behalf of a CMS RO location, whether the receipt was solicited or
unsolicited, then the account receivable balance must be transferred to the Medicare contractor that received
the collection. In these instances, the Medicare contractor receiving the collection would initiate the process
by completing the Collection Reconciliation/Acknowledgement Form and sending it to the CMS RO who is
reporting the receivable to notify them of the collection. The Medicare contractor that received the collection
would deposit any cash or checks received into unapplied receipts, which would be reported as a liability
until the transfer is complete.
In turn, the CMS RO reporting the receivable will complete the Transfer Request and Notification of
Acceptance Form (TRNA) described in §1960.17 of the MIM and §4960.10 of the MCM. (The use of the
TRNA is also discussed in question number 68.) Once both parties sign the TRNA, the transfer is considered
complete and the collection would then be applied to the account receivable. The CMS RO transferring the
receivable would record the account receivable on Line 5c, Transfer Out to other Medicare Contractors. The
Medicare contractor receiving the account receivable would record it on Line 5d/5f, Transfers In from other
CMS Locations POR/PSOR or Not on POR/PSOR and the applicable collection on either Line 4a,
Cash/Check Collections or Line 4b, Offset Collections.
Only in the instance where a collection is made by offset for an account receivable at a CMS RO location
can notification of the offset be e-mailed. The e-mail must be retained for audit trail purposes. The e-mail
notification must be followed-up with the actual Collection Reconciliation/Acknowledgement Form and the
Transfer Request and Notification of Acceptance form with all the appropriate signatures. Furthermore,
since offsets may only be identified after being applied, the offset transaction must be moved manually on
the Forms CMS-751A/B (i.e., the full amount of the accounts receivable prior to the offset must be shown as
a transfer in and the amount of the offset must be captured on Line 4b, Offset Collection.) To assist in
accounting for these offset transactions ONLY, Medicare contractors can prepare the Collection
Reconciliation/Acknowledgement Form(s) on a monthly basis.
Treatment of Collections Made by A Medicare Contractor for an Account Receivable at CO
Non-MSP: If Medicare contractors receive collections on debt that is at the Debt Collection Center (DCC),
and that debt is being reported by CO, the Medicare contractor must notify the CO by submitting the
Collection Reconciliation/Acknowledgement form (refer to §1960.18 of the MIM and §4960.11 of the
MCM). In addition, the receipt should be deposited into unapplied receipts until the actual account
receivable is transferred back to the Medicare contractor.
Once CO receives the Collection Reconciliation/Acknowledgement form, it will perform the necessary steps
to update the collection information in the Debt Collection System (DCS) and the Provider Overpayment
Reporting (POR) system or the Physician/Supplier Overpayment Reporting (PSOR) system. CO will change
the accounts receivable location code in DCS from "H," which means CO is reporting the account receivable
to "C," which means the Medicare contractor is reporting the account receivable. CO will also update the
POR/PSOR with the appropriate location code of "IDC," which means the fiscal intermediary at debt
collection or "CDC," which means the carrier at debt collection (i.e., the debt has been forwarded to debt
collection but the debt is still on the books of the fiscal intermediary or carrier). If a balance is remaining
after posting the collection, the debt will remain at DCC for cross servicing/TOP.
To allow the Medicare contractors to properly apply the collection in their internal systems, CO will then
transfer the receivable back to the Medicare contractor using the TRNA (refer to §1960.17 of the MIM and
§4960.10 of the MCM). Upon CO receiving the signed TRNA from the Medicare contractor, CO will cease
to report the receivable on its Form CMS-R751A/B. Once the TRNA has been signed and the receivable has
been transferred, the Medicare contractor will record the transfer in of the receivable on Line 5d, Transfers
In from other CMS Locations, POR/PSOR, or Line 5f, Transfers In from other CMS Locations, Not
POR/PSOR. The receipt would then be applied to the account receivable and the collection would be
recorded on Line 4a, Cash/Check Collections or Line 4b, Offset Collection on the appropriate Form CMS-
H751A/B.
MSP: If Medicare contractor X has an account receivable other than a debt which has been referred to the
Department of Health and Human Services (DHHS) Program Support Center (PSC) under the DCIA and the
CO/RO receives payment, the Medicare contractor should use Line 4c, Collections Deposited at Another
Location and footnote in the comments section of the Form CMS-M751A/B that the CO/RO received the
payment. An example of this type of receipt would be coordination of benefits contractor misrouted checks.
Usage of the Collection Reconciliation/Acknowledgement Form
In the instance where a Medicare contractor, RO or CO receives a collection (whether cash, checks, offset or
EFT) the entity receiving the collection must complete lines 1 through 10 of the form and attach all
documentation showing the collection and the re-issued check, if applicable. In the instance where a RO
receives cash/checks and does not maintain a Medicare bank account to deposit the funds received, the RO
must complete lines 1 through 10 of the form and attach the cash/check. This form should be forwarded to
the reporting entity no later than (15) fifteen days before the end of the quarter. The entity receiving the form
and the check must sign the form on line 11 and forward a copy of the form to the official who signed line
10, no later than (15) fifteen days after receipt of the form. This will acknowledge the receipt of the form
and the check.
Collection Reconciliation/Acknowledgement Form
1. Location of A/R_________________________(i.e., Medicare contractor, RO, or CO)
2. Location of the Collection _________________(i.e., Medicare contractor, RO, or CO. If RO
Collection, indicate such even though actual deposit is made at Central Office)
3. Region_________ Medicare contractor Name and Number_________________________
4. Non-MSP Accounts Receivable
Provider/Physician/Supplier) Number_______________
Provider/Physician/Supplier Name__________________________________
Provider/Physician/Supplier Name__________________________________
Overpayment Determination Date__________________
Claim Number_________________
Cost Report Year ___________________
MSP Accounts Receivable
Debtor Name ______________________________________
HIC # / Report ID___________________________________
Determination Date__________________
Beneficiary Name ___________________________________
5. Was debt in CNC status prior to this collection:__________________(Yes/No)
6. Date of Collection (Postmark or Government Collection date)______________
7. Type of Collection ____________________ (i.e., cash/check or offset)
Check Number or Government Collection Number _____________________________
Amount of Collection $__________________
Amount Applied to Principal $__________________
Amount Applied to Interest $__________________
8. Collection Reported in quarter ending__________________
9. A/R Reported in quarter ending_______________________
_____________________________
_____________________________
10. Signature of Official at Location
Where Collection is Reported
11. Signature of Official at Location Where
Reduction of A/R is Recorded
Phone #________________________
Fax #__________________________
Phone #________________________
Fax #__________________________
400.20 - Exhibit 20 - Procedures for Reporting Currently Not Collectible (CNC) Debt
(Rev. 18, 05-02-03)
(Rev. 315, Issued: 05-17-19, Effective: 06-18- 19, Implementation: 06-18-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare
identification number. For purposes of this manual, Medicare beneficiary identifier references both the
Health Insurance Claim Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new
Medicare card transition period and after for certain business areas that will continue to use the HICN as
part of their processes.
A1-1960.19, A1-1960.20, B1-4960.12, B1-4960.13
As part of its effort to improve financial reporting, CMS has implemented the category of currently not
collectible (CNC) for delinquent debt that is unlikely to be collected within a reasonable time frame. The
CMS' CNC policy provides that CNC debt will not be recognized as an active accounts receivable (A/R) for
financial statement reporting purposes because to do so would overstate the true economic value of the
assets on the financial statements. While CNC debts are not A/R reported on the financial statements,
Medicare contractors must continue appropriate recovery efforts for these debts until they are recommended
and approved by CMS for "write-off - closed" as such, these debts must remain in their internal system for
interest accrual and offset. The CNC process permits and requires the use of tools of the Debt Collection
Improvement Act (DCIA) of 1996. By using these tools delinquent debt will be worked until the end of its
statutory collection life cycle.
Criteria for Selection
All A/R, whether it is classified as Medicare Secondary Payer (MSP) or Non-MSP, that are 180 days
delinquent must be recommended for CNC reclassification. The A/R must be 180 days delinquent (i.e., 240
days old if the repayment time frame is 60 days or 210 days old if the repayment time frame is 30 days) as
of the last day of the quarter prior to the quarter in which the CNC recommendation is submitted for RO
approval.
All MSP A/R means all demanded debt, without regard to whether the debt is Group Health Plan (GHP)
based or liability/no-fault/workers' compensation based and without regard to the type of debtor (employer,
insurer, beneficiary, provider/supplier, etc.). Where the MSP recovery demand letter stated that the debt was
due and payable 30 days from the date of the demand, the debt is delinquent on day 31 if it has not been paid
in full or there is no valid documented defense for the unpaid amount. Where the MSP recovery demand
letter stated that the debt was due and payable 60 days from the date of the demand, the debt is delinquent on
day 61 if it has not been paid in full or there is no valid documented defense for the unpaid amount.
All Non-MSP A/R means all demanded debt without regard to whether the debt is
provider/physician/supplier or beneficiary-based. This includes debts that are not normally reported
(separately or in summary entries) in the POR/PSOR systems, as long as they meet the CNC criteria. These
debts should be listed separately, must be identified as not on the POR/PSOR, and the type of debt must be
listed on the CNC request form in the comments section. Debts that are excluded from this definition are as
follows:
• Debts with a principal balance of less than $25. Although these debts may satisfy the CNC criteria,
Medicare contractors should recommend the termination of collection activity and request approval
by the Regional Office (RO) to write this debt off as "write-off closed" in accordance with Title 42
of the Code of Federal Regulations, Section 405.376(e)(3), since the cost of further collection action
is likely to exceed any recovery.
• Debts with a collection within the last 180 days. Hence, the debt must be 180 days delinquent
without any collection/recoupment activity within the last 180 day time period for CNC
reclassification.
Additionally, all accounts receivable that meet the CNC criteria will be reclassified as CNC without regard
to whether or not the debt is in bankruptcy, under fraud and abuse investigation, has an appeal pending at
any level, is in litigation/negotiation, or is for a deceased debtor. However, if a Medicare contractor believes
that a particular A/R meets the criteria for both "write-off - closed" and CNC, the A/R should be
recommended for "write-off - closed." Medicare contractors may not recommend CNC for less than the full
amount of an outstanding debt.
NOTE: For GHP-based MSP A/R where the demand was issued to the employer, insurer, or third party
administrator, GHP, or other plan sponsor, the debt includes all of the claims in a demand to a debtor for a
particular beneficiary. For GHP Data Match (DM) recoveries, this would be all of the claims associated with
a particular Mistaken Payment and Recovery Tracking System (MPaRTS) Report ID although a single cover
letter might have been issued for multiple beneficiaries' Medicare reimbursed claims. For duplicate primary
payment recovery demands to a provider/supplier (including physician), the debt includes all claims in the
recovery demand regardless of the number of beneficiaries involved. For liability, no-fault, or workers'
compensation, the debt includes all claims in the recovery demand.
A debt's eligibility for DCIA referral to a Department of the Treasury designated Debt Collection Center
(DCC) for further collection efforts, including the Treasury Offset Program (TOP) has no bearing on or
relationship to whether or not the debt should be reclassified as CNC. As such, debts referred to the DCC
should also be recommended for CNC reclassification as long as it meets the CNC criteria.
The Department of the Treasury and the Office of Management and Budget require that Agencies submit
reports to them on financial management and performance data so that debt collection programs and policies
can be evaluated. Thus, CMS is requiring its Medicare contractors to report and monitor CNC debt on a
quarterly basis.
Quarterly Review of Debt for CNC Reclassification & Approval
Medicare contractors must continuously review all debt and quarterly request approval to reclassify debts as
CNC. Recommendations for the approval of MSP and Non-MSP CNC should be sent to your RO MSP
Coordinator or the RO Debt Collection staff respectively. These reports should be sent by hard copy
accompanied with a disk no later than the first day of the second month of each quarter (i.e., November 1,
February 1, May 1, and August 1). The CFO of Medicare Operations must sign the hard copy and include a
preprinted address label with the hard copy for the return of the approved CNC recommendations. Medicare
contractors are required to submit negative reports if there are no debts eligible for CNC for a particular
quarter.
ROs are responsible for approval or denial of all recommendations for CNC based upon the criteria set forth
in these instructions. RO approval will be by the Assistant Regional Administrator (ARA) for Financial
Management. ROs will complete their review of the Medicare contractors' recommended CNC and return
their approval or denial of such reclassifications by the first day of the last month of each quarter (i.e.,
December 1, March 1, June 1, and September 1). ROs may return a hard copy via fax or a soft copy via disk
annotated to show approval or denial by the RO ARA for Financial Management, in order to meet the
required time frame for approval, but this must be followed by a hard copy that was signed and dated by the
ARA for Financial Management. ROs will also send copies of the signed RO approval or denial letter only,
each quarter to CMS CO to the attention of the Director, Division of Financial Oversight, Office of
Financial Management (for both MSP and Non-MSP approvals). The ROs must maintain the detailed
reports that support the amounts approved/disapproved.
The CNC action should not be taken nor should any changes be made to the A/R on any internal systems
(Medicare contractor systems or other systems which Medicare contractors have responsibility for updating)
for CNC until the recommendation for CNC has been processed by CMS, approved in writing, and returned
to the Medicare contractor. The listing of approved CNC will be returned to the contractors by the ROs.
Receipt of this approval authorizes the Medicare contractor to reclassify the A/R, and update the A/R and
associated case in all appropriate systems. When the A/R is reclassified as CNC, the associated case file
must be annotated to show that a particular A/R was reclassified as CNC and the date/quarter of the action.
Reclassification as CNC does not close the associated case.
If a full or partial collection for the A/R is received between request and approval of CNC reclassification,
then the collection should be applied. The contractor must make the necessary adjustment to the debt to
reflect the payment and place the remaining amount, if any, in CNC when the RO approval is received.
However, when the approval is received, the contractor must then notify the RO of the change in the amount
originally approved for CNC as well as the reason why. If the contractor has this issue with multiple debts
recommended for CNC, they need to furnish this information to the RO on a debt specific basis, not just on
an aggregated basis. This must be communicated to the RO contact in writing. In addition, this
documentation should be maintained for audit/review purposes.
NOTE: MPaRTS does not need to be updated for Data Match debt when the MSP A/R is reclassified as
CNC.
The CMS approval of A/R reclassified as CNC must be retained and available upon request (from the Office
of the Inspector General or any other internal or external review organization) in accordance with retention
procedures in the Medicare Intermediary and Carrier Manuals. This CMS approval must also be annotated
by the Medicare contractor to indicate the date/quarter when the A/R was reclassified.
Data Requirements and Format for Recommendations for MSP CNC
MSP A/R recommended for CNC requires the submission of the following information to the Medicare
contractor's RO MSP coordinator: (see Attachment I for the recommended format)
• Medicare Contractor Name and Number
• Medicare Contractor Mailing Address
• Medicare Contractor Contact Person/Phone/Fax/E-mail
• Type of MSP Debt [GHP or non-GHP (this includes liability, no-fault, and workers' compensation)]
• Beneficiary Medicare beneficiary identifier
• Beneficiary Name
• Name of Debtor or Insurer for GHP-based debts where the current debtor is the
insurer/employer/third party administrator/GHP/other plan sponsor
• Type of Debtor [A=insurer/employer/third party administrator/GHP/other plan sponsor;
B=provider/supplier (including physicians); C=beneficiary, D=other (must specify)]
• Date of Initial Recovery Demand Letter to current debtor
• Delinquency Date
• Original A/R Amount for the current debtor
• Existing A/R Amount (principal and interest listed separately, as well as a total amount for principal
plus interest; HI/SMI must also be listed and reported separately)
• Date of Last Payment, Collection, Recoupment, Offset, or Adjustment Activity (provide date or
"none")
• Tax Identification Number (TIN) for debtor. The TIN is the Employer Identification Number (EIN)
or Social Security Number (SSN)
• DCS Status Code (if applicable).
NOTE: The debtor is the individual or entity to whom the last recovery demand was issued. Where the
demand was issued to an individual in their capacity as legal counsel or representative of any type, the
debtor is the beneficiary, provider/supplier (including physician), or other individual or entity being
represented. Where recovery is being pursued from the attorney or other representative in their own right,
the debtor is the attorney or other representative.
The above listed data elements are mandatory for CNC for all MSP A/R established October 1, 2000 or
later. It is also mandatory for all MSP A/R with a recovery demand date of October 1, 2000, or later,
regardless of when the MSP A/R was established. For CNC recommendations for MSP A/R established
prior to October 1, 2000, Medicare contractors may submit recommendations without the following data
elements if the CNC recommendation certifies that these data elements are not readily available: Beneficiary
name and Medicare beneficiary identifier where the beneficiary is not the debtor; Insurer name where the
insurer is not the debtor; and Type of debtor.
If a Medicare contractor has bulk MSP A/R on the GTE system for older Data Match and non-Data Match
GHP debt, the contractor - for these MSP A/R only - must: 1) Identify the A/R as a bulk receivable on the
GTE system, 2) Identify the insurer, 3) Identify the date of the demand, and 4) Identify the associated dollar
amounts for principal and interest. Any contractor who created bulk receivables for GHP-based MSP debt
using any system other than GTE must contact their RO for assistance. The RO will, in turn, discuss the
issue with CO.
Data Requirements and Format for Recommendations for Non-MSP CNC
Non-MSP A/R recommended for CNC require the submission of the following information to the Medicare
contractor's RO Debt Collection contact: (see Attachments II & III for the recommended format)
• Medicare Contractor Name and Number
• Medicare Contractor Mailing Address
• Medicare Contractor Contact Person/Phone/Fax
• Provider/Physician/Supplier/Beneficiary Name and Number (if applicable)
• Claim Number (PSOR)
• Claim Paid Date (PSOR) or Cost Report Date (POR)
• Overpayment Determination Date
• POR/PSOR Status Code
• Overpayment Type
• Original Amount of Debt
• Balance Outstanding (principal and accrued interest listed separately)
• Date Interest Accrued Through
• Date of Last Payment, Offset or Recoupment
• POR/PSOR Balance (principal and interest listed separately for POR; for PSOR, principal balance
only) - For Part A, indicate POR balance if Contractor submits request for Part B of A separately
• POR/PSOR Location Code
• DCS Status Code (if applicable)
• For FIs Only - Part B of A debt can be submitted on the same listing (principal and interest)
Each listing must contain a written certification that all of the required criteria for CNC are met. The CFO of
Medicare Operations must sign CNC recommendations. The CFO's signature constitutes his/her certification
to all information/statements contained in the recommendation.
Financial Reporting and Reconciliation of CNC Debts
Debts that have received approval for CNC reclassification must be reported in the following manner:
• On Form CMS-751A/B or CMS-M751A/B the amount reclassified as CNC, including principal and
interest, will be recorded on Line 6c, Transfers Out to CNC with a corresponding entry on Line 2,
New CNC Debt on Form CMS-C751A/B or CMS-MC751A/B. This will reduce the ending balance
reflected on the applicable form.
• Debts that are reclassified as CNC may still be collected. If a collection occurs, the following actions
should take place: (1) On Form CMS-C751A/B or CMS-MC751A/B an adjustment for the amount of
the collection should be recorded on Line 4a, Reclassified as Active A/R Due to Collection of Cash
or Line 4b, Reclassified as Active A/R Due to Collection by Offset; (2) The amount of the collection
should also be included in Section C - Collection Information of Form CMS-C751A/B or CMS-
MC751A/B; and (3) The amount of the collection should be simultaneously recorded on Line 6b,
Transfers in from CNC and Line 4a, Cash/Check Collections or Line 4b, Offset Collections of Form
CMS-751A/B or CMS-M751A/B. As such, if a collection takes place, only the collection would be
reclassified with the collection being applied against interest first, then principal. If the collection
does not satisfy the entire debt, the remaining balance of that debt would remain in CNC.
Medicare contractors must continue to accrue interest for debt that has been reclassified as CNC.
Additionally, CMS recognizes that for those systems where interest is updated automatically, the interest
submitted with a recommendation for CNC may differ from the interest shown in the Medicare contractor's
system at the time the Medicare contractor receives approval for CNC. The CMS approval of the principal
and interest recommended for CNC is sufficient support for the subsequent reclassification, including any
increase in the interest, as long as the principal remains the same. Any additional interest that accrues prior
to CNC reclassification would be reported on Form CMS-751A/B or CMS-M751A/B on Line 3, Interest
Earned. Then the debt would be reclassified to the appropriate form.
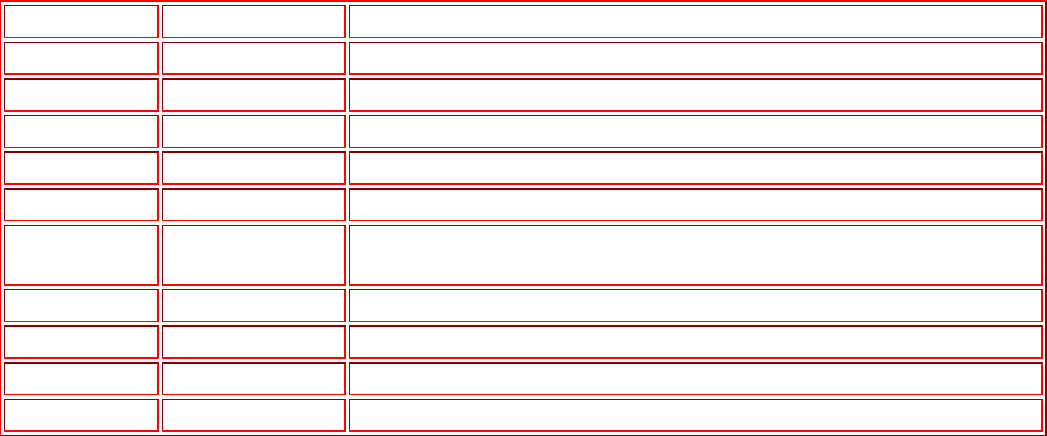
Medicare contractor systems must be able to maintain transaction level detail of debt that has been
reclassified as CNC to enable future collection activities and to maintain a proper audit trail.
Regional Offices will ensure that amounts approved as CNC are properly reported on contractor Forms
CMS-751A/B or CMS-M751A/B and CMS-C751A/B or CMS-MC751A/B.
Systems Update - Non-MSP Only
Medicare Contractor Internal Systems and POR/PSOR System:
Contractors are responsible for the timely update of CNC status in the POR/ PSOR systems and internal
systems. A CNC date field has been added in the POR/PSOR and additional status codes have been
developed. The date of CNC approval (i.e., the date of the cover letter signed by the ARA) must be entered
in the CNC date field. The update must be performed within ten calendar days of receiving the CNC
approval. Do not change the location code of the debt. Regional Offices will monitor the POR/PSOR
systems to ensure contractor compliance.
Additional Status Codes for POR/PSOR:
POR Codes
PSOR Codes
Code Description
01
1
CNC
02
2
Write-off Closed (disabled effective 2/6/02)
03
3
CNC - DCIA Letter Sent
04
4
Reactivate - Bankruptcy (will no longer be used)
05
5
Reactivate - Payment Received
06
6
Reactivate - Appeal/Litigation/Fraud & Abuse Investigation (will no
longer be used)
07
7
Reactivate - Compromise
08
8
Reactivate - Extended Repayment Agreement
09
9
CNC Debt - Written-off Closed
00
0
Reactivate - Other
NOTE: For debts that are at the DCC location and reclassified to CNC, the "3" (POR) or "03" (PSOR)
status code would be used. Furthermore, the "9" must be accompanied by a valid closed date. Cases with a
status code of "09" (POR) or "9" (PSOR) and a valid closed date will be rolled to the history file at the end
of the quarter. In addition to updating the POR/PSOR with the appropriate status codes for the reactivation,
the CNC date previously inputted should be removed. Updating the CNC Date field in the PSOR requires
the user to enter zeroes in the CNC Date field and pressing the enter key.
Debt Collection System (DCS)
The CMS' CO Division of Financial Reporting and Debt Referral staff will continue to update the Debt
Collection System (DCS) with approved CNC status for debts that have been referred for Cross
Servicing/TOP.
Additional Considerations for MSP A/R
These instructions only apply to established MSP A/R. They may not be used to close MSP liability/no-
fault/workers' compensation leads where no settlement, judgment or award exists and no recovery demand
has been issued.
Some Medicare contractors may still have old MSP-based provider/supplier (including physician) debt or
MSP-based beneficiary debt which has not been reported on their Form CMS-M751A/B and which has been
referred to the RO under non-MSP rules or otherwise treated as a non-MSP receivable. Old MSP-based debt
that has been treated as non-MSP debt (that is tracked and processed under non-MSP rules) should be
treated as non-MSP debt for CNC purposes as well.
Medicare contractors may only recommend CNC for a MSP A/R that is being reported as part of their
ending MSP A/R balance. MSP A/R that have been transferred to the ROs for referral to other agencies or
entities such as, the Department of Justice or Office of General Counsel will be addressed by the ROs. CO
will address MSP A/R with CO locations. MSP A/R that have been referred to another location, without
transfer, remain the responsibility of the Medicare contractor.
Previously some Medicare contractors processed/tracked MSP-based provider/supplier (including physician)
A/R and/or MSP-based beneficiary A/R as non-MSP A/R and did not include such A/R on their Form CMS-
M751A/B report. Medicare contractors may no longer do this for new MSP A/R. Any pre-existing MSP-
based provider/supplier (including physician) A/R and/or MSP-based beneficiary A/R that are not reflected
in the Medicare contractor's Form CMS-M751A/B report may not be recommended for MSP CNC. Pre-
existing MSP-based provider/supplier (including physician) A/R and/or MSP- based beneficiary A/R that
have been tracked/processed, or otherwise treated as non-MSP debt should follow the rules for non-MP
CNC
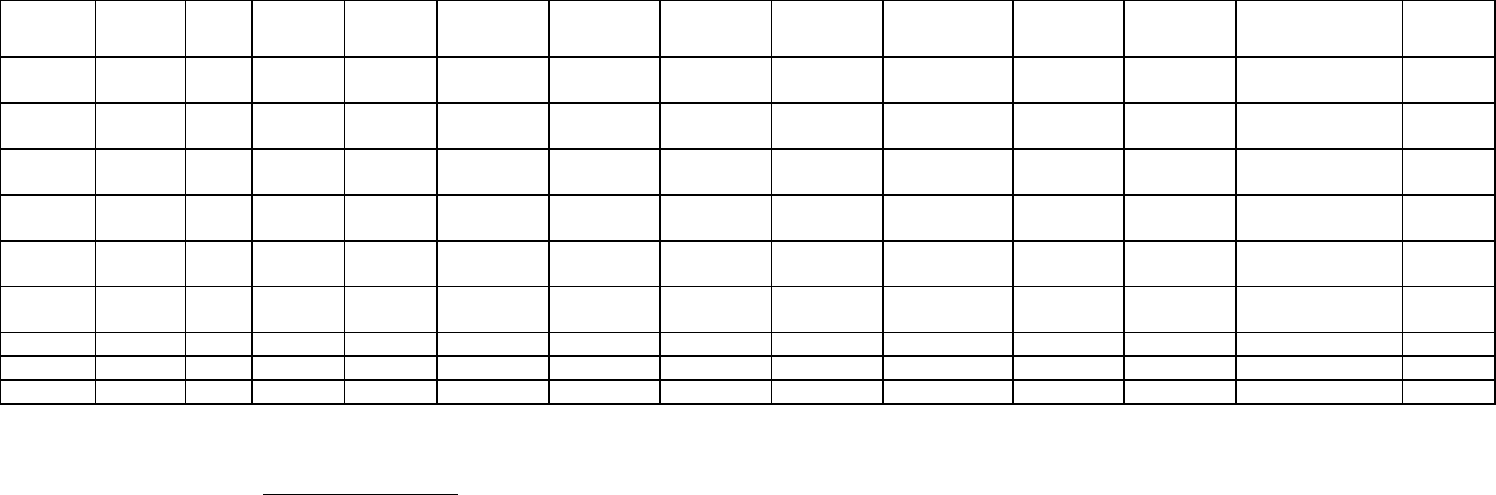
Exhibit 20 - Attachment I
MSP Accounts Receivable: Contractor Recommendation for Reclassification as CNC
Medicare Contractor Name and Number:
Medicare Contractor Contact Person/Phone/Fax/E-mail Address:
Medicare Contractor Mailing Address:
Part A-HI, or Part B-SMI - as applicable (show which)
Intermediaries report Part A and/or Part B
Carriers report Part B only
Type of MSP
Debt
Bene.
Medicare
beneficiary
identifier
Bene.
Name
Debtor
Name
Debtor Type
Date of
Initial
Demand
Original
AR
Amount
Current
Principal
Balance
(HI)
Current
Interest
Balance
(HI)
Current
Principal
Balance
(SMI)
Current
Interest
Balance
(SMI)
Total
Principal
and
Interest
Date of Last
Payment,
Offset, Recoup.
Or Adjustment
TIN of
Current
Debtor
(Provide totals for each column if applicable)
CFO of Medicare Operations: (signature required)
(Signature constitutes certification that all CMS specified criteria for CNC reclassification are met.)
Associate Regional Administrator/Division of Financial Management: (signature required) ___ Concur ___NonConcur
Date of Referral to RO : ___________
Date of RO decision: ___________
Date/quarter when approved MSP A/R were reclassified as CNC: ___________
Attachment II
This is an exact duplicate of Attachment 1, "MSP Accounts Receivable: Contractor
Recommendation for Reclassification as CNC" for Part B Intermediary Claim Activity.
The heading at the top of the spreadsheet is "Part B of A" - SMI, instead of "Part A - HI."
Intermediaries report their SMI data on this report.
400.21 - Exhibit 21 - CMS Policy for Recognizing Accounts Receivable -
(Rev. 5, 08-30-02)
A1-1960.21, B1-4960.21
CMS Policy for Recognizing Accounts Receivable
Overview
The majority of the Medicare accounts receivable balances reported by CMS in its
financial statements are comprised of overpayments made to providers, physicians,
suppliers, beneficiaries, insurers, employers and other entities. The primary responsibility
for identifying, recording, collecting, and reporting overpayments lies with CMS's
Medicare contractors. CMS defines an "overpayment" as Medicare funds that a provider,
physician/supplier, beneficiary, insurer, employer, or other entity has received in excess
of amounts due and payable under the Medicare statute and regulations. Once a
determination of an overpayment has been made, the amount so determined is a debt that
is owed to the Medicare program. For financial reporting purposes, this overpayment or
debt must be recognized as an accounts receivable and reported as an asset in CMS's
financial statements.
CMS has adopted the financial reporting definition for the recognition of an accounts
receivable set forth by the Federal Accounting Standards Advisory Board (FASAB). The
FASAB recommends generally accepted accounting standards and principles for the
Federal Government. The FASAB sets these standards and principles so that Federal
agencies' financial reports include understandable, relevant, and reliable information
about the financial position, activities, and results of operations of the United States
government and its component units.
According to the FASAB's Statement on Federal Financial Accounting Standard Number
1 (SFFAS No.1), Accounting for Selected Assets and Liabilities,
"Accounts receivables are amounts that an entity claims for payment
from others. They arise from claims to cash or other assets."
Additionally, the FASAB recommends, "A receivable should be
recognized when a Federal entity establishes a claim to cash or other
assets against other entities, either based on legal provisions, such as a
payment due date (e.g., taxes not received by the date they are due), or
goods or services provided. If the exact amount is unknown, a
reasonable estimate should be made."
For financial reporting purposes, recognition means the process of formally recording an
item into the financial statements of an entity as an asset, liability, revenue, expense, or
the like. In the case of Medicare contractors, recognition would equate to recording the
accounts receivable on Form CMS-H750A/B and Form CMS-H751A/B Contractor
Financial Reports.
Recognition Policy
CMS and its Medicare contractors will recognize and report an accounts receivable as of
the date a demand letter is sent to the debtor. Specifically, contractors will recognize and
record an accounts receivable (Non-Medicare Secondary Payer (MSP) and MSP
overpayments) as of the date of the demand letter on Line 2a, New Receivables of Form
CMS-H751A/B Status of Accounts Receivable Report. The act of sending out the
demand letter is the event that triggers the recognition of an accounts receivable. The
purpose of the demand letter is to notify the debtor of the existence of the overpayment,
and to request payment. Chapter 4, Debt Collection, §§10 and 130 outline the language
and information that, at a minimum, a demand letter must contain. A demand letter must
contain the name and address of the debtor, the amount of the overpayment, terms of how
interest will be assessed, date when repayment is due, and the debtor's rights to appeal.
All these items are consistent with the definition recommended by the FASAB as
outlined above.
It is important for Medicare contractors to ensure that they retain copies of a demand
letter(s) sent. The demand letter provides documentation or evidence of the actual debt
and recovery efforts taken. It must be kept in each case file with other associated case
documents or correspondence if the case is referred to the Department of Justice; referred
for debt cross-servicing; requested by CMS, Office of Inspector General (OIG) or
General Accounting Office (GAO) during audits/reviews. This information is necessary
and needed to support the debt.
Unless otherwise specifically noted, this policy is applicable to both non-MSP and MSP
overpayments. The following are specific circumstances where application of this policy
will not apply, i.e., when an accounts receivable would be recognized even though a
demand letter has not been issued or, vice versa, where sending a demand letter would
not necessarily require the recognition of an accounts receivable.
• Accounts Receivables Due to Unfiled Cost Reports; and
• Consent Settlement Agreements.
These two circumstances are not all inclusive. If there is a specific situation that is not
described above, Medicare contractors should consult CMS for further guidance.
Accounts Receivable Due to Unfiled Cost Reports
Through analysis of Federal financial accounting standards and regulations, CMS
believes that recognition of a receivable prior to the filing of a cost report significantly
overstates net assets and ultimately net position. Furthermore, CMS believes that current
accounting procedures for recognizing accounts receivables due to a provider's failure to
file a cost report timely does not adhere to the accounting principles articulated in
Statement of Federal Financial Accounting Standards Number (SFFAS No.) 1 -
Accounting for Selected Assets and Liabilities, SFFAS No. 5 - Accounting for Liabilities
of the Federal Government, and SFFAS No. 7 - Nonexchange Revenue (Measurement &
Recognition), as well as Generally Accepted Accounting Principles (GAAP) of
conservatism and matching. Based on this analysis, the failure to file a cost report does
not complete the earnings process, and accordingly, no accounting event has occurred. As
such, the recognition of a receivable prior to the completion of the earnings process
(receipt or filing of a cost report) is poor matching. In addition, SFFAS Nos. 5 and 7
states that liabilities and nonexchange revenue should only be recognized when a past
event or exchange transaction has occurred, use of resources (inflow or outflow) are
probable and can be reasonably estimated or measured. Without the actual submission of
the cost report, CMS cannot reasonably estimate the amount of the receivable, as required
by SFFAS No. 1.
Therefore, unfiled cost report receivables will no longer be reported on the Form CMS-
H;750 Contractor Financial Report and Form CMS-H751, Status of Accounts Receivable
Report. CMS's current financial reporting instructions require Medicare fiscal
intermediaries to place providers who have not filed a timely cost report on 100 percent
penalty withhold, and recognize and demand a receivable based on the value of all
interim payments made to the provider in, and subsequent to, the cost reporting period,
without considering the value of actual services performed during that period. Federal
debt collection regulations allow CMS to demand repayment of the full amount paid to a
provider during a cost reporting period if a provider fails to comply with the requirements
to file a cost report in a timely manner. However, for financial reporting purposes, CMS
recognizes that the entire amount being demanded does not truly represent funds owed to
CMS. Since the provider has performed services, the true economic value of the
receivable demanded is overstated. In fact, CMS may have a liability upon settlement.
Cost report receivables should not be accrued until related cost reports are received, and
CMS can support the existence of a receivable through provider agreement, such as filing
a cost report, filing a cost report without sufficient payment, or a court ruling in favor of
CMS.
As a result, for financial reporting purposes, CMS is revising its policy for reporting
unfiled cost reports as an accounts receivable, unless the fiscal intermediary is aware of a
unique situation where recording an accounts receivable would be appropriate. Fiscal
intermediaries will continue to reflect an overpayment on the Provider Overpayment
Reporting (POR) system based on the value of all interim payments made to the provider
in, and subsequent to, the cost reporting period.
However, effective for the March 31, 2001 reporting period, accounts receivable for
unfiled cost reports will no longer be reported on Form CMS-H750 and Form CMS-
H751. CMS will continue to monitor and manage the status of unfiled cost reports
through the POR system, without overstating accounts receivable on the financial
statements. All other processes related to unfiled cost reports remain unchanged. Fiscal
intermediaries must continue to: (1) Place the providers on 100 percent penalty withhold,
(2) Demand the submission of delinquent cost reports from providers based on current
debt collection regulations, and (3) Refer the debt in accordance with the requirements of
the Debt Collection Improvement Act of 1996.
Fiscal intermediaries must ensure that Line 7, Ending Balance, of Form CMS-H751 does
not include any receivables due to unfiled cost reports. If accounts receivables due to
unfiled cost reports were included in the December 31, 2000 Form CMS-H751, these
receivables must be zeroed out by recording a downward adjustment for these amounts
on Line 5a, Reclassified/Adjustments, on Form CMS-H751 and provide a specific
footnote in the remarks section of the report identifying the nature and amount of the
adjustment.
Consent Settlement Agreements Resulting from Comprehensive Medical Reviews
(CMRs)
Typically, postpayment reviews of claims are conducted for a specified
provider/physician/supplier or group in order to evaluate their billing patterns over a
selected period of time. CMRs are performed to determine whether a suspected
provider/physician/supplier or groups are providing noncovered or medically unnecessary
services. A CMR is a thorough analysis of a sample of processed claims and all pertinent
data (such as medical record, beneficiary payment history, etc.) for selected
providers/physicians/suppliers for a specified time period. CMRs are usually targeted to
providers/physicians/suppliers who have demonstrated aberrant billing and/or practice
patterns.
If a CMR determines that an incorrect amount of money has been paid to the
provider/physician/supplier, the contractor must assess an overpayment based on
instructions outlined in the contractor manuals. Per Chapter 3, Overpayments, there are
three different types of overpayments that result from a CMR: Actual overpayment,
projected overpayment, and limited projected overpayment. The type of sample used
during a CMR determines how Medicare contractors are to assess and demand money
back from the provider or physician/supplier who was overpaid.
An actual overpayment is, for the actual claims reviewed, the sum of the payments (based
on the amount paid to the provider/physician/supplier and Medicare approved amounts)
made to a provider/physician/supplier for services which were determined to be not
medically necessary or incorrectly billed. If an actual overpayment is assessed, Medicare
contractors must send a demand letter for the amount of the actual overpayment and
recognize an accounts receivable on Line 2a, New Receivables, of Form CMS-H751.
A projected overpayment is defined as the numeric overpayment obtained by projecting
an overpayment from a statistically valid random sample (SVRS) to all similar claims in
the universe under review. Medicare contractors must notify the provider or
physician/supplier of the overpayment, and refer the case to the Medicare contractor's
overpayment staff to demand and collect the overpayment. Medicare contractors must
send a demand letter for the amount of the projected overpayment and recognize an
accounts receivable on Line 2a, New Receivables, of Form CMS-H751.
A limited projected overpayment is the numeric overpayment obtained by projecting an
overpayment from a limited sample or limited SVRS subsample to all similar claims in
the universe under review. If this type of overpayment is assessed, Medicare contractors
have three overpayment assessment options. The Medicare contractor can assess an
actual overpayment; a projected overpayment based on a SVRS by performing an
expanded CMR; or can offer the provider or physician/supplier a consent settlement
based on the potential projected overpayment amount. Again, if an actual or project
overpayment is assessed, Medicare contractors must send a demand letter, and recognize
an accounts receivable on Line 2a, New Receivables, of Form CMS-H751.
If a consent settlement is offered to the debtor, the consent settlement document must
carefully explain what rights a debtor waives by accepting the consent settlement. It must
contain a binding statement that a debtor agrees to waive any rights to appeal the decision
regarding the potential overpayment determination. If this option is used, the Medicare
contractors must not recognize an account receivable until a consent settlement is signed
and agreed to by the debtor and CMS.
400.22 - Exhibit 22 - Accounts Receivable Trending Analysis Procedures
(Rev. 120, Issued: 04-27-07; Effective: 07-01-07; Implementation: 07-02-07)
The Centers for Medicare & Medicaid Services (CMS) utilizes contractors to manage and
administer the fee-for-service portion of the Medicare program. Medicare contractor
financial reports provide a method of reporting financial activities by the contractors as
required by the Chief Financial Officers (CFO) Act of 1990. The Medicare contractors
are required to maintain accounting records in accordance with federal government
accounting principles and applicable government laws and regulations and are required to
use double entry bookkeeping and accrual basis accounting. The due date for Medicare
contractors using the Healthcare Intergraded General Ledger Accounting System
(HIGLAS) Financial Statements, is seven calendar days after the close of the period and
twenty-one calendar days for Medicare contractors using the Contractor Administrative
and Financial Management (CAFM) system. If the date occurs on a holiday or a
weekend, the report is due the following Federal workday. These dates are subject to
change during the accelerated reporting periods. The major financial reports in HIGLAS
are the Balance Sheet, the Income Statement, Summary 2 Trial Balance, and the CMS
Report on Receivables Due From the Public (CMS TROR). The financial reports in
CAFM consist of the Statement of Financial Position (Form CMS-750) and Status of
Accounts Receivable (Form CMS-751). The system accumulates and reports by fund, as
there are separate reports for Part A Hospital Insurance (HI) trust fund, Part B
Supplementary Medical Insurance (SMI) trust fund, and the general fund (Interest). The
accounts receivable activity is reported for the fiscal year-to-date for the period of the
report. These reports include Accounts Receivable (AR) activity for Medicare Secondary
Payer (MSP) and non Medicare Secondary Payer (non-MSP) accounts.
Accounts receivable represent amounts owed by health care providers, insurers, third
party administrators, beneficiaries, employers, and other government agencies. Medicare
accounts receivable is comprised of various components with the balance derived from
MSP and non-MSP receivables, as well as miscellaneous amounts owed the program
from various sources. The Financial Statements include receivable balances consisting
of, or are due to cost report settlements, claims accounts receivable, periodic interim
payments (PIP) and other overpayments. The detailed activity for these components are
included in the 751 (CAFM) and TROR. Also, include on The Financial Statements HI
and SMI balances consisting of receivables specific to Data Match, non-Data Match,
liability (including workers compensation (WC), auto, no-fault) and MSP beneficiary
debts. The detailed activity for the MSP components is included in the M751 and/or
CMS TROR.
Medicare contractors must maintain and make available lead schedules and detailed
documentation to support all amounts reported.
Objective
To ensure that accounts receivable balances reported are reasonable, Medicare
contractors are required to perform trending procedures. Trending procedures can be
used as an important tool to identify potential errors, system weaknesses, or inappropriate
patterns of accounts receivable accumulation, collections, transfers or write-
offs. Trending procedures involve comparisons of recorded amounts to expectations
developed by the Medicare contractors. To properly apply trending procedures, it is
necessary to take the following steps:
Compare Current Year Amounts with Comparative Financial Data
In comparing current-period financial results with prior-period financial results, there is
an implied assumption that the volume of activity in the two periods is comparable. If
there has been a substantial change in volume, it is necessary to take this change into
account and to quantify the change, when making the comparisons. For example, if a
contractor's Accounts Receivable balance has increased by 10 percent, it is necessary to
determine and document the reason for the increase. The increase may be the result of
transitions of providers, new legislation, etc.
Understand Identified Variances and Document the Results
Medicare contractors must identify and provide an explanation for variances that meets
the thresholds outlined in these procedures. Typically, this will be accomplished
primarily through inquiry of operations personnel in the Audit and Reimbursement, MSP,
Medical Review, and other areas that report and track accounts receivable balances. If an
explanation does not adequately describe the variance, the Medicare contractors must
perform additional procedures such as review of detail transactions to identify the
underlying cause(s) of any unusual changes.
The causes for the variances should be quantified. For example, if the change was
mainly attributable to a contractor transition, then the total amount of receivables
transitioned should be identified and included in the Medicare contractors' work papers.
Methodology
Trending & Comparative Analysis for Accounts Receivables
The primary emphasis for performing trend analysis is focusing on the change in the
ending principal accounts receivable balance. The ending principal accounts receivable
balance is comprised of non-MSP and MSP accounts receivables. For FIs, the non-MSP
overpayment sections consist of four major components (cost report settlements, PIP,
claims accounts receivable, and credit balances). For Carriers, the non-MSP
overpayment section consists of two main areas: 1) amounts owed from beneficiaries and
2) amounts owed from physicians/suppliers.
These two areas consist of two major components (claims accounts receivable and credit
balances). For both FI’s and Carriers, the MSP section consists of three major
components (Data Match, non-Data Match, and liability (including WC, auto, no-fault)).
In order to properly identify and understand variances, an analysis must be performed at
the component level. Although the instructions specify ending principal accounts
receivable balance, Medicare contractors must have available an explanation of any
significant change in the ending interest accounts receivable balance and any other
sections on the CMS-750/751 and the TROR meeting these thresholds. The
explanation should be available for review by the CMS, Office of the Inspector
General, General Accounting Office and /or other related parties.
Prior to the certification of the CMS-750/751 and/or the CMS TROR, Balance Sheet and
Income Statement, each Medicare contractor must perform the following steps on a
quarterly basis. The CFO for Medicare Operations' certification of these reports is
indicative that trending procedures have been performed.
HIGLAS Financial Reports
HIGLAS Medicare contractor shall use the following HIGLAS reports to perform the
quarterly accounts receivable trend analysis.
• CMS TROR Reconciliation Worksheet (HIGLAS I) -The HIGLAS Medicare
contractor prepared excel spreadsheet.
• CMS Beginning Balance Report – This report identifies the beginning balances
by MSP/non-MSP category by fund (See Attachment BBrpt).
• CMS Transaction Register - This report identifies the new established receivables
by MSP/non-MSP category by fund (See Attachment TALn2rpt).
• CMS Transaction Register Report Line 3 – This report is the cumulated accrued
interest for the reporting period (See Attachment TALn3rpt).
• CMS Adjustment Register - The Line 3 report is the cumulated adjustments for
interest. The Line 5 & 6 report is the cumulated adjustments for principal (See
Attachments AdjLn3rpt and AdjLn5&6rpt).
• CMS AR Overpayment Report - This report is receivables balance by MSP/non-
MSP components (See Attachment AROvrrpt).
• CMS Applied Collection Register – This report identifies the cash receipts by
MSP/non-MSP category by fund (See Attachment AppCollrpt).
CMS TROR Detail Reconciliation (HIGLAS I)
Step (1)
Use the CMS TROR(s) to populate the Non-Federal and/or Federal sections
(Columns K and L) of the HIGLAS I worksheet.
Step (2)
Use the CMS Beginning Balance Report to populate Line 1 (Beginning FY
Balance) for HI-Fund 050961 (MSP/Non-MSP) Columns (Columns E and F),
SMI-Fund 050960 (MSP/Non-MSP) Columns (Columns G and H) and Interest-
Fund 050720 (MSP/Non-MSP) Columns (Columns I and J) of the HIGLAS I
worksheet (Non-Federal and/or Federal sections).
Step (3)
Use the CMS Transaction Register to populate Line 2 (New Receivables) for HI-
Fund 050961 (MSP/Non-MSP) Columns and SMI-Fund 050960 (MSP/Non-
MSP) Columns of the HIGLAS I worksheet (Non-Federal and/or Federal
sections).
Step (4)
Use the CMS Transaction Register (support Line 3) to populate Line 3a (Accruals
(+) New Interest Receivables) for the Interest-Fund 050720 (MSP/Non-MSP)
Columns of the HIGLAS I worksheet (Non-Federal and/or Federal sections)
Step (5)
Use the CMS Adjustment Register (support Line 3) to populate Line 3b (Accruals
(+) Interest Adjustments) for Interest-Fund 050720 (MSP/Non-MSP) Columns of
the HIGLAS I worksheet (Non-Federal and/or Federal sections).
Step (6)
Use the CMS Applied Collections Register to populate (Line 4, Collections On
Receivables), Line 4A (At Agency-Cash/Checks-Offsets), for HI-Fund 050961
(MSP/Non-MSP) Columns, SMI-Fund 050960 (MSP/Non-MSP) Columns and
Interest-Fund 050720 (MSP/Non-MSP) Columns of the HIGLAS I worksheet
(Non-Federal and/or Federal sections).
Step (7)
Use the CMS Adjustment Register to populate Line 5a (Reclassified/Adjusted
Amounts) for HI-Fund 050961 (MSP/Non-MSP) Columns, SMI-Fund 050960
(MSP/Non-MSP) Columns and Interest-Fund (MSP/Non-MSP) Columns of the
HIGLAS I worksheet (Non-Federal and/or Federal sections).
Step (8)
Use the CMS Adjustment Register to populate (Line 6, Amounts Written-Off))
Line 6A (Currently Not Collectible) and Line 6B (Written-Off and Closed) for
HI-Fund 050961 (MSP/Non-MSP) Columns, SMI-Fund 050960 (MSP/Non-
MSP) Columns and Interest-Fund 050720 (MSP/Non-MSP) Columns of the
HIGLAS I worksheet (Non-Federal and/or Federal sections). Note: Line 6 is the
sum of Line 6A plus Line 6B.
Step (9)
Compare the Line by Line activity of the Total Detail Activity Report (Column
B) to the Line by Line activity of the Total CMS TROR (Column A). The Total
Detail Activity Report is the sum of the HI-Fund Columns, SMI-Fund Columns
and the Interest-Fund Columns (Columns E through J). The Total CMS TROR
Column is the sum of the Non-Federal/Federal CMS TROR (Columns K and L).
The Medicare contractor must provide an explanation for variances identified in
Column C, when the total variance (Line 7, Column C) is more then +/- 10
percent of Line 7, Ending Balance of the CMS TROR (Column A).
Step (10)
Sum the amounts reported in Step 1 through Step 8 for HI-Fund 050961
(MSP/Non-MSP) Columns, SMI-Fund 050960 (MSP/Non-MSP) Columns and
Interest-Fund 050720 (MSP/Non-MSP) Columns of the HIGLAS I worksheet.
The total of the sum of the Columns shall equal the amount reported on Line 7,
Ending Balance of the CMS TROR (Column A), Detail Activity Report (Column
B) and the Summary 2 Trial Balance (HI-Fund 050961, SGL 131002, SMI-Fund
050960, SGL 131002 and Interest-Fund 050720 SGL 134004).
Step (11)
Use the CMS AR Overpayment Register to populate the AR Overpayments
Report section (component breakout) of the HIGLAS I worksheet for HI-Fund
050961 (MSP/Non-MSP) Columns, SMI-Fund 050960 (MSP/Non-MSP)
Columns and Interest-Fund 050720 (MSP/Non-MSP) Columns.
NOTE: HIGLAS Medicare contractors reporting Non-Federal/Federal accounts
receivable amounts shall repeat Step 1 through Step 11 for both types of debtors. The
HIGLAS contractor shall sum the Non-Federal/Federal activity and report the sum of the
amounts in the appropriate comparative Attachment (Attachments I, I-A, II, II-A, IV, IV-
A, V & V-A.
Accounts Receivable Trend Analysis Attachments (CAFM and/or HIGLAS)
Step (1)
Compare the current quarter Non-MSP overpayments section of Form(s) CMS-
H750 and/or CMS AR Overpayments section of the HIGLAS I worksheet
Columns F and H (FIs/Carriers) component line items to the same component line
items in the prior quarter (i.e. 06/30/02 versus 03/31/02) and the current quarter to
the prior year's quarter (i.e. 06/30/02 versus 06/30/01). Calculate the dollar and
percentage difference for each component line item. (See Attachments I & I-A for
the required format.)
NOTE: For FIs, due to the seasonal nature of the cost report settlements, PIP, etc.,
independent quarter activity in the current year should not be the only analysis compared
to the preceding quarter. Comparisons should always be performed from current period
year-to-date activity to prior period year-to-date activity for the same period of time (i.e.
06/30/02 versus 06/30/01).
Step (2)
Compare the current quarter MSP section of Form(s) CMS-H750 and/or CMS AR
Overpayments section of the HIGLAS I worksheet Columns E and G
(FIs/Carriers) component line items to the same component line items in the prior
quarter and prior year. Calculate the dollar and percentage difference for each
component line item. (See Attachments II & II-A for the required format.)
Step (3)
Verify that the dollar amount for each component line item is supported by lead
schedules (detailed documentation) and/or HIGLAS activity reports. Any errors
or misstatements identified as a result of this analysis must be corrected prior to
the submission of Forms CMS-750/751 and/or CMS TROR, Balance Sheet and
Income Statement.
Step (4)
The sum of the components for the Non-MSP overpayments sections (See
Attachments I & I-A) plus the sum of the components for the MSP sections (See
Attachments II & II-A) must equal the ending balances reported on Line 7, of
Form(s) CMS-H751A/B and/or detail report activity section of the HIGLAS I
worksheet Columns E, F, G, and H (FIs/Carriers). The sum of the components for
the Non-MSP overpayments sections must equal the ending balances reported on
Line 7, of Attachments IV and IV-A and/or detail report activity report section of
the HIGLAS I worksheet Columns F and H for the current and prior quarters. The
sum of the components for the MSP sections must equal the ending balances
reported on Line 7, of Form(s) CMS-M751 and/or detail report activity section of
the HIGLAS I worksheet Columns E and G (FIs/Carriers) (See Attachments V &
V-A) for the current and prior quarters.
Step (5)
Provide explanations for each component line item where the amount changed
meets the threshold of +/-15 percent and the amount changed is +/- 5 percent of
the components ending balance. (See Attachments I, I-A, II & II-A)
Supporting Analysis
Step (1)
Ensure the current year beginning balance is the same amount as the prior year's
ending balance and the beginning balance for the prior year's quarter is the same
as the beginning balance of the final quarterly report for that FY (i.e., 06/30/01
and 09/30/01). Additionally, for the second through fourth quarter periods, ensure
that the beginning balances are unchanged from the amount reported as the first
quarter beginning balances.
Note: In the first quarter following a contractor’s transition to HIGLAS the
beginning balance will not equal the previous quarters beginning balance and/or
the prior year beginning balance. The differences are related to the prior year PIP
accrual and/or transition clean up (e.g. approved write-offs of non-supported
debts, valid documented defense, etc.). Medicare contractors shall reconcile the
CAFM and HIGLAS beginning balances and provide an explanation for identified
variances.
Step (2)
Compare the current quarter Form(s) CMS-H/M751 and/or detail report section of
the HIGLAS I worksheet Columns E, F, G and H line items to the same line items
in the prior quarter and prior year. Calculate the dollar and percentage difference
for each line item for Section A of Forms CMS-H/M751. and/or detail report
section of the HIGLAS I worksheet Columns E, F, G and H (See Attachments IV,
IV-A, V & V-A)
NOTE: The Medicare contractors are not required to perform trending procedures or
provide variance explanations on the line items of Forms CMS-H/M751 and/or detail
report section of the HIGLAS I worksheet Columns E, F, G, and H. However, the above
steps should be used to assist the Medicare contractor in providing an explanation for the
variances identified in Attachments I, I-A, II & II-A.
Overall Summary
Step (1)
Document conclusions in a summary memorandum (See Attachment VI) to be
included with HIGLAS I worksheet, Attachments I, I-A, II, II-A, IV, IV-A, V &
V-A and submit to the CFO for Medicare Operations for sign off approval.
For example, the Medicare contractor must identify any external and/or internal
factors that attributed to the variances.
External factors might include (1) Medicare contractor transitions from the
Medicare program, (2) seasonal variances such as provider year-ends, (3) new
legislation impacting reimbursement policies, MSP policies, etc., (4) current
economic conditions (provider termination, bankruptcy, extended repayment
schedules, etc.).
Internal factors might include (1) turnover of key personnel, (2) changes in
accounting guidance or CMS priorities/initiatives, (3) reporting system
modifications, (4) number of contractor processing sites.
Step (2)
Medicare contractors shall submit a signed approved copy of the summary memorandum
(See Attachment VI). In addition, HIGLAS contractors shall submit the HIGLAS
Financial Reports, Attachments I, I-A, II, II-A, IV, IV-A, V & V-A, the CMS TROR
Reconciliation Worksheet (HIGLAS I), and the CMS HIGLAS Contractor Trend
Analysis Checklist (Attachment H-II), to the regional office for final approval.
Note: The summary memorandum (See Attachment VI) and the analysis schedules
(HIGLAS I, Attachments I, I-A, II, II-A, IV, IV-A, V & V-A) will be reviewed and
approved by the CFO for Medicare Operations and the region's Associate Regional
Administrator (ARA). The ARA will review the trend analysis submitted by the
Medicare contractor and either approve or request additional explanation and/or
documentation. The ARA must notify the Medicare contractor by phone, email or fax no
later than February 15, May 15, August 15, and November 8 as to the
approval/disapproval. The ARA must allow the Medicare contractor no less than two
days (upon receipt of the request) to provide the additional documentation needed to
support their variance. Upon receiving the request, the Medicare contractor has no more
than four days to provide the additional documentation to the ARA. If the ARA’s request
for any additional information can not be submitted by the due dates, the ARA must
notify the CO Division of Financial Reporting and Policy (DFRP) (by phone, email or
fax) and provide a date when the Medicare contractor’s trend analysis will be forwarded
to the CO. Upon receipt of notification that the CO review process is completed, the
ARA will submit a signed approved copy of the summary memorandum to the Medicare
contractors and CO, DFRP.
III. Due Date
The analysis must be submitted to each contractor's respective regional office on
February 8, May 8, August 8, and November 1 (The third/fourth quarter due dates may
change due to the accelerated time periods. Medicare contractors will be notified of these
changes by a Joint Signature Memorandum (JSM)). The ARA must review the Medicare
contractors' submissions and forward them to CO by February 15, May 15, August 15,
and November 8. If that date occurs on a holiday or a weekend, the report is due the
following Federal workday. The Medicare contractor and the ARA may email or fax the
analysis by the due dates and immediately follow up with a hard copy.
NOTE: The ARA will submit a copy of the Medicare contractors' summary
memorandums and the analysis schedules to the CO/DFRP. The CO will notify the RO
by email upon receipt of the Medicare contractors’ trend analysis. The CO will review
the Medicare contractors’ analysis schedules and may request additional documentation.
The CO is not responsible for approving or denying the Medicare contractors' trend
analysis. If additional documentation is needed, the CO will notify the RO by email
within 14 days upon receipt of the Medicare contractors’ analysis schedules. Upon the
completion of the CO’s review, CO will notify the RO by email that no additional
information is needed and the CO’s review process is completed. The ARA will sign and
approve the Medicare contractors’ summary memorandum, and submit a signed approved
copy to the CO, DFRP and to the Medicare contractors.

CMS HIGLAS TROR Reconciliation Worksheet
HIGLAS I (Non-Federal/Federal)
Part I - Status of Receivables
HIGLAS I
Section A (Col. A) (Col. B) (Col. C) (Col. D)
(Col. E) (Col. F) (Col. G) (Col. H) (Col. I) (Col. J) (Col. K) (Col. L)
(Total Non-Federal/Federal) (Col. K + L) (Col. E+F+G+H+I+J)
List of Detailed Reports
Receivables and Collections TROR Total Detail
Report Activity Registers Variance HIGLAS Source MSP Non-MSP MSP Non-MSP MSP Non-MSP Non-Fed Fed
(1) Beginning FY Balance 2,888 76,000,000 76,000,000
0
Beginning Balance Rpt
14,000,000 25,000,000 10,000,000 25,000,000 1,000,000 1,000,000 69,750,000 6,250,000
(2) New Receivables (+) 24,632 200,000,000 200,000,000
Transaction Register
35,000,000 100,000,000 15,000,000 50,000,000 0 0 187,500,000 12,500,000
(3) Accruals (+) (New Interest Receivables) 1,576,728 1,576,728 76,728 1,500,000 1,557,546 19,182
Transaction Register (support line 3) 500,000 500,000
Transaction Register
0 500,000 500,000 0
CMS Adjustment Register (support line 3) 1,076,728 1,076,728
Adjustment Register
76,728 1,000,000 1,057,546 19,182
(4) Collections on Receivables (-) (120,815,566) (120,815,566)
0 (4,081,254) (94,709,110) (3,000,000) (17,925,202) (100,000) (1,000,000) (119,020,253) (1,795,314)
(A) At Agency-Cash/Checks (9,231,254) (9,231,254)
Applied Collections
(4,081,254) (1,000,000) (3,000,000) (1,000,000) (100,000) (50,000) (7,435,941) (1,795,314)
-Offsets (111,584,312) (111,584,312)
Applied Collections
(93,709,110) (16,925,202) (950,000) (111,584,312) 0
(B) At Third Party 0 0
(C) Asset Sales 0 0
(D) Other - Must footnote 0 0
(5) Adjustments 1,093 (5,774,224) (5,774,224)
0
Adjustment Register
(975,538) (4,042,637) (296,554) (226,534) (59,757) (173,204) (5,441,262) (332,962)
(A) Reclassified/Adjusted Amounts (+ or -) 1,093 (5,774,224) (5,774,224) (975,538) (4,042,637) (296,554) (226,534) (59,757) (173,204) (5,441,262) (332,962)
(B) Adjustments Due to Sale of Assets (+ or -) 0 0
(C) Consolidations (+ or -) 0 0
(6) Amounts Written-Off (-) 152 (1,940,261) (1,940,261)
0 (220,610) (1,303,694) (50,464) (222,153) (23,149) (120,191) (1,866,706) (73,555)
(A) Currently Not Collectible (-) 146 (1,862,750) (1,862,750)
Adjustment Register
(209,275) (1,252,857) (37,313) (222,153) (22,991) (118,161) (1,795,355) (67,395)
(B) Written-Off and Closed Out (-) 6 (77,511) (77,511)
Adjustment Register
(11,335) (50,837) (13,151) 0 (158) (2,030) (71,351) (6,161)
(7) Ending Balance (TROR/Activity Registers) 2,889
149,046,677 149,046,677 0
(x)
43,722,598 24,944,559 21,652,982 56,626,111 893,822 1,206,605 132,479,326 16,567,351
AR Overpayments Report: HIGLAS Source MSP Non-MSP MSP Non-MSP MSP Non-MSP Total Total
Cost Report Settlements 19,800,000 19,800,000
AR Overpayment Rpt
9,000,000 10,000,000 800,000 19,800,000 0
Claims Accounts Receivable 49,308,754 49,308,754
AR Overpayment Rpt
12,000,000 37,308,754 0 49,308,754 0
Credit Balances 303,621 303,621
AR Overpayment Rpt
303,621 0 0 303,621 0
Other 13,359,902 13,359,902
AR Overpayment Rpt
5,000,000 7,958,297 401,605 13,359,902 0
Physician/Supplier 0 0 0 0
Beneficiary 0 0 0 0
GHP(Data/non-Data Match) 22,322,019 22,322,019
AR Overpayment Rpt
18,822,019 3,000,000 500,000 16,741,514 5,580,505
MSP Prov/Phys/Supp/Bene 0 0 0 0
MSP Beneficiary (Liability) 40,210,579 40,210,579
AR Overpayment Rpt
22,900,000 17,010,579 300,000 30,157,934 10,052,645
Other MSP (Liability) 3,741,803 3,741,803 2,000,000 1,642,982 98,821 2,806,352 935,451
Total Overpayment Reports 149,046,678 149,046,678 43,722,019 26,303,621 21,653,561 55,267,051 898,821 1,201,605 132,478,078 16,568,600
Difference (TROR/Activity Registers vs. Ovrpymnt Rpt) (1)
(a)
(1)
(b)
579 (1,359,062)
(579) 1,359,060 (4,999) 5,000 1,248 (1,249)
(x) = variance between the detail activity registers vs. the TROR
(a) = variance between the TROR vs.overpayments reports
(b) = variance between the detail activity registers vs. overpayments reports
Note: Contractors are required to provide variance explanations for the amounts reported on the AR Overpayments Report
CMS TROR
Interest - Fund 050720
HI - Fund 050961
SMI - Fund 050960
CMS Beginning Balance Report
Attachment BBrpt
Beginning Balance Report Report Date: 06-JAN-06 01:06 PM
As of Date: 30-SEP-2005 Page: X of X
ORGANIZATION: Contractor ABC User Name: GDH0
As of Date: 30-SEP-05
Workload Low: Contractor #
Workload High: Contractor #
Transaction Type Low:
Transaction Type High:
AR Number Low:
AR Number High:
Customer Number Low:
Customer Number High:
Customer Profile Class Low:
Customer Profile Class High:
Include CNC Receivables/Debit Memos: Y
Show Invoices with Negative Fund Level Balances Only?:
Open/Closed/Both:
Type of Receivable: A
Customer Class: NONFEDERAL
Summary Only: Y
Totals for all Workloads
HI Fund SMI Fund GEN Fund Total
------------------------- ------------------------- ------------------------- -------------------------
MSP Balances 14,000,000.00 10,000,000.00 1,000,000.00 25,000,000.00
NonMSP Balances 25,000,000.00 25,000,000.00 1,000,000.00 56,000,000.00
------------------------- ------------------------- ------------------------- -------------------------
Total 39,000,000.00 35,000,000.00 2,000,000.00 76,000,000.00
CMS Transaction Register
Attachment TALn2rpt
Transaction Register as of 31-DEC-05
Current Date 06-JAN-2006 01:08:36
Request ID 123456
Support TROR Line2 Y
Fiscal Year 2006
Workload Id Low Contractor ABC
Workload Id High Contractor ABC
Quarter
As of Date 31-DEC-05
Type Of Receivable A
Customer Class NONFEDERAL
GL Date Low
GL Date High
Invoice Date Low
Invoice Date High
Transaction Type Low
Transaction Type High
Invoice Class
Co. Segment Low
Co. Segment High
CMS SET OF BOOKS
Invoice Currency : USD
No. of Lines 24632
Summary Information :
----------------------
FUND YEAR MSP NON MSP Total
050960 XXXX 0.00 50,000,000.00 50,000,000.00
XXXX 15,000,000.00 0.00 15,000,000.00
--------------------------- ---------------------------- ----------------------------
Fund Total 15,000,000.00 50,000,000.00 65,000,000.00
050961 XXXX 0.00 100,000,000.00 100,000,000.00
XXXX 35,000,000.00 0.00 35,000,000.00
--------------------------- ---------------------------- ----------------------------
Fund Total 35,000,000.00 100,000,000.00 135,000,000.00
---------------------------- --------------------------- ---------------------------
Report Total 50,000,000.00 150,000,000.00 200,000,000.00
CMS Transaction Register
Attachment TALn3rpt
Transaction Register as of 31-DEC-05
Current Date 06-JAN-2006 01:09:15
Request ID 417123
Support TROR Line2 N
Fiscal Year 2006
Workload Id Low
Workload Id High
Quarter
As of Date 31-DEC-05
Type Of Receivable A
Customer Class NONFEDERAL
GL Date Low
GL Date High
Invoice Date Low
Invoice Date High
Transaction Type Low DM-INTEREST
Transaction Type High DM-LATE FEE INTEREST
Invoice Class
Co. Segment Low
Co. Segment High
CMS SET OF BOOKS
Invoice Currency : USD
No. of Lines 375
Summary Information :
----------------------
FUND YEAR MSP NON MSP Total
050720 XXXX 0.00 500,000.00 500,000.00
--------------------------- ---------------------------- ----------------------------
Fund Total 0.00 500,000.00 500,000.00
---------------------------- --------------------------- ---------------------------
Report Total 0.00 500,000.00 500,000.00
CMS Adjustment Register
Attachment AdjLn3rpt
Adjustment Register as of 31-DEC-05
Report Date: 06-JAN-06 13:09:50
Page 1 / 2Request ID 734123
Summary Report Y
Fiscal Year 2006
Quarter Number
As of Date 31-DEC-05
Type Of Receivable Administrative Receivables
Customer Class NONFEDERAL
Receivable Activity From
Receivable Activity To
Include Line 3 Only Y
TROR SUMMARY INFORMATION
------------------------------
3
FUND MSP NON MSP TOTAL COUNT
GEN -050720XXXX0D00 76,727.70 1,000,000.00 1,076,727.70 1414
-------------------- -------------------- --------------------- --------------
REPORT TOTAL 76,727.70 1,000,000.00 1,076,727.70 1414
CMS Adjustment Register
Attachment AdjLn5&6rpt
Adjustment Register as of 31-DEC-05
Report Date: 06-JAN-06 13:09:50
Page 1 / 2
Request ID 317123
Summary Report Y
Fiscal Year 2006
Quarter Number
As of Date 31-DEC-05
Type Of Receivable Administrative Receivables
Customer Class NONFEDERAL
Receivable Activity From
Receivable Activity To
Include Line 3 Only N
TROR SUMMARY INFORMATION
------------------------------
5A
FUND MSP NON MSP TOTAL COUNT
GEN -050720XXXX0D00 (59,756.87) (173,204.12) (232,960.99) 342
HI -050961XXXX0DC0 (975,538.15) (4,042,636.65) (5,018,174.80) 215
SMI -050960XXXX0DC0 (296,554.15) (226,533.54) (523,087.69) 272
-------------------- -------------------- --------------------- --------------
REPORT TOTAL (1,331,849.17) (4,442,374.31) (5,774,223.48) 829
6A
FUND MSP NON MSP TOTAL COUNT
GEN -050720XXXX0D00 (22,990.98) (118,160.76) (141,151.74) 65
HI -050961XXXX0DC0 (209,274.75) (1,252,856.76) (1,462,131.51) 38
SMI -050960XXXX0DC0 (37,313.17) (222,153.20) (259,466.37) 39
-------------------- -------------------- --------------------- --------------
REPORT TOTAL (269,578.90) (1,593,170.72) (1,862,749.62) 142
6B
FUND MSP NON MSP TOTAL COUNT
GEN -050720XXXX0D00 (158.36) (2,030.22) (2,188.58) 3
HI -050961XXXX0DC0 (11,334.88) (50,837.02) (62,171.90) 2
SMI -050960XXXX0DC0 (13,151.05) 0.25 (13,151.30) 2
-------------------- -------------------- --------------------- --------------
REPORT TOTAL (24,644.29) (52,867.49) (77,511.78) 7
CMS AR Overpayment Report
Attachment AROvrrpt
AR Overpayment Report as of 31-DEC-05
Report Date: 06-JAN-06 12:30:58
Page 1 / 3
Request ID: 476123
Workload Low..................................:
Workload High.................................:
Comparative Summary(Yes/No)...................: N
As of Date1 Summary Only(Yes/No)..............: Y
As of Date1...................................: 31-DEC-05
As of Date2(Comparative)......................:
Invoice Class.................................:
Customer Class................................: NONFEDERAL
Transaction Type Low..........................:
Transaction Type High.........................:
Co. Segment Low...............................:
Co. Segment High..............................:
SUMMARY OF OVERPAYMENTS AS OF 31-DEC-05
------------------------------------------------
MSP OVERPAYMENT HI -050961 SMI-050960 INT-050720 TOTAL
------------------------------------------------------------------------------------------------------------------------------------------
BENE-LIABILITY 22,900,000.00 17,010,579.00 300,000.00 40,210,579.00
GROUP HEALTH PLAN 18,822,019.00 3,000,000.00 500,000.00 22,322,019.00
MSP PROV/PHY/SUPP/BENE 0.00 0.00 0.00 0.00
OTHER-LIABILITY 2,000,000.00 1,642,982.00 98,821.00 3,741,803.00
------------------------ ----------------------- ---------------------- ----------------------
MSP TOTAL 43,722,019.00 21,653,561.00 898,821.00 66,274,401.00
NON MSP OVERPAYMENT HI -050961 SMI-050960 INT-050720 TOTAL
------------------------------------------------------------------------------------------------------------------------------------------
BENEFICIARY 0.00 0.00 0.00 0.00
CLAIMS ACCOUNT RECEIVABLE 12,000,000.00 37,308,754.00 0.00 49,308,754.00
COST REPORT SETTLEMENT 9,000,000.00 10,000,000.00 800,000.00 19,800,000.00
CREDIT BALANCES 303,621.00 0.00 0.00 303,621.00
OTHER 5,000,000.00 7,958,297.00 401,605.00 13,359,902.00
PIP ACCRUAL 0.00 0.00 0.00 0.00
------------------------ ----------------------- ---------------------- ----------------------
NON MSP TOTAL 26,303,621.00 55,267,051.00 1,201,605.00 82,772,277.00
------------------------- ---------------------- ---------------------- ----------------------
MSP AND NON-MSP TOTAL 70,025,640.00 76,920,612.00 2,100,426.00 149,046,678.00
====================== ==================== =================== ==================
CMS Applied Collection Register
Attachment AppCollrpt
CMS APPLIED COLLECTIONS REGISTER As of 31-DEC-05
Report Date: 06-JAN-06 01:10 PM
Page 2 of 8
Request ID: 422123
REPORT PARAMETERS
Show Detail : N
Support TROR : Y
Fiscal Year : 2006
As of Date : 31-DEC-2005
GL Date From :
GL Date To :
Cash Receipt Batch Number From :
Cash Receipt Batch Number To :
Cash Receipt Number From :
Cash Receipt Number To :
Credit Memo Number From :
Credit Memo Number To :
Invoice/Debit Memo Number From :
Invoice/Debit Memo Number To :
Customer Name From :
Customer Name To :
Workload ID From : Contractor #
Workload ID To : Contractor #
Type of Receivable : A
Customer Class : NONFEDERAL
TRENDING SUMMARY FOR ALL WORKLOADS AMOUNT SUBTOTAL/TOTAL
PRINCIPAL
GEN Non-MSP OFFSET
OTHER 8,633.00
Subtotal OFFSET 8,633.00
Total GEN Non-MSP 8,633.00
Total GEN Collections 8,633.00
HI MSP CASH
INSURER 31,254.00
EMPLOYER 150,000.00
BENEFICIARY 3,900,000.00
Subtotal CASH 4,081,254.00
Total HI MSP 4,081,254.00
Non-MSP 4A
PROVIDER -3,000,000.00
Subtotal 4A -3,000,000,00
CASH
PROVIDER 4,000,000.00
Subtotal CASH 4,000,000.00
OFFSET
PROVIDER 93,709,110.00
Subtotal OFFSET 93,709,110.00
Total HI Non-MSP 94,709,110.00
CMS Applied Collection Register
Attachment AppCollrpt
Total HI Collections 98,790,364.00
TRENDING SUMMARY FOR ALL WORKLOADS AMOUNT SUBTOTAL/TOTAL
SMI MSP CASH
EMPLOYER 100,000.00
BENEFICIARY 2,900,000.00
Subtotal CASH 3,000,000.00
Total SMI MSP 3,000,000.00
Non-MSP 4A
PROVIDER -1,000,000.00
Subtotal 4A -1,000,000.00
CASH
PROVIDER 2,000,000.00
Subtotal CASH 2,000,000.00
OFFSET
PROVIDER 16,925,202.00
Subtotal OFFSET 16,925,202.00
Total SMI Non-MSP 17,925,202.00
Total SMI Collections 20,925,202.00
Total Collections - PRINCIPAL $119,724,199.00
INTEREST
GEN MSP CASH
OTHER 100,000.00
Subtotal CASH 100,000.00
Total GEN MSP 100,000.00
Non-MSP CASH
OTHER 50,000.00
Subtotal CASH 50,000.00
OFFSET
OTHER 941,367.00
Subtotal OFFSET 941,367.00
Total GEN Non-MSP 991,367.00
Total GEN Collections 1,091,367.00
Total Collections - INTEREST $1,091,367.00
CMS Applied Collection Register
Attachment AppCollrpt
TOTAL COLLECTIONS - Principal and Interest By Debtor Type
OTHER 708,220.00
INSURER 12,003.00
EMPLOYER 240,073.00
ROVIDER 113,794,976.00
BENEFICIARY 6,060,294.00
--------------------
REPORT TOTAL $120,815,566.00
========================
CMS Medicare Accounts Receivable Non-MSP (Part A HI)
Contractor ABC
Attachment I
SOURCE: CMS AR Overpayment Report (HIGLAS I Worksheet)
SCOPE: If percentage change is greater than +/- 15% and amount change +/- 5 % of the combined component ending balances.
(A-B)
(C/B x 100%)
A
B
C D
12/31/2005 9/30/2005
$ Change % Change Note
Cost Report Settlements 14,000,000
$
17,000,000$
(3,000,000) -17.65% 1
Claims 12,000,000 13,000,000 (1,000,000) -7.69%
NER
PIP 0 0 0 0.00%
NER
Credit Balance 303,621 0
303,621 0.00%
NER
Other 0 0 0 0.00% NER
Total Non-MSP
26,303,621$ 30,000,000$
(3,696,379)$
-12.32%
Total TROR
24,944,560$
29,025,250
$
Variance (Over/Under Application) 1,359,061$
974,750$
5% of Combined Ending Balance
1,315,181
$ ($26,303,621 x 5%)
No Explanation Required (NER)
(1) Cost Report Settlements-The total variance for the Non-MSP (HI) balance for the current quarter reflects a decrease
of $3.7 million compared to the prior quarter. The bulk of this variance is a result of the change in Cost Report Settlements
a decrease of $3 million. The primary cause of this variance is due to the result of the larger hospitals with the potential
for large overpayments being settled in the last quarter of the year.
CMS Medicare Accounts Receivable Non-MSP (Part A HI)
Contractor ABC
Attachment I-A
SOURCE: CMS AR Overpayment Report (HIGLAS I Worksheet) & H750A
SCOPE: If percentage change is greater than +/- 15% and amount change +/- 5 % of the combined component ending balances.
(A-B) (C/B x 100%)
A B C D
12/31/2005 12/31/2004 $ Change % Change Note
Cost Report Settlements 14,000,000$ 13,000,951$ 999,049 7.68%
NER
Claims 12,000,000 13,000,000 (1,000,000) -7.69%
NER
PIP 0 14,000,000 (14,000,000) -100.00%
(4)
Credit Balance 303,621 0 303,621 0.00%
NER
Other 0 0 0 0.00% NER
Total Non-MSP 26,303,621$ 40,000,951$ (13,697,330)$
-34.24%
Total TROR 24,944,560$ 40,000,951$
Variance (Over/Under Application) 1,359,061$ -$
5% of Combined Ending Balance
1,315,181$ ($26,303,621 x 5%)
No Explanation Required (NER)
(4)
PIP Accrual - HIGLAS Medicare contractors are no longer required to report an estimate PIP accrual.
CMS Medicare Accounts Receivable MSP (Part A HI)
Contractor ABC
Attachment II
SOURCE: CMS AR Overpayment Report (HIGLAS I Worksheet)
SCOPE: If percentage change is greater than +/- 15% and amount change +/- 5 % of the combined component ending balances.
(A-B) (C/B x 100%)
A B C D
12/31/2005 9/30/2005 $ Change % Change Note
GHP(Data/non-Data Match)
18,822,019 23,050,000 (4,227,981) -18.34% (2)
MSP Provider/Physician/Supplier - - 0.00%
NER
MSP Beneficiary (Liability) 22,900,000 19,120,000 3,780,000 19.77% (3)
Other MSP (Liability) 2,000,000 - 2,000,000 0.00%
NER
Total MSP 43,722,019$ 42,170,000$ 1,552,019$
3.68%
Total TROR 43,722,598$ 41,317,525$
Variance (Over/Under Application) (579)$ 852,475$
5% of Combined Ending Balance
2,186,101$ ($43,722,019 x 5%)
No Explanation Required (NER)
(2) GHP-HIGLAS does not break down GHP between Data Match and Non-Data Match. GHP overall has
decreased by $4.2 million in comparison to the previous quarter. Non-Data Match receivables decreased by
$3 million, which reflects a significant decrease in the number of demands produced since the implementation of
ReMas during FY 2005.
CMS Medicare Accounts Receivable MSP (Part A HI)
Contractor ABC
Attachment II-A
SOURCE: CMS AR Overpayment Report (HIGLAS I Worksheet) & H750A
SCOPE: If percentage change is greater than +/- 15% and amount change +/- 5 % of the combined component ending balances.
(A-B)
(C/B x 100%)
A B
C D
12/31/2005
12/31/2004 $ Change
% Change
Note
GHP(Data/non-Data Match)
18,822,019
21,322,019
(2,500,000) -11.72%
(5)
MSP Provider/Physician/Supplier - - 0.00%
NER
MSP Beneficiary (Liability) 22,900,000
24,000,000
(1,100,000)
-4.58%
NER
Other MSP (Liability) 2,000,000
- 2,000,000 0.00%
NER
Total MSP 43,722,019$
45,322,019$ (1,600,000)
$
-3.53%
Total TROR
43,722,598
$
45,322,019
$
Variance (Over/Under Application)
(579)$
-$
5% of Combined Ending Balance
2,186,101$
($43,722,019 x 5%)
No Explanation Required (NER)
(5)
Currently GHP-HIGLAS does not break out Data Match and Non-Data Match. GHP overall has
decreased by $2.5 million in comparison to the previous year. Since the implementation of ReMAS during
FY 2005, the Non-Data Match receivables reflects the significant decrease.
CMS Medicare Accounts Receivable Non-MSP (Part A HI)
Contractor ABC
Attachment IV
SOURCE: Detail Activity Reports (HIGLAS I Worksheet)
Part I - Status of Receivables
Section A
Receivables and Collections
12/31/2005 9/30/2005 $ Change %Change
(1) Beginning FY Balance 25,000,000 22,613,882 2,386,118 10.55%
(2) New Receivables (+)
100,000,000 91,601,759 8,398,241 9.17%
(3) Accruals (+) (New Interest Receivables)
(4) Collections on Receivables (-) (94,709,110) (81,520,069) (13,189,041) 16.18%
(A) At Agency-Cash/Checks (1,000,000) (42,043,277) 41,043,277 -97.62%
-Offsets
(93,709,110) (39,476,792) (54,232,318) 137.38%
(B) At Third Party
(C) Asset Sales
(D) Other - Must footnote
(5) Adjustments (4,042,637) (3,655,694) (386,943) 10.58%
(A) Reclassified/Adjusted Amounts (+ or -) (4,042,637) (3,655,694) (386,943) 10.58%
(B) Adjustments Due to Sale of Assets (+ or -)
(C) Consolidations (+ or -)
(6) Amounts Written-Off (-) (1,303,694) (14,628) (1,289,066) 8812.32%
(A) Currently Not Collectible (-) (1,303,694) (14,628) (1,289,066) 8812.32%
(B) Written-Off and Closed Out (-) 0 0 0 0.00%
(7) Ending Balance (TROR/Activity Registers) 24,944,560 29,025,250
(4,080,690) -14.06%
Total Collections 94,709,110 81,520,069
Total Adjusted Receivables 119,653,670 110,545,319
Collection Percentage 79.15% 73.74%
HI - Fund 050961

CMS Medicare Accounts Receivable Non-MSP (Part A HI)
Contractor ABC
Attachment IV-A
SOURCE: Detail Activity Reports (HIGLAS I Worksheet), H751A & M751A
Part I - Status of Receivables
Section A
Receivables and Collections
12/31/2005 12/31/2004 $ Change %Change
(1) Beginning FY Balance 25,000,000 22,613,882 2,386,118 10.55%
(2) New Receivables (+)
100,000,000 90,976,509 9,023,491 9.92%
(3) Accruals (+) (New Interest Receivables) 14,000,000
(14,000,000)
(4) Collections on Receivables (-) (94,709,110) (83,384,118)
(11,324,992) 13.58%
(A) At Agency-Cash/Checks (1,000,000) (45,067,576) 44,067,576 -97.78%
-Offsets
(93,709,110) (38,316,542) (55,392,568) 144.57%
(B) At Third Party
(C) Asset Sales
(D) Other - Must footnote
(5) Adjustments (4,042,637) (4,155,694) 113,057 -2.72%
(A) Reclassified/Adjusted Amounts (+ or -) (4,042,637) (4,155,694) 113,057 -2.72%
(B) Adjustments Due to Sale of Assets (+ or -)
(C) Consolidations (+ or -)
(6) Amounts Written-Off (-) (1,303,694) (49,628) (1,254,066) 2526.93%
(A) Currently Not Collectible (-) (1,303,694) (49,628) (1,254,066) 2526.93%
(B) Written-Off and Closed Out (-) 0 0 0 0.00%
(7) Ending Balance (TROR/Activity Registers) 24,944,560 40,000,951 (1,056,391) -2.64%
Total Collections 94,709,110 83,384,118
Total Adjusted Receivables 119,653,670 109,385,069
Collection Percentage 79.15% 76.23%
HI - Fund 050961
CMS Medicare Accounts Receivable MSP (Part A HI)
Contractor ABC
Attachment V
SOURCE: Detail Activity Reports (HIGLAS I Worksheet)
Part I - Status of Receivables
Section A
Receivables and Collections
12/31/2005 9/30/2005 $ Change %Change
(1) Beginning FY Balance 14,000,000 18,000,000 (4,000,000) -22.22%
(2) New Receivables (+)
35,000,000 34,453,226 546,774 1.59%
(3) Accruals (+) (New Interest Receivables)
(4) Collections on Receivables (-) (4,081,254) (18,589,335) 14,508,081 -78.05%
(A) At Agency-Cash/Checks (4,081,254) (18,589,335) 14,508,081 -78.05%
-Offsets
0 0 0 0.00%
(B) At Third Party
(C) Asset Sales
(D) Other - Must footnote
(5) Adjustments (975,538) 12,142,077 (13,117,615) -108.03%
(A) Reclassified/Adjusted Amounts (+ or -) (975,538) 12,142,077 (13,117,615) -108.03%
(B) Adjustments Due to Sale of Assets (+ or -)
(C) Consolidations (+ or -)
(6) Amounts Written-Off (-) (220,610) (4,688,443) 4,467,833 -95.29%
(A) Currently Not Collectible (-) (209,275) (4,685,151) 4,475,876 -95.53%
(B) Written-Off and Closed Out (-) (11,335) (3,292) (8,043) 244.32%
(7) Ending Balance (TROR/Activity Registers) 43,722,598 41,317,525 2,405,073 5.82%
Total Collections 4,081,254 18,589,335
Total Adjusted Receivables 47,803,852 59,906,860
Collection Percentage 8.54% 31.03%
HI - Fund 050961
CMS Medicare Accounts Receivable MSP (Part A HI)
Contractor ABC
Attachment V-A
SOURCE: Detail Activity Reports (HIGLAS I Worksheet) & M751A
Part I - Status of Receivables
Section A
Receivables and Collections
12/31/2005 12/31/2004 $ Change %Change
(1) Beginning FY Balance 14,000,000 18,000,000 (4,000,000) -22.22%
(2) New Receivables (+)
35,000,000 31,074,736 3,925,264 12.63%
(3) Accruals (+) (New Interest Receivables)
(4) Collections on Receivables (-) (4,081,254) (2,598,173) (1,483,081) 57.08%
(A) At Agency-Cash/Checks (4,081,254) (2,598,173) (1,483,081) 57.08%
-Offsets
0 0 0 0.00%
(B) At Third Party
(C) Asset Sales
(D) Other - Must footnote
(5) Adjustments (975,538) (685,700) (289,838) 42.27%
(A) Reclassified/Adjusted Amounts (+ or -) (975,538) (685,700) (289,838) 42.27%
(B) Adjustments Due to Sale of Assets (+ or -)
(C) Consolidations (+ or -)
(6) Amounts Written-Off (-) (220,610) (468,844) 248,234 -52.95%
(A) Currently Not Collectible (-) (209,275) (468,515) 259,240 -55.33%
(B) Written-Off and Closed Out (-) (11,335) (329) (11,006) 3345.25%
(7) Ending Balance (TROR/Activity Registers) 43,722,598 45,322,019 (1,599,421) -3.53%
Total Collections 4,081,254 2,598,173
Total Adjusted Receivables 47,803,852 47,920,192
Collection Percentage 8.54% 5.42%
HI - Fund 050961
CMS Medicare Accounts Receivable (Part A HI)
Contractor ABC
AR Summary Memorandum
Period Ending ___________________________
Attachment VI
(1)
Cost Report Settlements-The total variance for the Non-MSP (HI) balance for the current quarter reflects a
decrease of $3.7 million compared to the prior quarter. The bulk of this variance is a result of the change in
cost report settlement a decrease of $3 million. The primary cause of this variance is due to the result of
of the larger hospitals with the potental for large overpayments being settled in the last quarter of the year.
(2)
GHP-HIGLAS does not break down GHP between Data Match and Non-Data Match. GHP overall has
decreased by $4.2 million in comparison to the previous quarter. Non-Data Match receivables decreased by
$3 million, which reflects a significant decrease in the number of demands produced since the implementation of
ReMas during FY 2005.
(3)
MSP Beneficiary-increased by $3.7 million and is the result of an increase in workload for total demands.
(4)
PIP Accrual - HIGLAS Medicare contractors are no longer required to report an estimate PIP accrual.
(5)
Currently GHP-HIGLAS does not break out Data Match and Non-Data Match. GHP overall has
decreased by $2.5 million in comparison to the previous year. Since the implementation of ReMAS during
FY 2005, the Non-Data Match receivables reflects the significant decrease.
Prepared by: Date
Reviewed by: Date
CFO for Medicare Operations approval: ________________________________
Date
ARA approval:___________________________________________________ Date
The following represents the summary for the changes in the accounts receivable balance for the current quarter.
Attachment H-II
CMS HIGLAS Contractor Trend Analysis Checklist
Contractor Number
Contractor Name
Period
Medicare Contractor has submitted the following HIGLAS reports.
_____ CMS Report On Receivables Due From the Public (Attachment
HI GLAS I
).
_____ CMS Beginning Balance Report (Attachment
BBrpt
).
_____ CMS Transaction Register Report Line 2 (Attachment
TALn2rpt
).
_____ CMS Transaction Register Report Line 3 (Attachment
TALn3rpt
).
_____ CMS Adjustment Register Report for Line 3 (Attachments
AdjLn3rpt
).
_____ CMS Adjustment Register Report for Lines 5 and 6 (Attachments
AdjLn5& 6rpt
).
_____ CMS AR Overpayment Report(Attachment
AROvrrpt
).
_____ CMS Applied Collections Report (Attachment
AppCollrpt
).
_____ CMS Summary 2 Trail Bal ance.
_______________________________________ Date: _________________________
Preparer Signature
400.23 – Exhibit 23 – Instructions for the Benefits Payable Survey
(Rev. 105, Issued: 08-25-06, Effective/Implementation: 09-30-06)
CMS is required to prepare fiscal year financial statements in accordance the Office of
Management and Budget’s (OMB’s) accelerated mandated schedule. In order to meet the
accelerated timeframes, CMS requests specific contractor financial data for the
preparation and audit of CMS’ annual financial statements.
For inclusion in the year-end CMS financial statements, the Office of the Actuary
(OACT) prepares the Medicare Incurred But Not Reported (IBNR) estimate which is
based on actuarial estimates. Due to the complexity of the actuarial estimate and the
availability of data, OACT prepares this estimate for yearend statements only. The
Medicare IBNR estimate represents the amount of CMS claims incurred but not yet paid
at the end of the fiscal year (FY) and is a summation of five different components:
(1) the incurred to approval of payment amount – represents Medicare Services
provided, for which, a corresponding claim has not been approved for payment
and also is referred to as the incurred to approved amount;
(2) the retroactive settlements on cost reports amount – represents the estimated net
liability for cost reports awaiting final settlement and is also referred to as the cost
settlement amount;
(3) the approval to actual payment amount – represents the aggregate claims
approved for payment, for which, the corresponding reimbursement has not been
issued and is also referred to as the approved to paid amount;
(4) the paid to cleared amount – represents the aggregate claims for which checks
have been issued, but have not cleared the Medicare contractor’s financial
institution and is also referred to as the outstanding checks amount; and
(5) the advance payments under Periodic Interim Payment (PIP) amount – represents
the bi-weekly payments for estimated benefit payments for plans under such a
payment plan and is also referred to as the PIP amount.
The data required for items (3) through (5) is obtained directly from the Medicare
contractors and is submitted via the Benefits Payable survey (Attachment I, II, and/or III).
Typically, the survey is sent to the Medicare contractors in May or June of the current
FY.
Due to the on-going transition to the Healthcare Integrated General Ledger Accounting
System (HIGLAS) by the Medicare contractors, the data elements on the survey which
are required for submission have been revised. Instructions for each data element on the
attachments are discussed below.
1) PIP – value of the first periodic interim payment (PIP) cycle paid in the ensuing
month for the end of the month being reviewed. (Fiscal intermediaries
ONLY)
CAFM contractors should continue to utilize their shared system to obtain this
amount. If the payment cycle has not been run, please provide an estimate of
this amount. Do not include pass through costs.
HIGLAS contractors should obtain this amount from their 810 interface report.
If the payment cycle has not been run, please provide an estimate of this
amount. Do not include pass through costs.
2) Claims on the payment floor – Adjudicated claims not yet paid for both Health
Insurance (HI) and Supplemental Medical Insurance (SMI), if applicable.
CAFM contractors should continue to utilize their shared system to obtain this
amount. The amount reported on the survey must agree to the amount reported
on the year-end Form CMS-750A and/or 750B, Statement of Financial Position.
HIGLAS contractors should obtain this amount from their Summary 2 Trial
Balance, GL account 216002, Entitlement Benefit Due/Payable – Adjudicated
Claims.
3) Claims on Hold –This amount would include claims held resulting from Do Not
Forward, providers being investigated for fraud, claims payments due to
bankrupt providers. This amount does not include the amount for claims
withheld for non-receipt of cost reports. Amounts must be provided for both HI
and SMI, if applicable. (CAFM Contractors only).
CAFM contractors should obtain this amount from their shared system. The
amount reported on this survey must agree to the applicable portion reported on
the Other Liabilities (footnote) line of the year end Form CMS-750, Statement
of Financial Position. The amount should include claims held in accordance
with CR 5047, Hold on Medicare Payments.
4) Outstanding Checks – The amount of checks and EFT payments that have been
issued, but have not cleared the Medicare contractor’s banking institution.
Amounts must be provided for both HI and SMI, if applicable.
CAFM contractors should obtain this amount from their banking institution or
internally generated documentation. The amount reported on the survey must
agree to outstanding check amount reported on the September 1522, Monthly
Contractor Financial Report.
HIGLAS contractors should obtain this amount from their Summary 2 Trial
Balance, GL account 212001 - Accounts Payable Disbursements in Transit.

5) Health Professional Shortage Area payments (HPSA) – the bonus amount paid
to physicians for eligible services rendered in zip code areas that fall fully
within a designated HPSA area or are dominant to the area based on a
determination by the U.S. Postal Service and/or;
Physician Scarcity Area (PSA) – the bonus amount paid to the primary care and
specialty physicians providing eligible services in the counties with the lowest
20% ratio of primary care or specialty physicians to Medicare beneficiaries
and/or;
Transitional Outpatient Payments (TOPs) - the amount paid to rural hospitals
having 100 or fewer beds that are not classified as a sole community hospital.
(Fiscal intermediaries ONLY)
If PSA/HPSA and/or TOPs payments were disbursed on or before the last day
of the quarter/month, enter amount as zero. If PSA/HPSA and/or TOPs
payments are disbursed on or after the first day of the quarter/month, provide
the amount of the payments. Contractors must provide these amounts for both
HI and SMI, if applicable.
CAFM contractors should obtain this information from their shared system, if
applicable.
HIGLAS contractors should obtain these amounts from their 810H and 810
files, if applicable. HIGLAS contractors should also provide a footnote to
disclose whether the amounts indicated for these payments are included in GL
account 216002, Entitlement Benefit Due/Payable – Adjudicated Claims.
Time Account Balances (Attachment IV)
The CMS reports the aggregate total Part A and total Part B Time Account balances as
Medicare trust fund “Cash and Other Monetary Assets” on the balance sheet in its annual
CMS Financial Report. Previously, these account balances were obtained from the Form
CMS-750 reports; however, the year-end 750 due date is typically extended until after
annual financial statements must be completed. Therefore, time account balances as of
September 30, FY end, must be submitted as part of the attached Benefits Payable Survey
– Attachment IV. Fiscal intermediaries should prorate their time account balances
between HI and SMI.
Due Dates
The annual Joint Signature Memorandum outlining the accelerated financial reporting
timeframes for FY end Medicare contractor financial reports will provide the due date for
the Benefits Payable Survey (Attachments I, II and/or III) as well as the Time Account
Balance information (Attachment IV).
Attachment 1
Contractor No. ______ HI BENEFITS PAYABLE SURVEY
INTERMEDIARY For Period Ending: September 30, 20xx
1. PIP Providers
Value of the First PIP Cycle Paid in the ensuing month ___________
for the end of the month being reviewed. (If the payment cycle has not been run,
please provide an estimate of this amount.
Do not include Pass Through Costs.)
NOTE: HIGLAS contractors should obtain this amount from their
810 interface file.
2. Claims on the Payment Floor (in dollars) ___________
(CAFM Contractors – Amount must agree to amount reported on the
September Form CMS-750)
NOTE: HIGLAS contractors should obtain this amount from their
Summary 2 Trial Balance GL account 216002, Entitlement
Benefit Due/Payable – Adjudicated Claims.
3. Claims on Hold (in dollars) – CAFM contractors ONLY ___________
(Amount should be obtained from the Other Liabilities line on the
Form CMS-751)
4. Outstanding Checks (in dollars) ___________
(Amount must include outstanding EFTs and agree to the
outstanding check amount on the September Form CMS-1522)
NOTE: HIGLAS contractors should obtain this amount from their
Summary 2 Trial Balance GL account 212001, Accounts Payable
Disbursements in Transit.
5. PSA/HPSA/TOPS payments (in dollars) ___________
(If payments were disbursed on or before the last day of the
quarter/month, enter amount as zero. If payments are disbursed
after the 1
st
day of the quarter/month, provide the amount of the payments)
NOTE: HIGLAS contractors should obtain these amounts from their
810H and 810 files, if applicable. HIGLAS contractors should also provide a
footnote to disclose whether the amounts indicated for these payments are
included in GL account 216002, Entitlement Benefit Due/Payable – Adjudicated
Claims
Attachment 2
Contractor No. ______ SMI BENEFITS PAYABLE SURVEY
INTERMEDIARY For Period Ending: September 30, 20xx
1. Claims on the Payment Floor (in dollars) ___________
(CAFM Contractors – Amount must agree to amount reported on the
September Form CMS-750)
NOTE: HIGLAS contractors should obtain this amount from their
Summary 2 Trial Balance GL account 216002, Entitlement
Benefit Due/Payable – Adjudicated Claims.
2. Claims on Hold (in dollars) – CAFM contractors ONLY ___________
(Amount should be obtained from the Other Liabilities line on the
Form CMS-751)
3. Outstanding Checks (in dollars) ___________
(Amount must include outstanding EFTs and agree to the
outstanding check amount on the September Form CMS-1522)
NOTE: HIGLAS contractors should obtain this amount from their
Summary 2 Trial Balance GL account 212001, Accounts Payable
Disbursements in Transit.
4. PSA/HPSA/TOPS payments (in dollars) ___________
(If payments were disbursed on or before the last day of the
quarter/month, enter amount as zero. If payments are disbursed
after the 1
st
day of the quarter/month, provide the amount of the payments)
NOTE: HIGLAS contractors should obtain these amounts from their
810H and 810 files, if applicable. HIGLAS contractors should also provide a
footnote to disclose whether the amounts indicated for these payments are
included in GL account 216002, Entitlement Benefit Due/Payable – Adjudicated
Claims
Attachment 3
Contractor No. ______ BENEFITS PAYABLE SURVEY
CARRIER For Period Ending: September 30, 20xx
1. Claims on the Payment Floor (in dollars) ___________
(CAFM Contractors – Amount must agree to amount reported on the
September Form CMS-750)
NOTE: HIGLAS contractors should obtain this amount from their
Summary 2 Trial Balance GL account 216002, Entitlement
Benefit Due/Payable – Adjudicated Claims.
2. Claims on Hold (in dollars) – CAFM contractors ONLY ___________
(Amount should be obtained from the Other Liabilities line on the
Form CMS-751)
3. Outstanding Checks (in dollars) ___________
(Amount must include outstanding EFTs and agree to the
outstanding check amount on the September Form CMS-1522)
NOTE: HIGLAS contractors should obtain this amount from their
Summary 2 Trial Balance GL account 212001, Accounts Payable
Disbursements in Transit.
4. PSA/HPSA payments (in dollars) ___________
(If payments were disbursed on or before the last day of the quarter,
enter amount as zero. If payments are disbursed after the 1
st
day of the
quarter, provide the amount of the payments)
NOTE: HIGLAS contractors should obtain these amounts from their 810H and
810 files, if applicable. HIGLAS contractors should also provide a footnote to
disclose whether the amounts indicated for these payments are included in GL
account 216002, Entitlement Benefit Due/Payable – Adjudicated Claims
Attachment 4
FEDERAL HEALTH INSURANCE TIME ACCOUNT
Contractor No. ______
INTERMEDIARY For Period Ending: September 30, 20xx
Part A Balance (in dollars) ____________
Part B Balance (in dollars): ____________
FEDERAL SUPPLEMENTARY MEDICAL INSURANCE
TIME ACCOUNT
Contractor No. ______
CARRIER For Period Ending: September 30, 20xx
Part B Balance (in dollars) ____________
400.24 - Exhibit 24 – Benefits Payable Trending Analysis Procedures
(Rev. 105, Issued: 08-25-06, Effective/Implementation: 09-30-06)
Objective
To ensure that benefit payable balances reported on the survey are reasonable, Medicare
contractors are required to perform trending procedures. Trending procedures can be used
as an important tool to identify potential errors, omissions, system weaknesses, or
inappropriate patterns of adjustments or accumulation. Trending procedures involve
comparisons of current fiscal year (FY) benefit payable data to prior year benefit payable
data submitted on the Benefits Payable surveys.
Compare Current Year Amounts with Comparative Financial Data
In comparing current-period financial results with prior-period financial results, there is
an implied assumption that the volume of activity in the two periods is comparable. If
there has been a substantial change in volume, it is necessary to take this change into
account and to quantify the change, when making the comparisons. For example, if a
contractor's PIP balance has increased by 10 percent, it is necessary to determine and
document the reason for the increase. The increase may be the result of new PIP
providers or increased settlement activity.
Understand Identified Variances and Document the Results
Medicare contractors must identify and provide an explanation for variances that meet the
thresholds outlined in these procedures. If an explanation does not adequately describe
the variance, the Medicare contractors must perform additional procedures such as a
review of detail transactions to identify the underlying cause(s) of any unusual changes.
The causes for the variances should be quantified. For example, if the change was
attributable to a change in the number of claim cycles, then include the number of
additional claims on the payment floor attributed to the additional cycles as well as the
reason why additional cycles were added.
Methodology
The primary reason for performing trend analysis is to focus on the change in the ending
balances of PIP, claims on the payment floor, and outstanding checks. All explanations
should be available for review by CMS, Office of the Inspector General, Government
Accountability Office and /or other related parties.
Each Medicare contractor must perform the following steps on a year end basis,
beginning with FY ending September 30, 2006. The CFO for Medicare Operations' must
submit the explanations via email as evidence that he/she has reviewed the trending
explanations. To properly apply trending procedures, it is necessary to complete the
following steps:
Benefits Payable Trending Analysis Procedures for FIs and carriers
Step (1)
Compare the value of the first PIP cycle paid in the ensuing month for the end of
the month being reviewed, the claims on the payment floor amount, and the
outstanding check amount reported on the current FY’s Benefits Payable survey
to the same line items reported on the prior year’s Benefits Payable survey (i.e.
9/30/06 vs. 9/30/05) for all lines of business applicable to each contractor number.
Calculate the dollar and percentage difference for each item. (See Attachments I,
II, and III for the required formats).
NOTE: Trending on the amount of Claims on hold and Physician Scarcity Area
(PSA) payments, Health Professional Shortage Area (HPSA) payments, and
Transitional Outpatient Payments (TOPs) will not be required until FY 2007.
Step (2)
Verify that the dollar amount for each item is supported by lead schedules and/or
detailed documentation. Any errors or misstatements identified as a result of this
analysis must be corrected prior to the submission of the Form CMS-750 report,
the Form CMS-1522 report and/or CMS Balance Sheet, CMS Income Statements
and CMS Summary 2 Trial Balance.
Step (3)
PIP (for FIs only)
Provide explanations where the dollar amount change is at least +/-$2 million or
equates to a 100 percentage change.
Claims on the payment floor
Provide explanations where the dollar amount change is at least +/- $10 million or
equates to a 100 percentage change.
Outstanding checks
Provide explanations where the dollar amount change is at least +/- $3 million or
equates to a 100 percentage change.
Step (4)
Document conclusions in a summary memorandum (See Attachment IV) to be
included with Attachments I, II, and III and provide to the CFO for Medicare
Operations for submission to CMS.
Due Date
The analysis must be submitted by the CFO of Medicare Operations via email to the
Division of Financial Reporting and Policy (DFRP) contact identified in the Joint
Signature Memorandum outlining the accelerated financial reporting timeframes for
Medicare contractor financial reports and is due the day following the submission of the
Benefits Payable Survey by 8:00 pm Eastern Daylight Time. If a copy of the analysis is
signed by the CFO, scanned, and attached to the email sent to the DFRP contact, the CFO
is not required to send the email directly. If this date occurs on a holiday or a weekend,
the analysis must still be submitted by this due date. Please notify the DFRP contact if a
problem arises.
The DFRP contact will review the summary memorandums and the analysis schedules
and may request additional explanations and/or documentation to support the Medicare
contractors' analysis schedules. The DFRP contact will contact the Medicare contractor
by phone to request any additional documentation needed to support existing variances.
A response is requested as soon as possible, but no later than two days from the day of
request.
410 – Unsolicited Voluntary Refunds
410.1 - General Information
(Rev. 50, 07-30-04)
All Medicare contractors receive unsolicited/voluntary refunds (i.e. monies received not
related to an open accounts receivable). Following are detailed instructions on how to
identify, process, track and report unsolicited/voluntary refund checks received from
providers/physicians/suppliers, and other entities (e.g., beneficiaries, insurers, employers,
third party administrators (TPAs), etc.). These instructions shall not supersede other
CMS guidance provided regarding the recovery and collection action on “demanded”
debt, where an accounts receivable has already been established. If monies are received
and the results of a contractor’s investigation identify the existence of an established
receivable, then the refund shall not be considered an “unsolicited/voluntary refund”
within the context of the following instructions, and would not be reported on Exhibit 2
of these instructions (see section 410.9).
Intermediaries generally receive unsolicited/voluntary refunds from providers in the form
of an adjustment bill, but may receive some unsolicited/voluntary refunds from providers
and third party payers as checks. Carriers generally receive checks from physicians,
suppliers and third party payers. Substantial funds are returned to the trust funds each
year through such unsolicited/voluntary refunds.
Acceptance/deposit of the voluntary refund check in no way limits the rights of the
Federal Government or any of its agents to pursue any appropriate criminal, civil, or
administrative remedies arising from or relating to these or any other claims.
410.2 - Office of the Inspector General (OIG) Initiatives

(Rev. 50, 07-30-04)
The OIG, working with the Department of Justice and CMS, has initiatives to help
combat health care fraud and abuse and to encourage health care
providers/physicians/suppliers, and other entities to comply with the rules and regulations
of Federal health care programs. Some of these initiatives include guidance, corporate
integrity agreements (CIAs), and the OIG Self-Disclosure Protocol. The OIG Self-
Disclosure Protocol is voluntary while the CIAs are mandatory. These initiatives are
designed to ensure that the providers/physicians/suppliers, and other entities refund
inappropriately received Medicare monies back to the trust funds.
CIAs are entered into between a health care provider/physician/supplier/other entity and
OIG as part of a global settlement of a fraud investigation. Under the CIA (which can be
for a period ranging from 3 to 5 years), the provider/physician/supplier or other entity is
required to undertake specific compliance obligations, such as designating a compliance
officer, undergoing training, and auditing. The provider/physician/supplier or other
entity must report regarding their compliance activities on an annual basis to the OIG,
which is responsible for monitoring the agreements.
The OIG Self-Disclosure Protocol was produced by the OIG to provide guidance to
health care providers/physicians/suppliers and other entities that decide to voluntarily
disclose irregularities in their dealings with the Federal health care programs. The
decision to follow the OIG Self-Disclosure Protocol rests exclusively with the
provider/physician/supplier and other entity. The OIG Self-Disclosure Protocol is
intended to facilitate the resolution of only matters that, in the provider/physician/supplier
and other entity’s reasonable assessment, potentially violates Federal, criminal, civil, or
administrative laws. It should be noted that providers/physicians/suppliers and other
entities who self-disclose to the OIG sign an agreement stating that any refunds submitted
as part of the self-disclosure process are not subject to appeal.
410.3 - Unsolicited/Voluntary Refund Accounts
(Rev. 50, 07-30-04)
All Medicare systems shall be able to separately distinguish and track
unsolicited/voluntary refund checks which result from a 1) provider/physician/supplier
and other entity under a CIA; 2) Provider/physician/supplier and other entity under the
OIG Self-Disclosure Protocol; and 3) Straight Refund (a straight refund is a refund from
a provider/physician/supplier, or other entity who is not under a CIA nor the OIG Self-
Disclosure Protocol). All Medicare systems shall have the ability to identify and produce
a report that distinguishes a refund as a CIA, OIG Self-Disclosure Protocol, or straight
refund at the point of disposition (i.e., after investigation of the origin of the refund).
To assist in identifying providers/physicians/suppliers under a CIA, Medicare contractors
should access the OIG Web site (http://www.oig.hhs.gov/fraud/cias.html) for a list of all
providers/physicians/suppliers, and other entities under a CIA. The OIG Web site will
also give the effective date of the CIA. To obtain the termination date of the CIA, click
on the CIA agreement. The time period of the CIA is contained within the agreement. If
the Web site does not provide enough information to determine whether a CIA agreement
is in existence, the contractor shall contact the provider as part of their
investigation/resolution of the unsolicited/voluntary refund. Because OIG Self-
Disclosure Protocol agreements are voluntary, contractors may not be aware of this
agreement unless a provider/physician/suppliers or other entity specifically notifies them.
Providers/physicians/suppliers under an OIG Self-Disclosure Protocol agreement are not
given on the OIG Web site. The OIG will send a letter directing the
provider/physician/supplier to refund money back to the Medicare contractor when the
OIG has completed the Self-Disclosure matter and determined that an
unsolicited/voluntary refund should be collected rather than a civil settlement pursued. A
copy of the letter is included as Exhibit 3. The OIG will also send a copy of the letter to
the attention of the Chief Financial Officer for Medicare Operations at the Medicare
contractor. The OIG will direct the provider/physician/supplier to identify that the refund
check is the result of an OIG Self-Disclosure Protocol agreement. The
provider/physician/supplier will have 30 days to refund the contractor. If the contractor
does not receive the refund within 30 days, the contractor shall notify the Office of
Counsel to the Inspector General (OCIG) attorney assigned to the OIG Self-Disclosure
Protocol matter, as identified in the letter.
410.4 - Receiving and Processing Unsolicited/Voluntary Refund Checks
When Identifying Information is Provided
(Rev. 315, Issued: 05-17-19, Effective: 06-18- 19, Implementation: 06-18-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a
beneficiary's Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
The following instructions shall not supersede the present Program Integrity Manual
(PIM) that references procedures for handling unsolicited refunds where there is a
voluntary repayment and referral to law enforcement. The following procedures shall be
followed when unsolicited/voluntary refund checks are received:
1) Do not return any check submitted by a provider/physician/supplier and other
entities that is made payable to the Medicare program.
2) To ensure that repayment of Medicare funds is handled properly, Medicare
contractors shall deposit such a check within 24 hours of receipt in accordance
with Chapter 5, Financial Reporting Manual, section 100.3 and record the check
in the account entitled “Other Liabilities – Unapplied Receipts” per Form CMS-
750 instructions found in Chapter 5, Financial Reporting, Section 210.
3) If any checks are not deposited within the 24-hour period, contractors shall
record those undeposited checks in the account entitled “Assets/Cash –
Undeposited Collections” per Form CMS-750 instructions found in Chapter 5,
Financial Reporting, Section 210. Medicare contractors shall implement
internal controls to ensure the safeguarding of these Medicare checks until
deposit.
4) If the specific Patient/Medicare beneficiary identifier information was provided,
the contractor shall deposit the check and make/initiate the appropriate
adjustments, depending on the entity making the refund and the purpose of the
refund, either to the claims and/or to the claim history file within 60 days from
the check’s date of deposit for Non-Medicare Secondary Payer (MSP), or 100
days from the initial ECRS inquiry for MSP. For those contractors whose
checks are received through a locked box, appropriate claims adjustments shall
be updated within 60 days of receipt of the bank’s notification of deposit for
Non-MSP, and 100 days from the initial ECRS inquiry for MSP.
5) If the provider/physician/supplier, or other entity is not participating in the Self-
Disclosure Protocol, contractors shall ensure that any MSN, or Remittance
Advice, generated as the result of the claims adjustment contains appeals
language, where appropriate. If necessary, contractors should determine the
proper handling of unsolicited/voluntary refunds on any open or re-openable
cost report.
6) No appeal rights shall be afforded, as stated in Exhibit 1, if the
provider/physician/supplier, or other entity 1) does not submit the specific
Patient/Medicare beneficiary identifier information, or 2) is participating in a
Self-Disclosure Protocol agreement.
7) The Medicare contractor shall establish an accounts receivable in the Medicare
system that shall be recognized on line 2a, New Accounts Receivable on Form
CMS-751 report within 60 days after the deposit of the voluntary refund for
Non-MSP, or 100 days from initial ECRS inquiry for MSP. In addition, the
Medicare contractor shall reduce the “Other Liabilities” account for the same
amount, and shall apply the refund to the established accounts receivable and
recognize the collection on line 4a, Cash/Check Collections on Form CMS-751
report.
8) The accounts receivable shall be established using the last name of the debtor
that issued the check or on whose behalf the check was issued, as well as the
debtor’s employer/tax identification number and/or provider or beneficiary
number. If the debtor’s employer/tax identification number or provider or
beneficiary number is unavailable, then the first four letters of the debtor’s name
and last four digits of the bank account number on the check shall be used as
identifying information for setting up the accounts receivable. All Medicare
systems shall have the ability to manually complete this procedure.
9) If the amount of the unsolicited/voluntary refund check exceeds the amount of
the original claim, Medicare contractors shall check all categories of open
account(s) receivable for that provider/physician/supplier or other entity
including those established as a result of medical review, benefit integrity (BI)
review, cost reports, other overpayment demands, and MSP demands. If an
outstanding receivable is identified, the contractor shall apply the remaining
amount of the unsolicited/voluntary refund to the outstanding receivable
balance. If there are multiple outstanding accounts receivables, then the excess
funds should be applied to the oldest accounts receivable first – interest then
principal.
10) Medicare contractors shall not automatically refund excess recoupments to the
provider/physician/supplier, or other entity. Contractors shall only refund
excess recoupments when no other outstanding accounts receivable exists, or
written documentation/evidence clearly supports that Medicare is not entitled to
the money or was not the intended recipient of the refund check. Contractors
shall follow the non-MSP provider/physician/supplier refund process when
encountering MSP provider/physician/supplier unsolicited/voluntary refunds.
Monies voluntarily sent in from beneficiaries (or a representative of) and/or
insurers or other third party payers may be refunded only if COBC determines,
after 100 days, no issue exists or an issue exists which results in the lead
contractor identifying Medicare’s claim to be less than the refunded amount.
For example, many times an attorney may remit payment for the total
conditional amount prior to a formal demand.
11) The Medicare contractor shall be responsible for completing Exhibit 1 (or
facsimile thereof) as appropriate and reporting it on Exhibit 2.
12) Contractors are not required to report the established accounts receivable on the
Physician Supplier Overpayment Reporting System (PSOR). (This requirement
does not preclude the contractor from reporting the receivable on the PSOR for
non-MSP, if current systems already do so. The contractor shall not report MSP
accounts receivable on the PSOR.)
410.5 - Handling Checks or Associated Correspondence with
Conditional Endorsements
(Rev. 50, 07-30-04)
Conditional endorsements are statements on the face of the check or associated
correspondence, which might suggest that the payer has discharged its obligation by
writing “paid in full” or like phrases that the payer intends as satisfaction/ extinguishment
of the debt. Guidelines from the General Accounting Office (GAO) state that agencies
must be extremely careful to avoid an unintended accord and satisfaction (i.e., an
agreement to accept a payment in full for an amount less than the amount claimed).

The following instruction shall be applied to checks or associated correspondence with a
conditional endorsement:
1) Medicare contractors shall deposit such a check within 24 hours of receipt in
accordance with CMS’s Medicare Financial Management Manual, Chapter 5
Financial Reporting, section 100.3 and record the check in the account entitled
“Other Liabilities – Unapplied Receipts” per Form CMS-750 instructions found
in Chapter 5, Financial Reporting, Section 210.
2) If any checks are not deposited within a 24-hour period, contractors shall record
those checks in the account entitled “Assets/Cash – Undeposited Collections”
per Form CMS-750 instructions found in Chapter 5, Financial Reporting,
section 210. Medicare contractors shall implement internal controls to ensure
the safeguarding of these Medicare checks until deposit.
3) Contractors shall immediately notify the debtor and/or the entity on whose
account the check is drawn, if not the debtor, by certified mail. The following
statement is suggested: This is to acknowledge the receipt of the repayment
in the amount of $XX, check number XX. The matter is being researched;
however, the amount of the repayment may be insufficient to discharge the
obligation and the debt may not be fully extinguished.
4) The check(s) shall than be processed as outlined under section 410.4 or 410.6 as
applicable.
The infrequent receipt of checks with conditional endorsements should not negatively
impact your production process. The standard letter needed to meet this requirement
shall be added to your automated letter processing or generated from a personal
computer.
410.6 - Receiving and Processing Unsolicited/Voluntary Refund Checks
When Identifying Information is not Provided
(Rev. 315, Issued: 05-17-19, Effective: 06-18- 19, Implementation: 06-18-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a
beneficiary's Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
After depositing unsolicited/voluntary refund checks in accordance with section 410.4
above, Medicare contractors shall do the following:
For Non-MSP Checks
1) If no specific Patient/Medicare beneficiary identifier information was provided
with the unsolicited/voluntary refund, the contractor shall contact the
provider/physician/supplier, or other entity sending the refund check for further
information. Exhibit 1 (overpayment refund) contains the minimum claim
specific data necessary to process the refund. The contractor should use this
form during phone inquiry or attach it to a letter to the
provider/physician/supplier requesting further information regarding the
submitted refund.
2) When there is no identifying information provided, the contractor shall perform
the research necessary to obtain the minimum data required to meet the
reporting requirements in Exhibit 2 (Summary Report). If the information is
being collected via a telephone inquiry, the contractor employee conducting the
inquiry shall inform the provider/physician/supplier, or other entity verbally that
if the specific Patient/ Medicare beneficiary identifier information is not
provided, no appeal rights can be afforded.
The minimum reporting data shall include:
a. Provider/physician/supplier, or other entity’s name, number, and Tax ID
number.
b. Identification of whether the provider/physician/supplier, or other entity
has a CIA with the OIG or are under the OIG Self-Disclosure Protocol;
and whether it is a straight refund (i.e., a provider not under a CIA or OIG
Self-Disclosure Protocol).
c. The reason(s) for each refund.
d. The total number of refund checks (in the case of a check with multiple
providers/reason codes, each instance shall be counted separately).
e. The total dollar amount of refunds.
3) Medicare contractors shall have 60 days from deposit of the check to obtain the
minimum claim specific data required to apply the check. The contractor shall
take at least one documented follow-up action during the 60-day period to
obtain the data.
4) If the minimum claim specific data required to apply the refund is obtained
from the provider/physician/supplier, or other entity within 60 days from the
check’s date of deposit, the contractor shall make/initiate any appropriate
adjustments to the identified claims and/or the claim history file for the amount
of the refund. The contractor shall establish an account(s) receivable and apply
the balance of the check to the account(s) receivable from the “Other
Liabilities” account within 60 days after the deposit of the voluntary refund.
The contractor shall ensure that any Remittance Advice or MSN generated as a
result of the claim adjustment contains the appropriate appeals language, if
applicable.
5) If the minimum claim specific data required to apply the refund is not obtained
from the provider/physician/supplier, or other entity within 60 days from the
check’s date of deposit, the “Other Liabilities” account shall be reduced and an
accounts receivable due to a straight refund shall be established for the amount
of the unapplied unsolicited/voluntary refund. All Medicare systems shall allow
contractors the ability to set up accounts receivable using either the
provider/physician/supplier, or other entity or beneficiary number.
6) In both instances, the Medicare contractor shall establish an accounts receivable
in the Medicare system that shall be recognized on line 2a, New Accounts
Receivable on Form CMS-751 report within 60 days after the deposit of the
voluntary refund. In addition, the Medicare contractor shall perform a
simultaneous transaction to apply the refund to the established accounts
receivable and recognize the collection on line 4a, Cash/Check Collections on
Form CMS-751 report.
7) The accounts receivable shall be established using the last name of the debtor
identified on the check, as well as the debtor’s employer/tax identification
number and/or provider or beneficiary number. If the debtor’s employer/tax
identification number or provider or beneficiary number is unavailable, then the
first four letters of the debtor’s name and last four digits of the bank account
number on the check shall be used as identifying information for setting up the
accounts receivable. All Medicare systems shall have the ability to manually
complete this procedure.
8) If the amount of the unsolicited/voluntary refund check exceeds the amount of
the original claim, Medicare contractors shall check all categories of open
account(s) receivable for that provider/physician/supplier including those
established as a result of medical review, BI review, cost reports, other
overpayment demands, and MSP demands. If an outstanding receivable is
identified, the contractor shall apply the remaining amount of the
unsolicited/voluntary refund to the outstanding receivable balance. If there are
multiple outstanding accounts receivables, then the excess funds should be
applied to the oldest accounts receivable first – interest then principal.
9) Medicare contractors shall not automatically refund excess recoupments to the
provider/physician/supplier, or other entity. Contractors shall only refund
excess recoupments when no other outstanding accounts receivable exists, or
written documentation/evidence clearly supports that Medicare is not entitled to
the money or was not the intended recipient of the refund check.

10) The Medicare contractor shall be responsible for ensuring the completion of
Exhibit 1 (or facsimile thereof) and reporting it on Exhibit 2 upon final
disposition of the unsolicited/voluntary refund (i.e., after investigation of the
origin of the refund).
11) Contractors are not required to report the established accounts receivable on the
PSOR. (This requirement does not preclude the contractor from reporting the
receivable on the PSOR if current systems already do so.)
For MSP Checks
1) The Medicare contractor shall determine if there is an existing case and/or
accounts receivable. If this is an existing case and/or accounts receivable, the
contractor shall follow normal recovery procedures. If there is no case and/or
accounts receivable, and there is indication of MSP involvement, the contractor
shall send an MSP inquiry via the Electronic Correspondence Referral System
(ECRS) to the MSP Coordination of Benefits Contractor (COBC) within 20
days from the check’s date of deposit. The 45-day correspondence timeframe is
not appropriate for addressing checks either solicited or unsolicited.
Contractors shall identify checks during the initial mail sort and place a priority
on their resolution and distribution. When referring information to the COBC
for MSP investigation, the contractor shall forward all pertinent data. All
fields on the ECRS Inquiry screen shall be completed if the data is
available on the returned check or any accompanying correspondence.
Information in the informant fields such as telephone numbers, point of
contact, etc. are critical to COBC development efforts.
2) Medicare contractors shall only allow 100 days from the date of the ECRS
inquiry for a response from the COBC before taking action with respect to the
“unapplied receipts.” This time period will also allow for the COBC to develop
the case. If additional information is obtained after the initial inquiry that would
help facilitate the processing and research of information, the COBC Consortia
Representative shall be contacted and provided the additional information, via
fax or telephone, to assist in completing the research. The contractor shall not
send a second ECRS inquiry. A total of 120 days from the check’s date of
deposit will be allowed to bring closure to the unapplied receipt.
3) If the minimum reporting information from the MSP COBC is provided within
100 days from the initial ECRS inquiry, the contractor shall make/initiate any
appropriate adjustments to either the identified claims and/or the claim history
file for the amount of the refund, depending on the entity making the refund and
the purpose of the refund. The Medicare contractor shall establish an account(s)
receivable and apply the balance of the check to the account(s) receivable from
the “Other Liabilities” account. If as a result of applying the voluntary refund
the contractor identifies additional dollars specific to the issue in CWF, a
demand letter shall be sent for the remaining amount owed.
4) If, within 100 days from the initial ECRS inquiry, 1) the minimum reporting
information is not provided, 2) a response has not been received from the MSP
COBC, or 3) a response from the COBC indicates they could not obtain a
response (e.g., CM Code 62), Medicare contractors shall establish an accounts
receivable and apply the balance of the check to the account(s) receivable from
the “Other Liabilities” account. For COBC no response codes specific to a
provider/physician/supplier unsolicited/voluntary refund, contractors should do
the full claim adjustment but use a non-MSP reason (i.e., billed in error), which
would then not need an MSP record to be established on CWF. The contractor
shall report the refund in Exhibit 2 (Unsolicited/Voluntary Refund - Summary
Report), and annotate with reason code 16. In addition, Exhibit 1 and/or the
contractor’s supporting documentation shall specify the refund as received with
no reason for refund and/or no MSP response.
5) The Medicare contractor shall establish an accounts receivable in the Medicare
system and that shall be recognized on line 2a, New Accounts Receivable on
Form CMS-M751 report within 100 days after the initial ECRS inquiry. In
addition, the Medicare contractor shall perform a simultaneous transaction to
apply the refund to the established accounts receivable and recognize the
collection on line 4a, Cash/Check Collections on Form CMS-M751 report. The
contractor shall initiate normal MSP recovery action for any remaining
outstanding balance owed.
6) The accounts receivable shall be established using the last name of the debtor
that issued the check or on whose behalf the check was issued, as well as the
debtor’s employer/tax identification number and/or provider or beneficiary
number. If the debtor’s employer/tax identification number or provider or
beneficiary number is unavailable, then the first four letters of the debtor’s name
and last four digits of the bank account number on the check shall be used as
identifying information for setting up the accounts receivable. All Medicare
systems shall have the ability to manually complete this procedure.
7) If the amount of the unsolicited/voluntary refund check exceeds the amount of
the original claim, Medicare contractors shall check all categories of open
account(s) receivable for that provider/physician/supplier or other entity
including those established as a result of medical review, BI review, cost
reports, other overpayment demands. If an outstanding receivable is identified,
the contractor shall apply the remaining amount of the unsolicited/voluntary
refund to the outstanding receivable balance. If there are multiple outstanding
accounts receivables, then the excess funds should be applied to the oldest
accounts receivable first – interest then principal.
8) Medicare contractors shall not automatically refund excess recoupments to the
provider/physician/supplier, or other entity. Contractors shall only refund
excess recoupments when no other outstanding accounts receivable exists, or
written documentation/evidence clearly supports that Medicare is not entitled to
the money or was not the intended recipient of the refund check. Contractors
shall follow the non-MSP provider/physician/supplier refund process when
encountering MSP provider/physician/supplier unsolicited/voluntary refunds.
Monies voluntarily sent in from beneficiaries (or a representative of) and/or
insurers or other third party payers may be refunded only if COBC determines,
after 100 days, no issue exists or an issue exists which results in the lead
contractor identifying Medicare’s claim to be less than the refunded amount.
For example, many times an attorney may remit payment for the total
conditional amount prior to a formal demand.
9) The Medicare contractor shall be responsible for ensuring the completion of
Exhibit 1 (or facsimile thereof) and reporting it on Exhibit 2 upon final
disposition of the unsolicited/voluntary refund (i.e., after investigation of the
origin of the refund).
10) Contractors shall not report the MSP accounts receivable on the PSOR.
410.7 - CMS Reporting Requirements With the Exception of MSP
(Rev. 122, Issued: 05-25-07, Effective: 06-25-07, Implementation: 06-25-07)
Contractors are exempt from including MSP unsolicited/voluntary refunds in their
unsolicited/voluntary refund reports. Contractors shall not make any system changes to
exclude MSP if the system already includes MSP in the reporting based on compliance
with the previous instructions.
With the exception noted above contractors shall report, in the provided Exhibit 2 format,
the receipt of all unsolicited/voluntary refund checks from providers/physicians/suppliers.
The reports may be run quarterly but contractors shall only submit reports to CMS when
requested. All contractors shall be required to submit a “negative” report, when reports
are requested, even if they have a $0 dollar reporting.
NOTE: HIGLAS will supply a report upon user request.
410.8 - Overpayment Refund Form
(Rev. 50, 07-30-04)
Exhibit 1 displays the required information needed to research and document
unsolicited/voluntary refunds received. Medicare contractors shall maintain files that
include copies of all unsolicited/voluntary refunds received and the completed report,
Exhibit 1. These documents shall serve as a tracking mechanism for audit trail purposes.
Contractors are not required to use Exhibit 1 verbatim; however, the alternative
documents used shall contain, at a minimum, all of the elements outlined in Exhibit 1.
410.9 - Unsolicited/Voluntary Refund Checks – Summary Report
(Rev. 50, 07-30-04)
Exhibit 2 displays reporting requirements for all CMS unsolicited/voluntary refund
checks. The contractor shall report all unsolicited/voluntary refunds from
providers/physicians/suppliers, and other entities identified on the OIG Web site, in
addition to those that identify themselves as having a CIA, OIG Self-Disclosure Protocol,
and/or straight refund. The following data shall be captured: the
provider/physician/supplier, or other entity’s name(s), provider number(s) Tax ID(s),
reason code for refund, number of refund checks, and the total dollar amount of refund
checks. Reason code #16 shall be used to identify that no reason was provided for the
refund.
The contractor is not required to list each check received for the quarter individually, but
may total all the checks on one line for the same provider/physician/supplier. Therefore,
multiple checks for the same provider/physician/supplier when totaled shall be grouped
by like categories for the following:
1. Same Provider/Physician/Supplier
2. Same Reason Code
3. CIA category
4. Self-Disclosure category
5. Straight Refund category
Example 1: Ten checks totaling $100.00 are received from Dr. X for Reason Code 02, but
5 checks are under a CIA and 5 checks are a straight refund.
Exhibit Columns:
Column 1, Provider/Physician/Supplier or Other Entity Name(s): Dr. X
Column 2, Provider/Physician/Supplier Number(s): 99999
Column 3, Tax ID Numbers: 9999999999
Column 4, Reason Codes: 02
Column 5, Line 1 CIA, SDP, Straight Refund: CIA
Column 5, Line 2 CIA, SDP, Straight Refund: Straight Refund
Column 6, Line 1 Total Number of Refund Checks: 5
Column 6, Line 2 Total Number of Refund Checks: 5
Column 7, Line 1 Total Amount of Refunds: $50.00
Column 7, Line 2 Total Amount of Refunds: $50.00
Example 2: Ten checks totaling $100.00 are received from Dr. Y, 8 checks are for
Reason Code 02 and 5 of these checks are a CIA and 3 are a straight refund, 2 checks are
for Reason Code 03 and 1 check is a CIA and 1 check is a straight refund.
Exhibit Columns:
Column 1, Provider/Physician/Supplier or Other Entity Name(s): Dr. Y

Column 2, Provider/Physician Supplier Number9s): 99999
Column 3, Tax ID Numbers: 9999999999
Column 4, Line 1 Reason Codes: 02
Column 4, Line 2 Reason Codes: 02
Column 4, Line 3 Reason Codes: 03
Column 4, Line 4 Reason Codes: 03
Column 5, Line 1 CIA, SDP, Straight Refund: CIA
Column 5, Line 2 CIA, SDP, Straight Refund: Straight Refund
Column 5, Line 3 CIA, SDP, Straight Refund: CIA
Column 5, Line 4 CIA, SDP, Straight Refund: Straight Refund
Column 6, Line 1 Total Number of Refund Checks: 5
Column 6, Line 2 Total Number of Refund Checks: 3
Column 6, Line 3 Total Number of Refund Checks: 1
Column 6, Line 4 Total Number of Refund Checks: 1
Column 7, Line 1 Total Amount of Refunds: $40.00
Column 7, Line 2 Total Amount of Refunds: $20.00
Column 7, Line 3 Total Amount of Refunds: $20.00
Column 7, Line 4 Total Amount of Refunds: $20.00
410.10 – Education
(Rev. 50, 07-30-04)
On an annual basis, the contractor shall include in the newsletter/bulletin the following
information: “The acceptance of a voluntary refund as repayment for the claims
specified in no way affects or limits the rights of the Federal Government, or any of its
agencies or agents, to pursue any appropriate criminal, civil, or administrative remedies
arising from or relating to these or any other claims.”
A provider education article related to this instruction will be available at
http://www.cms.hhs.gov/medlearn/matters shortly after the CR is released. You will
receive notification of the article release via the established "medlearn matters" listserv.
Contractors shall post this article, or a direct link to this article, on their Web site and
include information about it in a listserv message within one week of the availability of
the provider education article. In addition, the provider education article must be
included in your next regularly scheduled bulletin.
411 – Exhibits
(Rev. 50, 07-30-04)
411.1 - Exhibit 1 – Overpayment Refund Form
(Rev. 315, Issued: 05-17-19, Effective: 06-18- 19, Implementation: 06-18-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a
beneficiary's Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
SHALL BE COMPLETED BY MEDICARE CONTRACTOR
Date: ________________________________
Contractor Deposit Control # _____________Date of Deposit: _____________
Contractor Contact Name: ________________________ Phone #: _____________
Contractor Address: _________________________________________________
Contractor Fax: _____________________________________________________
________________________________________________________________________
______________
SHALL BE COMPLETED BY PROVIDER/PHYSICIAN/SUPPLIER, OR OTHER
ENTITY
Please complete and forward to your Medicare contractor. This form, or a similar
document containing the following information, should accompany every
unsolicited/voluntary refund so that receipt of check is properly recorded and applied.
PROVIDER/PHYSICIAN/SUPPLIER OR OTHER ENTITY NAME:
________________________________
ADDRESS: _____________________________________________________________
PROVIDER/PHYSICIAN/SUPPLIER #: _______________ TAX ID #:
______________
CONTACT PERSON: ______________________ PHONE #: _____________________
AMOUNT OF CHECK $: ___________ CHECK #: ___________ CHECK DATE:
______
REFUND INFORMATION
For each claim, provide the following:
Patient Name: ____________________________ Medicare beneficiary identifier:
_____________________
Medicare Claim Number: ___________________ Claim Amount Refunded $:
_________
Reason Code for Claim Adjustment: _______ (Select reason code from list below. Use
one reason per claim.)
(Please list all claim numbers involved. Attach separate sheet, if necessary)
Note: If Specific Patient/Medicare beneficiary identifier Amount data not available for all
claims due to Statistical Sampling, please indicate methodology and formula used to
determine amount and reason for overpayment:
________________________________________
NOTE: If specific patient Medicare beneficiary identifier information is not provided, no
appeal rights can be afforded with respect to this refund. Providers/physicians/suppliers,
and other entities who are submitting a refund under the OIG’s Self-Disclosure Protocol
are not afforded appeal rights as stated in the signed agreement presented by the OIG.
For Institutional Facilities Only:
Cost Report Year (s) ________________________
(If multiple cost report years are involved, provide a breakdown by amount and
corresponding cost report year.)
For OIG Reporting Requirements:
Do you have a Corporate Integrity Agreement with OIG? ___ Yes ___ No
Are you a participant in the OIG Self-Disclosure Protocol? ___ Yes ___No
________________________________________________________________________
______________
Exhibit 1 – Overpayment Refund Form (Cont.)
Reason Codes:
Billing/Clerical: MSP/Other Payer Involvement:
Miscellaneous:
01 – Corrected Date of Service 07 – MSP Group Health Plan Insurance 12 –
Insufficient Doc
02 – Duplicate 08 – MSP No Fault Insurance 13 – Patient
Enroll HMO
03 – Corrected CPT Code 09 – MSP Liability Insurance 14 – Svcs Not
Rendered
04 – Not Our Patient(s) 10 – MSP, Workers Comp. 15 –
Medical Necessity
05 – Mod. Add/Remove (Incl Black Lung) 16 – Other-
Please Specify
06 – Billed in Error 11 – Veterans Administration
_____________________
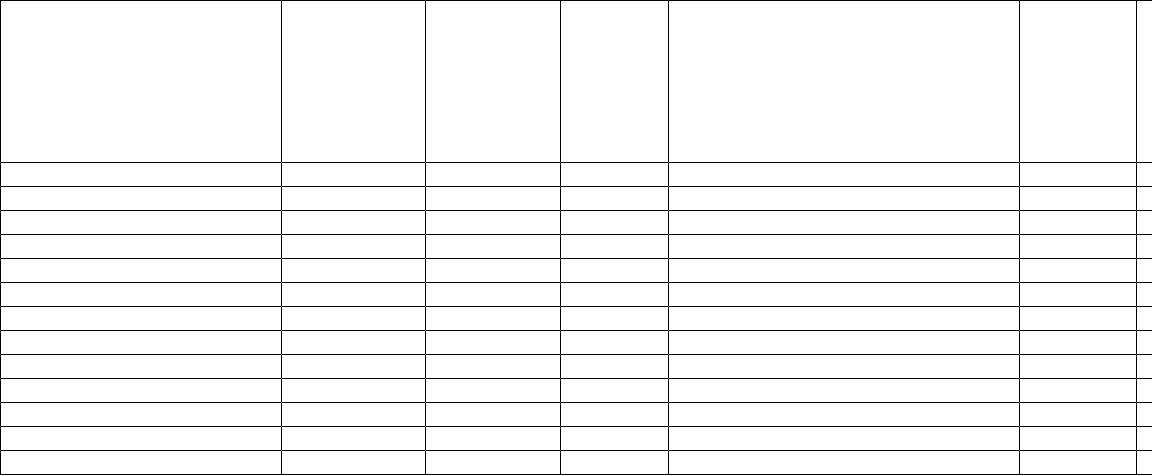
411.2 - Exhibit 2 - Unsolicited/Voluntary Refund Checks Summary Report
(Rev. 50, 07-30-04)
CONTRACTOR’S NAME ___________________________________
CONTRACTOR’S NUMBER (S): _____________________________
REPORTING PERIOD FROM _____________ TO ____________
DATE OF REPORT _____________
(1)
PROVIDER/
PHYSICIAN/
SUPPLIER, OR OTHER
ENTITY
NAME (S)
(2)
PROVIDER/
PHYSICIAN/
SUPPLIER
NUMBER(S)
(3)
TAX ID
NUMBER
(S)
(4)
REASON
CODES*
(5)
PROVIDERS/PHYSICIANS/SUPPLIE
RS, AND OTHER ENTITIES
UNDER A CIA, OIG SELF-
DISCLOSURE OR STRAIGHT
REFUNDS (Choose either A, B, or C
from description below
(6)
TOTAL
NUMBER
OF
REFUND
CHECKS
(
T
O
Example 1:
Dr. X
99999
9999999999
02
CIA
5
$
02
Straight Refund
5
$
Example 2:
Dr. Y
99999
9999999999
02
CIA
5
$
02
Straight Refund
3
$
03
CIA
1
$
03
Straight Refund
1
$
T
*These codes are found on Exhibit 1
A – Providers/Physicians/Suppliers and Other Entities under a CIA
B – Providers/Physicians/Suppliers and Other Entities under OIG Self-Disclosure Protocol
C – Straight Refunds
THIS REPORT SHALL BE USED TO REPORT ALL UNSOLICITED/VOLUNTARY REFUND CHECKS
RECEIVED DURING THIS PERIOD. INCLUDE THOSE REPORTED ON EXHIBIT 1 FOR CIA AND OIG
SELF-DISCLOSURE PROTOCOL PROVIDERS/PHYSICIANS/SUPPLIERS, AND OTHER ENTITIES.
411.3 - Exhibit 3 – OIG Law Enforcement Demand Letter
(Rev. 50, 07-30-04)
DEPARTMENT OF HEALTH & HUMAN SERVICES
Office of Inspector General
Office of Investigations
[Date]
[Provider]
Re: Provider Self-Disclosure
[Provider]
OIG Case Number [CIMS#]
Dear [---------]:
We are writing to follow up on your [date of initial submission] disclosure to the Office
of Inspector General (“OIG”) pursuant to the OIG’s Provider Self-Disclosure Protocol.
Based upon our review of the materials and information you furnished to us, it appears
that [Provider] should refund [$-----] in connection with claims it submitted to
[Medicare/Medicaid] from [-------] to [--------]. Please refund this amount to [contractor
or state payor] within 30 days. In addition to [Provider]’s refund check, please provide
[contractor or state payor] with the following information: (i) why the voluntary refund is
being made (i.e., Self-Disclosure Protocol submission); (ii) how it was identified; (iii)
what steps were taken to ensure that the issues leading to the Self-Disclosure Protocol
submission were corrected; (iv) the dates the corrective actions were in place; (v) the time
period and provider numbers involved in the voluntary refund; and (vi) the fact that a full
assessment was performed to determine the entire time frame.
To the extent that [Provider] seeks to receive reimbursement for underpayments
identified in connection with its investigation of the claims described above, it is our
understanding of CMS policy that [Provider] must resubmit those claims in accordance
with CMS’s [or state payor’s] policies and procedures. Medicare Part A claims may only
be reopened within the time limits prescribed by 42 C.F.R. § 405.750. See also 42 C.F.R.
§ 405.1885. Part B claims may only be reopened within the time limits prescribed by 42
C.F.R. § 405.841. See generally 42 C.F.R. §§ 405.701-.1889. In the event that the
applicable time limit for resubmission of [Provider]’s [Part A/Part B] claims has already
expired, the fact that [Provider] is making the refund described in the first paragraph
above does not extend those time limits.
Please provide [Special Agent Assigned] and [OCIG Attorney Assigned] with written
confirmation of [Provider’s] repayment of the overpayment described above so that we
may close our file. Thank you for bringing this matter to our attention.
Sincerely,
[Name of RIGI]
Regional Inspector General
for Investigations
cc: [OCIG Attorney Assigned]
[CMS Regional Office Contact Person]
[Contractor Benefit Integrity Manager or Coordinator]
420 - Procedures for Re-issuance and Stale Dating of Medicare Checks
(Rev. 49, Issued 07-16-04, Effective/Implementation: 08-16-04)
Introduction
As part of the Centers for Medicare & Medicaid Services’ (CMS) effort to improve
financial reporting, we are clarifying the policy for reissuing, stale dating, and reporting
outstanding Medicare checks. In December 1993, CMS issued 42 Code of Federal
Regulation’s (CFR) Subpart M – Replacement and Reclamation of Medicare Payments
424.352: Intermediary and carrier checks that are lost, stolen, defaced, mutilated,
destroyed, or paid on forged endorsements. This section provides instructions to
Medicare contractors and will establish a standard to manage and report outstanding
Medicare checks.
Re-issuing Medicare Checks
All Medicare contractors must reissue checks in accordance with 42 CFR 424.352:
Intermediary and carrier checks that are lost, stolen, defaced, mutilated, destroyed or paid
on forged endorsements.
The provisions of this regulation require that a Medicare contractor (fiscal intermediary
or carrier) perform certain tasks upon notification by a payee that a check has been lost,
stolen, defaced, mutilated, destroyed or paid on forged endorsements. These steps are as
follows:
A. The Medicare contractor must contact the financial institution on which the
check was drawn to determine whether the check has been negotiated.
B. If the check has been negotiated:
1. The Medicare contractor will provide the payee with a copy of the check
and other pertinent information (such as a claim form, affidavit or
questionnaire to be completed by the payee) required to pursue the
claim in accordance with State law and commercial banking regulations.
2. To pursue the claim, the payee must examine the check and certify (by
completing the claim form, questionnaire or affidavit) that the
endorsement is not the payee’s.
3. The claim form and other pertinent information are sent to the Medicare
contractor for review and processing of the claim.
4. The Medicare contractor reviews the payee’s claim. If the Medicare
contractor determines that the claim appears to be valid, it forwards the
claim and a copy of the check to the issuing bank. The Medicare
contractor takes further action to recover the proceeds of the check in
accordance with State law and regulations.
5. Once the Medicare contractor recovers the proceeds of the initial check,
the Medicare contractor issues a replacement check to the payee.
6. If the bank of first deposit refuses to settle on the check for good cause,
the payee must pursue the claim on their own, and the Medicare
contractor will not reissue the check to the payee.
C. If the check has not been negotiated:
1. The Medicare contractor arranges with the bank to stop payment on the
check; and
2. Except as provided in paragraph (D) of 42 CFR 424.352, the Medicare
contractor reissues the check to the payee.
D. No check may be reissued under (C)(2) unless the claim for a replacement
check is received by the contractor no later than 1 year from the date of
issuance of the original check, unless State law (including any applicable
Federal banking laws or regulations that may affect the relevant State
proceeding) provides a longer period which will control.
Medicare contractors may receive requests for reissuance of Medicare checks that are
older than 1 year. Based on 42 CFR 424.352 (summarized above), Medicare contractors
should inform beneficiaries and providers/ physicians/ suppliers regarding the possibility
that State law may provide a more favorable time frame for reissuance. Requests for re-
issuance based on State law should be forwarded by Medicare contractors to their
Regional Office. The Regional Office will work with the Regional Office General
Counsel to resolve these requests on a case-by-case basis.
Medicare contractors regularly receive requests for reissuance of Medicare checks that
are older than 1 year. Under 42 CFR 424.352 many of these requests must be denied.
However, 42 CFR 424.352 applies only to checks that have been lost, stolen, defaced,
mutilated, destroyed or paid on a forged endorsement. Accordingly, Medicare checks
that are in the physical possession of the payee, have not been defaced or mutilated, and
have not been negotiated are not subject to the 1 year time limit for reissuance of 42 CFR
424.352 (d). Therefore, if the criteria below are met, such checks may be reissued by the
Medicare contractor even if they are older than 1 year. The criteria are:
1. If the payee (beneficiary, physician, supplier, provider, etc.) and/or authorized
representative can present the physical check,
2 The Medicare contractor can confirm that the check was not previously
reissued, and
3 Reissuance is not barred by a Federal and/or state statute of limitations.
Any questions that the Medicare contractors have regarding application of the above
criteria should be forwarded to their Regional Office. The Regional Office will work
with the Regional Office General Counsel to resolve the questions.
Stale Dating of Checks
Medicare contractors are expected to continuously review all outstanding checks, take the
appropriate action to stale date checks in conformance with Federal and/or State/local
banking regulations, and adjust financial reporting for these actions. Medicare contractors
must advise their financial institution of the change in the status of a check.
Outstanding checks are checks that have been issued as payment for Medicare benefits,
and have not been presented for payment to a financial institution and subsequently
drawn from the Medicare trust funds. Checks are “voided” by rendering them non-
negotiable either physically or by placing a stop payment on them.
Stale dated checks are checks that have reached a specific age from date of issue (e.g., 1
year from the date of issuance), and have not been presented for payment to a financial
institution and subsequently drawn from the Medicare trust funds. Additionally, once a
check has been stale dated and is no longer negotiable, the financial institution must be
notified in writing. These checks should not be included in the amount reported as
outstanding checks on Form CMS-1522 (see Financial Reporting section below).
The CMS requires all Medicare contractors to have internal guidelines concerning
procedures for stale dating checks that are consistent with these instructions. All checks,
which reach 1 year from the date of issue and remain outstanding, must be stale dated in
accordance with these instructions. Medicare contractors must document their stale
dating procedures and activities as part of their written operating policies and procedures.
The CMS recognizes that some Medicare contractors may be required to establish a
different stale dating policy based on State or local banking regulations. The Medicare
contractor must notify CMS Regional Office (Assistant Regional Administrator (ARA)
for Medicare Financial Management) and Central Office (Office of Financial
Management/Accounting Management Group) in writing when these regulations exist. In
the event that a Medicare contractor must stale date checks in less than 1 year (due to
State or local banking regulations), that Medicare contractor must recognize and report
the value of these checks as an Other Liability-Other on Form CMS-750 (with a
corresponding footnote for the total amount of the checks) until 1 year from the date of
issue, since the payee has the right to reclaim the funds.
As described above, the general rule for financial reporting is that a liability will not be
recorded for checks that have reached the age of 1 year from date of issuance. If a
Medicare contractor determines that application of this rule is not appropriate based on
experience or knowledge regarding re-issuance of Medicare checks under deference to
State law, CMS Regional Office (Regional ARA for Medicare Financial Management)
and Central Office (Office of Financial Management/ Accounting Management Group)
should be notified in writing so that the accounting implications are properly addressed.
Undeliverable Checks
Medicare providers, physicians, suppliers, and beneficiaries are responsible for providing
the Medicare contractor with their current and accurate mailing address.
The Medicare contractors must comply with the policy established by the “Do Not
Forward (DNF) Initiative.” This policy requires Medicare contractors to reissue the check
based upon the receipt of updated verified address information per Form CMS-855; and
if no updated address information has been submitted, then Medicare contractors must
void any returned checks.
When a Medicare benefit check has been returned as undeliverable due to DNF, the
Medicare contractor will void the check immediately and recognize and report the value
of the check(s) as an Other Liability-Other on Form CMS-750 (with a corresponding
footnote) until 1 year from the date of issuance, since the payee has the right to reclaim
the funds. Checks voided due to DNF may be reissued in accordance with instructions in
the preceding section entitled “Re-issuing Medicare Checks.”
Financial Reporting
Outstanding checks must be reported on the Monthly Contractor Financial Report, Form
CMS-1522. Medicare contractors must have supportable and auditable documentation to
support balances reported.
The Medicare contractors must report:
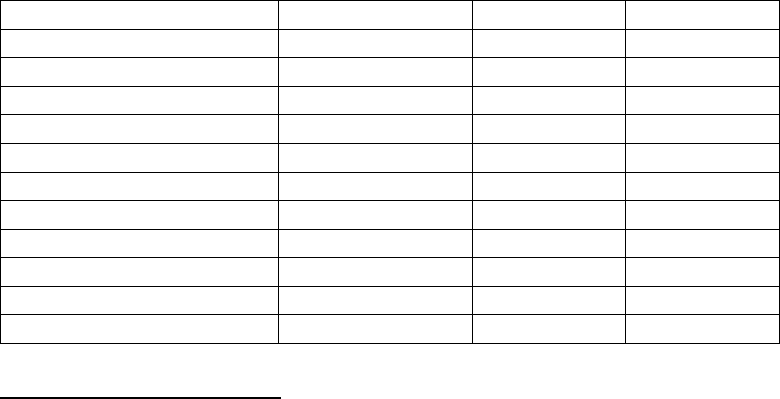
1. The balance of all outstanding checks at the end of each month in section D –
Reconciliation and Analysis of Special Bank Account, of Form CMS-1522;
2. The amount of any liability for stale dated checks less than 1 year from the
date of issue in the Other Liabilities section of Form CMS-750; and
3. The amount of any liability for undeliverable checks that are voided less than
1 year from the date of issue, in the Other Liabilities section of Form CMS-
750.
Medicare contractors’ systems must be able to obtain/maintain transaction level detail of
outstanding checks from their financial institution(s). The Medicare contractor must
reconcile outstanding checks monthly to Form CMS-1522 and the Medicare contractor’s
bank statement.
There are separate data screens for Part A, Hospital Insurance (HI), and Part B,
Supplementary Medical Insurance (SMI) in the Contractor Administrative Budget
Financial Management (CAFM) system. Enter outstanding checks data in both data
screens, as appropriate.
Medicare contractors must maintain an audit trail to identify and support actions taken
regarding all (beneficiary and provider/physician/supplier) issued checks.
Recording of Stale Dated/Voided Check
Activity
Transaction
Debit
Credit
Receipt of Claim
Program Expense
xxxxx
Accounts Payable
xxxxx
Payment of Claim
Accounts Payable
xxxxx
Cash
xxxxx
Stale Dated/Voided Check
Cash
xxxxx
Other Liability
xxxxx
Entry after 1 year
Other Liability
xxxxx
Program Expense
xxxxx
PROVIDER EDUCATION
This information must be shared with providers/physicians/suppliers through your Web
site within 2 weeks and published in your next regularly scheduled bulletin. It should be
made clear that providers/physicians/suppliers are responsible for monitoring Medicare
reimbursement, and requesting re-issuance of Medicare checks within applicable time
frames. Emphasize that providers/physicians/suppliers should ensure that correct address
information is on file, and complete Form CMS-855 to update their address if necessary.
500 - Procedures for the Reconciliation of Total Funds Expended for
Fiscal Intermediary Shared System (FISS) Medicare Contractors Used
in the Preparation of Form CMS-1522¸ Monthly Contractor Financial
Report
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
The Centers for Medicare & Medicaid Services (CMS) continues to have a material
internal control weakness for the reconciliation of total funds expended on Form
CMS-1522 resulting from the Chief Financial Officers Audit. The reconciliation of total
funds expended to adjudicated claims and standard system reports is an important control
that ensures that the amounts reported by Medicare contractors are accurate, supported,
complete, and properly classified.
The CMS requires that Medicare contractors provide a reconciliation of total funds
expended reported on the monthly Form CMS-1522 report by the 15
th
day of the
following month. Form CMS-1522 is a cash-based document and is prepared primarily
from FISS system reports, bank statements, and other internal reports. The financial
reconciliation includes adjudicated claims processed, other non-claims based payments,
overpayment recoveries, and other financial adjustment transactions.
Total funds expended represent payments made for claim and non-claim transactions
during each claims payment cycle (i.e., the total of all checks issued, electronic funds
transfers (EFT) payments, voided checks, overpayment recoveries, and other financial
adjustments). The claims payment cycle varies at each contractor and can be daily,
multi-weekly, or weekly.
Claims data files maintained by the fiscal intermediary, produced from FISS Job
#XXXX0054X, include all claims received and processed during a payment cycle –
adjudicated claims and non-adjudicated claims. Adjudicated claims represent those
claims that were processed for payment and included on the remittance advice report.
Non-adjudicated claims do not appear on the remittance advice and include
demonstration claims, claims returned to the quality improvement organization (QIO) or
provider, and other exception claims. The FISS Systems Maintainer will generate a
detailed claims data file that includes only the adjudicated claims records processed each
payment cycle in order for financial reporting personnel to complete the financial
reconciliation. Also, the FISS Systems Maintainer will generate a report that summarizes
the number and dollar value of adjudicated claims on the detailed claims data file.
Although the enclosed reconciliation format has been tested and proven adequate for
most situations, there may be unique situations at selected contractors that result in an
“unreconciled” reconciliation. When those situations occur, the contractor should
investigate those differences and identify the source of the difference. The standard
format can be adjusted to accommodate those differences so that the reconciliation and
Form CMS-1522 can be completed. Contractors should report those differences to CMS
for further review and adjustment of the standard format.
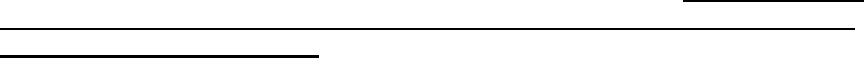
The lead reconciliation schedule (section 500.4) must be submitted electronically to the
CMS. FISS system reports, bank statements, and other internal reports used to create the
lead reconciliation schedule must be maintained and made available upon request for
audit and review by CMS financial personnel and other external auditors.
Methodology
Contractors are required to complete the financial reconciliation schedules for each
claims processing cycle, and provide a copy of the cumulative monthly totals in the
format established in Section 500.4. The reconciliation should be completed at the end of
each claims payment cycle to identify any differences as they occur and provide
sufficient time to resolve those differences before the next cycle ends. View Exhibit I by
clicking on this link to access the electronic spreadsheet in Microsoft® Excel format
to complete the following steps.
To complete the reconciliation for each claims payment cycle, FISS contractors must:
1. At the top of the Reconciliation Page, enter the estimated HI allocation
percentage in cell J2. The SMI allocation will be automatically calculated and
entered into cell J3. These allocation percentages are used in the calculation
of line 6-6, Settlement Payments (including interest); line 6-10, Refund
Provider Payments; line 6-11, Refund Other Payee Payments; and line 6-18,
Settlement Withholdings (including interest) if the FISS contractor does not
know the exact amounts for HI and SMI. Although the percentage is an
estimate, the previous method for calculating these lines using the
inpatient/outpatient ratio created problems in Schedule E of the worksheet
because the HI/SMI ratio would change after each cycle was entered into the
spreadsheet. Using this fixed HI percentage resolves those differences.
2. The FISS system maintainer will identify and summarize the adjudicated
claims for each claims payment cycle. The FISS system maintainer will
create a detailed claims data file and summary report that must be retained for
review and audit purpose (section 500.1).
a. Obtain the detailed claims data file and summary report (FISS Report
#7859R06) from the FISS system maintainer detailed claims data file
for each claims payment cycle.
b. Enter the detailed claims data file totals for each payment cycle onto
reference lines 1-1 through 1-4 of the electronic spreadsheet (section
500.3). Separate reference lines for inpatient and outpatient have been
added to the input schedule.
c. Obtain FISS Report #7859R01, Create Claim File Control Report, and
enter selected data onto reference lines 2-1 through 2-8 of the
electronic spreadsheet (section 500.3). The Error Records Out/Paid
lines were removed because they are no longer populated with data.
d. Review the Tape Reconciliation Check lines on reference lines 3-1
through 3-4. No entries should be made to these reference lines.
These reference lines verify the agreement of the 7859R06 and
7859R01 reports. The amounts on those reference lines must be
ZERO; research any differences that are identified and make
corrections to any of the amounts entered on reference lines 1-1
through 2-8 and correct as appropriate.
3. Obtain copies of the primary financial FISS system reports that are used in the
financial reconciliation process. A list of those report numbers and report
descriptions is included in section 500.2. Instructions for selected line entries
are included below, either to explain why the entry is necessary or how to
enter the information properly.
a. Enter selected financial information from FISS system reports into the
electronic spreadsheet (section 500.3) on reference lines 4-1 through
18-1. Information should only be entered into cells with a light blue
background. All other cells on the spreadsheet are locked to prevent
overwriting of the formulas used to complete the reconciliation.
b. The allocation for all amounts entered on reference lines 1-1 through
18-1 as either Part A (HI) or Part B (SMI) are determined based on the
allocation identified on FISS system reports or by financial personnel
who enter information from non-FISS system reports, except for the
following reference lines with a red background.
Line 6-6 – Settlement Payments (including interest)
Line 6-10 – Refund Provider Payments
Line 6-11 – Refund Other Payee Payments
Line 6-19 – Settlement Withholdings (including interest)
The spreadsheet has been changed to allow for entering exact amounts
for Part A and Part B or for entering a fixed HI/SMI percentage for
these reference lines. See ‘f.’ below for a discussion on the allocation
or actual methodology to allocate the total amounts for these reference
lines.
c. Obtain FISS Report #8074R01, Claim Payment Update Report –
Inpatient, and FISS Report #8074R02, Claim Payment Update Report
– Outpatient. Enter selected totals from those reports onto reference
lines 4-1 through 4-6 and 5-1 through 5-2 of the electronic
spreadsheet.

d. Obtain FISS Report #8014R01, Financial Summary Report and enter
selected amounts from the report onto reference lines 6-1 through 6-
23. Reference line 6-3 was added for Pass Thru Payments at 100%
(Part B). Some contractors indicated that they break out Pass Thru
Payments by Part A and Part B but there is no FISS system report that
identifies those amounts. Contractors should identify the amount that
is Part B and maintain a subsidiary record of those items that are
reported on reference line 6-3. Ensure that the total of reference line
6-2 and 6-3 equals the total reported on FISS report #8014R01.
e. Reference line 6-24 shows the total disbursements amount that should
appear on FISS Report #8014R01. If the amount on reference line 6-
24 differs from the report total amount, recheck the entries on
reference lines 6-1 through 6-23 and correct as necessary.
f. Allocating Amounts from the #8014R01 Report. While the electronic
spreadsheet automatically identifies the total for each expenditure
amount to the appropriate funding classification – Part A, hospital
insurance (HI) or Part B, supplemental medical insurance (SMI), the
allocation for four reference lines from the 8014R01 report cannot be
determined from FISS system reports. Consequently, the allocation
for those reference lines must be determined by the contractor using
one of the following methodologies.
i. If the contractor cannot accurately break out Part A from the
total amounts, the spreadsheet will automatically allocate the
amounts for four reference lines using the HI percentage that is
entered in cell J2 of the Reconciliation page of the worksheet.
ii. If a contractor can identify the actual allocation between HI
and SMI, then the actual amounts for Part A for the four
reference lines should be entered on reference lines 7-1
through 7-4, as appropriate. The contractor only has to enter
the amounts for those reference lines that are know, not
necessarily all four reference lines but the contractor must
identify those lines that are entered by placing a lower case ‘a’
in the highlighted space preceding the description on reference
lines 7-1 through 7-4.
iii. The spreadsheet will determine the Part B amounts for the lines
that are used by the contractor and a checkmark ‘’ will show
which lines they are. Although the spreadsheet will calculate
both the allocated amounts and the actual amount for Part A
and Part B for each of the five reference lines, only one of the
amounts (allocated or actual) will be used in the schedules.
The spreadsheet uses the checkmark ’’ to determine which
amounts to use and places them in reference lines 19-1 through
19-8.
g. Obtain FISS Reports #8015R01, Part A - Penalty Withholding Report,
and #8015R02, Part B – Penalty Withholding Report and enter
selected amounts on reference lines 8-1 thru 8-4, respectively. Please
note that this section has been changed. Only use the Penalty
Withholding Withheld Today and Penalty Medicare Recouped
Today amounts from these reports. Do not use the Penalty
Withholding Released Amount from those reports – those amounts
are not accurate.
h. Obtain FISS Reports #8015R05, Part A - Accelerated Payment
Withholding Report, and #8015R06, Part B – Accelerated Payment
Withholding Report and enter selected amounts on appropriate
reference lines in series 9 and 10. Although accelerated payments are
not directly provided on these reports, there is sufficient information
on those reports to determine the dollar amount of accelerated
payments made each cycle. Enter the beginning and ending balances
from the FISS reports onto the spreadsheet reference lines 9-1, 9-3, 10-
1, and 10-3 as positive numbers. Enter the amount withheld today on
reference lines 9-2 and 10-2 as negative numbers. The accelerated
payments for Part A and Part B will be calculated on reference lines 9-
4 and 10-4, respectively.
i. NOTE: Sometimes the beginning balance for one cycle does NOT
equal the ending balance for the prior period. This occurs when
an accelerated payment is not processed by FISS in the usual
sequence and the FISS reports don’t reflect the proper balances.
To account for those differences, add any “missing” amounts on
reference lines 9-5 and 10-5 as appropriate.
j. Obtain FISS Reports #8019R01, Disbursement Control Account,
#8021R05, HPSA Check Payment Register, and #8021R06, HPSA
EFT Payment Register. Checks and Electronic Funds Transactions are
made for regular payments whose transaction was processed in FISS
and other payments for Health Professional Shortage Area (HPSA)
payments. Enter the regular payment amounts on reference lines 11-1
(system checks) and 11-2 (system EFTs). Enter the quarterly HPSA
payments on reference lines 11-4 (HPSA checks) and 11-5 (HPSA
EFTs). Those amounts will be added together with any adjustments
entered on the series 12 reference lines (see j. below) to determine the
total net disbursements amount after adjustment for stripped checks
and EFTs.
k. Occasionally, financial personnel identify system checks and EFTs
that were written for the wrong amount and those errors are identified
before the check or EFT is sent to the provider. Additionally, other
CA and CB transactions are processed that need to be accounted for on
these reference lines. To account for those adjusting transactions,
financial personnel “strip” the payment before it is issued by
processing either a complete Part A (CA) or a complete Part B (CB)
payment reversal transaction. Because those reversal transactions can
only reverse the payment amount as either a complete Part A reversal
(CA) or as a complete Part B reversal (CB), that ultimately causes an
imbalance in the benefit payment amounts identified in Schedule E
(section 500.8).
i. To correct for that incorrect allocation of Part A and Part B
benefits, the Series 12 reference lines were added. Enter the
total dollar value of the CA or CB amounts processed in FISS
(checks and EFTs) on reference lines 12-1 and 12-2,
respectively. Likewise, when a replacement payment is
processed as a CA or CB transaction, enter the total dollar
value of the amounts processed in FISS (checks and EFTs) on
reference lines 12-5 or 12-6, respectively. Because those
transaction amounts are included in the FISS Report #8037R01
amounts entered on reference lines 13-1 and 13-2, but not
included in the amounts reported on FISS Reports #8014R01
and #8042R01 adjustments to various FISS report totals are
made using the amounts identified on the series 12 reference
lines.
ii. Enter the actual amounts of the CA or CB reversal adjustments
that relate to Part A on reference line 12-3 and to Part B on
reference line 12-4, and the actual amounts of the CA or CB
replacement adjustments that relate to Part A on reference line
12-7 and to Part B on reference line 12-8. The amounts
entered on those lines will be used to correct the
“misallocation” of those transactions resulting from processing
a CA and CB transaction. As noted above, the reconciliation
of total payments in Section 500.4 and the non-PIP
reimbursements in Section 500.6 will be adjusted to reflect the
correct Part A and Part B allocations.
l. Obtain FISS Reports #8037R01 and #8037R02, Monthly Benefits
Reconciliation Update reports and enter selected amounts on reference
lines 13-1 through 14-2. Please note that the Suspended Payment
Withheld Amounts (Part A and Part B) are no longer used because
they include the total amount of the Penalty Withholding Withheld
Today and Penalty Medicare Recouped Today.
m. Obtain FISS Report #8042R01, Form CMS-1522 Update Report and
enter selected interest and retroactive adjustment amounts on reference
lines 15-1 through 15-24.
n. The remaining financial information needed to complete the
spreadsheet is not available on FISS system reports. The contractor
should obtain that information from available sources, fully document
the totals for each entry, and enter those amounts onto reference lines
16-1 through 18-1 of the electronic spreadsheet (section 500.3).
i. The information for reference lines 16-1 through 16-15 should
be obtained from the list of deposits processed into FISS each
cycle. The Total Depository Items is on reference line 16-16.
ii. Reference lines 16-1 and 16-2 should represent the portion of
retroactive adjustments that is included in the amounts reported
on FISS Report #8042R01. These amounts are needed here to
account for the deposits but these amounts are not added to the
amounts reported in Section 500.8 to avoid duplicate counting
of those amounts.
iii. Reference lines 16-3 through 16-15 should represent all other
non-retroactive adjustment deposits that are not included in any
of the 8042R01 amounts used in the spreadsheet. The
information on these lines should also be obtained from the list
of deposits made to the bank account.
iv. The seven categories listed, identify the most common used by
Medicare contractors. The amount reported as a PIP
repayment, reference line 16-9, is included in the PIP Payments
total calculated for the CMS Form 1522 in Schedule E. The
other lines are included in the “Aged” category of Total
Benefits Paid for Part A and Part B, as appropriate on Section
500-8.
v. NOTE: When a deposit is returned by the bank, that
reversal should also be identified on reference lines 16-1
through 16-15 as a positive number to ensure that
Retroactive Adjustment, PIP Payments, and Total Benefits
Paid for Part A and Part B are accurately calculated and
reported in Schedule E (section 500-8).
vi. The information for reference lines 17-1 through 17-18 is
determined from various sources, including the bank
statements, the manual check listing, the voided and stale-dated
check listing, and other manually maintained listings or the
identified FISS system reports that identify correcting financial
transactions for the month. Lines for each type of transaction
are available for both Part A and Part B cycle totals.
1. The information for reference lines 17-1 through 17-8
are available for situations that do not occur on a
routine basis, generally related to bank problems with
processing a payment and deposit items or for other
correcting transactions processed by the bank.
2. The information for reference lines 17-9 through 17-12
relate to the issuance of manual checks. The amount
entered on reference line 17-9 and 17-10 includes all
manual checks that are not established using a CA or
CB transaction and checks written for transfers
between the disbursement and time accounts. As stated
above, CA and CB transactions should be posted on
reference lines 12-5 through 12-8. The check amount
for transfers to the time account is entered on reference
line 17-11. Because the transferred amount does not
impact total funds expended, the amount is also entered
automatically on reference line 17-12 as a negative
number.
3. The information for reference lines 17-13 through 17-
18 relate to stop payment checks, voided checks, and
stale-dated checks canceled during the month that are
identified on FISS reports #8010R01 or #8072R03, or
other manually maintained documentation that may be
more accurate. These lines should only be used for
transactions that are processed by a transaction type
other than a CA or CB transactions. Otherwise, the
transaction should be included on the Series 12
reference lines.
4. Obtain FISS Report #8047R02, and enter the amount
of Total IBPR payments on line 18-1. That amount
will be compared to other financial report amounts to
ensure that there is an agreement for the IBPR
reconciliation. Lines E-59 through E-69 in section
500.8 were added to perform the IBPR reconciliation.
Because FISS Report #8047R02 represents totals in
whole dollars, there will always be minor differences
to account for the rounding. Line E-68 represents the
rounding amount and generally should never be a
significant amount in excess of $10.
5. Finalize the standard reconciliation report, print the
supporting schedules (sections 500.5 through 500.8),
and submit the consolidated monthly report to CMS as
part of the monthly contractor financial reports (section
500.4).
After completing the process outlined in 1. and 2. above, all of the financial
information needed to identify total funds expended has been entered into the
standard report format. That information is transferred into five standard reports
that are used to document the financial information entered onto Form
CMS-1522. Those reports are illustrated in sections 500.4 through 500.8 of this
instruction.
a. After entering all of the financial information in reference lines 1-1
through 18-1 the value of total funds expended has been determined. The
next step is to verify that the amount allocated by HI and SMI have been
properly completed. As noted above, the standard report format performs
most of that process automatically. To identify any potential error, review
Column J on the electronic spreadsheet and research any entry on the
schedule reference line A-1 through E-58 that is not ZERO. For the
schedules to be reconciled, all entries in Column J must be ZERO.
b. If the contractor has overridden any of the HI and SMI allocation
formulas, extra effort should be made to ensure that the allocation amounts
equal the total amount for those categories. Again, the formula in Column
J should produce a value of ZERO if the line is in balance.
The standard report format in section 500.8 calculates the amounts that are
reported on the end of the Form CMS-1522 (i.e. the categorization of total funds
expended by payment categories).
Overall Summary
The methodology used to identify the number and dollar value of adjudicated claims on
the detailed claims data file provided in section 500.1, the FISS systems reports identified
in section 500.2, the electronic spreadsheet input schedule in Section 500.3, and the
standard report formats provided in sections 500.4 through 500.8 are a systematic
approach to reconcile financial activity for each claims payment cycle at Medicare FISS
contractors.
The information contained on the schedules provides a standard methodology to validate
financial information contained on FISS system reports to the source claims information
contained in the detailed claims data file. The methodology outlined above and the
information contained on the standard report formats document a standardized approach
to calculate and validate the total funds expended at Medicare contractors.
Also, the standard report formats assist in the preparation of a significant portion of the
Form CMS-1522. The methodology does not provide information relating to the Funds
Drawn from the Treasury presented on lines 1 through 6 of Form CMS-1522, or for the
bank reconciliation information presented on Form CMS-1522, Page 2 and 3, Lines 15
through 23.
Due Date
A copy of the schedule illustrated in section 500.4, Total Funds Expended (Net
Disbursements and Adjustments to Net Disbursements), must be provided electronically
to the appropriate CMS regional office’s Associate Regional Administrator for the
Division of Medicare Financial Management, by the 15
th
day of the following month,
concurrent with the submission of other Contractor Financial Reports and submitted
electronically to [email protected]. All of the schedules illustrated in sections
500.4 through 500.8 should be retained to support the information submitted to the
appropriate CMS regional office.
500.1 – Identification and summarization of Detailed Claims Data
Records for Use in the Financial Reconciliation of Total Funds
Expended to Fiscal Intermediary Shared System Reports
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
The FISS Systems Maintainer will generate a detailed claims data file for each FISS
contractor’s payment cycle, produced from FISS Job #XXXX0054X. During claims
processing, the FISS system maintains a record of all claims processed during the
payment cycle, including both adjudicated and non-adjudicated claims. Adjudicated
claims include all PIP and non-PIP reimbursement claims, and rejected and denied claims
that can be processed by FISS. The non-adjudicated claims include demonstration
claims, claims that could not be processed and must be returned to either the provider or
the Quality Improvement Organization (QIO), and other exception claims.
The FISS Systems Maintainer will identify only those adjudicated claims that appear on
remittance advices and that are identified on FISS Report #7859R01, and will record
those claims records onto a detailed claims data file.
The FISS Systems Maintainer will provide an independent report that shows the total
number of records on the electronic file and the total dollar value for each of the
following fields from FISS Report #7859R01:
Claims Records Out/Paid - Inpatient
Claims Records Out/Paid - Outpatient
Claims Records Out/Modified - Inpatient
Claims Records Out/Modified - Outpatient

The fiscal intermediary will obtain the detailed claims data file and the summary report
(FISS Report #7859R06) from the system maintainer for use in the financial
reconciliation of total funds expended that is reported on Form CMS-1522 each month.
The fiscal intermediary will retain the detailed data file and the summary report for each
payment cycle in order to document the information entered onto the standard electronic
spreadsheet and, when required, for use and review by CMS and other audit personnel.
500.2 – Using the Electronic Spreadsheet to Complete the Reconciliation
of the Detailed Claims Data File to Fiscal Intermediary Shared System
Reports.
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
This section describes the methodology to use the electronic spreadsheet (Section 500.3)
and identifies the primary FISS system reports needed to complete the financial
reconciliation.
The electronic spreadsheet (Exhibit 1) consists of two pages – PrintMenu and
Reconciliation. Each of those pages is protected to ensure that the user cannot write over
any formulas or linked areas of the spreadsheet. The electronic spreadsheet was created
in Microsoft Excel 2000 and macros must be enabled. When the spreadsheet is loaded,
you should receive a message concerning macros. You must ‘Enable Macros’ for the
automatic printing capability to work properly. Following are some general rules to
follow when using the electronic spreadsheet.
Protection
As noted above, the spreadsheet pages should be protected during use to avoid
overwriting any formulas. Press the “Tab” key to determine whether the page is
protected or not. If the page is protected, the tab key will move the cursor to the next
unprotected cell. If the cursor lands on a cell that should be protected – a description,
total or non-blue cell – then the page is probably not protected.
To protect the page, press ‘Tools’ on the menu bar, select ‘Protection’, and then select
‘Protect Sheet’. When prompted for a password, DO NOT enter a password, just press
‘OK’. If it becomes necessary to unprotect the page (rare, if ever), perform the same
process – Tools, Protection, Unprotect Sheet.
Print Menu
This page contains two basic functions: (1) identifying and filling in the cycle dates, and
(2) printing the cycle and monthly reports.
1. Cycle Dates. Generally, payment cycle dates are consistent throughout the
year (i.e., they occur on the same calendar day(s) each week). Consequently,
the actual dates can be determined automatically. At the top of the
‘PrintMenu’ enter the calendar year as a 4-digit number in block ‘J4’ and
enter the month as a 1- or 2-digit number in block ‘J5’. In blocks ‘J2’ through
‘R2’ enter an ‘X’ for each payment cycle day during the week. The monthly
cycles and the cycle payment dates will automatically be identified on the left
side of the screen in blocks ‘A1’ thru ‘D32’, including leap years. Those
cycle dates will also be entered onto the top of the cycle columns and the
Month and Year will be entered on the top of the Part A and Part B columns
on the ‘Reconciliation’ spreadsheet. When business is not conducted on a
regularly scheduled business day, primarily for holidays, delete the ‘X’ in
blocks ‘B2’ through ‘B32’ next to the appropriate dates. This will prevent a
blank column being allocated on the spreadsheet for those non-work days.
2. Printing Reports. The standard format reconciliation reports should be printed
after each cycle to document the cycle information and the reconciliation
process. Pressing the left mouse button when the cursor is positioned over
one of the buttons on the ‘PrintMenu’ screen and the cursor appears as a
pointing hand can print the reports. There are three types of buttons for
printing the reports.
a. Input Schedules - #X (Orange text on Grey background). There are
31 buttons on the left center of the screen that will print the input
schedules for each cycle. The report will include the reference line
number, source and description, the total amount to date, and the cycle
amount entered.
b. Cycle Report Schedules - Cycle XX (Sea Green text on Grey
background). There are 31 buttons in the right center of the screen
that will print the five reports for each cycle. The spreadsheet will
accommodate up to 31 daily cycles for each month. When selected,
the report will print the information in Columns A thru G plus the data
in the column for the selected cycle. Each report will provide the
‘Total Amount to Date’ plus the selected Cycle columns. Because
there is only one ‘Total Amount to Date’ column, it will change after
the data for each cycle is entered.
c. Monthly Reports - (Red/Blue text on Gray background) – There are
six buttons on the right side of the screen that will print either all five
of the monthly reports (Red text button) or each of the reports
separately (Blue text buttons). The monthly reports will print the
information in Columns A thru J that include the total amounts for the
month, the allocation by HI and SMI, and the Zero Check field.
Reconciliation
The reconciliation spreadsheet is the where most of the data is entered to complete the
financial reconciliation of the Form CMS-1522. As noted at the top of the page, only
enter data in designated cells and avoid entering data in selected unprotected cells unless
you are sure you want to overwrite the standard formulas. All cells with formulas or
transferred data are locked to prevent overwriting, except those with a red background.
Those cells contain formulas but if the contractor has more accurate information, those
formulas can be overwritten.
To complete the reconciliation, information from standard FISS system reports is entered
into a common data input area of the Reconciliation spreadsheet (see section 500.3). The
data input area is located on lines 9 thru 202 the electronic spreadsheet in columns L
through AP. The information for individual reports is grouped together for easy input
and is identified by references line numbers (found in Column A of the electronic
spreadsheet) that begin with a number (for example, FISS Report #7859R01 information
is found on reference line numbers 2-1 thru 2-12). The standard FISS reports or other
source documents used in the financial reconciliation, including the reference line
numbers, are identified in the following table.
Reference Lines
FISS Report Number and Report Description
1-1 thru 1-4
FISS #7859R06
– Detailed Claims Data Records Summary Report
2-1 thru 2-8
FISS #7859R01
– Claim File Control Report
3-1 thru 3-4
Tape Reconciliation Check Lines (NO ENTRY REQUIRED)
4-1 thru 4-6
FISS #8074R01
– Claim Payment Update Report - Inpatient
5-1 thru 5-2
FISS #8074R02
– Claim Payment Update Report - Outpatient
6-1 thru 6-24
FISS #8014R01
– Financial Summary Report
7-1 thru 7-8
Actual amounts for 4 selected lines from the #8014R01 report
8-1 thru 8-2
FISS #8015R01
– Part A – Penalty Withholding Report
8-3 thru 8-4
FISS #8015R02
– Part B – Penalty Withholding Report
9-1 thru 9-5
FISS #8015R05
– Part A – Accelerated Payment Withholding Report
10-1 thru 10-6
FISS #8015R06
– Part B – Accelerated Payment Withholding Report
11-1 thru 11-3
FISS #8019R01
– Disbursement Control Account
11-4
FISS
#8021R05 – HPSA Disbursement Register
11-5
FISS #8021R06
– HPSA EFT Register
12-1 thru 12-8
CA and CB Transaction Amounts
– EFTs and Checks
13-1 thru 13-5
FISS #8037R01
– Monthly Benefits Reconciliation Update
14-1 thru 14-2
FISS #8037R02
– Monthly Benefits Reconciliation Update

15-1 thru 15-24
FISS #8042R01
– Form CMS-1522 Update Report
16-1 thru 16-15
List of Daily Deposits for the Month or Other Contractor Prepared Schedules
17-1 thru 17-18
Bank Statements
– Time Account, Disbursement Account, Concentration Account
List of Manual Checks Issued During the Month, Bank Reconciliation (non
-CA/CB)
List of Stale
-Dated, Stop Payment and Voided Checks (non-CA/CB)
List of Other Financial Adjustment Transactions Occurring During the Month
18-1
FISS
#8047R02 – Monthly Intermediary Benefit Payment Report
Following are some general rules for using the electronic spreadsheet (Exhibit 1).
1. Entering Data. All data must be entered into a “data entry area” that has
reference line numbers in Column A that are all numeric (reference lines 1-1
thru 18-1). Those amounts are transferred directly into the reconciliation
reports (reference lines A-1 thru E-58). Consequently, you must enter data
into each cell directly. Do not copy and paste the amounts to different cells,
doing so will transfer the link to the reconciliation reports and invalidate the
process. If you make an error in a cell, edit it using the F2 function key,
delete the entry, or re-enter the correct amount directly.
2. Source FISS System Reports. Column B identifies the source FISS system
report for the data to be entered on each line of the “data entry area” on
reference lines 1-1 thru 18-1. Column B identifies the primary source FISS
system report and alternate sources for the same data on each line of the
reconciliation reports on reference lines A1 thru E-69.
3. BLUE Background Cells. Enter financial data only in spreadsheet cells that
have a BLUE background. Cycles 1 thru 31 are in Columns L thru AP,
respectively. Those lines will have references in Column A that are all
numeric (1-1 thru 18-1).
4. GRAY Background Cells. Do not enter financial data in spreadsheet cells that
have a GRAY background. Those cells transfer data from other cells and the
formulas in those cells cannot be changed without affecting the reconciliation
process.
5. RED Background Cells. Data in spreadsheet cells with a RED background
contain formulas that allocate total amounts by HI and SMI using the ratio of
Inpatient to Outpatient claims paid to date for the month. Unlike the formulas
in spreadsheet cells with GRAY backgrounds that are locked, the formulas in
the spreadsheet cells with RED backgrounds are unlocked and can be
overwritten. Only write over those formulas in those cells if you have more
accurate HI/SMI amounts that differ significantly from the amounts calculated
by the spreadsheet formulas and only during the end of month processing.
See the detailed instructions in Section 500, Paragraph 2.j.
6. GREEN Background Cells. Spreadsheet cells with a GREEN background are
check fields to ensure that the data entered from one FISS system report
reconciles with data entered from other FISS system reports into the data entry
section. In all cases, the amount must be zero or the financial reconciliation
will be unreconciled.
a. Spreadsheet lines 24 thru 27 (3-1 thru 3-4) verify the accuracy of the
claims processing tape file reconciliation. Any amounts other than
zero indicate that either a wrong amount was entered or there is an
imbalance between the tape and the FISS system report.

b. Spreadsheet reference line 10-6 checks to see if there is an imbalance
in the calculated amount of Accelerated Payments for Part A and Part
B. Any amount in that line indicates that either a wrong amount was
entered in reference lines 9-1 thru 9-3 or 10-1 thru 10-3, or that a
problem occurred with the FISS processing. Whatever the reason for
the difference, correcting entries need to be made on reference lines 9-
5 or 10-5.
c. Spreadsheet reference line A-43 in Section 500.4 verifies that system
payments agree with system report disbursements.
d. Spreadsheet reference lines B-23 thru B-25 in Section 500.5 verifies
the agreement of various Inpatient and Outpatient totals between
several system reports. Reference line B-36 verifies the accuracy of
the number of inpatient and outpatient claims identified from various
system reports.
e. Reference lines C-16 thru C-18 on the reconciliation report verify the
accuracy of the Non-PIP payment amounts used in the financial
reconciliation. The amounts on those lines should be zero because the
detailed line items supporting those amounts are adjusted for any
CA/CB transaction adjustments for electronic funds transfers and
checks removed on reference lines 12-1 through 12-8.
f. Reference lines D-26 thru D-31 on the reconciliation report verifies the
accuracy of the interest amounts paid, received, and reported on
various FISS system reports. There may be minor difference
identified on those lines that compare the amount on the 8037R02
report. Since the implementation of CELIP, the interest amounts on
that report are not always accurate.
7. YELLOW Background Cells. Data in spreadsheet cells with a YELLOW
background contain either totals for cells directly above it or data transferred
from one of the other reconciliation worksheets. Those cells are protected and
cannot be changed.
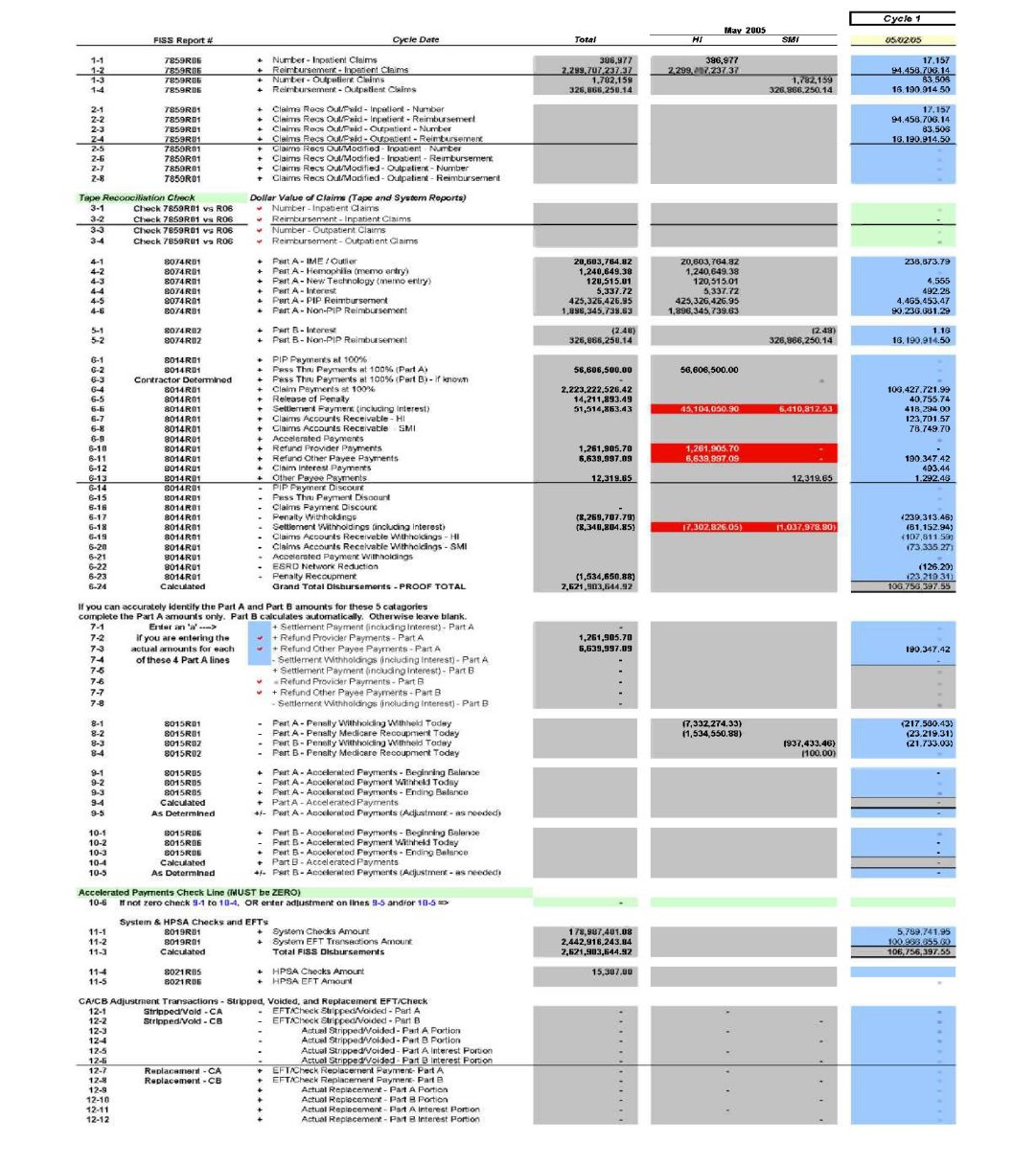
500.3 - Electronic Spreadsheet Input Schedule
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
This section is an illustration of the electronic spreadsheet (Exhibit 1) that will be used to input selected
financial information from the claims processed file and FISS reports.
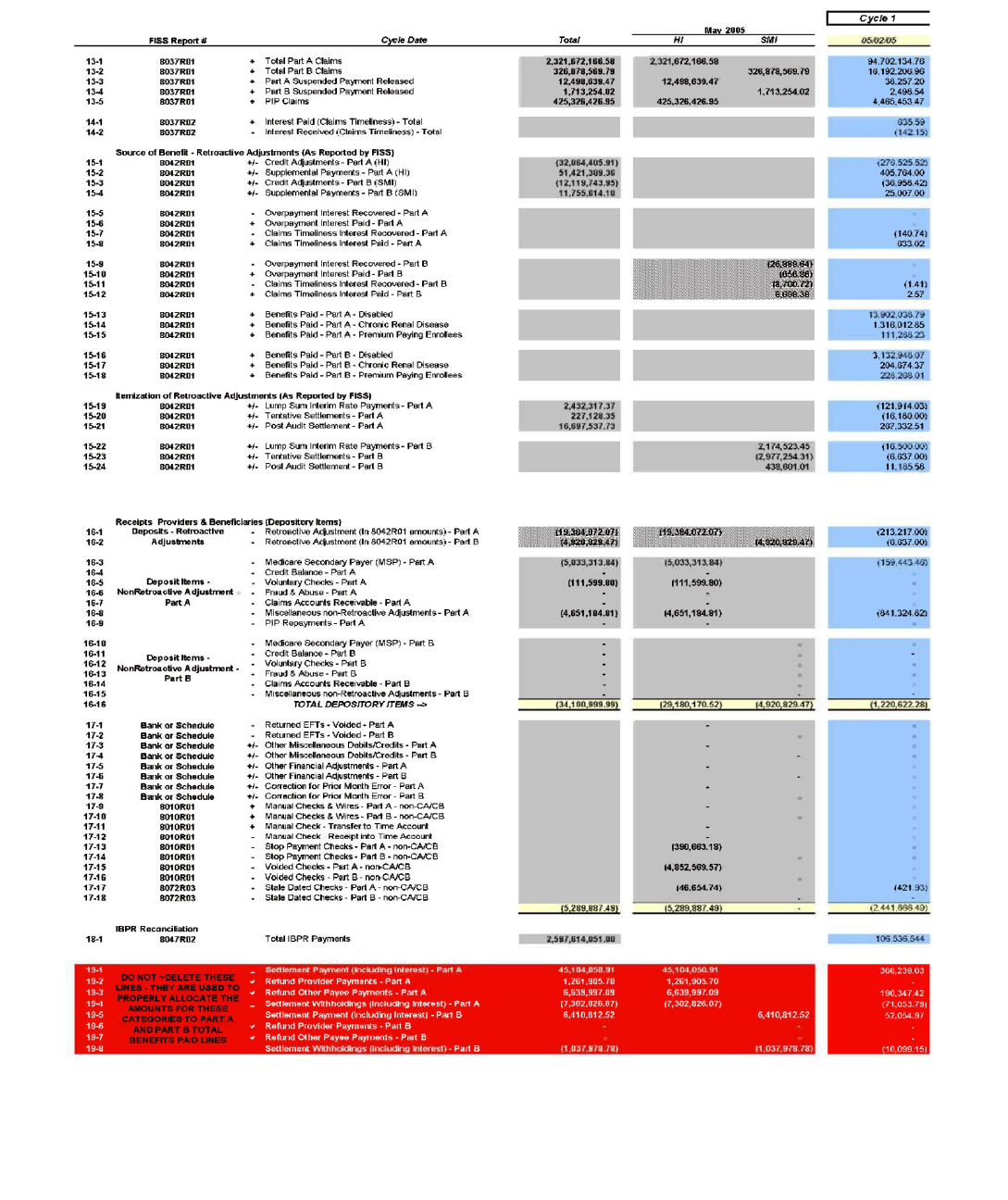
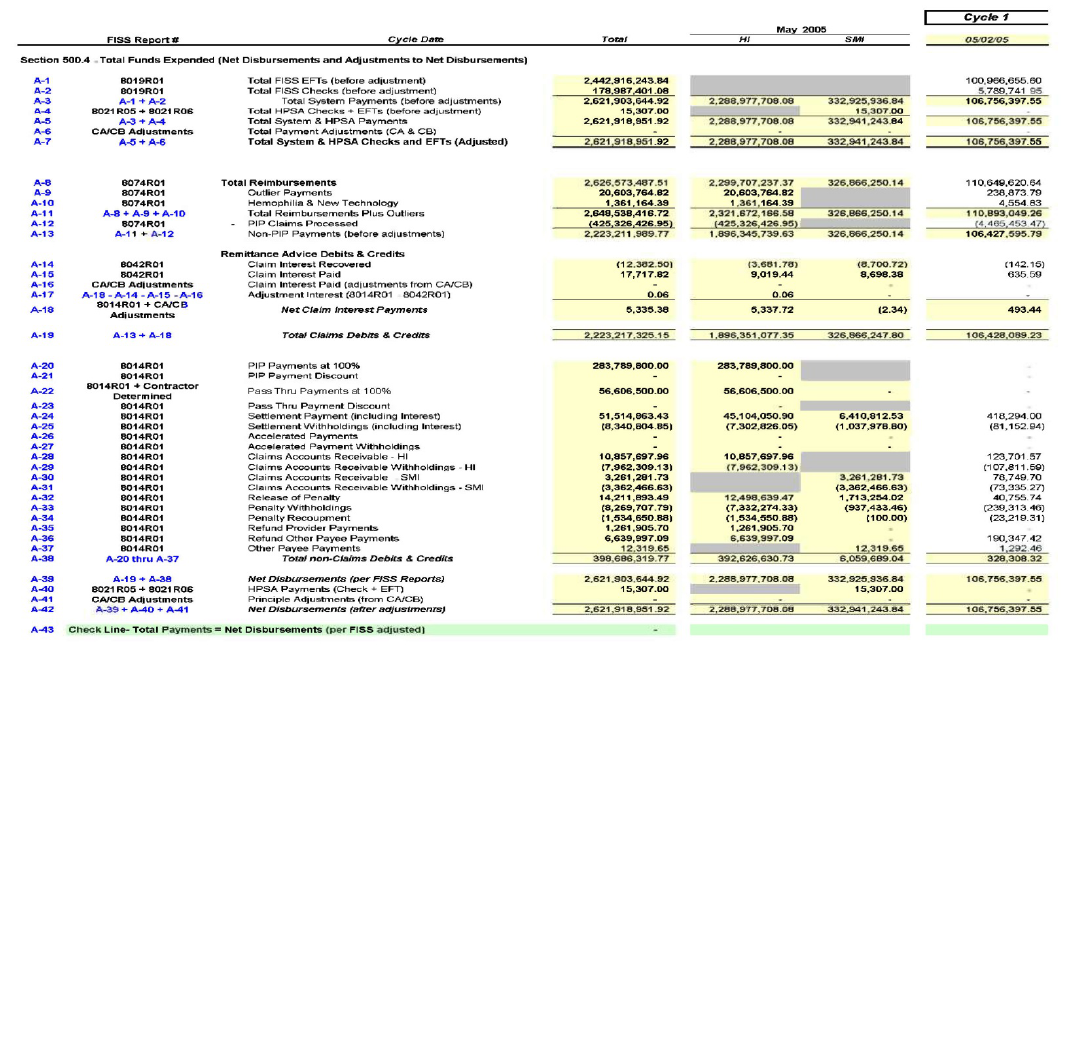
500.4 – Total Funds Expended (Net Disbursements and Adjustments to Net
Disbursements)
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
This section calculates the total system and non-system payments that equate to the Total Funds Expended
amount report on the Form CMS-1522. It also documents the source FISS system report used in determining
the amounts to report. This standard reconciliation format is the only document required to be submitted to
CMS, in addition to monthly financial reports (Form CMS-1522).
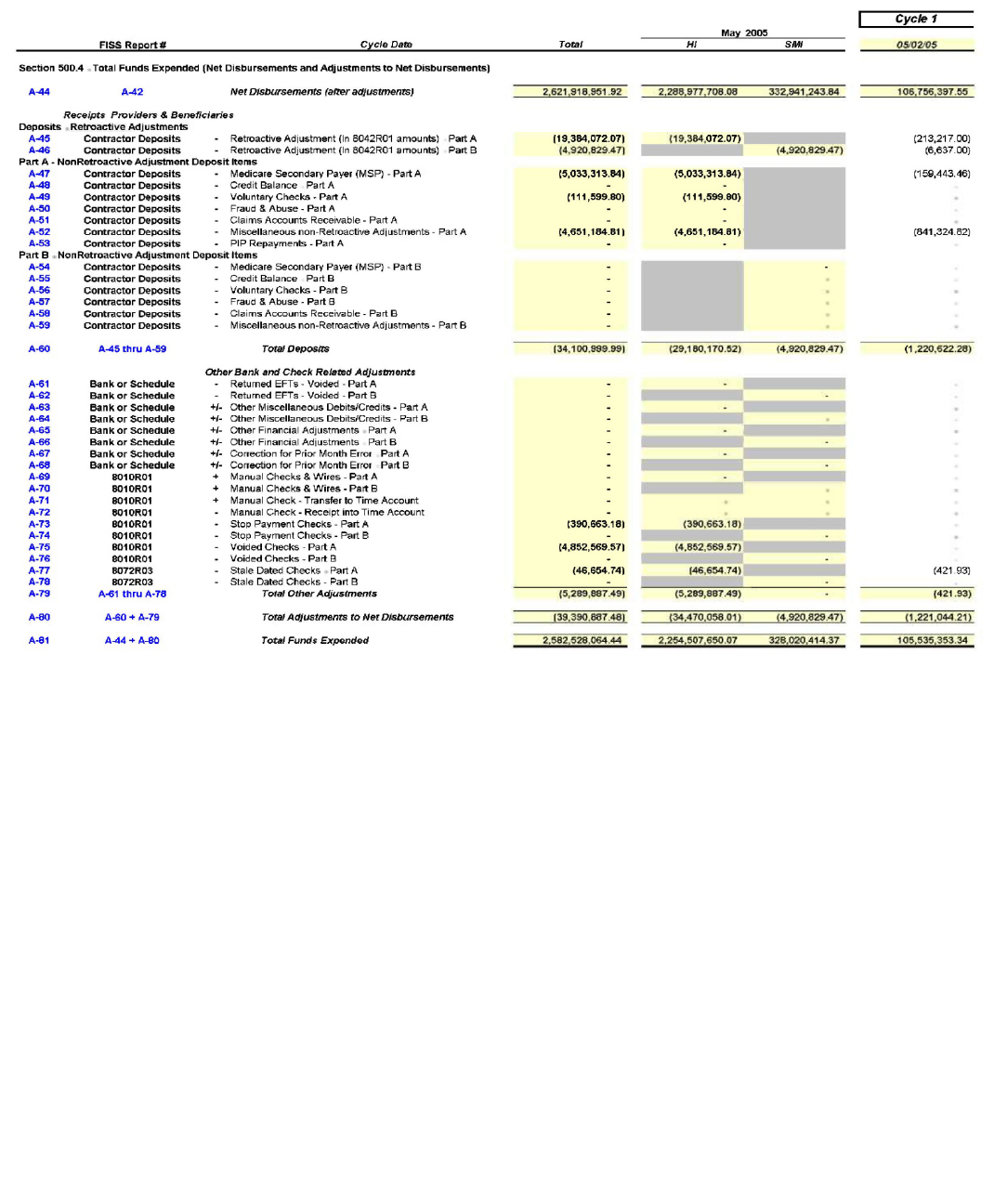
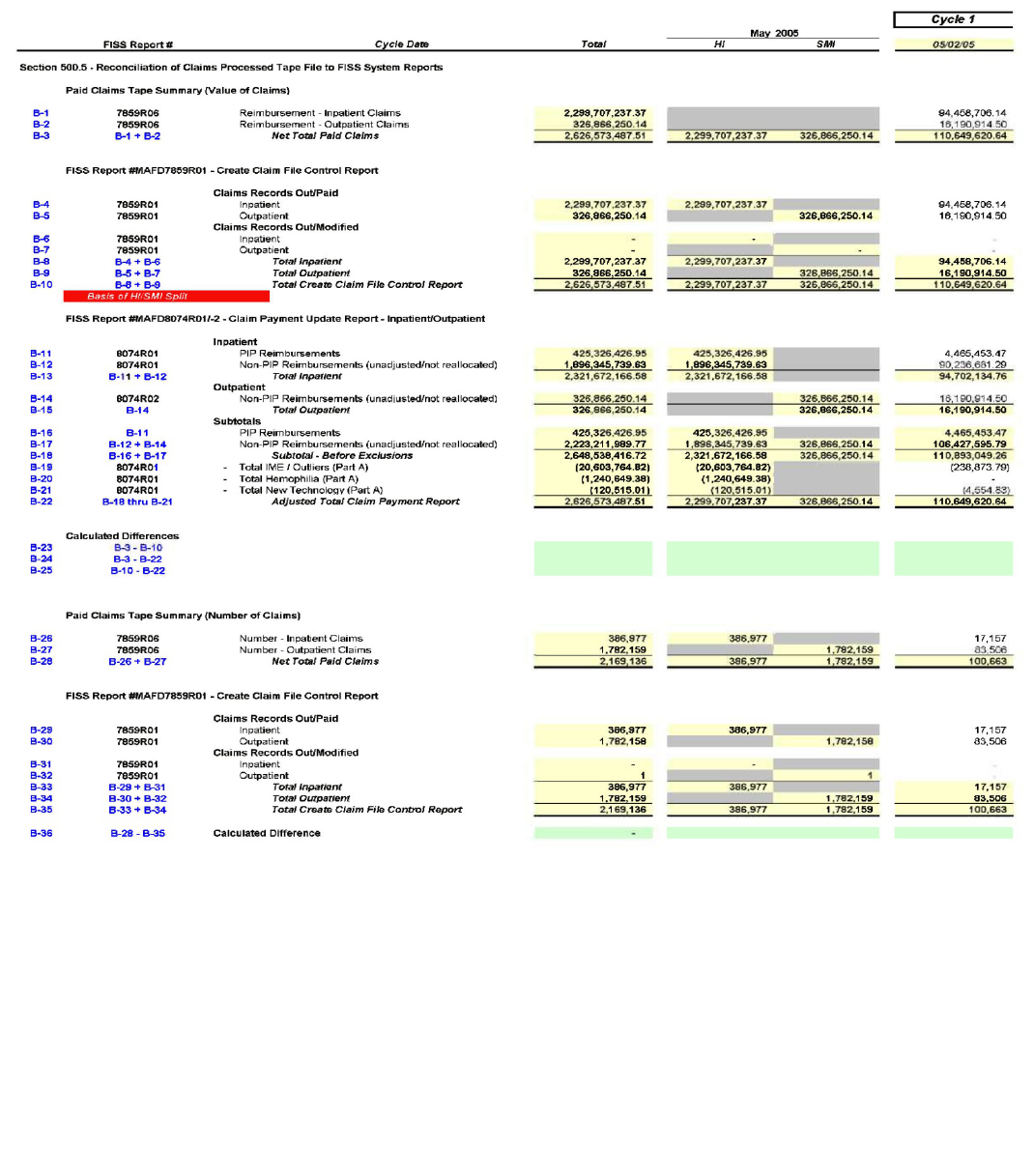
500.5 -- Reconciliation of Detailed Claims Data File to FISS System Reports
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
This section shows the reconciliation of the claims process tape file to the FISS system reports and identifies the
transactions used in reconciling those two amounts.
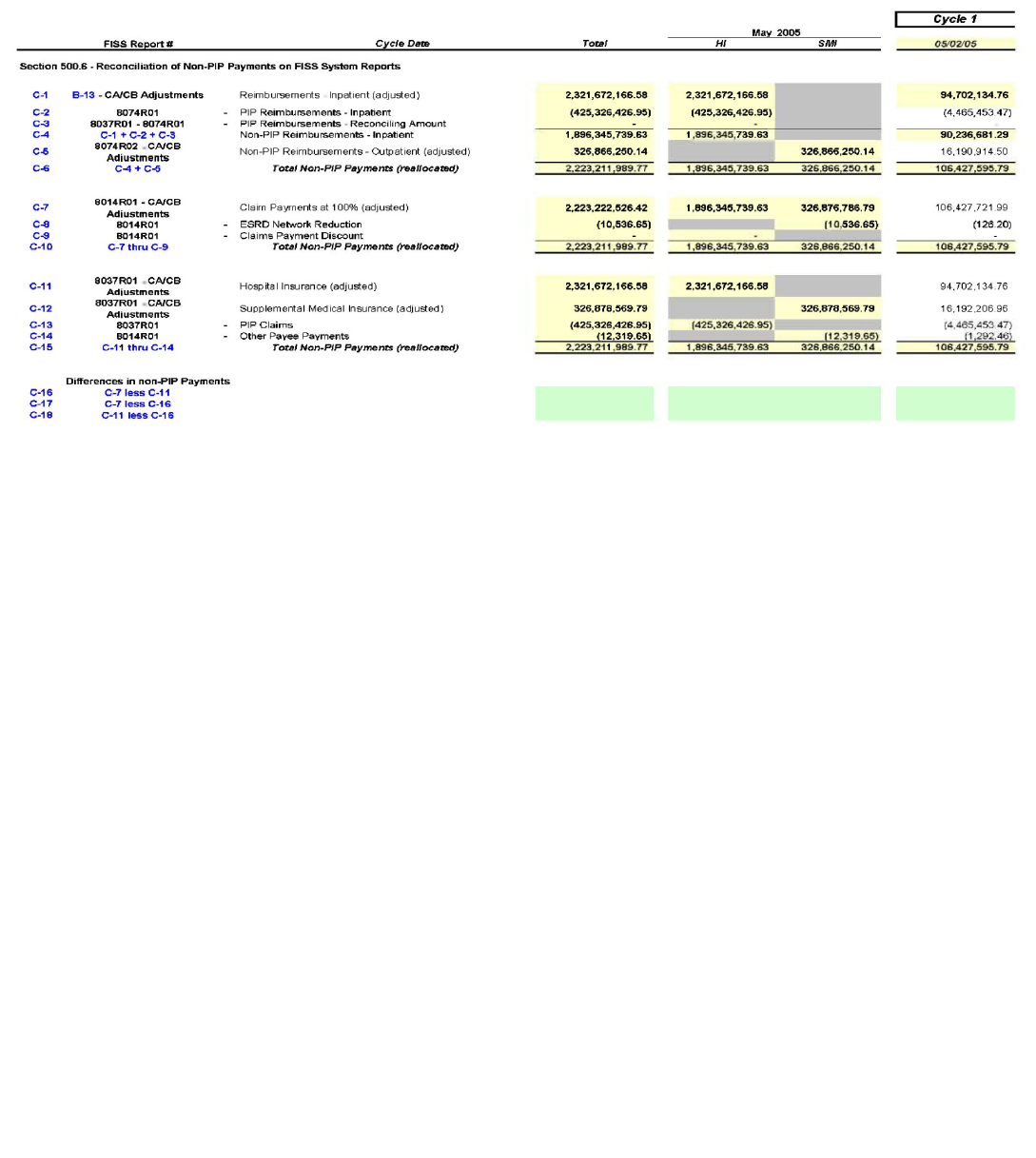
500.6 - Reconciliation of Non-PIP Payments on FISS System Reports
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
The non-PIP payments are identified on various FISS system reports and this section reconciles those amounts
to ensure that the amounts are equal and consistent among those reports. The non-PIP payment amounts are a
key amount used in the calculation for Total Funds Expended identified in Section 500.4 above.
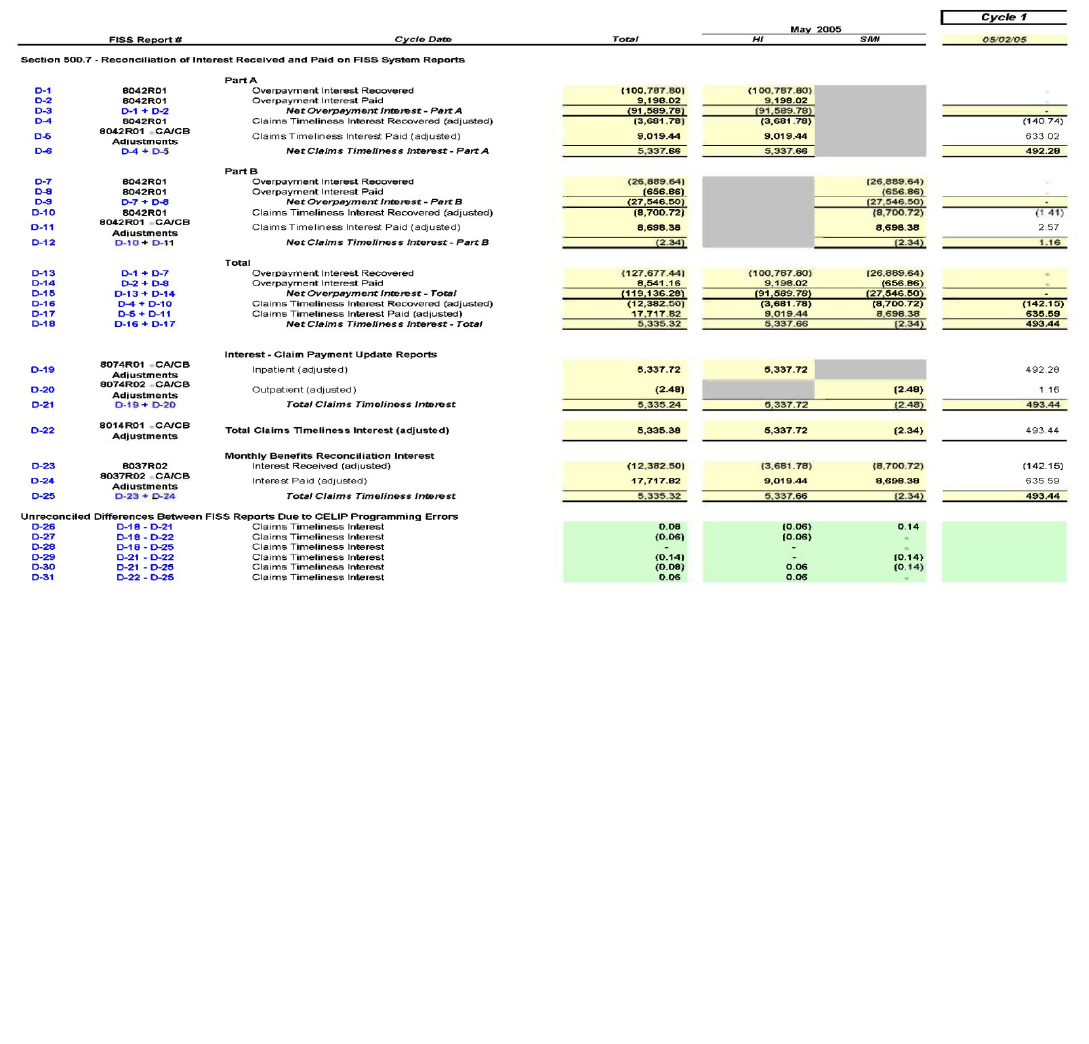
500.7 - Reconciliation of Interest Received and Paid on FISS system reports
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
The interest amount paid or received for overpayment interest or claims timeliness are identified on various
FISS system reports and this section reconciles those amounts to identify any differences. Differences in the
interest amounts reported on those FISS system reports have been identified since the implementation of CELIP
but those differences should be minor. The financial reconciliation uses the most reliable interest amounts from
those different reports. Major differences should be researched and corrective action should be taken if those
amounts are not minor.
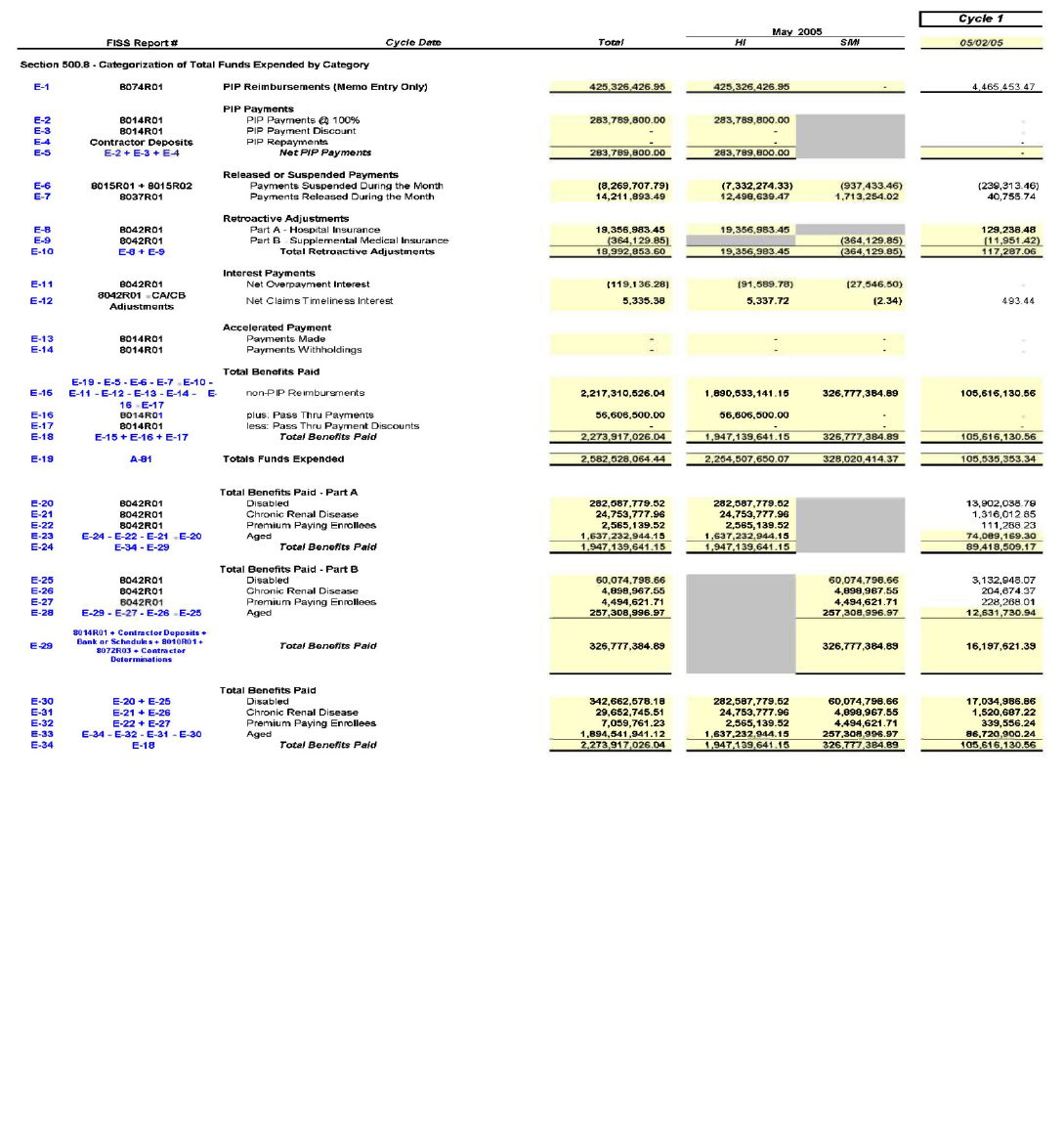
500.8 - Categorization of Total Funds Expended by Category
(Rev. 93, Issued: 04-04-06; Effective/Implementation Dates: 06-01-06)
This section takes the financial information that was input by the user and allocates those amounts to the various
descriptive categories identified on the Form CMS-1522 report. The amounts can generally be used to
complete the Form CMS-1522 with little additional effort.
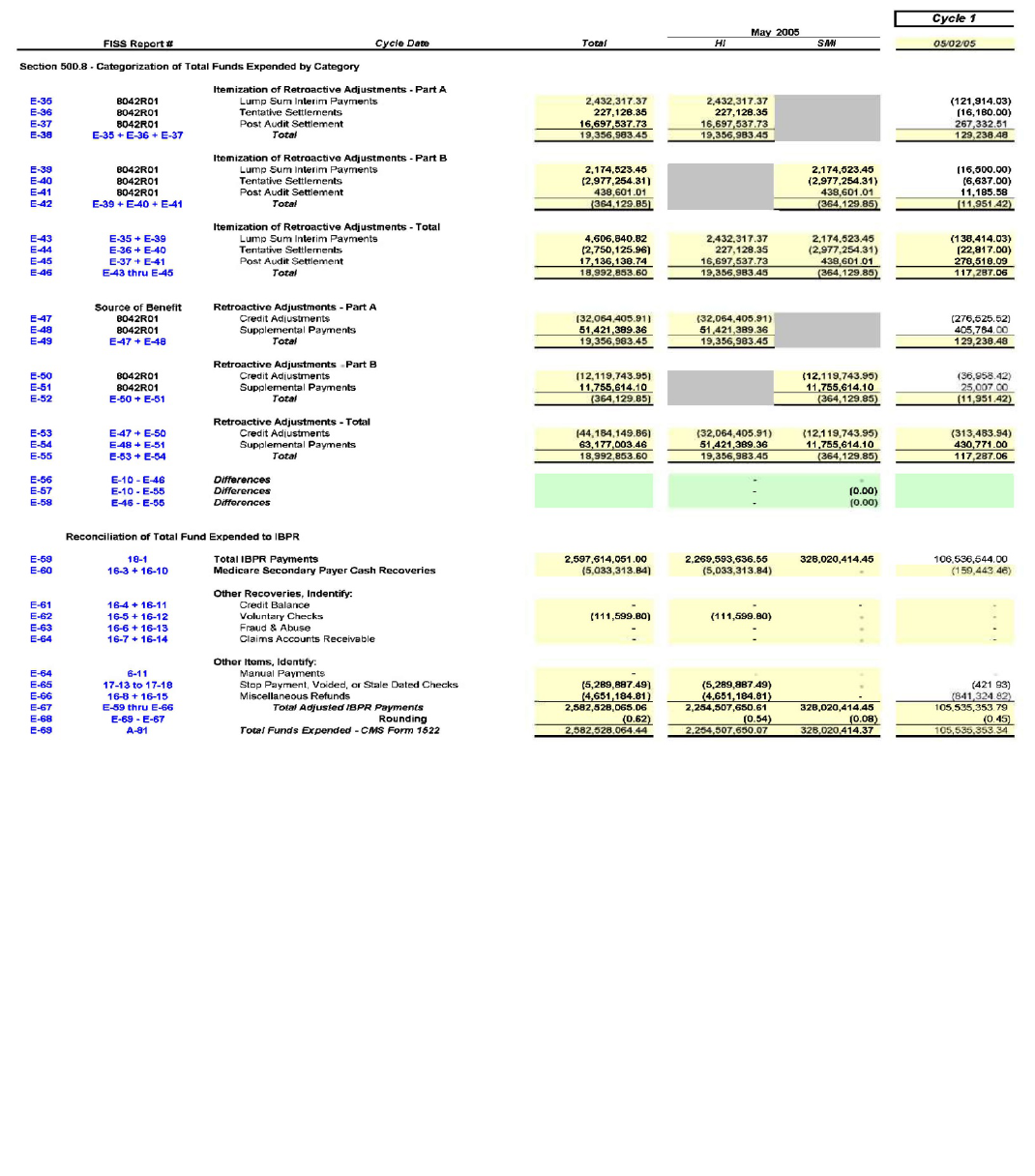
510 – Procedures for the Reconciliation of Total Funds Expended for
Multi-Carrier System (MCS) Medicare Contractors Used in the
Preparation of Form CMS-1522, Monthly Contractor Financial Report
(Rev. 21, 08-01-03)
The Centers for Medicare & Medicaid Services (CMS) continues to have a material
internal control weakness for the reconciliation of total funds expended on Form
CMS-1522 resulting from the Chief Financial Officers Audit. The reconciliation of total
funds expended to adjudicated claims and standard system reports is an important control
that validates that the amounts reported by Medicare contractors are accurate, supported,
and complete.
The CMS requires that Medicare contractors provide a reconciliation of total funds
expended reported on the monthly Form CMS-1522 report by the 15
th
day of the
following month. Form CMS-1522 is a cash-based document and is prepared primarily
from MCS system reports, bank statements, and other internal reports. The financial
reconciliation includes adjudicated claims processed, other non-claims based payments,
overpayment recoveries, and other financial adjustment transactions.
Total funds expended represent payments made for claim and non-claim transactions
during each claims payment cycle (i.e., the total of all checks issued, electronic funds
transfers (EFT) payments, voided checks, overpayment recoveries, and other financial
adjustments). The claims payment cycle varies at each contractor and can be daily,
multi-weekly, or weekly.
All claims submitted during a payment cycle include both adjudicated claims and non-
adjudicated claims. Adjudicated claims represent those claims that were processed for
payment (i.e., payments, denials, or adjustments) and included on the remittance advice
report. Non-adjudicated claims do not appear on the remittance advice and include
demonstration claims, returned to provider claims, and other exception claims. Each
MCS contractor must retain the electronic file received from the MCS Systems
Maintainer that documents the detailed claims records that supports the MCS Summary
Report #2002 for each payment cycle.
Although the enclosed reconciliation format has been tested and proven adequate for
most situations, there may be unique situations at selected contractors that result in an
“unreconciled” difference. When those situations occur, the contractor should investigate
those differences and identify the source and cause for the difference. The standard
format can be adjusted to accommodate those differences so that the reconciliation and
Form CMS-1522 can be completed. Contractors should report those differences to CMS
for further review and adjustment of the standard format.
The lead reconciliation schedule (Section 510.3) must be submitted electronically to the
applicable CMS regional office. MCS system reports, bank statements, and other internal
reports used to create the lead reconciliation schedule must be maintained for three years,
and made available upon request for audit and review by CMS financial personnel and
other external auditors.
Methodology
Contractors are required to complete the financial reconciliation schedules for each
claims processing cycle, and provide a copy of the cumulative monthly totals in the
format established in Section 510.3. The reconciliation should be completed at the end of
each claims payment cycle to identify any differences as they occur and provide
sufficient time to resolve those differences before the next cycle ends. View Exhibit I by
clicking on this link to access the electronic spreadsheet in Mircrosoft Excel®
format to complete the following steps.
To complete the reconciliation for each claims payment cycle, MCS contractors
must:
1. Identify and summarize the detailed claims data file. (Section 510.1)
a. Obtain and retain detailed claims data records that are produced by the
MCS Systems Maintainer (Section 510.1).
b. Identify, summarize, and retain a report of the number and dollar value
of adjudicated claims that are included on the detailed claims data file.
Adjudicated claims include all paid, denied and adjusted claims
processed by MCS. The non-adjudicated claims include
demonstration claims, claims that could not be processed and must be
returned to either the provider or other exceptions claims. Enter the
first day of each month in Column A, line 38 of the electronic
spreadsheet (Section 510.4). For the following specific fields, enter
the claim payments, adjustments, reissues, special issues, recoupments,
and manual issues from the detailed claims data file for each payment
cycle into Columns B, C, D, E, F, and H, respectively of the electronic
spreadsheet (Section 510.5), on reference lines 71 through 101.
c. Obtain MCS Report #2002 or HBDR 2002, Financial Report Month-
To-Date Analysis of Payments, and enter the claim payments,
adjustments, reissues, special issues, recoupments, and manual issues
in Columns B, C, D, E, F, and H, respectively of the electronic
spreadsheet (Section 510.6) on reference lines 105 to 135.
d. Review the daily claim and adjustment differences in Columns D and
G, respectively, on lines 38 to 68 (Section 510.4). The amounts on
those lines should be ZERO; research any differences that are
identified and make corrections to any of the amounts entered in Steps
1b and 1c above.
2. Obtain financial MCS system reports for each claims processing cycle and
enter selected data from those reports onto the electronic spreadsheet (Sections
510.6 through Section 510.8). The CMS will provide an electronic spreadsheet
in Excel® format. For those contractors that have multiple sites, the electronic
spreadsheet has separate tabs, to allow data input for up to 5 sites. The data input
for each site will be consolidated into a separate tab.
Obtain copies of the primary financial MCS system reports that are used in the
financial reconciliation process. A list of those report numbers and report
descriptions is included in Section 510.2.
a. Enter selected financial information from MCS system reports into the
electronic spreadsheet (Sections 510.6 through Section 510.8) that have a
yellow background and were not completed as part of Steps 1b, 1c, or 1d.
b. Review the Net Disbursements Check values in Columns F, lines 171 to
201 (Section 510.8). The amounts on those lines must be ZERO; research
any differences that are identified and make corrections to any of the amounts
entered in Step 2a above.
c. Enter financial information that is not available from MCS system reports
onto lines 204 to 234 of the electronic spreadsheet (Section 510.9).
i. The information for refunds/deposits listed in Column E
lines 204 to 234 (Section 510.9) generally will be supported by
cash logs or deposit tickets that were made to record deposits to
the contractor’s bank account. These refunds/deposits are
generally different from the recoupments generated within MCS
claims processing system and reported on line F of the MCS
HBDR 2002 report. These recoupments are generally controlled
by edits within the MCS system and represent system
withholdings and offsets.
d. The information for voids, stale checks, and stop pays listed in Columns
B, C, and D, lines 204 to 234 (Section 510.9) are generally supported from
the bank statements, bank reports, the manual check listing, the voided and
stale-dated check listing, and other manually maintained listings that identify
correcting financial transactions for the month. Experience has shown that
HBSR0342, HBSR0346, and HBSR0350 can be used to report monthly
voids, stops, and stale dates, respectively. Enter the amount of Do Not
Forward (DNF) checks into Column G, lines 204 to 234 (Section 510.9). The
amount of DNF checks for each payment cycle are generally found in
contractor report, HBDR 6003, Provider Check Register.
3. Finalize the standard reconciliation report (Section 510.3) and submit to CMS
as part of the monthly contractor financial reports.
After completing the process outlined in Steps 1 and 2 above, all of the
financial information needed to identify total funds expended should have
been entered into the standard report format (Section 510.3) automatically.
Overall Summary
The methodology used to identify and summarize the detailed claims data file provided in
Section 510.1, the MCS systems reports identified in Section 510.2, and the standard
report format provided in Section 510.3 are a systematic approach to reconcile financial
activity for each claims payment cycle at MCS Medicare contractors.
The information contained on the attachments provides a standard methodology to
validate financial information contained on the summary level MCS system reports to the
detail claims data or transaction level support. The methodology outlined above and the
information contained on the standard report formats document a standardized approach
to calculate and validate the total funds expended at Medicare contractors.
Also, the standard report formats assist in the preparation of a significant portion of the
Form CMS-1522. The methodology does not provide information relating to the Funds
Drawn from the Treasury presented on lines 1 through 6 of Form CMS-1522, or for the
bank reconciliation information presented on Form CMS-1522, Page 2 and 3, Lines 15
through 23.
Due Date
A copy of Section 510.3, Standard MCS 1522 Reconciliation Schedule, must be provided
electronically to the appropriate CMS regional office’s Associate Regional Administrator
for the Division of Medicare Financial Management by the 15
th
day of the following
month concurrent with the submission of other Contractor Financial Reports and
submitted electronically to [email protected]. All of the Sections (510.3 through
510.9) should be retained to support the information submitted to the appropriate regional
office.
510.1 - Reconciliation of Detailed Claims Data File to Multi-Carrier
System (MCS) Reports
(Rev. 21, 08-01-03)
This section provides the requirements for the detailed claims data file that the MCS
Systems Maintainer must generate for all MCS contractors.
This instruction provides a standard format to perform the reconciliation for contractors
that use the MCS and requires the MCS Systems Maintainer to generate an electronic file
for each contractor’s payment cycle, which includes all detail claim records that support
the totals found on MCS Report #2002. Also the MCS System Maintainer will provide
an independent report that shows the total number of records on the electronic file and the
total dollar value for each of the following fields.
A. Claim Payments
B. Adjustments
C. CPT Interest
D. Reissues
E. Special Issues
F. Recoupments
G. System Issues
H. Manual Issues
I. Total Issues
J. Voids
K. Stale Dates
L. Refunds
M. Stop Pays
N. Net Reimbursement
Each MCS Medicare contractor must enter the summary totals from each line item as
noted above (A through N) from the detailed claims data file into the Excel® spreadsheet
(Exhibit 1). By reconciling the summary totals from the detailed claims data file on a
payment cycle basis, to the summary totals from MCS Report #2002, each MCS
contractor will have assurance that the system report is supported by the detail.
The detailed claims data file must be retained and made available in a format that can be
reviewed by CMS or its external auditors.
510.2 - List of Primary MCS Reports Used in the Reconciliation of Total
Funds Expended – This section identifies the primary MCS system
reports needed to complete the financial reconciliation.
(Rev. 21, 08-01-03)
HBDR2002 - Financial Report Month-To-Date Analysis of Payments
HBDR2055 - EFT Transaction Report
HBDR6000 - Register Summary Report
HBDR6003
– Provider Check Register
HBSR0342
- Monthly Voids
HBSR0346
- Monthly Stops
HBSR0350 - Monthly Stale Dates
Beneficiary Check Register
Bank Statements – Time Account, Disbursement Account, Concentration Account
Bank Reconciliation
List of Daily Deposits for the Month
List of Manual Checks Issued During the Month
List of Voided and State-Dated Checks
List of Other Financial Adjustment Transactions Occurring During the Month
Comment:
The EFT payments reflected on MCS HBDR2055 Report are part of the provider
payments shown in the HBDR6000 report. As a result, the contractor can perform a
simple reconciliation to identify how payments were disbursed (i.e., EFT payments,
provider check payments, and beneficiary check payments).
510.3 - Standard MCS 1522 Reconciliation Lead Schedule – This section calculates the total system and non-system
payments that equate to the Total Funds Expended amount reported on the Form CMS-1522.
(Rev. 21, 08-01-03)
Total
Line #
Description
Amount
Source Document
Detailed Claims Data Reconciliation Activity
1
Detailed Claims Data Totals
15,810,912.00
Detailed Claims Data File/Report
2
Detailed Adjustment Totals
3
4
Subtotal
15,810,912.00
From Line 1
5
6
7
Claim Payments per MCS
15,597,653.42
HBDR2002 Report, Line A
8
Adjustments per MCS
215,103.80
HBDR2002 Report, Line B
9
10
Subtotal
15,812,757.22
Sum of lines 7 & 8
11
12
Difference
(1,845.22)
Line 4 - Line 10
Detailed Claims Data and Non-Claim System Issues
13
Detailed Claims Data Totals
15,810,912.00
From Line 4
14
15
16
Add: Reissues
42,631.55
HBDR2002 Report, Line D
17
Add: Special Issues
30,670.89
HBDR2002 Report, Line E
18
Less: Recoupments
(18,362.54)
HBDR2002 Report, Line F
19
0.00
20
Net Disbursements (System Issues)
15,865,851.90
Sum of Lines 13, 16, 17, & 18
21
22
Add: Manual Issues
0.00
HBDR2002 Report, Line H
23
24
Total Issues Per MCS
15,865,851.90
Line 20 + Line 22
Non-System/Manual adjustments (Cash Activity)
25
Voids
(55,088.48)
Bank Recs/HBSR 0342/General ledger
26
Stales
0.00
Bank Recs/HBSR 0350/General ledger

27
Stop Pays
0.00
Bank Recs/HBSR 0346/General ledger
28
Refunds/Deposits
(112,947.78)
Bank Recs/HBDR 2002/General ledger
39
Journal Entry Adjustments
0.00
Adjusting journal entries
30
Less: DNF (Do Not Forward)
HBDR6003 Report
31
32
Subtotal - Other Adjustments
(168,036.26)
Sum of lines 25 to 30
33
Net Funds Expended Per Reconcilation
15,697,815.64
Line 25 - Line 32
34
35
Net Funds Expended Per CMS-1522 Report
15,699,660.86
Form CMS-1522, Line 5D
36
37
Calculated Difference
(1,845.22)
Line 33 - Line 35
510.4 – Reconciliation of Claim Payments from the Detailed Claims Data File/Report to the Month-to-Date Analysis of
Payment (MCS Report #2002 or HBDR2002) - This attachment is an illustration of the electronic spreadsheet (Exhibit
1) that will be used to input the dollar value of the specific line items from the detailed claims data file on a cycle basis.
(Rev. 21, 08-01-03)
Section 510.4: Reconciliation of Claim Payments from the Detailed Claims Data File/Report to the Month-to-Date Analysis of Payment (HBDR2002)
Col. A
Col. B
Col. C
Col. D
Col. E
Col. F
Col. G
DETAILED
DAILY DIFFERENCE
DETAILED
DAILY DIFFERENCE
CLAIM PAYMENTS
CLAIM PAYMENTS
CLAIM PAYMENTS
ADJUSTMENTS
ADJUSTMENTS
ADJUSTMENTS
LINE
DATE
Report Title ##
HBDR2002
(B-C)
Report Title ##
HBDR2002
(E-F)
38
12/1/2002
0.00
0.00
0.00
0.00
0.00
0.00
39
12/2/2002
0.00
0.00
0.00
350,782.36
(350,782.36)
40
12/3/2002
0.00
0.00
0.00
386,166.12
(386,166.12)
41
12/4/2002
0.00
0.00
0.00
504,327.28
(504,327.28)
42
12/5/2002
0.00
0.00
0.00
309,629.56
(309,629.56)
43
12/6/2002
0.00
0.00
0.00
451,525.15
(451,525.15)
44
12/7/2002
0.00
0.00
0.00
0.00
0.00
45
12/8/2002
0.00
0.00
0.00
0.00
0.00
46
12/9/2002
0.00
0.00
0.00
360,978.06
(360,978.06)
47
12/10/2002
0.00
0.00
0.00
363,366.69
(363,366.69)
48
12/11/2002
0.00
0.00
0.00
361,998.44
(361,998.44)
49
12/12/2002
0.00
0.00
0.00
352,961.21
(352,961.21)
50
12/13/2002
0.00
0.00
0.00
372,426.91
(372,426.91)
51
12/14/2002
0.00
0.00
0.00
0.00
0.00
52
12/15/2002
0.00
0.00
0.00
0.00
0.00
53
12/16/2002
0.00
0.00
0.00
299,624.59
(299,624.59)
54
12/17/2002
0.00
0.00
0.00
695,311.73
(695,311.73)
55
12/18/2002
0.00
0.00
0.00
448,313.96
(448,313.96)
56
12/19/2002
0.00
0.00
0.00
378,403.93
(378,403.93)
57
12/20/2002
0.00
0.00
0.00
391,304.93
(391,304.93)
58
12/21/2002
0.00
0.00
0.00
0.00
0.00
59
12/22/2002
0.00
0.00
0.00
0.00
0.00
60
12/23/2002
0.00
0.00
0.00
338,378.43
(338,378.43)
61
12/24/2002
0.00
0.00
0.00
0.00
0.00
62
12/25/2002
0.00
0.00
0.00
0.00
0.00
63
12/26/2002
0.00
0.00
0.00
416,537.31
(416,537.31)
64
12/27/2002
0.00
0.00
0.00
347,191.72
(347,191.72)
65
12/28/2002
0.00
0.00
0.00
0.00
0.00
66
12/29/2002
0.00
0.00
0.00
0.00
0.00
67
12/30/2002
0.00
0.00
0.00
286,326.18
(286,326.18)
68
12/31/2002
0.00
0.00
0.00
0.00
0.00
69
70
Totals
15,810,912.00
15,597,653.42
(1,845.22)
0.00
215,103.80
(7,415,554.56)
510.5 - Proof of Net Disbursements and Total Issues per Detailed Claims Data File/Report
(Rev. 21, 08-01-03)
This attachment is an illustration of the electronic spreadsheet (Exhibit 1) that will be used to input selected financial information from the detailed
claims data file and MCS reports.
Section 510.5: Proof of Net Disbursements and Total Issues per Detailed Claims Data File/Report
Col. A
Col. B
Col. C
Col. D
Col. E
Col. F
Col. G
Col. H
Col. I
Net Disbursements
Total System
/ System Issues
Issues per MCS
CLAIMS
ADJUSTMENTS
REISSUES
SPECIAL ISSUES
RECOUPMENTS
per Report Title##
MANUAL ISSUES
Report Title ##
LINE
DATE
per Report Title##
per Report Title##
per Report Title##
per Report Title##
per Report Title##
(B + C + D + E - F)
(G + H)
71
12/1/2002
10,912.00
0.00
0.00
0.00
0.00
72
12/2/2002
0.00
0.00
0.00
0.00
73
12/3/2002
0.00
0.00
0.00
74
12/4/2002
0.00
0.00
0.00
75
12/5/2002
13,000,000.00
0.00
0.00
76
12/6/2002
0.00
0.00
0.00
77
12/7/2002
0.00
0.00
0.00
78
12/8/2002
0.00
0.00
0.00
79
12/9/2002
0.00
0.00
0.00
80
12/10/2002
0.00
0.00
0.00
81
12/11/2002
0.00
0.00
0.00
82
12/12/2002
0.00
0.00
0.00
83
12/13/2002
0.00
0.00
0.00
84
12/14/2002
2,000,000.00
0.00
0.00
85
12/15/2002
0.00
0.00
0.00
86
12/16/2002
0.00
0.00
0.00
87
12/17/2002
750,000.00
0.00
0.00
88
12/18/2002
0.00
0.00
0.00
89
12/19/2002
50,000.00
0.00
0.00
90
12/20/2002
0.00
0.00
0.00
91
12/21/2002
0.00
0.00
0.00
92
12/22/2002
0.00
0.00
0.00
93
12/23/2002
0.00
0.00
0.00
94
12/24/2002
0.00
0.00
0.00
95
12/25/2002
0.00
0.00
0.00
96
12/26/2002
0.00
0.00
0.00
97
12/27/2002
0.00
0.00
0.00
98
12/28/2002
0.00
215,103.80
0.00
0.00
99
12/29/2002
0.00
0.00
0.00
100
12/30/2002
0.00
0.00
0.00
101
12/31/2002
0.00
0.00
0.00
102
103
Totals
15,810,912.00
215,103.80
0.00
0.00
0.00
0.00

510.6 - Proof of Net Disbursements and Total Issues Per MCS Report #2002- This attachment is an illustration of the
electronic spreadsheet (Exhibit 1) that will be used to input selected financial information from the detailed claims
data file and MCS reports
(Rev. 21, 08-01-03)
Section 510.6: Proof of Net Disbursements and Total Issues per MCS Report 2002
Col. A
Col. B
Col. C
Col. D
Col. E
Col. F
Col. G
Col. H
Col. I
Net Disbursements
Total System
System Issues
Issues per MCS
Claim Payments
Adjustments
Reissues
Special Issues
Recoupments
per 2002 Rpt
Manual Issues
per 2002 Rpt
LINE
DATE
per 2002 Rpt
per 2002 Rpt
per 2002 Rpt
per 2002 Rpt
per 2002 Rpt
(B + C + D + E - F)
per 2002 Rpt
(G + H)
105
12/1/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
106
12/2/2002
56,837,614.91
350,782.36
0.00
0.00
19,577.76
57,168,819.51
0.00
57,168,819.51
107
12/3/2002
28,657,694.40
386,166.12
446,167.54
31,232.72
62,446.16
29,458,814.62
0.00
29,459,715.02
108
12/4/2002
25,836,609.72
504,327.28
458,444.77
4,215.56
24,027.84
26,779,569.49
0.00
26,779,569.49
109
12/5/2002
1,611,374.85
309,629.56
1,621,431.99
5,486.74
6,527.87
3,541,395.27
0.00
3,541,395.27
110
12/6/2002
36,459,555.90
451,525.15
993,362.07
6,094.26
25,019.12
37,885,518.26
0.00
37,885,518.26
111
12/7/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
112
12/8/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
113
12/9/2002
61,886,815.20
360,978.06
151,348.03
1,990.18
55,071.84
62,346,059.63
0.00
62,420,963.57
114
12/10/2002
6,746,915.52
363,366.69
281,943.38
4,916.06
10,154.04
7,386,987.61
0.00
7,386,987.61
115
12/11/2002
1,560,978.91
361,998.44
412,686.95
7,019.02
9,052.52
2,333,630.80
0.00
2,333,953.99
116
12/12/2002
1,438,627.03
352,961.21
110,819.57
22,974.50
4,249.05
1,921,133.26
0.00
1,921,133.26
117
12/13/2002
45,570,085.67
372,426.91
424,291.27
5,656.62
26,999.81
46,345,460.66
0.00
46,345,460.66
118
12/14/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
119
12/15/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
120
12/16/2002
54,844,402.41
299,624.59
130,391.23
348,707.86
73,868.17
55,549,257.92
0.00
55,549,257.92
121
12/17/2002
31,679,689.47
695,311.73
201,368.02
88,705.27
37,226.64
32,627,847.85
0.00
32,627,847.85
122
12/18/2002
24,924,910.27
448,313.96
311,922.33
283,847.01
15,539.89
25,953,453.68
0.00
25,953,453.68
123
12/19/2002
1,730,017.16
378,403.93
161,007.85
2,533.69
4,923.56
2,267,039.07
0.00
2,267,039.07
124
12/20/2002
38,248,499.74
391,304.93
221,290.52
18,299.27
26,548.11
38,852,846.35
0.00
38,852,846.35
125
12/21/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
126
12/22/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
127
12/23/2002
75,308,262.54
338,378.43
355,736.19
4,717.85
61,550.75
75,945,544.26
0.00
75,945,544.26
128
12/24/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
129
12/25/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
130
12/26/2002
25,424,150.73
416,537.31
141,062.01
2,293.54
24,470.26
25,959,573.33
0.00
25,959,573.33
131
12/27/2002
38,298,027.24
347,191.72
254,271.45
2,661.11
21,756.08
38,880,395.44
0.00
38,880,436.54
132
12/28/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00

133
12/29/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
134
12/30/2002
75,414,126.51
286,326.18
132,848.84
1,521.28
95,808.02
75,739,014.79
0.00
75,739,039.82
135
12/31/2002
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
136
137
Totals
15,597,653.42
215,103.80
42,631.55
30,670.89
(18,362.54)
15,865,851.90
0.00
647,018,555.46
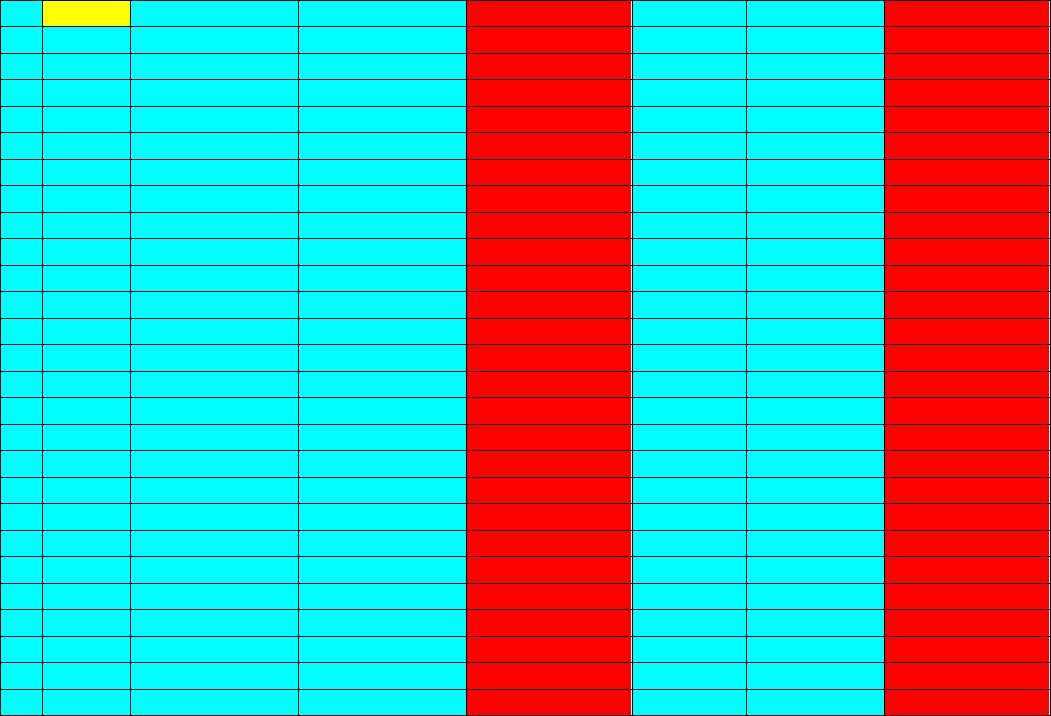
510.7 - Reconciliation of Net Disbursements and System Issues from the Detailed Claims Data File/Report to the
Month-to-Date Analysis of Payment (HBDR2002)
- This attachment is an illustration of the electronic spreadsheet (Exhibit 1) that will
be used to input selected financial information from the detailed claims data file and MCS reports.
(Rev. 21, 08-01-03)
Section 510.7: Reconciliation of Net Disbursements and System Issues from the Detailed Claims Data File/Report to the Month-to-Date
Analysis of Payment (HBDR2002)
Col. A
Col. B
Col. C
Col. D
Col. E
Col. F
Col. G
Net Disbursements
Net Disbursements
System Issues
System Issues
DAILY DIFFERENCE
Total Issues
Total Issues
DAILY DIFFERENCE
(Col. G)
(Col. G)
DISBURSEMENTS
(Col. I)
(Col. I)
ISSUES
LINE
DATE
Report Title ##
HBDR2002
(B-C)
Report Title ##
HBDR2002
(E-F)
138
12/1/2002
0.00
0.00
0.00
0.00
0.00
0.00
139
12/2/2002
0.00
57,168,819.51
(57,168,819.51)
0.00
57,168,819.51
(57,168,819.51)
140
12/3/2002
0.00
29,458,814.62
(29,458,814.62)
0.00
29,459,715.02
(29,459,715.02)
141
12/4/2002
0.00
26,779,569.49
(26,779,569.49)
0.00
26,779,569.49
(26,779,569.49)
142
12/5/2002
0.00
3,541,395.27
(3,541,395.27)
0.00
3,541,395.27
(3,541,395.27)
143
12/6/2002
0.00
37,885,518.26
(37,885,518.26)
0.00
37,885,518.26
(37,885,518.26)
144
12/7/2002
0.00
0.00
0.00
0.00
0.00
0.00
145
12/8/2002
0.00
0.00
0.00
0.00
0.00
0.00
146
12/9/2002
0.00
62,346,059.63
(62,346,059.63)
0.00
62,420,963.57
(62,420,963.57)
147
12/10/2002
0.00
7,386,987.61
(7,386,987.61)
0.00
7,386,987.61
(7,386,987.61)
148
12/11/2002
0.00
2,333,630.80
(2,333,630.80)
0.00
2,333,953.99
(2,333,953.99)
149
12/12/2002
0.00
1,921,133.26
(1,921,133.26)
0.00
1,921,133.26
(1,921,133.26)
150
12/13/2002
0.00
46,345,460.66
(46,345,460.66)
0.00
46,345,460.66
(46,345,460.66)
151
12/14/2002
0.00
0.00
0.00
0.00
0.00
0.00
152
12/15/2002
0.00
0.00
0.00
0.00
0.00
0.00
153
12/16/2002
0.00
55,549,257.92
(55,549,257.92)
0.00
55,549,257.92
(55,549,257.92)
154
12/17/2002
0.00
32,627,847.85
(32,627,847.85)
0.00
32,627,847.85
(32,627,847.85)
155
12/18/2002
0.00
25,953,453.68
(25,953,453.68)
0.00
25,953,453.68
(25,953,453.68)
156
12/19/2002
0.00
2,267,039.07
(2,267,039.07)
0.00
2,267,039.07
(2,267,039.07)
157
12/20/2002
0.00
38,852,846.35
(38,852,846.35)
0.00
38,852,846.35
(38,852,846.35)
158
12/21/2002
0.00
0.00
0.00
0.00
0.00
0.00
159
12/22/2002
0.00
0.00
0.00
0.00
0.00
0.00
160
12/23/2002
0.00
75,945,544.26
(75,945,544.26)
0.00
75,945,544.26
(75,945,544.26)
161
12/24/2002
0.00
0.00
0.00
0.00
0.00
0.00
162
12/25/2002
0.00
0.00
0.00
0.00
0.00
0.00
163
12/26/2002
0.00
25,959,573.33
(25,959,573.33)
0.00
25,959,573.33
(25,959,573.33)
164
12/27/2002
0.00
38,880,395.44
(38,880,395.44)
0.00
38,880,436.54
(38,880,436.54)
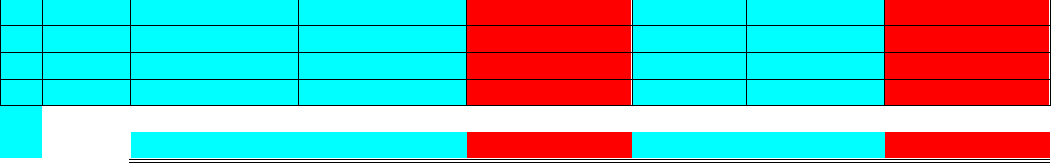
165
12/28/2002
0.00
0.00
0.00
0.00
0.00
0.00
166
12/29/2002
0.00
0.00
0.00
0.00
0.00
0.00
167
12/30/2002
0.00
75,739,014.79
(75,739,014.79)
0.00
75,739,039.82
(75,739,039.82)
168
12/31/2002
0.00
0.00
0.00
0.00
0.00
0.00
169
170
Totals
0.00
15,865,851.90
(646,942,361.80)
0.00
647,018,555.46
(647,018,555.46)
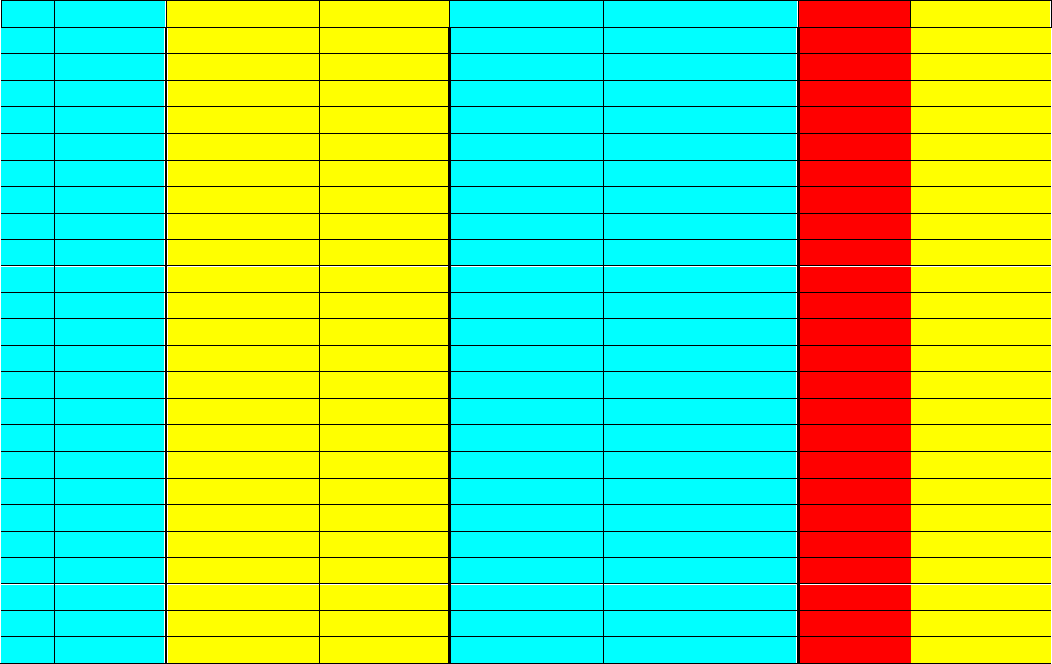
510.8 - Proof of Net Disbursement per MCS Register Summary Report (HBDR6000) to the Month-to-Date Analysis of
Payments (HBDR2002 Report, Line G)
- This attachment is an illustration of the electronic spreadsheet (Exhibit 1) that will be used to
input selected financial information from the detailed claims data file and MCS reports.
(Rev. 21, 08-01-03)
Section 510.8: Proof of Net Disbursement per MCS Register Summary Report
(HBDR6000)
to the Month-to-Date Analysis of Payments (HBDR2002 Report, Line
G)
Col. A
Col. B
Col. C
Col. D
Col. E
Col. F
Col. G
Net Disbursement
Provider
Beneficiary
(System Issues)
Amounts Per
Amounts Per
Total Amounts
HBDR2002 Line G /
Differences
LINE
DATE
HBDR6000
HBDR6000
(B + C)
Detail Data Report
(D - E)
REASON
171
12/1/2002
0.00
0.00
0.00
0.00
0.00
172
12/2/2002
56,797,987.94
370,831.57
57,168,819.51
57,168,819.51
0.00
173
12/3/2002
29,260,656.54
198,158.08
29,458,814.62
29,458,814.62
0.00
174
12/4/2002
26,639,387.24
140,182.25
26,779,569.49
26,779,569.49
0.00
175
12/5/2002
3,517,320.61
24,074.66
3,541,395.27
3,541,395.27
0.00
176
12/6/2002
37,581,035.44
304,482.82
37,885,518.26
37,885,518.26
0.00
177
12/7/2002
0.00
0.00
0.00
0.00
0.00
178
12/8/2002
0.00
0.00
0.00
0.00
0.00
179
12/9/2002
62,035,371.68
310,687.95
62,346,059.63
62,346,059.63
0.00
180
12/10/2002
7,304,404.76
82,582.85
7,386,987.61
7,386,987.61
0.00
181
12/11/2002
2,307,689.22
25,941.58
2,333,630.80
2,333,630.80
0.00
182
12/12/2002
1,887,402.09
33,731.17
1,921,133.26
1,921,133.26
0.00
183
12/13/2002
45,991,947.26
353,513.40
46,345,460.66
46,345,460.66
0.00
184
12/14/2002
0.00
0.00
0.00
0.00
0.00
185
12/15/2002
0.00
0.00
0.00
0.00
0.00
186
12/16/2002
55,267,001.36
282,256.56
55,549,257.92
55,549,257.92
0.00
187
12/17/2002
32,468,909.40
158,938.94
32,627,848.34
32,627,847.85
0.49
188
12/18/2002
25,867,280.72
86,172.96
25,953,453.68
25,953,453.68
0.00
189
12/19/2002
2,233,805.64
33,233.43
2,267,039.07
2,267,039.07
0.00
190
12/20/2002
38,529,814.78
323,031.57
38,852,846.35
38,852,846.35
0.00
191
12/21/2002
0.00
0.00
0.00
0.00
0.00
192
12/22/2002
0.00
0.00
0.00
0.00
0.00
193
12/23/2002
75,527,135.84
418,408.42
75,945,544.26
75,945,544.26
0.00
194
12/24/2002
0.00
0.00
0.00
0.00
0.00
195
12/25/2002
0.00
0.00
0.00
0.00
0.00
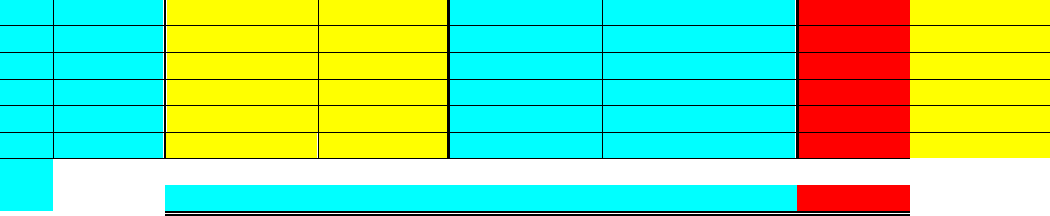
196
12/26/2002
25,872,664.06
86,909.27
25,959,573.33
25,959,573.33
0.00
197
12/27/2002
38,612,629.55
267,765.89
38,880,395.44
38,880,395.44
0.00
198
12/28/2002
0.00
0.00
0.00
0.00
0.00
199
12/29/2002
0.00
0.00
0.00
0.00
0.00
200
12/30/2002
75,266,723.33
472,291.46
75,739,014.79
75,739,014.79
0.00
201
12/31/2002
0.00
0.00
0.00
0.00
0.00
202
203
Totals
642,969,167.46
3,973,194.83
646,942,362.29
646,942,361.80
0.49
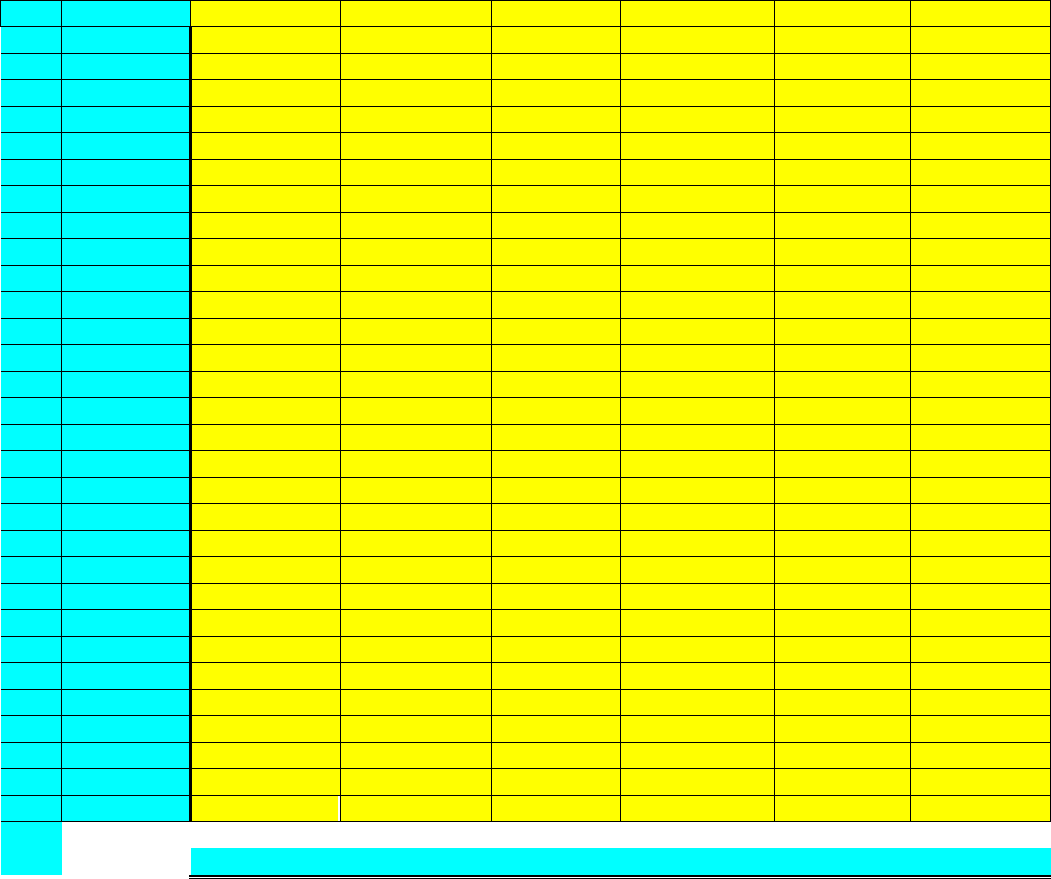
510.9 - Input Sheet for Cash Activity Items - This attachment is an illustration of the electronic
spreadsheet (Exhibit 1) that will be used to input selected financial information that is not available from
MCS system reports.
(Rev. 21, 08-01-03)
Section 510.9: Input Sheet for Cash Activity Items
Col. A
Col. B
Col. C
Col. D
Col. E
Col. F
Col. G
Journal Entry
LINE
DATE
Voids
Stale Checks
Stop Pays
Refunds/Deposits
Adjustments
Do Not Forward
204
12/1/2002
0.00
0.00
0.00
0.00
0.00
205
12/2/2002
0.00
14,703.51
0.00
210,449.81
0.00
206
12/3/2002
411,354.19
0.00
67,887.51
122,233.34
0.00
207
12/4/2002
486,321.97
0.00
54.98
70,959.51
0.00
208
12/5/2002
1,634,262.78
0.00
243.45
169,532.86
0.00
209
12/6/2002
987,998.85
0.00
9,652.67
67,502.88
0.00
210
12/7/2002
0.00
0.00
0.00
0.00
0.00
211
12/8/2002
0.00
0.00
0.00
0.00
0.00
212
12/9/2002
154,369.09
0.00
9,346.12
206,965.75
0.00
213
12/10/2002
263,936.94
0.00
25,719.05
79,635.48
0.00
214
12/11/2002
408,658.22
0.00
12,780.47
96,806.14
0.00
215
12/12/2002
91,313.72
0.00
25,012.61
58,085.88
0.00
216
12/13/2002
420,237.34
0.00
5,594.63
133,095.66
0.00
217
12/14/2002
0.00
0.00
0.00
0.00
0.00
218
12/15/2002
0.00
0.00
0.00
0.00
0.00
219
12/16/2002
126,330.56
0.00
25,884.59
99,784.51
0.00
220
12/17/2002
200,225.96
0.00
2,460.61
93,383.17
0.00
221
12/18/2002
322,815.37
0.00
114,260.96
51,931.80
0.00
222
12/19/2002
173,552.81
0.00
5,989.32
116,754.07
0.00
223
12/20/2002
144,426.08
0.00
78,315.05
134,309.62
0.00
224
12/21/2002
0.00
0.00
0.00
0.00
0.00
225
12/22/2002
0.00
0.00
0.00
0.00
0.00
226
12/23/2002
372,536.52
0.00
0.00
396,332.04
0.00
227
12/24/2002
0.00
0.00
0.00
0.00
0.00
228
12/25/2002
0.00
0.00
0.00
0.00
0.00
229
12/26/2002
136,346.03
0.00
4,980.70
128,880.21
0.00
230
12/27/2002
278,585.61
0.00
41.10
128,987.55
0.00
231
12/28/2002
0.00
0.00
0.00
0.00
0.00
232
12/29/2002
0.00
0.00
0.00
0.00
0.00
233
12/30/2002
133,114.31
0.00
0.00
93,635.05
0.00
234
12/31/2002
0.00
0.00
0.00
0.00
0.00
235
236
Totals
(55,088.48)
0.00
0.00
112,947.78
0.00
0.00
520 – Instructions for Completion of the Contractor’s Monthly Bank
Reconciliation Worksheet
(Rev. 125; Issued: 06-29-07; Effective/Implementation Dates: 07-30-07)
BACKGROUND
Before conversion to the Healthcare Integrated General Ledger Accounting System
(HIGLAS), Medicare Contractors (MC) were required to file the Centers for Medicare &
Medicaid Services (CMS) Form CMS 1521, Contractor Draws on Letter of Credit, and
the Form CMS 1522, Monthly Contractor Financial Report each month via the
Contractor Accounting and Financial Management System (CAFM). These reports are
designed to provide a reconciliation of Medicare program cash benefit payments between
CMS, the contractors, and the contractors’ bank. After conversion to HIGLAS,
transactions are integrated into the general ledger and those reports are no longer needed.
For non-HIGLAS MCs, the Form CMS 1521 reports the amount of “payment vouchers
drawn during the month,” which is an aggregate total of funds drawn down from the
Federal Reserve by the contractor’s bank each day during the month. The draw downs
are used to fund Medicare benefit payments and are based on current benefit payment and
overpayment activity. In HIGLAS, the draws are recorded directly into the general
ledger in account 119504, OTR Mon Aset-Contr LOC Dep.
For non-HIGLAS MCs, the Form CMS 1522 reports all monthly paid claim (i.e., benefit
payments) and non-claim transactions (i.e. periodic interim payments (PIP), accelerated
payments, settlement payments, interest income, and expenses) which, when netted,
account for “total funds expended” for the month. At the contractor level, “total funds
expended” is the sum of all checks drawn and electronic fund transfer payments issued
during the calendar month less voided checks, overpayment recoveries, and other
adjustments as necessary. CMS uses certain information from this report to prepare its
financial statements.
The Contractor’s Monthly Bank Reconciliation Worksheet (Worksheet) is designed to
provide a monthly reconciliation of the Medicare Contractor’s benefit and time account
activity to the CMS Monthly Balance Sheet and Summary 2 Trial Balance.
In HIGLAS, The Medicare Contractor bank reconciliation process is comprised of
reconciling the bank cleared check payments, the bank settled EFT payments, Zero
Dollar payments (Checks and EFTs) and creating and reconciling miscellaneous
transactions. The claim payments are adjudicated in the shared system (FISS and MCS)
and interfaced into HIGLAS. Payments are processed in HIGLAS and the relevant
payment and remittance information is sent to the shared systems. The bank cleared
check payments, bank settled EFT payments, Zero Dollar payments, and miscellaneous
transactions are maintained for each bank account in a separate bank statement for each
day.
DUE DATE
Contractor shall provide a copy of the Worksheet electronically to the appropriate CMS
regional office Associate Regional Administrator (ARA) for the Division of Medicare
Financial Management by the 15
th
day of the following month and shall be submitted
electronically to [email protected]. All bank statements and other internal
reports used to complete the Worksheet shall be maintained for three years and made
available upon request for audit and review by CMS financial personnel and other
external auditors. Internal reports may be saved as text files.
Section A. Bank Statement and Cash Balance
This section is to determine the total end-of-the-month cash balance using the bank
statement(s) from the Benefits Account and the Time Account.
Line 1. Balance Beginning of the Month (Benefits Account). Contractor shall
enter the balance in the Benefits Account as of the beginning of the calendar
month as shown on the bank statement.
Line 1a. Add: Line of Credit Draws. Contractor shall enter the total amount of
funds drawn on payment vouchers during the month and credited to the Benefits
Account as shown on the bank statement.
Line 1b. Cash Deposits. Contractor shall enter all other deposits credited during
the month to the Benefits Account as shown on the bank statement.
Line 1c. Transfer In From Time Account. Contractor shall include funds
withdrawn from the Time Account and deposited in the Benefits Account.
Line 1d. Miscellaneous Add Backs (Briefly explain in Section E—Remarks in
the area labeled Section A, Line 1d) Contractor shall enter any miscellaneous
adjustments, i.e., credit memos, to the Benefits Account during the calendar
month.
Line 1e. Total Additions. This is the total of Lines 1a through 1d. Contractor
shall make no entry on this line.
Line 1f. Less: Checks Honored By Bank. Contractor shall enter the total funds
charged to the Benefits Account as a result of checks honored by the bank during
the month. Transfers to the Time Account shall be excluded from this total.
Line 1g. EFTs. Contractor shall enter the electronic funds transferred by the
bank during the month. Transfers to the Time Account shall be excluded from
this total.
Line 1h. Transfer Out To Time Account. Contractor shall enter only amount
of funds withdrawn from the Benefits Account and deposited in the Time Account
during the month.
Line 1i. Miscellaneous Deductions (Briefly explain in Section E—Remarks in
the area labeled Section A, Line 1i). Contractor shall enter any miscellaneous
adjustments, i.e., debit memos, and charges made to the Benefits Account that are
part of the bank statement.
Line 1j. Total Deductions. This is the total of Lines 1f through 1i. Contractor
shall make no entry on this line.
Line 2. Balance End of Month Per Bank Statement(s) - This is the total of
Lines 1 + 1e – 1j. Contractor shall make no entry on this line. This total shall
equal the balance of the bank statement(s) for the Benefit Account(s) at month-
end.
Line 2a. Add: Deposits-In-Transit - Contractor shall enter deposits made and
recorded in the General Ledger during the month that the bank has not yet
credited to the Benefits Account according to the bank statement.
Line 3. Adjusted Bank Balance (Benefits Account) - (Explain in Section E—
Remarks, “Other,” if not equal to Section B, Line 1a, Col D) This is the total of
Lines 2 + 2a. Contractor shall make no entry on this line. This total should equal
the Benefits Account per the balance sheets as summarized in Section B, Line 1a,
Column D. Contractor shall explain any difference.
Line 4. Beginning Balance (Time Account) - Contractor shall enter the balance
in the Time Account as of the beginning of the calendar month.
Line 4a. Add: Transfer In From Benefits Account - Contractor shall include
funds withdrawn from the Benefits Account and deposited in the Time Account.
Line 4b. Less: Transfer Out To Benefits Account - Contractor shall enter only
amount of funds withdrawn from the Time Account and deposited in the Benefits
Account during the month.
Line 5. Ending Balance (Time Account) - (Explain in Section E—Remarks,
“Other,” if not equal to Section B, Line 1b, Col D) This is the total of Lines 4 +
4a – 4b. Contractor shall make no entry on this line. This total should equal the
Time Account per the balance sheets as summarized in Section B, Line 1b,
Column D. Contractor shall explain any difference.
Line 6. Add: Un-deposited Collections - (Explain in Section E—Remarks,
“Other,” if not equal to Section B, Line 1c, Col D) Contractor shall enter
collections received during the month, but not yet recorded as unapplied receipts
in HIGLAS and not yet deposited in the Benefits Account. This line should equal
the Un-deposited Collections per the balance sheets as summarized in Section B,
Line 1c, Column D. Contractor shall explain any difference.
Line 7. Adjusted Bank Statement Cash Balance - This is the total of Lines 3 +
5 + 6, the adjusted ending balance of the Benefits Account, the ending balance of
the Time Account and the balance of the Un-deposited Collections. This balance
should reconcile to the Total Cash per the balance sheets as summarized in
Section B, Line 2, Column D. Contractor shall make no entry on this line.
Section B. Balance Sheet & Summary 2 Trial Balance
This section summarizes the cash balances for the General Fund (050720), the SMI Trust
Fund (050960), and the HI Trust Fund (050961) using the corresponding end-of-the-
month Balance Sheets and Summary 2 Trial Balances for each fund. Contractor shall
compare these cash balances to the Adjusted Bank Statement Cash Balance computed in
Section A and verify that the total cash ending balance for the month reflected in the
General Ledger is properly reported in the Balance Sheets for the three funds
respectively. The Total amount for each line item is automatically computed after the
required amounts are entered for each of the three funds.
Line 1. Balance Sheet (Title)
Line 1a. Total Benefits Account - Using the three Balance Sheets, contractor
shall enter the Total Benefits Account ending balance for each corresponding
fund.
Line 1b. Total Time Account - Using the three Balance Sheets, contractor shall
enter the Total Time Account ending balance for each corresponding fund.
Line 1c. Un-deposited Collections - Using the three Balance Sheets, contractor
shall enter the Un-deposited Collections ending balance for each corresponding
fund.
Line 2. Total Cash (Per Balance Sheet) - This is the total of Lines 1a + 1b + 1c.
Contractor shall make no entry on this line.
Line 3. Summary 2 Trial Balance (Title)
Line 3a. 119502 Other Mon Asset-Disb Contrl - Using the three Summary 2
Trial Balances, contractor shall enter the ending balance from this GL account for
each corresponding fund.
Line 3b. 119503 Other Mon Asset-Contr Deposit - Using the three Summary 2
Trial Balances, contractor shall enter the ending balance from this GL account for
each corresponding fund.
Line 3c. 119504 Other Mon Asset-LOC - Using the three Summary 2 Trial
Balances, contractor shall enter the ending balance from this GL account for each
corresponding fund.
Line 3d. 119505 Other Mon Asset-Tsf Frm/To Time - Using the three
Summary 2 Trial Balances, contractor shall enter the ending balance from this GL
account for each corresponding fund.
Line 3e. 119520 Other Mon Asset-YE Rollover - Using the three Summary 2
Trial Balances, contractor shall enter the ending balance from this GL account for
each corresponding fund.
Line 4. Total Benefits Account Cash Balance - This is the total of Lines 3a
through 3e. Contractor shall make no entry on this line.
Line 4a. 119002 Other Cash-Time Account - Using the three Summary 2 Trial
Balances, contractor shall enter the ending balance from this GL account for each
corresponding fund.
Line 4b. 111002 Un-deposited Collections - Using the three Summary 2 Trial
Balances, contractor shall enter the ending balance from this GL account for each
corresponding fund.
Line 5. Total Cash (Per Summary 2 Trial Balance) - This is the total of Lines
4 + 4a + 4b. Contractor shall make no entry on this line.
Section C. Cash Reconciliation - Bank Statement, Balance Sheet & Summary 2 Trial
Balance
This section is a comparison of the cash balances of the Summary 2 Trial Balance,
balance sheets and the adjusted bank statement cash balance as computed in Section A of
the Worksheet.
Line 1. Cash Balance (per Summary 2 Trial Balance) – The amount for this
line is equal to Section B, Line 5, Column D of the Worksheet, Total Cash per the
Summary 2 Trial Balance. The cell reference for this value has been placed on
this line. Contractor shall make no entry.
Line 2. Less: Adjusted Bank Statement Cash Balance – The amount for this
line is equal to Section A, Line 7, Column B of the Worksheet, Adjusted Bank
Statement Cash Balance. The cell reference for this value has been placed on this
line. Contractor shall make no entry.
Line 3. Net Difference – The template computes the difference between Line 1
and Line 2 amounts. Contractor shall make no entry on this line. Ordinarily,
there should be no difference between total cash as computed from the Summary
2 Trial Balance account balances and the adjusted bank statement cash balance as
computed in Section A. If there is a difference, the contractor shall briefly
explain the difference in Section E. Remarks in the area labeled Section C, Line 3.
Line 4. Cash Balance (Per Summary 2 Trial Balance) – The amount for this
line is equal to Section B, Line 5, Column D of the Worksheet, Total Cash (per
Summary 2 Trial Balance). The cell reference for this value has been placed on
this line. Contractor shall make no entry.
Line 5. Less: Cash Balance (Per Balance Sheet) - The amount for this line is
equal to Section B, Line 2, Column D of the Worksheet, Total Cash (Per Balance
Sheet). The cell reference for this value has been placed on this line. Contractor
shall make no entry.
Line 6. Net Difference – The template computes the difference between Line 4
and Line 5 amounts. Contractor shall make no entry on this line. Ordinarily,
there should be no difference between total cash as computed from the Summary
2 Trial Balance account balances and the Total Cash (Per Balance Sheet). If there
is a difference, the contractor shall briefly explain the difference in Section E.
Remarks in the area labeled Section C, Line 6.
Section D. Disbursements in Transit
Disbursements in Transit is the HIGLAS term for what is commonly referred to as
outstanding checks and EFTs. This section is a verification of general ledger account
212001-A/P Disbursement in Transit and the line item in the balance sheet liability
section-Disbursements in Transit. The Disbursements in Transit Reconciliation is a proof
of the balance of the Disbursements in Transit amount as of the end of the current month,
starting from the month’s beginning balance of the CMS Cash in Transit Report and
computing the ending balance using HIGLAS summary reports and bank statement
information. The total of the computed CMS Cash in Transit Report as of the end of the
month is then compared to the ending balance of the Actual CMS Cash in Transit Report,
the ending balance of the Disbursements in Transit in the trial balance and the month end
balance of Disbursements in Transit line in the balance sheet. The contractor shall enter
all amounts in Lines 1a through 1f as positive numbers. The contractor shall enter a
positive number in Line 1g if the amount is intended to be added to the total in Line 1h
and shall enter a negative number in Line 1g if the amount is intended to be subtracted
from the total in Line 1h.
Line 1. HIGLAS Cash in Transit Report Reconciliation – (Title)
Line 1a. HIGLAS Cash in Transit Report – End of prior month – Contractor
shall enter the grand total from the prior month end CMS Cash in Transit Report.
This is the beginning balance for the reconciliation.
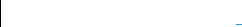
Line 1b. Less: Checks and EFTs honored by the bank in the previous month
but reconciled in HIGLAS in the current month – Contractor shall enter the
total checks and EFTs that the contractor reconciled in HIGLAS in the current
month that the bank honored in the prior month based on the total of the CMS
Cleared Transaction Report for the time period recorded. The contractor shall
enter zero if there are no checks or EFTs in this category.
Line 1c. Add: Checks and EFTs honored by the bank in the current month
but reconciled in HIGLAS in the next month – Contractor shall enter the total
checks and EFTs that the contractor reconciled in HIGLAS in the next month that
the bank honored in the current month based on the CMS Cleared Transaction
Report for the time period recorded. The contractor shall enter zero if there are no
checks or EFTs in this category.
Line 1d. Add: Checks and EFTs issued per the CMS Payment Register for
the month (excluding false confirms) – Contractor shall enter the total checks
and EFTs issued during the current month, including manual checks, per the total
of the CMS Payment Registers for each day of the current month less the amount
of false confirms for the month. This net amount of the checks and EFTs issued
during the month is an addition to the disbursements in transit.
Line 1e. Less: Checks and EFTs voided in HIGLAS (excluding false
confirms) – Contractor shall enter the total checks and EFTs voided during the
current month per the total of the CMS AP Daily Voids Report for the current
month less the amount of false confirms. This net amount of checks voided
during the month is a subtraction to the disbursements in transit.
Line 1f. Less: Checks and EFTs honored by the bank – This is an amount
computed by the template. It is the sum of the checks and EFTs entered on lines
1f and 1g of Section A. The checks and EFTs honored by the bank are
subtractions to the disbursements in transit. Contractor shall make no entry on
this line.
Line 1g. Add/(Less): Bank payment adjustments (Briefly explain in Section E.
Remarks in the section labeled Section D, Line 1g) – This is an amount of checks
and EFTs that have not been reconciled in HIGLAS because the bank charged a
different amount or bank adjustments that the contractor has not had time to enter
in HIGLAS before the month close. This can be a positive or negative amount.
The contractor shall enter zero if there are no bank payment adjustments in this
status.
Line 1h. Calculated HIGLAS Cash in Transit – End of current month – This
is an amount computed by the template. It is the net result of the additions and
subtractions to the beginning balance of the HIGLAS Cash in Transit Report.
This amount should reconcile to the balance of account 212001 A/P Disbursement
in Transit (Section D, Line 2a, Column D), the balance sheet line item amount,
Disbursement in Transit (Section D, Line 4a, Column D) and should equal the
actual HIGLAS Cash in Transit Report as of the end of the current month.
Contractor shall make no entry on this line.
Line 1i. Actual HIGLAS Cash in Transit – End of current Month –
Contractor shall enter the total checks and EFT’s outstanding at the end of the
current month per the total of the CMS Cash in Transit Report run in HIGLAS as
of the last day of the current month after all transactions affecting the report for
the month have been entered.
Line 2. Summary 2 Trial Balance – (Title)
Line 2a. 212001 A/P Disbursements in Transit - The template adds the ending
balance of account 212001 in the Summary 2 Trial Balance for the three funds,
General, SMI and HI to obtain the total Disbursements in Transit as of the end of
the month per the Summary 2 Trial Balance. Contractor shall enter the ending
balance of account 212001 from the Summary 2 Trial Balance for each fund. The
contractor shall enter credit balances as negative numbers and debit balances as
positive numbers. Fund 050720, General Fund, is entered in Line 2a, Column A;
Fund 050960, SMI Trust Fund, is entered in Line 2a, Column B; Fund 050961, HI
Trust Fund is entered in Line 2a, Column C. The formula for the sum of Line 2a,
Columns A, B and C has been entered in Line 2a, Column D. Contractor shall not
make an entry in Line 2a, Column D.
Line 3. Balance Sheet – (Title)
Line 3a. Disbursements in Transit – The template adds the balance of the
Disbursements in Transit line in the balance sheet for the three funds, General,
SMI and HI to obtain the total Disbursements in Transit for the current month per
the balance sheet. Contractor shall enter the balance of the Disbursement in
Transit line of the balance sheet for each fund for the current month. Fund
050720, General Fund, is entered in Line 3a, Column A; Fund 050960, SMI Trust
Fund, is entered in Line 3a, Column B; Fund 050961, HI Trust Fund is entered in
Line 3a, Column C. The formula for the sum of Line 3a, Columns A, B and C has
been entered in Line 3a, Column D. Contractor shall not make an entry in Line
3a, Column D.
Line 4. Differences – (Title)
Line 4a. Difference – Trial Balance and Actual HIGLAS Cash in Transit
Report total – The template computes the difference between Section D Line 2a
Column D and Section D Line 1i. If there is a difference between the ending
balance of the HIGLAS Cash in Transit Report as produced in HIGLAS and the
Disbursements in Transit per the Summary 2 Trial Balance, the contractor shall
briefly explain the difference in Section E Remarks in the area labeled Section D,
Line 4a. Contractor shall make no entry on this line.
Line 4b. Difference – Trial Balance and Balance Sheet – The template
computes the difference between Section D, Line 2a, Column D and Section D,
Line 3a, Column D. If there is a difference between the ending balance of
Disbursements in Transit per the month end balance sheet(s) and the
Disbursements in Transit per the Summary 2 Trial Balance, the contractor shall
briefly explain the difference in Section E Remarks in the area labeled Section D,
Line 4b. Contractor shall make no entry on this line.
Line 4c. Difference – Calculated and Actual Cash in Transit Reports – End
of current month – The template computes the difference between Section D,
Line 1h and Section D, Line 1i. If there is a difference between the end of month
totals of the Cash in Transit Reports as calculated in the template and as produced
by HIGLAS, the contractor shall briefly explain the difference in Section E
Remarks in the area labeled Section D, Line 4c. Contractor shall make no entry
on this line.
Section E. Remarks
This section of the Worksheet is for explanations of specific differences and
miscellaneous line items as previously described in other sections.
Section A, Line 1d – Contractor shall enter a brief description of the
miscellaneous add backs that the bank has reported in the current bank statement.
Section A, Line 1i – Contractor shall enter a brief description of the
miscellaneous deductions that the bank has reported in the current bank statement.
Section C, Line 3 – Contractor shall enter a brief explanation for the difference
between the cash balance per the Summary 2 Trial Balance and the adjusted bank
statement cash balance.
Section C, Line 6 – Contractor shall enter a brief explanation for the difference
between the cash balance per the Summary 2 Trial Balance and the cash balance
per the balance sheet(s).
Section D, Line 1g – Contractor shall enter a brief description of the bank
payment adjustments entered on this line.
Section D, Line 4a - Contractor shall enter a brief explanation for the difference
between the Disbursements in Transit per the Summary 2 Trial Balance and the
ending balance of the HIGLAS Cash in Transit Report.
Section D, Line 4b - Contractor shall enter a brief explanation for the difference
between the Disbursements in Transit per the Summary 2 Trial Balance and the
Disbursements in Transit per the balance sheet(s).

Section D, Line 4c – Contractor shall enter a brief explanation for the difference
between the calculated HIGLAS Cash in Transit amount as calculated in Section
D Line 1h and the total of the actual Cash in Transit Report run in HIGLAS as of
the end of the month.
Request ID’s – Contractor shall enter the HIGLAS request ID’s of the reports run
by the contractor that are the source of the information in Sections B and D.
False Confirms Excluded – Contractor shall enter the amount of the false
confirms subtracted from the CMS Payment Register Report total of the checks
and EFTs issued to compute the entry in Section D Line 1d. Contractor enters the
amount of the false confirms subtracted from CMS AP Daily Voids Report(s) to
compute the entry in Section D Line 1e.
Other – Contractor shall enter a brief explanation if any of the following
conditions are met:
The adjusted bank balance (Section A, Line 3) does not equal the total
benefits account per the balance sheet (Section B, Column D, Line 1a)
The ending balance of the Time Account (Section A, Line 5) does not
equal the total Time Account per the balance sheet (Section B, Column D,
Line 1b)
The Un-deposited Collections (Section A, Line 6) does not equal the Un-
deposited Collections per the balance sheet (Section B, Column D, Line
1c)
Contractor may enter any additional information relevant to this bank
reconciliation worksheet in this section of the worksheet.
HIGLAS contractor shall click on the following link to access the Contractor's Monthly
Bank Reconciliation Worksheet: HIGLAS~BankRecon-Worksheet 05-03-07 (2).xls
Transmittals Issued for this Chapter
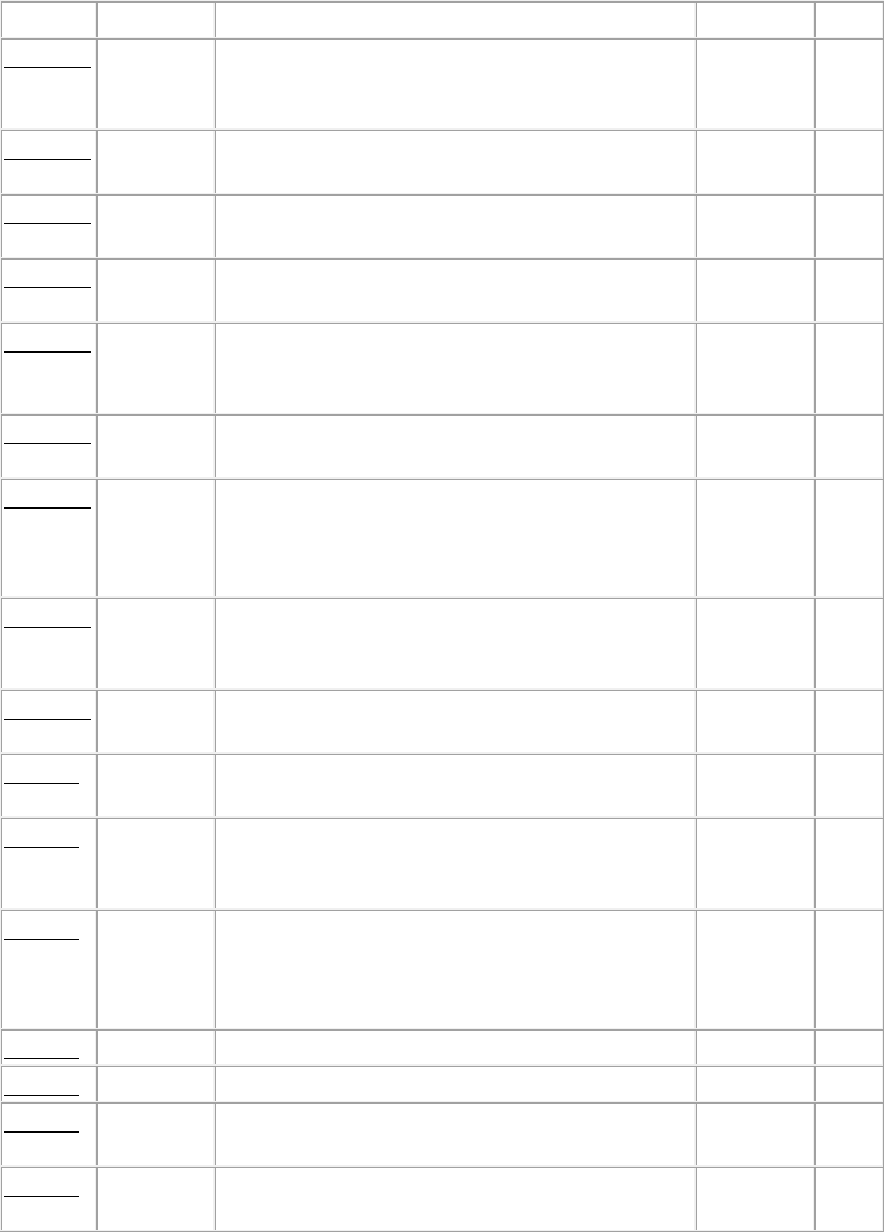
Rev #
Issue Date
Subject
Impl Date
CR#
R315FM
05/17/2019
Update to Publication (Pub.) 100-06 to Provide
Language-Only Changes for the New Medicare
Card Project
06/18/2019
11211
R236FM
06/13/2014
Revisions to Pub. 100-06, Section 100.2 –
Amending Letter of Credit
07/15/2014
8663
R158FM
09/25/2009
Revised Bank Account Analysis Procedure and
Letter-of-Credit List
10/26/2009
6644
R125FM
06/29/2007
Instructions for Completion of the Contractor’s
Monthly Bank Reconciliation Worksheet
07/30/2007
5592
R122FM
05/25/2007
CMS Reporting Requirements With the
Exception of MSP for Unsolicited/Voluntary
Refunds
06/25/2007
5570
R120FM
04/24/2007
Accounts Receivable Trending Analysis
Procedures
07/02/2007
5506
R115FM
01/26/2007
Clarification of the Protocol for Estimating
Allowance for Uncollectible Accounts From
CMS-H/M751A/B, Status of Accounts
Receivable
04/02/2007
5451
R111FM
10/27/2006
Status Codes for Financial Reporting of Debts
Once the MMA Section 935 Appeal Process Has
Been Completed
04/02/2007
5397
R105FM
08/25/2006
Benefits Payable Survey and Trending Analysis
Procedures
09/30/2006
5130
R93FM
04/04/2006
Clarification of the Form CMS-1522 Monthly
Contractor Financial Report
06/01/2006
4248
R92FM
03/10/2006
Clarification of the Form CMS-1522 Monthly
Contractor Financial Report - Replaced by
Transmittal 93
04/10/2006
4248
R91FM
02/17/2006
Clarification of Instructions in Pub. 100-06,
Chapter 5 Financial Reporting, Section 310.4-
Line 4(a) through (e), Reclassified CNC Debt
(Principal & Interest)
03/17/2006
4151
R80FM
10/21/2005
Medicare Contractors' Monthly Cash Collections
11/21/2005
4074
R50FM
07/30/2004
Unsolicited/Voluntary Refunds
10/04/2004
3274
R49FM
07/16/2004
Procedures For Re-Issuance and Stale Dating of
Medicare Checks
08/16/2004
2951
R48FM
07/09/2004
Unsolicited/Voluntary Refunds - Replaced by
Transmittal 50
10/04/2004
3274
R42FM
04/30/2004
Unsolicited/Voluntary Refunds - Replaced by
Transmittal 48
10/04/2004
3274
R35FM
02/09/2004
Unsolicited/Voluntary Refunds
10/04/2004
1444
R28FM
12/24/2003
Estimating Allowance for Uncollectible
Accounts
01/31/2004
2875
R21FM
08/01/2003
Funds Expended for Multi-Carrier System
(MCS)
01/01/2004
2795
R20FM
08/01/2003
Funds Expended for Fiscal Intermediary Shared
System (FISS)
01/01/2004
2794
R18FM
05/02/2003
Reporting Currently not Collectible (CNC) Debt
10/01/2003
2640
R17FM
05/02/2003
Reporting Debt and Receivables
10/01/2003
2641
R14FM
02/03/2003
Shared System Preparation of Financial Reports
07/01/2003
2514
R05FM
08/30/2002
Initial Publication of Chapter
N/A
N/A
Back to top of chapter
