ii
Western University of Health Sciences (Western University) is an independent, non-profit academic health
center, incorporated in the State of California, and dedicated to educating health care professionals qualified
to provide comprehensive health care to the family.
Accreditation(s)
Western University of Health Sciences is accredited by the Accrediting Commission for Senior Colleges
and Universities of the Western Association of Schools and Colleges (WASC, 895 Atlantic Avenue, Suite
100, Alameda, California, 94501, phone number: 510-748-9001), a regional accrediting body recognized by
the Council on Higher Education Accreditation and the U.S. Department of Education.
Professional accreditations for each academic program are indicated in the appropriate section of this
catalog.
Notice of Non-discrimination Policy
Western University of Health Sciences, in compliance with Titles VI and VII of the Civil Rights Act of
1964, Title IX of the Education Amendments of 1972, Sections 503 and 504 of the Rehabilitation Act of
1973, and Sections 102 and 302 of the Americans With Disabilities Act of 1990, does not discriminate on
the basis of race, color, national origin, religion, handicap, or sexual orientation in any of its policies,
procedures, or practices. In accordance with sex discrimination laws, the University forbids acts of sexual
harassment. In compliance with the Age Discrimination in Employment Act of 1967, Section 402 of the
Vietnam Era Veterans Readjustment Act of 1974, and Section 12940 of the State of California Government
Code, the University does not discriminate against any employees or applicants for employment on the basis
of their age, their ethnic origin, their marital status, their sexual orientation, or because they are disabled
veterans or veterans of the Vietnam Era, or because of their medical condition (as defined in Section 12926
of the California Government Code); nor does the University discriminate on the basis of citizenship, within
the limits imposed by law. This non-discrimination policy covers admission, access, and service in the
University programs and activities and application for and treatment in University employment.
Pursuant to Executive Orders 11246 and 11375, as amended, Section 503 of the Rehabilitation Act of 1973,
as amended, and Section 402 of the Vietnam Era Veterans Readjustment Act of 1974, as amended, Western
University of Health Sciences is an affirmative action and equal opportunity employer.
Access to Individuals with Disabilities
It is the policy of Western University to provide qualified persons with disabilities with access to its
programs and services, when viewed in their entirety, in the most integrated setting possible. Additional
information will be provided upon request from the Student Affairs Office.
Please Note:
Text for the catalog was prepared as of June 2002. The information herein applies to the academic year
2002-2003 and is subject to change at the discretion of the University.
Visitors are always welcome at the University and campus tours are available. Visitor badges are required
and can be obtained from the receptionist in the Administration Center.
Office of Admissions, Mondays, 8:30 am - 12 noon, Tuesdays-Fridays, 8:30 pm - 5 pm
University Switchboard - (909) 623-6116.
Western University of Health Sciences Catalog Vol. 13, No. 1, Summer, 2002
iii
The President's Message
Attending an academic health center such as Western University of Health Sciences is not an automatic
passport to becoming a good health professional. While a first-rate educational experience is essential, the
making of a good health professional is also rooted in the nature and quality of the people involved.
There is visible and strong sense of community, of family, at Western University. We are proud of the
fact that the institution is people-centered, that it seeks to develop in our students a blend between the
technical and the human skills required of health care professionals. The content and substance of the
curricula, as well as the instructional processes used to carry it out, reflect a humanistic approach to health
care.
The University's educational programs provide training that presumes the faculty and the students are the
masters and not the slaves to this institution. We believe, therefore, that it is imperative our students feel
they have a place in the learning environment and that they are active rather than passive recipients of their
education. Learning proceeds in ways directly related to the interests and needs of the students as well as to
the demands of the health professions.
Here at Western University, a student can expect an education that will assist him or her to become a
feeling, humane, sensitive and medically competent professional and not just a learned degree-holder. To
that end, the University encourages a flexible and innovative "learning" environment instead of a rigid,
closed "learned" one.
In a word, a student can expect the same treatment from Western University that a patient should look
for from an able health professional. Thus, in the final analysis, what a student can expect from the
University is measured by the success of our humanistic approach -one that requires an active partnership
between you and us.
That is what goes into the education that takes place here and what Western University of Health
Sciences is all about.
Sincerely,
Philip Pumerantz, PhD
iv
Table of Contents
iii The President's Message
iv Table of Contents
1 Western University of Health Sciences
4 Frequently Called Numbers
5 Student Life: Campus Facilities and
Services
9 Student Services
21 University Policies and Procedures
27 General Academic Policies and
Procedures
35 Tuition and Fees
37 Financial Aid
43 University Calendar
44 College of Osteopathic Medicine of
the Pacific
Doctor of Osteopathic Medicine
Degree Program
44 Accreditation
44 The Osteopathic Philosophy
44 Personal Competencies for Admission
and Matriculation
45 Admissions Policies and Procedures
47 Registration
48 Tuition and Fees
49 Academic Requirements
56 Curriculum
59 Course Descriptions
66 Honors and Awards
68 Academic Calendar
70 Osteopathic Oath
71 College of Pharmacy
Doctor of Pharmacy Degree Program
71 Accreditation
71 About the Profession
71 The Degree
71 Career Opportunities
72 The College of Pharmacy
73 Admissions Policies and Procedures
74 Tuition and Fees
75 Financial Assistance
75 Academic Policies and Procedures
81 Description of Blocks/Course
Descriptions
88 Honors and Awards
89 Academic Calendar
90 College of Allied Health Professions
90 Mission
91 Master of Science in Health Sciences
Program
91 The Department of Health Sciences
92 Personal Competencies for Admission
and Matriculation
93 Admissions Policies and Procedures
94 Registration Policies and Procedures
95 Academic Requirements
98 Tuition and Fees
98 Program of Studies
98 Course Descriptions
101 Honors and Awards
102 Academic Calendar
103 Master of Physical Therapy Degree
Program
103 Accreditation
103 The Practice of Physical Therapy
104 Personal Competencies for Admission
and Matriculation
106 Admissions Policies and Procedures
107 Tuition and Fees
108 Academic Requirements
115 Curriculum Organization
117 Course Descriptions and Credit Hours
122 Honors and Awards
124 Academic Calendar
125 Master of Science in Physician
Assistant Studies
125 Accreditation
125 Vision Statement
125 Mission Statement
125 The Physician Assistant Role
126 Program Goals
128 Personal Competencies for Admission
and Matriculation
129 Admissions Policies and Procedures
131 Tuition and Fees
131 Academic Requirements
144 Curriculum Organization
145 Course Descriptions
149 Honors and Awards
150 Academic Calendar
150 The Physician Assistant Oath
152 College of Graduate Nursing
Master of Science in Nursing/Family
Nurse Practitioner Program
Post-Masters Family Nurse
Practitioner Track
Advanced Practice Nurse to
Family Nurse Practitioner
Track
Master of Science in Nursing
Track
v
152 Accreditation
152 Mission
152 Philosophy
153 Outcome Competencies for Graduates
154 Curriculum
155 Admission Policies
157 MSN-Harbor Track
157 Registration
157 Tuition and Fees
158 Academic Policies and Procedures
165 Course Descriptions
170 Curriculum (MSN/FNP)
171 Curriculum (FNP-only Track)
171 Curriculum (MSN-only Track)
172 Curriculum (APN to FNP Track)
172 Curriculum (MSN-Harbor/UCLA
Track)
173 Honors and Awards
174 Academic Calendar
175 Board of Trustees, Administration and
Faculty
175 Board of Trustees
175 University and Academic
Administration
178 Faculty
185 Clinical and Adjunct Faculty
215 University Map
1
WESTERN UNIVERSITY
OF HEALTH SCIENCES
GENERAL INFORMATION
Western University of Health Sciences (Western University) is a non-profit, independent, academic
health center, founded as the College of Osteopathic Medicine of the Pacific (COMP) in 1977. The
founding mission of the institution was to educate primary care osteopathic physicians for the western
United States. Over the past two decades, Western University has preserved and enhanced its mission,
expanding it to include educational programs in the allied health professions, pharmacy, graduate nursing
and veterinary medicine.
INSTITUTIONAL MISSION
Western University is a graduate university of medical sciences that educates health professionals to
practice and teach with excellence and compassion. Within a learner-centered environment, the University
encourages lifelong learning, supports faculty and student scholarly activities, provides patient care in
support of clinical training, and enhances the quality of life in the region through community service.
VALUES
The people of Western University are dedicated to caring as they pursue their educational, scholarly,
patient care, and public service activities. The University encourages the diversity and interdisciplinarity of
its programs, students, faculty, staff, and administrators. The ideals of continuous quality improvement,
lifelong learning, long-term planning, fiscal strength, adaptability, and agility in the rapidly changing worlds
of health care and education are realized through innovation, teamwork, and collaboration within the
University as well as with its network of academic health centers and community partners.
VISION
To be the graduate university of medical sciences of choice in the western United States.
GOALS
To provide top quality, learner-centered educational programs in selected graduate medical sciences to
educate a health workforce that meets the needs of the State of California and the western United States.
To link educational, research and service activities and programs in a learner-centered environment
through partnerships with academic health centers and other health and education related organizations to
improve the quality of life of the surrounding communities.
To ensure top quality postgraduate education and training opportunities for graduates of its programs.
To be renowned for using the Internet to promote "e-ffectiveness," "e-fficiency," and "e-learning."
To ensure organizational effectiveness and development.
HISTORY
The founding institution, the College of Osteopathic Medicine of the Pacific (COMP), was established
in 1977 as a direct and important response to a critical shortage of primary care physicians in the western
United States. Philip Pumerantz, PhD, accepted the invitation of the college's board of directors to become
the founding president in September of 1977. In January 1978, COMP received pre-accreditation status
from the American Osteopathic Association. Provisional accreditation status was achieved in July of 1978
and full accreditation in February 1982.
2
COMP admitted its charter class of 36 students in 1978, and classes began on October 2. This occasion
marked the successful culmination of efforts begun in 1974 by the State Society of Osteopathic Physicians
and Surgeons of California "to seek the establishment of a college of osteopathic medicine in the State of
California." The charter class was graduated on June 13, 1982.
In response to a nationwide demand for qualified clinical educators, COMP initiated a Master of Science
in Health Professions Education degree program (known on campus as MSHPE) in September 1986. This
program was housed within a newly created Graduate Division, and its charter class graduated in June 1987.
The program has grown in subsequent years with an enrollment reflecting a wide spectrum of health
professionals.
As a new decade began, COMP accepted its first class of physician assistant (PA) students who
matriculated on February 2, 1990. With the addition of this program, the Graduate Division became the
Division of Allied Health Professions, and subsequently, the School of Allied Health Professions. The start
of the PA program signaled a new era in which COMP expanded its mission of educating family-oriented
health care professionals for the western United States.
In response to a growing need for physical therapists in this country, a master's degree program in
physical therapy (the MPT degree) was launched on January 6, 1992. Within the School of Allied Health
Professions, COMP enrolled 49 students in the charter class and hired five faculty members for the
program. The two-year, four-month MPT program educates physical therapists to function as generalists in
the field who are also concerned about wellness, health promotion and a humanistic approach to the care of
the whole patient.
In 1991 the institution achieved the status of an academic health center (ACH) due to its multi-faceted
programs in medical and allied health education. The academic health center formed a partnership with San
Bernardino County Medical Center, which moved to a state-of-the-art facility in Colton, California, and
changed its name to the Arrowhead Regional Medical Center (ARMC) in the spring of 1999. The
partnership, known as the Academic Center for Excellence in the Health Sciences (ACEHS), provides the
University with a primary teaching hospital. ARMC sponsors the largest family practice residency training
program in California and the second largest in the nation.
In August of 1996, in order to better reflect its stature, COMP was restructured into a university with a
new name: Western University of Health Sciences. The College of Pharmacy also welcomed its charter
class into the Doctor of Pharmacy (PharmD) program at that time. This program was the fourth college of
pharmacy to be established in the State of California and prepares students in a humanistic, interdisciplinary
tradition to become competent, qualified professionals. Graduates of Western University's College of
Pharmacy complement other health care team members by offering their expertise in comprehensive drug
therapy management.
In March of 1998 Western University created a College of Graduate Nursing in order to satisfy an
increasing demand for advanced practice nurses. The College offers a Master of Science in Nursing (MSN)
degree, a Family Nurse Practitioner (FNP) certificate program, and a joint MSN/FNP program for advanced
practice nurses in a distance-learning format. The arrival of the World Wide Web as an electronic
information management tool provides the university a unique opportunity to offer students individualized
learning experiences that would be impossible through other media. Online discussion forums and e-mail
also provide important lines of communication and support among distance learners, faculty, and other
program personnel.
Western University founded the College of Veterinary Medicine-its fifth college-in August 1998. Shirley
D. Johnston, DVM, PhD, was hired as the founding dean the following month. She is the first female dean
of a veterinary college in the United States. Western University is committed to providing an AVMA-
accredited educational program that will serve as a new paradigm in veterinary education. Western
University's College of Veterinary Medicine's goal is to enroll its charter class of students in the fall of
2003.
3
The University also founded the Center for Disability Issues and the Health Professions in August 1998.
Headed by Brenda Premo, MBA, the former director of the Department of Rehabilitation for the State of
California under Governor Pete Wilson, the Center works to improve the capabilities of primary health care
providers to meet the growing needs of people with disabilities.
In August 1999, the University changed its Primary Care Physician Assistant certificate program to the
master's degree level, effective with the class entering in August 2000. Students who complete the two-year
program will be awarded the Master of Science (MS) degree in Physician Assistant Studies. Current with
this program change, the faculty developed an on-line Master of Science in Health Sciences degree
program, designed for licensed physician assistants who possess a bachelor’s degree and seek advanced
education at the graduate level.
In this, the 2002-2003 academic year, Western University will be celebrating its 25
th
anniversary.
Having reached this milestone in its development, the University maintains its commitment to providing
responsive and responsible health professions educational programs. To take advantages of organizational
efficiency, the University’s Department of Health Professions Education in the College of Allied Health
Professionals has merged the MS in Health Professions Education into the MS in Health Sciences. The
Department was renamed the Department of Health Sciences in 2001, consistent with this curricular format.
Other MS programs are in various stages of development and review as potential educational offerings in
future years. In addition, the Department of Physical Therapy is in the final stages of review and approval
of its proposed Doctor of Physical Therapy degree program.
KEY FACTS ABOUT WESTERN UNIVERSITY
• Students in all educational programs consistently score at the top on national boards and state
licensure examinations.
• Graduates of COMP are sought by top residency programs nationally and many serve as chief
residents in their chosen specialties.
• Total number of alumni (1982 - 2001) is 3,545
• Enrollment 2001-2002 (as of April 15, 2002) was 1,425
• College of Osteopathic Medicine of the Pacific: 684
• College of Allied Health Professions: 312
- Physical Therapy: 97
- Health Professions Education: 17
- Physician Assistant: 195
- Health Sciences – LPAT: 3
• College of Pharmacy: 392
• Master of Science in Nursing/Family Nurse Practitioner: 38
DIVERSITY STATEMENT
The students, faculty, administration and staff of Western University of Health Sciences place great
value on diversity. For us, it is a philosophy of inclusion, where pluralism and academic freedom are at its
foundation. Western University is committed to an open environment that promotes, accepts and celebrates
different points of view.
Western University is comprised of a community of individuals in which diversity is recognized as being
the core of our intellectual, social, cultural, physical, emotional and moral lives. We are enriched by our
encounters with one another and we strive to learn from each other in an atmosphere of positive engagement
and mutual respect. Our understanding and acceptance of one another in the campus environment
contributes to our ability to care for our patients who live in a diverse society.
The University, in accordance with various laws and beliefs, does not discriminate on the basis of race,
color, ethnicity, national origin, religion, politics, disability, gender or sexual orientation in any of its
policies, procedures or practices. Sexual harassment is unacceptable.
4
We acknowledge our guaranteed rights of free expression under the First Amendment to the Constitution
of the United States. However, we also hold unique responsibilities as individuals, answerable for our own
behavior and fully accountable for our actions. Seeking balance between rights and responsibilities makes
us keenly aware of the dangers of defamatory, libelous or obscene behavior, the value of community and the
importance of respecting our differences and commonalties.
As individuals committed to health professions education in the osteopathic tradition, we embrace the
important principle of caring for the whole person-in body, mind and spirit.
FREQUENTLY CALLED NUMBERS
President (909) 469-5200
Academic Affairs (909) 469-5578
Finance and Administration (909) 469-5693
Admissions (DO) (909) 469-5335
Admissions (All Other Programs) (909) 469-5542
Student Affairs (909) 469-5340
Office of Student Services (909) 469-5616
Western University Medical Center (909) 865-2565
Department of Physical Therapy Education (909) 469-5300
Department of Physician Assistant Education (909) 469-5378
Department of Health Professions Education (909) 469-5397
College of Osteopathic Medicine of the Pacific (909) 469-5505
Director of Student Services (909) 469-5414
Clinical Rotations (909) 469-5260
Assistant Dean of Educational Affairs (909) 469-5257
College of Allied Health Professions (909) 469-5390
College of Graduate Nursing (909) 469-5523
College of Pharmacy (909) 469-5500
Financial Aid (909) 469-5353
Learning Enhancement and Academic Development (909) 469-5408
Bursar (909) 469-5403
Technical Support Services (909) 469-5432
Multimedia Services (909) 469-5432
Registrar (909) 469-5342
Bookstore (909) 469-5416
Center for Disability Issues & the Health Professions (909) 469-5380
Security (909) 469-5475
Library (909) 469-5323
College of Veterinary Medicine (909) 469-5627
5
STUDENT LIFE: CAMPUS FACILITIES
AND SERVICES
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 623-6116
The main campus of Western University is in Pomona (see map, inside back cover), a city of
approximately 150,000 residents, located about 35 miles east of Los Angeles near the foothills of the San
Gabriel Mountains. It is an area with a high concentration of private and state colleges and universities.
Mountain resorts are nearby, and Pacific Ocean beaches, Palm Springs, Hollywood, Pasadena, Los Angeles,
arboretums, theme parks, museums, art galleries, libraries, theaters, and concert halls are all within about an
hour's drive.
Alumni Center Building Hours: 7:00 am to 5:00 pm weekdays
Closed Weekends and Holidays
The Alumni Center is a 32,000 square-foot facility, located at the corner of Gibbs and Second Streets.
The main level of the Alumni Center includes the office of Alumni and Constituent Relations and three
lecture halls: Cooper Hall, Swift Hall and Trendle Hall. The lower level of the Alumni Center
accommodates the microbiology (The Rene‚ and Namey laboratories, the Oswald Suter Microbiology Prep
Room) laboratories, a multipurpose teaching lab, The Roy and Marion Kramer Research Laboratory, other
research labs and student lockers.
Booth University Bookstore Building Hours: 7:30 am to 5:00 pm weekdays
Closed Weekends and Holidays (except on special occasions)
The Booth University Bookstore is a convenient source for required textbooks, supplies, and insignia
gift items. Personal checks, Visa®, MasterCard, and DiscoverCard® are accepted. Telephone and mail
orders are accepted with shipment made via UPS. The bookstore is open from 7:30 am until 5:30 pm
Monday through Friday. Located in the rear of the bookstore is a popular gathering place, the Hop Shoppe.
Business Center Building Hours: 7:00 am to 5:00 pm weekdays
Closed Weekends and Holidays
The Business Center houses the departments of Business Services (Bursar's Office, Accounting and the
Treasurer's Office), Office of University Building and Security, and Human Resources.
Health Professions Center (HPC) Building Hours: 6:30 am to midnight weekdays
6:30 am to midnight weekends
8:00 am to 5:00 pm holidays, except
closed on Thanksgiving weekend and during Winter
Break
The Health Professions Center includes facilities for the College of Pharmacy, the College of Graduate
Nursing, and the College of Osteopathic Medicine of the Pacific (COMP) as well as other university
services.
The first floor includes a 54-seat auditorium; a 200 seat lecture hall; three "in-the-round" high-tech
classrooms; break-out rooms for small group learning activities; Feldsher Hall; a large student lounge with
two kitchens, 80-inch screen television, pool table, ping pong table, and vending machines; administrative
and faculty offices for the College of Pharmacy; and a pharmacy/medical office museum. The offices of the
Center for Academic and Professional Education and the office of Learning Enhancement and Development
are also located on the first floor of the Health Professions Center.
The second floor of the HPC has a 200-seat lecture hall, administrative and faculty offices for the
College of Osteopathic Medicine of the Pacific and the College of Graduate Nursing, clinical skills
6
laboratories, research laboratories, conference rooms, and offices for the Multimedia Department and the
Department of Strategic Planning and Institutional Effectiveness.
Health Sciences Center (HSC) Building Hours: 7:00 am to 11:00 pm weekdays;
7:00 am to 10:00 pm weekends;
8:00 am to 5:00 pm holidays, except
closed on Thanksgiving weekend and during Winter
Break
The 72,000 square-foot Health Sciences Center features a unique central staircase. The first floor
consists of two large amphitheater-style lecture halls; Tribute Walk, a donor recognition area; and
Compatriot's Hall, an elegant meeting room with kitchen facilities. The first floor also houses the offices of
the Provost, and the administrative and faculty offices of the College of Allied Health Professions, including
the departments of Physician Assistant Education and the Master of Science in Health Professions
Education.
The second floor of the Health Sciences Center consists of an anatomy laboratory, the administrative
and faculty offices of the Physical Therapy Education Department; physical therapy clinical skills
laboratories; physical therapy faculty research laboratories, the osteopathic manipulative medicine teaching
laboratory; offices for the Center for Disability Issues and the Health Professions; and offices for the
department of Risk Management and temporary offices for the faculty and administration of the College of
Veterinary Medicine.
Health Sciences Library and Learning Resources Center
Building Hours: 7:00 am to 11:00 pm Monday through Thursday
7:00 am to 6:00 pm Fridays
11:00 am to 7:00 pm weekends
Closed on Holidays
The recently opened Health Sciences Library and Learning Resources Center houses the University’s
book, journal and media collections. It also provides office space for the library staff, the staff of the
Department of Instructional and Informational Technology, and the Learning Enhancement and Academic
Development office. The ground floor is reserved for library circulation services, the Edward Tessier
Learning Center, historical museum, and study space where students may use laptops and connect to the
University’s network. Books and serial collections are housed on the second and third floors, respectively,
and offices for library and instructional and information technology staff are found on the fourth floor. The
basement serves as the University’s Network Operations Center and provides office and work space for the
Technical Support Staff.
The mission of the Health Sciences Library is to educate by providing library materials and information
services to students, faculty and staff of the University. To further student adaptability and life-long
learning, it has become the goals of the staff of the Health Sciences Library to:
• monitor and evaluate the growing electronic sources on the Internet;
• add links to these sources to our internal computer collection; and
• educate our students, faculty, administration, staff and alumni so that they are able to use these
resources at home, in the office, and at public and hospital libraries.
Student Services Center/South Campus Building Building Hours: 7:00 am to 5:00 pm weekdays
Closed weekends and holidays
The offices of Student Affairs/Registrar and University Admissions are located on the first floor of the
Student Services Center. The second floor houses the office of Financial Aid.
University Administration Center Building Hours: 7:00 am to 5:00 pm weekdays
Closed weekends and holidays
The University Administration Center houses the University's executive offices. The first floor contains
the offices for the Executive Vice President for Administration and Finance, Vice President of Policy and
Research, Vice President of University Advancement, and the offices of Major Gifts, Special Events,
7
Communications, Publications, and Foundation, Corporate and Government Relations. The office of the
University Counsel is located in the basement.
The Office of the President and the Office of the Executive Vice President of Academic Affairs are
located on the second floor. The Saul Bernat Board Room and the VIP Lounge with a kitchen provide space
for meetings and special events.
Western University Campus Gourmet
The Western University Campus Gourmet is a food court providing a Subway sandwich shop, a TCBY
yogurt store, and Mamma Ilardo's pizza. The 1950s diner-themed eating establishment is designed to serve
the Western University community, shoppers at Antique Row, neighboring business populations, and the
general public. A lounge for Western University students occupies the back part of the Campus Gourmet
building (Open 7:00 am to 3:30 pm weekdays). Hours of the food court are: 7:30 am to 6 pm Monday
through Friday and Saturdays and Sundays from 10 am until 4 pm.
Western University Medical Center Building Hours: 8:00 to 5:00 pm weekdays
Closed weekends and holidays
Western University Health Care Facilities and Medical Centers comprise a health care delivery network
of the institution, which operates two medical centers. These medical centers have been established to meet
the needs of the communities in which they are located and also to serve as training facilities for Western
University students.
Western University Medical Center
360 E. Mission Boulevard
Pomona, CA 91766-1889
(909) 865-2565
Opened in 1984, Western University Medical Center is an ambulatory, primary care medical center that
addresses the health care needs of Pomona's less advantaged communities, as well as those from
participating managed care organizations, and provides clinical learning opportunities for Western
University students. Osteopathic family physicians and physician assistants, who are also Western
University faculty, and support personnel staff the medical center. In addition to health care services, the
Center provides health screenings for youth athletic programs. The Center is also a member of the Pomona
Clinic Coalition, made up of the County of Los Angeles Department of Health and a group of area health
providers, which provides preventive and primary care health services to people who do not have medical
insurance or can not afford medical care.
The physicians and physician assistants who work at Western University Medical Center have faculty
appointments at Western University of Health Sciences and are involved in both the didactic and clinical
teaching aspects of the curriculum.
PERSONAL SAFETY
The University strongly suggests the following precautions for its students, faculty and staff:
• Since some streets through the campus are open to vehicular traffic, please use extreme caution when
crossing between buildings and do not congregate on the street.
• Please make sure your car is locked at all times in the parking lot.
• You should be advised that the doors to some buildings are locked at 5:00 p.m. It would be to your
advantage to walk to the parking lot with a friend or close associate if you are leaving after business
hours. If you find it necessary to work or study late, you should advise security personnel on campus
before leaving the building so that someone can watch you walk to your car.
8
• During the daytime hours, security guards are assigned to patrol the parking lots directly north, and
northeast behind the North Campus buildings along First Street, and they patrol the lots behind the
South Campus building, Health Sciences Center and Health Professions Center. It is strongly
suggested that you do not leave your car overnight in any of the parking lots or streets surrounding the
campus, as a security guard is not on duty after 11:00 p.m. Mondays - Thursdays, after 7:00 p.m. on
Fridays, and after 10:00 p.m. on Saturdays and Sundays.
• Do not admit an unknown person into the building. If someone says they need help, offer to call the
proper person (police, paramedics, etc.).
In case of emergency, if someone from the University needs to be informed or contacted, please call:
Campus Security (909) 623-6116, ext. 3000
9
STUDENT SERVICES
Recreational Facilities
Western University provides YMCA or designated fitness club individual memberships for students at
no cost. If interested, students may sign up at registration. The YMCA is within walking distance of the
Pomona campus and offers coeducational facilities for swimming, racquetball, basketball, exercise
programs, etc. The fitness club provides non-prime time racquetball courts, Nautilus exercise equipment,
aerobics, Jacuzzi, steam rooms, etc. Family memberships may be purchased at reduced rates throughout the
year.
On the Pomona campus, the HPC Student Commons provides billiards, television, ping pong, and the
parks offer picnic tables, basketball and volleyball. There are also numerous tennis courts, golf courses, ski
slopes, and hiking trails in the immediate area.
Upon request, discount cards for all major southern California amusement parks are available in the
Student Affairs Office.
Community Activities
The Western University "This Week," which is updated every week, lists Western University seminars
and events that are open to students, faculty, staff and families.
Area colleges publish monthly calendars of social, cultural and educational events that are posted on the
student bulletin board behind the lecture halls. Events are usually open to the public.
Student Government
Over 37 organizations have been established within the student body. The umbrella for all of the other
organizations is the Student Government Association, which is charged with official representation of the
student body.
Student Government Association - Students are encouraged, individually and collectively, to express
their views on issues and administrative policy on campus. Through the elected representatives of the
student body and membership on various University committees, students have the opportunity to
participate in the administrative activities of the University. This body represents the students in all matters
of concern with regard to faculty and administration.
The objective of the Student Government Association is:
a. To act as elected representatives of the student body in all matters with regard to the
faculty, administration, fellow professionals and the public-at-large.
b. To ascertain and express student opinion in matters pertaining to the University.
c. To formulate and execute policy on matters relative to the student body.
d. To budget and disburse funds for student activities or other related functions.
e. To organize and implement various educational, social and community service projects.
Students are invited to select representatives on the following University committees:
Commencement Committee - The purpose of this committee is to plan and, in some areas, implement
the University's graduation ceremony and related events. The committee submits to the President the results
of its deliberations for this consideration and approval. The committee and its chair are appointed by the
President. The Student Government Association President and the President (or an appointee) of the MSIV
class are also voting members.
Financial Aid Committee - Student Body Treasurer, PAI Class Treasurer, MSII Class Treasurer,
PharmDII Class Treasurer and MPTI Class Treasurer, will be voting members. The student members may
be excluded from certain meetings if the discussion includes confidential material from other students' files.
The Humanism in Health Sciences Committee - To create a climate for defining, teaching, and
implementing humanism and diversity through various ongoing programs. These programs are grounded in
a philosophy that fosters valuing the diversity and humanness of persons on our campuses and in our
communities. The committee will support and encourage scholarly activities that promote humanism and
diversity.
10
Library Committee - One representative from each class on campus will be a voting member. The
duty of the Committee is to advise the Librarian in matters of concern to the faculty and students relevant to
the Library.
University Student Conduct Committee - The function of the Student Conduct Committee is to
investigate alleged violations brought to its attention by the Academic Deans. The Committee may
recommend a course of action if a violation has been identified.
STUDENT ORGANIZATIONS
The following organizations are currently approved and active on campus:
American College of Osteopathic Family Physicians (ACOFP) - Promotes the training of osteopathic
family physicians and provides a better understanding of the scope of services rendered by the osteopathic
family physician. Advisor Emeritus: Dr. Burton Routman.
American Geriatric Society – Educates students in geriatric medicine, enhances the visibility of
Western University’s Geriatrics Program, and provides a forum in which students and clinicians can interact
and serve as a link between students and outside organizations. Advisors: Drs. Ehab Tuppo, Karen Shapiro,
and Reza Taheri.
The American Medical Women's Association (AMWA) and the National Osteopathic Women
Physicians' Association (NOWPA) - These are two national and on-campus organizations that exist for the
purpose of supporting women in medicine. Our on-campus chapters are very active in supporting women
medical students by hosting both DO and MD speakers, sending members to National Women's Health Care
Conventions, networking through the annual Mentor Dinner, running the Nursery Nutrition Project,
supporting the Los Angeles Babies with AIDS Walk-a-Thon and developing Board Review Notes. In
addition, both organizations have access to low interest student loans, grants and fellowships. Most
importantly, AMWA and NOWPA exist for the purpose of making friends, lending support and rendering
service within our campus and local community. Advisor: Drs. Lony Castro and Kay Kalousek
American Pharmaceutical Association-Academy of Students (APhA-ASP) - APhA exists to serve its
members, to enhance pharmacists' abilities to provide pharmaceutical care, and to further the public's
recognition of the pharmacists' value as a health resource. As an academy of APhA, ASP promotes the
professional practice interests of pharmacy students, establishes programs/activities for members, and
provides a means for members to participate in APhA's policy-making process. Advisor: Dr. Joanne
Yasuda.
Asian-American Health Profession Student Association (AAMSA) - Enhances the awareness of the
Asian communities to the osteopathic profession and provides services to the University and Asian
communities. Advisor: Dr. Stanley Wong.
Biomedical Research & Literature Club (BIOMED R & L) - Reviews current medical literature and
presents reviews and case studies. Advisor: Dr. James Martin
California Doctors Ought to Care (CAL-DOC) - Through patient education, to get people to stop
smoking, and thereby have them live longer, healthier lives. Advisor: Dr. Richard Sugerman.
California Society of Health-System Pharmacists-Western University (CSHP-Western University)
- The purpose of CSHP-Western University is to provide students an opportunity to become knowledgeable
about pharmacy practices in organized healthcare settings. Advisor: Dr. Kari Franson.
Chicano/Latino Medical Student Association (CMSA) - Serves as part of a statewide communication
and support network for medical and pre-medical students interested in developing health care services for
Hispanic underserved communities. Advisor: Ms. Susan Hanson.
Christian Medical/Dental Society (CMDS) - Encourages and aids Christian students in their spiritual
and professional growth through weekly meetings and other special events. Advisor: Ms. Bonnie MacKay
Digital Medicine Association (DMA) – The purpose of the DMA is to explore the integration of
information technology in health care and to enhance health professions education programs through the
inclusion of informatics. Advisor: Scott Helf, DO
Emergency Medicine Club (EMC) - Promotes the interest and education of students in emergency
medicine and exposes them to a variety of common emergencies. Students will be exposed to practical
procedures they can use in their third and fourth years. Instruction and practice will be provided of
11
invaluable techniques necessary in the field of emergency medicine. Advisor: Dr. Jonathan Leo; Dr.
Francis Yang
Golf Association
– Unites golfers of any caliber from all disciplines within the university.
Hillel - Provides access on the Western University campus to Jewish culture. Meets to discuss pertinent
aspects of Jewish life through seminars and invited speakers. Also seeks to establish a link between
students and the surrounding Jewish community. Advisor: Dr. Richard Sugerman.
Humor and Medicine (HAM)
– Brings humor into the lives of patients in hospitals and nursing homes.
International Medicine Club - Promotes cross-cultural experience and community involvement to
better appreciate primary care. Students invite physicians to share their experiences in international health.
The club also sponsors medical student foreign exchange through the International Federation Medical
Student Association (IFMSA). Advisor: Dr. Rafi Younoszai.
Islamic Medical Society of Western University - Serves as a religious outlet and meeting place for the
growing number of Muslim students on the Western University campus. Activities include campus
celebrations of two holidays, Eld ul'Fitre, Eld ul'Adha, speakers and a companion program with Pilgrim
Place, a convalescent home in Claremont. Advisors: Drs. Nadir Kahn and Rafi Younoszai.
Latter-Day Saints Student Association (LDSSA) - This organization was founded to establish and
provide a spiritual balance to medical education through discussions and activities geared to that purpose.
Advisor: Dr. Jonathan Leo.
Los Angeles County Medical Association – Medical Student Section, Western University of Health
Sciences Osteopathic Chapter. The Western U chapter of the LACMA – Medical Student Section promotes
osteopathic principles and practice in Los Angeles County via educational presentations to other health
professionals and potential practitioners. The organization serves educate members about issues pertinent
to the field of medicine and provide students with access to legislative policy surrounding organized
medicine. Students serve on policy-making committees and attend seminars, conventions and political
rallies to insure adequate representation of COMP. Advisor: Michael Jeong, DO
Middle Eastern Medical Students Organization (MEMSO) - This organization is to unite students of
Middle Eastern background and promote their cultures on campus. Advisor: Dr. Nadir Khan.
Military Club - The Military Club is open to all students regardless of military affiliation. Those
students on military scholarships will have the opportunity to join student chapters of the Association of
Military Osteopathic Physicians and Surgeons (AMOPS) and the Uniformed Services Academy of Family
Physicians (USAFP). The primary goals of the club are to: provide information concerning rotations,
internships and residencies in military facilities, provide information concerning the practice of osteopathic
medicine and family practice medicine within the armed forces, to provide information concerning life and
opportunities in the military in general. Advisor: Dr. Richard Sugerman.
Montclair Clinic - Students volunteer to provide health services at a "free" clinic in Montclair.
Neocortex Yearbook - A yearbook is published annually for the University. Students write, draw,
design, edit and take photos for the yearbook. Advisor: Toni Lawrence.
Osteopathic Physicians and Surgeons of California - Medical Students Section (OPSC-MSS) -
Provides an avenue for student input to the state medical association and allows early involvement in OPSC.
Helps DO candidates to enhance their career opportunities through collegial relationships with practicing
physicians via participation in CME seminars; clinical preceptorships, and guidance of physician mentors.
Advisor: Dr. Jay Porcelli; Dr. Alan Cundari
Outdoor Adventure Club
– Encourage fellow students to enjoy the outdoors. Provide stress relief via
outdoor activities. Immediate Goal: set-up club hub, find out van rental and group rates at local snow areas
as well as write student- by-laws. Future: establish a solid club that will continue after graduation.
Continue to provide outdoor events each semester and involve the community.
Physical Therapy Awareness Club (PTAC) - Provides opportunities for all students to partake in
various PT related lectures, convocations, debate panels including current issues and legislation and
technique demonstrations. Activities include guest speakers, participation in APTA functions and hands-on
treatment techniques. Advisor: Dr. LeeAnne Carrothers.
Pomona Community Health Action Team (PCHAT) - The purpose of this club is to provide and
serve the medical needs of the Pomona Community. Advisors: Dr. Rafi Younoszai and Dr. Burt Routman.
Santa's Workshop - Western University students provide assistance to disadvantaged families during
the holiday season. Advisor: Ms. Gisele Tackoor.
12
SANUS: The World's Only Osteopathic Theater Troupe - Promotes health through artistic expression.
Theatrical production company composed of production staff and cast who will select two plays to be
presented annually. Advisors: Drs. Jeffrey Felton and Dennis Kiick.
Sigma Sigma Phi - This fraternity was established to provide service to the University and profession
and is the official osteopathic honorary fraternity. It promotes educational programs for the entire student
body and participation in community projects, health fairs, high school athletic physicals and blood pressure
checks. Advisor: Dr. George Charney.
South Asian Student Association (SASA) - The purpose of this organization is to raise awareness of
South Asian Students in osteopathic medicine and to provide an interdisciplinary forum for South Asian
students to share their cultural identity. Advisor: Dr. Nadir Khan.
Sports Medicine Club - The purpose of this group is to provide seminars, speakers and other
educational avenues for students interested in Sports Medicine. Also, to sponsor school and club health
checks, act as liaison to area athletic events and possibly engage in research. Advisor: Dr. Casey Chaney;
Dr. Alan Cundari.
Student Associate Auxiliary (COMPlements-SAA) - COMPlements is the Student Associate
Auxiliary (SAA) for spouses and partners of students and is chartered by the national Auxiliary to the
American Osteopathic Association (AAOA). It has been organized by the Auxiliary to the Osteopathic
Physicians and Surgeons of California to further the goals of the University and the osteopathic medical
profession, to serve the local community and to promote fellowship and unity within the school. SAA
COMPlements regularly plans social, cultural and charitable activities for the benefit of the students,
spouses, University and community. Advisor: Mrs. Jeanne Charney.
Student National Medical Association (SNMA) - Fosters a commitment for students to excel and
mentor. Our goal is to produce quality health care team members armed with the knowledge, skill and
insight needed to practice medicine within underrepresented communities. Advisor: Dr. Beverly Guidry.
Student Osteopathic Internal Medicine Association (SOIMA) - the purpose of this organization is to
represent aspiring internists through an early exposure to the field of internal medicine. Advisor: Dr. Kevin
Jenkins.
Student Osteopathic Medical Association (SOMA) - Provides community service to increase
awareness of osteopathic medicine. Sponsors lecturers, blood pressure clinics, etc. Advisor: Dr. Donald
Krpan.
Student Osteopathic Surgical Association (SOSA) - Provides opportunities for all students to learn
about surgery as a career and helps students develop basic skills for their clinical rotations. Activities
include operating room shifts for all interested students and procedure workshops including suturing,
casting, central lines, chest tubes and lumbar puncture. Advisor: Dr. Jonathan Leo.
Undergraduate American Academy of Osteopathy (UAAO) - Promotes the instruction and
understanding of unique osteopathic principles and technique. Guest lecturers are invited to the campus to
speak to members on manipulative therapy and osteopathic philosophy. Advisor: Dr. David Redding
Women's Health Interest Group - To further the interest of students considering a career in Obstetrics
and Gynecology, Family Medicine, or other Primary Care women's health. Advisor: Dr. Kay Kalousek.
Western University of Health Sciences/Physician Assistant Student Society (WUHS/PASS) - To
promote the Physician Assistant profession and represent the University at the national level. Advisor: Mr.
Roy Guizado.
STUDENT EMPLOYMENT
Because of the nature of the academic program of the University, students are urged to use great caution
in seeking employment during the academic year.
The University does have a work-study program for students who qualify. For more information,
contact the Financial Aid Office.
13
HEALTH SCIENCES LIBRARY AND LEARNING RESOURCES CENTER
Location: Corner of Third and Gibbs Streets – entrance is on Gibbs Street
Hours: Monday – Thursday 7:00 am to 11:00 pm
Friday 7:00 am to 6:00 pm
Saturday, Sunday 11:00 am to 7:00 pm
Study Rooms – The library has seven study rooms that may be used for study groups on a first-come,
first-served basis. Laptops may be used on the first floor or on the second and third floors in the study
rooms only.
Audio-Visual Lab – The lab may be used by WesternU students, faculty and staff only. Videos and
slides are available for use with televisions, VCRs, and slide projectors. There are also six computers that
may be used with several CD-ROMs that are available in the Lab.
Computer Lab – This lab may be used by Western University students, faculty and staff. There are
twelve computers that may be used to search the Library’s WebCat (online public catalog), or do research
on the Internet. Workshops will be held in this lab periodically.
Interlibrary Loan – Material not owned by the University Library may be requested via interlibrary loan
by Western University faculty, staff and students. There is a charge for this service.
Borrowing Privileges and Policies – Western University faculty, staff and students are eligible to borrow
library materials. Other interested users may be eligible and should inquire at the Circulation Desk.
• Books: On campus students may check out items for seven days and renew them twice if there is
not a hold at that time. Students on rotation and distance education students may check out items
for one month with no renewal. Fines are charged for overdue books. Renewals may be made by
phone. A “hold” may be placed on books that are charged out. You must have your student
ID/employee ID with you in order to borrow books.
• Journals: Bound or unbound journals (periodicals, newsletters, etc.) do not circulate.
Note: More detailed information regarding library policies and procedures may be found on the Library’s
Web site, or in the Library Handbook at the circulation desk.
CENTER FOR DISABILITY ISSUES AND THE HEALTH PROFESSIONS
(SECOND FLOOR, HEALTH SCIENCES CENTER)
The Center for Disability Issues and the Health Professions assists students with disabilities from the
time of admission to graduation. The Center is located on campus at 309 E. Second Street/College Plaza,
(909) 469-5385 voice, (909) 469-5520 TDD or email bpremo@westernu.edu.
CDIHP Services
Each student at Western University is unique. Only upon consultation with the student, dean and faculty
member can specific plans for accommodations be made. To assist with a documented disability, staff from
CDIHP may communicate, when appropriate, with the instructor and may also ask the student to discuss
his/her needs with the instructor. Decisions on appropriate accommodations, auxiliary aids and/or services
are made following an individualized assessment of each request and after discussion of the options
available with one of the CDHIP staff.
The following is a sample list of the types of services and accommodations that might be provided,
based upon CDIHP’s assessment of each student’s specialized needs:
• academic modifications
• disability management advising
• auxiliary aids
• examination accommodations
• mobility assistance
• physical access and architectural modification (i.e., building platforms or adding disabled parking
spots)

14
• reader services
• study skills advisement
• taping of academic lectures
• transcription services for specific classes
• extended time for examinations
• a private, quiet, well-lit room for examinations
• alternative testing formats
• consultation with staff of CHIHP and professors regarding facilitation of education of students with
disabilities
It is a student’s responsibility to provide timely and sufficient written medical documentation about the
student’s disability or disabilities. Students must check with the Center about documentation requirements.
Students must request services or accommodations directly from the Center, which in consultation with the
student, can recommend the appropriate services or accommodations. There is no charge to students for
services that are specifically needed to support the educational program.
For additional information, contact Ms. Sharon McCrary at (909) 469-5447; TDD (909) 469-5520 or
check the Center’s web page at www.westernu.edu/cdihp
.
OFFICE OF INTERNATIONAL AND CROSS-CULTURAL PROGRAMS
The Office of International and Cross-cultural Programs (OICP) was established in 1989 to promote
student cross-cultural experiences locally and internationally. The program's goals are to:
• Develop foreign-based clinical training opportunities for interested Western University students to
experience primary health care in foreign countries as part of their professional growth;
• Instill in students the knowledge and skill needed to provide quality health promotion and disease
prevention services in cross-cultural settings;
• Develop student and faculty awareness of the principles and goals of the international primary
health care movement and its adaptation locally to improve the status of primary health care in our
communities, the state, and the country;
• Encourage research in cross-cultural primary health care delivery and education in foreign
countries; and
• Advocate for osteopathic approaches to health care delivery and education in foreign countries.
HUMANISM AND THE HEALTH SCIENCES
(BASEMENT, UNIVERSITY ADMINISTRATION CENTER)
In 1996 the University established the Humanism in the Health Sciences Committee. The committee's
working definition of humanism is: Humanism is a way of caring that is fundamental to positive interaction
and is manifested as a responsiveness to the needs of fellow human beings through respect, compassion,
empathy and understanding.
The mission statement of the Humanism in the Health Sciences Committee states: To create a climate for
defining, teaching, and implementing humanism throughout the University. Programs are grounded in the
philosophy, which fosters valuing the diversity and humanness of persons at our locations and in our
communities. The committee will support and encourage scholarly activities that promote humanism.
Activities of the committee include:
• The annual publication of a scholarly journal, Humanism in the Health Sciences, which features
articles, poetry, commentaries and essays. The journal is student run, edited and produced;
• Curriculum development: Belief System and Patient Care Program funded by the National Institute
of HealthCare Research; and
• Care Teams and Monthly Care Teams News.
STUDENT HOUSING
The University does not provide on-campus or off-campus housing accommodations for its students;
however, there is an off-campus housing referral system to help students locate houses, apartments,
roommates, etc. A local map, the real estate sections of local newspapers, and information on activities in
the surrounding communities are available in the Student Affairs Office and on the WesternU website.
Incoming students may wish to subscribe to the local newspapers: the Claremont Courier, 111 South
15
College Avenue, Claremont, 91711; and the Inland Valley Daily Bulletin, 2041 E. 4th Street, Ontario,
91761-1020.
All students on clinicals/clerkships are responsible for making their own housing arrangements. Some
hospitals offer housing on a first-come, first-served basis during your assignment at their facility. It is the
student's responsibility to contact the hospital for information regarding availability and cost of housing.
The COMP Office of Clinical Rotations has a housing book available for the perusal of DO students and
will assist as much as possible with guidance regarding housing, but the final responsibility for housing
arrangements will be the student's.
Please note: the University provides a housing referral service as a courtesy only. The University
assumes no responsibility for the accuracy of information provided by property owners or other third
parties, and each student should independently verify the condition of any property, its amenities, security
arrangements, etc. Under no circumstances shall the University have any responsibility or be liable for
damages, losses, injuries or liabilities of any nature relating to any housing provided by third parties.
STUDENT PARKING
Students have the option to purchase an annual parking sticker for $180. The purchase of a yearly
parking sticker can be included as part of a student's Financial Aid package, with the submission of a paid
receipt.
The collection of the funds will be conducted by the Bursar's Office, and students will be permitted to
charge the parking fees on their student accounts.
The University will provide full-time security for this parking lot between the hours of 7:00 a.m. to 6:00
p.m. Monday through Friday. If students are planning to be on campus after 6:00 p.m. during the week,
they should move their cars to the Health Sciences Center parking lots after 6:00 p.m. Students should park
their cars in the Health Sciences Center parking lots on Saturdays, Sundays or holidays.
City Parking Lots - Annual parking permits are also available at a significant discount ($140, or
quarterly at $40) through the City of Pomona for those individuals wishing to pay for their parking in this
manner. Applications are available in the Student Affairs Office, or contact the Pomona City Hall
Treasurer's Office, 505 South Garey Avenue, Pomona, CA 91766, (909) 620-2262. Those who elect to
park in the metered lots without a permit will be required to pay 75 cents per day per vehicle.
Parking along the streets is permitted with certain posted restrictions.
Secured bicycle parking is available on the west side of the Student Services building. Motorcycles
must be parked in the parking lots.
PSYCHOLOGICAL COUNSELING SERVICES:
877- WESTRNU (877-937-8768) OR (949) 650-2217
In an effort to respond to the needs of our students, the University has developed a student assistance
program, which provides confidential psychological counseling services for students and their families.
This service is provided by Mental Health Alternatives and assists students with problems of living
(including personal, marital, family, stress, financial and legal issues) that may impair a student’s ability to
perform adequately in his or her professional training program. The service is accessible 24 hours a day,
365 days per year.
Mental Health Alternatives
Dominic J. Bronell, Ph.D.
W. Doyle Edson, Ph.D.
Locations
4B-4 Village Loop Road 881 Dover Drive #390
Phillips Ranch, CA 91766 Newport Beach, CA 92663

16
OFFICE OF LEARNING ENHANCEMENT AND ACADEMIC DEVELOPMENT
(Second Floor, Room 235, Health Professions Center)
The Office of Learning Enhancement and Academic Development (LEAD) is a division of Student
Affairs. The LEAD Office’s goal is to help each Western University student successfully complete his or
her course of instruction. The Office assists students in many ways. The Director interviews students in
academic difficulty and evaluates their respective approaches to learning, study and processing information.
The Director devises and implements methods to solve identified barriers to successful learning and aids
individual students during their processes of resolution. The Director plans and implements group
workshops to enhance learning skills each year for students in each Western University program. The
Director also prepares and distributes handouts to students on learning styles, time management, group
study, processing information, memory, test preparation, group study, anxiety and stress management,
listening, note taking, comprehension, and critical reading and thinking. Additional learning enrichment
forums, workshops, and the establishment of on-campus reviews for course exams or licensing/certifying
examinations are developed by this Office in response to the expressed needs and interest of students.
The LEAD Office administers the Tutorial Assistance Program (TAP), working with tutors, tutees, and
the faculty as a team. TAP provides supplemental academic instruction for students in academic difficulty.
Competent and sensitive peer tutors selected by the faculty from each college facilitate course content
instruction. Students are scheduled individually or in small groups to work with a tutor. The LEAD Office
works closely with the tutors and tutees during the tutoring process to ensure that effective tutoring is
maintained.
The LEAD Office assist in the administration of the Summer Anatomy Prematriculation Program
(SAPP). SAPP is a three-week program designed to orient incoming, first-year osteopathic medical students
to the Western University campus and community, and to ease adjustment to the demands of their academic
environment. It serves as a “head-start” for students with little or no background in anatomy. The LEAD
Office endeavors to enhance all students’ sense of belonging by working closely with individual students in
overcoming environmental, social, cultural, or academic barriers that may interfere with their learning.
The LEAD Office serves all Western University students. All academic and personal counseling and
referrals to other campus services are completely confidential. The Director is available for students on a
walk-in basis or appointments can be made by phone or e-mail. The office is located in the Health
Professions Center on the second floor, Room 235. Office hours are 8:30 a.m. to 4:30 p.m., Monday
through Friday. The Director can be reached by phone at (909) 469-5408 or e-mail dhacker@westernu.edu
.
UNIVERSITY REGISTRAR
(FIRST FLOOR, STUDENT SERVICES CENTER)
Student Files: Access and Privacy
The Family Educational Rights and Privacy Act of 1974, also known as the Buckley Amendment, (a)
establishes a post-secondary student's general right to inspect and review his/her academic records and (b)
generally prohibits outside parties from obtaining the information contained in such records without the
student's written consent. A student may choose to waive access to certain confidential recommendations
placed in the file.
The paragraphs below delineate the procedures under which Western University will meet the law's
requirements. Western University currently maintains the following types of educational records that are
directly related to its students.
Admissions Files
The Director of Admissions is responsible for maintaining files that contain letters of recommendation
for admission to the University, transcripts of work performed at other institutions, required standardized
test scores, plus the applicant's supplementary application. The Director of Admissions, Members of the
Admissions Committee and the President have access to these files for the purpose of carrying out the
admissions function. After an applicant has been admitted and is actually registered, the files are combined
with those of the Registrar.
17
Registrar's Files
The Registrar is responsible for maintaining files that contain official Western University transcripts and
copies of occasional letters written by faculty and administration, along with students' replies. These letters
generally concern academic progress, examinations, etc. Members of the faculty and administration have
access to the files for use in student advisement. The Registrar also has access to the files to maintain them
and to provide authorized data to authorized persons.
If any material or document in the educational record of the student includes information on other
students, the University will not supply the actual material or document. Instead, only the specific
information contained therein that directly relates to the student seeking access will be provided. In
addition, no student may have access to:
(a) Financial records of parents or any information contained
therein, or
(b) Any confidential recommendations to which the student has
properly waived the right of access.
A student who desires to have any material in the files altered or expunged on the grounds that such
material is inaccurate or misleading, or that is being maintained in violation of his/her right to privacy or
other rights, may obtain a hearing before a special committee. The special committee will be composed of
representatives of students, faculty, and administrators. At the hearing, the student will be afforded a full
and fair opportunity to present evidence relevant to the issues raised. The committee's decision will be made
in writing within a reasonable period of time after the conclusion of the hearing. The committee's
conclusions may then be appealed by means of a complaint filed with the U.S. Department of Education.
Whether or not a student requests a hearing and regardless of the outcome of any such hearing, the student
may in any event insert into his/her files a personal written explanation concerning any material the student
believes is inaccurate, misleading, or otherwise inappropriate.
Reviewing the File
Students and former students may review any of the above files that directly relate to them upon
completion of a form available from the Registrar. On this form the student will specify the records he/she
wishes to examine. The Registrar will then collect the desired material. In no case will access be withheld
more than 45 days after the proper request has been made. If the student wishes, the University will also
supply copies of material in the file at 25 cents per page.
The privacy of student files is and will continue to be scrupulously maintained. Western University will
make public without consent only certain "directory information." This information consists of a student's
name, address, telephone listing, e-mail address, photograph, class schedule, full- or part-time status, major
field of study, dates of attendance, degrees and awards received, and the most recent previous educational
institution or agency attended by the student. A student who prefers that some or all of such "directory
information" not be made public, must notify the Registrar in writing.
Except for directory information and except as to certain parties listed in FERPA, the University will not
release to outsiders any student's file, or information contained in it, unless prior written consent has been
obtained from the student. The outside parties excepted by the Act generally consist of certain federal and
state officials, accrediting organizations, educational agencies who need the information for valid
educational purposes, and financial aid lenders. The University is also authorized to release information
contained in a student's file in any emergency situation involving the need to protect the health or safety of
the student or other persons.
A student (or applicant for admission) is permitted to waive access to confidential recommendations
written on his/her behalf regarding, (1) admission to any educational agency or institution, (2) an
application for employment, or (3) the receipt of an honor or honorary recognition.
A student who consents to release to outside parties any part of his/her file must do so in writing,
personally signed and dated. Such writing must specify the records to be released, the reasons for such
release, and the names of the parties to whom such records will be released. A form is available in the
Registrar's Office for this purpose. A student whose consent is required may also request a personal copy of
the specific records in question. As stated previously, there is a copying fee.
The University will maintain a record identifying all outside parties who have requested or obtained
access to a student's educational records and the specific interest they had in obtaining such access. This
18
record will be available only to the student and to the University officials previously named who are
responsible for maintaining the various files.
All such records are made available to students with the following limitations:
a. Recommendations submitted to the department by third parties under conditions of confidence,
e.g., letters of recommendation, will be shown only upon receipt of a signed release by the third
party;
b. Student records requiring the interpretation of a professional, i.e., medical, psychiatric,
psychological testing, etc., must be reviewed in consultation with the appropriate professional;
c. Generally, the school must have written permission from the student before releasing any
information from a student's record. However, the law allows schools to disclose records, without
consent, to the following parties:
• School employees who have a need-to-know
• Other schools to which a student is transferring
• Certain government officials in order to carry out lawful
functions
• Appropriate parties in connection with financial aid to a
student
• Organizations doing certain studies for the school
• Accrediting organizations
• Individuals who have obtained court orders or subpoenas
• Persons who need to know in cases of health and safety
emergencies
• State and local authorities to whom disclosure is required by state laws adopted before
November 19, 1974.
Three items of information from student records are considered "public" information:
• the fact of attendance
• the dates of attendance and
• the fact and date of graduation
With the exception of the above, no other student record information is divulged or released to persons
or agencies outside the University without the expressed written request or authorization of the student.
d. Under certain circumstances, the program may request written permission of the student to provide
demographic data such as names, addresses, etc., to persons or agencies outside the University
conducting research or other scholarly activities.
Other Student Files: Records of students and graduates are maintained by the program in accordance
with University rules. The original application and supporting materials are maintained by the Registrar. In
addition, the program maintains an academic profile record for each student, including information related
to academic and clinical performance in all phases of the program. Course grades are recorded on the
appropriate profile sheet as soon as computed. This file is maintained for department and student use. It is
NOT meant to serve as an official record of grades. Final course grades are submitted to the University
Registrar and only then become part of the official record/transcripts.
Transcripts of the work completed are maintained and may be requested from the University Registrar.
TRANSCRIPTS
Enrolled students my view their transcript on-line. No verbal grades or class ranks will be given at any
time. A grade change report will be generated upon request whenever a grade change occurs.
No grade will be changed unless the instructor certifies in writing to the Registrar that an error occurred
in computing or recording the grade or that the student has remediated an Unsatisfactory grade after being
directed to do so by the appropriate Academic Dean as recommended by the committee in each respective
College responsible for student academic progress. All recorded grades remain on the official transcript
unless a clerical error occurs. Remediated grades are recorded next to a grade of "U" or "I". Only the
remediated grade is calculated into the GPA.
19
To request an official transcript, a form must be completed in the Registrar's Office. There is a $5.00
fee for an official transcript. Official transcripts are mailed directly to the recipient by the University.
Official transcripts bear the signature of the Registrar and the seal of the University. In extreme
emergencies, transcripts may be faxed for a fee of $10.00, provided that a Fax Disclaimer form is
completed and the fee is paid. Transcripts will not be provided to students who are delinquent in their
financial obligations to the University, including the Library, or to any of its affiliated hospitals or clinics.
Transcript requests will be processed within two weeks. If the University has knowledge that a student or
graduate is in default on any federal, state, outside agency, institutional loan or service obligation, the
University will withhold all official transcripts, State or National Board Scores, and letters of
recommendation for internships, residencies, employment, staff privileges, specialty certification, and
licensing. Remember to allow two weeks for processing of transcript requests. Rush transcripts are
available for a $20 fee each. Transcripts ordered by 5 p.m. will be available for pickup after 9 a.m. the
following working day.
To maintain the integrity of academic transcripts, educational institutions certify only academic work
completed at that institution. This is the expectation of Western University when it issues its own official
transcripts, and this is what Western University respects when official transcripts are entrusted to it during
the application process. Therefore, the university will not produce or certify copies of official transcripts
from other institutions.
DIPLOMAS
Diplomas will be issued approximately six to eight weeks after the Registrar receives all final grades
verifying that a student has completed all academic requirements for a specific program.
CLASS RANK
Student's class ranking, with the exception of MSHPE, FNP/MSN and PharmD, may be obtained from
the Registrar's Office in writing, with appropriate identification. The class ranking is based on letter grades
and/or percentages.
STUDENT LOAN DEFERMENT PROCESSING
Western University of Health Sciences participates in the National Student Clearinghouse, located in
Herndon, Virginia. Three times a semester, the University submits a report of students' enrollment status to
the Clearinghouse, which in turn supplies verification of enrollment to lending agencies.
A number of lenders and loan servicing organizations that are members of the Clearinghouse participate
in a Paperless Deferment Process. With this process, no paper forms need to be completed by either
students or schools - the student simply calls his or her servicer to request a deferment. The servicer then
posts a deferment to the student's account after the student's verbal order is matched against the
Clearinghouse electronic data verifying in-school status.
If a lender needs a deferment form processed, bring it to the Registrar’s Office. The Registrar’s Office
will then forward all deferment forms to the Clearinghouse, which will verify the student’s enrollment to the
lender. Western University of Health Sciences does not supply this information directly to lending agencies
that participate in the National Student Clearinghouse.
If a student has registered late, this information may not be reported until the submission of the next
tape. The Clearinghouse requests the student take the following steps if a collection letter has been received:
1. Call the lending agency to see if a deferment form was received between the time the
Clearinghouse supplied the information and the lending agency sent the collection letter.
2. If, after calling the servicer, it still appears that the deferment has not been processed, the
student may call the Clearinghouse at (703) 742-7791 and ask for a Student Service
Representative. The representative will verify the date on which the deferment form was received
by the Clearinghouse, the date the deferment was certified and mailed, the enrollment status that
was certified, and where the forms were sent.
3. If an emergency exists -- for example, the student is 150 days delinquent and being threatened
with default -- the Clearinghouse will intervene on the student's behalf by faxing another
enrollment certification to the servicer. Further, it will work with the servicer to ensure that the
form is processed on a high-priority basis.
20
The Registrar’s Office will continue to process deferment requests to lending agencies that do not
participate in the Clearinghouse, however.
21
UNIVERSITY POLICIES AND PROCEDURES
NON-DISCRIMINATION
The Western University of Health Sciences, in compliance with Titles VI and VII of the Civil Rights Act
of 1964, Title IX of the Education Amendments of 1972, Sections 503 and 504 of the Rehabilitation Act of
1973, and Sections 102 and 302 of the Americans With Disabilities Act of 1990, does not discriminate on
the basis of race, color, national origin, religion, handicap or sexual orientation in any of its policies,
procedures, or practices. In accordance with sex discrimination laws, the University will not tolerate acts of
sexual harassment. In compliance with the Age Discrimination in Employment Act of 1967, Section 402 of
the Vietnam Era Veterans Readjustment Act of 1974, and Section 12940 of the State of California
Government Code, the University does not discriminate against any employees or applicants for
employment on the basis of age, ethnic origin, marital status, sexual orientation, or because of their status as
disabled veterans or veterans of the Vietnam Era, or because of medical condition (as defined in Section
12926 of the California Government Code); nor does the University discriminate on the basis of citizenship,
within the limits imposed by law. This non-discrimination policy covers admission, access, and service in
the University programs and activities, and application for and treatment in University employment.
Discrimination Complaint Procedure
Any student believing that he/she has been discriminated against in violation of the above policy of non-
discrimination may file a complaint with the Dean of Student Affairs or her designee. Complaint forms may
be obtained from the Dean of Student Affairs office. Retaliation against a person who reports, complains
about, or participates in the investigation of alleged discrimination is prohibited. A student who believes
that he/she is the victim of sexual harassment should follow the procedures specified in Western
University's Sexual Harassment Policy (See below).
All complaints of discrimination shall be investigated promptly and resolved equitably. The Dean of
Student Affairs will refer the matter to the appropriate Academic Dean, the Executive Vice President for
Academic Affairs/CAO, or to the Executive Vice President of Finance and Administration, (the
"responsible official"), depending upon the nature of the discrimination that is believed to have occurred.
The responsible official will investigate the complaint, and make a decision with regard thereto. The
responsible official may appoint an ad hoc committee to conduct a hearing, and to make recommendations
concerning any corrective action to be taken. The responsible official, taking into consideration the
recommendations of the ad hoc committee (if applicable), will decide, in writing, what action is appropriate
under the circumstances.
If a student is dissatisfied with the decision of the responsible official, he/she may appeal the decision to
the President. The appeal shall be made, in writing, within seven working days of the written decision of
the responsible official, and shall state any reasons why the person filing the appeal believes that the
decision of the responsible official is incorrect. The President may affirm or reverse the decision, modify
the action to be taken, or remand the matter for further proceedings. For purposes of action to be taken by
Western University, the decision of the President shall be final. Any person who believes that he/she has
been the victim of discrimination is, however, entitled to file a complaint with an applicable state or federal
agency at any time during Western University's proceedings.
UNIVERSITY FACILITIES, RESOURCES, AND SERVICES FOR
STUDENTS WITH DISABILITIES
General Policy:
The University endeavors to provide a welcoming and supportive community environment for students
with disabilities.
Western University is committed to the fundamental principles of non-discrimination and
accommodation in all of its academic programs as set forth in the Rehabilitation Act of 1973 and the
Americans with Disabilities Act of 1990. These laws establish that students with disabilities may not, on
the basis of their disabilities, be excluded from participation in, be denied the benefits of, or otherwise be
subjected to discrimination under any program or activity at Western University.
22
In that spirit, the University acknowledges its obligations to make reasonable adjustments and
accommodations to provide students with disabilities access to its programs in the most integrated setting
possible.
1. Programs and Facilities:
a. While the University cannot provide a totally barrier-free environment, it does provide students
with disabilities access to its programs and activities. Thus, while not every academic and nonacademic
building is fully accessible, sufficient access exists to allow students with disabilities the equal
opportunity to participate in the academic and social life of the University.
b. Although the University endeavors to make its programs accessible to individuals with
disabilities, it recognizes that some disabilities may preclude an individual from successfully completing
a given academic program. To provide guidance to individuals with disabilities, the University provides
a description of what it considers to be the Minimum Technical Standards for Admission and
Matriculation to each of its programs. Because it is not possible to address every possible circumstance,
these Minimum Technical Standards should be considered as guidelines. Any student with a disability
who believes that he or she is unable to meet the Minimum Technical Standards, but believes that a
reasonable accommodation will permit that student to complete the program successfully, should contact
the Learning Enhancement and Academic Development Office (LEAD) as soon after admission as
possible. The University will determine whether it is appropriate to modify its Minimum Technical
Standards.
c. As soon after admission to the University as possible, students with disabilities should contact
the Learning Enhancement and Academic Development Office, which serves to coordinate disability
services and to discuss any reasonable accommodation that may be required. Each case is dealt with on
an individual basis.
d. Since the University is prohibited by law from making pre-admission inquiries regarding
disability, the University relies on the voluntary provision of whatever information it needs to make
reasonable accommodation for students with disabilities.
2. Resources, Services, and Auxiliary Aids:
The University provides certain services and reasonable accommodations, the nature and extent of
which are based on the Center for Disability Issues and the Health Profession's assessment of individual
need to achieve academic success. Those services and accommodations, provided in consultation with the
student, are intended to allow qualified students with disabilities to pursue their educational careers in the
most equitable and independent fashion possible.
3. Accessibility and Construction:
The Western University of Health Sciences, in compliance with sections 503 and 504 of the
Rehabilitation Act of 1973, and in compliance with the Americans with Disabilities Act of 1990, does not
discriminate on the basis of disability in any of its policies, procedures or practices. It is the policy of the
University to provide qualified persons with disabilities with access to its programs in the most integrated
setting possible. The following statement on construction, renovation, and alteration flows from the spirit
of that non-discrimination principle.
a. Construction of New Buildings and Facilities:
1. New construction will comply with the guidelines and regulations set forth in
Section 504, Title 234, and relevant state and local building codes. The primary standards for such
construction are derived from the Uniform Federal Accessibility Standards (UFAS, 1984), the
Amended Architectural Barriers Act (1984), and the Americans With Disabilities Act of 1990.
2. The University endeavors to employ the most barrier-free design and materials
in new construction to provide superior access to the functions and programs that take place in
those new facilities. The University's goal is to ensure full accessibility and usability of its new
buildings.
b. Renovation and Alteration of Existing Buildings and Facilities:
1. The renovation and alteration of existing facilities will comply with Section 504 and
applicable federal regulations, as well as relevant state and local codes, to enhance program
accessibility. The University recognizes that Section 504 does not require structural changes to
existing facilities where other methods are effective in achieving overall accessibility to the
programs and services of the University.
23
2. Any renovation or alteration will, to the maximum extent feasible, be pursued in
a way that makes the renovated or altered portion of the building accessible to a student with a
disability. However, the design of many existing facilities makes it impractical or prohibitively
expensive to renovate or alter them in such a way as to make them barrier-free.
SEXUAL HARASSMENT
It is the policy of Western University that all persons, regardless of their gender, should enjoy freedom
from discrimination of any kind. Sexual harassment is a form of sexual discrimination, and Western
University will not tolerate such conduct by any member of the University community.
For purposes of this policy, "sexual harassment" means unwelcome sexual advances, requests for sexual
favors, and other verbal, visual, or physical conduct of a sexual nature, made by someone from or in the
educational setting, under any of the following circumstances:
1. Submission to the conduct is explicitly or implicitly made a term or a condition of an
individual's employment, academic status, or progress.
2. Submission to, or rejection of, the conduct by the individual is used as a basis of employment or
academic decisions affecting the individual.
3. The conduct has the purpose or effect of having a negative impact upon the individual's work or
academic performance, or of creating an intimidating, hostile, or offensive work or educational
environment.
4. Submission to, or rejection of, the conduct by the individual is used as the basis for any
decision affecting the individual regarding benefits and services, honors, programs, or activities
available at or through Western University.
5. Creating, transmitting, uploading, or downloading obscene materials not intended for academic
use is strictly prohibited.
Examples of sexual harassment include, but are not limited to: pressure, subtle or overt, for sexual
favors, accompanied by implied or overt threats concerning one's job, grades, or letters of recommendation;
inappropriate display of sexually suggestive objects or pictures; unnecessary touching, pinching, patting or
the constant brushing against another's body; use of sexually abusive language (including remarks about a
person's clothing, body or bodily movement, or sexual activities).
Any student believing that he/she has experienced sexual harassment should resist such harassment and
may file a complaint with the Dean of Student Affairs, or her designee. Complaint forms may be obtained
from the Dean of Student Affairs' office.
To protect all parties involved, Western University handles sexual harassment complaints as
confidentially as the circumstances permit. If the student believes that any official specified in these
procedures was involved in any act of sexual harassment, he/she may file a complaint with another
appropriate official specified in these procedures. Retaliation against a person who reports, complains
about, or participates in the investigations of sexual harassment is prohibited.
All complaints of sexual harassment shall be investigated promptly and resolved equitably. Charges of
sexual harassment may be handled through formal procedures, or, with the consent of both the complaining
party and the alleged harasser, through informal procedures. Informal resolution of a charge of sexual
harassment may take any of the following forms:
a. A meeting among the Dean of Student Affairs, or her designee, the complainant, and the alleged
harasser;
b. A meeting among the Dean of Student Affairs, or her designee, and the alleged harasser; or
c. A recommendation of professional counseling for either principal.
If a formal grievance procedure is requested by either the complainant or the alleged harasser, the Dean
of Student Affairs will refer the matter to an appropriate official of Western University, as follows:
a. In the case of an offending student, the complaint will be directed to the appropriate Academic
Dean. The responsible official will investigate the complaint, and may refer the matter to the Student
Conduct Committee. In this event, the hearing and appeal procedures applicable to the Student Conduct
Committee shall apply.
b. In all other cases regarding administrators, faculty or staff, the complaint will be made to the
Executive Vice President for Academic Affairs/CAO, the Executive Vice President of Finance and
24
Administration, or the Director of Human Resources. The responsible official may appoint an ad hoc
committee to conduct a hearing, and to make recommendations concerning the appropriate disciplinary
action to be taken if the alleged harasser is found to have violated Western University's policy against
sexual harassment. Both the complainant and the alleged harasser will be given notice of, and an
opportunity to participate in, any hearing by the ad hoc committee.
Except for matters referred to the Student Conduct Committee, the responsible official, taking into
consideration the recommendations of the ad hoc committee (if applicable), will decide, in writing, what
action is appropriate under the circumstances. If either the complainant or the alleged harasser is
dissatisfied with the decision of the responsible official, he/she may appeal the decision to the President.
The appeal shall be made, in writing, within seven working days of the written decision of the responsible
official, and shall state any reasons why the person filing the appeal believes that the decision of the
responsible official is incorrect. The President may affirm or reverse the decision, modify the action to be
taken, or remand the matter for further proceedings. For purposes of action to be taken by Western
University, the decision of the President shall be final. Any person who believes that he/she has been the
victim of sexual harassment at Western University is, however, entitled to file a complaint with an
applicable state or federal agency at any time during Western University's proceedings.
DRUG-FREE ENVIRONMENT
Western University is committed to maintaining a drug-free environment in compliance with applicable
laws. The unlawful possession, use, distribution, sale or manufacture of controlled substances is prohibited
on the University's campuses or any of its medical facilities. Violation of this policy may result in the
appropriate disciplinary action up to and including termination or dismissal.
The illegal use of controlled substances can injure the health of fellow students seriously; adversely
impair the performance of their responsibilities; and endanger the safety and well being of other students
and members of the general public. Therefore, the University urges students engaged in the illegal use of
controlled substances to seek professional advice and treatment. Any student who has a drug problem is
invited to contact the Student Affairs Office anonymously at (909) 469-5341, to obtain information about
available assistance. The Western University counseling center, (contact the Student Affairs Office for
name and phone number), offers assistance to students. Students are encouraged to check with their private
insurance carrier for available programs. For those with Western University insurance, the name and phone
number for the insurance carrier is Renaissance, (800) 537-1777.
No one is immune from state or federal laws regarding the use of drugs. Anyone using drugs runs the
risk of legal action and court conviction. Examples of local and state laws are listed below:
• Unlawful possession of a narcotic drug is punishable by imprisonment in the state prison.
• The purchase, possession or consumption of any alcoholic beverage (including beer and wine) by
any person under the age of 21 is prohibited.
• It is not permissible to provide alcohol to a person under the age of 21.
• Selling, either directly or indirectly, any alcoholic beverage to anyone, except under the authority
of the California alcoholic beverage control license, is prohibited.
• It is a felony to induce another person to take various drugs and "intoxicating agents" with the
intent of enabling oneself or the drugged person to commit a felony. The person who induced the other
may be a principal in any crime committed.
• It is a misdemeanor for any person found to be under the influence of an intoxicating liquor or drug
in a public place and unable to care for his/her own safety or disorderly conduct.
As a condition of employment, an employee of the University, including any work-study students, shall
notify his/her supervisor if he/she is convicted of a criminal drug offense occurring in the workplace within
five days of the conviction. Failure to report a conviction may be grounds for dismissal. In the event that
25
any such conviction involves an employee working on a federal grant or contract, the University is
obligated to notify the granting or contracting federal agency within ten days of receiving notice of the
conviction.
Students are required to notify the Dean of Student Affairs within five days of a conviction if they are
convicted of a criminal alcohol or drug offense occurring on the campus. For the purpose of this policy,
"campus" includes all experiential sites. Remedial actions and/or sanctions may be applied, up to and
including dismissal.
Students who are Pell Grant recipients must report convictions for criminal drug violations, occurring on
or off campus, in writing to the Director of Grants and Contracts Service at the U.S. Department of
Education within 10 calendar days of such conviction.
This statement is being set in accordance with the Drug-Free Workplace Act of 1988 (Public Law 100-
690) and the Drug-Free Schools and Communities Act Amendments of 1989 (Public Law Nos. 101-226,
103 stat 1928 - enacted December 12, 1989). The University will continue its efforts to maintain a drug-
free environment by adhering to the above policy and providing drug awareness programs.
STUDENT HEALTH AND SAFETY
Matriculants into Western University's health professions programs must submit evidence that they are
in good health and should, therefore, be able to withstand the physical and mental pressures commonly
placed upon professional students. The nature of health professions education necessarily brings students in
close contact with a variety of illnesses and diseases, and the following policy has been established as a
protective mechanism for students and patients alike. Students must maintain a health insurance policy for
the duration of their education at Western University. Proof of such coverage is required at the time of each
registration. Health insurance is available through the University at a reasonable cost.
DRESS CODE/IDENTIFICATION
Students are required to dress in a professional manner at all times.
During classroom lectures, students are required to wear clothing that is in good repair (no patches).
Footwear is required at all times. Dress for skills labs should not be worn outside the laboratory area. Tank
tops, halters, scrubsuits and headgear (hats/helmets) are not to be worn in the classrooms. Shorts may be
worn, but no more than 3” above the knee. Hair, beards, and mustaches must be clean, net, trimmed at all
times. Students are expected to conform to the commonly acceptable social standards of personal hygiene.
White clinic jackets must be worn at Honors Day, Awareness Conferences, Health Fairs, and in all
clinical settings.
Name pins must be worn at all times on rotations. University identification badges are also provided
and must be worn at all times while on campus.
Students must dress professionally throughout the duration of every clinical rotation/assignment unless
the preceptor of that rotation/assignment directs otherwise.
Exceptions to the dress code may be requested from the appropriate Academic Dean.
SMOKING
As a graduate university of medical health sciences committed to training and educating health care
professionals, we have a responsibility to be a role model for proper health maintenance and prevention.
We are concerned about the health and well-being of all individuals who learn and work here, as well as
those who visit. Out of respect and loyalty to the University, its mission and its constituents, smoking is not
permitted inside campus buildings, health care facilities where patient care is delivered, or inside University
vehicles.
REQUIRED IMMUNIZATIONS
Since students will have some exposure to patients during the first year, NO STUDENTS WILL BE
ALLOWED TO MATRICULATE UNTIL THEY HAVE SUPPLIED PROOF THAT THEY ARE
26
CURRENT ON THE FOLLOWING IMMUNIZATIONS AND HEALTH SCREENINGS: MMR
(measles, mumps, rubella) (proof of immunization or serologic titers showing immunity), Polio,
Tetanus/Diphtheria (within 10 years), Hepatitis B (proof of completion of 3 shot series or serologic titers
showing immunity), P.P.D. (Purified Protein Derivative) (within the last six months) or chest x-ray (within
the last year), Varicella (chicken pox) - proof of completion of the age appropriate immunization series or
positive serologic titers. These immunizations/tests may require updating on a more frequent basis prior to
beginning clinical training if specified in the affiliation agreement with the clinical training site. POSITIVE
PPD OR CHEST X-RAY MUST BE FOLLOWED UP AT THE UNIVERSITY CLINIC.
Such proof is not required for an individual who submits an affidavit or certificate signed by a physician,
duly registered and licensed to practice in the United States, in which it is stated that, in the physician's
opinion, the immunization required would be injurious to the health and well-being of the student or any
member of his or her family or household. Unless a lifelong condition is specified, the affidavit or
certificate is valid for only one year from the date signed by the physician and must be renewed each year
for the exclusion to remain in effect.
No student will be permitted to register or attend classes without having proof of completing required
immunizations.
FOOD IN LECTURE HALLS, LABORATORIES AND LIBRARY
Food is not allowed in the lecture halls or laboratories. Drinks in closed containers are permitted.
Occasionally, noon-hour lectures or seminars are scheduled in lecture halls. At these times, students are
permitted to bring their lunches; however, care must be taken to dispose of all refuse in trash containers
after the lecture. The student lounges may be used for eating.
No food or drink is allowed in the Library at any time.
VIDEOTAPING, AUDIOTAPING, STILL PHOTOGRAPHY AND DIGITIZED NOTE TAKING IN
LABORATORIES AND LECTURE HALLS
Videotaping, audiotaping, still photography and digitized note taking are not permitted in University
laboratories and lecture halls without the express permission of the involved instructor. If a student wishes
to utilize one of these recording methods, each student must request permission of the instructor prior to or
at the first day of a given lecture series or laboratory class. The Center for Disability Issues and the Health
Professions will obtain permission from the instructor on behalf of any students requiring such approved
accommodations prior to the start of a given semester or course, or as soon as possible if a student’s
disability arises or is declared after the start of a semester or course.
Such materials are only for the personal use of the individual student, and any further duplication,
dissemination or retransmission of these materials in any format is prohibited without the expressed written
permission of the instructor and the Office of Academic Affairs.
ELECTRONIC COMMUNICATIONS
Every student of Western University is provided access to a westernu.edu e-mail address. Most official
communications to students will be sent to this e-mail address. It is therefore expected that each student
will check their e-mail on a regular basis to keep informed. Computer terminals are available in the library
and in the computer lab on the second floor of the Health Sciences Center for student use.
27
GENERAL ACADEMIC POLICIES AND PROCEDURES
The University endeavors to provide an environment in which students may develop into effective health
care providers. Freedom of inquiry and expression are essential to a learning environment. Students are
encouraged to develop a capacity for critical judgment and engage in an independent search for truth. The
responsibility for securing an environment conducive to freedom of inquiry and learning is shared by the
students, faculty and administration. As a part of that shared responsibility, the University has adopted
Standards of Academic and Professional Conduct.
Educational Philosophy
The educational programs of Western University are based on the belief that schooling not be allowed to
get in the way of education and that the content and substance of the curriculum, as well as the instructional
and planning processes used to carry it out, reflect a humanistic approach. In short, the University strives to
provide people-oriented programs so that its students become people-centered practitioners.
1. Standards of Academic and Professional Conduct
Complete confidence in the honor and integrity of the health professions student and health care
professional is essential. Such confidence depends entirely on the exemplary behavior of the individual
health care provider in his or her relations with patients. Strict honesty as a personal way of life should be
nurtured during the period of education for professional service. The student shall conduct all aspects of his
or her life with honor and integrity. This includes accountability to oneself and to relationships with fellow
students, future colleagues, faculty, and patients who come under the student's care and contribute to his or
her training and growth.
Upon accepting admission to the University, each student subscribes to and pledges complete
observance to the Standards of Academic and Professional Conduct as outlined in this Catalog. A violation
of these standards is an abuse of the trust placed in every student and could lead to suspension or dismissal.
2. Orientation/Registration
Attendance at Orientation is mandatory for all incoming first-year students for the DO, PharmD, MPT,
MSPA, and MSN/FNP programs.
a. Students will be required to register in person on the registration day specified in the University
Calendar or as otherwise directed by the Registrar. Assessed tuition and fees and all prior debts must be
paid in full on or before registration day each academic year.
b. Matriculation is subject to satisfactory completion of all academic requirements and payment of all
outstanding debts to the University.
c. The receipt of final transcripts from undergraduate colleges and a physical examination with
documentation of required immunizations are additional requirements for incoming students.
d. All DO, MPT, MSPA, PharmD and MSN/FNP students must show proof of current health insurance
coverage at the time of registration. This coverage must be maintained in effect throughout the period of
matriculation at Western University. If there is no proof of current coverage, a health insurance policy
provided by the University is available.
3. Withdrawal from University/Program
Matriculation at the University is a privilege granted in consideration of specified levels of performance
and of maintaining the established standards of scholarship and personal and professional conduct. The
University reserves the right to require withdrawal at any time it deems necessary to safeguard its standards
of scholarship, conduct and orderly operation. The student concedes this right by act of matriculation. See
Program Specific sections of this Catalog.
Application for voluntary withdrawal from the University/Program must be made in writing to the
appropriate Academic Dean. Except in rare and special circumstances, the application will be accompanied
by a personal interview. Every effort should be made by the student to assure that no misunderstandings or
errors occur in the withdrawal process. Students who leave the University/Program without notifying the
office of the Dean and the office of the Registrar, and without completing the established withdrawal
procedures within 30 days, will be terminated automatically from the University.
28
In addition, students must report to the Registrar's Office to sign the withdrawal form to officially
withdraw from the University/Program. Students who do not complete this application for voluntary
withdrawal will not be considered for re-admission at a later date.
Students who withdraw "in good academic standing" are not assured of re-admission unless it is a part of
the final decision and/or agreement made between the appropriate Academic Dean and the withdrawing
student. This final decision and/or agreement must be in writing so that it is clear to all parties involved.
Students who are granted re-admission following withdrawal in good academic standing usually re-enter at
the beginning of the next academic year and register for all courses scheduled during the academic year of
their withdrawal, including those previously completed and passed, unless so stipulated.
Students who withdraw "not in good academic standing" must request re-admission through the
University's Admissions Application process unless otherwise stipulated.
4. Leave of Absence
A student may request a Leave of Absence with the occurrence of a medical problem, serious personal
problems, or health related issues.
Students requesting a Leave of Absence must apply in writing to the appropriate Academic Dean. In the
event of a medical problem, the request must be accompanied by a letter from a physician describing the
nature of the disability for which the leave is requested and the estimated length of time needed for
recovery.
After consultation with the student, the respective Academic Dean will decide whether or not the leave is
to be granted and the conditions under which the student may return to school. A student requesting a leave
of absence during or at the end of the academic year must go through the following procedure:
a. In writing, request a Leave of Absence from the appropriate Academic Dean.
b. Obtain a Leave of Absence form from the Registrar. After completing the student’s portion, meet
personally with the appropriate Academic Dean or designee to discuss the reason for the leave. After
consulting with the appropriate Academic Dean/designee, the Dean/designee will sign the Leave of
Absence form indicating his/her approval to proceed with the remainder of the exit process.
c. Take the form to the faculty advisor, who will provide counsel and sign the form.
d. Take the signed Leave of Absence form to the other listed administrative officials for their
signatures.
e. Return the signed form to the Registrar, who will sign and date the Leave of Absence form.
Provided the leave of absence is approved, the official date of the leave of absence will be the original
date of receipt of the student's request and any tuition charged will be in accordance with the institution's
refund policy.
Leaves of absence requested for a full academic year will be for one year only with expected
reinstatement at registration for the following year. Leaves of absence requested after registration for any
given academic year will be granted for a period not to exceed the number of months remaining until the
registration date for the next academic year. During the leave of absence, students are entitled to library
privileges, use of the student lounges, and participation in student clubs. It is required that the student
maintains a health insurance plan throughout the period of the leave.
A student who is granted a leave of absence for one year or more, must submit a letter of intent to re-
enroll to the appropriate Academic Dean, at least three months prior to the requested date of return. The
letter must also be accompanied by a $500 tuition deposit. It is the student's responsibility to keep the
Registrar informed of any change of address while on a leave of absence.
If the student has not paid 100% of the tuition during the year in which the leave is granted, the balance
of the tuition plus any increase of tuition or fees will be payable in the next year of attendance. All
appropriate tuition and mandatory fees are due prior to graduation.
Leaves of absence will be limited to a maximum of 2 years.
The term and conditions of any leave will be determined by the appropriate Academic Dean.
5. Academic Advisement
Students will be assigned a faculty advisor upon matriculation. Advisement by a faculty advisor should
be viewed by the student as a part of the academic process. If either the student or faculty member does not
find the relationship helpful, either is free to seek a change. This request should be made to the appropriate
29
Academic Dean or designee. It is the student's responsibility to meet periodically with his/her advisor. A
student on probation must contact his/her faculty advisor at least once a month.
6. Attendance and Absences
Attendance is required at all scheduled instructional periods. Absence from instructional periods for any
reason does not relieve the student from responsibility for the material covered during the periods missed.
7. Student Academic Progress Committee
See the appropriate Program Specific section of this catalogue.
8. Standards of Professional Conduct: Statement and Procedures
Complete confidence in the honor and integrity of the health professional is essential. Such confidence
depends entirely on the exemplary behavior of the individual in his/her relations with patients, faculty and
colleagues. Strict honesty as a personal way of life should be nurtured during the period of education for
professional service.
The student shall conduct all aspects of his/her life with honor and integrity. This includes
accountability to oneself, to relations with fellow students, future colleagues, faculty and patients who come
under the student's care or contribute to his/her training and growth, and members of the general public.
This applies to personal conduct that reflects on the student's honesty and integrity in both academic and
non-academic settings, whether or not involving a University sponsored activity.
Professional Concerns - Upon accepting admission to the University, each student agrees to abide by
basic standards of honesty and academic integrity. Students should only matriculate here if they agree with
these basic standards. They include, but are not limited to, the following:
a. A student never represents the work of others as his/her own.
b. A student should acknowledge the other members of the group when work is carried out jointly.
c. A student never gives or receives assistance during an exam.
d. A student is always accountable to clinical faculty while on clinical training.
Acts of dishonesty, invasion of privacy, theft, acts of violence, sexual harassment and disrespect for
personal and University property are examples of unacceptable behavior.
The administration, faculty and staff are here to serve the students. Personal gifts are discouraged, and
monetary gifts are prohibited.
Reporting Alleged Violations - Upon witnessing a possible professional violation, any member of the
academic community should report the incident to the respective Academic Dean or other appropriate
University official. If the conduct involves a particular course of program, the classroom instructor or the
clinical training program supervisor should be advised. Depending on the nature of the conduct, an
individual witnessing a possible violation may choose to talk to the transgressor on an individual basis to
attempt to resolve the problem before reporting it to University officials. The individual receiving the
report will dispose of the violation in an appropriate manner. If there appears to be adequate cause, a report
should be submitted in writing to the appropriate Academic Dean. The report should include the name and
signature of the individual making the report.
In most circumstances, the Academic Dean will meet with the student to discuss the nature of the
possible violations that have been reported and the actions, if any, that the Dean intends to take. The Dean
may resolve the matter without convening a hearing before the Student Conduct Committee, unless the
student requests that a hearing be convened. In some circumstances, the Academic Dean or the Executive
Vice President for Academic Affairs/Chief Academic Officer may refer the matter directly to the Student
Conduct Committee for hearing.
When a matter is referred to the Student Conduct Committee, the University shall prepare appropriate
written charges based on all information reported or known. Any appropriate representative of the
University acting with the consent of the Dean or the Executive Vice President of Academic Affairs/Chief
Academic Officer may prepare the written charges. The Chair of the Student Conduct Committee, or the
chairperson of the hearing panel that will hear the matter, will notify the student of the time and date of the
hearing and shall provide the student with a copy of the written charges.

30
9. Student Conduct Committee
Purpose - The Student Conduct Committee considers violations of the Standards of Professional
Conduct when requested by the respective Academic Dean.
Composition - The Student Conduct Committee is composed of elected faculty members and student
representatives. The Dean of Student Affairs is a non-voting, ex officio
member of the committee. When
the Dean of Student Affairs is absent or unavailable, a designated representative will participate in Student
Conduct Committee proceedings or hearings. Student representatives shall participate as members of
hearing panels when a matter concerning a student is referred to the Student Conduct Committee for
hearing.
Hearing Panels - When a matter concerning a student is referred to the Student Conduct Committee, it
will be determined by a hearing panel comprised of three faculty members serving on the Student Conduct
Committee and two student representatives. Student representatives shall be from the same College as the
student involved, and shall be selected from the Vice Presidents and Secretaries of each class on campus.
The Chair of the Student Conduct Committee shall appoint the individuals who will serve on the hearing
panel, and shall designate one member of the hearing panel as its Chairperson. If it is not reasonably
feasible for the Chair of the Student Conduct Committee to appoint hearing panel members from the
foregoing individuals, either because of a conflict of interest or for any other reason, the Chair may appoint
alternate faculty members or student representatives to serve on the hearing panel. The Dean of Student
Affairs, or a representative of the Dean of Student Affairs, is entitled and normally participates as a non-
voting, ex officio
member of each hearing panel. Each hearing panel acts with the full authority of the
Student Conduct Committee, and the hearing panel's determination constitutes the determination of the
Student Conduct Committee as a whole.
Protocol for Meetings on Alleged Violations of Professional Conduct -
a. The chairperson of the Student Conduct Committee, or the chairperson of the hearing panel, will
notify the student in writing of the specific charges and the time and date of the hearing when the
charges will be considered. The notice also shall state whether expulsion from the University may be
considered if the charges are found to be true.
b. Except as provided below, the meeting will be closed to all individuals not directly involved. The
hearing panel may exclude witnesses, except during the time they are testifying.
c. If the notice of the hearing states that expulsion from the University will be considered if the charges
are found to be true, or if other circumstances warrant, the student may request permission for a mentor
to appear at the meeting to assist the student. The advisor is normally limited to advising the student and
is not permitted to examine witnesses or otherwise participate directly in the proceeding. However, the
hearing panel may permit the mentor to participate directly where special circumstances are shown that
warrant such participation. The student shall make any request for permission for a mentor to appear or
participate in writing, which shall identify the mentor the student desires and provide any additional
information the student deems relevant to the request. Normally, the chairperson of the hearing panel
will inform the student within three business days of receipt of the request whether the mentor will be
permitted to attend the hearing.
d. If requested, the specific charges will be read to the student by the chairperson of the hearing panel.
If the charges are not read, the charges will be deemed to be those specified in the notice of the hearing.
e. The student may testify and present evidence and witnesses on his/her behalf. The student is subject
to questioning by members of the hearing panel, as are all witnesses.
f. The student may question witnesses called by the hearing panel.
g. The hearing panel may, if it chooses, consider affidavits, declarations and other written statements
and documents. Under normal circumstances, the student shall be provided copies of any such
documents at least two days prior to the hearing. If the student desires to present any written documents,
they must be provided to the hearing panel at least two days prior to the hearing. The hearing panel
shall give such weight to the documents, as it deems appropriate under the circumstances.
h. The chairperson of the hearing panel, at his/her discretion, may continue any hearing if warranted due
to the unavailability of a person considered important to the hearing or due to other circumstances. It
shall be the responsibility of the student to present all evidence he/she deems relevant at the scheduled
hearing unless such evidence cannot be presented due to circumstances beyond the student's control.
i. The hearing panel shall determine whether, based on the evidence presented, it is more likely than not
that the charges made are true.
31
j. The hearing panel determines that the charges are true, it shall also make a recommendation with
respect to sanctions to be imposed. The hearing panel may consider any prior disciplinary action against
the student and any other information it deems pertinent in making a recommendation. The student shall
have the right to present evidence of any mitigating circumstances he/she deems relevant, but such
evidence must normally be submitted within two days of notification to the student that the hearing panel
has found the charges to be true.
k. No deviation from the procedures specified herein shall be grounds for objection by the student
unless the student calls an error to the attention of the hearing panel in time to permit the hearing panel
to conform to the specified procedure. Moreover, procedural deviations shall not be grounds of
objection where, under all of the facts and circumstances, the student has been provided fair notice of
the charges and a fair hearing.
l. The hearing panel will make its recommendations to the appropriate Academic Dean.
Status of Student Pending Action - Pending a determination by the appropriate Academic Dean
following a hearing and a recommendation by a hearing panel of the Student Conduct Committee, the status
of the student will not be altered except for reasons of his/her physical and emotional well being or for
reasons relating to the safety of other students and University personnel. Thereafter, the status of the
student will not be altered pending determination of a timely appeal by the student, except that the
Executive Vice President for Academic Affairs/Chief Academic Officer shall have the discretion and
authority to suspend the student or take other action at any time during the appeal process, if consistent with
the decision of the Academic Dean. The University further reserves the right to withhold the award of any
degree at any time disciplinary charges are pending against a student.
Right of Appeal - See Student Appeal Process
10. Promotion
Promotion is defined as progression from one academic year or program phase to the next.
a. A student will be recommended to the appropriate Academic Dean for promotion by the respective
Student Academic Progress Committee.
b. A student may not be recommended for progression from one academic year to the next with any
outstanding grades of "I", "U", "R", or "NCr" on his/her academic record or with a yearly grade point
average or cumulative percentage score of less than the minimum required for promotion (see
appropriate Program Specific section of this catalogue).
c. When considering a student for promotion, his/her professional, ethical, and personal conduct may
also be taken into consideration (as described under Probation a-3).
d. A student will be promoted provided that all academic, legal and financial requirements of the
University, as stated elsewhere in the University Catalogue, have been satisfied.
11. Probation
a. Probation is defined as a period of time, specified by the appropriate Academic Dean, during which
the student's progress will be closely monitored by the respective Student Academic Progress Committee
and the respective Dean. To monitor a student on probation closely during clinical training, the
individual program reserves the right to assign his/her remaining clinical rotations/assignments. A
student will be placed on probation for any of the following reasons:
1. Inadequate academic progress as determined by the specific Student Academic Progress
Committee (see appropriate Program Specific section of this Catalog).
2. When directed to repeat a year for academic reasons.
3. Seriously deficient ethical, professional, or personal conduct.
Professional and personal conduct includes: attendance, cooperation with instructors, interest
shown in assigned work, attitude toward fellow students and associates and toward personnel of
hospitals, approach to and interaction with patients, as well as personal appearance appropriate to
the circumstances.
32
The terms of probation for ethical, professional, or personal conduct will be specified at the time
the student is placed on probation.
b. When a student is placed on probation, he/she will be notified in writing by the appropriate
Academic Dean and the reasons will be stated. Notification must be sent by Certified Mail or hand-
delivered and acknowledged by signatures of the student and the appropriate Academic Dean or his
designee. Copies of the letter will be placed in the student's permanent file and distributed to the
Chairman of the Student Academic Progress Committee and the student's Faculty Advisor. The Student
Academic Progress Committee will consider when the terms of the academic probation have been
satisfied and recommend to the appropriate Academic Dean that probation can be rescinded.
c. A student on probation may not serve as an officer of any official University or College club or
organization and should not engage in time-consuming extracurricular activities. No student on
probation will be permitted to enroll in an elective course.
d. On-campus students on probation must meet with their faculty advisor at least once each month. Off-
campus students on probation must contact their faculty advisor once a month. It is the student's
responsibility to contact the faculty advisor to arrange for these meetings.
e. A student will remain on probation until the program specific minimal acceptable academic standards
are met again.
f. A student will be removed from probation when the specified terms of probation for ethical,
professional, or personal conduct are met. The student will be notified in writing.
12. Remediation
Every effort will be made to provide each student ample opportunity to demonstrate competency in each
area of the academic program. Please see appropriate Program Specific section.
13. Remediation: Financial Aid Policy
Students who are required to repeat coursework due to an unsuccessful prior attempt must contact a
Financial Aid officer in regard to financial aid eligibility.
Students who have been recommended by the Student Academic Progress Committee and appropriate
Academic Dean to repeat the year due to unsatisfactory progress (GPA) or in cases where there is a
satisfactory GPA, but deficiencies are noted that impede promotion, the following criteria must be met to be
eligible for financial aid:
a. Full time attendance recorded.
b. Placed on one-year probation.
c. Must be tested and graded.
d. Must be monitored closely.
It is the student's choice to audit course work to strengthen skills as long as he/she has met satisfactory
progress such as GPA and is fully aware that he/she will not be eligible to apply for any financial aid to
cover these audit costs. The student will be financially responsible for himself/herself until promoted by the
appropriate Academic Dean.
If, at the end of the academic year, the student is still considered to be making unsatisfactory progress
and must remediate, he/she is removed from the list of Title IV and Title VII financial aid recipients.
Summer remediation is not covered by financial aid and cannot be considered an expense item on the
next year's budget
Appropriate tuition and fees will be determined by the Executive Vice President of Finance and
Administration.
14. Summary Suspension
Each student is expected to govern his/her conduct with concern for other individuals and for the entire
University community. Actions that threaten or endanger, in any way, the personal safety and/or well being
of self or others, or that disrupt or interfere with the orderly operation of the University are cause for
immediate disciplinary action.
Either the President, Executive Vice President for Academic Affairs/CAO, or appropriate Academic
Dean has the authority to summarily suspend a student when the student admits to guilt or when, in the
33
opinion of the President, Executive Vice President for Academic Affairs/CAO or appropriate Academic
Dean, such action is appropriate to protect the health or safety of any individual, or to preserve the orderly
operation of the University.
When a student is summarily suspended, the student shall be informed, in writing, of the specific charges
on which such suspension is based. Such notice shall be delivered personally to the student or mailed by
certified mail within forty-eight (48) hours of the imposition of the suspension. Such conduct by a student
shall be considered a violation of the Standards of Professional Conduct and suspected violations will be
handled by the procedures outlined under Standards of Professional Conduct section of this Catalog.
Appeal of the decision of the respective Academic Dean can be made to the Executive Vice President
for Academic Affairs/CAO. Any student who has been summarily suspended may also request, in writing
to the appropriate Academic Dean, a hearing by the Student Conduct Committee, and a hearing shall be
convened within ten (10) working days of the date such request is made. Students who are suspended are
not entitled to remain in class or on clinical rotations/assignments during the appeal.
15. Dismissal
The University may dismiss at any time it deems necessary to safeguard its standards of scholarship,
conduct and orderly operation. The Student Academic Progress Committee or the Student Conduct
Committee may recommend dismissal of a student for any reason it deems appropriate. Furthermore,
conviction of a felony while a matriculant at Western University may be grounds for dismissal.
The Student Academic Progress Committee may recommend dismissal of a student as provided in the
Program Specific section of this Catalog.
The Student Conduct Committee may recommend dismissal of a student for matters pertaining to
suspected personal or professional misconduct that include, but are not limited to: academic integrity,
unsatisfactory attendance, inappropriate interaction with instructors, fellow students, and University and
hospital personnel, improper approach to and interaction with patients, and inappropriate personal
dress/appearance.
In its deliberations, the Student Conduct Committee/Student Academic Progress Committee may
consider the student's academic record and will also consult with the student's faculty advisor, the student,
and other faculty and administrators when appropriate. After considering all pertinent information, the
Student Conduct Committee/Student Academic Progress Committee will forward its written
recommendation regarding dismissal to the appropriate Academic Dean.
The decision will be made by the appropriate Academic Dean, based upon the recommendation of the
Student Academic Progress Committee or Student Conduct Committee. The Student Academic Progress
Committee or Student Conduct Committee will base its recommendation not only on the student's academic
record, but will also consult with the student's faculty advisor, other faculty and administrators, and the
student involved, when appropriate.
16. Student Appeal Process
The appropriate Academic Dean shall have the authority to make decisions regarding a student's status
in matters of academic suspension, student conduct, academic progression/promotion, and graduation. The
decision will be based on input from appropriate sources that may include the following: individual
instructors, faculty, and appropriate committees.
a. Within five (5) working days following written notification to the student of the action of the
respective Academic Dean, the student may appeal the decision in writing to the Executive Vice
President for Academic Affairs/CAO. Upon written request from the student, the Executive Vice
President for Academic Affairs/CAO shall review the case and, within seven (7) working days, shall
issue a decision in writing to the student, which may affirm, modify, or reverse the previous action. A
copy of that letter shall be sent to the Dean, and other appropriate individuals.
The decision of the Executive Vice President for Academic Affairs/CAO will be final.
b. The student may remain in class or on clinical rotations/assignments pending the outcome of appeals,
except in cases of summary suspension, and except when the Executive Vice President for Academic
Affairs/Chief Academic Officer has suspended the student or has otherwise determined that it is
inappropriate for the student to remain in class or participate in clinical rotations/assignments, consistent
with the decision of the Academic Dean that is being appealed.
34
c. If a student is suspended for any reason, all student financial aid will be withheld until the appeal
process is resolved by reinstatement of the student or dismissal of the student. If reinstated, the financial
aid funds can be released to the student. If the student is dismissed, the funds will be returned to the
proper agency/lender respectively.
17. Protocol for Input on Matters of Student Concern
When a student has a personal concern involving a teacher or course that is not of general interest to the
class, he/she should speak to the professor directly.
If the concern might involve more of the class, he/she should take the concern to the appropriate class
representative (e.g., curriculum representative or class president) so they might sample class opinion to find
out the extent of concern.
If, in the opinion of the class representative, the concern is valid, the class representative should bring
the matter to the attention of the class professor with the object of resolving it at that level.
If the matter cannot be solved between the class and the professor, it should be taken to the Academic
Dean or designee. If the matter cannot be handled properly by the respective Dean, or if the students feel it
was not, it should be taken to the Executive vice President of Academic Affairs/CAO, whose decision shall
be final.
Note: Grade appeals may not be pursued under this protocol.
18. Legal Limitations on Practice of Health Care
It is a violation of the law and contrary to the policy of this University for any unlicensed person to
attempt to engage in professional practice of health care. Students, therefore, are cautioned to confine such
activities to duly licensed and supervised teaching clinics.
35
TUITION AND FEES
Tuition and fees are subject to change without notice upon approval by the Board of Trustees.
Mandatory fees for each student are non-refundable. For complete information about tuition and fees, refer
to the appropriate section for each program.
FUTURE TUITION RATE INCREASES
You can expect that tuition increases will be part of your educational experience at Western University;
however, one should know that the Board of Trustees and the administration of this University strive each
year to keep tuition at a reasonable level. For example, in recent years the rate of tuition increase has been
kept at or below five percent. While we are committed to quality educational programs, the inevitable
increases in operating costs each year make it necessary to adjust tuition accordingly. The administration
will communicate tuition rate adjustments as soon as they are determined by the Board of Trustees.
TUITION AND MANDATORY FEES
Tuition and Fee Payments
Tuition is assessed in two installments. The first assessment of tuition and fees occurs at the beginning
of each academic year, and the second is assessed approximately half-way through the academic year.
Depending on the academic program, each required payment corresponds to a “period of enrollment.”* A
refund policy for a withdrawal or a leave of absence has been established to address the receipt of private
payment and Title IV Student Financial Aid funds (see Tuition Refund Policy below).
Western University charges tuition based on an “academic” year and covers two period of enrollment.
The number of weeks of instructional time during the period of enrollment is measured beginning on the
first day of class and/or rotation and ends on the last day of class and/or rotation.
*Students in the Master of Science in Health Professions Education program will pay tuition and fees on a
trimester year. Refunds will be based on the trimester.
Other Fees
a. Audit/Remediation Fee: The fee charged for auditing or remediating a class will be calculated on a
prorata basis.
b. Other Fees and Expenses
Late Registration Fee $ 30 per day
Breakage Fee Cost of Replacement
Lost I.D. Badge $ 10
Lost Locker Key $ 40
Copy of Official Transcript (each) $ 5
Faxed Transcript $ 10
Copy of Student File Material 25 cents per page
PRE-PAID TUITION PLAN
The Prepaid Tuition Plan allows for payment of future years’ tuition at the current tuition rate. This
option will assist in avoiding future tuition increases. The payment must be received at least one year
before the start of the next academic year.
Mandatory fees will be charged annually and are not included in the prepayment provisions. For
additional information, please contact the Financial Aid Office at (909) 469-5354 or the Bursar’s Office at
(909) 469-5403.
36
WESTERN UNIVERSITY TUITION REFUND POLICY
Western University has established a refund policy for all students who find it necessary to withdraw
from the University. Students who elect to withdraw or take a leave of absence during the academic year
must submit prior written notification to the appropriate Academic Dean according to the procedures
specified in this Catalog for their program. Western University may amend its institutional refund policy at
any time. Amendments will become effective for the academic year that follows official notification of the
amendment. Any questions concerning Western University's refund policy should be directed to the
Bursar’s Office.
Calculation of Amount of Eligible Tuition Refund
The amount of tuition refund for which the student is eligible is computed as follows:
• If the day the student withdrew was on or before the student completed 60 percent of the enrollment
period for which tuition was paid, the percentage refund is computed as one hundred percent minus the
percentage of the enrollment period that has elapsed up to the date of withdrawal.
• Students who withdraw after completing 60 percent of the enrollment period for which tuition was paid
are not entitled to a refund.
Determining the Withdrawal Date
The withdrawal date is:
a. The date the student begins the withdrawal process prescribed by the respective College;
b. The date that the student otherwise provided official notification to the respective College of
the intent to withdraw; or
c. The midpoint of the payment period for which Student Financial Aid Programs Assistance was
disbursed or a later date documented by the respective College, if the student did not begin the
withdrawal process or otherwise notify the respective College of the intent to withdraw.
If the College determines that a student did not begin the withdrawal process or otherwise notify the
respective College of the intent to withdraw due to illness, accident, grievous personal loss or other
circumstances beyond the student's control, the College may determine the appropriate withdrawal date.
For additional information regarding refund policies for student participating in Student Financial Aid
Programs, see Financial Aid below.
COMPREHENSIVE HEALTH PLAN
It is mandatory that all Western University students have a health insurance plan in force at the time of
registration. If a student can show valid proof of personal health insurance to the Plan Administrator, at
least equal in benefits to the plan recommended by the University, it will not be necessary to purchase any
additional insurance. If valid proof of other insurance cannot be shown, the student will automatically be
enrolled in the health insurance plan made available by the University. This is described in the health plan
brochure provided at the time of registration. There are several available options. The plan with the better
benefits is recommended. Dependent coverage, although not required, is optional at an additional premium
(see Health Plan Brochure).

37
FINANCIAL AID
Financial aid is not intended to replace the financial responsibility of the student; rather, it is intended to
supplement what the family can provide. Students are required to complete the Free Application for Federal
Student Aid (FAFSA) each year they are seeking financial aid. The information provided is used to create
an analysis of each student’s financial ability to contribute toward their educational costs. Students may
complete the FAFSA application via the Internet at www.fafsa.ed.gov
. Students are required to inform
Western University’s Financial Aid Office of all financial assistance (including scholarships) they receive.
More detailed information on the various types of scholarships and awards can be found at Western
University’s website under “Financial Aid.” Western University reviews and administers all of its programs
without discrimination as to race, creed, sex, national origin, or non-disqualifying handicap.
FINANCIAL AID AND THE WORLD OF PRIVATE PHILANTHROPY
Beyond the various federal, state, and other public and commercial funding sources, there is another
sector that provides valuable support to Western University students. It is the world of private philanthropy:
those individuals, corporations, and foundations who willingly accept the responsibility of serving as good
citizens of the larger society. These benefactors contribute to assisting students in achieving their education
goals and, ultimately, to the quality of health care delivered to the public.
DEPARTMENT of EDUCATION
TITLE IV PROGRAMS
Federal Financial Aid Program Criteria
To be eligible for federal financial aid programs, students must be U.S. citizens or permanent residents
of the United States, attending at least half-time, and making satisfactory progress toward their degrees. The
amount of financial aid awarded by the school can never exceed the educational cost of attendance.
Students can not be in default on any educational loan or owe a refund on any state or federal educational
grant. In addition, all male students must have completed U.S. Selective Service registration requirements to
qualify.
Federal Subsidized Stafford Loan: Available to undergraduate and graduate students by participating
lending institutions and guaranteed by the federal government. The interest on these loans is subsidized
(paid) by the federal government while the student is enrolled at least half-time in school.
Federal Unsubsidized Stafford Loan: Available to undergraduate and graduate students by participating
lending institutions and guaranteed by the federal government. However, the federal government does not
pay the interest while the student is in school. Subsidized Stafford loan eligibility must be determined first,
before a student can apply for an Unsubsidized Stafford loan.
Federal Subsidized and Unsubsidized Annual Loan Limits: The maximum annual Subsidized and
Unsubsidized Stafford loan limits per program are as follows for the 2002/2003 academic year:
Subsidized
Unsubsidized
Doctor of Osteopathic Medicine (DO) Program
First Year $8,500 $32,222
Second Year $8,500 $32,222
Third Year $8,500 $36,667
Fourth Year $8,500 $34,444
Doctor of Pharmacy (PharmD) Program
First Year $8,500 $23,889
Second Year $8,500 $23,889
Third Year $8,500 $26,667
Fourth Year $8,500 $23,889
38
Master of Science in Health Professions Education (MSHPE) Program $8,500 $10,000
Master of Physical Therapy (MPT) Program $8,500 $26,667
Master of Physician Assistant (MSPA) Program $8,500 $26,667
Master of Science Nursing/Family Nurse Practitioner (MSN/FNP) Program $8,500 $26,667
Master of Science Nursing (MSN) Program $8,500 $26,667
Master of Science Nursing Harbor Program $8,500 $26,667
Family Nurse Practitioner (FNP) Program $2,625 $ 4,000
Aggregate Loan Limits for Subsidized & Unsubsidized Stafford Loans:
The total loan debt a student
may have outstanding from all Stafford loans combined is different depending on their academic program.
Outstanding loans include student loans received while the student completed undergraduate and graduate
work. The Family Nurse Practitioner (FNP) certificate program has a subsidized aggregate of $23,000 and a
total combined aggregate of $46,000.
For the graduate and professional programs, the subsidized Stafford maximum may not exceed $65,500.
MSHPE Program: $138,500 (less the aggregate amount of any subsidized loans made to the
student).
Because Western University participated in the Health Education Assistance Loan (HEAL) program
before its phase out in 1998, students who are enrolled full time are allowed an increase in annual
unsubsidized Stafford loan amounts. As a result, they also have a higher aggregate as indicated below.
DO Program: $189,125 (less the aggregate amount of any subsidized loans made to the student).
Within this aggregate, the additional HEAL unsubsidized maximum is $80,000.
PharmD, MPT, MSPA, and MSN/FNP Programs: $189,125 (less the aggregate amount of any
subsidized loans made to the student). Within this aggregate the additional HEAL unsubsidized maximum is
$50,000.
Federal Perkins Loan: For eligible undergraduate and graduate students and subject to availability of
funds. The amount awarded varies, depending on financial need and federal allocation to our school. The
Perkins undergraduate aggregate is $20,000, and graduate students have a $40,000 total aggregate. Perkins
loans have a fixed interest rate at five percent.
DEPARTMENT OF HEALTH AND HUMAN SERVICES
TITLE VII PROGRAMS LOANS & SCHOLARSHIPS
Loans for Disadvantaged Students (LDS): Provides long-term, five percent interest loans to eligible
osteopathic medical students from disadvantaged backgrounds, subject to fund availability.
Primary Care Loans (PCL): For eligible students and subject to availability of funds. The long-term five
percent fixed simple interest loan amounts vary, depending on financial need and federal allocation.
Students must provide parental income information and sign a contract to practice in primary care until the
loan is paid in full.
39
Scholarships with Service Requirements
National Health Service Corps Scholarships (NHSC): This scholarship provides full tuition, fees, books,
and a monthly stipend for osteopathic medical, physician assistant, and family nurse practitioner students.
Students must serve in a designated medically underserved area (rural, inner city or Indian health).
Minimum obligation is two years and a student must be an U.S. citizen.
Military Health Professions Scholarships: The Army, Navy and Air Force offer Health Professions
Scholarship programs to medical students for tuition, fees, books and supplies, and a monthly stipend.
While in school, students are expected to serve forty-five days of active duty per year, when possible, with
pay. One year of active service as a medical officer (after internship and/or residency) is required for each
year of support in the scholarship program, with a minimum requirement of three years.
UNIVERSITY ADMINISTERED SCHOLARSHIPS
The Dr. Robert E. Corey Memorial Scholarship Fund:
Established January 1983 as a memorial to
Robert Corey, DO. Recipients are selected from second, third and fourth year students for their commitment
to osteopathic medicine, outstanding community service and demonstrated financial need as determined by
the institution.
The Albert Victor and Mary P. Kalt Scholarship Fund: Established June 1977, and is available for
students of all disciplines who express a desire to work in primary care in an underserved/rural area.
Asian American Scholarship: Awarded to students of Asian descent, who are in good academic standing,
demonstrates financial need and is dedicated to serving the Asian community.
UNIVERSITY ADMINISTERED LOANS
WesternU Emergency Loan Programs: Limited funds made available on a short-term basis to meet
financial emergencies. The maximum loan is $500 interest-free. Since this is a revolving loan fund, it is
expected to be repaid in ninety days.
Roger E. Coe Loan Fund #1: Established in March 1981 by a gift from Roger M. and Ruby M. Coe. Two
loans of $2,500 are made in the spring of each year. Loans will be made to osteopathic medical students
who have completed their second or third year at Western University and are particularly interested in
osteopathic manipulative skills. Interest begins to accrue at the time the loan is disbursed at the rate of eight
percent. First payment begins immediately after graduation with full repayment of loan funds within five
year.
VETERANS’ EDUCATIONAL BENEFITS
The Student Affairs Office will provide certification of enrollment services for veterans attending
Western University. The Financial Aid Office will serve as a direct liaison between our University and
Veterans’ Administration regarding underpayment, overpayment, or non-payment benefits. Students
expecting to collect educational benefits may obtain further information from Western University’s
Financial Aid Office. As of this publication DO, MSN/FNP, MPT, MSPA, and PharmD programs are
eligible. In order to continue collecting benefits, a veteran must be making satisfactory progress towards a
degree.
GRADUATE TEACHING FELLOWS IN THE DEPARTMENT OF OSTEOPATHIC
MANIPULATIVE MEDICINE
This Fellowship program in the Department of Osteopathic Manipulative Medicine of the College of
Osteopathic Medicine of the Pacific (COMP) is designed to expand the educational opportunities for
osteopathic medical students while they assist in all phases of the department’s operation. OMM Fellows
assist in lecturing and teaching practical skills to graduate students. In order to participate in the Fellowship
program, each student takes five years, instead of four, to complete all of their educational requirements,
including hospital and private practice clinical rotations, for the Doctor of Osteopathic Medicine degree.
Fellows receive a full tuition/fees waiver their third and fourth years and an annual stipend for the fifth year.
Fellows are selected from each MSII class annually.
40
TUITION REFUND POLICY
Western University of Health Sciences has adopted the Department of Education refund policy for all
students who find it necessary to withdraw from the University or take a leave of absence during the
academic year. It is a universal policy that applies to all students, those receiving and not receiving financial
aid. Students who elect to withdraw or take a leave of absence during the academic year must submit prior
written notification to the appropriate Academic Dean according to the procedures specified in the
Catalogue for their program. Western University may amend its institution refund policy at any time.
Amendments will become effective for the academic year that follows official notification of the
amendment. Any questions concerning Western University’s refund policy should be directed to the
Bursar’s Office.
If a recipient of Student Financial Aid (SFA) loan funds withdraws from school after beginning
attendance, the amount of SFA loan assistance earned by the student must be determined. If the amount
disbursed to the student is greater than the amount the student earned, unearned funds must be returned. If
the amount disbursed to the student is less than the amount the student earned, and for which the student is
otherwise eligible, he or she is eligible to receive a post-withdrawal disbursement of the earned aid that was
not received. Title IV funds are awarded to a student under the assumption that the student will attend
school for the entire period for which the assistance is awarded. When a student withdraws, the student may
no longer be eligible for the full amount of Title IV funds that the student was originally scheduled to
receive.
Definition of a Title IV recipient
A recipient of loan assistance is a student who has actually received Title IV funds or has met the
conditions that entitle the student to a late disbursement. If the student never actually began attendance for
the payment period or period of enrollment, the refund policy does not apply. Similarly, if a student began
attendance, but was not and could not have been disbursed Title IV funds prior to withdrawal, the student is
not considered to have been a Title IV recipient and the requirements of this refund policy do not apply.
Funds to include in the Calculation
The calculation of earned Title IV program assistance loan funds that were disbursed or could have been
disbursed to a student. This includes Subsidized and Unsubsidized loan funds, and funds from the Federal
Perkins Loan Program.
Title IV Aid Disbursed
A student’s Title IV funds are disbursed when the school credits a student’s account with the funds or
pays a student directly with Title IV funds received from the Department and/or Federal Family Education
Loan (FFEL) funds received from a lender. A student’s aid is counted as disbursed for the calculation if it is
disbursed as of the date of the institution’s determination that the student withdrew.
Calculation of Amount of SFA Program Assistance Earned
The amount of SFA Program assistance earned is the percentage of SFA Program assistance earned
multiplied by the total amount of SFA Program assistance that was disbursed (and that could have been
disbursed) for the payment period as of the day the student withdrew. The percentage earned is one of the
following:
• If the day the student withdrew on or before the student completed 60 percent of the enrollment period
for which the assistance was awarded, the percentage earned is equal to the percentage of the
enrollment period from which assistance was awarded.
• If the day the student withdrew after the student has completed 60 percent of the payment period the
percentage earned is 100 percent.
41
Determining the Withdrawal Date
The definition of withdrawal date is for determining the amount of aid a student has earned. The chart
below lists the withdrawal date for the various types of withdrawals, as well as the date of the institution’s
determination that the student withdrew for each type of withdrawal.
Withdrawal Type Circumstance Student’s Withdrawal
Date*
Date of the Institution’s
Determination that the
Student has Withdrawn**
Official Notification The student begins the
school’s withdrawal process,
or
The student otherwise
provides official notification
to the school of intent to
withdraw.
The date the student
begins the school’s
withdrawal process, or
The date that the student
otherwise provides the
notification.
(If both circumstances
occur, use the earlier
withdrawal date.)
The date the student provides
official notification or begins
the withdrawal process
whichever is later.
Official Notification
Not Provided
Official notification not
provided by the student
because of circumstances
beyond the student’s control.
All other instances where
student withdraws without
providing official
notification.
The date that the school
determines is related to
the circumstance beyond
the student’s control.
The midpoint of the
payment period or period
of enrollment, as
applicable.
The date that the school
becomes aware that the student
has ceased attendance.
Leave of Absence
Related
The students does not return
from an approved leave of
absence, or
The student takes an
unapproved leave of absence
The date that the student
began the leave of
absence.
The earliest of the dates of the
end of the leave of absence or
the date the student notifies the
school he or she will not be
returning to that school. (In the
case of an unapproved
absence, the date that the
student began the leave of
absence.)
Withdrawal After
Rescission of
Official Notification
The student withdraws after
rescinding a previous official
notification of withdrawal.
The student’s original
withdrawal date from the
previous notification.
The date the school becomes
aware that the student did not,
or will not, complete the
program period or period of
enrollment.
*In place of the dates listed, a school may always use as a student’s withdrawal date the student’s last
date of attendance at an academically related activity, if the school documents that the activity is
academically related and that the student attended the activity.
**For a student who withdraws without providing notification to the school, the school must determine
the withdrawal date no later than 30 days after the end of the earlier of the (1) payment period or period of
enrollment (as appropriate), (2) academic year, or (3) education program.
Return of Unearned SFA Program Funds
When a return of Title IV funds is due, the school and the student both have a responsibility for
returning funds. Whatever funds are not returned by the school must be returned by the student. Although
this requirement speaks in terms of returning funds, a school is not required to actually return its share
42
before the student. Rather, it is the calculation of the amount of assistance the school is responsible for
returning to the Title IV accounts that must be calculated first. The student’s repayment obligation is
determined after the school’s share is calculated. If the student receives more SFA Program assistance than
the amount earned, the school, or the student, or both, must return the unearned funds as required. Western
University must return the lesser of
• The amount of SFA Program funds that the student does not earn; or
• The amount of institutional costs that the student incurred for the payment period or period of
enrollment multiplied by the percentage of funds that was not earned.
The student must return or repay, as appropriate, the remaining unearned SFA Program funds.
Order of Return of Title IV Funds
A school must return Title IV funds to the program from which the student received aid during the
payment period or period of enrollment as applicable, in the following order, up to the net amount disbursed
from each source:
• Unsubsidized Federal Stafford Loans
• Subsidized Federal Stafford Loans
• Federal Perkins Loans
Method of Order of Return of SFA Program Refunds
The student returns funds to loan programs in accordance with the terms of the loan. In other words, the
student will repay any unearned loan funds in the same manner that he or she will be repaying earned loan
funds.
Reference: Department of Education, Student Financial Aid Handbook, 2001-2002 Award Year.
43
WESTERN UNIVERSITY CALENDAR*
INDEPENDENCE DAY Thursday, Jul. 4, 2002
Last day of classes Wednesday, Jul. 3. 2002
Classes resume Monday, Jul. 8, 2002
CONVOCATION Saturday, Aug. 10, 2002
LABOR DAY
(no classes) Monday, Sept. 2, 2002
COLUMBUS DAY
(no classes) Monday, Oct. 14, 2002
THANKSGIVING RECESS
Last Day of Classes Wednesday (noon), Nov. 27, 2002
Classes Resume Monday, Dec. 2, 2002
WINTER RECESS
Last Day of Classes Friday, Dec. 20, 2002
Classes Resume Monday, Jan. 6, 2003
MARTIN LUTHER KING
HOLIDAY (no classes) Monday, Jan. 20, 2003
PRESIDENTS DAY
(no classes) Monday, Feb. 17, 2003
HONORS DAY Monday, Apr. 14, 2003
MEMORIAL DAY
(no classes) Monday, May 26, 2003
COMMENCEMENT TBA
*The College of Osteopathic Medicine of the Pacific, the College of Pharmacy, the College of Graduate
Nursing, and the programs of the College of Allied Health (MPT, PA, and MSHPE) maintain specific,
detailed program calendars. Please consult the appropriate program to determine additional official dates.

44
COLLEGE OF OSTEOPATHIC MEDICINE OF THE
PACIFIC
Doctor of Osteopathic Medicine Program
Accreditation
The academic program of the College of Osteopathic Medicine of the Pacific (COMP) is accredited by
the Bureau of Professional Education of the American Osteopathic Association.
The Osteopathic Philosophy
Osteopathic medicine is a contemporary school of medical thought and practice, founded on the concept
that the normal state of a person is health. The philosophy of osteopathic medicine has its roots in antiquity,
long before the life of its founder, Dr. Andrew Taylor Still. The philosophy of Dr. Still can be directly
related to the concepts and teachings of the Greek physician-philosopher, Hippocrates. This “father of
medicine” taught that disease is a natural process and that natural powers are the healers of disease. The
physician must assist nature, said Hippocrates, but attention should be focused on the patient rather than on
the disease. Dr. Still revived this concept and gave it a new meaning and implementation with a system of
diagnosis and treatment that made it the cornerstone of osteopathic medicine.
There are four fundamental principles of osteopathic diagnosis and treatment:
1. The body tends to be self-healing and self-regulatory in the disease processes. The ability to
maintain integrity in a continually changing external environment is mediated through an elaborate
communication network. The communication network embraces the circulatory and neuromusculoskeletal
systems.
2. Intimate interrelationships exist between structure and function at all levels of biologic
organization.
3. Abnormalities of the neuromusculoskeletal system are invariably present during disease. When
subjected to manually applied forces, these abnormalities are ameliorated coincidentally with the clinical
improvement of the patient.
4. Health is an equilibrium state and maintaining this state requires constant biological adjustment.
While employing osteopathic manipulation, the osteopathic physician utilizes other recognized
modalities for diagnosis and treatment. All modalities of treatment are based upon an evaluation of the
patient’s personal developmental stage, and family and social environment.
PERSONAL COMPETENCIES FOR ADMISSION AND MATRICULATION
A candidate for admission to the Doctor of Osteopathic Medicine Program must have the use of certain
sensory and motor functions, or reasonable accommodations, to permit him/her to carry out the activities
described in the sections that follow. Graduation from the program signifies that the individual is prepared
for entry into osteopathic postgraduate training programs. It follows that graduates must have the
knowledge and skills needed to function in a broad variety of clinical situations and to render a wide
spectrum of osteopathic patient care. The osteopathic medical student must be able consistently, quickly,
and accurately to integrate all information received by whatever sense(s) are employed. Also, he/she must
have the intellectual ability to learn, integrate, analyze, and synthesize data.
A candidate for the DO degree must exhibit abilities and skills in the five areas identified below. When
appropriate technological assistance is provided in the program, it may be permitted only as a reasonable
accommodation. Under all circumstances, a candidate should be able to perform the following in a
reasonably independent manner:
Observation
: Candidates and students must have sufficient vision to be able to observe demonstrations,
experiments, and microscopic laboratory exercises. They must be able to observe a patient accurately at a
distance and close at hand.
Communication
: Candidates and students must be able to communicate with patients and colleagues.
They should be able to hear with or without reasonable accommodations. Candidates and students must be
able to read English.
45
Motor
: Candidates and students should have sufficient motor functions to enable them to execute
movements (with or without reasonable accommodations) which are reasonably required to provide general
care and emergency treatment of patients (i.e., palpation, auscultation, percussion, and other diagnostic and
therapeutic modalities). Examples of emergency treatment reasonably required of osteopathic physicians
include: cardiopulmonary resuscitation, administration of intravenous medication, the application of
pressure to stop bleeding, the opening of obstructed airways, the suturing of simple wounds, and the
performance of simple obstetrical maneuvers and osteopathic manipulation. These actions require
coordination of both gross and fine muscular movements, equilibrium, and functional use of the senses of
touch and vision.
Intellectual, Conceptual, Integrative, and Quantitative Abilities
: Students must demonstrate problem
solving skills, which involve intellectual, conceptual, integrative and quantitative abilities. These abilities
include measurement, calculation, reasoning, analysis, and synthesis. Problem solving, the critical
intellectual skill demanded of an osteopathic physician, requires all of these intellectual abilities. In
addition, candidates and students should be able to comprehend three-dimensional relationships and
understand the spatial relationships of structures.
Behavioral and Social Attributes
: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgement, the prompt completion of all
responsibilities attendant to the assessment and care of patients, and the development of mature, sensitive,
and effective relationships with patients. Candidates and students must be able to tolerate physically taxing
workloads, adapt to changing environments, display flexibility, and learn to function in the face of
uncertainties inherent in the clinical problems of many patients. Compassion, integrity, concern for others,
interpersonal skills, interest, and motivation are all personal qualities to be assessed during the admissions
and educational processes.
The Doctor of Osteopathic Medicine program, along with all other programs at Western University of
Health Sciences, shares a commitment to develop creative ways of opening the DO curriculum to
competitive, qualified individuals with disabilities. In doing so, however, the DO degree program must
maintain the integrity of its curriculum and preserve those elements deemed essential to educating
candidates to become effective osteopathic physicians.
ADMISSIONS POLICIES AND PROCEDURES
Western University/COMP accepts applications from all qualified candidates. More applications are
received from qualified candidates than can be admitted. While grades and Medical College Admission
Test (MCAT) scores are important in selecting candidates for admission and may suggest future academic
success, the Admissions Committee recognizes that these statistics, by themselves, do not guarantee later
success as a physician. Therefore, non-academic criteria are also important in making the selection. Western
University/COMP seeks a diverse and balanced student population and considers factors such as a well-
rounded background, work experiences, letters of recommendation, interest in and knowledge of
osteopathic medicine, and professional promise. To ascertain these factors, an on-campus interview is
required prior to action on an application. The College may exercise its discretion to rely upon additional
considerations. Western University/COMP is committed to admitting competitive, qualified individuals
with disabilities.
Early Admission Decision Program
Western University COMP is pleased to offer an Early Admission Decision Program. Qualified
applicants may take advantage of the Early Admission Decision Program if they apply only to Western
University/COMP and submit their application to ACOMAS prior to June 15.
Highly qualified candidates who have a strong preference for Western University/COMP are eligible for
an early admission decision. Candidates must have a minimum science GPA of 3.30, a minimum overall
GPA of 3.30, and a minimum average MCAT score of 9. All prerequisite coursework must be completed at
the time of application. The AACOMAS application must be filed prior to June 15. The Western
University/COMP supplementary application and all supporting documents must be filed prior to August 1.
Interviews and decisions are granted August through September. If you apply as an Early Admission
Decision candidate, you must apply only to Western University/COMP. For further information, and to
request an Early Admission Decision Program application form, contact the Admissions Office at (909)
469-5335, or write to:
46
Western University of Health Sciences
College of Osteopathic Medicine of the Pacific
Admissions Office
309 E. Second Street
Pomona, CA 91766-1854
Entrance Requirements
Candidates for admission to Western University/COMP must meet these requirements at the time of
application:
• Completion of ninety semester hours, or three-fourths of the credits required for a baccalaureate
degree, from a regionally accredited college or university.
• Completion of one academic year (or its equivalent) in English, biology, physics, inorganic
chemistry, organic chemistry, and behavioral sciences.
Applicants must submit their Medical College Admission Test (MCAT) scores. Information concerning
this test may be obtained from the pre-professional advisor at one’s college or directly from the MCAT
Program Office, 2255 North Dubuque Road, P.O. Box 4056, Iowa City, Iowa, 52243; phone (319) 337-
1357. This examination is offered in the spring and summer. Applicants are encouraged to take the
examination in the spring of their junior year. To be considered for admission, the MCAT examination must
be taken prior to January of the entering year.
Please note that the majority of candidates accepted for admission will have completed four or more
years of pre-professional study prior to matriculation, and that the quality of Western University/COMP
students is therefore relatively high. Successful candidates typically have both science and overall grade
point averages of 3.2 or above on a 4.0 scale and a mean MCAT score over 8.0. Please keep in mind that
academic grades and the MCAT score are just two of the factors used in the evaluation process.
AACOMAS
Western University /COMP, along with the other colleges of osteopathic medicine, participates in a
centralized application service through the American Association of Colleges of Osteopathic Medicine
Application Service, 5550 Friendship Blvd., Suite 310, Chevy Chase, Maryland 20815-7231. Individuals
interested in applying to Western University/COMP should write directly to AACOMAS for information
and application materials or obtain application request cards from the Western University/COMP
Admissions Office. At this time, applicants should also make arrangements to have official transcripts of all
prior undergraduate and graduate course work forwarded to AACOMAS.
Upon receipt of the initial application and transcript(s), AACOMAS will collate materials, compute
grades, and transmit standardized information to the applicant and to those osteopathic medical colleges
that the applicant designates. AACOMAS takes no part in the evaluation or selection of applicants. After
Western University /COMP conducts a review of the AACOMAS application, if both a minimum grade
point average of 2.5 on a 4.0 scale has been achieved overall, as well as in the sciences, and a minimum of
90 semester hours has been completed, the Admissions Committee may request additional information from
the applicant for further consideration. The above grade point average is a minimum, and candidates in the
2.5 GPA range need to be sure this represents sufficient academic strength to meet the academic challenges
at Western University/COMP. Previously, candidates admitted to Western University/COMP have had
substantially higher grade point averages.
Additional information will include the following:
• A supplementary application provided by Western University/COMP. This will be sent only after
receipt of the initial application from AACOMAS. There is a non-refundable supplementary
application fee of $60.
• An evaluation of the applicant’s work and accomplishments submitted by the Pre-Health Professions
Committee of the applicant’s college. If the college has no such committee, the student may submit
evaluations from three classroom professors, two of whom must be in the sciences.
• A letter of recommendation from a physician. A letter from a DO is preferred.
The supplementary required information must be returned within 30 days to the Director of Admissions,
Western University of Health Sciences/COMP, 309 E. Second Street, Pomona, California 91766-1854.
After the applicant’s file is complete, the Admissions Committee reviews it to determine whether the
candidate will be granted an interview. If a candidate is deemed promising, he or she is invited to the
47
campus at his or her expense. The candidate should plan to spend a full day on campus for orientation and
the interview. Orientation consists of information on the curriculum, financial aid, student services, and
clinical rotations; lunch with a Western University/COMP student; a personal interview with members of
the Admissions Committee and faculty; and a tour of the facilities. The Committee evaluates the candidate’s
application and interview. The candidate is notified regarding the status of his or her application in
approximately three weeks.
Note: Candidates accepted to Western University/COMP must have a complete set of official transcripts
mailed to the Admissions Office no later than July 1. AACOMAS retains the original set of transcripts it
receives from applicants.
Transfers from Other Schools
Western University/COMP offers a transfer program for persons who have completed one or more years
of medical studies at a medical school accredited by the American Osteopathic Association (AOA).
Candidates seeking transfer must be in good academic standing at the school where they are enrolled and
be eligible for continuation there. Candidates are expected to meet the minimum entrance requirements that
are required of our entering first-year students. Please refer to the Admissions Policies and Procedures
section in the catalog for specific information regarding these requirements.
Transfers from an LCME accredited medical school or college to Western University/COMP requires
that no less than the last fifty-percent (50%) of instruction is completed at Western University/COMP. In
the case of such transfers, requirements for osteopathic manipulative medicine must be completed before
graduation.
Transfer applications are available from the Admissions Office after September 1. The application
deadline for students wishing to transfer into the second year is March 1
st
. The deadline for students wishing
to transfer into the third year is January 1. Requests for transfer into the fourth year are not accepted.
Transfer candidates must provide:
• Official transcripts from all colleges and universities attended.
• Official transcripts showing the successful completion of studies at the osteopathic medical school
where currently enrolled.
• Official MCAT scores.
• Letters of recommendation from three science professors at your college of osteopathic medicine are
required, as is a letter from a DO.
• A completed transfer application, accompanied by a non-refundable application fee of $100
Upon request, candidates must submit a letter of good academic standing from the Academic Dean of
the osteopathic medical school where currently enrolled. If an interview is granted, candidates are invited to
the campus at their own expense. Candidates should plan to spend a half day on campus for orientation and
interview. Approximately three weeks after the interview, candidates will receive a letter stating the
decision of the Admissions Committee. Acceptance of a transfer student will be dependent upon the
student’s current academic good standing, qualifications, and academic compatibility. and available space at
Western University/COMP. Confirmation of available seats does not occur until mid-June.
Decisions of the Admissions Committee regarding the admission of applicants to the Doctor of
Osteopathic Medicine program are final.
Applications materials are to be sent directly to:
Western University/COMP, Admissions Office
309 E. Second Street
Pomona, California 91766-1854
REGISTRATION
First year students are required to register by the registration date specified in the University Calendar
by the Registrar. Students in subsequent years must complete registration materials, including financial
arrangements, prior to the dates specified in the Program Calendar (below). Matriculation and graduation
are subject to the satisfactory completion of all academic requirements and payment of all outstanding debts
to the University. The receipt of a final transcript from an undergraduate college and a physical examination
with documentation of required immunizations prior to registration are additional requirements for
incoming students. Also, all students must show proof of current health insurance coverage at the time of
48
registration. This coverage must be in effect throughout the academic year. If there is no proof of current
coverage, a policy provided by the University is available. Attendance at Orientation is mandatory for all
incoming first-year students.
TUITION AND FEES
By action of the Board of Trustees, DO tuition and fees for the 2002-03 academic year (subject to
change) are as follows:
ACADEMIC YEAR 2002 - 2003
$29,410 Tuition (Annual)
For DO applicants accepted at Western University, the tuition deposit is $1,000, payable within two
weeks after notification of acceptance. This payment is nonrefundable. An additional payment of $1,000 is
due by May 15 for those accepted for admission prior to May 1 and by June 15 for those accepted after May
1. This additional payment is non-refundable. Upon matriculation the entire $2,000 is applied toward the
total tuition. For applicants who are granted deferred admission to the DO program, the entire $2,000
deposit required to hold a seat in the next year’s class is non-refundable. An additional enrollment deposit
of $500 is due on May 15 of the entering year. This total deposit of $2,500 is non-refundable and will be
applied toward tuition, upon registration and matriculation. If an applicant fails to register, all tuition
deposits are forfeited.
$40 Student Body Fee (1
st
and 2
nd
year). Covers student government expenditures, social activities and
public relations.
$20 Student Body Fee (3
rd
and 4
th
year)
Other Fees and Expenses
$600 Medical Equipment
$800 Required and Recommended Texts-Fall
$300 Required and Recommended Texts-Spring
$45 Anatomy Supplies-Gloves, Scrub, Dissection Kit
$30 (per day) Late Registration Fee
$50 Special Examination Fee
$40 Lost Locker Key
$10 Lost ID Badge
$5 (each) Copy of Official Transcript
$0.25 (per page) Copy of Student File Material
Replacement cost Breakage Fee
National Board Fees
The College requires students to take all sections of COMLEX Level 1 and Level 2 of the National
Board of Osteopathic Medical Examiners as one of the requirements for graduation. These fees, which are
subject to change by NBOME, are currently as follows:
$315 NBOME, COMLEX Level 1 (end of second year)
$315 NBOME, COMLEX Level 2 (end of fourth year)
Clinical Rotations Expenses
During the third and fourth years, some students may elect to do some clinical rotations away from the
Pomona area. In addition, students are required to return to campus several times during the clinical years
for various educational experiences, conferences, etc. Any travel, food, housing or other expenses incurred
by these activities or plans are the student’s responsibility. Some rotations done at or through other
institutions (e.g., certain hospitals or other medical schools) may involve application fees and/or other
charges. Because of the elective and individual nature of the experience, these fees are also the student’s
responsibility.

49
ACADEMIC REQUIREMENTS
Academic Advisement
Students will be assigned a faculty advisor upon matriculation. The academic advisor-student
relationship can become one of the most valuable aspects of medical education. It provides an opportunity
to develop sustained individual contacts between faculty and students on both academic and personal levels.
If either the student or the instructor does not find the relationship helpful, either is free to seek a change.
Such changes are arranged through the Director of COMP Student Services.
Grading Policies and Credit Hours
Official grades are turned in to the Registrar from the Dean of COMP, at which time the online student
records system, BanWeb, is updated. Official grade reports and unofficial transcripts will be available on
the BanWeb student records system throughout the academic year. For more information on how to access
the BanWeb student records system, visit the Registrar’s website at http://www.westernu.edu/registrar
.
COMP uses a combination of numeric scores and letter grades. A numeric score—listed as a
percentage—is used in the MS I and II years. A 4-value letter grade is used in the last two years.
Grades are reported according to the following values:
MS I, II MS III, IV
Percentage
Interpretation Letter Grade Equivalent Percentage*
90-100 Excellent (numeric range 90-100) A (95)
80-89 Good (numeric range 80-89) B (85)
70-79 Satisfactory (numeric range 70-79) C (75)
Below 70 Unsatisfactory (numeric range less than 70) U (69)
I Incomplete 0
M Missing 0
W Withdrawal 0
Cr Credit 0
NCr No Credit 0
Cert Certification 0
AU Audit 0
*Percentages are used in the third and fourth years only to calculate cumulative numeric scores and class
rankings.
Credit Calculations: Courses are rated at one credit hour for each 12 hours of lecture or 24 hours of
laboratory and/or practice sessions. Credit hours of 2.5 will be assigned for each week of clinical rotations.
A cumulative numeric score/grade point average will be calculated and posted on the transcript. Class
ranking is also computed, and will appear on the transcript at the student’s request only. Class ranking is
also available upon request in the Registrar’s Office. Cumulative class ranking for transfer students will not
be calculated. Osteopathic undergraduate teaching fellows will not be ranked until their final year.
Cumulative Numeric Scores/Grade Point Average: The cumulative numeric score will be calculated
at the end of each semester during the first two years of the curriculum with the average of all course
numeric scores weighted by the number of course credit hours attempted. The grade point average will be
calculated at the end of each semester for 3
rd
and 4
th
year students with the sum of earned grade points
divided by the sum of credit hours passed and failed. If a course, system, or clinical rotation is repeated or
remediated, only the last score/grade earned enters into the computation of the cumulative numeric
score/grade point average, but the original numeric score/grade remains on the student’s transcript.
After completion of the second year program, a student with a cumulative numeric score of 75% or less
may have all third year clinical rotations assigned by the Associate Dean for Academic Affairs & Clinical
Education.
Grade Changes: No numeric score or grade will be changed unless the instructor certifies in writing to
the Associate/Assistant Dean for Academic Affairs and the Registrar that an error in computing or recording
the grade/score occurred. Changes are also recorded when the student has remediated a numeric score of
below 70% or an Unsatisfactory grade after being directed to do so by the Dean of Osteopathic Medicine,
as recommended by the Student Academic Progress Committee.
50
For on-campus courses, students have a maximum of two weeks from the time examination results are
returned to them to bring any errors or irregularities in grading to the attention of the instructor. All
recorded grades remain on the official transcript unless a clerical error has occurred. Remediated grades are
re-recorded along with the original numeric score in the first two years. Only the remediated score/grade is
calculated into the GPA/cumulative numeric score.
For third- and fourth-year students, no grade will be changed after one month from the time the grade is
recorded in the Office of the Registrar. Within the above-designated time, grade changes for clinical
rotations will be considered only under the following three conditions:
1. When the Office of Clinical Rotations receives a signed written statement from the preceptor
specifying that a clerical error has been made regarding a grade, and that the purpose of the change is to
correct that clerical error.
2. When the preceptor to whom the student was assigned submits a signed written request to have the
grade changed. The request must include justification for making the change.
3. When a remediation process that has been directed by the Student Academic Progress Committee
and authorized by the Dean is completed and a written evaluation is received in the Office of Clinical
Rotations.
All grade changes must have the approval of the Dean of Osteopathic Medicine or his/her designee. The
student should make every effort to discuss his/her evaluation(s) with the assigned preceptor(s) prior to
leaving the clinical rotation.
Incomplete Rotations: If a student leaves a rotation before it is finished without the permission of the
Assistant Dean for Academic Affairs, or is asked to leave a rotation by the Preceptor or the Director of
Medical Education of a hospital, a grade of “U” on that rotation may be assigned by the Dean of
Osteopathic Medicine or Assistant Dean for Academic Affairs.
Incomplete Grade (I): An Incomplete (I) indicates that a student has not been able to finish all required
work for issuance of a letter grade. An “I” is not counted in the grade point calculations until a letter grade
is issued to replace the “I.” An “I” must be replaced before the student registers for the next academic term,
unless other arrangements are made with the instructor and the Dean of Osteopathic Medicine.
Replacement of an “I” will be under the direction of the instructor with the approval of the Dean or
his/her designee. If the required work is not completed within the specified time, the “I” will be converted
to the score provided by the faculty. It is to the student’s advantage to arrange to make up any incomplete
work as soon as possible. The incomplete (I) remains on the transcript indicated by an asterisk and followed
by the grade/numeric score earned.
Credit Courses (Cr/NCr): Courses graded for Credit/No Credit are those designated by the faculty as
courses required for promotion but not assigned letter grades. The student must satisfy the requirements of
these courses to receive credit.
Exemption from Individual Core Curriculum Course
Students with advanced work or degrees in a particular subject may formally petition the professor and
the Dean of Osteopathic Medicine for credit for an individual core curriculum course. The petition must
include the reasons for the request and all necessary documentation, and must be submitted by the end of
the first week of class. The student must comply with the attendance policy until notification that exemption
has been granted. The professor(s), before recommending exemption, will require acceptable performance
on an examination. The professor(s), in consultation with the Dean of Osteopathic Medicine may suggest
other alternative or additional criteria for determining exemption.
Standards of Satisfactory Progress
Students must maintain a cumulative numeric score of at least 70% on a yearly basis during the first two
years and a “C” average during the last two years to be considered making satisfactory academic and
professional progress. A final numeric score below 70% during the first two years or a “U” in the last two
years must be remediated for promotion or graduation.
Examination Policies
For most examinations, students may be given assigned seats and are expected to place themselves
accordingly, unless prior arrangements have been made with the appropriate coordinator or instructor.
51
Students will rigorously avoid any situation that lends either the opportunity to give, or the appearance
of giving, information that can benefit another student’s examination score. Students are not to discuss
examination questions with other students during any examination that is administered in segments or over
extended time periods.
During scheduled examination hours, students will not be allowed to leave the exam room except in an
emergency and as excused by the proctor. If a student is excused to leave the room temporarily, the proctor
will hold the student’s examination until his/her return.
Once a student finishes an exam and leaves the examination room, he or she will not be permitted to re-
enter the room until the exam is declared over.
All students’ belongings, such as notebooks, calculators, headwear, and headsets, will be kept in front of
the room. No food or drink will be allowed during examinations.
No student questions related to the exam or its content will be answered during the examination period.
Students are permitted to point out typographical errors in the examination notebook.
Violations of Examination Policies
Violations of these examination policies or the Standards of Professional Conduct will be brought to the
attention of the Dean and, subsequently, may be brought before the Student Conduct Committee.
Students who observe a suspected violation during an exam should report this to the proctor rather than
attempt a personal intervention. Persons making verbal allegation must submit a written report to the Dean
or his/her designee during the same day that the incident occurs.
The Dean may make an executive decision on the matter or, if deemed appropriate, convene the Student
Conduct Committee as soon as possible to investigate the allegation. The student may also request a
convening of the Committee. If conclusive evidence that a violation has occurred is presented to the Student
Conduct Committee, recommendations to the Dean may include, but are not limited to, the following
sanctions:
1. Dismissal from the academic program.
2. Suspension from the program for a designated period of time.
3. Academic probation, the period to be recommended by the Committee.
4. Make-up examination, including written and/or oral. The numerical grade on a make-up
examination will be 80% of the grade attained.
While an alleged violation is being examined by the Student Conduct Committee, the status of the
students involved in the case will remain unchanged pending the outcome of the investigation on this issue.
In the case of insufficient evidence, the committee will recommend to the Dean that no action be taken
against the student(s).
After the receipt of the recommendation of the Student Conduct Committee by the Dean, the disposition
of the incident will be conveyed to the involved student(s) by the Dean, in writing, as soon as possible.
Students on Clinical Rotations – COMLEX Examinations
Students on rotation when the COMLEX Levels 1 and 2 examinations are offered may arrange to take
time off immediately prior to and during administration of the examination. Western University/COMP
requests all training program directors and/or preceptors to release students three working days (weekends
included) before the exam. Students should be released by 7:00 a.m. and expected to return to duty by 7:00
a.m. on the day after the examination is concluded. For example, if the exam is administered on Tuesday
and Wednesday, the student should be released from duty on Saturday morning at 7:00 a.m., returning by
7:00 a.m. on Thursday morning. For clarification and assistance on these matters, students on rotations may
contact the Rotations Office toll-free at 1-800-249-9131.
Promotion
Promotion is defined as academic and professional progression from one academic year to the next. The
Student Academic Progress Committee will recommend a student to the Dean of Osteopathic Medicine for
promotion. A student may not be recommended for progression from one academic year to the next with an
outstanding grade of “I,” “NCr” in a required course, a “U” or final numeric score of less than 70%, or a
yearly cumulative numeric score of less than 70% (or grade point average below 2.0).
When considering a student for promotion, ethical, professional, and personal conduct may also be taken
into consideration (see Probation in University Academic Policies section).
52
A student will be promoted provided that all legal and financial requirements of the University, as stated
in the University Catalog, have been satisfied. All academic requirements must be met within a maximum of
six academic years as a condition for recommendation for graduation.
All students entering after July 1, 2001 are required to pass Level 1 of the COMLEX examination before
they are allowed to enter into the fourth year. Students will have taken and passed Clinical Performance
Evaluation before promotion to the third year.
Veterans
Veterans who fail to maintain satisfactory progress for more than one semester will not be certified to
receive any Veteran’s benefits until they have corrected the situation and are making satisfactory progress.
Graduation
A student will be recommended for the degree Doctor of Osteopathic Medicine provided he/she:
1. Has completed at least four years in an accredited osteopathic college or equivalent.
2. Has been enrolled in Western University of Health Sciences/COMP during his/her final two
academic years.
3. Is not on probation and has completed all prescribed academic requirements with a cumulative
numeric score of at least 70% (a grade point average of at least 2.0) and has no outstanding grade
of I or U or a grade of “NCr” in a required Credit/No Credit course.
4. Has successfully taken all sections of Level 1 of the COMLEX examination of the NBOME.
Beginning with the Class of 2003 (entering in 1999), he/she has taken all sections of Level 1 and
Level 2 of the COMLEX.
5. Has demonstrated appropriate ethical, professional, or personal conduct, as defined in the
University Catalog, “General Academic Policies and Procedures” section, thus making it
appropriate to award the degree of Doctor of Osteopathic Medicine.
6. Has complied with all the legal and financial requirements of the University as stated in the
University Catalog.
7. Is expected to complete all requirements for graduation by the subsequent December 31 and is
expected to march with his/her class in the graduation ceremony. Diplomas will be dated as
appropriate to the completion date of the academic requirements.
8. Unless special permission has been granted by the President of the University, all students must
participate in person in the commencement program at which the degree is conferred. If the
President grants special permission to be excused from graduation, the graduate may be required to
present himself or herself at a later date to the Dean of Osteopathic Medicine to receive the
diploma and take the required oath.
Probation
Students may be placed on Probation for the following reasons (these are in addition to the reasons listed
in the General Academic Requirements section on Probation):
1. Inadequate academic progress as determined by the Student Academic Progress Committee. These
include, but are not limited to, receiving a numeric score less than 70% in the first two years in any
course or system, a grade of NCr in a required Cr/NCr course, or a “U” in any clinical rotation or EFM
course.
2. A cumulative percentage score of less than 70% in the first two years, or a GPA of less than 2.0 in the
last two years.
3. When directed to repeat a year for academic reasons.
4. Seriously deficient ethical, professional, or personal conduct.
On campus students on probation must meet with their faculty advisor at least once a month. Off campus
students on probation must contact their faculty advisor once a month. It is the student’s responsibility to
contact the faculty advisor to arrange these meetings.
A first or second year student on probation for a score less than 70% in the first semester will be
removed from probation after one semester provided he/she has regained a cumulative score of at least a
70% and has remediated the course.
A first or second year student will be removed from probation when all scores below a 70% have been
remediated satisfactorily according to the following Remediation section.
53
A third or fourth year student on probation because of a “U” grade in a clinical rotation or in an EFM
course must remediate the “U.” The student will then be reviewed by the Student Academic Progress
Committee at the end of the academic year and may be recommended for continuation of, or removal from,
probation.
Students on probation are to remove themselves from all leadership roles in co-curricular activities
associated with the University and/or with professional associations.
Remediation
The educational objectives that underlie remedial teaching and evaluation should be the same as the
educational objectives that underlie regular courses in the curriculum.
Students who receive a final numeric score below 70% in a course or system during the first two years, a
cumulative numeric score below 70%, or a “U” in a clinical rotation in years three or four, will be reviewed
by the Student Academic Progress Committee.
Where deemed appropriate, the Student Academic Progress Committee, after consultation with the
course instructor, system coordinator, and/or Director of Clinical Rotations, may recommend any one of the
following options:
1. Take a comprehensive examination.
2. Complete special projects or studies in the deficient area(s).
3. Repeat the course, system, or rotation
4. Repeat the academic year.
5. Withdraw from the University (see Dismissal section for criteria for this option).
The score/grade achieved by remediation will be the score/grade recorded except that the highest
score/grade a student may earn by options 1 or 2 (above) is a score of 70% in the first two years and a “C”
in the last two years. The score/grade achieved by remediation will be re-recorded on the transcript along
with the original score/grade.
Numerical scores or grades earned during an attempted remediation of a course, system, or clinical
rotation will be reviewed critically by the Student Academic Progress Committee, Associate/Assistant Dean
for Academic Affairs, and the Dean of Osteopathic Medicine. Failure to earn at least a 70% in the first two
years or a “C” in the last two years or “Cr” may result in dismissal from the College or repeating the
academic year.
Decisions regarding remediation will be made on an individual basis after considering all pertinent
circumstances. The decision will be made by the Dean of Osteopathic Medicine, based upon the
recommendation of the Student Academic Progress Committee. The Committee will base its
recommendation on the student’s academic record and other considerations after consultation with the
student’s faculty advisor, course instructor, system coordinator, Director of Clinical Rotations, clinical
preceptor, and the student involved, as is appropriate.
A student who is required to remediate a course must be notified in writing by the Dean of Osteopathic
Medicine at least 15 working days prior to the remediation date, or within 15 working days after the close of
the academic year in which the student is presently enrolled, whichever comes first.
Notification must either be sent by Certified Mail or hand-delivered to the student and must be
acknowledged with the signatures of the Dean of Osteopathic Medicine or his/her designee and the student.
Remediation: Financial Aid Policy
If the student, at the end of the academic year, is still considered to be making unsatisfactory progress
and must remediate, he/she is removed from the list of eligible Title IV and Title VII financial aid
recipients.
Remediation of courses during the summer is not covered by any financial aid and cannot be considered
an expense item for the following year. Students will attend at their own expense. Appropriate tuition and
fees will be determined by the Executive Vice President of Finance and Administration in consultation with
the Executive Vice President for Academic Affairs and the Dean of Osteopathic Medicine.
Five Year Program
Effective July 1, 2000, students will no longer be admitted to the Five Year program. The following
rules and requirements remain applicable only for students currently enrolled in the Five Year Program.
54
The decision to enter the Five Year Program is a one-time student option. At the time the student opts
for the Five Year Program, prior courses completed and graded will be shown on the transcript. The words
“Five Year Program” will be printed at the beginning of the transcript.
During the second semester of the first year (I-A portion), the student will audit the Dermal,
Neurosensory, Musculoskeletal Systems, and Introduction to Clinical Medicine. These will be listed on the
transcript along with the designation “Au.” If a student chooses to take the examinations in audited courses
and does well, it will not be possible to convert the “Au” to a grade.
Before going on the Five Year Program, the student will be required to repeat any courses that were
completed and graded in which a “U” grade was received. Courses that are remediated will be taken
concurrently with the courses taken in the second year (I-B portion) of the Five Year Program.
Recommendations for remediation will be made to the Dean of Osteopathic Medicine by the Student
Academic Progress Committee.
The student’s progress will be monitored carefully each semester by the Student Academic Progress
Committee, the Associate/Assistant Dean for Academic Affairs, and the Dean of Osteopathic Medicine.
Students in the first two years of the Five Year Program will be dismissed if their grade point average is
below 2.0 at the end of any semester or if they receive a final grade of “U” or “NCr” in any course.
Students admitted to this program will be charged one year of full tuition for year I-A of the Five Year
Program. Western University charges tuition for five years, however, the tuition charged for years IB, II, III
and IV are seventy-five percent of the published tuition for other DO students.
Five Year Program Schedule
YEAR I-A:
First Semester Credit Hours Second Semester Credit Hours
Gross Anatomy 14.5 OP&P 2.5
OP&P 2.0 Medical Ethics Cr
Embryology 1.0 Substance Abuse Cr
Histology 2.0 BCLS (during orientation)
TOTAL 19.5 TOTAL 2.5
(Audit: Introduction to Clinical Medicine, Dermal, Neurosensory, and Musculoskeletal Systems)
Summer I: Enrollment in and successful completion of a Study Skills Course
YEAR I-B:
First Semester Credit Hours Second Semester Credit Hours
Biochemistry 4.5 Introduction to Clinical Medicine Week 2.0
Microbiology 5.5 Dermal System 4.0
Pathology 2.5 Neurosensory System 19.0
Physiology 1.5 Musculoskeletal System 8.5
Pharmacology 3.5
TOTAL 17.5 TOTAL 33.5
(The student must attend the MS I Classes that OP&P TA’s attend and, at the discretion of the OP&P
Department Chair, may be used as an OP&P TA.)
YEARS II, III, & IV: In year II, the student will re-enter the standard COMP curriculum, and will
continue in the standard curriculum throughout years II, III and IV.
Dismissal
The University may require withdrawal at any time it deems necessary to safeguard its standards of
scholarship, conduct, and orderly operation. The Student Academic Progress Committee may recommend
dismissal of a student for the following reasons:
1. Receiving a cumulative numeric score of less than 70% at the end of the first or second year.
2. Receiving a final percentage scores below 70% in two or more courses or systems totaling more than
25% of the total credit hours for the first or second year.
3. Receiving unsatisfactory grades in three clinical rotations in one academic year.
4. Receiving a final percentage score of below 70% (in the first two years) or a “U” (in the last two years)
in a remediated course, system, or clinical rotation.
55
In addition, the Student Conduct Committee may recommend dismissal (see General University
Academic Policies section of this catalog for more information.)
Student Academic Progress Committee
The Student Academic Progress Committee is comprised of five faculty members with the following ex
officio members: the Director of COMP Student Services, the University Dean of Student Services, the
Assistant/Associate Deans for Academic Affairs, and Director of the LEAD Office.
The Student Academic Progress Committee shall periodically review the academic achievements and
performance of all students. The Registrar shall provide the names and grades of students in academic
difficulty to the Student Academic Progress Committee. Additional input may be obtained as appropriate
from the Dean of Osteopathic Medicine and the Office of Clinical Education.
After reviewing a student’s performance records, the Student Academic Progress Committee may
recommend to the Dean any of the following courses of action: promotion, probation, remediation,
dismissal from the College, educational assessment and other appropriate recommendations. It may also
recommend that no action be taken.
The Student Academic Progress Committee also has the responsibility of recommending to the Faculty
as a whole the awarding of the degree of Doctor of Osteopathic Medicine to all students who satisfactorily
complete all requirements for graduation as stated in the University Catalog.
All recommendations of the Student Academic Progress Committee shall be in writing to the Dean, who
will make the information available to the affected student.
Attendance and Absences
Attendance is required at all scheduled instructional periods. Absence from instructional periods for any
reason does not relieve the student from responsibility for the material covered during the periods. Frequent
absences will be viewed as violations of the Standards of Academic and Professional Conduct.
Implementation of the attendance policy for on-campus courses will be the responsibility of the
Assistant/Associate Dean for Academic Affairs.
Students are required to be present for all scheduled examinations and cannot begin an examination
more than 15 minutes after the scheduled time without permission from the Assistant/Associate Dean for
Academic Affairs or his designee. For a student to be considered to take any examination at other than the
scheduled time, the student must have prior approval by the Assistant/Associate Dean for Academic Affairs.
A student who cannot attend an exam due to unforeseen circumstances, including illness, should phone or e-
mail the Assistant/Associate Dean for Academic Affairs and Course instructor/System Coordinator as soon
as possible prior to or after the exam has been administered. A written explanation of the absence (including
documentation on physician letterhead, in the case of illness) must be provided to the Office of the
Associate/Assistant Dean for Academic Affairs and the Course Instructor/System Coordinator the next day
the student is on campus.
If a student misses an examination, the Assistant/Associate Dean for Academic Affairs, in consultation
with the Course Instructor/System Coordinator, will determine whether the absence is excused or
unexcused. If the absence is excused, the student will be permitted to take a make-up examination, the
nature and time of which will be at the discretion of the Course Instructor/System Coordinator; the student
will receive full credit for the makeup examination.
If the absence is unexcused (e.g., failure to show up for a written or practical examination without a
valid excuse as determined by the Assistant/Associate Dean for Academic Affairs and the Course
Instructor/System Coordinator), this is grounds for summary failure (a score of zero) for that examination.
In the case of an unexcused absence, the student who fails the examination will be referred to the Student
Academic Progress Committee for recommendations regarding remediation or dismissal. In this case, if the
Student Academic Progress Committee recommends that the student take a remediation examination, the
maximum score that the student can achieve on the examination will be 70%. If the student fails to take
either a make-up or a remediation examination at the time designated by the Course Instructor/System
Coordinator, without a valid excuse as delineated above, this will be grounds for summary failure (a score
of zero) of that examination and referral to the Student Academic Progress Committee, as described above.
In such a case, a written report will be sent by the Course Instructor/System Coordinator to the Office of the
Assistant/Associate Dean for Academic Affairs, with a copy sent to the Chair of the Student Academic
Progress Committee and the Dean of Osteopathic Medicine for appropriate disposition.
56
Policies for attendance and absences during the third and fourth years are published in the COMP
Clinical Rotations Manual.
CURRICULUM
The curriculum at COMP is a four-year, full-time academic and clinical program leading to granting the
degree of Doctor of Osteopathic Medicine (DO). This curriculum stresses the interdependence of the
biological, clinical, behavioral, and social sciences. The emphasis is on educating physicians for primary
care medicine, employing the distinctive osteopathic principles, for the maintenance of health and treatment
of disease.
COMP’s educational program is centered around the basic concepts of osteopathic medicine. The
College of Osteopathic Medicine of the Pacific identifies and develops the knowledge, the cognitive and
psychomotor skills, and the personal and professional behaviors required of an osteopathic primary care
physician in order to provide competent and comprehensive health care to all members of a family on a
continuing basis. This academic program is intended to meet the following goals:
• To accord primacy to the role of the musculoskeletal system in the total body economy.
• To recognize and emphasize the inherent capacity within the total person to overcome disease and
maintain health; to educate physicians to cooperate with this therapeutic capacity in their methods of
treatment.
• To provide sufficient academic training to make students aware of health needs that must be referred to
a specialist.
A primary care physician must be skilled in problem solving and demonstrate expertise in diagnosis. In
order to achieve this goal, the COMP curriculum emphasizes the integration of basic and clinical sciences in
medical practice. With this approach, practice in problem solving becomes a part of the learning
experience.
The curriculum is divided into three phases:
1. Introduction to the basic sciences.
2. Correlated system teaching, incorporating basic and clinical sciences in the study of ten (10) organ
systems of the body.
3. Clinical experiences.
Various extracurricular activities also contribute to the personal and professional growth of students.
The four-year curriculum has been developed to prepare the graduate for the post-doctoral training years
of his/her choice.
Summer Preparatory Program
The College offers an optional three-week introductory preparatory program to a selected number of
incoming DO students. Students will purchase a workbook and remit a tuition fee of $300. (See course
description for DO 5001 below for additional information.)
PRE-CLINICAL CURRICULUM
PHASE I: First Year, First Semester (Core courses)
The first semester of the first year is designed to introduce the students to the basic concepts of anatomy
(gross, embryology, and histology), biochemistry, microbiology, pathology, pharmacology, and physiology.
Osteopathic principles and practice are interwoven throughout the curriculum.
DO 5010 Biochemistry (4.5 credit hours)
DO 5025 Medical Genetics (1 credit hour)
DO 5030 Gross Anatomy (12.5 credit hours) or DO 5002 (12.5 credit hours)
DO 5035 Developmental Histology (3 credit hours)
DO 5050 Microbiology (5 credit hours)
DO 5060 Pathology (2.5 credit hours)
DO 5070 Pharmacology (2.5 credit hours)
DO 5080 Physiology (1.5 credit hours)
DO 5090 Osteopathic Principles and Practice I (2 credit hours)
57
PHASE II: First year, second semester through second year, second semester
This phase begins in the second semester of the first year and continues throughout the second year. The
basic and clinical sciences concerned with one particular organ system of the body are integrated in
classroom instruction. This approach emphasizes the relevance of basic sciences to clinical practice. The
osteopathic approach is continually emphasized by lecture and laboratory demonstration, including
manipulative techniques. Other courses not directly related to a system are also included in Phase II.
First Year, Second Semester:
DO 5110 Dermal System (3.5 credit hours, 4 weeks)
DO 5120 Neurosensory System (15.5 credit hours, 10 weeks)
DO 5130 Musculoskeletal System (6.5 credit hours, 4 weeks)
DO 5140 Medical Ethics (Cr/NCr)
DO 5150 Introduction to Clinical Medicine (ICM) I (2 credit hours, 1 week)
DO 5160 Behavioral Science and Substance Abuse (4 credit hours)
DO 5190 Osteopathic Principles and Practice II (2.5 credit hours)
Second Year, First Semester
DO 6010 Blood and Reticuloendothelial System (6.5 credit hours, 3 weeks)
DO 6020 Cardiovascular System (9.5 credit hours, 9 weeks)
DO 6030 Public Health (1.5 credit hours, 1 week)
DO 6040 Respiratory System (9 credit hours, 7 weeks)
DO 6050 Psychiatry (2 credit hours)
DO 6090 Osteopathic Principles and Practice III (2.5 credit hours)
Second Year, Second Semester
DO 6110 Renal System (5 credit hours, 3 weeks)
DO 6120 Endocrine System (5.5 credit hours, 3 weeks)
DO 6130 Reproductive System (7 credit hours, 4 weeks)
DO 6140 Gastrointestinal System (11 credit hours, 7 weeks)
DO 6150 Introduction to Clinical Medicine (ICM) II (Cr/NCr)
DO 6160 Medical Jurisprudence (1.5 credit hours)
DO 6171 Differential Diagnosis (Cr/NCr)
DO 6172 Emergency Medicine (Cr/NCr)
DO 6173 Geriatrics (Cr/NCr)
DO 6174 Human Sexuality (Cr/NCr)
DO 6175 Nutrition (Cr/NCr)
DO 6176 Pediatrics (Cr/NCr)
DO 6190 Osteopathic Principles and Practice IV (2.5 credit hours)
*Clinical Performance Evaluation will be administered at the end of Phase II of the curriculum. Students are
required to pass this evaluation in order to be promoted to Phase III of the curriculum.
PHASE III: Clinical Training - Third and Fourth Years
Rotations Office
The Director of Clinical Education and the Rotations Office staff are dedicated to providing our students
with the best possible clinical education and providing exceptional service to everyone with whom they
interact. The Office assists COMP and its students with planning for and completion of their clinical
training in the third and fourth years.
Goals
The goals of COMP’s clinical curriculum include preparing each COMP student with the knowledge,
attitudes, and skills to excel in their chosen postdoctoral training program. Specifically, the student will be
able to:
• Identify the wide range of normal human functioning.
• Recognize, diagnose and treat the most commonly encountered health conditions in a primary care
practice.
• Recognize, diagnose and treat the acute, life-threatening conditions encountered by the primary care
physician.
58
• Differentiate common health problems from less common diseases.
• Recognize conditions or situations that are best handled by consultation and/or referral.
• Provide continuity of health care beginning with initial patient contact.
• Assess and treat chronic medical conditions in various stages of progression.
• Develop appropriate, professionally intimate relationships with patients.
• Understand patients’ individual concerns and incorporate those concerns into routine patient care.
• Integrate osteopathic philosophy and practices into routine patient care.
• Access medical references, including up-to-date medical literature, to understand current medical
knowledge and thought.
• Understand and apply the concepts of community-oriented primary care, epidemiology, health
screening, and prevention.
• Understand and work with the family unit to improve the health and welfare of the individual patient
and his/her family.
Clinical Curriculum
COMP’s clinical curriculum consists of the following four-week rotations:
Third Year
1 Family Practice
3 Internal Medicine (2 General; 3
rd
General or other, such as GI, Cardiology, or Pulmonology)
1 Surgery (General)
1 Pediatrics
1 Psychiatry
1 Obstetrics/Gynecology
1 Osteopathic Manipulative Medicine
1 Primary Care Selective (Geriatrics, Family Medicine, Internal Medicine, Pediatrics, Ob/Gyn)
1 Elective
1 Vacation (not as first rotation)
Fourth year
1 Family Practice
2 Internal Medicine (General and or subspecialty such as GI, Cardiology, Pulmonology, or
Neurology)
1 Surgery (General or subspecialty)
1 Emergency Medicine
5 Electives
1 Vacation
Each year’s curriculum requirements may be completed in any order. There is a mandatory four-week
break at the end of the MS III year. The minimum length of a rotation is four weeks. Rotations may not be
split. A substantial number of rotations may be assigned for MS III and IV years by the Rotations Office,
including a block of rotations (four to six). The student may express a preference for preceptors and
geographic locations for the remaining rotations.
Implementation
Preceptors and hospitals will implement the curriculum in a manner that balances the learning needs of
the students and the educational resources available at the site. Preceptors and sites are encouraged to use a
variety of teaching techniques including observation, monitored participation, video and audio recordings,
computers, readings, individual discussions, and presentations by students, faculty and others to enhance
learning.
Non-Clinical Experiences
Non-clinical experiences like conferences, tumor boards, quality assurance meetings, hospital
committees, etc., are important for students to observe in order to help them understand and appreciate the
full spectrum of activities expected of physicians. Supervising physicians are encouraged to invite students
to participate in as many non-clinical experiences as are practical.
59
Procedural Skills
Part of the College’s expectation is that students will gain a knowledge and understanding of various
procedural skills. In addition to proficiency in the manual aspects of procedural skills, the College expects
that the student will understand the indications, contraindications, risks, benefits, and alternatives for
various procedures. Student performance of any procedure on a patient must be under the direct supervision
of the assigned preceptor or their professional designee.
Evaluation of Students on Clinical Rotations
The “preceptor of record” is the physician to whom the student is assigned for a given rotation according
to the Rotations Office records. That physician is responsible for the rotation evaluation, including
assigning a rotation grade. If the preceptor of record does not assign a grade, the Assistant Dean for
Academic Affairs will determine a grade for the rotation.
Recording of Grades
For any reason other than a clerical error, no grade may be changed more than 20 business days after the
Clinical Rotations Office reports it to the Registrar. Within those 20 days, a grade may be changed only if
the Rotations Office receives a signed statement from the preceptor specifying that such a clerical error had
been.
COURSE DESCRIPTIONS
Courses listed in this catalog are subject to change through normal academic channels. New courses and
changes in existing course work are initiated by the appropriate disciplines, departments, or programs,
approved by the Curriculum Committee, the faculty, the Dean of Osteopathic Medicine, and the Executive
Vice President of Academic Affairs. COMP uses a combination of numeric scores and letter grades. A
numeric score—listed as a percentage—is used in the MS I and II years and a 4-value letter grade is used in
the last two years.
DO 5001 Summer Preparatory Program (0 credit hours, Cr/NCr)
The Summer Preparatory Program prepares incoming students for the Gross Anatomy course and
provides an introduction to Biochemistry. The anatomy component focuses on the skeletal, muscular,
cardiovascular and nervous systems, and a brief overview of other body systems. Presentations also focus
on enhancing student study and test-taking skills. Designed for students without prior coursework in human
anatomy. Acceptance into this program is at the discretion of the instructor/coordinator. The course is
elective and does not meet any requirements of the Doctor of Osteopathic Medicine curriculum. A separate
tuition of $300 is charged.
DO 5002 Intensive Summer Anatomy Course (ISAC) (12.5 credit hours, Numeric Score)
Prerequisite: Application to the course and permission of instructor. The Intensive Summer Anatomy
Course (ISAC) is equivalent to the DO5030, given in 6.5 weeks (covering the first semester of the course)
to highly qualified incoming students. In addition to this Summer Phase, students will complete the final
section of the course in January, along with the students enrolled in DO5030. ISAC students who score
80% and above at the end of this initial 6.5-week period are selected to serve as facilitators (peer leaders) in
the regular gross anatomy course. Facilitators participate in peer-led team learning (PLTL) and experiential
learning during the regular gross anatomy course. Properly trained facilitators lead dissection and
discussion groups at intervals during the course, and some are selected as teaching assistants for the ISAC
the following summer.
DO 5010 Biochemistry (4.5 credit hours, Numeric Score)
This course presents the molecular basis of life and how human physiology can be understood in
biochemical terms, providing a foundation for future presentations on the biochemistry of each organ
system, the disease states caused by biochemical abnormalities, and the biochemical basis for clinical
diagnosis and therapy.
60
DO 5025 Medical Genetics (1 credit hour, Numeric Score)
This course presents an introduction to genetic principles and practices applicable to the contemporary
practice of medicine. Topics may include (but are not limited to) pedigree analysis, structural gene
mutations, the human genome, X-linked genetic transmission, triple repeat diseases, inborn errors of
metabolism, and newborn screening.
DO 5030 Gross Anatomy (12.5 credit hours, Numeric Score)
This course presents an understanding of the structure and arrangement of the gross anatomical features
of the human body. Through lectures and laboratory dissection of cadavers, students are introduced to the
language of anatomy and to clinically important relationships. Models, radiographs and special
demonstrations are employed to emphasize areas useful to the physician.
DO 5035 Developmental Histology (3 credit hours, Numeric Score)
This course traces, through lectures and demonstrations, the basic developmental stages of the human
from fertilization to organogenesis. Specific attention is given to anomalies of early development. The
student is also introduced to an understanding of the structure and function of cells and tissues, utilizing
images from light and electron microscopy. Emphasis is on the structural specialization, function, and
interaction of cells in forming the four basic tissues and the study of structural arrangements of the basic
tissues in organs. A Web-based laboratory provides an opportunity for visual examination of cells, tissues,
and organs.
DO 5050 Microbiology (5 credit hours, Numeric Score)
This course presents the major groups of microorganisms responsible for infectious diseases, enabling
students to recognize and describe them. The course stresses the structure, physiology, and genetics of
microorganisms in relation to their pathogenicity. The salient features of bacteria, fungi, protozoa, viruses,
and viroids are discussed. In addition, the host-parasite relationship, including characteristics of organisms
contributing to disease and host-defense mechanisms, are stressed. Fundamental concepts of immunology,
including the structure of antigens and antibodies, serological reactions, their underlying principles, and
their diagnostic applications are emphasized. Through laboratory experiments, students appreciate the
functioning of a diagnostic laboratory.
DO 5060 Pathology (2.5 credit hours, Numeric Score)
This course presents the basic pathogenesis and morphology of disease. Cell injury and death,
inflammation, the repair process, hemodynamic changes, neoplasia, and chemical and physical injuries are
discussed. The laboratory is designed to supplement the lectures, utilizing various instructional
technologies. Lectures on introductory laboratory medicine are presented.
DO 5070 Pharmacology (2.5 credit hours, Numeric Score)
This course orients medical students to the effects of drugs on biological systems. The course deals
initially with general principles in pharmacology, including drug absorption, distribution, action, toxicity,
biotransformation and elimination. The course then focuses on chemotherapeutic agents used in treating
infectious diseases. Concepts and principles are introduced that are vital for the rational evaluation and
utilization of drugs in the practice of osteopathic medicine.
DO 5080 Physiology (1.5 credit hours, Numeric Score)
This course presents the general physiology of cells, with a special emphasis on excitable cells such as
the neuron and muscle cell. Basic concepts on the functions of cells and control of cellular activities are
reviewed. The course provides a foundation for the first-year medical student in basic physiologic theory,
organ and system function, and an appreciation of total-body physiology.
DO 5090 Osteopathic Principles and Practice (2 credit hours, Numeric Score)
This course presents osteopathic history, philosophy, principles, problem-solving and patient
management, incorporating direct and indirect, traditional, and contemporary manipulative techniques.
61
DO 5110 Dermal System (3.5 credit hours, Numeric Score)
This course presents problems of the skin from a clinical perspective. Lectures are coordinated with
embryology, histology, physiology, biochemistry, pharmacology, microbiology, pathology, and
dermatopathology.
DO 5120 Neurosensory System (15.5 credit hours, Numeric Score)
This course presents basic understandings of the brain, spinal cord, and peripheral nervous system. Basic
science topics include embryology, histology, neuroanatomy, biochemistry, physiology, and pharmacology.
Clinical topics include infections of the nervous system, pathology, neurology, ophthalmology,
otorhinolaryngology, overviews of sleep disorders, cerebrovascular disorders, aging, and dementia.
DO 5130 Musculoskeletal System (6.5 credit hours, Numeric Score)
This course presents common conditions and disorders of the musculoskeletal system. The course also
presents embryology, histology, and functional anatomy—including kinesiology, biochemistry,
pharmacology, physiology, and microbiology. The pathology and clinical aspects of this system are
discussed, as are the related aspects of sports medicine, rehabilitative medicine, exercise, rheumatoid
diseases and orthopedics. Focus is on the relevance of these topics to the primary care practice of
osteopathic medicine.
DO 5140 Medical Ethics (0 credit hours, Cr/NCr)
This course is an introduction to the ethical principles and methods of analysis used in medical ethics.
The course presents a systematic framework for resolving ethical dilemmas encountered in the practice of
medicine. Medical Ethics is covered in Phases II and III.
DO 5150 Introduction to Clinical Medicine I (ICM I) (2 credit hours, Numeric Score)
The Introduction to Clinical Medicine sequence prepares students for clinical rotations. This preparation
emphasizes doctor-patient communication and clinical skills. ICM-I is designed to introduce the clinical
skills that are essential to becoming an osteopathic physician. This introductory course is presented during
the MS I year. Students are presented with basic history taking and physical examination skills. The course
emphasizes the cognitive and affective skills needed for clinical reasoning and for effective doctor-patient
communication. Utilizing both actual and simulated patients, verbal and non-verbal communication
techniques are illustrated.
DO 5160 Behavioral Science and Substance Abuse (4 credit hours, Numeric Score)
This course presents biological, psychological, and social aspects of behavior in relation to medical
practice. Major topics include etiology and treatment of substance abuse, the physician-patient relationship,
emotion and personality, etiology of gender identity and sexual orientation, evolutionary origins of
behavior, genetic, and environmental aspects of behavioral disorders. The course addresses how patients’
behaviors contribute to their health and/or disease. The physician’s role in the education of, and behavior
change in, patients, peers, and the community are also discussed.
DO 5190 Osteopathic Principles and Practice II (2.5 credit hours, Numeric Score)
Continuation of DO 5090.
DO 6010 Blood and Reticuloendothelial System (6.5 credit hours, Numeric Score)
This course presents the embryology, histology and biochemistry of the hemopoietic and
lymphoreticular organs. During this system, the influences of microbiologic and pharmacologic agents are
discussed. Basic immunology, the mechanisms of immunologic injury and immune tolerance,
transplantation, tumor immunology, and the immunodeficiency states are also covered. The pathology and
clinical aspects of hematologic diseases and diseases of the lympho-reticular system are presented along
with the pertinent laboratory tests. Laboratory experience provides opportunities to examine normal and
abnormal blood smears, perform blood tests, and examine lymph node neoplasms.
62
DO 6020 Cardiovascular System (9.5 credit hours, Numeric Score)
This course presents the embryology, histology, and gross anatomy of the heart and blood vessels. The
biochemistry, pharmacology, physiology, and microbiology as related to this system are also discussed.
Cardiovascular pathologies are presented, along with the clinical diagnostic and treatment modalities.
DO 6030 Public Health (1.5 credit hours, Numeric Score)
This course presents an understanding of public health and its importance to the practicing physician.
Epidemiology, community health, immunization procedures, communicable disease control, environmental,
and occupational health are discussed. Interaction of the physician with public health agencies is stressed, as
are skills in working with public health statistics.
DO 6040 Respiratory System (9 credit hours, Numeric Score)
This course presents the embryology, histology, and gross anatomy of the lungs and
nasotracheobronchial tree. Respiratory physiology and defense mechanisms, as well as microbiology,
biochemistry, and pharmacology relating to the system are discussed. Pathology of the upper and lower
respiratory system is presented along with clinical presentations of diagnostic and treatment modalities.
DO 6050 Psychiatry (2 credit hours, Numeric Score)
This course builds upon the bio-psycho-social foundation presented during Behavioral Science. Major
DSM-IV diagnoses will be explored. Implications for medical practice will be emphasized. The course
develops the physician's ability to recognize and deal with, or to refer, specific psychiatric cases.
Perspectives on the use of ancillary personnel, and on cooperating with psychiatrists, are presented.
DO 6090 Osteopathic Principles and Practice III (2.5 credit hours, Numeric Score)
Continuation of DO 5190.
DO 6110 Renal System (5 credit hours, Numeric Score)
This course presents basic science topics in embryology and histology of the kidneys and urinary system,
the biochemistry, physiology, and pharmacology of fluid and electrolyte balance with emphasis on kidney
function, microbiology, pharmacology. Clinical topics include management of urinary infections, and the
identification, diagnosis, and treatment of renal and urinary disorders.
DO 6120 Endocrine System (5.5 credit hours, Numeric Score)
This course explores the anatomy of the hormone secreting glands, the biochemical description of a
hormone, how hormones are studied and measured, and the physiology of homeostasis. Pathologies of the
endocrine system and the pharmacology of endocrine drugs are presented. Clinical manifestations of
endocrine disorders of various ages are presented, with emphasis on identification, diagnosis, and treatment.
The course also considers the evaluation and management of endocrine emergencies.
DO 6130 Reproductive System (7 credit hours, Numeric Score)
This course presents the anatomy, embryology, and histology of both the female and male reproductive
systems. The physiology, biochemistry, pathology, pharmacology, and microbiology of both reproductive
systems are also discussed. In addition, the basic science disciplines present principles regarding the
relationships between mother and fetus during pregnancy. Clinical lectures on obstetrics, gynecology,
perinatology, and nutrition, and the problem of child abuse and the management of pregnancy, are
presented. Perspectives on human sexuality are also presented.
DO 6140 Gastrointestinal System (11 credit hours, Numeric Score)
This course presents various aspects of the gastrointestinal system, including its embryology and
histology. The biochemistry, physiology, the influence of pharmacology, and the problems with
microbiology are presented along with the clinical and pathological aspects of the system. The nutrition
course is incorporated into this system.
63
DO 6150 Introduction to Clinical Medicine II (0 credit hours, Cr/NCr)
This course presents opportunities to practice clinical patient assessment skills during the pre-clinical
phase of medical education. These clinical experiences provide the opportunity to learn the skills, values,
and attitudes essential for the development of compassionate osteopathic physicians. ICM-II is taught in
conjunction with each major system. All ICM segments are aligned with the system being presented
concurrently in the curriculum. ICM-II is required for promotion to the clinical phase.
DO 6160 Medical Jurisprudence (1.5 credit hours, Numeric Score)
Using California laws as a base, this course presents the general rules of medical practice. The
obligations of the physician to the community, the patient, the hospital, colleagues, and society are
explored. The course discusses the physician’s duties and responsibilities in the context of the medical,
legal, and ethical aspects of medicine. Standards of care, vicarious liability, and negligence are discussed.
Additional symposia are conducted during the Essentials of Family Medicine courses in Phase III of the
curriculum.
DO 6171 Differential Diagnosis (0 credit hours, Cr/NCr)
This course provides students with exposure and practice in case presentations and in the application of
differential diagnosis skills to selected problems in formulating evaluation or therapeutic intervention plans.
Facilitators provide for case-based clinical thinking and experience to assist students in developing these
skills. This course prepares students for conducting case presentations during clinical rotations, and for
demonstrating skill in case evaluation and management. The course is integrated with each of the systems.
DO 6172 Emergency Medicine (0 credit hours, Cr/NCr)
This course is taught during the systems in Phase II, with subsequent lectures interspersed within Phase
III. The course presents the basics of emergency medicine. Areas covered are physical and emotional
trauma, poisonings, the paramedic system, and emergency cases from various areas of clinical medicine as
they relate to a given body system.
DO 6173 Geriatrics (0 credit hours, Cr/NCr)
This course provides supervised clinical education in geriatrics, which may be provided in the nursing
home, hospital inpatient ward, outpatient clinic, private home, or assisted living setting. Students will gain
knowledge in clinical management, interpretation of diagnostic data, patient education, development of
diagnostic and management plans, procedural skills, inter-professional communication, and skills related to
working within a multidisciplinary team.
DO 6174 Human Sexuality (0 credit hours, Cr/NCr)
This course promotes student understanding of human sexuality by presenting issues related to both
normal and dysfunctional sexuality. Taught as a segment of the Reproductive System (DO 6130), the course
covers human sexuality issues, including the anatomy and physiology of reproduction, pathology, normal
sexual response, and psychosexual development throughout the life cycle. The theory and practice of
treatment for sexual dysfunction are considered. Current therapeutic concepts and techniques are discussed,
along with case reviews, which include diagnosis, treatment plans, and prognosis.
DO 6175 Nutrition (0 credit hours, Cr/NCr)
This course provides the basic information on which to evaluate the nutritional requirements of the body
in health and disease. A review of vitamins and their indications and limitations, the use and need for the
trace minerals, and the proportions of carbohydrates, fats, and proteins in a balanced diet are discussed.
Clinical nutrition is emphasized. This course is presented during the Gastrointestinal System (DO 6140).
DO 6176 Pediatrics (0 credit hours, Cr/NCr)
This course is devoted to the special problems of childhood. These subjects are integrated during Phase
II in each system as appropriate. All systems contain an element of pediatrics and this course is designed to
cover those aspects that are particular to pediatrics (infancy to adolescence). Additional pediatric
presentations are given in Phase III during the Essentials of Family Medicine courses.
64
DO 6190 Osteopathic Principles and Practice IV (2.5 credit hours, Numeric Score)
Continuation of DO 6090.
DO 7010 Family Practice I (10 credit hours, Letter Grade)
This course provides supervised clinical education in family medicine, including clinical management,
technical and procedural skills, interpretation of diagnostic data, patient education, development of
diagnostic and management plans, and inter-professional communication. In subsequent courses in this
series, students are exposed to progressive involvement and independence in patient management.
Repeatable to a maximum of 20 credit hours.
DO 7020 Internal Medicine I (10 credit hours, Letter Grade)
This course provides supervised clinical education in general internal medicine including clinical
management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and inter-professional communication. In subsequent
courses in this series, students are exposed to progressive involvement and independence in patient
management.
DO 7021 Internal Medicine II (10 credit hours, Letter Grade)
Prerequisite: DO 7020. Continuation of DO 7020.
DO 7022 Internal Medicine III (10 credit hours, Letter Grade)
This course provides supervised clinical education in general internal medicine and/or in an internal
medicine subspecialty such as gastroenterology, pulmonology, or cardiology. Expected competencies
include clinical management, technical and procedural skills, interpretation of diagnostic data, patient
education, development of diagnostic and management plans, and inter-professional communication. In
subsequent courses in this series, students are exposed to progressive involvement and independence in
patient management. Prerequisite: DO 7020. Repeatable to a maximum of 20 credit hours.
DO 7030 Surgery I (General) (10 credit hours, Letter Grade)
This course provides supervised clinical education in general surgery including clinical management,
technical and procedural skills, interpretation of diagnostic data, patient education, development of
diagnostic and management plans, and inter-professional communication. In subsequent courses in this
series, students are exposed to progressive involvement and independence in patient management.
DO 7050 Elective (10 credit hours, Letter Grade)
This course provides supervised clinical education in one of the clinical disciplines including clinical
management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and inter-professional communication. The discipline
and clinical training site must be approved in advance by the Office of Rotations.
DO 7060 Osteopathic Manipulative Medicine (10 credit hours, Letter Grade)
This course provides supervised clinical education in osteopathic manipulative medicine including
clinical management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and inter-professional communication.
DO 7070 Pediatrics (10 credit hours, Letter Grade)
This course provides supervised clinical education in pediatrics including clinical management,
technical and procedural skills, interpretation of diagnostic data, patient education, development of
diagnostic and management plans, and inter-professional communication. Repeatable to a maximum of 20
credit hours.
DO 7080 Psychiatry (10 credit hours, Letter Grade)
This course provides supervised clinical education in psychiatry including clinical management,
technical and procedural skills, interpretation of diagnostic data, patient education, development of
65
diagnostic and management plans, and inter-professional communication. Prerequisite: DO 7010 or DO
7020.
DO 7090 Obstetrics/Gynecology (10 credit hours, Letter Grade)
This course provides supervised clinical education in obstetrics/gynecology including clinical
management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and inter-professional communication. Prerequisite: DO
7010 or DO 7020. Repeatable to a maximum of 20 credit hours.
DO 7100 Geriatrics (10 credit hours, Letter Grade)
This course provides supervised clinical education in geriatrics including clinical management, technical
and procedural skills, interpretation of diagnostic data, patient education, development of diagnostic and
management plans, and inter-professional communication.
DO 7510 Family Practice II (10 credit hours, Letter Grade)
Prerequisite: DO 7010. Continuation of DO 7010.
DO 7520 Internal Medicine IV (10 credit hours, Letter Grade)
This course provides supervised clinical education in general internal medicine and/or in one of the
internal medicine subspecialties such as gastroenterology, pulmonology, neurology, or cardiology. Expected
competencies include clinical management, technical and procedural skills, interpretation of diagnostic data,
patient education, development of diagnostic and management plans, and inter-professional communication.
In subsequent courses in this series, greater involvement and independence in patient management are
expected. Prerequisite: DO 7021 and 7022.
DO 7521 Internal Medicine V (10 credit hours, Letter Grade)
This course provides supervised clinical education in general internal medicine and/or in an internal
medicine subspecialties such as gastroenterology, pulmonology, neurology, or cardiology. Expected
competencies include clinical management, technical and procedural skills, interpretation of diagnostic data,
patient education, development of diagnostic and management plans and inter-professional communication.
Prerequisite: DO 7520.
DO 7530 Surgery II (10 credit hours, Letter Grade)
This course provides supervised clinical education in general surgery or one of the surgical
subspecialties such as ophthalmology, orthopedics, urology or cardiovascular/thoracic. Expected
competencies include clinical management, technical and procedural skills, interpretation of diagnostic data,
patient education, development of diagnostic and management plans, and inter-professional communication.
In subsequent courses in this series, greater involvement and independence in patient management are
expected. Prerequisite: DO 7030.
DO 7540 Emergency Medicine (10 credit hours, Letter Grade)
This course provides supervised clinical education in emergency medicine including clinical
management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and inter-professional communication. Prerequisite: DO
7010 or DO 7020.
DO 7550 Elective (10 credit hours; repeatable to a maximum of 50 credit hours, Letter Grade)
This course provides supervised clinical education in one of the clinical disciplines including clinical
management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and inter-professional communication. The discipline
and clinical training site must be approved in advance by the Office of Rotations.
DO 8050 Essentials of Family Medicine I (EFM-I) (3.5 credit hours, Letter Grade)
The Essentials of Family Medicine-I course is taken during the MS III year and serves as a review of,
and assessment tool for, basic clinical knowledge. This program reviews and amplifies clinical material
66
presented during the MS I and MS II years. It also provides the opportunity for the student to obtain
information and skills essential to rotations, residency, and medical practice. Topics include clinical, legal
and ethical issues that are presented from a primary care perspective. Additionally, the course addresses
special topics such medical professionalism, cultural sensitivity, and alternative healthcare. Throughout the
course, the tools essential to becoming a competent practicing physician and lifelong learner are
emphasized. Guided learning is accomplished through on-line projects that enable students to demonstrate
competence in completing clinically-oriented problems and case scenarios. Information may also be
presented through one or more on-campus sessions held on designated weekends. Participation in the on-
line projects and attendance at on-campus session(s) are mandatory. EFM-I must be successfully completed
in order for the student to be advanced to MS IV status.
DO 8550 Essentials of Family Medicine II (EFM-II) (3.5 credit hours, Letter Grade)
Essentials of Family Medicine-II builds upon the essential knowledge and skills learned during the
student’s first three years of Osteopathic medical school, with the goal of helping the student to be able to
successfully transition into his or her post-graduate training program and future medical practice. This is
accomplished by enabling the student to apply general knowledge to specific clinical applications. In
addition, EFM-II emphasizes medical professionalism and helps the student to sharpen skills vital to
lifelong learning. Information is presented through one or more on-campus sessions held on designated
weekends. Guided learning is also accomplished through on-line projects that enable students to
demonstrate competence in completing clinically-oriented problems and case scenarios. Attendance at the
on-campus session(s) and participation in the on-line projects are mandatory. Successful completion of
EFM-II is a requirement for graduation.
HONORS AND AWARDS
The following awards for DO students are presented annually on Honors Day in April:
Provost’s Student Government Award
Dean’s Award
William G. Woodman, MD, Humanitarian Memorial Award
Russell B. McCaughan Award
Neocortex Award
William G. Stahl, DO, FACOS, Memorial Scholarship
Anthony Joseph Ronzo, Sr., Memorial Award
Auxiliary to the Osteopathic Physicians and Surgeons of California Scholarship Award
COMP Western University Service Award
Community Clinic Service Award
Class of 1989 Award
McGraw-Hill Award
Joseph and Dorothy Gendron Journalism Award
Dr. V. Gladys Shutt Memorial Award
Richard E. Eby Leadership Scholarship
Mickey and Nell Clamage Memorial Scholarship Award
Roy G. and Marion L. Kramer Endowment Fund Award
Muriel Chapman, DO, Memorial Award
Robert W. Finegan Memorial Award
Jeff Plumb Memorial Award
The President’s Society Award
Dr. Alex M. Rene Memorial Scholarship Award
Linda Fox Memorial Endowment Fund Award
Louise Kramer Memorial Scholarship Award
Guy M. Allmon Scholarship Fund Award
Glen Scheresky Memorial Scholarship Award
American Association of Colleges of Osteopathic Medicine
Council of Student Council Presidents Student DO of the Year Award
Dr. Sheila Xenos Memorial Award
Osteopathic Physicians and Surgeons of California Matthew L. Weyuker Scholarship Award
67
The following awards are presented annually to graduates at Commencement:
President’s Award
Dean’s Award
Gate Pharmaceutical Student Award
Edward B. Parris and Jacqueline A. Parris Award
Dr. Frank T. Carr Memorial Award
Steven W. Dyer Memorial Award
Janet M. Glasgow Memorial Achievement Citation of the American Medical Women’s Association
American College of Osteopathic Family Physicians Award
Pauline Weiss Pumerantz Memorial Award
Richard H. and Anna Kaiser Memorial Award
New Mexico Osteopathic Medical Association Foundation for Osteopathic Education and
Professional Development Award for Academic Excellence
Osteopathic Physicians and Surgeons of California Award
Shirley Jane Watters Memorial Award
Rev. & Mrs. Al and Verna Braswell Award
Leonard E. Peck, Sr., Memorial Award
Phoenix Award
Charles Vowels, MD, Memorial Award
Alumni Memorial Award
Society of Academic Emergency Medicine Excellence in Emergency Medicine Award.
James R. Sawrey Memorial Award
Dr. Alex M. Rene Memorial Award
National American Osteopathic Foundation: The Donna Jones Moritsugu Memorial Award
68
ACADEMIC CALENDAR 2002-2003
DO PROGRAM
Friday, May 24, 2002
Fall Semester Registration Forms Due (4
th
years)
Friday, May 10, 2002
Fall Semester Registration Forms Due (3
rd
years)
Friday, May 17, 2002
Fall Semester Registration Ends (2
nd
years)
Tuesday, Wednesday, Jun. 4-5, 2002
NBOME COMLEX Level 1
Thursday, Jun. 6, 2002
ISAC Registration Forms Due
Monday, Jun. 10, 2002
Fall Semester Tuition Due (ISAC Students)
Tuesday, Wednesday, Jun. 11-12, 2002
NBOME COMLEX Level 3
Friday, Jun. 14, 2002
ISAC Orientation
Monday, Jun. 17, 2002
ISAC Begins
Monday, Jun. 17, 2002
Fall Semester Rotations Begin (3
rd
& 4
th
years)
Fall Semester Tuition Due (3
rd
& 4
th
years)
Thursday, Jul. 4, 2002
Independence Day
Friday, Jul. 5, 2002
Campus Closed (no classes)
Friday, Jul. 26, 2002
Fall Semester Registration (1
st
years)
Wed.-Fri., Aug 7-9, 2002
Orientation
Thursday, August 8, 2002
Fall Semester Tuition Due (1
st
& 2
nd
years)
Saturday, Aug. 10, 2002
Convocation/White Coat Ceremony
Monday, Aug. 12, 2002
Classes Begin (1
st
and 2
nd
years)
Tues.-Wed., Aug. 27-28, 2002
COMLEX Level 2
Monday, Sept. 2, 2002
Labor Day - no classes
Monday, Oct. 14, 2002
Columbus Day - no classes
Tuesday, Wednesday, Oct. 15-16, 2002
COMLEX Level 1
Monday, Nov. 11, 2001
Spring Semester Tuition Due (4
th
years)
Spring Semester Rotations Begin (4
th
years)
Wednesday, Nov. 27, 2002
Thanksgiving Recess – Noon
Monday, Dec. 2, 2002
Classes Resume (1
st
& 2
nd
years)
Spring Semester Tuition Due (3
rd
years)
Friday, Dec. 6, 2002
Last Day of Fall Semester Rotations (3
rd
years)
Monday, Dec. 9, 2002
Spring Semester Rotations Begin (3
rd
years)
Tuesday, Wednesday, Dec. 10-11, 2002
COMLEX Level 3
Friday, Dec. 20, 2002
Last Day of Fall Semester Classes (1
st
and 2
nd
years)
Spring Semester Tuition Due (1
st
and 2
nd
years)
Monday, Dec. 23, 2002
Winter Recess Begins
Monday, Jan. 6, 2003
Spring Semester Begins (1
st
& 2
nd
years)
Tuesday, Wednesday, Jan. 14-15, 2003
COMLEX Level 2
Monday, Jan. 20, 2003
Martin Luther King Holiday - no classes
69
Monday, Feb. 17, 2003
President’s Day - no classes
Friday - Sunday, Feb. 28-Mar. 2, 2003
On-campus EFM Weekend (4
th
years)
Monday, Mar. 17, 2003
Spring Vacation Begins
Monday, Mar. 24, 2003
Classes Resume
Monday, Apr. 14, 2003
Honors Day
Friday, Apr. 25, 2002
Last Day of Classes (4
th
years)
Friday, May 16, 2003
Last Day of Classes (2
nd
year)
Friday, May 23, 2003
Last Day of Classes (1
st
year)
TBA
Commencement
Tuesday, Wednesday, Jun. 3-4, 2003
COMLEX Level 1
Tuesday, Wednesday, Jun. 10-11, 2003
COMLEX Level 3
70
THE OSTEOPATHIC OATH
I do hereby affirm my loyalty to the profession I am about to enter. I will be mindful always of my great
responsibility to preserve the health and life of my patients, to retain their confidence and respect both as a
physician and a friend who will guard their secrets with scrupulous honor and fidelity, to perform fruitfully
my professional duties, to employ only those recognized methods of treatment consistent with good
judgment and with my skill and ability, keeping in mind always nature’s laws and the body’s inherent
capacity for recovery. I will be ever vigilant in aiding the general welfare of the community, sustaining its
laws and institutions, not engaging in those practices which will in any way bring shame or discredit upon
myself or my profession. I will give no drugs for deadly purposes to any person, though it be asked of me. I
will endeavor to work in accord with my colleagues in a spirit of progressive cooperation and never by
word or by act cast imputations upon them or their rightful practices. I will look with respect and esteem
upon all those who have taught me my art. To my college I will be loyal and strive always for its best
interests and for the interests of the students who will come after me. I will be ever alert to further the
application of basic biologic truths to the healing arts and to develop the principles of osteopathic medicine
as taught by my profession. In the presence of this gathering I bind myself to my oath.
71
COLLEGE OF PHARMACY
Doctor of Pharmacy Program
ACCREDITATION
The College of Pharmacy is accredited by the American Council on Pharmaceutical Education.
PHARMACY: ABOUT THE PROFESSION
The practice of pharmacy has evolved from a historical emphasis on the preparation and distribution of
drug products to new activities and responsibilities that focus on the rational, safe and cost-effective use of
drugs. Just as it is generally assumed that physicians are primarily involved in providing medical care and
nurses in providing nursing care, pharmacists are the primary providers of pharmaceutical care. The mission
of the pharmacy profession, therefore, is to meet the pharmaceutical care needs of the public.
Pharmaceutical care is patient-centered, outcome-oriented, contemporary pharmacy practice that requires
the pharmacist to work in concert with the patient and the patient's other health care providers to promote
health, prevent disease, and assess, monitor, initiate and modify medication use so that pharmacotherapy is
safe and effective.
The provision of pharmaceutical care to patients requires an understanding of the chemistry of drug
entities, the delivery characteristics of dosage formulations, the disposition of drugs within the body, the
physiologic and pharmacologic outcome of drugs' interactions with the human body and the social systems
in which medications are used.
As a pharmacist you will be able to care for your patients in many important ways:
• Participate in the planning and implementation of effective drug therapy.
• Monitor and evaluate drug therapy to identify and solve patient-specific drug therapy problems.
• Evaluate clinical literature.
• Prepare medications.
• Select the drug product dosage form.
• Calculate the dose and determine the dosing schedule.
• Educate and counsel patients, and;
• Work with other health care providers and the patient to promote health and prevent disease.
THE DEGREE
The Doctor of Pharmacy degree (PharmD) is awarded in recognition of the highest level of professional
education in pharmacy in the United States. To earn the PharmD degree, students complete four years of
professional study following a minimum of two years of preprofessional education at an accredited college
or university.
Students who complete this program are eligible to take state pharmacy licensing examinations. After
passing this examination, graduates are licensed to perform all the duties and responsibilities of a practicing
pharmacist.
CAREER OPPORTUNITIES
Our graduates find a vast array of exciting career pathways open to them. The opportunities below
represent only a small list of possible career options.
Community Practice
Pharmacy offers a variety of professional opportunities in the community setting. Independent
pharmacies, corporately owned pharmacies and neighborhood health care clinics all provide opportunities
for direct patient care. Other examples of community practice include specialized home health care,
consulting for nursing home patients and conducting patient education programs.
72
Institutional Practice
Pharmacists in hospitals and other health care institutions may be involved in direct patient care,
teaching, drug use evaluation, clinical research studies, public service and administration.
Managed Care Pharmacy
Pharmacists practice in a variety of managed care organizations including health maintenance
organizations and preferred provider organizations. In these settings, pharmacists develop formularies,
implement drug utilization reviews and analyze physician prescribing patterns.
Pharmaceutical Companies
Research and development, testing of drugs in humans, production, quality control, marketing, public
relations, sales, and management are some of the career opportunities available in industry.
Public Service Practice
Pharmacists practice in federal government agencies and services including the Food and Drug
Administration (FDA); Drug Enforcement Administration (DEA); the Army, Navy and Air Force; Public
Health Service; and Department of Veterans Affairs.
Academia
Opportunities for careers in colleges or schools of pharmacy include administration, teaching, research
and clinical service. Additional opportunities in teaching, research, or practice may required post-graduate
education or training beyond the doctor of pharmacy degree.
THE COLLEGE OF PHARMACY
A major goal of the College of Pharmacy is to prepare competent and caring practitioners. We are
prepared to offer you a quality educational experience.
Modern Facilities
You will receive instruction in a modern facility with classrooms and breakout rooms furnished with
state-of-the-art equipment.
A Friendly Environment
You will be treated as a colleague and a professional who is seeking to become a competent pharmacy
practitioner.
Supportive Faculty
You will receive instruction from faculty members who are committed to excellence in pharmaceutical
education. Many faculty members are practicing clinical pharmacists who are actively providing primary
care or consultative services to patients in a variety of practice settings.
A Rich Student Life
You will have an opportunity to participate in a number of professional pharmacy organizations as well
as other school-wide activities.
ACADEMIC COURSE WORK
To obtain the PharmD degree you will complete a curriculum that contains both didactic and clinical
components.
The Didactic Component
In the core didactic component of the program, you will learn about biological systems and about drugs
and their effect on the body. You will take courses in areas such as therapeutics, health care administration,
pharmacology and pharmacokinetics and learn how to apply this knowledge to pharmacy practice. Your
studies will include communication skills, patient counseling, laws about drugs and pharmacy practice,
health care systems, physical assessment and evaluation of the drug literature.
73
The Clinical Training Component
In several different patient-centered training sessions, particularly during the third and fourth years, you
will be given an opportunity to put into practice what you have learned in the classroom. Under the
supervision of a clinical pharmacist faculty member, you will assess and counsel patients and monitor their
drug therapies. You will spend a total of 42 weeks in these training sessions, called advanced pharmacy
practice experiences. Such pharmacy practice experiences will take place in hospitals as well as in clinics,
community pharmacies and other settings where pharmacists practice.
ADMISSIONS POLICIES AND PROCEDURES
Admission to the College of Pharmacy is on a highly competitive basis. Each year we receive many
more applications than we can accommodate in our program. At Western University, we retain smaller class
sizes, offering you a closer relationship with your faculty and fellow students. The College of Pharmacy is
looking for individuals who have excellent communication skills, who care for people and are
compassionate, who are dedicated and determined, who are dependable and who display good judgment.
Application Requirements
The College of Pharmacy Admissions Committee will consider applicants with a minimum of two years
of college (60 academic semester hours or 90 quarter hours) of pre-pharmacy study at an accredited college
or university. The minimum cumulative prepharmacy and science grade point average requirement is 2.5.
Grades of "C-" in any of the prerequisite courses are not accepted. Prerequisite courses are subject to
review each year. For the latest information, you should consult our web site at www.westernu.edu.
1. Prerequisite Courses
College English (1 semester)
English Composition (1 semester)
Speech Communication (1 semester)
General Chemistry with lab (2 semesters)
Organic Chemistry with lab (2 semesters)
Human Anatomy with lab* (1 semester)
Human Physiology with lab* (1 semester)
Microbiology with lab-Medical Microbiology is preferred (1 semester)
Calculus (1 semester)
Electives (2 semesters)-Electives must be met from two of the three following areas: public
speaking/debate, social sciences, or economics.
*If anatomy and physiology are combined, we will accept a minimum of 5 semester units. Anatomy and
physiology must be taken out of the anatomy, physiology, A&P, biology or zoology departments.
We do not accept substitutions or waive any of the prerequisite courses. English as a Second Language
(ESL) courses are not accepted for the English requirement. All prerequisite course work in progress must
be completed no later than the spring semester or quarter immediately preceding matriculation.
2. Test of English as a Foreign Language (TOEFL)
TOEFL (including essay) is required for all applicants submitting course work from foreign schools, and
all permanent and temporary residents of the United States. EXCEPTION: The TOEFL exam will be
waived for students graduating with a confirmed baccalaureate or higher degree from a United States
institution at the time of application. A minimum score of 550 on the paper based test or 213 on the
computer-based test is required. TOEFL scores must be submitted at the time of application. TOEFL
scores are valid for 2 years.
3. Recommendations
Three satisfactory recommendations (forms are provided by the College) are required as part of the
admissions application. The recommendations should state the nature and extent to which the
recommender knows you and should elaborate on the applicant's attributes and abilities including
communication skills, ethics, interpersonal skills, motivation toward the profession and maturity.
74
Application Procedures and Deadlines
Candidates may obtain an application as early as August of the academic year preceding the year in
which they plan to matriculate. Applicants are considered without regard to race, color, national origin, age
or gender. Western University strives to accommodate individuals with disabilities. The application
postmark deadline for the class entering in the fall is December 1 of the preceding year.
To request an information brochure and/or an application, contact the Admissions Office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 623-6116
In addition to submitting a completed application, the applicant must submit a non-refundable
application fee of $60, three letters of recommendation, an academic/professional record form, must
complete a personal questionnaire (form provided by the University) and submit official transcripts from all
colleges attended. All application materials are to be included in the application packet. After receipt of the
packet, the Admissions Office will evaluate the applicant's transcripts to ascertain that all prerequisite
courses have been completed and that the applicant's cumulative GPA is satisfactory. Applicants who wish
to use course work completed outside of the United States must submit their transcripts for evaluation to
World Education Services or Josef Silny and Associates. A course-by-course evaluation is required and all
course work must be designated as undergraduate, graduate, or professional. Western University will only
honor evaluations from one of the above services. The evaluation must be included with the application
packet.
Faculty in the College of Pharmacy will screen each applicant's admissions file to determine whether or
not an applicant will be granted an on-campus interview. Candidates selected for an interview will
participate in an assessment of written and verbal communication skills. Interviews are typically held in
January and February. Decisions of the Admissions Committee regarding the admission of applicants to the
Doctor of Pharmacy program are final.
TUITION AND FEES
In estimating costs for one academic year of study at Western University's College of Pharmacy, you
should include tuition and fees, laptop computer and printer, books and supplies, room and board, and other
miscellaneous expenses. Actions of the Board of Trustees setting tuition and fees for the academic year are
established during the previous spring term. The most current tuition and fees are as follows:
• Tuition - $26,915 in 2002-2003 Academic Year.
• Mandatory fees specific to the College of Pharmacy will be provided separately.
• Application Fee - Non-refundable $60 fee for those applying to the Western University College of
Pharmacy.
• Enrollment Deposit- $500 for students admitted to the College of Pharmacy. Upon enrollment, this
deposit is applied toward the tuition for the academic year. Persons who fail to
enroll forfeit the entire deposit.
Other Fees
$30 (per day) Late Registration Fee
$40 Lost Mail Locker Key
$5 (each) Copy of Official Transcript
$10 (each) Copy of Official Transcript Faxed
$10 Lost ID Badge
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
75
The College of Pharmacy requires that each enrolled student have a notebook or laptop computer during
class, after class hours and while on rotations.
FINANCIAL ASSISTANCE
All PharmD students are eligible to apply for need-based financial aid. For information, please write to
the Financial Aid Office, Western University of Health Sciences, 309 E. Second Street, Pomona, California
91766-1854
ACADEMIC POLICIES AND PROCEDURES
Grading Policy
Students are required to meet a specified set of outcome objectives in each block in the curriculum. The
block facilitator will provide the student with a syllabus at the beginning of the block that includes the
required outcome objectives, instructional methods, assessment methods, a day-by-day schedule, and
grading criteria. Achievement of the outcome objectives will be assessed through individual quizzes,
examinations, and individual performance on any assignments given in that block. The minimum passing
score (P) in any block is 80%. Students who earn a grade of 90% or higher will receive a grade of “high
pass” (HP). A student who fails to meet the minimum requirement of 80% will receive a grade of “no pass”
(NP) and will be automatically placed on academic probation (see Probation below). Policies requiring
remediation of failed blocks are set forth under Failure to Meet Standards, below. All recorded grades
will remain on the official transcript except in cases where clerical errors have occurred. The grading
policies for the professional practice component of the curriculum (the Introductory Professional Practice
Experience [IPPE], the Advanced Pharmacy Practice Experiences [APPE] and the Advanced Electives
[AEs]) are set forth in separate policies.
Grading procedures
Block grades: end of block grades will be assigned as follows:
HP = High Pass; a student has achieved a minimum of 90%.
P = Pass; a student has achieved a minimum of 80%.
NP = No Pass; indicates the student has not achieved the minimum of 80% in
the block (See Failure to Meet Standards section).
NP/P = Indicates a student has successfully remediated a block. The “NP” will
remain on the student’s transcript.
I = Incomplete (Refer to the policy on Attendance and Absences).
I/P = Indicates a student has successfully completed a block following receipt
of an incomplete grade. The “I” will remain on the student’s transcript.
I/NP = Indicates a student has unsuccessfully completed a block following
receipt of an incomplete grade.
M = Missing
W = Withdrawal (Refer to the General Academic Policies and Procedures
above).
Advanced Pharmacy Practice Experiences (APPE)/Advanced Electives (AE) grades will be assigned as
follows:
P = Pass.
NP = No Pass; student has not achieved the rotation outcomes.
NP/P = Indicates a student has successfully remediated APPE/AE. The NP will
remain on the student’s transcript.
I = Incomplete (Refer to the policy on Attendance and Absences and on
Student Progress).
I/P = Indicates a student has successfully completed an APPE/AE following
receipt of an incomplete grade. The “I” will remain on the student’s
transcript.
I/NP = Indicates a student has unsuccessfully completed an APPE/AE
76
following receipt of an incomplete grade.
M = Missing
W = Withdrawal (Refer to the General Academic Policies and Procedures
above).
Credit hours
To be eligible for graduation, a student must complete the following required components of the Doctor
of Pharmacy program:
Year # of Credits per year
1 40
2 40
3 44
4 50
Total 174
Learning Assurance
Competency-based education provides students opportunities to achieve block outcomes, thus, learning
assurance will be provided in each block. Block faculty will work with students to help them achieve the
required standards as stated in the block syllabus. Assessment methods are intended to ensure that
outcomes are met, and if not, they are to be used as a means of assessing the area(s) of difficulty. Various
methods will be employed to help students via the block syllabus. If additional points are assessed for any
assignment or examination for which learning assurance has been provided, the actual numerical score will
be recorded as no greater than 80%.
Failure to Meet Standards
Students who fail to achieve the 80% standard in a block will be given a grade of “NP” and will be
placed on academic probation automatically by the Dean (See General Academic Policies and
Procedures on Probation). Students who receive a designation of “NP” in up to two blocks during one
academic year will be required to enroll for remediation for each block for which a grade of “NP” has been
recorded. Block remediation may include a variety of activities such as faculty-student conferences,
independent study and other types of coursework. However, in all cases, a final comprehensive remediation
examination will be required to demonstrate successful attainment of the required standards. It is the
student’s responsibility to prepare for the comprehensive remediation examination and other assigned
coursework that may be required. Students will be required to pay a fee of $250 for each block remediated.
The Academic Performance and Standards Committee will coordinate the block remediation schedule.
If remediation is successful, the student’s transcript will reflect a grade change of NP to NP/P. The
original grade of NP will remain on the official transcript. If a student fails any block remediation, he/she
may be dismissed from the program. The Academic Performance and Standards Committee will review
each case of failure of block remediation and make a recommendation to the Dean.
Remediation for Blocks in the First and Second Professional Years
The Office of the Association Dean for Academic Affairs will post the schedule for the comprehensive
remediation examinations the week following the end of the last block of the academic year.
Comprehensive remediation examinations will take place during the four weeks following the last block of
the academic year. Students must be available for any scheduled comprehensive remediation examination
they are required to take.
One comprehensive remediation examination will be administered that covers all block objectives (those
areas the student failed plus all other required competencies). Each block requiring remediation will have a
separate examination. Students must pass the comprehensive remediation examination to be promoted to the
next academic year. Students will be required to pay a fee of $250 for each comprehensive remediation
examination.
77
Remediation for Blocks in the Third Professional Year
The Office of the Associate Dean for Academic Affairs will post the schedule for the comprehensive
remediation examinations the week following the end of the last block of the third year. The comprehensive
remediation examinations for P3 students (Blocks 3.1-3.5) will be scheduled in January. Students will not
be scheduled to start Advanced Pharmacy Practice Experiences (APPEs) until all blocks are successfully
remediated. The Academic Performance and Standards Committee must approve any exceptions. One
comprehensive remediation examination will be administered that covers all block objectives within each
block the student failed (those areas the student failed plus all other required outcomes). Each block
requiring remediation will have a separate exam. The consequences of not passing remediation are outlined
below under Student Progress.
Attendance and Absences
Students are to be in class Monday-Friday from 8 am to 3 p.m., unless the block schedule notes
otherwise.
When a student must be absent, he/she must contact the Block Facilitator as soon as possible. If unable
to reach the Facilitator, the student must leave a message with a contact telephone number. Accommodation
for excused absences will be made, whenever possible, to assist students in situations involving illness or
other emergencies. The Block Facilitator may require documentation of the reason(s) for the absence. The
Block Facilitator/Faculty will determine how the missed materials will be completed.
If the absence is over three class days in duration, the case will be referred to the Academic Performance
and Standards Committee, to determine, in consultation with Block Faculty, if ongoing accommodation can
be made given the anticipated length of absence. The Committee may, at its discretion, recommend that the
student be assigned an Incomplete Grade (I) for the block. Refer to Student Progress (below) for
procedures to remove an Incomplete Grade. If the Committee determines that it is not possible for the
student to continue in the program, a leave of absence may be recommended. Leaves of absence are
governed by University policy. The Academic Performance and Standards Committee will make these
determinations on a case-by-case basis after review of the facts and forward a recommendation to the Dean.
This policy also applies to students on APPE/AE. These students are also governed by policies
contained in the Syllabus of Advanced Pharmacy Practice Experiences and by rotation-specific
requirements.
Independent Study: Because of the unique and intensive nature of the College of Pharmacy’s
curriculum, the collaborative teaching and learning processes among team members, and the sequencing of
key blocks, the Faculty does not believe that independent learning of core coursework meets the goals of the
Doctor of Pharmacy program. In special cases, e.g. involving illness, reasonable accommodation will be
made to permit the student to continue in his/her course of study if possible. Additionally, the collaborative
learning process among team members is a critical element of the curriculum. Students accepted into the
program must understand that their grades require successful collaboration with team members.
Independent study of blocks in the core curriculum in the College of Pharmacy is not permitted either in
summer or during the academic year. The only independent study that is permitted is via learning assurance
and remediation.
Holidays: Western University publishes an annual list of holidays recognized by the University. A
student who requests time off for a holiday other than those observed by Western University must do so in
writing to the Block Facilitator a minimum of 5 school days before the start of the block in which the
holiday falls. If the request is approved, the student is responsible for any work missed on the date(s)
absent. All assignments must be completed by the scheduled time. However, if the student fails to notify the
Block Facilitator in the timeframe noted, the absence will be considered an unexcused absence, and no
remediation will be permitted. The Western University holiday schedule does not apply to students on
Advanced Pharmacy Practice Experiences and on off-campus Advanced Electives. Students will follow the
rotation site holiday schedule on Advanced Pharmacy Practice Experiences and on Advanced Electives.
Professional Meetings and Other Related Absences: All students are required to attend one
professional meeting each year as indicated on the College’s academic calendar.
78
Policy for Academic Dishonesty
The faculty takes the position that honesty and integrity are among the most valued traits of a
professional person. As future professionals, each student must assume personal responsibility for honesty
and integrity.
The College of Pharmacy faculty will not tolerate academic dishonesty. Verification of an offense is
grounds for dismissal. Academic dishonesty includes, but is not limited to activities such as changing
examination answers after the graded examination has been returned, cheating, plagiarism, bringing in
unauthorized resources to exams or other assessed exercises, and signing another student’s name on
attendance records or team examinations/assignments.
All incidents that compromise academic integrity must be documented and referred to the Dean for
review. This Dean will investigate all allegations, and either resolve the issue or forward the issue to the
University Student Conduct Committee. The student may appeal the action following policies listed in the
General Academic Policies and Procedures section of this Catalog.
Student Examination and Assignment Policies and Grade Appeals
Excused Absence from an Exam: Excused absences are for emergencies. In the case of an emergency
the student must notify the Block Facilitator at the earliest time possible (see Attendance and Absences
Section above). Students who are excused from an examination/assignment will be permitted to
take/complete the examination/assignment at a time designated by the block faculty. [NOTE:
Examination/Assignment refers to any graded assessment in the block.] The student will be eligible to earn
full credit for the examination/assignment under these circumstances. However, a student who does not
take/complete the individual examination/assignment and who is not excused by the Block Facilitator will
received a zero for the examination/assignment. If emergencies arise that require a student to miss more
than one examination or assignment in a block, the student’s performance will automatically be referred to
the Academic Performance and Standards Committee for review.
Requests for an Examination or Assignment Regrade: This section applies to all graded assessments.
Any request by a student to have an examination or assignment regraded must be made in writing and
submitted to the Block Facilitator within two working days of return of the examination or assignment.
The student must specify which question(s) and answer(s) are to be reconsidered in the request. The
request should be accompanied by lecture notes or referenced sources that support the student’s original
answer. On receipt of the request, the Block Facilitator will consider the request and document the decision
regarding the request in writing to the student. The Block Facilitator will maintain a copy of the request and
action taken. If the request for a regrade concerns a faculty member other than the Block Facilitator, the
faculty member has the option of regrading the examination/assignment in its entirety. The Block
Facilitator will respond to the student within two working days of receiving the written request.
If the student disagrees with the decision and has adhered to the timelines specified for regarding, he/she
may petition the Academic Performance and Standards Committee for an appeal of the regrade decision.
Grade Appeals: A Grade Appeals Sub-Committee, if required, shall be constituted by the Academic
Performance and Standards Committee. It shall consist of at least one member of the Academic
Performance and Standards Committee, who shall serve as Chair, two voting faculty members not on the
Committee, and one student representative. All members of the Grade Appeals Sub-Committee have full
voting privileges. The Committee will conduct its own investigation in conjunction with such an appeal
following established procedural guidelines for handling student appeals of an academic nature. An
alternate appointed by the Dean will replace members of the Committee who may have a conflict of interest
in a particular case, e.g., a faculty member on the Committee may be the person who administered the grade
that is being appealed.
Appeal Process
Students may appeal decisions regarding suspension, student conduct, academic progression/promotion
and graduation according to the regulations listed in the General Academic Policies and Procedures
section in the front section of this Catalogue.
79
Student Progress
Academic Progression Blocks 1.1 through 3.5: To progress to the next academic year, a student must
pass all blocks in the current academic year. The Academic Performance and Standards Committee will
review each student’s progress at the end of every block.
Failure to Meet Standards – First Block Actions: When a student does not achieve the required
standard in a block, the Dean will automatically place him/her on academic probation. The Dean will notify
the student in writing within two weeks of receiving his/her final block grade. Letters will be distributed
either by the Dean or via certified and regular mail delivery. Student confidentiality will be maintained.
The terms of probation will be specified at the time a student is placed on probation. If a student is placed
on probation, he/she must meet with his/her faculty advisor monthly and may not hold office in any
University or College organization. The student will develop a corrective plan and submit it to his/her
faculty advisor within five working days. This plan should include problems the student is experiencing
(e.g., the number of hours the student is working, illness), the need for assistance from the Learning
Enhancement & Academic Development (LEAD) program, and actions the student will take to prevent
further difficulties. The faculty advisor will approve the plan and make appropriate referrals as necessary.
Both the student and the faculty advisor will sign the plan, and both parties will retain a copy. The student
will submit a copy of the plan to the Academic Performance and Standards Committee in a timely manner.
On a monthly basis, the student and faculty advisor will evaluate the plan and make changes as necessary.
Failure to Meet Standards – Second Block Actions: When a student does not achieve the required
standard in a second block in an academic year, the Academic Performance and Standards Committee will
schedule a meeting with the student. The student may invite his/her faculty advisor to the meeting. During
the meeting the corrective plan previously developed will be reviewed carefully, revised, and appropriate
additional referrals will be recommended, if needed. The student will continue on probation.
Failure to Meet Standards – Third Block Actions: When a student does not achieve the required
standards in a third block in an academic year, he/she will meet with the Academic Performance and
Standards Committee. The student may invite his/her faculty advisor to the meeting. At this time, the
Committee may recommend one of the following actions to the Dean: (1) The student may be required to
withdraw from the program “not in good academic standing,” and allowed to repeat the entire academic
year; or (2) be dismissed from the program (see Dismissal in General Academic Policies and Procedures
section). A recommendation regarding the disposition of a particular student’s case will be made by the
Academic Performance and Standards Committee based on review of the student’s overall academic
performance and with input from the student’s advisor, block faculty or other individuals the Committee
may consult. The Committee will send a written recommendation to the Dean, who will make a final
decision regarding the course of action to be taken. The student has the right to appeal this decision
according to established policy (see Student Appeal Process in General Academic Policies and
Procedures section). If a student is required to repeat an entire year of the program, he/she is responsible
for meeting with the Associate Dean for Academic Affairs to establish his/her schedule to ensure that all
required blocks are completed.
Incomplete grade (I): An Incomplete grade (I) indicates that a student has not been able to complete all
required work for issuance of a letter grade. An incomplete grade must be replaced before the student
registers for the next academic year, unless other arrangements are made with the Dean. The activities to
replace an incomplete grade may vary depending on individual circumstances. In some cases, Faculty may
require the student to take the block in the year following. The procedures for making up an incomplete
grade must not be in conflict with the College’s policy on Independent Study. The Block Facilitator and
Block Faculty should have a plan for removing the incomplete grade when assigning the I grade.
Replacement of an incomplete will be under the direction of the Block Facilitator and Block Faculty and
will be processed by the Office of the Associate Dean for Academic Affairs. A fee may be assessed. The
incomplete grade (I) remains on the transcript followed by the Pass grade when earned (I/P).
Eligibility to participate in Advanced Pharmacy Practice Experiences (APPEs): Courses in the first
through third years must be completed successfully before beginning APPEs. Students may not start an
APPE until the Academic Performance and Standards Committee has been notified that all blocks have
been remediated successfully. The Academic Performance and Standards Committee will ensure that
students are eligible to begin APPEs.
Progression to the Fourth Professional Year: Students must have completed at least three rotations
successfully by the end of July in their P3 year to progress to the fourth year of the program. As a general
80
rule, no “off rotations” will be given during the first three APPEs unless a student is required to remediate a
block during Rotation 1 or if there is an extenuating circumstance (e.g., maternity leave, illness). The
Academic Performance and Standards Committee will monitor the progress of any student who is on
academic probation.
Failure to Meet Standards on APPE: When a student receives a NP or an Incomplete grade (I) in a
rotation, the faculty member directing APPE assignments will notify the committee in a timely manner.
He/she will make recommendations to the committee regarding remediation. The Academic Performance
and Standards Committee will approve the remediation plan. The student will be placed on academic
probation until he/she remediates the APPE. To monitor the quality of a student’s performance on APPEs,
all students must complete at least one APPE with a voting, full-time faculty member. If a student drops or
fails this required APPE, he/she must complete another APPE successfully with another voting, full-time
faculty member.
Progression to Advanced Electives/Comprehensive Review and Assessment: Students may not begin
elective requirements (coursework, Advanced Electives, Research Elective) until all APPE rotations are
completed successfully. Students may not complete the Comprehensive Review and Assessment until all
other requirements are completed. Any students requesting an exception to this policy will be considered on
a case by case basis by the Academic Performance and Standards Committee. The recommendation of the
Academic Performance and Standards Committee will be forwarded to the Dean for his/her action.
Incivility
The College of Pharmacy does not tolerate incivility by any member of the College/University
community. This includes faculty, staff, students, guests, and visitors. Examples of incivility include rude,
sarcastic, obscene, disruptive or disrespectful behavior, threats, and damage to property. Complaints of
incidences of incivility will be reported to the Dean. Should violations by students be determined to have
occurred, the Dean either will resolve the issue or forward the issue to the Student Conduct Committee.
Students have the right of appeal through the Student Appeal Process.
Veterans
Veterans who fail to maintain satisfactory progress for more than five (5) blocks will not be certified to
receive any Veterans’ benefits until they have corrected the situation and are making satisfactory progress.
Research Activities
Students in the College of Pharmacy are encouraged to participate in research under the direction of
faculty advisor(s). Students with appropriate interests and academic preparation may participate in research
as part of the elective program.
Program Completion and Eligibility for Graduation
All coursework in the College of Pharmacy must be completed within six (6) years of beginning the
program. Exceptions may be made only upon recommendation of the Academic Performance and Standards
Committee in consultation with the Dean. Students eligible for graduation must be approved by a vote of
the College Faculty.
Graduation
A student will be recommended for the Doctor of Pharmacy degree provided he/she:
• Has been enrolled in the Western University of Health Sciences, College of Pharmacy, for the duration
of the Pharm.D. program.
• Is not on probation and has completed all prescribed academic requirements and has no outstanding
grade of “I” or “NP”.
• Has demonstrated no serious deficiencies in ethical, professional, or personal conduct that would make
it inappropriate to award the Doctor of Pharmacy degree.
• Has complied with all the legal and financial requirements of the University as stated in the University
Catalogue.
No student will receive his/her diploma until that student has successfully completed all requirements for
graduation.
81
All students must attend and participate in the Commencement program at which time the degree is
conferred, unless special permission has been granted by the President of Western University of Health
Sciences. If the President grants special permission to be excused from graduation, the graduate may be
required to present himself or herself to the Provost, Executive Vice President of Academic Affairs or
appropriate Dean at a later date in order to take the required oath (if relevant) to receive his or her diploma.
DESCRIPTION OF BLOCKS/COURSE DESCRIPTIONS
Blocks listed in this catalog are subject to change through established academic channels. New blocks
and changes in existing blocks are approved by the College of Pharmacy Curriculum Committee and the
Faculty.
FIRST YEAR
The 5000 series is assigned to didactic blocks in the Basic Science Foundations and Professional
Practice Foundation blocks for the first-year pharmacy students (P1).
PHRM 5111 Foundations of Clinical Practice I (4 credits)
This block is designed to introduce the student to the knowledge, skills and attitudes necessary for
successful completion of the Pharm.D. curriculum, and to begin to develop foundation skills for patient-
centered pharmacy practice. General topics include an introduction to contemporary pharmacy practice and
the role of the pharmacist as a health care provider, written and verbal communication skills, developing
team collaboration skills, humanism, introduction to ethics and professionalism, time management, resume
writing, pharmacy abbreviations and equivalents, medical terminology, pharmaceutical calculations,
pharmacy law, introduction to over the counter medications and pharmaceutical care, introduction to drug
information, and introduction to the US health care system. (Formerly PHRM 5101)
PHRM 5112 Foundations of Clinical Practice II (4 credits)
This block is designed to further advance and reinforce the knowledge, skills and attitudes initially
introduced to the student in PHRM 5111 and to develop clinical foundation skills necessary for patient-
centered pharmacy practice. General topics include written and verbal communication skills, developing
team collaboration skills, medical terminology, pharmaceutical calculations, pharmacy law, over the counter
medications and pharmaceutical care, introduction of patient medical history and the patient medical record,
drug information, the top 200 drugs and drug cards, physical assessment skills, patient counseling skills,
belief systems and pharmaceutical care, introduction to pharmacy practice-community pharmacy and
inpatient hospital pharmacy clerkships. Prerequisite: PHRM 5111. (Formerly PHRM 5105)
PHRM 5113 Foundations of Clinical Practice III (4 credits)
This block is designed to further advance and reinforce the knowledge, skills and attitudes initially
introduced to the student in PHRM 5111, and further enhanced in PHRM 5112, and to develop clinical
foundation skills necessary for patient-centered pharmacy practice. General topics include written and
verbal communication skills, developing team collaboration skills, medical terminology, pharmaceutical
calculations, pharmacy law, over the counter medications and pharmaceutical care, introduction to patient
SOAP notes, the top 200 drugs and drug cards, First Aid certification, patient counseling skills, introduction
to pharmacy practice-community pharmacy and inpatient hospital pharmacy clerkships, current issues in
pharmacy practice and the medication use system. Prerequisite: PHRM 5112. (Formerly PHRM 5110)
PHRM 5114 Comprehensive Review (1 credit)
This block summarizes and provides a final integration of materials and skills learned during the first
year. A final comprehensive examination and a clinical skills assessment examination are administered and
year-long team assignments are finalized with presentations and poster sessions.
PHRM 5211 Introduction to the Pharmaceutical Sciences (1 credit)
This course introduces the chemical, physicochemical, biopharmaceutical and mathematical principles
and concepts that are fundamental to the study of the pharmaceutical sciences. Functional group chemistry
is introduced with emphasis on acid-base properties, contributions to solubility, chemical stability and
chemical incompatibilities. An introduction to the basic mathematical and graphical principles relevant to
82
students in pharmaceutics, biopharmaceutics and pharmacokinetics is also presented. Rational approaches
to problem-solving in the pharmaceutical sciences is an important component.
PHRM 5212 Integrated Biological Sciences I (3 credits)
This series of blocks (PHRM 5212, 5213, 5214 and 5215) presents general principles of biochemistry,
molecular biology, physiology, pharmacology and medicinal chemistry. The purpose of these blocks is to
demonstrate their interdependence and to provide an integrated, scientific basis for the development and
therapeutic use of drugs. The series focuses on the human system and provides the organizational
knowledge and background relevant to the management of homeostasis blocks of the second and third
years. The biochemistry and molecular biology portions present the common features of most biochemical
pathways and their relevance in diagnosing and treating disease, as well as developing therapeutic agents.
With physiology, the organization of biological systems (homeostasis) is emphasized with the objective of
demonstrating how the breakdown of organization leads to disease and the manipulation (interference or
enhancement) of organization provides the basis for therapeutic intervention. The intent is to demonstrate
how an understanding of biochemistry and molecular biology is fundamental toward developing an
appreciation of medicinal chemistry and the development of drug entities. Principles addressing cellular and
tissue physiology provide a conceptual framework to introduce pharmacology by emphasizing
commonalties of drug mechanism with drug classification. Fundamental principles are emphasized with the
intent of providing their relevance for prevention and treatment of disease using therapeutic agents, which
themselves can be considered as modifications of intrinsic, biological compounds. (Formerly PHRM 5102)
PHRM 5213 Integrated Biological Sciences II (3 credits)
Continuation of PHRM 5212. Prerequisite: PHRM 5212. (Formerly PHRM 5103)
PHRM 5214 Integrated Biological Sciences III (3 credits)
Continuation of PHRM 5213. Prerequisite: PHRM 5213. (Formerly PHRM 5104)
PHRM 5215 Integrated Biological Sciences IV (4 credits)
Continuation of PHRM 5214. Prerequisite: PHRM 5214.
PHRM 5301 Pharmaceutics/Biopharmaceutics I (3 credits)
This block introduces the student to physicochemical principles and their applications in order to
develop an understanding of the manufacture, compounding, and proper use of liquid (homogeneous and
disperse systems) and solid dosage forms. Prerequisite: PHRM 5211. (Formerly PHRM 5107)
PHRM 5302 Pharmaceutics/Biopharmaceutics II (3 credits)
This block deals with the manufacture, compounding and proper use of different dosage forms (topicals,
suppositories, aerosols, parenterals and novel drug delivery systems). Additionally, students will be
introduced to innovations in biotechnology processes and products. Prerequisite: PHRM 5301. (Formerly
PHRM 5108)
PHRM 5401 Immunology (3 credits)
The first part of this block introduces students to the basics of immunology including cells, organs and
effector systems involved in both cell mediated and humoral mediated immune activity. The second part of
the block focuses on regulatory interactions between different components of the immune system and the
deleterious effects of aberrant immune processes. (Formerly PHRM 5106)
PHRM 5501 Pharmacokinetics (4 credits)
This block gives the student an introduction to principles of pharmacokinetics. The relationships
between physicochemical characteristics and physiological factors to drug disposition are discussed. The
relevance of pharmacokinetics to drug therapy is presented. Prerequisites: PHRM 5111, PHRM 5301 and
PHRM 5302. (Formerly PHRM 5109)
83
SECOND YEAR AND FIRST HALF OF THE THIRD YEAR
The 6200 series describes the didactic curriculum for second-year pharmacy students (P2). The 6300
series denotes the didactic curriculum for the first half of the third year (P3).
PHRM 6201 Health Care Administration/Drug Information (4 credits)
This block covers Health Care Administration and Drug Information. Health Care Administration
provides an overview of the health care system in the US in terms of its evolution, structure, function,
components and interrelationships between stakeholders of the system. The Drug Information component of
this block continues the student's development in drug information. Introduces the student to research
methodology and biostatistics.
PHRM 6212 Introduction to Homeostasis and Nutrition (4 credits)
This block introduces homeostasis and covers materials from basic biochemistry to advanced
pharmacotherapeutics as they relate to nutrition. Introductory topics such as laboratory interpretations,
fluid-electrolytes, and acid-base disorders will be covered in addition to the nutrition related topics.
Accordingly, the overall goal of this block is to equip pharmacy students with elemental tools essential for
providing pharmaceutical care as well as to integrate knowledge, skills, and attitudes to provide an
individualized nutrition pharmacotherapeutic plan for a given patient. (Formerly PHRM 6207)
PHRM 6213 Gastrointestinal and Hepatobiliary Systems (4 credits)
This block provides the student with an understanding of the gastrointestinal and the hepatobiliary
systems. Specific emphasis is placed on the pharmacological treatment of peptic ulcer disease,
inflammatory bowel disease, alcoholic liver disease, and hepatitis. (Formerly PHRM 6202)
PHRM 6214 Nephrology and Pulmonary Systems (4 credits)
This block is designed to teach the student how to solve patient-based pharmacotherapeutic problems in
nephrology (kidney diseases) and pulmonology (lung diseases). Hypertension pathophysiology and
treatment are introduced in this course, including national guidelines for diagnosis and treatment.
Nephrology topics include evaluation of renal function, acute renal failure, chronic renal failure (e.g.
diabetic nephropathy and primary glomerular diseases), complications of renal failure (e.g. fluids and
electrolytes, anemia, and secondary hyperparathyroidism), renal transplant, and appropriate drug dosing in
renal disease. Pulmonary topics include asthma (adult and pediatric), chronic bronchitis, emphysema, and
cystic fibrosis. Students learn the proper use of inhalers, spacers, nebulizers, and peak flow meters. Several
critical care medicine topics and venous thromboembolism are also components of this block. Major
concepts of prior block material is reinforced throughout the block. (Formerly PHRM 6204)
PHRM 6215 Foundations of Clinical Practice IV (4 credits)
This block is designed to allow the student an opportunity to strengthen their knowledge in the content
areas previously covered in the second year blocks. Students will engage in team case discussions, which
incorporate and integrate aspects of those disease states previously covered. In addition, students will
continue to expand their knowledge of individual drug therapies by the construction of individual drug
cards. Skills (e.g., counseling, patient education, calculation applications, drug information applications)
relevant to the practice of pharmacy will be practiced in this block. Students will receive certification for
the administration of immunizations. Prerequisite: PHRM 5113. (Formerly PHRM 6205)
PHRM 6216 Endocrine and Reproductive Systems (4 credits)
This block provides students with the knowledge, skills and attitudes to manage pharmacotherapeutic
regimens in endocrine-related diseases, such as diabetes and thyroid disorders, and reproductive medicine.
Gender-related health concerns are also addressed. (Formerly PHRM 6203)
PHRM 6217 Cardiovascular System (4 credits)
This block contains epidemiology, anatomy, physiology, pharmacology, and pharmacotherapy as they
relate to cardiology. Accordingly, the overall goal of this block is to enable students to integrate their
knowledge of these topics in the context of formulating an individualized pharmacotherapeutic plan for a
given patient with cardiac disease(s). (Formerly PHRM 6206)
84
PHRM 6208 Neurosensory System (4 credits)
This block focuses on the pathophysiology, pharmacology, and pharmacotherapy relevant to diseases
affecting the central nervous system. The main goal of this block is to provide students with the
fundamental knowledge, skills and attitudes required to provide optimal pharmaceutical care to patients
with neurologic disorders. Disease states covered include dementias, epilepsy, headache, Parkinsonism,
acute and chronic pain and stroke.
PHRM 6209 Psychiatry (4 credits)
The purpose of this block is to enable students to integrate the pathophysiology, medicinal chemistry,
pharmacology and therapeutic knowledge in the management of specific disease states. The content of the
block will span psychiatric diseases, substance abuse and toxicological states. Students are provided the
opportunity to practice clinical problem assessment and therapeutic drug monitoring in preparation for
providing pharmaceutical care.
PHRM 6210 Foundations of Clinical Practice V (4 credits)
This block is designed to allow the student an opportunity to strengthen their knowledge in the content
areas previously covered in the second year blocks. Students will engage in team discussions, which
incorporate and integrate aspects of those disease states previously covered. In addition, students will
continue to expand their knowledge of individual drug therapies by the construction of individual drug
cards. Skills (e.g., counseling, patient education, calculation applications, drug information applications)
relevant to the practice of pharmacy will be practiced during this block. Students will receive instruction on
the pharmacist’s role in investigational drug services. Prerequisite: PHRM 6215.
PHRM 6301 Infectious Disease (4 credits)
This block is an integrated approach to microbiology, antimicrobial pharmacology and infectious
disease syndromes. The initial part of the block deals with the identification, laboratory diagnosis,
epidemiology and modes of spread of the medically important pathogens. Pharmacology of the major
classes of antimicrobial agents will be discussed. The latter part of the block will focus on the microbiology,
epidemiology, pathogenesis, pathophysiology, diagnosis, clinical features, preventive and infection control
measures associated with major infectious syndromes due to common bacteria and parasites.
PHRM 6302 HIV, AIDS and Organ Transplantation (4 credits)
This block is an extension of PHRM 6301 with a focus on special patient populations and opportunistic
infections including fungal and viral infections. Pharmacology of antiviral and antifungal agents and the
applications in treating infections will be discussed. The latter part of the block will focus on basic
pharmacology of immunotherapeutic agents and their applications in transplantation.
PHRM 6303 Drug Information/Pharmacy Administration (4 credits)
This block covers Drug Information and Pharmacy Administration. The Drug Information component of
this block continues the students' development of the knowledge, skills and attitudes in drug information.
Pharmacy Administration covers the components of the pharmaceutical distribution system, including
production, logistics, utilization and external subsystems. This block also presents an introduction to human
resource management, strategic planning and marketing, purchasing and inventory, financial management
and continuous quality improvement; and their applications to pharmacy and health care.
PHRM 6304 Oncology (4 credits)
The objective of this block is to provide an introduction in the pathophysiology, medicinal chemistry,
pharmacology, and therapeutic knowledge in the management of hematological disorders, hematological
malignancies and solid tumors. Students will receive instruction in the following areas: appropriate cancer
screening and prevention information to the general public; basic pharmacology of the commonly used
antineoplastic agents in clinical settings; supportive care in oncology and patient specific treatments; and
appropriate treatments for the common types of hematological disorders.
85
PHRM 6305 Pharmacoeconomics (4 credits)
This block provides students with an understanding of the fundamentals of pharmacoeconomics and its
value to decision making in health care. The block will include the terminology of pharmacoeconomics and
involve understanding, performing and evaluating different types of pharmacoeconomic analysis. Students
will be able to use their background in research methodology and statistics to conduct a 10-step evaluation
of published pharmacoeconomic studies.
ADVANCED PHARMACY PRACTICE EXPERIENCES (APPEs): SECOND HALF OF THE 3RD
YEAR (P3) AND FIRST HALF OF THE 4TH YEAR (P4)
The APPE rotations provide one year of supervised clinical education. Students advance their
knowledge in areas such as taking drug histories, providing patient education, interpreting diagnostic data
and dispensing and compounding medications. The 7000 series are designated for the APPE rotations.
Required rotations:
PHRM 7110 Ambulatory care externship (8 credits)
Supervised patient care experience in an outpatient setting under the supervision of a preceptor or
faculty member of the College of Pharmacy.
PHRM 7120 Institutional care externship (8 credits)
Supervised patient care experience in a hospital or other institutional setting under the direct supervision
of a preceptor or faculty member of the College of Pharmacy.
PHRM 7210 Ambulatory care clinical (8 credits)
Supervised clinical pharmacy experience emphasizing the development of pharmaceutical care skills in
an out-patient setting.
PHRM 7220 Institutional care clinical (8 credits)
Supervised clinical pharmacy experience emphasizing the development of pharmaceutical care skills in a
hospital or other institutional setting such as a long term care facility.
Elective Rotations:
PHRM 7330 Elective clerkship I (8 credits)
Supervised education in clinical, administrative or research settings that provide additional experience in
specialty areas such as pediatrics, geriatrics, infectious disease, drug information, oncology, pharmaceutical
research, pharmacy administration, etc.
PHRM 7340 Elective clerkship II (8 credits)
Supervised education in clinical, administrative or research settings that provide additional experience in
specialty areas such as pediatrics, geriatrics, infectious disease, drug information, oncology, pharmaceutical
research, pharmacy administration etc.
Prerequisite: PHRM 7330.
PHRM 7350 Elective clerkship III (8 credits)
Supervised education in clinical, administrative or research settings that provide additional experience in
specialty areas such as pediatrics, geriatrics, infectious disease, drug information, oncology, pharmaceutical
research, pharmacy administration etc.
Prerequisite: PHRM 7340.
Electives:
FOURTH YEAR (P4): 16 credits of elective coursework and 2 credits in the comprehensive review and
assessment are required.
The 8000 series is designed for elective coursework and the comprehensive assessment/review weeks.
The elective program is a capstone experience designed to prepare the student for his/her role as an entry
level practitioner. Electives are offered in areas such as research, teaching, and advanced clinical practice.
86
A project is required of each student. Finally, each student completes a required comprehensive two-week
review and assessment at the end of the program.
PHRM 8200 Elective Coursework (4 credits)
Advanced level coursework in an area of special interest beyond that presented as part of the previous
didactic coursework of the Doctor of Pharmacy Curriculum. Repeatable to a maximum of 16 credits.
PHRM 8400 Elective Apprenticeships (16 credits)
Advanced clinical educational experiences in an area of special interest beyond that provided as part of
the previous clinical coursework of the Doctor of Pharmacy Curriculum. Repeatable to a maximum of 16
credits.
PHRM 8600 Research Electives (16 credits)
Supervised participation in pharmacy related research under the direct supervision of a faculty member.
Repeatable to a maximum of 16 credits.
PHRM 8800 Other Electives (4-16 credits)
Individualized, supervised educational experiences in an area of special interest related to pharmacy
practice beyond that provided by previous coursework in the Doctor of Pharmacy curriculum and not
eligible for credit within PHRM 8200, 8400 or 8600. Repeatable to a maximum of 16 credits.
PHRM 8999 Comprehensive Review and Assessment (2 credits)
A two-week series of didactic and other educational experiences designed to provide students with a
review of the Doctor of Pharmacy Curriculum and conduct assessments of the student's competency for
pharmacy practice.
87
Sample Schedule: The following schedule represents an example of the schedule for the blocks in one
academic year. This schedule is subject to change.
Year Block No. Block Title
First Year
Fall
5111 Foundations of Clinical Practice I-Introduction to Pharmacy
5112 Foundations of Clinical Practice II
5211 Introduction to Pharmaceutical Sciences
5212 Integrated Biological Sciences I
5213 Integrated Biological Sciences II
5301 Pharmaceutics/Biopharmaceutics I
5302 Pharmaceutics/Biopharmaceutics II
Spring
5214
Integrated Biological Sciences III
5215 Integrated Biological Sciences IV
5401 Immunology
5501 Pharmacokinetics
5113 Foundations of Clinical Practice III
5114 Comprehensive Review
Second Year
Fall
6201
Health Care Administration/Drug Information
6212 Intro. Homeostasis/Nutrition
6213 Gastrointestinal and Hepatobiliary Systems
6214 Nephrology and Pulmonary Systems
6215 Foundations of Clinical Practice IV
Spring
6216
Endocrine and Reproductive Systems
6217 Cardiovascular System
6208 Neurosensory System
6209 Psychiatry
6210 Foundations of Clinical Practice V
Third year
Fall
6301
Infectious Diseases
6302 HIV, AIDS and Transplantation
6303 Oncology
6304 Drug Information and Administration
6305 Pharmacoeconomics
Spring
R1 Inpatient Care Experiential (IX)
R2 Ambulatory Care Experiential (AX)
R3 Inpatient Care Clinical (IC)
Fourth Year
R4 Ambulatory Care Clinical (AC)
R5 Elective rotation
R6 Elective rotation
R7 Elective rotation
R8 Off
January-
May
Advanced Electives: Apprenticeships, coursework, research
May Comprehensive assessment and review
88
HONORS AND AWARDS
The following awards for PharmD students are presented annually on Honors Day in April.
President's Society Award
Provost's Student Government Award
Dean's Award
American Society of Health Systems Pharmacists Student Leadership Award
Eli Lilly and Company Award
Linda Fox Memorial Endowment Fund Award
Guy M. Allmon Scholarship Fund Award
The following awards are presented annually to graduates at the Commencement Dinner Dance:
Merck Award
APhA-ASP Mortar & Pestle Professionalism Award
Roche Pharmacy Communications Award
Dr. Arasb Ateshkadi Memorial Award
SmithKline Beecham Award
Facts & Comparisons Award of Excellence in Clinical Communication
Pfizer US Pharmaceuticals Outstanding Leader Award
TEVA Pharmaceuticals Outstanding Student Award
Perrigo Award for Excellence in Nonprescription Medication Studies
Mylan Pharmaceuticals Award
Dean's Award
89
Academic Calendar 2002-2003
PharmD PROGRAM
(subject to change)
Friday, May 17, 2002
Fall Semester Registration Forms due (2
nd
years)
Wednesday, Jul. 24, 2002
Fall Semester Registration (1
st
years)
Wednesday, Aug. 5, 2002
Fall Semester Tuition Due (1
st
, 2
nd
and 3
rd
years)
Tuesday, Aug. 6-Friday, Aug. 9, 2002
Orientation
Saturday, Aug. 10, 2002
Convocation/White Coat Ceremony
Monday, Aug. 12, 2002
Fall Semester Tuition Due (4
th
years)
Monday, Aug. 12, 2002
Classes begin (1
st
, 2
nd
& 3
rd
years)
Monday, Aug. 19, 2002
Fall Semester Classes Begin (4
th
years)
Monday, Sept. 2, 2002
Labor Day:
Friday, Oct. 4, 2002
Professional Association Day
Monday, Oct. 148, 2002
Columbus Day
Wednesday, Nov. 27, 2002 (12:00 noon)
Thanksgiving recess
Monday, Dec. 2, 2002
Classes Resume
Monday, Dec. 2-Friday, Dec. 6, 2002
Spring Semester Registration (1
st
& 2
nd
years)
Friday, Dec. 20, 2002
Spring Semester Tuition Due (all years)
Friday, Dec. 20, 2002
Last Day of Classes, Autumn Semester
Wednesday, Jan. 2, 2002
Spring Semester Tuition Due (1
st
, 2
nd
& 4
th
years)
Monday, Jan. 6, 2003
Spring Semester Classes begin (all years)
Monday, Jan. 20, 2003
Martin Luther King Holiday
Monday, Feb. 17, 2003
Presidents Day
Friday, May 23, 2003
Last Day of Spring Semester (1
st
, 2
nd
& 4
th
years)
Monday, May 26, 2003
Memorial Day
Friday, Jun. 27, 2003
Last Day of Spring Semester (3
rd
years)
90
COLLEGE OF ALLIED HEALTH PROFESSIONS
MISSION
The College of Allied Health Professions supports the mission of Western University of Health Sciences by
providing high quality professional and graduate education. The College utilizes the team approach to develop
competent and compassionate professionals who provide service to the community and continually develop their
skills, knowledge, and abilities through independent lifelong learning activities.
GOALS
1. To educate an allied health workforce that helps to meet the healthcare and educational needs of the State of
California and the west.
2. To achieve an environment and culture that support all members of the College.
3. To ensure an environment and culture that empower all persons in the College to maximize their potential as
contributing members in the education of students, in research and clinical activities, and in service to the
community.
91
COLLEGE OF ALLIED HEALTH PROFESSIONS
Master of Science in Health Sciences Program
The Department of Health Sciences
The Department of Health Sciences aims to sustain an integrative response to methodological issues in order to
equip students with a critical appreciation of the diverse approaches now practiced in science and medicine. In order
to improve the quality of health care, the Department recognizes its responsibility by ensuring and improving the
quality of graduate health science educational experiences. Students are urged to enrich their professional
preparation by integrating knowledge in other disciplines within Health Sciences. The Department of Health
Sciences supports Western University of Health Sciences’ mission to increase the availability of health care
providers and to serve the needs of the people living in the western region. The Department of Health Sciences' aims
provide educational programs to students with diverse backgrounds, who are committed to rational, compassionate
health care. Classes are offered in an environment intended to foster respect for the uniqueness of humanity. The
students are provided with classroom, clinical, and on-line experiences designed to prepare them to function as
competent health care practitioners and educators.
Faculty includes scholars, researchers and administrators from a variety of backgrounds and disciplines. All are
committed to the improvement of teaching and practice in the health professions through the process of professional
development. The future of health care is rapidly expanding through technology and other changes thereby
increasing the demands made upon the health care professional. The graduating student should be able to participate
in and adapt to the ever-changing environment.
Academic Programs
The Department of Health Sciences offers opportunities for students to pursue degrees in two concentrations:
Health Professions Education and Advanced Physician Assistant Practice. Both concentrations lead to a Master of
Science degree in Health Sciences. The broad interest of the faculty provides special opportunities to cross the
boundaries between various health care fields and education, depending on the field of experience of the student.
The curriculum is designed to meet the educational demands on health care education and delivery within an
integrated context of theory and practice that meets the academic requirements for a graduate degree in Health
Sciences. Course work is formulated and designed to promote knowledge, values and skills essential for competent
clinical teaching and continuing education.
The Health Professions Education concentration is designed for professionals who are planning or currently
teaching in the health sciences. The Department of Health Sciences utilizes learning activities based on the
functional requirements of health professionals to illustrate educational concepts and methodologies in varied
settings. In addition to acquiring expertise in the principles of teaching and learning theory, program planning and
evaluation, students are encouraged to develop educational research projects that benefit the academic endeavors in
Health Science Education and supporting advances in patient care, community service, research and education.
The Advanced Physician Assistant Practice concentration is designed for clinically practicing physician assistants
who wish to complete their Master of Science in Health Science degree through a combination of online and
traditional classroom approaches. Licensed physician assistants can choose opportunities for continuing education
and advanced education for clinical practice, focusing on community health and education.
Goals of the Department of Health Sciences
The Department of Health Sciences, through the two selective areas of concentration, provides students with the
necessary background and skills in theory and practical application in both clinical and non-clinical settings. In
fulfillment of the mission of the University, the Department’s goals are to:
1. Provide educational experiences, which will enable the health care professional to function as teachers in a
variety of health care settings.
2. Promote and encourage graduates and students to maintain life long learning and the pursuit of supporting
advances in patient care, community service, research and education.
3. Educate health care professionals who will function as academic leaders in various health care settings.
4. Assist students in the integration of theory and practice to ensure health care education will be relevant to
the needs of society.
5. Encourage students to engage in productive professional relationships to acquire, evaluate and communicate
information about the health sciences.
92
6. Create and be responsive to the needs of health care professionals, thereby providing opportunities for
educational expansion.
7. Enhance continuing professional education in health care.
8. Further develop clinical education partnerships through the United States (West).
9. Continue to provide educational service to all professionals in the health care community.
Objectives of the Department of Health Sciences
The department is designed to prepare health care professionals with skills in teaching, learning, scholarship and
research. Upon completion of the program, students will be able to:
1. Demonstrate proficiency in adult education practices based upon rational principles and theories.
2. Apply educational theories, models and concepts in the health care setting.
3. Create, implement and analyze valid research projects in health professions education or the clinical
environment.
4. Collaborate with academic health care specialists to further the advancement of the health sciences.
5. Maintain a high standard of academic excellence and pursuit of learning.
6. Contribute scholarly research to the health care professions.
PERSONAL COMPETENCIES FOR ADMISSION AND MATRICULATION
A candidate for admission to the degree programs in the Department of Health Sciences must have the use of
certain sensory and motor functions, or reasonable accommodations thereto; to permit them to carry out the activities
described in the sections that follow. Graduates of the program are eligible for employment in a wide variety of
academic and clinical teaching programs, using an extensive variety of educational methodologies. As a result, they
must have the intellectual ability to learn, integrate, analyze, and synthesize numerical, visual and textual information
in the health professions fields. They must also be able to effectively and accurately integrate this information and
communicate it to others by both oral and written means.
A candidate for the degree programs in the Department of Health Sciences ordinarily must have abilities and
skills of five general varieties, including: (1) observation; (2) communication; (3) motor; (4) intellectual, conceptual,
integrative and quantitative; and (5) behavioral and social. Reasonable accommodations will be provided in
appropriate situations. Under all circumstances, however, a candidate should be able to perform in a reasonably
independent manner. The following provides an overview of the five general varieties of minimal technical standards
that must be met by all successful applicants to the degree programs in the Department of Health Sciences.
1. Observation: Candidates and students must have sufficient vision, with or without reasonable
accommodations, to be able to observe demonstrations and presentations by faculty and other students.
2. Communication: Candidates and students must be able to communicate with students and colleagues. They
should be able to hear, with or without reasonable accommodations. Candidates and students must be able
to read, write, and speak English.
3. Motor: Candidates and students should have sufficient motor function, or reasonable accommodations to
enable them to operate commonly used educational equipment (including, but not limited to, computers,
videotape players, overhead projectors) and design and produce educational materials. These activities
require coordination of both gross and fine muscular movements, equilibrium, and functional use of the
senses of touch or vision.
4. Intellectual, Conceptual, Integrative, and Quantitative Abilities: Students must demonstrate problem-solving
skills, which include measurement, calculation, reasoning, analysis, and synthesis. Instructional design and
the preparations of a thesis or special project require all of these intellectual abilities.
5. Behavioral and Social Abilities: Candidates and students must possess the emotional health required for full
utilization of the intellectual abilities, the exercise of good judgment, the prompt completions of all
responsibilities attendant to an instructor in an educational setting, and the development of mature,
sensitive, and effective relationships with students and colleagues. Candidates and students must be able to
adapt to changing environments and display flexibility in dealing with students at various educational
levels in the health professions. Compassion, integrity, concerns for others, interpersonal skills, interest,
and motivation are all personal qualities to be assessed during the admissions and educational processes.
93
ADMISSIONS POLICY AND PROCEDURES
Admission to the degree program is through the Department of Health Sciences. Students may apply for either the
fall or spring semesters. Western University is committed to admitting competitive, qualified individuals with
disabilities.
Application Requirements: Advanced Physician Assistant Practice students
Candidates must meet the following academic requirements:
1. A bachelor’s degree from an accredited institution.
2. A 2.5 GPA or above for undergraduate work, 3.0 for graduate work.
Applicants must also submit the following materials for application:
1. Copy of State PA licensure and NCCPA card (for applicants still in the licensure process, proof of an
interim PA license will satisfy this requirement)
2. Official transcripts from all undergraduate and graduate institutions attended.
3. Completed application form and $35.00 a nonrefundable application fee.
Application Requirements: HPE students
Applicants to the HPE concentration should be a health professional or in a career that involves education of
health professionals. Candidates must meet the following academic requirements:
1. A bachelor’s degree from an accredited institution is preferred. However, consideration will be given on a
case-by-case basis to applicants holding an advanced professional degree, provided that the applicant has
completed at least 90 semester hours at the undergraduate level from a regionally accredited college or
university. Thirty (30) units must consist of upper division coursework, i.e., junior or senior level courses.
2. A 2.5 GPA or above for undergraduate work, 3.0 or above for graduate work.
Applicants must also submit the following materials for application
1. Official transcripts from all undergraduate and graduate institutions attended.
2. Completed application form and a $35.00 nonrefundable application fee.
Application Procedures and Deadlines
Students are advised to submit applications materials as early as possible prior to the semester in which they wish
to begin their program of studies. Deadline for receipt of application materials is no later than 30 days prior to the
first day of classes for each semester.
To request an informational brochure and/or an application, contact the admissions office at
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766
(909) 469-5336
Or on the internet at http://www.westernu.edu.
Transfer of Credits
The maximum number of graduate units that may be transferred from another institution offering programs of
graduate studies is six semester units. Only graduate credit relevant to the Master of Science in Health Science
degree concentration at Western University, which has been completed within the last five years, may be applied
toward completion of the Master of Science degree. To be considered for transfer credit, the course must have been
taken after the award of a bachelor’s degree and be eligible for graduate studies credit at the issuing institution. The
student must have received a grade B or above in the course. An official transcript and a course description should
be submitted to the Chair of the Department of Health Sciences for consideration of the faculty. The Department of
Health Sciences faculty will determine whether or not courses undertaken at other institutions qualify for transfer. No
transfer credit will be given HSCI 5999, HPE 5300, or HPE 5208.
94
Continuing Education and Non-degree students
An applicant who has a bachelor’s degree and/or advanced degree and does not wish to pursue a master’s degree
in health sciences at Western University of Health Sciences at the present time, but who wishes to engage in graduate
study for (a) personal development, (b) continuing education, or (c) other professional development needs, may
consider enrollment as a non-degree student. A limited number of applicants may enroll as non-degree students each
semester. The usual admission and registration procedures must be followed. Admission as a non-degree student
does not assure acceptance as a degree candidate, should the student at a later time wish to change enrollment status.
An unlimited number of semester units may be completed while in non-degree status. Should the student wish to
change enrollment status, the usual admission procedures must be followed. Questions about transferring from non-
degree to degree status should be directed to the Chairperson, Department of Health Sciences.
REGISTRATION POLICIES AND PROCEDURES
Prior to each semester, a class schedule mailed to students by the Registrar. All candidates for the MSHS degree
are required to register on-line or in person. Advisement is available from the Department Chair and faculty in order
to promote greater efficiency in the registration and enrollment process. Enrollment occurs during the week prior to
the first class meetings, on an appointment basis. Enrollment is available biannually, during the Fall and Spring
semesters.
Students may be denied admission to a specific class due to availability or limited enrollment. Courses with less
than three students registered may be cancelled. An individual must enroll for a minimum of three semester hours of
credit for each semester in which they wish to be identified as students.
New Graduate Students
New graduate students are notified by electronic or US mail of their admission status. This notification will
include a list of courses available during the next semester and the necessary registration materials. Completed
registration materials and fees may be submitted through the US mail, or in person, two weeks prior to the first week
of classes.
Readmission
Graduate students who have not been enrolled for more than one calendar year must submit a new application
form and fee, unless other arrangements have been made at the time of withdrawal/leave from the program. The
application will be assessed according to the current admissions policies, and students will be required to fulfill
program requirements in place at the time of readmission.
Continuing Graduate Students
Continuing students will receive registration information and materials on-line prior to the beginning of the
semester. Should this information not arrive for any reason, it is the student's responsibility to contact the office of
Student Affairs for the appropriate materials. Completed registration materials and fees may be submitted to the
Registrar through the mail or in person, two weeks prior to the first week of classes.
Late Registration
Students must follow the registration procedures and timelines printed in the Class Schedule provided at the
beginning of each regular semester. The days of registration and late registration are listed in the Schedule of
Courses mailed to each student prior to the start of the semester by the Registrar. Appropriate fees for late
registration will be assessed.
Add/Drop and Withdrawal from Courses
In order to add or drop a class, the student must obtain a Change of Registration form on-line or from the Health
Sciences Department office, complete and submit it prior to the end of the third week of classes of each semester.
Withdrawal from a course (not the program) requires completion and submission of the appropriate withdrawal form.
Please note that this will not result in an "incomplete" (I) grade.
95
ACADEMIC POLICIES AND PROCEDURES
Course Load
A graduate student at Western University of Health Sciences in the Master of Science in Health Sciences program
must enroll in at least eight semester hours per term to be considered full-time. To be considered full-time when
enrolled in fewer than eight hours, the student must be registered in all remaining courses necessary for completion
of the graduation requirements for the degree.
Reasonable Academic Progress
All students are expected to make reasonable progress each year toward the degree objective. Full-time graduate
students are considered to be making reasonable academic progress when they maintain an overall GPA of at least
3.0 and complete 16 semester hours during the calendar year. Both part-time and full-time students must complete
the graduation requirements within the time limits described under Graduation Requirements.
For part-time students, reasonable academic progress will be determined by the faculty on an annual basis upon
consultation with the student.
Student Rights and Responsibilities
It is the responsibility of the student to be familiar with the contents of the catalog and to observe all policies and
procedures relative to the completion of requirements for the graduate degree that were in effect at the time of initial
enrollment in the specific degree concentration in the Department of Health Sciences.
A student may opt to complete the program of study and degree requirements described in the catalog at the time
of his or her graduation, provided all revised policies of the later catalog are followed. Students are required to keep
the Registrar informed of their current address and telephone number. Forms for this purpose are available in the
Student Affairs office.
Grading System
Official grades are turned in to the Registrar from the Dean of Allied Health Professions, at which time the online
student records system, BanWeb, is updated. Official grade reports and unofficial transcripts will be available on the
BanWeb student records system throughout the academic year. For more information on how to access the BanWeb
student records system, visit the Registrar’s website at http://www.westernu.edu/registrar.
Western University of Health Sciences makes use of letter grades, which may include a plus/minus (+ / -) system
of grading. The Department of Health Sciences makes use of letter grades only. A four-valued letter grade scale will
be given, indicating:
Grade Quality Points
A - Excellent 4
B - Good 3
C - Satisfactory 2
U - Unsatisfactory 0
I - Incomplete 0
Au - Audit 0
W - Withdrawal 0
Cr - Credit 0
NCr - Non-credit 0
Courses are rated at one semester hour for each 12 contact hours. The grade point average is calculated at the end
of each semester as the sum of earned grade points divided by the sum of semester hours passed and failed. A
cumulative grade point average will be calculated and posted on the transcript.
No grade will be changed unless the instructor certifies in writing that an error in computing or recording the
grade has occurred or that the student has completed course requirements for an Incomplete grade or remediated an
Unsatisfactory grade.
Incomplete
An Incomplete grade ("I") will only be assigned to students whose professional commitments and/or personal
responsibilities prevent him or her from completing the requirements of the course. A student may remove an
incomplete by completing course requirements within the following academic semester. Should extenuating
circumstances arise, the student may petition the instructor in writing for a one-semester extension to complete the
96
course work. Prior to the end of the semester in which the original incomplete grade was assigned, the instructor
must approve arrangements for the Incomplete and its removal. The instructor must certify any grade changes.
Academic Standing
An overall grade point average of 3.0 (B) must be maintained during graduate work undertaken at Western
University of Health Sciences in order to qualify for advancement to candidacy. A 2.0 (C) grade earned in any class
may be applied toward graduation only if the overall grade point average at the time of application for graduation
continues at a minimum 3.0 (B) overall grade point average. Any grade below a 2.0 (C) may not be applied toward
graduation. Any student whose grade point average falls below a 3.0 average will be placed on probation.
Graduation Requirements
A 32-unit requirement exists for the award of the Master of Science in Health Sciences degree. A total of 9 credit
hours of Core Master of Science in Health Science courses are required of all MSHS candidates. Students also need
to complete the Required Core credit hours in their degree concentration (15 credit hours for HPE concentration and
14 credit hours for the APAP concentration). The remaining credit hours required for the degree will be taken from
among the selective courses available in the particular concentration.
REQUIRED CORE COURSES, MASTER OF SCIENCE IN HEALTH SCIENCES
Course Number
Course Name Credit Hours Delivery Mode
HSCI 5014 Introduction to Community Health 3 traditional
HSCI 5016 Success Strategies for Distance Learning 1 online
HSCI 5106 Research Methods I 2 online
HSCI 5206 Research Methods II 3 online
Total: 9
HEALTH PROFESSIONS EDUCATION CONCENTRATION REQUIRED CORE
(15 credit hours)
Course Number
Course Name Credit Hours Delivery Mode
HSCI 5100 Teaching and Learning Theory 3 traditional
HSCI 5102 Principles of Instructional Design and Clinical
Teaching 6 traditional
HSCI 5104 Evaluation Methods 3 traditional
HSCI 5108 Instructional Technology 3 traditional
Total: 15
ADVANCED PHYSICIAN ASSISTANT PRACTICE CONCENTRATION REQUIRED CORE
(14 credit hours)
Course Number
Course Name Credit Hours Delivery Mode
HSCI 5000 Pathophysiology 3 online
HSCI 5010 PA Assessment 2 online
HSCI 5012 Pharmacotherapeutics 3 online
HSCI 5071 Advanced Studies in Special Populations I 3 online
HSCI 5072 Advanced Studies in Special Populations II 3 online
Total: 14

97
HEALTH PROFESSIONS EDUCATION CONCENTRATION SELECTIVES
Students will select a minimum of eight (8) credit hours from the following:
HSCI 5071 Advanced Studies in Special Populations I 3 online
HSCI 5200 Historical Issues in Health Professions Education 3 traditional
HSCI 5202 Legal and Ethical Issues in Health Professions
Education 3 traditional
HSCI 5204 Educational Administration/Leadership 3 traditional
HSCI 5208 Special Topics 3 traditional/online
HSCI 5210 Disabilities in the Health Professions 3 traditional
HSCI 5300 Directed Field Experience 1-3 traditional
HSCI 5302 Independent Study 1-3 traditional
HSCI 5999 Thesis/Special Project 3-6 traditional
ADVANCED PHYSICIAN ASSISTANT PRACTICE CONCENTRATION SELECTIVES
Students will select a minimum of nine (9) credit hours from the following:
HSCI 5018 Practicum in Community Health Education 3 online
HSCI 5160 Health Care Delivery Systems 3 online
HSCI 5200 Historical Issues in Health Professions Education 3 traditional
HSCI 5202 Legal/Ethical Issues in Health Professions Education 3 traditional
HSCI 5208 Special Topics 3 traditional/online
HSCI 5999 Thesis/Special Project 3-6 traditional
Time Limits
All requirements for the degree must be fulfilled within five years from the date of initial registration.
Extensions of this time limit may be granted through petition to the faculty.
Advancement to Candidacy
At least one semester prior to when the student plans to complete the unit requirements, he or she must file an
"Application for Advancement to Candidacy”. The Master of Science in Health Sciences degree is awarded
following satisfactory completion of all coursework, including thesis/special project. Names of candidates for
graduation are presented to the Student Academic Progress Committee the Dean of Allied Health Professions, and to
the Western University of Health sciences faculty for approval.
Final Integrative Exercise
The Master of Science in Health Sciences degree is awarded following satisfactory completion of all coursework.
The student select and complete either (1) a thesis, (2) a special project, or (3) a comprehensive examination. Prior
to graduation, the student must complete the Master of Science in Health Sciences graduation requirements options
form and return it to the Chairperson, Department of Health Science.
All students who have completed graduation requirements must attend, in person, and participate in the
Commencement program at which time the degree is conferred. The President may approve exemptions to this
requirement.
Thesis/Special Project Option
A student who selects either the thesis or special project option is responsible for selecting a Thesis/Special
Project Committee. This committee consists of a committee chair and one additional committee member. After a
student has been advanced to candidacy, the candidate is responsible for obtaining and completing the Master of
Science Committee form from the chair of the Department of Health Sciences. Students are responsible for meeting
with the Department of Health Sciences chairperson, who will assist the student in obtaining a thesis/special project
committee chairperson. The committee chairperson must be a full-time employee at Western University with a
faculty appointment in the Department of Health Sciences. Students must also obtain a committee member from the
thesis/special project option. The committee members may be a scholar from outside the University, but must be
approved by the Department Chairperson. The student has five years from the date of matriculation to complete the
Master of Science in Health Sciences degree requirements.
98
Summary
A student will be recommended for the degree of Master of Science in Health Sciences provided he or she:
1. Has satisfactorily completed the 32-unit course requirement in the MSHS curriculum, of which 26 units
must be completed at Western University of Health Sciences in the MSHS degree concentration of their
choice.
2. Has completed one of the following: 1) thesis, 2) special project, or 3) comprehensive examination
3. Is not on probation.
4. Has complied with all the legal and financial requirements of the University as stated in the University
Catalog.
5. Has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined
previously.
6. Attends in person and participates in the commencement program at which time the degree is awarded,
unless special permission has been granted by the President of the University. If the President grants special
permission to be excused from graduation, the graduate may be required to present himself or herself to the
Dean at a later date to receive his or her diploma.
TUITION AND FEES
Schedule of Fees
$225 Unit cost per semester hour (32 semester hours minimum for MSHS degree)
Other Fees and Expenses
$35. Application Fee
$50. Continuous Registration Fee
$30. (per day) Late Registration Fee
$10 Lost ID Badge
$5. (each) Copy of Official Transcript
$0.25 (per page) Copy of Student File Material
Tuition and fees are subject to change without notice upon approval by the Board of Trustees. All fees are
mandatory for each student and are non-refundable. Obligation for payment in full of tuition and fees is due upon
matriculation. The Department of Health Sciences can offer a schedule of divided payments for students
demonstrating financial need (for more information see the Bursar).
PROGRAM OF STUDIES
The Master of Science in Health Sciences is designed to be completed in one to two academic years. The
curriculum is multi-disciplinary, with a specialized focus for each degree concentration.
COURSE DESCRIPTIONS
The courses listed below comprise all course offerings of the Department of Health Sciences offered by the
Western University of Health Sciences.
HSCI 5000 Pathophysiology (3 credit hours)
This course integrates basic knowledge of human anatomy and physiology with pathological changes in various
body systems to facilitate the diagnosis and treatment of common, acute, chronic, and complex health problems. The
differential impact of these health problems and their treatment on patients throughout the life cycle (e.g. pediatric,
adult/family, obstetric, geriatric) will also be discussed.
HSCI 5010 PA Assessment (2 credit hours)
The PA assessment course provides prospective Masters students with a means of validating their current
knowledge of Physician Assistant practices. This comprehensive course, which is based on concepts assessed
through the Physician Assistant National Certification Exam or PANCE, may be completed entirely through
independent study, using materials provided over the World Wide Web. This course is open only to Board Eligible
Physician Assistants.
99
HSCI 5012 Pharmacotherapeutics (3 credit hours)
This course presents advanced pharmaceutical principles and practices that will facilitate the PA’s ability to
prescribe and monitor the effects of medications on patients with common, acute, chronic, and complex health
problems.
HSCI 5014 Introduction to Community Health Education (3 credit hours)
This course provides an overview of the development and implementation of patient education programs in the
community and in acute, long-term clinical settings. Models for preparing health education programs will be
presented, including design considerations, appropriate for age, ethnic, cultural, and socioeconomic differences.
Assessment of need, developing objectives, designing learning activities, implementation, and evaluation are
emphasized. Practical application will include the design and implementation of one curriculum unit of instruction
based on a health education subject.
HSCI 5016 Success Strategies for Distance Learning (1 credit hour)
This course is a requirement for all entering students and provides new students with a comprehensive
introduction to Western University’s distance learning courses. Following an overview of the most important
University policies, instructional methods, and resources, the students will have an opportunity to assess their own
readiness for distance learning. Knowledge and skills derived will help ensure successful completion of distance
learning courses.
HSCI 5018 Practicum in Community Health Education (3 credit hours)
This course provides students working in the community with an opportunity to demonstrate their application of
community health education principles in the practice setting. The student will be expected to design a community
health project to improve health care outcomes.
HSCI 5071 Advanced Studies in Special Populations I (formerly PA 5071)
(3 credit hours)
This course surveys issues confronted by health care providers while treating and evaluating patients with
existing disabilities. Topics include the history of disabilities in the health professions, ethics, communication,
language, accessibility, and the responsibilities of health care providers under the Americans with disabilities Act.
Not open to students with credit for PA 5071.
HSCI 5072 Advanced Studies in Special Populations II (formerly PA 5072) (3 credit hours)
This second exploration of special populations builds on themes and concepts presented in HSCI 5071. Not
open to students with credit for PA 5072.
HSCI 5100 Teaching and Learning Theories (formerly HPE 5100) (3 credit hours)
This survey course is designed to introduce the student to teaching and learning theories as they apply to the adult
learner. The interrelationship between learning and teaching styles and how these impact the learning environment
are covered. Teaching methods and strategies designed to enhance classroom learning in the health professions are
emphasized. The design of practical learning activities is underscored. Not open for students with credit for HPE
5100.
HSCI 5102 Principles of Instructional Design and Clinical Teaching (formerly HPE 5102)
(6 credit hours)
This course is designed to provide the student with the skills needed to develop educational programs in the
health professions and incorporating the role of the clinical instructor. Practice is given in applying descriptive
principles of teaching and learning to the design of a unit of instruction. Included will be the construction of a needs
assessment, data analysis, writing instructional objectives, defining instructional strategies, designing learning
activities, selecting media and planning evaluation. Not open for students with credit for HPE 5102.
100
HSCI 5104 Evaluation Methods (formerly HPE 5104) (3 credit hours)
The purpose of this course is to assist the student to acquire the skills necessary to conduct student performance
and program evaluations. Measurement of student performance in the formal educational and clinical setting includes
construction and use of written examinations, simulations, rating scales, chart audits, observation techniques, and
other measures of cognitive, affective and psychomotor behavior. Included is an overview of procedures for item
analysis and test validation. Not open for students with credit for HPE 5104.
HSCI 5106 Research Methods I (formerly HPE 5106) (2 credit hours)
This introductory course is designed to prepare the health professions student to understand principles for the
analysis and interpretation of quantitative data in health professions education research. It will include measurement
theory, the graphical presentation of data, probability theory, and the use of descriptive and inferential statistics in
the interpretation of data. As a result, the student will be able to read original research reports in a more critical
manner. Not open for students with credit for HPE 5106.
HSCI 5108 Instructional Technology (formerly HPE 5108) (3 credit hours)
This course provides an overview of the principles and applications of instructional media in the realm of adult
and health education settings. The goal of this course is to provide for competence in the planning, selection and use
of various forms of instructional technology for health care training programs. Emphasis will be made on an
understanding of the principles of teaching and learning. Utilizing those principles, practical applications will be
addressed, including the design and development of various instructional approaches as well as the appropriate
selection and application of the various media forms. Students will function as members of a seminar, will produce a
media-based instructional presentation and will write a limited research paper on current trends in instructional
technology applications. Not open for students with credit for HPE 5108.
HSCI 5160 Health Care Delivery Systems (formerly PA 5160) (3 credit hours)
This course provides an overview of the American health care system in regards to health finance and the quest
for quality care. Special emphasis is given to the emergence of managed care and its subsequent impact on
contemporary health care planning, delivery and evaluation. In addition, the course introduces the need for, and
tools currently available for measuring, quality health care in this country. Case management and disease
management are introduced as strategies for achieving cost-effective, high quality care. Not open for students with
credit for PA 5160.
HSCI 5200 Historical Issues in Health Professions Education (formerly HPE 5200)
(3 credit hours)
This course provides a survey of the historical development of issues in health care, including early types of
medicine and medical education in antiquity through contemporary issues in health professions education. Not open
for students with credit for HPE 5200.
HSCI 5202 Legal/Ethical Issues in Health Care (formerly HPE 5202)
(3 credit hours)
This course will introduce the student to the ethical and legal challenges of modern heath care and health care
education. Insight into the basic ethical and philosophical concepts involved in health care education will be stressed.
The historical background on laws that define the roles and responsibilities of health care professionals and
educators will be presented. Students will be given the opportunity to explore personal values regarding a variety of
issues facing health care workers and educators today. Not open for students with credit for HPE 5202
HSCI 5204 Educational Administration/Leadership (formerly HPE 5204)
(3 credit hours)
This course will introduce the student to selected management theories. Leadership styles will be emphasized.
Motivation and human behavior theories related to the functions of health care organizations, including the
development of human resources and fiscal responsibilities, will be stressed. Trends in health care management will
be surveyed. Not open for students with credit for HPE 5204.
101
HSCI 5206 Research Methods II (formerly HPE 5206) (3 credit hours)
The purpose of this course is to introduce students to a variety of research methodologies employed in both
clinical and educational settings. Included will be historical studies, case studies, observational studies, the survey,
quasi-experimental designs, and experimental designs. Generalizability issues and validity/reliability issues related to
research are presented. Prerequisite: HSCI 5106 or equivalent. Not open for students with credit for HPE 5206.
HSCI 5208 Special Topics (formerly HPE 5208) (1-3 credit hours)
This format is designed to permit in-depth study of a single issue in health professions education. Current issues
and/or trends may be included.
HSCI 5210 Disabilities in the Health Professions (formerly HPE 5210) (3 credit hours)
This is an introductory course presenting issues involved in educating health professions students with cognitive,
physical and sensory disabilities. Topics include history and culture of disabilities in the health professions, assistive
technology, legal aspects, and communication. Not open for students with credit for HPE 5210.
HSCI 5300 Directed Field Experience (formerly HPE 5300) (1-3 credit hours)
This course is designed for health professionals who are teaching in a classroom/clinical/laboratory setting. Under
the supervision of MSHPE faculty, students will design and implement instruction appropriate to the learning
environment in which they are participating. Three to four lectures represent one semester credit hour. Self
evaluation and revision of presentations are required. Student may enroll up to a maximum of 3 credit hours per
semester, repeatable to a maximum of 6 credit hours. Not open for students with 6 or more credits of HPE 5300.
Graded Cr/NCr.
HSCI 5302 Independent Study (formerly HPE 5302) (1-3 credit hours)
Registration in this course permits students, under MSHPE faculty supervision, to contract for special
educational projects or readings in education which relate to individual professional needs and interests. A
maximum of 3 credit units may be taken per semester, repeatable to a maximum of 6 credit hours. Not open for
students with 6 or more credits of HPE 5302. Graded Cr/NCr.
HSCI 5999 Thesis/Special Project (formerly HPE 5999) (3-6 credit hours)
This course allows the student to prepare and complete a scholarly thesis or special project under the supervision
of an assigned faculty member. Open only to students who select the Thesis or Special Project options for the Final
Integrative Exercise. Not open for students with credit for HPE 5999. Graded Cr/NCr.
HONORS AND AWARDS
The following awards are presented annually at the University’s Honors Day ceremony in April:
President’s Society Award
Guy M. Allmond Scholarship Fund
Linda Fox Memorial Endowment Fund
The following awards are presented annually at the University’s commencement dinner:
Dean’s Award
Don and Jean Griva Memorial Award
102
Academic Calendar 2002-2003
Fall 2002
Monday, Sept. 9, 2002
Classes begin
Friday, Sept. 20, 2002
Last day to Add/Drop class
Monday, October 7, 2002
Columbus Day observed (no class)
Wednesday, Nov. 27, 2002
Thanksgiving recess (noon)
December 2, 2002
Classes resume
December 2-13, 2002
Registration for Spring 2003
December 20, 2002
Last day of Fall class
Last day to for advancement to Candidacy
Spring Semester
January 6, 2003
Classes begin
January 20, 2003
Martin Luther King Day (no classes)
January 24, 2003
Last day to Add/ Drop classes
February 17, 2003
President’s Day
March 17, 2003
Spring vacation
March 23, 2003
Classes resume
April 13, 2003
Honors Day
May 2, 2003
Last day for Oral examinations
May 9, 2003
Last day of classes
TBA
Commencement

103
COLLEGE OF ALLIED HEALTH PROFESSIONS
Master of Physical Therapy Degree Program
Note: The Department of Physical Therapy is in the final stages of obtaining approval to convert
the Master of Physical Therapy degree program to a Doctor of Physical Therapy program. Once
approved by WASC, offers for acceptance to the published MPT program will be rescinded and
replaced by offers of acceptance for the DPT program. For the 2002-2003 academic year, the
admissions requirements published below for the MPT program will be those of the proposed DPT
program. For additional information about the proposed DPT program, please view the description
at http://www.westernu.edu/cahp/pdf/DPTproposal.pdf.
Accreditation
The Master of Physical Therapy Program in the College of Allied Health Professions is accredited by
the Commission on Accreditation in Physical Therapy Education (CAPTE).
The Practice of Physical Therapy
The physical therapist is a health care provider who is academically and clinically prepared to provide
physical therapy services to individuals with dysfunctions of the neuromusculoskeletal, cardiovascular,
pulmonary and integumentary systems. These services include evaluating and diagnosing movement
dysfunctions, setting goals and determining patient prognosis, planning and implementing treatment
intervention, and reassessing patient progress. In addition, the physical therapist educates the patient/client
to prevent injury, maintain and promote health and wellness. The physical therapist also contributes to
society and the profession through administration, education, consultation, and research.
MPT Degree Program
The Master of Physical Therapy (MPT) Degree program at Western University was initiated in January
1992. The educational philosophy of the program emphasizes student-centered, problem-solving learning
and the role of the physical therapist as a health care provider and a member of the health care team.
Mission of the Program
In keeping with the University's mission, the mission of the Physical Therapy program is to educate
competent, caring, culturally sensitive, reflective practitioners who will:
• participate as members of the health care team to provide high quality care to patients;
• as life-long learners, acquire, analyze, synthesize and apply knowledge in new settings;
• contribute to the verification of physical therapy evaluation and intervention techniques, and discover
new, more effective methods of patient care;
• be leaders in providing health care service and education to promote health and fitness of community
members; and
• play important roles in developing health policy and appropriate standards for physical therapy
practice.
Program Goals
The graduate of the MPT program will be a mature individual whose professional education is based
on a foundation of the requisite preparation in the biological, behavioral and social sciences, and
humanities. The graduate will have the necessary knowledge, skills and attitudes to function as a clinician
generalist; will have an appreciation for the value of all aspects of the research process; and will be a
responsible member of the community and the profession. Upon completion of the educational program in
physical therapy, the graduate will be able to:
• Have an understanding of the osteopathic philosophy with its emphasis on caring for, and appreciation
of the patient as a whole person;
• Demonstrate respect for all individuals;
104
• Practice physical therapy as an entry-level clinician generalist by assuming responsibility for the
components of that role;
• Communicate with peers, colleagues, patients, clients, family members and the community-at- large in
a style that is commensurate with their level of understanding;
• Appreciate the place of research in the advancement of physical therapy;
• Serve as a role model for healthy behaviors in both the clinical setting and community;
• Participate in the community as a representative of the physical therapy profession, as an advocate for
the patient or client in a health care environment, and as a concerned citizen;
• Continue lifelong learning through continuing education, specialization and participation in
professional organizations; and
• Establish priorities in order to maintain a balance between personal and professional life.
Description of the MPT Program
The curriculum for the Master of Physical Therapy Program will prepare the graduate to be a PT
generalist. The curriculum consists of modules, each having a particular emphasis.
Curriculum Design
The MPT program is two years plus 16 weeks in length. Didactic education, which includes classroom
and PT laboratories to practice procedures on classmates, is followed by clinical education assignments in
a wide variety of clinical settings. Year I consists of two 15-week modules and one 18-week module.
Clinical Practicum I is a component of Module III.
Year II consists of the following activities: a 12-week didactic education phase followed break a
Clinical Practicum II for 12 weeks; a five week break followed by one 12 week and one ten week didactic
period.
Year III (the final phase) consists of a Clinical Practicum for 12 weeks, followed by four weeks of
elective courses given in the continuing education format. Students will give research presentations to the
faculty and the PT community during this final four weeks on campus.
MPT students will complete their education in May and participate in the University-wide June
graduation. State licensure examinations are now computerized and can be taken following completion of
the program.
The faculty includes scholars, researchers, administrators and clinicians from the professions of
physical therapy, psychology, education, osteopathy, medicine and the basic sciences. All faculty are
committed to the preparation of the Master of Physical Therapy professional who will be well versed in all
aspects of physical therapy and dedicated to their profession and to the patients they serve.
PERSONAL COMPETENCIES FOR ADMISSION AND MATRICULATION
A candidate for admission to the MPT program must have the use of certain sensory and motor
functions to permit them to carry out the activities described in the sections that follow. Graduation from
the program signifies that the individual is prepared for entry into clinical practice. Therefore, it follows
that graduates must have the knowledge and skills needed to function in a broad variety of clinical
situations and to render a wide spectrum of physical therapy evaluation and treatment techniques. The
candidate and student must be able to consistently, quickly, and accurately integrate all information
received by whatever sense(s) are employed. Also, they must have the intellectual ability to learn,
integrate, analyze, and synthesize data.
Examples of essential functions of a physical therapist include, but are not limited to:
a. Use appropriate verbal, non-verbal, and written communication with patients, families, and others.
b. Determine the physical therapy needs of any patient with potential movement dysfunction.
c. Safely, reliably, and efficiently perform appropriate physical therapy procedures used to assess the
function of the movement system.
d. Perform treatment procedures in a manner that is appropriate to the patient's status and desired
goals.
105
A candidate for MPT ordinarily must have abilities and skills of five varieties including (1)
observation; (2) communication; (3) motor; (4) intellectual, conceptual, integrative and quantitative; and
(5) behavioral and social. Where technological assistance is available in the program, it may be permitted
for disabilities in certain areas. Under all circumstances, a candidate should be able to perform all physical
therapist functions at entry-level competency in a reasonably independent, timely manner.
1. Observation: Candidates and students ordinarily must have sufficient vision to be able to observe
demonstrations and laboratory exercises. They must be able to observe a client accurately at a distance
and close at hand.
2. Communication: Candidates and students ordinarily must be able to communicate with clients and
colleagues. They should be able to hear, but if technological compensation is available, it may be
permitted for some people with disabilities in this area. Candidates and students must be able to read,
write, and communicate verbally in English.
3. Motor: Candidates and students ordinarily should have sufficient motor function such that they are
able to execute movements reasonably required to provide assessment and physical therapy treatment
procedures to clients.
Examples of reasonable required assessment procedures include, but are not limited to:
a. Functional abilities
b. Pain
c. Gait
d. Strength
e. Joint motion & stability
f. Balance
g. Movement patterns
Examples of reasonably required treatment procedures include:
a. Balance training
b. Exercise techniques
c. Gait training
d. Activities of daily living training and functional activities
These actions require coordination of both gross and fine muscular movements, equilibrium and
functional use of the senses of touch and vision. The role of the physical therapist often requires upright
posture with sufficient upper and lower extremity strength, as well as overall body strength; therefore,
individuals with significant limitations in these areas would be unlikely to succeed.
4. Intellectual, Conceptual, Integrative, and Quantitative Abilities: These abilities include measurement,
calculation, reasoning, analysis, and synthesis. Problem solving, the critical intellectual skill demanded
of a physical therapist, requires all of these intellectual abilities. In addition, candidates and students
should be able to comprehend three-dimensional relationships and understand the spatial relationships
of structures.
5. Behavioral and Social Abilities: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgment, the prompt completion of
all responsibilities attendant to the assessment and care of clients, and the development of mature,
sensitive, and effective relationships with clients. Candidates and students must be able to tolerate
physically taxing workloads, adapt to changing environments, display flexibility, and learn to function
in the face of uncertainties inherent in the clinical problems of many clients. Compassion, integrity,
concern for others, interpersonal skills, interest, and motivation are all personal qualities to be assessed
during the admissions and educational processes.
The MPT program, along with all other programs at Western University of Health Sciences, shares a
commitment to develop creative ways of opening the MPT curriculum to competitive, qualified disabled
individuals. In doing so, however, the MPT program must maintain the integrity of its curriculum and
preserve those elements deemed essential to educating candidates to become effective physical therapists.
106
ADMISSIONS POLICIES AND PROCEDURES
Western University will accept applications for admission from all qualified candidates. Western
University is committed to admitting competitive, qualified disabled individuals. For technical guidelines,
please see above.
Application Requirements
The applicant must have earned a BA or BS degree from a regionally accredited college or university
by the time he/she matriculates in the MPT program. The minimum acceptable grade point average in
overall science and in the baccalaureate degree is 2.5 on a 4.0 scale. Exception: the undergraduate GPA
requirement of 2.5 will be waived for applicants who have attained a GPA of 3.0 or above in 15 or more
post-graduate units or who have been awarded a master's degree with a minimum GPA of 3.0.
The MPT program is looking for students who come from a broad, liberal arts background with the
baccalaureate degree being obtained in any field of study other than physical therapy. A high degree of
intellectual curiosity and accomplishment along with excellent verbal and written communication skills
need to be evident in the applicant. The graduate of Western University will be able to problem-solve in
clinical practice and will also be able to communicate appropriately with the client about the client/patient
care plan.
1.Prerequisite Courses
English Composition - 1 course (minimum of 3 semester units or 4 quarter units)
Psychology - 2 courses, must be out of the Psychology Department (minimum of 3 semester units
each or 4 quarter units each)
Statistics - 1 course, only statistics courses that are cross listed in math, statistics or biometry will
be accepted (minimum of 3 semester units or 4 quarter units)
Human Anatomy - 1 course of lecture and lab (minimum of 4 semester units or 6 quarter units)
Human Physiology - 1 course of lecture and lab (minimum of 4 semester units or 6 quarter units)
General Chemistry - a full course sequence of lecture and lab (minimum of 8 semester units or 12
quarter units)
Physics - a full course sequence of lecture and lab – emphasis on light, heat, sound, and electricity
(minimum of 8 semester units or 12 quarter units)
Anatomy and Physiology must be taken out of the Anatomy, Physiology, A&P, Biology or Zoology
departments. The Anatomy and Physiology must be "human." Combined Anatomy and Physiology courses
will be considered only if a combined course sequence is completed.
Grades of "C" or better are required in each prerequisite course. A grade of "C-" in any prerequisite
course is not acceptable. No prerequisite course work may be taken on a pass/no pass or credit/no credit
basis. For courses completed in California, all science prerequisites must be University of California (UC)
or California State University (CSU) transferable.
Three prerequisite courses may be in progress at the time of application during the spring, summer or
fall semester or quarter. Please submit official transcripts directly to the Admissions office upon
completion of course work in progress. Final transcripts and/or final grades (including degree verification)
for all course work in progress must be received prior to registration date in January.
2. Graduate Record Examination (GRE) Score Report
Official GRE Score Report must be mailed directly to Western University from Educational Testing
Service (ETS). It is expected that applicants will have a combined minimum score of 1500 on the three
sections of the GRE.
3. Clinical Experience
Credit will be given for up to 500 hours of volunteer or work experience in a variety of physical
therapy settings. Extra credit will be given for different types of settings, provided that at least 100 hours is
spent in each setting. Types of settings may include acute hospital, outpatient, rehabilitation, pediatric and
home health. Preference will be given to applicants who have experience at more than one setting.
4. Recommendations
Three satisfactory recommendations (forms provided) are required as part of the admissions
application. We require one academic recommendation, one from a physical therapist, and the third
recommendation may be academic or from a physical therapist.
107
Application Procedures and Deadline
The MPT program has a January matriculation date. The application postmark deadline is September 1.
The Department of Physical Therapy will make admissions decisions on a rolling basis. They will review
applications, conduct interviews and make admissions decisions throughout the admissions cycle. We
encourage students with complete application packets to apply early. Applicants who cannot attend and
wish to reapply for the following year will be considered with the new applicant pool.
To request an information brochure and/or an application, contact the admissions office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 469-5541
In addition to submitting an application, the applicant must submit a non-refundable application fee of
$60, three letters of reference, academic/professional record form, work experience form, a written
personal statement, and official transcripts from all colleges attended. After receipt of the packet, the
Admissions Office will evaluate the applicant's transcripts to ascertain the science and baccalaureate grade
point average.
Applicants who wish to use course work completed outside of the United States must submit their
transcripts for evaluation to World Education Services, Josef Silny and Associates, Educational Credential
Evaluators, Inc., or International Education Research Foundation, Inc. A course-by-course evaluation is
required and all course work must be designated as undergraduate, graduate or professional. Western
University will only honor evaluations from the above services. The evaluation must be included with the
application packet.
The Admissions Committee reserves the right to select potential candidates for personal interviews.
These interviews are designed to allow the applicant to learn more about Western University's MPT
program as well as allow the Admissions Committee to learn about the applicant. The interview process is
conducted at various times throughout the admissions cycle.
Decisions of the Admissions Committee regarding the admission of applicants to the Master of
Physical Therapy program are final.
Registration
MPT students are required to register by the date established by the Registrar. Failure to register may
be grounds for dismissal. Full tuition and fees and all prior debts must be paid in full on or before the
registration deadline each academic year. Matriculation is subject to satisfactory completion of all
academic requirements and payment of all outstanding debts to the University. Prior to registration, the
receipt of final transcripts from undergraduate colleges, a physical examination, and immunizations as
outlined on the physical examination form, are additional requirements for incoming students. Attendance
at Orientation Day is also mandatory for incoming first-year students.
TUITION AND FEES
By action of the Board of Trustees, the tuition and fees effective January 1, 2003, (subject to change)
are as follows:
*$1,250 Tuition Deposit for incoming students
(Payable two weeks after acceptance)
**$500 Enrollment Deposit
(Students returning from leave of absence only -
Due by October 15)
$27,690 Total Tuition Annual
$9,230 Final Phase - Year III
$40 Student Body Fee, year I and II MPTs,
covers student council, social activities, public relations.
$20 Student Body Fee, final phase MPTs.
108
*Upon matriculation, the entire $1,250 is applied toward the total tuition.
**For accepted candidates who are students returning from leave of absence, a $500 enrollment deposit
is due October 15 prior to enrollment. The deposit is nonrefundable and credited toward tuition upon
enrollment.
Tuition and fees are subject to change without notice upon approval by the Board of Trustees. All the
above-listed fees are mandatory for each student and are nonrefundable.
Other Fees and Expenses
$500 Required and Recommended Texts
$10 (per day) Late Registration Fee
$40 Lost Locker Key
$10 Lost ID Badge
$5 (each) Copy of Official Transcript
$10 (each) Copy of Official Transcript Faxed
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
ACADEMIC REQUIREMENTS
Academic Advisement Policy
Students will be assigned a faculty advisement upon matriculation. Advisement by faculty should be
viewed by the student as a part of the academic process. If either the student or faculty member does not
find the relationship helpful, either is free to seek a change. This request should be made to the
Department Chair.
It is the student’s responsibility to meet periodically with his/her advisor. A student on probation must
meet with his/her faculty advisor at least once a month.
Standards of Academic Performance
Good academic standing implies that a student maintained a minimum GPA of 2.70 or higher.
All grading and evaluation is based on the student's ability to attain the competencies within the
objectives outlined for each area of study.
A student whose performance falls below the minimum acceptable standard(s) for any area of study
will be notified of such deficiency by the instructor of the course and Department Chairperson as soon as
evidence of such substandard performance is available.
Grade Scale/Grade Points/Class Ranking
The following academic standards and grading scale applies to students enrolled in the Physical
Therapy Program:
Percentage Letter Grade Grade Points
93 - 100 A Excellent 4.0
90 - 92 A- Excellent 3.7
87 - 89 B+ Good 3.3
83 - 86 B Good 3.0
80 - 82 B- Good 2.7
77 - 79 * C+ Passing, but below required overall GPA 2.3
73 - 76 * C Passing, but below required overall GPA 2.0
Below 73 U Unsatisfactory 0
NCr No Credit 0
Cr Credit 0
I Incomplete 0
M Missing 0
Au Audit 0
W Withdrawal 0
109
* A "C" or "C+" grade in and of itself is a passing grade. However, a "C" or "C+" grade is below the
required overall grade point average of 2.7. If the number of "C's" and "C+'s" totals an amount to bring the
student's GPA to below 2.7, the performance, based on professional expectations, is considered
unsatisfactory.
Clinical Practica Grades Cr Satisfactory Performance/Completion
of clinical practicum assignment
NCr Unsatisfactory Performance/Completion
of clinical practicum assignment
Official grades are turned in to the Registrar from the Dean of Allied Health Professions, at which time
the online student records system, BanWeb, is updated. Official grade reports and unofficial transcripts
will be available throughout the academic year. For more information on how to access the BanWeb
student records system, visit the Registrar’s website at http://www.westernu.edu/registrar.
Credit Hours
Courses are rated at one credit hour for each 12 hours of lecture or 24 hours of laboratory and/or
practice sessions. Credit hours of 1.0 will be assigned for each week of Clinical Practica experience. A
cumulative grade point average will be calculated and posted on the transcript.
The grade point average will be calculated at the end of each Module and if a course is repeated, only
the last grade earned enters into the computation of the grade point average, but the original grade remains
on the student's transcript.
No course grade will be changed unless the instructor certifies in writing to the Registrar that an error
in computing or recording the grade occurred. If the student believes there is just cause to dispute a grade
for a course, the procedure is as follows:
a. If the student has reason to dispute the grade, it should be done in writing within five (5) working
days to the Department of Physical Therapy Education Chairperson. Upon written request from the
student, the Department Chairperson shall review the case with the instructor(s) and a decision shall be
made by the course instructor(s) to affirm or modify the grade. Within seven (7) working days the
Department Chairperson shall notify the student in writing of the decision. A copy of the letter shall be
sent to the appropriate faculty member(s). The faculty member(s) has the sole responsibility to make
the official grade change.
b. If the student is not satisfied with the outcome of the grade dispute procedure to the Department
Chairperson, the student may then appeal in writing to the Dean of the College of Allied Health
Professions within five (5) working days. The Dean of the College of Allied Health Professions shall
review the case with the student, Chairperson of the Department of Physical Therapy Education and the
course instructor(s) and a decision shall be made by the course instructor(s) to affirm or modify the
grade. Within seven (7) working days the Dean shall notify the student in writing of the decision. A
copy of the letter shall be sent to the appropriate faculty member(s) and Chairperson. The faculty
member(s) has the sole responsibility to make the official grade change.
Evaluation
a. General: The modules/trimesters of the program are designed so that students' work toward
achievement of competencies is measured by written and practical examinations and by evaluations of
clinical performance and professional development. Specific behavioral objectives are defined for
each modular component to assist the students and the faculty members in evaluating the degree of
attainment of the objectives throughout the 28-month curriculum.
b. Evaluation Methods: Overall student performance is evaluated during each phase using one or a
combination of the following methods:
1. Written examinations: Written examinations will vary based on the content of the individual
course. A combination of multiple choice, matching, true/false, short answer, essay and patient
problem solving questions are used.
2. Practical or Laboratory Examinations: In selected courses, students will be observed
performing components of physical therapy practice activities on lab exams. They also may be
110
asked to "problem solve" based on a patient database, and in some cases students will be
videotaped for self-evaluation.
3. Student Presentations: Students may be asked to orally present individual or group projects,
patient cases, research papers, etc. These oral presentations may or may not be accompanied by a
written report.
4. Written reports: At various times, students will be evaluated on written reports of assigned
topics, SOAP notes, evaluations, treatment plans and home programs.
5. Clinical Evaluations: Supervising Clinical Instructors are asked to assess the student's level of
attainment of competencies related to selected parameters within the domains of knowledge, skills
and attitudes, and to evaluate the student's overall performance while on Clinical Practica. The
Clinical Performance Instrument (CPI), which incorporates entry-level physical therapist clinical
performance criteria, is utilized.
Students are responsible for securing their CPI or other evaluation tools from the Center
Coordinator of Clinical Education/Clinical Instructor (CCCE/CI) on each practicum and ensuring
that it is completed and returned to the Director of Clinical Education after each practicum.
CCCE/CI's are encouraged to discuss the student's performance and progress throughout the
clinical assignment and to discuss the final evaluation prior to completion of the practicum. The
CI will indicate whether the Clinical Practicum was a successful experience in accordance with
designated objectives, or was unsuccessful in meeting clinical objectives. While the CI may
recommend success or failure of the Clinical Practicum, the Director of Clinical Education
determines and administers the actual course grade.
c. Grade Reports: Final grade reports are available on the BanWeb student records system.
Due to the nature of the curriculum, modular/trimester completion dates do not coincide with
traditional grading periods.
In some courses when final grades are not available at grade reporting time, a grade of "M"
(Missing) is submitted to the Registrar in lieu of the course grade. "M" grades are entered on the grade
reports and are converted to student achieved grades at the earliest possible opportunity. An up-to-date
summary of student performance is maintained in the Department Office and is available to each
student for review.
d. Review of Examinations: Examinations are graded as soon as possible and are kept on file for
student review. Student performance in clinical courses is monitored closely by the Director of Clinical
Education. Students whose performance in any portion of the curriculum is determined to be
unsatisfactory are notified of such substandard performance as soon as it can be determined.
Professional Performance
a. Ability-based Assessment: The faculty supports the concept of development of professional
behaviors throughout the program. These behaviors include: (1) commitment to learning; (2)
interpersonal skills; (3) communication skills; (4) effective use of time; (5) use of constructive
feedback; (6) problem solving; (7) professionalism; (8) responsibility; (9) critical thinking; and (10)
stress management.
Professional behavior is vital to the success of each student, the Western University Physical
Therapy program, and the Physical Therapy profession. The process of becoming an effective physical
therapist involves attaining competency in professional knowledge, skill, and behavior. Thus, the ten
generic abilities that exemplify the professional behaviors valued by the physical therapy profession
will be used as a guide throughout this program. To facilitate development of competency in the
generic abilities, the faculty will provide the students opportunities to practice them and formal and
informal feedback throughout the program. The student will be responsible for ongoing self-
assessment and for seeking feedback from faculty and fellow students.
Students’ progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behavior and attitudes. At the completion of
each module/trimester/year of the program and before the student is allowed to progress to the next
module/trimester/year, the student’s record of achievement is reviewed by the faculty. The quality of
professional behavior expected of Western University MPT graduates is exemplified by the generic
abilities and the three levels of associated behavioral criteria. Satisfactory progress is demonstrated by
111
exhibiting beginning-level criteria by the end of the first year, developing-level criteria by the end of
the second year, and entry-level criteria by the end of the final clinical practicum.
The faculty determines if the student has demonstrated the knowledge, skills, and attitudes
necessary to be eligible for progress for the next module/trimester/year. In special instances, the
faculty may be convened at other than scheduled times to consider cases of unusual circumstances, such
as probationary or dismissal cases.
b. Attendance: Students are expected to attend all scheduled activities and observe the following
policies:
Excused Absences
1. All unanticipated absences due to illness, accident, other unexpected events must be reported
immediately to the department secretary and course instructor.
2. Absences requested for physician/dentist appointments for student or dependents will be
considered excused only if requested in advance of the appointment. Due to the intense nature of
the curriculum, students are encouraged strongly to schedule appointments for days when classes
are not held, evenings, or Saturdays.
3. All anticipated absences for any reason, regardless of length, must have the prior approval by
the Faculty to be considered excused.
4. Students on Clinical Practica are responsible for notifying their supervising CI, CCCE, and the
Director of Clinical Education regarding all absences, whether anticipated or unanticipated.
Unexcused Absences
1. Any discovered or reported absence for which the Chairperson/Faculty does not have an
explanation will be considered unexcused.
2. Students whose absence is determined to be unexcused will be required to provide an
explanation regarding the circumstances involved. The Chairperson/Faculty will determine if the
absence remains unexcused.
3. Unexcused absences may be sufficient cause for placing a student on professional probation
and continued unexcused absences may be grounds for dismissal from the program.
4. Absences on the first or last day of a module/trimester or Clinical Practicum, or on the day
before or after a scheduled break, vacation, or weekend, are considered unexcused unless prior
written approval has been granted. If such an absence is the result of a sudden unavoidable
circumstance, the Department Chairperson should be notified as soon as possible and provided
with an explanation for the absence.
c. Student Examination Policy
1. Students are not to communicate in any way during examinations and are to face the front of
the classroom at all times.
2. During scheduled examination hours, students are highly discouraged from going to the
bathroom, but will be allowed to go one at a time. Student will be required to turn in the exam
and Scantron® sheet as he/she leaves the room.
3. Once a student finishes an exam, the student will turn in the exam and the Scantron® form to
the proctor, and after he/she leaves the examination room, he/she will not be permitted to re-enter
the room until the exam is declared over.
4. All students' belongings, i.e., notebooks, calculators, and headsets, etc., will be kept in front of
the room.
5. Questions will be answered at the discretion of the proctor during the examination period.
Students should be permitted to point out typographical or other errors present in the examination
to the proctor.
6. Alternate seating shall be utilized for all examinations unless precluded by space availability.
7. Violations of these examination policies or of Standards of Professional Conduct will be
brought before the Student Conduct Committee.
Student Academic Progress Committee
a. The Student Academic Progress Committee of the College of Allied Health Professions is
comprised of Department Chairs, the Dean of Student Affairs/Registrar and elected faculty members.
112
b. Each year, the Student Academic Progress Committee shall review as needed the academic
achievements and the performance of all students. The names and grades of students in academic
difficulty shall be made available to the Student Academic Progress Committee by the Department
Chair.
c. After reviewing a student’s achievement and performance records, the Student Academic Progress
Committee may recommend to the Dean of Allied Health Professions any of the following courses of
action for a student: Promotion, probation, remediation, dismissal from the University, psychological
and educational assessment and recommendation, or no action.
d. The Student Academic Progress Committee also has the responsibility of recommending to the
Faculty as a whole the awarding of the degree of Master of Physical Therapy upon satisfactory
completion of all requirements for graduation as stated in the Catalogue.
e. All recommendations of the Student Academic Progress Committee shall be made in writing to the
Dean of Allied Health Professions, who will make a final decision and inform the student in writing.
Promotion
Promotion is defined as progression from one academic year to the next.
a. A student will be recommended to the Dean of the College of Allied Health Professions for
promotion by the Student Academic Progress Committee.
b. A student may not be recommended for progression from one academic year to the next with any
outstanding grades of “I” or “U” on his/her academic record or with a yearly grade point average of
less than 2.7.
c. When considering a student for promotion, professional, ethical, and personal conduct may also be
taken into consideration.
d. A student will be promoted provided that all legal and financial requirements of the University as
stated in the Catalogue have been satisfied.
Graduation
A student will be recommended for the degree of Master of Physical Therapy provided he/she:
a. Has satisfactorily completed all required courses at the University in the MPT curriculum.
b. Is not on probation and has completed all prescribed academic and clinical education requirements
with a cumulative grade point average of at least 2.7 and has no outstanding grade of “I” or “U,” or
“NCr” in a required course.
c. Has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined
previously.
d. Has complied with all the legal and financial requirements of the University as stated in the
Catalogue.
e. Unless special permission has been granted by the President of the University, all students must
attend in person and participate in the Commencement program at which time the degree is conferred.
If the President grants special permission to be excused from graduation, the graduate may be required
to present himself or herself to the Provost or appropriate Dean at a later date in order to take the
required oath (if relevant) to receive his or her diploma.
Academic Warning
The student who demonstrates unacceptable performance in any unit of study during any portion of the
program is notified of such performance by the Instructor of the course, as well as the Department
Chairperson, in writing, as soon as it becomes evident. This constitutes an academic warning. Continued
poor academic performance can lead to academic probation and/or dismissal.
Academic Probation
a. Unsatisfactory or No Credit Course Grades
"U" or “NCr” in any required course constitutes a failing grade, and places the student on academic
probation, requiring that the course be remediated or retaken based upon the recommendation of the
course instructor. A grade of “U” or “NCr” in a required course will prevent participation in a clinical
practicum until the course is successfully remediated and requires that the Director of Clinical
Education determine an appropriate clinical placement.
113
1. As in all cases in which remediation of a course is required, this requirement may extend the
length of the program beyond 28 months.
2. The highest grade a student may achieve by obtaining a 73 percent or higher score through
remediation of a course is a grade of "C" or “Cr”. The "C" or “Cr” grade achieved by remediation
of a course will be recorded on the official transcript beneath the original course grade of "U"
(Unsatisfactory) or “NCr” (No Credit).
3. Failure to earn a grade of “C" or “Cr” when remediation of a course is attempted will render the
student subject to dismissal from the program.
4. If a student repeats a course the next time that course is offered in the MPT curriculum, the
student will have that new grade for the course recorded on the official transcript beneath the
original course grade of "U" (Unsatisfactory) or “NCr” (No Credit).
5. Failure to earn a grade of "C" or higher, or “Cr,” on repeating a course of study will render a
student subject to dismissal from the program.
6. A third "U" or “NCr” in required coursework in the program will render a student subject to
dismissal from the program.
b. Module/Trimester/Overall GPA
1. Students must attain a modular GPA of 2.7 and maintain an overall GPA of 2.7. The
Module/Trimester GPA and overall GPA will be calculated at the end of each Module.
2. A student whose modular or overall GPA falls below 2.7 must meet with the Department
Chairperson and the Director of Clinical Education. In order to closely monitor clinical
performance, the Director of Clinical Education will determine the subsequent clinical placement.
3. If the modular or overall GPA falls below 2.7, a student will be placed on academic probation
immediately. Length of academic probation will be determined by the Dean of the College of
Allied Health Professions.
4. If a student attains a modular GPA below 2.7 in two consecutive Modules the student will be
subject to dismissal from the program.
Tutorial Assistance Program
A Tutorial Assistance Program (TAP) has been established at the University to assist students
experiencing academic difficulty. Students will be recommended for this program by a faculty advisor or
professor. The tutors will be chosen from the student body on the recommendation of the faculty of record
for the class.
General Procedures
a. The student may request a tutor by:
1. contacting the course instructor and/or the Department Chairperson,
2. contacting his/her advisor or,
3. going directly to the Learning Enhancement and Academic Development (LEAD) Office.
Student requests will be reviewed by the course instructor and/or the Department Chairperson. Upon
approval, the student will be deemed eligible for services under TAP. Five hours per course is the
maximum number of hours for which a student may be tutored per week.
b. The course instructor may recommend that the student seek a tutor, based upon a poor performance
on a single exam or poor cumulative score.
c. The student’s advisor may recommend that the student seek a tutor, based upon any knowledge he or
she may have about the student’s academic difficulty. In addition, the advisors will receive copies of
letters from the Chairperson to students having academic difficulty.
d. To initiate tutoring following a recommendation or student request for tutoring, the student follows
these steps:
1. The student obtains from the LEAD Office a list of names of tutors available for the course in
which the student is having problems.
2. The student is assigned a tutor by the LEAD Director from the list of available tutors.
3. Once assigned, the tutor and tutee meet with the course instructor to discuss the student’s
specific problems. The instructor should make some recommendations as to what areas the tutor
should emphasize.
4. The tutor and student arrange mutually agreeable times for the tutoring sessions.
114
5. The tutor must have the course instructor sign the time sheet before it is turned in to the LEAD
Office.
Modified Year I MPT Curriculum
The MPT program offers Modified Year I curriculum for students experiencing academic difficulties or
students with disabilities. This modified program extends the regular curriculum by an additional year in
that the first year standing curriculum is spread over a two-year period. Guidelines for this program
include:
a. Potential candidates for the Modified Year I MPT Curriculum will be identified by the midway
point of Module I after midterm examinations.
b. The Modified Curriculum is not an option unless the student manifests serious academic problems
by the midway point of Module I.
c. Recommendation of individual students for the Modified Curriculum shall be made through the
Dean of the College of Allied Health Professions by recommendations from the Department of Physical
Therapy Education Faculty and the College of Allied Health Professions, Student Academic Progress
Committee.
d. The decision to enter the Modified Curriculum is a onetime student option.
e. At the time the student opts for the Modified Curriculum, the modified curriculum will be based
upon courses in which the student is receiving satisfactory grades by midterm of Module I. The
Modified Curriculum will be outlined for the student, so that Year I of the MPT curriculum will be
taken over two years. As the student enters Year II of the curriculum, it is expected that the student
would attend all classes and clinical assignments as defined in the standard curriculum.
f. The student's progress will be monitored carefully each module by the Department Chairperson for
the Department of Physical Therapy Education, College of Allied Health Professions Student
Academic Progress Committee, and the Dean of the College of Allied Health Professions.
g. Students admitted to this program will pay consecutive years of tuition and mandatory fees as if
enrolling in the regular curriculum, and only mandatory fees for the final additional year in the
curriculum.
Professional Probation
Violations of the Standard of Professional Conduct will be dealt with as described under the General
University Academic Policies and Regulations of this catalogue.
Dismissal
A student may be subject to dismissal from the program for substandard academic or professional
performance, as follows:
a. A second grade of "U" or “NCr” in the same required course;
b. A third grade of "U" or “NCr” in required courses in the program;
c. Unacceptable performance on more than one of the clinical practica;
d. Lack of professional or personal attributes considered appropriate for continuance in the program
and profession;
e. Any event that could result either in academic or professional probation for a student currently on
academic or professional probation;
f. Violation of the terms of probation as stated in a letter at the time the student is placed on probation.
Exemption from Individual Course
Students with advanced work or degrees in a particular subject formally may petition the instructor and
the Department Chairperson for credit for an individual course. The petition must include the reasons for
the request and all necessary documentation and must be submitted by the end of the first week of the
course. The student must comply with the attendance policy until notification that exemption has been
granted by the Dean, based upon recommendation of the Department Chairperson. The instructor, before
recommending exemption, may require acceptable performance on an examination. The instructor, in
consultation with the Department Chairperson, may suggest other alternative or additional criteria for
determining exemption.
115
Confidentiality of Medical Records and Health History Information
All data gathered about patients and their illnesses, including all items within patients’ medical histories
are privileged information.
a. Students should not discuss patients’ records in a manner or a situation that would reveal any
information about these patients or their records to persons not involved in their health care.
b. Charts or contents, e.g., lab reports, etc., are not to be removed from the hospital or clinical setting.
Use of Physical Therapy Equipment and Laboratories
The DPTE policy for use of the PT equipment in the PT Skills Laboratories is as follows: No one is to
use the PT equipment except MPT students who have received education and have had practice on the
equipment in the laboratory. These MPT students must be checked out by a faculty member as being
competent to use the equipment. MPT students using the equipment should be doing so in conjunction
with a class they are taking, or in preparation for a clinical practicum, or to conduct a clinical research
project. If equipment is used for a research project, the MPT faculty advisor will be responsible to check
out student competency in using the equipment.
Physical Therapy skills and research labs may be used after regular class hours, with permission of the
Department Chair. Use of these facilities must be scheduled with the Department Chair five (5) working
days in advance of the intended date of use.
CURRICULUM ORGANIZATION
The MPT curriculum is continually evaluated to assure the best educational experience and outcomes.
With this consideration, the following is an outline of curriculum organization. The curriculum sequence
provided below applies to students entering in January 2003.
Year I
Course number Semester Hours
Module I - 15 Weeks
PT 5000 Psychosocial Aspects of Health Care 2.5
PT 5040 Histology and Tissue Healing 2
PT 5070 Patient Care Skills 2
PT 5075 Physical Agents & Procedures 3
PT 5100 Physiology/Pathophysiology 5
PT 5130 Research Methodology in Health Care 3
PT 5220 Principles of Teaching and Learning 2
PT 5230 Clinical Medicine I 2
Total 21.5
Module II - 15 Weeks
PT 5060 Human Morphology & Movement I 7
PT 5065 Human Morphology & Movement II 7
PT 5141 Preparation for Clinical Practicum I 1
Total 15
Module III - 18 Weeks
PT 5015 Physical Therapy in the Health Care System 3
PT 5120 Human Life Sequences 2
PT 5140 Research Statistics in Health Care 2
PT 5200 Differential Diagnosis of Musculoskeletal Disorders 3
PT 5210 Eval. & Treatment of Lower Quarter Musculoskeletal Dysfunction 6
PT 5235 Clinical Medicine II 2
PT 7010 Clinical Practicum I 4
Total 22
Year II
Module IV – 12 weeks
116
PT 5142 Preparation for Clinical Practicum II 1
PT 5205 Eval. & Treatment of Upper Quarter Musculoskeletal Dysfunction 6.5
PT 6020 Principles of Electrotherapeutic Eval. & Treatment 3
PT 6030 Physiology of Exercise 4
PT 6040 Eval. & Treatment of Cardiovascular System 4
Total 18.5
Module V – 12 weeks
PT 7020 Clinical Practicum II 12
Total 12
Module VI – 12 weeks
PT 6000 Neuroanatomy 4
PT 6005 Neurophysiology 4
PT 6010 Eval. & Treatment of Neurological Disorders 8
PT 6070 Prevention & Management of Problems in Adult Aging 3
PT 6075 Prevention & Management of Problems in Pediatric Populations 3
Total 22
Module VII – 10 weeks
PT 5143 Preparation for Clinical Practicum III 1
PT 6050 Principles of Administration and Management 3
PT 6060 Prosthetics, Orthotics and Gait 3
PT 6100 Rehabilitation: Neuromusculoskeletal & Cardiopulmonary 5
PT 6200 Applied Research I 1
Total 13
Year III
Module VIII – 12 weeks
PT 7030 Clinical Practicum III 12
Total 12
Module IX – 4 weeks
PT 6210 Applied Research II 1
PT 6500 Electives 4
Total 5
Graduation – Total Credit Hours 141
The following curriculum schedule applies to student enrolled in the MPT program prior to January
2003.
Year II
Module VI - 12 Weeks
PT 5143 Preparation for Clinical Practicum III 0.5
PT 6000 Neuroanatomy 4
PT 6005 Neurophysiology 4
PT 6010 Evaluation and Treatment of Neurologic
Disorders 8
PT 6020 Principles of Electrotherapeutic
Evaluation and Treatment 4
Total 20.5
Module VII - 12 Weeks
PT 7030 Clinical Practicum III 12
117
Total 12
Module VIII - 12 Weeks
PT 5144 Preparation for Clinical Practicum IV 0.5
PT 6030 Physiology of Exercise 4
PT 6040 Evaluation and Treatment of the
Cardiopulmonary System 4
PT 6050 Principles of Administration and Management 3
PT 6060 Prosthetics, Orthotics and Gait 3
PT 6070 Prevention and Management of Problems in
the Aging Adult 3
PT 6200 Applied Research II 1
Total 18.5
Module IX - 6 Weeks
PT 6075 Prevention and Management of Problems in
the Pediatric Patient 3
PT 6100 Rehabilitation: The Neuro-Musculoskeletal
and Cardiopulmonary Systems 5
Total 8
Final Phase (Year III)
Module X - 12 Weeks
PT 7040 Clinical Practicum IV 12
Total 12
Module XI - 4 Weeks
PT 6500 Electives 4
PT 6210 Applied Research II 1
Total 5
Graduation - Total Semester Hours 144
COURSE DESCRIPTIONS AND CREDIT HOURS
All courses are awarded letter grades, except when indicated otherwise.
PT 5000 Psychosocial Aspects of Health Care (2.5 credit hours)
(Formerly PT 500)
Prerequisite: Acceptance to program. Introduction to the psychological and sociological effects of
acute, chronic, terminal, traumatic and congenital medical problems on the patient, family and therapist;
communication skills including interviews, verbal and non-verbal communication.
PT 5015 Physical Therapy in the Health Care System (3 credit hours)
(Formerly PT 501and 502; Formerly PT 5010 and 5020)
Prerequisite: Acceptance to program. Emphasis on concepts presented in the Guide to Physical
Therapist Practice and the APTA Code of Ethics. Includes a broad perspective of world, nation and state
health care factors, legal aspects of physical therapy practice, and documentation and reimbursement in a
variety of practice settings.
PT 5040 Histology and Tissue Healing (2 credit hours)
Prerequisite: Acceptance to the program. Includes tissue types and composition of organ systems;
structure and function of cells and cellular components related to each body system; collagen formation
and deposition. Discusses process of tissue repair, remodeling and regeneration for each body system,
including cellular responses to injury, inflammatory response and the time frame for healing.
118
PT 5060 Human Morphology and Movement I (7 credit hours)
(Formerly PT 503, 505 and 509; Formerly PT 5030, 5050 and 5080). Prerequisite: Acceptance to
program. This is a fully integrated course on human anatomy and kinesiology. The course includes an
introduction to theoretical and functional principles of human structure with an emphasis on their clinical
relevance and applications. Topics include kinetics, kinematics, manual muscle testing, and evaluation of
gait with an emphasis on normal function. Techniques covered include goniometry, surface palpation and
posture evaluation. Critical review of pertinent published literature will be utilized and will include
electromyographic studies of normal and pathologic movement. Anatomical topics in the first semester
include musculoskeletal, vascular, and nervous structures of the trunk, abdomen and posterior neck with an
emphasis on the form and function of the hypaxial and epaxial regions. The structure and function of the
upper quadrant and thoracic viscera will also be covered. Human cadaver dissection by all participants is
a requirement. Pathology is addressed as an aid in identification of major concepts and to introduce
clinical relevance. Lecture and Laboratory.
PT 6065 Human Morphology and Movement II (7 credit hours)
(Formerly PT 504, 506 and 509; Formerly PT 5035, 5055 and 5080)
Prerequisite: PT 5060. Continuation of PT 5060. Introduction to theoretical principles and clinical
application of kinetics and kinematics of the extremity joints and muscles of the lower quadrant with
emphasis on normal function. Also covers head, neck and abdominal viscera, including cardiovascular,
pulmonary, nervous, digestive, excretory and reproductive systems as relevant. Introduces the structures
of the autonomic and somatic neural systems. Pathokinesiology is addressed as an aid in identifying major
concepts and introducing clinical relevance. Gait analysis and special tests for orthopedic evaluation and
differential diagnosis are integrated with detailed dissection and thorough anatomical study of the limbs.
Lecture and Laboratory.
PT 5070 Patient Care Skills (2 credit hours)
(Formerly PT 507)
Prerequisite: Acceptance to program. Introduction to the physical therapy skills of transfers, gait
training, bed mobility, wheelchair selection and management, cushions, range of motion and monitoring of
physiological responses. Includes medical terminology. Lecture and laboratory.
PT 5075 Physical Agents and Procedures (3 credit hours)
(Formerly PT 508)
Prerequisite: Acceptance to program. Application of sterile technique and universal precautions,
physiologic principles and applications of heat and cold modalities, ultrasound, massage and hydrotherapy.
Includes relaxation techniques. Lecture and laboratory.
PT 5100 Physiology/Pathophysiology (4 credit hours)
(Formerly PT 511)
Prerequisite: Acceptance to program. Human physiology, including homeostasis, cell transport,
endocrine and neural signaling, pain, and body defenses. Emphasis is placed on the physiology of the
major body systems and includes discussion of commonly encountered clinical conditions within each
system. Also includes an introduction to neuroanatomy and neurophysiology.
PT 5120 Human Life Sequences (2 credit hours)
(Formerly PT 510)
Prerequisite: PT 5100. The developmental process from conception to death with the emphasis on
human motor performance. Sequence of study includes fetal life, infancy, early and middle childhood, late
childhood, adolescence, early and middle adulthood, and the aging adult including: neuroanatomical and
neurophysiological mechanisms in relationship to developmental changes in performance, and
musculoskeletal development in relationship to the human life span.
119
PT 5130 Research Design I (2 credit hours)
(Formerly PT 512)
Prerequisite: Acceptance to program. Application of research methods to clinical studies. Examines the
methods used for the objective and systematic study and evaluation of clinical practices.
PT 5140 Research Statistics in Health Care (2 credit hours)
Prerequisite: PT 5130. Application of statistical concepts to analyze quantitative data in health care
research.
PT 5141 Preparation for Clinical Practicum I (1 credit hour)
(Formerly PT 514)
Prerequisite: Acceptance to program. This one hour seminar course will offer an introduction to clinical
education in physical therapy to include an overview of the affiliation agreement. Scheduling and
assignment for Clinical Practicum I will also be incorporated herein. Cr/NCr.
PT 5142 Preparation for Clinical Practicum II (1 credit hour)
(Formerly PT 515)
Prerequisite: PT 5141. This one hour seminar course will continue from PT 5141 on various aspects of
clinical education, including expectations of clinical performance and utilization of the evaluation tool.
Scheduling and assignment for Clinical Practicum II will also be incorporated herein. Cr/NCr.
PT 5143 Preparation for Clinical Practicum III (0.5 credit hour)
(Formerly PT 516)
Prerequisite: PT 5141, 5142. This one hour seminar course will continue from PT 5142 on various
aspects of clinical education including issues of professionalism in the physical therapy field. Scheduling
and assignment for Clinical Practicum III will also be incorporated herein. Cr/NCr.
PT 5144 Preparation for Clinical Practicum IV (0.5 credit hour)
(Formerly PT 517)
Prerequisite: PT 5141, 5142, 5143. This one hour seminar course will continue from PT 5143 on
various aspects of clinical education including the role of the health care team and the licensure process.
Scheduling and assignment for Clinical Practicum IV will also be incorporated herein. Cr/NCr.
PT 5200 Differential Diagnosis of Musculoskeletal Disorders (3 credit hours)
(Formerly PT 522)
Prerequisite: Satisfactory completion of PT 5020, 5060, 5065, 5100 and 5230. Introduction to topics of
pain, medical imaging, pharmacology for musculoskeletal conditions and key clinical pathologies of the
musculoskeletal system. This discussion of pathologies will include epidemiology, etiology and medical
management, including diagnostic tests, laboratory studies, medication and surgical management, and
differential diagnosis.
PT 5205 Evaluation and Treatment of Upper Quarter Musculoskeletal Dysfunction (6.5 credit
hours)
(Formerly PT 523)
Prerequisite: PT 5015, 5040, 5060, 5065, 5100, 5200, 5210, 5230 and 5235. Evaluation and treatment
of neuromusculoskeletal problems of cranio-facial region, cervical spine, upper extremity, and upper trunk,
using a regional approach. Foundational content from PT 5210, including the framework for subjective
and objective examinations, assessment and treatment of patients, is applied to upper quarter body regions.
Common single and multi-region problems are also covered. Lecture and laboratory.
PT 5210 Evaluation and Treatment of Lower Quarter Musculoskeletal Dysfunction (6 credit hours)
(Formerly PT 524)
Prerequisite: PT 5040, 5060, 5065, 5070, 5075, 5100, 5230 and concurrent enrollment n PT 5105,
5200 and 5235. Evaluation and treatment of neuromusculoskeletal problems of the lower extremity and
lower trunk, using a regional approach. Includes foundational topics necessary for evaluation and
120
treatment of neuromusculoskeletal problems such as principles and practice of muscle strengthening,
muscle endurance, muscle stretching, soft tissue mobilization, joint mobilization, and PNF. Other
foundation content includes the framework for the subjective (interview) and objective (physical)
examination of patients, including assessment and treatment. This framework is then applied using
problem-solving and evidenced-based approaches by region, individually and in combination, to the
thoracolumbar spine, sacroiliac joints and pelvis, hip, knee, ankle and foot. Common single and multi-
region problems are also covered, including pathological gait. Lecture and laboratory.
PT 5220 Principles of Teaching and Learning (2 credit hours)
(Formerly PT 530)
Prerequisites: Acceptance to the program. Teaching-learning theory applied to clinical practice with
clients and their families. Includes teaching techniques for being a clinical instructor of presenting in-
services. Final class session includes presentation of micro-teach with self and group evaluations.
PT 5230 Clinical Medicine I (2 credit hours)
(Formerly PT 533)
Prerequisite: Acceptance to program. Introduction to pharmacodynamics and key laboratory values and
their importance in PT decision making. General medical conditions and their epidemiology, etiology,
clinical manifestations, medical management, and issues related to PT examination, screening and
interview are included.
PT 5235 Clinical Medicine II (2 credit hours)
Prerequisite: PT 5230. Continuation of PT 4230. Includes laboratories on physical examination skills
related to visceral structures for purposes of medical screening. Also includes indications for referral to
medical practitioner or other appropriate health care providers. Lecture and Laboratory.
PT 6000 Neuroanatomy (4 credit hours)
(Formerly PT 526)
Prerequisite: Acceptance to the program. Normal anatomy and function of the central, peripheral, and
autonomic nervous systems; laboratory with specimens. Lecture and laboratory.
PT 6005 Neurophysiology (4 credit hours)
(Formerly PT 527)
Prerequisite: PT 5100. Human neurophysiology with emphasis on normal cellular and systemic
functions of the central and peripheral nervous systems.
PT 6010 Evaluation and Treatment of Neurologic Disorders (8 credit hours)
(Formerly PT 528)
Prerequisite: PT 50300, 5035, 5070, 5080; concurrent enrollment in PT 6000, 6005. Systematic
approach to a variety of neurologic problems of the central and peripheral nervous systems. Emphasis is on
the impairments and clinical manifestations of the anatomical lesions, evaluation techniques and
interventions. Lecture and Laboratory.
PT 6020 Principles of Electrotherapeutic Evaluation and Treatment (4 credit hours)
(Formerly PT 529)
Prerequisites: PT 5100, 6000, 6005. Basic concepts in electrical safety and instrumentation, detailed
concepts and applications of electrotherapy introducing principles of electrophysiologic testing and
therapeutic application of electrical stimulation (ES), including strengthening (NMES), re-education, pain
reduction (TENS), tissue repair (ESTR) and iontophoresis. Electrophysiologic testing to include an
introduction to electromyography (EMG), nerve conduction velocity (NCV) and other electrophysiological
tests. Lecture and laboratory.
121
PT 6030 Physiology of Exercise (4 credit hours)
(Formerly PT 531)
Prerequisite: PT 5100. This course addresses bioenergetics as well as the acute and chronic
physiological responses of the human body during exercise and other special conditions. The physiological
basis of therapeutic exercise is the foundation for this course. Lecture and laboratory.
PT 6040 Evaluation and Treatment of Cardiopulmonary System (4 credit hours)
(Formerly PT 532)
Prerequisite: PT 5030, 5100. Introduction to evaluation and treatment of diseases of the cardio-
pulmonary system; includes physiology and pathophysiology, evaluation methods, treatment methods and
prevention. Lecture and laboratory.
PT 6050 Principles of Administration and Management (3 credit hours)
(Formerly PT 534)
Prerequisite: PT 5010, 5020. Organization and administration of a physical therapy department
including budget considerations, hiring-interviewing techniques, marketing, and medical-legal issues.
PT 6060 Prosthetics, Orthotics, and Gait (3 credit hours)
(Formerly PT 538)
Prerequisite: PT 5030, 5035, 5050, 5055, 5080. Evaluation and application of prosthetic and orthotic
devices to physical therapy clients. Evaluation of abnormal and pathological gait patterns. Lecture and
laboratory.
PT 6070 Prevention and Management of Problems in the Aging Adult (3 credit hours)
(Formerly PT 535)
Prerequisite: PT 5000 through 5120, 5200 through 5230, 6000 through 6020; concurrent enrollment in
PT 6030, 6040, 6050. Systematic, problem solving approach to the geriatric client with emphasis on
prevention, etiology, clinical manifestations, evaluation, treatment and resources.
PT 6075 Prevention and Management of Problems in the Pediatric Population (3 credit hours)
(Formerly PT 536)
Prerequisite: PT 5030, 5035, 5070, 5080, 5100, 5120, 6000, 6005, 6010. Systematic, problem solving
approach to the pediatric client with emphasis on prevention, etiology, clinical manifestations, evaluation
and treatment. Lecture and laboratory.
PT 6100 Rehabilitation: The Neuromusculoskeletal and Cardiopulmonary Systems (5 credit hours)
(Formerly PT 537)
Prerequisite: PT 5000 through 5120, 5141 through 5144, 5200 through 5230, 6000 through 6070.
Emphasis is on the various roles of physical therapy throughout the process of rehabilitation. Exposure to
patients with complex problems and special needs is included. There is a potential for off site experience
as a member of a rehabilitation team and work with experts in other medical professions. Experiences
provided to expose students to rehabilitation measures and techniques with real and/or simulated patients.
Lecture and laboratory.
PT 6200 Applied Research I (1 credit hour)
(Formerly PT 540)
Prerequisite: PT 5130, 5135. Individually planned studies under the direction of a senior investigator.
Studies to be pertinent to work in physical therapy. Cr/NCr.
PT 6210 Applied Research II (1 credit hour)
(Formerly PT 541)
Prerequisite: PT 5130, 5135, 6200. Students give presentation of research proposal to PT community.
Cr/NCr.
122
PT 6500 Electives (4 credit hours)
(Formerly PT 539)
Prerequisite: Approval of instructor. Students select from a variety of topics presented in the style of
continuing education courses and attend an average of 12 hours/week for four weeks. Laboratory
experiences may be included. Cr/NCr.
CLINICAL PRACTICA
PT 7010 Clinical Practicum I (4 credit hours)
(Formerly PT 518)
Prerequisite: Satisfactory completion of all coursework in Modules I and II. Forty hours per week for
four weeks under the direct supervision of a physical therapist serving as the clinical instructor.
Application of Modules I and II will be emphasized in this clinical experience. Cr/NCr.
PT 7020 Clinical Practicum II (12 credit hours)
(Formerly PT 519)
Prerequisite: Satisfactory completion of all coursework in Modules I through IV, PT 6080, 6090, and
7010. Forty hours per week for twelve weeks under the direct supervision of a physical therapist serving as
the clinical instructor. Application of Modules I through IV will be emphasized in this clinical experience.
Cr/NCr.
PT 7030 Clinical Practicum III (12 credit hours)
(Formerly PT 520)
Prerequisite: Satisfactory completion of PT 5000 through 5143, 5200 through 5230, 6000 through
6020. Forty hours per week for twelve weeks under the direct supervision of a physical therapist serving as
the clinical instructor. Application of Modules I through VI will be emphasized in this clinical experience.
Cr/NCr.
PT 7040 Clinical Practicum IV (12 credit hours)
(Formerly PT 521)
Prerequisite: Satisfactory completion of all courses, except PT 6210 and 6500. Forty hours per week
for twelve weeks under the direct supervision of a physical therapist serving as the clinical instructor.
Application of Modules I through IX will be emphasized in this clinical experience. Cr/NCr.
PT 8100 Pharmacology for the Physical Therapist (3 credit hours)
Prerequisite: Bachelor’s or Master’s degree in Physical Therapy. This course addresses basic and
applied pharmacology for the practicing physical therapist. The content includes the effects of
pharmacotherapy on the health and well-being of physical therapy patients.
PT 8120 Medical Screening and Systems Review (3 credit hours)
Prerequisite: Graduate of an accredited Physical Therapy program and current licensure as a physical
therapist. This course familiarizes the physical therapist with patient history and systems review from the
medical and physical therapy perspectives. Lecture notes, internet discussions, and case discussions are
used to prepare the PT for the appropriate medical screening and physical examination skills required to
practice in a direct access environment. A systems approach is used to discuss common medical
conditions, their epidemiology, etiology, clinical manifestations, medical management and issues related to
PT screening, examination, interventions, and red flags.
HONORS AND AWARDS
The following awards are presented to PT students annually on Honors Day in April:
Physical Therapy Student Recognition Award
Physical Therapy Class Award
Elizabeth A. Rogers Chairperson's Award
Asian American Physical Therapy Scholarship Award
123
Roy G. and Marion L. Kramer Endowment Fund Award
Guy M. Allmon Scholarship Fund Award
Linda Fox Memorial Endowment Fund Award
President's Society Award
Rebecca E. Pabst Memorial Scholarship Award
Shannon Marie Fogard Memorial Scholarship Award
Casa Colina Centers for Rehabilitation Scholarship Award
Dean's Award
The following are presented at graduation:
Dean's Award
Physical Therapy Faculty Award
Physical Therapy Outstanding Clinical Performance Award
Physical Therapy Outstanding Service Award
Physical Therapy Academic Achievement Award
Outstanding Research Proposal Award
124
ACADEMIC CALENDAR
Program Year 2003 MPT PROGRAM
(subject to change)
Friday, Dec. 20, 2002
Spring Semester Registration Ends (All years)
Friday, Dec. 20, 2002
Spring Semester Tuition Due (All years)
Monday, Jan. 6, 2003
MPT '05 Registration
MPT '05 Module I Begins
MPT '04 Module VI Begins
MPT '03 Module X Begins
Sunday, Jan. 12, 2003
MPT '05 Welcome Luncheon and White Coat
Ceremony
Monday, Jan. 20, 2003
Martin Luther King, Jr. Holiday
Monday, Feb. 17, 2003
President's Day Holiday
Monday, Mar. 31, 2003
MPT '03 Spring Break
MPT '04 Module VII Begins
Friday, April 4, 2003
MPT’05 Fall Semester Registration
Monday, Apr. 7, 2003
MPT '03 Module XI Begins
Monday, Apr. 21, 2003
MPT '05 Spring Break
Monday, Apr. 28, 2003
MPT '05 Module II Begins
Friday, May 2, 2003
MPT '03 Last Day of Classes
Monday, May 26, 2003
Memorial Day - No Classes
TBA
Graduation MPT '03
Monday, Jun. 23, 2003
MPT '04 Summer Break
Friday, Jul. 4, 2003
Independence Day - No Classes
Friday, Jul. 25, 2003
MPT ’05 Fall Semester Registration Ends
Monday, Aug. 4, 2003
MPT '04 Module VIII Begins
MPT ’05 Fall Semester Tuition Due
Monday, Aug. 11-Friday, Aug. 15, 2003
MPT ’04 Fall Semester Registration
Monday, Aug. 18, 2003
MPT '05 Module III Begins
Friday, Aug. 28, 2003
MPT ’04 Fall Semester Tuition Due
Monday, Sept. 1, 2003
Labor Day Holiday - No classes
Monday, Oct. 13, 2003
Columbus Day - No classes
Monday, Oct. 27, 2003
MPT '04 Module IX Begins
Monday, Nov. 23-Dec. 1, 2003
Thanksgiving Break - No classes
Monday, Dec. 1, 2003
MPT '04 Module IX Resumes
Monday, Dec. 15, 2003
MPT '04 Winter Break Begins
Monday, Dec. 22, 2003
MPT '05 Winter Break Begins
125
COLLEGE OF ALLIED HEALTH PROFESSION
Master of Science in Physician Assistant Studies
Primary Care Physician Assistant Program
ACCREDITATION
The Primary Care Physician Assistant Program of the College of Allied Health Professions is
accredited by the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA).
VISION STATEMENT
The Western University of Health Sciences Primary Care Physician Assistant Program will be
nationally respected and recognized as an innovative leader in Physician Assistant education. Our faculty
will continue to be leaders in our profession as educators and clinicians. This will be accomplished by the
continued acquisition of knowledge and utilization of effective teaching methods. Our faculty will educate
a diverse student body who will provide compassionate and comprehensive primary care medicine.
The program will continue to seek out applicants and foster in our students attributes that will enhance
their role as effective health care professionals. Core attributes that will be valued are integrity,
compassion, respect, moral principles, and an aspiration for life-long learning.
Our students, graduates and faculty will serve in key leadership positions on a local, state and national
level, to steer the future of the physician assistant profession, while striving to continue personal and
professional development. Physicians and health care delivery teams will seek our graduates. Through
these partnerships, comprehensive patient care will be accessible for all populations.
MISSION STATEMENT
The Primary Care Physician Assistant Program supports the University’s mission by educating
Physician Assistants to deliver high quality competent and compassionate health care as team members
within the health care delivery system.
THE PHYSICIAN ASSISTANT ROLE
Physician assistants are health care professionals licensed to practice medicine with physician
supervision. Within the physician/physician assistant relationship, physician assistants exercise autonomy
in medical decision making and provide a broad range of diagnostic, therapeutic, preventive, and health
maintenance services. The clinical role of the physician assistant includes primary and specialty care in
medicine and surgical practice settings. Physician assistant practice is centered on patient care and may
include educational, research and administrative activity. As part of their comprehensive responsibilities,
PAs conduct physical exams, diagnose and treat illnesses, order and interpret tests, counsel on preventive
health care, assist in surgery, and can write medical orders.
The role of the physician assistant demands intelligence, sound judgment, intellectual honesty,
appropriate interpersonal skills, and the capacity to react to emergencies in a calm and reasoned manner.
An attitude of respect for self and others, adherence to the concepts of privilege and confidentiality in
communicating with patients, and a commitment to the patient's welfare are essential attributes.
The specific tasks performed by an individual physician assistant cannot be delineated precisely
because of variations in practice requirements mandated by geographic, political, economic, and social
factors. At a minimum, however, physician assistants are educated in those areas of basic medical science
and clinical disciplines and specific problem solving.
Physician assistant practice is characterized by clinical knowledge and skills in areas traditionally
defined by family medicine, internal medicine, pediatrics, obstetrics, gynecology, surgery, and
psychiatry/behavioral medicine.
Physician assistants practice in ambulatory, emergency and long-term settings. Physician assistants
provide health care services to diverse patient populations of all ages with a range of acute and chronic
medical and surgical conditions. They need knowledge and skills which allow them to function effectively
in an ever changing health care environment.
126
Services performed by physician assistants include, but are not limited to the following:
1. Evaluations: eliciting a detailed and accurate history, performing an appropriate physical
examination, ordering appropriate diagnostic studies, delineating problems, developing
management plans, and recording and presenting data.
2. Diagnostics: ordering, performing and/or interpreting diagnostic studies to identify and follow
pathophysiology process.
3. Monitoring: implementing patient management plans, recording progress notes and participating
in the process of the continuity of care.
4. Therapeutic: performing therapeutic procedures and managing or assisting in the management of
medical and surgical conditions, which may include assisting surgeries in the conduct of operations
and taking initiative in performing evaluations and therapeutic procedures in life-threatening
procedures.
5. Patient Evaluation: counseling patients regarding issues of health care management to include
compliance with prescribed therapeutic regimens, normal growth and development, family planning,
and emotional problems of daily living.
6. Referral: facilitating the referral of patients to other health care providers or agencies as
appropriate.
Certification/Licensure
The written examination for certification as a physician assistant is administered by the National
Commission on Certification of Physician Assistants (NCCPA) three times yearly. Successful completion
requires that the applicant achieve the passing score established by the NCCPA for that examination. It is
the responsibility of the applicant to ensure that certification of his or her examination score is received by
the Physician Assistant Committee (PAC). The NCCPA phone number is 770-399-9971. The PAC phone
number is 916-263-2323.
The PAC may grant interim approval to an applicant for licensure as a physician assistant provided that
the applicant provides evidence that he or she is a graduate of an approved program and has applied for,
and therefore not taken, the first examination required by Section 1399.507 subsequent to the applicant's
successful completion of the approved program. If the applicant fails the examination, the interim approval
automatically terminates upon the applicant's receipt of notice of failure by the PAC or by the NCCPA.
An applicant who has been granted interim approval and who is subsequently notified by the NCCPA
or by the PAC that he or she has passed the examination required in Section 1399.507 shall complete the
licensure process by paying the initial licensure fee as requested within 90 days from notification that the
applicant is now ready for licensure. If the applicant does not complete the licensure process by end of the
90-day period, the interim approval shall automatically terminate. Applicants who do not pass the national
certifying exam, can not work as a PA. The applicant may retake the exam at the next test date offered by
the NCCPA.
PROGRAM GOALS
The primary goal of the Western University Physician Assistant Program is to educate individuals to
serve as physician assistants in primary care medicine. PA students are educated to provide health care to
all patient populations. PAs work with the direction and supervision of a physician. The education
provided by the program will prepare the entry-level graduate with the knowledge skills and attitudes to
perform in a primary care setting and function in a variety of roles within numerous clinical settings. The
program goal of educating individuals to serve as PAs in primary care medicine is founded on the
understanding that the broad-based education needed to prepare an individual to serve in a primary care
setting is the most effective form of initial preparation. This goal also permits the development of
attributes that will serve the graduate in the greatest spectrum of potential employment opportunities.
The program has also established the goal of incorporating appropriate elements of the traditional
osteopathic philosophy into the training of physician assistants. These elements include:
• An understanding of the patient as a "whole person."
• Emphasis on those aspects of health education that stress "wellness" and disease prevention.
• An appreciation of the role of physical medicine in the diagnosis and management of illness.
127
The curriculum is designed to accomplish the following objectives. Students attain these objectives as
they progress through the curriculum.
Knowledge
Upon completion of this program the graduate should know:
1. The pre-clinical, clinical and behavioral sciences that form the foundation for functioning as a PA.
2. The spectrum of normal measurements that define the healthy individual at all ages.
3. The pathophysiologic processes that commonly cause deviations in normal clinical measurements.
4. The fundamentals of health maintenance.
5. Patient management regimens for common primary health care problems.
6. Accepted strategies for disease prevention.
7. How to apply a systematic process of problem solving to the diagnosis of disease.
8. The components of normal human behavior and the major deviations from these patterns.
9. The health care resources available to the health care provider and patient.
10. The role of the physician in a variety of health care environments.
11. How the various health care delivery systems function and the role of the PA within each system.
12. The general principles of managed care as it applies to patients and primary care providers.
13. The fundamentals of various types of research modalities.
14. The research modalities and applications for problem solving in regards to disease, health
promotion and disease prevention.
Skills
Upon completion of this program the graduate should be able to:
1. Obtain a medical history.
2. Perform a complete physical examination.
3. Perform and interpret diagnostic tests.
4. Accurately report information obtained from a patient.
5. Manage, with the supervision of a physician, common health care problems.
6. Assess mental health status.
7. Recognize signs and symptoms of disease processes.
8. Communicate empathetically with a patient.
9. Formulate differential diagnosis to aid in diagnosis.
10. Critically interpret medical literature and apply it appropriately in clinical practice.
11. Gather community resources for patients.
12. Implement community health projects and guidelines.
13. Participate in quality assurance programs.
14. Develop health care resources for other providers and patients.
15. Participate in medical research activities.
Attitudes
Program graduates should exhibit respect and appreciation for:
1. All individuals who seek their care.
2. Self and other members of the health care team/profession.
3. An individual's right to confidentiality.
4. The sanctity of human life.
5. The dignity of patients.
6. The multiple physical and emotional factors that influence the health of individuals.
7. The many value systems in our society.
8. The importance of continuing medical education after graduation.
9. The effectiveness as a contributing team member in health care.
10. An increased PA role in regards to the medical community, health care delivery systems and the
patient.
128
FUNCTIONS AND TASKS OF PHYSICIAN ASSISTANT GRADUATES
General Entry-Level Competencies Expected of a Graduate
The physician assistant will be able to:
• Elicit a comprehensive, accurate history and perform a complete routine physical examination on
patients of any age group; elicit a pertinent and accurate history and perform a problem-oriented
screening examination in situations requiring an interval evaluation.
• Select, perform and/or interpret the appropriate routine laboratory and diagnostic studies/ procedures
for the purpose of completing an adequate data base.
• Identify problems, organize and integrate data, record and present.
• Accurately present an oral case.
• Implement a management plan, including performing or assisting.
• Instruct and counsel patients regarding physical and mental health to include diet, health maintenance,
therapy, normal growth and development, family planning, referral and follow-up services.
• Provide life support and emergency evaluation/care in response to life-threatening situations in the
absence of a physician and/or other appropriate health professionals.
• Initiate and follow up on appropriate referrals to specialists.
Associated Competencies
In addition to the above entry-level competencies, physician assistant graduates are expected to
function in a variety of environments, interact appropriately with diverse populations, and engage in many
activities for continued professional and personal growth. The role of the physician assistant as a primary
health care provider imposes many legal and ethical restrictions on behavior. Although not strictly related
to the "clinical role" of the physician assistant, there are a large number of activities that contribute to the
broad process of "professional development" and "role identity" which are essential for optimal
performance as a health professional. These activities are related to areas such as administration,
education, consultation, ethical, and legal considerations of the profession. The program will endeavor to
provide its students with educational experiences that will introduce these attitudinal objectives.
PERSONAL COMPETENCIES FOR ADMISSION AND MATRICULATION
A candidate for admission to the Primary Care Physician Assistant Program must have the use of
certain sensory and motor functions to permit them to carry out the activities described in the sections that
follow. Graduation from the program signifies that the individual is prepared for entry into clinical practice
or into postgraduate training programs. Therefore, it follows that graduates must have the knowledge and
skills needed to function in a broad variety of clinical situations and to render a wide spectrum of
diagnostic and therapeutic care. The candidate and student must be able consistently, quickly and
accurately to integrate all information received by whatever sense(s) are employed. Also, they must have
the intellectual ability to learn, integrate, analyze and synthesize data.
A candidate for the Master of Science in Physician Assistant Studies degree ordinarily must have
abilities and skills of five varieties including: observation; communication; motor; intellectual, conceptual,
integrative and quantitative; and behavioral and social. Where technological assistance is available in the
program, it may be permitted as a reasonable accommodation when appropriate. Under all circumstances,
a candidate should be able to perform in a reasonably independent manner.
a. Observation: Candidates and students ordinarily must have sufficient vision to be able to observe
demonstrations, experiments and laboratory exercises. They must be able to observe a patient
accurately at a distance and close at hand.
b. Communication: Candidates and students must be able to communicate with patients and colleagues.
They should be able to hear, with or without a reasonable accommodation. Candidates and students
must be able to read, write, and speak English.
c. Motor: Candidates and students ordinarily should have sufficient motor function such that they are
able to execute movements reasonably required to provide general care and emergency treatment to
patients. Examples of emergency treatment reasonably required of physician assistants are
cardiopulmonary resuscitation, administration of intravenous medication, the application of pressure to
stop bleeding, the opening of obstructed airways, the suturing of simple wounds, and the performance
129
of simple obstetrical maneuvers. These actions require coordination of both gross and fine muscular
movements, equilibrium and functional use of the senses of touch and vision.
d. Intellectual, Conceptual, Integrative and Quantitative Abilities: These abilities include measurement,
calculation, reasoning, analysis and synthesis. Problem solving, the critical intellectual skill demanded
of a physician assistant, requires all of these intellectual abilities. In addition, candidates and students
should be able to comprehend three-dimensional relationships and understand the spatial relationships
of structures.
e. Behavioral and Social Abilities: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgment, the prompt completion of
all responsibilities attendant to the assessment and care of patients, and the development of mature,
sensitive and effective relationships with patients. Candidates and students must be able to tolerate
physically taxing workloads, adapt to changing environments, display flexibility, and learn to function
in the face of uncertainties inherent in the clinical problems of many patients. Compassion, integrity,
concern for others, interpersonal skills, interest and motivation are all personal qualities to be assessed
during the admissions and educational processes.
The Primary Care PA Program, along with all the other programs at Western University of Health
Sciences, shares a commitment to develop creative ways of opening the PA curriculum to competitive,
qualified disabled individuals. In doing so, however, the Primary Care PA Program must maintain the
integrity of its curriculum and preserve those elements deemed essential to educating candidates to become
effective physician assistants.
ADMISSIONS POLICIES AND PROCEDURES
Admission to the PA program is on a competitive basis and is open to citizens and permanent residents
of the United States. Western University is committed to admitting competitive, qualified disabled
individuals. For technical guidelines, please see above.
Application Requirements
The admissions committee will consider applicants with a minimum of a bachelor's degree from a
regionally accredited institution or who will complete their bachelor's degree before matriculation. The
minimum overall GPA required is 2.5 on a 4.0 scale and GPA of 2.7 on a 4.0 scale in all course work
listed as prerequisites for the PA program. Grades of "C-" in any of the prerequisite courses are not
accepted. Candidates should possess the oral and written communication skills necessary to interact with
patients and colleagues.
1. Prerequisite Courses:
College English and English Composition* (6 semester units, a full year sequence)
College Algebra (3 semester units)
Human Anatomy with lab** (3 semester units)
Human Physiology with lab** (3 semester units)
Microbiology with lab (3 semester units)
General or Inorganic Chemistry with lab (6 semester units, a full year sequence)
Psychology (General or Introductory only - 3 semester units)
Sociology (General or Introductory only - 3 semester units)
Humanities (9 semester units)
Introductory Statistics (3 semester units, preferably from the math or statistics department)
Spanish is strongly recommended.
Genetics is strongly recommended.
*Note: English prerequisites must be taken from the English department. English as a Second
Language (ESL) courses are not accepted for the English prerequisites.
**Note: Anatomy and physiology must be taken out of the anatomy, physiology, A&P, biology,
or zoology departments. If anatomy and physiology are combined, a minimum of five semester
units is required.
Advanced placement, transfer of credit, CLEP examination, or credit for experiential learning is not
recognized by the program as meeting these prerequisites.
130
Introductory level courses in the sciences are not acceptable (i.e., courses taken in the sciences for non-
science majors).
Prerequisite courses must be transferable. Transferable courses are those designated for baccalaureate
credit by the college or university offering the courses.
2. Health Care Experience
Health care experience is not required. However, engagement in extracurricular or community
activities that reflect people or service orientation is considered essential. The extracurricular or
community activity does not need to be medical in nature.
Application Procedures and Deadlines
Beginning with the entering class of August 2002, the PA program will be participating in the first
central application service for physicians assistant programs. The Central Application Service for
Physician Assistants (CASPA) was created by the Association of Physician Assistant Programs (APAP) as
a service to applicants and member programs. CASPA will collect one set of materials from each
applicant. CASPA will then authenticate, photocopy, and distribute them to each member school an
applicant designates. Western University’s application deadline to apply to CASPA is November 1, 2002.
Applicants are considered without discrimination on the basis of race, color, national origin, age, or sex.
To request an informational brochure and/or information about the CASPA application, contact the
Office of Admissions or the CASPA office at:
Office of Admissions CASPA
Western University of Health Sciences apply@caspaonline.org
309 E. Second Street (240) 497-1895
Pomona, CA 91766-1854
(909) 469-5541
In addition to the CASPA application, applicants must submit a supplemental application. After the
CASPA application has been received, a supplemental application (provided by Western University) will
be sent to all applicants who meet the overall GPA of 2.5. However, this does not ensure that you will
meet our minimum prerequisite of 2.7 or that all prerequisite classes will be acceptable. A final evaluation
and calculation will be completed upon receipt of your supplemental application. The supplemental
application deadline for the class entering in August 2003 is 30 days after receiving notification to file a
supplemental application or February 1, 2003, whichever comes first. The supplemental application
consists of forms requesting additional information, one letter of reference, and a personal statement. A
non-refundable application fee of $45 must be submitted with the supplemental application materials. All
application materials must be returned as part of one supplemental application packet.
Applicants who wish to use course work completed outside of the United States must submit their
transcripts for evaluation to World Education Services, Josef Silny and Associates, Educational Credential
Evaluators, Inc., or International Education Research Foundation, Inc. In preparation for CASPA, a
course-by-course evaluation is required, and all course work must be designated as undergraduate,
graduate, or professional. Western University will only honor evaluations from the above services. The
evaluation must be submitted to CASPA.
Once the applicant's personal statement and file is reviewed, the applicant may be granted an on-
campus interview. During the interview process, the applicant meets individually with an interview team,
which may consist of the PA Program Director, PA Admissions Committee Chair, PA faculty, Dean of the
College of Allied Health Professions, University faculty, students, PA alumni, and community PAs. The
interviewers question the applicant regarding academics, personal preparedness and commitment to the PA
program and the PA profession. Interviewees are rated on a standard evaluation form relative to each of
these variables. After the conclusion of the interviews, the evaluation forms are reviewed by the PA
Admissions Committee, which decides to admit, deny admission, or place the applicant on an alternate list.
An applicant previously on the alternate list must reapply for admissions into the PA Program. The
Western University PA program does not accept transfer students, nor is admission to the program
deferrable. Decisions of the Admissions Committee regarding the admission of applicants to the Master of
Science in Physician Assistant Studies program are final. Candidates accepted to Western University must
131
have a complete set of official transcripts mailed to the Admissions Office no later than July 1. For your
information, CASPA retains the original set of transcripts it receives from applicants.
Registration
First year students are required to register in person on the registration day specified in the University
Calendar or as otherwise directed by the Registrar. Failure to register on that day may be grounds for
dismissal. Full tuition and fees and all prior debts must be paid in full on or before registration day each
academic year. Matriculation is subject to the satisfactory completion of all academic requirements and
payment of all outstanding debts to the University. The receipt of a final transcript from an undergraduate
college and a physical examination with documentation of required immunizations prior to registration are
additional requirements for incoming students. Also, all students must show proof of current health
insurance coverage at the time of registration. This coverage must be maintained or in effect throughout
the academic year. If there is no proof of current coverage, a policy provided by the University is
available. Attendance at Orientation is mandatory for all incoming first-year students.
TUITION AND FEES
By action of the Board of Trustees, PA tuition and fees for the 2001-2002 academic year (subject to
change) are as follows:
$20,045 Tuition Annual
For PA applicants accepted at Western University, an entrance fee of $250
payable upon acceptance is applied to tuition.
$40 Student Body Fee, 1
st
year
Covers student council expenditures, social activities and public relations.
$20 Student Body Fee, 2
nd
year
Other Fees and Expenses
$1900 Required and Recommended Texts
$45 Uniform Jacket/Patch, Name Badge
$1200 Diagnostic Equipment Kit
$30 (per day) Late Registration Fee
$40 Lost Mail Locker Key
$5 (each) Copy of Official Transcript
$10 (each) Copy of Official Transcript Faxed
$10 Lost ID Badge
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
ACADEMIC REQUIREMENTS
Academic Advisement
Students will be assigned a faculty advisor by the Dean upon matriculation. Advisement by faculty
should be viewed by the student as a part of the academic process. The student or faculty member may
seek a change of advisor/advisee. This request should be made to the appropriate Dean or Dean’s
designee. It is the student's responsibility to meet periodically with his/her advisor. A student on
probation must meet with his/her faculty advisor at least once a month.
Promotion
A student’s progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behaviors and attitudes. At the completion of
each phase of the program, before the student is allowed to progress to the next phase, the student’s record
of achievement is reviewed by the Program Chair and faculty.
The faculty determines if the student has demonstrated the knowledge, skills, and attitudes necessary to
be eligible to progress to the next phase.
132
In special instances, the faculty may be convened at other than the scheduled times to consider cases
relating to unusual circumstances, such as probation or dismissal.
Promotion is defined as progression from one academic year to the next.
a. A student will be recommended to the Dean of the College of Allied Health Professions for
promotion by the Allied Health Student Academic Progress Committee.
b. A student may not be recommended for progression from one semester or phase to the next with any
outstanding grades of “I” or “U” on his/her academic record or with a semester grade point average of
less than 2.5. Grades of “D” must be remediated before progression to next phase.
c. When considering a student for promotion, professional, ethical, and personal conduct may also be
taken into consideration (as described under Probation, a-4).
d. A student will be promoted provided that all legal and financial requirements of the University as
stated in the University Catalogue have been satisfied.
Graduation
A student will be recommended for the Master of Science in Physician Assistant Studies Degree
provided he/she:
a. has completed at least two years of the Western University Primary Care PA program.
b. has been enrolled in the Western University Primary Care PA program during his/her final academic
year.
c. is not on probation and has completed all prescribed academic and clinical requirements with a
cumulative grade point average of at least 2.5 and has no outstanding grade of “D”, “I” or “U”.
d. has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined in
Probation guidelines, which would make it inappropriate to award the degree of Master of Science in
Physician Assistant Studies.
e. has complied with all the legal and financial requirements of the University as stated in the
University Catalogue.
f. has attended in person and participated in the Commencement program at which time the Master of
Science in Physician Assistant Studies is conferred, unless special permission is received from the
President. If the President grants special permission to be excused from graduation, the graduate may
be required to present himself or herself to the Provost or appropriate Dean at a later date in order to
take the required oath (if relevant) to receive his or her degree.
g. is within one clinical rotation of completion of all requirements for graduation to be able to march
with his or her class in the graduation ceremony. At the discretion of the Dean of the College of Allied
Health Professions, an exception may be made for a student with an authorized leave during the Senior
year. No student will receive his or her degree until the student has completed all requirements for
graduation. Degrees will be dated as appropriate to completion date.
Probation
a. Probation is defined as a period of time specified by the Dean of the College of Allied Health
Professions during which the student's progress will be closely monitored by the Allied Health Student
Academic Progress Committee, faculty advisor and the Program Chairperson. In order to closely
monitor 2nd year students on probation, the PA program reserves the right to assign their clinical
rotations. A student will be recommended for probation for any of the following reasons:
1. Immediately upon receiving a course grade of "D" or "U" in any course.
2. A grade point average of less than 2.5 at end of the semester.
3. When directed to repeat a year for academic reasons.
4. Seriously deficient ethical, professional, or personal conduct.
Members of the faculty or administration will render a special report in writing to the Dean of the
College of Allied Health Professions regarding any student whose professional or personal conduct is
deemed unsatisfactory. Professional and personal conduct includes, but is not limited to, attendance,
cooperation with faculty, interest shown in assigned work, attitude toward fellow students and
associates and toward personnel of hospitals, approach to and interaction with patients, as well as
personal appearance appropriate to the circumstances.
The terms of probation for ethical, professional, or personal conduct will be specified at the time the
student is placed on probation.
133
b. When a student is placed on probation, he/she will be notified in writing by the Dean of the College
of Allied Health Professions and the reasons will be stated. Notification must be by Certified mail or
hand-delivered and acknowledged by signatures of the student and the Dean of the College of Allied
Health Professions or his designee. Copies of the letter will be placed in the student's permanent file
and distributed to the Chairman of the Allied Health Student Academic Progress Committee and the
student's faculty advisor. The Allied Health Student Academic Progress Committee will ascertain when
the terms of the probation have been satisfied and recommend to the Dean that probation can be
rescinded.
c. A student on probation may not serve as an officer of any official University club or organization
and shall not engage in time-consuming extracurricular activities.
d. A 1st year student on probation must meet with his/her faculty advisor at least once a month. A 2nd
year student on probation must contact his/her Faculty Advisor once a month.
e. Students are removed from probation when the following occur:
1. After one semester, provided he/she has regained a semester grade point average of 2.5.
2. When all “D” or “U” grades have been satisfactorily remediated according to the Remediation
section of the Catalogue (below).
3. When the specified terms of probation for ethical, professional, or personal conduct are met.
4. When 2nd year students are on probation for a clinical rotation grade of “U”, they will be
removed from probation when they have met the terms of their probation.
Remediation
a. Every effort will be made to give each student ample opportunity to demonstrate competency in
each area of the academic program. However, remediation is to be regarded as a privilege that must be
earned by a student through an active participation in the educational program as demonstrated by
regular attendance, individual initiative, and utilization of resources available to him/her.
b. If a student receives a “D” or “U” grade in a course or has a semester grade point average of less
than 2.5, that student will be reviewed by the Allied Health Student Academic Progress Committee and
procedures for remediation by the Physician Assistant faculty will be recommended to the SAPC, who
in turn makes a recommendation to the Dean. In reviewing the student's academic deficiencies, the
following guidelines shall be used:
1. Educational objectives underlie remedial teaching and evaluation should be the same as the
educational objectives that underlie regular courses in the curriculum. Where deemed
appropriate, the Allied Health Student Academic Progress Committee, after consultation with the
course instructor and/or Physician Assistant Faculty, may recommend one or a combination of the
following options:
(a) Take a comprehensive examination (this option is not available if the original earned
grade is a “U”).
(b) Complete special projects or studies in the deficient area(s).
(c) Repeat the course, with or without promotion into the subsequent semester. The
student cannot start Phase II or Phase III until the grade of “D” or “U” has been
remediated.
(d) Repeat the academic year.
(e) Dismissal from the University (see Dismissal section for criteria for this option).
2. Students receiving a “U” grade for a clinical rotation education/preceptorship will repeat the
entire rotation/preceptorship. The above a-d options do not apply to clinical education.
3. The grade achieved by remediation will be the grade recorded EXCEPT that the highest grade
a student may earn by options (a) or (b) is a grade of “C”. The grade achieved by remediation
will be recorded on the transcript beneath the original grade.
4. Grades earned during an attempted remediation of a course will be reviewed critically by the
Allied Health Student Academic Progress Committee and the Dean of the College of Allied
Health Professions. Failure to earn at least a “C” grade may result in dismissal from the
University or repeating the course.
5. Decisions regarding remediation will be made on an individual basis after considering all
pertinent circumstances in each case. The decision will be made by the Dean of the College of
Allied Health Professions Education, based upon the recommendation of the Allied Health
134
Student Academic Progress Committee. The Allied Health Student Academic Progress
Committee will base its recommendation on the student's academic record and considerations
after consultation with the Physician Assistant Faculty Student Advisor, course instructor, and the
student.
6. Any student who is required to remediate a course will be notified in writing by the Dean of
the College of Allied Health Professions Education at least two weeks prior to the remediation
date (or within two weeks after the close of the academic year in which the student is presently
enrolled, whichever comes first). Notification must be by Certified Mail or hand-delivered to the
student and must be acknowledged with the signatures of the Dean of the School of Allied Health
Professions, or his designee, and the student.
c. Students who have been required by the Dean of the School of Allied Health Professions to repeat a
course(s) due to unsatisfactory grades (GPA) or in cases where there is a satisfactory GPA, but
deficiencies are noted which impedes promotion, the following criteria must be met to be eligible for
financial aid:
1. Full-time attendance recorded
2. Placed on at least one semester probation
3. Must be tested and graded
4. Close monitoring
It is the student's choice if he/she has made satisfactory progress such as GPA, but wants to audit only
to strengthen skills, as long as he/she is fully aware he/she will not be eligible to apply for any financial
aid. Students will be financially responsible for themselves until promoted by the Dean of the School of
Allied Health Professions.
Clinical Education/Preceptorship Remediation
Any student who receives a grade of “U” for a clinical education/preceptorship grade will be required
to repeat the entire clinical education/preceptorship. The student must complete all deficiencies for the
clinical education/preceptorship prior to completion of the program. The grade achieved by repeating the
rotation/preceptorship will be recorded on the transcript. Remediated grades are recorded below a grade
of “U.” Only the remediated grade is calculated into the G.P.A.
Remediation: Financial Aid Policy
If the student, at the end of the academic year, is still considered to be making unsatisfactory progress
and must remediate, he/she is removed from the list of Title IV and Title VII financial aid recipients.
Tutorial Assistance Program
A Tutorial Assistance Program (TAP) has been established to assist students experiencing academic
difficulty. Students will be recommended for this program by a faculty advisor or professor. Students may
self-identify to TAP to receive assistance. The tutors will be chosen on the recommendation of the faculty
in each discipline. For assistance, contact the Learning Enhancement and Academic Development Office.
Standards of Academic Progress
Good academic standing implies that a student has not been requested to withdraw and is not under
academic probation/suspension.
Academic performance encompasses those areas of knowledge and skills outlined in the section
entitled "Program Objectives". The level of attainment listed in these areas is that expected of graduates of
the program. However, students are expected to attain these goals as they progress through the Program
and certain patterns of attainment are expected along the temporal course of the curriculum.
All grading and evaluation is based on the student's ability to attain the competencies within the
objectives outlined for each area of study.
A student whose performance falls below the minimum acceptable standard(s) for any area of study
will be notified of such deficiency by the instructor of the course as soon as evidence of such sub-standard
performance is available.
135
The following academic standards apply to students enrolled in the Primary Care Physician Assistant
Program. Academic performance is considered sub-standard and unacceptable if any one or more of these
standards are not met:
a. Phase I:
During Phase I (Didactic Phase), students must earn a grade of "C" or better in each course. All
“D's” or “U’s” will be remediated to a "C" (see Remediation Section). If a remediated grade of
"C" is not earned, the student may be dismissed or be required to repeat the entire course of study.
Students must maintain a GPA of 2.5 during Phase I. In addition, the following applies regarding
cumulative GPA:
1. Students whose GPA falls below 2.5 must meet with the department chairperson prior
to registration for the next semester.
2. Students whose GPA falls below 2.5 are not eligible for further registration unless
probationary status is granted by the Dean of the College of Allied Health Professions
Education.
3. Students will not be allowed to advance to Phase II (clinical education) until all
deficient grades are remediated.
4. First year students who receive a “U” in any course may only advance from one
semester to the next with special consent from the faculty.
b. Phase II:
Senior Seminar I, II and III Requirement
1. In Senior Seminar I and II, a grade of "C" or better must be earned. All "D's" will be
remediated to a "C". If a remediated grade of "C" is not earned, the student will be
required to repeat the entire course of study.
2. If a student receives a "U" in Senior Seminar I, he/she must repeat the course;
however, the student is allowed to progress to Senior Seminar II. If the Student receives
a "U" in Senior Seminar II, he/she must repeat the course, and he/she will not be able to
advance to Phase III.
3. If a student receives a “U” in Senior Seminar III, he/she must remediate to a “C”
grade.
c. Clinical Education Phase II and Phase III
Students’ progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behaviors and attitudes. If students fail
to meet the pre-designated clinical objectives, their academic achievements will be reviewed by
the PA faculty. The faculty and preceptors determine if students have demonstrated the
knowledge, skills and attitudes necessary to be eligible for progress to the next phase. Upon
eligibility, the faculty recommends advancement to the Allied Health Student Academic Progress
Committee.
If a student receives a grade of “U” in Phase II, he/she must repeat the rotation before advancing
to Phase III.
The Allied Health Student Academic Progress Committee and the Professional Conduct
Committee may be convened to consider cases relating to unusual circumstances.
Out-of-Area Clinical Education
Clinical Education that is greater than 180 miles in any direction from Western University, Pomona
Campus, is considered an out-of-area rotation clinical education. Permission for out-of-area rotations
clinical education is granted by the Clinical Education Coordinators and the PA Faculty.
To participate in out-of-area rotations, students must:
• Exemplify ethical and professional behavior throughout their didactic and clinical rotations
phase.
• Have a GPA of 3.0 from Phase I, receive a “B” or better on all preceptor assigned grades and
maintain a “B” or better in Senior Seminar I and II.
136
• Provide the Clinical Education Coordinators with transportation and room and board for out-
of-area site visits.
• Sign a waiver releasing Western University from any responsibility regarding NCCPA Board
performance.
• Have confirmation of housing and travel arrangements available to the clinical coordinators
at the time of scheduling.
Clinical Rotation Education Assignment Appeal
A change in clinical rotation education assignment may be requested in writing by the student for the
following reasons:
a. After completing one week in the rotation, the student deems the rotation is not of high quality.
b. The student is requesting a change in a clinical rotation assignment for a specific month under a
preceptor not affiliated with the PA Program.
Completed paperwork requesting an upcoming rotation change must be submitted to the Clinical
Education Coordinators 60 days before the rotation is scheduled to begin. The student will be notified of
the approval/non-approval of the request within 24 hours.
Reassignment of Clinical Rotation Education
Any student who receives one or more “C’s” on a preceptor assigned grade for the clinical rotation,
may have the remainder of their clinical rotations reassigned by the Clinical Education Coordinators.
Rotational Clinical Education Observation
Any student who has been "deemed unsafe" may be placed in an observational mode for the remainder
of his/her rotation. A student may be placed in observation mode for one month only, then summary
suspension may occur. Summary suspension may be implemented instead of observation mode.
Personal Appearance
Personal appearance is extremely important in facilitating acceptance by other health professionals and
patients. The poor appearance of one individual is often generalized to the entire profession. Adherence
to the following dress code is, therefore, the responsibility of each student while in clinical training.
a. Primary Care Physician Assistant Program name tags/badges are to be worn at all times while on
campus, and at clinical rotation education sites.
b. Short white “intern” type jackets are required at all times, beginning with Phase II of the curriculum.
c. Female students may wear slacks or other appropriate dress. Modesty must be a consideration for
necklines and hemlines.
d. Shirt and tie are considered appropriate dress for male students when they are present in a setting
where patient contact can be expected. Students must receive the approval of the supervising
practitioner to wear “scrubs” during the rotation. The white coat must be worn over scrubs except
while in the surgical suite.
e. “Blue jeans” are NOT appropriate dress for either male or female students during the clinical
phases.
f. “Tennis Shoes”, “Joggers”, and other forms of athletic shoes are NOT considered appropriate attire.
g. Students should consider the image projected to the patient and others with regard to hairstyle and
length, beards, mustaches and jewelry.
Professional Conduct During Clinical Education
Professional and personal conduct includes, but is not limited to attendance, cooperation with
preceptors, interest shown in assigned work, attitude toward fellow students, associates and personnel of
hospitals and approach to and interaction with patients.
• Students will introduce themselves as physician assistant students.
• Students will wear their Western University identifying nametags when in a clinical setting at all
times.
• Students will be able to explain what a PA is concisely and confidently to patient(s) and staff.

137
• Students who introduce themselves as a physician are subject to dismissal from the program.
• Students will not engage in any activity that may be construed as being unethical, immoral or
inconsistent with the practice of medicine.
Students breaching the Professional Conduct Policy will go through the following process:
The student will be required to have a student conference with the Program Chair and/or Clinical
Education Coordinators. The breach of conduct will be investigated and the student will be notified of the
results of the investigation. A verbal warning may be issued and/or a letter of unprofessional conduct may
be placed in the student’s file. A student may be placed in observational mode by the Program Chair
during the investigation, or may request that the student be summarily suspended during the investigation.
Academic Warning
The student who demonstrates unacceptable performance in any unit of study during any phase of the
program is notified of such performance by the Instructor of the course as soon as it becomes evident.
He/she is notified that continued poor academic performance can lead to academic probation and
dismissal.
Students whose performance is considered unacceptable as a result of not meeting the Standards of
Academic Progress will be placed on probation. The duration and conditions of the probationary period
will be recommended to the Dean of the College of Allied Health Professions on an individual basis by the
Allied Health Student Academic Progress Committee. The Committee may recommend remedial study
and/or repetition of a unit of study. This may result in extending the length of the program beyond 24
months. See, also, section on Probation, in the General Academic Policies and Procedures section for the
University.
a. Phase I: Students will be placed on academic probation as a result of "D” or “U" work in any unit
of study.
b. Phase II: Students will be placed on academic probation as a result of any of the following:
1. A final grade of "U" in any clinical rotation.
2. A final grade of “D” or “U” in Senior Seminar I and II.
3. Unacceptable performance on any component of clinical rotations education.
4. Receiving no credit in any of the Applied Clinical Projects.
c. Phase III: Students will be placed on academic probation as a result of any of the following:
1. Unacceptable performance in Senior Seminar III (the comprehensive examination.)
Students failing to achieve a passing score on the program comprehensive examination will be
required to demonstrate attainment of competencies related to the areas of deficiency through re-
evaluation. If the student has not attained the necessary competencies in the areas of deficiency
through re-evaluation, he/she may be required to complete a course of remedial study.
2. Less than “C” performance on any portion of the preceptorship grades.
3. Students will not be allowed to graduate until all competencies have been achieved.
Attendance
Attendance is expected for all lectures, classes, and academic-related activities. The individual faculty
members will make their own policy about attendance in their syllabus. It is required that students observe
the following policy:
a. Absences
1. All
unanticipated absences due to illness, accident, or other unexpected events must be
reported to the program within 24 hours.
2. Absences requested for physician/dentist appointments for student or dependents will be
considered only if requested in advance of the appointment. Due to the intense nature of the
curriculum, students are strongly encouraged to schedule appointments for evening and Saturday
hours to avoid class conflicts.
3. All anticipated absences for any reason, regardless of length, must have the prior approval by
the faculty.
All requests for anticipated absences must be submitted in writing at least two weeks prior to the
proposed absence. Requests will be considered on an individual basis and written notification of
approval or disapproval will be provided to the student within one week of receipt of request.
138
4. Students in clinical education/preceptorship are responsible for notifying both their
supervising physician(s), and the Physician Assistant program, regarding all absences whether
anticipated or unanticipated. Prolonged absences require notification each day to preceptors and
the program.
5. When an absence is the result of a sudden unavoidable circumstance, the program should be
notified as soon as possible and provided with an explanation for the absence.
6. Clinical rotation education/preceptorship absences and tardies will be made up at the
convenience of the preceptor or the program.
7. Five or more absences from a clinical rotation education can result in any of the following:
(a) repeat the entire rotation
(b) make up days assigned at the convenience of the preceptor
(c) grade of Incomplete assigned
Confidentiality of Medical Record and Health History Information
All data gathered about the patient and his/her illness, including all items within a patient's medical
history is privileged information.
a. Students should not discuss a patient's records in a manner or a situation that would reveal any
information about that patient or his/her records to persons not involved in his/her health care.
b. Charts or contents, e.g., lab reports, etc., are not to be removed from the hospital or clinical setting.
Patient Records - Physician Review and Countersignature
On each clinical rotation education, it is the student's responsibility to insure that ALL patients seen by
the student are also seen by the supervising practitioner. The supervising practitioner should also review
all student notes written in medical records and countersign these documents. Countersignatures should be
obtained before the patient is released on outpatient and in patient rotations.
Under no circumstances should a student initiate orders for any patient on any clinical educational
rotation without immediate physician consultation and countersignature. In addition, under no
circumstances should a student sign medical drug orders.
Under no circumstances should a student accept samples from pharmaceutical representatives on behalf
of the preceptor or himself.
These guidelines must be strictly adhered to for the student's protection and the protection of the patients
seen by students. Violation of these policies are viewed as transgressions in professional and/or academic
standards.
Falsifying a patient’s exam findings or record is considered a breech of professional conduct.
Title Identification/Representation
Role and title confusion are common problems encountered in dealing with patients, e.g., some patients
identify all those wearing short white coats as physicians. Students should be aware of this problem and
avoid misrepresentation by politely explaining their role and position.
a. In professional interactions with patients and others, a student should introduce himself or herself as
a "physician assistant student" using the title of Mr. or Miss, Mrs., or Ms.
b. Students should use the designation, "P.A.-Student" (PA-S), following all notations in charts,
records, and other medical forms.
Dismissal Recommendations
A student may be subject to dismissal from the program for substandard academic or professional
performance, as follows:
a. Students who earn two or more "D's”, “U's” or a combination of one “D” and one “U” throughout
the 24-month program may be dismissed from the program.
b. Lack of professional attributes considered appropriate for continuance in the program and
profession.
c. Any event that could result in either academic or professional probation for a student currently on
academic or professional probation.
d. Violation of the terms of probation.
e. Presenting him/herself as a physician.
139
Examination Policies
a. Students are not to communicate in any way during the examination and are to face the front of the
classroom at all times.
b. During scheduled examination hours, students are highly discouraged from going to the bathroom,
but will be allowed to go one at a time. The student will be required to turn in the exam and scantron
sheet as he/she goes to the bathroom.
c. Once a student finishes an exam, the student will turn in the exam and the scantron form to the
proctor, and after he/she leaves the examination room, he/she will not be permitted to re-enter the room
until the exam is declared over.
d. All students' belongings, i.e., notebooks, calculators, and headsets, etc., will be kept in front of the
room.
e. Questions will be answered at the discretion of the proctor during the examination period. Students
should be permitted to point out typographical or other errors present in the examination to the proctor.
f. Alternate seating shall be utilized for all examinations unless precluded by space availability.
g. Students are not to communicate in any way during the examination, are not to look at any other
student’s examination paper, and are to face the front of the classroom at all times. All pagers, cellular
phones, etc. are to be turned to vibrate mode
h. Violations of these examination policies and of Standards of Academic and Social Conduct will be
brought before the Student Conduct Committee.
i. The course instructor sets the date of assignments, midterms, and final examination. All tests and
assignments are to be taken as indicated in the course syllabus. Examination dates can only be changed
by the instructor after reviewed and approved by the department chair.
Evaluation and Grading
a. General: The degree of competency expected of all program graduates upon completion of the
professional curriculum is defined by the "Functions and Tasks of Physician Assistant Graduates". The
curricular components of the program are designed so that students' work toward achievement of these
competencies is measured via written and practical examinations and by evaluations of clinical
performance and professional development. Specific behavioral objectives have been defined for each
curricular component to assist the student and the program faculty in evaluating the degree of
attainment of these expected competencies throughout the 24-month curriculum.
b. Evaluation Methods: Overall student performance is evaluated differently during each phase using
one or a combination of the following methods:
1. Written examinations: Written examinations will vary based on the content of the individual
course. A combination of single answer multiple choice, matching, True/False, short answer,
essay and patient management type questions are used.
2. Practical or Laboratory Examinations: In selected courses, students will be observed obtaining
histories or performing physical exam components on simulated patients. They may also be
asked to "problem solve" based on a patient database. At times, they will be evaluated on their
ability to perform laboratory tests.
3. Student Presentations: Students may be asked to orally present individual or group projects,
patient cases, research papers, etc. These oral presentations may or may not be accompanied by a
written report.
4. Written reports: At various times, students will be evaluated on written reports of assigned
topics, written histories, physicals, discharge summaries, research papers, etc.
5. Professional Development Assessments: Assessments of each student's academic, professional
and interpersonal growth and development are shared with them on an individual basis
periodically during each phase of training.
6. Clinical Evaluations: Supervising preceptors are asked to assess the student's level of
attainment of competencies related to selected parameters within the domains of knowledge, skills
and attitudes, and to evaluate the student's overall performance while on clerkship. Evaluation
forms, which incorporate these areas to be evaluated, are utilized.
Students are responsible for securing these evaluations from the supervising preceptor(s) on
each rotation and ensuring that they are completed and returned to the program office in a timely
140
fashion. Preceptors are encouraged to discuss the student's performance and progress throughout
the rotation with him/her and to discuss the final evaluation prior to completion of the rotation.
Since the clinical evaluation is an essential part of the overall assessment of the student's
performance on a given rotation, course grades will not be computed without it. Students who
fail to obtain clinical evaluations prior to the end of the respective clinical rotation will be given a
grade of incomplete "I" for that clinical course. Courses with incomplete grades must be
completed prior to advancing to preceptorship (Phase III).
Clinical evaluation forms become a part of the student's academic profile record. Students are
required to sign each evaluation and are encouraged to sign at the time the evaluation is discussed
with the supervising preceptor. Students are provided copies of all their clinical evaluations when
these are submitted by the preceptor to the program.
7. Patient Write-ups: Students on clinical rotations are required to submit a minimum of one
patient write-up each month in the S.O.A.P. format. The chosen case must represent conditions
listed in the objectives for each module. The write-ups are due in the PA Program Office on or
before the last day of the clinical rotation.
8. Literature Review: Students can be requested to review current literature and complete a
critique. The critique will be evaluated on content, validity, clarity and clinical relevance.
9. Final Comprehensive Examination: A comprehensive examination is administered during the
Senior Seminar III and serves as a summative examination. This examination evaluates the
student's accumulated knowledge and skills while familiarizing him/her with the format of the
certification examination. Like the NCCPA certification examination, this examination consists
of a written multiple choice exam including questions on clinical skills competency.
10. Grade Reports: Official grades are turned in to the Registrar from the Dean of Allied Health
Professions, at which time the online student records system, BanWeb, is updated. Official grade
reports and unofficial transcripts will be available on the BanWeb student records systems
throughout the academic year. For more information on how to access the BanWeb student
records system, visit the Registrar’s website at http://www.westernu.edu/registrar.
Due to the nature of the clinical curriculum, i.e., variable duration and sequencing of clinical
courses education, course completion dates rarely coincide with traditional grading periods.
In these cases when final grades are not available at grade reporting time beyond the control of
the student and/or program, a grade of “M” is submitted to the Registrar in lieu of the course
clinical education grade. “M” grades are entered on the grade reports and are converted to
student achieved grades at the earliest possible opportunity.
An up-to-date summary of student performance is maintained in the Program Office Files and
is available to each student for his/her review.
11. Review of Examinations: Examinations are graded as soon as possible and one examination
is kept on file for student review.
12. Grading Scale: Final course grades are given based upon the traditional 4-point letter system,
as follows:
Grade Points
A 90% - 100% 4
B 80% - 89% 3
C 70% - 79% 2
D 65% - 69% 1
U Less than 64% 0
Cr/NCr 0
I Incomplete 0
M Missing 0
13. Clinical Rotation Education Grading Criteria: The Clinical Education grade is based on the
student’s singular performance as assessed by the preceptor, the student’s patient write-up, and
rotation exam.
1. Students are required to earn a final course grade of “C” or better in each clinical
rotation. Students cannot earn two or more “U’s” or “D’s” or a combination of one “D”
and one “U” throughout the entire 24 months of the program. Students will not be
141
allowed to advance to Phase III (Advanced Clinical Preceptorship) until all deficient
clinical rotation Education grade(s) are completed/remediated. Remediation will delay
the student’s progress to preceptorship and extend the program completion date.
The following applies regarding Cumulative GPA:
a. Students whose GPA falls below 2.5 must meet with the Program Chair prior
to registration for the next semester.
b. Students whose GPA falls below 2.5 are not eligible for further registration
unless probationary status is granted by the Dean of the College of Allied
Health Professions.
c. Students participating in Out-of-Area Rotations Clinical Education must
maintain a cumulative GPA of 3.00 in all preceptor assigned grades and Senior
Seminar I and II. The program may revoke the privilege of the Out-of-Area
Rotation Clinical Education if the student’s GPA falls below a 3.00.
2. To receive a complete grade for each clinical rotation education, all assigned
documents must be submitted to the PA Department, Pomona campus:
a. Time Records
b. Monthly Schedules
c. Returned Preceptor/Site Evaluation Form
Failure to submit items a and b and c at the end of each month will result in a grade of
Incomplete (I).
14. Preceptorship Grading Criteria Phase III: Advanced Clinical Preceptorship grades is are
based on the student’s performance as assessed by the preceptor and the student’s patient write-
up.
1. Students are required to receive a grade of “C” or better on their preceptorship
evaluation. The preceptor is responsible for evaluating the student's performance
monthly during the preceptorship. Students will be evaluated on the basis of their
clinical medical knowledge, diagnostic skills and treatment plans, as well as their
motivation, willingness to accept responsibility and interaction with patients, staff and
supervisors. It is the student’s responsibility to ensure that the preceptorship evaluation
entitled THE STUDENT PERFORMANCE FORM, (3) are returned to the program by
the last day of each month.
2. The following documents must be submitted in order to receive a final grade:
a. Time Records/Monthly Schedules
b. Returned Preceptor/Site Evaluation Form.
c. Final resume by July 31st.
Failure to submit items a-c will result in a grade of Incomplete (I).
Appealing a Course Grade
No course grade will be changed unless the instructor certifies in writing to the Registrar that an error
in computing or recording the grade occurred. If the student believes there is just cause to dispute a grade
for a course, the procedure is as follows:
Make an appointment to talk to the course instructor(s) who issued the grade. Upon written request
from the student, the course instructor(s) shall review the case with the student and a decision shall be
made by the course instructor to affirm or modify the grade. Within ten (10) working days, the course
instructor shall notify the student in writing of the decision. A copy of the letter shall be sent to the student
and the Department Chair of the PA program.
Upon written request from the student, the Department Chairperson shall review the case with the
instructor(s) and a decision shall be made by the course instructor(s) to affirm or modify the grade. Within
seven (7) working days, the Department Chairperson shall notify the student in writing of the decision. A
copy of the letter shall be sent to the appropriate course instructor(s). The course instructor(s) has the sole
responsibility to make the official grade change.
142
If the student is not satisfied with the outcome of the grade dispute procedure by the Department
Chairperson, the student may then appeal in writing to the Dean of the College of Allied Health
Professions within five (5) working days. The Dean of the College of Allied Health Professions shall
review the case with the student, Chairperson of the PA program and the course instructor(s) and a
decision shall be made by the course instructor(s) to affirm or modify the grade. Within seven (7) working
days the Dean shall notify the student in writing of the decision. A copy of the letter shall be sent to the
appropriate course instructor(s) and Chairperson. The course instructor(s) has the sole responsibility to
make the official grade change. Within five (5) working days following written notification to the student
of the action of the Dean of the College of Allied Health Professions, the student may appeal the decision
in writing to the Executive Vice President for Academic Affairs/Chief Academic Officer (CAO). Upon
written request from the student, the Executive Vice President for Academic Affairs/CAO shall review the
case and, within seven (7) working days, shall issue a decision in writing to the student, which may affirm,
modify, or reverse the previous action. A copy of that letter shall be sent to the Dean, and other
appropriate individuals. The decision of the Executive Vice President for Academic Affairs/CAO will be
final.
The student may remain in class or on clinical rotations pending the outcome of appeals, except in
cases of summary suspension, and except when the Executive Vice President for Academic Affairs/CAO
has suspended the student or has otherwise determined that it is inappropriate for the student to remain in
class or participate in clinical rotations, consistent with the appealed decision of the Dean of the College of
Allied Health Professions.
Appealing a Clinical Education Grade
Any student who has a dispute with a grade that was assigned by their clinical preceptor, will utilize the
following appeal process:
Contact the Clinical Education Coordinators, and notify them in writing of their concerns in reference
to their clinical performance grade.
The Clinical Education Coordinators will contact the preceptor to schedule a meeting to discuss the
student’s grade. The grade may or may not be re-assigned contingent upon the information that is gathered
by the Clinical Education Coordinators. The student will be notified in writing by the Clinical Education
Coordinators of the outcome. If the student does not agree with the outcome of the investigation, he/she
may appeal this decision to the Department Chair. If the student does not agree with the Department
Chair’s decision, the student has the right to appeal to the Dean of the College of Allied Health
Professions. (See the Appeal Process in Appealing a Course Grade)
Communications
Lockers: To improve the communication network and to foster student-staff and student-student
interchanges, lockers are located in the Health Sciences Center Student Commons. Students are expected
to follow the guidelines below in checking their lockers and will be held accountable for absences at
activities announced via the locker system. In the event that time constraints necessitate quick dispersal of
information, the program will disseminate this information via the U.S. Postal Service or through
telephone communication.
a. Each student will be assigned one locker.
b. During any portion of the program for which the student is present in the Physicians Assistant
Program on a daily basis, i.e., lecture series, he/she should check his locker and e-mail daily.
c. During Phase I of the program, each student should check his/her locker daily and electronic mail.
d. During Phase II & III of the program, correspondence from the program will be mailed to the
student either traditional mail or electronic mail.
e. During any portion of the program for which the student is out of town, e.g., remote clinical site,
holidays, correspondence from the program will be mailed or electronically mailed to the student.
Telephone:
a. During the course of the program, it is frequently necessary for members of the program staff to
contact students regarding scheduling and re-scheduling of classes, meetings, and other program
events, etc. Each class is responsible for developing a telephone communication network to include
names and home phone numbers for each member of the class. This "chaining" is utilized to
143
communicate last minute changes, announcements, etc. Each student is responsible for advising the
program departmental secretary of telephone number changes as soon as they occur.
b. Use of the program telephones is allowed only in emergency situations or with special permission
from the program faculty or staff; students are not to make or receive personal calls on the office
telephones.
c. Pagers and cell phones must be in silent/vibrate mode during all class times and examinations.
Returning from Leave of Absence While in Phase II or Phase III
A student returning from a leave of absence of 3 months or more is required to complete one ½ day
review session (arranged by the clinical education department). The review session must be completed
successfully before continuing with clinical education.
Student must:
a. Demonstrate proficiency performing
1. Complete Physical Exam
2. POP with a SOAP Note
b. Review the following videos:
Universal Precautions
Sterile Techniques
A second session may be scheduled if deficiencies are noted by the faculty.
Children in the Classroom/Labs
The PA classroom is an environment for enhanced learning and should be free from unnecessary
distraction. For this reason, children are not permitted in the classroom during examinations, no
exceptions.
During the Pediatrics Course children will be invited to class to participate in the pediatric workshop.
Student Academic Progress Committee
a. The Student Academic Progress Committee is comprised of department chairs and faculty members
of the College of Allied Health Professions.
b. Each year, the Student Academic Progress Committee shall periodically review the academic
achievements and the performance of all students. The names and grades of students in academic
difficulty shall be made available to the Student Academic Progress Committee by the department
chairs and faculty members.
c. After reviewing the student's achievement and performance records, the Student Academic Progress
Committee may recommend to the Dean of the College of Allied Health Professions any of the
following courses of action for a student: promotion, probation, remediation, dismissal from the
College, psychological and educational assessment and recommendation, or no action.
d. The Student Academic Progress Committee also has the responsibility of recommending to the
faculty, as a whole, the awarding of the Master of Science degree upon satisfactory completion of all
requirements for graduation as stated in the University Catalogue.
e. All recommendations of the Student Academic Progress Committee shall be in writing to the Dean
of the College of Allied Health Professions, who will make the information available to the student.
144
CURRICULUM ORGANIZATION
PHASE I
First Semester
Year I Students
Course # Title Sem. Hours
PA5005 Medical Terminology 1 (Cr/NCr)
PA5010 Structure & Function I 4
PA5020 Clinical Skills I 3
PA5030 Physical Assessment I 3
PA5040 Health Promotion/Disease Prevention I 3
PA5050 Introduction to Adult Medicine & Pathophysiology I 5
PA5060 Pharmacology and Therapeutics I 3
PA5070 Psychosocial Dynamics 3
Total 25
Second Semester
Year I Students
Course # Title Sem. Hours
PA5011 Structure & Function II 4
PA5021 Clinical Skills II 3
PA5031 Physical Assessment II 3
PA5041 Health Promotion & Disease Prevention II 2
PA5051 Introduction to Adult Medicine & Pathophysiology II 5
PA5061 Pharmacology and Therapeutics II 3
PA5100 Pediatrics 3
HSCI5206 Research Methods II 3
Total 26
Third Semester
Year I Students
Course # Title Sem. Hours
PA5110 OB/GYN 3
PA5120 Geriatrics 3
PA5130 Emergency Medicine 3
PA5140 Professional Roles & Responsibilities 3
PA5160 Health Care Delivery System 3
Total 15
PHASE II
Fourth Semester
Year II Students
Course # Title Sem. Hours
PA6020 Senior Seminar I 3
### Clinical Rotations I (4) 12
PA6970 Applied Clinical Project I 1
Total 16
Fifth Semester
Year II Students
Course # Title Sem. Hours
PA6030 Senior Seminar II 3
### Clinical Rotations (4) 12
PA6980 Applied Clinical Project II 1
Total 16

145
PHASE III
Sixth Semester
Year II Students
Course # Title Sem. Hours
PA6040 Senior Seminar III 2
PA7900 Advanced Clinical Preceptorship 9
PA6990 Applied Clinical Project III 7
Total 18
COURSE DESCRIPTIONS
PA 5005 Medical Terminology (1 credit hour, Cr/NCr)
This course is designed to provide a framework for building a comprehensive medical vocabulary. The
basic techniques of medical word building will be used to enhance appropriate use and spelling of medical
terms in oral and written presentations.
PA 5010 Structure and Function I (4 credit hours)
An integration of sciences: anatomy, physiology, and biochemistry as they contribute to the
understanding of clinical medicine. This course is correlated to the Introduction to Adult Medicine course.
PA 5011 Structure and Function II (4 credit hours)
Continuation of PA 5010.
PA 5020 Clinical Medical Skills I (3 credit hours)
This practical course exposes the physician assistant student to basic clinical skills used in the primary
care office. Skills include, but are not limited to, venipuncture, universal precautions, suturing, casting and
sterile procedures.
PA 5021 Clinical Skills II (3 credit hours)
Continuation of PA 5020.
PA 5030 Physical Assessment I (3 credit hours)
This course is designed to provide students with fundamental cognitive knowledge of interviewing,
formulating write-ups and physical assessment techniques. Students also learn how to analysis data and the
formulation of a therapeutic plan based on the health history, and physical examination. This course is
correlated with the Introduction to Adult Medicine.
PA 5031 Physical Assessment II (3 credit hours)
Continuation of PA 5030.
PA 5040 Health Promotion and Disease Prevention I (3 credit hours)
This course stresses the principles of wellness including detailed discussions of nutrition, exercise,
alcohol and tobacco as they relate to culturally diverse patient populations.
PA 5041 Health Promotion and Disease Prevention II (2 credit hours)
Continuation of PA 5040.
PA 5050 Introduction to Adult Medicine and Pathophysiology I (5 credit hours)
This course represents an introduction to clinical adult medical and surgical disorders as well as
pathophysiology from a primary health care perspective. This course is correlated with structure and
function, pharmacology, and physical assessment. It also incorporates signs, symptoms, differential
diagnosis, laboratory diagnosis and treatment modalities for selected disciplines.
PA 5051 Introduction of Adult Medicine and Pathophysiology (5 credit hours)
Continuation of PA 5050.
146
PA 5060 Pharmacology and Therapeutics I (3 credit hours)
This course stresses the principles of drug action and is correlated with the system orientation of the
"Introduction to Adult Medicine." Current aspects of drug therapy are studied with particular emphasis on
the activity.
PA 5061 Pharmacology and Therapeutics II (3 credit hours)
Continuation of PA 5060.
PA 5070 Psychosocial Dynamics (3 credit hours)
This course provides students with the necessary skills to diagnose and treat common mental health
disorders seen in an ambulatory family practice population. It also provides the students with information
that enable them to factor "humanity" into their assessment, diagnosis and intervention strategies. The
course also includes modules on family structure and functioning, the dynamics of aging, death and dying,
and human sexuality.
PA 5100 Pediatrics (3 credit hours)
This course will provide the primary care physician assistant student with an introduction to the basic
principles of pediatrics. This pediatric course will provide the students with the basic cognitive skills
required to obtain and perform an appropriate newborn, pediatric and adolescent history and physical.
PA 5110 Obstetrics/Gynecology (3 credit hours)
This course is designed to introduce the PA student to the fundamental principles and practice of
obstetrics and gynecology and the unique physical and emotional health care needs of female patients.
Emphasis will be placed on the pathophysiology, etiology, management and prevention of clinical
problems that transpire in a woman's life cycle from infancy through menopause. Students will also learn
the essential details of the OB-GYN clinical evaluation and strategies in the diagnosis and treatment of
common OB-GYN medical, surgical, and obstetric disorders of women.
PA 5120 Geriatrics (3 credit hours)
This course introduces the students to all aspects of geriatrics. The course provides a framework for
common geriatric illness, diseases, diagnoses and treatment. It discusses normal and pathologic changes of
aging. It explores health care financing for the elderly. Common ethical and legal issues in caring for the
elderly are discussed.
PA 5130 Emergency Medicine (3 credit hours)
This course emphasizes assessment skills in emergency medicine. It would provide students with an
overview of emergency medicine, history and physical examinations. The course will introduce current
diagnosis and treatment for commonly encountered medical emergencies. The student should be able to
develop a working knowledge and framework for the evaluation and treatment of common medical and
surgical procedures.
PA 5140 Professional Roles and Responsibilities (3 credit hours)
This course examines the different professional roles that can be assumed by a physician assistant. Also
included are discussions of the laws in which PA's are required to follow to practice medicine and the
health care delivery system.
PA 5160 Health Care Delivery Systems (3 credit hours)
This course will introduce the student to the current models of health care delivery systems utilized
within healthcare. It will also identify the roles of a PA within the current health care delivery systems.
HSCI 5206 Research Methods II (3 credit hours)
The purpose of this course is to introduce students to a variety of research methodologies. Included will
be historical studies, case studies, observational studies, the survey, quasi-experimental designs, and
147
experimental designs. Generalizability issues and validity/reliability issues related to research are
presented. HPE 5106 or its equivalent is a prerequisite for this course.
PA 6020 Senior Seminar I (3 credit hours)
Senior Seminar consists of a series of examinations and discussions. Clinical skill problems, case
presentations, and problem oriented physical examinations are used as teaching tools to help the physician
assistant student understand his/her role as a practicing PA.
PA 6030 Senior Seminar II (3 credit hours)
Senior Seminar II consists of a series of examinations and discussions. The purpose of the course is to
further develop the physician assistant student's clinical skills and test-taking abilities.
PA 6040 Senior Seminar III (3 credit hours)
Senior Seminar III consists of a comprehensive examination and a problem oriented physical. The
purpose of the course is to further develop the physician assistant students' clinical skills and prepare for
the National Certification examination.
PA 6970 Applied Clinical Project I (1 Credit Hour, Cr/NCr)
Preparation of a clinical project, under the supervision of a member of the PA faculty, that will be
completed and presented in PA 6990.
PA 6980 Applied Clinical Project II (1 Credit Hour, Cr/NCr)
Continuation of PA 6970.
PA 6990 Applied Clinical Project III (7 credit hours, Cr/NCr)
In this course, the student presents the Clinical Project in partial fulfillment of requirements for the
degree of Master of Science in Physician Assistant Studies.
PA 7010 Family Practice I (3 credit hours)
A clinical rotation that provides students with experience in a primary health care setting and will focus
on medical problems most commonly encountered by a family practitioner and certified physician
assistant.
PA 7020 Family Practice II (3 credit hours)
This rotation is an extension of the Family Practice I experience and will permit students to extend their
experiences in primary health care. Students may elect to return to the site of their initial family practice
rotation or select a second type of primary care experience including such opportunities as migrant, or
Indian Health Service activities.
PA 7030 Internal Medicine (3 credit hours)
A clinical rotation that provides students with the opportunity to diagnose, manage, and treat patients in
an in/out patient setting. The student will participate in the direct care of patients including initial
interview, physical examination, hospital rounds, clinical conferences and management decision sessions.
PA 7040 Emergency Medicine (3 credit hours)
Students obtain experience in the management of acute medical and surgical care with an emphasis on
the development of skills required to treat life-threatening illness and injury.
PA 7050 Urgent Care (3 credit hours)
Students obtain experience in the management of acute medical and surgical care with an emphasis on
the development of skills required to treat non-life-threatening illness and injury as well as triage and
assess true emergent cases.
148
PA 7060 Pediatrics (3 credit hours)
Students gain knowledge in the care of infants and children, including an understanding of normal
development, and the recognition and management of common childhood illness, immunization updates
and patient education opportunities.
PA 7070 Obstetrics and Gynecology (3 credit hours)
Students learn about women's health issues: preventive care, prenatal care and post natal care, current
contraceptive technology, and medical therapeutics which aid in the well being of the female patient.
PA 7080 General Surgery I (3 credit hours)
Students are involved in the direct care of patients undergoing surgery including both pre-surgical
evaluation and post-surgical maintenance. Students may select either in-patient or out-patient surgical
settings.
PA 7090 Public Health (3 credit hours)
This rotation provides the students with an insight into epidemiology and how various public health
agencies play a significant role in health promotion and disease prevention.
PA 7110 Community Medicine Service (3 credit hours)
This rotation provides experience in community health. It exposes students to common problems seen
in family medicine as well as conditions seen in public health. This allows the student to understand how
community clinics play a significant role in health promotion and disease prevention.
PA 7120 Neurology (3 credit hours)
This rotation provides the student with the opportunity to learn initial diagnosis, differential diagnosis,
work-up and follow-up of inpatients with new or complicating neurological problems.
PA 7500 Extended Core Selectives (3 credit hours)
Students can pursue additional experience in a variety of clinical specialties and sub-specialties or they
can extend their knowledge by repeating one of the required clinical rotations. Repeatable for a maximum
of 6 credit hours. Repeating the same decimal subdivision is not permitted, except for PA7500.99.
PA 7500A Orthopedics
PA 7500B Oncology
PA 7500C Family Practice III
PA 7500D Infectious Disease
PA 7500E Cardiology
PA 7500F Cardiothoracic Surgery
PA 7500G Geriatrics
PA 7500H General Surgery II
PA 7500J Rheumatology
PA 7500K Endocrinology
PA 7500L Dermatology
PA 7500M Occupational Medicine
PA 7500N Trauma Surgery
PA 7500P Psychiatry
PA 7500Q Otolaryngology
PA 7500R Directed Research/Independent Study
PA 7500Z Other
PA 7900 Advanced Clinical Preceptorship (9 credit hours)
Advanced Clinical Preceptorships prepare the second year PA student for the transition from student to
primary care practitioner. This course is three months in length and provides the student with valuable
patient management data while also emphasizing continuity of care.
149
HONORS AND AWARDS
The following are presented on Honors Day:
Dean's Award
PA Class President Award
PA Class Morale Award
PA Class Award
Joseph and Dorothy Gendron Journalism Award
Western University PA Service Award
The President's Society Award
Linda Fox Memorial Endowment Fund Award
Guy M. Allmon Scholarship Fund Award
The following are presented at graduation:
Dean's Award
PA Class President Award
PA Class Morale Award
PA Class Award
Western University PA Service Award
Blake Award of Academic Excellence
Martha Medina Memorial Award
The Bertha Oliver Memorial Award
Andrea J. Reina Memorial Award
150
ACADEMIC CALENDAR
2002-2003
PA PROGRAM
Aug. 5-9, 2002
Orientation/Registration
Monday, Aug. 5, 2002
Fall Semester Tuition Due (1
st
years)
Saturday, August 10, 2002
Convocation/White Coat Ceremony
Monday, August 12, 2002
Classes begin (1st year)
Monday, Aug. 26, 2002
Fall Semester Tuition due (2
nd
years)
Sunday, September 1, 2002
Rotations begin (2nd year)
Monday, September 2, 2002
Labor Day - No Class
Monday, October 14, 2002
Columbus Day - No Class
October 17-20, 2002
CAPA Convention - No Classes
Wednesday, November 27, 2002
Thanksgiving recess - Noon
Monday, December 2, 2002
Classes Resume
Friday, December 13, 2002
Last Day of Lectures for Fall Semester
December 16-20, 2002
Finals Week
Monday, December 23, 2002
Winter Recess
2003
Monday, January 6, 2003
Classes Resume
Friday, Jan. 31, 2003
Spring Semester Tuition Due (1
st
years)
Monday, January 20, 2003
Martin Luther King Day - No Classes
Monday, February 17, 2003
President's Day - No Classes
Tuesday, Feb. 18, 2003
Spring Semester Tuition due (2
nd
years)
Monday, March 17, 2003
Spring Break Begins
Monday, March 24, 2003
Classes Resume
Monday, April 14, 2003
Honor's Day
Friday, May 9, 2003
Last Day of Lectures for Spring Semester
May 12-16, 2003
Spring Semester Finals
TBA
Graduation
Monday, June 2, 2003
First Day of the Summer Session
Friday, July 4, 2003
Independence Day - No Classes
Friday, August 1, 2003
Last Day of Summer Semester
THE PHYSICIAN ASSISTANT OATH
I pledge to perform the following duties with honesty, integrity, and dedication, remembering always
that my primary responsibility is to the health, safety, welfare, and dignity of all human beings:
I recognize and promote the value of diversity and I will treat equally all persons who seek my care.
I will uphold the tenets of patient autonomy, beneficence, non-maleficence, justice, and the principle of
informed consent.
I will hold in confidence the information shared with me in the course of practicing medicine, except
where I am authorized to impart such knowledge.
151
I will be diligent in understanding both my personal capabilities and my limitations, striving always to
improve my practice of medicine.
I will actively seek to expand my intellectual knowledge and skills, keeping abreast of advances in
medical art and science.
I will work with other members of the health care team to assure compassionate and effective care of
patients.
I will uphold and enhance community values and use the knowledge and experience acquired as a PA
to contribute to an improved community.
I will respect my professional relationship with the physician and act always with guidance and
supervision provided by that physician, except where to do so would cause harm.
I recognize my duty to perpetuate knowledge with in the profession.
These duties are pledged with sincerity and on my honor.
152
College of Graduate Nursing
Master of Science in Nursing/Family Nurse Practitioner Program
Master of Science in Nursing Track
Post-Masters Family Nurse Practitioner Track
Advanced Practice Nurse to Family Nurse Practitioner Track
ACCREDITATION
The programs of the College of Graduate Nursing are California Board of Registered Nursing approved
and accredited by the Commission on Collegiate Nursing Education (CCNE). Graduates are eligible to
apply for state certification and to sit for the appropriate national certification examinations.
MISSION
The Western University College of Graduate Nursing (CGN) has established a community for learning
that offers bachelor-prepared nurses an opportunity to expand their education through a web-based Master
of Science in Nursing and Family Nurse Practitioner certificate program in preparation for providing
primary health care for their community. The CGN faculty members foster excellence, creativity,
innovation, self-reflection, personal and professional accountability, collaboration, cultural sensitivity, a
passion for caring, leadership, and lifelong scholarship through a mentoring relationship with students.
In accordance with the mission of Western University of Health Sciences, the faculty endeavor to:
• improve the health of the community through the preparation of professional advanced practice nurses
with expertise for effective provision of family-centered care for primary health care needs of a
rapidly changing society; and,
• develop each student’s potential through role modeling, empowerment, sharing of knowledge, caring,
and advocating mutual respect.
PHILOSOPHY
The College of Graduate Nursing is distinguished by the faculty’s beliefs about nursing, persons,
environment, health and nursing education:
Nursing, as a professional discipline, is an art and a humanistic science of caring. The art of nursing is
in its understanding of the meaning of a holistic health-illness experience and the perception of the moral
and ethical significance of care, as well as the integration of technical skill with relevant theory. The art of
nursing employs critical thinking and respect; it fosters open and effective oral and written communication
with clients and colleagues. The humanistic science of nursing is the generation and application of the
body of theoretical nursing knowledge, behavioral and natural science, the humanities, and the arts,
employed in a caring, respectful manner.
The professional practice of nursing is the directing of knowledge, competencies and processes toward
assisting persons to achieve quality of life, health, well-being, or peaceful death. Advanced practice
nursing competencies are complex psychomotor and interpersonal skills, leadership, collaboration, self-
evaluation, and scientific application and inquiry that are guided by professional standards. Processes
include critical thinking, accountability, problem solving, decision-making, caring, advocacy, and
involvement. Knowledge for Advanced Practice Nursing is built upon the foundation acquired in a
Bachelor of Science in Nursing and its related arts and sciences, as well as information gained from prior
nursing experience. Expertise for Advanced Practice focuses on socio-cultural, ethical, economic and
political issues, advanced technology, theory, research, and advanced physical and psychological sciences.
Evidence-based professional nursing practice demands recognition that each individual has unique needs
that can be assessed and incorporated into a research-based nursing plan.
Persons who participate in family-centered nursing care are individuals with unique lifestyles,
knowledge, beliefs and values, needs, and goals and are able to make autonomous decisions. These clients
of nursing involve complex biological, behavioral, emotional, sociocultural, philosophical and spiritual
dimensions and interact dynamically with their environment. Clients interact through relationships with
families, in various forms, and communities. Persons have a right and responsibility to participate
153
collaboratively with nurses and other health professionals in decisions and shared accountability for
outcomes.
Environment is both the internal and external contexts of the individual. Environment involves
reciprocal multidimensional and dynamic forces that affect the person’s health and well being.
Health is a multidimensional, adaptive state of being reflecting internal and external environmental and
developmental influences. Health is a relative condition, characterized by wellness, illness, disease, or
dysfunction. Health may be a reflection of individual perceptions of balance and harmony.
Nursing Education is a process that provides opportunities to expand and extend knowledge for
continued growth and competency of the individual and the profession. It draws on multiple disciplines
and involves organized learning experiences that augment previous knowledge and skills in preparation for
professional nursing practice. Nursing education is a flexible process that fosters creativity and
independent and critical thinking. We value self-directed learners, continual learning, and active
engagement in a teaching/learning partnership. The educational process supports personal, social and
intellectual development while assisting students to attain academic and professional goals. Through the
provision of meaningful learning experiences, nursing education seeks to assist the learner to formulate
and structure nursing knowledge, while distinguishing relevant from non-relevant information and
developing safe and effective nursing practice. The educational program seeks to evoke honesty,
excitement of discovery, encourage self-expression and serve as a catalyst for lifelong learning.
Teachers and learners in the learning community engage in interactive processes that enhance the
potential and respect of each person. Teachers act as facilitators, and through their expertise and skill, are
role models for student professional practice. The faculty as a whole focuses on the provision and
organization of the curriculum and provides a milieu that encourages questioning, growth and mutual
evaluation.
The CGN faculty believes that students are active, self-directed, adult learners who are committed to
safe and effective professional practice and rigorous courses of study. Students are accountable for
integrity of academic accomplishments, professional practice and self-assessment. Students bring unique
backgrounds and have individual goals that create differing responses to the learning process. Learning is
a personal responsibility.
OUTCOME COMPETENCIES FOR GRADUATES
Graduate education for Advanced Practice Nursing is based on undergraduate nursing knowledge and
experience. The CGN places emphasis on critical thinking, clinical competence, communication, decision-
making, accountability, writing, and technological competence.
The course of study, including specifically stated learning activities, is a series of sequential courses
designed to assist learners in attaining the following behaviors prior to being approved for program
completion.
Graduates of the Western University of Health Sciences College of Graduate Nursing, as candidates for
state and national certification will:
1. Critically analyze literature for the purpose of evidence-based advanced nursing practice, education,
and life-long scholarship.
2. Participate in the development of new nursing knowledge through the application
and development of theory and research.
3. Apply knowledge from the humanities and physical, social, psychological, nursing, medical, and
pharmacological sciences to decision-making in order to provide and evaluate accountable primary
health care which is commensurate with professional and legal parameters of the role of Family Nurse
Practitioner.
4. Provide individualized client and family-centered health care that demonstrates recognition of
reciprocal environmental interaction and diversity of socio-cultural values and beliefs among members
of a rapidly changing society.
5. Apply comprehension of changing national and local public policy related to health care standards,
health care systems and financing when planning and providing health care for individuals, families,
and communities.
6. Empower client collaboration and decision-making for desired health care outcomes and quality of
life through advocacy, caring, and the application of critical thinking skills, theories of learning and
communication, and ethical principles.
154
7. Integrate health promotion, illness prevention, and health maintenance strategies into holistic health
care provided for diverse individuals, families, and communities.
8. Provide leadership through participation in professional and community development activities and
advocacy of the advanced nursing practice role.
9. Demonstrate mastery of traditional and electronic access to information resources for research,
study, and practice.
CURRICULUM
The College of Graduate Nursing currently offers a combined Master of Science in Nursing/Family
Nurse Practitioner program, two Post-Master’s Family Nurse Practitioner tracks, and a Master of Science
in Nursing track.
The Master of Science in Nursing/Family Nurse Practitioner Program (MSN/FNP) curriculum requires
the completion of 50 semester units over a two- or three-year period. The Post-Masters Family Nurse
Practitioner (FNP-only) track curriculum requires 37 semester units for completion and can be completed
in one year. Both of these tracks require the completion of 675 preceptored clinical hours.
The Advanced Practice Nurse to Family Nurse Practitioner (APN-FNP) track requires 19 semester
units for completion and can be completed in one year. The APN-FNP track requires the completion of
180 clinical hours.
The Master of Science in Nursing track requires 17-21 semester units to be completed in a year. This
degree track is designed for Advanced Practice Nurses.
Graduates will be prepared to meet the criteria established by the California Board of Registered
Nursing as advanced practice nurses. Nurse practitioners work in a variety of health care settings
independently, or in groups of health care professionals, under collaboratively developed and agreed upon
standardized procedures.
Instructional Design: Distance Learning
The College of Graduate Nursing programs are designed for the adult learner. The design uses
educational and instructional learning theories that emphasize outcome competencies as the desired goal,
rather than time on task, and individualized instructional strategies as well as classroom and clinical
instruction.
12 Month Academic Year
The twelve month academic calendar begins in August and includes three 15-week semesters with two-
week intersessions between each semester.
Integrated Courses
For the clinical programs (MSN/FNP or FNP-only) health care issues are studied across the life span
with a focus on groups of specific health care problems, namely, Common, Acute, Chronic and Complex
health care problems for each age group. The course of study is planned to allow for integration of
knowledge and skills across each area of study (courses).
Essential Intellectual Skills
In addition to essential academic content and performance skills, each course requires learning
activities that foster intellectual skill development for critical thinking and decision making as well as oral
and written communication.
Web-based Learning
The instructional modality that is most evident in this curriculum is web-based learning. The majority
of courses include required asynchronous discussion sessions in which students and faculty participate in
collaborative learning of the assigned readings. Students are expected to be on-line and engaged in
learning activities from the first day of the first semester. The CGN Web site is designed to provide the
learner with the information needed to be successful in each course including learning objectives, content,
learning activities, evaluation methods and grading criteria.
155
Weekend Seminars
Each semester students are required to attend two intensive, two- to three-day weekends on campus.
These classes provide valuable time for faculty and peer interaction, student presentations, lectures,
clinical and didactic testing, skills laboratories, and selected clinical practice with faculty.
Culminating Experience
Master's degree education usually culminates with a required research or research-based project or
thesis. The MSN/FNP program and MSN track, however, require that each student complete a project that
features the implementation of a clinical improvement project (one credit hour). Students enrolled in the
MSN/FNP program must complete a minimum of 540 clinical hours prior to beginning their culminating
project or enrolling in CGN 5608
Program Completion
Students who have met the following requirements will be considered candidates for the degree of
Master of Science in Nursing and/or Family Nurse Practitioner Certificate:
• Completion of all course requirements with a minimum overall GPA of 3.0.
• Completion of 675 clinical practice hours (MSN/FNP and FNP-only) or 180 hours for APN-FNP
students. Students must satisfactorily demonstrate all clinical competencies.
• Completion of the culminating experience project (MSN/FNP and MSN students).
• Has complied with all the legal and financial requirements of the University as stated in the University
Catalogue.
• Has demonstrated no serious deficiencies in ethical, professional or personal conduct as outlined in
Standards of Professional Conduct
• Students enrolled in a post-Master's track (APN-FNP or FNP-only) will be candidates for the FNP
Certificate only.
Unless the President of the University has granted special permission, all students must attend in person
and participate in the Commencement program at which time the degree is conferred. If the President
grants special permission to be excused from graduation, the graduate may be required to present himself
or herself to the Executive Vice President of Academic Affairs or appropriate Dean at a later date in order
to receive his or her diploma.
ADMISSION POLICIES
Prerequisite Requirements for MSN/FNP Program*
• Bachelor of Science in Nursing** from a National League of Nursing (NLN) or Commission on
Collegiate Nursing Education (CCNE) accredited program
• GPA of 3.0 overall in the last 60 semester units or 90 quarter units
• Pathophysiology
• Statistics
• Registered Nurse (RN) licensure in the state where preceptored clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
Prerequisite Requirements for Post-Masters Track (FNP-Only)*
• Master of Science in Nursing or related field
• BSN in Nursing** from a National League of Nursing (NLN) or Commission on Collegiate Nursing
Education (CCNE) accredited program
• GPA of 3.0 overall in the last 60 semester units or 90 quarter units
• Pathophysiology
• Statistics
• Registered Nurse (RN) licensure in the state where preceptored clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
Prerequisite Requirements for MSN-only Track*
• BSN Degree in Nursing** from a National League of Nursing (NLN) or Commission on Collegiate
Nursing Education (CCNE) accredited program
• Nurse Practitioner, FNP, PNP, Adult, GNP, CRNA, or CNM
156
• GPA 3.0 overall in the last 60 semester units or 90 quarter units
• Statistics
• Registered Nurse (RN) licensure in the state where preceptored clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
Prerequisite Requirements for Advanced Practice Nurse to Family Nurse Practitioner (APN-FNP)
Track*
• Master of Science in Nursing or related field
• BSN in Nursing** from a National League of Nursing (NLN) or Commission on Collegiate Nursing
Education (CCNE) accredited program
• GPA of 3.0 overall in the last 60 semester units or 90 quarter units
• Pathophysiology
• Statistics
• Registered Nurse (RN) and/or Nurse Practitioner (NP) licensure in the state where preceptored
clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
• Verification of Advance Practice Nurse Specialty
*Students who do not meet the requirements for admission may petition the Admissions Committee for
special consideration. If admitted on probationary status, a student must achieve a GPA of 3.0 in pre-
program and first semester courses with no options for remediation.
** Bachelors in a related field will be reviewed on a case-by-case basis.
Requirements for Admissions (All Tracks)
• Completed Application
• Three Letters of Reference (faculty & employers within past two years)
• Resume
• Personal Statement which addresses your understanding of advanced practice nursing, personal career
goals and how your background strengthens your aptitude to become an Advanced Practice Nurse
• Application Fee of $60
• Official transcripts from all colleges/universities attended
• All graduates must agree to sit for the national certification examination within six months of
graduation
Decisions of the Admissions Committee regarding the admission of applicants to its programs are final.
Computer Requirements
The following is a list of computer equipment necessary for the Web-based programs:
• PC System - Minimum 133 MHz Intel Pentium® processor or equivalent
• Windows 95 or higher
• Minimum 64 MB RAM
• 1GB of free hard disk space
• Modem – 56 kbps or higher
• CD-ROM drive
• Newest version of Internet Explorer
• Microsoft Office Standard Suite 97 or higher with Word, Excel and PowerPoint
• New version of virus protection that supports weekly updates
• Newest version of Real Player plug-in
• Newest version of Adobe Acrobat plug-in
• 16-bit sound card and speakers
• Internet service provider (flat rate recommended)
• Printer
• Dedicated telephone line (recommended)
157
MSN-Harbor Track
In conjunction with the Harbor-UCLA Research and Education Institute's Women's Health Care Nurse
Practitioner Program, an accelerated Master of Science in Nursing degree is available for graduates and
currently enrolled students of the Women's Health Care Nurse Practitioner Program. For more information,
please contact the Western University College of Graduate Nursing. Students admitted to this track must
complete at least 17 units of Western University coursework. Additional units may be required based
upon assessment of transfer coursework.
REGISTRATION
Following completion of the admissions procedure and written documentation of acceptance into
Western University's College of Graduate Nursing, an orientation packet will be mailed directly to the
student. All students will complete registration at the campus-based orientation in Pomona. Registration
will be completed via mail for continuing students and will be done annually prior to each academic year.
Orientation and Pre-Program Courses
All students enrolled in the College of Graduate Nursing will be required to complete two mandatory
orientation seminars on the Pomona campus. Orientation will include computer skill training (e-mail, e-
mail attachments, address book use, file management, and Microsoft software use), an introduction to
computer-based learning, and an overview of Western University curriculum. Students will complete
registration, purchase medical equipment and orient to the services of the University at this time. All
students will begin a Communication and Information Management course (CGN 5000), which prepares
students for success in Western University of Health Sciences' computer-based courses. Students enrolled
in the Advanced Physical Assessment course (CGN 5601) will participate in clinical exam skills training.
All students must successfully complete the Pre-Program courses in order to continue in the curriculum.
Students must successfully complete the Advanced Physical Assessment course prior to beginning their
clinical preceptored experience.
Medical Information
Verification of the following must be on file in the Office of the Registrar at the time of registration:
• Completion of Western University's History and Physical form
• Medical clearance for participation in program/clinical
• A recent (within past six months) PPD or Chest X-ray report indicating that the student is free of
tuberculosis (all students). Students are required to submit documentation of PPD/Chest X-ray
annually while enrolled at Western University
In addition, student enrolled in clinical tracks must file:
• Verification of immunization or immunity for: Polio, MMR, Varicella, Diphtheria/tetanus (within past
10 years) and completion of the Hepatitis B series
• Current CPR certification (and maintained throughout the program of study)
Health Insurance
All students must be covered by health insurance throughout the program. Proof of health insurance must
be provided at the time of registration annually.
TUITION AND FEES
By action of the Board of Trustees, the tuition and fees for the 2002-2003 year are as follows:
MSN/FNP Program 50 units @ $450/unit
FNP-Only Track 37 units @ $450/unit
APN-FNP Track 19 units @ $450/unit
MSN-Only Track 21 units @ $400/unit
MSN-Harbor Track 17 units (minimum) @ $400/unit
Student Body Fee $40/year
158
Other Fees and Expenses
Application Fee $60
Required Textbooks $1800 MSN/FNP & FNP first
year (approximate)
Medical Equipment $400 MSN/FNP & FNP students
(approximate)
Computer with Modem $1500 (approximate)
Lodging/Meals/Travel varies, depending on distance and mode of travel.
Lost ID Badge $10
Note: All tuition and fees are subject to change.
Library Services
Western University's library resources can be accessed on the Internet at: http://www.westernu.edu.
Database access is available to distance students following registration. Nursing students will access the
internet sites for some resources and perform database searches for class assignments or research projects.
Full text articles are not always available via the World Wide Web, therefore, students are expected to
utilize traditional library services for research assignments, whether in the student's community or near
their home
Required Supplies for Clinical
Physical Exam Equipment:
• Lab Coats (to be worn at all times)
• Name Tag (to be worn at all times)
• Ophthalmoscope
• Otoscope
• Pen Light
• Reflex Hammer
• Ruler (cm)
• Stethoscope
• Tuning Fork # 512
• Hand Held Snellen Chart
Bookstore
Textbooks, medical equipment and software are available through the University Bookstore. All items
can be ordered by phone and mailed directly to your home using a credit card.
ACADEMIC POLICIES AND PROCEDURES
Academic/Clinical Advisement
All students are assigned a faculty advisor upon matriculation into the program. Entering students
should contact this faculty advisor no later than the first Seminar Weekend of enrollment in the program.
Such contact may take place in person, on-line, or through both methods. Although advisors are assigned,
the student may, with the agreement of the faculty request a different advisor. Reasonable efforts will be
made to assign a student to the advisor of choice, although scheduling problems may make this impossible.
Continuing students have the opportunity to contact designated faculty advisors and/or individual
instructors on-line, by appointment in person or telephone, or at any Seminar Weekend. Regular and on-
going contact with the academic advisor is encouraged as one method to enhance success in the program.
All students must meet with their faculty advisor in the semester prior to their anticipated completion for a
final review of graduation requirements and approve to file for graduation.
Standards of Academic Performance
As a College of Graduate Nursing, the standard for successful progress is higher than that for
undergraduate education. An overall grade point average of 3.0 is required for graduation. Each student
will also demonstrate an acceptable level of performance for all Outcome Competencies (as outlined in the
159
curriculum). Each graduate is also expected to demonstrate critical thinking skills as well as competence
in written and oral communication. Students who are placed on academic probation are required to
contact their academic advisor.
Academic Progression
Regular admission and matriculation to any of the CGN programs is for full-time enrollment. Each of
the programs of the CGN is built around a sequence of courses that build on prior courses. Consequently,
academic progression is based on successful completion of each course in a program, in sequence.
Students are expected to enroll in and successfully complete each course in a sequential progression.
Part-time enrollment is possible, however, students anticipating part-time enrollment should discuss
plans with an academic advisor prior to matriculation. Students who decide to switch from full-time
enrollment to part-time enrollment should discuss plans with the academic advisor.
A grade of B or Cr (Credit) is required in each course in the program. Students who earn less than a B
in a theory course must successfully remediate the course to continue in the program. Students who earn a
grade less than a B or earn NCr (No Credit) in a clinical course must remediate the course to continue in
the program.
Minimal competency, as outlined in the course syllabi for clinical courses, is required to achieve a
passing grade of A, B, or Cr. A grade of No Credit (NCr) is the equivalent of a U grade in clinical courses.
A grade of U or NCr denotes unacceptable performance and students must successfully remediate the
course to continue in the program.
Course Challenge Policy
a. Course challenge is defined as a student request for exemption from a specific Western University
course requirement due to prior equivalent coursework (see #3 below). Students who successfully
challenge a course are exempted from all requirements in the required Western University course and
do not receive Western University credit for the course. The transferable equivalent course will be
noted on the student’s Western University transcript. A maximum of seven (7) credit units may be
transferred in from another academic institution for course challenge credit.
b. Students may request a partial course challenge as well. In this case, the appropriate Western
University faculty member will determine what elements must be completed by the student to fulfill a
specific course’s requirements including:
1. seminar attendance
2. written papers
3. class presentations
4. examinations
Students will receive Western University credit and a letter grade for partially challenged courses.
Students also pay full Western University tuition and fees for partially challenged courses since
Western University credit is given.
c. A student may request to challenge a course if either of the following situations exist:
1. he/she can demonstrate that an equivalent, transferable, graduate course was taken at
another regionally accredited academic institution, within the past five years, with a
minimum grade of B earned in that course. Equivalent course is defined as a course that
covers a significant portion of the Western University course content (to be determined by
the Western University course instructor) and has a course unit value equal to or exceeding
that of the Western University course.
2. he/she can demonstrate that an equivalent continuing education (CE) course was taken
within the past five years, and the student can document content mastery was achieved at an
80% level or higher. Equivalent course is defined as a course that covers a significant portion
of the Western University course content (to be determined by the Western University course
instructor) and that the awarded continuing education hours equals or exceeds that of the
hours represented by the unit value of the corresponding Western University course.
d. The following courses in the College of Graduate Nursing curriculum may be challenged by
students:
1. CGN 5015 – Clinical Reasoning
2. CGN 5101 – Health Systems I
160
3. CGN 5102 – Health Systems II
4. CGN 5111 – Advanced Studies in Health Systems
5. CGN 5200 – Nursing Theory
6. CGN 5301 – Nursing Research I
7. CGN 5302 – Nursing Research II
8. CGN 5401 – Primary Care Management I
9. CGN 5402 – Primary Care Management II
10. CGN 5403 – Primary Care Management III
11. CGN 5501 – Pharmacology I
12. CGN 5502 – Pharmacology II
13. CGN 5550 – Advanced Pharmacology
14. CGN 5601 – Advanced Physical Assessment
15. CGN 5602 – Health Promotion Over the Life Span
16. CGN 5603 – Current Social Issues Affecting Family Health
17. CGN 5604 – Advanced Therapeutic Skills
18. CGN 5605 – Cultural Diversity
19. CGN 5606 – Complementary Medicine
20. CGN 5607 – Professional Issues
21. CGN 5611 – Advanced Studies in Social Systems
22. CGN 5850 – Advanced Role
e. The following courses in the College of Graduate Nursing curriculum may NOT
be challenged by
students:
1. CGN 5000 – Communication and Information Management
2. CGN 5608 – Advanced Applications in Family Nurse Practice
3. CGN 5801 – Collaborative Project I
4. CGN 5802 – Collaborative Project II
5. CGN 5950 – Certification Review
6. CGN 5990 – Culminating Project
7. CGN 7570 – Clinical Experience
f. Procedure for Challenging a Course: Any student who wishes to challenge a course must:
1. submit in writing, to the Academic Coordinator of the CGN, his/her intent to challenge a
course at least
three weeks prior to registration for the academic semester in which the course
would normally be taken, and
2. submit written documentation including course description, course outlines, transcripts,
CE certificate, etc. to demonstrate course equivalency, to the Academic Coordinator of the
CGN at least
three weeks prior to registration for the academic semester in which the course
would normally be taken.
Upon receipt of the student’s intent to challenge and the written documentation of course
equivalency, the Academic Coordinator of the CGN will submit the written documentation to the
faculty member teaching the Western University course that is being challenged for review and
consideration of challenge approval. The faculty member will review said documentation and
issue a recommendation to allow or deny the challenge to the Academic Coordinator of the CGN
at least 10 days
prior to the date of registration for the academic semester in which the course
would normally be taken. This faculty recommendation will be forwarded to the student within
48 hours of its receipt by the Academic Coordinator.
g. Appealing Course Challenge Decisions: Students have a right to appeal the faculty member’s
recommendation to deny a course challenge. Such appeals will be forwarded to the Dean of the
CGN who has final authority in the challenge determination. The Registrar will be informed of
the final determination of the course challenge request.
Student Academic Progress Committee
The Student Academic Progress Committee is composed of the Academic Coordinator who shall serve
as chair, and three other faculty members serving for a two year term. The chair of the committee will be
responsible for communicating all decisions of the committee to the student and the dean.
The SAP Committee shall periodically review the academic progress of all students. Based on the
161
standards for academic progression, the committee shall recommend any of these courses of action for a
student: promotion, probation, suspension from the program, dismissal from the program, psychological
and/or educational assessment.
The SAP Committee has the responsibility of recommending to the College the MSN degree and/or
FNP certificate to all students who satisfactorily complete the requirements of the various programs.
The SAP Committee shall hear all appeals of grades, requirements for remediation, and other academic
disputes and make a recommendation to the dean for the outcome of the appeal.
The SAP Committee will review and approve all remediation contracts developed by the faculty of
record.
Evaluation and Grading
Competency-based learning is the underlying principle for the instructional design of the program and
the evaluation of student achievement. Each course has specific learning objectives, evaluative criteria and
expected outcomes. Assessment methods are stated clearly in each syllabus.
The cumulative letter grade of “B” or better must be attained for each course to indicate competency
for this graduate program. The grade for each evaluative component for courses 5015, 5401-3, 5550,
5501-2, 5601-8, 5950, and 7570 must be at least a “B” or 80% to demonstrate an acceptable level of
performance and enable the student to progress in the curriculum. The grade for each evaluative
component for courses 5000, 5101-2, 5111, 5200, 5301-2, 5611, 5801-2, 5850, and 5990 must be at least
70% with a cumulative letter grade of “B” or better to demonstrate an acceptable level of performance and
enable the student to progress in the curriculum. Evaluative criteria for each course are included in the
course syllabus. Students have the opportunity to remediate one learning component within a course to
meet the cumulative letter grade requirement.
Grade point average is based on the following numerical values for letter grade:
A = 4.0 Achievement of an “A” for a course exceeds the acceptable level of
performance in a graduate level program.
B = 3.0 Achievement of an “B” for a course meets the acceptable level of
performance in a graduate level program.
U = 0 Achievement of an “U” denotes an unacceptable performance.
Students who do not meet the remediation standards for an Incomplete
will be given the grade of “U”. Students who receive a “U” for any
course will be unable to progress in the curriculum without a formal
review by the Student Academic Progress Committee. If the
Committee finds that the student demonstrates the potential for
remediation, then the student will be placed on Academic Probation
with a formal signed progression contract. A signed copy of this
contract will be filed with the Dean. Probation is defined as a period of
time specified by the Dean, Chair of the SAP Committee and the
faculty of record for the course(s). If a student does not comply with
the remediation contract, the student will be dismissed from the
College.
Credit/No Credit: CGN 7570 (Primary Care Clinical) is graded as credit/no-credit and is not included
in the numerical values for computing grade point averages.
Credit (Cr) = Achievement of the grade “Credit” signifies that a student meets the
acceptable level of performance in a graduate level program.
No Credit (NCr)= Achievement of the grade “No Credit” indicates an unacceptable level
of performance in a graduate level program. A grade of “No Credit” is
the equivalent of an “U” grade.
I = Achievement of an "I" denotes an incomplete, which signifies that a
portion of the required coursework has not been completed and
evaluated. Students must submit a plan for completion that meets
approval by the faculty of record. Students who receive two
162
incompletes in one semester will be placed on academic probation.
Students who are enrolled in sequential theory courses will not be able
to progress in the curriculum unless the course is completed
successfully prior to the next semester or instructor approval is given.
The grade of “incomplete” will be recorded on the official transcript
until completion of course work is completed. If the student does not
complete the contractual agreement satisfactorily, a grade of “U” will
be given with recommendation for dismissal from the College of
Graduate Nursing.
IP = Students who do not complete 90 hours of clinical (2 units) within a
semester or 45 hours of clinical (1 unit) in the first semester will be
assigned a grade of “In Progress”. A grade of “IP” is replaced with a
grade of “Cr” when the necessary number of hours is achieved.
Students must complete outstanding clinical hours and an additional
90 hours minimum in the following semester to progress in their
clinical experience. Students who fail to meet the 90 hours minimum
for two consecutive semesters will be placed on Academic Probation
and are at risk for dismissal.
Remediation
Because CGN programs are sequential and presume successful completion of all courses in sequence, a
student who does not achieve a grade of A or B in a theory course or a grade of A, B, or Credit in a clinical
course must participate in remediation in order to continue in the program. The College will provide each
student with ample opportunity to demonstrate competency, however, remediation is a privilege, not a
right. Students must have demonstrated the likelihood of success in the remediation process by active
participation in the educational program including course attendance and participation, active involvement
in clinical experiences, individual initiative, and use of resources.
Students receiving grades of U or NCr for a course will be assigned a remediation contract by the
faculty member of record for the course in which the unacceptable grade was received. The contract will
be developed by the faculty member in consultation with the Student Academic Progress Committee. The
student may participate in developing the contract, however the faculty member will determine the actual
requirements for remediation.
Options for remediation include:
a. Successfully taking a comprehensive examination on the course content.
b. Successfully completing special projects or studies in the area(s) of deficiency.
c. Successfully repeating the course.
d. Successfully repeating a specific learning objective.
The remediation contract will outline the activities required for remediation, the outcomes expected for
successful completion, and a date for completion. Copies of the remediation contract, signed by the faculty
member and the student, will be filed with the CGN.
Upon completion of the remediation contract, the instructor will submit a recommendation to the
Student Academic Progress (SAP) Committee and the Dean. A grade of B is the highest possible grade
that can be achieved through remediation.
Grade Appeal Process
A student who believes that a grade for a course does not accurately reflect his/her performance in that
course should first submit a written request for a grade appeal to the faculty member of record. The written
request must specify the specific learning activities to be reconsidered, with the original submissions and
supporting documentation. The faculty member of record will either revise the grade or will retain it as
originally assigned. If the grade remains unchanged, the student may appeal to the SAP Committee. The
SAP Committee will review the course curriculum, learning objectives, evaluative criteria, and expected
outcomes. The SAP Committee will make a recommendation to the Dean to either revise the grade or
retain it as originally assigned.
163
Should the student disagree with the SAP Committee’s recommendation, s/he may appeal to the Dean.
The Dean will review the course curriculum, learning objectives, evaluative criteria, and expected
outcomes. The Dean will make the final decision regarding the disposition of the grade appeal.
Students whose grade remains as a “U” will be referred back to the SAP Committee and placed on
Academic Probation. Guidelines for academic progression will be followed according to the policies and
procedures stated in this Catalog. Every effort will be made to expedite the grade appeal process.
Administrative Fee for Additional Term
Students who do not complete coursework or clinical hours during the final semester will be charged an
additional administrative fee for making up coursework or clinical hours after the semester. This option is
only available with the approval of the Academic Coordinator and the Dean.
Leave of Absence/Withdrawal
Students who find that they are unable to continue in the program due to personal or medical reasons
may apply for a Leave of Absence. The Request for a Leave of Absence must be submitted in writing and
approved by the Dean on the recommendation of the Student Academic Progress Committee. The student
will need to obtain the endorsement of at least one instructor on the Leave of Absence form that the student
has the potential for program completion. Leaves may be granted for the balance of an academic year and
may be extended if the student seeks approval from the Dean at least one month prior to the start of the
subsequent academic year.
Probation/Dismissal
A request for Student Probation or Dismissal may be initiated by an individual faculty member, the
Student Academic Progress Committee, or the Dean, and submitted to the Chief Academic Officer. The
grounds for such an action may be based on academic, character or professional issues. The basis for
making the decision will be the University policy for student conduct as outlined in the 2002-2003
Catalog.
Seminar Weekend Attendance
Two campus-based seminar weekends are held each semester (after completing orientation sessions).
The first seminar weekend usually occurs during week 5, and the second seminar weekend usually occurs
during week 10 of the semester. Seminar weekends begin at 8 a.m. on Friday and conclude by 3 p.m. on
Sunday.
Dates of the weekend seminars are published and distributed at the beginning of each semester.
Attendance is mandatory for all seminars. Students who do not comply with this policy must make an
appointment with the Academic Coordinator immediately to avoid termination of their enrollment for the
semester in question. Based on the recommendation from the SAP Committee, the Dean will make a
determination about a student’s continued enrollment. A student’s right to appeal this decision is
described in the General Academic Policies and Procedures section of this Catalog.
Clinical Training
Clinical training begins after the student has: (1) completed the Advanced Physical Assessment course,
(2) successfully completed the Advanced Physical Assessment competency based physical assessment
testing, and (3) complied with the documentation of all the University’ health, safety and immunization
requirements.
Preceptors: Students are encouraged to identify a qualified preceptor in their community prior to
starting the program. A student’s primary preceptor may be a physician trained in family practice or
internal medicine, preferably board certified, or a master’s degree prepared, certified FNP working in
primary care. The College encourages multiple rotations for specific experience if needed to optimize
student learning. A student’s primary preceptor and/or clinical instructor may suggest or assist with
identifying and scheduling these rotations. If the preceptor is a physician, the student should also work
with a nurse practitioner to promote role development.
Preceptors working within specific guidelines established by the program will be responsible for
assuring appropriate and adequate learning experiences, as well as supervising students for safe practice.
164
Preceptors and clinical sites must be approved by the Western University faculty. A Preceptor Guide will
be provided to all preceptors.
As expected with professional practice, all data gathered about a patient and his/her health/illness,
including all items within the medical record, are privileged information. Client confidentiality must be
maintained.
Students must consult with their preceptors on all patients seen by the student. The supervising
practitioner must review and countersign all student notes written in the medical record. Students are not
allowed to prescribe medications or sign any prescription order.
Students are required to wear student identification and lab coats at all times while in the clinical
setting. Western University maintains malpractice and accident insurance coverage for enrolled students.
Professional nursing malpractice insurance (in the student role) is recommended but not required.
Scheduling: While the College encourages students to schedule the same clinical day(s) each week to
provide consistency for the agency and patient follow-up, scheduled days may be individualized to
accommodate illness, employment, or family responsibilities.
Clinical Hours: Eight-to-16 hours per week of clinical training are required of full-time students
throughout the two academic years to complete 675 hours. Following successful completion of the
Physical Assessment course, full-time students are expected to complete 1-5 units of clinical training each
semester. Forty-five hours must be completed for each unit, for a total of 15 units. A student, by special
arrangement with a faculty advisor, may complete a minimum of 90 clinical hours per semester (2 units)
and complete the remaining hours in subsequent semesters or at the end of the program. This arrangement
would require a student to enroll for another semester(s) to complete required clinical hours. An
administrative fee will be charged for the additional semester(s).
Clinical Progression: Student productivity is expected to increase with each semester's experience.
Initially, students may see approximately 4-6 patients per day. The student is expected to gather complete
subjective and objective data on each patient, even though early in the program the student may not be able
to fully assess the problem or develop a complete treatment plan. Later in the program, students will be
expected to see approximately 4-8 patients per day and provide comprehensive care including assessment
and plan of treatment. Students will be guided to transition from novice to advanced beginner as they
progress in the clinical practicum.
It is recommended that MSN/FNP and FNP-only students see approximately 810 patients during their
program. The goal for patient mix is: Pediatrics 15%, Adults 40%, Geriatrics 20%, GYN 15%, OB 10%.
Students are encouraged to obtain other rotations to complete clinical objectives if they are not in a
family practice setting. In addition, students are advised to find Urgent Care and Emergency Room
rotations for a semester. The clinical faculty of record will review students’ clinical e-logs each semester.
Students are required to submit clinical e-logs periodically throughout the semester. In addition, Preceptor
Evaluations are documented periodically.
Record Keeping and Clinical e-Logs: Clinical e-Logs for the College of Graduate Nursing are
provided to the student. Students will record each patient visit into the Clinical e-Log. Students may print
the e-Logs to use for manual recording in clinic, but must enter the data into the Clinical e-Logs before
submitting to the College. Students will receive an orientation to e-Log use. E-Logs will be submitted via
e-mail attachment biweekly, upon request, and at the end of each semester. In addition, students are
required to submit other documentation (i.e. Preceptor Evaluation, Student Evaluation of the Preceptor,
Student Objectives) at the end of the semester. Failure to do so may result in an incomplete grade and/or
failure to progress in the curriculum.
Students will maintain a calendar of hours, which is included in their evaluation of short-term goals and
initialed/verified by the preceptor.
Clinical Site Visits: Faculty visits to the clinical site are a major key to the success of this program.
Student clinical competency will be evaluated at this time by direct observation of the student's
performance and interaction with patients, preceptors, and staff. In addition, the clinical faculty provides
guidance and support as well as assistance with clinical decision making. Chart documentation of patient
care is also reviewed and assessed. Students who receive an unsatisfactory site visit evaluation must
complete a remediation process. Note: Students who live a great distance from the campus may be
required to perform clinical competency evaluation, as needed, at a Western University faculty member’s
clinic setting or at a Western University clinical training site. Efforts will be made to have these
evaluations coincide with seminar weekends to minimize travel costs.
165
COURSE DESCRIPTIONS
CGN 5000 Communication and Information Management in the MSN/FNP Program (1 unit)
This course provides new students with a comprehensive introduction to Western University's Nursing
Programs. In addition to learning about Western University of Health Sciences, students will discover in
more detail what will be expected of them as MSN/FNP students, and what they can expect from Western
University's faculty and staff. Following an overview of the most important services, policies, instructional
methods and resources, students will have an opportunity to assess your own readiness for the program and
an ability to succeed as a self-directed learner. Students will also be oriented to the technological skills
needed to complete their program. The awareness, knowledge and skills derived from this part of the
course will help ensure successful completion of the program.
CGN 5015 Clinical Reasoning (1 unit)
This course is designed for advanced nurse practitioner students to refine their history and physical
examination skills for the clinical setting. Its purpose is to take the students to the “next step” of health
assessment – beyond the basic history and physical examination to using a diagnostic reasoning process.
By integrating knowledge gained from this course with that learned in concurrent and subsequent courses,
students will continue to refine their ability to diagnose common problems. Students will also learn how to
evaluate and use assessment information with patients across the lifespan and with patients who present
with sensitive issues. This systematic approach to clinical problem-solving will provide the undergirding
structure to guide students as they tackle increasingly complex patient management problems.
CGN 5101 Health Systems I (2 units)
This course provides an overview of the American health care system with special emphasis given to
the emergence of managed care and its subsequent impact on health care planning, delivery and evaluation.
The various institutions and workforce segments that currently make up the American health care system
are introduced and compared with those of other industrialized countries. The course includes an overview
of health care economics, with particular attention given to the impact of health insurance (private and
government funded) on health care spending in this country. Managed care is presented as a major
emerging force in health care decision making and delivery. The impact of managed care reforms on the
Family Nurse Practitioner role is emphasized.
CGN 5102 Health Systems II (2 units)
The second part of Health Systems introduces the need for and tools currently available to measure the
quality of health care in this country. Special emphasis is given to identifying and measuring nursing-
sensitive patient outcomes and how they are related to treatment options and resource use. The course also
introduces case management and disease management as strategies for achieving desired patient outcomes
through the coordination of care. Students will learn about the multitude of means by which quality of
health care is currently assessed and measured in this country, including research based quality initiatives
such as standardized clinical practice guidelines, benchmarking, and report cards.
CGN 5111 Advanced Studies in Health Systems (2 units)
This two-unit course for FNP-only and MSN-only students provides an overview of the American health
care system in regards to health finance and the quest for quality care. Special emphasis is given to the
emergence of managed care and its subsequent impact on contemporary health care planning, delivery and
evaluation. In addition, the course introduces the need for and tools currently available to measure the
quality of health care in this country. Case management and disease management are emphasized as
strategies for achieving cost effective, high quality care. Pre-requisite: Admission to FNP only or MSN
only programs.
CGN 5200 Nursing Theory (3 units)
This course explores the theoretical context of contemporary nursing practice that serves to guide
nursing practice and primary health care. In addition, this course will integrate knowledge from the
physical, biological and behavioral sciences to systematically and critically apply selected conceptual
frameworks to the study of nursing, family systems and the response to illness. Through this experience,
166
the graduate nursing student will develop an appreciation for the process of theory development in nursing,
compare and contrast various theoretical perspectives used in nursing practice, and apply these nursing
theories critically.
CGN 5301 Nursing Research I (2 units)
Nursing Research I is designed to lay the foundation for understanding the research process and its
importance in advancing nursing practice. The course emphasizes research critique and application to
advanced practice nursing. Evaluation of quantitative and qualitative research literature, literature review
skills, and decision-making related to clinical significance are explored.
CGN 5302 Nursing Research II (2 units)
Nursing Research II focuses on the design and implementation of a research study. Review of research
methodology, research process, rights of subjects, grant writing and dissemination of findings are explored
in this course.
CGN 5401 Primary Care Management I (2 units)
Primary Care Management I integrates the basic knowledge of human anatomy and physiology with an
understanding of the pathologic changes and clinical manifestations that characterize common and acute
disorders in adult, obstetric, pediatric, and elderly clients. This new understanding of pathophysiology and
the student’s evolving clinical decision-making skills is applied to the interpretation of assessment data and
the diagnosis and treatment of primary care clients and their families across the life cycle.
CGN 5402 Primary Care Management II (2 units)
Primary Care Management II continues to help students integrate their basic knowledge of human
anatomy and physiology with an understanding of the pathological changes and clinical manifestations that
characterize common, chronic, and complex disorders in pediatric, adult, obstetric, and elderly clients.
Students will apply their new understanding of pathophysiology and their evolving clinical decision-
making skills to the interpretation of assessment data and the diagnosis and treatment of primary care
clients and their families across the life cycle.
CGN 5403 Primary Care Management III (2 units)
Primary Care Management III enhances the student’s ability to integrate a basic knowledge of human
anatomy and physiology with an understanding of the pathologic changes and clinical manifestations that
characterize common, acute, chronic, and complex disorders in pediatric, obstetric, and geriatric clients.
Students will apply their understanding of pathophysiology and their evolving clinical decision-making
skills to the interpretation of assessment data and the diagnosis and treatment of primary care clients and
their families across the life cycle within the special populations of pediatrics, obstetrics and geriatrics.
CGN 5501 Pharmacology I (2 units)
Pharmacology I provides the means for learning the necessary pharmaceutical principles and practices
to enable students to prescribe and monitor the effects of medications on the health and well being of
clients with common, acute, or infectious health problems. The course will address the effects of these
problems and related pharmacotherapy on patients from the various stages of the life cycle, i.e., pediatrics,
adult/family, obstetrics and geriatrics.
CGN 5502 Pharmacology II (2 units)
Pharmacology II provides the means for learning the necessary pharmaceutical principles and practices
to enable students to prescribe and monitor the effects of medications on the health and well being of
clients with chronic and complex health problems. The course will address the effects of these problems
and related pharmacotherapy on patients from the various stages of the life cycle, i.e., pediatrics,
adult/family, obstetrics and geriatrics.
167
CGN 5550 Advanced Pharmacology (3 units)
This course is designed to provide advanced practice nurses enrolled in the MSN-only and APN-to-
FNP track students with an accelerated review of current pharmacotherapeutic concepts. The course will
prepare students to prescribe and monitor the effects of medication on the health and well being of
patients. The course qualifies the master’s-prepared FNP to receive a Furnishing Number in the State of
California. Note: Not required for students with a furnishing number or who have completed an equivalent
pharmacology course within five years.
CGN 5601 Advanced Physical Assessment (2 units)
This FNP Role Development course introduces skills that build on undergraduate education and
experience with respect to basic physical assessment. These advanced skills, which draw on knowledge
from nursing, medicine, and other disciplines, include more sophisticated assessment techniques,
recognition and interpretation of clinical assessment data, diagnostic and therapeutic decision-making, and
medical record keeping. Over the course of the program, students will be expected to integrate these skills
with knowledge of common, acute, chronic, and complex illnesses in order to assess and manage patients
across the life cycle.
CGN 5602 Health Promotion Over the Life Span (1 unit)
This FNP Role Development course is designed to encourage the Family Nurse Practitioner student to
apply preventive health concepts and health promotion strategies across the life span, using the U.S. Public
Health Service guidelines as a resource. Students will learn how to apply health promotion lifestyle
changes in the primary care patient population. Concepts such as health screening and
immunization/prophylaxis in pediatric and adult clients will be examined. Methods of counseling clients
in lifestyle behaviors such as nutrition, physical activity, smoking cessation, and violence prevention will
also be explored.
CGN 5603 Current Social Issues Affecting Family Health (1 unit)
This FNP Role Development course focuses on the social issues that often arise when providing
primary health care to clients over the life span. The interdependence of these social and clinical issues
mandate that the health care provider become aware of the relevant legal, ethical, and medical implications
of child abuse, domestic violence, substance abuse, adolescent pregnancy, and poverty; as well as
geriatrics issues related to functional independence, polypharmacy, dementia, depression, and elder
homelessness.
CGN 5604 Advanced Therapeutic Skills (1 unit)
In this FNP Role Development course, students will learn diagnostic and therapeutic procedures and
skills critical to advanced practice nursing. These procedures and skills include microscopy, Norplant and
IUD insertion and removal, endometrial biopsy, x-ray interpretation, colposcopy and cryotherapy,
suturing, office orthopedic appliances and treatment techniques, and cardiovascular monitoring.
CGN 5605 Cultural Diversity (1 unit)
This FNP Role Development course explores the impact of patients’ cultural beliefs and values on
medical practice and the health care provider. The course emphasizes the importance of cultural
sensitivity and cultural competency in delivering high quality care. Culturally determined folk beliefs and
health traditions are examined in the context of community health and family health care.
CGN 5606 Complementary Medicine (1 unit)
This FNP Role Development course focuses on the scientific basis for practices of alternative or
complementary therapy utilized by health care consumers in this country. Among the complementary
therapies students will consider are acupuncture, yoga, biofeedback, chiropractic, dietary supplements,
exercise, herbs, homeopathy, hypnosis, imagery, massage, relaxation, meditation, spiritual healing and
energy work.
168
CGN 5607 Professional Issues (1 unit)
This FNP Role Development course presents a variety of role-related topics designed to prepare the
prospective Nurse Practitioner for professional practice. Beginning with a historical overview of the NP
profession, the course will take students on a guided tour of some of the critical issues that determine the
practitioner’s scope of practice, career options, and political involvement. In addition, the course presents
guidelines for resolving legal and ethical issues that are often confronted by the NP. Finally, students will
be introduced to some valuable tools for ongoing professional development such as professional
organizations and journals.
CGN 5608 Advanced Applications in Family Nurse Practice (1 unit)
This culminating FNP Role Development course provides an opportunity for students to synthesize
concepts, skills and techniques from previous courses and apply their learning toward assessing and
managing advanced case studies across the life span.
CGN 5611 Advanced Studies in Social Systems (2 units)
This course is designed for nurse practitioners enrolled in the APN to FNP track. This course focuses
on the diverse array of social issues and systems that the Nurse Practitioner must negotiate. The areas of
focus in this course are: health care ethics; social issues such as management of domestic violence and
substance abuse; cultural diversity skills; complementary and alternative therapeutics; and health
promotion and disease prevention concepts across the lifespan.
CGN 5801 Collaborative Project I (0.5 unit)
Collaborative Projects are based on a problem or a project that requires a collective solution. Each
Collaborative Project provides the opportunity for small groups of students to work together in a learning
experience that integrates their current coursework, encourages the application of new concepts, and
stimulates the kind of thinking and interaction that are relevant to students’ ongoing advanced practice role
development.
CGN 5802 Collaborative Project II (0.5 unit)
As with Collaborative Project I, the second Collaborative Project is based on a problem or a project
that requires a collective solution. The Collaborative Project provides the opportunity for small groups of
students to work together in a learning experience that integrates current coursework, encourages the
application of new concepts, and stimulates the kind of thinking and interaction that are relevant to
students’ ongoing advanced practice role development.
CGN 5850 Advanced Role (3 units)
This is a culminating course than examines transitional roles for the advanced practice nurse (APN), with
focus on understanding and applying leadership and other related theories, exploring diverse leadership
roles and associated issues, and development of knowledge and skills needed for leadership roles. An
overall goal of the course is to expand the student’s understanding of the broad scope of responsibilities of
APNs through the assumption of leadership roles within the profession.
CGN 5950 Certification Review (1 unit)
This course is required to be completed prior to graduation for all students enrolled in the MSN/FNP
and FNP-only programs. This comprehensive testing review will further assist the MSN/FNP and FNP-
only student to prepare for the national certifying examination to become an Advanced Practice Nurse.
Testing and review modules are systems-based. Following a pre-assessment examination (self-evaluation),
students will have access to a detailed modular review program during the Clinical Experience (CGN
7570) course. Students are required to achieve a score of 80% or higher on the final examination.
Students may repeat the final examination one time if they do not achieve a score of 80% or higher.
CGN 5990 Culminating Project (1 unit)
The Culminating Project is an independent study project that serves as a culminating experience for the
FNP program. The project requires the student to develop a clinical improvement initiative that will offer
169
valuable insights into high-risk patient populations and the kinds of contributions FNPs can make in
providing care for these populations.
CGN 7570 Clinical Experience (1-5 Units per Semester; Repeatable to a total of 15 units; Cr/NCr)
The Clinical Experience course offers FNP, ANP-FNP, and MSN/FNP students the opportunity to
begin providing comprehensive health care to individuals and families within a culturally diverse
environment in collaboration with physicians, nurse practitioners and other health care professionals.
Students are expected to draw on their preceptored experiences to develop sound clinical judgment applied
to health promotion, health maintenance, and diagnosis and management of common, acute, chronic and
complex health problems for individuals across the life cycle.
170
CURRICULUM
MSN/FNP Program
Prerequisites: Statistics and Pathophysiology
YEAR 1
YEAR 2
Pre-
Communications (CGN 5000)
1
Program
Physical Assess (CGN 5601)
2
Total Units
3
TERM 1
TERM 4
Clinical Reasoning (CGN 5015)
1
Nursing Theory (CGN 5200)
3
Health Systems I (CGN 5101)
2
Nursing Research I (CGN 5301)
2
PC Management I (CGN 5401)
2
Cultural Diversity (CGN (5605)
1
Health Promotion (CGN 5602)
1
Collab Project I (CGN 5801)
.5
Clinical Exp (CGN 7570)* 1
Clinical Exp (CGN 7570)*
3
Total Units 7
9.5
TERM 2
TERM 5
PC Management II (CGN 5402)
2
Health Systems II (CGN 5102)
2
Pharm I (CGN 5501)
2
Nursing Research II (CGN 5302)
2
Social Issues (CGN 5603)
1
Collab Project II (CGN 5802)
.5
Adv. Therap. Skills (CGN 5604)
1
Clinical Exp (CGN 7570)*
3
Clinical Exp (CGN 7570)*
2
Total Units
8
7.5
TERM 3
TERM 6
PC Management III (CGN 5403)
2
Professional Issues (CGN 5607)
1
Pharm II (CGN 5502) 2
Adv. Apps. (CGN 5608)
1
Complementary Med (CGN 5606)
1
Cert. Rev. (CGN 5950)
1
Clinical Exp (CGN 7570)*
3
Culminating Project (CGN 5990)
1
Clinical Exp (CGN 7570)*
3
Total Units
8
7
Year 1 Total Units
26
Year 2 Total Units
24
Total Program Units
50
* Additional semesters can be taken to complete clinical hours. Students are expected to complete a minimum of 90 hours (2
units) per semester to progress in the curriculum.
171
CURRICULUM
FNP-Only Track MSN-Only Track
Prerequisites: Statistics and Pathophysiology Prerequisites: Statistics and Pathophysiology
YEAR 1
YEAR 1
Pre-
Communications (CGN 5000)
1
Pre-
Communications (CGN 5000)
1
Program
Physical Assess (CGN 5601)
2
Program
Phys Assess (elect) (CGN 5601)
(2)
Total Units 3
Total Units 1
(3)
TERM 1
TERM 1
Clinical Reasoning (CGN 5015)
1
Adv. Study Hlth Sys (CGN 5111)
2
Adv. Study Hlth Sys (CGN 5111)
2
Nursing Theory (CGN 5200)
3
PC Management I (CGN 5401)
2
Nursing Research I (CGN 5301)
2
Clinical Exp (CGN 7570)*
5
Collab. Project I (CGN 5801)
.5
Total Units 12
Total Units 7.5
TERM 2
TERM 2
PC Management II (CGN 5402)
2
Research II (CGN 5302)
2
Pharm I (CGN 5501)
2
Skills (elective) (CGN 5604)
(1)
Adv. Therap. Skills (CGN 5604)
1
Adv. Social Syst. (CGN 5611)
2
Adv. Social Syst. (CGN 5611)
2
Collab Project II (CGN 5802)
.5
Clinical Exp (CGN 7570)*
5
Total Units
12
Total Units
4.5
(5.5)
TERM 3
TERM 3
PC Management III (CGN 5403)
2
Pharm II (CGN 5502)
2
Advanced Pharm. (CGN 5550)**
3
Prof Issues (CGN 5607)
1
Prof. Issues (CGN (5607)
1
Adv. Apps. (CGN 5608)
1
Advanced Role (CGN 5850)
3
Cert. Rev. (CGN 5950)
1
Culminating Project (CGN 5990)
1
Clinical Exp (CGN 7570)*
5
Total Units
12
Total Units
8
Total Program Units
37
Total Program Units
21
(24)
* Additional semesters can be taken to complete clinical hours. Students are expected to complete a minimum of 90 hours (2 units) per
semester to progress in the curriculum.
** Not required for students with a furnishing number or who have completed an equivalent pharmacology course within five years.
172
CURRICULUM
APN to FNP Track MSN-Harbor/UCLA Track
Prerequisites: Statistics and Pathophysiology Prerequisites: Statistics and Pathophysiology
YEAR 1
YEAR 1
Pre-
Communications (CGN 5000)
1
Pre-
Communications (CGN 5000)
1
Program
Physical Assess (CGN 5601)
2
Program
Total Units 3
Total Units 1
TERM 1
TERM 1
PC Management I (CGN 5401)
2
Health Systems I (CGN 5101)
2
Clinical Exp (CGN 7570)
2
Nursing Theory (CGN 5200)
3
Total Units 4
Nursing Research I (CGN 5301)
2
Collab. Project I (CGN 5801)
.5
Total Units 7.5
TERM 2
TERM 2
PC Management II (CGN 5402)
2
Health Systems II (CGN 5102)
2
Adv. Social Syst. (CGN 5611)
2
Research II (CGN 5302)
2
Clinical Exp (CGN 7570)
2
Collab Project II (CGN 5802)
.5
Total Units
6
Total Units
4.5
TERM 3
TERM 3
Adv. Pharm. (CGN 5550)
3
Advanced Role (CGN 5850)
3
Prof Issues (CGN 5607)
1
Culminating Proj. (CGN 5990)
1
Adv. Apps. (CGN 5608)
1
Cert. Rev. (CGN 5950)
1
Total Units
6
Total Units
4
Total Program Units
19
Total Program Units
17
173
HONORS AND AWARDS
The following honors and awards are presented annually at the University's Honors Day ceremony in
April:
Academic Achievement Award
Spirit Award
CGN Leadership and Community Excellence Award
President's Society Award
Guy M. Allmon Scholarship Fund
Linda Fox Memorial Endowment Fund
Dean's Award
The following honors and awards are presented annually to graduates at the University's
Commencement Dinner:
FNP Primary Care Award
Class of 2000 Award
Academic Achievement Award
Class Service Award
University Graduate Award (Alumni)
Dean's Award
174
Academic Calendar
2002-2003
Semester Format (15 Week)
Thursday, Jun. 27-Monday, Jul. 1, 2002
First Preprogram Seminar (new students)
Thursday, Jul. 4, 2002
Independence Day - No classes
Friday, Jul. 5, 2002
Campus Offices Closed
Jul. 12-14, 2002
Seminar Weekend (continuing students)
Aug. 7-11, 2002
Second Preprogram Seminar (new students)
Friday, Aug. 9, 2002
Summer Semester Ends (continuing students)
Sunday, Aug. 18, 2002
Preprogram end (new students)
Monday, Aug. 19, 2002
Fall Semester Tuition Due
Monday, Sept. 2, 2002
Labor Day – No classes
Tuesday, Sept. 3, 2002
Fall Semester Begins
Sept. 27-29, 2002
Seminar Weekend
Monday, Oct. 14, 2002
Columbus Day – No classes
Nov. 1-3, 2002
Seminar Weekend
Wednesday, Nov. 27 (12:00 noon)-Sunday, Dec.
1, 2002
Thanksgiving Recess
Friday, Dec. 13, 2002
Fall Semester Ends
Monday, Jan. 6, 2003
Spring Semester Begins
Monday, Jan. 20, 2003
Martin Luther King, Jr. Day – No classes
Feb. 7-9, 2003
Seminar Weekend
Monday, Feb. 10, 2003
Spring Semester Tuition Due
Mar. 14-16, 2003
Seminar Weekend
Monday, Apr. 14, 2003
Honor’s Day
Friday, Apr. 18, 2003
Spring Semester Ends
Monday, May 5, 2003
Summer Semester Begins (continuing students)
Monday, May 26, 2003
Memorial Day – No classes
Jun. 2-6, 2003
Summer Semester Registration (new students)
Jun. 6-8, 2003
Seminar Weekend (continuing students)
TBA
Graduation
Monday, Jun. 16, 2003
Preprogram Begins (new students)
TBA
First Preprogram Seminar (new students)
Friday, Jul. 4, 2003
Independence Day – No classes
Jul. 11-13, 2003
Seminar Weekend (continuing students)
TBA
Second Preprogram Seminar (new students)
Friday, Aug. 15, 2003
Summer Semester Ends (continuing students)
Friday, Aug. 24, 2003
Preprogram Ends (new students)
175
BOARD OF TRUSTEES, ADMINISTRATION & FACULTY
WESTERN UNIVERSITY OF HEALTH SCIENCES
Board of Trustees
Warren Lawless, LHD (Hon.), Chairman
Wesley V. Boudette, DO, DEd (Hon.), FAOCR, Vice Chairman
John A. Forbing, Secretary
Ethan R. Allen, DO, DSc (Hon.), Treasurer
Philip Pumerantz, PhD, LHD (Hon.), President (ex officio)
Richard A. Bond, DO, FAAFP
Wen Chang, MBA
LaDonna Johnson, DO
Cassandra Malry, MBA
John T. McGwire, DDS
Sam Tanenbaum, PhD
Richard E. Eby, DO, FACOOG, DSc (Hon.), DEd (Hon.),
PhD (Hon.), Trustee Emeritus
Lawrence L. Leyba, DO, DEd (Hon.), Trustee Emeritus
UNIVERSITY AND ACADEMIC ADMINISTRATION
University Administration
President: Philip Pumerantz, PhD, LHD (Hon.)
Executive Vice President of Academic Affairs/Chief Academic
Officer: George Charney, DO, FAOCA, FAODME
Executive Vice President of Finance & Business: Christopher Oberg, PhD
Provost: Donald J. Krpan, DO, FACOFP
Senior Vice President, Policy and Research/Assistant to the
Executive Vice President of Academic Affairs: Gary M. Gugelchuk, PhD
Vice President, Strategic Planning and Institutional Effectiveness:
Suellen Crano, PhD
Vice President, University Advancement: Richard M. Nordin
Dean, Student Affairs: Beverly A. Guidry, EdD
Treasurer: Kevin D. Shaw
Registrar: Jeanne Hewson, MA
Assistant Vice President of University Advancement, Alumni and Constituent Relations:
Mari Penshurst-Gersten
Assistant Vice President of University Advancement, Major Gifts: Hart Roussel
Assistant Vice President of Advancement and Sponsored Programs:
Matthew D. Katz, MHA
Associate Treasurer, Finance: Joseph Ocampo
Assistant Treasurer, Fiscal Operations: Chris Crow
Director, Admissions (Allied Health, Pharmacy, Graduate Nursing):
Kathy Ford
Director, Admissions (Medicine): Susan D. Hanson
Director, Annual Giving: Laura Wensley
Director, Bookstore: Elizabeth V. Guerra
Director, Center for Academic and Professional Enhancement:
Thomas Levitan, MA
Director, Center for Disability Issues and the Health Professions:
Brenda Premo, MBA
Director, Communications: Jean Henshaw
Director, Curriculum Development, Center for Disability Issues and the
Health Professions: LeeAnne Carrothers, PhD, PT
176
Director, Financial Aid: Otto Reyer, MA
Director, Foundation Relations: Garth Clayton
Director, Health and Safety: Ron Redden
Director, Health Professions Library: Pat Vader, MS
Director, Human Resources: Sinclair Hugh, MPA, SPHA
Director, Instructional Technology & Distance Learning: Miary Andriamiarisoa
Director, Learning Enhancement & Academic Development:
David Hacker, MA
Director, Network Operations: Gary Priddy
Director, Publications: Rick Clapper
Director, Student Affairs: Toni Lawrence
Director, Events and Programs: Julie Wade
Director, University Recruitment/Strategic Enrollment
Management: Ann Ellis, MEd
Director, Willed Body Program: Niña McCoy
Alumni Dean Emerita: Janet M. Dyer
Gift Planning Specialist: James S. Williams, CFRE
Manager, Facilities: Larry Thomas
College of Osteopathic Medicine of the Pacific
Dean, College of Osteopathic Medicine: Craig J. Lenz, DO, FAODME
Associate Dean, Academic Affairs/Director of Clinical Education:
Ron Berezniak, PhD
Assistant Dean, Academic Affairs and Curriculum: Richard Winn, EdD
Chairperson, Department of Anatomy: Richard Sugerman, PhD
Chairperson, Department of Basic Medical Sciences: Robert Fiorindo, PhD
Chairperson, Department of Family Medicine: Alan D. Cundari, DO, MS
Chairperson (Acting), Department of Geriatrics: Ehab Tuppo, DO
Chairperson, Department of Internal Medicine: J. Michael Finley, DO
Chairperson, Department of Obstetrics/Gynecology: Lony C. Castro, MD
Chairperson, Department of Osteopathic Manipulative Medicine:
Raymond Hruby, DO
Chairperson, Department of Pediatrics: Frances Yang, DO
Chairperson, Department of Surgery: J. Vivian Davis III, DO
Director, Student Services: Gisele Tackoor, JD
Manager, Western University Medical Center: Joanna Varner
College of Allied Health Professions
Dean, College of Allied Health Professions: Stephanie D. Bowlin, EdD, PA-C
Chairperson, Department of Health Sciences:
Michael Burney, EdD, PA-C
Chairperson, Department of Physician Assistant Education:
Roy Guizado, MS, PA-C
Chairperson, Department of Physical Therapy Education:
Donna Redman-Bentley, PhD, PT
177
Director of Clinical Education, Department of Physical
Therapy Education: Georgeanne Vlad, MA, PT
Academic Coordinator of Clinical Education, Department of Physician
Assistant Education: Rebecca Maldonado, BS, PA-C
Coordinator, Clinical Education, Department of Physician
Assistant Education: Jane Riplog
College of Pharmacy
Dean, College of Pharmacy: Max D. Ray, PharmD, MS
Associate Dean, Academic Affairs: Wallace Murray, PhD
Assistant Dean, Graduate Education and Research: TBN
Assistant Dean, Development: Sam K. Shimomura, PharmD
Director, Advanced Professional Practice Experience: Jack Chen, PharmD
Director, Center for Drug Development: William Garner
Director, Center of Pharmacy Practice Research & Development: Katherine K. Knapp, PhD
Director, Introductory Professional Practice Experience: Craig Hitchman, BPharm
Curriculum Development and Assessment Specialist: Nancy E. Kawahara, PharmD, MS
Director, Student Services: Mark Iannuzzo
College of Graduate Nursing
Dean, College of Graduate Nursing/Director, MSN/FNP Program:
Karen Hanford, MSN, FNP, PA-C
Academic Coordinator, MSN/FNP Program: Margaret J. Rowberg, MSN, ANP-C
Assistant Program Director: Sarah Douville
College of Veterinary Medicine
Dean, College of Veterinary Medicine: Shirley D. Johnston, PhD, DVM
178
FACULTY
Hugo Arias, Assistant Professor of Pharmaceutical Sciences (2002). Lic, PhD, Universidad Nacional del
Sur
Dayle Chakerian Armstrong, Assistant Professor of Physical Therapy Education (2000). AS, BS, Mount
St. Mary's College; MS, University of Southern California.
Mary K. Bailey, Assistant Professor of Physical Therapy Education, 1999. BS, California State University,
Long Beach; MS, California State University, Fullerton.
Gerald Bales, Associate Professor of Anatomy, 1996. BA, MA, Chico State University; PhD, University of
Southern California.
Ronald Berezniak, Associate Professor of Health Professions Education, 1999. BS, Bloomsburg State
College; MA, Glassboro State College; PhD, University of Pennsylvania.
Gurupadappa V. Betageri, Professor of Pharmaceutical Sciences, 1998. BS, Karnatak University; MS,
Bangalore University; PhD, University of Alberta.
Nancy Bjerke, Assistant Professor of Physical Therapy Education, 1997. BS, Loma Linda University;
MPT, Loma Linda University.
Stephanie D. Bowlin, Associate Professor of Physician Assistant Education, 1990. BS, California State
University, Dominguez Hills; MS, College of Osteopathic Medicine of the Pacific; PA-C, Charles R. Drew
University of Medicine and Science; EdD, University of La Verne.
Michael Burney, Assistant Professor of Physician Assistant Education, 1996. BS, University of Southern
California; PA, MS, College of Osteopathic Medicine of the Pacific; EdD, University of La Verne.
Rosslynn S. Byous, Assistant Professor of Physician Assistant Education, 1991. BA, University of
California, Santa Barbara; MS, University of LaVerne; PA, Charles Drew University of Medicine and
Science; DPA, University of LaVerne.
LeeAnne Carrothers, Adjunct Associate Professor of Physical Therapy Education, 1992. BS, University of
California, Davis; MS, PT, University of Southern California; PhD, California Graduate Institute.
Lony C. Castro, Associate Professor of Obstetrics and Gynecology, 2001. BA, University of California,
San Diego; MD, University of California, San Francisco.
Casey Chaney, Associate Professor of Physical Therapy Education, 1993. BS, MS, Russell Sage College;
PhD University of Utah, College of Health.
George Charney, Professor of Surgery/Anesthesiology, 1997. BA, Brooklyn College; DO, Philadelphia
College of Osteopathic Medicine.
Jack J. Chen, Assistant Professor of Pharmacy Practice, 2000. BA, University of California, San Diego;
BS, Massachusetts College of Pharmacy and Allied Health Sciences; PharmD, University of Utah.
Eunice P. Chung, Assistant Professor of Pharmacy Practice, 1999. BS, University of California, Berkeley;
PharmD, University of California, San Francisco.
Suellen Crano, Associate Professor of Health Professions Education, 1999. BA, MA, EdS, The George
Washington University; PhD, Michigan State University.
179
Alan D. Cundari, Professor of Family Medicine, 1987. AS, University of Albuquerque; MS, College of
Osteopathic Medicine of the Pacific; DO, College of Osteopathic Medicine of the Pacific.
J. Vivian Davis III, Associate Professor of Surgery,2000. BA, MA, University of Texas, Austin; DO,
Texas College of Osteopathic Medicine; MA, William Woods University.
Jeffrey Felton, Professor of Microbiology, 1993. BS, Massachusetts Institute of Technology; PhD, Tufts
University.
J. Michael Findley, Associate Professor of Internal Medicine, 2000. BS, Michigan State University; DO,
Chicago College of Osteopathic Medicine.
Robert P. Fiorindo, Professor of Physiology, 1980. BS, Albright College; MS, University of Maryland;
PhD, University of California, Berkeley.
Duane H. Foley, Professor of Physiology, 1984. BS, University of California, Davis; PhD, University of
California, Davis.
James Dana Foster, Associate Professor of Anatomy, 2000. BS, MS, Oakland University; PhD, Temple
University.
Viola M. Frymann, Professor of Family Medicine/Osteopathic Manipulative Medicine, 1978. MB, BS,
University of London; DO, College of Osteopathic Physicians and Surgeons, Los Angeles.
Spencer B. Gilbert, Professor of Pathology, 1995. MD, Chicago Medical School.
Robert A. Graf, Assistant Professor of Pharmaceutical Sciences, 1999. AB, University of California,
Berkeley; PhD, University of Hawaii.
Lee R. Grunden, Professor of Pharmacology (Emeritus), 1980. BS Oregon State University; PhD,
University of California, San Francisco Medical Center.
Vitalita Genove Grunden, Professor of Pathology (Emerita), 1980. AA, Sillman University; MD,
University of Santa Tomas.
Gary M. Gugelchuk, Associate Professor of Health Professions Education, 1986. BA, MA, PhD, The Ohio
State University.
Beverly Guidry, Instructor of Health Professions Education, 1997. BA, MS, EdD, University of LaVerne.
Roy A. Guizado, Assistant Professor of Physician Assistant Education, 1995. PA-C, College of
Osteopathic Medicine of the Pacific; MS, Western University of Health Sciences.
Karen J. Hanford, Associate Professor of Nursing, 1997. BSN, San Francisco State University; MSN,
California State University, Chico; FNP, PA, University of North Dakota.
Rick M. Hirsh, Assistant Professor of Family Medicine, 2000. AS, Fullerton College; BS, Loma Linda
University; DO; Western University of Health Sciences.
Raymond J. Hruby, Professor of Family Medicine/Osteopathic Manipulative Medicine, 1999. BA, St.
Vincent College; DO, College of Osteopathic Medicine and Surgery; MS, West Coast University.
Carol J. Huston, Adjunct Professor of Nursing, 1998. BS, University of Iowa; MSN, California State
University, Chico; MPA, DPA, University of Southern California.
180
Christine Jacobson, Instructor of Family Medicine, 2001. BA, California State University, Fullerton; MA,
California State University, Los Angeles.
Kevin Jenkins, Professor of Internal Medicine, 1981. BS, Capital University; DO, College of Osteopathic
Medicine & Surgery.
Gary R. Johnston, Professor of Veterinary Medicine, 1999. BA, University of Washington; DVM,
Washington State University; MS, University of Minnesota.
Shirley D. Johnston, Professor of Veterinary Medicine, 1998. BS, University of Washington; DVM,
Washington State University; MS, PhD, University of Minnesota.
H. James Jones, Assistant Professor of Osteopathic Manipulative Medicine, 1997. BS, California State
University, Long Beach; DO, College of Osteopathic Medicine of the Pacific.
Anita Kay Kalousek, Assistant Professor of Family Medicine, 2000. BA, Loma Linda University; DO,
MS, College of Osteopathic Medicine of the Pacific.
Sylvia Kamath, Professor of Anatomy, 1995. MS, Bangalore University; MBBS, Madras University.
Nancy Edman Kawahara, Assistant Professor of Pharmacy Practice, 2000. PharmD, MSEd, University of
Southern California.
Jerry Kellogg, Adjunct Assistant Professor of Nursing, 1998. BA, University of California, Riverside; MA,
California State University, Los Angeles.
Nadir Khan, Professor of Microbiology, 1978. BS, DJ, Government Science College; MS, University of
Karachi; PhD, University of Missouri.
Dennis M. Kiick, Associate Professor of Biochemistry, 1995. BS, San Diego State University; PhD,
University of North Texas.
Katherine K. Knapp, Professor of Social and Administrative Sciences, 2001. BA, MA, MS, University of
Michigan; PhD, University of California, Davis.
Donald J. Krpan, Professor of Family Medicine, 1987. BS, University of Nevada; DO, University of
Health Sciences, College of Osteopathic Medicine, Kansas City.
Craig S. Kuehn, Professor of Anatomy, 1985. BS, California State Polytechnic University, Pomona; PhD,
University of Southern California.
Maria Lambros, Assistant Professor of Pharmaceutical Science, 1999. BS, University of Athens; MS,
University of Cincinnati; PhD, University of Minnesota.
Anandi V. Law, Assistant Professor of Social and Administrative Sciences, 1999. BPharm, University of
Bombay; MS, PhD, The Ohio State University.
Jennifer Le, Assistant Professor of Pharmacy Practice, 2002. BS, University of California, Los Angeles;
PharmD, University of California, San Francisco.
Craig L. Lenz, Associate Professor of Family Medicine, 1999. BSE, Princeton University; MEd,
University of Pennsylvania; DO, Philadelphia College of Osteopathic Medicine.
Jonathan Leo, Associate Professor of Anatomy, 1995. BA, MacAlister College; PhD, University of Iowa.
181
Diane Lithgow, Professor of Nursing, 1997. BS, University of California, Irvine; BSN, MSN, California
State University, Long Beach.
Rebecca Maldonado, Instructor of Physician Assistant Education (2000). BS, California State University,
Long Beach; PA, College of Osteopathic Medicine of the Pacific.
James T. Martin, Professor of Physiology and Behavioral Science, 1986. BA, West Virginia University;
MS, University of Connecticut; Dr. re. Nat., University of Munich and Max Planck Institute, Seewiesen,
Germany.
James F. May, Professor of Anatomy, 1981. BS, California State College, Los Angeles; MS, Occidental
College; PhD, University of Southern California.
Miguel A. Medina, Instructor of Physician Assistant Education, 1992. AA, East Los Angeles Junior
College; PA-C, University of Southern California.
Kenneth Mengel, Instructor of Physical Therapy Education, 2000. BA, Whittier College; MPT, University
of Southern California.
Christian G. Merkel, Professor of Biochemistry, 1979. BA, University of Cincinnati; MA, University of
California, Santa Barbara; PhD, University of Cincinnati.
Tony Mosconi, Assistant Professor of Anatomy, 1997. BS, Allegheny College; MS, PhD, Albany Medical
College.
Wallace J. Murray, Associate Professor of Pharmaceutical Sciences, 1999. BS, San Diego State
University; PhD, University of California, San Francisco.
Amelia Naccarto-Coleman, Assistant Professor of Physician Assistant Education, 1995. BA, West Virginia
University; BS, MAS, Johns Hopkins University.
Gayle H. Nelson, Professor of Anatomy (Emeritus), 1980. BA, Walla Walla College; MS, University of
Maryland; PhD, University of Michigan.
Nancy Nielsen-Brown, Instructor of Physician Assistant Education, 1995. BTh, University of La Verne;
AS, Cypress College; PA, University of Southern California.
Stephen A. O'Barr, Assistant Professor of Pharmaceutical Sciences, 1999. BS, University of California,
San Diego; PhD, Arizona State University.
Christopher Oberg, Associate Professor of Health Professions Education, 1998. BA, University of
California, San Diego; PhD, The Claremont Graduate School.
Alice Shoemaker Oglesby, Professor of Microbiology (Emerita), 1979. BS, University of Oklahoma; MA,
University of Kansas; PhD, University of California, Berkeley.
Mark P. Okamoto, Associate Professor of Social and Administrative Sciences & Pharmacy Practice, 2000.
BS, University of California, Los Angeles; PharmD, University of Southern California.
Cyrus Parsa, Professor of Pathology, 1992. BS, California State University, Northridge; DO, University of
Health Sciences, Kansas City.
Cynthia J. Pentz, Assistant Professor of Physician Assistant Education, 2002. AS, Pasadena City College;
BS, University of Southern California; MPAS, University of Nebraska.
182
Sunil Prabhu, Associate Professor of Pharmaceutical Sciences, 1996. PhD, School of Pharmacy, Western
Virginia University; BPharm, Birla Institute of Technology.
Brenda Premo, Associate Professor of Health Professions Education, 1999. BA, California State
University, Long Beach; MBA, Pepperdine University.
Lara M. Rasmussen, Assistant Professor of Veterinary Medicine, 1999. BS, DVM, University of
California, Davis; MS, University of Minnesota.
Max D. Ray, Professor of Pharmacy Practice, 1996. BS, University of South Carolina, MS, PharmD,
University of Tennessee.
David Redding, Associate Professor of Family Medicine/Osteopathic Manipulative Medicine, 1996. BS,
PT, California State University, Long Beach; DO, College of Osteopathic Medicine of the Pacific; MS,
College of Osteopathic Medicine of the Pacific.
Donna Redman-Bentley, Professor of Physical Therapy Education, 1998. BS, Pennsylvania State
University; MS, The Ohio State University; PhD, University of Southern California.
Elizabeth A. Rega, Assistant Professor of Anatomy, 2000. BA, Valparaiso University; MA, PhD,
University of Chicago.
R. Ashley Robinson, Professor of Veterinary Medicine, 1998. BVSc, University of Sydney; Dip.
Microbiol, Otago University; MPH, PhD, University of Minnesota.
Burton N. Routman, Professor of Family Medicine, 1995. BA, Johns Hopkins University; DO, University
of Osteopathic Medicine and Health Sciences.
Margaret J. Rowberg, Assistant Professor of Nursing, 2000. BSN, MSN, California State University, Long
Beach.
Stanley Saul, Professor of Surgery/Urology, 1985. BS, Albright College; DO, Philadelphia College of
Osteopathic Medicine.
Beatrice J. Saviola, Assistant Professor of Microbiology, 2002. BS, University of Delaware; PhD, The
Johns Hopkins University.
James D. Scott, Assistant Professor of Pharmacy Practice, 2000. BS, MEd, PharmD, University of Florida.
Michael A. Seffinger, Assistant Professor of Family Medicine/Osteopathic Manipulative Medicine, 1999.
BA, University of California, Santa Cruz; DO, Michigan State University.
David M. Selkowitz, Associate Professor of Physical Therapy Education, 2000. BS, State University of
New York, Buffalo; MS, Boston University; PhD, The Union Institute.
Natalie Semaan, Assistant Professor of Pharmacy Practice, 2000. BS, Portland State University; PharmD,
University of the Pacific.
Karen Shapiro, Assistant Professor of Pharmacy Practice, 2000. BA, Boston University, PharmD,
University of Southern California.
Sam Shimomura, Professor of Pharmacy Practice, 1997. PharmD, University of California, San Francisco.
Gail L. Singer-Chang, Assistant Professor of Family Medicine, 1999. BA, San Diego State University,
MA, PsyD, California School of Professional Psychology, Los Angeles.
183
Sandra Stuckey, Assistant Professor of Physical Therapy Education, 1991. BS, Michigan State University;
MA, California State University, Los Angeles; PT, Stanford University.
Ruth Ann Subach, Assistant Professor of Pharmacy Practice, 1999. BS, St. John's University; PharmD,
University of Utah.
Richard A. Sugerman, Professor of Anatomy, 1980. BA, California State University, San Diego; MS, PhD,
University of New Mexico.
Reza Taheri, Assistant Professor of Pharmacy Practice, 2000. BA, PharmD, University of Minnesota.
M. Elizabeth Towner, Adjunct Professor of Nursing, 2000. BS, Duquesne University; MSN, University of
California, San Francisco; FNP, Indiana University; PhD, University of Texas.
Carl E. Trinca, Professor of Social and Administrative Sciences, 1995. BS, MS, PhD, University of
Arizona.
Ehab Tuppo, Assistant Professor of Geriatrics/Internal Medicine, 2000. BS, MS, MA, Wayne State
University; DO Michigan State University.
Guillermo Valenzuela, Associate Professor of Obstetrics/Gynecology, 1995. MD, Catholic University
Medical School.
Georgeanne Vlad, Assistant Professor of Physical Therapy Education, 1991. BS, California State
Polytechnic University, Pomona; MA, University of California, Santa Barbara; PT, Children's Hospital,
Los Angeles.
Edward J. Wagner, Assistant Professor of Physiology, 2001. BS, University of California, Los Angeles;
PhD, Michigan State University.
Donald E. Walters, Associate Professor of Pharmacology, 2001. BS, St. Louis College of Pharmacy; PhD,
University of Louisville.
Sompon Wanwimolruk, Associate Professor of Pharmaceutical Sciences, 2001. BSc, MSc, Mahidol
University; PhD, Flinders University of South Australia.
Paul W. Willis, Jr., Assistant Professor of Family Medicine, 2001. BA, University of Southern Florida;
DO, College of Osteopathic Medicine of the Pacific.
Richard Winn, Instructor of Family Medicine, 2001. BA, Pacific Union College; MA, M.Div., Andrews
University; EdD, University of La Verne.
Siu-Fun Wong, Associate Professor of Pharmacy Practice, 1997. BS, University of California, Los
Angeles; PharmD, University of California, San Francisco.
Stanley K. Wong, Professor of Pharmacology, 1981. BS, MS, PhD, University of Wisconsin.
Annie Wong-Beringer, Associate Professor of Pharmacy Practice, 1997. PharmD, University of Southern
California, Los Angeles.
Frances Yang, Assistant Professor of Pediatrics, 1999. BS, California State Polytechnic University,
Pomona; DO, Western University of Health Sciences.
184
Bartley Yee, Assistant Professor of Family Medicine, 1999. BS, University of California, Los Angeles;
DO, Michigan State University.
Rafi Younoszai, Professor of Anatomy, 1979. BS, University of California, Berkeley; PhD, University of
Minnesota.
185
CLINICAL AND ADJUNCT FACULTY
Julie Abraham, PharmD
Assistant Professor of Pharmacy Practice
Mary L. Adair, PA-C
Instructor of Physician Assistant Education
Ross Mitchell Adams, DO
Assistant Professor of Pediatrics
Cyrus Afrasiabi, MD
Associate Professor of Internal Medicine
Afshin Afrookhteh, JD
Assistant Professor of Physician Assistant
Education
Chandrahas Agarwal, MD
Assistant Professor of Internal Medicine/
Cardiology
Vandana Agarwal, MD
Assistant Professor of Internal Medicine/
Oncology & Hematology
Luz del Carmen Aguirre, MD
Assistant Professor of Physician Assistant
Education
Joseph Aiello, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Laye Akinloye, PA-C
Associate Professor of Physician Assistant
Education
Murtadha Al-Marashi, MD
Associate Professor of Internal
Medicine/Neurology
Steven Alder, MD
Assistant Professor of Internal Medicine/
Pathology
John G. Alevizos, DO
Assistant Professor of Family Medicine
Brent R. Allan, MPH, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Ethan R. Allen, DO
Professor of Family Medicine
Larkin Allen, DO
Assistant Professor of Surgery/Ophthalmology
Robert F. Altamura, DO
Associate Professor of Internal Medicine
Louis R. Alvarez, MD, MPH
Assistant Professor of Family Medicine/
Psychiatry
M. Mark Alwan, MD
Assistant Professor of Obstetrics/Gynecology
Suyng-Hye An, PharmD
Assistant Professor of Pharmacy Practice
Deepak Anand, Ph.D.
Assistant Professor of Pharmacy Practice
Kenneth Anderson III, DO
Assistant Professor of Family Medicine
Ray E. Anderson, DO
Assistant Professor of Family Medicine
Wayne E. Anderson, DO
Assistant Professor of Internal Medicine/
Neurology
William G. Anderson, DO, FACOS
Professor of Surgery
Lawrence R Andreatta, MS
Assistant Professor of Pharmacy Practice
Elias I. Anoub, MD
Assistant Professor of
Surgery/Otorhinolaryngology
Jeffrey P. Anthony, DO
Assistant Professor of Family Medicine/
Sports Medicine
Michael D. Antos, MD
Assistant Professor of Internal Medicine/
Pediatrics
Y. Paul Aoyagi, MD
Associate Professor of Physician Assistant
Education
186
Rubina Aqueel, MD
Assistant Professor of Internal Medicine/
Endocrinology
Neal S. Archer, DO
Associate Professor of Family Medicine
John J. Aryanpur, MD
Assistant Professor of Surgery
Mohammad Aslam, MD
Assistant Professor of Internal Medicine/
Cardiology
Allison Atkinson, PA-C
Assistant Professor of Physician Assistant
Education
Gary K. Augter, MS, DO
Assistant Professor of Family Medicine/
Dermatology
Gino Aveni, PA-C
Instructor of Physician Assistant Education
Paul A. Aversano, DO
Associate Professor of Internal Medicine/
Neurology
Aziz F. Awad, DO
Assistant Professor of Family Medicine
Mg San Aye, MD
Assistant Professor of Surgery/Ophthalmology
Muhammad A. Azam, MD
Assistant Professor of Physician Assistant
Education
Richard M. Bachrach, DO
Assistant Professor of Family Medicine
Peter A. Badua, PA-C
Assistant Professor of Physician Assistant
Education
Pejman Bady-Moghaddam, DO
Assistant Professor of Physician Assistant
Education
Rana A. Bahl, MD
Associate Professor of Internal Medicine/
Cardiology
O.J. (Jerry) Bailes, DO
Professor of Family Medicine
Henry Bakhit, PhD
Assistant Professor of Pharmacy Practice
Farhan Bakir, MD, MS
Professor of Internal Medicine
Bradley A. Baldwin, DO
Assistant Professor of Surgery
Vijaya Bansal, MD
Assistant Professor of Obstetrics/Gynecology
Steven H. Barag, DO, MS
Assistant Professor of Family Medicine
Rebecca Barnett, PA-C
Assistant Professor of Physician Assistant
Education
Rodolfo Cantu Barrera, DO
Assistant Professor of Pediatrics
Connie P. Bartlett, DO
Assistant Professor of Pediatrics
Jonathan S. Bartlett, MS, RPh
Assistant Professor of Pharmacy Practice
Roy W. Bartlett, DO
Assistant Professor of Surgery/Ophthalmology
Geoffrey Baum, DO
Assistant Professor of Surgery
William Chandler Bearce, PharmD
Assistant Professor of Pharmacy Practice
Daniel J. Beavers, DO
Associate Professor of Family Medicine/
Psychiatry
Robert D. Belanger, DO
Professor of Family Medicine
Joseph W. Bell Jr., DO
Assistant Professor of Obstetrics/Gynecology
Robert B. Bell, DO
Professor of Family Medicine
Linda Beth Benaderet, DO
Professor of Internal Medicine/Oncology
187
Michael Benavidez, DO
Assistant Professor of Family Medicine
Paul Benchwick, DO
Professor of Internal Medicine
Irvin S. Benowitz, DO
Associate Professor of Family Medicine
Mark P. Berland, DO
Assistant Professor of Obstetrics/Gynecology
Yoopin Bernbrock, PharmD
Assistant Professor of Pharmacy Practice
Steven M. Beutler, MD
Assistant Professor of Internal Medicine/
Infectious Diseases
A. Raja Bhupathy, DO
Assistant Professor of Family Medicine/
Dermatology
Vellore R. Bhupathy, MD, FACOG
Associate Professor of Obstetrics/Gynecology
Henry B. Bikhazi, MD, FACS
Assistant Professor of Surgery/
Otorhinolaryngology
Lori B. Birndorf, DO
Assistant Professor of Surgery/Ophthalmology
Murray L. Black, DO
Adjunct Assistant Professor of Family Medicine
Eliot S. Blackman, DO
Assistant Professor of Family Medicine
Andre V. Blaylock, MD
Assistant Professor of Family Medicine
William A. Blee, MD
Assistant Professor of Internal Medicine
Russell C. Bloom, DO
Assistant Professor of Family Medicine
Robert J. Bohr, MD
Assistant Professor of Surgery/Orthopedics
Richard A. Bond, DO
Associate Professor of Family Medicine
Gregory R. Bonomo, MD
Assistant Professor of Internal Medicine/
Neurology
Timothy R. Borman, DO
Assistant Professor of Surgery/Orthopedics
Allen D. Bott, MD
Assistant Professor of Internal
Medicine/Neurology
James B. Boyd, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Cory D. Boyles, MD
Assistant Professor of Physician Assistant
Education
John D. Branch, DO
Assistant Professor of Family Medicine
Michael Brand, MD
Assistant Professor of Internal Medicine/
Radiology
Rodney D. Brandt, MD
Assistant Professor of Surgery/Orthopedics
David A. Brauner, DO
Associate Professor of Pediatrics
Marc D. Braunstein, DO
Assistant Professor of Family Medicine
Randy J. Brazie, MD
Assistant Professor of Family Medicine/
Psychiatry
Mary Lou Breslin, MS
Adjunct Assistant Professor of Health
Professions Education
Paul C. Bressman, MD
Assistant Professor of Surgery
Sister Anne E. Brooks, DO
Associate Professor of Family Medicine
Kevin R. Brown, PharmD
Assistant Professor of Pharmacy Practice
Thomas C. Brown, PhD
Associate Professor of Family Medicine/
Behavioral Sciences
188
Karen E. Brungardt, DO
Assistant Professor of Family Medicine
Bernard Buchanan, MD
Assistant Professor of Family Medicine/
Psychiatry
Timothy W. Burke, DO
Associate Professor of Internal Medicine/
Gastroenterology
Patrick J. Burns, DO
Assistant Professor of Internal Medicine/
Neurology
Michael S. Burton, MD
Assistant Professor of Family Medicine
Robert D. Bush, MD
Assistant Professor of Family Medicine
Jay M. Butterman, DO
Assistant Professor of Family Medicine/
Psychiatry
Grethel A. Cabison, MD
Assistant Professor of Surgery/Anesthesiology
Carol T. Cahill, DO
Assistant Professor of Pediatrics
William J. Cairney, PhD
Adjunct Professor of Family Medicine
Paul H. Caldron, DO
Assistant Professor of Internal Medicine/
Rheumatology
John B. Campbell, MD
Assistant Professor of Internal Medicine/
Pathology
Dennis M. Carden, DO
Associate Professor of Obstetrics/Gynecology
Samuel A. Carlis, DO
Assistant Professor of Family Medicine
Sherie Carnegie, DO
Assistant Professor of Family Medicine
Michael A. Carnevale, DO
Assistant Professor of Internal Medicine
Dale M. Carrison, DO
Assistant Professor of Family
Medicine/Emergency Medicine
John Joseph Cassani, DO
Assistant Professor of Family Medicine
Angela Jo Castro, PA-C
Instructor of Physician Assistant Education
Mary Caizza Cerni, DO
Assistant Professor of Family Medicine
Ramon M. Cestero, MD
Associate Professor of Obstetrics/Gynecology
Mikyung Chai, BS
Assistant Professor of Pharmacy Practice
Francis Y.-M. Chan, PharmD
Assistant Professor of Pharmacy Practice
Sammy C. Chan, MD
Assistant Professor of Physician Assistant
Education
Jonathan L. Chang, MD
Assistant Professor of Surgery/Orthopedics
Laura Chang-Strauss, MD
Assistant Professor of Pediatrics
Janet Cheetham, PharmD
Assistant Professor of Pharmacy Practice
Joy H. Chen, PharmD
Assistant Professor of Pharmacy Practice
Cindy P. Cheng, PharmD
Assistant Professor of Pharmacy Practice
Kenneth S. Cheng, DO
Assistant Professor of Physician Assistant
Education
Peter F.-P. Cheng, PharmD
Assistant Professor of Pharmacy Practice
Stuart B. Chesky, DO
Professor of Obstetrics/Gynecology
Gary Lee Child, DO
Assistant Professor of Family Medicine
189
Dan Chiles, MD
Associate professor of Pediatrics
William L. Chin, DO
Assistant Professor of Internal Medicine
Fred K. Cho, PharmD
Assistant Professor of Pharmacy Practice
William T. Choctaw, MD
Associate Professor of Surgery
Michael S. Choi, MD
Assistant Professor of Surgery/Anesthesiology
Serina Chong, PharmD
Assistant Professor of Pharmacy Practice
Miriam M.-C. Chou, RPh
Assistant Professor of Pharmacy Practice
Yushu Jack Chou, MD
Assistant Professor of Physician Assistant
Education
Don L. Christensen, MD, FACS
Professor of Surgery
Lance W. Christiansen, DO
Assistant Professor of Family Medicine
Philip S. Cifarelli, MD, JD
Professor of Internal Medicine/Gastroenterology
Robin D. Clark, MD
Professor of Pediatrics/Medical Genetics
Susan J. Clark, MD
Associate Professor of Pediatrics/Endocrinology
Therese Sage Clark, PharmD
Assistant Professor of Pharmacy Practice
Trence Clark, MD
Assistant Professor of Family Medicine/
Emergency Medicine
John O. Clune, MD
Assistant Professor of Internal Medicine/
Hematology &Oncology
Ellen Clymer, EdD
Adjunct Associate Professor of Health
Professions Education
Alan L. Cohen, DO
Assistant Professor of Family Medicine
Donald A. Cohen, DO
Adjunct Assistant Professor of Physician
Assistant Education
Murray H. Cohen, DO
Professor of Internal Medicine
Robert S. Cohen, DO
Associate Professor of Internal Medicine/
Nephrology
Samantha Cohen, PA-C
Instructor of Physician Assistant Education
Steven W. Cohen, DO
Assistant Professor of Family Medicine
William C. Cohen, DO
Assistant Professor of Surgery/
Otorhinolaryngology
Wilbur Cole III, DO
Assistant Professor of Family Medicine
Stacey L. Coleman, DO
Assistant Professor of Family Medicine
Randy E. Collins, DO
Assistant Professor of Obstetrics/Gynecology
Francis L. Comunale, MD
Professor of Surgery/Anesthesiology
Ralph E. Conner, DO
Assistant Professor of Family Medicine/
Emergency Medicine
David A. Connett, DO
Associate Professor of Family Medicine
Eugene T. Conte, DO
Assistant Professor of Family Medicine/
Dermatology
Milissa A. Cooper, DO
Assistant Professor of Family Medicine
Joel B. Cooperman, DO
Associate Professor of Family Medicine
Marshall Cooperson, DO
Assistant Professor of Internal Medicine
190
M. Larry Copeland, DO
Assistant Professor of Surgery/Orthopedics
Joe Corless, MD
Associate Professor of Pediatrics
Michael Coronado, PharmD
Assistant Professor of Pharmacy Practice
Conrad A. Cox, MD
Assistant Professor of Internal Medicine
Gary W. Crawford, MD
Assistant Professor of Internal Medicine
Linda L. Crawford, DO
Assistant Professor of Family Medicine
Gary M. Critser, DO
Assistant Professor of Family Medicine
Bruce S. Cromer, PharmD
Assistant Professor of Pharmacy Practice
James A. Crosby, DO
Assistant Professor of Internal
Medicine/Neurology
Michael P. Curley, MD
Assistant Professor of Physician Assistant
Education
Jack Dabbert, MS, PT
Adjunct Assistant Professor of Physical Therapy
Education
Himmet Dajee, MD
Assistant Professor of Surgery
Maria F. Daly, DO
Assistant Professor of Family Medicine
Joseph Damiani, DO
Assistant Professor of Surgery/Plastic Surgery
Kathleen Damiani, MD
Assistant Professor of Surgery/
Otorhinolaryngology
Stephen Damiani, DO
Assistant Professor of Internal Medicine/
Endocrinology
Sid Danesh, MD
Assistant Professor of Family Medicine
Nghiem Duc Dang, MD
Assistant Professor of Surgery
Sarah G. Daum, EdD
Adjunct Associate Professor of Health
Professions Education
Bert J. (Hans) Davidson, MD, PhD
Assistant Professor of Obstetrics/Gynecology
Richard C. Davies, DO
Assistant Professor of Family Medicine
Steven E. Davis, DO, MS
Assistant Professor of Family Medicine
Anil Daya, MD
Assistant Professor of Internal Medicine
Douglas Deans, PharmD
Assistant Professor of Pharmacy Practice
James J. Dearing, DO
Assistant Professor of Family Medicine
Lori de Bold, MD
Associate Professor of Physician Assistant
Education
Lino J. de Guzman, MD
Assistant Professor of Internal Medicine/
Gastroenterology
Cheryl Delgado, PharmD
Assistant Professor of Pharmacy Practice
Ricardo E. de Napoli, DO
Assistant Professor of Family Medicine
Harry W. Depew, MD
Assistant Professor of Family Medicine
Angela de Rosa, DO
Instructor of Internal Medicine
Christian Derefield, BS, PA-C
Instructor of Physician Assistant Education
Sunita Dergalust, PharmD
Assistant Professor of Pharmacy Practice
191
Bela Desai, PharmD
Assistant Professor of Pharmacy Practice
Nilesh Desai, MD
Assistant Professor of Internal Medicine
Steven M. Deterville, MD
Assistant Professor of Family Medicine
Lorane Dick, DO
Associate Professor of Family Medicine/
Osteopathic Manipulative Medicine
Joel Dickerman, DO
Professor of Family Medicine
Dinh V. Dinh, DO
Assistant Professor of Family Medicine
Lew B. Disney, MD, PhD
Assistant Professor of Surgery
Stephen D. Docherty, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Neil E. Doherty III, MD
Assistant Professor of Internal Medicine/
Cardiology
Sretenka Dokich, MD
Assistant Professor of Physician Assistant
Education
Eric J. Dolgin, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
William C. Domb, DMD
Associate Professor of Family Medicine/
Dentistry
Thomas K. Donaldson, MD
Associate Professor of Surgery
Tennison S. Dong, MD
Assistant Professor of Surgery
Gregory J. Downs, MD
Assistant Professor of Surgery/Anesthesiology
Phat Van Du, PharmD
Assistant Professor of Pharmacy Practice
Roger D. Duber, DO
Professor of Internal Medicine/Cardiology
Patrick Duke, PA-C
Instructor of Physician Assistant Education
Ian R. Duncan, DO
Assistant Professor of Family Medicine
Sheila K. Dunlop, DO
Assistant Professor of Family Medicine
Virginia (Ginny) D. Dunn, MS, PT
Adjunct Assistant Professor of Physical Therapy
Education
Tanya T. Duong, PharmD
Assistant Professor of Pharmacy Practice
Nguyen (Andy) D. Duy, MD
Assistant Professor of Surgery/Vascular Surgery
Emily A. Ebert, MD
Associate Professor of Family Medicine
Richard E. Eby, DO
Professor of Obstetrics/Gynecology
Joel B. Edelstein, DO
Assistant Professor of Internal Medicine
Roy Egari, MD
Assistant Professor of Surgery/Urology
Hisham El-Bayer, MD
Assistant Professor of Surgery
Mohamad Eletreby, PharmD
Assistant Professor of Pharmacy Practice
Joshua D. Ellenhorn, MD
Associate Professor of Physician Assistant
Education
Dale A. Elleson, DO
Assistant Professor of Surgery/
Otorhinolaryngology
Bernard T. Elpedes, DO
Assistant Professor of Family Medicine
Larry I. Emdur, DO, PhD
Assistant Professor of Internal Medicine/
Pulmonary Medicine
192
Richard J. Emerson, DO
Professor of Surgery/Orthopedics
Paul E. Emmans Jr., DO
Assistant Professor of Family Medicine
Diane Endo-Okada, PharmD
Assistant Professor of Pharmacy Practice
Emily Engelbrecht, PharmD
Assistant Professor of Pharmacy Practice
Jack D. England, DO
Professor of Family Medicine/Emergency
Medicine
Scott Engwall, MD
Assistant Professor of Surgery
Carl M. Erikson, DO
Assistant Professor of Family Medicine
Steven Ernst, MD
Assistant Professor of Family Medicine/
Emergency Medicine
J. Yusuf Erskine, DO
Assistant Professor of Family Medicine
Brenda Espe, DO
Assistant Professor of Family Medicine
Mohammad R. Etminan, MS, RPh
Assistant Professor of Pharmacy Practice
James T. Evans, MD
Assistant Professor of Family Medicine
Thomas W. Eyler, DO
Assistant Professor of Family Medicine
Wade Faerber, DO
Associate Professor of Surgery/Orthopedics
Robert R. Fajardo, PA-C
Instructor of Physician Assistant Education
Rachel Farrell, PA-C
Instructor of Physician Assistant Education
John R. Feeney, DO
Assistant Professor of Family Medicine
Gary M. Feinberg, MD
Assistant Professor of Surgery/
Otorhinolaryngology
Michael J. Feinstein, DO
Professor of Family Medicine
Rodney J. Felber, DO
Assistant Professor of Internal Medicine
Edward M. Feldman, DO
Assistant Professor of Obstetrics/Gynecology
George Ferenczi, MD
Assistant Professor of Internal Medicine/
Gastroenterology
Carl E. Ferguson, DO
Assistant Professor of Family Medicine
Ronald B. Ferris, MD
Associate Professor of Family Medicine
Henie A. Fialkoff, MD
Assistant Professor of Pediatrics
George Fields, DO
Associate Professor of Family Medicine
Joseph P. Figlow, PharmD
Assistant Professor of Pharmacy Practice
Elizabeth Finebaum, PA-C
Instructor of Physician Assistant Education
Dan Fisher, PharmD
Assistant Professor of Pharmacy Practice
David E. Fisher, MD
Associate Professor of Physician Assistant
Education
Katherine L. Fisher, DO
Assistant Professor of Internal Medicine
Steven M. Fitzmorris, MD
Assistant Professor of Internal Medicine/
Cardiology
Bruce D. Flagg, DO
Assistant Professor of Family Medicine
Paul M. Fleiss, MD, MPH
Professor of Pediatrics
193
Stanley L.K. Flemming, DO
Associate Professor of Family Medicine
Jon W. Fong, DO
Assistant Professor of Family Medicine
Nicole Foster, PA-C, MS
Assistant Professor of Physician Assistant
Education
Tina C.S. Foster, MD
Assistant Professor of Obstetrics/Gynecology
Ali Fouladi, MD
Assistant Professor of Surgery
Paul A. Fredrick, MD
Associate Professor of Internal Medicine
Susan Lohr Freeman, PharmD
Assistant Professor of Pharmacy Practice
John B. Freitas, DO
Assistant Professor of Family Medicine
Richard Frelinger, DO
Assistant Professor of Family Medicine
Gerald Stanley Friedman, MD
Associate Professor of Family Medicine
Theodore A. Friedman, MD
Associate Professor of Internal Medicine/
Pathology
Leonard M. Fromer, MD
Assistant Professor of Family Medicine
Byron Fujimoto, MD
Assistant Professor of Internal Medicine/
Radiology
Ronald Y. Fujimoto, DO
Assistant Professor of Family Medicine
Michele Fujiokon, PharmD
Assistant Professor of Pharmacy Practice
Wendy Fukushima, PharmD
Assistant Professor of Pharmacy Practice
Geoffrey Furman, MD
Assistant Professor of Family Medicine
Mark J. Gabriel, DO
Assistant Professor of Internal Medicine/
Gastroenterology
Balu Gadhe, MD
Assistant Professor of Internal Medicine
Karen L. Gaio, MD
Assistant Professor of Obstetrics/Gynecology
John A. Gama, PharmD
Assistant Professor of Pharmacy Practice
Anil K. Gandhi, MB/BS
Assistant Professor of Family Medicine
Vinod K. Garg, MD
Assistant Professor of Surgery
James E. Garmon Jr., PA-C
Assistant Professor of Physician Assistant
Education
Ronny G. Ghazal, MD
Associate Professor of Surgery/Orthopedics
Bharati Ghosh, MD
Associate Professor of Pediatrics
Mark Gibson, PA-C
Instructor of Physician Assistant Education
Ulric Gilkes, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Lawrence S. Glass, DO
Assistant Professor of Family Medicine
Jeffrey W. Glassheim, DO
Assistant Professor of Pediatrics
Reid M. Gliddon, MS, RPh
Assistant Professor of Pharmacy Practice
Justin R. Glodowski, DO
Assistant Professor of Family Medicine
Appanagari (Dev) Gnanadev, MD
Associate Professor of Surgery
Sergio Y. Go Jr, MD
Assistant Professor of Internal Medicine
194
Edward Goering, DO, MS
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Stanley A. Golanty, MD
Professor of Internal Medicine
Allan P. Goldman, DO
Associate Professor of Family Medicine
Frank C. Gomez, DrPH.
Assistant Professor of Physician Assistant
Education
Myron J. Gomez, MD
Assistant Professor of Surgery/Vascular Surgery
Allen E. Gorenberg, MD
Assistant Professor of Internal Medicine/Allergy
Daniel Gorenberg, MD
Assistant Professor of Internal Medicine/Allergy
Dale J. Gorski, DO
Assistant Professor of Family Medicine
David C. Gorsulowsky, MD
Assistant Professor of Family Medicine/
Dermatology
Lawrence F. Gosenfeld, DO
Assistant Professor of Family Medicine/
Psychiatry
May M. Goto, PharmD
Assistant Professor of Pharmacy Practice
Galal S. Gough, MD
Associate Professor of Obstetrics/Gynecology
David S. Goya, DO
Assistant Professor of Internal Medicine/
Pulmonary Diseases
William M. Graham, DO
Associate Professor of Surgery
Howard Graitzer, DO
Associate Professor of Internal Medicine
Barry S. Grames, MD
Assistant Professor of Surgery
Gary A. Gramm, DO
Assistant Professor of Family Medicine
Bradley C. Grant, DO
Associate Professor of Family Medicine
David Greenberg, PA-C
Instructor of Physician Assistant Education
Gerald R. Greene, MD
Professor of Pediatrics/Infectious Diseases
Roger Greenham, PharmD
Assistant Professor of Pharmacy Practice
Fred O. Gregorian, PharmD
Assistant Professor of Pharmacy Practice
Lindy S. Griffin, DO
Assistant Professor of Family Medicine
Peter D. Grimm, DO
Associate Professor of Internal Medicine/
Oncology
James W. Groff, DO
Assistant Professor of Family Medicine/
Dermatology
Debra L. Gromacki-Blyth, PA-C
Instructor of Physician Assistant Education
Jeotsna Grover, MD
Assistant Professor of Obstetrics & Gynecology
Joel S. Grubbs, DO
Assistant Professor of Family Medicine
David Gu, DO
Assistant Professor of Internal Medicine
Edward Guerrero, PharmD
Assistant Professor of Pharmacy Practice
Gary W. Gulizia, DO
Assistant Professor of Family Medicine
Mahesh C. Gupta, MD
Assistant Professor of Internal Medicine
Suresh Gurbani, MD, PhD
Assistant Professor of Pediatrics
Thomas C. Gustafson, DO
Assistant Professor of Family Medicine
195
Richard G. Gwinn, MD
Assistant Professor of Physician Assistant
Education
Mark Haddad, PharmD
Assistant Professor of Pharmacy Practice
Angeline Hadiwidhaha, MD
Assistant Professor of Pediatrics
Thomas A. Haffey, DO
Professor of Internal Medicine/Cardiology
Samir E. Hage, DO
Assistant Professor of Obstetrics & Gynecology
David B. Hagie, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Stefan L.J. Hagopian, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Roger Hall, DO
Assistant Professor of Family Medicine
Issa Y. Hallaq, DO
Associate Professor of Internal Medicine
Norman Hamada, PharmD
Assistant Professor of Pharmacy Practice
Robert C. Hamilton, MD
Assistant Professor of Pediatrics
Curtis R. Handler, MD
Assistant Professor of Internal Medicine/
Radiology
Lofty R. Hanna, MD
Assistant Professor of Internal Medicine
Charles E. Hansing, MD
Assistant Professor of Internal Medicine/
Cardiology
Ben Hara, DPM
Professor of Family Medicine/Podiatry
W. Benson Harer, MD
Professor of Obstetrics/Gynecology
Pamela J. Harford, DO
Assistant Professor of Family Medicine
Jon Frederic Harrell, DO, FACS
Assistant Professor of Surgery
Clyde O. Harris III, MD
Assistant Professor of Surgery
Elliot A. Harris, MD
Professor of Family Medicine/Psychiatry
Imran Hasnain, MD
Assistant Professor of Internal Medicine
John R. Hawes Jr., DO
Associate Professor of Family Medicine
Todd Hee, MD
Associate Professor of Internal Medicine
Ole A. Heggeness, DO
Assistant Professor of Family Medicine
Joseph J. Helak, DO
Professor of Surgery
Helge S. Helgesen, PA-C
Instructor of Physician Assistant Education
William W. Henning, DO
Assistant Professor of Family Medicine
Joseph J. Herbert, MD
Assistant Professor of Pediatrics
Guillermo Hernandez, DO
Assistant Professor of Family Medicine
Raul Hernandez, MD
Assistant Professor of Physician Assistant
Education
Stanley S. Herr, DO
Assistant Professor of Family Medicine
Jose Francisco Herrera, MD
Associate Professor of Family Medicine
Edward A. Heusch, DO
Associate Professor of Surgery
Michael L. Hicks, BA, PA-C
Assistant Professor of Physician Assistant
Education
Miles J. Hildebrand, PharmD
Assistant Professor of Pharmacy Practice
196
Cynthia A. Hill, DO
Assistant Professor of Family Medicine
Ronald H. Hino, MD
Assistant Professor of Physician Assistant
Education
Roger Hirsh, MS, MBA
Assistant Professor of Pharmacy Practice
Craig Hitchman, BPharm
Assistant Professor of Pharmacy Practice
Jerry W. Hizon, MD
Assistant Professor of Physician Assistant
Education
George L. Hobeich, MD
Associate Professor of Internal Medicine
Timothy P. Hodges, DO
Assistant Professor of Family Medicine
Joseph O. Hoffman, DO
Associate Professor of Family Medicine
Marc A. Hoffman, DO
Assistant Professor of Family Medicine
David P. Hofheins, DO
Assistant Professor of Family Medicine
E. Carlisle Holland, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Philip Holman, PharmD
Assistant Professor of Pharmacy Practice
Lorin G. Holst, MD
Assistant Professor of Internal Medicine
Charles Holzner, MD
Professor of Internal Medicine
Theresa A. Hong, DO
Assistant Professor of Family Medicine
William K. Hooks III, MD
Assistant Professor of Internal Medicine/
Radiology
Fran Hopkins, PharmD
Assistant Professor of Pharmacy Practice
Katherine R. Horad, BS, PA-C
Instructor of Physician Assistant Education
Franklin Horowitz, MD
Professor of Surgery (Emeritus)
Mark Horowitz, DO
Assistant Professor of Family Medicine/
Dermatology
Joseph Hourany, MD
Assistant Professor of Internal Medicine/
Pulmonology
Bruce R. Hoyle, MD
Assistant Professor of Physician Assistant
Education
David W. P. Huang, MD
Assistant Professor of Surgery/Orthopedics
Kuo-Liang Huang, MD
Assistant Professor of Internal Medicine/
Infectious Diseases
W. Luke Huang, MD
Assistant Professor of Pediatrics
Anna O. Huh, PharmD
Assistant Professor of Pharmacy Practice
Catherine Ann Hunter, DO
Assistant Professor of Obstetrics/Gynecology
Nga N. Huynh, PharmD
Assistant Professor of Pharmacy Practice
Paul V.B. Hyde, MD
Assistant Professor of Surgery
John Hyun, PharmD
Assistant Professor of Pharmacy Practice
Robert A. Innocenzi, DO
Assistant Professor of Surgery/Ophthalmology
Anthony L. Jackson, MD
Assistant Professor of Physician Assistant
Education
Marianne B. Jacobs, DO
Assistant Professor of Internal Medicine/
Neurology
197
Arthur J. Jaffee, JD
Professor of Medical Jurisprudence
David S. James, DO
Assistant Professor of Family Medicine
Wen-Feng Jan, MD
Assistant Professor of Pediatrics/Endocrinology
Carl Jansen, MD
Professor of Internal Medicine/Radiology
Kedy Ying Jao, DO
Assistant Professor of Family Medicine
Mahmood J. Jazayeri, MD
Assistant Professor of Surgery/Orthopedics
W. Craig Jeffers, RPh
Assistant Professor of Pharmacy Practice
Richard R. Jeffries, DO
Associate Professor of Family Medicine
Kraig K. Jenson, MD
Assistant Professor of Family Medicine/
Dermatology
Debra L. Johnson, RN, NP, PA-C
Assistant Professor of Physician Assistant
Education
Elizabeth G. Johnson, PharmD
Assistant Professor of Pharmacy Practice
Eric G. Johnson, MPT
Adjunct Assistant Professor of Physical Therapy
Education
Gary R. Johnson, DO, DVM
Assistant Professor of Family Medicine
Jacqueline A. Johnson, MD
Assistant Professor of Family Medicine
John Johnson, PharmD
Assistant Professor of Pharmacy Practice
Larry Johnson, PharmD
Assistant Professor of Pharmacy Practice
Robert C. Jones, MD
Assistant Professor of Internal Medicine
Christopher Jordan, MD
Associate Professor of Surgery/ Orthopedics
Layne S. Jorgensen, DO
Assistant Professor of Family Medicine
Randal Carl Juengel, MD
Assistant Professor of Internal Medicine/
Pathology
Anthony A Juguilon, MD
Assistant Professor of Internal Medicine/
Pathology
Nami Jun, PharmD
Assistant Professor of Pharmacy Practice
Nancy R. Kahaner, DO
Assistant Professor of Obstetrics/Gynecology
June Isaacson Kailes, MSW
Adjunct Associate Professor of Health
Professions Education
Stanley A. Kaller, DO
Assistant Professor of Family Medicine
Charles L. Kaluza, DO
Associate Professor of Surgery/
Otorhinolaryngology
Steven D. Kamajian, DO
Associate Professor of Family Medicine
Frank G. Karneges, DO
Assistant Professor of Internal Medicine
Thomas J. Karras, MD
Associate Professor of Internal Medicine/
Cardiology
Andre M. Kasko, DO
Assistant Professor of Physician Assistant
Education
Hooshang Kasravi, MD
Assistant Professor of Surgery
Michael D. Kasseles, DO
Assistant Professor of Internal Medicine
Louis B. Kasunic, DO
Assistant Professor of Family Medicine
198
Lionel B. Katchem, DO
Associate Professor of Family Medicine
Lia Katz, MD
Assistant Professor of Family Medicine
Brian I. Kawahara, PharmD
Assistant Professor of Pharmacy Practice
Martin H. Kay, MD, PhD
Assistant Professor of Family Medicine/
Dermatology
Christopher Keenan, MD
Assistant Professor of Family Medicine
Lori A. Kemper, DO
Associate Professor of Family Medicine
Darlina M. Keseg-Manthei, DO
Assistant Professor of Family Medicine
Stephen E. Kessler, DO
Assistant Professor of Family Medicine/
Dermatology
Rosita Z. Kheibari, PharmD
Assistant Professor of Pharmacy Practice
Ahmed Khosrowshahi, MD
Assistant Professor of Physician Assistant
Education
Karen S. Kiefer, DO
Assistant Professor of Family Medicine/
Psychiatry
Peter V. Kilburn, DO
Professor of Surgery
Karine Kim, PharmD
Assistant Professor of Pharmacy Practice
Lauren Kim, PharmD
Assistant Professor of Pharmacy Practice
Emily A. King, PharmD
Assistant Professor of Pharmacy Practice
Hwa-Kou King, MD
Professor of Internal Medicine/Anesthesiology
Neil E. Klein, MD
Assistant Professor of Surgery/Plastic &
Reconstructive
Calvin N. Kobluk, DVM, DVSc
Professor of Veterinary Medicine
Johannes Koch, MD
Assistant Professor of Internal Medicine
Sandra Kochaon, BS, PA-C
Instructor of Physician Assistant Education
Shahrokh Kohanim, DO
Assistant Professor of Family Medicine
Benjamin L. Konell, DO
Assistant Professor of Family Medicine
Choon Won Koo, MD
Assistant Professor of Obstetrics/Gynecology
Mark S. Kosins, MD
Professor of Family Medicine/Psychiatry
Dana Kosmala, DO
Assistant Professor of Pediatrics
Richard T. Kotomori, Jr., MD
Assistant Professor of Family Medicine
John C. Koumas, DO
Associate Professor of Family Medicine
Thomas Koumas, MD
Associate Professor of Family Medicine
Alan P. Kratz, MD
Assistant Professor of Surgery/Ophthalmology
David E. Kreshek, MD
Assistant Professor of Surgery
Divakar R. Krishnareddy, MD
Assistant Professor of Surgery/Orthopedics
Pamela C. Krochalk, DrPH.
Professor of Physician Assistant Education
Ellen B. Kruusmagi, MD
Assistant Professor of Family Medicine
Vanessa J. Kumpf, PharmD
Assistant Professor of Pharmacy Practice
Donald J. Kurth, MD
Assistant Professor of Family Medicine/
Emergency Medicine
199
Michael Z. Kurtz, DO
Assistant Professor of Family Medicine
Veronika R. Kurucz, MD
Assistant Professor of Internal Medicine
Mary Jo Kutler, DO
Assistant Professor of Pediatrics
Albert I. Kwan, PharmD
Assistant Professor of Pharmacy Practice
Eugene L. Kwong, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Grant Lackey, PharmD
Assistant Professor of Pharmacy Practice
Jennifer Lackey, PharmD
Assistant Professor of Pharmacy Practice
Linda D. Lafferty, DO, MS
Associate Professor of Family Medicine
Elizabeth M. Laine, PA-C
Instructor of Physician Assistant Education
James M. Lally, DO, MS
Assistant Professor of Family Medicine
Peter Lam, BS
Assistant Professor of Pharmacy Practice
Richard E. Land, DO
Associate Professor of Family Medicine/
Psychiatry
Carol L. Lang, DO
Assistant Professor of Family Medicine
Elizabeth C. Laqui, MD
Assistant Professor of Physician Assistant
Education
Lawrence A. Larson, DO
Assistant Professor of Pediatrics
Laurence J. Lasky, MD
Assistant Professor of Family Medicine
David M. Laufer, PharmD
Assistant Professor of Pharmacy Practice
Ronald E. Lazar, MD
Assistant Professor of Internal Medicine/
Anesthesiology
Arthur J. Lazik, MD, PhD
Assistant Professor of Internal Medicine/
Cardiology
Ha M. Le, MD
Assistant Professor of Internal Medicine/
Radiology
Peter C. Le Port, MD
Assistant Professor of Surgery
Scott C. Lederhaus, MD
Assistant Professor of Surgery
Carol Hyeun Lee, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Eun Hee Lee, PharmD
Assistant Professor of Pharmacy Practice
James T. Lee, DO
Associate Professor of Family Medicine
Jongmi Lee, PharmD
Assistant Professor of Pharmacy Practice
Laura E. Lee, PharmD
Assistant Professor of Pharmacy Practice
Thomas T. Lee, MD, FACOG
Assistant Professor of Obstetrics/Gynecology
William Y.W. Lee, DO
Assistant Professor of Family Medicine
David P. Leibel, DO
Assistant Professor of Surgery/Urology
Steven Leifheit, DO
Assistant Professor of Family Medicine
John F. Lennox, DO
Associate Professor of Obstetrics/Gynecology
Catherine Jones Lesnick, MS, PT
Adjunct Assistant Professor of Physical Therapy
Education
William R. Letendre Sr, MS, MBA
Adjunct Professor of Pharmaceutical Sciences
200
David Z. Levine, DO
Assistant Professor of Family Medicine
M. Richard Levinson, DO
Assistant Professor of Pediatrics
Gwen A. Levitt, DO
Assistant Professor of Family Medicine/
Psychiatry
Elaine Levy, BS
Assistant Professor of Pharmacy Practice
David O. Lewis, MD
Assistant Professor of Family Medicine
Judith L. Lewis, DO
Assistant Professor of Family Medicine
Sherman N. Lewis, DO
Assistant Professor of Surgery/Plastic &
Reconstructive
Lawrence Leyba, DO
Professor of Surgery/Anesthesiology
David Y. Li, DO
Assistant Professor of Internal
Medicine/Radiology
Robert Ligorsky, DO
Associate Professor of Internal Medicine/
Hematology and Oncology
Joseph L. Lillo, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Alice Lim, PharmD
Assistant Professor of Pharmacy Practice
Raymond Limansky, MD
Associate Professor of Obstetrics/Gynecology
Howard B. Limmer, DO
Associate Professor of Family Medicine
Augustin Lin, DO
Assistant Professor of Family Medicine
Matthew Y.C. Lin, MD
Assistant Professor of Surgery/Orthopedics
Leonard M. Linde, MD
Professor of Pediatrics
Cathleen Lindsay, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Ronald Liskanich, DO
Assistant Professor of Family Medicine/
Dermatology
Patricia Liu, PharmD
Assistant Professor of Pharmacy Practice
Sol Lizerbram, DO
Professor of Family Medicine
David A. Lyon, DO, DSc
Assistant Professor of Internal Medicine
Hedy C. Loa, MD
Assistant Professor of Internal Medicine/
Geriatrics
William T. Long, MD
Assistant Professor of Physician Assistant
Education
Paul K. Longmore, PhD
Adjunct Professor of Health Professions
Education
Christopher Lopatosky, PA-C
Assistant Professor of Physician Assistant
Education
Felice L. Loverso, Ph.D.
Assistant Professor of Health Professions
Education
Nelman C. Low, MD
Assistant Professor of Surgery/
Otorhinolaryngology
Kenneth Luck, PharmD
Assistant Professor of Pharmacy Practice
Bing Keung Kum, PharmD
Assistant Professor of Pharmacy Practice
Grant Lum, PharmD
Assistant Professor of Pharmacy Practice
Lisa M. Lupo, MD
Assistant Professor of Obstetrics/Gynecology
201
Hector F. Luque, DO
Assistant Professor of Internal Medicine
Pamela Renee Archer Lux, DO
Assistant Professor of Family Practice/
Emergency Medicine
Marc E. Lynch, DO
Assistant Professor of Surgery/Anesthesiology
Alfred C. Ma, MD, PhD, MBA
Professor of Internal Medicine/Anesthesiology
Richard H. Mabie, MD
Assistant Professor of Pediatrics
Daryl K. MacCarter, MD
Assistant Professor of Internal Medicine/
Rheumatology
F. Roy MacKintosh, MD, PhD
Professor of Internal Medicine
Gregory R. Maddex, DO
Assistant Professor of Family Medicine
Julie Madorsky, MD
Professor of Family Medicine/Physical Medicine
and Rehabilitation
Lon Madsen, DO
Assistant Professor of Family Medicine
Harold I. Magoun Jr., DO
Professor of Family Medicine/Osteopathic
Manipulative Medicine
Michael J. Mahon, DO
Associate Professor of Family Medicine/
Dermatology
Mark B. Maine, MSHSA
Instructor of Health Professions Education
Lisa L. Majer, DO
Assistant Professor of Family Medicine/Sports
Medicine
Manisha M. Malavia, PharmD
Assistant Professor of Pharmacy Practice
Samuel A. Malayan, MD, PhD
Assistant Professor of Internal Medicine
Barry D. Malina, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Ronald S. Mandel, DO
Assistant Professor of Family Medicine
John F. Manfredonia, DO
Assistant Professor of Family Medicine
Andrew J. Manos, DO
Associate Professor of Family Medicine
Rudy R. Manthei, DO
Assistant Professor of Surgery/Ophthalmology
Scott E. Manthei, DO
Assistant Professor of Surgery/
Otorhinolaryngology
Krishna N. Manvi, MD
Associate Professor of Internal Medicine/
Cardiology
Charles M. Maples, DO
Assistant Professor of Family Medicine
Shoaib U. Maqvi, MD
Assistant Professor of Internal Medicine
Calvin Marantz, MD
Associate Professor of Internal Medicine/
Pathology
Rod Marchiando, PharmD
Assistant Professor of Pharmacy Practice
Dante E. Marinelli, MD
Associate Professor of Surgery/Urology
Kevin F. Mark, PharmD
Assistant Professor of Pharmacy Practice
Steven Marks, DO
Assistant Professor of Internal Medicine
David E. Marshburn, DO
Assistant Professor of Surgery/Ophthalmology
Michael J. Martelli, DO
Associate Professor of Family Medicine
Katherine A. Martin, DO
Assistant Professor of Family Medicine
202
Timothy B. Martin, DO
Assistant Professor of Family Medicine
Kathryn Martinazzi, PharmD
Assistant Professor of Pharmacy Practice
Robert V. Mason, DVM, MS
Associate Professor of Veterinary Medicine
James D. Matiko, MD
Associate Professor of Surgery/Orthopedics
Karol K. Matsune, PharmD
Assistant Professor of Pharmacy Practice
H. Preston Matthews, DO
Assistant Professor of Family Medicine
Robert J. Maurer, DO
Associate Professor of Pediatrics
C. L. McArthur III, MD, MBA
Associate Professor of Family Medicine/
Emergency Medicine
Melissa McCourt, BS, RPh
Assistant Professor of Pharmacy Practice
Shari F. McDaniel, BS, RPh
Assistant Professor of Pharmacy Practice
Edward P. McDermott, DO
Assistant Professor of Surgery/Orthopedics
Sharon S. McGarrity, DO
Assistant Professor of Family Medicine
Maj. Thomas A. McGerty, DO
Assistant Professor of Pediatrics
William H. McGhee, MD
Professor of Family Medicine/Psychiatry
Paul McHugh, DO
Assistant Professor of Family Medicine
Kelly L. McKerahan, DO
Assistant Professor of Family Medicine
Ronald L. McKibben, PharmD
Assistant Professor of Pharmacy Practice
Cori A. McMahon, PA-C, MSEd
Assistant Professor of Physician Assistant
Education
Matthew J. McMahon, DO
Assistant Professor of Internal Medicine/
Cardiology
John M. Medeiros, PhD, PT
Assistant Professor of Surgery/Orthopedics
Luz Patricia Medina, MD
Assistant Professor of Physician Assistant
Education
Fred Meister, PharmD
Assistant Professor of Pharmacy Practice
James J. Mendola, DO
Professor of Surgery/Otorhinolaryngology
Max Mener, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Norman S. Merchant, MD
Associate Professor of Obstetrics/Gynecology
Clifford D. Merkel, MD
Associate Professor of Surgery/Orthopedics
Donna Merrigan, PharmD
Assistant Professor of Pharmacy Practice
Frank J. Metzger, DO
Professor of Internal Medicine
Barry S. Meyer, DO
Assistant Professor of Internal Medicine
Wafa F. Michael, MD
Assistant Professor of Internal Medicine/
Pathology
Constantine A. Michas, MD, MPH
Assistant Professor of Surgery
Alexander Miller, MD
Assistant Professor of Family Medicine/
Dermatology
Howard G. Milstein, MD
Assistant Professor of Family Practice/
Dermatology
John S. Missanelli, DO
Professor of Obstetrics/Gynecology
203
Gary S. Mono, DO
Assistant Professor of Surgery
Louis H. Monty, MD
Assistant Professor of Family Medicine/
Psychiatry
Robert L. Moody, DO
Assistant Professor of Family Medicine
Sylvia Moore, PharmD
Assistant Professor of Pharmacy Practice
Cheryl L. Morell, MD
Assistant Professor of Pediatrics
Candis Morello, PharmD
Assistant Professor of Pharmacy Practice
Cynthia Moreno, DO
Instructor of Osteopathic Manipulative Medicine
Jorge L. Moreno, DO
Assistant Professor of Osteopathic Manipulative
Medicine
James A. Morrow, DO
Assistant Professor of Family Medicine
Glynnis M. Morton, MD
Assistant Professor of Obstetrics/Gynecology
Bassam Mouazzen, MD
Assistant Professor of Internal Medicine
Angela K. Moultrie-Lizana, DO
Assistant Professor of Family Medicine
M. Kenneth Mudge, MB, ChB
Professor of Surgery/Orthopedics
Sharon K. Muenchow, MD
Assistant Professor of Surgery/Pediatrics
Moses T. Mukai Jr., DO
Assistant Professor of Obstetrics/Gynecology
Pramod Multani, MD
Assistant Professor of Internal Medicine/
Cardiology
Debra Foreman Munsell, PA-C
Associate Professor of Physician Assistant
Education
Wadsworth H. Murad, DO
Assistant Professor of Family Medicine/
Psychiatry
Vellore G. Muraligopal, MD
Associate Professor of Pediatrics
John Lamont Murdoch, MD
Professor of Internal Medicine
Ronald E. Nagata Jr, PharmD
Assistant Professor of Pharmacy Practice
Mohan S. Nair, MD
Associate Professor of Family Medicine/
Psychiatry
G. Nalinajith Nanayakkara, MD
Assistant Professor of Obstetrics/Gynecology
Christopher Nee, PharmD, MBA
Assistant Professor of Pharmacy Practice
J. Michael Nelson, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Robert G. Nelson, MD
Assistant Professor of Physician Assistant
Education
William E. Newsome, MD
Associate Professor of Internal Medicine
Anh Ngoc Nguyen, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Brigitte Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Dana Huong Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Khiem Thanh Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Lan-Phuong Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Nhut M. Nguyen, BSc, RPh
Assistant Professor of Pharmacy Practice
204
Phong K. Nguyen, MD
Assistant Professor of Physician Assistant
Education
Phuong Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Thi Nguyen, BS
Assistant Professor of Pharmacy Practice
Trang T. Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Trinh T. Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Tuan Duc Nguyen, BS, RPh
Assistant Professor of Pharmacy Practice
Tuyen Ngoc Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Karen J. Nichols, DO
Associate Professor of Internal Medicine
Peter J. Niciforos, MD
Assistant Professor of Family Medicine
Reid A. Nishikawa, PharmD
Assistant Professor of Pharmacy Practice
Andre M. Noe, MD
Assistant Professor of Physician Assistant
Education
James W. Norcross, DO
Assistant Professor of Family Medicine
Robert E. Norcross, MD
Associate Professor of Surgery
Jeffrey C. Northup, DO
Associate Professor of Obstetrics/Gynecology
William H. Nuesse, MD
Assistant Professor of Family Medicine
Chinyere N. Obasi, MD
Instructor of Surgery/Neurosurgery
Zaida Olivia Obeso, MD
Associate Professor of Family Medicine
Udoh O. Obioha, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Cynthia Odegard, PharmD
Assistant Professor of Pharmacy Practice
So-Jeong Oh, PharmD
Assistant Professor of Pharmacy Practice
Ikechukwu Ohiaeri, MD
Assistant Professor of Family Medicine/
Psychiatry
Joseph L. Olivarez, PA-C
Instructor of Physician Assistant Education
Terrence Olivier, PharmD
Assistant Professor of Pharmacy Practice
Daniel Olson, DO
Assistant Professor of Family Medicine
Robert W. Olson, DO
Assistant Professor of Internal Medicine/
Cardiology
Edward Onuma, MD
Assistant Professor of Internal Medicine/
Gastroenterology
Stephen Eric Osburn, MD
Assistant Professor of Pediatrics
Mark P. Owens, MD
Associate Professor of Surgery
Edward E. Packer, DO
Associate Professor of Pediatrics
Jeffrey Packer, DO
Assistant Professor of Internal Medicine/
Nephrology
James A. Padova, MD
Assistant Professor of Internal Medicine
Joseph T. Palermo Jr., DO
Associate Professor of Internal Medicine
Shi-Hui Pan, PharmD, MS
Assistant Professor of Pharmacy Practice
205
George C. Parides, DO
Assistant Professor of Internal Medicine/
Pulmonary Diseases
Heran Angela Park, MD
Assistant Professor of Pediatrics
Samuel Kyung Uk Park, MD
Assistant Professor of Family Medicine
Dennis R. Parker, DO
Assistant Professor of Family Medicine
Richard A. Parker, DO
Assistant Professor of Family Medicine/Sports
Medicine
David M. Parrack, DO
Assistant Professor of Surgery/Urology
Anjana Patel, PharmD
Assistant Professor of Pharmacy Practice
Neemish N. Patel, PharmD
Assistant Professor of Pharmacy Practice
Michael Pavlovich, PharmD
Assistant Professor of Pharmacy Practice
Daniel D. Pearce, DO
Assistant Professor of Family Medicine
David J. Peck, DO
Assistant Professor of Family Medicine
Lydia Percy, PharmD
Assistant Professor of Pharmacy Practice
Luis Jesus Mejia Perez, MD
Assistant Professor of Physician Assistant
Education
Robert G. Peterson, MD
Assistant Professor of Family Medicine
Warren A. Peterson, DO
Assistant Professor of Family Medicine/
Dermatology
Sara D. Petry, MD
Assistant Professor of Family Medicine/
Psychiatry
Beverly Pettit, PharmD
Assistant Professor of Pharmacy Practice
John Pettit, MD
Assistant Professor of Surgery
William J. Pevsner, DO
Assistant Professor of Family Medicine
Anthony Pham, MD
Assistant Professor of Physician Assistant
Education
Thang Pham, MD
Assistant Professor of Physician Assistant
Education
Hai Phan, MD
Assistant Professor of Internal Medicine/
Nephrology
Craig M. Phelps, DO
Associate Professor of Family Medicine/Sports
Medicine
Mitchel E. Phillips, DO, MS
Assistant Professor of Family Medicine
Wendell B. Phillips, DO
Assistant Professor of Family Medicine
John R. Piconi, MD
Assistant Professor of Surgery/Urology
Allyn M. Pierce, DO
Associate Professor of Obstetrics/Gynecology
Harry A. Pierce, DO
Associate Professor of Internal Medicine
Remy A. Piibe, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Ronald E. Pinkerton, MD
Professor of Family Medicine
Lynne B. Pirie, DO
Assistant Professor of Family Medicine/Sports
Medicine
Richard T. Pitts, DO
Associate Professor of Family Medicine/
Emergency Medicine
M. Jay Porcelli, DO, MS
Professor of Family Medicine
206
Gregson J. Porteous, DO
Assistant Professor of Surgery/Anesthesiology
Stuart Brent Porter, DO
Assistant Professor of Family Medicine
Larry Potts, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Michael A. Pousti, MD
Assistant Professor of Surgery/Plastic and
Reconstructive
Michael J. Powell, DO
Assistant Professor of Internal Medicine/
Rheumatology
Vance M. Powell, DO
Assistant Professor of Obstetrics/Gynecology
Na’Imah D. Powell-Williams, MD
Assistant Professor of Physician Assistant
Education
Venu Prabaker, MD
Associate Professor of Internal Medicine
Arudi L. Prabhakar, MD
Assistant Professor of Surgery
William J. Previte, DO
Assistant Professor of Surgery/
Orthopedics/Sports Medicine
Todd O. Primack, DO
Assistant Professor of Surgery/Anesthesiology
Charles Edward Pritchard Jr., DO
Assistant Professor of Pediatrics
Andrew S. Pumerantz, DO
Assistant Professor of Internal Medicine
Mark Purnell, MD
Assistant Professor of Surgery/Orthopedics
Paul A. Pyka, DO
Associate Professor of Obstetrics/Gynecology
John F. Quinn, MD
Assistant Professor of Family Medicine
Robert Quint, PharmD
Assistant Professor of Pharmacy Practice
David C. Rabinowitz, DO
Professor of Internal Medicine/Pulmonary
Medicine
Richard L. Ragle, DO
Assistant Professor of Family Medicine
Stephen R. Rakower, MD
Associate Professor of Surgery
Laura T. Rampil, DO
Assistant Professor of Family Medicine
John F. Randolph, MD
Associate Professor of Family Medicine
Lawrence D. Raphael, MD
Associate Professor of Internal Medicine
Hugo F. Rauld, MD
Assistant Professor of Obstetrics & Gynecology
Niren A. Raval, DO
Assistant Professor of Family Medicine
Simon Reyhanabad, MD
Assistant Professor of Physician Assistant
Education
Carl A. Recine, MD
Assistant Professor of Internal Medicine/
Radiology
Joe W. Redd, DO
Assistant Professor of Family Medicine
Linda Reynolds, PharmD
Assistant Professor of Pharmacy Practice
David E. Rhodes, MD
Assistant Professor of Family Medicine
Terence P. Rhone, DO
Assistant Professor of Internal Medicine
E. Lee Rice, DO
Professor of Family Medicine/Sports Medicine
Robin (Rob) L. Richardson, DO
Assistant Professor of Family Medicine
Joel S. Richmon, MD
Assistant Professor of Internal Medicine/
Neurology
207
Ronald D. Richmond, MD
Assistant Professor of Physician Assistant
Education
Jerome B. Riebman, MD
Associate Professor of Surgery
Jeffrey D. Ries, DO
Associate Professor of Internal Medicine/
Neurology
Donna Rios, BS, PA-C, RN
Instructor of Physician Assistant Education
Albert Rizos, PharmD
Assistant Professor of Pharmacy Practice
Andrea A. Roberson, DO
Assistant Professor of Family Medicine
Natalie Roberts, DO
Assistant Professor of Internal Medicine
Ward A. Robidart, PA-C
Instructor of Physician Assistant Education
Mark I. Robinson, MD
Assistant Professor of Internal Medicine/
Pulmonology
Zenia Robinson, PA-C
Assistant Professor of Physician Assistant
Education
Robert Robitaille, DO
Assistant Professor of Family Medicine
Tari L. Roche, DO
Assistant Professor of Family Medicine
Arturo Rodrigues, PA-C
Instructor of Physician Assistant Education
Jose L. Rodriguez, MD
Professor of Surgery
Jose L. Rodriguez, MD
Assistant Professor of Surgery
Michael J. Rodriguez, MD
Professor of Surgery
Michael L. Rohrenback, DO
Assistant Professor of Family Medicine
Lorenzo Romney, DO
Assistant Professor of Family Medicine
Andrew J. Rooks, MD
Professor of Family Medicine/Psychiatry
Marc R. Rose, MD
Assistant Professor of Surgery/Ophthalmology
Michael R. Rose, MD
Assistant Professor of Surgery/Ophthalmology
Mark E. Rosen, DO
Assistant Professor of Family
Medicine/Osteopathic Manipulative Medicine
Alan S. Rosenthal, DO
Professor of Internal Medicine
Melvyn B. Ross, MD
Assistant Professor of Internal Medicine/
Cardiology
Phyllis M. Ross, PA-C
Instructor of Physician Assistant Education
Timothy J. Roth, DO
Assistant Professor of Family Medicine
Horst R. Rudrich, DO
Assistant Professor of Family Medicine
Michael Rudolph, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Michael N. Rutman, DO
Assistant Professor of Internal Medicine
David M. Ryan, DO
Assistant Professor of Family Medicine
Thomas K. Ryu, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Shida Saam, DO
Assistant Professor of Family Medicine
Lovina Sabnani, DO
Assistant Professor of Surgery/Ophthalmology
Suresh Sabnani, DO
Assistant Professor of Family Medicine
208
Mazin Q. Sabri, MD
Assistant Professor of Surgery/Orthopedics
Michael Sachs, DO
Assistant Professor of Internal Medicine
Steven Sackrin, MD
Assistant Professor of Internal Medicine
Gurbinder S. Sadana, MD
Assistant Professor of Internal Medicine
Richard I. Sakai, PharmD
Assistant Professor of Pharmacy Practice
Conrad Salinas, MD
Associate Professor of Family Medicine/
Emergency Medicine
Christopher James Sando, PharmD
Assistant Professor of Pharmacy Practice
David Saperia, MD
Assistant Professor of Physician Assistant
Education
David J. Saperstein, DO
Professor of Internal Medicine/Radiology
Phisit Saphyakhajon, MD
Assistant Professor of Pediatrics
Jan O. Sarkin, MD
Associate Professor of Surgery
Arthur Saroughian, PharmD
Assistant Professor of Pharmacy Practice
Marcus Sasiadek, PharmD
Assistant Professor of Pharmacy Practice
Sampat S. Saste, MD
Assistant Professor of Internal Medicine
John D. Schaeffer, DO
Assistant Professor of Internal Medicine/
Neurology
Irving Schaffner, MD
Assistant Professor of Family Medicine
Hershel Schaftel, PharmD
Assistant Professor of Pharmacy Practice
Ivan B. Schatz, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Kenneth Schell, PharmD
Assistant Professor of Pharmacy Practice
Kenneth C.J. Scherbarth, DO
Assistant Professor of Family Medicine
Clifton S. Schermerhorn, MD
Associate Professor of Family Medicine/
Psychiatry
Mark D. Schneider, DO
Associate Professor of Family Medicine
Robert B. Schorr, DO
Assistant Professor of Pediatrics/Psychiatry
Andrew O. Schreiber, MD
Assistant Professor of Internal Medicine/
Neurology
Saul E. Schreiber, DO
Associate Professor of Family Medicine/
Dermatology
Robert C. Schreiman, MD
Assistant Professor of Family Medicine
Lawrence Schuyler, DO
Assistant Professor of Family Medicine
Ernest R. Schwab, PhD
Adjunct Associate Professor of Physical
Therapy Education
Paul E. Schwartz, MD
Associate Professor of Physician Assistant
Education
Charles Schwengel, DO
Assistant Professor of Family Medicine
James H. Scott, DO
Assistant Professor of Family Medicine
Kendall G. Scott, MD
Associate Professor of Physician Assistant
Education
David Searle, RPh
Assistant Professor of Pharmacy Practice
209
Martin T. Sechrist, DO
Associate Professor of Family Medicine
David Sellen, DMin
Associate Professor of Health Professions
Education
Avedik Semerjian, MD
Assistant Professor of Internal Medicine/
Nephrology
Manohar R. Senra, MD
Assistant Professor of Internal Medicine
Michael A. Sequeira, MD
Assistant Professor of Physician Assistant
Education
Stephen R. Severance, MD
Associate Professor of Internal Medicine/
Gastroenterology
Conrado C. Sevilla III, MD
Assistant Professor of Family Medicine/
Psychiatry
Baljit K. Sharma, MD
Assistant Professor of Surgery/Cardiothoracic
Robert C. Sharp, MD
Professor of Pediatrics
Frank P. Sheridan, MD
Assistant Professor of Internal Medicine/
Pathology
Julie Ann Sherman, DO, MS
Assistant Professor of Family Medicine
Christan T. Shimoda, DO
Associate Professor of Family Medicine
Kathleen Jane Shimoda, RN
Assistant Professor of Family Medicine
Amy Y. Shin, PharmD
Assistant Professor of Pharmacy Practice
Dong-Soo Shin, MD
Assistant Professor of Surgery
William L. Shoemaker, DO
Assistant Professor of Surgery/Orthopedics
Henrietta (Hennie) B. Sholars, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Victoria Lynn Shook, MD
Assistant Professor of Physician Assistant
Education
Randall G. Shue, DO
Assistant Professor of Family Medicine
Annie Shugarman, PA-C
Assistant Professor of Physician Assistant
Education
Javed Siddiqi, MD
Assistant Professor of Surgery/Neurosurgery
John L. Sie, PharmD
Assistant Professor of Pharmacy Practice
Antonio R. Silva, MD
Assistant Professor of Surgery/Oncology
Arnold Sin, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Ravinder P. Singh, MD
Assistant Professor of Family
Medicine/Psychiatry
Tejinder Singh, MD
Assistant Professor of Internal Medicine
Prem Singla, MD
Associate Professor of Family Medicine
C. Paul Sinkhorn, MD
Assistant Professor of Obstetrics/Gynecology
Harry B. Skinner, MD, PhD
Professor of Physician Assistant Education
Daniel M. Skotte Sr., DO
Assistant Professor of Family Medicine
Carl M. Smith, MD
Professor of Internal Medicine/Radiology
Carl W. Smith, MD
Assistant Professor of Surgery/Orthopedics
210
David E. Smith, MD
Professor of Family Medicine/Addiction
Medicine
Keith U. Smith, DO
Assistant Professor of Internal Medicine/
Anesthesiology
Kenneth R. Smith, DO
Assistant Professor of Family Medicine
Larry D. Smith, DO
Assistant Professor of Internal Medicine
Wyatt S. Smith, DO
Assistant Professor of Internal Medicine/
Hematology & Oncology
Dorian D. Snyder, MD
Assistant Professor of Family
Medicine/Emergency Medicine
Mehrzad M. Soleimani, DO
Assistant Professor of Family Medicine
Hamilton M. Solomon, PhD
Adjunct Assistant Professor of Physical Therapy
Education
Joseph K. Song, MD
Assistant Professor of Internal
Medicine/Cardiology
Willes Wolfe Sonnefield, MA, PT
Adjunct Assistant Professor of Physical Therapy
Education
Andrei Soran, MS
Assistant Professor of Health Professions
Education
Rose M. Sparks, BS, RPh
Assistant Professor of Pharmacy Practice
Trang Huong Sparks, PA-C, BS
Instructor of Physician Assistant Education
Michelle Spencer, PharmD
Assistant Professor of Pharmacy Practice
Richard Spini, PharmD
Assistant Professor of Pharmacy Practice
Yemelyan L. Spivak, MD
Assistant Professor of Surgery
Ruth Stanhiser, MD
Assistant Professor of Family Medicine
Robert A. Steedman, MD
Associate Professor of Surgery
Lisa M. Steffensen-Gambrath, DO
Assistant Professor of Family Medicine
Paul J. Steier, DO
Assistant Professor of Family Medicine
Michael A. Steingard, DO
Assistant Professor of Surgery/ Orthopedics
Paul M. Steingard, DO
Professor of Family Medicine/Sports Medicine
Scott A. Steingard, DO
Assistant Professor of Family Medicine
John C. Steinmann, DO
Associate Professor of Surgery/Orthopedics
Craig Stephen Stern, PharmD, MBA
Assistant Professor of Pharmacy Practice
Gloria J. Stevens, MD
Assistant Professor of Family
Medicine/Dermatology
Kristine Stille, PharmD
Assistant Professor of Pharmacy Practice
William C. Stonecipher, DO
Associate Professor of Family Medicine
John Strathakis, DO
Assistant Professor of Family Medicine/
Dermatology
Howard N. Straub, DO
Professor of Surgery/Ophthalmology
Josef Strazynski, DO
Associate Professor of Family Medicine
Gregory D. Strebel, DO
Assistant Professor of Family Medicine
Angela Y. Su, PharmD
Assistant Professor of Pharmacy Practice
211
Michael W. Sue, MD
Associate Professor of Physician Assistant
Education
Jocelyn L. Sumcad, MD
Assistant Professor of Physician Assistant
Education
Gretchen Swanson, DPT
Adjunct Associate Professor of Physical
Therapy Education
Jamie L. Switzer, DO
Assistant Professor of Family Medicine
Brian M. Swope, DO
Assistant Professor of Pediatrics
Khanh Ta-Le, PharmD
Assistant Professor of Pharmacy Practice
Joanne A. Tabata, PharmD
Assistant Professor of Pharmacy Practice
Parvis Taherpour, MD
Assistant Professor of Family Medicine
Benjamin C. Tam, MD
Assistant Professor of Surgery/Orthopedics
Andrew Tan, PharmD
Assistant Professor of Pharmacy Practice
Bruce L.M. Tannenbaum, MD
Professor of Family Medicine/Psychiatry
Mark A. Tapscott, DO
Assistant Professor of Surgery/Proctology
Collin Teguh, DO
Assistant Professor of Family Medicine
Edward Tessier, BA
Adjunct Instructor of Health Professions
Education
Stephen W. Thacker, DO
Associate Professor of Family Medicine
Jack (John) L. Thomas, DO
Assistant Professor of Family Medicine
Larry L. Thomas, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Julie G. Thompson-Dobkin, DO
Assistant Professor of Internal Medicine/
Neurology
Nguyen Thong, MD
Assistant Professor of Internal Medicine
Rama K.P. Thumati, MD
Assistant Professor of Internal Medicine/
Cardiology
Brian L. Tiep, MD
Assistant Professor of Family Medicine/
Pulmonary Rehabilitation
Jeffrey Tipton, DO, MPH
Assistant Professor of Family Medicine/Public
Health
Shohreh Sherrie Todd, RPh
Assistant Professor of Pharmacy Practice
Eric M. Toder, DO
Assistant Professor of Family Medicine
Gilbert J. Toffol, DO
Assistant Professor of Internal
Medicine/Neurology
Ernest Victor Tom, PharmD
Assistant Professor of Pharmacy Practice
Helen Tonnu, PharmD
Assistant Professor of Pharmacy Practice
Michael E.L. Toole, PharmD
Assistant Professor of Pharmacy Practice
Cynthia J. Toy, PharmD
Assistant Professor of Pharmacy Practice
Stanley M. Toy Jr, MD
Assistant Professor of Physician Assistant
Education
Bao Cong Tran, MD
Assistant Professor of Internal Medicine
Doug Dung Anh Tran, MD
Associate Professor of Surgery/
Otorhinolaryngology
Ellen T. Tran, PharmD
Assistant Professor of Pharmacy Practice
212
Tanya Tuyen Tran, PharmD
Assistant Professor of Pharmacy Practice
Ingrid E. Trenkle, MD
Assistant Professor of Family Medicine/
Dermatology
Vincent M. Tristan, PA-C
Instructor of Physician Assistant Education
Rohiit R. Trivedi, MD
Assistant Professor of Surgery
Lawrence Troxell, PharmD
Assistant Professor of Pharmacy Practice
William Tsai, DO
Assistant Professor of Family Medicine
Jonathan C. Tsao, DO
Assistant Professor of Family Medicine
Cam Tsaowimonsiri, PharmD
Assistant Professor of Pharmacy Practice
Stephen W. Turay, MD
Assistant Professor of Family Medicine
Alfred L. Turner, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Sheri R. Tysch, DO
Assistant Professor of Pediatrics
Paul M. Umof, MD
Assistant Professor of Family Medicine/
Emergency Medicine & Occupational Medicine
Khushro B. Unwalla, MD
Assistant Professor of Family Medicine/
Psychiatry
Sukhdev Uppal, MD
Assistant Professor of Pediatrics
Geraldine N. Urse, DO
Assistant Professor of Family Medicine
Daryoosh Valamanesh, MD
Assistant Professor of Internal Medicine
Fidel Valenzuela, PharmD
Assistant Professor of Pharmacy Practice
Guillermo J. Valenzuela, MD
Professor of Obstetrics/Gynecology
James P. Veen, DO
Assistant Professor of Physician Assistant
Education
Roger Vielbig, MD
Assistant Professor of Internal Medicine/
Cardiology
Rafael Villarosa, MD
Assistant Professor of Internal Medicine
William Vineyard, PharmD
Assistant Professor of Pharmacy Practice
Norman E. Vinn, DO
Associate Professor of Family Medicine
Michael P. Vitullo, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Jacqueline H. Vo, PharmD
Assistant Professor of Pharmacy Practice
Monique Ngoc Vo, PharmD
Assistant Professor of Pharmacy Practice
Lee E. Vranna, MD
Assistant Professor of Family Medicine/Physical
Medicine and Rehabilitation
Helga B. Wachholz, PharmD
Assistant Professor of Pharmacy Practice
Barton H. Wachs, MD
Assistant Professor of Surgery/Urology
Jeffrey A. Wachs, DO
Assistant Professor of Family Medicine
Ralph D. Wade, DO
Assistant Professor of Family Medicine
Paul E. Wakim, DO
Assistant Professor of Surgery/
Orthopedics/Sports Medicine
Wendy Waldman, RPh
Assistant Professor of Pharmacy Practice
213
Bryan D. Walls, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Jiangnan Wang, MD
Assistant Professor of Internal Medicine
James P. Warren, MD
Assistant Professor of Internal Medicine/
Radiology
Harry C. Watters, DO
Assistant Professor of Obstetrics/Gynecology
Gerald Weingarden, DO
Assistant Professor of Family Medicine/
Dermatology
Elliot Weinstein, MD
Assistant Professor of Pediatrics
Frederick R. Weiss, MD
Assistant Professor of Internal Medicine
Michael Weiss, DO
Associate Professor of Pediatrics
Jill Weissman, PharmD
Assistant Professor of Pharmacy Practice
Erna L. Wells, MPA, RN, CCM
Professor of Physician Assistant Education
Randall M. West, DO
Assistant Professor of Family Medicine
H. Eric Westman, DO
Associate Professor of Surgery/
Otorhinolaryngology
Frederick E. White, DO
Assistant Professor of Internal Medicine/
Radiology
Peter J. White, MD
Assistant Professor of Surgery/Anesthesiology
Rosamond C. White, PhD, RN, NP
Assistant Professor of Physician Assistant
Education
Janette M. Wilcox, DO
Assistant Professor of Family Medicine
Imani S. Williams, PA-C
Assistant Professor of Physician Assistant
Education
Kenneth L. Williams Jr., DO
Assistant Professor of Family Medicine
Brian C. Wilson, MD
Assistant Professor of Internal Medicine/
Radiology
Rochelle L. Wilson, DO
Assistant Professor of Family Medicine
Tien T. Kiat Winarko, PharmD
Assistant Professor of Pharmacy Practice
Deborah Kay Winberry, PA-C
Instructor of Physician Assistant Education
Heidi A. Winkler, MD
Assistant Professor of Pediatrics
Lydia A. Winter, PharmD
Assistant Professor of Pharmacy Practice
Barry R. Wiss, DO
Assistant Professor of Internal Medicine/
Gastroenterology
Albert A. Witte, DO
Professor of Internal Medicine/Cardiology
Sandy Witzling, MD
Associate Professor of Surgery
Laurie M. Woll, DO
Associate Professor of Family Medicine/
Dermatology
Brian Wong, PharmD
Assistant Professor of Pharmacy Practice
Donna Wong, DO
Assistant Professor of Family Medicine
Elaine Wong, PharmD
Assistant Professor of Pharmacy Practice
Noreen T. Wong, PharmD
Assistant Professor of Pharmacy Practice
Dora Woo, PharmD
Assistant Professor of Pharmacy Practice
214
Thomas A. Woodbury, DO
Assistant Professor of Family Medicine
Clarence Woods Jr., MD
Associate Professor of Physician Assistant
Education
Sandor J. Woren, DO
Associate Professor of Family Medicine/
Emergency Medicine
R. Bruce Worth, MD
Assistant Professor of Family Medicine
George D. Wright, MD
Assistant Professor of Family Medicine
Craig J. Wronski, DO
Assistant Professor of Family Medicine/
Psychiatry
Brett Wyrick, DO
Associate Professor of Surgery
Anthony P. Yang, MD
Assistant Professor of Surgery/Orthopedics
Lovelle M. Yano, PharmD
Assistant Professor of Pharmacy Practice
Cecile Yared, PharmD
Assistant Professor of Pharmacy Practice
Ralph A. Yates, DO
Assistant Professor of Family Medicine
Florence Yee, PharmD
Assistant Professor of Pharmacy Practice
Jeffrey C. Young, DO
Assistant Professor of Family Medicine
David Yousef, PharmD
Assistant Professor of Pharmacy Practice
John Yuen, PharmD
Assistant Professor of Pharmacy Practice
Ray M. Yutani, DO, PharmD, MS
Assistant Professor of Pharmacy Practice
Mehrnaz Zahiri, PharmD
Assistant Professor of Pharmacy Practice
Joseph A. Zammuto, DO
Assistant Professor of Family Medicine
Stephen W. Zecher, MPT
Adjunct Assistant Professor of Physical Therapy
Education
Robert Zelman, DO
Assistant Professor of Internal Medicine/
Cardiology
Nicole Zimmerman, PhD
Instructor of Health Professions Education
Sheldon S. Zinberg, MD
Professor of Internal Medicine
Phillip C. Zinni III, DO
Assistant Professor of Family Medicine
Robert D. Zipser, MD
Associate Professor of Internal Medicine/
Gastroenterology
John P. Zopfi, DO
Assistant Professor of Surgery/Trauma Surgery
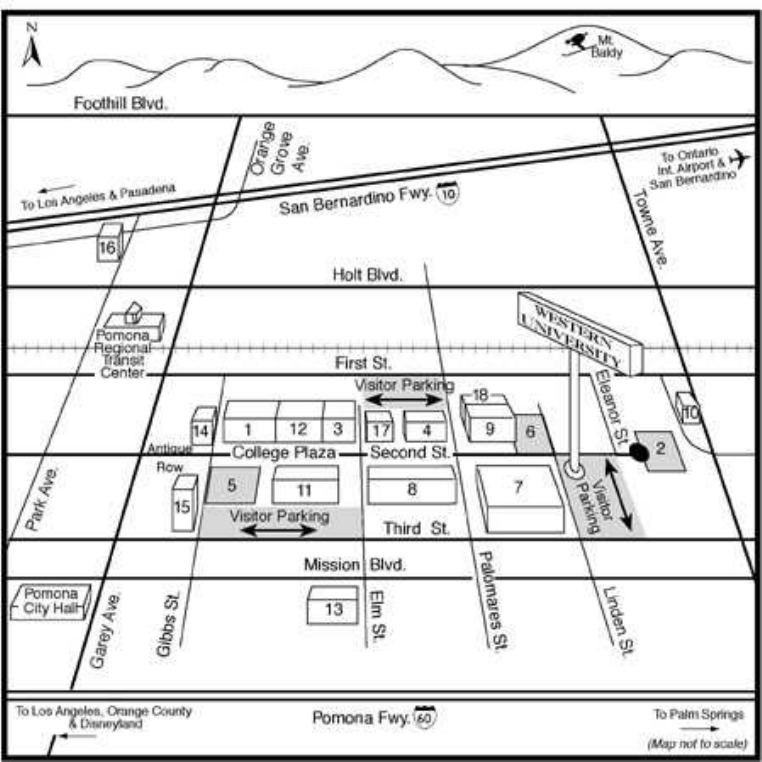
215
1. ALUMNI CENTER
2. UNIVERSITY PARK
3. BOOTH CENTER
4. BUSINESS CENTER
5. CENTENNIAL PARK
6. FOUNDERS PARK
7. HEALTH PROFESSIONS CENTER
8. HEALTH SCIENCES CENTER
9. VETERINARY SCIENCES CENTER
(future site)
10. MAINTENANCE/AUXILIARY SERVICES
FACILITY
11. STUDENT SERVICES CENTER
12. UNIVERSITY ADMINISTRATION
CENTER
13. WESTERN UNIVERSITY MEDICAL
CENTER
14. WESTERN UNIVERSITY CAMPUS
GOURMET/STUDENT LOUNGE
15. HEALTH SCIENCES LIBRARY AND
LEARNING RESOURCES CENTER
16. WESTERN UNIVERSITY VETERINARY
MEDICAL CENTER (future site)
17. INLAND EMPIRE CREDIT UNION
18. VETERINARY SCIENCES (future site)
How to Reach Western University
The University's main campus is located about 35 miles east of Los Angeles, in the City of Pomona. Ontario
International Airport is six miles east of the University and Los Angeles International Airport is located 60
miles west.
1
Western University of Health Sciences
Department of Physical Therapy Education
Doctor of Physical Therapy Program
ABOUT THE DOCTOR OF PHYSICAL THERAPY PROGRAM
The DPT program is designed to provide students a didactic augmentation of physical therapy
knowledge and skills that has occurred over the past 5-7 years and to provide additional experience in
the clinical setting prior to graduation. The courses included in this curriculum reflect and are consistent
with the patient/client management model described in the Guide to Physical Therapist Practice and the
curricular content for professional education in A Normative Model of Physical Therapist Professional
Education: Version 2000.
The reason for moving toward a DPT degree is based on the new and expanding role of the physical
therapist. Changes are occurring in the field and the future role will include practice in primary care and
direct access. As such, physical therapists will be expected to perform medical screening, have a
stronger knowledge base of the medical and clinical sciences, and be able to perform higher level
problem-solving and clinical decision-making.
In addition to the first professional doctoral degree, the program offers the DPT degree to licensed
physical therapists. The clinician who holds a bachelor or master’s degree in physical therapy may enter
the DPT program as a student with advanced standing to complete requirements for the DPT degree.
The required courses will depend upon the student’s previous academic coursework and
clinical/professional experiences. The student with advanced standing may take many courses online
with 2-3 weekends on campus. The mission and program goals are the same for the first professional
and advanced standing students. Policies related to admissions, registration, and tuition and fees are
different for students entering with advanced standing. A description of the policies for students with
advanced standing is provided separately at the end of the section on the first professional DPT program.
All other policies are the same for both first professional DPT students and those admitted to the DPT
program with advanced standing.
MISSION OF THE PROGRAM
In keeping with the University's mission, the mission of the Physical Therapy program is to educate
competent, caring, culturally sensitive, reflective practitioners who will:
• participate as members of the health care team to provide high quality care to patients;
• as life-long learners, acquire, analyze, synthesize and apply knowledge in new settings;
• contribute to the verification of physical therapy evaluation and intervention techniques, and
discover new, more effective methods of patient care;
• be leaders in providing health care service and education to promote health and fitness of
community members; and
• play important roles in developing health policy and appropriate standards for physical therapy
practice.
PROGRAM GOALS
The graduate of the DPT program will be a mature individual whose professional education is based
on a foundation of the requisite preparation in the biological, behavioral and social sciences, and
humanities. The graduate will have the necessary knowledge, skills and attitudes to function as a
clinician generalist; will have an appreciation for the value of all aspects of the research process; and
will be a responsible member of the community and the profession. Upon completion of the educational
program in physical therapy, the graduate will be able to:

2
• Have an understanding of the osteopathic philosophy with its emphasis on caring for, and
appreciation of the patient as a whole person;
• Demonstrate respect for all individuals;
• Practice physical therapy as an entry-level clinician generalist by assuming responsibility for the
components of that role;
• Communicate with peers, colleagues, patients, clients, family members and the community-at-
large in a style that is commensurate with their level of understanding;
• Appreciate the place of research in the advancement of physical therapy;
• Serve as a role model for healthy behaviors in both the clinical setting and community;
• Participate in the community as a representative of the physical therapy profession, as an
advocate for the patient or client in a health care environment, and as a concerned citizen;
• Continue lifelong learning through continuing education, specialization and participation in
professional organizations; and
• Establish priorities in order to maintain a balance between personal and professional life.
DESCRIPTION OF THE DPT PROGRAM
The curriculum for the Doctor of Physical Therapy (DPT) Program will prepare the graduate to be a
PT generalist. The curriculum consists of 9 trimesters, each having a particular emphasis.
Curriculum Design
The DPT program is three years in length. Didactic education, which includes classroom and PT
laboratories to practice procedures on classmates, is followed by clinical education assignments in a
wide variety of clinical settings. Year I consists of two 15-week trimesters and one 18-week trimester
which includes a 3-week clinical experience.
Year II consists of three 15-week trimesters, including one 12-week clinical practicum.
Year III consists of a 15-week trimester followed by an 18-week and 12-week trimester. Didactic
courses are presented in the first trimester and the first 6 weeks of the second trimester during this year.
The student completes the remaining 24 weeks of the program in two 12-week clinical practica.
Students will present formally their research proposals to the faculty and the PT community during
the second year. They have the option to carryout their proposed research during the second year and
first part of the third years. Research studies must be completed prior to the final clinical practica.
Selective topics courses will be offered during the first six weeks of the eighth trimester, or students may
opt to complete an additional six week clinical at that time.
DPT students will complete their education in August, but may participate in the University-wide
graduation in the prior May/June. State licensure examinations are now computerized and can be taken
following completion of the program. The faculty includes scholars, researchers, administrators and
clinicians from the professions of physical therapy, psychology, education, osteopathy, medicine and the
basic sciences. All faculty are committed to the preparation of the Doctor of Physical Therapy
professional who will be well versed in all aspects of physical therapy and dedicated to their profession
and to the patients they serve.
LIBRARY SERVICES
The library is open Monday-Friday from 7 am to 11 pm and Saturday and Sunday from 8 am to 10
pm. The library is closed for all University holidays. Western University’s library resources can be
accessed on the Internet at: http://www.westernu.edu. It is assumed that students will access the Internet
sites for some resources and perform database searches for class assignments or research projects. Full
text articles are not always available via the World Wide Web, therefore, students are expected to utilize
traditional library services for research assignments, whether in the student’s community or near their
home.
3
BOOKSTORE
Western University Bookstore hours are 7:30 am to 5 pm Monday-Friday for ordering or purchasing
textbooks. Software and media resources are also available. Textbooks may be ordered by phone and
mailed directly to student’s home using a credit card.
TECHNICAL GUIDELINES FOR ADMISSION AND MATRICULATION
A candidate for admission to the DPT program must have the use of certain sensory and motor
functions to permit them to carry out the activities described in the sections that follow. Graduation from
the program signifies that the individual is prepared for entry into clinical practice. Therefore, it follows
that graduates must have the knowledge and skills needed to function in a broad variety of clinical
situations and to render a wide spectrum of physical therapy evaluation and treatment techniques. The
candidate and student must be able to consistently, quickly, and accurately integrate all information
received by whatever sense(s) are employed. Also, they must have the intellectual ability to learn,
integrate, analyze, and synthesize data.
Examples of essential functions of a physical therapist include, but are not limited to:
a. Use appropriate verbal, non-verbal, and written communication with patients, families, and
others.
b. Determine the physical therapy needs of any patient with potential movement dysfunction.
c. Safely, reliably, and efficiently perform appropriate physical therapy procedures used to assess
the function of the movement system.
d. Perform treatment procedures in a manner that is appropriate to the patient's status and desired
goals.
A candidate for DPT ordinarily must have abilities and skills of five varieties including (1)
observation; (2) communication; (3) motor; (4) intellectual, conceptual, integrative and quantitative; and
(5) behavioral and social. Where technological assistance is available in the program, it may be
permitted for disabilities in certain areas. Under all circumstances, a candidate should be able to perform
all physical therapist functions at entry-level competency in a reasonably independent, timely manner.
1. Observation: Candidates and students ordinarily must have sufficient vision to be able to
observe demonstrations and laboratory exercises. They must be able to observe a client
accurately at a distance and close at hand.
2. Communication: Candidates and students ordinarily must be able to communicate with clients
and colleagues. They should be able to hear, but if technological compensation is available, it
may be permitted for some people with disabilities in this area. Candidates and students must be
able to read, write, and communicate verbally in English.
3. Motor: Candidates and students ordinarily should have sufficient motor function such that they
are able to execute movements reasonably required to provide assessment and physical therapy
treatment procedures to clients.
Examples of reasonable required assessment procedures include, but are not limited to:
a. Functional abilities
b. Pain
c. Gait
d. Strength
e. Joint motion and stability
f. Balance
g. Movement patterns
Examples of reasonably required treatment procedures include:
a. Balance training
b. Exercise techniques
4
c. Gait training
d. Activities of daily living training and functional activities
These actions require coordination of both gross and fine muscular movements, equilibrium and
functional use of the senses of touch and vision. The role of the physical therapist often requires
upright posture with sufficient upper and lower extremity strength, as well as overall body
strength; therefore, individuals with significant limitations in these areas would be unlikely to
succeed.
4. Intellectual, Conceptual, Integrative, and Quantitative Abilities: These abilities include
measurement, calculation, reasoning, analysis, and synthesis. Problem solving, the critical
intellectual skill demanded of a physical therapist, requires all of these intellectual abilities. In
addition, candidates and students should be able to comprehend three-dimensional relationships
and understand the spatial relationships of structures.
5. Behavioral and Social Abilities: Candidates and students must possess the emotional health
required for full utilization of the intellectual abilities, the exercise of good judgment, the prompt
completion of all responsibilities attendant to the assessment and care of clients, and the
development of mature, sensitive, and effective relationships with clients. Candidates and
students must be able to tolerate physically taxing workloads, adapt to changing environments,
display flexibility, and learn to function in the face of uncertainties inherent in the clinical
problems of many clients. Compassion, integrity, concern for others, interpersonal skills,
interest, and motivation are all personal qualities to be assessed during the admissions and
educational processes.
The DPT program, along with all other programs at Western University of Health Sciences, shares a
commitment to develop creative ways of opening the DPT curriculum to competitive, qualified disabled
individuals. In doing so, however, the DPT program must maintain the integrity of its curriculum and
preserve those elements deemed essential to educating candidates to become effective physical
therapists.
ADMISSIONS POLICIES AND PROCEDURES
Western University will accept applications for admission from all qualified candidates. Western
University is committed to admitting competitive, qualified disabled individuals. For technical
guidelines, please see above.
Application Requirements
The applicant must have earned a BA or BS degree from a regionally accredited college or university
by the time he/she matriculates in the DPT program. The minimum acceptable grade point average in
the baccalaureate degree program is 2.5 on a 4.0 scale.
The DPT program is looking for students who come from a broad, liberal arts background with the
baccalaureate degree being obtained in any field of study other than physical therapy. A high degree of
intellectual curiosity and accomplishment along with excellent verbal and written communication skills
need to be evident in the applicant. The graduate of Western University will be able to problem-solve in
clinical practice and will also be able to communicate appropriately with the client/patient and other
health care providers about the client/patient care plan.
1. Prerequisite Courses
English Composition - 1 course (minimum of 3 semester units or 4 quarter units)
Psychology - 2 courses, must be out of the Psychology Department (minimum of 3 semester
units each or 4 quarter units each)
Statistics - 1 course, only statistics courses that are cross listed in math, statistics or biometry will
be accepted (minimum of 3 semester units or 4 quarter units)
Human Anatomy - 1 course of lecture and lab (minimum of 4 semester units or 6 quarter units)
5
Human Physiology - 1 course of lecture and lab (minimum of 4 semester units or 6 quarter units)
General Chemistry - a full course sequence of lecture and lab (minimum of 8 semester units or
12 quarter units)
Physics - a full course sequence of lecture and lab – emphasis on light, heat, sound, and
electricity (minimum of 8 semester units or 12 quarter units)
Anatomy and Physiology must be taken out of the Anatomy, Physiology, A&P, Biology or Zoology
departments. The Anatomy and Physiology must be "human." Combined Anatomy and Physiology
courses will be considered only if a combined course sequence is completed.
In addition the following courses are recommended to enhance success in the program:
Oral communication skills
Computer literacy
General biology
Microbiology
Kinesiology/biomechanics
Exercise Physiology
Nutrition
Human/Child Development
Additional Psychology courses
Grades of "C" or better are required in each prerequisite course. A grade of "C-" in any prerequisite
course is not acceptable. No prerequisite coursework may be taken on a pass/no pass or credit/no credit
basis. For courses completed in California, all science prerequisites must be University of California
(UC) or California State University (CSU) transferable.
Three prerequisite courses may be in progress at the time of application during the spring, summer or
fall semester or quarter. Please submit official transcripts directly to the Admissions office upon
completion of coursework in progress. Final transcripts and/or final grades (including degree
verification) for all coursework in progress must be received prior to registration date of July 1st.
2. Science GPA includes all science courses and must be a minimum of 2.5.
3. Graduate Record Examination (GRE) Score Report
Official GRE Score Report must be mailed directly to Western University from Educational
Testing Service (ETS).
4. Clinical Experience
Credit will be given for up to 500 hours and extra credit will be awarded for different types of
settings, provided that at least 100 hours is spent in each setting. Types of settings may include
acute hospital, outpatient, rehabilitation, pediatric, and home health. Preference will be given to
applicants who have experience at more than one setting. All experience must be in physical
therapy and under the direct supervision of a PT to meet these minimal requirements.
5. Recommendations
Three satisfactory recommendations (forms provided) are required as part of the admissions
application. We require one academic recommendation and two from physical therapists.
Application Procedures and Deadlines
The DPT program has an August matriculation date. The application postmark deadline is February
1, 2003. The Department of Physical Therapy will make admissions decisions on a rolling basis. They
will review applications, conduct interviews and make admissions decisions throughout the admissions
cycle. We encourage students with complete application packets to apply early. Applicants who cannot
attend and wish to reapply for the following year will be considered with the new applicant pool.
6
To request an information brochure and/or an application, contact the admissions office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 469-5541
In addition to submitting an application, the applicant must submit a non-refundable application fee
of $60, three letters of reference, academic/professional record form, work experience form, a written
personal statement, and official transcripts from all colleges attended. After receipt of the packet, the
Admissions Office will evaluate the applicant's transcripts to ascertain the prerequisite and overall grade
point average.
Applicants who wish to use coursework completed outside of the United States must submit their
transcripts for evaluation to World Education Services, Josef Silny and Associates, Educational
Credential Evaluators, Inc., or International Education Research Foundation, Inc. A course-by-course
evaluation is required and all coursework must be designated as undergraduate, graduate or professional.
Western University will only honor evaluations from the above services. The evaluation must be
included with the application packet.
The Admissions Committee reserves the right to select potential candidates for personal interviews.
These interviews are designed to allow the applicant to learn more about Western University's DPT
program as well as allow the Admissions Committee to learn about the applicant. The interview process
is conducted at various times throughout the admissions cycle.
Decisions of the Admissions Committee regarding the admission of applicants to the Doctor of
Physical Therapy program are final.
ADMISSIONS POLICIES AND PROCEDURES – ADVANCED STANDING
Admission to the DPT program for students with advanced standing is through the Admissions
Office. Students may apply for the fall, spring or summer trimesters. Western University is committed
to admitting competitive, qualified individuals with disabilities. For technical guidelines, see the section
under the DPT program (above).
Application Requirements
The applicant must have graduated from a Commission on Accreditation in Physical Therapy
Education (CAPTE) accredited physical therapy program and/or be licensed to practice in the United
States. Foreign-prepared therapists must be licensed to practice physical therapy in the State of
California. Additional requirements include:
• A minimum of 1 year (2000 hours) clinical experience in any setting.
• Letters of recommendation (3 with at least one from a PT supervisor/colleague; remaining letters
may be from non-PT health care professionals).
• Writing sample including why the applicant desires to pursue this degree and what he/she will
plan to accomplish with it; i.e., a statement of purpose.
• Computer access and skills.
Students who do not meet the admissions requirements may petition the Admissions Committee for
special consideration.
7
Application Procedures and Deadlines
Students are advised to submit application materials as early as possible prior to the trimester in
which they wish to begin their program of studies. The deadline for application materials is no later
than 45 days prior to the first day of classes for each trimester.
To request an informational brochure and/or an application, contact the Admissions Office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 469-5335
In addition to submitting an application, the applicant must submit a non-refundable application fee
of $60 and official transcripts from all undergraduate and graduate institutions attended.
Portfolio Review
Upon acceptance to the program, as part of the application process, students will be asked to submit a
portfolio of past education and experiences related to physical therapy. This information will be
reviewed by the faculty advisor and may be analyzed by a credentialing agency. There is a separate fee
if the credentialing agency is used to analyze the portfolio. Decisions regarding required courses will be
based on review of the portfolio. Some courses may be waived if sufficient evidence is provided to
demonstrate fulfillment of competencies and program outcomes in specified areas.
Readmission
Students with advanced standing who have not been enrolled for more than one calendar year must
submit a new application form and fee, unless other arrangements have been made at the time of
withdrawal/leave from the program. The application will be assessed according to the current
admissions policies, and students will be required to fulfill all program requirements in place at the time
of readmission.
For more information, including registration requirements, tuition, fees and additional academic
requirements and policies, see the section entitled Description of the DPT Program for Students with
Advanced Standing (below).
REGISTRATION
DPT students are required to register as directed by the Registrar. Failure to register may be grounds
for dismissal. Assessed tuition and fees and all prior debts must be paid in full on or before the
registration deadline each academic year. Matriculation is subject to satisfactory completion of all
academic requirements and payment of all outstanding debts to the University. Prior to registration, the
receipt of final transcripts for all college coursework, a physical examination, and immunizations as
outlined on the physical examination form, are additional requirements for incoming students.
Attendance at Orientation Day is mandatory for incoming first-year students.
Continuing Education and Non-Degree Students
An applicant holding a bachelor’s or master’s degree in Physical Therapy and licenses to practice in
the United States, who does not wish to pursue the DPT degree at Western University at the present
time, but who wishes to engage in graduate study for personal development, continuing education, or
other professional development needs, may consider enrollment as a non-degree student. A limited
number of applicants may enroll as non-degree students each trimester. The usual admission and
registration procedures must be followed. Admission as a non-degree student does not assure
acceptance as a degree candidate, should the student at a later time wish to change enrollment status. An
8
unlimited number of credit hours may be completed while in non-degree status. Should the student wish
to change enrollment status, the usual admissions procedures must be followed. Up to nine units of
previous coursework taken as a non-degree student at Western University can be transferred into the
DPT degree program. Questions about transferring from non-degree to degree status should be directed
to the Chairperson, Department of Physical Therapy Education.
TUITION AND FEES
The tuition for the DPT program has yet to be determined for the 2003-2004 Academic Year. We
project the annual tuition to be between $25,000 and $26,000. The tuition amount will be published in
the 2003-2004 University Catalog. Other fees/payments are as follow:
*$1,250 Tuition Deposit for incoming students
(Payable two weeks after acceptance)
**$500 Enrollment Deposit
(Students returning from leave of absence only - Due by May 15)
$ TBD Total Tuition Annual
$40 Student Body Fee, covers student council, social activities, public relations.
*Upon matriculation, the entire $1,250 is applied toward the total tuition.
**For accepted candidates who are students returning from leave of absence, a $500 enrollment
deposit is due May 15 prior to enrollment. The deposit is nonrefundable and credited toward tuition
upon enrollment.
Tuition and fees are subject to change without notice upon approval by the Board of Trustees. All the
above-listed fees are mandatory for each student and are nonrefundable.
Other Fees and Expenses
$500 Required and Recommended Texts
$10 (per day) Late Registration Fee
$40 Lost Locker Key
$10 Lost ID Badge
$5 (each) Copy of Official Transcript
$10 (each) Copy of Official Transcript Faxed
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
ACADEMIC REQUIREMENTS
Academic Advisement Policy
Students will be assigned a faculty advisor upon matriculation. Advisement by faculty should be
viewed by the student as a part of the academic process. If either the student or faculty member does not
find the relationship helpful, either is free to seek a change. This request should be made to the
Department Chair.
It is the student’s responsibility to meet periodically with his/her advisor. A student on probation
must meet with his/her faculty advisor at least once a month.
Standards of Academic Performance
Good academic standing implies that a student maintains a minimum GPA of 2.70 (B-) or higher.
All grading and evaluation is based on the student's ability to attain the competencies within the
objectives outlined for each area of study.

9
A student whose performance falls below the minimum acceptable standard(s) for any area of study
will be notified of such deficiency by the instructor of the course and Department Chairperson as soon
as evidence of such substandard performance is available.
Grade Scale/Grade Points/Class Ranking
The following academic standards and grading scale applies to students enrolled in the Physical
Therapy Program:
Percentage Letter Grade Grade Points
93 - 100 A Excellent 4.0
90 - 92 A- Excellent 3.7
87 - 89 B+ Good 3.3
83 - 86 B Good 3.0
80 - 82 B- Good 2.7
77 - 79 *C+ Passing, but below required overall GPA 2.3
73 - 76 *C Passing, but below required overall GPA 2.0
Below 73 U Unsatisfactory 0
NCr No Credit 0
Cr Credit 0
I Incomplete 0
M Missing 0
Au Audit 0
W Withdrawal 0
* A "C" or "C+" grade in and of itself is a passing grade. However, a "C" or "C+" grade is below the
required overall grade point average of 2.7. If the number of "C's" and "C+'s" totals an amount to bring
the student's GPA to below 2.7, then the performance, based on professional expectations, is considered
unsatisfactory. In addition to maintaining a minimum 2.7 GPA, no more than 24 units can be with a C
or C+ grade.
Clinical Practica Grades:
Cr Satisfactory Performance/Completion
of clinical practicum assignment
NCr Unsatisfactory Performance/Completion
of clinical practicum assignment
The class ranking is computed at the end of each graded trimester, based upon overall GPA.
Incomplete
An Incomplete grade (“I”) will be assigned only to students whose professional commitments and/or
personal responsibilities prevent him or her from completing the requirements for the course. A student
may remove an Incomplete by completing course requirements by the end of the following academic
trimester. Should extenuating circumstances arise, the student may petition for a one-trimester
extension to complete the course work. Arrangements for the Incomplete and its removal must be
approved by the instructor prior to the end of the trimester in which the original Incomplete grade was
assigned. Grade changes must be certified by the instructor prior to the end of the trimester following
the original grade assignment, except in the instance of an approved extension to the next trimester.
10
Credit Hours
Courses are rated at one credit hour for each 15 hours of lecture or 30 hours of laboratory and/or
practice sessions. Credit hours of 1.0 will be assigned for each week of Clinical Practica experience
(i.e., Clinical Practicum I is three weeks and receives 3 credits). A cumulative grade point average will
be calculated and posted on the transcript. Class ranking is also computed and will appear on the
transcript at the student's request only. Class ranking is also available upon request in the Registrar's
Office.
The grade point average will be calculated at the end of each trimester and if a course is repeated,
only the last grade earned enters into the computation of the grade point average, but the original grade
remains on the student's transcript.
Official grades are turned in to the Registrar from the Dean of Allied Health Professions, at which
time the online student records system, BanWeb, is updated. Official grade reports and unofficial
transcripts will be available throughout the academic year. For more information on how to access the
BanWeb student records system, visit the Registrar’s website at http://www.westernu.edu/registrar.
No course grade will be changed unless the instructor certifies in writing to the Registrar that an error
in computing or recording the grade occurred. If the student believes there is just cause to dispute a
grade for a course, the procedure is as follows:
a. If, following distribution of unofficial transcripts on BanWeb, the student has reason to dispute
the grade, it should be done in writing within five (5) working days to the Department of
Physical Therapy Education Chairperson. Upon written request from the student, the
Department Chairperson shall review the case with the instructor(s) and a decision shall be made
by the course instructor(s) to affirm or modify the grade. Within seven (7) working days the
Department Chairperson shall notify the student in writing of the decision. A copy of the letter
shall be sent to the appropriate faculty member(s). The faculty member(s) has the sole
responsibility to make the official grade change.
b. If the student is not satisfied with the outcome of the grade dispute procedure to the Department
Chairperson, the student may then appeal in writing to the Dean of the College of Allied Health
Professions within five (5) working days. The Dean of the College of Allied Health Professions
shall review the case with the student, Chairperson of the Department of Physical Therapy
Education and the course instructor(s) and a decision shall be made by the course instructor(s) to
affirm or modify the grade. Within seven (7) working days the Dean shall notify the student in
writing of the decision. A copy of the letter shall be sent to the appropriate faculty member(s)
and Chairperson. The faculty member(s) has the sole responsibility to make the official grade
change.
Evaluation
a. General: The program trimesters are designed so that students' work toward achievement of
competencies is measured by written and practical examinations and by evaluations of clinical
performance and professional development. Specific behavioral objectives are defined for each
program component to assist the students and the faculty members in evaluating the degree of
attainment of the objectives throughout the 36-month curriculum.
b. Evaluation Methods: Overall student performance is evaluated during each phase using one or a
combination of the following methods:
1. Written examinations: Written examinations will vary based on the content of the individual
course. A combination of multiple choice, matching, true/false, short answer, essay and
patient problem solving questions are used.
2. Practical or Laboratory Examinations: In selected courses, students will be observed
performing components of physical therapy practice activities on lab exams. They also may
11
be asked to "problem solve" based on a patient database, and in some cases students will be
videotaped for self-evaluation.
3. Student Presentations: Students may be asked to orally present individual or group projects,
patient cases, research papers, etc. These oral presentations may or may not be accompanied
by a written report.
4. Written reports: At various times, students will be evaluated on written reports of assigned
topics, SOAP notes, evaluations, treatment plans and home programs.
5. Clinical Evaluations: Supervising Clinical Instructors are asked to assess the student's level
of attainment of competencies related to selected parameters within the domains of
knowledge, skills and attitudes, and to evaluate the student's overall performance while on
Clinical Practica.
The Clinical Performance Instrument (CPI), which incorporates entry-level physical therapist
clinical performance criteria, is utilized.
Students are responsible for securing their CPI or other evaluation tools from the Center
Coordinator of Clinical Education/Clinical Instructor (CCCE/CI) on each practicum and ensuring
that it is completed and returned to the Director of Clinical Education after each practicum.
CCCE/CI's are encouraged to discuss the student's performance and progress throughout the
clinical assignment and to discuss the final evaluation prior to completion of the practicum. The
CI will indicate whether the Clinical Practicum was a successful experience in accordance with
designated objectives, or was unsuccessful in meeting clinical objectives. While the CI may
recommend success or failure of the Clinical Practicum, the Director of Clinical Education
determines and administers the actual course grade.
c. Grade Reports: Final grade reports are issued at the completion of each trimester and will be
available on BanWeb. Due to the nature of the curriculum, trimester completion dates may not
coincide with traditional grading periods. In some courses when final grades are not available at
grade reporting time, a grade of "M" (Missing) is submitted to the Registrar in lieu of the course
grade. "M" grades are entered on the grade reports and are converted to student achieved grades
at the earliest possible opportunity. An up-to-date summary of student performance is maintained
in the Department Office and is available to each student for review.
d. Review of Examinations: Examinations are graded as soon as possible and are kept on file for
student review. Student performance in clinical courses is monitored closely by the Director of
Clinical Education. Students whose performance in any portion of the curriculum is determined
to be unsatisfactory are notified of such substandard performance as soon as it can be
determined.
Professional Performance
a. Ability-based Assessment: The faculty supports the concept of development of professional
behaviors throughout the program. These behaviors include: (1) commitment to learning; (2)
interpersonal skills; (3) communication skills; (4) effective use of time; (5) use of constructive
feedback; (6) problem solving; (7) professionalism; (8) responsibility; (9) critical thinking; and
(10) stress management.
Professional behavior is vital to the success of each student, the Western University Physical
Therapy program, and the Physical Therapy profession. The process of becoming an effective
physical therapist involves attaining competency in professional knowledge, skill, and behavior.
Thus, the ten generic abilities that exemplify the professional behaviors valued by the physical
therapy profession will be used as a guide throughout this program. To facilitate development of
competency in the generic abilities, the faculty will provide the students opportunities to practice
them and formal and informal feedback throughout the program. The student will be responsible
for ongoing self-assessment and for seeking feedback from faculty and fellow students.
12
Students’ progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behavior and attitudes. At the
completion of each trimester/year of the program, before the student is allowed to progress to the
next trimester/year, the student’s record of achievement is reviewed by the faculty. The quality
of professional behavior expected of Western University DPT graduates is exemplified by the
generic abilities and the three levels of associated behavioral criteria. Satisfactory progress is
demonstrated by exhibiting beginning-level criteria by the end of the first year, developing-level
criteria by the end of the second year, and entry-level criteria by the end of the final clinical
practicum.
The faculty determines if the student has demonstrated the knowledge, skills, and attitudes
necessary to be eligible for progress for the next trimester/year. In special instances, the faculty
may be convened at other than scheduled times to consider cases of unusual circumstances, such
as probationary or dismissal cases.
b. Attendance: Students are expected to attend all scheduled activities and observe the following
policies:
Excused Absences
1. All unanticipated absences due to illness, accident, other unexpected events must be reported
immediately to the department secretary and course instructor.
2. Absences requested for physician/dentist appointments for student or dependents will be
considered excused only if requested in advance of the appointment. Due to the intense
nature of the curriculum, students are encouraged strongly to schedule appointments for days
when classes are not held, evenings, or Saturdays.
3. All anticipated absences for any reason, regardless of length, must have the prior approval by
the Faculty to be considered excused.
4. Students on Clinical Practica are responsible for notifying their supervising CI, CCCE, and
the Director of Clinical Education regarding all absences, whether anticipated or
unanticipated.
Unexcused Absences
1. Any discovered or reported absence for which the Chairperson/Faculty does not have an
explanation will be considered unexcused.
2. Students whose absence is determined to be unexcused will be required to provide an
explanation regarding the circumstances involved. The Chairperson/Faculty will determine
if the absence remains unexcused.
3. Unexcused absences may be sufficient cause for placing a student on professional probation
and continued unexcused absences may be grounds for dismissal from the program.
4. Absences on the first or last day of a module or Clinical Practicum, or on the day before or
after a scheduled break, vacation, or weekend, are considered unexcused unless prior written
approval has been granted. If such an absence is the result of a sudden unavoidable
circumstance, the Department Chairperson should be notified as soon as possible and
provided with an explanation for the absence.
c. Student Examination Policy
1. Students are not to communicate in any way during examinations and are to face the front of
the classroom at all times.
2. During scheduled examination hours, students are highly discouraged from going to the
bathroom, but will be allowed to go one at a time. Student will be required to turn in the
exam and Scantron® sheet as he/she leaves the room.
3. Once a student finishes an exam, the student will turn in the exam and the Scantron® form to
the proctor, and after he/she leaves the examination room, he/she will not be permitted to re-
enter the room until the exam is declared over.
13
4. All students' belongings, i.e., notebooks, calculators, and headsets, etc., will be kept in front
of the room.
5. Questions will be answered at the discretion of the proctor during the examination period.
Students should be permitted to point out typographical or other errors present in the
examination to the proctor.
6. Alternate seating shall be utilized for all examinations unless precluded by space availability.
7. Violations of these examination policies or of Standards of Professional Conduct will be
brought before the Student Conduct Committee.
Student Academic Progress Committee
a. The Student Academic Progress Committee of the College of Allied Health Professions is
comprised of Department Chairs, the Dean of Student Affairs/Registrar and elected faculty
members.
b. Each year, the Student Academic Progress Committee shall review as needed the academic
achievements and the performance of all students. The names and grades of students in
academic difficulty shall be made available to the Student Academic Progress Committee by the
Department Chair.
c. After reviewing a student’s achievement and performance records, the Student Academic
Progress Committee may recommend to the Dean of Allied Health Professions any of the
following courses of action for a student: Promotion, probation, remediation, dismissal from the
University, psychological and educational assessment and recommendation, or no action.
d. The Student Academic Progress Committee also has the responsibility of recommending to the
Faculty as a whole the awarding of the degree of Doctor of Physical Therapy upon satisfactory
completion of all requirements for graduation as stated in the University Catalogue.
e. All recommendations of the Student Academic Progress Committee shall be made in writing to
the Dean of Allied Health Professions, who will make a final decision and inform the student in
writing.
Promotion
Promotion is defined as progression from one academic year to the next.
a. A student will be recommended to the Dean of the College of Allied Health Professions for
promotion by the Student Academic Progress Committee.
b. A student may not be recommended for progression from one academic year to the next with any
outstanding grades of “I” or “U” on his/her academic record or with a yearly grade point average
of less than 2.7.
c. When considering a student for promotion, professional, ethical, and personal conduct may also
be taken into consideration.
d. A student will be promoted provided that all legal and financial requirements of the University as
stated in the Catalogue have been satisfied.
Graduation
A student will be recommended for the degree of Doctor of Physical Therapy provided he/she:
a. Has satisfactorily completed a minimum of three years education at the University in the DPT
curriculum, except if the student has been granted advanced standing in the program.
b. Is not on probation and has completed all prescribed academic and clinical education
requirements with a cumulative grade point average of at least 2.7 and has no outstanding grade
of “I” or “U,” or “NCr” in a required course.
c. Has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined
previously.
14
d. Has complied with all the legal and financial requirements of the University as stated in the
Catalogue.
e. Unless special permission has been granted by the President of the University, all students must
attend in person and participate in the Commencement program at which time the degree is
conferred. If the President grants special permission to be excused from graduation, the graduate
may be required to present himself or herself to the Provost or appropriate Dean at a later date in
order to take the required oath (if relevant) to receive his or her diploma.
Academic Warning
The student who demonstrates unacceptable performance in any unit of study during any portion of
the program is notified of such performance by the Instructor of the course, as well as the Department
Chairperson, in writing, as soon as it becomes evident. This constitutes an academic warning.
Continued poor academic performance can lead to academic probation and/or dismissal.
Academic Probation
a. Unsatisfactory or No Credit Course Grades
"U" or “NCr” in any required course constitutes a failing grade, and places the student on
academic probation, requiring that the course be remediated or retaken based upon the
recommendation of the course instructor. A grade of “U” or “NCr” in a required course will
prevent participation in a clinical practicum until the course is successfully remediated and
requires that the Director of Clinical Education (DCE) determine an appropriate clinical
placement.
1. As in all cases in which remediation of a course is required, this requirement may extend the
length of the program beyond 36 months.
2. The highest grade a student may achieve by obtaining a 73 percent or higher score through
remediation of a course is a grade of "C" or “Cr”. The "C" or “Cr” grade achieved by
remediation of a course will be recorded on the official transcript beneath the original course
grade of "U" (Unsatisfactory) or “NCr” (No Credit).
3. Failure to earn a grade of “C" or “Cr” when remediation of a course is attempted will render
the student subject to dismissal from the program.
4. If a student repeats a course the next time that course is offered in the DPT curriculum, the
student will have that new grade for the course recorded on the official transcript beneath the
original course grade of "U" (Unsatisfactory) or “NCr” (No Credit).
5. Failure to earn a grade of "C" or higher or “Cr” on repeating a course of study will render a
student subject to dismissal from the program.
6. A third "U" or “NCr” in required coursework in the program will render a student subject to
dismissal from the program.
b. Trimester/Overall GPA
1. Students must attain a trimester GPA of 2.7 and maintain an overall GPA of 2.7. The
trimester GPA and overall GPA will be calculated at the end of each trimester.
2. A student whose trimester or overall GPA falls below 2.7 must meet with the Department
Chairperson and the DCE. In order to closely monitor clinical performance, the DCE will
determine the subsequent clinical placement.
3. If the trimester or overall GPA falls below 2.7, a student will be placed on academic
probation immediately. Length of academic probation will be determined by the Dean of the
College of Allied Health Professions.
4. If a student attains a trimester GPA below 2.7 in two consecutive trimesters the student will
be subject to dismissal from the program.
15
Remediation
Every effort will be made to give each student ample opportunity to demonstrate competency in each
area of the academic program. However, remediation is to be regarded as a privilege, which must be
earned by a student through an active participation in the educational program as demonstrated by
regular attendance, individual initiative, and utilization of resources available to him or her.
Tutorial Assistance Program
A Tutorial Assistance Program (TAP) has been established at the University to assist students
experiencing academic difficulty. Students will be recommended for this program by a faculty advisor
or professor. The tutors will be chosen from the student body on the recommendation of the faculty of
record for the class.
General Procedures
a. The student may request a tutor by:
1. contacting the course instructor and/or the Department Chairperson,
2. contacting his/her advisor or,
3. going directly to the Learning Enhancement and Academic Development (LEAD) Office.
Student requests will be reviewed by the course instructor and/or the Department Chair. Upon
approval, the student will be deemed eligible for services under TAP. Five hours per course is the
maximum number of hours for which a student may be tutored per week.
b. The course instructor may recommend that the student seek a tutor, based upon a poor
performance on a single exam or poor cumulative score.
c. The student’s advisor may recommend that the student seek a tutor, based upon any knowledge
he or she may have about the student’s academic difficulty. In addition, the advisors will receive
copies of letters from the Chairperson to students having academic difficulty.
d. To initiate tutoring following a recommendation or student request for tutoring, the student
follows these steps:
1. The student obtains from the LEAD Office a list of names of tutors available for the course
in which the student is having problems.
2. The student is assigned a tutor by the LEAD Director from the list of available tutors.
3. Once assigned, the tutor and tutee meet with the course instructor to discuss the student’s
specific problems. The instructor should make some recommendations as to what areas the
tutor should emphasize.
4. The tutor and student arrange mutually agreeable times for the tutoring sessions.
5. The tutor must have the course instructor sign the time sheet before it is turned in to the
LEAD Office.
A student may obtain up to five hours of tutoring per course per week during the module. By
example: A Year I DPT student may be tutored in Physiology and Research I for a total of 10 hours per
week during the trimester. Generally, tutoring begins after a student has received grades at 73 percent or
lower on an exam. The student may continue to be tutored for a course until he/she has obtained a B-
(80%), or higher average grade for the course. As the student moves into trimester III, the student may
qualify for up to 20 hours of tutorial assistance per week (4 courses). Any time a student has received
73 percent or less on an exam, the student, faculty member or student’s faculty advisor may immediately
request tutorial assistance.
Modified Year I DPT Curriculum
The DPT program offers Modified Year I curriculum for students experiencing academic difficulties
or students with disabilities. This modified program is a four-year curriculum in which the first year
standing curriculum is spread over a two-year period. Guidelines for this program include:
16
a. Potential candidates for the Modified Year I DPT Curriculum will be identified by the midway
point of Trimester 1 or 2 after the first midterm examinations.
b. The Modified Curriculum is not an option unless the student manifests serious academic
problems by the midway point of Trimester 1 or 2.
c. Recommendation of individual students for the Modified Curriculum shall be made through the
Dean of the College of Allied Health Professions by recommendations from the Department of
Physical Therapy Education Faculty and the College of Allied Health Professions, Student
Academic Progress Committee.
d. The decision to enter the Modified Curriculum is a onetime student option.
e. At the time the student opts for the Modified Curriculum, the modified curriculum will be based
upon courses in which the student is receiving satisfactory grades by midterm of Trimester 1 or
2. The Modified Curriculum will be outlined for the student, so that Year I of the DPT
curriculum will be taken over two years. As the student enters Year II of the curriculum, it is
expected that the student would attend all classes and clinical assignments as defined in the
standard curriculum.
f. The student's progress will be monitored carefully each trimester by the department chair,
College of Allied Health Professions Student Academic Progress Committee, and the Dean of
the College of Allied Health Professions.
g. Students admitted to this program will pay three consecutive years of tuition and mandatory fees,
and only mandatory fees for the additional year in the curriculum.
Professional Probation
Violations of the Standard of Professional Conduct will be dealt with as described under the General
University Academic Policies and Regulations of this catalogue.
Dismissal
A student may be subject to dismissal from the program for substandard academic or professional
performance, as follows:
a. A second grade of "U" or “NCr” in the same required course;
b. A third grade of "U" or “NCr” in required courses in the program;
c. More than 24 units of C or C+ grades in didactic coursework.
d. Unacceptable performance on more than one of the clinical practica;
e. Lack of professional or personal attributes considered appropriate for continuance in the program
and profession;
f. Any event that could result either in academic or professional probation for a student currently
on academic or professional probation;
g. Violation of the terms of probation as stated in a letter at the time the student is placed on
probation.
Exemption from Individual Course
Students with advanced work or degrees in a particular subject formally may petition the instructor
and the Department Chairperson for credit for an individual course. The petition must include the
reasons for the request and all necessary documentation and must be submitted by the end of the first
week of the course. The student must comply with the attendance policy until notification that
exemption has been granted by the Dean, based upon recommendation of the Department Chairperson.
The instructor, before recommending exemption, may require acceptable performance on an
examination. The instructor, in consultation with the Department Chairperson, may suggest other
alternative or additional criteria for determining exemption.
17
Confidentiality of Medical Records and Health History Information
All data gathered about patients and their illnesses, including all items within patients’ medical
histories are privileged information.
a. Students should not discuss patients’ records in a manner or a situation that would reveal any
information about these patients or their records to persons not involved in their health care.
b. Charts or contents, e.g., lab reports, etc., are not to be removed from the hospital or clinical
setting.
Use of Physical Therapy Equipment and Laboratories
The DPTE policy for use of the PT equipment in the PT Skills Laboratories is as follows: No one is
to use the PT equipment except DPT students who have received education and have had practice on the
equipment in the laboratory. These DPT students must be checked out by a faculty member as being
competent to use the equipment. DPT students using the equipment should be doing so in conjunction
with a class they are taking, or in preparation for a clinical practicum, or to conduct a clinical research
project. If equipment is used for a research project, the DPT faculty advisor will be responsible to check
out student competency in using the equipment.
Physical Therapy skills and research labs may be used after regular class hours, with permission of
the Department Chair. Use of these facilities must be scheduled with the Department Chair five (5)
working days in advance of the intended date of use.
CURRICULUM ORGANIZATION
The DPT curriculum is continually evaluated to assure the best educational experience and outcomes.
With this consideration, the following is an outline of curriculum organization.
Year I
Course number Semester Hours
Trimester I - 15 Weeks
PT 5000 Psychosocial Aspects of Health Care 2.5
PT 5040 Histology and Tissue Healing 2
PT 5070 Patient Care Skills 3
PT 5075 Physical Agents & Procedures 3
PT 5100 Physiology/Pathophysiology 5
PT 5220 Principles of Teaching and Learning 2
PT 5230 Medical Screening and Systems Review I 2
Total 19.5
Trimester II - 15 Weeks
PT 5060 Human Morphology & Movement I 7.5
PT 5065 Human Morphology & Movement II 7.5
PT 5130 Research Methodology in Health Care 3
PT 5141 Clinical Education & Professional Development I 1
Total 19
Trimester III - 18 Weeks
PT 5015 Physical Therapy in the Health Care System 3
PT 5120 Human Life Sequences 2
PT 5140 Research in Evidence Based Practice 2
PT 5200 Differential Diagnosis of Musculoskeletal
18
Disorders 3
PT 5210 Evaluation and Treatment of Lower Quarter
Musculoskeletal Dysfunction 6.5
PT 5235 Medical Screening and Systems Review II 2
PT 7010 Clinical Education I 3
Total 21.5
Year II
Trimester IV -15 Weeks
PT 5142 Clinical Education and Professional Development II 1
PT 5205 Evaluation and Treatment of Upper Quarter
Musculoskeletal Dysfunction 6
PT 6020 Principles of Electrotherapeutic Evaluation
& Treatment 3
PT 6030 Physiology of Exercise 4
PT 6040 Evaluation & Treatment of the
Cardiopulmonary System 4
PT 6220 Application of Research to Clinical Practice 0.5
PT 8100 Pharmacology for Physical Therapists 3
Total 21.5
Trimester V - 15 Weeks
PT 8110 Structural Imaging in Physical Therapy
Diagnosis 2
PT 7020 Clinical Education II 12
Total 14
Trimester VI - 15 Weeks
PT 6000 Neuroanatomy 4
PT 6005 Neurophysiology 4
PT 6010 Evaluation & Treatment of Neurological
Disorders I 4
PT 6015 Differential Diagnosis of Neurological
Disorders 4
PT 6075 Prevention and Management of Problems in
the Pediatric Patient 3
Total 19
Year III
Trimester VII - 15 Weeks
PT 5143 Clinical Education & Professional Development III 1
PT 6011 Evaluation & Treatment of Neurological
Disorders II 4
PT 6045 Differential Diagnosis of the Integumentary
System/Wound Care 3
PT 6050 Principles of Administration and Management 3
PT 6060 Prosthetics, Orthotics and Gait 3
PT 6070 Prevention and Management of Problems in
19
the Aging Adult 3
PT 6220 Application of Research to Clinical Practice 0.5
PT 8400 Research Investigation (optional) 0-2
Total 17.5-19.5
Trimester VIII - 18 Weeks
PT 7030 Clinical Internship I 12
PT 8500 Selected Topics 4-6
Total 16-18
Trimester IX - 12 Weeks
PT 7040 Clinical Internship II 12
Total 12
Graduation - Total Semester Hours 162
DESCRIPTION OF THE DPT PROGRAM FOR STUDENTS WITH ADVANCED
STANDING
See Admissions Requirements (above) for Admission with Advanced Standing information.
Curriculum Design and Organization
The DPT program for students with advanced standing is designed for the adult learner. Adult
learners are students who have life roles other than student, which make demands on their time and
resources, such as being a parent and/or an employee. The design uses contemporary educational and
instructional learning theories that emphasize outcome behaviors as the desired goal, rather than time on
task. Individualized instructional strategies that include mediated learning as well as classroom
instruction are also used. The program features several non-traditional instructional strategies.
Advanced students may chose to take web-based courses or enroll in the same on-campus classes
offered to the first professional degree students. The instructional modality that is most evident in the
curriculum for advanced students is web-based distance learning. Students are prepared to understand
the characteristics of the adult learner role and are shown how to acquire adequate computer literacy
during an introductory course entitled “Strategies for Successful Learning” (PT 6600). They are
expected to be online and engaged in learning activities from the first day of the first trimester. The
DPT web site is designed to provide the learner with all of the direction that is needed to be successful in
each course, including learning objectives, content, learning activities, evaluation methods and grading
criteria.
An on-campus orientation is required prior to starting the first course of the program. The PT
6600 Strategies for Successful Learning course is completed at that time. One or more on-campus
seminar weekends are held each trimester, depending on the individual courses enrolled in during that
trimester. At least two weekend seminar classes are held for each course. Weekend classes may be held
Friday afternoon through Saturday, all day Saturday only, or Saturday morning through Sunday
afternoon. Seminar sessions may include lecture, testing, skills training, student presentations, and
student group work. The seminar periods are conducted as problem-solving sessions where the learner
has the opportunity to demonstrate knowledge and skill that have been acquired through self-directed
study and obtain feedback and stimulation from instructors and fellow students.
Cooperative learning is emphasized throughout the program. Students may be assigned to groups to
work on applying their collective problem-solving skills toward the resolution of case-based scenarios.
The online courses require student participation in asynchronous discussions. Students are required to
20
submit original comments based on relevant research as part of evidence-based practice. In addition,
they are expected to respond to other comments from students and the instructor(s).
REGISTRATION POLICIES AND PROCEDURES
New Students in Advanced Standing
New students admitted with advanced standing are notified by mail of their admission status. This
notification will include a list of courses available during the next trimester and the necessary
registration materials. Completed registration materials and fees must be submitted through the mail or
in person, prior to the first week of classes. Classes may fill quickly; therefore, the student is
encouraged to register early.
Continuing Students in Advanced Standing
Continuing students will receive registration information and materials by mail prior to the beginning
of the trimester. Should this information not arrive for any reason, it is the student’s responsibility to
contact the Office of Student Affairs for the appropriate materials. Completed registration materials and
fees may be submitted to the Registrar through the mail or in person, prior to the first week of classes.
Classes may fill quickly; therefore, the student is encouraged to register early.
Late Registration
Students must follow the registration procedures and timelines printed in the Class Schedule provided
at the beginning of each regular trimester. The days of registration and late registration are listed in that
document. Appropriate fees for late registration will be assessed.
Add/Drop and Withdrawal from Courses
In order to add or drop a class, the student must obtain a Change of Registration form from the
chairperson, complete and submit it prior to the end of the second week of classes of that trimester.
Withdrawal from a course (not the program) requires completion and submission of the appropriate
withdrawal from obtained from the chairperson. Please note that this will not result in an “incomplete”
(I) grade.
TUITION AND FEES
Tuition and Fees for the 2002-2003 academic year (subject to change) for students admitted with
Advanced Standing are as follow:
Tuition
$300 cost per credit unit
Other Fees
$60 application fee
All fees are mandatory for each student and are non-refundable. Obligation for payment in full of
tuition and fees is due upon matriculation.
COMPUTER REQUIREMENTS
The following is a list of minimum computer equipment necessary for the Web-based program:
• At least 500 MHz Intel Celeron, Pentium III or AMD K6-2 Processor
• Windows 98, 2000 or Windows XP operating system
• 12.1” Active Matrix Display (15” recommended)
• 8 MB RAM video (16 MB RAM preferred)
21
• 192 MB RAM system memory (256 MB RAM or higher recommended)
• 10 GB free space on hard drive (20 GB preferred)
• 1.44 MB, 3.5” Internal or External floppy drive
• CD-ROM (CD-RW (read and write) recommended)
• Microsoft Office 2000 (Word, PowerPoint, Excel, and Outlook); Internet Explorer 5.0, Norton
Antivirus, Windows Media Player 6.4 or higher
• 56K modem
• 16-bit sound card and speakers
• Internet Service Provider (ISP) and e-mail account (dedicated telephone line recommended)
• Printer
ACADEMIC REQUIREMENTS
Unless otherwise stipulated in this section, all other Academic Requirements of the DPT
program must also be met (see above).
Course Load
A student with advanced standing at Western University must enroll in at least eight units per term to
be considered full-time. It is expected that students with advanced standing in the DPT program will be
enrolled less than full-time, i.e., no more than two courses per trimester.
Student’s Rights and Responsibilities
It is the responsibility of the student to be familiar with the contents of the catalog and to observe all
policies and procedures relative to the completion of requirements for the graduate degree that were in
effect at the time of initial enrollment in the DPT program.
A student may opt to complete the program of study and degree requirements described at the time of
his or her graduation, provided all revised policies of the later catalog are followed. Students are
required to keep the Registrar informed of their current address and telephone number. Forms for this
purpose are available in the Student Affairs office.
Reasonable Academic Progress
All students with advanced standing are expected to make reasonable progress each year toward the
degree objective. Students with advanced standing are considered to be making reasonable academic
progress when they maintain an overall GPA of at least 2.7 and complete 4-6 units during the calendar
year. Students must complete the graduation requirements within the time limits described under Time
Limits (below).
Seminar Weekend Attendance for Web-based Courses
Attendance is mandatory for all seminars. Dates of the weekend seminar program are published and
distributed at the beginning of each trimester. Students who do not comply with this policy must make
an immediate appointment with the DPTE chairperson to avoid termination of their enrollment for the
trimester in question. The DPTE chairperson will forward this information to the department faculty.
The department faculty will then make a recommendation to the Student Academic Progress Committee
(SAPC). SAPC will review the student’s performance and make a recommendation to the dean of the
College of Allied Health Professions who will make a determination about the student’s continued
enrollment.
22
CURRICULUM ORGANIZATION FOR STUDENTS WITH ADVANCED STANDING
Students must meet all the requirements for the DPT program as listed in the previous section. Credit
will be given for previous coursework. It is anticipated that students will be required to complete at
least the following courses, unless their portfolio shows evidence of mastery of course content:
PT 5130 Research Methodology in Health Care 3 units
PT 5140 Research in Evidence-based Practice 2 units
PT 6220 Application of Research to Clinical Practice 1 unit
PT 6600 Strategies for Successful Learning 0 unit
PT 8100 Pharmacology for the Physical Therapist 3 units
PT 8110 Structural Imaging in Physical Therapy Diagnosis 2 units
PT 8120 Medical Screening & Systems Review 4 units
PT 8130 Advanced Differential Diagnosis I 2 units
PT 8135 Advanced Differential Diagnosis II 2 units
Total: 19 units
Additional Courses
PT 8200 Professional Leadership and Ethics 2 units
PT 8210 Documentation and Health Care Financing 2 units
PT 8230 Wellness & Prevention/Community Education 3 units
These additional courses have been specifically designed for students with advanced standing who
may not have met a minimal level of proficiency in these areas prior to admission to the program.
Proficiency level will be determined through a review of the applicant’s portfolio. Students may opt to
take equivalent course offered in the first professional DPT degree program to fulfill content not
obtained through previous academic programs, continuing education, or clinical experience.
Residency Requirements
A minimum of 12 units must be completed with course work offered by the DPT program at Western
University.
Time Limits
The DPT program for students with advanced standing may be completed within 2 ½ years of part-
time study. All requirements for the degree must be fulfilled within four years form the date of initial
registration. Extensions of this time limit may be granted through petition to the faculty.
COURSE DESCRIPTIONS AND CREDIT HOURS
All courses are awarded letter grades, except when indicated otherwise.
PT 5000 Psychosocial Aspects of Health Care (2.5 credit hours)
(Formerly PT 500)
Prerequisite: Acceptance to program. Introduction to the psychological and sociological effects of
acute, chronic, terminal, traumatic and congenital medical problems on the patient, family and therapist;
communication skills including interviews, verbal and non-verbal communication. Includes discussion
of ethical issues in health care.
23
PT 5015 Physical Therapy in the Health Care System (3 credit hours)
(Formerly PT 501 and 502 or PT 5010 and 5020)
Prerequisite: Acceptance to program. Emphasis on concepts presented in the Guide to Physical
Therapist Practice and the APTA Code of Ethics. Includes a broad perspective of world, national and
state health care factors, legal aspects of physical therapy practice, and documentation and
reimbursement in a variety of practice settings.
PT 5040 Histology and Tissue Healing (2 credit hours)
Prerequisite: Acceptance to the program. Includes tissue types and composition of organ systems;
structure and function of cells and cellular components related to each body system; collagen formation
and deposition. Discusses process of tissue repair, remodeling and regeneration for each body system
including cellular responses to injury, inflammatory response, and time frame for healing.
PT 5060 Human Morphology and Movement I (7.5 credit hours)
(Formerly PT 503, 505 and 509 or PT 5030, 5050 and 5080)
Prerequisite: Acceptance to program. This is a fully integrated course on human anatomy and
kinesiology. Includes introduction to theoretical and functional principles of human structure, with
emphasis on clinical relevance and applications. Topics include kinetics, kinematics, manual muscle
testing and evaluation of gait with emphasis on normal function. Techniques covered include
goniometry, surface palpation and posture evaluation. Critical review of pertinent published literature
will be utilized and will include electromyographic studies of normal and pathologic movement.
Anatomical topics in the first semester include musculoskeletal, vascular, and nervous structures of the
trunk, abdomen, and posterior neck, with emphasis on the form and function of the hypaxial and epaxial
regions. The structures and function of the upper quadrant and thoracic viscera will also be covered.
Human cadaver dissection by all participants is a requirement. Pathology is addressed as an aid in
identification of major concepts and to introduce clinical relevance. Lecture and Laboratory.
PT 5065 Human Morphology and Movement II (7.5 credit hours)
(Formerly PT 504, 506 and 509 or PT 5035, 5055 and 5080)
Prerequisite: PT 5060. Continuation of PT 5060. Introduction to theoretical principles and clinical
application of kinetics and kinematics of the extremity joints and muscles of the lower quadrant with
emphasis on normal function. Also covers head, neck and abdominal viscera, including cardiovascular,
pulmonary, nervous, digestive, excretory and reproductive systems as relevant. Introduces thee
structures of the autonomic and somatic neural systems. Pathokinesiology addressed as an aid in
identifying major concepts and introducing clinical relevance. Introduction to gait analysis and special
tests for orthopedic evaluation and differential diagnosis is integrated with detailed dissection and
thorough anatomical study of the limbs. Lecture and Laboratory.
PT 5070 Patient Care Skills (3 credit hours)
(Formerly PT 507)
Prerequisite: Acceptance to program. Introduction to the physical therapy skills of transfers, gait
training, bed mobility, wheelchair selection and management, cushions, range of motion and monitoring
of physiological responses. Discussion of nature of PT in acute care environment with introduction to
lines and tubes in critical care, typical diagnoses treated, and the appropriate delegation to support
personnel and discharge planning, including recommendation for disposition of the patient, ordering of
DME, and family training. Includes medical terminology. Lecture and laboratory.
24
PT 5075 Physical Agents and Procedures (3 credit hours)
(Formerly PT 508)
Prerequisite: Acceptance to program. Application of sterile technique and universal precautions,
physiologic principles and applications of heat and cold modalities, ultrasound, massage and
hydrotherapy. Includes relaxation techniques. Lecture and laboratory.
PT 5100 Physiology/Pathophysiology (5 credit hours)
(Formerly PT 511)
Prerequisite: Acceptance to program. Human physiology including homeostasis, cell transport,
endocrine and neural signaling, pain and body defenses. Emphasis will be placed on the physiology of
the major body systems, and will include discussion of commonly encountered clinical conditions within
each system. Also includes an introduction to neuroanataomy and neurophysiology.
PT 5120 Human Life Sequences (2 credit hours)
(Formerly PT 510)
Prerequisite: PT 5100. The developmental process from conception to death with the emphasis on
human motor performance. Sequence of study includes fetal life, infancy, early and middle childhood,
late childhood, adolescence, early and middle adulthood, and the aging adult including: neuroanatomical
and neurophysiological mechanisms in relationship to developmental changes in performance, and
musculoskeletal development in relationship to the human life span.
PT 5130 Research Methodology in Health Care (3 credit hours)
(Formerly PT 512)
Prerequisite: Acceptance to program. This course will cover basic quantitative, qualitative, and
epidemiologic methods and designs of research. Topics include ethical issues related to research,
validity and reliability of measures, sampling methods, and appropriate statistical analysis for various
types of research. Students will work on group or individual projects, which include a critical appraisal
of the literature and development of a research proposal for a pilot study. Course may be offered online.
PT 5140 Research Evidence-based Practice (2 credit hours)
Prerequisite: PT 5130 or equivalent. Application of research methods to clinical studies. Examines
the methods used for the objective and systematic study and evaluation of clinical practices.
PT 5141 Clinical Education and Professional Development I (1 credit hour)
(Formerly PT 514)
Prerequisite: Acceptance to program. This one hour seminar course will offer an introduction to
clinical education in physical therapy to include an overview of the affiliation agreement. Scheduling
and assignment for Clinical Practicum I will also be incorporated herein. Cr/NCr.
PT 5142 Clinical Education and Professional Development II (1 credit hour)
(Formerly PT 515)
Prerequisite: PT 5141. This one credit seminar course will continue from PT 5141 on various aspects
of clinical education, including expectations of clinical performance and utilization of the evaluation
tool. Scheduling and assignment for Clinical Practicum II will also be incorporated herein. Cr/NCr.
25
PT 5143 Clinical Education and Professional Development III (1 credit hour)
(Formerly PT 516 and PT 517)
Prerequisite: PT 5141, 5142. This one credit seminar course will continue from PT 5142 on various
aspects of clinical education including issues of professionalism in the physical therapy field, the role of
the health care team, and the licensure process. Scheduling and assignment for Clinical Practicum III
and IV will also be incorporated herein. Cr/NCr.
PT 5200 Differential Diagnosis of Musculoskeletal Disorders (3 credit hours)
Prerequisite: PT 5040, 5060, 5065, 5100, 5230. Introduction to topics of pain, medical imaging,
pharmacology for musculoskeletal conditions, and key clinical pathologies of the musculoskeletal
system. The discussion of pathologies will include epidemiology, etiology, and medical management,
including diagnostic tests, lab studies, medication and surgical management, and differential diagnosis.
PT 5205 Evaluation and Treatment of Upper Quarter Musculoskeletal Dysfunction (6.5 credit
hours)
(Formerly PT 523)
Prerequisites: PT 5015, 5040, 5060, 5065, 5070, 5075, 5100, 5200, 5210, 5230, 5235. Evaluation
and treatment of neuromusculoskeletal problems of cranio-facial region, cervical spine, upper extremity,
and upper trunk using regional approach. Foundational content from PT 5210 including the framework
for subjective and objective examinations, assessment, and treatment of patients, is applied to upper
quarter body regions. Common single and multi-region problems also covered. Lecture and laboratory.
PT 5210 Evaluation and Treatment of Lower Quarter Musculoskeletal Dysfunction (6 credit
hours)
(Formerly PT 524)
Prerequisites: PT 5040, 5060, 5065, 5070, 5075, 5100, 5230, and concurrent enrollment in PT 5015,
5200, 5235. Evaluation and treatment of neuromusculoskeletal problems of the lower extremity and
lower trunk using regional approach. Includes foundational topics necessary for evaluation and
treatment of neuromusculoskeletal problems, such as principles and practice of muscle strengthening,
muscle endurance, muscle stretching, soft tissue mobilization, joint mobilization, and PNF. Other
foundational content includes the framework for the subjective (interview) and objective (physical)
examination of patients, including assessment and treatment. Framework is then applied using problem-
solving and evidenced-based approach by region, individually and in combination, to the thoracolumbar
spine, sacroiliac joints and pelvis, hip, knee, ankle, and foot. Common single and multi-region problems
also covered, including pathological gait. Lecture and laboratory.
PT 5220 Principles of Teaching and Learning (2 credit hours)
(Formerly PT 530)
Prerequisites: Acceptance to the program. Teaching-learning theory applied to clinical practice with
clients and their families. Includes teaching techniques for being a clinical instructor or presenting in-
services. Final class session for presentation of micro-teach with self and group-evaluations.
PT 5230 Medical Screening & Systems Review I (2 credit hours)
Prerequisite: Acceptance to the program. The course uses a systems approach to discuss common
medical conditions, their epidemiology, etiology, clinical manifestations, medical management, and
issues related to PT screening, examination, interventions, and appropriate referral to other medical
practitioners.
26
PT 5235 Medical Screening & Systems Review II (2 credit hours)
Prerequisite: PT 5230. Continuation of 5230. Includes labs on physical exam related to visceral
structures for purposes of medical screening and indications for referral to medical practitioner or other
appropriate health care providers. Lecture and laboratory.
PT 6000 Neuroanatomy (4 credit hours)
(Formerly PT 526)
Prerequisite: Acceptance to the program. Normal anatomy and function of the central, peripheral, and
autonomic nervous systems; laboratory with specimens. Lecture and laboratory.
PT 6005 Neurophysiology (4 credit hours)
(Formerly PT 527)
Prerequisite: PT 5040, 5100. Human neurophysiology with emphasis on normal cellular and systemic
functions of the central and peripheral nervous systems.
PT 6010 Evaluation and Treatment of Neurological Disorders I (4 credit hours)
(Formerly PT 528)
Prerequisite: PT 5060, 5065, 5070; concurrent enrollment in PT 6000, 6005. Systematic approach to a
variety of neurological problems of the central and peripheral nervous systems. Emphasis is on the
impairments and clinical manifestations of the anatomical lesions, evaluation techniques and
interventions. Lecture and Laboratory.
PT 6011 Evaluation and Treatment of Neurological Disorders II (4 credit hours)
Prerequisite: PT 5060, 5065, 5070, 6010. Continuation of PT 6010.
PT 6015 Differential Diagnosis of Neurological Disorders (4 credit hours)
Prerequisite: PT 5230, 5235; concurrent enrollment in PT 6000, 6005, 6010. Introduction to the
causal factors, anatomical and physiological impairments, and symptoms related to congenital and
acquired neurological disorders in the adult population. Pathologies of common neurological disorders
will be discussed. Includes principles of EMG/NCV testing.
PT 6020 Principles of Electrotherapeutic Evaluation and Treatment (3 credit hours)
(Formerly PT 529)
Prerequisites: PT 5015, 5040, 5060, 5065, 5070, 5075, 5200, 5210, 5230, 5235, and concurrent
enrollment in PT 6045. Clinical, scientific, and theoretical evidence, and the practical clinical
applications of electrotherapeutic strategies in the physical therapy management of dysfunction.
Includes basic foundational concepts in electrical stimulation and electrophysics, neurophysiology,
electrical safety and instrumentation, and electrotherapy terminology; the parameters of electrical
stimulation; and the neurophysiological and biological responses to electrical stimulation. Covers
treatment purposes including muscle strengthening and endurance, functional electrical stimulation,
spasticity control, denervated muscle stimulation, pain control, circulation enhancement, edema control,
tissue healing, and iontophoresis. Evaluation of appropriateness of using a given electrotherapy device
for the different treatment purposes. Lecture and laboratory.
PT 6030 Physiology of Exercise (4 credit hours)
(Formerly PT 531)
Prerequisite: PT 5060, 5065, 5100. This course addresses bioenergetics as well as the acute and
chronic physiological responses of the human body during exercise and other special conditions. The
physiological basis of therapeutic exercise is the foundation for this course. Lecture and laboratory.
27
PT 6040 Evaluation and Treatment of Cardiopulmonary System (4 credit hours)
(Formerly PT 532)
Prerequisite: PT 5060, 5065, 5100. Introduction to evaluation and treatment of diseases of the cardio-
pulmonary system; includes physiology and pathophysiology, evaluation and treatment methods,
differential diagnosis, and prevention. Lecture and laboratory.
PT 6045 Differential Diagnosis of the Integumentary System/Wound Care (3 credit hours)
Prerequisite: PT 5040, 5060, 5065, 5100. Discussion of screening for pathological conditions of the
integumentary system including medical management and testing methods. Emphasis on wound healing
and factors which facilitate or impede the healing process; physical therapy methods of evaluation and
intervention techniques; and interdisciplinary case management. Lecture and Laboratory.
PT 6050 Principles of Administration and Management (3 credit hours)
(Formerly PT 534)
Prerequisite: PT 5015. Organization and administration of a physical therapy department including
budget considerations, hiring-interviewing techniques, marketing, and medical-legal issues.
PT 6060 Prosthetics, Orthotics, and Gait (3 credit hours)
(Formerly PT 538)
Prerequisite: PT 5060, 5065. Evaluation and application of prosthetic and orthotic devices to physical
therapy clients. Evaluation of abnormal and pathological gait patterns. Lecture and laboratory.
PT 6070 Prevention and Management of Problems in the Aging Adult (3 credit hours)
(Formerly PT 535)
Prerequisite: PT 5000 through 5120, 5200 through 5230, 6000 through 6020; concurrent enrollment
in PT 6030, 6040, 6050. Systematic, problem solving approach to the geriatric client with emphasis on
prevention, etiology, clinical manifestations, evaluation, treatment and resources.
PT 6075 Prevention and Management of Problems in the Pediatric Population (3 credit hours)
(Formerly PT 536)
Prerequisite: PT 5060, 5065, 5070, 5100, 5120, 6000, 6005, 6010. Systematic, problem solving
approach to the pediatric client with emphasis on prevention, etiology, clinical manifestations,
evaluation and treatment. Lecture and laboratory.
PT 6220 Application of Research to Clinical Practice (0.5 credit hour )
(Formerly PT 540)
Prerequisite: PT 5130 and 5140 or equivalent. Individually planned studies under the direction of a
senior investigator. Studies to be pertinent to work in physical therapy. Students give presentation of
research proposal to PT community. Repeatable to a maximum of 1 credit hour. Cr/NCr.
PT 6600 Strategies for Successful Learning (0 credit hours)
Prerequisite: Admission to DPT program. This course provides new students entering with advanced
standing an introduction to the DPT program. Following an overview of the most important services,
policies, instructional methods and resources, students will have an opportunity to assess their readiness
for the program. The awareness, knowledge and skills derived from this part of the course will help
ensure successful completion of the program. This course is provided on campus only and must be
taken prior to beginning the first trimester in the program. Cr/NCr.
28
PT 7010 Clinical Education I (3 credit hours)
(Formerly PT 518)
Prerequisite: Satisfactory completion of all coursework in Trimesters I and II. Forty hours per week
for three weeks under the direct supervision of a physical therapist serving as the clinical instructor.
Application of course content in Trimesters I and II will be emphasized in this clinical experience.
Cr/NCr.
PT 7020 Clinical Education II (12 credit hours)
(Formerly PT 519)
Prerequisite: Satisfactory completion of all coursework in Trimesters I through IV, PT 6080, 6090,
7010. Forty hours per week for twelve weeks under the direct supervision of a physical therapist serving
as the clinical instructor. Application of course content in Trimesters I through IV and PT 6080 and
6090 will be emphasized in this clinical experience. Cr/NCr.
PT 7030 Clinical Internship I (12 credit hours)
(Formerly PT 520)
Prerequisite: Satisfactory completion of all didactic courses and PT 7010, 7020. Forty hours per
week for twelve weeks under the direct supervision of a physical therapist serving as the clinical
instructor. Application of all previous coursework will be emphasized in this clinical experience.
Cr/NCr.
PT 7040 Clinical Internship II (12 credit hours)
(Formerly PT 521)
Prerequisite: Satisfactory completion of all didactic courses and PT 7010, 7020, 7030. Forty hours per
week for twelve weeks under the direct supervision of a physical therapist serving as the clinical
instructor. Application of all previous coursework will be emphasized in this clinical experience.
Cr/NCr.
PT 8100 Pharmacology for Physical Therapists (3 credit hours)
Prerequisite: PT 5100, 5230, 5235 or equivalent courses. Basic and applied pharmacology for the
physical therapist. Includes the effects of pharmacotherapy on the health and well being of patients.
PT 8110 Structural Imaging in Physical Therapy Diagnosis (2 credit hours)
Prerequisite: PT 5040, 5060, 5065, 5100, 5230, 5235, or equivalent. This course will familiarize the
DPT student with the indication, instrumentation, and clinical interpretation of orthopedic imaging
techniques, including plain film x-ray, magnetic resonance, computerized tomography, and radioisotope
imaging. Selection protocols for each will be discussed to acquaint the student with advantages and
disadvantages of each method and what type of information each technique best presents. This course
will focus on the clinical interpretation and practical integration of imaging data into rehabilitation
regimen design and communication with other medical professionals. Course may be offered online.
PT 8120 Medical Screening and Systems Review (4 credit hours)
Prerequisite: Acceptance to the program. The course uses a systems approach to discuss common
medical conditions, their epidemiology, etiology, clinical manifestations, medical management and
issues related to PT screening, examination, interventions, and red flags. Includes labs on physical exam
related to visceral structures for purposes of medical screening and indications for referral to medical
practitioner or other appropriate health care providers. May include online lectures/discussions and in
class laboratory.
29
PT 8130 Advanced Differential Diagnosis I (2 credit hours)
Prerequisite: PT 8120, licensed physical therapist with at least one year clinical experience. This
course includes detailed skills for differentiating pathologies within the musculoskeletal system as
described in the Guide to Physical Therapist Practice. The reliability and validity of relevant PT tests
and measures will be explored. The physical therapist will develop higher level clinical reasoning skills
related to developing a PT diagnosis and interventions. Cases will include those with complex
presentations, multi-systems involvement, and will encompass the life span.
PT 8135 Advanced Differential Diagnosis II (2 credit hours)
Prerequisite: PT 8120, licensed physical therapist with at least one year clinical experience. This
course includes detailed skills for differentiating pathologies within the neuromuscular, cardiovascular-
pulmonary, and integumentary systems as described in the Guide to Physical Therapist Practice. The
reliability and validity of relevant PT tests and measures will be explored. The physical therapist will
develop higher level clinical reasoning skills related to developing a PT diagnosis and interventions.
Cases will include those with complex presentations, multi-systems involvement, and will encompass
the life span.
PT 8200 Professional Leadership and Ethics (2 credit hours)
Potential leadership roles of the physical therapist will be discussed. Issues related to professional
development and reflective practice, collaboration with other health care providers, and knowledge of
advocacy will be examined. Group discussions will include legal/ethical issues experienced in the
clinical setting and in relation to the role of the physical therapist in primary care/direct access.
PT 8210 Documentation and Health Care Financing (2 credit hours)
Government, private insurance and managed care changes in health care financing will be presented.
Students will review and critique documentation as a means to developing their own skills in this area.
PT 8230 Wellness and Prevention/Community Education (3 credit hours)
The application of primary, secondary and tertiary prevention and the therapist’s role in wellness and
health promotion will be discussed. Teaching/learning principles are applied to community education
programs including those related to wellness, prevention and health promotion.
PT 8400 Research Investigation (0-2 credit hours)
Prerequisite: PT 5130, 5140, 6200. Students have the option to carryout the proposal developed in
Applied Research I under the supervision of faculty or senior investigator. Final project includes write-
up of results in journal format. Cr/NCr.
PT 8500 Selectives (4-6 credit hours)
(Formerly PT 539 or 6500)
Prerequisite: Approval of instructor. Special topics in physical therapy presented in workshop format.
Laboratory experiences may be included. Students have the option to complete a specialized 6 week
clinical practicum in lieu of coursework. Cr/NCr.
Page 122: Insert the following course description after PT 8100
PT 8110 Structural Imaging in PT Diagnosis (3 units)
Prerequisite: Graduation from an accredited physical therapy program and current licensure as a physical therapist.
This course will familiarize the student with the indications, instrumentation, and clinical interpretation of orthopedic
imaging techniques including plain film x-ray, magnetic resonance, computerized tomography, and radioisotope imaging.
Selection protocols for each will be discussed to acquaint the student with advantages and disadvantages of each method and
what type of information each technique best presents. This course will focus on the clinical interpretation and practical
integration of imaging data into rehabilitation treatment regimen design and communication with other medical professionals.
Page 123: Insert The Bertha Oliver Memorial Award as an award presented at graduation.
Page 147: PA 6040 Senior Seminar III should read 2 credit hours instead of 3 credit hours.
Page 174: Insert the following Calendar addition:
Thursday, May 15, 2003
Graduating Student Seminar (Graduating Students only,
in lieu of the June 6-8, 2003 Weekend Seminar)
