i
ii
Western University of Health Sciences (Western University) is an independent, non-profit academic health
center, incorporated in the State of California, and dedicated to educating health care professionals qualified
to provide comprehensive health care to the family.
Accreditation(s)
Western University of Health Sciences is accredited by the Accrediting Commission for Senior Colleges
and Universities of the Western Association of Schools and Colleges (WASC, 895 Atlantic Avenue, Suite
100, Alameda, California, 94501, phone number: 510-748-9001), a regional accrediting body recognized by
the Council on Higher Education Accreditation and the U.S. Department of Education.
Professional accreditations for each academic program are indicated in the appropriate section of this
catalog.
Notice of Non-discrimination Policy
Western University of Health Sciences, in compliance with Titles VI and VII of the Civil Rights Act of
1964, Title IX of the Education Amendments of 1972, Sections 503 and 504 of the Rehabilitation Act of
1973, and Sections 102 and 302 of the Americans With Disabilities Act of 1990, does not discriminate on
the basis of race, color, national origin, religion, handicap, or sexual orientation in any of its policies,
procedures, or practices. In accordance with sex discrimination laws, the University forbids acts of sexual
harassment. In compliance with the Age Discrimination in Employment Act of 1967, Section 402 of the
Vietnam Era Veterans Readjustment Act of 1974, and Section 12940 of the State of California Government
Code, the University does not discriminate against any employees or applicants for employment on the basis
of their age, their ethnic origin, their marital status, their sexual orientation, or because they are disabled
veterans or veterans of the Vietnam Era, or because of their medical condition (as defined in Section 12926
of the California Government Code); nor does the University discriminate on the basis of citizenship, within
the limits imposed by law. This non-discrimination policy covers admission, access, and service in the
University programs and activities and application for and treatment in University employment.
Pursuant to Executive Orders 11246 and 11375, as amended, Section 503 of the Rehabilitation Act of 1973,
as amended, and Section 402 of the Vietnam Era Veterans Readjustment Act of 1974, as amended, Western
University of Health Sciences is an affirmative action and equal opportunity employer.
Access to Individuals with Disabilities
It is the policy of Western University to provide qualified persons with disabilities with access to its
programs and services, when viewed in their entirety, in the most integrated setting possible. Additional
information will be provided upon request from the Student Affairs Office.
Please Note:
Text for the catalog was prepared as of June 2001. The information herein applies to the academic year
2001-2002 and is subject to change at the discretion of the University.
Visitors are always welcome at the University and campus tours are available. Visitor badges are required
and can be obtained from the receptionist in the Administration Center.
Office of Admissions, Mondays, 8:30 am - 12 noon, Tuesdays-Fridays, 8:30 pm - 5 pm
University Switchboard - (909) 623-6116.
Western University of Health Sciences Catalog Vol. 12, No. 1, Summer, 2001
iii
The President's Message
Attending an academic health center such as Western University of Health Sciences is not an automatic
passport to becoming a good health professional. While a first-rate educational experience is essential, the
making of a good health professional is also rooted in the nature and quality of the people involved.
There is visible and strong sense of community, of family, at Western University. We are proud of the
fact that the institution is people-centered, that it seeks to develop in our students a blend between the
technical and the human skills required of health care professionals. The content and substance of the
curricula, as well as the instructional processes used to carry it out, reflect a humanistic approach to health
care.
The University's educational programs provide training that presumes the faculty and the students are the
masters and not the slaves to this institution. We believe, therefore, that it is imperative our students feel
they have a place in the learning environment and that they are active rather than passive recipients of their
education. Learning proceeds in ways directly related to the interests and needs of the students as well as to
the demands of the health professions.
Here at Western University, a student can expect an education that will assist him or her to become a
feeling, humane, sensitive and medically competent professional and not just a learned degree-holder. To
that end, the University encourages a flexible and innovative "learning" environment instead of a rigid,
closed "learned" one.
In a word, a student can expect the same treatment from Western University that a patient should look
for from an able health professional. Thus, in the final analysis, what a student can expect from the
University is measured by the success of our humanistic approach -one that requires an active partnership
between you and us.
That is what goes into the education that takes place here and what Western University of Health
Sciences is all about.
Sincerely,
Philip Pumerantz, PhD
iv
Table of Contents
iii The President's Message
iv Table of Contents
1 Western University of Health Sciences
4 Frequently Called Numbers
5 Student Life: Campus Facilities and
Services
9 Student Services
21 University Policies and Procedures
27 General Academic Policies and
Procedures
35 Tuition and Fees
37 Financial Aid
42 University Calendar
43 College of Osteopathic Medicine of
the Pacific
Doctor of Osteopathic Medicine
Degree Program
43 Accreditation
43 The Osteopathic Philosophy
43 Technical Guidelines for Admission and
Matriculation
44 Admissions Policies and Procedures
47 Registration
47 Tuition and Fees
48 Academic Requirements
56 Curriculum
59 Course Descriptions
67 Honors and Awards
68 Academic Calendar
69 Osteopathic Oath
70 College of Pharmacy
Doctor of Pharmacy Degree Program
70 Accreditation
70 About the Profession
70 The Degree
70 Career Opportunities
71 The College of Pharmacy
72 Admissions Policies and Procedures
73 Tuition and Fees
74 Financial Assistance
74 Academic Policies and Procedures
80 Description of Blocks/Course
Descriptions
87 Honors and Awards
87 Academic Calendar
88 College of Allied Health Professions
88 Mission
89 Master of Science in Health
Professions Education Program
89 About the MSHPE Program
90 Technical Guidelines for Admission and
Matriculation
90 Admissions Policies and Procedures
91 Registration Policies and Procedures
92 Academic Requirements
95 Tuition and Fees
95 Program of Studies
95 Course Descriptions
97 Honors and Awards
98 Academic Calendar
99 Master of Physical Therapy Degree
Program
99 Accreditation
99 The Practice of Physical Therapy
100 Technical Guidelines for Admission and
Matriculation
101 Admissions Policies and Procedures
103 Tuition and Fees
104 Academic Requirements
111 Curriculum Organization
113 Curriculum
118 Honors and Awards
119 Academic Calendar
120 Master of Science in Physician
Assistant Studies
120 Accreditation
120 Vision Statement
120 Mission Statement
120 The Physician Assistant Role
121 Program Goals
123 Technical Guidelines for Admission and
Matriculation
124 Admissions Policies and Procedures
126 Tuition and Fees
126 Academic Requirements
139 Curriculum Organization
140 Course Descriptions
144 Honors and Awards
145 Academic Calendar
146 The Physician Assistant Oath
147 Master of Science in Health Science -
Licensed Physician Assistant Track
147 Goals of the MSHS-LPAT Program
147 Admissions Policies and Procedures
149 Academic Requirements
152 Tuition and Fees
152 Course Descriptions
154 Academic Calendar
v
155 College of Graduate Nursing
Master of Science in Nursing/Family
Nurse Practitioner Program
Post-Masters Family Nurse
Practitioner Track
Advanced Practice Nurse to
Family Nurse Practitioner
Track
Master of Science in Nursing
Track
155 Mission
155 Philosophy
156 Accreditation
156 Outcome Competencies for Graduates
157 Curriculum
158 MSN-Harbor Track
158 Admission Policies
160 Registration
160 Tuition and Fees
161 Academic Policies and Procedures
166 Course Descriptions
170 Curriculum (MSN/FNP)
171 Curriculum (FNP-only Track)
171 Curriculum (MSN-only Track)
172 Curriculum (APN to FNP Track)
173 Honors and Awards
174 Academic Calendar
175 Board of Trustees, Administration and
Faculty
175 Board of Trustees
175 University and Academic
Administration
177 Faculty
185 Clinical and Adjunct Faculty
211 University Map
1
WESTERN UNIVERSITY
OF HEALTH SCIENCES
GENERAL INFORMATION
Western University of Health Sciences (Western University) is a non-profit, independent, academic
health center, founded as the College of Osteopathic Medicine of the Pacific (COMP) in 1977. The
founding mission of the institution was to educate primary care osteopathic physicians for the western
United States. Over the past two decades, Western University has preserved and enhanced its mission,
expanding it to include educational programs in the allied health professions, pharmacy, graduate nursing
and veterinary medicine.
INSTITUTIONAL MISSION
Western University is a graduate university of medical sciences that educates health professionals to
practice and teach with excellence and compassion. Within a learner-centered environment, the University
encourages lifelong learning, supports faculty and student scholarly activities, provides patient care in
support of clinical training, and enhances the quality of life in the region through community service.
VALUES
The people of Western University are dedicated to caring as they pursue their educational, scholarly,
patient care, and public service activities. The University encourages the diversity and interdisciplinarity of
its programs, students, faculty, staff, and administrators. The ideals of continuous quality improvement,
lifelong learning, long-term planning, fiscal strength, adaptability, and agility in the rapidly changing worlds
of health care and education are realized through innovation, teamwork, and collaboration within the
University as well as with its network of academic health centers and community partners.
VISION
To be the graduate university of medical sciences of choice in the western United States.
GOALS
To provide top quality, learner-centered educational programs in selected graduate medical sciences to
educate a health workforce that meets the needs of the State of California and the western United States.
To link educational, research and service activities and programs in a learner-centered environment
through partnerships with academic health centers and other health and education related organizations to
improve the quality of life of the surrounding communities.
To ensure top quality postgraduate education and training opportunities for graduates of its programs.
To be renowned for using the Internet to promote "e-ffectiveness," "e-fficiency," and "e-learning."
To ensure organizational effectiveness and development.
HISTORY
The founding institution, the College of Osteopathic Medicine of the Pacific (COMP), was established
in 1977 as a direct and important response to a critical shortage of primary care physicians in the western
United States. Philip Pumerantz, PhD, accepted the invitation of the college's board of directors to become
the founding president in September of 1977. In January 1978, COMP received pre-accreditation status
from the American Osteopathic Association. Provisional accreditation status was achieved in July of 1978
and full accreditation in February 1982.
2
COMP admitted its charter class of 36 students in 1978, and classes began on October 2. This occasion
marked the successful culmination of efforts begun in 1974 by the State Society of Osteopathic Physicians
and Surgeons of California "to seek the establishment of a college of osteopathic medicine in the State of
California." The charter class was graduated on June 13, 1982.
In response to a nationwide demand for qualified clinical educators, COMP initiated a Master of Science
in Health Professions Education degree program (known on campus as MSHPE) in September 1986. This
program was housed within a newly created Graduate Division, and its charter class graduated in June 1987.
The program has grown in subsequent years with an enrollment reflecting a wide spectrum of health
professionals.
As a new decade began, COMP accepted its first class of physician assistant (PA) students who
matriculated on February 2, 1990. With the addition of this program, the Graduate Division became the
Division of Allied Health Professions, and subsequently, the School of Allied Health Professions. The start
of the PA program signaled a new era in which COMP expanded its mission of educating family-oriented
health care professionals for the western United States.
In response to a growing need for physical therapists in this country, a master's degree program in
physical therapy (the MPT degree) was launched on January 6, 1992. Within the School of Allied Health,
COMP enrolled 49 students in the charter class and hired five faculty members for the program. The two-
year, four-month MPT program educates physical therapists to function as generalists in the field who are
also concerned about wellness, health promotion and a humanistic approach to the care of the whole patient.
In 1991 the institution achieved the status of an academic health center (ACH) due to its multi-faceted
programs in medical and allied health education. The academic health center formed a partnership with San
Bernardino County Medical Center, which moved to a state-of-the-art facility in Colton, California, and
changed its name to the Arrowhead Regional Medical Center (ARMC) in the spring of 1999. The
partnership, known as the Academic Center for Excellence in the Health Sciences (ACEHS), provides the
University with a primary teaching hospital. ARMC sponsors the largest family practice residency training
program in California and the second largest in the nation.
In August of 1996, in order to better reflect its stature, COMP was restructured into a university with a
new name: Western University of Health Sciences. The College of Pharmacy also welcomed its charter
class into the Doctor of Pharmacy (PharmD) program at that time. This program was the fourth college of
pharmacy to be established in the State of California and prepares students in a humanistic, interdisciplinary
tradition to become competent, qualified professionals. Graduates of Western University's College of
Pharmacy will complement other health care team members by offering their expertise in comprehensive
drug therapy management.
In March of 1998 Western University created a College of Graduate Nursing in order to satisfy an
increasing demand for advanced practice nurses. The College offers a Master of Science in Nursing (MSN)
degree, a Family Nurse Practitioner (FNP) certificate program, and a joint MSN/FNP program for advanced
practice nurses.
The arrival of the World Wide Web as an electronic information management tool provide a unique
opportunity to offer students individualized learning experiences that would be impossible through other
media. Online discussion forums and e-mail also provide important lines of communication and support
among distance learners, faculty, and other program personnel.
Western University founded the College of Veterinary Medicine-its fifth college-in August 1998. Shirley
D. Johnston, DVM, PhD, was hired as the founding dean the following month. She is the first female dean
of a veterinary college in the United States. Western University is committed to providing an AVMA-
accredited educational program that will serve as a new paradigm in veterinary education. Western
University's College of Veterinary Medicine's goal is to enroll its charter class of students in the fall of
2003.
3
The University also founded the Center for Disability Issues and the Health Professions in August 1998.
Headed by Brenda Premo, MBA, the former director of the Department of Rehabilitation for the State of
California under Governor Pete Wilson, the Center works to improve the capabilities of primary health care
providers to meet the growing needs of people with disabilities.
In August 1999, the University changed its Primary Care Physician Assistant certificate program to the
master's degree level, effective with the class entering in August 2000. Students who complete the two-year
program will be awarded the Master of Science (MS) degree in Physician Assistant Studies. Current with
this program change, the faculty developed an on-line Master of Science in Health Sciences degree
program, designed for licensed physician assistants who possess a bachelor’s degree and seek advanced
education at the graduate level.
KEY FACTS ABOUT
WESTERN UNIVERSITY
• Western University of Health Sciences had the highest percentage of graduates of the nation's
medical schools entering family medicine, according to New Physician magazine's 1995 Annual
Primary Care Scorecard. Approximately 65 percent of the doctor of osteopathic medicine
graduates are practicing in primary health care fields.
• Students in all educational programs consistently score at the top on national boards and state
licensure examinations.
• Graduates of COMP are sought by top residency programs nationally and many serve as chief
residents in their chosen specialties.
• Total number of alumni (1982 - 2000) is 3,094
• Enrollment 2000-2001 (as of January 15, 2001) was 1,500
• College of Osteopathic Medicine of the Pacific: 696
• College of Allied Health Professions: 352
- Physical Therapy: 133
- Health Professions Education: 18
- Physician Assistant: 196
- Health Sciences – LPAT: 5
• College of Pharmacy: 404
• Master of Nursing/Family Nurse Practitioner: 48
DIVERSITY STATEMENT
The students, faculty, administration and staff of Western University of Health Sciences place great
value on diversity. For us, it is a philosophy of inclusion, where pluralism and academic freedom are at its
foundation. Western University is committed to an open environment that promotes, accepts and celebrates
different points of view.
Western University is comprised of a community of individuals in which diversity is recognized as being
the core of our intellectual, social, cultural, physical, emotional and moral lives. We are enriched by our
encounters with one another and we strive to learn from each other in an atmosphere of positive engagement
and mutual respect. Our understanding and acceptance of one another in the campus environment
contributes to our ability to care for our patients who live in a diverse society.
The University, in accordance with various laws and beliefs, does not discriminate on the basis of race,
color, ethnicity, national origin, religion, politics, disability, gender or sexual orientation in any of its
policies, procedures or practices. Sexual harassment is unacceptable.
We acknowledge our guaranteed rights of free expression under the First Amendment to the Constitution
of the United States. However, we also hold unique responsibilities as individuals, answerable for our own
behavior and fully accountable for our actions. Seeking balance between rights and responsibilities makes
4
us keenly aware of the dangers of defamatory, libelous or obscene behavior, the value of community and the
importance of respecting our differences and commonalties.
As individuals committed to health professions education in the osteopathic tradition, we embrace the
important principle of caring for the whole person-in body, mind and spirit.
FREQUENTLY CALLED NUMBERS
President (909) 469-5200
Academic Affairs (909) 469-5578
Finance and Administration (909) 469-5693
Admissions (DO) (909) 469-5335
Admissions (All Other Programs) (909) 469-5542
Student Affairs (909) 469-5340
Office of Student Services (909) 469-5616
Western University Medical Center (909) 865-2565
Department of Physical Therapy Education (909) 469-5300
Department of Physician Assistant Education (909) 469-5378
Department of Health Professions Education (909) 469-5397
College of Osteopathic Medicine of the Pacific (909) 469-5505
Director of Student Services (909) 469-5414
Clinical Rotations (909) 469-5260
Assistant Dean of Educational Affairs (909) 469-5257
College of Allied Health Professions (909) 469-5390
College of Graduate Nursing (909) 469-5523
College of Pharmacy (909) 469-5500
Financial Aid (909) 469-5353
Learning Enhancement and Academic Development (909) 469-5408
Bursar (909) 469-5403
Technical Support Services (909) 469-5432
Multimedia Services (909) 469-5432
Registrar (909) 469-5342
Bookstore (909) 469-5416
Center for Disability Issues & the Health Professions (909) 469-5380
Security (909) 469-5475
Library (909) 469-5321
College of Veterinary Medicine (909) 469-5627
5
STUDENT LIFE: CAMPUS FACILITIES
AND SERVICES
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 623-6116
The main campus of Western University is in Pomona (see map, inside back cover), a city of
approximately 150,000 residents, located about 35 miles east of Los Angeles near the foothills of the San
Gabriel Mountains. It is an area with a high concentration of private and state colleges and universities.
Mountain resorts are nearby, and Pacific Ocean beaches, Palm Springs, Hollywood, Pasadena, Los Angeles,
arboretums, theme parks, museums, art galleries, libraries, theaters, and concert halls are all within about an
hour's drive.
Alumni Center
The Alumni Center is a 32,000 square-foot facility, located at the corner of Gibbs and Second Streets.
The main level of the Alumni Center includes the office of Alumni and Constituent Relations and three
lecture halls: Cooper Hall, Swift Hall and Trendle Hall. The lower level of the Alumni Center
accommodates the microbiology (The Rene‚ and Namey laboratories, the Oswald Suter Microbiology Prep
Room) laboratories, a multipurpose teaching lab, The Roy and Marion Kramer Research Laboratory, other
research labs and student lockers.
Booth University Bookstore
The Booth University Bookstore is a convenient source for required textbooks, supplies, and insignia
gift items. Personal checks, Visa®, MasterCard, and DiscoverCard® are accepted. Telephone and mail
orders are accepted with shipment made via UPS. The bookstore is open from 7:30 am until 5:30 pm
Monday through Friday. Located in the rear of the bookstore is a popular gathering place, the Hop Shoppe.
Business Center
The Business Center houses the departments of Business Services (Bursar's Office, Accounting and the
Treasurer's Office), Office of Facilities Management and Physical Plant, Human Resources, and Security.
Health Professions Center (HPC)
The Health Professions Center includes facilities for the College of Pharmacy, the College of Graduate
Nursing, and the College of Osteopathic Medicine of the Pacific (COMP) as well as other university
services.
The first floor includes a 54-seat auditorium; a 200 seat lecture hall; three "in-the-round" high-tech
classrooms; break-out rooms for small group learning activities; Feldsher Hall; a large student lounge with
two kitchens, 80-inch screen television, pool table, ping pong table, and vending machines; administrative
and faculty offices for the College of Pharmacy; and a pharmacy/medical office museum. The offices of the
Center for Academic and Professional Education and the office of Learning Enhancement and Development
are also located on the first floor of the Health Professions Center.
The second floor of the HPC has a 200-seat lecture hall, administrative and faculty offices for the
College of Osteopathic Medicine of the Pacific and the College of Graduate Nursing, clinical skills
laboratories, research laboratories, conference rooms, and offices for the Multimedia Department and the
Department of Strategic Planning and Institutional Effectiveness.
Health Sciences Center (HSC)
The 72,000 square-foot Health Sciences Center features a unique central staircase. The first floor
consists of two large amphitheater-style lecture halls; Tribute Walk, a donor recognition area; and
Compatriot's Hall, an elegant meeting room with kitchen facilities. The first floor also houses the offices of
the Provost, and the administrative and faculty offices of the College of Allied Health Professions, including
6
the departments of Physician Assistant Education and the Master of Science in Health Professions
Education.
The second floor of the Health Sciences Center consists of an anatomy laboratory, the administrative
and faculty offices of the Physical Therapy Education Department; physical therapy clinical skills
laboratories; physical therapy faculty research laboratories, the osteopathic manipulative medicine teaching
laboratory; offices for the Center for Disability Issues and the Health Professions; and offices for the
department of Risk Management and temporary offices for the faculty and administration of the College of
Veterinary Medicine.
Health Sciences Library and Learning Resources Center
The newly opened Health Sciences Library and Learning Resources Center houses the University’s
book, journal and media collections. It also provides office space for the library staff, the staff of the
Department of Instructional and Informational Technology, and the Learning Enhancement and Academic
Development office. The ground floor is reserved for library circulation services, a disability center,
historical museum, and study space where students may use laptops. Books and serial collections are
housed on the second and third floors, respectively, and offices for library and instructional and information
technology staff are found on the fourth floor. The basement serves as the University’s Network Operations
Center and provides office and work space for the Technical Support Staff.
The mission of the Health Sciences Library is to educate by providing library materials and information
services to students, faculty and staff of the University. To further student adaptability and life-long
learning, it has become the goals of the staff of the Health Sciences Library to:
• monitor and evaluate the growing electronic sources on the Internet;
• add links to these sources to our internal computer collection; and
• educate our students, faculty, administration, staff and alumni so that they are able to use these
resources at home, in the office, and at public and hospital libraries.
Student Services Center/South Campus Building
The offices of Student Affairs/Registrar and University Admissions are located on the first floor of the
Student Services Center. The second floor houses the office of Financial Aid.
University Administration Center
The University Administration Center houses the University's executive offices. The first floor contains
the offices for the Executive Vice President for Administration and Finance, Vice President of Policy and
Research, Vice President of University Advancement, and the offices of Major Gifts, Special Events,
Communications, Publications, and Foundation, Corporate and Government Relations. The office of the
University Counsel is located in the basement.
The Office of the President and the Office of the Executive Vice President of Academic Affairs are
located on the second floor. The Saul Bernat Board Room and the VIP Lounge with a kitchen provide space
for meetings and special events.
Western University Campus Gourmet
The Western University Campus Gourmet is a food court providing a Subway sandwich shop, a TCBY
yogurt store, and Mamma Ilardo's pizza. The 1950s diner-themed eating establishment is designed to serve
the Western University community, shoppers at Antique Row, neighboring business populations, and the
general public. A lounge for Western University students occupies the back part of the Campus Gourmet
building. Hours of the food court are: 7:30 am to 6 pm Monday through Friday and Saturdays and Sundays
from 10 am until 4 pm.
Western University Health Care Facilities and Medical Centers
Western University Health Care Facilities and Medical Centers comprise a health care delivery network
of the institution, which operates two medical centers. These medical centers have been established to meet
the needs of the communities in which they are located and also to serve as training facilities for Western
University students.
7
Western University Medical Center
360 E. Mission Boulevard
Pomona, CA 91766-1889
(909) 865-2565
Opened in 1984, Western University Medical Center is an ambulatory, primary care medical center that
addresses the health care needs of Pomona's less advantaged communities, as well as those from
participating managed care organizations, and provides clinical learning opportunities for Western
University students. Osteopathic family physicians and physician assistants, who are also Western
University faculty, and support personnel staff the medical center. In addition to health care services, the
Center provides health screenings for youth athletic programs. The Center is also a member of the Pomona
Clinic Coalition, made up of the County of Los Angeles Department of Health and a group of area health
providers, which provides preventive and primary care health services to people who do not have medical
insurance or can not afford medical care.
Osteopathic Center for Children (OCC)
4235 54th Place
San Diego, CA 92105-2303
(619) 583-7611
The Osteopathic Center for Children, the only one of its kind in the world, was founded by Viola M.
Frymann, DO, FAAO, an internationally-recognized osteopathic physician and one of the founders of
Western University. OCC's program helps its young patients to perform at their optimum potential. The
science of osteopathy in diagnosis and treatment is integrated with music therapy, nutritional education, and
other modalities that assist growth and development in the child. An educational program for families
enables them to better understand and help their children. Research is an integral part of the center's
operation, as is teaching osteopathic medical students about the diagnosis and treatment of exceptional
children through formal instruction and observation. Dr. Frymann's staff at OCC consists of osteopathic
physicians, a developmental optometrist, a neurological developmentalist, a therapeutic musician, and
support staff.
The physicians and physician assistants who work at Western University Medical Centers have faculty
appointments at Western University of Health Sciences and are involved in both the didactic and clinical
teaching aspects of the curriculum.
PERSONAL SAFETY
The University strongly suggests the following precautions for its students, faculty and staff:
• Since some streets through the campus are open to vehicular traffic, please use extreme caution when
crossing between buildings and do not congregate on the street.
• Please make sure your car is locked at all times in the parking lot.
• You should be advised that the doors to some buildings are locked at 5:00 p.m. It would be to your
advantage to walk to the parking lot with a friend or close associate if you are leaving after business
hours. If you find it necessary to work or study late, you should advise security personnel on campus
before leaving the building so that someone can watch you walk to your car.
• During the daytime hours, security guards are assigned to patrol the parking lots directly north, and
northeast behind the North Campus buildings along First Street, and they patrol the lots behind the
South Campus building, Health Sciences Center and Health Professions Center. It is strongly
suggested that you do not leave your car overnight in any of the parking lots or streets surrounding the
campus, as a security guard is not on duty after 11:00 p.m. Mondays - Thursdays, after 7:00 p.m. on
Fridays, and after 10:00 p.m. on Saturdays and Sundays.
8
• Do not admit an unknown person into the building. If someone says they need help, offer to call the
proper person (police, paramedics, etc.).
In case of emergency, if someone from the University needs to be informed or contacted, please call the
following in the order listed.
Campus Security (909) 623-6116, ext. 3000
Dr. Christopher N. Oberg, Executive Vice President (909) 621-5022
of Finance and Administration
Dr. George Charney, Executive Vice President of Academic Affairs (909) 593-1776
Dr. Philip Pumerantz, President (909) 985-0224
9
STUDENT SERVICES
Recreational Facilities
Western University provides YMCA or designated fitness club individual memberships for students at
no cost. If interested, students must sign up at registration. The YMCA is within walking distance of the
Pomona campus and offers coeducational facilities for swimming, racquetball, basketball, exercise
programs, etc. The fitness club provides non-prime time racquetball courts, Nautilus exercise equipment,
aerobics, Jacuzzi, steam rooms, etc. Family memberships may be purchased at reduced rates until the end
of the month in which students begin matriculation. Western University will contribute up to $80.00 for the
1999-00 academic year for students in the MSN/FNP at the Las Vegas Track only, for a paid membership in
the student's name at a fitness facility. Proof of a fitness membership is required prior to the University
approving the reimbursement.
On the Pomona campus, the HPC Student Commons provides billiards, television, ping pong, and the
parks offer picnic tables, basketball and volleyball.
There are also numerous tennis courts, golf courses, ski slopes, and hiking trails in the immediate area.
Upon request, discount cards for all major southern California amusement parks are available in the
Student Affairs Office.
Community Activities
The Western University "This Week," which is updated every week, lists Western University seminars
and events that are open to students, faculty, staff and families.
Area colleges publish monthly calendars of social, cultural and educational events that are posted on the
student bulletin board behind the lecture halls. Events are usually open to the public.
Student Government
Over 35 organizations have been established within the student body. The umbrella for all of the other
organizations is the Student Government Association, which is charged with official representation of the
student body.
Student Government Association - Students are encouraged, individually and collectively, to express
their views on issues and administrative policy on campus. Through the elected representatives of the
student body and membership on various University committees, students have the opportunity to
participate in the administrative activities of the University. This body represents the students in all matters
of concern with regard to faculty and administration.
The objective of the Student Government Association is:
a. To act as elected representatives of the student body in all matters with regard to the
faculty, administration, fellow professionals and the public-at-large.
b. To ascertain and express student opinion in matters pertaining to the University.
c. To formulate and execute policy on matters relative to the student body.
d. To budget and disburse funds for student activities or other related functions.
e. To organize and implement various educational, social and community service projects.
Students are invited to select representatives on the following University committees:
Commencement Committee - The purpose of this committee is to plan and, in some areas, implement
the University's graduation ceremony and related events. The committee submits to the President the results
of its deliberations for this consideration and approval. The committee and its chair are appointed by the
10
President. The Student Government Association President and the President (or an appointee) of the MSIV
class are also voting members.
Financial Aid Committee - Student Body Treasurer, PAI Class Treasurer, MSII Class Treasurer,
PharmDII Class Treasurer and MPTI Class Treasurer, will be voting members. The student members may
be excluded from certain meetings if the discussion includes confidential material from other students' files.
The duties of this Committee are to select students for scholarships and assist the Director of Financial Aid
in formulating policy regarding financial aid programs. The Committee is comprised of faculty
representatives, the Dean of Student Affairs, the Director of Financial Aid and two students.
The Humanism in Health Sciences Committee - To create a climate for defining, teaching, and
implementing humanism and diversity through various ongoing programs. These programs are grounded in
a philosophy that fosters valuing the diversity and humaneness of persons on our campuses and in our
communities. The committee will support and encourage scholarly activities that promote humanism and
diversity.
Library Committee - One representative from each class on campus will be a voting member. The
duty of the Committee is to advise the Librarian in matters of concern to the faculty and students relevant to
the Library.
University Student Conduct Committee - The function of the Student Conduct Committee is to
investigate alleged violations brought to its attention by the Academic Deans. The Committee may
recommend a course of action if a violation has been identified.
STUDENT ORGANIZATIONS
The following organizations are currently approved and active on campus:
American College of Osteopathic Family Physicians (ACOFP) - Promotes the training of osteopathic
family physicians and provides a better understanding of the scope of services rendered by the osteopathic
family physician. Advisor Emeritus: Dr. Burton Routman.
The American Medical Women's Association (AMWA) and the National Osteopathic Women
Physicians' Association (NOWPA) - These are two national and on-campus organizations that exist for the
purpose of supporting women in medicine. Our on-campus chapters are very active in supporting women
medical students by hosting both DO and MD speakers, sending members to National Women's Health Care
Conventions, networking through the annual Mentor Dinner, running the Nursery Nutrition Project,
supporting the Los Angeles Babies with AIDS Walk-a-Thon and developing Board Review Notes. In
addition, both organizations have access to low interest student loans, grants and fellowships. Most
importantly, AMWA and NOWPA exist for the purpose of making friends, lending support and rendering
service within our campus and local community. Advisor: TBA
American Pharmaceutical Association-Academy of Students (APhA-ASP) - APhA exists to serve its
members, to enhance pharmacists' abilities to provide pharmaceutical care, and to further the public's
recognition of the pharmacists' value as a health resource. As an academy of APhA, ASP promotes the
professional practice interests of pharmacy students, establishes programs/activities for members, and
provides a means for members to participate in APhA's policy-making process. Advisor: Dr. Joanne
Yasuda.
Asian-American Health Profession Student Association (AAMSA) - Enhances the awareness of the
Asian communities to the osteopathic profession and provides services to the University and Asian
communities. Advisor: Dr. Stanley Wong.
11
Biomedical Research & Literature Club (BIOMED R & L) - Reviews current medical literature and
presents reviews and case studies. Advisor: Dr. James Martin
California Doctors Ought to Care (CAL-DOC) - Through patient education, to get people to stop
smoking, and thereby have them live longer, healthier lives. Advisor: Dr. Richard Sugerman.
California Society of Health-System Pharmacists-Western University (CSHP-Western University)
- The purpose of CSHP-Western University is to provide students an opportunity to become knowledgeable
about pharmacy practices in organized healthcare settings. Advisor: Dr. Kari Franson.
Chicano/Latino Medical Student Association (CMSA) - Serves as part of a statewide communication
and support network for medical and pre-medical students interested in developing health care services for
Hispanic underserved communities. Advisor: Ms. Susan Hanson.
Christian Medical/Dental Society (CMDS) - Encourages and aids Christian students in their spiritual
and professional growth through weekly meetings and other special events. Advisor: Ms. Bonnie MacKay
Digital Medicine Association (DMA) – The purpose of the DMA is to explore the integration of
information technology in health care and to enhance health professions education programs through the
inclusion of informatics. Advisor: Scott Helf, DO
Emergency Medicine Club (EMC) - Promotes the interest and education of students in emergency
medicine and exposes them to a variety of common emergencies. Students will be exposed to practical
procedures they can use in their third and fourth years. Instruction and practice will be provided of
invaluable techniques necessary in the field of emergency medicine. Advisor: Dr. Jonathan Leo; Dr.
Francis Yang
Hillel - Provides access on the Western University campus to Jewish culture. Meets to discuss pertinent
aspects of Jewish life through seminars and invited speakers. Also seeks to establish a link between
students and the surrounding Jewish community. Advisor: Dr. Richard Sugerman.
International Medicine Club - Promotes cross-cultural experience and community involvement to
better appreciate primary care. Students invite physicians to share their experiences in international health.
The club also sponsors medical student foreign exchange through the International Federation Medical
Student Association (IFMSA). Advisor: Dr. Rafi Younoszai.
Islamic Medical Society of Western University - Serves as a religious outlet and meeting place for the
growing number of Muslim students on the Western University campus. Activities include campus
celebrations of two holidays, Eld ul'Fitre, Eld ul'Adha, speakers and a companion program with Pilgrim
Place, a convalescent home in Claremont. Advisors: Drs. Nadir Kahn and Rafi Younoszai.
Latter-Day Saints Student Association (LDSSA) - This organization was founded to establish and
provide a spiritual balance to medical education through discussions and activities geared to that purpose.
Advisor: Dr. Jonathan Leo.
Los Angeles County Medical Association – Medical Student Section, Western University of Health
Sciences Osteopathic Chapter. The Western U chapter of the LACMA – Medical Student Section promotes
osteopathic principles and practice in Los Angeles County via educational presentations to other health
professionals and potential practitioners. The organization serves educate members about issues pertinent
to the field of medicine and provide students with access to legislative policy surrounding organized
medicine. Students serve on policy-making committees and attend seminars, conventions and political
rallies to insure adequate representation of COMP. Advisor: Michael Jeong, DO
12
Middle Eastern Medical Students Organization (MEMSO) - This organization is to unite students of
Middle Eastern background and promote their cultures on campus. Advisor: Dr. Nadir Khan.
Military Club - The Military Club is open to all students regardless of military affiliation. Those
students on military scholarships will have the opportunity to join student chapters of the Association of
Military Osteopathic Physicians and Surgeons (AMOPS) and the Uniformed Services Academy of Family
Physicians (USAFP). The primary goals of the club are to: provide information concerning rotations,
internships and residencies in military facilities, provide information concerning the practice of osteopathic
medicine and family practice medicine within the armed forces, to provide information concerning life and
opportunities in the military in general. Advisor: Dr. Richard Sugerman.
Montclair Clinic - Students volunteer to provide health services at a "free" clinic in Montclair.
Neocortex Yearbook - A yearbook is published annually for the University. Students write, draw,
design, edit and take photos for the yearbook. Advisor: Ms. Patti Delesante.
Osteopathic Physicians and Surgeons of California - Medical Students Section (OPSC-MSS) -
Provides an avenue for student input to the state medical association and allows early involvement in OPSC.
Helps DO candidates to enhance their career opportunities through collegial relationships with practicing
physicians via participation in CME seminars; clinical preceptorships, and guidance of physician mentors.
Advisor: Dr. Jay Porcelli; Dr. Alan Cundari
Physical Therapy Awareness Club (PTAC) - Provides opportunities for all students to partake in
various PT related lectures, convocations, debate panels including current issues and legislation and
technique demonstrations. Activities include guest speakers, participation in APTA functions and hands-on
treatment techniques. Advisor: Dr. LeeAnne Carrothers.
Pomona Community Health Action Team (PCHAT) - The purpose of this club is to provide and
serve the medical needs of the Pomona Community. Advisors: Dr. Rafi Younoszai and Dr. Burt Routman.
Santa's Workshop - Western University students provide assistance to disadvantaged families during
the holiday season. Advisor: Ms. Gisele Tackoor.
SANUS: The World's Only Osteopathic Theater Troupe - Promotes health through artistic expression.
Theatrical production company composed of production staff and cast who will select two plays to be
presented annually. Advisors: Drs. Jeffrey Felton and Dennis Kiick.
Sigma Sigma Phi - This fraternity was established to provide service to the University and profession
and is the official osteopathic honorary fraternity. It promotes educational programs for the entire student
body and participation in community projects, health fairs, high school athletic physicals and blood pressure
checks. Advisor: Dr. George Charney.
South Asian Student Association (SASA) - The purpose of this organization is to raise awareness of
South Asian Students in osteopathic medicine and to provide an interdisciplinary forum for South Asian
students to share their cultural identity. Advisor: Dr. Nadir Khan.
Sports Medicine Club - The purpose of this group is to provide seminars, speakers and other
educational avenues for students interested in Sports Medicine. Also, to sponsor school and club health
checks, act as liaison to area athletic events and possibly engage in research. Advisor: Dr. Casey Chaney;
Dr. Alan Cundari.
Student Associate Auxiliary (COMPlements-SAA) - COMPlements is the Student Associate
Auxiliary (SAA) for spouses and partners of students and is chartered by the national Auxiliary to the
American Osteopathic Association (AAOA). It has been organized by the Auxiliary to the Osteopathic
13
Physicians and Surgeons of California to further the goals of the University and the osteopathic medical
profession, to serve the local community and to promote fellowship and unity within the school. SAA
COMPlements regularly plans social, cultural and charitable activities for the benefit of the students,
spouses, University and community. Advisor: Mrs. Jeanne Charney.
Student National Medical Association (SNMA) - Fosters a commitment for students to excel and
mentor. Our goal is to produce quality health care team members armed with the knowledge, skill and
insight needed to practice medicine within underrepresented communities. Advisor: Dr. Beverly Guidry.
Student Osteopathic Internal Medicine Association (SOIMA) - the purpose of this organization is to
represent aspiring internists through an early exposure to the field of internal medicine. Advisor: Dr. Kevin
Jenkins.
Student Osteopathic Medical Association (SOMA) - Provides community service to increase
awareness of osteopathic medicine. Sponsors lecturers, blood pressure clinics, etc. Advisor: Dr. Donald
Krpan.
Student Osteopathic Surgical Association (SOSA) - Provides opportunities for all students to learn
about surgery as a career and helps students develop basic skills for their clinical rotations. Activities
include operating room shifts for all interested students and procedure workshops including suturing,
casting, central lines, chest tubes and lumbar puncture. Advisor: Dr. Jonathan Leo.
Undergraduate American Academy of Osteopathy (UAAO) - Promotes the instruction and
understanding of unique osteopathic principles and technique. Guest lecturers are invited to the campus to
speak to members on manipulative therapy and osteopathic philosophy. Advisor: Dr. David Redding
Women's Health Interest Group - To further the interest of students considering a career in Obstetrics
and Gynecology, Family Medicine, or other Primary Care women's health. Advisor: Dr. Kay Kalousek.
Western University of Health Sciences/Physician Assistant Student Society (WUHS/PASS) - To
promote the Physician Assistant profession and represent the University at the national level. Advisor: Mr.
Roy Guizado.
STUDENT EMPLOYMENT
Because of the nature of the academic program of the University, students are urged to use great caution
in seeking employment during the academic year.
The University does have a work-study program for students who qualify. For more information,
contact the Financial Aid Office.
HEALTH SCIENCES LIBRARY AND LEARNING RESOURCES CENTER
Location: Corner of Third and Gibbs Streets – entrance is on Gibbs Street
Hours: Monday – Thursday 7:00 am to 11:00 pm
Friday 7:00 am to 6:00 pm
Saturday, Sunday 11:00 am to 7:00 pm
Study Rooms – The library has seven study rooms that may be used for study groups on a first-come,
first-served basis. Laptops may be used on the first floor or on the second and third floors in the study
rooms only.
14
Audio-Visual Lab – The lab may be used by WesternU students, faculty and staff only. Videos and
slides are available for use with televisions, VCRs, and slide projectors. There are also six computers that
may be used with several CD-ROMs that are available in the Lab.
Computer Lab – This lab may be used by Western University students, faculty and staff. There are
twelve computers that may be used to search the Library’s WebCat (online public catalog), or do research
on the Internet. Workshops will be held in this lab periodically.
Interlibrary Loan – Material not owned by the University Library may be requested via interlibrary loan
by Western University faculty, staff and students. There is a charge for this service.
Borrowing Privileges and Policies – Western University faculty, staff and students are eligible to borrow
library materials. Other interested users may be eligible and should inquire at the Circulation Desk.
• Books: On campus students may check out items for seven days and renew them twice if no one
else has requested the time. Students on rotation and distance education students may check out
items for one month with no renewal. Fines are charged for overdue books. Renewals may be
made by phone. A “hold” may be placed on books that are charged out. You must have your
student ID/employee ID with you in order to borrow books.
• Journals: Bound or unbound journals (periodicals, newsletters, etc.) do not circulate.
Note: More detailed information, especially in regard to library fines and student conduct within the
Library, may be found in the Library Handbook at the Circulation Desk.
CENTER FOR DISABILITY ISSUES AND THE HEALTH PROFESSIONS
(SECOND FLOOR, HEALTH SCIENCES CENTER)
The Center for Disability Issues and the Health Professions assists students with disabilities from the
time of admission to graduation. The Center is located on campus at 309 E. Second Street/College Plaza,
(909) 469-5385 voice, (909) 469-5520 TDD or email bpremo@westernu.edu.
CDIHP Services
Each student at Western University is unique. Only upon consultation with the student, dean and faculty
member can specific plans for accommodations be made. To assist with a documented disability, staff from
CDIHP may communicate, when appropriate, with the instructor and may also ask the student to discuss
his/her needs with the instructor. Decisions on appropriate accommodations, auxiliary aids and/or services
are made following an individualized assessment of each request and after discussion of the options
available with one of the CDHIP staff.
The following is a sample list of the types of services and accommodations that might be provided,
based upon CDIHP’s assessment of each student’s specialized needs:
• academic modifications
• disability management advising
• auxiliary aids
• examination accommodations
• mobility assistance
• physical access and architectural modification (i.e., building platforms or adding disabled parking
spots)
• reader services
• study skills advisement
• taping of academic lectures
• transcription services for specific classes
• extended time for examinations
• a private, quiet, well-lit room for examinations

15
• alternative testing formats
• consultation with staff of CHIHP and professors regarding facilitation of education of students with
disabilities
It is a student’s responsibility to provide timely and sufficient written medical documentation about the
student’s disability or disabilities. Students must check with the Center about documentation requirements.
Students must request services or accommodations directly from the Center, which in consultation with the
student, can recommend the appropriate services or accommodations. There is no charge to students for
services that are specifically needed to support the educational program.
For additional information, contact Ms. Sharon McCrary at (909) 469-5447; TDD (909) 469-5520 or
check the Center’s web page at www.westernu.edu/cdihp
.
OFFICE OF INTERNATIONAL AND CROSS-CULTURAL PROGRAMS
The Office of International and Cross-cultural Programs (OICP) was established in 1989 to promote
student cross-cultural experiences locally and internationally. The program's goals are to:
• Develop foreign-based clinical training opportunities for interested Western University students to
experience primary health care in foreign countries as part of their professional growth;
• Instill in students the knowledge and skill needed to provide quality health promotion and disease
prevention services in cross-cultural settings;
• Develop student and faculty awareness of the principles and goals of the international primary
health care movement and its adaptation locally to improve the status of primary health care in our
communities, the state, and the country;
• Encourage research in cross-cultural primary health care delivery and education in foreign
countries; and
• Advocate for osteopathic approaches to health care delivery and education in foreign countries.
HUMANISM AND THE HEALTH SCIENCES
(BASEMENT, UNIVERSITY ADMINISTRATION CENTER)
In 1996 the University established the Humanism in the Health Sciences Committee. The committee's
working definition of humanism is: Humanism is a way of caring that is fundamental to positive interaction
and is manifested as a responsiveness to the needs of fellow human beings through respect, compassion,
empathy and understanding.
The mission statement of the Humanism in the Health Sciences Committee states: To create a climate for
defining, teaching, and implementing humanism throughout the University. Programs are grounded in the
philosophy, which fosters valuing the diversity and humanness of persons at our locations and in our
communities. The committee will support and encourage scholarly activities that promote humanism.
Activities of the committee include:
• The annual publication of a scholarly journal, Humanism in the Health Sciences, which features
articles, poetry, commentaries and essays. The journal is student run, edited and produced;
• Curriculum development: Belief System and Patient Care Program funded by the National Institute
of HealthCare Research (Course Director, Dr. Mahtab Jafari); and
• Care Teams and Monthly Care Teams News.
STUDENT HOUSING
The University does not provide on-campus or off-campus housing accommodations for its students;
however, there is an off-campus housing referral system to help students locate houses, apartments,
roommates, etc. A local map, the real estate sections of local newspapers, and information on activities in
the surrounding communities are available in the Student Affairs Office. Incoming students may wish to
subscribe to the local newspapers: the Claremont Courier, 111 South College Avenue, Claremont, 91711;
and the Inland Valley Daily Bulletin, 2041 E. 4th Street, Ontario, 91761-1020.
16
All students on clinical rotations are responsible for making their own housing arrangements. Some
hospitals offer housing on a first-come, first-served basis. It is the student's responsibility to contact the
hospital for information regarding availability and cost of housing. The COMP Office of Clinical Rotations
has a housing book available for the perusal of DO students and will assist as much as possible with
guidance regarding housing, but the final responsibility for housing arrangements will be the student's.
Please note: the University provides a housing referral service as a courtesy only. The University assumes
no responsibility for the accuracy of information provided by property owners or other third parties, and
each student should independently verify the condition of any property, its amenities, security arrangements,
etc. Under no circumstances shall the University have any responsibility or be liable for damages, losses,
injuries or liabilities of any nature relating to any housing provided by third parties.
STUDENT PARKING
Students have the option to purchase an annual parking sticker for $180. The purchase of a yearly
parking sticker can be included as part of a student's Financial Aid package, with the submission of a paid
receipt.
The collection of the funds will be conducted by the Bursar's Office, and students will be permitted to
charge the parking fees on their student accounts.
The University will provide full-time security for this parking lot between the hours of 7:00 a.m. to 6:00
p.m. Monday through Friday. If students are planning to be on campus after 6:00 p.m. during the week,
they should move their cars to the Health Sciences Center parking lots after 6:00 p.m. Students should park
their cars in the Health Sciences Center parking lots on Saturdays, Sundays or holidays.
City Parking Lots - Annual parking permits are also available at a significant discount ($140, or
quarterly at $40) through the City of Pomona for those individuals wishing to pay for their parking in this
manner. Applications are available in the Student Affairs Office, or contact the Pomona City Hall
Treasurer's Office, 505 South Garey Avenue, Pomona, CA 91766, (909) 620-2262. Those who elect to
park in the metered lots without a permit will be required to pay 75 cents per day per vehicle.
Parking along the streets is permitted with certain posted restrictions.
Secured bicycle parking is available on the west side of the Student Services building. Motorcycles
must be parked in the parking lots.
PSYCHOLOGICAL COUNSELING SERVICES:
877- WESTRNU (877-937-8768) OR (949) 650-2217
In an effort to respond to the needs of our students, the University has developed a student assistance
program, which provides confidential psychological counseling services for students and their families.
This service is provided by Mental Health Alternatives and assists students with problems of living
(including personal, marital, family, stress, financial and legal issues) that may impair a student’s ability to
perform adequately in his or her professional training program. The service is accessible 24 hours a day,
365 days per year.
Mental Health Alternatives
Dominic J. Bronell, Ph.D.
W. Doyle Edson, Ph.D.
Locations
4B-4 Village Loop Road 881 Dover Drive #390
Phillips Ranch, CA 91766 Newport Beach, CA 92663

17
OFFICE OF LEARNING ENHANCEMENT AND ACADEMIC DEVELOPMENT
(SECOND FLOOR, HEALTH PROFESSIONS CENTER)
The Office of Learning Enhancement and Academic Development (LEAD) is a division of the Office of
Strategic Planning and Institutional Effectiveness. The LEAD Office’s goal is to help each Western
University student successfully complete his or her course of instruction. The Office assists students in
many ways. The Director interviews students in academic difficulty and evaluates their respective
approaches to learning, study and processing information. The Director devises and implements methods to
solve identified barriers to successful learning and aids individual students during their processes of
resolution. The Director plans and implements group workshops to enhance learning skills each year for
students in each Western University program. The Director also prepares and distributes handouts to
students on learning styles, time management, group study, processing information, memory, test
preparation, group study, anxiety and stress management, listening, note taking, comprehension, and critical
reading and thinking. Additional learning enrichment forums, workshops, and the establishment of on-
campus reviews for course exams or licensing/certifying examinations are developed by this Office in
response to the expressed needs and interest of students.
The LEAD Office administers the Tutorial Assistance Program (TAP), working with tutors, tutees, and
the faculty as a team. TAP provides supplemental academic instruction for students in academic difficulty.
Competent and sensitive peer tutors selected by the faculty from each college facilitate course content
instruction. Students are scheduled individually or in small groups to work with a tutor. The LEAD Office
works closely with the tutors and tutees during the tutoring process to ensure that effective tutoring is
maintained.
The LEAD Office assist in the administration of the Summer Anatomy Prematriculation Program
(SAPP). SAPP is a three-week program designed to orient incoming, first-year osteopathic medical students
to the Western University campus and community, and to ease adjustment to the demands of their academic
environment. It serves as a “head-start” for students with little or no background in anatomy. The LEAD
Office endeavors to enhance all students’ sense of belonging by working closely with individual students in
overcoming environmental, social, cultural, or academic barriers that may interfere with their learning.
The LEAD Office serves all Western University students. All academic and personal counseling and
referrals to other campus services are completely confidential. The Director is available for students on a
walk-in basis or appointments can be made by phone or e-mail. The office is located in the Health
Professions Center on the second floor. Office hours are 8:30 a.m. to 4:30 p.m., Monday through Friday.
The Director can be reached by phone at (909) 469-5408 or e-mail dhacker@westernu.edu
.
UNIVERSITY REGISTRAR
(FIRST FLOOR, STUDENT SERVICES CENTER)
STUDENT FILES: PRIVACY AND ACCESS
The Family Educational Rights and Privacy Act of 1974, also known as the Buckley Amendment, (a)
establishes a post-secondary student's general right to inspect and review his/her academic records and (b)
generally prohibits outside parties from obtaining the information contained in such records without the
student's written consent. A student may choose to waive access to certain confidential recommendations
placed in the file.
The paragraphs below delineate the procedures under which Western University will meet the law's
requirements. Western University currently maintains the following types of educational records that are
directly related to its students.
Admissions Files
The Director of Admissions is responsible for maintaining files that contain letters of recommendation
for admission to the University, transcripts of work performed at other institutions, required standardized
test scores, plus the applicant's supplementary application. The Director of Admissions, Members of the
Admissions Committee and the President have access to these files for the purpose of carrying out the
admissions function. After an applicant has been admitted and is actually registered, the files are combined
with those of the Registrar.
18
Registrar's Files
The Registrar is responsible for maintaining files that contain official Western University transcripts and
copies of occasional letters written by faculty and administration, along with students' replies. These letters
generally concern academic progress, examinations, etc. Members of the faculty and administration have
access to the files for use in student advisement. The Registrar also has access to the files to maintain them
and to provide authorized data to authorized persons.
If any material or document in the educational record of the student includes information on other
students, the University will not supply the actual material or document. Instead, only the specific
information contained therein that directly relates to the student seeking access will be provided. In
addition, no student may have access to:
(a) Financial records of parents or any information contained
therein, or
(b) Any confidential recommendations to which the student has
properly waived the right of access.
A student who desires to have any material in the files altered or expunged on the grounds that such
material is inaccurate or misleading, or that is being maintained in violation of his/her right to privacy or
other rights, may obtain a hearing before a special committee. The special committee will be composed of
representatives of students, faculty, and administrators. At the hearing, the student will be afforded a full
and fair opportunity to present evidence relevant to the issues raised. The committee's decision will be made
in writing within a reasonable period of time after the conclusion of the hearing. The committee's
conclusions may then be appealed by means of a complaint filed with the U.S. Department of Education.
Whether or not a student requests a hearing and regardless of the outcome of any such hearing, the student
may in any event insert into his/her files a personal written explanation concerning any material the student
believes is inaccurate, misleading, or otherwise inappropriate.
Reviewing the File
Students and former students may review any of the above files that directly relate to them upon
completion of a form available from the Registrar. On this form the student will specify the records he/she
wishes to examine. The Registrar will then collect the desired material. In no case will access be withheld
more than 45 days after the proper request has been made. If the student wishes, the University will also
supply copies of material in the file at 25 cents per page.
The privacy of student files is and will continue to be scrupulously maintained. Western University will
make public without consent only certain "directory information." This information consists of a student's
name, address, telephone listing, e-mail address, photograph, class schedule, full- or part-time status, date
and place of birth, major field of study, dates of attendance, degrees and awards received, and the most
recent previous educational institution or agency attended by the student. A student who prefers that some
or all of such "directory information" not be made public, must notify the Registrar in writing within ten
(10) days after registration day.
Except for directory information and except as to certain parties listed in the Act, the University will not
release to outsiders any student's file, or information contained in it, unless prior written consent has been
obtained from the student. The outside parties excepted by the Act generally consist of certain federal and
state officials, accrediting organizations and educational agencies who need the information for valid
educational purposes. The University is also authorized to release information contained in a student's file
in any emergency situation involving the need to protect the health or safety of the student or other persons.
A student (or applicant for admission) is permitted to waive access to confidential recommendations
written on his/her behalf regarding, (1) admission to any educational agency or institution, (2) an
application for employment, or (3) the receipt of an honor or honorary recognition.
A student who consents to release to outside parties any part of his/her file must do so in writing,
personally signed and dated. Such writing must specify the records to be released, the reasons for such
release, and the names of the parties to whom such records will be released. A form is available in the
Registrar's Office for this purpose. A student whose consent is required may also request a personal copy of
the specific records in question. As stated previously, there is a copying fee.
The University will maintain a record identifying all outside parties who have requested or obtained
access to a student's educational records and the specific interest they had in obtaining such access. This
19
record will be available only to the student and to the University officials previously named who are
responsible for maintaining the various files.
All such records are made available to students with the following limitations:
a. Recommendations submitted to the department by third parties under conditions of confidence,
e.g., letters of recommendation, will be shown only upon receipt of a signed release by the third
party;
b. Student records requiring the interpretation of a professional, i.e., medical, psychiatric,
psychological testing, etc., must be reviewed in consultation with the appropriate professional;
c. Generally, the school must have written permission from the student before releasing any
information from a student's record. However, the law allows schools to disclose records, without
consent, to the following parties:
• School employees who have a need-to-know
• Other schools to which a student is transferring
• Certain government officials in order to carry out lawful
functions
• Appropriate parties in connection with financial aid to a
student
• Organizations doing certain studies for the school
• Accrediting organizations
• Individuals who have obtained court orders or subpoenas
• Persons who need to know in cases of health and safety
emergencies
• State and local authorities to whom disclosure is required by state laws adopted before
November 19, 1974.
Three items of information from student records are considered "public" information:
• the fact of attendance
• the dates of attendance and
• the fact and date of graduation
With the exception of the above, no other student record information is divulged or released to persons
or agencies outside the University without the expressed written request or authorization of the student.
d. Under certain circumstances, the program may request written permission of the student to provide
demographic data such as names, addresses, etc., to persons or agencies outside the University
conducting research or other scholarly activities.
Records of students and graduates are maintained by the program in accordance with University rules.
The original application and supporting materials are maintained by the Registrar. In addition, the program
maintains an academic profile record for each student, including information related to academic and
clinical performance in all phases of the program. Course grades are recorded on the appropriate profile
sheet as soon as computed. This file is maintained for department and student use. It is NOT meant to serve
as an official record of grades. Final course grades are submitted to the University Registrar and only then
become part of the official record/transcripts.
Transcripts of the work completed are maintained and may be requested from the University Registrar.
TRANSCRIPTS
Enrolled students will receive one unofficial copy of their transcripts after grades have been posted at
the conclusion of each academic year. No verbal grades or class ranks will be given at any time. A grade
change report will be generated upon request whenever a grade change occurs.
No grade will be changed unless the instructor certifies in writing to the Registrar that an error occurred
in computing or recording the grade or that the student has remediated an Unsatisfactory grade after being
directed to do so by the appropriate Academic Dean as recommended by the committee in each respective
College responsible for student academic progress. All recorded grades remain on the official transcript
unless a clerical error occurs. Remediated grades are recorded below a grade of "U" or "I". Only the
remediated grade is calculated into the GPA.
20
To request an official transcript, a form must be completed in the Registrar's Office. There is a $5.00
fee for an official transcript. Official transcripts are mailed directly to the recipient by the University.
Official transcripts bear the signature of the Registrar and the seal of the University. In extreme
emergencies, transcripts may be faxed for a fee of $10.00, provided that a Fax Disclaimer form is
completed and the fee is paid. Transcripts will not be provided to students who are delinquent in their
financial obligations to the University, including the Library, or to any of its affiliated hospitals or clinics.
Transcript requests will be processed within two weeks. If the University has knowledge that a student or
graduate is in default on any federal, state, outside agency, institutional loan or service obligation, the
University will withhold all official transcripts, State or National Board Scores, and letters of
recommendation for internships, residencies, employment, staff privileges, specialty certification, and
licensing. Remember to allow two weeks for processing of transcript requests.
DIPLOMAS
Diplomas will be issued approximately six to eight weeks after the Registrar receives all final grades
verifying that a student has completed all academic requirements for a specific program.
CLASS RANK
Student's class ranking, with the exception of MSHPE, FNP/MSN and PharmD, may be obtained from
the Registrar's Office in writing, with appropriate identification. The class ranking is based on letter grades
and/or percentages.
21
UNIVERSITY POLICIES AND PROCEDURES
NON-DISCRIMINATION
The Western University of Health Sciences, in compliance with Titles VI and VII of the Civil Rights Act
of 1964, Title IX of the Education Amendments of 1972, Sections 503 and 504 of the Rehabilitation Act of
1973, and Sections 102 and 302 of the Americans With Disabilities Act of 1990, does not discriminate on
the basis of race, color, national origin, religion, handicap or sexual orientation in any of its policies,
procedures, or practices. In accordance with sex discrimination laws, the University will not tolerate acts of
sexual harassment. In compliance with the Age Discrimination in Employment Act of 1967, Section 402 of
the Vietnam Era Veterans Readjustment Act of 1974, and Section 12940 of the State of California
Government Code, the University does not discriminate against any employees or applicants for
employment on the basis of age, ethnic origin, marital status, sexual orientation, or because of their status as
disabled veterans or veterans of the Vietnam Era, or because of medical condition (as defined in Section
12926 of the California Government Code); nor does the University discriminate on the basis of citizenship,
within the limits imposed by law. This non-discrimination policy covers admission, access, and service in
the University programs and activities, and application for and treatment in University employment.
Discrimination Complaint Procedure
Any student believing that he/she has been discriminated against in violation of the above policy of non-
discrimination may file a complaint with the Dean of Student Affairs or her designee. Complaint forms may
be obtained from the Dean of Student Affairs office. Retaliation against a person who reports, complains
about, or participates in the investigation of alleged discrimination is prohibited. A student who believes
that he/she is the victim of sexual harassment should follow the procedures specified in Western
University's Sexual Harassment Policy (See below).
All complaints of discrimination shall be investigated promptly and resolved equitably. The Dean of
Student Affairs will refer the matter to the appropriate Academic Dean, the Executive Vice President for
Academic Affairs/CAO, or to the Executive Vice President of Finance and Administration, (the
"responsible official"), depending upon the nature of the discrimination that is believed to have occurred.
The responsible official will investigate the complaint, and make a decision with regard thereto. The
responsible official may appoint an ad hoc committee to conduct a hearing, and to make recommendations
concerning any corrective action to be taken. The responsible official, taking into consideration the
recommendations of the ad hoc committee (if applicable), will decide, in writing, what action is appropriate
under the circumstances.
If a student is dissatisfied with the decision of the responsible official, he/she may appeal the decision to
the President. The appeal shall be made, in writing, within seven working days of the written decision of
the responsible official, and shall state any reasons why the person filing the appeal believes that the
decision of the responsible official is incorrect. The President may affirm or reverse the decision, modify
the action to be taken, or remand the matter for further proceedings. For purposes of action to be taken by
Western University, the decision of the President shall be final. Any person who believes that he/she has
been the victim of discrimination is, however, entitled to file a complaint with an applicable state or federal
agency at any time during Western University's proceedings.
UNIVERSITY FACILITIES, RESOURCES, AND SERVICES FOR
STUDENTS WITH DISABILITIES
General Policy:
The University endeavors to provide a welcoming and supportive community environment for students
with disabilities.
Western University is committed to the fundamental principles of non-discrimination and
accommodation in all of its academic programs as set forth in the Rehabilitation Act of 1973 and the
Americans with Disabilities Act of 1990. These laws establish that students with disabilities may not, on
the basis of their disabilities, be excluded from participation in, be denied the benefits of, or otherwise be
subjected to discrimination under any program or activity at Western University.
22
In that spirit, the University acknowledges its obligations to make reasonable adjustments and
accommodations to provide students with disabilities access to its programs in the most integrated setting
possible.
1. Programs and Facilities:
a. While the University cannot provide a totally barrier-free environment, it does provide students
with disabilities access to its programs and activities. Thus, while not every academic and nonacademic
building is fully accessible, sufficient access exists to allow students with disabilities the equal
opportunity to participate in the academic and social life of the University.
b. Although the University endeavors to make its programs accessible to individuals with
disabilities, it recognizes that some disabilities may preclude an individual from successfully completing
a given academic program. To provide guidance to individuals with disabilities, the University provides
a description of what it considers to be the Minimum Technical Standards for Admission and
Matriculation to each of its programs. Because it is not possible to address every possible circumstance,
these Minimum Technical Standards should be considered as guidelines. Any student with a disability
who believes that he or she is unable to meet the Minimum Technical Standards, but believes that a
reasonable accommodation will permit that student to complete the program successfully, should contact
the Learning Enhancement and Academic Development Office (LEAD) as soon after admission as
possible. The University will determine whether it is appropriate to modify its Minimum Technical
Standards.
c. As soon after admission to the University as possible, students with disabilities should contact
the Learning Enhancement and Academic Development Office, which serves to coordinate disability
services and to discuss any reasonable accommodation that may be required. Each case is dealt with on
an individual basis.
d. Since the University is prohibited by law from making pre-admission inquiries regarding
disability, the University relies on the voluntary provision of whatever information it needs to make
reasonable accommodation for students with disabilities.
2. Resources, Services, and Auxiliary Aids:
The University provides certain services and reasonable accommodations, the nature and extent of
which are based on the Center for Disability Issues and the Health Profession's assessment of individual
need to achieve academic success. Those services and accommodations, provided in consultation with the
student, are intended to allow qualified students with disabilities to pursue their educational careers in the
most equitable and independent fashion possible.
3. Accessibility and Construction:
The Western University of Health Sciences, in compliance with sections 503 and 504 of the
Rehabilitation Act of 1973, and in compliance with the Americans with Disabilities Act of 1990, does not
discriminate on the basis of disability in any of its policies, procedures or practices. It is the policy of the
University to provide qualified persons with disabilities with access to its programs in the most integrated
setting possible. The following statement on construction, renovation, and alteration flows from the spirit
of that non-discrimination principle.
a. Construction of New Buildings and Facilities:
1. New construction will comply with the guidelines and regulations set forth in
Section 504, Title 234, and relevant state and local building codes. The primary standards for such
construction are derived from the Uniform Federal Accessibility Standards (UFAS, 1984), the
Amended Architectural Barriers Act (1984), and the Americans With Disabilities Act of 1990.
2. The University endeavors to employ the most barrier-free design and materials
in new construction to provide superior access to the functions and programs that take place in
those new facilities. The University's goal is to ensure full accessibility and usability of its new
buildings.
b. Renovation and Alteration of Existing Buildings and Facilities:
1. The renovation and alteration of existing facilities will comply with Section 504 and
applicable federal regulations, as well as relevant state and local codes, to enhance program
accessibility. The University recognizes that Section 504 does not require structural changes to
existing facilities where other methods are effective in achieving overall accessibility to the
programs and services of the University.
23
2. Any renovation or alteration will, to the maximum extent feasible, be pursued in
a way that makes the renovated or altered portion of the building accessible to a student with a
disability. However, the design of many existing facilities makes it impractical or prohibitively
expensive to renovate or alter them in such a way as to make them barrier-free.
SEXUAL HARASSMENT
It is the policy of Western University that all persons, regardless of their gender, should enjoy freedom
from discrimination of any kind. Sexual harassment is a form of sexual discrimination, and Western
University will not tolerate such conduct by any member of the University community.
For purposes of this policy, "sexual harassment" means unwelcome sexual advances, requests for sexual
favors, and other verbal, visual, or physical conduct of a sexual nature, made by someone from or in the
educational setting, under any of the following circumstances:
1. Submission to the conduct is explicitly or implicitly made a term or a condition of an
individual's employment, academic status, or progress.
2. Submission to, or rejection of, the conduct by the individual is used as a basis of employment or
academic decisions affecting the individual.
3. The conduct has the purpose or effect of having a negative impact upon the individual's work or
academic performance, or of creating an intimidating, hostile, or offensive work or educational
environment.
4. Submission to, or rejection of, the conduct by the individual is used as the basis for any
decision affecting the individual regarding benefits and services, honors, programs, or activities
available at or through Western University.
5. Creating, transmitting, uploading, or downloading obscene materials not intended for academic
use is strictly prohibited.
Examples of sexual harassment include, but are not limited to: pressure, subtle or overt, for sexual
favors, accompanied by implied or overt threats concerning one's job, grades, or letters of recommendation;
inappropriate display of sexually suggestive objects or pictures; unnecessary touching, pinching, patting or
the constant brushing against another's body; use of sexually abusive language (including remarks about a
person's clothing, body or bodily movement, or sexual activities).
Any student believing that he/she has experienced sexual harassment should resist such harassment and
may file a complaint with the Dean of Student Affairs, or her designee. Complaint forms may be obtained
from the Dean of Student Affairs' office.
To protect all parties involved, Western University handles sexual harassment complaints as
confidentially as the circumstances permit. If the student believes that any official specified in these
procedures was involved in any act of sexual harassment, he/she may file a complaint with another
appropriate official specified in these procedures. Retaliation against a person who reports, complains
about, or participates in the investigations of sexual harassment is prohibited.
All complaints of sexual harassment shall be investigated promptly and resolved equitably. Charges of
sexual harassment may be handled through formal procedures, or, with the consent of both the complaining
party and the alleged harasser, through informal procedures. Informal resolution of a charge of sexual
harassment may take any of the following forms:
a. A meeting among the Dean of Student Affairs, or her designee, the complainant, and the alleged
harasser;
b. A meeting among the Dean of Student Affairs, or her designee, and the alleged harasser; or
c. A recommendation of professional counseling for either principal.
If a formal grievance procedure is requested by either the complainant or the alleged harasser, the Dean
of Student Affairs will refer the matter to an appropriate official of Western University, as follows:
a. In the case of an offending student, the complaint will be directed to the appropriate Academic
Dean. The responsible official will investigate the complaint, and may refer the matter to the Student
Conduct Committee. In this event, the hearing and appeal procedures applicable to the Student Conduct
Committee shall apply.
b. In all other cases regarding administrators, faculty or staff, the complaint will be made to the
Executive Vice President for Academic Affairs/CAO, the Executive Vice President of Finance and
24
Administration, or the Director of Human Resources. The responsible official may appoint an ad hoc
committee to conduct a hearing, and to make recommendations concerning the appropriate disciplinary
action to be taken if the alleged harasser is found to have violated Western University's policy against
sexual harassment. Both the complainant and the alleged harasser will be given notice of, and an
opportunity to participate in, any hearing by the ad hoc committee.
Except for matters referred to the Student Conduct Committee, the responsible official, taking into
consideration the recommendations of the ad hoc committee (if applicable), will decide, in writing, what
action is appropriate under the circumstances. If either the complainant or the alleged harasser is
dissatisfied with the decision of the responsible official, he/she may appeal the decision to the President.
The appeal shall be made, in writing, within seven working days of the written decision of the responsible
official, and shall state any reasons why the person filing the appeal believes that the decision of the
responsible official is incorrect. The President may affirm or reverse the decision, modify the action to be
taken, or remand the matter for further proceedings. For purposes of action to be taken by Western
University, the decision of the President shall be final. Any person who believes that he/she has been the
victim of sexual harassment at Western University is, however, entitled to file a complaint with an
applicable state or federal agency at any time during Western University's proceedings.
DRUG-FREE ENVIRONMENT
Western University is committed to maintaining a drug-free environment in compliance with applicable
laws. The unlawful possession, use, distribution, sale or manufacture of controlled substances is prohibited
on the University's campuses or any of its medical facilities. Violation of this policy may result in the
appropriate disciplinary action up to and including termination or dismissal.
The illegal use of controlled substances can injure the health of fellow students seriously; adversely
impair the performance of their responsibilities; and endanger the safety and well being of other students
and members of the general public. Therefore, the University urges students engaged in the illegal use of
controlled substances to seek professional advice and treatment. Any student who has a drug problem is
invited to contact the Student Affairs Office anonymously at (909) 469-5341, to obtain information about
available assistance. The Western University counseling center, (contact the Student Affairs Office for
name and phone number), offers assistance to students. Students are encouraged to check with their private
insurance carrier for available programs. For those with Western University insurance, the name and phone
number for the insurance carrier is Renaissance, (800) 537-1777.
No one is immune from state or federal laws regarding the use of drugs. Anyone using drugs runs the
risk of legal action and court conviction. Examples of local and state laws are listed below:
• Unlawful possession of a narcotic drug is punishable by imprisonment in the state prison.
• The purchase, possession or consumption of any alcoholic beverage (including beer and wine) by
any person under the age of 21 is prohibited.
• It is not permissible to provide alcohol to a person under the age of 21.
• Selling, either directly or indirectly, any alcoholic beverage to anyone, except under the authority
of the California alcoholic beverage control license, is prohibited.
• It is a felony to induce another person to take various drugs and "intoxicating agents" with the
intent of enabling oneself or the drugged person to commit a felony. The person who induced the other
may be a principal in any crime committed.
• It is a misdemeanor for any person found to be under the influence of an intoxicating liquor or drug
in a public place and unable to care for his/her own safety or disorderly conduct.
As a condition of employment, an employee of the University, including any work-study students, shall
notify his/her supervisor if he/she is convicted of a criminal drug offense occurring in the workplace within
five days of the conviction. Failure to report a conviction may be grounds for dismissal. In the event that
25
any such conviction involves an employee working on a federal grant or contract, the University is
obligated to notify the granting or contracting federal agency within ten days of receiving notice of the
conviction.
Students are required to notify the Dean of Student Affairs within five days of a conviction if they are
convicted of a criminal alcohol or drug offense occurring on the campus. For the purpose of this policy,
"campus" includes all experiential sites. Remedial actions and/or sanctions may be applied, up to and
including dismissal.
Students who are Pell Grant recipients must report convictions for criminal drug violations, occurring on
or off campus, in writing to the Director of Grants and Contracts Service at the U.S. Department of
Education within 10 calendar days of such conviction.
This statement is being set in accordance with the Drug-Free Workplace Act of 1988 (Public Law 100-
690) and the Drug-Free Schools and Communities Act Amendments of 1989 (Public Law Nos. 101-226,
103 stat 1928 - enacted December 12, 1989). The University will continue its efforts to maintain a drug-
free environment by adhering to the above policy and providing drug awareness programs.
STUDENT HEALTH AND SAFETY
Matriculants into Western University's health professions programs must submit evidence that they are
in good health and should, therefore, be able to withstand the physical and mental pressures commonly
placed upon professional students. The nature of health professions education necessarily brings students in
close contact with a variety of illnesses and diseases, and the following policy has been established as a
protective mechanism for students and patients alike. Students must maintain a health insurance policy for
the duration of their education at Western University. Proof of such coverage is required at the time of each
registration. Health insurance is available through the University at a reasonable cost.
DRESS CODE/IDENTIFICATION
Students are required to dress in a professional manner at all times.
During classroom lectures, students are required to wear clothing that is in good repair (no patches).
Footwear is required at all times. Dress for skills labs should not be worn outside the laboratory area. Tank
tops, halters, scrubsuits and headgear (hats/helmets) are not to be worn in the classrooms. Shorts may be
worn, but no more than 3” above the knee. Hair, beards, and mustaches must be clean, net, trimmed at all
times. Students are expected to conform to the commonly acceptable social standards of personal hygiene.
White clinic jackets must be worn at Honors Day, Awareness Conferences, Health Fairs, and in all
clinical settings.
Name pins must be worn at all times on rotations. University identification badges are also provided
and must be worn at all times while on campus.
Students must dress professionally throughout the duration of every clinical rotation/assignment unless
the preceptor of that rotation/assignment directs otherwise.
Exceptions to the dress code may be requested from the appropriate Academic Dean.
SMOKING
As a graduate university of medical health sciences committed to training and educating health care
professionals, we have a responsibility to be a role model for proper health maintenance and prevention.
We are concerned about the health and well-being of all individuals who learn and work here, as well as
those who visit. Out of respect and loyalty to the University, its mission and its constituents, smoking is not
permitted inside campus buildings, health care facilities where patient care is delivered, or inside University
vehicles.
REQUIRED IMMUNIZATIONS
Since students will have some exposure to patients during the first year, NO STUDENTS WILL BE
ALLOWED TO MATRICULATE UNTIL THEY HAVE SUPPLIED PROOF THAT THEY ARE
26
CURRENT ON THE FOLLOWING IMMUNIZATIONS AND HEALTH SCREENINGS: MMR
(measles, mumps, rubella) (proof of immunization or serologic titers showing immunity), Polio,
Tetanus/Diphtheria (within 10 years), Hepatitis B (proof of completion of 3 shot series or serologic titers
showing immunity), P.P.D. (Purified Protein Derivative) (within the last six months) or chest x-ray (within
the last year), Varicella (chicken pox) - proof of completion of the age appropriate immunization series or
positive serologic titers. These immunizations/tests may require updating on a more frequent basis prior to
beginning clinical training if specified in the affiliation agreement with the clinical training site. POSITIVE
PPD OR CHEST X-RAY MUST BE FOLLOWED UP AT THE UNIVERSITY CLINIC.
Such proof is not required for an individual who submits an affidavit or certificate signed by a physician,
duly registered and licensed to practice in the United States, in which it is stated that, in the physician's
opinion, the immunization required would be injurious to the health and well-being of the student or any
member of his or her family or household. Unless a lifelong condition is specified, the affidavit or
certificate is valid for only one year from the date signed by the physician and must be renewed each year
for the exclusion to remain in effect.
No student will be permitted to register or attend classes without having proof of completing required
immunizations.
FOOD IN LECTURE HALLS, LABORATORIES AND LIBRARY
Food is not allowed in the lecture halls or laboratories. Drinks in closed containers are permitted.
Occasionally, noon-hour lectures or seminars are scheduled in lecture halls. At these times, students are
permitted to bring their lunches; however, care must be taken to dispose of all refuse in trash containers
after the lecture. The student lounges may be used for eating.
No food or drink is allowed in the Library at any time.
27
GENERAL ACADEMIC POLICIES AND PROCEDURES
The University endeavors to provide an environment in which students may develop into effective health
care providers. Freedom of inquiry and expression are essential to a learning environment. Students are
encouraged to develop a capacity for critical judgment and engage in an independent search for truth. The
responsibility for securing an environment conducive to freedom of inquiry and learning is shared by the
students, faculty and administration. As a part of that shared responsibility, the University has adopted
Standards of Academic and Professional Conduct.
Educational Philosophy
The educational programs of Western University are based on the belief that schooling not be allowed to
get in the way of education and that the content and substance of the curriculum, as well as the instructional
and planning processes used to carry it out, reflect a humanistic approach. In short, the University strives to
provide people-oriented programs so that its students become people-centered practitioners.
1. Standards of Academic and Professional Conduct
Complete confidence in the honor and integrity of the health professions student and health care
professional is essential. Such confidence depends entirely on the exemplary behavior of the individual
health care provider in his or her relations with patients. Strict honesty as a personal way of life should be
nurtured during the period of education for professional service. The student shall conduct all aspects of his
or her life with honor and integrity. This includes accountability to oneself and to relationships with fellow
students, future colleagues, faculty, and patients who come under the student's care and contribute to his or
her training and growth.
Upon accepting admission to the University, each student subscribes to and pledges complete
observance to the Standards of Academic and Professional Conduct as outlined in this Catalog. A violation
of these standards is an abuse of the trust placed in every student and could lead to suspension or dismissal.
2. Orientation/Registration
Attendance at Orientation is mandatory for all incoming first-year students for the DO, PharmD, MPT,
MSPA, and MSN/FNP programs.
a. Students will be required to register in person on the registration day specified in the University
Calendar or as otherwise directed by the Registrar. Assessed tuition and fees and all prior debts must be
paid in full on or before registration day each academic year.
b. Matriculation is subject to satisfactory completion of all academic requirements and payment of all
outstanding debts to the University.
c. The receipt of final transcripts from undergraduate colleges and a physical examination with
documentation of required immunizations are additional requirements for incoming students.
d. All DO, MPT, MSPA, PharmD and MSN/FNP students must show proof of current health insurance
coverage at the time of registration. This coverage must be maintained in effect throughout the period of
matriculation at Western University. If there is no proof of current coverage, a health insurance policy
provided by the University is available.
3. Withdrawal from University/Program
Matriculation at the University is a privilege granted in consideration of specified levels of performance
and of maintaining the established standards of scholarship and personal and professional conduct. The
University reserves the right to require withdrawal at any time it deems necessary to safeguard its standards
of scholarship, conduct and orderly operation. The student concedes this right by act of matriculation. See
Program Specific sections of this Catalog.
Application for voluntary withdrawal from the University/Program must be made in writing to the
appropriate Academic Dean. Except in rare and special circumstances, the application will be accompanied
by a personal interview. Every effort should be made by the student to assure that no misunderstandings or
errors occur in the withdrawal process. Students who leave the University/Program without notifying the
office of the Dean and the office of the Registrar, and without completing the established withdrawal
procedures within 30 days, will be terminated automatically from the University.
28
In addition, students must report to the Registrar's Office to sign the withdrawal form to officially
withdraw from the University/Program. Students who do not complete this application for voluntary
withdrawal will not be considered for re-admission at a later date.
Students who withdraw "in good academic standing" are not assured of re-admission unless it is a part of
the final decision and/or agreement made between the appropriate Academic Dean and the withdrawing
student. This final decision and/or agreement must be in writing so that it is clear to all parties involved.
Students who are granted re-admission following withdrawal in good academic standing usually re-enter at
the beginning of the next academic year and register for all courses scheduled during the academic year of
their withdrawal, including those previously completed and passed, unless so stipulated.
Students who withdraw "not in good academic standing" must request re-admission through the
University's Admissions Application process unless otherwise stipulated.
4. Leave of Absence
A student may request a Leave of Absence with the occurrence of a medical problem, serious personal
problems, or health related issues.
Students requesting a Leave of Absence must apply in writing to the appropriate Academic Dean. In the
event of a medical problem, the request must be accompanied by a letter from a physician describing the
nature of the disability for which the leave is requested and the estimated length of time needed for
recovery.
After consultation with the student, the respective Academic Dean will decide whether or not the leave is
to be granted and the conditions under which the student may return to school. A student requesting a leave
of absence during or at the end of the academic year must go through the following procedure:
a. In writing, request a Leave of Absence from the appropriate Academic Dean.
b. Obtain a Leave of Absence form from the Registrar. After completing the student’s portion, meet
personally with the appropriate Academic Dean or designee to discuss the reason for the leave. After
consulting with the appropriate Academic Dean/designee, the Dean/designee will sign the Leave of
Absence form indicating his/her approval to proceed with the remainder of the exit process.
c. Take the form to the faculty advisor, who will provide counsel and sign the form.
d. Take the signed Leave of Absence form to the other listed administrative officials for their
signatures.
e. Return the signed form to the Registrar, who will sign and date the Leave of Absence form.
Provided the leave of absence is approved, the official date of the leave of absence will be the original
date of receipt of the student's request and any tuition charged will be in accordance with the institution's
refund policy.
Leaves of absence requested for a full academic year will be for one year only with expected
reinstatement at registration for the following year. Leaves of absence requested after registration for any
given academic year will be granted for a period not to exceed the number of months remaining until the
registration date for the next academic year. During the leave of absence, students are entitled to library
privileges, use of the student lounges, and participation in student clubs. It is required that the student
maintains a health insurance plan throughout the period of the leave.
A student who is granted a leave of absence for one year or more, must submit a letter of intent to re-
enroll to the appropriate Academic Dean, at least three months prior to the requested date of return. The
letter must also be accompanied by a $500 tuition deposit. It is the student's responsibility to keep the
Registrar informed of any change of address while on a leave of absence.
If the student has not paid 100% of the tuition during the year in which the leave is granted, the balance
of the tuition plus any increase of tuition or fees will be payable in the next year of attendance. All
appropriate tuition and mandatory fees are due prior to graduation.
Leaves of absence will be limited to a maximum of 2 years.
The term and conditions of any leave will be determined by the appropriate Academic Dean.
5. Academic Advisement
Students will be assigned a faculty advisor upon matriculation. Advisement by a faculty advisor should
be viewed by the student as a part of the academic process. If either the student or faculty member does not
find the relationship helpful, either is free to seek a change. This request should be made to the appropriate
29
Academic Dean or designee. It is the student's responsibility to meet periodically with his/her advisor. A
student on probation must contact his/her faculty advisor at least once a month.
6. Attendance and Absences
Attendance is required at all scheduled instructional periods. Absence from instructional periods for any
reason does not relieve the student from responsibility for the material covered during the periods missed.
7. Student Academic Progress Committee
See the appropriate Program Specific section of this catalogue.
8. Standards of Professional Conduct: Statement and Procedures
Complete confidence in the honor and integrity of the health professional is essential. Such confidence
depends entirely on the exemplary behavior of the individual in his/her relations with patients, faculty and
colleagues. Strict honesty as a personal way of life should be nurtured during the period of education for
professional service.
The student shall conduct all aspects of his/her life with honor and integrity. This includes
accountability to oneself, to relations with fellow students, future colleagues, faculty and patients who come
under the student's care or contribute to his/her training and growth, and members of the general public.
This applies to personal conduct that reflects on the student's honesty and integrity in both academic and
non-academic settings, whether or not involving a University sponsored activity.
Professional Concerns - Upon accepting admission to the University, each student agrees to abide by
basic standards of honesty and academic integrity. Students should only matriculate here if they agree with
these basic standards. They include, but are not limited to, the following:
a. A student never represents the work of others as his/her own.
b. A student should acknowledge the other members of the group when work is carried out jointly.
c. A student never gives or receives assistance during an exam.
d. A student is always accountable to clinical faculty while on clinical training.
Acts of dishonesty, invasion of privacy, theft, acts of violence, sexual harassment and disrespect for
personal and University property are examples of unacceptable behavior.
The administration, faculty and staff are here to serve the students. Personal gifts are discouraged, and
monetary gifts are prohibited.
Reporting Alleged Violations - Upon witnessing a possible professional violation, any member of the
academic community should report the incident to the respective Academic Dean or other appropriate
University official. If the conduct involves a particular course of program, the classroom instructor or the
clinical training program supervisor should be advised. Depending on the nature of the conduct, an
individual witnessing a possible violation may choose to talk to the transgressor on an individual basis to
attempt to resolve the problem before reporting it to University officials. The individual receiving the
report will dispose of the violation in an appropriate manner. If there appears to be adequate cause, a report
should be submitted in writing to the appropriate Academic Dean. The report should include the name and
signature of the individual making the report.
In most circumstances, the Academic Dean will meet with the student to discuss the nature of the
possible violations that have been reported and the actions, if any, that the Dean intends to take. The Dean
may resolve the matter without convening a hearing before the Student Conduct Committee, unless the
student requests that a hearing be convened. In some circumstances, the Academic Dean or the Executive
Vice President for Academic Affairs/Chief Academic Officer may refer the matter directly to the Student
Conduct Committee for hearing.
When a matter is referred to the Student Conduct Committee, the University shall prepare appropriate
written charges based on all information reported or known. Any appropriate representative of the
University acting with the consent of the Dean or the Executive Vice President of Academic Affairs/Chief
Academic Officer may prepare the written charges. The Chair of the Student Conduct Committee, or the
chairperson of the hearing panel that will hear the matter, will notify the student of the time and date of the
hearing and shall provide the student with a copy of the written charges.

30
9. Student Conduct Committee
Purpose - The Student Conduct Committee considers violations of the Standards of Professional
Conduct when requested by the respective Academic Dean.
Composition - The Student Conduct Committee is composed of six elected faculty members. The Dean
of Student Affairs is a non-voting, ex officio
member of the committee. When the Dean of Student Affairs
is absent or unavailable, a designated representative will participate in Student Conduct Committee
proceedings or hearings. Student representatives shall participate as members of hearing panels when a
matter concerning a student is referred to the Student Conduct Committee for hearing.
Hearing Panels - When a matter concerning a student is referred to the Student Conduct Committee, it
will be determined by a hearing panel comprised of three faculty members serving on the Student Conduct
Committee and two student representatives. Student representatives shall be from the same College as the
student involved, and shall be selected from the Vice Presidents and Secretaries of each class on campus.
The Chair of the Student Conduct Committee shall appoint the individuals who will serve on the hearing
panel, and shall designate one member of the hearing panel as its Chairperson. If it is not reasonably
feasible for the Chair of the Student Conduct Committee to appoint hearing panel members from the
foregoing individuals, either because of a conflict of interest or for any other reason, the Chair may appoint
alternate faculty members or student representatives to serve on the hearing panel. The Dean of Student
Affairs, or a representative of the Dean of Student Affairs, is entitled and normally participates as a non-
voting, ex officio
member of each hearing panel. Each hearing panel acts with the full authority of the
Student Conduct Committee, and the hearing panel's determination constitutes the determination of the
Student Conduct Committee as a whole.
Protocol for Meetings on Alleged Violations of Professional Conduct -
a. The chairperson of the Student Conduct Committee, or the chairperson of the hearing panel, will
notify the student in writing of the specific charges and the time and date of the hearing when the
charges will be considered. The notice also shall state whether expulsion from the University may be
considered if the charges are found to be true.
b. Except as provided below, the meeting will be closed to all individuals not directly involved. The
hearing panel may exclude witnesses, except during the time they are testifying.
c. If the notice of the hearing states that expulsion from the University will be considered if the charges
are found to be true, or if other circumstances warrant, the student may request permission for a mentor
to appear at the meeting to assist the student. The advisor is normally limited to advising the student and
is not permitted to examine witnesses or otherwise participate directly in the proceeding. However, the
hearing panel may permit the mentor to participate directly where special circumstances are shown that
warrant such participation. The student shall make any request for permission for a mentor to appear or
participate in writing, which shall identify the mentor the student desires and provide any additional
information the student deems relevant to the request. Normally, the chairperson of the hearing panel
will inform the student within three business days of receipt of the request whether the mentor will be
permitted to attend the hearing.
d. If requested, the specific charges will be read to the student by the chairperson of the hearing panel.
If the charges are not read, the charges will be deemed to be those specified in the notice of the hearing.
e. The student may testify and present evidence and witnesses on his/her behalf. The student is subject
to questioning by members of the hearing panel, as are all witnesses.
f. The student may question witnesses called by the hearing panel.
g. The hearing panel may, if it chooses, consider affidavits, declarations and other written statements
and documents. Under normal circumstances, the student shall be provided copies of any such
documents at least two days prior to the hearing. If the student desires to present any written documents,
they must be provided to the hearing panel at least two days prior to the hearing. The hearing panel
shall give such weight to the documents, as it deems appropriate under the circumstances.
h. The chairperson of the hearing panel, at his/her discretion, may continue any hearing if warranted due
to the unavailability of a person considered important to the hearing or due to other circumstances. It
shall be the responsibility of the student to present all evidence he/she deems relevant at the scheduled
hearing unless such evidence cannot be presented due to circumstances beyond the student's control.
i. The hearing panel shall determine whether, based on the evidence presented, it is more likely than not
that the charges made are true.
31
j. The hearing panel determines that the charges are true, it shall also make a recommendation with
respect to sanctions to be imposed. The hearing panel may consider any prior disciplinary action against
the student and any other information it deems pertinent in making a recommendation. The student shall
have the right to present evidence of any mitigating circumstances he/she deems relevant, but such
evidence must normally be submitted within two days of notification to the student that the hearing panel
has found the charges to be true.
k. No deviation from the procedures specified herein shall be grounds for objection by the student
unless the student calls an error to the attention of the hearing panel in time to permit the hearing panel
to conform to the specified procedure. Moreover, procedural deviations shall not be grounds of
objection where, under all of the facts and circumstances, the student has been provided fair notice of
the charges and a fair hearing.
l. The hearing panel will make its recommendations to the appropriate Academic Dean.
Status of Student Pending Action - Pending a determination by the appropriate Academic Dean
following a hearing and a recommendation by a hearing panel of the Student Conduct Committee, the status
of the student will not be altered except for reasons of his/her physical and emotional well being or for
reasons relating to the safety of other students and University personnel. Thereafter, the status of the
student will not be altered pending determination of a timely appeal by the student, except that the
Executive Vice President for Academic Affairs/Chief Academic Officer shall have the discretion and
authority to suspend the student or take other action at any time during the appeal process, if consistent with
the decision of the Academic Dean. The University further reserves the right to withhold the award of any
degree at any time disciplinary charges are pending against a student.
Right of Appeal - See Student Appeal Process
10. Promotion
Promotion is defined as progression from one academic year or program phase to the next.
a. A student will be recommended to the appropriate Academic Dean for promotion by the respective
Student Academic Progress Committee.
b. A student may not be recommended for progression from one academic year to the next with any
outstanding grades of "I", "U", "R", or "NCr" on his/her academic record or with a yearly grade point
average or cumulative percentage score of less than the minimum required for promotion (see
appropriate Program Specific section of this catalogue).
c. When considering a student for promotion, his/her professional, ethical, and personal conduct may
also be taken into consideration (as described under Probation a-3).
d. A student will be promoted provided that all academic, legal and financial requirements of the
University, as stated elsewhere in the University Catalogue, have been satisfied.
11. Probation
a. Probation is defined as a period of time, specified by the appropriate Academic Dean, during which
the student's progress will be closely monitored by the respective Student Academic Progress Committee
and the respective Dean. To monitor a student on probation closely during clinical training, the
individual program reserves the right to assign his/her remaining clinical rotations/assignments. A
student will be placed on probation for any of the following reasons:
1. Inadequate academic progress as determined by the specific Student Academic Progress
Committee (see appropriate Program Specific section of this Catalog).
2. When directed to repeat a year for academic reasons.
3. Seriously deficient ethical, professional, or personal conduct.
Professional and personal conduct includes: attendance, cooperation with instructors, interest
shown in assigned work, attitude toward fellow students and associates and toward personnel of
hospitals, approach to and interaction with patients, as well as personal appearance appropriate to
the circumstances.
32
The terms of probation for ethical, professional, or personal conduct will be specified at the time
the student is placed on probation.
b. When a student is placed on probation, he/she will be notified in writing by the appropriate
Academic Dean and the reasons will be stated. Notification must be sent by Certified Mail or hand-
delivered and acknowledged by signatures of the student and the appropriate Academic Dean or his
designee. Copies of the letter will be placed in the student's permanent file and distributed to the
Chairman of the Student Academic Progress Committee and the student's Faculty Advisor. The Student
Academic Progress Committee will consider when the terms of the academic probation have been
satisfied and recommend to the appropriate Academic Dean that probation can be rescinded.
c. A student on probation may not serve as an officer of any official University or College club or
organization and should not engage in time-consuming extracurricular activities. No student on
probation will be permitted to enroll in an elective course.
d. On-campus students on probation must meet with their faculty advisor at least once each month. Off-
campus students on probation must contact their faculty advisor once a month. It is the student's
responsibility to contact the faculty advisor to arrange for these meetings.
e. A student will remain on probation until the program specific minimal acceptable academic standards
are met again.
f. A student will be removed from probation when the specified terms of probation for ethical,
professional, or personal conduct are met. The student will be notified in writing.
12. Remediation
Every effort will be made to provide each student ample opportunity to demonstrate competency in each
area of the academic program. Please see appropriate Program Specific section.
13. Remediation: Financial Aid Policy
Students who are required to repeat coursework due to an unsuccessful prior attempt must contact a
Financial Aid officer in regard to financial aid eligibility.
Students who have been recommended by the Student Academic Progress Committee and appropriate
Academic Dean to repeat the year due to unsatisfactory progress (GPA) or in cases where there is a
satisfactory GPA, but deficiencies are noted that impede promotion, the following criteria must be met to be
eligible for financial aid:
a. Full time attendance recorded.
b. Placed on one-year probation.
c. Must be tested and graded.
d. Must be monitored closely.
It is the student's choice to audit course work to strengthen skills as long as he/she has met satisfactory
progress such as GPA and is fully aware that he/she will not be eligible to apply for any financial aid to
cover these audit costs. The student will be financially responsible for himself/herself until promoted by the
appropriate Academic Dean.
If, at the end of the academic year, the student is still considered to be making unsatisfactory progress
and must remediate, he/she is removed from the list of Title IV and Title VII financial aid recipients.
Summer remediation is not covered by financial aid and cannot be considered an expense item on the
next year's budget
Appropriate tuition and fees will be determined by the Executive Vice President of Finance and
Administration.
14. Summary Suspension
Each student is expected to govern his/her conduct with concern for other individuals and for the entire
University community. Actions that threaten or endanger, in any way, the personal safety and/or well being
of self or others, or that disrupt or interfere with the orderly operation of the University are cause for
immediate disciplinary action.
Either the President, Executive Vice President for Academic Affairs/CAO, or appropriate Academic
Dean has the authority to summarily suspend a student when the student admits to guilt or when, in the
33
opinion of the President, Executive Vice President for Academic Affairs/CAO or appropriate Academic
Dean, such action is appropriate to protect the health or safety of any individual, or to preserve the orderly
operation of the University.
When a student is summarily suspended, the student shall be informed, in writing, of the specific charges
on which such suspension is based. Such notice shall be delivered personally to the student or mailed by
certified mail within forty-eight (48) hours of the imposition of the suspension. Such conduct by a student
shall be considered a violation of the Standards of Professional Conduct and suspected violations will be
handled by the procedures outlined under Standards of Professional Conduct section of this Catalog.
Appeal of the decision of the respective Academic Dean can be made to the Executive Vice President
for Academic Affairs/CAO. Any student who has been summarily suspended may also request, in writing
to the appropriate Academic Dean, a hearing by the Student Conduct Committee, and a hearing shall be
convened within ten (10) working days of the date such request is made. Students who are suspended are
not entitled to remain in class or on clinical rotations/assignments during the appeal.
15. Dismissal
The University may dismiss at any time it deems necessary to safeguard its standards of scholarship,
conduct and orderly operation. The Student Academic Progress Committee or the Student Conduct
Committee may recommend dismissal of a student for any reason it deems appropriate. Furthermore,
conviction of a felony while a matriculant at Western University may be grounds for dismissal.
The Student Academic Progress Committee may recommend dismissal of a student as provided in the
Program Specific section of this Catalog.
The Student Conduct Committee may recommend dismissal of a student for matters pertaining to
suspected personal or professional misconduct that include, but are not limited to: academic integrity,
unsatisfactory attendance, inappropriate interaction with instructors, fellow students, and University and
hospital personnel, improper approach to and interaction with patients, and inappropriate personal
dress/appearance.
In its deliberations, the Student Conduct Committee/Student Academic Progress Committee may
consider the student's academic record and will also consult with the student's faculty advisor, the student,
and other faculty and administrators when appropriate. After considering all pertinent information, the
Student Conduct Committee/Student Academic Progress Committee will forward its written
recommendation regarding dismissal to the appropriate Academic Dean.
The decision will be made by the appropriate Academic Dean, based upon the recommendation of the
Student Academic Progress Committee or Student Conduct Committee. The Student Academic Progress
Committee or Student Conduct Committee will base its recommendation not only on the student's academic
record, but will also consult with the student's faculty advisor, other faculty and administrators, and the
student involved, when appropriate.
16. Student Appeal Process
The appropriate Academic Dean shall have the authority to make decisions regarding a student's status
in matters of academic suspension, student conduct, academic progression/promotion, and graduation. The
decision will be based on input from appropriate sources that may include the following: individual
instructors, faculty, and appropriate committees.
a. Within five (5) working days following written notification to the student of the action of the
respective Academic Dean, the student may appeal the decision in writing to the Executive Vice
President for Academic Affairs/CAO. Upon written request from the student, the Executive Vice
President for Academic Affairs/CAO shall review the case and, within seven (7) working days, shall
issue a decision in writing to the student, which may affirm, modify, or reverse the previous action. A
copy of that letter shall be sent to the Dean, and other appropriate individuals.
The decision of the Executive Vice President for Academic Affairs/CAO will be final.
b. The student may remain in class or on clinical rotations/assignments pending the outcome of appeals,
except in cases of summary suspension, and except when the Executive Vice President for Academic
Affairs/Chief Academic Officer has suspended the student or has otherwise determined that it is
inappropriate for the student to remain in class or participate in clinical rotations/assignments, consistent
with the decision of the Academic Dean that is being appealed.
34
c. If a student is suspended for any reason, all student financial aid will be withheld until the appeal
process is resolved by reinstatement of the student or dismissal of the student. If reinstated, the financial
aid funds can be released to the student. If the student is dismissed, the funds will be returned to the
proper agency/lender respectively.
17. Protocol for Input on Matters of Student Concern
When a student has a personal concern involving a teacher or course that is not of general interest to the
class, he/she should speak to the professor directly.
If the concern might involve more of the class, he/she should take the concern to the appropriate class
representative (e.g., curriculum representative or class president) so they might sample class opinion to find
out the extent of concern.
If, in the opinion of the class representative, the concern is valid, the class representative should bring
the matter to the attention of the class professor with the object of resolving it at that level.
If the matter cannot be solved between the class and the professor, it should be taken to the Academic
Dean or designee. If the matter cannot be handled properly by the respective Dean, or if the students feel it
was not, it should be taken to the Executive vice President of Academic Affairs/CAO, whose decision shall
be final.
Note: Grade appeals may not be pursued under this protocol.
18. Legal Limitations on Practice of Health Care
It is a violation of the law and contrary to the policy of this University for any unlicensed person to
attempt to engage in professional practice of health care. Students, therefore, are cautioned to confine such
activities to duly licensed and supervised teaching clinics.
35
TUITION AND FEES
Tuition and fees are subject to change without notice upon approval by the Board of Trustees.
Mandatory fees for each student are non-refundable. For complete information about tuition and fees, refer
to the appropriate section for each program.
FUTURE TUITION RATE INCREASES
You can expect that tuition increases will be part of your educational experience at Western University;
however, one should know that the Board of Trustees and the administration of this University strive each
year to keep tuition at a reasonable level. For example, in recent years the rate of tuition increase has been
kept at or below five percent. While we are committed to quality educational programs, the inevitable
increases in operating costs each year make it necessary to adjust tuition accordingly. The administration
will communicate tuition rate adjustments as soon as they are determined by the Board of Trustees.
TUITION AND MANDATORY FEES
Tuition and Fee Payments
Tuition is assessed in two installments. The first assessment of tuition and fees occurs at the beginning
of each academic year, and the second is assessed approximately half-way through the academic year.
Depending on the academic program, each required payment corresponds to a “period of enrollment.”* A
refund policy for a withdrawal or a leave of absence has been established to address the receipt of private
payment and Title IV Student Financial Aid funds (see Tuition Refund Policy below).
Western University charges tuition based on an “academic” year and covers two period of enrollment.
The number of weeks of instructional time during the period of enrollment is measured beginning on the
first day of class and/or rotation and ends on the last day of class and/or rotation.
*Students in the Master of Science in Health Professions Education program will pay tuition and fees on a
trimester year. Refunds will be based on the trimester.
Other Fees
a. Audit/Remediation Fee: The fee charged for auditing or remediating a class will be calculated on a
prorata basis.
b. Other Fees and Expenses
Late Registration Fee $ 30 per day
Breakage Fee Cost of Replacement
Lost I.D. Badge $ 10
Lost Locker Key $ 40
Copy of Official Transcript (each) $ 5
Faxed Transcript $ 10
Copy of Student File Material 25 cents per page
PRE-PAID TUITION PLAN
The Prepaid Tuition Plan allows for payment of future years’ tuition at the current tuition rate. This
option will assist in avoiding future tuition increases. The payment must be received at least one year
before the start of the next academic year.
Mandatory fees will be charged annually and are not included in the prepayment provisions. For
additional information, please contact the Financial Aid Office at (909) 469-5354 or the Bursar’s Office at
(909) 469-5403.
36
WESTERN UNIVERSITY TUITION REFUND POLICY
Western University has established a refund policy for all students who find it necessary to withdraw
from the University. Students who elect to withdraw or take a leave of absence during the academic year
must submit prior written notification to the appropriate Academic Dean according to the procedures
specified in this Catalog for their program. Western University may amend its institutional refund policy at
any time. Amendments will become effective for the academic year that follows official notification of the
amendment. Any questions concerning Western University's refund policy should be directed to the
Bursar’s Office.
Determining the Withdrawal Date
The withdrawal date is:
a. The date the student begins the withdrawal process prescribed by the respective College;
b. The date that the student otherwise provided official notification to the respective College of
the intent to withdraw; or
c. The midpoint of the payment period for which Student Financial Aid Programs Assistance was
disbursed or a later date documented by the respective College, if the student did not begin the
withdrawal process or otherwise notify the respective College of the intent to withdraw.
If the College determines that a student did not begin the withdrawal process or otherwise notify the
respective College of the intent to withdraw due to illness, accident, grievous personal loss or other
circumstances beyond the student's control, the College may determine the appropriate withdrawal date.
For additional information regarding refund policies for student participating in Student Financial Aid
Programs, see Financial Aid below.
COMPREHENSIVE HEALTH PLAN
It is mandatory that all Western University students have a health insurance plan in force at the time of
registration. If a student can show valid proof of personal health insurance to the Plan Administrator, at
least equal in benefits to the plan recommended by the University, it will not be necessary to purchase any
additional insurance. If valid proof of other insurance cannot be shown, the student will automatically be
enrolled in the health insurance plan made available by the University. This is described in the health plan
brochure provided at the time of registration. There are several available options. The plan with the better
benefits is recommended. Dependent coverage, although not required, is optional at an additional premium
(see Health Plan Brochure).

37
FINANCIAL AID
Financial aid is not intended to replace the financial responsibility of the student; rather, it is intended to
supplement what the family can provide. Students are required to complete the Free Application for Federal
Student Aid (FAFSA) each year they are seeking financial aid. The information provided is used to create
an analysis of each student’s financial ability to contribute toward their educational costs. Students may
complete the FAFSA application via the Internet at www.fafsa.ed.gov
. Students are required to inform
Western University’s Financial Aid Office of all financial assistance (including scholarships) they receive.
More detailed information on the various types of scholarships and awards can be found at Western
University’s website under “Financial Aid”. Western University reviews and administers all of its programs
without discrimination as to race, creed, sex, national origin, or non-disqualifying handicap.
FINANCIAL AID AND THE WORLD OF PRIVATE PHILANTHROPY
Beyond the various federal, state, and other public and commercial funding sources, there is another
sector that provides valuable support to Western University students. It is the world of private philanthropy:
those individuals, corporations, and foundations who willingly accept the responsibility of serving as good
citizens of the larger society. These benefactors contribute to assisting students in achieving their education
goals and, ultimately, to the quality of health care delivered to the public.
DEPARTMENT of EDUCATION
TITLE IV PROGRAMS
Federal Financial Aid Program Criteria
To be eligible for federal financial aid programs, students must be U.S. citizens or permanent residents
of the United States, attending at least half-time, and making satisfactory progress toward their degrees. The
amount of financial aid awarded by the school can never exceed the educational cost of attendance.
Students can not be in default on any educational loan or owe a refund on any state or federal educational
grant. In addition, all male students must have completed U.S. Selective Service registration requirements to
qualify.
Federal Subsidized Stafford Loan: Available to undergraduate and graduate students by participating
lending institutions and guaranteed by the federal government. The interest on these loans is subsidized
(paid) by the federal government while the student is enrolled at least half-time in school. The maximum
annual Subsidized Stafford loan limits per program are as follows:
$ 8,500 DO, PharmD, MSHPE, MPT, MPA, and MSN/FNP programs
$ 2,625 FNP certificate program
Federal Unsubsidized Stafford Loan: Available to undergraduate and graduate students by participating
lending institutions and guaranteed by the federal government. However, the federal government does not
pay the interest while the student is in school. Subsidized Stafford loan eligibility must be determined first,
before a student can apply for an Unsubsidized Stafford loan. The maximum annual Unsubsidized loan
limits per program are as follows:
$32,222 DO (1
st
& 2
nd
year) program
$36,667 DO (3
rd
year) program
$34,444 DO (4
th
year) program
$23,889 PharmD (1
st
, 2
nd
& 4
th
year) program
$26,667 PharmD (3
rd
year) program
$10,000 MSHPE program
$26,667 MPT, MSN/FNP, MPA programs
$ 4,000 FNP certificate program
Aggregate Loan Limits for Subsidized & Unsubsidized Stafford Loans: The total loan debt a student
may have outstanding from all Stafford Loans combined are separated below by program. Outstanding
loans include student loans received while the student completed undergraduate and graduate work. Within
the aggregate amounts below, the subsidized Stafford maximum may not exceed $65,500.
MSHPE Program: $138,500 (less the aggregate amount of any subsidized loans made to the
student).
38
Because Western University participated in the Health Education Assistance Loan (HEAL) program
before its phase out in 1998, students who are enrolled full time are allowed an increase in annual
unsubsidized Stafford loan amounts. As a result, they also have a higher aggregate as indicated below.
DO Program: $189,125 (less the aggregate amount of any subsidized loans made to the student).
Within this aggregate, the additional HEAL unsubsidized maximum is $80,000.
PharmD, MPT, PA, and MSN/FNP Programs: $189,125 (less the aggregate amount of any
subsidized loans made to the student). Within this aggregate the additional HEAL unsubsidized maximum is
$50,000.
Federal Perkins Loan: For eligible undergraduate and graduate students and subject to availability of
funds. The amount awarded varies, depending on financial need and federal allocation to our school. The
Perkins undergraduate aggregate is $20,000, and graduate students have a $40,000 total aggregate. Perkins
loans have a fixed interest rate at five percent.
DEPARTMENT OF HEALTH AND HUMAN SERVICES
TITLE VII PROGRAMS LOANS & SCHOLARSHIPS
Loans for Disadvantaged Students (LDS): Provides long-term, five percent interest loans to eligible
osteopathic medical students from disadvantaged backgrounds, subject to fund availability.
Primary Care Loans (PCL): For eligible students and subject to availability of funds. The long-term five
percent fixed simple interest loan amounts vary, depending on financial need and federal allocation.
Students must provide parental income information and sign a contract to practice in primary care until the
loan is paid in full.
Scholarships with Service Requirements
National Health Service Corps Scholarships (NHSC): This scholarship provides full tuition, fees, books,
and a monthly stipend for osteopathic medical students and physician assistants who possess a bachelor’s
degree. Students must serve in a designated medically underserved area (rural, inner city or Indian health).
Minimum obligation is two years and a student must be an U.S. citizen.
Military Health Professions Scholarships: The Army, Navy and Air Force offer Health Professions
Scholarship programs to medical students for tuition, fees, books and supplies, and a monthly stipend.
While in school, students are expected to serve forty-five days of active duty per year, when possible, with
pay. One year of active service as a medical officer (after internship and/or residency) is required for each
year of support in the scholarship program, with a minimum requirement of three years.
UNIVERSITY ADMINISTERED SCHOLARSHIPS
The Dr. Robert E. Corey Memorial Scholarship Fund: Established January 1983 as a memorial to Robert Corey,
DO. Recipients are selected from second, third and fourth year students for their commitment to osteopathic medicine,
outstanding community service and demonstrated financial need as determined by the institution.
The Albert Victor and Mary P. Kalt Scholarship Fund: Established June 1977, and is available for
students of all disciplines who express a desire to work in primary care in an underserved/rural area.
Asian American Scholarship: Awarded to students of Asian descent, who are in good academic standing,
demonstrates financial need and is dedicated to serving the Asian community.
UNIVERSITY ADMINISTERED LOANS
WesternU Emergency Loan Programs: Limited funds made available on a short-term basis to meet
financial emergencies. The maximum loan is $500 interest-free. Since this is a revolving loan fund, it is
expected to be repaid in ninety days.
Roger E. Coe Loan Fund #1: Established in March 1981 by a gift from Roger M. and Ruby M. Coe. Two
loans of $2,500 are made in the spring of each year. Loans will be made to osteopathic medical students
who have completed their second or third year at Western University and are particularly interested in
osteopathic manipulative skills. Interest begins to accrue at the time the loan is disbursed at the rate of eight
39
percent. First payment begins immediately after graduation with full repayment of loan funds within five
year.
VETERANS’ EDUCATIONAL BENEFITS
The Student Affairs Office will provide certification of enrollment services for veterans attending
Western University. The Financial Aid Office will serve as a direct liaison between our University and
Veterans’ Administration regarding underpayment, overpayment, or non-payment benefits. Students
expecting to collect educational benefits may obtain further information from Western University’s
Financial Aid Office. As of this publication DO, MSN/FNP, MPT, MPA, and PharmD programs are
eligible. In order to continue collecting benefits, a veteran must be making satisfactory progress towards a
degree.
GRADUATE TEACHING FELLOWS IN THE DEPARTMENT OF OSTEOPATHIC
MANIPULATIVE MEDICINE
This Fellowship program in the Department of Osteopathic Manipulative Medicine of the College of
Osteopathic Medicine of the Pacific (COMP) is designed to expand the educational opportunities for
osteopathic medical students while they assist in all phases of the department’s operation. OMM Fellows
assist in lecturing and teaching practical skills to graduate students. In order to participate in the Fellowship
program, each student takes five years, instead of four, to complete all of their educational requirements,
including hospital and private practice clinical rotations, for the Doctor of Osteopathic Medicine degree.
Fellows receive a full tuition/fees waiver their third and fourth years and an annual stipend for the fifth year.
Fellows are selected from each MSII class annually.
TUITION REFUND POLICY
Western University of Health Sciences has established a refund policy for all students who find it
necessary to withdraw from the University or take a leave of absence during the academic year. Students
who elect to withdraw or take a leave of absence during the academic year must submit prior written
notification to the appropriate Academic Dean according to the procedures specified in the Catalogue for
their program. Western University may amend its institution refund policy at any time. Amendments will
become effective for the academic year that follows official notification of the amendment. Any questions
concerning Western University’s refund policy should be directed to the Bursar’s Office.
If a recipient of Student Financial Aid (SFA) loan funds withdraws from school after beginning
attendance, the amount of SFA loan assistance earned by the student must be determined. If the amount
disbursed to the student is greater than the amount the student earned, unearned funds must be returned. If
the amount disbursed to the student is less than the amount the student earned, and for which the student is
otherwise eligible, he or she is eligible to receive a post-withdrawal disbursement of the earned aid that was
not received. Title IV funds are awarded to a student under the assumption that the student will attend
school for the entire period for which the assistance is awarded. When a student withdraws, the student may
no longer be eligible for the full amount of Title IV funds that the student was originally scheduled to
receive.
Definition of a Title IV recipient
A recipient of loan assistance is a student who has actually received Title IV funds or has met the
conditions that entitle the student a late disbursement. If the student never actually began attendance for the
payment period or period of enrollment, the refund policy does not apply. Similarly, if a student began
attendance, but was not and could not have been disbursed Title IV funds prior to withdrawal, the student is
not considered to have been a Title IV recipient and the requirements of this refund policy do not apply.
Funds to include in the Calculation
The calculation of earned Title IV program assistance loan funds that were disbursed or could have been
disbursed to a student. This includes Subsidized and Unsubsidized loan funds, and funds from the Federal
Perkins Loan Program.
Title IV Aid Disbursed
A student’s Title IV funds are disbursed when the school credits a student’s account with the funds or
pays a student directly with Title IV funds received from the Department and/or Federal Family Education
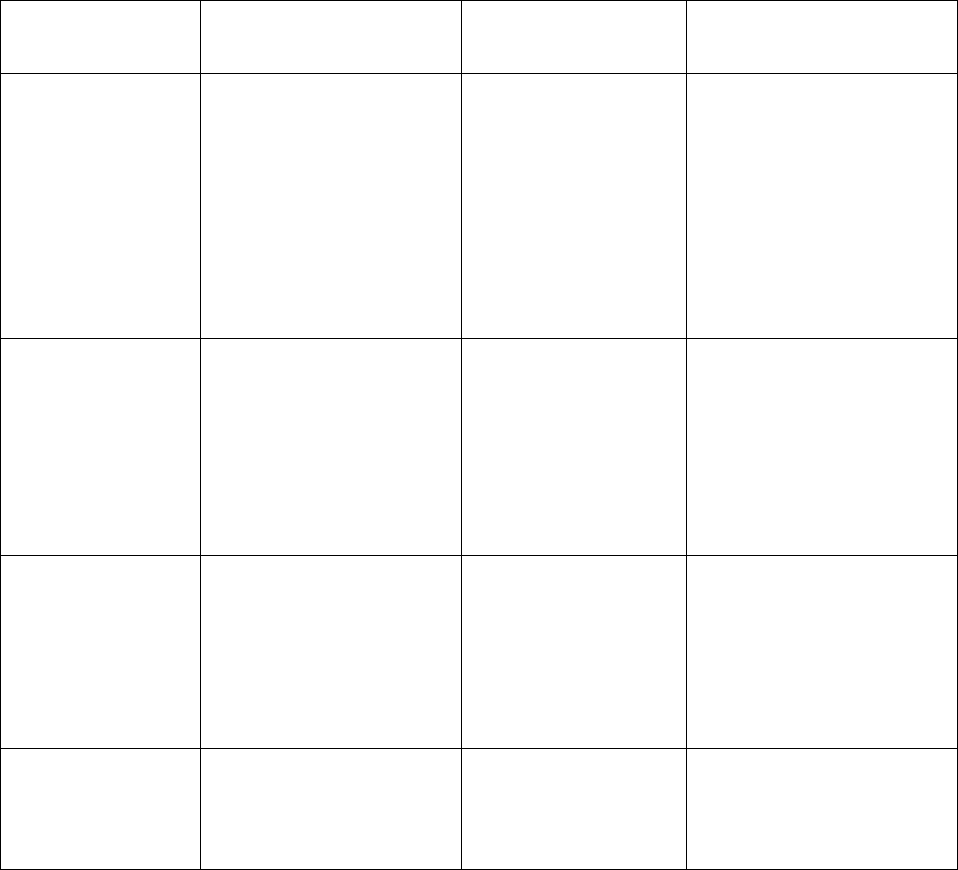
40
Loan (FFEL) funds received from a lender. A student’s aid is counted as disbursed for the calculation if it is
disbursed as of the date of the institution’s determination that the student withdrew.
Calculation of Amount of SFA Program Assistance Earned
The amount of SFA Program assistance earned is the percentage of SFA Program assistance earned
multiplied by the total amount of SFA Program assistance that was disbursed (and that could have been
disbursed) for the payment period as of the day the student withdrew. The percentage earned is one of the
following:
• If the day the student withdrew on or before the student completed 60 percent of the enrollment period
for which the assistance was awarded, the percentage earned is equal to the percentage of the
enrollment period from which assistance was awarded.
• If the day the student withdrew after the student has completed 60 percent of the payment period the
percentage earned is 100 percent.
Determining the Withdrawal Date
The definition of withdrawal date is for determining the amount of aid a student has earned. The chart
below lists the withdrawal date for the various types of withdrawals, as well as the date of the institution’s
determination that the student withdrew for each type of withdrawal.
Withdrawal Type Circumstance Student’s Withdrawal
Date*
Date of the Institution’s
Determination that the
Student has Withdrawn**
Official Notification The student begins the
school’s withdrawal process,
or
The student otherwise
provides official notification
to the school of intent to
withdraw.
The date the student
begins the schools
withdrawal process, or
The date that the student
otherwise provides the
notification.
(If both circumstances
occur, use the earlier
withdrawal date.)
The date the student provides
official notification or begins
the withdrawal process
whichever is later.
Official Notification
Not Provided
Official notification not
provided by the student
because of circumstances
beyond the student’s control.
All other instances where
student withdraws without
providing official
notification.
The date that the school
determines is related to
the circumstance beyond
the student’s control.
The midpoint of the
payment period or period
of enrollment, as
applicable.
The date that the school
becomes aware that the student
has ceased attendance.
Leave of Absence
Related
The students does not return
from an approved leave of
absence, or
The student takes an
unapproved leave of absence
The date that the student
began the leave of
absence.
The earliest of the dates of the
end of the leave of absence or
the date the student notifies the
school he or she will not be
returning to that school. (In the
case of an unapproved absence,
the date that the student began
the leave of absence.)
Withdrawal After
Rescission of
Official Notification
The student withdraws after
rescinding a previous official
notification of withdrawal.
The student’s original
withdrawal date from the
previous notification.
The date the school becomes
aware that the student did not,
or will not, complete the
program period or period of
enrollment.
41
*In place of the dates listed, a school may always use as a student’s withdrawal date the student’s last
date of attendance at an academically related activity, if the school documents that the activity is
academically related and that the student attended the activity.
**For a student who withdraws without providing notification to the school, the school must determine
the withdrawal date no later than 30 days after the end of the earlier of the (1) payment period or period of
enrollment (as appropriate), (2) academic year, or (3) education program.
Return of Unearned SFA Program Funds
When a return of Title IV funds is due, the school and the student both have a responsibility for
returning funds. Whatever funds are not returned by the school must be returned by the student. Although
this requirement speaks in terms of returning funds, a school is not required to actually return its share
before the student. Rather, it is the calculation of the amount of assistance the school is responsible for
returning to the Title IV accounts that must be calculated first. The student’s repayment obligation is
determined after the school’s share is calculated. If the student receives more SFA Program assistance than
the amount earned, the school, or the student, or both, must return the unearned funds as required. Western
University must return the lesser of
• The amount of SFA Program funds that the student does not earn; or
• The amount of institutional costs that the student incurred for the payment period or period of
enrollment multiplied by the percentage of funds that was not earned.
The student must return or repay, as appropriate, the remaining unearned SFA Program funds.
Order of Return of Title IV Funds
A school must return Title IV funds to the program from which the student received aid during the
payment period or period of enrollment as applicable, in the following order, up to the net amount disbursed
from each source:
• Unsubsidized Federal Stafford Loans
• Subsidized Federal Stafford Loans
• Federal Perkins Loans
Method of Order of Return of SFA Program Refunds
The student returns funds to loan programs in accordance with the terms of the loan. In other words, the
student will repay any unearned loan funds in the same manner that he or she will be repaying earned loan
funds.
Reference: Department of Education, Student Financial Aid Handbook, 2001-2002 Award Year.
42
WESTERN UNIVERSITY CALENDAR*
INDEPENDENCE DAY Wednesday, Jul. 4, 2001
Last day of classes Tuesday, Jul. 3. 2001
Classes resume Thursday, Jul. 5, 2001
CONVOCATION Saturday, Aug. 11, 2001
LABOR DAY
(no classes) Monday, Sept. 3, 2001
COLUMBUS DAY
(no classes) Monday, Oct. 8, 2001
THANKSGIVING RECESS
Last Day of Classes Wednesday (noon), Nov. 21, 2001
Classes Resume Monday, Nov. 26
WINTER RECESS
Last Day of Classes Friday, Dec. 21, 2001
Classes Resume Monday, Jan. 7, 2002
MARTIN LUTHER KING
HOLIDAY (no classes) Monday, Jan. 21, 2002
PRESIDENTS DAY
(no classes) Monday, Feb. 18, 2002
HONORS DAY Monday, Apr. 8, 2002
MEMORIAL DAY
(no classes) Monday, May 27, 2002
COMMENCEMENT Friday, May 31, 2002
*The College of Osteopathic Medicine of the Pacific, the College of Pharmacy, the College of Graduate
Nursing, and the programs of the College of Allied Health (MPT, PA, and MSHPE) maintain specific,
detailed program calendars. Please consult the appropriate program to determine additional official dates.
43
COLLEGE OF OSTEOPATHIC MEDICINE OF THE
PACIFIC
Doctor of Osteopathic Medicine Program
Accreditation
The academic program of the College of Osteopathic Medicine of the Pacific (COMP) is accredited by
the Bureau of Professional Education of the American Osteopathic Association.
The Osteopathic Philosophy
Osteopathic medicine is a contemporary school of medical thought and practice, founded on the concept
that the normal state of a person is health. The philosophy of osteopathic medicine has its roots in antiquity,
long before the life of its founder, Dr. Andrew Taylor Still. The philosophy of Dr. Still can be directly
related to the concepts and teachings of the Greek physician-philosopher, Hippocrates. This "father of
medicine" taught that disease is a natural process and that natural powers are the healers of disease. The
physician must assist nature, said Hippocrates, but attention should be focused on the patient rather than on
the disease. Dr. Still revived this concept, and gave it a new meaning and implementation with a system of
diagnosis and treatment that made it the cornerstone of osteopathic medicine.
There are four fundamental principles of osteopathic diagnosis and treatment:
1. The body tends to be self-healing and self-regulatory in the disease processes. The ability to
maintain integrity in a continually changing external environment is mediated through an elaborate
communication network. The communication network embraces the circulatory and
neuromusculoskeletal systems.
2. Intimate interrelationships exist between structure and function at all levels of biologic
organization.
3. Abnormalities of the neuromusculoskeletal system are invariably present during disease. When
subjected to manually applied forces, these abnormalities are ameliorated coincidentally with the clinical
improvement of the patient.
4. Health is an equilibrium state and maintaining this state requires constant biological adjustment.
While employing osteopathic manipulation, the osteopathic physician utilizes other recognized
modalities for diagnosis and treatment. All modalities of treatment are based upon an evaluation of the
patient's personal state of development, family and social environment.
TECHNICAL GUIDELINES FOR ADMISSION AND MATRICULATION
A candidate for admission to the Doctor of Osteopathic Medicine Program must have the use of certain
sensory and motor functions, or reasonable accommodations, to permit them to carry out the activities
described in the sections that follow. Graduation from the program signifies that the individual is prepared
for entry into osteopathic postgraduate training programs. Therefore, it follows that graduates must have the
knowledge and skills needed to function in a broad variety of clinical situations and to render a wide
spectrum of osteopathic patient care. The osteopathic medical student must be able consistently, quickly,
and accurately to integrate all information received by whatever sense(s) are employed. Also, they must
have the intellectual ability to learn, integrate, analyze, and synthesize data.
A candidate for the DO degree must have abilities and skills of five varieties including: (1) observation;
(2) communication; (3) motor; (4) intellectual, conceptual, integrative and quantitative; and (5) behavioral
and social. Where technological assistance is available in the program, it may be permitted as a reasonable
accommodation, when appropriate. Under all circumstances, a candidate should be able to perform in a
reasonably independent manner:
1. Observation: Candidates and students must have sufficient vision to be able to observe
demonstrations, experiments, and microscopic laboratory exercises. They must be able to observe a
patient accurately at a distance and close at hand.
44
2. Communication: Candidates and students must be able to communicate with patients and colleagues.
They should be able to hear, with or without a reasonable accommodation. Candidates and students must
be able to read English.
3. Motor: Candidates and students should have sufficient motor functions that enable them to execute
movements, with or without reasonable accommodation, which are reasonably required to provide
general care and emergency treatment of patients (i.e., palpation, auscultation, percussion, and other
diagnostic and therapeutic modalities). Examples of emergency treatment reasonably required of
osteopathic physicians include: cardiopulmonary resuscitation, administration of intravenous
medication, the application of pressure to stop bleeding, the opening of obstructed airways, the suturing
of simple wounds, and the performance of simple obstetrical maneuvers and osteopathic manipulation.
These actions require coordination of both gross and fine muscular movements, equilibrium and
functional use of the senses of touch and vision.
4. Intellectual, Conceptual, Integrative, and Quantitative Abilities: Students must demonstrate problem-
solving skills, which involve intellectual, conceptual, integrative and quantitative abilities. These
abilities include measurement, calculation, reasoning, analysis, and synthesis. Problem solving, the
critical intellectual skill demanded of a osteopathic physician, requires all of these intellectual abilities.
In addition, candidates and students should be able to comprehend three-dimensional relationships and
understand the spatial relationships of structures.
5. Behavioral and Social Attributes: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgement, the prompt completion of
all responsibilities attendant to the assessment and care of patients, and the development of mature,
sensitive, and effective relationships with patients. Candidates and students must be able to tolerate
physically taxing workloads, adapt to changing environments, display flexibility, and learn to function in
the face of uncertainties inherent in the clinical problems of many patients. Compassion, integrity,
concern for others, interpersonal skills, interest, and motivation are all personal qualities to be assessed
during the admissions and educational processes.
The Doctor of Osteopathic Medicine program, along with all other programs at Western University of
Health Sciences, shares a commitment to develop creative ways of opening the DO curriculum to
competitive, qualified individuals with disabilities. In doing so, however, the DO Degree Program must
maintain the integrity of its curriculum and preserve those elements deemed essential to educating
candidates to become effective osteopathic physicians.
ADMISSIONS POLICIES AND PROCEDURES
Western University/COMP accepts applications from all qualified candidates. More applications are
received from qualified candidates than can be admitted. While grades and Medical College Admission
Test (MCAT) scores are important in selecting candidates for admission and may suggest future academic
success, the Admissions Committee recognizes that these statistics, by themselves, do not guarantee later
success as a physician. Therefore, non-academic criteria are also important in making the selection. Western
University/COMP seeks a diverse and balanced student population and considers factors such as a well-
rounded background, work experiences, letters of recommendation, interest in and knowledge of
osteopathic medicine, and professional promise. To ascertain these factors, an on-campus interview is
required before acceptance is given. The College may exercise its discretion to rely upon additional
considerations. Western University/COMP is committed to admitting competitive, qualified individuals
with disabilities.
Early Admission Decision Program
Western University of Health Sciences/College of Osteopathic Medicine of the Pacific is pleased to
offer an Early Admission Decision Program. Qualified applicants may take advantage of the Early
Admission Decision Program if they apply only to Western University/COMP and submit their application
to AACOMAS prior to June 15.
Highly qualified candidates who have a strong preference for Western University/COMP are eligible for
an early admission decision. Candidates must have a minimum science GPA of 3.30, a minimum overall
GPA of 3.30, and a minimum average MCAT score of 9. All prerequisite coursework must be completed at
the time of application. The AACOMAS application must be filed prior to June 15. The Western
45
University/COMP supplementary application and all supporting documents must be filed prior to August 1.
Interviews and decisions are granted August through September. If you apply as an Early Admission
Decision candidate, you must apply only to Western University/COMP. For further information, and to
request an Early Admission Decision Program application form, contact the Admissions Office at (909)
469-5335, or write to:
Western University of Health Sciences
College of Osteopathic Medicine of the Pacific
Admissions Office
309 E. Second Street
Pomona, CA 91766-1854
Entrance Requirements
Candidates for admission to Western University/COMP must meet these requirements at the time of
application:
1. Ninety semester hours, or three-fourths of the credits required for a baccalaureate degree, from a
regionally accredited college or university.
2. One academic year or its equivalent in English, biology, physics, inorganic chemistry, organic
chemistry and behavioral sciences.
3. Applicants must submit their Medical College Admission Test (MCAT) scores. Information
concerning this test may be obtained from the pre-professional advisor at one's college or directly from
the MCAT Program Office, 2255 North Dubuque Road, P.O. Box 4056, Iowa City, Iowa 52243, phone
(319) 337-1357. This examination is offered in the spring and summer. Applicants are encouraged to
take the examination in the spring of their junior year. To be considered for admission, the MCAT
examination must be taken prior to January of the entering year.
Please note that the majority of candidates accepted for admission will have completed four or more
years of pre-professional study prior to matriculation, and that the quality of Western University/COMP
students is quite high. Successful candidates typically have both science and overall grade point averages of
3.2 or above on a 4.0 scale and a mean MCAT score over 8.0. Please keep in mind that academic grades
and the MCAT score are just two of the factors used in the evaluation process.
AACOMAS
The College of Osteopathic Medicine of the Pacific of Western University of Health Sciences, along
with the other colleges of osteopathic medicine, participates in a centralized application service, the
American Association of Colleges of Osteopathic Medicine Application Service, 5550 Friendship Blvd.,
Suite 310,Chevy Chase, Maryland 20815-7231. Individuals interested in applying to Western
University/COMP should write directly to AACOMAS for information and application materials or obtain
application request cards from the Western University/COMP Admissions Office. At this time, applicants
should also make arrangements to have official transcripts of all prior undergraduate and graduate course
work forwarded to AACOMAS.
Upon receipt of the initial application and transcript(s), AACOMAS will collate materials, compute
grades, and transmit standardized information to the applicant and to those osteopathic medical colleges
that the applicant designates. AACOMAS takes no part in the evaluation or selection of applicants. After a
review of the AACOMAS application, if both a minimum grade point average of 2.5 on a 4.0 scale has been
achieved overall, as well as in the sciences, and a minimum of 90 semester hours has been completed, the
Admissions Committee may request additional information from the applicant for further consideration.
Keep in mind, however, that the above grade point average is only the bare minimum, and candidates in the
2.5 range need to be sure this is a sufficiently strong GPA to meet the academic challenges at Western
University/COMP successfully. Previously, candidates admitted to Western University/COMP have had
substantially higher grade point averages.
Additional information will include the following:
1. A supplementary application provided by Western University/COMP will be sent only after receipt
of the initial application from AACOMAS. There is a non-refundable supplementary application fee of
$60.
46
2. An evaluation of the applicant's work and accomplishments submitted by the Pre-Health
Professions Committee of the applicant's college. If the college has no committee, the student may
submit evaluations from three classroom professors, two of whom must be in the sciences, and;
3. A letter of recommendation from a physician. A letter from a DO is preferred.
The supplementary required information must be returned within 30 days to the Director of Admissions,
Western University of Health Sciences/COMP, 309 E. Second Street, Pomona, California 91766-1854.
After the applicant's file is complete, the Admissions Committee reviews it to determine whether the
candidate will be granted an interview. If a candidate is deemed of interest to Western University/COMP,
he or she is invited to the campus at his or her own expense. The candidate should plan to spend a full day
on campus for orientation and the interview. Orientation consists of information on the curriculum, financial
aid, student services, and clinical rotations; lunch with a Western University/COMP student; a personal
interview with members of the Admissions Committee and faculty; and a tour of the facilities. The
candidate's application and interview are evaluated by the Committee and the candidate is notified of the
status of his or her application in approximately three weeks.
Note: Candidates accepted to Western University/COMP must have a complete set of official transcripts
mailed to the Admissions Office no later than July 1. For your information, AACOMAS retains the original
set of transcripts it receives from applicants.
Transfer Policy
Western University/COMP offers a transfer program for persons who have completed one or more years
of medical studies at a medical school accredited by the American Osteopathic Association (AOA).
Candidates seeking transfer must be in good academic standing at the school where they are enrolled and be
eligible for continuation there. Candidates are expected to meet the minimum entrance requirements that are
required of our entering first-year students. Please refer to the Admissions Policies and Procedures section
in the catalog for specific information regarding these requirements.
Transfer applications are available from the Admissions Office after September 1. Application deadline
for students wishing to transfer into the second year is March 1st. Application deadline for students wishing
to transfer into the third year is January 1.
Candidates must provide:
1. Official transcripts from all colleges and universities attended. Official transcripts showing the
successful completion of studies at the osteopathic medical school where currently enrolled.
2. Official MCAT scores.
3. Letters of recommendation from three science professors at your college of osteopathic medicine
are required, as is a letter from a DO.
4. A fully completed transfer application, accompanied by a non-refundable application fee of $100;
and,
5. Upon request, candidates must submit a letter of good academic standing from the Academic Dean
of the osteopathic medical school where currently enrolled. If an interview is granted, candidates are
invited to the campus at their own expense. Candidates should plan to spend a half day on campus for
orientation and interview. Approximately three weeks after the interview, candidates will receive a letter
stating the decision of the Admissions Committee. Acceptance of a transfer student will be dependent
upon the student's current academic good standing, qualifications, academic compatibility and available
space. Confirmation of available seats does not occur until mid-June.
Applications are to be sent directly to:
Western University/COMP, Admissions Office
309 E. Second Street
Pomona, California 91766-1854
Decisions of the Admissions Committee regarding the admission of applicants to the Doctor of
Osteopathic Medicine program are final.
47
REGISTRATION
All students are required to register in person on the registration day specified in the University Calendar
or as otherwise directed by the Registrar. Failure to register on that day may be grounds for dismissal.
Third- and fourth-year DO students must complete registration materials, including financial arrangements,
prior to June 15. Failure to register by June 15 may be grounds for dismissal. Full tuition and fees and all
prior debts must be paid in full on or before registration day each academic year. Matriculation and
graduation are subject to the satisfactory completion of all academic requirements and payment of all
outstanding debts to the University. The receipt of a final transcript from an undergraduate college and a
physical examination with documentation of required immunizations prior to registration are additional
requirements for incoming students. Also, all students must show proof of current health insurance coverage
at the time of registration. This coverage must be maintained or in effect throughout the academic year. If
there is no proof of current coverage, a policy provided by the University is available. Attendance at
Orientation is mandatory for all incoming first-year students.
TUITION AND FEES
By action of the Board of Trustees, DO tuition and fees for the 2001-02 academic year (subject to
change) are as follows:
ACADEMIC YEAR 2001 - 2002
$28,010 Tuition (Annual)
For DO applicants accepted at Western University, the tuition deposit is $1,000,
payable within two weeks after notification of acceptance. This payment is non-
refundable.
An additional payment of $1,000 is due by May 15 for those accepted for
admission prior to May 1 and by June 15 for those accepted after May 1. This
additional payment is non-refundable.
Upon matriculation the entire $2,000 is applied toward the total tuition.
For applicants who are granted deferred admission to the DO program, the entire
$2,000 deposit required to hold a seat in the next year's class is non-refundable.
An additional enrollment deposit of $500 is due on May 15 of the entering year.
This total deposit of $2,500 is non-refundable and will be applied toward tuition,
upon registration and matriculation. If an applicant fails to register, all tuition
deposits are forfeited.
$40 Student Body Fee (1st and 2nd year)
Covers student government expenditures, social activities and public relations.
$20 Student Body Fee (3rd and 4th year)
Other Fees and Expenses
$600. Medical Equipment
$800. Required and Recommended Texts-Fall
$300. Required and Recommended Texts-Spring
$45. Anatomy Supplies-Gloves, Scrub, Dissection Kit
$30. (per day) Late Registration Fee
$50. Special Examination Fee
$40. Lost Locker Key
$10 Lost ID Badge
$5. (each) Copy of Official Transcript
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
48
National Board Fees (DO Program)
The College requires students to take all sections of COMLEX Level 1 and Level 2 of the National
Board of Osteopathic Medical Examiners as one of the requirements for graduation. These fees, which are
subject to change by NBOME, are as follows:
$255 NATIONAL BOARD EXAMINATION, COMLEX LEVEL 1 (end of second year)
$255 NATIONAL BOARD EXAMINATION, COMLEX LEVEL 2 (end of fourth year)
Clinical Rotation Expenses
During the third and fourth years, some students may elect to do some clinical rotations away from the
Pomona area. In addition, students are required to return to campus several times during the clinical years
for various educational experiences, conferences, etc. Any travel, food, housing or other expenses incurred
by these activities or plans are the student's responsibility. Some rotations done at or through other
institutions (e.g., certain hospitals or other medical schools) may involve application fees and/or other
charges. Because of the elective and individual nature of the experience, these fees are also the student's
responsibility.
ACADEMIC REQUIREMENTS
Academic Advisement
Students will be assigned a faculty advisor upon matriculation. Advisement by the faculty should be
viewed by the student as a privileged part of the academic process. The academic advisor-student
relationship can become one of the most valuable aspects of medical education. It will provide an
opportunity to develop sustained individual contacts between faculty and students on both academic and
personal levels. If either the student or the instructor does not find the relationship helpful, either is free to
seek a change.
Grading Policies and Credit Hours
a. Official grades are turned into the Registrar from the Dean of Osteopathic Medicine, at which time,
official grade reports are deposited in the student mail lockers. Enrolled students will receive an unofficial
copy of their transcript after grades have been posted at the conclusion of each academic year. COMP
makes use of a combination of numeric scores and letter grades. A numeric score is utilized in the first two
years, and a 4-value letter grade is used in the last two years.
Years 1 & 2 Years 3 & 4
Interpretation Letter Grade Grade Points
90-100 Excellent (numeric range 90-100) A 4
80-89 Good (numeric range 80-89) B 3
70-79 Satisfactory (numeric range 70-79) C 2
Below 70 Unsatisfactory (numeric range less than 70) U 0
I Incomplete 0
Au Audit 0
M Missing 0
W Withdrawal 0
Cr Credit 0
NCr No Credit 0
Cert Certification 0
Courses are rated at one credit hour for each 12 hours of lecture or 24 hours of laboratory and/or
practice sessions. Credit hours of 2.5 will be assigned for each week of clinical rotations. A cumulative
numeric score/grade point average will be calculated and posted on the transcript. Class ranking is also
computed, and will appear on the transcript at the student’s request only. Class ranking is also available
upon request in the Registrar’s Office. Cumulative class ranking for transfer students will not be calculated
until they complete one full academic year. Five-year program students will not be ranked until they have
49
completed 1A and 1B of the five-year program. Osteopathic undergraduate teaching fellows will not be
ranked until their final year.
b. The cumulative numeric score will be calculated at the end of each semester during the first two
years of the curriculum and is the average of all course numeric scores weighted by the number of course
credit hours attempted. The grade point average will be calculated at the end of each semester for 3rd and
4th year students and is the sum of earned grade points divided by the sum of credit hours passed and failed.
If a course, system, or clinical rotation is repeated or remediated, only the last score/grade earned enters
into the computation of the cumulative numeric score/grade point average, but the original numeric
score/grade remains on the student’s transcript.
After completion of the Second Year program, a student with a cumulative numeric score of 75 or less
may have all Third Year clinical rotations assigned by the Assistant Dean for Academic Affairs. After
completion of eight (8) clinical rotations, the Student Academic Progress Committee will review the
student’s progress. The Student Academic Progress Committee will recommend to the Dean of Osteopathic
Medicine the manner in which the scheduling of the student’s Fourth Year clinical rotations should proceed.
No numeric score or grade will be changed unless the instructor certifies in writing to the Registrar that
an error in computing or recording the grade/score occurred or that the student has remediated a numeric
score of below 70 or an Unsatisfactory grade after being directed to do so by the Dean of Osteopathic
Medicine, as recommended by the Student Academic Progress Committee.
For on-campus courses, students have a maximum of two weeks from the time examination results are
returned to them to bring any errors or irregularities in grading to the attention of the instructor.
All recorded grades remain on the official transcript unless a clerical error occurs. Remediated grades
are recorded below the original numeric score in the first two years or below the original “U”, “NCr”, or I
in the last two years. Only the remediated score/grade is calculated into the GPA/cumulative numeric score.
c. For 3rd and 4th year students, no grade will be changed after one month from the time the grade is
recorded in the Office of the Registrar.
Within the above designated time, grade changes for clinical rotations will be considered ONLY under
the following three conditions:
1. When the Office of Clinical Rotations receives a signed written statement from the
preceptor specifying that a clerical error has been made regarding a grade, and that the
purpose of the change is to correct that clerical error.
2. When the preceptor to whom the student was assigned submits a signed written request to
have the grade changed. The request must include justification for making the change.
3. When a remediation process, that has been directed by the Student Academic Progress
Committee and authorized by the Dean, is completed and a written evaluation is received
in the Office of Clinical Rotations.
All grade changes must have the approval of the Dean of Osteopathic Medicine.
The student should make every effort to discuss his/her evaluation(s) with the assigned preceptor(s)
prior to leaving the clinical rotation.
d. If a student leaves a rotation before it is finished without the permission of the Assistant Dean for
Academic Affairs, or is asked to leave a rotation by the Preceptor or the Director of Medical Education of a
hospital, a grade of “U” on that rotation may be assigned by the Dean of Osteopathic Medicine or Assistant
Dean for Academic Affairs.
e. Standards of Satisfactory Progress - Students must maintain at least a cumulative score of 70 on a
yearly basis during the first two years and a “C” average during the last two years to be considered making
satisfactory academic and professional progress.
A numeric score below a 70 during the first two years or a “U” in the last two years must be remediated
for promotion or graduation.
Incomplete Grade (I) - An Incomplete (I) indicates that a student has not been able to finish all required
work for issuance of a letter grade. An “I” is not counted in the grade point calculations until a letter grade
is issued to replace the “I”. An “I” must be replaced before the student registers for the next academic year,
unless other arrangements are made with the instructor and the Dean of Osteopathic Medicine.
Replacement of an “I” will be under the direction of the instructor with the approval of the Dean. If the
required work is not completed within the specified time, the “I” will be converted automatically to a “60”.
It is to the student’s advantage to arrange to make up any incomplete work as soon as possible. The
50
incomplete (I) remains on the transcript indicated by an asterisk and followed by the grade/numeric score
earned.
Credit Courses (Cr/NCr) - Courses graded for Credit/No Credit are those designated by the faculty as
courses required for promotion but not assigned letter grades. The student must satisfy the requirements of
these courses to receive credit.
Audit Classes (Au) - Students will not be eligible for Financial Aid if they are auditing classes only, and
are not taking tests and having their progress monitored.
Exemption from Individual Core Curriculum Course
Students with advanced work or degrees in a particular subject may formally petition the professor and
the Dean of Osteopathic Medicine for credit for an individual core curriculum course. The petition must
include the reasons for the request and all necessary documentation, and must be submitted by the end of
the first week of class. The student must comply with the attendance policy until notification that
exemption has been granted. The professor(s), before recommending exemption, will require acceptable
performance on an examination. The professor(s), in consultation with the Dean of Osteopathic Medicine
may suggest other alternative or additional criteria for determining exemption.
Student Examination Policies
a. Students will be seated for examinations such that there will be a vacant seat between them and the
students on either side, and this alternate seating shall be utilized for examinations unless precluded by
space availability.
b. Students are not to communicate in any way during the examination, are not to look at any other
students’ examination paper, and are to face the front of the classroom at all times.
c. There will be at least two different versions of the same examination.
d. During scheduled examination hours, students will not be allowed to leave the exam room except in
an emergency and as excused by the proctor. If the student has to leave the room, his/her examination will
be turned into the proctor.
e. Once a student finishes an exam and leaves the examination room, he or she will not be permitted to
re-enter the room until the exam is declared over.
f. All students’ belongings, i.e. notebooks, calculators, headwear, and head sets, etc., will be kept in
front of the room. No food or drink will be allowed during examinations.
g. No student questions will be answered during the examination period. Students should be permitted
to point out typographical errors present in the examination notebook. If students have questions, they can
be written on the back of the examination booklet.
h. Violations of these examination policies as stated in the Student Handbook or Standards of
Professional Conduct, will be brought before the Student Conduct Committee.
Violations of Examination Policies
a. If there is reason to suspect a violation of examination policies during an exam, the proctor(s)
suspecting a violation should share the information with the other proctor(s) in the classroom immediately.
b. Proctors immediately should attempt to confirm the violation.
c. If the proctors agree that a violation has occurred, then the examination booklet(s) and the scantron(s)
will be confiscated, in which case the student(s) will be asked to leave the examination room.
d. The proctor responsible for the conduct of the examination, after the completion of the examination,
will immediately make a verbal report to the Assistant Dean of Academic Affairs and the Dean of
Osteopathic Medicine, that a violation has been observed. The individuals making the verbal report must
submit a written report to the Dean of Osteopathic Medicine during the same day as the incident occurs.
e. The Dean of Osteopathic Medicine may convene the Student Conduct Committee as soon as possible
to investigate the violation, if deemed appropriate.
f. If the evidence presented to the Student Conduct Committee is conclusive, the recommendations to
the Dean of Osteopathic Medicine may include, but not be limited to:
1. Dismissal from the academic program.
2. Academic Probation - Period to be recommended by the Committee.
51
3. Make-up examination, including written and/or oral.
4. The numerical grade on a make-up examination will be 80% of the grade attained.
g. In the case of insufficient evidence, the committee will recommend to the Dean of Osteopathic
Medicine that no action be taken against the student.
h. After the receipt of the recommendation of the Student Conduct Committee by the Dean, the
disposition of the incident will be conveyed to the involved student(s) by the Dean of Osteopathic
Medicine, in writing, as soon as possible, but not exceeding three working days.
Examination Proctoring Policy
a. The number of rooms for any examination will be determined by the Assistant Dean of Academic
Affairs in consultation with the system or course coordinator or discipline leader.
b. The Assistant Dean of Academic Affairs will receive a copy of the proctoring schedule from the
discipline leader/coordinator, by noon on the last working day before the scheduled exam.
c. A minimum of two proctors per exam will be in the exam room at all times.
d. Typographical or other errors pointed out by students should be brought to the attention of the system
or course coordinator immediately.
e. Proctors will not answer questions during the examination period, and will see that students are
looking at their own examination paper.
f. Proctors will be responsible for handing out examinations/Scantrons® to each student, assuring
proper seating, and collection of examination notebooks and Scantrons®.
g. Proctors should see to it that all students’ belongings are kept at the front of the examination room.
Students on Clinical Rotations - NBOME Examination (COMLEX, Level 2)
Fourth year medical students on rotation at the time NBOME, COMLEX Level 2 examination is offered,
may arrange for time-off just prior to, and during administration of the examination. Western
University/COMP requests all training program directors and/or preceptors to release students three
working days (weekends included) before the exam, at 7:00 am, and expect their return to duty at 7:00 am
the day after the examination is concluded. For example, if the exam is administered on Tuesday and
Wednesday, the student should be released from duty on Saturday morning at 7:00 am, and will return to
duty at 7:00 am on Thursday morning.
Students on Clinical Rotations may contact the Rotations Office toll-free at 1-800-249-9131.
Promotion
Promotion is defined as academic and professional progression from one academic year to the next.
a. A student will be recommended to the Dean of Osteopathic Medicine for promotion by the Student
Academic Progress Committee.
b. A student may not be recommended for progression from one academic year to the next with any
outstanding grades of “I”, “NCr” in a required course, “U” or numeric score of less than 70 on his/her
academic record, or with a yearly grade point average of less than 2.0/cumulative numeric score of less than
70.
c. When considering a student for promotion, ethical, professional, and personal conduct may also be
taken into consideration (see Probation in University Academic Policies, section a-3).
d. A student will be promoted provided that all legal and financial requirements of the University as
stated in the University Catalogue have been satisfied.
e. All academic requirements must be met prior to recommendation for graduation within a maximum of
six academic years.
f. All students beginning with the incoming class of 2005 are required to pass Part I of the COMLEX
examination before they are allowed to enter into the 4
th
year.
Veterans
Veterans who fail to maintain satisfactory progress for more than one semester will not be certified to
receive any Veteran’s benefits until they have corrected the situation and are making satisfactory progress.
52
Graduation
A student will be recommended for the degree Doctor of Osteopathic Medicine provided he/she:
a. Has completed at least four years in an accredited osteopathic college or equivalent.
b. Has been enrolled in the Western University of Health Sciences/College of Osteopathic Medicine of
the Pacific during his/her final two academic years.
c. Is not on probation and has completed all prescribed academic requirements with a cumulative
numeric score of at least 70/grade point average of at least 2.0 and has no outstanding grade of I or U or a
grade of “NCr” in a required Credit/No Credit course.
d. Has taken all sections of Level I of the COMLEX examination of the NBOME (National Board of
Osteopathic Medical Examiners). Beginning with the Class of 2003 (entering in 1999), he/she has taken all
sections of Level I and Level II of COMLEX.
e. Has taken and passed Clinical Performance Examinations I and II. Students who have not passed
either Clinical Performance Examination I or II are required to remediate the examination they did not pass.
f. Has demonstrated superior ethical, professional, or personal conduct, as defined in Probation in the
University Academic Requirements section, which would make it appropriate to award the degree of Doctor
of Osteopathic Medicine.
g. Has complied with all the legal and financial requirements of the University as stated in the
University Catalogue.
h. Unless special permission has been granted by the President of the University, all students must
attend in person and participate in the commencement program at which time the degree is conferred. If the
President grants special permission to be excused from graduation, the graduate may be required to present
him or herself to the Provost or appropriate Dean, at a later date, to take the required oath (if relevant) to
receive the diploma.
i. Is expected to complete all requirements for graduation by July 31 and is expected to march with
his/her class in the graduation ceremony. At the discretion of the Dean of Osteopathic Medicine, an
exception may be made for a student with an authorized leave during the senior year. No student will
receive his/her diploma until the student has completed all requirements for graduation. Diplomas should
be dated as appropriate to completion date of the academic requirements.
Probation
All statements in the General Academic Requirements section on Probation apply, plus the following:
a. Inadequate academic progress as determined by the Student Academic Progress Committee. These
include, but are not limited to, receiving a numeric score less than 70 in the first two years in any course or
system, a grade of NCr in a required Cr/NCr course, or a “U” in any clinical rotation or EFM course.
b. A cumulative score of less than 70 in the first two years or a GPA of less than 2.0 in the last two
years.
c. When directed to repeat a year for academic reasons.
d. Seriously deficient ethical, professional, or personal conduct.
e. On-campus students on probation must meet with their faculty advisor at least once a month. Off-
campus students on probation must contact their faculty advisor once a month. It is the student’s
responsibility to contact the faculty advisor to arrange these meetings.
f. A first or second year student on probation for a score less than 70 in the first semester will be
removed from probation after one semester provided he/she has regained a cumulative score of at least a 70
and has remediated the course
g. A first or second year student will be removed from probation when all scores below a 70 have been
remediated satisfactorily according to the following Remediation section.
h. A third or fourth year student on probation because of a “U” grade in a clinical rotation or in an EFM
course must remediate the “U” and will then be subject for review by the Student Academic Progress
Committee at the end of the third or fourth year, respectively, and may be recommended for continuation on
or removal from probation at that time.
53
Remediation
If a student receives a final numeric score below 70 in a course or system during the first two years, or
has a cumulative numeric score below 70, that student will be reviewed by the Student Academic Progress
Committee.
If a student receives a “U” in a clinical rotation in years three or four, that student will be reviewed by
the Student Academic Progress Committee.
In reviewing the student’s academic deficiencies, the following guidelines shall be used:
Educational objectives underlie remedial teaching and evaluation should be the same as the educational
objectives that underlie regular courses in the curriculum.
a. Where deemed appropriate, the Student Academic Progress Committee, after consultation with the
course instructor, system coordinator, or Director of Clinical Rotations, may recommend any one of the
following options:
1. Take a comprehensive examination.
2. Complete special projects or studies in the deficient area(s).
3. Repeat the course.
4. Repeat the academic year.
5. Withdraw from the University (see Dismissal section for criteria for this option).
b. The score/grade achieved by remediation will be the score/grade recorded EXCEPT that the highest
score/grade a student may earn by options a-(1) or a-(2) is a score of 70 in the first two years and a “C” in
the last two years. The score/grade achieved by remediation will be recorded on the transcript beneath the
original score/grade.
c. Numerical scores or grades earned during an attempted remediation of a course, system, or clinical
rotation will be reviewed critically by the Student Academic Progress Committee and the Dean of
Osteopathic Medicine. Failure to earn at least a 70 in the first two years or a “C” in the last two years or
“Cr” may result in dismissal from the College or repeating the year.
d. Decisions regarding remediation will be made on an individual basis after considering all pertinent
circumstances in each case. The decision will be made by the Dean of Osteopathic Medicine, based upon
the recommendation of the Student Academic Progress Committee. The Student Academic Progress
Committee will base its recommendation on the student’s academic record and considerations after
consultation with the student’s faculty advisor, course instructor, system coordinator, Director of Clinical
Rotations, clinical preceptor, and the student involved, when appropriate.
e. Any student who is required to remediate a course must be notified in writing by the Dean of
Osteopathic Medicine at least 15 working days prior to the remediation date, (or within 15 working days
after the close of the academic year in which the student is presently enrolled, whichever comes first).
Notification must be sent by Certified Mail or hand-delivered to the student and must be acknowledged with
the signatures of the Dean of Osteopathic Medicine or his/her designee and the student.
Remediation: Financial Aid Policy
If the student, at the end of the academic year, is still considered to be making unsatisfactory progress
and must remediate, he/she is removed from the list of Title IV and Title VII financial aid recipients.
Remediation of courses during the summer is not covered by any financial aid and cannot be considered
an expense item on the next year’s budget. Students attend at their own expense.
Appropriate tuition and fees will be determined by the Executive Vice President of Finance and
Administration in consultation with the Executive Vice President for Academic Affairs and the Dean of
Osteopathic Medicine.
Five-Year Program
Effective July 1, 2000, students will no longer be admitted to this program. The following rules and
requirements remain applicable for students currently enrolled in the Five-Year Program only.
a. The decision to enter the Five-Year Program is a one-time student option.
b. At the time the student opts for the Five-Year Program, prior courses completed and graded will be
shown on the transcript.
c. The words “Five-Year Program” will be printed at the beginning of the transcript.
54
d. During the second semester of the first year (I-A portion), the student will audit the Dermal,
Neurosensory, Musculoskeletal Systems and Introduction to Clinical Medicine. These will be listed on the
transcript along with the designation “Au”. If a student chooses to take the examinations in audited courses
and does well, it will not be possible to convert the “Au” to a grade.
e. The student will be required to repeat any courses that were completed and graded before going on
the Five Year Program if a “U” grade was received. Courses that are remediated will be taken concurrently
with the courses taken in the second year (I-B portion) of the Five Year Program. Recommendations for
remediation will be made to the Dean of Osteopathic Medicine by the Student Academic Progress
Committee.
f. The student’s progress will be monitored carefully each semester by the Student Academic Progress
Committee, the Assistant Dean of Academic Affairs and the Dean of Osteopathic Medicine. Students in the
first two years of the Five-Year Program will be dismissed if their grade point average is below 2.0 at the
end of any semester or if they receive a final grade of “U” or “NCr” in any course.
g. Students admitted to this program will be charged one year of full tuition for year I-A of the Five-
Year Program. Western University charges tuition for five years, however, the tuition charged for years I-
B, II, III and IV are seventy-five percent of the published tuition for other DO students.
Five-Year Program Schedule
YEAR I-A:
First Semester Credit Hours Second Semester Credit Hours
Gross Anatomy 14.5 OP&P 2.5
OP&P 2.0 Medical Ethics Cr
Embryology 1.0 Substance Abuse Cr
Histology 2.0 BCLS (during orientation)
____ ____
TOTAL 19.5 TOTAL 2.5
(Audit Introduction to Clinical Med. Week, Dermal, Neurosensory & Musculoskeletal Systems)
Summer I: Enrollment in and successful completion of a Study Skills Course
YEAR I-B:
First Semester Credit Hours Second Semester Credit Hours
Biochemistry 4.5 Introduction to Clinical
Microbiology 5.5 Medicine Week 2.0
Pathology 2.5 Dermal System 4.0
Physiology 1.5 Neurosensory System 19.0
Pharmacology 3.5 Musculoskeletal System 8.5
____ ____
TOTAL 17.5 TOTAL 33.5
(The student must attend the MS I Classes that OP&P TA’s attend, and at the discretion of the OP&P
Department Chair, may be used as an OP&P TA.)
YEARS II, III, & IV: In year II, the student will re-enter the standard COMP curriculum, and
will continue in the standard curriculum throughout years II, III and IV.
Dismissal
The University may require withdrawal at any time it deems necessary to safeguard its standards of
scholarship, conduct, and orderly operation. The Student Academic Progress Committee or the Student
Conduct Committee may recommend dismissal of a student for appropriate reasons as stated below:
55
a. A student with a yearly score of less than 70 at the end of the First or Second year will be
recommended for dismissal.
b. A student who received final scores below 70 in two or more courses or systems totaling more than
25% of the total credit hours for the First or Second year will be recommended for dismissal.
c. A student who received Unsatisfactory grades in three clinical rotations in one academic year will be
recommended for dismissal.
d. A student who receives a score of below 70 in the first two years or a “U” in the last two years in a
remediated course, system, or clinical rotation may be recommended for dismissal.
Student Academic Progress Committee
a. The Student Academic Progress Committee is comprised of five faculty members with the following
ex officio members: Dean of Student Affairs; Assistant Dean of Academic Affairs; and the Associate Dean
of Clinical Affairs & Research.
b. Each year, the Student Academic Progress Committee shall periodically review the academic
achievements and the performance of all students. The names and grades of students in academic difficulty
shall be made available to the Student Academic Progress Committee by the Registrar with additional input
from the Dean of Osteopathic Medicine and the Director of Clinical Rotations, where appropriate.
c. After reviewing a student’s achievement and performance records, the Student Academic Progress
Committee may recommend to the Dean of Osteopathic Medicine any of the following courses of action for
a student: promotion, probation, remediation, dismissal from the University, psychological and educational
assessment and other appropriate recommendations, or no action.
d. The Student Academic Progress Committee also has the responsibility of recommending the
awarding of the degree of Doctor of Osteopathic Medicine to all students who satisfactorily complete all
requirements for graduation as stated in the University Catalogue and this Student Handbook to the Faculty
as a whole.
e. All recommendations of the Student Academic Progress Committee shall be in writing to the Dean of
Osteopathic Medicine, who will make the information available to the affected student.
Attendance and Absences
Attendance is required at all scheduled instructional periods. Absence from instructional periods for any
reason does not relieve the student from responsibility for the material covered during the periods.
Frequent absences will be viewed as violations of the Standards of Academic and Professional Conduct.
Implementation of the attendance policy for on-campus courses will be the responsibility of the Assistant
Dean of Academic Affairs.
Students are required to be present for all scheduled examinations and cannot begin an examination
more than 15 minutes after the scheduled time without permission from the Assistant Dean of Academic
Affairs or his designee. For a student to be considered to take any examination at other than the scheduled
time, the student must have prior approval by the Assistant Dean of Academic Affairs.
A student who cannot attend an exam due to unforeseen circumstances including illness, should phone
or e-mail the Assistant Dean of Academic Affairs and Course Instructor/System Coordinator as soon as
possible prior to or after the exam has been administered. A written explanation of the absence (including
documentation on physician letterhead stationery, if it is an illness) must be provided the next day the
student is on campus to the Office of the Assistant Dean of Academic Affairs and the Course
Instructor/System Coordinator). If a student misses an examination, the Assistant Dean of Academic
Affairs in consultation with the Course Instructor/System Coordinator will rule on whether the absence is
excused or unexcused. If the absence is ruled excused, the student will be permitted to take a make-up
examination, the nature and time of the examination will be at the discretion of the Course
Instructor/System Coordinator. If the absence is excused, the student will receive full credit for the make-
up examination. If the absence is unexcused (e.g., failure to show up for a written or practical examination
without a valid excuse as determined by the Assistant Dean of Academic Affairs and the Course
Instructor/System Coordinator, this is grounds for summary failure (a score of zero) of that examination.
In the case of an unexcused absence, the student who fails the examination will be referred to the
Student Academic Progress Committee for recommendations regarding remediation or dismissal. If the
Student Academic Progress Committee recommends that the student take a remediation examination, the
maximum score that the student can achieve on a remediation examination will be 70%. If the student fails
to take either a make-up or a remediation examination at the time designated by the Course
56
Instructor/System Coordinator, without a valid excuse as delineated above, this will be grounds for
summary failure (a score of zero) of that examination with referral to the Student Academic Progress
Committee as depicted above. In such a case, a written report will be sent by the Course Instructor/System
Coordinator to the Office of the Assistant Dean of Academic Affairs, with a copy sent to the Chair of the
Student Academic Progress Committee and the Dean of Osteopathic Medicine for appropriate disposition.
Attendance and absences during the third and fourth years are outlined in the COMP Clinical Rotations
Manual.
CURRICULUM
The curriculum at COMP is a four-year full-time academic and clinical program leading to the granting
of the degree of Doctor of Osteopathic Medicine (DO).
This curriculum stresses the interdependence of the biological, clinical, behavioral, and social sciences.
The emphasis is to educate physicians for primary care medicine with specific roles of osteopathic
principles in the maintenance of health and treatment of disease.
The educational program is centered around the basic concepts of osteopathic medicine. The College of
Osteopathic Medicine of the Pacific identifies and develops the knowledge, cognitive and psychomotor
skills, and the personal and professional behaviors required of an osteopathic primary care physician in
order to provide competent and comprehensive health care to all members of a family, on a continuing
basis. This academic program is intended to meet the following goals:
a. To accord primacy to the role of the musculoskeletal system in the total body economy.
b. To recognize and emphasize the inherent capacity within the total person to overcome disease and
maintain health; to educate physicians to cooperate with this therapeutic capacity in their methods of
treatment, and;
c. To provide sufficient academic training to make students aware of health needs that must be referred
to a specialist.
A primary care physician must first of all be capable of problem-solving and develop expertise in
diagnosis. In order to achieve this goal, the curriculum adopted at COMP emphasizes the integration of
basic and clinical science aspects of medical practice. With this approach, practice in problem-solving
becomes a part of the learning experience.
The curriculum is divided into three phases:
I. Introduction to the basic sciences.
II. Correlated system teaching, incorporating basic and clinical sciences in the study of ten (10) organ
systems of the body, and;
III. Clinical experiences.
The four-year curriculum has been developed to appropriately prepare the graduate for the post-doctoral
training years of his/her choice.
In addition to the regular curriculum, COMP offers elective courses. These focus on the art of medicine
and seek to sensitize the future physician to the important aspects of life and to instill a greater sense of
ethics and human values. Various extracurricular activities also contribute to the personal and professional
growth of students, among them a student drama troupe called SANUS.
Summer Preparatory Program
The College offers an optional three-week introductory preparatory program to a selected number of
incoming DO students. The students will have to purchase a workbook and remit a tuition fee of $300. See
course description for DO 5001, below, for additional information.
PHASE I: First Year-First Semester (CORE courses)
The first semester of the first year is designed to introduce the students to the basic concepts of anatomy
(gross, embryology, and histology), biochemistry, microbiology, pathology, pharmacology, and physiology.
Interwoven throughout the curriculum are osteopathic principles and practice.
DO 5010 Biochemistry (4.5 credit hours)
DO 5020 Embryology (1 credit hour)
DO 5025 Medical Genetics (1 credit hour)
DO 5030 Gross Anatomy (14.5 credit hours)
57
DO 5040 Histology (2 credit hours)
DO 5050 Microbiology (5.5 credit hours)
DO 5060 Pathology (2.5 credit hours)
DO 5070 Pharmacology (3.5 credit hours)
DO 5080 Physiology (1.5 credit hours)
DO 5090 Osteopathic Principles and
Practice I (2 credit hours)
PHASE II: Second semester-first year through Second semester-second year
This phase begins in the second semester of the first year and continues throughout the second year. The
basic and clinical sciences concerned with one particular organ system of the body are integrated in
classroom instruction. This approach emphasizes the relevance of basic sciences to clinical practice. The
osteopathic approach is continually emphasized by lecture and laboratory demonstration including
manipulative techniques. Other courses not directly related to a system are also included in Phase II as
Family Medicine Core Courses.
First Year-Second Semester
DO 5110-Dermal System (4 credit hours, 4 weeks)
DO 5120-Neurosensory System (17.5 credit hours, 10 weeks)
DO 5130 Musculoskeletal System (7.5 credit hours, 4 weeks)
DO 5140 Medical Ethics (Cr/NCr)
DO 5150 Introduction to Clinical Medicine (ICM) I (2 credit hours, 1 week)
DO 5160 Behavioral Science and Substance Abuse (2.5 credit hours)
DO 5190 Osteopathic Principles and Practice II (2.5 credit hours)
Second Year-First Semester
DO 6010 Blood and Reticuloendothelial System (7.5 credit hours, 3 weeks)
DO 6020 Cardiovascular System (14.5 credit hours, 9 weeks)
DO 6030 Public Health (1 credit hour, 1 week)
DO 6040 Respiratory System (9.5 credit hours, 7 weeks)
DO 6050 Psychiatry (2 credit hours)
DO 6090 Osteopathic Principles and Practice III (2.5 credit hours)
Second Year-Second Semester
DO 6110 Renal System (5.5 credit hours, 3 weeks)
DO 6120 Endocrine System (5.5 credit hours, 3 weeks)
DO 6130 Reproductive System (8 credit hours, 4 weeks)
DO 6140 Gastrointestinal System (13 credit hours, 7 weeks)
DO 6150 Introduction to Clinical Medicine (ICM) II (Cr/NCr)
DO 6160 Medical Jurisprudence (1 credit hour)
DO 6190 Osteopathic Principles and Practice IV (5 credit hours)
*Clinical Performance Examination I will be administered at the end of the second year of the curriculum.
Students are required to pass this examination in order to be promoted to Phase III of the curriculum.
PHASE III: Clinical Training-Third and Fourth Years
Rotations Office
The Director of Clinical Education and the Rotations Office staff are dedicated to providing our students
with the best possible clinical education and providing exceptional service to everyone with whom they
interact. The Office assists the College of Osteopathic Medicine of the Pacific and its students with
planning for and completion of their clinical training in the third and fourth years.
Goals
The goal of COMP's clinical curriculum is to prepare each COMP student with the knowledge, attitudes
and skills to excel in their chosen postdoctoral training program. Specifically, the student will be able to:
• Identify the wide range of normal human functioning.
58
• Recognize, diagnose and treat the most commonly encountered health conditions in a family
practice;
• Recognize, diagnose and treat the acute, life-threatening conditions encountered by the family
physician.
• Differentiate health and common health problems from less common diseases.
• Recognize conditions or situations which are best handled by consultation and/or referral.
• Provide continuity of health care beginning with initial patient contact.
• Assess and treat chronic medical conditions in various stages of progression.
• Develop appropriate, professionally intimate relationships with patients.
• Understand patients' individual concerns and incorporate those concerns into routine patient care.
• Integrate osteopathic philosophy and practices into routine patient care.
• Access medical references including up-to-date medical literature to understand current medical
knowledge and thought.
• Understand and apply the concepts of community oriented primary care, epidemiology, health
screening and prevention, and;
• Understand and work with the family unit to improve the health and welfare of the individual
patient and his/her family.
Clinical Curriculum
COMP's clinical curriculum consists of the following four-week rotations:
Third Year
1 Family Practice
3 Internal Medicine (2 General; 3rd General, GI, CARD, or PULM)
1 Surgery (General)
2 Pediatrics
1 Psychiatry
1 Obstetrics/Gynecology
1 Osteopathic Manipulative Medicine
1 Geriatrics
1 Vacation (not first rotation)
Fourth year
1 Family Practice
2 Internal Medicine (General, GI, CARD, PULM, NEURO)
1 Surgery (General or subspecialty)
1 Emergency Medicine
5 Electives
1 Vacation
** Clinical Performance Examination II will be administered during the fourth year of the DO curriculum.
Students are required to pass Clinical Performance Examination II in order to graduate from the Doctor of
Osteopathic Medicine program.
Each year's curriculum requirements may be completed in any order. There is a mandatory four week
break at the end of the MSIII year.
The minimum length of a rotation is four weeks. Rotations may not be split. A substantial number of
rotations may be assigned for MSIII and IV years by the Rotations Office, including a block of rotations
(four - six) . The student may express a preference for preceptors, geographic locations, etc. for the
remaining rotations.
59
Implementation
Preceptors and hospitals will implement the curriculum in a manner which balances the learning needs
of the students and the educational resources available at the site. Preceptors and sites are encouraged to use
a variety of teaching techniques including observation, monitored participation, video and audio recordings,
computers, readings, individual discussions, and presentations by students, faculty and others to enhance
learning.
Non-Clinical Experiences
Non-clinical experiences like conferences, tumor board, quality assurance meetings, hospital
committees, etc. are important for students to observe in order to help them understand and appreciate the
full spectrum of activities expected of physicians. We hope that physicians will invite students to participate
in as many non-clinical experiences as are practical.
Procedural Skills
Part of the College's expectation is that students will gain a knowledge and understanding of various
procedural skills. In addition to proficiency in the manual aspects of procedural skills, the College expects
that the student will understand the indications, contraindications, risks, benefits and alternatives for various
procedures. Student performance of any procedure on a patient must be under the direct supervision of the
assigned preceptor or their professional designate.
Evaluation of Students on Clinical Rotations
The "preceptor of record" is the physician to whom the student is assigned for a given rotation according
to the Rotations Office records. That physician is responsible for the rotation evaluation including a rotation
grade. If the preceptor of record cannot or will not assign a grade, the Assistant Dean for Academic Affairs
will determine a grade for the rotation.
Recording of Grades
No grade may be changed more than 20 business days after it is reported by the Clinical Rotations
Office to the Registrar for any reason other than a clerical error. Within those 20 days, a grade may only be
changed if the Rotations Office receives a signed statement from the preceptor specifying that a clerical
error had been made regarding the grade.
COURSE DESCRIPTIONS
Courses listed in this catalog are subject to change through normal academic channels. New courses and
changes in existing course work are initiated by the appropriate disciplines, departments, or programs,
approved by the Medical School Curriculum Committee, the faculty, the Dean of Osteopathic Medicine and
the Executive Vice President of Academic Affairs. Unless otherwise noted, student performance in these
courses is graded using the College's numerical score system during the first two years and a letter grade in
the final two years of the curriculum.
DO 5001 Summer Preparatory Program (0 credit hours, Cr/NCr)
The purpose of the Summer Preparatory Program is to prepare incoming students for the Gross Anatomy
course and to provide an introduction to Biochemistry. The anatomy component focuses on the skeletal,
muscular, cardiovascular and nervous systems, along with a brief overview of the other body systems. Also
included in the program are presentations that focus on enhancing student study and test-taking skills. This
course is designed for students not having prior coursework in human anatomy. Acceptance into this
program is at the discretion of the instructor/coordinator. The course is elective and does not count toward
meeting the requirements of the Doctor of Osteopathic Medicine curriculum. A separate tuition of $300 is
charged for this program.
DO 5010 Biochemistry (4.5 credit hours, Numeric Score)
This course explains the molecular basis of life and how human physiology can be understood in
biochemical terms. The broad objective is to contribute to the formation of a solid foundation of knowledge
for future comprehension of the biochemistry of each organ system, the disease states caused by
biochemical abnormalities and the biochemical basis for clinical diagnosis and therapy.
60
DO 5020 Embryology (1 credit hour, Numeric Score)
This course traces, through lectures and demonstrations, the basic developmental stages of the human
from fertilization to organogenesis. Specific attention is given to anomalies of early development and
teratology. Basic information necessary to understand the development of organ systems is provided.
DO 5025 Medical Genetics (1 credit hour, Numeric Score)
This course provides the student with an introduction to genetic principles and practices applicable to
the contemporary practice of medicine. Topics covered include pedigree analysis, structural gene
mutations, the human genome, X-linked genetic transmission, triple repeat diseases, inborn errors of
metabolism and newborn screening.
DO 5030 Gross Anatomy (14.5 credit hours, Numeric Score)
The objective is to provide the student with an understanding of the structure and arrangement of the
gross anatomical features of the human body. Students are introduced to the language of anatomy and the
clinically important relationships through lectures and laboratory dissection of cadavers. Models,
radiographs and special demonstrations are used to help emphasize areas useful to the physician.
DO 5040 Histology (2 credit hours, Numeric Score)
The course introduces the student to an understanding of the structure and function of cells and tissues
using light and electron microscopy. Emphasis is on the structural specialization, function and interaction of
cells in forming the four basic tissues and the study of the structural arrangements of the basic tissues in
organs. The aim of the lectures is to introduce and amplify the laboratory work and stress current concepts.
The laboratory provides an opportunity for the visual examination of cells, tissues and organs using the light
microscope.
DO 5050 Microbiology (5.5 credit hours, Numeric Score)
The objective of the course is to enable students to recognize and describe major groups of
microorganisms responsible for infectious diseases. The course stresses the structure, physiology and
genetics of microorganisms in relation to their pathogenicity. The salient features of bacteria, fungi,
protozoa, viruses and viroids are discussed. In addition, a thorough knowledge of the host-parasite
relationship, including characteristics of organisms contributing to disease and host-defense mechanisms,
are stressed. Fundamental concepts of immunology, including the structure of antigens and antibodies,
serological reactions, their underlying principles and their diagnostic applications are emphasized.
Laboratory experiments are designed to augment the lectures and to provide the student with an
appreciation of the functioning of a diagnostic laboratory.
DO 5060 Pathology (2.5 credit hours, Numeric Score)
The course is devoted to the basic pathogenesis and morphology of disease. Cell injury and death,
inflammation, the repair process, hemodynamic changes, neoplasia, chemical and physical injuries are
discussed. The laboratory is designed to supplement the lectures, utilizing glass slides, gross specimens and
Kodachrome slides. Introductory lectures on laboratory medicine are presented.
DO 5070 Pharmacology (3.5 credit hours, Numeric Score)
This is a basic course designed to orient medical students to the effect of drugs on biological systems.
The initial part of the course deals with general principles in pharmacology, including drug absorption,
distribution, action, toxicity, biotransformation and elimination. The latter part of the course focuses upon
chemotherapeutic agents used in treating infectious diseases. Concepts and principles will be introduced
which are important for the rational evaluation and utilization of drugs in the practice of osteopathic
medicine.
DO 5080 Physiology (1.5 credit hours, Numeric Score)
This course is an integrated approach to the general physiology of cells, with a special emphasis on
excitable cells, i.e., the neuron and muscle cell. Basic concepts on the functions of cells and control of
cellular activities are reviewed. The course is designed to provide a solid foundation for the first-year
61
medical student to comprehend basic physiologic theory and to integrate these principles into a better
understanding of organ and system function and, ultimately, enable a better appreciation of total body
physiology.
DO 5090 Osteopathic Principles and Practice (2 credit hours, Numeric Score)
This core course is designed as an introduction and development of the basic philosophy and principles
of osteopathic health care. The course is offered throughout the four semesters of Phase I and Phase II.
Emphasis is on the sequential development of palpatory diagnostic and therapeutic skills of osteopathic
manipulative medicine. Recognizing the contribution of the musculoskeletal system to health and disease,
the course integrates the osteopathic philosophy of patient care with the systems approach of medical
education. The course teaches osteopathic history, philosophy, problem-solving and patient management,
incorporating multiple osteopathic manipulative techniques as appropriate, including: muscle energy,
myofascial release, high velocity and low amplitude, counterstrain, articulatory techniques, trigger point and
osteopathy in the cranial field.
DO 5110 Dermal System (4 credit hours, Numeric Score)
The first system studied is the Dermal System. Problems of the skin are discussed by qualified medical
professionals. The clinical lectures are coordinated with embryology, histology, physiology, biochemistry,
pharmacology, microbiology, pathology and dermatopathology.
DO 5120 Neurosensory System (17.5 credit hours, Numeric Score)
This course deals with the brain, spinal cord and the peripheral nervous system. The embryology,
histology and neuroanatomy along with biochemistry, physiology and pharmacology are considered. In
addition to infections of the nervous system, pathology, neurology, ophthalmology, otorhinolaryngology are
important components. Sleep disorders, cerebrovascular disorders, aging and dementia are also considered.
DO 5130 Musculoskeletal System (7.5 credit hours, Numeric Score)
The importance of the musculoskeletal system is readily apparent, being the largest system of the body,
comprising nearly 70 percent of the body mass. The embryology, histology and functional anatomy,
including kinesiology, are presented in this course as well as biochemistry, pharmacology, physiology and
microbiology. The pathology and clinical aspects of this system are discussed along with the related topics
of sports medicine, rehabilitative medicine, exercise, rheumatoid diseases and orthopedics as they all relate
to the primary care practice of osteopathic medicine.
DO 5140 Medical Ethics (0 credit hours, Cr/NCr)
This is an introduction to the ethical principles and methods of analysis used in medical ethics. The aim
is to provide a systematic framework for resolving ethical dilemmas encountered in the practice of
medicine. Medical Ethics is covered in Phases II and III.
DO 5150 Introduction to Clinical Medicine I (ICM I) (2 credit hours, Numeric Score)
The primary purpose of the Introduction to Clinical Medicine sequence is to prepare students for clinical
rotations. The preparation is geared both to communication and clinical skills. ICM-I is designed to
introduce the clinical skills believed to be the most important in becoming an osteopathic physician. It is a
one-week introductory course taught during the MSI year. Students are taught basic history taking and
physical examination skills. The course emphasizes the cognitive and affective skills needed for clinical
reasoning and communication between the patient and the physician. Verbal and non-verbal communication
techniques are taught utilizing real, as well as simulated, patients.
DO 5160 Behavioral Science and Substance Abuse (2.5 credit hours, Numeric Score)
This course deals with biological, psychological and social aspects of behavior in relation to medicine.
Major topics include etiology and treatment of substance abuse, the physician-patient relationship, emotion
and personality, etiology of gender identity and sexual orientation, evolutionary origins of behavior, genetic
and environmental aspects of behavioral disorders. The course is designed to challenge students and to
show them how their patients' behaviors are a major contributor to health and disease. The course also
62
deals with the physician's role in educating and bringing about behavior change in patients, peers and the
community.
DO 5172 Sports Medicine (0 credit hours, Cr/NCr)
DO 5190 Osteopathic Principles and Practice II (2.5 credit hours, Numeric Score)
Continuation of DO 5090.
DO 6010 Blood and Reticuloendothelial System (7.5 credit hours, Numeric Score)
Besides considering the embryology, histology and biochemistry of the hemopoietic and lympho-
reticular organs, during this system, the influences of microbiologic and pharmacologic agents are
discussed. Basic immunology, the mechanisms of immunologic injury and immune tolerance,
transplantation, tumor immunology and the immunodeficiency states are covered in this course. In addition,
the pathology and clinical aspects of hematologic diseases and diseases of the lympho-reticular system are
presented along with the pertinent laboratory tests. The laboratories provide hands-on experience to
examine normal and abnormal blood smears, perform blood tests and examine lymph node neoplasms.
DO 6020 Cardiovascular System (14.5 credit hours, Numeric Score)
The embryology, histology and gross anatomy of the heart and blood vessels are reviewed. The
biochemistry, pharmacology, physiology and microbiology as related to this system are discussed. The
pathology is presented as well as the clinical diagnostic and treatment modalities. Included in this system is
the Advanced Cardiac Life Support (ACLS) course in which students receive certification as ACLS
Providers.
DO 6030 Public Health (1 credit hour, Numeric Score)
The purpose of this course is to help students understand public health and its importance to the
practicing physician. Epidemiology, community health, immunization procedures, communicable disease
control, environmental and occupational health are discussed. Interaction of the physician with public health
agencies is stressed as is working with public health statistics.
DO 6040 Respiratory System (9.5 credit hours, Numeric Score)
The embryology, histology and gross anatomy of the lungs and nasotracheobronchial tree are presented.
Respiratory physiology and defense mechanisms as well as microbiology, biochemistry and pharmacology
relating to the system are discussed. Pathology of the upper and lower respiratory system is presented along
with clinical presentations of diagnostic and treatment modalities.
DO 6050 Psychiatry (2 credit hours, Numeric Score)
The psychiatric component of illness forms a major part of the practice of medicine. The ability to
recognize and deal with, or to refer, such cases poses a formidable challenge to the practitioner. Using
personal and professional skills, using ancillary personnel wisely, and cooperating with the psychiatrists
requires background knowledge and skill. This course is designed to provide that help and is taught during
the Cardiovascular System.
DO 6071 Advanced Cardiac Life Support (0 credit hours, Cr/NCr)
A series of didactic and practical educational exercises designed to meet the requirements for Advanced
Cardiac Life Support certification from the American Heart Association.
DO 6090 Osteopathic Principles and Practice III (2.5 credit hours, Numeric Score)
Continuation of DO 5190.
DO 6110 Renal System (5.5 credit hours, Numeric Score)
The embryology and histology of the kidneys and urinary system are initially presented. The
biochemistry, physiology and pharmacology of fluid and electrolyte balance with major emphasis on kidney
function are presented. The microbiology, pharmacology, and clinical management of urinary infections are
fully discussed. The identification, diagnosis and treatment of renal and urinary disorders are explored.
63
DO 6120 Endocrine System (5.5 credit hours, Numeric Score)
Endocrinology is a subject of broad range spreading over many disciplines. The system is approached in
a logical sequence by a consideration of the anatomy of the hormone secreting glands, the biochemical
description of what a hormone is, how hormones are studied and measured and the physiology in
maintaining homeostasis. Pathologies of the endocrine system are discussed and the pharmacology of
endocrine drugs is presented. Clinical manifestations of endocrine disorders of all ages are presented with
emphasis on identification, diagnosis and treatment. The system concludes with a consideration of
evaluation and management of endocrine emergencies.
DO 6130 Reproductive System (8 credit hours, Numeric Score)
The anatomy, embryology and histology of both the female and male reproductive systems are
considered. The physiology, biochemistry, pathology, pharmacology and microbiology of both reproductive
systems are also discussed in depth. In addition, the basic science disciplines discuss their principles with
respect to the relationships which exist between mother and fetus during pregnancy. Clinical lectures on
obstetrics, gynecology, perinatology, nutrition, the problem of child abuse and the management of
pregnancy are presented during this segment. Human sexuality is incorporated.
DO 6140 Gastrointestinal System (13 credit hours, Numeric Score)
The gastrointestinal system is one of the more complex and involved systems of the body. The
embryology and histology are discussed. The complicated biochemistry and physiology, the influence of
pharmacology and the problems with microbiology are presented along with the clinical and pathological
aspects of the system. The nutrition course is incorporated in this system.
DO 6150 Introduction to Clinical Medicine II (ICM-II) (Cr/NCr)
ICM-II provides students with opportunities to learn and practice clinical patient assessment skills
during the pre-clinical phase of osteopathic education. The early integration of these pre-clinical
experiences provides students the opportunity to learn the skills, values and attitudes that are most important
for the development of caring, compassionate osteopathic physicians. ICM-II is taught in conjunction with
each major system. All ICMs are concerned with the system being presented concurrently in the curriculum.
This is a required course for credit and promotion to the clinical phase.
DO 6160 Medical Jurisprudence (1 credit hour, Numeric Score)
Despite variance in state laws, the major factors of medical legal practice are rather common to all
geographic areas. Using California laws as a base, the general rules of medical practice are presented. The
obligations of the physician to the community, the patient, the hospital, colleagues and society form a small
but important part of the study. The course in Phase II discusses duties and responsibilities and the medical,
legal, and ethical aspects of medicine. Standards of care, vicarious liability and negligence are also
included. Additional symposiums are conducted during the Essentials of Family Medicine courses in Phase
III of the curriculum.
DO 6171 Differential Diagnosis (0 credit hours, Cr/NCr)
This course provides students with exposure and practice in case presentations and the application of
differential diagnosis skills to selected problems in formulating evaluation or therapeutic intervention plans.
Facilitators provide real-world thinking and experience to assist students in developing the above skills.
This course helps prepare students for clinical rotations, where they will be asked to present cases that they
are evaluating and managing. The course is integrated with each of the systems.
DO 6172 Emergency Medicine (0 credit hours, Cr/NCr)
This course is taught during the systems in Phase II, with subsequent lectures interspersed in Phase III.
The purpose is to educate osteopathic medical students in the basics of emergency medicine, utilizing a
structural and functional approach wherever possible. Basic areas covered in detail are physical and
emotional trauma, poisonings, the paramedic system and emergency cases from all areas of clinical
medicine as they relate to a given body system.
64
DO 6173 Geriatrics (0 credit hours, Cr/NCr)
This challenging and difficult area of clinical practice requires additional skills and knowledge not
readily derived from standard textbooks of medicine. The student is instructed on special problems of the
elderly with emphasis on improving his/her clinical skills to deal with the unique diagnostic, therapeutic and
psychosocial problems of the elderly. This sequence is integrated into the Systems.
DO 6174 Human Sexuality (0 credit hours, Cr/NCr)
The purpose of this course is to promote student understanding of human sexuality by presenting a
variety of issues ranging from normal to dysfunctional sexuality. It is a one-week course taught as a portion
of the Reproductive System (DO 6130). The course covers a range of human sexuality issues including the
anatomy and physiology of reproduction, pathology, normal sexual response and psychosexual development
throughout the life cycle. The theory and practice of treatment for sexual dysfunction are considered.
Current therapeutic concepts and techniques are discussed along with required case reviews, which include
diagnosis, treatment plan and prognosis.
DO 6175 Nutrition (0 credit hours, Cr/NCr)
The body is capable of handling most problems within a reasonably balanced nutritional state.
Furthermore, healing and recovery from surgery or illness is facilitated by a good nutritional state. The
course provides the basic information on which to evaluate the nutritional requirements of the body in
health and disease. A review of the vitamins and their indications as well as limitations, the use and need for
the trace minerals and the proportion of carbohydrates, fats and proteins of the balanced diet are discussed.
Clinical nutrition is also emphasized in this course, which is taught during the Gastrointestinal System (DO
6140).
DO 6176 Pediatrics (0 credit hours, Cr/NCr)
Recognizing that the child is not just a small adult, this lecture series is devoted to the special problems
of childhood. These subjects are integrated during Phase II in each system as appropriate. All systems
contain an element of pediatrics and this course is designed to cover those aspects that are peculiar to
pediatrics (infancy to adolescence). Additional pediatric presentations are given in Phase III during the
Essentials of Family Medicine courses.
DO 6190 Osteopathic Principles and Practice IV (5 credit hours, Numeric Score)
Continuation of DO 6090.
DO 7010 Family Practice I (10 credit hours, Letter Grade)
Supervised clinical education in family medicine including clinical management, technical and
procedural skills, interpretation of diagnostic data, patient education, development of diagnostic and
management plans, and interprofessional communication. In subsequent courses in this series, greater
involvement and independence in patient management are expected.
DO 7020 Internal Medicine I (10 credit hours, Letter Grade)
Supervised clinical education in general internal medicine including clinical management, technical and
procedural skills, interpretation of diagnostic data, patient education, development of diagnostic and
management plans, and interprofessional communication. In subsequent courses in this series, greater
involvement and independence in patient management are expected.
DO 7021 Internal Medicine II (10 credit hours, Letter Grade)
Prerequisite DO 7020. Continuation of DO 7020.
DO 7022 Internal Medicine III (10 credit hours, Letter Grade)
Prerequisite DO 7020. Supervised clinical education in general internal medicine or one of the internal
medicine subspecialties of gastroenterology, pulmonology or cardiology. Expected competencies include
clinical management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and interprofessional communication. In subsequent
courses in this series, greater involvement and independence in patient management are expected.
65
DO 7030 Surgery I (General) (10 credit hours, Letter Grade)
Supervised clinical education in general surgery including clinical management, technical and
procedural skills, interpretation of diagnostic data, patient education, development of diagnostic and
management plans, and interprofessional communication. In subsequent courses in this series, greater
involvement and independence in patient management are expected.
DO 7060 Osteopathic Manipulative Medicine (10 credit hours, Letter Grade)
Supervised clinical education in osteopathic manipulative medicine including clinical management,
technical and procedural skills, interpretation of diagnostic data, patient education, development of
diagnostic and management plans and interprofessional communication.
DO 7070 Pediatrics I (10 credit hours, Letter Grade)
Supervised clinical education in pediatrics including clinical management, technical and procedural
skills, interpretation of diagnostic data, patient education, development of diagnostic and management plans
and interprofessional communication.
DO 7071 Pediatrics II (10 credit hours, Letter Grade)
Prerequisite: DO 7070. Continuation of DO 7070.
DO 7080 Psychiatry (10 credit hours, Letter Grade)
Prerequisite: DO 7010 or DO 7020. Supervised clinical education in psychiatry including clinical
management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans and interprofessional communication.
DO 7090 Obstetrics/Gynecology (10 credit hours, Letter Grade)
Prerequisite: DO 7010 or DO 7020. Supervised clinical education in obstetrics/gynecology including
clinical management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans and interprofessional communication.
DO 7100 Geriatrics (10 credit hours, Letter Grade)
Supervised clinical education in geriatrics including clinical management, technical and procedural
skills, interpretation of diagnostic data, patient education, development of diagnostic and management plans
and interprofessional communication.
DO 7510 Family Practice II (10 credit hours, Letter Grade)
Prerequisite: DO 7010. Continuation of DO 7010.
DO 7520 Internal Medicine IV (10 credit hours, Letter Grade)
Prerequisite DO 7021 and 7022. Supervised clinical education in general internal medicine or one of the
internal medicine subspecialties of gastroenterology, pulmonology, neurology, or cardiology. Expected
competencies include clinical management, technical and procedural skills, interpretation of diagnostic data,
patient education, development of diagnostic and management plans, and interprofessional communication.
In subsequent courses in this series, greater involvement and independence in patient management are
expected.
DO 7521 Internal Medicine V (10 credit hours, Letter Grade)
Prerequisite DO 7520. Supervised clinical education in general internal medicine or one of the internal
medicine subspecialties of gastroenterology, pulmonology, neurology, or cardiology. Expected
competencies include clinical management, technical and procedural skills, interpretation of diagnostic data,
patient education, development of diagnostic and management plans and interprofessional communication.
DO 7530 Surgery II (10 credit hours, Letter Grade)
Prerequisite DO 7030. Supervised clinical education in general surgery or one of the surgical
subspecialties of ophthalmology, orthopedics, urology or cardiovascular/thoracic. Expected competencies
include clinical management, technical and procedural skills, interpretation of diagnostic data, patient
66
education, development of diagnostic and management plans, and interprofessional communication. In
subsequent courses in this series, greater involvement and independence in patient management are
expected.
DO 7540 Emergency Medicine (10 credit hours, Letter Grade)
Prerequisite: DO 7010 or DO 7020. Supervised clinical education in emergency medicine including
clinical management, technical and procedural skills, interpretation of diagnostic data, patient education,
development of diagnostic and management plans, and interprofessional communication
DO 7550 Elective (10 credit hours; repeatable to a maximum of 50 credit hours, Letter Grade)
Supervised clinical education in one of the clinical disciplines including clinical management, technical
and procedural skills, interpretation of diagnostic data, patient education, development of diagnostic and
management plans, and interprofessional communication. The discipline and clinical training site must be
approved in advance by the Office of Rotations.
DO 8050 Essentials of Family Medicine I (EFM-I) (3.5 credit hours, Letter Grade)
The primary purpose of the Essentials of Family Medicine sequence is to serve as an assessment tool
and review of basic clinical knowledge, as well as special topics critical to the student's becoming a
complete osteopathic physician and lifelong clinical learner. The program is designed to review, augment,
and amplify clinical material presented to the students during the first two years of medical school, as well
as provide advanced information and techniques that will be valuable during rotations, residency and
eventual medical practice. Classes are presented in a multidisciplinary format that includes lectures,
workshops, demonstrations, multi-media presentations and other modalities. It is geared toward providing
practical and up-to-date information regarding recent innovations in medicine.
EFM-I is designed to help students gain the essential knowledge and skills that form the foundation for
their clinical rotations and medical careers. Course content focuses on helping students begin to apply
theoretical information in real world contexts. Topics include clinical, medico-legal and ethical issues.
Sessions are scheduled over 3 weekends. Attendance is mandatory at all sessions.
DO 8550 Essentials of Family Medicine II (EFM-II) (3.5 credit hours, Letter Grade)
Continuation of EFM I (DO 8050). EFM-II is designed to promote mastery of the essential knowledge
and skills learned during EFM-I, while also promoting lifelong learning and preparation for board exams. It
is designed to assist students in moving from their general knowledge base to more specific applications of
medical material. Overall, the course is designed to help students pull together their vast base of medical
knowledge and apply this information effectively in the practice of medicine. To accomplish this, the course
more closely resembles a continuing-education format, with physicians from specialty fields as presenters.
The sessions are scheduled over 3 weekends. Attendance is mandatory at all sessions.
Elective Courses
DO 6181 An Osteopathic Approach to Challenged Children (Cr/NCr)
This course provides interested second year-students with an introduction to the causes, prevention, and
treatment of brain injury and its resulting neurological impairments commonly classified as mental
retardation, cerebral palsy, and learning and behavior problems. The course emphasizes osteopathic
palpatory diagnosis and treatment but recognizes the essential contribution of other supportive modalities.
IS 5010 Literature and Medicine (Cr/NCr)
An elective course is offered to second-year students during the spring semester. The course is designed
to expose medical students to selected themes and approaches to the humanities, focusing on literature that
relates to medical concerns of the healthcare professionals and the general public.
67
IS 5030 Art Experience (Cr/NCr)
Goals of the course focus on the student being able to have a meaningful art experience that addresses
the connection between art and life. Students will also acquire a general understanding of the basic
constructs of art including art appreciation and learn how to think creatively through their work.
HONORS AND AWARDS
The following awards for DO students are presented annually on Honors Day in April:
Provost's Student Government Award
Dean's Award
William G. Woodman, MD Humanitarian Memorial Award
Russell B. McCaughan Award
Neocortex Award
William G. Stahl, DO, FACOS Memorial Scholarship
Anthony Joseph Ronzo, Sr. Memorial Award
Auxiliary to the Osteopathic Physicians and Surgeons of California Scholarship Award
COMP Western University Service Award
Community Clinic Service Award
Class of 1989 Award
McGraw-Hill Award
Joseph and Dorothy Gendron Journalism Award
Dr. V. Gladys Shutt Memorial Award
Richard E. Eby Leadership Scholarship
Mickey and Nell Clamage Memorial Scholarship Award
Roy G. and Marion L. Kramer Endowment Fund Award
Muriel Chapman, DO, Memorial Award
Robert W. Finegan Memorial Award
Jeff Plumb Memorial Award
The President's Society Award
Dr. Alex M. Rene‚ Memorial Scholarship Award
Linda Fox Memorial Endowment Fund Award
Louise Kramer Memorial Scholarship Award
Guy M. Allmon Scholarship Fund Award
Glen Scheresky Memorial Scholarship Award
American Association of Colleges of Osteopathic Medicine
Council of Student Council Presidents, Student DO of the Year Award
Dr. Sheila Xenos Memorial Award
Osteopathic Physicians and Surgeons of California Matthew L. Weyuker Scholarship Award
The following awards are presented annually to graduates at the Commencement Dinner Dance:
President's Award
Dean's Award
Gate Pharmaceutical Student Award
Edward B. Parris and Jacqueline A. Parris Award
Dr. Frank T. Carr Memorial Award
Steven W. Dyer Memorial Award
Janet M. Glasgow Memorial Achievement Citation of the American Medical Women's Association
American College of Osteopathic Family Physicians Award
Pauline Weiss Pumerantz Memorial Award
Richard H. and Anna Kaiser Memorial Award
New Mexico Osteopathic Medical Association Foundation for Osteopathic Education and
Professional Development Award for Academic Excellence
Osteopathic Physicians and Surgeons of California Award
Shirley Jane Watters Memorial Award
Rev. & Mrs. Al and Verna Braswell Award
Leonard E. Peck, Sr. Memorial Award
Phoenix Award
68
Charles Vowels, MD, Memorial Award
Alumni Memorial Award
Society of Academic Emergency Medicine Excellence in Emergency Medicine Award.
James R. Sawrey Memorial Award
Dr. Alex M. Rene‚ Memorial Award
National American Osteopathic Foundation: The Donna Jones Moritsugu Memorial Award
ACADEMIC CALENDAR 2001-2002
DO PROGRAM
Tuesday, Wednesday, Jun. 5-6, 2001
NBOME COMLEX Level 1
Wednesday, Jun. 6, 2001
Fall Semester Tuition Due (ISAC students)
Tuesday, Wednesday, Jun. 12-13, 2001
NBOME COMLEX Level 3
Wednesday, Jun. 20, 2001
Registration (3rd & 4th years)
Fall Semester Tuition Due (3
rd
& 4
th
years)
Monday, Jun. 25, 2001
Clinical Rotations Begin
Wednesday, Jul. 4, 2001
Independence Day
Friday - Sunday, Jul. 20-22, 2001
II-4 EFM Weekend
Thursday, Aug. 9, 2001
Registration (1st and 2nd year)
Fall Semester Tuition Due (1
st
& 2
nd
years)
Saturday, Aug. 11, 2001
Convocation/White Coat Ceremony
Monday, Aug. 13, 2001
Classes Begin (1st and 2nd years)
Saturday, Aug. 25, 2001
OMAC
Tuesday, Wednesday, Aug. 28-29, 2001
COMLEX Level 2
Monday, Sept. 3, 2001
Labor Day - no classes
Friday - Sunday, Sept. 14-16, 2001
I-1 EFM Weekend
Monday, Oct. 8, 2001
Columbus Day - no classes
Tuesday, Wednesday, Oct. 16-17, 2001
COMLEX Level 1
Wednesday, Nov. 7, 2001
Spring Semester Tuition Due (4
th
years)
Friday - Sunday, Nov. 9-11, 2001
II-5 EFM Weekend
Saturday, Nov. 10, 2001
OMAC
Wednesday, Nov. 21, 2001
Thanksgiving Recess - Noon
Monday, Nov. 26, 2001
Classes Resume
Thursday, Dec. 6, 2001
Spring Semester Tuition Due (3
rd
years)
Tuesday, Wednesday, Dec. 4-5, 2001
COMLEX Level 3
Friday - Sunday, Dec. 7-9, 2001
I-2 EFM Weekend
Friday, Dec. 21, 2001
Last Day of Classes
Monday, Dec. 24, 2001
Winter Recess Begins
Wednesday, Jan. 2, 2002
Spring Semester Tuition Due (1
st
& 2
nd
years)
Monday, Jan. 7, 2002
Classes Resume
Tuesday, Wednesday, Jan. 15-16, 2002
COMLEX Level 2
Monday, Jan. 21, 2002
69
Martin Luther King Holiday - no classes
Friday - Sunday, Feb. 1-3, 2002
II-6 EFM Weekend
Monday, Feb. 18, 2002
President's Day - no classes
Friday - Sunday, Mar. 1-3, 2002
I-3 EFM Weekend
Monday, Mar. 18, 2002
Spring Vacation Begins
Monday, Mar. 25, 2002
Classes Resume
Monday, April 8, 2002
Honors Day
Wednesday, May 15, 2002
Last Day of Classes (2nd year)
Tuesday, May 21, 2002
Last Day of Classes (1st year)
May 31,2001
Commencement
Tuesday, Wednesday, Jun. 4-5, 2002
COMLEX Level 1
Tuesday, Wednesday, Jun. 11-12, 2002
COMLEX Level 3
The Osteopathic Oath
I do hereby affirm my loyalty to the profession I am about to enter.
I will be mindful always of my great responsibility to preserve the health and life of my patients, to
retain their confidence and respect both as a physician and a friend who will guard their secrets with
scrupulous honor and fidelity, to perform fruitfully my professional duties, to employ only those recognized
methods of treatment consistent with good judgment and with my skill and ability, keeping in mind always
nature's laws and the body's inherent capacity for recovery.
I will be ever vigilant in aiding the general welfare of the community, sustaining its laws and institutions,
not engaging in those practices which will in any way bring shame or discredit upon myself or my
profession. I will give no drugs for deadly purposes to any person, though it be asked of me.
I will endeavor to work in accord with my colleagues in a spirit of progressive cooperation and never by
word or by act cast imputations upon them or their rightful practices.
I will look with respect and esteem upon all those who have taught me my art. To my College I will be
loyal and strive always for its best interests and for the interests of the students who will come after me. I
will be ever alert to further the application of basic biologic truths to the healing arts and to develop the
principles of osteopathic medicine as taught by my profession.
In the presence of this gathering I bind myself to my oath.
70
COLLEGE OF PHARMACY
Doctor of Pharmacy Program
ACCREDITATION
The College of Pharmacy is accredited by the American Council on Pharmaceutical Education.
PHARMACY: ABOUT THE PROFESSION
The practice of pharmacy has evolved from a historical emphasis on the preparation and distribution of
drug products to new activities and responsibilities that focus on the rational, safe and cost-effective use of
drugs. Just as it is generally assumed that physicians are primarily involved in providing medical care and
nurses in providing nursing care, pharmacists are the primary providers of pharmaceutical care. The mission
of the pharmacy profession, therefore, is to meet the pharmaceutical care needs of the public.
Pharmaceutical care is patient-centered, outcome-oriented, contemporary pharmacy practice that requires
the pharmacist to work in concert with the patient and the patient's other health care providers to promote
health, prevent disease, and assess, monitor, initiate and modify medication use so that pharmacotherapy is
safe and effective.
The provision of pharmaceutical care to patients requires an understanding of the chemistry of drug
entities, the delivery characteristics of dosage formulations, the disposition of drugs within the body, the
physiologic and pharmacologic outcome of drugs' interactions with the human body and the social systems
in which medications are used.
As a pharmacist you will be able to care for your patients in many important ways:
• Participate in the planning and implementation of effective drug therapy.
• Monitor and evaluate drug therapy to identify and solve patient-specific drug therapy problems.
• Evaluate clinical literature.
• Prepare medications.
• Select the drug product dosage form.
• Calculate the dose and determine the dosing schedule.
• Educate and counsel patients, and;
• Work with other health care providers and the patient to promote health and prevent disease.
THE DEGREE
The Doctor of Pharmacy degree (PharmD) is awarded in recognition of the highest level of professional
education in pharmacy in the United States. To earn the PharmD degree, students complete four years of
professional study following a minimum of two years of preprofessional education at an accredited college
or university.
Students who complete this program are eligible to take state pharmacy licensing examinations. After
passing this examination, graduates are licensed to perform all the duties and responsibilities of a practicing
pharmacist.
CAREER OPPORTUNITIES
Our graduates find a vast array of exciting career pathways open to them. The opportunities below
represent only a small list of possible career options.
Community Practice
Pharmacy offers a variety of professional opportunities in the community setting. Independent
pharmacies, corporately owned pharmacies and neighborhood health care clinics all provide opportunities
for direct patient care. Other examples of community practice include specialized home health care,
consulting for nursing home patients and conducting patient education programs.
71
Institutional Practice
Pharmacists in hospitals and other health care institutions may be involved in direct patient care,
teaching, drug use evaluation, clinical research studies, public service and administration.
Managed Care Pharmacy
Pharmacists practice in a variety of managed care organizations including health maintenance
organizations and preferred provider organizations. In these settings, pharmacists develop formularies,
implement drug utilization reviews and analyze physician prescribing patterns.
Pharmaceutical Companies
Research and development, testing of drugs in humans, production, quality control, marketing, public
relations, sales, and management are some of the career opportunities available in industry.
Public Service Practice
Pharmacists practice in federal government agencies and services including the Food and Drug
Administration (FDA); Drug Enforcement Administration (DEA); the Army, Navy and Air Force; Public
Health Service; and Department of Veterans Affairs.
Academia
Opportunities for careers in colleges or schools of pharmacy include administration, teaching, research
and clinical service. Additional opportunities in teaching, research, or practice may required post-graduate
education or training beyond the doctor of pharmacy degree.
THE COLLEGE OF PHARMACY
A major goal of the College of Pharmacy is to prepare competent and caring practitioners. We are
prepared to offer you a quality educational experience.
Modern Facilities
You will receive instruction in a modern facility with classrooms and breakout rooms furnished with
state-of-the-art equipment.
A Friendly Environment
You will be treated as a colleague and a professional who is seeking to become a competent pharmacy
practitioner.
Supportive Faculty
You will receive instruction from faculty members who are committed to excellence in pharmaceutical
education. Many faculty members are practicing clinical pharmacists who are actively providing primary
care or consultative services to patients in a variety of practice settings.
A Rich Student Life
You will have an opportunity to participate in a number of professional pharmacy organizations as well
as other school-wide activities.
ACADEMIC COURSE WORK
To obtain the PharmD degree you will complete a curriculum that contains both didactic and clinical
components.
The Didactic Component
In the core didactic component of the program, you will learn about biological systems and about drugs
and their effect on the body. You will take courses in areas such as therapeutics, health care administration,
pharmacology and pharmacokinetics and learn how to apply this knowledge to pharmacy practice. Your
studies will include communication skills, patient counseling, laws about drugs and pharmacy practice,
health care systems, physical assessment and evaluation of the drug literature.
72
The Clinical Training Component
In several different patient-centered training sessions, particularly during the third and fourth years, you
will be given an opportunity to put into practice what you have learned in the classroom. Under the
supervision of a clinical pharmacist faculty member, you will assess and counsel patients and monitor their
drug therapies. You will spend a total of 42 weeks in these training sessions, called advanced pharmacy
practice experiences. Such pharmacy practice experiences will take place in hospitals as well as in clinics,
community pharmacies and other settings where pharmacists practice.
ADMISSIONS POLICIES AND PROCEDURES
Admission to the College of Pharmacy is on a highly competitive basis. Each year we receive many
more applications than we can accommodate in our program. At Western University, we retain smaller class
sizes, offering you a closer relationship with your faculty and fellow students. The College of Pharmacy is
looking for individuals who have excellent communication skills, who care for people and are
compassionate, who are dedicated and determined, who are dependable and who display good judgment.
Application Requirements
The College of Pharmacy Admissions Committee will consider applicants with a minimum of two years
of college (60 academic semester hours or 90 quarter hours) of pre-pharmacy study at an accredited college
or university. The minimum cumulative prepharmacy and science grade point average requirement is 2.5.
Grades of "C-" in any of the prerequisite courses are not accepted. Prerequisite courses are subject to
review each year. For the latest information, you should consult our web site at www.westernu.edu.
1. Prerequisite Courses
College English (1 semester)
English Composition (1 semester)
Speech Communication (1 semester)
General Chemistry with lab (2 semesters)
Organic Chemistry with lab (2 semesters)
Human Anatomy with lab* (1 semester)
Human Physiology with lab* (1 semester)
Microbiology with lab-Medical Microbiology is preferred (1 semester)
Calculus (1 semester)
Electives (2 semesters)-Electives must be met from two of the three following areas: public
speaking/debate, social sciences, or economics.
*If anatomy and physiology are combined, we will accept a minimum of 5 semester units. Anatomy and
physiology must be taken out of the anatomy, physiology, A&P, biology or zoology departments.
We do not accept substitutions or waive any of the prerequisite courses. English as a Second Language
(ESL) courses are not accepted for the English requirement. All prerequisite course work in progress must
be completed no later than the spring semester or quarter immediately preceding matriculation.
2. Test of English as a Foreign Language (TOEFL)
TOEFL (including essay) is required for all applicants submitting course work from foreign schools, and
all permanent and temporary residents of the United States. EXCEPTION: The TOEFL exam will be
waived for students graduating with a confirmed baccalaureate or higher degree from a United States
institution at the time of application. A minimum score of 550 on the paper based test or 213 on the
computer-based test is required. TOEFL scores must be submitted at the time of application. TOEFL
scores are valid for 2 years.
3. Recommendations
Three satisfactory recommendations (forms are provided by the College) are required as part of the
admissions application. The recommendations should state the nature and extent to which the
recommender knows you and should elaborate on the applicant's attributes and abilities including
communication skills, ethics, interpersonal skills, motivation toward the profession and maturity.
73
Application Procedures and Deadlines
Candidates may obtain an application as early as August of the academic year preceding the year in
which they plan to matriculate. Applicants are considered without regard to race, color, national origin, age
or gender. Western University strives to accommodate individuals with disabilities. The application
postmark deadline for the class entering in the fall is December 1 of the preceding year.
To request an information brochure and/or an application, contact the Admissions Office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 623-6116
In addition to submitting a completed application, the applicant must submit a non-refundable
application fee of $60, three letters of recommendation, an academic/professional record form, must
complete a personal questionnaire (form provided by the University) and submit official transcripts from all
colleges attended. All application materials are to be included in the application packet. After receipt of the
packet, the Admissions Office will evaluate the applicant's transcripts to ascertain that all prerequisite
courses have been completed and that the applicant's cumulative GPA is satisfactory. Applicants who wish
to use course work completed outside of the United States must submit their transcripts for evaluation to
World Education Services or Josef Silny and Associates. A course-by-course evaluation is required and all
course work must be designated as undergraduate, graduate, or professional. Western University will only
honor evaluations from one of the above services. The evaluation must be included with the application
packet.
Faculty in the College of Pharmacy will screen each applicant's admissions file to determine whether or
not an applicant will be granted an on-campus interview. Candidates selected for an interview will
participate in an assessment of written and verbal communication skills. Interviews are typically held in
January and February. Decisions of the Admissions Committee regarding the admission of applicants to the
Doctor of Pharmacy program are final.
TUITION AND FEES
In estimating costs for one academic year of study at Western University's College of Pharmacy, you
should include tuition and fees, laptop computer and printer, books and supplies, room and board, and other
miscellaneous expenses. Actions of the Board of Trustees setting tuition and fees for the academic year are
established during the previous spring term. The most current tuition and fees are as follows:
• Tuition - $25,635 in 2001-2002 Academic Year.
• Mandatory fees specific to the College of Pharmacy will be provided separately.
• Application Fee - Non-refundable $60 fee for those applying to the Western University College of
Pharmacy.
• Enrollment Deposit- $500 for students admitted to the College of Pharmacy. Upon enrollment, this
deposit is applied toward the tuition for the academic year. Persons who fail to
enroll forfeit the entire deposit.
Other Fees
$30 (per day) Late Registration Fee
$40 Lost Mail Locker Key
$5 (each) Copy of Official Transcript
$10 (each) Copy of Official Transcript Faxed
$10 Lost ID Badge
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
74
The College of Pharmacy requires that each enrolled student have a notebook or laptop computer during
class, after class hours and while on rotations.
FINANCIAL ASSISTANCE
All PharmD students are eligible to apply for need-based financial aid. For information, please write to
the Financial Aid Office, Western University of Health Sciences, 309 E. Second Street, Pomona, California
91766-1854
ACADEMIC POLICIES AND PROCEDURES
Grading Policy
Students are required to meet a specified set of outcome objectives in each block in the curriculum. The
block facilitator will provide the student with a syllabus at the beginning of the block that includes the
required outcome objectives, instructional methods, assessment methods, a day-by-day schedule, and
grading criteria. Achievement of the outcome objectives will be assessed through individual quizzes,
examinations, and individual performance on any assignments given in that block. The minimum passing
score (P) in any block is 80%. Students who earn a grade of 90% or higher will receive a grade of “high
pass” (HP). A student who fails to meet the minimum requirement of 80% will receive a grade of “no pass”
(NP) and will be automatically placed on academic probation (see Probation below). Policies requiring
remediation of failed blocks are set forth under Failure to Meet Standards, below. All recorded grades
will remain on the official transcript except in cases where clerical errors have occurred. The grading
policies for the professional practice component of the curriculum (the Introductory Professional Practice
Experience [IPPE], the Advanced Pharmacy Practice Experiences [APPE] and the Advanced Electives
[AEs]) are set forth in separate policies.
Grading procedures
Block grades: end of block grades will be assigned as follows:
HP = High Pass; a student has achieved a minimum of 90%.
P = Pass; a student has achieved a minimum of 80%.
NP = No Pass; indicates the student has not achieved the minimum of 80% in
the block (See Failure to Meet Standards section).
NP/P = Indicates a student has successfully remediated a block. The “NP” will
remain on the student’s transcript.
I = Incomplete (Refer to the policy on Attendance and Absences).
I/P = Indicates a student has successfully completed a block following receipt
of an incomplete grade. The “I” will remain on the student’s transcript.
I/NP = Indicates a student has unsuccessfully completed a block following
receipt of an incomplete grade.
M = Missing
W = Withdrawal (Refer to the General Academic Policies and Procedures
above).
Advanced Pharmacy Practice Experiences (APPE)/Advanced Electives (AE) grades will be assigned as
follows:
P = Pass.
NP = No Pass; student has not achieved the rotation outcomes.
NP/P = Indicates a student has successfully remediated APPE/AE. The NP will
remain on the student’s transcript.
I = Incomplete (Refer to the policy on Attendance and Absences and on
Student Progress).
I/P = Indicates a student has successfully completed an APPE/AE following
receipt of an incomplete grade. The “I” will remain on the student’s
transcript.
I/NP = Indicates a student has unsuccessfully completed an APPE/AE
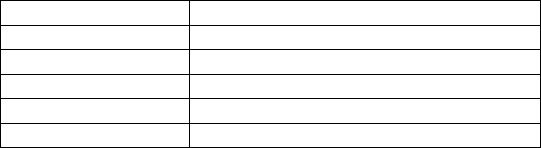
75
following receipt of an incomplete grade.
M = Missing
W = Withdrawal (Refer to the General Academic Policies and Procedures
above).
Credit hours
To be eligible for graduation, a student must complete the following required components of the Doctor
of Pharmacy program:
Year # of Credits per year
1 40
2 40
3 44
4 50
Total 174
Learning Assurance
Competency-based education provides students opportunities to achieve block outcomes, thus, learning
assurance will be provided in each block. Block faculty will work with students to help them achieve the
required standards as stated in the block syllabus. Assessment methods are intended to ensure that
outcomes are met, and if not, they are to be used as a means of assessing the area(s) of difficulty. Various
methods will be employed to help students via the block syllabus. If additional points are assessed for any
assignment or examination for which learning assurance has been provided, the actual numerical score will
be recorded as no greater than 80%.
Failure to Meet Standards
Students who fail to achieve the 80% standard in a block will be given a grade of “NP” and will be
placed on academic probation automatically by the Dean (See General Academic Policies and
Procedures on Probation). Students who receive a designation of “NP” in up to two blocks during one
academic year will be required to enroll for remediation for each block for which a grade of “NP” has been
recorded. Block remediation may include a variety of activities such as faculty-student conferences,
independent study and other types of coursework. However, in all cases, a final comprehensive remediation
examination will be required to demonstrate successful attainment of the required standards. It is the
student’s responsibility to prepare for the comprehensive remediation examination and other assigned
coursework that may be required. Students will be required to pay a fee of $250 for each block remediated.
The Academic Performance and Standards Committee will coordinate the block remediation schedule.
If remediation is successful, the student’s transcript will reflect a grade change of NP to NP/P. The
original grade of NP will remain on the official transcript. If a student fails any block remediation, he/she
may be dismissed from the program. The Academic Performance and Standards Committee will review
each case of failure of block remediation and make a recommendation to the Dean.
Remediation for Blocks in the First and Second Professional Years
The Office of the Association Dean for Academic Affairs will post the schedule for the comprehensive
remediation examinations the week following the end of the last block of the academic year.
Comprehensive remediation examinations will take place during the four weeks following the last block of
the academic year. Students must be available for any scheduled comprehensive remediation examination
they are required to take.
One comprehensive remediation examination will be administered that covers all block objectives (those
areas the student failed plus all other required competencies). Each block requiring remediation will have a
separate examination. Students must pass the comprehensive remediation examination to be promoted to the
next academic year. Students will be required to pay a fee of $250 for each comprehensive remediation
examination.
76
Remediation for Blocks in the Third Professional Year
The Office of the Associate Dean for Academic Affairs will post the schedule for the comprehensive
remediation examinations the week following the end of the last block of the third year. The comprehensive
remediation examinations for P3 students (Blocks 3.1-3.5) will be scheduled in January. Students will not
be scheduled to start Advanced Pharmacy Practice Experiences (APPEs) until all blocks are successfully
remediated. The Academic Performance and Standards Committee must approve any exceptions. One
comprehensive remediation examination will be administered that covers all block objectives within each
block the student failed (those areas the student failed plus all other required outcomes). Each block
requiring remediation will have a separate exam. The consequences of not passing remediation are outlined
below under Student Progress.
Attendance and Absences
Students are to be in class Monday-Friday from 8 am to 3 p.m., unless the block schedule notes
otherwise.
When a student must be absent, he/she must contact the Block Facilitator as soon as possible. If unable
to reach the Facilitator, the student must leave a message with a contact telephone number. Accommodation
for excused absences will be made, whenever possible, to assist students in situations involving illness or
other emergencies. The Block Facilitator may require documentation of the reason(s) for the absence. The
Block Facilitator/Faculty will determine how the missed materials will be completed.
If the absence is over three class days in duration, the case will be referred to the Academic Performance
and Standards Committee, to determine, in consultation with Block Faculty, if ongoing accommodation can
be made given the anticipated length of absence. The Committee may, at its discretion, recommend that the
student be assigned an Incomplete Grade (I) for the block. Refer to Student Progress (below) for
procedures to remove an Incomplete Grade. If the Committee determines that it is not possible for the
student to continue in the program, a leave of absence may be recommended. Leaves of absence are
governed by University policy. The Academic Performance and Standards Committee will make these
determinations on a case-by-case basis after review of the facts and forward a recommendation to the Dean.
This policy also applies to students on APPE/AE. These students are also governed by policies
contained in the Syllabus of Advanced Pharmacy Practice Experiences and by rotation-specific
requirements.
Independent Study: Because of the unique and intensive nature of the College of Pharmacy’s
curriculum, the collaborative teaching and learning processes among team members, and the sequencing of
key blocks, the Faculty does not believe that independent learning of core coursework meets the goals of the
Doctor of Pharmacy program. In special cases, e.g. involving illness, reasonable accommodation will be
made to permit the student to continue in his/her course of study if possible. Additionally, the collaborative
learning process among team members is a critical element of the curriculum. Students accepted into the
program must understand that their grades require successful collaboration with team members.
Independent study of blocks in the core curriculum in the College of Pharmacy is not permitted either in
summer or during the academic year. The only independent study that is permitted is via learning assurance
and remediation.
Holidays: Western University publishes an annual list of holidays recognized by the University. A
student who requests time off for a holiday other than those observed by Western University must do so in
writing to the Block Facilitator a minimum of 5 school days before the start of the block in which the
holiday falls. If the request is approved, the student is responsible for any work missed on the date(s)
absent. All assignments must be completed by the scheduled time. However, if the student fails to notify the
Block Facilitator in the timeframe noted, the absence will be considered an unexcused absence, and no
remediation will be permitted. The Western University holiday schedule does not apply to students on
Advanced Pharmacy Practice Experiences and on off-campus Advanced Electives. Students will follow the
rotation site holiday schedule on Advanced Pharmacy Practice Experiences and on Advanced Electives.
Professional Meetings and Other Related Absences: All students are required to attend one
professional meeting each year as indicated on the College’s academic calendar.
77
Policy for Academic Dishonesty
The faculty takes the position that honesty and integrity are among the most valued traits of a
professional person. As future professionals, each student must assume personal responsibility for honesty
and integrity.
The College of Pharmacy faculty will not tolerate academic dishonesty. Verification of an offense is
grounds for dismissal. Academic dishonesty includes, but is not limited to activities such as changing
examination answers after the graded examination has been returned, cheating, plagiarism, bringing in
unauthorized resources to exams or other assessed exercises, and signing another student’s name on
attendance records or team examinations/assignments.
All incidents that compromise academic integrity must be documented and referred to the Dean for
review. This Dean will investigate all allegations, and either resolve the issue or forward the issue to the
University Student Conduct Committee. The student may appeal the action following policies listed in the
General Academic Policies and Procedures section of this Catalog.
Student Examination and Assignment Policies and Grade Appeals
Excused Absence from an Exam: Excused absences are for emergencies. In the case of an emergency
the student must notify the Block Facilitator at the earliest time possible (see Attendance and Absences
Section above). Students who are excused from an examination/assignment will be permitted to
take/complete the examination/assignment at a time designated by the block faculty. [NOTE:
Examination/Assignment refers to any graded assessment in the block.] The student will be eligible to earn
full credit for the examination/assignment under these circumstances. However, a student who does not
take/complete the individual examination/assignment and who is not excused by the Block Facilitator will
received a zero for the examination/assignment. If emergencies arise that require a student to miss more
than one examination or assignment in a block, the student’s performance will automatically be referred to
the Academic Performance and Standards Committee for review.
Requests for an Examination or Assignment Regrade: This section applies to all graded assessments.
Any request by a student to have an examination or assignment regraded must be made in writing and
submitted to the Block Facilitator within two working days of return of the examination or assignment.
The student must specify which question(s) and answer(s) are to be reconsidered in the request. The
request should be accompanied by lecture notes or referenced sources that support the student’s original
answer. On receipt of the request, the Block Facilitator will consider the request and document the decision
regarding the request in writing to the student. The Block Facilitator will maintain a copy of the request and
action taken. If the request for a regrade concerns a faculty member other than the Block Facilitator, the
faculty member has the option of regrading the examination/assignment in its entirety. The Block
Facilitator will respond to the student within two working days of receiving the written request.
If the student disagrees with the decision and has adhered to the timelines specified for regarding, he/she
may petition the Academic Performance and Standards Committee for an appeal of the regrade decision.
Grade Appeals: A Grade Appeals Sub-Committee, if required, shall be constituted by the Academic
Performance and Standards Committee. It shall consist of at least one member of the Academic
Performance and Standards Committee, who shall serve as Chair, two voting faculty members not on the
Committee, and one student representative. All members of the Grade Appeals Sub-Committee have full
voting privileges. The Committee will conduct its own investigation in conjunction with such an appeal
following established procedural guidelines for handling student appeals of an academic nature. An
alternate appointed by the Dean will replace members of the Committee who may have a conflict of interest
in a particular case, e.g., a faculty member on the Committee may be the person who administered the grade
that is being appealed.
Appeal Process
Students may appeal decisions regarding suspension, student conduct, academic progression/promotion
and graduation according to the regulations listed in the General Academic Policies and Procedures
section in the front section of this Catalogue.
78
Student Progress
Academic Progression Blocks 1.1 through 3.5: To progress to the next academic year, a student must
pass all blocks in the current academic year. The Academic Performance and Standards Committee will
review each student’s progress at the end of every block.
Failure to Meet Standards – First Block Actions: When a student does not achieve the required
standard in a block, the Dean will automatically place him/her on academic probation. The Dean will notify
the student in writing within two weeks of receiving his/her final block grade. Letters will be distributed
either by the Dean or via certified and regular mail delivery. Student confidentiality will be maintained.
The terms of probation will be specified at the time a student is placed on probation. If a student is placed
on probation, he/she must meet with his/her faculty advisor monthly and may not hold office in any
University or College organization. The student will develop a corrective plan and submit it to his/her
faculty advisor within five working days. This plan should include problems the student is experiencing
(e.g., the number of hours the student is working, illness), the need for assistance from the Learning
Enhancement & Academic Development (LEAD) program, and actions the student will take to prevent
further difficulties. The faculty advisor will approve the plan and make appropriate referrals as necessary.
Both the student and the faculty advisor will sign the plan, and both parties will retain a copy. The student
will submit a copy of the plan to the Academic Performance and Standards Committee in a timely manner.
On a monthly basis, the student and faculty advisor will evaluate the plan and make changes as necessary.
Failure to Meet Standards – Second Block Actions: When a student does not achieve the required
standard in a second block in an academic year, the Academic Performance and Standards Committee will
schedule a meeting with the student. The student may invite his/her faculty advisor to the meeting. During
the meeting the corrective plan previously developed will be reviewed carefully, revised, and appropriate
additional referrals will be recommended, if needed. The student will continue on probation.
Failure to Meet Standards – Third Block Actions: When a student does not achieve the required
standards in a third block in an academic year, he/she will meet with the Academic Performance and
Standards Committee. The student may invite his/her faculty advisor to the meeting. At this time, the
Committee may recommend one of the following actions to the Dean: (1) The student may be required to
withdraw from the program “not in good academic standing,” and allowed to repeat the entire academic
year; or (2) be dismissed from the program (see Dismissal in General Academic Policies and Procedures
section). A recommendation regarding the disposition of a particular student’s case will be made by the
Academic Performance and Standards Committee based on review of the student’s overall academic
performance and with input from the student’s advisor, block faculty or other individuals the Committee
may consult. The Committee will send a written recommendation to the Dean, who will make a final
decision regarding the course of action to be taken. The student has the right to appeal this decision
according to established policy (see Student Appeal Process in General Academic Policies and
Procedures section). If a student is required to repeat an entire year of the program, he/she is responsible
for meeting with the Associate Dean for Academic Affairs to establish his/her schedule to ensure that all
required blocks are completed.
Incomplete grade (I): An Incomplete grade (I) indicates that a student has not been able to complete all
required work for issuance of a letter grade. An incomplete grade must be replaced before the student
registers for the next academic year, unless other arrangements are made with the Dean. The activities to
replace an incomplete grade may vary depending on individual circumstances. In some cases, Faculty may
require the student to take the block in the year following. The procedures for making up an incomplete
grade must not be in conflict with the College’s policy on Independent Study. The Block Facilitator and
Block Faculty should have a plan for removing the incomplete grade when assigning the I grade.
Replacement of an incomplete will be under the direction of the Block Facilitator and Block Faculty and
will be processed by the Office of the Associate Dean for Academic Affairs. A fee may be assessed. The
incomplete grade (I) remains on the transcript followed by the Pass grade when earned (I/P).
Eligibility to participate in Advanced Pharmacy Practice Experiences (APPEs): Courses in the first
through third years must be completed successfully before beginning APPEs. Students may not start an
APPE until the Academic Performance and Standards Committee has been notified that all blocks have
been remediated successfully. The Academic Performance and Standards Committee will ensure that
students are eligible to begin APPEs.
Progression to the Fourth Professional Year: Students must have completed at least three rotations
successfully by the end of July in their P3 year to progress to the fourth year of the program. As a general
79
rule, no “off rotations” will be given during the first three APPEs unless a student is required to remediate a
block during Rotation 1 or if there is an extenuating circumstance (e.g., maternity leave, illness). The
Academic Performance and Standards Committee will monitor the progress of any student who is on
academic probation.
Failure to Meet Standards on APPE: When a student receives a NP or an Incomplete grade (I) in a
rotation, the faculty member directing APPE assignments will notify the committee in a timely manner.
He/she will make recommendations to the committee regarding remediation. The Academic Performance
and Standards Committee will approve the remediation plan. The student will be placed on academic
probation until he/she remediates the APPE. To monitor the quality of a student’s performance on APPEs,
all students must complete at least one APPE with a voting, full-time faculty member. If a student drops or
fails this required APPE, he/she must complete another APPE successfully with another voting, full-time
faculty member.
Progression to Advanced Electives/Comprehensive Review and Assessment: Students may not begin
elective requirements (coursework, Advanced Electives, Research Elective) until all APPE rotations are
completed successfully. Students may not complete the Comprehensive Review and Assessment until all
other requirements are completed. Any students requesting an exception to this policy will be considered on
a case by case basis by the Academic Performance and Standards Committee. The recommendation of the
Academic Performance and Standards Committee will be forwarded to the Dean for his/her action.
Incivility
The College of Pharmacy does not tolerate incivility by any member of the College/University
community. This includes faculty, staff, students, guests, and visitors. Examples of incivility include rude,
sarcastic, obscene, disruptive or disrespectful behavior, threats, and damage to property. Complaints of
incidences of incivility will be reported to the Dean. Should violations by students be determined to have
occurred, the Dean either will resolve the issue or forward the issue to the Student Conduct Committee.
Students have the right of appeal through the Student Appeal Process.
Veterans
Veterans who fail to maintain satisfactory progress for more than five (5) blocks will not be certified to
receive any Veterans’ benefits until they have corrected the situation and are making satisfactory progress.
Research Activities
Students in the College of Pharmacy are encouraged to participate in research under the direction of
faculty advisor(s). Students with appropriate interests and academic preparation may participate in research
as part of the elective program.
Program Completion and Eligibility for Graduation
All coursework in the College of Pharmacy must be completed within six (6) years of beginning the
program. Exceptions may be made only upon recommendation of the Academic Performance and Standards
Committee in consultation with the Dean. Students eligible for graduation must be approved by a vote of
the College Faculty.
Graduation
A student will be recommended for the Doctor of Pharmacy degree provided he/she:
• Has been enrolled in the Western University of Health Sciences, College of Pharmacy, for the duration
of the Pharm.D. program.
• Is not on probation and has completed all prescribed academic requirements and has no outstanding
grade of “I” or “NP”.
• Has demonstrated no serious deficiencies in ethical, professional, or personal conduct that would make
it inappropriate to award the Doctor of Pharmacy degree.
• Has complied with all the legal and financial requirements of the University as stated in the University
Catalogue.
No student will receive his/her diploma until that student has successfully completed all requirements for
graduation.
80
All students must attend and participate in the Commencement program at which time the degree is
conferred, unless special permission has been granted by the President of Western University of Health
Sciences. If the President grants special permission to be excused from graduation, the graduate may be
required to present himself or herself to the Provost, Executive Vice President of Academic Affairs or
appropriate Dean at a later date in order to take the required oath (if relevant) to receive his or her diploma.
DESCRIPTION OF BLOCKS/COURSE DESCRIPTIONS
Blocks listed in this catalog are subject to change through established academic channels. New blocks
and changes in existing blocks are approved by the College of Pharmacy Curriculum Committee and the
Faculty.
FIRST YEAR
The 5000 series is assigned to didactic blocks in the Basic Science Foundations and Professional
Practice Foundation blocks for the first-year pharmacy students (P1).
PHRM 5111 Foundations of Clinical Practice I (4 credits)
This block is designed to introduce the student to the knowledge, skills and attitudes necessary for
successful completion of the Pharm.D. curriculum, and to begin to develop foundation skills for patient-
centered pharmacy practice. General topics include an introduction to contemporary pharmacy practice and
the role of the pharmacist as a health care provider, written and verbal communication skills, developing
team collaboration skills, humanism, introduction to ethics and professionalism, time management, resume
writing, pharmacy abbreviations and equivalents, medical terminology, pharmaceutical calculations,
pharmacy law, introduction to over the counter medications and pharmaceutical care, introduction to drug
information, and introduction to the US health care system. (Formerly PHRM 5101)
PHRM 5112 Foundations of Clinical Practice II (3 credits)
This block is designed to further advance and reinforce the knowledge, skills and attitudes initially
introduced to the student in PHRM 5111 and to develop clinical foundation skills necessary for patient-
centered pharmacy practice. General topics include written and verbal communication skills, developing
team collaboration skills, medical terminology, pharmaceutical calculations, pharmacy law, over the counter
medications and pharmaceutical care, introduction of patient medical history and the patient medical record,
drug information, the top 200 drugs and drug cards, physical assessment skills, patient counseling skills,
belief systems and pharmaceutical care, introduction to pharmacy practice-community pharmacy and
inpatient hospital pharmacy clerkships. Prerequisite: PHRM 5111. (Formerly PHRM 5105)
PHRM 5113 Foundations of Clinical Practice III (5 credits)
This block is designed to further advance and reinforce the knowledge, skills and attitudes initially
introduced to the student in PHRM 5111, and further enhanced in PHRM 5112, and to develop clinical
foundation skills necessary for patient-centered pharmacy practice. General topics include written and
verbal communication skills, developing team collaboration skills, medical terminology, pharmaceutical
calculations, pharmacy law, over the counter medications and pharmaceutical care, introduction to patient
SOAP notes, the top 200 drugs and drug cards, First Aid certification, patient counseling skills, introduction
to pharmacy practice-community pharmacy and inpatient hospital pharmacy clerkships, current issues in
pharmacy practice and the medication use system. Prerequisite: PHRM 5112. (Formerly PHRM 5110)
PHRM 5114 Comprehensive Review (1 credit)
This block summarizes and provides a final integration of materials and skills learned during the first
year. A final comprehensive examination and a clinical skills assessment examination are administered and
year-long team assignments are finalized with presentations and poster sessions.
PHRM 5211 Introduction to the Pharmaceutical Sciences (1 credit)
This course introduces the chemical, physicochemical, biopharmaceutical and mathematical principles
and concepts that are fundamental to the study of the pharmaceutical sciences. Functional group chemistry
is introduced with emphasis on acid-base properties, contributions to solubility, chemical stability and
chemical incompatibilities. An introduction to the basic mathematical and graphical principles relevant to
81
students in pharmaceutics, biopharmaceutics and pharmacokinetics is also presented. Rational approaches
to problem-solving in the pharmaceutical sciences is an important component.
PHRM 5212 Integrated Biological Sciences I (3 credits)
This series of blocks (PHRM 5212, 5213, 5214 and 5215) presents general principles of biochemistry,
molecular biology, physiology, pharmacology and medicinal chemistry. The purpose of these blocks is to
demonstrate their interdependence and to provide an integrated, scientific basis for the development and
therapeutic use of drugs. The series focuses on the human system and provides the organizational
knowledge and background relevant to the management of homeostasis blocks of the second and third
years. The biochemistry and molecular biology portions present the common features of most biochemical
pathways and their relevance in diagnosing and treating disease, as well as developing therapeutic agents.
With physiology, the organization of biological systems (homeostasis) is emphasized with the objective of
demonstrating how the breakdown of organization leads to disease and the manipulation (interference or
enhancement) of organization provides the basis for therapeutic intervention. The intent is to demonstrate
how an understanding of biochemistry and molecular biology is fundamental toward developing an
appreciation of medicinal chemistry and the development of drug entities. Principles addressing cellular and
tissue physiology provide a conceptual framework to introduce pharmacology by emphasizing
commonalties of drug mechanism with drug classification. Fundamental principles are emphasized with the
intent of providing their relevance for prevention and treatment of disease using therapeutic agents, which
themselves can be considered as modifications of intrinsic, biological compounds. (Formerly PHRM 5102)
PHRM 5213 Integrated Biological Sciences II (3 credits)
Continuation of PHRM 5212. Prerequisite: PHRM 5212. (Formerly PHRM 5103)
PHRM 5214 Integrated Biological Sciences III (3 credits)
Continuation of PHRM 5213. Prerequisite: PHRM 5213. (Formerly PHRM 5104)
PHRM 5215 Integrated Biological Sciences IV (4 credits)
Continuation of PHRM 5214. Prerequisite: PHRM 5214.
PHRM 5301 Pharmaceutics/Biopharmaceutics I (3 credits)
This block introduces the student to physicochemical principles and their applications in order to
develop an understanding of the manufacture, compounding, and proper use of liquid (homogeneous and
disperse systems) and solid dosage forms. Prerequisite: PHRM 5211. (Formerly PHRM 5107)
PHRM 5302 Pharmaceutics/Biopharmaceutics II (3 credits)
This block deals with the manufacture, compounding and proper use of different dosage forms (topicals,
suppositories, aerosols, parenterals and novel drug delivery systems). Additionally, students will be
introduced to innovations in biotechnology processes and products. Prerequisite: PHRM 5301. (Formerly
PHRM 5108)
PHRM 5401 Immunology (3 credits)
The first part of this block introduces students to the basics of immunology including cells, organs and
effector systems involved in both cell mediated and humoral mediated immune activity. The second part of
the block focuses on regulatory interactions between different components of the immune system and the
deleterious effects of aberrant immune processes. (Formerly PHRM 5106)
PHRM 5501 Pharmacokinetics (4 credits)
This block gives the student an introduction to principles of pharmacokinetics. The relationships
between physicochemical characteristics and physiological factors to drug disposition are discussed. The
relevance of pharmacokinetics to drug therapy is presented. Prerequisites: PHRM 5111, PHRM 5301 and
PHRM 5302. (Formerly PHRM 5109)
82
SECOND YEAR AND FIRST HALF OF THE THIRD YEAR
The 6200 series describes the didactic curriculum for second-year pharmacy students (P2). The 6300
series denotes the didactic curriculum for the first half of the third year (P3).
PHRM 6201 Health Care Administration/Drug Information (4 credits)
This block covers Health Care Administration and Drug Information. Health Care Administration
provides an overview of the health care system in the US in terms of its evolution, structure, function,
components and interrelationships between stakeholders of the system. The Drug Information component of
this block continues the student's development in drug information. Introduces the student to research
methodology and biostatistics.
PHRM 6212 Introduction to Homeostasis and Nutrition (4 credits)
This block introduces homeostasis and covers materials from basic biochemistry to advanced
pharmacotherapeutics as they relate to nutrition. Introductory topics such as laboratory interpretations,
fluid-electrolytes, and acid-base disorders will be covered in addition to the nutrition related topics.
Accordingly, the overall goal of this block is to equip pharmacy students with elemental tools essential for
providing pharmaceutical care as well as to integrate knowledge, skills, and attitudes to provide an
individualized nutrition pharmacotherapeutic plan for a given patient. (Formerly PHRM 6207)
PHRM 6213 Gastrointestinal and Hepatobiliary Systems (4 credits)
This block provides the student with an understanding of the gastrointestinal and the hepatobiliary
systems. Specific emphasis is placed on the pharmacological treatment of peptic ulcer disease,
inflammatory bowel disease, alcoholic liver disease, and hepatitis. (Formerly PHRM 6202)
PHRM 6214 Nephrology and Pulmonary Systems (4 credits)
This block is designed to teach the student how to solve patient-based pharmacotherapeutic problems in
nephrology (kidney diseases) and pulmonology (lung diseases). Hypertension pathophysiology and
treatment are introduced in this course, including national guidelines for diagnosis and treatment.
Nephrology topics include evaluation of renal function, acute renal failure, chronic renal failure (e.g.
diabetic nephropathy and primary glomerular diseases), complications of renal failure (e.g. fluids and
electrolytes, anemia, and secondary hyperparathyroidism), renal transplant, and appropriate drug dosing in
renal disease. Pulmonary topics include asthma (adult and pediatric), chronic bronchitis, emphysema, and
cystic fibrosis. Students learn the proper use of inhalers, spacers, nebulizers, and peak flow meters. Several
critical care medicine topics and venous thromboembolism are also components of this block. Major
concepts of prior block material is reinforced throughout the block. (Formerly PHRM 6204)
PHRM 6215 Foundations of Clinical Practice IV (4 credits)
This block is designed to allow the student an opportunity to strengthen their knowledge in the content
areas previously covered in the second year blocks. Students will engage in team case discussions, which
incorporate and integrate aspects of those disease states previously covered. In addition, students will
continue to expand their knowledge of individual drug therapies by the construction of individual drug
cards. Skills (e.g., counseling, patient education, calculation applications, drug information applications)
relevant to the practice of pharmacy will be practiced in this block. Students will receive certification for
the administration of immunizations. Prerequisite: PHRM 5113. (Formerly PHRM 6205)
PHRM 6216 Endocrine and Reproductive Systems (4 credits)
This block provides students with the knowledge, skills and attitudes to manage pharmacotherapeutic
regimens in endocrine-related diseases, such as diabetes and thyroid disorders, and reproductive medicine.
Gender-related health concerns are also addressed. (Formerly PHRM 6203)
PHRM 6217 Cardiovascular System (4 credits)
This block contains epidemiology, anatomy, physiology, pharmacology, and pharmacotherapy as they
relate to cardiology. Accordingly, the overall goal of this block is to enable students to integrate their
knowledge of these topics in the context of formulating an individualized pharmacotherapeutic plan for a
given patient with cardiac disease(s). (Formerly PHRM 6206)
83
PHRM 6208 Neurosensory System (4 credits)
This block focuses on the pathophysiology, pharmacology, and pharmacotherapy relevant to diseases
affecting the central nervous system. The main goal of this block is to provide students with the
fundamental knowledge, skills and attitudes required to provide optimal pharmaceutical care to patients
with neurologic disorders. Disease states covered include dementias, epilepsy, headache, Parkinsonism,
acute and chronic pain and stroke.
PHRM 6209 Psychiatry (4 credits)
The purpose of this block is to enable students to integrate the pathophysiology, medicinal chemistry,
pharmacology and therapeutic knowledge in the management of specific disease states. The content of the
block will span psychiatric diseases, substance abuse and toxicological states. Students are provided the
opportunity to practice clinical problem assessment and therapeutic drug monitoring in preparation for
providing pharmaceutical care.
PHRM 6210 Foundations of Clinical Practice V (4 credits)
This block is designed to allow the student an opportunity to strengthen their knowledge in the content
areas previously covered in the second year blocks. Students will engage in team discussions, which
incorporate and integrate aspects of those disease states previously covered. In addition, students will
continue to expand their knowledge of individual drug therapies by the construction of individual drug
cards. Skills (e.g., counseling, patient education, calculation applications, drug information applications)
relevant to the practice of pharmacy will be practiced during this block. Students will receive instruction on
the pharmacist’s role in investigational drug services. Prerequisite: PHRM 6215.
PHRM 6301 Infectious Disease (4 credits)
This block is an integrated approach to microbiology, antimicrobial pharmacology and infectious
disease syndromes. The initial part of the block deals with the identification, laboratory diagnosis,
epidemiology and modes of spread of the medically important pathogens. Pharmacology of the major
classes of antimicrobial agents will be discussed. The latter part of the block will focus on the microbiology,
epidemiology, pathogenesis, pathophysiology, diagnosis, clinical features, preventive and infection control
measures associated with major infectious syndromes due to common bacteria and parasites.
PHRM 6302 HIV, AIDS and Organ Transplantation (4 credits)
This block is an extension of PHRM 6301 with a focus on special patient populations and opportunistic
infections including fungal and viral infections. Pharmacology of antiviral and antifungal agents and the
applications in treating infections will be discussed. The latter part of the block will focus on basic
pharmacology of immunotherapeutic agents and their applications in transplantation.
PHRM 6303 Drug Information/Pharmacy Administration (4 credits)
This block covers Drug Information and Pharmacy Administration. The Drug Information component of
this block continues the students' development of the knowledge, skills and attitudes in drug information.
Pharmacy Administration covers the components of the pharmaceutical distribution system, including
production, logistics, utilization and external subsystems. This block also presents an introduction to human
resource management, strategic planning and marketing, purchasing and inventory, financial management
and continuous quality improvement; and their applications to pharmacy and health care.
PHRM 6304 Oncology (4 credits)
The objective of this block is to provide an introduction in the pathophysiology, medicinal chemistry,
pharmacology, and therapeutic knowledge in the management of hematological disorders, hematological
malignancies and solid tumors. Students will receive instruction in the following areas: appropriate cancer
screening and prevention information to the general public; basic pharmacology of the commonly used
antineoplastic agents in clinical settings; supportive care in oncology and patient specific treatments; and
appropriate treatments for the common types of hematological disorders.
84
PHRM 6305 Pharmacoeconomics (4 credits)
This block provides students with an understanding of the fundamentals of pharmacoeconomics and its
value to decision making in health care. The block will include the terminology of pharmacoeconomics and
involve understanding, performing and evaluating different types of pharmacoeconomic analysis. Students
will be able to use their background in research methodology and statistics to conduct a 10-step evaluation
of published pharmacoeconomic studies.
ADVANCED PHARMACY PRACTICE EXPERIENCES (APPEs): SECOND HALF OF THE 3RD
YEAR (P3) AND FIRST HALF OF THE 4TH YEAR (P4)
The APPE rotations provide one year of supervised clinical education. Students advance their
knowledge in areas such as taking drug histories, providing patient education, interpreting diagnostic data
and dispensing and compounding medications. The 7000 series are designated for the APPE rotations.
Required rotations:
PHRM 7110 Ambulatory care externship (8 credits)
Supervised patient care experience in an outpatient setting under the supervision of a preceptor or
faculty member of the College of Pharmacy.
PHRM 7120 Institutional care externship (8 credits)
Supervised patient care experience in a hospital or other institutional setting under the direct supervision
of a preceptor or faculty member of the College of Pharmacy.
PHRM 7210 Ambulatory care clinical (8 credits)
Supervised clinical pharmacy experience emphasizing the development of pharmaceutical care skills in
an out-patient setting.
PHRM 7220 Institutional care clinical (8 credits)
Supervised clinical pharmacy experience emphasizing the development of pharmaceutical care skills in a
hospital or other institutional setting such as a long term care facility.
Elective Rotations:
PHRM 7330 Elective clerkship I (8 credits)
Supervised education in clinical, administrative or research settings that provide additional experience in
specialty areas such as pediatrics, geriatrics, infectious disease, drug information, oncology, pharmaceutical
research, pharmacy administration, etc.
PHRM 7340 Elective clerkship II (8 credits)
Supervised education in clinical, administrative or research settings that provide additional experience in
specialty areas such as pediatrics, geriatrics, infectious disease, drug information, oncology, pharmaceutical
research, pharmacy administration etc.
Prerequisite: PHRM 7330.
PHRM 7350 Elective clerkship III (8 credits)
Supervised education in clinical, administrative or research settings that provide additional experience in
specialty areas such as pediatrics, geriatrics, infectious disease, drug information, oncology, pharmaceutical
research, pharmacy administration etc.
Prerequisite: PHRM 7340.
Electives:
FOURTH YEAR (P4): 16 credits of elective coursework and 2 credits in the comprehensive review and
assessment are required.
The 8000 series is designed for elective coursework and the comprehensive assessment/review weeks.
The elective program is a capstone experience designed to prepare the student for his/her role as an entry
level practitioner. Electives are offered in areas such as research, teaching, and advanced clinical practice.
85
A project is required of each student. Finally, each student completes a required comprehensive two-week
review and assessment at the end of the program.
PHRM 8200 Elective Coursework (4 credits)
Advanced level coursework in an area of special interest beyond that presented as part of the previous
didactic coursework of the Doctor of Pharmacy Curriculum. Repeatable to a maximum of 16 credits.
PHRM 8400 Elective Apprenticeships (16 credits)
Advanced clinical educational experiences in an area of special interest beyond that provided as part of
the previous clinical coursework of the Doctor of Pharmacy Curriculum. Repeatable to a maximum of 16
credits.
PHRM 8600 Research Electives (16 credits)
Supervised participation in pharmacy related research under the direct supervision of a faculty member.
Repeatable to a maximum of 16 credits.
PHRM 8800 Other Electives (4-16 credits)
Individualized, supervised educational experiences in an area of special interest related to pharmacy
practice beyond that provided by previous coursework in the Doctor of Pharmacy curriculum and not
eligible for credit within PHRM 8200, 8400 or 8600. Repeatable to a maximum of 16 credits.
PHRM 8999 Comprehensive Review and Assessment (2 credits)
A two-week series of didactic and other educational experiences designed to provide students with a
review of the Doctor of Pharmacy Curriculum and conduct assessments of the student's competency for
pharmacy practice.
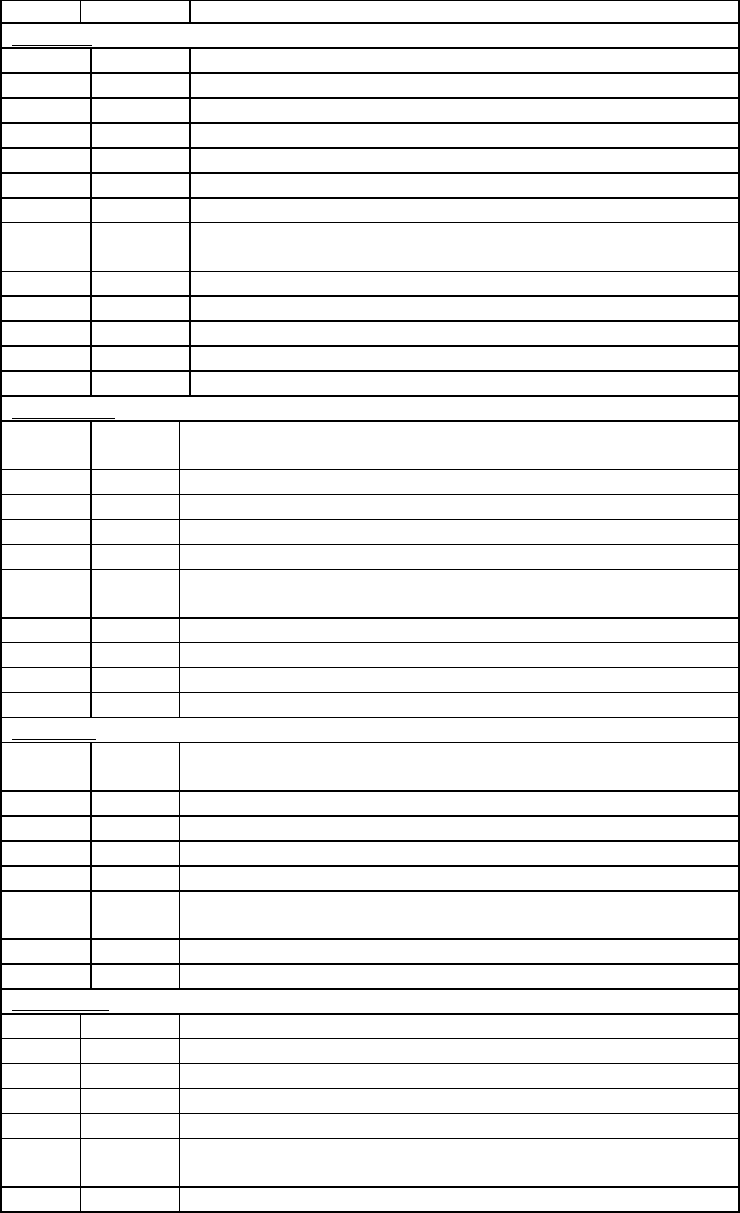
86
Sample Schedule: The following schedule represents an example of the schedule for the blocks in one
academic year. This schedule is subject to change.
Year Block No. Block Title
First Year
Fall
5111 Foundations of Clinical Practice I-Introduction to Pharmacy
5112 Foundations of Clinical Practice II
5211 Introduction to Pharmaceutical Sciences
5212 Integrated Biological Sciences I
5213 Integrated Biological Sciences II
5301 Pharmaceutics/Biopharmaceutics I
5302 Pharmaceutics/Biopharmaceutics II
Spring
5214
Integrated Biological Sciences III
5215 Integrated Biological Sciences IV
5401 Immunology
5501 Pharmacokinetics
5113 Foundations of Clinical Practice III
5114 Comprehensive Review
Second Year
Fall
6201
Health Care Administration/Drug Information
6212 Intro. Homeostasis/Nutrition
6213 Gastrointestinal and Hepatobiliary Systems
6214 Nephrology and Pulmonary Systems
6215 Foundations of Clinical Practice IV
Spring
6216
Endocrine and Reproductive Systems
6217 Cardiovascular System
6208 Neurosensory System
6209 Psychiatry
6210 Foundations of Clinical Practice V
Third year
Fall
6301
Infectious Diseases
6302 HIV, AIDS and Transplantation
6303 Oncology
6304 Drug Information and Administration
6305 Pharmacoeconomics
Spring
R1 Inpatient Care Experiential (IX)
R2 Ambulatory Care Experiential (AX)
R3 Inpatient Care Clinical (IC)
Fourth Year
R4 Ambulatory Care Clinical (AC)
R5 Elective rotation
R6 Elective rotation
R7 Elective rotation
R8 Off
January-
May
Advanced Electives: Apprenticeships, coursework, research
May Comprehensive assessment and review
87
HONORS AND AWARDS
The following awards for PharmD students are presented annually on Honors Day in April.
President's Society Award
Provost's Student Government Award
Dean's Award
American Society of Health Systems Pharmacists Student Leadership Award
Eli Lilly and Company Award
Linda Fox Memorial Endowment Fund Award
Guy M. Allmon Scholarship Fund Award
The following awards are presented annually to graduates at the Commencement Dinner Dance:
Merck Award
APhA-ASP Mortar & Pestle Professionalism Award
Roche Pharmacy Communications Award
Dr. Arasb Ateshkadi Memorial Award
SmithKline Beecham Award
Facts & Comparisons Award of Excellence in Clinical Communication
Pfizer US Pharmaceuticals Outstanding Leader Award
TEVA Pharmaceuticals Outstanding Student Award
Perrigo Award for Excellence in Nonprescription Medication Studies
Mylan Pharmaceuticals Award
Dean's Award
ACADEMIC CALENDAR 2001-2002
(subject to change)
Wednesday, Aug. 1, 2001
Fall Semester Tuition Due (4
th
years)
Wednesday, Aug. 8, 2001
Fall Semester Tuition Due (1
st
, 2
nd
and 3
rd
years)
Wednesday, Aug. 8-Thursday, Aug. 9, 2001
Orientation
Saturday, Aug. 11, 2001
Convocation/White Coat Ceremony
Monday, Aug. 13, 2001
Classes begin
Friday, Sept. 1, 2001
Fall Semester Tuition Due (4
th
years)
Monday, Sept. 3, 2001
Labor Day:
Friday, Oct. 5, 2001
Professional Association Day
Monday, Oct. 8, 2001
Columbus Day
Wednesday, Nov. 21, 2001 (12:00 noon)
Thanksgiving recess
Monday, Nov. 26, 2001
Classes Resume
Friday, Dec. 21, 2001
Last Day of Classes, Autumn Semester
Wednesday, Jan. 2, 2002
Spring Semester Tuition Due (1
st
, 2
nd
& 4
th
years)
Monday, Jan. 7, 2002
Classes resume
Monday, Jan. 21, 2002
Martin Luther King Holiday
Friday, Feb. 2, 2002
Spring Semester Tuition Due (3
rd
years)
Monday, Feb. 18, 2002
Presidents Day
Friday, May 24, 2002
Last Day of Classes, Spring Semester
Friday, May 31, 2002
Graduation
88
COLLEGE OF ALLIED HEALTH PROFESSIONS
MISSION
The College of Allied Health Professions supports the mission of Western University of Health Sciences
by providing high quality professional and graduate education. The College utilizes the team approach to
develop competent and compassionate professionals who provide service to the community and continually
develop their skills, knowledge, and abilities through independent lifelong learning activities.
GOALS
1. To educate an allied health workforce that helps to meet the healthcare and educational needs of the
State of California and the west.
2. To achieve an environment and culture that support all members of the College.
3. To ensure an environment and culture that empower all persons in the College to maximize their
potential as contributing members in the education of students, in research and clinical activities, and in
service to the community.
89
COLLEGE OF ALLIED HEALTH PROFESSIONS
Master of Science in Health Professions Education Program
ABOUT THE MASTER OF SCIENCE IN HEALTH PROFESSIONS EDUCATION PROGRAM
The curriculum for the Master of Science in Health Professions Education places graduate studies in
health professions education within a framework of theory and practice that integrates the functional needs
of the working health practitioner with the scholarship and professional experiences necessary to meet
requirements for an advanced degree in education. Course work is designed to promote knowledge, values
and skills essential for competent teaching, as well as attitudes that foster a continuing interest in education.
Strategies employed to conduct instructional activities reflect principles of adult learning. Small group
discussions, one-to-one teaching, and individual consultation are frequently utilized to promote discussion
and group problem-solving among program participants.
Designed for professionals who are currently teaching or plan to teach in any of a number of health
disciplines, the Master of Science in Health Professions Education program utilizes learning activities that
draw on the functional requirements of health professionals to illustrate educational concepts and
methodologies. In addition to acquiring expertise in the principles of teaching and learning, program
planning and evaluation, participants are encouraged to develop educational research projects of their own.
Facilities and personnel of the College of Allied Health Professions are accessible for technical support and
consultation throughout the program.
The faculty includes scholars, researchers and administrators from a variety of backgrounds. All are
committed to the improvement of teaching in the health professions through the process of professional
development.
EDUCATIONAL PHILOSOPHY
The College of Allied Health Professions supports Western University of Health Sciences' mission to
increase the availability of health care providers to serve the needs of the people living in the western region
of the United States. In addition, the College of Allied Health Professions provides educational
opportunities for students in a variety of health careers. Classes are offered in an environment intended to
foster respect for the uniqueness of humanity. Students are provided with classroom and clinical
experiences designed to prepare them to function as competent health care practitioners.
Goals of the Department of Health Professions Education
The MSHPE program provides students with a background in theory and practical application in health
professions education. In fulfillment of the mission of the University, the Department’s goals are to:
1. Educate healthcare professions who will function as teachers in a variety of healthcare settings.
2 Educate healthcare professionals who will function as academic leaders in various healthcare settings.
3. Create educational opportunities for healthcare professionals.
4. Enhance continuing professional education in healthcare.
5. Further develop clinical education partnerships throughout the United States (West).
6. Provide educational service to the healthcare community.
Objectives of the Department of Health Professions Education
The MSHPE program is designed to prepare healthcare professionals with skills in teaching and
learning, educational administration, scholarship, and research. Upon completion of the program, students
should be able to:
1. Demonstrate proficiency in adult education practices based upon sound principles.
72. Apply educational theories, models, and concepts in a healthcare setting.
3. Create, implement and analyze valid research projects in health professions education or the clinical
setting.
4. Collaborate with other academic healthcare specialists.
5. Teach in a health professions setting.
6. Contribute research to the health professions.
90
TECHNICAL GUIDELINES FOR ADMISSION AND MATRICULATION
A candidate for admission to the MSHPE Program must have the use of certain sensory and motor
functions, or reasonable accommodations thereto, to permit them to carry out the activities described in the
sections that follow. Graduates of the program are eligible for employment in a wide variety of academic
and clinical teaching programs, using an extensive variety of educational methodologies. As a result, they
must have the intellectual ability to learn, integrate, analyze, and synthesize numerical, visual, and textual
information in the health professions fields. They must also be able to effectively and accurately integrate
this information and communicate it to others by both oral and written means.
A candidate for the Master of Science in Health Professions Education ordinarily must have abilities and
skills of five general varieties, including: (1) observation; (2)communication; (3)motor; (4) intellectual,
conceptual, integrative and quantitative; and (5) behavioral and social. Reasonable accommodations will be
provided in appropriate situations. Under all circumstances, however, a candidate should be able to perform
in a reasonably independent manner. The following provides an overview of the five general varieties of
minimal technical standards that must be met by all successful applicants to the MSHPE Program.
1. Observation: Candidates and students must have sufficient vision, with or without reasonable
accommodations, to be able to observe demonstrations and presentations by faculty and other students.
2. Communication: Candidates and students must be able to communicate with students and colleagues.
They should be able to hear, with or without reasonable accommodations. Candidates and students must
be able to read, write, and speak English.
3. Motor: Candidates and students should have sufficient motor function, or reasonable accommodations
to enable them to operate commonly used educational equipment (including, but not limited to,
computers, videotape players, overhead projectors) and design and produce educational materials. These
activities require coordination of both gross and fine muscular movements, equilibrium, and functional
use of the senses of touch or vision.
4. Intellectual, Conceptual, Integrative, and Quantitative Abilities: Students must demonstrate problem-
solving skills, which include measurement, calculation, reasoning, analysis, and synthesis. Instructional
design and the preparation of a thesis or special project requires all of these intellectual abilities.
5. Behavioral and Social Abilities: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgment, the prompt completion of
all responsibilities attendant to an instructor in an educational setting, and the development of mature,
sensitive, and effective relationships with students and colleagues. Candidates and students must be able
to adapt to changing environments and display flexibility in dealing with students at various educational
levels in the health professions. Compassion, integrity, concern for others, interpersonal skills, interest,
and motivation are all personal qualities to be assessed during the admissions and educational processes.
The MSHPE program, along with all the other programs at Western University of Health Sciences,
shares a commitment to develop creative ways of opening the MSHPE curriculum to competitive, qualified
individuals with disabilities. In doing so, however, the MSHPE Program must maintain the integrity of its
curriculum and preserve those elements deemed essential to educating candidates to become effective
teachers and role models.
ADMISSIONS POLICIES AND PROCEDURES
Admission to the Master of Science in Health Professions Education Program is through the Department
of Health Professions Education. Students may apply for either the fall or spring semesters. Western
University is committed to admitting competitive, qualified individuals with disabilities. For technical
guidelines, please see above.
Application Requirements
Applicants to the MSHPE Program should be health professionals or in a career that involves education
of health professionals. Candidates must meet the following academic requirements:
1. A bachelor's degree from an accredited institution is preferred. However, consideration will be given
on a case-by-case basis to applicants holding an advanced professional degree, provided that the
applicant has completed at least 90 semester hours at the undergraduate level from a regionally
91
accredited college or university, 30 units of which must consist of upper division coursework; i.e., junior
or senior level courses.
2. A 2.5 GPA or above for undergraduate work; 3.0 or above for graduate work.
Decisions of the Admissions Committee regarding the admission of applicants to the Master of Science
in Health Professions Education program are final.
Application Procedures and Deadlines
Students are advised to submit application materials as early as possible prior to the semester in which
they wish to begin their program of studies. Deadline for receipt of application materials is no later than 30
days prior to the first day of classes for each semester.
To request an informational brochure and/or an application, contact the admissions office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766
(909) 469-5336
In addition to submitting an application, the applicant must submit a nonrefundable application fee of
$35, a written statement of the manner in which this training will be used within the context of the
candidate's career and official transcripts from all undergraduate and graduate institutions attended.
Transfer of Credits
The maximum number of graduate units that may be transferred from another institution offering
programs of graduate studies is six semester units. Only graduate credit relevant to the MSHPE Program at
Western University completed within the last five years may be applied toward completion of the master's
degree. To be considered for transfer credit, the course must have been taken after the award of a bachelor's
degree and be eligible for graduate studies credit at the issuing institution. The student must have received a
grade of B or above in the course. An official transcript and a course description should be submitted to the
chair of the HPE Department. The MSHPE faculty will determine whether or not work undertaken at other
institutions qualifies for transfer. No transfer credit will be given for HPE 5999, HPE 5300, or HPE 5208.
Continuing Education and Non-degree students
An applicant who has a bachelor's degree and/or advanced degree and does not wish to pursue a master's
degree at Western University of Health Sciences at the present time, but who wishes to engage in graduate
study for (a) personal development, (b) continuing education, or (c) other professional development needs,
may consider enrollment as a non-degree student. A limited number of applicants may enroll as non-degree
students each semester. The usual admission and registration procedures must be followed. Admission as a
non-degree student does not assure acceptance as a degree candidate, should the student at a later time wish
to change enrollment status. An unlimited number of semester units may be completed while in non-degree
status. Should the student wish to change enrollment status, the usual admission procedures must be
followed. Previous course work will be reviewed by program faculty to determine acceptable courses to be
transferred into the master's level program. Questions about transferring from non-degree to degree status
should be directed to the Chairperson, Department of Health Professions Education.
Readmission
Graduate students who have not been enrolled for more than one calendar year must submit a new
application form and fee, unless other arrangements have been made at the time of withdrawal/leave from
the program. The application will be assessed according to the current admissions policies, and students will
be required to fulfill program requirements in place at the time of readmission.
REGISTRATION POLICIES AND PROCEDURES
Prior to each semester a class schedule is compiled and made available to students. All candidates for
the MSHPE degree are required to obtain pre-registration advisement in order to promote greater efficiency
in the registration and enrollment process. Enrollment occurs during the weeks prior to the first class
92
meetings, on an appointment basis. Students may register at the initial class meeting, but could be denied
admission to a specific class due to space availability. An individual must enroll for a minimum of three
semester hours of credit for each semester in which they wish to be identified as students.
New Graduate Students
New graduate students are notified by mail of their admission status. This notification will include a list
of courses available during the next semester and the necessary registration materials. Completed
registration materials and fees may be submitted through the mail, or in person, prior to the first week of
classes.
Continuing Graduate Students
Continuing students will receive registration information and materials by mail prior to the beginning of
the semester. Should this information not arrive for any reason, it is the student's responsibility to contact
the office of Student Affairs for the appropriate materials. Completed registration materials and fees may be
submitted to the Registrar through the mail or in person, prior to the first week of classes.
Late Registration
Students must follow the registration procedures and timelines printed in the Class Schedule provided at
the beginning of each regular semester. The days of registration and late registration are listed in that
document. Appropriate fees for late registration will be assessed.
Add/Drop and Withdrawal from Courses
In order to add or drop a class, the student must obtain a Change of Registration form from the
Chairperson, complete and submit it prior to the end of the third week of classes of each semester.
Withdrawal from a course (not the program) requires completion and submission of the appropriate
withdrawal form obtained from the Chairperson. Please note that this will not result in an "incomplete" (I)
grade.
ACADEMIC REQUIREMENTS
Course Load
A graduate student at Western University of Health Sciences must enroll in at least eight semester hours
per term to be considered full-time. To be considered full-time when enrolled in fewer than eight hours, the
student must be registered in all remaining courses necessary for completion of the graduation requirements
for the master's degree.
Reasonable Academic Progress
All students are expected to make reasonable progress each year toward the degree objective. Full-time
graduate students are considered to be making reasonable academic progress when they maintain an overall
GPA of at least 3.0 and complete 18 semester hours during the calendar year. Both part-time and full-time
students must complete the graduation requirements within the time limits described under Graduation
Requirements.
For part-time students, reasonable academic progress will be determined by the faculty on an annual
basis upon consultation with the student. A letter specifying terms of the continued enrollment will be
mailed to the student.
Student Rights and Responsibilities
It is the responsibility of the student to be familiar with the contents of the catalog and to observe all
policies and procedures relative to the completion of requirements for the graduate degree that were in
effect at the time of initial enrollment in the MSHPE Program.
A student may opt to complete the program of study and degree requirements described in the catalog at
the time of his or her graduation, provided all revised policies of the later catalog are followed. Students are
required to keep the Registrar informed of their current address and telephone number. Forms for this
purpose are available in the Student Affairs office.
93
Grading System
Official grades are turned in to the Chairperson of the MSHPE Program from the course instructors.
Official grade reports are then prepared by the Registrar and mailed to the student. Western University of
Health Sciences makes use of letter grades, which may include a plus/minus (+ / -) system of grading. A
four-valued letter grade scale will be given, indicating:
Grade Quality Points
A - Excellent 4
B - Good 3
C - Satisfactory 2
U - Unsatisfactory 0
I - Incomplete 0
Au - Audit 0
W - Withdrawal 0
Cr - Credit 0
NCr - Non-credit 0
Courses are rated at one semester hour for each 12 contact hours. The grade point average is calculated
at the end of each semester as the sum of earned grade points divided by the sum of semester hours passed
and failed. A cumulative grade point average will be calculated and posted on the transcript.
No grade will be changed unless the instructor certifies in writing that an error in computing or
recording the grade has occurred or that the student has completed course requirements for an Incomplete
grade or remediated an Unsatisfactory grade.
Incomplete
An Incomplete grade ("I") will only be assigned to students whose professional commitments and/or
personal responsibilities prevent him or her from completing the requirements of the course. A student may
remove an incomplete by completing course requirements within the following academic semester. Should
extenuating circumstances arise, the student may petition for a one-semester extension to complete the
course work. Arrangements for the Incomplete and its removal must be approved by the instructor prior to
the end of the semester in which the original Incomplete grade was assigned. Grade changes must be
certified by the instructor prior to the end of the semester following the original grade assignment.
Academic Standing
An overall grade point average of 3.0 (B) must be maintained during graduate work undertaken at
Western University of Health Sciences in order to qualify for advancement to candidacy. A 2.0 (C) grade
earned in any class may be applied toward graduation only if the overall grade point average at the time of
application for graduation continues at a minimum 3.0 (B) overall grade point average. Any grade below a
2.0 (C) may not be applied toward graduation. Any student whose grade point average falls below a 3.0 (B)
average will be placed on probation.
Academic Requirements
REQUIRED CORE
HPE 5100 Teaching and Learning Theory 3 credit hours
HPE 5102 Principles of Instructional Design and
Clinical Teaching 6 credit hours
HPE 5104 Evaluation Methods 3 credit hours
HPE 5106 Research Methods I 2 credit hours
HPE 5108 Instructional Technology 3 credit hours
Total: 17 credit hours
SELECTIVES (Select at least nine credit hours)
HPE 5200 Historical Issues in Health
Professions Education 3 credit hours
HPE 5202 Legal/Ethical Issues in Health Care 3 credit hours
94
HPE 5204 Educational Administration/Leadership 3 credit hours
HPE 5206 Research Methods II 3 credit hours
HPE 5208 Special Topics 1-3 credit hours
HPE 5210 Disabilities in the Health Professions 3 credit hours
HSCI 5014 Introduction to Community
Health Education 3 credit hours
ELECTIVES
(Maximum of nine credit units counted towards the degree)
HPE 5300 Directed Field Experience 1-3 credit hours
(repeatable to a maximum of 6 units)
HPE 5302 Independent Study 1-3 credit hours
(repeatable to a maximum of 6 units)
HPE 5999 Thesis/Special Project 3-6 credit hours
Residency Requirements
Of the 32 required units, 26 must be completed with course work offered by the MSHPE Program.
Language Requirements
No foreign language classwork or test of proficiency is required of candidates for the MSHPE degree.
Time Limits
All requirements for the degree must be fulfilled within five years from the date of initial registration.
Extensions of this time limit may be granted through petition to the faculty.
Advancement to Candidacy
At least one semester prior to when the student plans to complete the unit requirements, he or she must
file an "Application for Advancement to Candidacy" form. This step is undertaken as a prelude to sitting for
the Comprehensive Examinations or scheduling the final oral examination for students selecting the thesis
or special project options.
Final Integrative Exercise
The Master of Science degree is awarded following satisfactory completion of all course work and one
of the following three options described below: (1) a thesis, reporting the results of an original research
project on a topic related to the program goals; (2) a special project report, which presents the results of
development or implementation of a formal health professions educational activity; or (3) a comprehensive
examination. Prior to graduation, the student must complete the Master of Science in Health Professions
Education graduation requirements options form and return it to the Chairperson, Master of Science in
Health Professions Education. Names of candidates for graduation are presented to the Student Academic
Progress Committee, the Dean of Allied Health Professions and to the Western University of Health
Sciences faculty for approval.
All students who have completed graduation requirements must attend, in person, and participate in the
Commencement program at which time the degree is conferred. The President may approve exemptions to
this last requirement.
Thesis/Special Project Option
A student who selects either the thesis or special project option is responsible for selecting a
Thesis/Special Project Committee. This committee consists of a committee chair and one additional
committee member. After a student has been advanced to candidacy, the candidate is responsible for
obtaining and completing the Master of Science Committee form from the chair of the HPE department.
Students are responsible for meeting with the HPE department chairperson, who will assist the student in
obtaining a thesis/special project committee chairperson. The committee chairperson must be a full-time
employee at Western University with a faculty appointment in the HPE program. No committee chairs of
95
the thesis/special project option will be permitted from outside Western University. Students must also
obtain a committee member for the thesis/special project option. The committee members may be a scholar
from outside the University, but must be approved by the Department Chairperson.
Graduation Requirements
A student will be recommended for the degree of Master of Science in Health Professions Education
provided he or she:
1. Has satisfactorily completed the 32-unit course requirement in the MSHPE curriculum.
2. Has satisfactorily completed a thesis, special project or comprehensive examination.
3. Is not on probation and has completed all prescribed academic requirements.
4. Has complied with all the legal and financial requirements of the University as stated in the
University catalog.
5. Has demonstrated no serious deficiencies in ethical, professional personal conduct, as defined
previously, and;
6. Attends in person and participates in the Commencement program at which time the degree is
awarded, unless special permission has been granted by the President of the University. If the President
grants special permission to be excused from graduation, the graduate may be required to present
himself or herself to the Provost or appropriate Dean at a later date in order to take the required oath (if
relevant) to receive his or her diploma.
TUITION AND FEES
Schedule of Fees
$225 Unit cost per semester hour (32 semester hours minimum for MSHPE degree)
Other Fees and Expenses
$35. Application Fee
$50. Continuous Registration Fee
$30. (per day) Late Registration Fee
$10 Lost ID Badge
$5. (each) Copy of Official Transcript
$0.25 (per page) Copy of Student File Material
Tuition and fees are subject to change without notice upon approval by the Board of Trustees. All fees
are mandatory for each student and are non-refundable.
Obligation for payment in-full of tuition and fees is due upon matriculation. The MSHPE Program can
offer a schedule of divided payments for students demonstrating financial need (for more information see
the Bursar).
PROGRAM OF STUDIES
The Master of Science degree can be completed with one year of full-time study (two regular semesters
and one summer session). However, most candidates elect part-time participation and plan a program of
study that requires four regular semesters and one or two summer sessions.
The courses listed below comprise the Master of Science in Health Professions Education curriculum
offered by Western University of Health Sciences.
COURSE DESCRIPTIONS
HPE 5100 Teaching and Learning Theories (3 credit hours)
This survey course is designed to introduce the student to teaching and learning theories as they apply to
the adult learner. The interrelationship between learning and teaching styles and how these impact the
learning environment are covered. Teaching methods and strategies designed to enhance classroom learning
in the health professions are emphasized. The design of practical learning activities is underscored. Not
open for student with credit for HPE 503
96
HPE 5102 Principles of Instructional Design & Clinical Teaching (6 credit hours)
This course is designed to provide the student with the skills needed to develop educational programs in
the health professions and incorporating the role of the clinical instructor. Practice is given in applying
descriptive principles of teaching and learning to the design of a unit of instruction. Included will be the
construction of a needs assessment, data analysis, writing instructional objectives, defining instructional
strategies, designing learning activities, selecting media and planning evaluation. Not open for students with
credit for HPE 512 or HPE 520.
HPE 5104 Evaluation Methods (3 credit hours)
The purpose of this course is to assist the student to acquire the skills necessary to conduct student
performance and program evaluations. Measurement of student performance in the formal educational and
clinical setting includes construction and use of written examinations, simulations, rating scales, chart
audits, observation techniques, and other measures of cognitive, affective and psychomotor behavior.
Included is an overview of procedures for item analysis and test validation. Not open for students with
credit for HPE 514.
HPE 5106 Research Methods I (2 credit hours)
This introductory course is designed to prepare the health professions student to understand principles
for the analysis and interpretation of quantitative data in health professions education research. It will
include measurement theory, the graphical presentation of data, probability theory, and the use of
descriptive and inferential statistics in the interpretation of data. As a result, the student will be able to read
original research reports in a more critical manner. Not open for students with credit for HPE 518.
HPE 5108 Instructional Technology (3 credit hours)
This course provides an overview of the principles and applications of instructional media in the realm
of adult and health education settings. The goal of this course is to provide for competence in the planning,
selection and use of various forms of instructional technology for health care training programs. Emphasis
will be made on an understanding of the principles of teaching and learning. Utilizing those principles,
practical applications will be addressed, including the design and development of various instructional
approaches as well as the appropriate selection and application of the various media forms. Students will
function as members of a seminar, will produce a media-based instructional presentation and will write a
limited research paper on current trends in instructional technology applications. Not open for students with
credit for HPE 513.
HPE 5200 Historical Issues in Health Professions Education (3 credit hours)
This course provides a survey of the historical development of issues in health care, including early
types of medicine and medical education in antiquity through contemporary issues in health professions
education. Not open for students with credit for HPE 501.
HPE 5202 Legal/Ethical Issues in Health Care (3 credit hours)
This course will introduce the student to the ethical and legal challenges of modern heath care and health
care education. Insight into the basic ethical and philosophical concepts involved in health care education
will be stressed. The historical background on laws that define the roles and responsibilities of health care
professionals and educators will be presented. Students will be given the opportunity to explore personal
values regarding a variety of issues facing health care workers and educators today. Not open for students
with credit for HPE 509.
HPE 5204 Educational Administration/Leadership (3 credit hours)
This course will introduce the student to selected management theories. Leadership styles will be
emphasized. Motivation and human behavior theories related to the functions of health care organizations,
including the development of human resources and fiscal responsibilities, will be stressed. Trends in health
care management will be surveyed. Not open for students with credit for HPE 511.
97
HPE 5206 Research Methods II (3 credit hours)
The purpose of this course is to introduce students to a variety of research methodologies employed in
both clinical and educational settings. Included will be historical studies, case studies, observational studies,
the survey, quasi-experimental designs, and experimental designs. Generalizability issues and
validity/reliability issues related to research are presented. HPE 5106 or its equivalent is a prerequisite for
this course. Not open for students with credit for HPE 530.
HPE 5208 Special Topics (formerly HPE 599) (1-3 credit hours)
This format is designed to permit in-depth study of a single issue in health professions education.
Current issues and/or trends may be included.
HPE 5210 Disabilities in the Health Professions (3 credit hours)
This is an introductory course presenting issues involved in educating health professions students with
cognitive, physical and sensory disabilities. Topics include history and culture of disabilities in the health
professions, assistive technology, legal aspects, and communication.
HSCI 5014 Introduction to Community Health Education (3 credit hours)
This course provides an overview of the development and implementation of patient education programs
in the community and in acute, long-term clinical settings. Models for preparing health education programs
will be presented, including design considerations, appropriate for age, ethnic, cultural, and socioeconomic
differences. Assessment of need, developing objectives, designing learning activities, implementation, and
evaluation are emphasized. Practical application will include the design and implementation of one unit of
instruction based on a health education subject.
HPE 5300 Directed Field Experience (3-6 credit hours)
This course is designed for health professionals who are teaching in a classroom/clinical/laboratory
setting. Under the supervision of MSHPE faculty, students will design and implement instruction
appropriate to the learning environment in which they are participating. Three to four lectures represent one
semester credit hour. Self evaluation and revision of presentations are stressed. Student may enroll up to a
maximum of 3 credit hours per semester, repeatable to a maximum of 6 credit hours. Graded Cr/NCr. Not
open for students with 6 or more credits for HPE 515.
HPE 5302 Independent Study (1-6 credit hours)
Registration in this course permits students, under MSHPE faculty supervision, to contract for special
educational projects or readings in education which relate to individual professional needs and interests. A
maximum of 3 credit units may be taken per semester, repeatable to a maximum of 6 credit hours. Graded
Cr/NCr. Not open for students with 6 or more credits of HPE 590.
HPE 5999 Thesis/Special Project (3-6 credit hours)
Students who plan to partially fulfill graduation requirements for the Master of Science degree by
writing a thesis or completing a Special Project must register in this course. Graded Cr/NCr. Not open for
students with 6 or more credits for HPE 580.
HONORS AND AWARDS
The following awards are presented annually at the University's Honors Day ceremony in April:
President's Society Award
Guy M. Allmon Scholarship Fund
Linda Fox Memorial Endowment Fund
The following awards are presented annually at the University's commencement dinner:
Dean's Award
Don and Jean Griva Memorial Award
98
ACADEMIC CALENDAR
2001-2002
MSHPE PROGRAM
(subject to change)
Fall Semester
Tuesday, Sept. 4 - Friday, Sept. 14, 2001
Registration
Wednesday, Sept. 5, 2001
Fall Semester Tuition Due
Monday, Sept. 10, 2001
Classes begin
Friday, Sept. 21, 2001
Last day to add/drop class
Monday, Oct. 8, 2001
Columbus Day (no class)
Wednesday, Nov. 21, 2001
Thanksgiving recess (noon)
Monday, Nov. 26, 2001
Classes resume
Friday, Dec. 21, 2001
Last day of classes
Last day to file for Advancement to Candidacy
Spring Semester
Wednesday, Jan. 2, 2002
Spring Semester Tuition Due
Thursday, Jan. 3- Friday, Jan. 11, 2002
Registration
Monday, Jan. 7, 2002
Classes begin
Monday, Jan. 21, 2002
Martin Luther King Jr. holiday (no class)
Friday, Jan. 25, 2002
Last day to add/drop class
Monday, Feb. 18, 2002
President's Day (no class)
Monday, Mar. 18, 2002
Spring Break
Monday, Mar. 25, 2002
Classes resume
Monday, April 8, 2002
Honors Day
Wednesday, May 1, 2002
Last day for Oral Examinations
Friday, May 10, 2002
Last day of classes
Friday, May 31, 2002
Commencement
Summer Semester
Monday, Jun. 10 - Friday, Jun. 4, 2002
Registration
Monday, Jun. 10, 2002
Summer Semester Tuition Due
Monday, Jun. 17, 2002
Classes begin
Thursday, Jul. 4, 2002
Independence Day observed (no class)
Monday, Jul. 8, 2002
Last day to add/drop class
Friday, Aug. 30, 2002
Last day of classes
99
COLLEGE OF ALLIED HEALTH PROFESSIONS
Master of Physical Therapy Degree Program
Accreditation
The Master of Physical Therapy Program in the College of Allied Health Professions is accredited by
the Commission on Accreditation in Physical Therapy Education (CAPTE).
The Practice of Physical Therapy
The physical therapist is a health care provider who is academically and clinically prepared to provide
physical therapy services to individuals with dysfunctions of the neuromusculoskeletal, cardiovascular,
pulmonary and integumentary systems. These services include evaluating and diagnosing movement
dysfunctions, setting goals and determining patient prognosis, planning and implementing treatment
intervention, and reassessing patient progress. In addition, the physical therapist educates the patient/client
to prevent injury, maintain and promote health and wellness. The physical therapist also contributes to
society and the profession through administration, education, consultation, and research.
MPT Degree Program
The Master of Physical Therapy (MPT) Degree program at Western University was initiated in January
1992. The educational philosophy of the program emphasizes student-centered, problem-solving learning
and the role of the physical therapist as a health care provider and a member of the health care team.
Mission of the Program
In keeping with the University's mission, the mission of the Physical Therapy program is to educate
competent, caring, culturally sensitive, reflective practitioners who will:
• participate as members of the health care team to provide high quality care to patients;
• as life-long learners, acquire, analyze, synthesize and apply knowledge in new settings;
• contribute to the verification of physical therapy evaluation and intervention techniques, and discover
new, more effective methods of patient care;
• be leaders in providing health care service and education to promote health and fitness of community
members; and
• play important roles in developing health policy and appropriate standards for physical therapy
practice.
Program Goals
The graduate of the MPT program will be a mature individual whose professional education is based
on a foundation of the requisite preparation in the biological, behavioral and social sciences, and
humanities. The graduate will have the necessary knowledge, skills and attitudes to function as a clinician
generalist; will have an appreciation for the value of all aspects of the research process; and will be a
responsible member of the community and the profession. Upon completion of the educational program in
physical therapy, the graduate will be able to:
• Have an understanding of the osteopathic philosophy with its emphasis on caring for, and appreciation
of the patient as a whole person;
• Demonstrate respect for all individuals;
• Practice physical therapy as an entry-level clinician generalist by assuming responsibility for the
components of that role;
• Communicate with peers, colleagues, patients, clients, family members and the community-at- large in
a style that is commensurate with their level of understanding;
• Appreciate the place of research in the advancement of physical therapy;
• Serve as a role model for healthy behaviors in both the clinical setting and community;
• Participate in the community as a representative of the physical therapy profession, as an advocate for
the patient or client in a health care environment, and as a concerned citizen;
100
• Continue lifelong learning through continuing education, specialization and participation in
professional organizations; and
• Establish priorities in order to maintain a balance between personal and professional life.
Description of the MPT Program
The curriculum for the Master of Physical Therapy Program will prepare the graduate to be a PT
generalist. The curriculum consists of 11 modules, each having a particular emphasis.
Curriculum Design
The MPT program is two years plus 16 weeks in length. Didactic education, which includes classroom
and PT laboratories to practice procedures on classmates, is followed by clinical education assignments in
a wide variety of clinical settings. Year I consists of one 15-week and one 11-week didactic education
periods, followed by Clinical Practicum I for two weeks. To complete year I, the student has a 15 week
didactic phase, followed by Clinical Practicum II for two weeks.
Year II consists of the following activities: the 12-week didactic education phase followed by a one
week break and a Clinical Practicum III for 12 weeks; a five week break followed by one 12 week and one
six week didactic period.
Year III (the final phase) consists of Clinical Practicum IV for 12 weeks, followed by four weeks of
elective courses given in the continuing education format. Students will give research presentations to the
faculty and the PT community during this final four weeks on campus.
MPT students will complete their education in May and participate in the University-wide June
graduation. State licensure examinations are now computerized and can be taken following graduation.
The faculty includes scholars, researchers, administrators and clinicians from the professions of physical
therapy, psychology, education, osteopathy, medicine and from the basic sciences. All faculty are
committed to the preparation of the Master of Physical Therapy professional who will be well versed in all
aspects of physical therapy and dedicated to their profession and to the patients they serve.
TECHNICAL GUIDELINES FOR ADMISSION AND MATRICULATION
A candidate for admission to the MPT program must have the use of certain sensory and motor
functions to permit them to carry out the activities described in the sections that follow. Graduation from
the program signifies that the individual is prepared for entry into clinical practice. Therefore, it follows
that graduates must have the knowledge and skills needed to function in a broad variety of clinical
situations and to render a wide spectrum of physical therapy evaluation and treatment techniques. The
candidate and student must be able to consistently, quickly, and accurately integrate all information
received by whatever sense(s) are employed. Also, they must have the intellectual ability to learn,
integrate, analyze, and synthesize data.
Examples of essential functions of a physical therapist include, but are not limited to:
a. Use appropriate verbal, non-verbal, and written communication with patients, families, and others.
b. Determine the physical therapy needs of any patient with potential movement dysfunction.
c. Safely, reliably, and efficiently perform appropriate physical therapy procedures used to assess the
function of the movement system.
d. Perform treatment procedures in a manner that is appropriate to the patient's status and desired
goals.
A candidate for MPT ordinarily must have abilities and skills of five varieties including (1)
observation; (2) communication; (3) motor; (4) intellectual, conceptual, integrative and quantitative; and
(5) behavioral and social. Where technological assistance is available in the program, it may be permitted
for disabilities in certain areas. Under all circumstances, a candidate should be able to perform all physical
therapist functions at entry-level competency in a reasonably independent, timely manner.
1. Observation: Candidates and students ordinarily must have sufficient vision to be able to observe
demonstrations and laboratory exercises. They must be able to observe a client accurately at a distance
and close at hand.
2. Communication: Candidates and students ordinarily must be able to communicate with clients and
colleagues. They should be able to hear, but if technological compensation is available, it may be
101
permitted for some people with disabilities in this area. Candidates and students must be able to read,
write, and communicate verbally in English.
3. Motor: Candidates and students ordinarily should have sufficient motor function such that they are
able to execute movements reasonably required to provide assessment and physical therapy treatment
procedures to clients.
Examples of reasonable required assessment procedures include, but are not limited to:
a. Functional abilities
b. Pain
c. Gait
d. Strength
e. Balance
f. Movement patterns
Examples of reasonably required treatment procedures include:
a. Balance training
b. Exercise techniques
c. Gait training
d. Activities of daily living training and functional activities
These actions require coordination of both gross and fine muscular movements, equilibrium and
functional use of the senses of touch and vision. The role of the physical therapist often requires upright
posture with sufficient upper and lower extremity strength, as well as overall body strength; therefore,
individuals with significant limitations in these areas would be unlikely to succeed.
4. Intellectual, Conceptual, Integrative, and Quantitative Abilities: These abilities include measurement,
calculation, reasoning, analysis, and synthesis. Problem solving, the critical intellectual skill demanded
of a physical therapist, requires all of these intellectual abilities. In addition, candidates and students
should be able to comprehend three-dimensional relationships and understand the spatial relationships
of structures.
5. Behavioral and Social Abilities: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgment, the prompt completion of
all responsibilities attendant to the assessment and care of clients, and the development of mature,
sensitive, and effective relationships with clients. Candidates and students must be able to tolerate
physically taxing workloads, adapt to changing environments, display flexibility, and learn to function
in the face of uncertainties inherent in the clinical problems of many clients. Compassion, integrity,
concern for others, interpersonal skills, interest, and motivation are all personal qualities to be assessed
during the admissions and educational processes.
The MPT program, along with all other programs at Western University of Health Sciences, shares a
commitment to develop creative ways of opening the MPT curriculum to competitive, qualified disabled
individuals. In doing so, however, the MPT program must maintain the integrity of its curriculum and
preserve those elements deemed essential to educating candidates to become effective physical therapists.
ADMISSIONS POLICIES AND PROCEDURES
Western University will accept applications for admission from all qualified candidates. Western
University is committed to admitting competitive, qualified disabled individuals. For technical guidelines,
please see above.
Application Requirements
The applicant must have earned a BA or BS degree from a regionally accredited college or university
by the time he/she matriculates in the MPT program. The minimum acceptable grade point average in
overall science and in the baccalaureate degree is 2.5 on a 4.0 scale. Exception: the undergraduate GPA
requirement of 2.5 will be waived for applicants who have attained a GPA of 3.0 or above in 15 or more
post-graduate units or who have been awarded a master's degree with a minimum GPA of 3.0.
The MPT program is looking for students who come from a broad, liberal arts background with the
baccalaureate degree being obtained in any field of study other than physical therapy. A high degree of
intellectual curiosity and accomplishment along with excellent verbal and written communication skills
102
need to be evident in the applicant. The graduate of Western University will be able to problem-solve in
clinical practice and will also be able to communicate appropriately with the client about the client/patient
care plan.
1.Prerequisite Courses
English Composition - 1 course (minimum of 3 semester units or 4 quarter units)
Psychology - 2 courses, must be out of the Psychology Department (minimum of 3 semester units
each or 4 quarter units each)
Statistics - 1 course, only statistics courses that are cross listed in math, statistics or biometry will
be accepted (minimum of 3 semester units or 4 quarter units)
Human Anatomy - 1 course of lecture and lab (minimum of 4 semester units or 6 quarter units)
Human Physiology - 1 course of lecture and lab (minimum of 4 semester units or 6 quarter units)
General Chemistry - a full course sequence of lecture and lab (minimum of 8 semester units or 12
quarter units)
Physics - a full course sequence of lecture and lab – emphasis on light, heat, sound, and electricity
(minimum of 8 semester units or 12 quarter units)
Anatomy and Physiology must be taken out of the Anatomy, Physiology, A&P, Biology or Zoology
departments. The Anatomy and Physiology must be "human." Combined Anatomy and Physiology courses
will be considered only if a combined course sequence is completed.
Grades of "C" or better are required in each prerequisite course. A grade of "C-" in any prerequisite
course is not acceptable. No prerequisite course work may be taken on a pass/no pass or credit/no credit
basis. For courses completed in California, all science prerequisites must be University of California (UC)
or California State University (CSU) transferable.
Three prerequisite courses may be in progress at the time of application during the spring, summer or
fall semester or quarter. Please submit official transcripts directly to the Admissions office upon
completion of course work in progress. Final transcripts and/or final grades (including degree verification)
for all course work in progress must be received prior to registration date in January.
2. Graduate Record Examination (GRE) Score Report
Official GRE Score Report must be mailed directly to Western University from Educational Testing
Service (ETS).
3. Clinical Experience
Credit will be given for up to 500 hours of volunteer or work experience in a variety of physical
therapy settings. Extra credit will be given for different types of settings, provided that at least 100 hours is
spent in each setting. Types of settings may include acute hospital, outpatient, rehabilitation, pediatric and
home health. Preference will be given to applicants who have experience at more than one setting.
4. Recommendations
Three satisfactory recommendations (forms provided) are required as part of the admissions
application. We require one academic recommendation, one from a physical therapist, and the third
recommendation may be academic or from a physical therapist.
Application Procedures and Deadline
The MPT program has a January matriculation date. The application postmark deadline is September 1.
The Department of Physical Therapy will make admissions decisions on a rolling basis. They will review
applications, conduct interviews and make admissions decisions throughout the admissions cycle. We
encourage students with complete application packets to apply early. Applicants who cannot attend and
wish to reapply for the following year will be considered with the new applicant pool.
To request an information brochure and/or an application, contact the admissions office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street
Pomona, CA 91766-1854
(909) 469-5541
In addition to submitting an application, the applicant must submit a non-refundable application fee of
$60, three letters of reference, academic/professional record form, work experience form, a written
103
personal statement, and official transcripts from all colleges attended. After receipt of the packet, the
Admissions Office will evaluate the applicant's transcripts to ascertain the science and baccalaureate grade
point average.
Applicants who wish to use course work completed outside of the United States must submit their
transcripts for evaluation to World Education Services, Josef Silny and Associates, Educational Credential
Evaluators, Inc., or International Education Research Foundation, Inc. A course-by-course evaluation is
required and all course work must be designated as undergraduate, graduate or professional. Western
University will only honor evaluations from the above services. The evaluation must be included with the
application packet.
The Admissions Committee reserves the right to select potential candidates for personal interviews.
These interviews are designed to allow the applicant to learn more about Western University's MPT
program as well as allow the Admissions Committee to learn about the applicant. The interview process is
typically held during July and August.
Decisions of the Admissions Committee regarding the admission of applicants to the Master of
Physical Therapy program are final.
Registration
First-year and second-year MPT students are required to register in person on the registration day in
January. Final phase (Year III) students must register before leaving campus at the end of Year II. Failure
to register may be grounds for dismissal. Full tuition and fees and all prior debts must be paid in full on or
before the registration deadline each academic year. Matriculation is subject to satisfactory completion of
all academic requirements and payment of all outstanding debts to the University. Prior to registration, the
receipt of final transcripts from undergraduate colleges, a physical examination, and immunizations as
outlined on the physical examination form, are additional requirements for incoming students. Attendance
at Orientation Day is also mandatory for incoming first-year students.
TUITION AND FEES
By action of the Board of Trustees, the tuition and fees effective January 1, 2002, (subject to change)
are as follows:
*$1,250 Tuition Deposit for incoming students
(Payable two weeks after acceptance)
**$500 Enrollment Deposit
(Students returning from leave of absence only -
Due by October 15)
$26,375 Total Tuition Annual
$8,790 Final Phase - Year III
$40 Student Body Fee, year I and II MPTs,
covers student council, social activities, public relations.
$20 Student Body Fee, final phase MPTs.
*Upon matriculation, the entire $1,250 is applied toward the total tuition.
**For accepted candidates who are students returning from leave of absence, a $500 enrollment deposit
is due October 15 prior to enrollment. The deposit is nonrefundable and credited toward tuition upon
enrollment.
Tuition and fees are subject to change without notice upon approval by the Board of Trustees. All the
above-listed fees are mandatory for each student and are nonrefundable.
Other Fees and Expenses
$500 Required and Recommended Texts
$10 (per day) Late Registration Fee
$40 Lost Locker Key
$10 Lost ID Badge
$5 (each) Copy of Official Transcript
104
$10 (each) Copy of Official Transcript Faxed
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
ACADEMIC REQUIREMENTS
Academic Advisement Policy
Students will be assigned a faculty advisement upon matriculation. Advisement by faculty should be
viewed by the student as a part of the academic process. If either the student or faculty member does not
find the relationship helpful, either is free to seek a change. This request should be made to the
Department Chair.
It is the student’s responsibility to meet periodically with his/her advisor. A student on probation must
meet with his/her faculty advisor at least once a month.
Standards of Academic Performance
Good academic standing implies that a student maintained a minimum GPA of 2.70 or higher.
All grading and evaluation is based on the student's ability to attain the competencies within the
objectives outlined for each area of study.
A student whose performance falls below the minimum acceptable standard(s) for any area of study
will be notified of such deficiency by the instructor of the course and Department Chairperson as soon as
evidence of such substandard performance is available.
Grade Scale/Grade Points/Class Ranking
The following academic standards and grading scale applies to students enrolled in the Physical
Therapy Program:
Percentage Letter Grade Grade Points
93 - 100 A Excellent 4.0
90 - 92 A- Excellent 3.7
87 - 89 B+ Good 3.3
83 - 86 B Good 3.0
80 - 82 B- Good 2.7
77 - 79 * C+ Passing, but below required overall GPA 2.3
73 - 76 * C Passing, but below required overall GPA 2.0
Below 73 U Unsatisfactory 0
NCr No Credit 0
Cr Credit 0
I Incomplete 0
M Missing 0
Au Audit 0
W Withdrawal 0
* A "C" or "C+" grade in and of itself is a passing grade. However, a "C" or "C+" grade is below the
required overall grade point average of 2.7. If the number of "C's" and "C+'s" totals an amount to bring the
student's GPA to below 2.7, then this is not satisfactory performance based on professional expectations.
Clinical Practica Grades Cr Satisfactory Performance/Completion
of clinical practicum assignment
NCr Unsatisfactory Performance/Completion
of clinical practicum assignment
The class ranking is computed at the end of each graded module, based upon overall GPA.
105
Credit Hours
Courses are rated at one credit hour for each 12 hours of lecture or 24 hours of laboratory and/or
practice sessions. Credit hours of 1.0 will be assigned for each week of Clinical Practica experience (i.e.,
Clinical Practicum I is two weeks and receives 2 credits). A cumulative grade point average will be
calculated and posted on the transcript. Class ranking is also computed and will appear on the transcript at
the student's request only. Class ranking is also available upon request in the Registrar's Office.
The grade point average will be calculated at the end of each module and if a course is repeated, only
the last grade earned enters into the computation of the grade point average, but the original grade remains
on the student's transcript.
Official grades are turned in to the Registrar from the Department Chairperson, at which time official
grade reports are deposited in the student mail lockers. Enrolled students will receive an unofficial copy of
their transcript in July and January of each academic year.
No course grade will be changed unless the instructor certifies in writing to the Registrar that an error
in computing or recording the grade occurred. If the student believes there is just cause to dispute a grade
for a course, the procedure is as follows:
a. If, following distribution of unofficial transcripts in the student's locker, the student has reason to
dispute the grade, it should be done in writing within five (5) working days to the Department of
Physical Therapy Education Chairperson. Upon written request from the student, the Department
Chairperson shall review the case with the instructor(s) and a decision shall be made by the course
instructor(s) to affirm or modify the grade. Within seven (7) working days the Department Chairperson
shall notify the student in writing of the decision. A copy of the letter shall be sent to the appropriate
faculty member(s). The faculty member(s) has the sole responsibility to make the official grade
change.
b. If the student is not satisfied with the outcome of the grade dispute procedure to the Department
Chairperson, the student may then appeal in writing to the Dean of the College of Allied Health
Professions within five (5) working days. The Dean of the College of Allied Health Professions shall
review the case with the student, Chairperson of the Department of Physical Therapy Education and the
course instructor(s) and a decision shall be made by the course instructor(s) to affirm or modify the
grade. Within seven (7) working days the Dean shall notify the student in writing of the decision. A
copy of the letter shall be sent to the appropriate faculty member(s) and Chairperson. The faculty
member(s) has the sole responsibility to make the official grade change.
Evaluation
a. General: The Modules of the program are designed so that students' work toward achievement of
competencies is measured by written and practical examinations and by evaluations of clinical
performance and professional development. Specific behavioral objectives are defined for each
modular component to assist the students and the faculty members in evaluating the degree of
attainment of the objectives throughout the 28-month curriculum.
b. Evaluation Methods: Overall student performance is evaluated during each phase using one or a
combination of the following methods:
1. Written examinations: Written examinations will vary based on the content of the individual
course. A combination of multiple choice, matching, true/false, short answer, essay and patient
problem solving questions are used.
2. Practical or Laboratory Examinations: In selected courses, students will be observed
performing components of physical therapy practice activities on lab exams. They also may be
asked to "problem solve" based on a patient database, and in some cases students will be
videotaped for self-evaluation.
3. Student Presentations: Students may be asked to orally present individual or group projects,
patient cases, research papers, etc. These oral presentations may or may not be accompanied by a
written report.
4. Written reports: At various times, students will be evaluated on written reports of assigned
topics, SOAP notes, evaluations, treatment plans and home programs.
5. Clinical Evaluations: Supervising Clinical Instructors are asked to assess the student's level of
attainment of competencies related to selected parameters within the domains of knowledge, skills
and attitudes, and to evaluate the student's overall performance while on Clinical Practica. The
106
Clinical Performance Instrument (CPI), which incorporates entry-level physical therapist clinical
performance criteria, is utilized.
Students are responsible for securing their CPI or other evaluation tools from the Center
Coordinator of Clinical Education/Clinical Instructor (CCCE/CI) on each practicum and ensuring
that it is completed and returned to the Director of Clinical Education after each practicum.
CCCE/CI's are encouraged to discuss the student's performance and progress throughout the
clinical assignment and to discuss the final evaluation prior to completion of the practicum. The
CI will indicate whether the Clinical Practicum was a successful experience in accordance with
designated objectives, or was unsuccessful in meeting clinical objectives. While the CI may
recommend success or failure of the Clinical Practicum, the Director of Clinical Education
determines and administers the actual course grade.
c. Grade Reports: Final grade reports are issued at the completion of each module and will be placed in
student lockers.
Due to the nature of the curriculum, modular completion dates do not coincide with traditional
grading periods.
In some courses when final grades are not available at grade reporting time, a grade of "M"
(Missing) is submitted to the Registrar in lieu of the course grade. "M" grades are entered on the grade
reports and are converted to student achieved grades at the earliest possible opportunity. An up-to-date
summary of student performance is maintained in the Department Office and is available to each
student for review.
d. Review of Examinations: Examinations are graded as soon as possible and are kept on file for
student review. Student performance in clinical courses is monitored closely by the Director of Clinical
Education. Students whose performance in any portion of the curriculum is determined to be
unsatisfactory are notified of such substandard performance as soon as it can be determined.
Professional Performance
a. Ability-based Assessment: The faculty supports the concept of development of professional
behaviors throughout the program. These behaviors include: (1) commitment to learning; (2)
interpersonal skills; (3) communication skills; (4) effective use of time; (5) use of constructive
feedback; (6) problem solving; (7) professionalism; (8) responsibility; (9) critical thinking; and (10)
stress management.
Professional behavior is vital to the success of each student, the Western University Physical
Therapy program, and the Physical Therapy profession. The process of becoming an effective physical
therapist involves attaining competency in professional knowledge, skill, and behavior. Thus, the ten
generic abilities that exemplify the professional behaviors valued by the physical therapy profession
will be used as a guide throughout this program. To facilitate development of competency in the
generic abilities, the faculty will provide the students opportunities to practice them and formal and
informal feedback throughout the program. The student will be responsible for ongoing self-
assessment and for seeking feedback from faculty and fellow students.
Students’ progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behavior and attitudes. At the completion of
each module/year of the program, before the student is allowed to progress to the next module/year, the
student’s record of achievement is reviewed by the faculty. The quality of professional behavior
expected of Western University MPT graduates is exemplified by the generic abilities and the three
levels of associated behavioral criteria. Satisfactory progress is demonstrated by exhibiting beginning-
level criteria by the end of the first year, developing-level criteria by the end of the second year, and
entry-level criteria by the end of the final clinical practicum.
The faculty determines if the student has demonstrated the knowledge, skills, and attitudes
necessary to be eligible for progress for the next module/year. In special instances, the faculty may be
convened at other than scheduled times to consider cases of unusual circumstances, such as
probationary or dismissal cases.
b. Attendance: Students are expected to attend all scheduled activities and observe the following
policies:
107
Excused Absences
1. All unanticipated absences due to illness, accident, other unexpected events must be reported
immediately to the department secretary and course instructor.
2. Absences requested for physician/dentist appointments for student or dependents will be
considered excused only if requested in advance of the appointment. Due to the intense nature of
the curriculum, students are encouraged strongly to schedule appointments for days when classes
are not held, evenings, or Saturdays.
3. All anticipated absences for any reason, regardless of length, must have the prior approval by
the Faculty to be considered excused.
4. Students on Clinical Practica are responsible for notifying their supervising CI, CCCE, and the
Director of Clinical Education regarding all absences, whether anticipated or unanticipated.
Unexcused Absences
1. Any discovered or reported absence for which the Chairperson/Faculty does not have an
explanation will be considered unexcused.
2. Students whose absence is determined to be unexcused will be required to provide an
explanation regarding the circumstances involved. The Chairperson/Faculty will determine if the
absence remains unexcused.
3. Unexcused absences may be sufficient cause for placing a student on professional probation
and continued unexcused absences may be grounds for dismissal from the program.
4. Absences on the first or last day of a module or Clinical Practicum, or on the day before or
after a scheduled break, vacation, or weekend, are considered unexcused unless prior written
approval has been granted. If such an absence is the result of a sudden unavoidable circumstance,
the Department Chairperson should be notified as soon as possible and provided with an
explanation for the absence.
c. Student Examination Policy
1. Students are not to communicate in any way during examinations and are to face the front of
the classroom at all times.
2. During scheduled examination hours, students are highly discouraged from going to the
bathroom, but will be allowed to go one at a time. Student will be required to turn in the exam
and Scantron® sheet as he/she leaves the room.
3. Once a student finishes an exam, the student will turn in the exam and the Scantron® form to
the proctor, and after he/she leaves the examination room, he/she will not be permitted to re-enter
the room until the exam is declared over.
4. All students' belongings, i.e., notebooks, calculators, and headsets, etc., will be kept in front of
the room.
5. Questions will be answered at the discretion of the proctor during the examination period.
Students should be permitted to point out typographical or other errors present in the examination
to the proctor.
6. Alternate seating shall be utilized for all examinations unless precluded by space availability.
7. Violations of these examination policies or of Standards of Professional Conduct will be
brought before the Student Conduct Committee.
Student Academic Progress Committee
a. The Student Academic Progress Committee of the College of Allied Health Professions is
comprised of Department Chairs, the Dean of Student Affairs/Registrar and elected faculty members.
b. Each year, the Student Academic Progress Committee shall review as needed the academic
achievements and the performance of all students. The names and grades of students in academic
difficulty shall be made available to the Student Academic Progress Committee by the Department.
c. After reviewing a student’s achievement and performance records, the Student Academic Progress
Committee may recommend to the Dean of Allied Health Professions any of the following courses of
action for a student: Promotion, probation, remediation, dismissal from the University, psychological
and educational assessment and recommendation, or no action.
108
d. The Student Academic Progress Committee also has the responsibility of recommending to the
Faculty as a whole the awarding of the degree of Master of Physical Therapy upon satisfactory
completion of all requirements for graduation as stated in the Catalogue.
e. All recommendations of the Student Academic Progress Committee shall be made in writing to the
Dean of Allied Health Professions, who will make a final decision and inform the student in writing.
Promotion
Promotion is defined as progression from one academic year to the next.
a. A student will be recommended to the Dean of the College of Allied Health Professions for
promotion by the Student Academic Progress Committee.
b. A student may not be recommended for progression from one academic year to the next with any
outstanding grades of “I” or “U” on his/her academic record or with a yearly grade point average of
less than 2.7.
c. When considering a student for promotion, professional, ethical, and personal conduct may also be
taken into consideration.
d. A student will be promoted provided that all legal and financial requirements of the University as
stated in the Catalogue have been satisfied.
Graduation
A student will be recommended for the degree of Master of Physical Therapy provided he/she:
a. Has satisfactorily completed two years and four months education at the University in the MPT
curriculum.
b. Is not on probation and has completed all prescribed academic and clinical education requirements
with a cumulative grade point average of at least 2.7 and has no outstanding grade of “I” or “U,” or
“NCr” in a required course.
c. Has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined
previously.
d. Has complied with all the legal and financial requirements of the University as stated in the
Catalogue.
e. Unless special permission has been granted by the President of the University, all students must
attend in person and participate in the Commencement program at which time the degree is conferred.
If the President grants special permission to be excused from graduation, the graduate may be required
to present himself or herself to the Provost or appropriate Dean at a later date in order to take the
required oath (if relevant) to receive his or her diploma.
Academic Warning
The student who demonstrates unacceptable performance in any unit of study during any portion of the
program is notified of such performance by the Instructor of the course, as well as the Department
Chairperson, in writing, as soon as it becomes evident. This constitutes an academic warning. Continued
poor academic performance can lead to academic probation and/or dismissal.
Academic Probation
a. Unsatisfactory or No Credit Course Grades
"U" or “NCr” in any required course constitutes a failing grade, and places the student on academic
probation, requiring that the course be remediated or retaken based upon the recommendation of the
course instructor. A grade of “U” or “NCr” in a required course will prevent participation in a clinical
practicum until the course is successfully remediated and requires that the ACCE determine an
appropriate clinical placement.
1. As in all cases in which remediation of a course is required, this requirement may extend the
length of the program beyond 28 months.
2. The highest grade a student may achieve by obtaining a 73 percent or higher score through
remediation of a course is a grade of "C" or “Cr”. The "C" or “Cr” grade achieved by remediation
of a course will be recorded on the official transcript beneath the original course grade of "U"
(Unsatisfactory) or “NCr” (No Credit).
109
3. Failure to earn a grade of “C" or “Cr” when remediation of a course is attempted will render the
student subject to dismissal from the program.
4. If a student repeats a course the next time that course is offered in the MPT curriculum, the
student will have that new grade for the course recorded on the official transcript beneath the
original course grade of "U" (Unsatisfactory) or “NCr” (No Credit).
5. Failure to earn a grade of "C" or higher or “Cr” on repeating a course of study will render a
student subject to dismissal from the program.
6. A third "U" or “NCr” in required coursework in the program will render a student subject to
dismissal from the program.
b. Module/Overall GPA
1. Students must attain a modular GPA of 2.7 and maintain an overall GPA of 2.7. The module
GPA and overall GPA will be calculated at the end of each Module.
2. A student whose modular or overall GPA falls below 2.7 must meet with the Department
Chairperson and the ACCE. In order to closely monitor clinical performance, the ACCE will
determine the subsequent clinical placement.
3. If the modular or overall GPA falls below 2.7, a student will be placed on academic probation
immediately. Length of academic probation will be determined by the Dean of the College of
Allied Health Professions.
4. If a student attains a modular GPA below 2.7 in two consecutive modules the student will be
subject to dismissal from the program.
Tutorial Assistance Program
A Tutorial Assistance Program (TAP) has been established at the University to assist students
experiencing academic difficulty. Students will be recommended for this program by a faculty advisor or
professor. The tutors will be chosen from the student body on the recommendation of the faculty of record
for the class.
General Procedures
a. The student may request a tutor by:
1. contacting the course instructor and/or the Department Chairperson,
2. contacting his/her advisor or,
3. going directly to the Learning Enhancement and Academic Development (LEAD) Office.
Student requests will be reviewed by the course instructor and/or the Department Chairperson. Upon
approval, the student will be deemed eligible for services under TAP. Five hours per course is the
maximum number of hours for which a student may be tutored per week.
b. The course instructor may recommend that the student seek a tutor, based upon a poor performance
on a single exam or poor cumulative score.
c. The student’s advisor may recommend that the student seek a tutor, based upon any knowledge he or
she may have about the student’s academic difficulty. In addition, the advisors will receive copies of
letters from the Chairperson to students having academic difficulty.
d. To initiate tutoring following a recommendation or student request for tutoring, the student follows
these steps:
1. The student obtains from the LEAD Office a list of names of tutors available for the course in
which the student is having problems.
2. The student is assigned a tutor by the LEAD Director from the list of available tutors.
3. Once assigned, the tutor and tutee meet with the course instructor to discuss the student’s
specific problems. The instructor should make some recommendations as to what areas the tutor
should emphasize.
4. The tutor and student arrange mutually agreeable times for the tutoring sessions.
5. The tutor must have the course instructor sign the time sheet before it is turned in to the LEAD
Office.
A student may obtain up to five hours of tutoring per course per week during the module. By example:
A Year I MPT student may be tutored in Anatomy I and Kinesiology I for a total of 10 hours per week
during the module. Generally, tutoring begins after a student has received grades at 73 percent or lower on
an exam. The student may continue to be tutored for a course until he/she has obtained a B- (80%), or
110
higher average grade for the course. As the student moves into Module V, the student may qualify for up
to 20 hours of tutorial assistance per week (three musculoskeletal courses plus Research Design II). Any
time a student has received 73 percent or less on an exam, the student, faculty member or student’s faculty
advisor may immediately request tutorial assistance.
Modified Year I MPT Curriculum
The MPT program offers Modified Year I curriculum for students experiencing academic difficulties or
students with disabilities. This modified program is a three-year and four-month curriculum in which the
first year standing curriculum is spread over a two-year period. Guidelines for this program include:
a. Potential candidates for the Modified Year I MPT Curriculum will be identified by the midway
point of Module I after midterm examinations in the following five courses: Anatomy I, Kinesiology I,
PT Science I, PT Science II, and Physiology.
b. The Modified Curriculum is not an option unless the student manifests serious academic problems
by the midway point of Module I.
c. Recommendation of individual students for the Modified Curriculum shall be made through the
Dean of the College of Allied Health Professions by recommendations from the Department of Physical
Therapy Education Faculty and the College of Allied Health Professions, Student Academic Progress
Committee.
d. The decision to enter the Modified Curriculum is a onetime student option.
e. At the time the student opts for the Modified Curriculum, the modified curriculum will be based
upon courses in which the student is receiving satisfactory grades by midterm of Module I. The
Modified Curriculum will be outlined for the student, so that Year I of the MPT curriculum will be
taken over two years. As the student enters Year II of the curriculum, it is expected that the student
would attend all classes and clinical assignments as defined in the standard curriculum.
f. The student's progress will be monitored carefully each module by the Department Chairperson for
the Department of Physical Therapy Education, College of Allied Health Professions Student
Academic Progress Committee, and the Dean of the College of Allied Health Professions.
g. Students admitted to this program will pay two years, four months consecutive years of tuition and
mandatory fees, and only mandatory fees for the additional year in the curriculum.
Professional Probation
Violations of the Standard of Professional Conduct will be dealt with as described under the General
University Academic Policies and Regulations of this catalogue.
Dismissal
A student may be subject to dismissal from the program for substandard academic or professional
performance, as follows:
a. A second grade of "U" or “NCr” in the same required course;
b. A third grade of "U" or “NCr” in required courses in the program;
c. Unacceptable performance on more than one of the clinical practica;
d. Lack of professional or personal attributes considered appropriate for continuance in the program
and profession;
e. Any event that could result either in academic or professional probation for a student currently on
academic or professional probation;
f. Violation of the terms of probation as stated in a letter at the time the student is placed on probation.
Exemption from Individual Course
Students with advanced work or degrees in a particular subject formally may petition the instructor and
the Department Chairperson for credit for an individual course. The petition must include the reasons for
the request and all necessary documentation and must be submitted by the end of the first week of the
course. The student must comply with the attendance policy until notification that exemption has been
granted by the Dean, based upon recommendation of the Department Chairperson. The instructor, before
recommending exemption, may require acceptable performance on an examination. The instructor, in
111
consultation with the Department Chairperson, may suggest other alternative or additional criteria for
determining exemption.
Confidentiality of Medical Records and Health History Information
All data gathered about patients and their illnesses, including all items within patients’ medical histories
are privileged information.
a. Students should not discuss patients’ records in a manner or a situation that would reveal any
information about these patients or their records to persons not involved in their health care.
b. Charts or contents, e.g., lab reports, etc., are not to be removed from the hospital or clinical setting.
Use of Physical Therapy Equipment and Laboratories
The DPTE policy for use of the PT equipment in the PT Skills Laboratories is as follows: No one is to
use the PT equipment except MPT students who have received education and have had practice on the
equipment in the laboratory. These MPT students must be checked out by a faculty member as being
competent to use the equipment. MPT students using the equipment should be doing so in conjunction
with a class they are taking, or in preparation for a clinical practicum, or to conduct a clinical research
project. If equipment is used for a research project, the MPT faculty advisor will be responsible to check
out student competency in using the equipment.
Physical Therapy skills and research labs may be used after regular class hours, with permission of the
Department Chair. Use of these facilities must be scheduled with the Department Chair five (5) working
days in advance of the intended date of use.
CURRICULUM ORGANIZATION
The MPT curriculum is continually evaluated to assure the best educational experience and outcomes.
With this consideration, the following is an outline of curriculum organization.
Year I
Course number Semester Hours
Module I - 15 Weeks
PT 5000 Psychosocial Aspects of Health Care 3
PT 5010 Today's Health Care System 2
PT 5030 Anatomy I 6
PT 5050 Kinesiology I 3
PT 5070 Physical Therapy Science I 2
PT 5075 Physical Therapy Science II 3
PT 5100 Physiology 4
Total 23
Module II - 11 Weeks
PT 5020 Medical Terminology & Documentation 1
PT 5035 Anatomy II 5
PT 5055 Kinesiology II 3
PT 5080 Physical Therapy Science III 3
PT 5120 Human Life Sequences 2
PT 5130 Research Design I 2
PT 5141 Preparation for Clinical Practicum I 1
Total 17
Module III - 2 Weeks
PT 7010 Clinical Practicum I 2
Total 2
Module IV -15 Weeks
PT 5135 Research Design II 2
PT 5142 Preparation for Clinical Practicum II 1
112
PT 5200 Foundations of Musculoskeletal Intervention 4
PT 5205 Evaluation and Treatment of Upper Quarter
Musculoskeletal Problems 5
PT 5210 Evaluation and Treatment of Lower Quarter
Musculoskeletal Problems 6
PT 5220 Principles of Teaching and Learning 2
PT 5230 Role of Physical Therapy in Clinical
Medicine Problems 4
Total 24
Module V - 2 Weeks
PT 7020 Clinical Practicum II 2
Total 2
Year II
Module VI - 12 Weeks
PT 5143 Preparation for Clinical Practicum III 0.5
PT 6000 Neuroanatomy 4
PT 6005 Neurophysiology 4
PT 6010 Evaluation and Treatment of Neurologic
Disorders 8
PT 6020 Principles of Electrotherapeutic
Evaluation and Treatment 4
Total 20.5
Module VII - 12 Weeks
PT 7030 Clinical Practicum III 12
Total 12
Module VIII - 12 Weeks
PT 5144 Preparation for Clinical Practicum IV 0.5
PT 6030 Physiology of Exercise 4
PT 6040 Evaluation and Treatment of the
Cardiopulmonary System 4
PT 6050 Principles of Administration and Management 3
PT 6060 Prosthetics, Orthotics and Gait 3
PT 6070 Prevention and Management of Problems in
the Aging Adult 3
PT 6200 Applied Research II 1
Total 18.5
Module IX - 6 Weeks
PT 6075 Prevention and Management of Problems in
the Pediatric Patient 3
PT 6100 Rehabilitation: The Neuro-Musculoskeletal
and Cardiopulmonary Systems 5
Total 8
Final Phase (Year III)
Module X - 12 Weeks
PT 7040 Clinical Practicum IV 12
Total 12
Module XI - 4 Weeks
PT 6500 Electives 4
113
PT 6210 Applied Research II 1
Total 5
Graduation - Total Semester Hours 144
CURRICULUM
Course Descriptions and credit hours
All courses are awarded letter grades, except when indicated otherwise.
PT 5000 Psychosocial Aspects of Health Care (3 credit hours)
(Formerly PT 500)
Prerequisite: Acceptance to program. Introduction to the psychological and sociological effects of
acute, chronic, terminal, traumatic and congenital medical problems on the patient, family and therapist;
communication skills including interviews, verbal and non-verbal communication.
PT 5010 Today's Health Care Systems (2 credit hours)
(Formerly PT 501)
Prerequisite: Acceptance to program. World and national factors that affect today's health care systems,
who gets care and how it is paid for, legal and ethical responsibilities of health care providers, role of
physical therapy, the team approach, and the professional organization.
PT 5020 Medical Terminology and Documentation (1 credit hour)
(Formerly PT 502)
Prerequisite: Acceptance to program. Medical terminology and appropriate abbreviations used for
patient care documentation. Survey of basic skills of written communication in areas of patient evaluation,
treatment notes and discharge summaries. Introduction to the concepts of impairments, disabilities and
handicaps, and how the concepts apply to documentation and patient problem solving. May require some
clinical observations.
PT 5030 Anatomy I (6 credit hours)
(Formerly PT 503)
Prerequisite: Acceptance to program. Two courses of normal human anatomy including upper and
lower extremities, trunk and neck; cadaver dissection. Emphasis on neuromusculoskeletal and
cardiopulmonary systems. Lecture and laboratory.
PT 5035 Anatomy II (5 credit hours)
(Formerly PT 504)
Prerequisite: PT 5030. Continued from Module I. Lecture and laboratory.
PT 5050 Kinesiology I (3 credit hours)
(Formerly PT 505)
Prerequisite: Acceptance to program, concurrent enrollment in or successful completion of PT 5030.
Introduction to biomechanics, theoretical principles and clinical application of these principles to the joints
and muscles of the upper quarter. Emphasis is on normal function, but pathokinesiology is addressed to
introduce clinical relevance. Lecture and Laboratory.
PT 5055 Kinesiology II (3 credit hours)
(Formerly PT 506)
Prerequisite: PT 5030, 5050, and concurrent enrollment in PT 5035. Continued from Module I, and
applied to the lower quarter. Includes analysis of open and closed chain kinematics of the lower extremity.
Observation skills and analysis of normal gait are emphasized. Lecture and laboratory.
114
PT 5070 Physical Therapy Science I (2 credit hours)
(Formerly PT 507)
Prerequisite: Acceptance to program. Introduction to the physical therapy skills of transfers, gait
training, bed mobility, wheelchair selection and management, cushions, range of motion and monitoring of
physiological responses. Lecture and laboratory.
PT 5075 Physical Therapy Science II (3 credit hours)
(Formerly PT 508)
Prerequisite: Acceptance to program. Application of sterile technique and universal precautions,
physiologic principles and applications of heat and cold modalities, ultrasound, massage and hydrotherapy.
Lecture and laboratory.
PT 5080 Physical Therapy Science III (3 credit hours)
(Formerly PT 509)
Prerequisite: PT 5030, concurrent enrollment in PT 5035. Basic skills of manual muscle testing, gait
and postural evaluation. Practice on real and simulated patients. May require some clinical observation.
Lecture and laboratory.
PT 5100 Physiology (4 credit hours)
(Formerly PT 511)
Prerequisite: Acceptance to program. Human physiology with emphasis on the various body systems.
PT 5120 Human Life Sequences (2 credit hours)
(Formerly PT 510)
Prerequisite: PT 5100. The developmental process from conception to death with the emphasis on
human motor performance. Sequence of study includes fetal life, infancy, early and middle childhood, late
childhood, adolescence, early and middle adulthood, and the aging adult including: neuroanatomical and
neurophysiological mechanisms in relationship to developmental changes in performance, and
musculoskeletal development in relationship to the human life span.
PT 5130 Research Design I (2 credit hours)
(Formerly PT 512)
Prerequisite: Acceptance to program. Application of research methods to clinical studies. Examines and
explains the process of testing and improving what health professionals do to and for clients or patients.
PT 5135 Research Design II (2 credit hours)
(Formerly PT 513)
Prerequisite: PT 5130. Guided instruction in the development, planning and writing of a proposal for a
research project. Cr/NCr only.
PT 5141 Preparation for Clinical Practicum I (1 credit hour)
(Formerly PT 514)
Prerequisite: Acceptance to program. This one hour seminar course will offer an introduction to clinical
education in physical therapy to include an overview of the affiliation agreement. Scheduling and
assignment for Clinical Practicum I will also be incorporated herein. Cr/NCr.
PT 5142 Preparation for Clinical Practicum II (1 credit hour)
(Formerly PT 515)
Prerequisite: PT 5141. This one hour seminar course will continue from PT 5141 on various aspects of
clinical education, including expectations of clinical performance and utilization of the evaluation tool.
Scheduling and assignment for Clinical Practicum II will also be incorporated herein. Cr/NCr.
115
PT 5143 Preparation for Clinical Practicum III (.05 credit hour)
(Formerly PT 516)
Prerequisite: PT 5141, 5142. This one hour seminar course will continue from PT 5142 on various
aspects of clinical education including issues of professionalism in the physical therapy field. Scheduling
and assignment for Clinical Practicum III will also be incorporated herein. Cr/NCr.
PT 5144 Preparation for Clinical Practicum IV (0.5 credit hour)
(Formerly PT 517)
Prerequisite: PT 5141, 5142, 5143. This one hour seminar course will continue from PT 5143 on
various aspects of clinical education including the role of the health care team and the licensure process.
Scheduling and assignment for Clinical Practicum IV will also be incorporated herein. Cr/NCr.
PT 5200 Foundations of Musculoskeletal Intervention (4 credit hours)
(Formerly PT 522)
Prerequisite: Satisfactory completion of PT 5020 through 5100. Basic concepts of evaluation and
treatment of musculoskeletal problems are presented to prepare the student for application to specific
regional problems in the later sequenced courses. Content includes the overall process, general pathology,
interpretation of diagnostic testing, trauma and healing, tissue mutability, strengthening, pain modulation,
management of limited problems, strategies for identification of problems, strategies for treatment and
documentation. Lecture and laboratory.
PT 5205 Evaluation and Treatment of Upper Quarter Musculoskeletal Problems (5 credit hours)
(Formerly PT 523)
Prerequisite: Satisfactory completion of PT 5020 through 5100, 5200. Evaluation and treatment of
upper extremity musculoskeletal problems will be approached regionally beginning from distal to
proximal. Content includes subjective interview, physical examination, treatment and documentation of
specific problems of the hand, wrist and forearm, elbow, shoulder and scapula, cervical spine and head.
Lecture and laboratory.
PT 5210 Evaluation and Treatment of Lower Quarter Musculoskeletal Problems (6 credit hours)
(Formerly PT 524)
Prerequisite: Satisfactory completion of PT 5020 through 5100, 5200, 5205. Evaluation and treatment
of lower extremity musculoskeletal problems will be approached regionally beginning from distal to
proximal. Content includes subjective interview, physical examination, treatment and documentation of
specific problems of the foot and ankle, knee, hip, thoracic and lumbar spine and sacroiliac joints. Lecture
and laboratory.
PT 5220 Principles of Teaching and Learning (2 credit hours)
(Formerly PT 530)
Prerequisites: Acceptance to the program. Introduction to the aspects of: 1) verbal and non-verbal
communication, 2) communication with patients and others with respect to learning styles, gender
differences, culture, disabilities, 3) group dynamics and teamwork, 4) learning theories, and 5) the variety
of teaching methods available. Student projects and presentations required.
PT 5230 Role of Physical Therapy in Clinical Medicine Problems (4 credit hours)
(Formerly PT 533)
Prerequisite: PT 5030, 5035, 5100. General medical and surgical disorders, their etiology and clinical
manifestations. General pathological conditions and mechanisms of disease processes; treatment for
selected medical problems, including arthritis, cancer, immune disorders, endocrine disorders and wounds.
PT 6000 Neuroanatomy (4 credit hours)
(Formerly PT 526)
Prerequisite: Acceptance to the program. Normal anatomy and function of the central, peripheral, and
autonomic nervous systems; laboratory with specimens. Lecture and laboratory.
116
PT 6005 Neurophysiology (4 credit hours)
(Formerly PT 527)
Prerequisite: PT 5100. Human neurophysiology with emphasis on normal cellular and systemic
functions of the central and peripheral nervous systems.
PT 6010 Evaluation and Treatment of Neurologic Disorders (8 credit hours)
(Formerly PT 528)
Prerequisite: PT 5030, 5035, 5070, 5080; concurrent enrollment in PT 6000, 6005. Systematic
approach to a variety neurologic problems of the central and peripheral nervous systems. Emphasis is on
the impairments and clinical manifestations of the anatomical lesions, evaluation techniques and
interventions. Lecture and Laboratory.
PT 6020 Principles of Electrotherapeutic Evaluation and Treatment (4 credit hours)
(Formerly PT 529)
Prerequisites: PT 5100, 6000, 6005. Basic concepts in electrical safety and instrumentation, detailed
concepts and applications of electrotherapy introducing principles of electrophysiologic testing and
therapeutic application of electrical stimulation (ES), including strengthening (NMES), re-education, pain
reduction (TENS), tissue repair (ESTR) and iontophoresis. Electrophysiologic testing to include an
introduction to electromyography (EMG), nerve conduction velocity (NCV) and other electrophysiological
tests. Lecture and laboratory.
PT 6030 Physiology of Exercise (4 credit hours)
(Formerly PT 531)
Prerequisite: PT 5100. This course addresses bioenergetics as well as the acute and chronic
physiological responses of the human body during exercise and other special conditions. The physiological
basis of therapeutic exercise is the foundation for this course. Lecture and laboratory.
PT 6040 Evaluation and Treatment of Cardiopulmonary System (4 credit hours)
(Formerly PT 532)
Prerequisite: PT 5030, 5100. Introduction to evaluation and treatment of diseases of the cardio-
pulmonary system; includes physiology and pathophysiology, evaluation methods, treatment methods and
prevention. Lecture and laboratory.
PT 6050 Principles of Administration and Management (3 credit hours)
(Formerly PT 534)
Prerequisite: PT 5010, 5020. Organization and administration of a physical therapy department
including budget considerations, hiring-interviewing techniques, marketing, and medical-legal issues.
PT 6060 Prosthetics, Orthotics, and Gait (3 credit hours)
(Formerly PT 538)
Prerequisite: PT 5030, 5035, 5050, 5055, 5080. Evaluation and application of prosthetic and orthotic
devices to physical therapy clients. Evaluation of abnormal and pathological gait patterns. Lecture and
laboratory.
PT 6070 Prevention and Management of Problems in the Aging Adult (3 credit hours)
(Formerly PT 535)
Prerequisite: PT 5000 through 5120, 5200 through 5230, 6000 through 6020; concurrent enrollment in
PT 6030, 6040, 6050. Systematic, problem solving approach to the geriatric client with emphasis on
prevention, etiology, clinical manifestations, evaluation, treatment and resources.
PT 6075 Prevention and Management of Problems in the Pediatric Population (3 credit hours)
(Formerly PT 536)
Prerequisite: PT 5030, 5035, 5070, 5080, 5100, 5120, 6000, 6005, 6010. Systematic, problem solving
approach to the pediatric client with emphasis on prevention, etiology, clinical manifestations, evaluation
and treatment. Lecture and laboratory.
117
PT 6100 Rehabilitation: The Neuromusculoskeletal and Cardiopulmonary Systems (5 credit hours)
(Formerly PT 537)
Prerequisite: PT 5000 through 5120, 5141 through 5144, 5200 through 5230, 6000 through 6070.
Emphasis is on the various roles of physical therapy throughout the process of rehabilitation. Exposure to
patients with complex problems and special needs is included. There is a potential for off site experience
as a member of a rehabilitation team and work with experts in other medical professions. Experiences
provided to expose students to rehabilitation measures and techniques with real and/or simulated patients.
Lecture and laboratory.
PT 6200 Applied Research I (1 credit hour )
(Formerly PT 540)
Prerequisite: PT 5130, 5135. Individually planned studies under the direction of a senior investigator.
Studies to be pertinent to work in physical therapy. Cr/NCr.
PT 6210 Applied Research II (1 credit hour)
(Formerly PT 541)
Prerequisite: PT 5130, 5135, 6200. Students give presentation of research proposal to PT community.
Cr/NCr.
PT 6500 Electives (4 credit hours)
(Formerly PT 539)
Prerequisite: Approval of instructor. Students select from a variety of topics presented in the style of
continuing education courses and attend an average of 12 hours/week for four weeks. Laboratory
experiences may be included. Cr/NCr.
CLINICAL PRACTICA
PT 7010 Clinical Practicum I (2 credit hours)
(Formerly PT 518)
Prerequisite: Satisfactory completion of PT 5000 through 5130, PT 5141. Forty hours per week for two
weeks under the direct supervision of a physical therapist serving as the clinical instructor. Application of
Modules I and II will be emphasized in this clinical experience. Cr/NCr.
PT 7020 Clinical Practicum II (2 credit hours)
(Formerly PT 519)
Prerequisite: Satisfactory completion of PT 5000 through 5142, 5200 through 5230. Forty hours per
week for two weeks under the direct supervision of a physical therapist serving as the clinical instructor.
Application of Modules I through IV will be emphasized in this clinical experience. Cr/NCr.
PT 7030 Clinical Practicum III (12 credit hours)
(Formerly PT 520)
Prerequisite: Satisfactory completion of PT 5000 through 5143, 5200 through 5230, 6000 through
6020. Forty hours per week for twelve weeks under the direct supervision of a physical therapist serving as
the clinical instructor. Application of Modules I through VI will be emphasized in this clinical experience.
Cr/NCr.
PT 7040 Clinical Practicum IV (12 credit hours)
(Formerly PT 521)
Prerequisite: Satisfactory completion of all courses, except PT 6210 and 6500. Forty hours per week
for twelve weeks under the direct supervision of a physical therapist serving as the clinical instructor.
Application of Modules I through IX will be emphasized in this clinical experience. Cr/NCr.
118
HONORS AND AWARDS
The following awards are presented to PT students annually on Honors Day in April:
Physical Therapy Student Recognition Award
Physical Therapy Class Award
Elizabeth A. Rogers Chairperson's Award
Asian American Physical Therapy Scholarship Award
Roy G. and Marion L. Kramer Endowment Fund Award
Guy M. Allmon Scholarship Fund Award
Linda Fox Memorial Endowment Fund Award
President's Society Award
Rebecca E. Pabst Memorial Scholarship Award
Shannon Marie Fogard Memorial Scholarship Award
Casa Colina Centers for Rehabilitation Scholarship Award
Dean's Award
The following are presented at graduation:
Dean's Award
Physical Therapy Faculty Award
Physical Therapy Outstanding Clinical Performance Award
Physical Therapy Outstanding Service Award
Physical Therapy Academic Achievement Award
Outstanding Research Proposal Award
119
ACADEMIC CALENDAR
Program Year 2002 PT PROGRAM
(subject to change)
Jan. 2, 2002
Spring Semester Tuition Due
Monday, Jan. 7, 2002
MPT '04 Registration
MPT '04 Module I Begins
MPT '03 Module VI Begins
MPT '02 Module X Begins
Sunday, Jan. 13, 2002
MPT '04 Welcome Luncheon and White Coat
Ceremony
Monday, Jan. 21, 2002
Martin Luther King, Jr. Holiday
Monday, Feb. 18, 2002
President's Day Holiday
Monday, Apr. 1, 2002
MPT '02 Spring Break
MPT '03 Module VII Begins
Monday, Apr. 8, 2002
MPT '02 Module XI Begins
Monday, Apr. 22, 2002
MPT '04 Spring Break
Monday, Apr. 29, 2002
MPT '04 Module II Begins
Friday, May 3, 2002
MPT '02 Last Day of Classes
Monday, May 27, 2002
Memorial Day - No Classes
Friday, May 31, 2002
Graduation MPT '02
Monday, Jun. 24, 2002
MPT '03 Summer Break
Thursday, Jul. 4, 2002
Independence Day - No Classes
Monday, Jul. 15, 2002
MPT '04 2-week Clinical Practicum
(Module III) and 2-week Summer Break
Monday, Aug. 5, 2002
MPT '03 Module VIII Begins
Monday, Aug. 12, 2002
MPT '04 Module IV Begins
Monday, Sept. 2, 2002
Labor Day Holiday - No classes
Monday, Oct. 14, 2002
Columbus Day - No classes
Monday, Oct. 28, 2002
MPT '03 Module IX Begins
Monday, Nov. 25-29, 2002
Thanksgiving Break - No classes
MPT '04 may begin 2-week Clinical
Practicum II (Module V) pending
assignment
Monday, Dec. 2, 2002
MPT '03 Module IX Resumes
Monday, Dec. 16, 2002
MPT '03 Winter Break Begins
Monday, Dec. 23, 2002
MPT '04 Winter Break Begins
120
COLLEGE OF ALLIED HEALTH PROFESSIONS
Master of Science in Physician Assistant Studies
Primary Care Physician Assistant Program
ACCREDITATION
The Primary Care Physician Assistant Program of the College of Allied Health Professions is
accredited by the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA).
VISION STATEMENT
The Western University of Health Sciences Primary Care Physician Assistant Program will be
nationally recognized as an innovative leader in Physician Assistant education. Our faculty will continue to
educate a diverse student body who will provide humanistic and comprehensive primary care medicine
with a special focus on the underserved populations.
Our students will be the cornerstone for providing primary health care services. Employers will seek
our graduates to join their health care teams and participate as integral members. Through these
partnerships, access to comprehensive patient care will increase for underserved populations. Our students
and graduates will serve in key political positions, on a state and national level, to steer the future of the
physician assistant profession.
Our graduates, students and faculty will provide quality health care to underserved populations. The
faculty will forge and fortify educational experiences so that our students can ensure quality health care.
We will offer job-matching strategies to ensure that our graduates work in primary care medicine.
Quality health care education and services will be provided by interdisciplinary teams. The medical team
concept of teaching and patient care will be assured though the faculty's continued acquisition of
knowledge.
MISSION STATEMENT
The Primary Care Physician Assistant Program supports the University's mission by educating primary
care providers who are trained in delivering humanistic care as integral members of a health care
environment, and to meet the growing demands for primary care providers to provide health care to
underserved populations. The mission of Western University's Primary Care PA Program is to provide
education in primary care medicine to PA students in a humanistic and comprehensive manner. The
education and skills gained will allow students to provide culturally sensitive care to underserved
populations.
THE PHYSICIAN ASSISTANT ROLE
Physician assistants are health care professionals licensed to practice medicine with physician
supervision. Within the physician/physician assistant relationship, physician assistants exercise autonomy
in medical decision making and provide a broad range of diagnostic, therapeutic, preventive, and health
maintenance services. The clinical role of the physician assistant includes primary and specialty care in
medicine and surgical practice settings. Physician assistant practice is centered on patient care and may
include educational, research and administrative activity. As part of their comprehensive responsibilities,
PAs conduct physical exams, diagnose and treat illnesses, order and interpret tests, counsel on preventive
health care, assist in surgery, and can write medical orders.
The role of the physician assistant demands intelligence, sound judgment, intellectual honesty,
appropriate interpersonal skills, and the capacity to react to emergencies in a calm and reasoned manner.
An attitude of respect for self and others, adherence to the concepts of privilege and confidentiality in
communicating with patients, and a commitment to the patient's welfare are essential attributes.
The specific tasks performed by an individual physician assistant cannot be delineated precisely
because of variations in practice requirements mandated by geographic, political, economic, and social
factors. At a minimum, however, physician assistants are educated in those areas of basic medical science
and clinical disciplines and specific problem solving.
121
Physician assistant practice is characterized by clinical knowledge and skills in areas traditionally
defined by family medicine, internal medicine, pediatrics, obstetrics, gynecology, surgery, and
psychiatry/behavioral medicine.
Physician assistants practice in ambulatory, emergency and long-term settings. Physician assistants
provide health care services to diverse patient populations of all ages with a range of acute and chronic
medical and surgical conditions. They need knowledge and skills which allow them to function effectively
in an ever changing health care environment.
Services performed by physician assistants include, but are not limited to the following:
1. Evaluations: eliciting a detailed and accurate history, performing an appropriate physical
examination, ordering appropriate diagnostic studies, delineating problems, developing
management plans, and recording and presenting data.
2. Diagnostics: ordering, performing and/or interpreting diagnostic studies to identify and follow
pathophysiology process.
3. Monitoring: implementing patient management plans, recording progress notes and participating
in the process of the continuity of care.
4. Therapeutic: performing therapeutic procedures and managing or assisting in the management of
medical and surgical conditions, which may include assisting surgeries in the conduct of operations
and taking initiative in performing evaluations and therapeutic procedures in life-threatening
procedures.
5. Patient Evaluation: counseling patients regarding issues of health care management to include
compliance with prescribed therapeutic regimens, normal growth and development, family planning,
and emotional problems of daily living.
6. Referral: facilitating the referral of patients to other health care providers or agencies as
appropriate.
CERTIFICATION/LICENSURE
The written examination for certification as a physician assistant is administered by the National
Commission on Certification of Physician Assistants (NCCPA) in mid-October and April of each year.
Successful completion requires that the applicant achieve the passing score established by the NCCPA for
that examination. It is the responsibility of the applicant to ensure that certification of his or her
examination score is received by the Physician Assistant Committee (PAC). The NCCPA phone number is
770-399-9971. The PAC phone number is 916-263-2323.
The PAC may grant interim approval to an applicant for licensure as a physician assistant provided that
the applicant provides evidence that he or she is a graduate of an approved program and has applied for,
and therefore not taken, the first examination required by Section 1399.507 subsequent to the applicant's
successful completion of the approved program. If the applicant fails the examination, the interim approval
automatically terminates upon the applicant's receipt of notice of failure by the PAC or by the NCCPA.
An applicant who has been granted interim approval and who is subsequently notified by the NCCPA
or by the PAC that he or she has passed the examination required in Section 1399.507 shall complete the
licensure process by paying the initial licensure fee as requested within 90 days from notification that the
applicant is now ready for licensure. If the applicant does not complete the licensure process by end of the
90-day period, the interim approval shall automatically terminate.
PROGRAM GOALS
The primary goal of the Western University Physician Assistant Program is to educate individuals to
serve as physician assistants in primary care medicine. PA students are educated to provide health care to a
variety of patient populations with a special emphasis placed on the underserved. PAs work with the
direction and supervision of a physician. The education provided by the program will prepare the entry-
level graduate with the knowledge skills and attitudes to perform in a primary care setting and function in a
variety of roles within numerous clinical settings. The program goal of educating individuals to serve as
PAs in primary care medicine is founded on the understanding that the broad-based education needed to
prepare an individual to serve in a primary care setting is the most effective form of initial preparation.
122
This goal also permits the development of attributes that will serve the graduate in the greatest spectrum of
potential employment opportunities.
The program has also established the goal of incorporating appropriate elements of the traditional
osteopathic philosophy into the training of physician assistants. These elements include:
• An understanding of the patient as a "whole person."
• Emphasis on those aspects of health education that stress "wellness" and disease prevention.
• An appreciation of the role of physical medicine in the diagnosis and management of illness.
The curriculum is designed to accomplish the following objectives. Students attain these objectives as
they progress through the curriculum.
Knowledge
Upon completion of this program the graduate should know:
1. The pre-clinical, clinical and behavioral sciences that form the foundation for functioning as a PA.
2. The spectrum of normal measurements that define the healthy individual at all ages.
3. The pathophysiologic processes that commonly cause deviations in normal clinical measurements.
4. The fundamentals of health maintenance.
5. Patient management regimens for common primary health care problems.
6. Accepted strategies for disease prevention.
7. How to apply a systematic process of problem solving to the diagnosis of disease.
8. The components of normal human behavior and the major deviations from these patterns.
9. The health care resources available to the health care provider and patient.
10. The role of the physician in a variety of health care environments.
11. How the various health care delivery systems function and the role of the PA within each system.
12. The general principles of managed care as it applies to patients and primary care providers.
13. The fundamentals of various types of research modalities.
14. The research modalities and applications for problem solving in regards to disease, health
promotion and disease prevention.
Skills
Upon completion of this program the graduate should be able to:
1. Obtain a medical history.
2. Perform a complete physical examination.
3. Perform and interpret diagnostic tests.
4. Accurately report information obtained from a patient.
5. Manage, with the supervision of a physician, common health care problems.
6. Assess mental health status.
7. Recognize signs and symptoms of disease processes.
8. Communicate empathetically with a patient.
9. Formulate differential diagnosis to aid in diagnosis.
10. Critically interpret medical literature and apply it appropriately in clinical practice.
11. Gather community resources for patients.
12. Implement community health projects and guidelines.
13. Participate in quality assurance programs.
14. Develop health care resources for other providers and patients.
15. Participate in medical research activities.
Attitudes
Program graduates should exhibit respect and appreciation for:
1. All individuals who seek their care.
2. Self and other members of the health care team/profession.
3. An individual's right to confidentiality.
4. The sanctity of human life.
5. The dignity of patients.
6. The multiple physical and emotional factors that influence the health of individuals.
123
7. The many value systems in our society.
8. The importance of continuing medical education after graduation.
9. The effectiveness as a contributing team member in health care.
10. An increased PA role in regards to the medical community, health care delivery systems and the
patient.
FUNCTIONS AND TASKS OF PHYSICIAN ASSISTANT GRADUATES
General Entry-Level Competencies Expected of a Graduate
The physician assistant will be able to:
• Elicit a comprehensive, accurate history and perform a complete routine physical examination on
patients of any age group; elicit a pertinent and accurate history and perform a problem-oriented
screening examination in situations requiring an interval evaluation.
• Select, perform and/or interpret the appropriate routine laboratory and diagnostic studies/ procedures
for the purpose of completing an adequate data base.
• Identify problems, organize and integrate data, record and present.
• Accurately present an oral case.
• Implement a management plan, including performing or assisting.
• Instruct and counsel patients regarding physical and mental health to include diet, health maintenance,
therapy, normal growth and development, family planning, referral and follow-up services.
• Provide life support and emergency evaluation/care in response to life-threatening situations in the
absence of a physician and/or other appropriate health professionals.
• Initiate and follow up on appropriate referrals to specialists.
Associated Competencies
In addition to the above entry-level competencies, physician assistant graduates are expected to
function in a variety of environments, interact appropriately with diverse populations, and engage in many
activities for continued professional and personal growth. The role of the physician assistant as a primary
health care provider imposes many legal and ethical restrictions on behavior. Although not strictly related
to the "clinical role" of the physician assistant, there are a large number of activities that contribute to the
broad process of "professional development" and "role identity" which are essential for optimal
performance as a health professional. These activities are related to areas such as administration,
education, consultation, ethical, and legal considerations of the profession. The program will endeavor to
provide its students with educational experiences that will introduce these attitudinal objectives.
TECHNICAL GUIDELINES FOR ADMISSION AND MATRICULATION
A candidate for admission to the Primary Care Physician Assistant Program must have the use of
certain sensory and motor functions to permit them to carry out the activities described in the sections that
follow. Graduation from the program signifies that the individual is prepared for entry into clinical practice
or into postgraduate training programs. Therefore, it follows that graduates must have the knowledge and
skills needed to function in a broad variety of clinical situations and to render a wide spectrum of
diagnostic and therapeutic care. The candidate and student must be able consistently, quickly and
accurately to integrate all information received by whatever sense(s) are employed. Also, they must have
the intellectual ability to learn, integrate, analyze and synthesize data.
A candidate for the Master of Science in Physician Assistant Studies degree ordinarily must have
abilities and skills of five varieties including: observation; communication; motor; intellectual, conceptual,
integrative and quantitative; and behavioral and social. Where technological assistance is available in the
program, it may be permitted as a reasonable accommodation when appropriate. Under all circumstances,
a candidate should be able to perform in a reasonably independent manner.
a. Observation: Candidates and students ordinarily must have sufficient vision to be able to observe
demonstrations, experiments and laboratory exercises. They must be able to observe a patient
accurately at a distance and close at hand.
124
b. Communication: Candidates and students must be able to communicate with patients and colleagues.
They should be able to hear, with or without a reasonable accommodation. Candidates and students
must be able to read, write, and speak English.
c. Motor: Candidates and students ordinarily should have sufficient motor function such that they are
able to execute movements reasonably required to provide general care and emergency treatment to
patients. Examples of emergency treatment reasonably required of physician assistants are
cardiopulmonary resuscitation, administration of intravenous medication, the application of pressure to
stop bleeding, the opening of obstructed airways, the suturing of simple wounds, and the performance
of simple obstetrical maneuvers. These actions require coordination of both gross and fine muscular
movements, equilibrium and functional use of the senses of touch and vision.
d. Intellectual, Conceptual, Integrative and Quantitative Abilities: These abilities include measurement,
calculation, reasoning, analysis and synthesis. Problem solving, the critical intellectual skill demanded
of a physician assistant, requires all of these intellectual abilities. In addition, candidates and students
should be able to comprehend three-dimensional relationships and understand the spatial relationships
of structures.
e. Behavioral and Social Abilities: Candidates and students must possess the emotional health required
for full utilization of the intellectual abilities, the exercise of good judgment, the prompt completion of
all responsibilities attendant to the assessment and care of patients, and the development of mature,
sensitive and effective relationships with patients. Candidates and students must be able to tolerate
physically taxing workloads, adapt to changing environments, display flexibility, and learn to function
in the face of uncertainties inherent in the clinical problems of many patients. Compassion, integrity,
concern for others, interpersonal skills, interest and motivation are all personal qualities to be assessed
during the admissions and educational processes.
The Primary Care PA Program, along with all the other programs at Western University of Health
Sciences, shares a commitment to develop creative ways of opening the PA curriculum to competitive,
qualified disabled individuals. In doing so, however, the Primary Care PA Program must maintain the
integrity of its curriculum and preserve those elements deemed essential to educating candidates to become
effective physician assistants.
ADMISSIONS POLICIES AND PROCEDURES
Admission to the PA program is on a competitive basis and is open to citizens and permanent residents
of the United States. Western University is committed to admitting competitive, qualified disabled
individuals. For technical guidelines, please see above.
Application Requirements
The admissions committee will consider applicants with a minimum of a bachelor's degree from a
regionally accredited institution or who will complete their bachelor's degree before matriculation. The
minimum overall GPA required is 2.5 on a 4.0 scale and GPA of 2.7 on a 4.0 scale in all course work
listed as prerequisites for the PA program. Grades of "C-" in any of the prerequisite courses are not
accepted. Candidates should possess the oral and written communication skills necessary to interact with
patients and colleagues.
1. Prerequisite Courses:
College English and English Composition* (6 semester units, a full year sequence)
College Algebra (3 semester units)
Human Anatomy with lab** (3 semester units)
Human Physiology with lab** (3 semester units)
Microbiology with lab (3 semester units)
General or Inorganic Chemistry with lab (6 semester units, a full year sequence)
Psychology (General or Introductory only - 3 semester units)
Sociology (General or Introductory only - 3 semester units)
Humanities (9 semester units)
Introductory Statistics (3 semester units, preferably from the math or statistics department)
Spanish is strongly recommended.
Genetics is strongly recommended.
125
*Note: English prerequisites must be taken from the English department. English as a Second
Language (ESL) courses are not accepted for the English prerequisites.
**Note: Anatomy and physiology must be taken out of the anatomy, physiology, A&P, biology,
or zoology departments. If anatomy and physiology are combined, a minimum of five semester
units is required.
Advanced placement, transfer of credit, CLEP examination, or credit for experiential learning is not
recognized by the program as meeting these prerequisites.
Introductory level courses in the sciences are not acceptable (i.e., courses taken in the sciences for non-
science majors).
Prerequisite courses must be transferable. Transferable courses are those designated for baccalaureate
credit by the college or university offering the courses.
2. Health Care Experience
Health care experience is not required. However, engagement in extracurricular or community
activities that reflect people or service orientation is considered essential. The extracurricular or
community activity does not need to be medical in nature.
Application Procedures and Deadlines
Beginning with the entering class of August 2002, the PA program will be participating in the first
central application service for physicians assistant programs. The Central Application Service for
Physician Assistants (CASPA) was created by the Association of Physician Assistant Programs (APAP) as
a service to applicants and member programs. CASPA will begin accepting applications late spring 2001.
CASPA will collect one set of materials from each applicant. CASPA will then authenticate, photocopy,
and distribute them to each member school an applicant designates. Western University’s application
deadline to apply to CASPA is December 1, 2001. Applicants are considered without discrimination on
the basis of race, color, national origin, age, or sex.
To request an informational brochure and/or information about the CASPA application, contact the
Office of Admissions or the CASPA office at:
Office of Admissions CASPA
Western University of Health Sciences apply@caspaonline.org
309 E. Second Street (240) 497-1895
Pomona, CA 91766-1854
(909) 469-5541
In addition to the CASPA application, applicants must submit a supplemental application. After the
CASPA application has been received, a supplemental application (provided by Western University) will
be sent to all applicants who meet the overall GPA of 2.5. However, this does not ensure that you will
meet our minimum prerequisite of 2.7 or that all prerequisite classes will be acceptable. A final evaluation
and calculation will be completed upon receipt of your supplemental application. The supplemental
application deadline for the class entering in August 2002 is February 15, 2002. The supplemental
application consists forms requesting additional information, one letter of reference, and a personal
statement. A non-refundable application fee of $45 must be submitted with the supplemental application
materials. All application materials must be returned as part of one supplemental application packet.
Applicants who wish to use course work completed outside of the United States must submit their
transcripts for evaluation to World Education Services, Josef Silny and Associates, Educational Credential
Evaluators, Inc., or International Education Research Foundation, Inc. In preparation for CASPA, a
course-by-course evaluation is required, and all course work must be designated as undergraduate,
graduate, or professional. Western University will only honor evaluations from the above services. The
evaluation must be submitted to CASPA.
The applicant's personal statement is reviewed. The applicant may be granted an on-campus interview.
During the interview process, the applicant meets individually with an interview team, which may consist
of the PA Program Director, PA Admissions Committee Chair, PA faculty, University faculty, students,
PA alumni, and community PAs. The interviewers question the applicant regarding academics, personal
preparedness and commitment to the PA program and the PA profession. Interviewees are rated on a
126
standard evaluation form relative to each of these variables. After the conclusion of the interviews, the
evaluation forms are reviewed by the PA Admissions Committee, which decides to admit, deny admission,
or place the applicant on an alternate list. The Western University PA program does not accept transfer
students, nor is admission to the program deferrable. Decisions of the Admissions Committee regarding
the admission of applicants to the Master of Science in Physician Assistant Studies program are final.
Candidates accepted to Western University must have a complete set of official transcripts mailed to the
Admissions Office no later than July 1. For your information, CASPA retains the original set of transcripts
it receives from applicants.
REGISTRATION
First year students are required to register in person on the registration day specified in the University
Calendar or as otherwise directed by the Registrar. Failure to register on that day may be grounds for
dismissal. Full tuition and fees and all prior debts must be paid in full on or before registration day each
academic year. Matriculation is subject to the satisfactory completion of all academic requirements and
payment of all outstanding debts to the University. The receipt of a final transcript from an undergraduate
college and a physical examination with documentation of required immunizations prior to registration are
additional requirements for incoming students. Also, all students must show proof of current health
insurance coverage at the time of registration. This coverage must be maintained or in effect throughout
the academic year. If there is no proof of current coverage, a policy provided by the University is
available. Attendance at Orientation is mandatory for all incoming first-year students.
TUITION AND FEES
By action of the Board of Trustees, PA tuition and fees for the 2001-2002 academic year (subject to
change) are as follows:
$19,095 Tuition Annual
For PA applicants accepted at Western University, an entrance fee of $250
payable upon acceptance is applied to tuition.
$40 Student Body Fee, 1
st
year
Covers student council expenditures, social activities and public relations.
$20 Student Body Fee, 2
nd
year
Other Fees and Expenses
$1200 Required and Recommended Texts
$45 Uniform Jacket/Patch, Name Badge
$6500 Diagnostic Equipment Kit
$30 (per day) Late Registration Fee
$40 Lost Mail Locker Key
$5 (each) Copy of Official Transcript
$10 (each) Copy of Official Transcript Faxed
$10 Lost ID Badge
$0.25 (per page) Copy of Student File Material
(replacement cost) Breakage Fee
ACADEMIC REQUIREMENTS
Academic Advisement
Students will be assigned a faculty advisor by the Dean upon matriculation. Advisement by faculty
should be viewed by the student as a part of the academic process. If either the student or faculty member
does not find the relationship helpful, either is free to seek a change. This request should be made to the
appropriate Dean or Dean’s designee. It is the student's responsibility to meet periodically with his/her
advisor. A student on probation must meet with his/her faculty advisor at least once a month.
127
Promotion
A student’s progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behaviors and attitudes. At the completion of
each phase of the program, before the student is allowed to progress to the next phase, the student’s record
of achievement is reviewed by the Program Chair and faculty.
The faculty determines if the student has demonstrated the knowledge, skills, and attitudes necessary to
be eligible to progress to the next phase.
In special instances, the faculty may be convened at other than the scheduled times to consider cases
relating to unusual circumstances, such as probation or dismissal.
Promotion is defined as progression from one academic year to the next.
a. A student will be recommended to the Dean of the College of Allied Health Professions for
promotion by the Allied Health Student Academic Progress Committee.
b. A student may not be recommended for progression from one semester or phase to the next with any
outstanding grades of “I” or “U” on his/her academic record or with a semester grade point average of
less than 2.5. Grades of “D” must be remediated before progression to next phase.
c. When considering a student for promotion, professional, ethical, and personal conduct may also be
taken into consideration (as described under Probation, a-4).
d. A student will be promoted provided that all legal and financial requirements of the University as
stated in the University Catalogue have been satisfied.
Graduation
A student will be recommended for the Master of Science in Physician Assistant Studies provided
he/she:
a. has completed at least two years of the Western University Primary Care PA program.
b. has been enrolled in the Western University Primary Care PA program during his/her final academic
year.
c. is not on probation and has completed all prescribed academic and clinical requirements with a
cumulative grade point average of at least 2.5 and has no outstanding grade of “D”, “I” or “U”.
d. has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined in
Probation guidelines, which would make it inappropriate to award the degree of Master of Science in
Physician Assistant Studies.
e. has complied with all the legal and financial requirements of the University as stated in the
University Catalogue.
f. All students must attend in person and participate in the Commencement program at which time the
Master of Science in Physician Assistant Studies is conferred, unless special permission is received
from the President. If the President grants special permission to be excused from graduation, the
graduate may be required to present himself or herself to the Provost or appropriate Dean at a later date
in order to take the required oath (if relevant) to receive his or her degree.
g. is within one clinical rotation of completion of all requirements for graduation to be able to march
with his or her class in the graduation ceremony. At the discretion of the Dean of the College of Allied
Health Professions, an exception may be made for a student with an authorized leave during the Senior
year. No student will receive his or her degree until the student has completed all requirements for
graduation. Degrees will be dated as appropriate to completion date.
Probation
a. Probation is defined as a period of time specified by the Dean of the College of Allied Health
Professions during which the student's progress will be closely monitored by the Allied Health Student
Academic Progress Committee, faculty advisor and the Program Chairperson. In order to closely
monitor 2nd year students on probation, the PA program reserves the right to assign their clinical
rotations. A student will be recommended for probation for any of the following reasons:
1. Immediately upon receiving a course grade of "D" or "U" in any course.
2. A grade point average of less than 2.5 at end of the semester.
3. When directed to repeat a year for academic reasons.
4. Seriously deficient ethical, professional, or personal conduct.
128
Members of the faculty or administration will render a special report in writing to the Dean of the
College of Allied Health Professions regarding any student whose professional or personal conduct is
deemed unsatisfactory. Professional and personal conduct includes, but is not limited to, attendance,
cooperation with faculty, interest shown in assigned work, attitude toward fellow students and
associates and toward personnel of hospitals, approach to and interaction with patients, as well as
personal appearance appropriate to the circumstances.
The terms of probation for ethical, professional, or personal conduct will be specified at the time the
student is placed on probation.
b. When a student is placed on probation, he/she will be notified in writing by the Dean of the College
of Allied Health Professions and the reasons will be stated. Notification must be by Certified mail or
hand-delivered and acknowledged by signatures of the student and the Dean of the College of Allied
Health Professions or his designee. Copies of the letter will be placed in the student's permanent file
and distributed to the Chairman of the Allied Health Student Academic Progress Committee and the
student's faculty advisor. The Allied Health Student Academic Progress Committee will ascertain when
the terms of the probation have been satisfied and recommend to the Dean that probation can be
rescinded.
c. A student on probation may not serve as an officer of any official University club or organization
and shall not engage in time-consuming extracurricular activities.
d. A 1st year student on probation must meet with his/her faculty advisor at least once a month. A 2nd
year student on probation must contact his/her Faculty Advisor once a month.
e. Students are removed from probation when the following occur:
1. After one semester, provided he/she has regained a semester grade point average of 2.5.
2. When all “D” or “U” grades have been satisfactorily remediated according to the Remediation
section of the Catalogue (below).
3. When the specified terms of probation for ethical, professional, or personal conduct are met.
4. When 2nd year students are on probation for a clinical rotation grade of “U”, they will be
removed from probation when they have met the terms of their probation.
Remediation
a. Every effort will be made to give each student ample opportunity to demonstrate competency in
each area of the academic program. However, remediation is to be regarded as a privilege that must be
earned by a student through an active participation in the educational program as demonstrated by
regular attendance, individual initiative, and utilization of resources available to him/her.
b. If a student receives a “D” or “U” grade in a course or has a semester grade point average of less
than 2.5, that student will be reviewed by the Allied Health Student Academic Progress Committee and
procedures for remediation by the Physician Assistant faculty will be recommended to the SAPC, who
in turn makes a recommendation to the Dean. In reviewing the student's academic deficiencies, the
following guidelines shall be used:
1. Educational objectives underlie remedial teaching and evaluation should be the same as the
educational objectives that underlie regular courses in the curriculum. Where deemed
appropriate, the Allied Health Student Academic Progress Committee, after consultation with the
course instructor and/or Physician Assistant Faculty, may recommend one or a combination of the
following options:
(a) Take a comprehensive examination (this option is not available if the original earned
grade is a “U”).
(b) Complete special projects or studies in the deficient area(s).
(c) Repeat the course, with or without promotion into the subsequent semester. The
student cannot start Phase II or Phase III until the grade of “D” or “U” has been
remediated.
(d) Repeat the academic year.
(e) Dismissal from the University (see Dismissal section for criteria for this option).
2. Students receiving a “U” grade for a clinical rotation education/preceptorship will repeat the
entire rotation/preceptorship. The above options do not apply to clinical education.
129
3. The grade achieved by remediation will be the grade recorded EXCEPT that the highest grade
a student may earn by options (a) or (b) is a grade of “C”. The grade achieved by remediation
will be recorded on the transcript beneath the original grade.
4. Grades earned during an attempted remediation of a course will be reviewed critically by the
Allied Health Student Academic Progress Committee and the Dean of the College of Allied
Health Professions. Failure to earn at least a “C” grade may result in dismissal from the
University or repeating the course.
5. Decisions regarding remediation will be made on an individual basis after considering all
pertinent circumstances in each case. The decision will be made by the Dean of the College of
Allied Health Professions Education, based upon the recommendation of the Allied Health
Student Academic Progress Committee. The Allied Health Student Academic Progress
Committee will base its recommendation on the student's academic record and considerations
after consultation with the Physician Assistant Faculty Student Advisor, course instructor, and the
student, when appropriate.
6. Any student who is required to remediate a course will be notified in writing by the Dean of
the College of Allied Health Professions Education at least two weeks prior to the remediation
date (or within two weeks after the close of the academic year in which the student is presently
enrolled, whichever comes first). Notification must be by Certified Mail or hand-delivered to the
student and must be acknowledged with the signatures of the Dean of the School of Allied Health
Professions, or his designee, and the student.
c. Students who have been required by the Dean of the School of Allied Health Professions to repeat a
course(s) due to unsatisfactory grades (GPA) or in cases where there is a satisfactory GPA, but
deficiencies are noted which impedes promotion, the following criteria must be met to be eligible for
financial aid:
1. Full-time attendance recorded
2. Placed on at least one semester probation
3. Must be tested and graded
4. Close monitoring
It is the student's choice if he/she has made satisfactory progress such as GPA, but wants to audit only
to strengthen skills, as long as he/she is fully aware he/she will not be eligible to apply for any financial
aid. Students will be financially responsible for themselves until promoted by the Dean of the School of
Allied Health Professions.
Clinical Education/Preceptorship Remediation
Any student who receives a grade of “U” for a clinical education/preceptorship grade will be required
to repeat the entire clinical education/preceptorship. The student must complete all deficiencies for the
clinical education/preceptorship prior to completion of the program. The grade achieved by repeating the
rotation/preceptorship will be recorded on the transcript. Remediated grades are recorded below a grade
of “U.” Only the remediated grade is calculated into the G.P.A.
Remediation: Financial Aid Policy
If the student, at the end of the academic year, is still considered to be making unsatisfactory progress
and must remediate, he/she is removed from the list of Title IV and Title VII financial aid recipients.
Tutorial Assistance Program
A Tutorial Assistance Program (TAP) has been established to assist students experiencing academic
difficulty. Students will be recommended for this program by a faculty advisor or professor. The tutors
will be chosen from the second year class and a list of alumni on the recommendation of the faculty in each
discipline. For assistance, contact the Learning Enhancement and Academic Development Office.
Students can also self identify for TAP.
130
Standards of Academic Progress
Good academic standing implies that a student has not been requested to withdraw and is not under
academic probation/suspension.
Academic performance encompasses those areas of knowledge and skills outlined in the section
entitled "Program Objectives". The level of attainment listed in these areas is that expected of graduates of
the program. However, students are expected to attain these goals as they progress through the Program
and certain patterns of attainment are expected along the temporal course of the curriculum.
All grading and evaluation is based on the student's ability to attain the competencies within the
objectives outlined for each area of study.
A student whose performance falls below the minimum acceptable standard(s) for any area of study
will be notified of such deficiency by the instructor of the course as soon as evidence of such sub-standard
performance is available.
The following academic standards apply to students enrolled in the Primary Care Physician Assistant
Program. Academic performance is considered sub-standard and unacceptable if any one or more of these
standards are not met:
a. Phase I:
During Phase I (Didactic Phase), students must earn a grade of "C" or better in each course. All
“D's” or “U’s” will be remediated to a "C" (see Remediation Section). If a remediated grade of
"C" is not earned, the student will be required to repeat the entire course of study.
Students must maintain a GPA of 2.5 during Phase I. In addition, the following applies regarding
cumulative GPA:
1. Students whose GPA falls below 2.5 must meet with the department chairperson prior
to registration for the next semester.
2. Students whose GPA falls below 2.5 are not eligible for further registration unless
probationary status is granted by the Dean of the College of Allied Health Professions
Education.
3. Students will not be allowed to advance to Phase II (clinical education) until all
deficient grades are remediated.
b. Phase II:
Senior Seminar I, II and III Requirement
1. In Senior Seminar I and II, a grade of "C" or better must be earned. All "D's" will be
remediated to a "C". If a remediated grade of "C" is not earned, the student will be
required to repeat the entire course of study.
2. If a student receives a "U" in Senior Seminar I, he/she must repeat the course;
however, the student is allowed to progress to Senior Seminar II. If the Student receives
a "U" in Senior Seminar II, he/she must repeat the course, and he/she will not be able to
advance to Phase III.
3. If a student receives a “U” in Senior Seminar III, he/she must remediate to a “C”
grade.
c. Clinical Education Phase II and Phase III
Students’ progress through the program is based upon successful completion of expected
competencies and demonstration of expected professional behaviors and attitudes. If students fail
to meet the pre-designated clinical objectives, their academic achievements will be reviewed by
the PA faculty. The faculty and preceptors determine if students have demonstrated the
knowledge, skills and attitudes necessary to be eligible for progress to the next phase. Upon
eligibility, the faculty recommends advancement to the Allied Health Student Academic Progress
Committee.
If a student receives a grade of “U” in Phase II, he/she must repeat the rotation before advancing
to Phase III.
The Allied Health Student Academic Progress Committee and the Professional Conduct
Committee may be convened to consider cases relating to unusual circumstances.
131
Out-of-Area Clinical Education
Clinical Education that is greater than 180 miles in any direction from Western University, Pomona
Campus, is considered an out-of-area rotation clinical education. Permission for out-of-area rotations
clinical education is granted by the Clinical Education Coordinators and the PA Faculty.
To participate in out-of-area rotations, students must:
• Exemplify ethical and professional behavior throughout their didactic and clinical rotations
phase.
• Have a GPA of 3.0 from Phase I, receive a “B” or better on all preceptor assigned grades and
maintain a “B” or better in Senior Seminar I and II.
• Provide the Clinical Education Coordinators with transportation and room and board for out-
of-area site visits.
• Sign a waiver releasing Western University from any responsibility regarding NCCPA Board
performance.
Clinical Rotation Education Assignment Appeal
A change in clinical rotation education assignment may be requested in writing by the student for the
following reasons:
a. After completing one week in the rotation, the student deems the rotation is not of high quality.
b. The student is requesting a change in a clinical rotation assignment for a specific month under a
preceptor not affiliated with the PA Program.
Completed paperwork requesting an upcoming rotation change must be submitted to the Clinical
Education Coordinators 30-60 days before the rotation is scheduled to begin. The student will be notified
of the approval/non-approval of the request within 24 hours.
Reassignment of Clinical Rotation Education
Any student who receives one or more “C’s” on a preceptor assigned grade for the clinical rotation,
may have the remainder of their clinical rotations reassigned by the Clinical Education Coordinators.
Rotational Clinical Education Observation
Any student who has been "deemed unsafe" may be placed in an observational mode until further
notice. for the remainder of his/her rotation. A student may be placed in observation mode for one month
only, then summary suspension may occur. Summary suspension may be implemented instead of
observation mode.
Personal Appearance
Personal appearance is extremely important in facilitating acceptance by other health professionals and
patients. The poor appearance of one individual is often generalized to the entire profession. Adherence
to the following dress code is, therefore, the responsibility of each student while in clinical training.
a. Primary Care Physician Assistant Program name tags/badges are to be worn at all times while on
campus, and at clinical rotation education sites.
b. Short white “intern” type jackets are required at all times, beginning with Phase II of the curriculum.
c. Female students may wear slacks or other appropriate dress. Modesty must be a consideration for
necklines and hemlines.
d. Shirt and tie are considered appropriate dress for male students when they are present in a setting
where patient contact can be expected. Students must receive the approval of the supervising
practitioner to wear “scrubs” during the rotation.
e. “Blue jeans” are NOT appropriate dress for either male or female students during the clinical
phases.
f. “Tennis Shoes”, “Joggers”, and other forms of athletic shoes are NOT considered appropriate attire.
g. Students should consider the image projected to the patient and others with regard to hairstyle and
length, beards, mustaches and jewelry.

132
Professional Conduct During Clinical Education
Professional and personal conduct includes, but is not limited to attendance, cooperation with
preceptors, interest shown in assigned work, attitude toward fellow students, associates and personnel of
hospitals and approach to and interaction with patients.
• Students will introduce themselves as physician assistant students.
• Students will wear their Western University identifying nametags when in a clinical setting at all
times.
• Students will be able to explain what a PA is concisely and confidently to patient(s) and staff.
• Students who introduce themselves as a physician are subject to dismissal from the program.
• Students will not engage in any activity that may be construed as being unethical, immoral or
inconsistent with the practice of medicine.
Students breaching the Professional Conduct Policy will go through the following process:
The student will be required to have a student conference with the Program Chair and/or Clinical
Education Coordinators. The breach of conduct will be investigated and the student will be notified of the
results of the investigation. A verbal warning may be issued and/or a letter of unprofessional conduct may
be placed in the student’s file. A student may be placed in observational mode by the Program Chair
during the investigation, or may request that the student be summarily suspended during the investigation.
Academic Warning
The student who demonstrates unacceptable performance in any unit of study during any phase of the
program is notified of such performance by the Instructor of the course as soon as it becomes evident.
He/she is notified that continued poor academic performance can lead to academic probation and
dismissal.
Students whose performance is considered unacceptable as a result of not meeting the Standards of
Academic Progress will be placed on probation. The duration and conditions of the probationary period
will be recommended to the Dean of the College of Allied Health Professions on an individual basis by the
Allied Health Student Academic Progress Committee. The Committee may recommend remedial study
and/or repetition of a unit of study. This may result in extending the length of the program beyond 24
months. See, also, section on Probation, in the General Academic Policies and Procedures section for
the University.
a. Phase I: Students will be placed on academic probation as a result of "D” or “U" work in any unit
of study.
b. Phase II: Students will be placed on academic probation as a result of any of the following:
1. A final grade of "U" in any clinical rotation.
2. A final grade of “D” or “U” in Senior Seminar I and II.
3. Unacceptable performance on any component of clinical rotations education.
c. Phase III: Students will be placed on academic probation as a result of any of the following:
1. Unacceptable performance in Senior Seminar III (the comprehensive examination.)
Students failing to achieve a passing score on the program comprehensive examination will be
required to demonstrate attainment of competencies related to the areas of deficiency through re-
evaluation. If the student has not attained the necessary competencies in the areas of deficiency
through re-evaluation, he/she may be required to complete a course of remedial study.
2. Less than “C” performance on any portion of the preceptorship grades.
3. Students will not be allowed to graduate until all competencies have been achieved.
Attendance
Attendance is expected for all lectures, classes, and academic-related activities. It is required that
students observe the following policy:
a. Excused Absences
1. All
unanticipated absences due to illness, accident, or other unexpected events must be
reported to the program within 24 hours.
2. Absences requested for physician/dentist appointments for student or dependents will be
considered excused only if requested in advance of the appointment. Due to the intense nature of
133
the curriculum, students are strongly encouraged to schedule appointments for evening and
Saturday hours to avoid class conflicts.
3. All anticipated absences for any reason, regardless of length, must have the prior approval by
the faculty to be considered excused.
All requests for anticipated absences must be submitted in writing at least two weeks prior to the
proposed absence. Requests will be considered on an individual basis and written notification of
approval or disapproval will be provided to the student within one week of receipt of request.
4. Students in clinical education/preceptorship are responsible for notifying both their
supervising physician(s), and the Physician Assistant program, regarding all absences whether
anticipated or unanticipated. Prolonged absences require notification each day to preceptors and
the program.
5. When an absence is the result of a sudden unavoidable circumstance, the program should be
notified as soon as possible and provided with an explanation for the absence.
6. Clinical rotation education/preceptorship absences and tardies will be made up at the
convenience of the preceptor or the program.
7. Five or more absences from a clinical rotation education can result in any of the following:
(a) repeat the entire rotation
(b) make up days assigned at the convenience of the preceptor
(c) grade of Incomplete assigned
Confidentiality of Medical Record and Health History Information
All data gathered about the patient and his/her illness, including all items within a patient's medical
history is privileged information.
a. Students should not discuss a patient's records in a manner or a situation that would reveal any
information about that patient or his/her records to persons not involved in his/her health care.
b. Charts or contents, e.g., lab reports, etc., are not to be removed from the hospital or clinical setting.
Patient Records - Physician Review and Countersignature
On each clinical rotation education, it is the student's responsibility to insure that ALL patients seen by
the student are also seen by the supervising practitioner. The supervising practitioner should also review
all student notes written in medical records and countersign these documents. Countersignatures should be
obtained before the patient is released on outpatient and in patient rotations.
Under no circumstances should a student initiate orders for any patient on any rotation clinical
educational rotation without immediate physician consultation and countersignature. In addition, under no
circumstances should a student sign transmittal medical orders.
Under no circumstances should a student accept samples from pharmaceutical representatives on behalf
of the preceptor or himself.
These guidelines must be strictly adhered to for the student's protection and the protection of the
patients seen by students.
Title Identification/Representation
Role and title confusion are common problems encountered in dealing with patients, e.g., some patients
identify all those wearing short white coats as physicians. Students should be aware of this problem and
avoid misrepresentation by politely explaining their role and position.
a. In professional interactions with patients and others, a student should introduce himself or herself as
a "physician assistant student" using the title of Mr. or Miss, Mrs., or Ms.
b. Students should use the designation, "P.A.-Student" (PA-S), following all notations in charts,
records, and other medical forms.
Dismissal Recommendations
A student may be subject to dismissal from the program for substandard academic or professional
performance, as follows:
a. Students who earn two or more "D's”, “U's” or a combination of one “D” and one “U” throughout
the 24-month program may be dismissed from the program.
134
b. Lack of professional attributes considered appropriate for continuance in the program and
profession.
c. Any event that could result in either academic or professional probation for a student currently on
academic or professional probation.
d. Violation of the terms of probation.
e. Presenting him/herself as a physician.
Examination Policies
a. Students are not to communicate in any way during the examination and are to face the front of the
classroom at all times.
b. During scheduled examination hours, students are highly discouraged from going to the bathroom,
but will be allowed to go one at a time. The student will be required to turn in the exam and scantron
sheet as he/she goes to the bathroom.
c. Once a student finishes an exam, the student will turn in the exam and the scantron form to the
proctor, and after he/she leaves the examination room, he/she will not be permitted to re-enter the room
until the exam is declared over.
d. All students' belongings, i.e., notebooks, calculators, and headsets, etc., will be kept in front of the
room.
e. Questions will be answered at the discretion of the proctor during the examination period. Students
should be permitted to point out typographical or other errors present in the examination to the proctor.
f. Alternate seating shall be utilized for all examinations unless precluded by space availability.
g. Students are not to communicate in any way during the examination, are not to look at any other
student’s examination paper, and are to face the front of the classroom at all times. All pagers, cellular
phones, etc. are to be turned to vibrate mode
h. Violations of these examination policies and of Standards of Academic and Social Conduct will be
brought before the Student Conduct Committee.
i. The course instructor sets the date of assignments, midterms, and final examination. All tests and
assignments are to be taken as indicated in the course syllabus. Examination dates can only be changed
by the instructor after reviewed and approved by the department chair.
Evaluation and Grading
a. General: The degree of competency expected of all program graduates upon completion of the
professional curriculum is defined by the "Functions and Tasks of Physician Assistant Graduates". The
curricular components of the program are designed so that students' work toward achievement of these
competencies is measured via written and practical examinations and by evaluations of clinical
performance and professional development. Specific behavioral objectives have been defined for each
curricular component to assist the student and the program faculty in evaluating the degree of
attainment of these expected competencies throughout the 24-month curriculum.
b. Evaluation Methods: Overall student performance is evaluated differently during each phase using
one or a combination of the following methods:
1. Written examinations: Written examinations will vary based on the content of the individual
course. A combination of single answer multiple choice, matching, True/False, short answer,
essay and patient management type questions are used.
2. Practical or Laboratory Examinations: In selected courses, students will be observed obtaining
histories or performing physical exam components on simulated patients. They may also be
asked to "problem solve" based on a patient database. At times, they will be evaluated on their
ability to perform laboratory tests.
3. Student Presentations: Students may be asked to orally present individual or group projects,
patient cases, research papers, etc. These oral presentations may or may not be accompanied by a
written report.
4. Written reports: At various times, students will be evaluated on written reports of assigned
topics, written histories, physicals, discharge summaries, research papers, etc.
135
5. Professional Development Assessments: Assessments of each student's academic, professional
and interpersonal growth and development are shared with them on an individual basis
periodically during each phase of training.
6. Clinical Evaluations: Supervising preceptors are asked to assess the student's level of
attainment of competencies related to selected parameters within the domains of knowledge, skills
and attitudes, and to evaluate the student's overall performance while on clerkship. Evaluation
forms, which incorporate these areas to be evaluated, are utilized.
Students are responsible for securing these evaluations from the supervising preceptor(s) on
each rotation and ensuring that they are completed and returned to the program office in a timely
fashion. Preceptors are encouraged to discuss the student's performance and progress throughout
the rotation with him/her and to discuss the final evaluation prior to completion of the rotation.
Since the clinical evaluation is an essential part of the overall assessment of the student's
performance on a given rotation, course grades will not be computed without it. Students who
fail to obtain clinical evaluations prior to the end of the respective clinical rotation will be given a
grade of incomplete "I" for that clinical course. Courses with incomplete grades must be
completed prior to advancing to preceptorship (Phase III).
Clinical evaluation forms become a part of the student's academic profile record. Students are
required to sign each evaluation and are encouraged to sign at the time the evaluation is discussed
with the supervising preceptor. Students are provided copies of all their clinical evaluations when
these are submitted by the preceptor to the program.
7. Patient Write-ups: Students on clinical rotations are required to submit a minimum of one
patient write-up each month in the S.O.A.P. format. The chosen case must represent conditions
listed in the objectives for each module. The write-ups are due in the PA Program Office by the
10th of the month following the rotation. end of the rotation/month
8. Literature Review: Students can be requested to review current literature and complete a one-
page, typed and double spaced critique. The critique will be evaluated on content, validity,
clarity and clinical relevance.
9. Final Comprehensive Examination: A comprehensive examination is administered during the
Senior Seminar III and serves as a summative examination. This examination evaluates the
student's accumulated knowledge and skills while familiarizing him/her with the format of the
certification examination. Like the NCCPA certification examination, this examination consists
of a written multiple choice exam and a clinical skills component.
10. Grade Reports: Final grade reports are mailed to students at their home addresses upon
completion of each semester by the Registrar.
A class ranking may be obtained from the Registrar’s Office in writing with appropriate
identification. The class ranking is based solely on letter grades, not percentages.
Due to the nature of the clinical curriculum, i.e., variable duration and sequencing of clinical
courses education, course completion dates rarely coincide with traditional grading periods.
In these cases when final grades are not available at grade reporting time, a grade of “M” is
submitted to the Registrar in lieu of the course clinical education grade. “M” grades are entered
on the grade reports and are converted to student achieved grades at the earliest possible
opportunity.
An up-to-date summary of student performance is maintained in the Program Office Files and
is available to each student for his/her review.
11. Review of Examinations: Examinations are graded as soon as possible and one examination
is kept on file for student review.
12. Grading Scale: Final course grades are given based upon the traditional 4-point letter system,
as follows:
Grade Points
A 90% - 100% 4
B 80% - 89% 3
C 70% - 79% 2
D 65% - 69% 1
U Less than 64% 0

136
Cr/NCr 0
I Incomplete 0
M Missing 0
13. Clinical Rotation Education Grading Criteria: The Clinical Education grade is based on the
student’s singular performance as assessed by the preceptor and the patient write-up.
(a) Student Performance from supervising preceptor 60%
(b) Patient Write-Up (one per month) 40%
100%
1. Students are required to earn a final course grade of “C” or better in each clinical
rotation. Students cannot earn two or more “U’s” or “D’s” or a combination of one “D”
and one “U” throughout the entire 24 months of the program. Students will not be
allowed to advance to Phase III (Advanced Clinical Preceptorship) until all deficient
clinical rotation Education grade(s) are completed/remediated. Remediation will delay
the student’s progress to preceptorship and extend the program completion date.
The following applies regarding Cumulative GPA:
a. Students whose GPA falls below 2.5 must meet with the Program Chair prior
to registration for the next semester.
b. Students whose GPA falls below 2.5 are not eligible for further registration
unless probationary status is granted by the Dean of the College of Allied
Health Professions.
c. Students participating in Out-of-Area Rotations Clinical Education must
maintain a cumulative GPA of 3.00 in all preceptor assigned grades and Senior
Seminar I and II. The program will revoke the privilege of the Out-of-Area
Rotation Clinical Education if the student’s GPA falls below a 3.00.
2. To receive a complete grade for each clinical rotation education, all assigned
documents must be submitted to the PA Department, Pomona campus:
a. Twice Monthly Time Records
b. Time records/Monthly Schedules
c. Returned Preceptor/Site Evaluation Form
Failure to submit items a and b and c at the end of each month will result in a grade of
Incomplete (I).
14. Preceptorship Grading Criteria: Advanced Clinical Preceptorship grades is are based on the
student’s performance as assessed by the preceptor and the patient write-up.
a. Student Performance Form from supervising preceptor 80%
(one per month)
b. Patient Write-up (one per month) 20%
100%
1. Students are required to receive a grade of “C” or better on their preceptorship
evaluation. The preceptor is responsible for evaluating the student's performance
monthly during the preceptorship. Students will be evaluated on the basis of their
clinical medical knowledge, diagnostic skills and treatment plans, as well as their
motivation, willingness to accept responsibility and interaction with patients, staff and
supervisors. It is the student’s responsibility to ensure that THE STUDENT
PERFORMANCE FORM for the preceptorship evaluations (3) are returned to the
program by the last day of each month.
2. The following documents must be submitted in order to receive a final grade:
a. Twice Monthly Time Records/Monthly Schedules
b. Returned Preceptor/Site Evaluation Form.
c. Final resume by July 31st.
Failure to submit items a-c will result in a grade of Incomplete (I).
137
Appealing a Course Grade
No course grade will be changed unless the instructor certifies in writing to the Registrar that an error
in computing or recording the grade occurred. If the student believes there is just cause to dispute a grade
for a course, the procedure is as follows:
Make an appointment to talk to the course instructor(s) who issued the grade. Upon written request
from the student, the course instructor(s) shall review the case with the student and a decision shall be
made by the course instructor to affirm or modify the grade. Within ten (10) working days, the course
instructor shall notify the student in writing of the decision. A copy of the letter shall be sent to the student
and the Department Chair of the PA program.
Upon written request from the student, the Department Chairperson shall review the case with the
instructor(s) and a decision shall be made by the course instructor(s) to affirm or modify the grade. Within
seven (7) working days, the Department Chairperson shall notify the student in writing of the decision. A
copy of the letter shall be sent to the appropriate course instructor(s). The course instructor(s) has the sole
responsibility to make the official grade change.
If the student is not satisfied with the outcome of the grade dispute procedure to the Department
Chairperson, the student may then appeal in writing to the Dean of the College of Allied Health
Professions within five (5) working days. The Dean of the College of Allied Health Professions shall
review the case with the student, Chairperson of the PA program and the course instructor(s) and a
decision shall be made by the course instructor(s) to affirm or modify the grade. Within seven (7) working
days the Dean shall notify the student in writing of the decision. A copy of the letter shall be sent to the
appropriate course instructor(s) and Chairperson. The course instructor(s) has the sole responsibility to
make the official grade change.
Appealing a Clinical Education Grade
Any student who has a dispute with a grade that was assigned by their clinical preceptor, will utilize the
following appeal process:
Contact the Clinical Education Coordinators, and notify them in writing of their concerns in reference
to their clinical performance grade.
The Clinical Education Coordinators will contact the preceptor to schedule a meeting to discuss the
student’s grade. The grade may or may not be re-assigned contingent upon the information that is gathered
by the Clinical Education Coordinators. The student will be notified in writing by the Clinical Education
Coordinators of the outcome. If the student does not agree with the outcome of the investigation, he/she
may appeal this decision to the Department Chair. If the student does not agree with the Department
Chair’s decision, the student has the right to appeal to the Dean of the College of Allied Health
Professions.
Communications
Lockers: To improve the communication network and to foster student-staff and student-student
interchanges, lockers are located in the Health Sciences Center Student Commons. Students are expected
to follow the guidelines below in checking their lockers and will be held accountable for absences at
activities announced via the locker system. In the event that time constraints necessitate quick dispersal of
information, the program will disseminate this information via the U.S. Postal Service or through
telephone communication.
a. Each student will be assigned one locker.
b. During any portion of the program for which the student is present in the Physicians Assistant
Program on a daily basis, i.e., lecture series, he/she should check his locker daily.
c. During Phase I of the program, each student should check his/her locker daily.
d. During Phase II & III of the program, correspondence from the program will be mailed to the
student.
e. During any portion of the program for which the student is out of town, e.g., remote clinical site,
holidays, correspondence from the program will be mailed to the student.
Telephone:
a. During the course of the program, it is frequently necessary for members of the program staff to
contact students regarding scheduling and re-scheduling of classes, meetings, and other program

138
events, etc. Each class is responsible for developing a telephone communication network to include
names and home phone numbers for each member of the class. This "chaining" is utilized to
communicate last minute changes, announcements, etc. Each student is responsible for advising the
program departmental secretary of telephone number changes as soon as they occur.
b. Use of the program telephones is allowed only in emergency situations or with special permission
from the program faculty or staff; students are not to make or receive personal calls on the office
telephones.
c. Pagers and cell phones must be in silent/vibrate mode during all class times and examinations.
Returning from Leave of Absence While in Phase II or Phase III
A student returning from a leave of absence of 3 months or more is required to complete one ½ day
review session (arranged by the clinical education department). The review session must be completed
successfully before continuing with clinical education.
Student must:
a. Demonstrate proficiency performing
1. Complete Physical Exam
2. POP with a SOAP Note
b. Review the following videos:
Universal Precautions
Sterile Techniques
A second session may be scheduled if deficiencies are noted by the faculty.
Children in the Classroom/Labs
The PA classroom is an environment for enhanced learning and should be free from unnecessary
distraction. For this reason, children are not permitted in the classroom during examinations, no exception.
In rare
instances a child will be permitted in the classroom for lecture if:
a. an immediate childcare emergency develops, and
b. the student calls the PA program before the child is brought onto campus, and
c. permission is obtained and granted by the instructor for the child’s presence in the classroom.
During the Pediatrics Course children will be invited to class to participate in the pediatric workshop.
Any student deemed overusing this privilege, will have it revoked.
Student Academic Progress Committee
a. The Student Academic Progress Committee is comprised of department chairs and faculty members
of the College of Allied Health Professions.
b. Each year, the Student Academic Progress Committee shall periodically review the academic
achievements and the performance of all students. The names and grades of students in academic
difficulty shall be made available to the Student Academic Progress Committee by the department
chairs and faculty members.
c. After reviewing the student's achievement and performance records, the Student Academic Progress
Committee may recommend to the Dean of the College of Allied Health Professions any of the
following courses of action for a student: promotion, probation, remediation, dismissal from the
College, psychological and educational assessment and recommendation, or no action.
d. The Student Academic Progress Committee also has the responsibility of recommending to the
faculty, as a whole, the awarding of the Master of Science degree upon satisfactory completion of all
requirements for graduation as stated in the University Catalogue.
e. All recommendations of the Student Academic Progress Committee shall be in writing to the Dean
of the College of Allied Health Professions, who will make the information available to the student.
139
CURRICULUM ORGANIZATION
First Semester
Year I Students
Course # Title Sem. Hours
PA5000 CPR 0.5 (Cr/NCr)
PA5005 Medical Terminology 1 (Cr/NCr)
PA5010 Structure & Function I 5
PA5020 Clinical Skills I 3
PA5030 Physical Assessment I 4
PA5040 Health Promotion/Disease Prevention I 3
PA5050 Introduction to Adult Medicine & Pathophysiology I 5
PA5060 Pharmacology and Therapeutics I 3
PA5070 Psychosocial Dynamics 3
Total 27.5
Second Semester
Year I Students
Course # Title Sem. Hours
PA5011 Structure & Function II 5
PA5021 Clinical Skills II 3
PA5031 Physical Assessment II 4
PA5041 Health Promotion & Disease Prevention II 3
PA5051 Introduction to Adult Medicine & Pathophysiology II 5
PA5061 Pharmacology and Therapeutics II 3
HPE5206 Research Methods II 3
Total 26
Third Semester
Year I Students
Course # Title Sem. Hours
PA5100 Pediatrics 3
PA5110 OB/GYN 3
PA5120 Geriatrics 3
PA5130 Emergency Medicine 3
PA5140 Professional Roles & Responsibilities 3
PA5160 Health Care Delivery System 3
Total 18
PHASE II
Fourth Semester
Year II Students
Course # Title Sem. Hours
PA6020 Senior Seminar I 3
### Clinical Rotations I (4) 12
PA6970 Applied Clinical Project I 1
Total 16
Fifth Semester
Year II Students
Course # Title Sem. Hours
PA6030 Senior Seminar II 3
### Clinical Rotations (4) 12
PA6980 Applied Clinical Project II 1
Total 16

140
PHASE III
Sixth Semester
Year II Students
Course # Title Sem. Hours
PA6040 Senior Seminar III 2
PA7900 Advanced Clinical Preceptorship 9
PA6990 Applied Clinical Project III 7
Total 18
COURSE DESCRIPTIONS
PA 5000 Cardiopulmonary Resuscitation (0.5 credit hour, Cr/NCr)
This course is taught in accordance with the American Heart Association (AHA) guidelines. Students
will gain a basic knowledge of the resuscitation process and the required techniques. Upon successful
completion, the student will receive a certificate of completion from the AHA.
PA 5005 Medical Terminology (1 credit hour, Cr/NCr)
This course is taught in accordance with the American Heart Association (AHA) guidelines. Students
will gain the knowledge and skills, beyond basic life support, of advanced cardiac resuscitation. Upon
successful completion, the student will receive a certificate of completion from the AHA.
PA 5010 Structure and Function I (5 credit hours)
An integration of sciences: anatomy, physiology, and biochemistry as they contribute to the
understanding of clinical medicine. This course is correlated to the Introduction to Adult Medicine course.
PA 5011 Structure and Function II (5 credit hours)
Continuation of PA 5010.
PA 5020 Clinical Medical Skills I (3 credit hours)
This practical course exposes the physician assistant student to basic clinical skills used in the primary
care office. Skills include, but are not limited to, venipuncture, universal precautions, suturing, casting and
sterile procedures.
PA 5021 Clinical Skills II (3 credit hours)
Continuation of PA 5020.
PA 5030 Physical Assessment I (4 credit hours)
This course is designed to provide students with fundamental cognitive knowledge of interviewing,
formulating write-ups and physical assessment techniques. Students also learn how to analysis data and the
formulation of a therapeutic plan based on the health history, and physical examination. This course is
correlated with the Introduction to Adult Medicine.
PA 5031 Physical Assessment II (4 credit hours)
Continuation of PA 5030.
PA 5040 Health Promotion and Disease Prevention I (3 credit hours)
This course stresses the principles of wellness including detailed discussions of nutrition, exercise,
alcohol and tobacco as they relate to culturally diverse patient populations.
PA 5041 Health Promotion and Disease Prevention II (3 credit hours)
Continuation of PA 5040.
141
PA 5050 Introduction to Adult Medicine and Pathophysiology I (5 credit hours)
This course represents an introduction to clinical adult medical and surgical disorders as well as
pathophysiology from a primary health care perspective. This course is correlated with structure and
function, pharmacology, and physical assessment. It also incorporates signs, symptoms, differential
diagnosis, laboratory diagnosis and treatment modalities for selected disciplines.
PA 5051 Introduction of Adult Medicine and Pathophysiology (5 credit hours)
Continuation of PA 5050.
PA 5060 Pharmacology and Therapeutics I (3 credit hours)
This course stresses the principles of drug action and is correlated with the system orientation of the
"Introduction to Adult Medicine." Current aspects of drug therapy are studied with particular emphasis on
the activity.
PA 5061 Pharmacology and Therapeutics II (3 credit hours)
Continuation of PA 5060.
PA 5070 Psychosocial Dynamics (3 credit hours)
This course provides students with the necessary skills to diagnose and treat common mental health
disorders seen in an ambulatory family practice population. It also provides the students with information
that enable them to factor "humanity" into their assessment, diagnosis and intervention strategies. The
course also includes modules on family structure and functioning, the dynamics of aging, death and dying,
and human sexuality.
PA 5100 Pediatrics (3 credit hours)
This course will provide the primary care physician assistant student with an introduction to the basic
principles of pediatrics. This pediatric course will provide the students with the basic cognitive skills
required to obtain and perform an appropriate newborn, pediatric and adolescent history and physical.
PA 5110 Obstetrics/Gynecology (3 credit hours)
This course is designed to introduce the PA student to the fundamental principles and practice of
obstetrics and gynecology and the unique physical and emotional health care needs of female patients.
Emphasis will be placed on the pathophysiology, etiology, management and prevention of clinical
problems that transpire in a woman's life cycle from infancy through menopause. Students will also learn
the essential details of the OB-GYN clinical evaluation and strategies in the diagnosis and treatment of
common OB-GYN medical, surgical, and obstetric disorders of women.
PA 5120 Geriatrics (3 credit hours)
This course introduces the students to all aspects of geriatrics. The course provides a framework for
common geriatric illness, diseases, diagnoses and treatment. It discusses normal and pathologic changes of
aging. It explores health care financing for the elderly. Common ethical and legal issues in caring for the
elderly are discussed.
PA 5130 Emergency Medicine (3 credit hours)
This course emphasizes assessment skills in emergency medicine. It would provide students with an
overview of emergency medicine, history and physical examinations. The course will introduce current
diagnosis and treatment for commonly encountered medical emergencies. The student should be able to
develop a working knowledge and framework for the evaluation and treatment of common medical and
surgical procedures.
PA 5140 Professional Roles and Responsibilities (3 credit hours)
This course examines the different professional roles that can be assumed by a physician assistant. Also
included are discussions of the laws in which PA's are required to follow to practice medicine and the
health care delivery system.
142
PA 5160 Health Care Delivery Systems (3 credit hours)
This course will introduce the student to the current models of health care delivery systems utilized
within healthcare. It will also identify the roles of a PA within the current health care delivery systems.
HPE 5206 Research Methods II (3 credit hours)
The purpose of this course is to introduce students to a variety of research methodologies. Included will
be historical studies, case studies, observational studies, the survey, quasi-experimental designs, and
experimental designs. Generalizability issues and validity/reliability issues related to research are
presented. HPE 5106 or its equivalent is a prerequisite for this course.
PA 6020 Senior Seminar I (3 credit hours)
Senior Seminar consists of a series of examinations and discussions. Clinical skill problems, case
presentations, and problem oriented physical examinations are used as teaching tools to help the physician
assistant student understand his/her role as a practicing PA.
PA 6030 Senior Seminar II (3 credit hours)
Senior Seminar II consists of a series of examinations and discussions. The purpose of the course is to
further develop the physician assistant student's clinical skills and test-taking abilities.
PA 6040 Senior Seminar III (3 credit hours)
Senior Seminar III consists of a comprehensive examination and a problem oriented physical. The
purpose of the course is to further develop the physician assistant students' clinical skills and prepare for
the National Certification examination.
PA 6970 Applied Clinical Project I (1 Credit Hour, Cr/NCr)
Preparation of a clinical project, under the supervision of a member of the PA faculty, that will be
completed and presented in PA 6990.
PA 6980 Applied Clinical Project II (1 Credit Hour, Cr/NCr)
Continuation of PA 6970.
PA 6990 Applied Clinical Project III (7 credit hours, Cr/NCr)
In this course, the student presents the Clinical Project in partial fulfillment of requirements for the
degree of Master of Science in Physician Assistant Studies.
PA 7010 Family Practice I (3 credit hours)
A clinical rotation that provides students with experience in a primary health care setting and will focus
on medical problems most commonly encountered by a family practitioner and certified physician
assistant.
PA 7020 Family Practice II (3 credit hours)
This rotation is an extension of the Family Practice I experience and will permit students to extend their
experiences in primary health care. Students may elect to return to the site of their initial family practice
rotation or select a second type of primary care experience including such opportunities as migrant, or
Indian Health Service activities.
PA 7030 Internal Medicine (3 credit hours)
A clinical rotation that provides students with the opportunity to diagnose, manage, and treat patients in
an in/out patient setting. The student will participate in the direct care of patients including initial
interview, physical examination, hospital rounds, clinical conferences and management decision sessions.
PA 7040 Emergency Medicine (3 credit hours)
Students obtain experience in the management of acute medical and surgical care with an emphasis on
the development of skills required to treat life-threatening illness and injury.
143
PA 7050 Urgent Care (3 credit hours)
Students obtain experience in the management of acute medical and surgical care with an emphasis on
the development of skills required to treat non-life-threatening illness and injury as well as triage and
assess true emergent cases.
PA 7060 Pediatrics (3 credit hours)
Students gain knowledge in the care of infants and children, including an understanding of normal
development, and the recognition and management of common childhood illness, immunization updates
and patient education opportunities.
PA 7070 Obstetrics and Gynecology (3 credit hours)
Students learn about women's health issues: preventive care, prenatal care and post natal care, current
contraceptive technology, and medical therapeutics which aid in the well being of the female patient.
PA 7080 General Surgery I (3 credit hours)
Students are involved in the direct care of patients undergoing surgery including both pre-surgical
evaluation and post-surgical maintenance. Students may select either in-patient or out-patient surgical
settings.
PA 7090 Public Health (3 credit hours)
This rotation provides the students with an insight into epidemiology and how various public health
agencies play a significant role in health promotion and disease prevention.
PA 7110 Community Medicine Service (3 credit hours)
This rotation provides experience in community health. It exposes students to common problems seen
in family medicine as well as conditions seen in public health. This allows the student to understand how
community clinics play a significant role in health promotion and disease prevention.
PA 7120 Neurology (3 credit hours)
This rotation provides the student with the opportunity to learn initial diagnosis, differential diagnosis,
work-up and follow-up of inpatients with new or complicating neurological problems.
PA 7500 Extended Core Selectives (3 credit hours)
Students can pursue additional experience in a variety of clinical specialties and sub-specialties or they
can extend their knowledge by repeating one of the required clinical rotations. Repeatable for a maximum
of 6 credit hours. Repeating the same decimal subdivision is not permitted, except for PA7500.99.
PA 7500.01 Orthopedics
PA 7500.02 Oncology
PA 7500.03 Family Practice III
PA 7500.04 Infectious Disease
PA 7500.05 Cardiology
PA 7500.06 Cardiothoracic Surgery
PA 7500.07 Geriatrics
PA 7500.08 General Surgery II
PA 7500.09 Rheumatology
PA 7500.10 Endocrinology
PA 7500.11 Dermatology
PA 7500.12 Occupational Medicine
PA 7500.13 Trauma Surgery
PA 7500.14 Psychiatry
PA 7500.15 Otolaryngology
PA 7500.90 Directed Research/Independent Study
PA 7500.99 Other
144
PA 7900 Advanced Clinical Preceptorship (9 credit hours)
Advanced Clinical Preceptorships prepare the second year PA student for the transition from student to
primary care practitioner. This course is three months in length and provides the student with valuable
patient management data while also emphasizing continuity of care.
HONORS AND AWARDS
The following are presented on Honors Day:
Dean's Award
PA Class President Award
PA Class Morale Award
PA Class Award
Joseph and Dorothy Gendron Journalism Award
Western University PA Service Award
The President's Society Award
Linda Fox Memorial Endowment Fund Award
Guy M. Allmon Scholarship Fund Award
The following are presented at graduation:
Dean's Award
PA Class President Award
PA Class Morale Award
PA Class Award
Western University PA Service Award
Blake Award of Academic Excellence
Martha Medina Memorial Award
The Bertha Oliver Memorial Award
Andrea J. Reina Memorial Award
145
ACADEMIC CALENDAR
2000-2001
PA PROGRAM
Aug. 6-9, 2001
Orientation/Registration
Wednesday, Aug. 8, 2001
Fall Semester Tuition Due (1
st
years)
Saturday, August 11, 2001
Convocation/White Coat Ceremony
Monday, August 13, 2001
Classes begin (1st year)
Monday, Aug. 27, 2001
Fall Semester Tuition due (2
nd
years)
Saturday, September 1, 2001
Rotations begin (2nd year)
Monday, September 3, 2001
Labor Day - No Class
Monday, October 8, 2001
Columbus Day - No Class
October 18-21, 2001
CAPA Convention - No Classes
Wednesday, November 21, 2001
Thanksgiving recess - Noon
Monday, November 26, 2001
Classes Resume
Friday, December 14, 2001
Last Day of Lectures for Fall Semester
December 17-21, 2001
Finals Week
Monday, December 24, 2001
Winter Recess
2002
Monday, January 7, 2002
Classes Resume
Thursday, Jan. 17, 2002
Spring Semester Tuition Due (1
st
years)
Monday, January 21, 2002
Martin Luther King Day - No Classes
Thursday, Feb. 14, 2002
Spring Semester Tuition due (2
nd
years)
Monday, February 18, 2002
President's Day - No Classes
Monday, March 18, 2002
Spring Break Begins
Monday, March 25, 2002
Classes Resume
Monday, April 8, 2002
Honor's Day
Friday, May 10, 2002
Last Day of Lecture for Spring Semester
May 13-17, 2002
Spring Semester Finals
Friday, May 31, 2002
Graduation
Monday, June 3, 2002
First Day of the Summer Session
Thursday, July 4 - Friday, July 5, 2002
Independence Day - No Classes
Friday, August 2, 2001
Last Day of Summer Semester
146
THE PHYSICIAN ASSISTANT OATH
I pledge to perform the following duties with honesty, integrity, and dedication, remembering always
that my primary responsibility is to the health, safety, welfare, and dignity of all human beings:
I recognize and promote the value of diversity and I will treat equally all persons who seek my care.
I will uphold the tenets of patient autonomy, beneficence, non-malfience, justice, and the principle of
informed consent.
I will hold in confidence the information shared with me in the course of practicing medicine, except
where I am authorized to impart such knowledge.
I will be diligent in understanding both my personal capabilities and my limitations, striving always to
improve my practice of medicine.
I will actively seek to expand my intellectual knowledge and skills, keeping abreast of advances in
medical art and science.
I will work with other members of the health care team to assure compassionate and effective care of
patients.
I will uphold and enhance community values and use the knowledge and experience acquired as a PA
to contribute to an improved community.
I will respect my professional relationship with the physician and act always with guidance and
supervision provided by that physician, except where to do so would cause harm.
I recognize my duty to perpetuate knowledge with in the profession.
These duties are pledged with sincerity and on my honor.
147
COLLEGE OF ALLIED HEALTH PROFESSIONS
Master of Science in Health Sciences –
Licensed Physician Assistant Track
About the Master of Science in Health Sciences -Licensed Physician Assistant Track (MSHS-LPAT)
The curriculum for the on-line Master of Science in Health Sciences Licensed Physician Assistant
Track is an innovative program designed for working Physician Assistants with Baccalaureate degrees who
wish to obtain a Masters degree. Course work is designed to be multi-disciplinary in approach. Delivering
the coursework on-line takes into consideration the busy lives of everyday working Physician Assistants.
Facilities and personnel of the College of Allied Health Professions are accessible for technical support
and consultation throughout the program. The faculty includes Physician Assistants, scholars, researchers,
and administrators from a variety of backgrounds. All are committed to the multi-disciplinary approach in
teaching in the health professions.
GOALS OF THE MSHS-LPAT PROGRAM
In fulfillment of the mission of the College of Allied Health Professions, the MSHS-LPAT program's
goals are to:
1. Educate health care professionals who function as physician assistants in health
care settings.
2. Create advanced educational opportunities for physician assistants.
3. Enhance continuing professional education in health care.
4. Provide an educational service to the physician assistant community.
Objectives of the Program
1. Relate classroom and clinical instructional methodologies to a variety of health care settings.
2. Develop scholarly activities that will increase knowledge in physician assistant practice.
3. Provide an opportunity to complete a comprehensive summative examination demonstrating core
knowledge of physician assistant studies.
4. Enhance research opportunities for MSHS-LPAT candidates.
ADMISSIONS POLICIES AND PROCEDURES
Admission to the Master of Sciences in Health Science - Licensed Physician Assistant Track (MSHS-
LPAT) is through the Department of Physician Assistant Education. Students may apply for either the fall
or spring semesters. Western University is committed to admitting competitive, qualified individuals with
disabilities.
Application Requirements
Applicants must submit the following:
1. proof of Interim PA licensure or
2. copy of state PA Licensure and
3. copy of NCCPA card
4. proof of Baccalaureate Degree from an accredited institution
5. transcripts of all undergraduate course work.
6. completed application form and $35 non-refundable application fee
Candidates must meet the following academic requirements:
1. A bachelor's degree from an accredited institution.
2. A 2.5 GPA or above for undergraduate work; 3.0 for graduate work.
148
Application Procedures and Deadlines
Students may submit application materials on-line. Students are advised to submit application materials
on-line as early as possible prior to the semester in which they wish to begin their program of studies.
Deadline for receipt of application materials is no later than 30 days prior to the first day of classes for
each semester.
To request an informational brochure and/or an application, contact the admissions office at:
Office of Admissions
Western University of Health Sciences
309 E. Second Street/College Plaza
Pomona, CA 91766
(909) 469-5336
or on the Internet at http://www.westernu.edu.
In addition to submitting an application, the applicant must submit a nonrefundable application fee of
$35, and official transcripts from all undergraduate and graduate institutions attended.
Transfer of Credits
The maximum number of graduate units that may be transferred from another institution offering
programs of graduate studies is nine semester units. Only graduate credit relevant to the MSHS-LPAT
Program at Western University completed within the last five years may be applied toward completion of
the master's degree. To be considered for transfer credit, the course must have been taken after the award
of a bachelor's degree and be eligible for graduate studies credit at the issuing institution. The student must
have received a grade of B or above in the course. An official transcript and a course description should be
submitted to the Chair of the PA Department. The PA faculty will determine whether or not work
undertaken at other institutions qualifies for transfer. No transfer credit will be given HSCI 5999.
Re-Admission
Graduate students who have not been enrolled for more than one calendar year must submit a new
application form and fee, unless other arrangements have been made at the time of withdrawal/leave from
the program. The application will be assessed according to the current admissions policies, and students
will be required to fulfill program requirements in place at the time of readmission.
Registration policies and procedures
Prior to each semester, a class schedule is compiled and made available to students. All candidates for
the MSHS-LPAT degree are required to pre-register on-line. Advisement is available in order to promote
greater efficiency in the registration and enrollment process. Enrollment occurs during the weeks prior to
the first class meetings, on an appointment basis. Enrollment is available biannually, during the Fall and
Spring semesters. Students may register at the initial class on-line, but could be denied admission to a
specific class due to on-line availability. An individual must enroll for a minimum of six (6) semester
hours of credit for each semester in which they wish to be identified as students.
New Graduate Students
New graduate students are notified on-line of their admission status. This notification will include a list
of courses available during the next semester and the necessary registration materials. Completed
registration materials and fees may be submitted through the mail, or in person, prior to the first week of
classes.
Continuing Graduate Students
Continuing students will receive registration information and materials on-line prior to the beginning of
the semester. Should this information not arrive for any reason, it is the student's responsibility to contact
the office of Student Affairs for the appropriate materials. Completed registration materials and fees may
be submitted to the Registrar on-line, through the mail, or in person, prior to the first week of classes.
149
Late Registration
Students must follow the registration procedures and timelines printed in the Class Schedule provided
at the beginning of each regular semester. The date of registration and late registration are listed.
Appropriate fees for late registration will be assessed.
Add/Drop and Withdrawal from Courses
In order to add or drop a class, the student must obtain a Change of Registration form on-line, complete
and submit it prior to the end of the third week of classes of each semester. Withdrawal from a course (not
the program) requires completion and submission of the appropriate withdrawal form. Please note that this
will not result in an "incomplete" (I) grade.
ACADEMIC REQUIREMENTS
Course Load
The program is designed to be completed in two academic years.
A graduate student at Western University of Health Sciences must enroll in at least six semester hours
per term to be considered full-time. To be considered full-time when enrolled in fewer than six hours, the
student must be registered in all remaining courses necessary for completion of the graduation
requirements for the master's degree.
Reasonable Academic Progress
All students are expected to make reasonable progress each year toward the degree objective. Full-time
graduate students are considered to be making reasonable academic progress when they maintain an
overall GPA of at least 3.0 and complete 16 semester hours during the calendar year. Both part-time and
full-time students must complete the graduation requirements within the time limits described under
Graduation Requirements. For part-time students, reasonable academic progress will be determined by the
faculty on an annual basis upon consultation with the student. A letter specifying terms of the continued
enrollment will be sent on-line to the student.
Student Rights and Responsibilities
It is the responsibility of the student to be familiar with the contents of the catalogue and to observe all
policies and procedures relative to the completion of requirements for the graduate degree that were in
effect at the time of initial enrollment in the MSHS-LPAT Program.
A student may opt to complete the program of study and degree requirements described in the
catalogue at the time of his or her graduation, provided all revised policies of the later catalogue are
followed. Students are required to keep the Registrar informed of their current address and telephone
number. Forms for this purpose are available in the Student Affairs Office.
Grading System
Official grades are turned in to the Chair of the Department of Physician Assistant Education from the
course instructors. Official grade reports are then prepared by the Registrar and mailed to the student.
Western University of Health Sciences makes use of letter grades, which may include a plus/minus (+ / -)
system of grading. A four-valued letter grade scale will be given, indicating:
Grade Quality Points
A - Excellent 4
B - Good 3
C - Satisfactory 2
U - Unsatisfactory 0
I - Incomplete 0
Au - Audit 0
W - Withdrawal 0
Cr - Credit 0
NCr - Non-credit 0

150
Courses are rated at one semester hour for each 12 contact hours. The grade point average is calculated
at the end of each semester as the sum of earned grade points divided by the sum of semester hours passed
and failed. A cumulative grade point average will be calculated and posted on the transcript.
No grade will be changed unless the instructor certifies in writing that an error in computing or
recording the grade has occurred or that the student has completed course requirements for an Incomplete
grade or remediated an Unsatisfactory grade.
Incomplete
An Incomplete grade ("I") will only be assigned to students whose professional commitments and/or
personal responsibilities prevent him or her from completing the requirements of the course. A student may
remove an incomplete by completing course requirements within the following academic semester. Should
extenuating circumstances arise, the student may petition for a one-semester extension to complete the
course work. Arrangements for the Incomplete and its removal must be approved by the instructor prior to
the end of the semester in which the original Incomplete grade was assigned. Grade changes must be
certified by the instructor prior to the end of the semester following the original grade assignment.
Academic Standing
An overall grade point average of 3.0 (B) must be maintained during graduate work undertaken at
Western University of Health Sciences in order to qualify for advancement to candidacy. A 2.0 (C) grade
earned in any class may be applied toward graduation only if the overall grade point average at the time of
application for graduation continues at a minimum 3.0 (B) overall grade point average. Any grade below a
2.0 (C) may not be applied toward graduation. Any student whose grade point average falls below a 3.0
(B) average will be placed on probation.
Graduation Requirements
A 33-unit requirement exists for the award of the Master of Science-Licensed Physician Assistant
Track. A total of 18 credit hours of Core Requirements are required of all MSHS-LPAT candidates.
Students need to select at least 15 credit hours of Selectives and are responsible for finding their Clinical
Residency requirement. The student will also be required to complete one of the following: 1) thesis, or 2)
special project.
CORE MASTER OF SCIENCE
HPE 5106 Research Methods I 2 credit hours
HPE 5206 Research Methods II 3 credit hours
HSCI 5016 Success Strategies for Distance Learning 1 credit hour
HSCI 5999 Thesis/Special Project 5 credit hours
Total 11 credit hours
CORE HEALTH SCIENCE
PA 5071 Advanced Studies in Special Populations I 3 credit hours
PA 5072 Advanced Studies in Special Populations II 3 credit hours
PA 5160 Health Care Delivery Systems 3 credit hours
Total 9 credit hours
CORE PHYSICIAN ASSISTANT
HSCI 5000 Pathophysiology 3 credit hours
HSCI 5012 Pharmacotherapeutics 3 credit hours
HSCI 5014 Community Health Education 3 credit hours
HSCI 5018 Practicum in Community Health Education 3 credit hours
HSCI 5010 PA Assessment 1 credit hour
Total 13 credit hours
Grand Total 33 credit hours
151
Language Requirements
No foreign language class work or test of proficiency is required of candidates for the MSHS-LPAT
degree.
Time Limits
All requirements for the MSHS-LPAT must be fulfilled within five years from the date of initial
registration. Extensions of this time limit may be granted through petition to the faculty.
Advancement to Candidacy
At least one semester prior to when the student plans to complete the unit requirements, he or she must
file an "Application for Advancement to Candidacy" form. The Master of Science in Health Sciences –
Licensed PA Track Degree is awarded following satisfactory completion of all coursework, including
thesis/special project. Names of candidates for graduation are presented to the Student Academic Progress
Committee, the Dean of Allied Health Professions, and to the Western University of Health Sciences
faculty for approval.
The Master of Science-Licensed Physician Assistant Track degree is awarded following satisfactory
completion of all course work. The student will also be required to complete one of the following: 1)
thesis, or 2) special project. Prior to graduation, the student must complete the Master of Science-Licenses
Physician Assistant Track "Application for Advancement to Candidacy" form. Names of candidates for
graduation are presented to the Student Academic Progress Committee, the Dean of Allied Health
Professions, and to the University Board of Trustees for approval.
All students who have completed graduation requirements must attend, in person, and participate in the
Commencement program at which time the degree is conferred. The President may approve exemptions to
this last requirement.
Summary
A student will be recommended for the degree of Master of Science-Licensed Physician Assistant
Track provided he or she:
1. Has satisfactorily completed the 33-unit course requirement in the MSHS-LPAT curriculum.
2. Has completed one of the following: 1) thesis, or 2) special project.
3. Is not on probation and has completed all prescribed academic requirements.
4. Has complied with all the legal and financial requirements of the University as stated in the
University catalogue;
5. Has demonstrated no serious deficiencies in ethical, professional, or personal conduct, as defined
previously,
6. Attends in person and participates in the Commencement program at which time the degree is
awarded, unless special permission has been granted by the President of the University. If the President
grants special permission to be excused from graduation, the graduate may be required to present
himself or herself to the appropriate Dean at a later date in order to take the required oath (if relevant)
to receive his or her diploma.
152
TUITION AND FEES
Schedule of Fees
$225 Unit cost per semester hour (33 semester hours minimum for MSHS-LPAT
degree)
Other Fees and Expenses
$35. Application Fee
$50. Continuous Registration Fee
$30. (per day) Late Registration Fee
$10 Lost ID Badge
$5. (each) Copy of Official Transcript
$0.25 (per page) Copy of Student File Material
Tuition and fees are subject to change without notice upon approval by the Board of Trustees. All fees
are mandatory for each student and are non-refundable. Obligation for payment in-full of tuition and fees is
due upon matriculation. The MSHS-LPAT Program can offer a schedule of divided payments for students
demonstrating financial need (for more information see the Bursar).
COURSE DESCRIPTIONS
The Master of Science-Licensed Physician Assistant Track is designed to be completed in one to two
academic years. The curriculum is designed to be multi-disciplinary in approach. This program has been
designed to accommodate the needs of the everyday working PA. The courses below comprise the Master
of Science-Licensed Physician Assistant Track curriculum offered by the Western University of Health
Sciences.
Core Master of Science in Health Sciences Requirements
HSCI 5016 Success Strategies for Distance Learning (1 credit hour)
This course provides new students with a comprehensive introduction to Western University's distance
learning program for Physician Assistants. Following an overview of the most important services, policies,
instructional methods, and resources, the student will have an opportunity to assess their own readiness for
the program. Knowledge and skills derived will help ensure successful completion of the program.
HPE 5106 Research Methods I (2 credit hours)
This introductory course is designed to prepare the health professions student to understand principles
for the analysis and interpretation of quantitative date in health professions education research. It will
include measurement theory, the graphical presentation of date, probability theory, and the use of
descriptive and inferential statistics in the interpretation of data. As a result, the student will be able to
read original research reports in a more critical manner.
HPE 5206 Research Methods II (3 credit hours)
The purpose of this course is to introduce student sot a variety of research methodologies. Included
will be historical studies, case studies, observational students, the survey, quasi-experimental designs, and
experimental designs. Generalizability issues and validity/reliability issues related to research are
presented. HPE 5106 or its equivalent is a prerequisite for this course.
HSCI 5999 Thesis/Special Project (5 credit hours)
Students are required to write a thesis or special project .
153
Core Health Science Courses
PA 5071 Advanced Studies in Special Populations I (3 credit hours)
This course surveys issues confronted by healthcare providers while treating and evaluating patients
with existing disabilities. Topics include the history of disabilities in the health professions, ethics,
communication, language, accessibility, and the responsibilities of healthcare providers under the
Americans with Disabilities Act.
PA 5072 Advanced Studies in Special Populations II (3 credit hours)
This second exploration of Special Populations builds on themes and concepts presented in PA 5071.
PA 5160 Health Care Delivery Systems (3 credit hours)
This course introduces students to current models of health care delivery utilized in the American
health care system. It will also explore the current role of a PA within the system and how it is evolving.
Core Physician Assistant Courses
HSCI 5000 Pathophysiology (3 credit hours)
This course integrates basic knowledge of human anatomy and physiology with pathological changes in
various body systems to facilitate the diagnosis and treatment of common, acute, chronic, and complex
health problems. The differential impact of these health problems and their treatment on patients
throughout the life cycle (e.g., pediatric, adult/family, obstetric, geriatric) will also be discussed.
HSCI 5010 PA Assessment (1 credit hour)
The PA Assessment course provides prospective masters students with a means of validating their
current knowledge of Physician Assistant practices. This comprehensive course, which is based on
concepts assessed through the Physician Assistant National Certification Exam or PANCE, may be
completed entirely through independent study, using materials provided over the world wide web.
HSCI 5012 Pharmacotherapeutics (3 credit hours)
This course presents advanced pharmaceutical principles and practices that will facilitate the PA’s
ability to prescribe and monitor the effects of medications on patients with common, acute, chronic, and
complex health problems.
HSCI 5014 Introduction to Community Health Education (3 credit hours)
This course provides an overview of the development and implementation of patient education
programs in the community and in acute, long-term clinical settings. Models for preparing health
education programs will be presented, including design considerations, appropriate for age, ethnic,
cultural, and socioeconomic differences. Assessment of need, developing objectives, designing learning
activities, implementation, and evaluation are emphasized. Practical application will include the design
and implementation of one unit of instruction based on a health education subject.
HSCI 5018 Practicum in Community Health Education (3 credit hours)
This course provides students working in the community with an opportunity to demonstrate their
application of community health education principles in the practice setting. The student will be expected
to design a community health project to improve healthcare outcomes.
154
ACADEMIC CALENDAR 2001-2002
Fall Semester
Sept. 4 - 14, 2001
Registration
Wednesday, Sept. 5, 2001
Fall Semester Tuition Due
Monday, Sept. 10, 2001
Classes begin
Friday, Sept. 21, 2001
Last day to add/drop class
Monday, Oct. 8, 2001
Columbus Day (no class)
Friday, Nov. 16, 2001
Application Deadline for Spring 2002
Wednesday, Nov. 21, 2001
Thanksgiving recess (noon)
Monday, Nov. 26, 2001
Classes resume
Friday, Dec. 21, 2001
Last day of classes
Last Day to file for
Advancement to Candidacy
Spring Semester
Jan. 3-11, 2002
Registration
Monday, Jan. 7, 2002
Classes begin
Monday, Jan. 21, 2002
Martin Luther King, Jr. holiday (no class)
Friday, Jan. 25, 2002
Last day to add/drop class
Monday, Feb. 18, 2002
President's Day (no class)
Monday, Mar. 18, 2002
Spring Break begins
Monday, Mar. 25, 2002
Classes resume
Monday, April 8, 2002
Honors Day
Wednesday, May 1, 2002
Last day for Oral Examinations
Friday, May 10, 2002
Last day of classes
Friday, May 31, 2002
Commencement
Summer Semester
Monday, May 27, 2002
Memorial Day (no classes)
May 28-31, 2002
Registration
Thursday, July 4, 2002
Independence Day (no classes)
Monday, July 8, 2002
Classes resume
Last day to add/drop class
Friday, August 2, 2002
Last day of classes
155
COLLEGE OF GRADUATE NURSING
Master of Science in Nursing/Family Nurse Practitioner Program
Post-Masters Family Nurse Practitioner Track
Advanced Practice Nurse to Family Nurse Practitioner Track
Master of Science in Nursing Track
MISSION
The Western University College of Graduate Nursing (CGN) has established a community for learning
that offers bachelor-prepared nurses an opportunity to expand their education through a web-based Master
of Science in Nursing and Family Nurse Practitioner certificate program in preparation for providing
primary health care for their community. The CGN faculty members foster excellence, creativity,
innovation, self-reflection, personal and professional accountability, collaboration, cultural sensitivity, a
passion for caring, leadership, and lifelong scholarship through a mentoring relationship with students.
In accordance with the mission of Western University of Health Sciences, the faculty endeavor to:
• improve the health of the community through the preparation of professional advanced practice nurses
with expertise for effective provision of family-centered care for primary health care needs of a
rapidly changing society; and,
• develop each student’s potential, reflect democratic values and ethical principles through role
modeling, sharing of knowledge, caring, and advocating mutual respect.
PHILOSOPHY
The College of Graduate Nursing is distinguished by the faculty’s beliefs about nursing, persons,
environment, health and nursing education:
Nursing, as a professional discipline, is an art and a humanistic science of caring. The art of nursing is
in its understanding of the meaning of a holistic health-illness experience and the perception of the moral
and ethical significance of care, as well as the integration of technical skill with relevant theory. The art of
nursing employs critical thinking and respect; it fosters open and effective oral and written communication
with clients and colleagues. The humanistic science of nursing is the generation and application of the
body of theoretical nursing knowledge, behavioral and natural science, the humanities, and the arts,
employed in a caring, respectful manner.
The professional practice of nursing is the directing of knowledge, competencies and processes toward
assisting persons to achieve quality of life, health, well-being, or peaceful death. Advanced practice
nursing competencies are complex psychomotor and interpersonal skills, leadership, collaboration, self-
evaluation, and scientific application and inquiry that are guided by professional standards. Processes
include critical thinking, accountability, problem solving, decision-making, caring, advocacy, and
involvement. Knowledge for Advanced Practice Nursing is built upon the foundation acquired in a
Bachelor of Science in Nursing and its related arts and sciences, as well as information gained from prior
nursing experience. Expertise for Advanced Practice focuses on socio-cultural, ethical, economic and
political issues, advanced technology, theory, research, and advanced physical and psychological sciences.
Evidence-based professional nursing practice demands recognition that each individual has unique needs
that can be assessed and incorporated into a research-based nursing plan.
Persons who participate in family-centered nursing care are individuals with unique lifestyles,
knowledge, beliefs and values, needs, and goals and are able to make autonomous decisions. These clients
of nursing involve complex biological, behavioral, emotional, sociocultural, philosophical and spiritual
dimensions and interact dynamically with their environment. Clients interact through relationships with
families, in various forms, and communities. Persons have a right and responsibility to participate
collaboratively with nurses and other health professionals in decisions and shared accountability for
outcomes.
156
Environment is both the internal and external contexts of the individual. Environment involves
reciprocal multidimensional and dynamic forces that affect the person’s health and well being.
Health is a multidimensional, adaptive state of being reflecting internal and external environmental and
developmental influences. Health is a relative condition, characterized by wellness, illness, disease, or
dysfunction. Health may be a reflection of individual perceptions of balance and harmony.
Nursing Education is a process that provides opportunities to expand and extend knowledge for
continued growth and competency of the individual and the profession. It draws on multiple disciplines
and involves organized learning experiences that augment previous knowledge and skills in preparation for
professional nursing practice. Nursing education is a flexible process that fosters creativity and
independent and critical thinking. We value self-directed learners, continual learning, and active
engagement in a teaching/learning partnership. The educational process supports personal, social and
intellectual development while assisting students to attain academic and professional goals. Through the
provision of meaningful learning experiences, nursing education seeks to assist the learner to formulate
and structure nursing knowledge, while distinguishing relevant from non-relevant information and
developing safe and effective nursing practice. The educational program seeks to evoke honesty,
excitement of discovery, encourage self-expression and serve as a catalyst for lifelong learning.
Teachers and learners in the learning community engage in interactive processes that enhance the
potential and respect of each person. Teachers act as facilitators, and through their expertise and skill, are
role models for student professional practice. The faculty as a whole focuses on the provision and
organization of the curriculum and provides a milieu that encourages questioning, growth and mutual
evaluation.
The CGN faculty believes that students are active, self-directed, adult learners who are committed to
safe and effective professional practice and rigorous courses of study. Students are accountable for
integrity of academic accomplishments, professional practice and self-assessment. Students bring unique
backgrounds and have individual goals that create differing responses to the learning process. Learning is
a personal responsibility.
ACCREDITATION
The Western Association of Colleges and Universities accredits Western University of Health
Sciences. In addition, the programs of the College of Graduate Nursing are Board of Registered Nursing
approved and designed to comply with national accrediting and approval agencies. Graduates are eligible
to apply for state certification and to sit for the appropriate national certification examinations. The
College of Graduate Nursing has completed the process for national professional accreditation through the
Commission on Collegiate Nursing Education (CCNE) and anticipates approval in Fall 2001.
OUTCOME COMPETENCIES FOR GRADUATES
Graduate education for Advanced Practice Nursing is based on undergraduate nursing knowledge and
experience. The CGN places emphasis on critical thinking, clinical competence, communication, decision-
making, accountability, writing, and technological competence.
The course of study, including specifically stated learning activities, is a series of sequential courses
designed to assist learners in attaining the following behaviors prior to being approved for program
completion.
Graduates of the Western University of Health Sciences College of Graduate Nursing, as candidates for
state and national certification will:
1. Critically analyze literature for the purpose of evidence-based advanced nursing practice, education,
and life-long scholarship.
2. Participate in the development of new nursing knowledge through the application
and development of theory and research.
3. Apply knowledge from the humanities and physical, social, psychological, nursing, medical, and
pharmacological sciences to decision-making in order to provide and evaluate accountable primary
health care which is commensurate with professional and legal parameters of the role of Family Nurse
Practitioner.
4. Provide individualized client and family-centered health care that demonstrates recognition of
reciprocal environmental interaction and diversity of socio-cultural values and beliefs among members
of a rapidly changing society.
157
5. Apply comprehension of changing national and local public policy related to health care standards,
health care systems and financing when planning and providing health care for individuals, families,
and communities.
6. Empower client collaboration and decision-making for desired health care outcomes and quality of
life through advocacy, caring, and the application of critical thinking skills, theories of learning and
communication, and ethical principles.
7. Integrate health promotion, illness prevention, and health maintenance strategies into holistic health
care provided for diverse individuals, families, and communities
8. Provide leadership through participation in professional and community development activities and
advocacy of the advanced nursing practice role.
9. Demonstrate mastery of traditional and electronic access to information resources for research,
study, and practice.
CURRICULUM
The College of Graduate Nursing currently offers two Post-Master’s Family Nurse Practitioner tracks,
a Master of Science in Nursing track, and a combined Master of Science in Nursing/Family Nurse
Practitioner program.
The Master of Science in Nursing/Family Nurse Practitioner Program (MSN/FNP) curriculum requires
the completion of 50 semester units over a two- or three-year period. The Post-Masters Family Nurse
Practitioner (FNP-only) Track curriculum requires 41 semester units for completion and can be completed
in one year. Both of these tracks require the completion of 675 preceptored clinical hours.
The Advanced Practice Nurse to Family Nurse Practitioner (APN-FNP) track requires 20 semester
units for completion and can be completed in one year. The APN-FNP track requires the completion of
180 clinical hours.
The Master of Science in Nursing track requires 25 semester units to be completed in a year. This
degree track is designed for Advanced Practice Nurses.
Graduates will be prepared to meet the criteria established by the California Board of Registered
Nursing as advanced practice nurses. Nurse practitioners work in a variety of health care settings
independently, or in groups of health care professionals, under collaboratively developed and agreed upon
standardized procedures.
Instructional Design: Distance Learning
The College of Graduate Nursing programs are designed for the adult learner. The design uses
educational and instructional learning theories that emphasize outcome competencies as the desired goal,
rather than time on task, and individualized instructional strategies as well as classroom and clinical
instruction.
12 Month Academic Year
The twelve month academic calendar begins in August and includes three 15-week semesters with two-
week breaks between each semester.
Integrated Courses
For the clinical programs (MSN/FNP or FNP-only) health care issues are studied across the life span
with a focus on groups of specific health care problems, namely, Common, Acute, Chronic and Complex
health care problems for each age group. The course of study is planned to allow for integration of
knowledge and skills across each area of study (courses).
Essential Intellectual Skills
In addition to essential academic content and performance skills, each course requires learning
activities that foster intellectual skill development for critical thinking and decision making as well as oral
and written communication.
Web-based Learning
The instructional modality that is most evident in this curriculum is web-based learning. The majority
of courses include required asynchronous discussion sessions in which students and faculty participate in
158
collaborative learning of the assigned readings. Students are expected to be on-line and engaged in
learning activities from the first day of the first semester. The CGN Web site is designed to provide the
learner with the information needed to be successful in each course including learning objectives, content,
learning activities, evaluation methods and grading criteria.
Weekend Seminars
Each semester students are required to attend two intensive, two- to three-day weekends on campus.
These classes provide valuable time for faculty and peer interaction, student presentations, lectures,
clinical and didactic testing, skills laboratories, and selected clinical practice with faculty.
Culminating Experience
Master's degree education usually culminates with a required research or research-based project or
thesis. The MSN/FNP program and MSN programs, however, require that each student complete a project
that features the implementation of a clinical improvement project (one credit hour). Students enrolled in
the MSN/FNP program must complete a minimum of 540 clinical hours prior to beginning their
culminating project in enrolling and CGN 5608
Program Completion
Students who have met the following requirements will be considered candidates for the degree of
Master of Science in Nursing and/or Family Nurse Practitioner Certificate:
• Completion of all course requirements with a minimum overall GPA of 3.0
• Completion of 675 clinical practice hours (MSN/FNP and FNP-only) or 180 hours for APN-FNP
students. Students must satisfactorily demonstrate all clinical competencies.
• Completion of the culminating experience project (MSN/FNP and MSN students).
• Has complied with all the legal and financial requirements of the University as stated in the University
Catalogue.
• Has demonstrated no serious deficiencies in ethical, professional or personal conduct as outlined in
Standards of Professional Conduct
• Students enrolled in Post-Master's Tracks (APN-FNP or FNP-only) will be candidates for the FNP
Certificate only
Unless the President of the University has granted special permission, all students must attend in person
and participate in the Commencement program at which time the degree is conferred. If the President
grants special permission to be excused from graduation, the graduate may be required to present himself
or herself to the Provost Executive Vice President of Academic Affairs or appropriate Dean at a later date
in order to receive his or her diploma.
ADMISSION POLICIES
Prerequisite Requirements for MSN/FNP Program*
• Bachelor of Science in Nursing** from a National League of Nursing (NLN) or Commission on
Collegiate Nursing Education (CCNE) accredited program
• GPA of 3.0 overall in the last 60 semester units or 90 quarter units
• Pathophysiology
• Statistics
• Registered Nurse (RN) licensure in the state where preceptored clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
Prerequisite Requirements for Post-Masters Track (FNP-Only)*
• Master of Science in Nursing or related field
• BSN in Nursing** from a National League of Nursing (NLN) or Commission on Collegiate Nursing
Education (CCNE) accredited program
• GPA of 3.0 overall in the last 60 semester units or 90 quarter units
• Pathophysiology
• Statistics
• Registered Nurse (RN) licensure in the state where preceptored clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
159
Prerequisite Requirements for MSN-only Track*
• BSN Degree in Nursing** from a National League of Nursing (NLN) or Commission on Collegiate
Nursing Education (CCNE) accredited program
• Nurse Practitioner, FNP, PNP, Women's Health, Adult, GNP, CRNA, CNM, or CNS
• GPA 3.0 overall in the last 60 semester units or 90 quarter units
• Statistics
• Registered Nurse (RN) licensure in the state where preceptored clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
Prerequisite Requirements for Advanced Practice Nurse to Family Nurse Practitioner (APN-FNP)
Track
• Master of Science in Nursing or related field
• BSN in Nursing** from a National League of Nursing (NLN) or Commission on Collegiate Nursing
Education (CCNE) accredited program
• GPA of 3.0 overall in the last 60 semester units or 90 quarter units
• Pathophysiology
• Statistics
• Registered Nurse (RN) and/or Nurse Practitioner (NP) licensure in the state where preceptored
clinical hours will be completed
• 1 year experience as a Registered Nurse (RN)
• Verification of Advance Practice Nurse Specialty
*Students who do not meet the requirements for admission may petition the Admissions Committee for
special consideration.
** Bachelors in a related field will be reviewed on a case-by-case basis.
Requirements for Admissions (All Tracks)
• Completed Application
• Three Letters of Reference (faculty & employers within past two years)
• Resume
• Personal Statement which addresses your understanding of advanced practice nursing, personal career
goals and how your background strengthens your aptitude to become an Advanced Practice Nurse
• Application Fee of $60
• Official transcripts from all colleges/universities attended
• All graduates must agree to sit for the national certification examination within six months of
graduation
Decisions of the Admissions Committee regarding the admission of applicants to its programs are final.
Computer Requirements
The following is a list of computer equipment necessary for the Web-based programs:
• PC System - Minimum 133 MHz Intel Pentium® processor or equivalent
• 100 MB of free hard disk space
• Minimum 32 MB RAM
• Modem - 56k or higher
• Newest version of Internet Explorer
• Windows 95 or higher
• New version of Microsoft Office Suite (Standard Suite or higher)
• New version of virus protection that supports weekly updates
• CD-ROM drive
• 16-bit sound card and speakers
• Internet service provider (flat rate recommended)
• Printer
• Real Player plug-in, G2 or better
160
• Dedicated telephone line (recommended)
• E-mail account (by registration)
MSN-Harbor Track
In conjunction with the Harbor-UCLA Research and Education Institute's Women's Health Care Nurse
Practitioner Program, an accelerated Master of Science in Nursing degree is available for graduates and
currently enrolled students of the Women's Health Care Nurse Practitioner Program. For more information,
please contact the Western University College of Graduate Nursing. Students admitted to this track must
complete at least 17 units of Western University coursework. Additional units may be required based
upon assessment of transfer coursework.
REGISTRATION
Following completion of the admissions procedure and written documentation of acceptance into
Western University's College of Graduate Nursing, an orientation packet will be mailed directly to the
student. All students will complete registration at the campus-based orientation in Pomona. Registration
will be completed via mail for continuing students and will be done annually prior to each academic year.
Orientation and Pre-Program Independent Study
All students enrolled in the College of Graduate Nursing will be required to complete two mandatory
seminars on the Pomona campus. Orientation will include computer skill training (e-mail, e-mail
attachments, address book use, file management, and Microsoft software use), an introduction to
computer-based learning, and an overview of Western University curriculum. Students will complete
registration, purchase medical equipment and orient to the services of the University at this time. Students
will begin a Strategies for Success course, which is an example of Western University of Health Sciences'
computer-based courses. Students enrolled in Advanced Physical Assessment will begin skills training.
Students who successfully complete the Advanced Physical Assessment course will be able to begin
their clinical preceptored experience.
Medical Information
Verification of the following must be on file in the Office of the Registrar at the time of registration:
• Completion of Western University's History and Physical form
• Medical clearance for participation in program/clinical
• A recent (within past six months) PPD or Chest X-ray report indicating that the student is free of
tuberculosis (all students). Students are required to submit documentation of PPD/Chest X-ray
annually while enrolled at Western University
In addition, student enrolled in clinical tracks must file:
• Verification of immunization or immunity for: Polio, MMR, Diphtheria/tetanus (within past 10 years)
and completion of the Hepatitis B series
• Current CPR certification (and maintained throughout the program of study)
Health Insurance
All students must be covered by health insurance throughout the program. Proof of health insurance must
be provided at the time of registration annually.
TUITION AND FEES
By action of the Board of Trustees, the tuition and fees for the 2001-2002 year are as follows:
MSN/FNP Program 50 units @ $450/unit
FNP-Only Track 41 units @ $450/unit
APN-FNP Track 20 units @ $450/unit
MSN-Only Track 25 units @ $400/unit
MSN-Harbor Track 17 units (minimum) @ $400/unit
Student Body Fee $40/year
161
Other Fees and Expenses
Application Fee $60
Required Textbooks $1500 MSN/FNP & FNP first
year (approximate)
Medical Equipment $400 MSN/FNP & FNP students
(approximate)
Computer with Modem $1500 (approximate)
Lodging/Meals/Travel varies, depending on distance and mode of travel.
Lost ID Badge $10
Note: All tuition and fees are subject to change.
Library Services
Western University's library resources can be accessed on the Internet at: http://www.westernu.edu.
Database access is available to distance students following registration. Nursing students will access the
internet sites for some resources and perform database searches for class assignments or research projects.
Full text articles are not always available via the World Wide Web, therefore, students are expected to
utilize traditional library services for research assignments, whether in the student's community or near
their home
Required Supplies for Clinical
Physical Exam Equipment:
• Lab Coats (to be worn at all times)
• Name Tag (to be worn at all times)
• Ophthalmoscope
• Otoscope
• Pen Light
• Reflex Hammer (brush & pin set)
• Ruler (cm)
• Stethoscope
• Tuning Fork # 512
• Hand Held Snellen Chart
Bookstore
Textbooks, medical equipment and software are available through the University Bookstore. All items
can be ordered by phone and mailed directly to your home using a credit card.
ACADEMIC POLICIES AND PROCEDURES
Academic/Clinical Advisement
Entering students are offered academic advisement both on-line and in person as they prefer. On-going
students have the opportunity to make appointments to see the designated faculty advisor or individual
instructors on-line, by appointment, or on any on-site Seminar Weekend. All students must meet with an
advisor in the semester prior to their anticipated completion date for a final review of graduation
requirements and approval to file for graduation. All students will be assigned a faculty advisor during the
first semester.
Standards of Academic Performance
An overall grade point average of 3.0 is required for graduation. The curriculum is designed to assure
that every graduate will demonstrate the desired level of performance for all Outcome Competencies (See
section on Curriculum). In addition, graduates are expected to demonstrate critical thinking skills as well
as excellence in written and oral communication.
162
Academic Progression
The College of Graduate Nursing offers a variety of academic tracks for flexibility of program
completion. Part-time students will need to work with an academic advisor to complete a Plan for
Program Completion. Therefore, it is expected that each student will enroll in and successfully complete
every course in a sequential progression. An administrative fee will be charged for additional semesters
that exceed the timeframe for the program/track and are needed to complete coursework.
A passing grade of a "B" is required for each theory course. Students who earn less than this passing
grade and wish to continue in the program must remediate to progress in the program.
Minimum competency, as outlined in course syllabi for clinical courses, is required to achieve a
passing grade of “Credit”. A grade of “No Credit” is the equivalent of a “U” grade for 7570 courses. A
“U” denotes an unacceptable level of performance, and students are not able to progress in the program.
(See Evaluation and Grading below)
Student Academic Progress Committee
The Student Academic Progress Committee is comprised of a minimum of two faculty members, the
Dean, and is chaired by the Academic Coordinator. The committee chair will be responsible for
communicating all recommendations of the committee in writing to the student and Dean.
The Student Academic Progress Committee shall periodically review the academic achievements and
the performance of all students. Following review of a student's achievement and performance, the
Student Academic Progress Committee Chair may recommend to the Dean any of the following courses of
action for a student: promotion, probation, remediation, dismissal from the University, psychological
and/or education assessment and other appropriate recommendations.
The Student Academic Progress Committee also has the responsibility of recommending to the faculty
as a whole the awarding of the degree of Master of Science in Nursing to all students who satisfactorily
complete all requirements for the Master of Science in Nursing/Family Nurse Practitioner Program or
MSN-only Track. Students completing all requirements for the AFP-only or APN-FNP tracks will be
eligible for state licensure as a Family Nurse Practitioner.
Evaluation and Grading
Competency-based learning is the underlying principle for the instructional design of the program and
the evaluation of student achievement. Each course has specific learning objectives, evaluative criteria and
expected outcomes. Assessment methods are stated clearly in each syllabus.
The cumulative letter grade of “B” or better must be attained for each course to indicate competency
for this graduate program. The grade for each evaluative component for courses 5015, 5401-3, 5550,
5501-2, 5601-8, 5950, and 7570 must be at least a “B” or 80% to demonstrate an acceptable level of
performance and enable the student to progress in the curriculum. The grade for each evaluative
component for courses 5000, 5101-2, 5200, 5301-2, 5611, 5801-2, 5850, and 5990 must be at least a “C”
or 70% to demonstrate an acceptable level of performance and enable the student to progress in the
curriculum.
Grade point average is based on the following numerical values for letter grade:
A = 4.0 Achievement of an “A” for a course exceeds the acceptable level of
performance in a graduate level program.
B = 3.0 Achievement of an “B” for a course meets the acceptable level of
performance in a graduate level program.
C = 2.0 Achievement of a “C” minimally meets the requirement for evaluative
components within a course. Achievement of a “C” for a course grade
does not meet the performance level for this graduate level program.
(See section on Remediation).
U = 0 Achievement of an “U” denotes an unacceptable performance.
Students receiving a “U” grade are not able to progress in the program.
Students who do not meet the remediation standards for an Incomplete
will be given the grade of “U”. Students who receive a “U” for any
course will be unable to progress in the curriculum without a formal
review by the Student Academic Progress Committee. If the
163
Committee finds that the student demonstrates the potential for
remediation, then the student will be placed on Academic Probation
with a formal signed progression contract. A signed copy of this
contract will be filed with the Dean. Probation is defined as a period of
time specified by the Dean, Chair of the Student Academic Progress
Committee and the faculty of record for the course(s). If a student does
not comply with the remediation contract, the student will be
dismissed from the College.
Credit/No Credit: CGN 5000 (Strategies for Success) and CGN 7570 (Primary Care Clinical) are
graded as credit/no-credit and are not included in the numerical values for computing grade point averages.
Credit (Cr) = Achievement of the grade “Credit” signifies that a student meets the
acceptable level of performance in a graduate level program.
No Credit (NCr)= Achievement of the grade “No Credit” indicates an unacceptable level
of performance in a graduate level program. A grade of “No Credit” is
the equivalent of an “U” grade.
I = Achievement of an "I" denotes an incomplete, which signifies that a
portion of the required coursework has not been completed and
evaluated. Students must submit a plan for completion that meets
approval by the faculty of record. Students who receive two
incompletes in one semester will be placed on academic probation.
Students who are enrolled in sequential theory courses will not be able
to progress in the curriculum unless the course is completed
successfully prior to the next semester or instructor approval is given.
The grade of “incomplete” will be recorded on the official transcript
until completion of course work is completed. If the student does not
complete the contractual agreement satisfactorily, a grade of “U” will
be given with recommendation for dismissal from the College of
Graduate Nursing.
IP = Students who do not complete 90 hours of clinical (2 units) within a
semester or 45 hours of clinical (1 unit) in the first semester will be
assigned a grade of “In Progress”. A grade of “IP” is replaced with a
grade of “Cr” when the necessary number of hours is achieved.
Students must complete outstanding clinical hours and an additional
90 hours minimum in the following semester to progress in their
clinical experience. Students who fail to meet the 90 hours minimum
for two consecutive semesters will be placed on Academic Probation
and are at risk for dismissal.
Remediation
Every effort will be made to provide each student with ample opportunity to demonstrate competency
in each area of the academic program. However, remediation is to be regarded as a privilege, which must
be earned by a student through active participation in the educational program as demonstrated by regular
attendance at seminar sessions and clinical experience, individual initiative, and utilization of available
resources.
Remediation options may include any of the following:
a. Taking a comprehensive exam
b. Completing special projects or studies in a deficient area
c. Repeating the course(s)
d. Repeating a specific learning objective
Eligible students who achieve a “U” or “No-Credit” may be given a Remediation Contract, which will
outline the Remediation Plan and date for completion. This plan will be written by the Faculty Member of
Record with input from the Student Academic Progress Committee and Dean. A signed copy of this
contract for remediation will be filed with the Dean.
164
Upon completion of the student remediation contract, the instructor will submit a recommendation to
the Student Academic Progress Committee and the Dean. Approval of both the Committee and the Dean
is required for the student to continue. Successful completion will be recorded as a letter grade of “B” or
“Cr” with removal of the “Unsatisfactory” on the official transcript for the course in the identified
semester. A "B" is the highest letter grade that can be attained in a theory course upon successful
remediation, or credit (“Cr”) for a non-theory course.
Administrative Fee for Additional Term
Students who do not complete coursework or clinical hours during the final semester will be charged an
additional administrative fee for making up coursework or clinical hours after the semester. This option is
only available with the approval of the Instructor of Record and the Dean.
Leave of Absence/Withdrawal
Students who find that they are unable to continue in the program due to personal or medical reasons
may apply for a Leave of Absence. The Request for a Leave of Absence must be submitted in writing and
approved by the Dean on the recommendation of the Student Academic Progress Committee. The student
will need to obtain the endorsement of at least one instructor on the Leave of Absence form that the student
has the potential for program completion. Leaves may be granted for the balance of an academic year and
may be extended if the student seeks approval from the Dean at least one month prior to the start of the
subsequent academic year.
Probation/Dismissal
A request for Student Probation or Dismissal may be initiated by an individual faculty member, the
Student Academic Progress Committee, or the Dean, and submitted to the Chief Academic Officer. The
grounds for such an action may be based on academic, character or professional issues. The basis for
making the decision will be the University policy for student conduct as outlined in the 2001-2002
Catalog.
Seminar Weekend Attendance
Two campus-based seminar weekends are held each semester (after completing orientation sessions).
The first seminar weekend usually occurs during week 5, and the second seminar weekend usually occurs
during week 10 of the semester. Seminar weekends begin at 8 a.m. on Friday and conclude by 3 p.m. on
Sunday.
Dates of the weekend seminars are published and distributed at the beginning of each semester.
Attendance is mandatory for all seminars. Students who do not comply with this policy must make an
appointment with the Dean immediately to avoid termination of their enrollment for the semester in
question. Based on the recommendation from concerned faculty, the Dean will make a determination about
a student’s continued enrollment. A student’s right to appeal this decision is described in the General
Academic Policies and Procedures Section of this Catalog.
Clinical Training
Clinical training begins after the student has: (1) completed the Advanced Physical Assessment course,
(2) successfully completed the Advanced Physical Assessment competency based physical assessment
testing, and (3) complied with the documentation of all the University’ health, safety and immunization
requirements.
Preceptors: Students are encouraged to identify a qualified preceptor in their community prior to
starting the program. A student’s primary preceptor may be a physician trained in family practice or
internal medicine, preferably board certified, or a master’s degree prepared, certified FNP working in
primary care. The College encourages multiple rotations for specific experience if needed to optimize
student learning. A student’s primary preceptor and/or clinical instructor may suggest or assist with
identifying and scheduling these rotations. If the preceptor is a physician, the student should also work
with a nurse practitioner to promote role development.
Preceptors working within specific guidelines established by the program will be responsible for
assuring appropriate and adequate learning experiences, as well as supervising students for safe practice.
165
Preceptors and clinical sites must be approved by the Western University faculty. A Preceptor Guide will
be provided to all preceptors.
As expected with professional practice, all data gathered about a patient and his/her health/illness,
including all items within the medical record, are privileged information. Client confidentiality must be
maintained.
Students must consult with their preceptors on all patients seen by the student. The supervising
practitioner must review and countersign all student notes written in the medical record. Students are not
allowed to prescribe medications or sign any prescription order.
Students are required to wear student identification and lab coats at all times while in the clinical
setting. Western University maintains malpractice and accident insurance coverage for enrolled students.
Professional nursing malpractice insurance (in the student role) is recommended but not required.
Scheduling: While the College encourages students to schedule the same clinical day(s) each week to
provide consistency for the agency and patient follow-up, scheduled days may be individualized to
accommodate illness, employment, or family responsibilities.
Clinical Hours: Eight-to-16 hours per week of clinical training are required of full-time students
throughout the two academic years to complete 675 hours. Following successful completion of the
Physical Assessment course, full-time students are expected to complete 3-5 units of clinical training each
semester. Forty-five hours must be completed for each unit, for a total of 15 units. A student, by special
arrangement with a faculty advisor, may complete a minimum of 90 clinical hours per semester (2 units)
and complete the remaining hours in subsequent semesters or at the end of the program. This arrangement
would require a student to enroll for another semester(s) to complete required clinical hours before being
awarded a certificate of completion for the program. An administrative fee will be charged for the
additional semester(s).
Clinical Progression: Student productivity is expected to increase with each semester's experience.
Initially, students may see approximately 4-6 patients per day. The student is expected to gather complete
subjective and objective data on each patient, even though early in the program the student may not be able
to fully assess the problem or develop a complete treatment plan. Later in the program, students will be
expected to see approximately 4-8 patients per day and provide comprehensive care including assessment
and plan of treatment. Students will be guided to transition from novice to advanced beginner as they
progress in the clinical practicum.
It is recommended that MSN/FNP and FNP-only students see approximately 810 patients during their
program. The goal for patient mix is: Pediatrics 15%, Adults 40%, Geriatrics 20%, GYN 15%, OB 10%.
Students are encouraged to obtain other rotations to complete clinical objectives if they are not in a
family practice setting. In addition, students are advised to find Urgent Care and Emergency Room
rotations for a semester. The clinical faculty of record will review students’ clinical e-logs each semester.
Students are required to submit clinical e-logs periodically throughout the semester. In addition, Preceptor
Evaluations are documented periodically.
Record Keeping and Clinical e-Logs: Students will record each patient seen in the Clinical e-Log.
Clinical e-Logs for the College of Graduate Nursing are provided to the student. Students may print the e-
Logs to use for manual recording in clinic, but must enter the data into the Clinical e-Logs before
submitting to the College. Students will receive an orientation to e-Log use. E-Logs will be submitted
biweekly via e-mail attachment to the clinical instructor of record, clinical coordinator and/or Dean upon
request and at the end of each semester. In addition, students are required to submit other documentation
(i.e. Preceptor Evaluation, Student Evaluation of the Preceptor, Student Objectives) at the end of the
semester. Failure to do so may result in an incomplete grade and/or failure to progress in the curriculum.
Students will maintain a calendar of hours, which is included in their evaluation of short-term goals and
initialed/verified by the preceptor.
Clinical Site Visits: Faculty visits to the clinical site are a major key to the success of this program.
Student competency will be evaluated at this time by observing the student's interaction with patients,
preceptors, and staff. In addition, the clinical faculty provides guidance and support as well as assistance
with problem solving. Chart documentation is also reviewed and assessed. Students who receive an
unsatisfactory site visit evaluation must complete a remediation process. Note: Students who live a great
distance from the campus may be required to perform clinical competency evaluation, as needed, at a
Western University faculty member’s clinic setting or at a Western University clinical training site. Efforts
will be made to have these evaluations coincide with seminar weekends to minimize travel costs.
166
COURSE DESCRIPTIONS
CGN 5000 Strategies for Success in the FNP Program (1 unit, Cr/NCr)
This course provides new students with a comprehensive introduction to Western University's Nursing
Programs. In addition to learning about Western University of Health Sciences, students will discover in
more detail what will be expected of them as MSN/FNP students, and what they can expect from Western
University's faculty and staff. Following an overview of the most important services, policies, instructional
methods and resources, students will have an opportunity to assess your own readiness for the program and
an ability to succeed as a self-directed learner. Students will also be oriented to the technological skills
needed to complete their program. The awareness, knowledge and skills derived from this part of the
course will help ensure successful completion of the program.
CGN 5015 Clinical Reasoning (1 unit)
This course is designed for advanced nurse practitioner students to refine their history and physical
examination skills for the clinical setting. Its purpose is to take the students to the “next step” of health
assessment – beyond the basic history and physical examination to using a diagnostic reasoning process.
By integrating knowledge gained from this course with that learned in concurrent and subsequent courses,
students will continue to refine their ability to diagnose common problems. Students will also learn how to
evaluate and use assessment information with patients across the lifespan and with patients who present
with sensitive issues. This systematic approach to clinical problem-solving will provide the undergirding
structure to guide students as they tackle increasingly complex patient management problems.
CGN 5101 Health Systems I (2 units)
This course provides an overview of the American health care system with special emphasis given to
the emergence of managed care and its subsequent impact on health care planning, delivery and evaluation.
The various institutions and workforce segments that currently make up the American health care system
are introduced and compared with those of other industrialized countries. The course includes an overview
of health care economics, with particular attention given to the impact of health insurance (private and
government funded) on health care spending in this country. Managed care is presented as a major
emerging force in health care decision making and delivery. The impact of managed care reforms on the
Family Nurse Practitioner role is emphasized.
CGN 5102 Health Systems II (2 units)
The second part of Health Systems introduces the need for and tools currently available to measure the
quality of health care in this country. Special emphasis is given to identifying and measuring nursing-
sensitive patient outcomes and how they are related to treatment options and resource use. The course also
introduces case management and disease management as strategies for achieving desired patient outcomes
through the coordination of care. Students will learn about the multitude of means by which quality of
health care is currently assessed and measured in this country, including research based quality initiatives
such as standardized clinical practice guidelines, benchmarking, and report cards.
CGN 5200 Nursing Theory (3 units)
This course explores the theoretical context of contemporary nursing practice that serves to guide
nursing practice and primary health care. In addition, this course will integrate knowledge from the
physical, biological and behavioral sciences to systematically and critically apply selected conceptual
frameworks to the study of nursing, family systems and the response to illness. Through this experience,
the graduate nursing student will develop an appreciation for the process of theory development in nursing,
compare and contrast various theoretical perspectives used in nursing practice, and apply these nursing
theories critically.
CGN 5301 Nursing Research I (2 units)
Nursing Research I is designed to lay the foundation for understanding the research process and its
importance in advancing nursing practice. The course emphasizes research critique and application to
167
advanced practice nursing. Evaluation of quantitative and qualitative research literature, literature review
skills, and decision-making related to clinical significance are explored.
CGN 5302 Nursing Research II (2 units)
Nursing Research II focuses on the design and implementation of a research study. Review of research
methodology, research process, rights of subjects, grant writing and dissemination of findings are explored
in this course.
CGN 5401 Primary Care Management I (2 units)
Primary Care Management I integrates the basic knowledge of human anatomy and physiology with an
understanding of the pathologic changes and clinical manifestations that characterize common and acute
disorders in adult, obstetric, pediatric, and elderly clients. This new understanding of pathophysiology and
the student’s evolving clinical decision-making skills is applied to the interpretation of assessment data and
the diagnosis and treatment of primary care clients and their families across the life cycle.
CGN 5402 Primary Care Management II (2 units)
Primary Care Management II continues to help students integrate their basic knowledge of human
anatomy and physiology with an understanding of the pathological changes and clinical manifestations that
characterize common, chronic, and complex disorders in pediatric, adult, obstetric, and elderly clients.
Students will apply their new understanding of pathophysiology and their evolving clinical decision-
making skills to the interpretation of assessment data and the diagnosis and treatment of primary care
clients and their families across the life cycle.
CGN 5403 Primary Care Management III (2 units)
Primary Care Management III enhances the student’s ability to integrate a basic knowledge of human
anatomy and physiology with an understanding of the pathologic changes and clinical manifestations that
characterize common, acute, chronic, and complex disorders in pediatric, obstetric, and geriatric clients.
Students will apply their understanding of pathophysiology and their evolving clinical decision-making
skills to the interpretation of assessment data and the diagnosis and treatment of primary care clients and
their families across the life cycle within the special populations of pediatrics, obstetrics and geriatrics.
CGN 5501 Pharmacology I (2 units)
Pharmacology I provides the means for learning the necessary pharmaceutical principles and practices
to enable students to prescribe and monitor the effects of medications on the health and well being of
clients with common, acute, or infectious health problems. The course will address the effects of these
problems and related pharmacotherapy on patients from the various stages of the life cycle, i.e., pediatrics,
adult/family, obstetrics and geriatrics.
CGN 5502 Pharmacology II (2 units)
Pharmacology II provides the means for learning the necessary pharmaceutical principles and practices
to enable students to prescribe and monitor the effects of medications on the health and well being of
clients with chronic and complex health problems. The course will address the effects of these problems
and related pharmacotherapy on patients from the various stages of the life cycle, i.e., pediatrics,
adult/family, obstetrics and geriatrics.
CGN 5550 Advanced Pharmacology (3 units)
This course is designed to provide advanced practice nurses enrolled in the MSN-only and APN-to-
FNP track students with an accelerated review of current pharmacotherapeutic concepts. The course will
prepare students to prescribe and monitor the effects of medication on the health and well being of
patients. The course qualifies the master’s-prepared FNP to receive a Furnishing Number in the State of
California.
CGN 5601 Advanced Physical Assessment (2 units)
This FNP Role Development course introduces skills that build on undergraduate education and
experience with respect to basic physical assessment. These advanced skills, which draw on knowledge
168
from nursing, medicine, and other disciplines, include more sophisticated assessment techniques,
recognition and interpretation of clinical assessment data, diagnostic and therapeutic decision-making, and
medical record keeping. Over the course of the program, students will be expected to integrate these skills
with knowledge of common, acute, chronic, and complex illnesses in order to assess and manage patients
across the life cycle.
CGN 5602 Health Promotion Over the Life Span (1 unit)
This FNP Role Development course is designed to encourage the Family Nurse Practitioner student to
apply preventive health concepts and health promotion strategies across the life span, using the U.S. Public
Health Service guidelines as a resource. Students will learn how to apply health promotion lifestyle
changes in the primary care patient population. Concepts such as health screening and
immunization/prophylaxis in pediatric and adult clients will be examined. Methods of counseling clients
in lifestyle behaviors such as nutrition, physical activity, smoking cessation, and violence prevention will
also be explored.
CGN 5603 Current Social Issues Affecting Family Health (1 unit)
This FNP Role Development course focuses on the social issues that often arise when providing
primary health care to clients over the life span. The interdependence of these social and clinical issues
mandate that the health care provider become aware of the relevant legal, ethical, and medical implications
of child abuse, domestic violence, substance abuse, adolescent pregnancy, and poverty; as well as
geriatrics issues related to functional independence, polypharmacy, dementia, depression, and elder
homelessness.
CGN 5604 Advanced Skills (1 unit)
In this FNP Role Development course, students will learn diagnostic and therapeutic procedures and
skills critical to advanced practice nursing. These procedures and skills include microscopy, Norplant and
IUD insertion and removal, endometrial biopsy, x-ray interpretation, colposcopy and cryotherapy,
suturing, office orthopedic appliances and treatment techniques, and cardiovascular monitoring.
CGN 5605 Cultural Diversity (1 unit)
This FNP Role Development course explores the impact of patients’ cultural beliefs and values on
medical practice and the health care provider. The course emphasizes the importance of cultural
sensitivity and cultural competency in delivering high quality care. Culturally determined folk beliefs and
health traditions are examined in the context of community health and family health care.
CGN 5606 Complementary Medicine (1 unit)
This FNP Role Development course focuses on the scientific basis for practices of alternative or
complementary therapy utilized by health care consumers in this country. Among the complementary
therapies students will consider are acupuncture, yoga, biofeedback, chiropractic, dietary supplements,
exercise, herbs, homeopathy, hypnosis, imagery, massage, relaxation, meditation, spiritual healing and
energy work.
CGN 5607 Professional Issues (1 unit)
This FNP Role Development course presents a variety of role-related topics designed to prepare the
prospective Nurse Practitioner for professional practice. Beginning with a historical overview of the NP
profession, the course will take students on a guided tour of some of the critical issues that determine the
practitioner’s scope of practice, career options, and political involvement. In addition, the course presents
guidelines for resolving legal and ethical issues that are often confronted by the NP. Finally, students will
be introduced to some valuable tools for ongoing professional development such as professional
organizations and journals.
CGN 5608 Advanced Applications in Family Nurse Practice (1 unit)
This culminating FNP Role Development course provides an opportunity for students to synthesize
concepts, skills and techniques from previous courses and apply their learning toward assessing and
managing advanced case studies across the life span.
169
CGN 5611 Advanced Studies in Social Systems (2 units)
This course is designed for nurse practitioners enrolled in the APN to FNP track. This course focuses
on the diverse array of social issues and systems that the Nurse Practitioner must negotiate. The areas of
focus in this course are: health care ethics; social issues such as management of domestic violence and
substance abuse; cultural diversity skills; complementary and alternative therapeutics; and health
promotion and disease prevention concepts across the lifespan.
CGN 5801 Collaborative Project I (0.5 unit)
Collaborative Projects are based on a problem or a project that requires a collective solution. Each
Collaborative Project provides the opportunity for small groups of students to work together in a learning
experience that integrates their current coursework, encourages the application of new concepts, and
stimulates the kind of thinking and interaction that are relevant to students’ ongoing advanced practice role
development.
CGN 5802 Collaborative Project II (0.5 unit)
As with Collaborative Project I, the second Collaborative Project is based on a problem or a project
that requires a collective solution. The Collaborative Project provides the opportunity for small groups of
students to work together in a learning experience that integrates current coursework, encourages the
application of new concepts, and stimulates the kind of thinking and interaction that are relevant to
students’ ongoing advanced practice role development.
CGN 5850 Advanced Role (3 units)
This is a culminating course than examines transitional roles for the advanced practice nurse (APN), with
focus on understanding and applying leadership and other related theories, exploring diverse leadership
roles and associated issues, and development of knowledge and skills needed for leadership roles. An
overall goal of the course is to expand the student’s understanding of the broad scope of responsibilities of
APNs through the assumption of leadership roles within the profession.
CGN 5950 Certification Review (1 unit)
This course is required to be completed prior to graduation for all students enrolled in the MSN/FNP
and FNP-only programs. This comprehensive testing review will further assist the MSN/FNP and FNP-
only student to prepare for the national certifying examination to become an Advanced Practice Nurse.
Testing and review modules are systems-based. Following a pre-assessment examination (self-evaluation),
students will have access to a detailed modular review program during the Clinical Experience (CGN
7570) course. Students are required to achieve a score of 80% or higher on the final examination.
Students may repeat the final examination one time if they do not achieve a score of 80% or higher.
CGN 5990 Culminating Project (1 unit)
The Culminating Project is an independent study project that serves as a culminating experience for the
FNP program. The project requires the student to develop a clinical improvement initiative that will offer
valuable insights into high-risk patient populations and the kinds of contributions FNPs can make in
providing care for these populations.
CGN 7570 Clinical Experience (2-5 Units per Semester; Repeatable to a total of 15 units; Cr/NCr)
The Clinical Experience course offers FNP, ANP-FNP, and MSN/FNP students the opportunity to
begin providing comprehensive health care to individuals and families within a culturally diverse
environment in collaboration with physicians, nurse practitioners and other health care professionals.
Students are expected to draw on their preceptored experiences to develop sound clinical judgment applied
to health promotion, health maintenance, and diagnosis and management of common, acute, chronic and
complex health problems for individuals across the life cycle.
170
CURRICULUM
MSN/FNP Program
Prerequisites: Statistics and Pathology Review
YEAR 1
YEAR 2
Pre-
Strategies (CGN 5000)
1
Program
Physical Assess (CGN 5601)
2
Total Units
3
TERM 1
TERM 4
Clinical Reasoning (CGN 5015)
1
Nursing Theory (CGN 5200)
3
Health Systems I (CGN 5101)
2
Nursing Research I (CGN 5301)
2
PC Management I (CGN 5401)
2
Cultural Diversity (CGN (5605)
1
Health Promotion (CGN 5602)
1
Collab Project I (CGN 5801)
.5
Clinical Exp (CGN 7570) 1
Clinical Exp (CGN 7570)
3
Total Units 7
9.5
TERM 2
TERM 5
PC Management II (CGN 5402)
2
Health Systems II (CGN 5102)
2
Pharm I (CGN 5501)
2
Nursing Research II (CGN 5302)
2
Social Issues (CGN 5603)
1
Collab Project II (CGN 5802)
.5
Advanced Skills (CGN 5604)
1
Clinical Exp (CGN 7570)
3
Clinical Exp (CGN 7570)
2
Total Units
8
7.5
TERM 3
TERM 6
PC Management III (CGN 5403)
2
Prof Issues (CGN 5607)
1
Pharm II (CGN 5502) 2
Adv. Apps. (CGN 5608)
1
Complementary Med (CGN 5606)
1
Cert. Rev. (CGN 5950)
1
Clinical Exp (CGN 7570)
3
Culminating Project (CGN 5990)
1
Clinical Exp (CGN 7570)
3
Total Units
8
7
Year 1 Total Units
26
Year 2 Total Units
24
Total Program Units
50
* One additional semester can be taken to complete clinical hours. Students are expected to complete a minimum of 90 hours (2
units) per semester to progress in the curriculum.
171
CURRICULUM
FNP-Only Program MSN-Only Program
Prerequisites: Statistics and Pathology Review Prerequisites: Statistics and Pathology Review
YEAR 1
YEAR 1
Pre-
Strategies (CGN 5000)
1
Pre-
Strategies (CGN 5000)
1
Program
Physical Assess (CGN 5601)
2
Program
Physical Assess (CGN 5601)
2
Total Units 3
Total Units 3
TERM 1
TERM 1
Clinical Reasoning (CGN 5015)
1
Health Systems I (CGN 5101)
2
Health Systems I (CGN 5101)
2
Nursing Theory (CGN 5200)
3
PC Management I (CGN 5401)
2
Nursing Research I (CGN 5301)
2
Health Promotion (CGN 5602)
1
Collab. Project I (CGN 5801)
.5
Cultural Diversity (CGN 5605)
1
Clinical Exp (CGN 7570)*
5
Total Units 12
Total Units 7.5
TERM 2
TERM 2
Health Systems II (CGN 5102)
2
Health Systems II (CGN 5102)
2
PC Management II (CGN 5402)
2
Research II (CGN 5302)
2
Pharm I (CGN 5501)
2
Skills (elective) (CGN 5604)
(1)
Advanced Skills (CGN 5604)
1
Adv. Social Syst. (CGN 5611)
2
Social Issues (CGN 5603)
1
Collab Project II (CGN 5802)
.5
Clinical Exp (CGN 7570)
5
Total Units
13
Total Units
5.5
(6.5)
TERM 3
TERM 3
PC Management III (CGN 5403)
2
Pharm II (CGN 5502)
2
Advanced Pharm. (CGN 5550)
3
Complementary Med (CGN 5606)
1
Prof. Issues (CGN (5607)
1
Prof Issues (CGN 5607)
1
Advanced Role (CGN 5850)
3
Adv. Apps. (CGN 5608)
1
Culminating Project (CGN
5990)
1
Cert. Rev. (CGN 5950)
1
Clinical Exp (CGN 7570)*
5
Total Units
13
Total Units
8
Total Program Units
41
Total Program Units
25
(26)
* One additional semester can be taken to complete clinical hours. Students are expected to complete a minimum of 90 hours (2
units) per semester to progress in the curriculum.

172
CURRICULUM
APN to FNP Track
Prerequisites: Statistics and Pathology Review
YEAR 1
Pre-
Strategies (CGN 5000)
1
Program
Physical Assess (CGN 5601)
2
Total Units 3
TERM 1
PC Management I (CGN 5401)
2
Clinical Exp (CGN 7570)*
2
Total Units 4
TERM 2
PC Management II (CGN 5402)
2
Adv. Social Syst. (CGN 5611)
2
Clinical Exp (CGN 7570)
2
Total Units
6
TERM 3
Adv. Pharm. (CGN 5550)
3
Prof Issues (CGN 5607)
1
Adv. Apps. (CGN 5608)
1
Cert. Rev. (CGN 5950)
1
Total Units
6
Total Program Units
19
173
HONORS AND AWARDS
The following honors and awards are presented annually at the University's Honors Day ceremony in
April:
Academic Achievement Award
Spirit Award
CGN Leadership and Community Excellence Award
President's Society Award
Joseph and Dorothy Gendron Journalism Award
Guy M. Allmon Scholarship Fund
Linda Fox Memorial Endowment Fund
Dean's Award
The following honors and awards are presented annually to graduates at the University's
Commencement Dinner:
FNP Primary Care Award
Class of 2000 Award
Academic Achievement Award
Class Service Award
Dean's Award
174
Academic Calendar
2001-2002
Semester Format (15 Week)
Thursday, Jul. 4, 2001
Independence Day - No classes
Friday, Jul. 5 - 9, 2001
First Preprogram Seminar (new students)
Jul 13-15, 2001
Seminar Weekend (continuing students)
Aug., 4-10, 2001
Second Preprogram Seminar (new students)
Aug. 10, 2001
Summer Semester Ends (continuing students)
Aug. 19, 2001
Preprogram end (new students)
Aug. 22, 2001
Fall Semester Tuition Due
Aug. 27, 2001
Fall Semester Begins
Sept. 21-23, 2001
Seminar Weekend
Nov. 9-11, 2001
Seminar Weekend
Dec. 10, 2001
Fall Semester Ends
Dec. 11, 2001 - Jan. 1, 2002
Semester Break
Jan. 2, 2002
Spring Semester Begins
Feb. 1-3, 2002
Seminar Weekend
Feb. 7, 2002
Spring Semester Tuition Due
Mar. 1, 2002
Application Deadline (Fall 2002)
Mar. 8-10, 2002
Seminar Weekend
Apr. 12, 2002
Spring Semester Ends
Apr. 13-28, 2002
Spring Break
Apr. 29, 2002
Summer Semester Begins (continuing students)
May 31-Jun. 2, 2002
Seminar Weekend (continuing students)
TBA, Jun., 2002
Graduation
Jun. 27, 2002
Preprogram Begins (new students)
Jun. 27-Jul. 1, 2002
First Preprogram Seminar (new students)
Jul. 12-13, 2002
Seminar Weekend (continuing students)
Aug. 4-8, 2002
Second Preprogram Seminar (new students)
Aug. 9, 2002
Summer Semester Ends (continuing students)
Aug. 18, 2002
Preprogram Ends (new students)
175
BOARD OF TRUSTEES, ADMINISTRATION & FACULTY
WESTERN UNIVERSITY OF HEALTH SCIENCES
Board of Trustees
Warren Lawless, LHD (Hon.), Chairman
Wesley V. Boudette, DO, DEd (Hon.), FAOCR, Vice Chairman
John A. Forbing, Secretary
Ethan R. Allen, DO, DSc (Hon.), Treasurer
Philip Pumerantz, PhD, LHD (Hon.), President (ex officio)
Richard A. Bond, DO, FAAFP
Wen Chang
LaDonna Johnson, DO
Cassandra Malry, MBA
John T. McGwire, DDS
Sam Tanenbaum, PhD
Richard E. Eby, DO, FACOOG, DSc (Hon.), DEd (Hon.),
PhD (Hon.), Trustee Emeritus
Lawrence L. Leyba, DO, DEd (Hon.), Trustee Emeritus
UNIVERSITY AND ACADEMIC ADMINISTRATION
University Administration
President: Philip Pumerantz, PhD, LHD (Hon.)
Executive Vice President of Academic Affairs/Chief Academic
Officer: George Charney, DO, FAOCA, FAODME
Executive Vice President of Finance & Business: Christopher Oberg, PhD
Provost: Donald J. Krpan, DO, FACOFP
Vice President, Policy and Research/Assistant to the
Executive Vice President of Academic Affairs: Gary M. Gugelchuk, PhD
Vice President, Strategic Planning and Institutional Effectiveness:
Suellen Crano, PhD
Vice President, University Advancement: Richard M. Nordin
Dean, Student Affairs: Beverly A. Guidry, EdD
Treasurer: Kevin D. Shaw
Registrar: Jeanne Hewson, MA
Assistant Vice President of University Advancement, Alumni and Constituent Relations:
Mari Penshurst-Gersten
Assistant Vice President of University Advancement, Major Gifts: Hart Roussel
Assistant Vice President of University Advancement, Major Gifts: Jeanette Janik
Assistant Vice President of Advancement and Sponsored Programs:
Matthew D. Katz, MHA
Associate Treasurer, Finance: Joseph Ocampo
Assistant Treasurer, Fiscal Operations: Chris Crow
Assistant Treasurer, Budgeting: Louis Mansur
Director, Academic Center for Excellence in the Health Sciences: John Hurtado
Director, Admissions (Allied Health, Pharmacy, Graduate Nursing):
Kathy Ford
Director, Admissions (Medicine): Susan D. Hanson
Director, Annual Giving: Laura Wensley
Director, Bookstore: Elizabeth V. Guerra
Director, Center for Academic and Professional Enhancement:
Thomas Levitan, MA
Director, Center for Disability Issues and the Health Professions:
Brenda Premo, MBA
176
Director, Communications: Jean Henshaw
Director, Curriculum Development, Center for Disability Issues and the
Health Professions: LeeAnne Carrothers, PhD, PT
Director, Financial Aid: Otto Reyer, MA
Director, Foundation Relations: Garth Clayton
Director, Health and Safety: Ron Redden
Director, Health Professions Library: Pat Vader, BS
Director, Human Resources: Sinclair Hugh, MPA, SPHA
Acting Director, Instructional Technology & Distance Learning: Miary Andriamiarisoa
Director, Learning Enhancement & Academic Development:
David Hacker, MA
Acting Director, Network Operations: Gary Priddy
Director, Publications: Rick Clapper
Director, Student Affairs: Patricia Delesante
Director, Events and Programs: Julie Wade
Director, University Recruitment/Strategic Enrollment
Management Ann Ellis, MEd
Director, Willed Body Program: Niña McCoy
Alumni Dean Emerita: Janet M. Dyer
Gift Planning Specialist: James S. Williams, CFRE
Faculty Development Specialists: Maja Altarac, MD, PhD, MPH;
Alana Olschwang, MA; Ryan Quist, MA
Coordinator, Security: Dave Trenholm
Manager, Facilities: Larry Thomas
College of Osteopathic Medicine of the Pacific
Dean, College of Osteopathic Medicine: Craig J. Lenz, DO, FAODME
Assistant Dean, Clinical Affairs: Allen Zagoren, DO
Assistant Dean, Academic Education/Director of Clinical Education:
Ron Berezniak, PhD
Chairperson, Department of Anatomy: Richard Sugerman, PhD
Chairperson, Department of Basic Medical Sciences: Robert Fiorindo, PhD
Chairperson, Department of Family Medicine: Alan D. Cundari, DO, MS
Chairperson (Acting), Department of Geriatrics: Ehab Tuppo, DO
Chairperson, Department of Internal Medicine: J. Michael Finley, DO
Chairperson, Department of Obstetrics/Gynecology: TBN
Chairperson, Department of Osteopathic Manipulative Medicine:
Raymond Hruby, DO
Chairperson, Department of Pathology: Cyrus Parsa, DO
Chairperson, Department of Pediatrics: Frances Yang, DO
Chairperson, Department of Surgery: J. Vivian Davis III, DO
Director, Education and Academic Research: Richard Winn, MA
Director, Osteopathic Center for Children: Viola M. Frymann, DO, FAAO
Director, Student Services: Gisele Tackoor, JD
Manager, Western University Medical Center: Joanna Varner
College of Allied Health Professions
Dean, College of Allied Health Professions: Stephanie D. Bowlin, EdD, PA-C
Chairperson, Department of Health Professions Education:
Michael Burney, MS, PA-C
Chairperson, Department of Physician Assistant Education:
Roy Guizado, MS, PA-C
Chairperson, Department of Physical Therapy Education:
Donna Redman-Bentley, PhD, PT
177
Director of Clinical Education, Department of Physical
Therapy Education: Georgeanne Vlad, MA, PT
Academic Coordinator of Clinical Education, Department of Physician
Assistant Education: Rebecca Maldonado, BS, PA-C
Coordinator, Clinical Education, Department of Physician
Assistant Education: Jane Riplog
College of Pharmacy
Dean, College of Pharmacy: Max D. Ray, PharmD, MS
Associate Dean, Academic Affairs: Wallace Murray, PhD
Assistant Dean, Graduate Education and Research: Ed Soltis, PhD
Assistant Dean, Development: Sam K. Shimomura, PharmD
Director, Center for Drug Development: William Garner
Director, Center of Pharmacy Practice Research & Development: Katherine K. Knapp, PhD
Director, Introductory Professional Practice Experience:
Craig Hitchman, BPharm
Curriculum Development and Assessment Specialist:
Nancy E. Kawahara, PharmD, MS
Coordinator, Student Services: Mark Iannuzzo
College of Graduate Nursing
Dean, College of Graduate Nursing/Director, MSN/FNP Program:
Karen Hanford, MSN, FNP, PA-C
Associate Dean, M. Elizabeth Towner, PhD, FNP
Academic Coordinator, MSN/FNP Program: Margaret J. Rowberg, MSN, ANP-C
Clinical Education Coordinator, MSN/FNP Program:
Susan E. Lominska, MN, RN
College of Veterinary Medicine
Dean, College of Veterinary Medicine: Shirley D. Johnston, PhD, DVM
FACULTY
Maja Altarac, Adjunct Assistant Professor of Social and Administrative Sciences, 2000. MD, University of
Sarajevo; MPH, PhD, Johns Hopkins University
Dayle Chakerian Armstrong, Assistant Professor of Physical Therapy Education (2000). AS, BS, Mount
St. Mary's College; MS, University of Southern California.
Mary K. Bailey, Assistant Professor of Physical Therapy Education, 1999. BS, California State University,
Long Beach; MS, California State University, Fullerton.
Gerald Bales, Assistant Professor of Anatomy, 1996. BA, MA, Chico State University; PhD, University of
Southern California.
Ronald Berezniak, Associate Professor of Health Professions Education, 1999. BS, Bloomsburg State
College; MA, Glassboro State College; PhD, University of Pennsylvania.
Gurupadappa V. Betageri, Professor of Pharmaceutical Sciences, 1998. BS, Karnatak University; MS,
Bangalore University; PhD, University of Alberta.
Nancy Bjerke, Assistant Professor of Physical Therapy Education, 1997. BS, Loma Linda University;
MPT, Loma Linda University.
178
Stephanie D. Bowlin, Associate Professor of Physician Assistant Education, 1990. BS, California State
University, Dominguez Hills; MS, College of Osteopathic Medicine of the Pacific; PA-C, Charles R. Drew
University of Medicine and Science; EdD, University of La Verne.
Dion R. Brocks, Associate Professor of Pharmaceutical Sciences, 1998. BSc, MPharm, PhD, University of
Alberta.
Sherry A. Brown, Assistant Professor of Pharmacy Practice, 2000. BS, PharmD, Philadelphia College of
Pharmacy and Science.
Michael Burney, Assistant Professor of Physician Assistant Education, 1996. BS, University of Southern
California; PA, MS, College of Osteopathic Medicine of the Pacific.
Rosslynn S. Byous, Assistant Professor of Physician Assistant Education, 1991. BA, University of
California, Santa Barbara; MS, University of LaVerne; PA, Charles Drew University of Medicine and
Science; DPA, University of LaVerne.
LeeAnne Carrothers, Adjunct Associate Professor of Physical Therapy Education, 1992. BS, University of
California, Davis; MS, PT, University of Southern California; PhD, California Graduate Institute.
Shawn K. Centers, Assistant Professor of Pediatrics, 1999. BS, Georgetown College; DO, Nova
Southeastern University.
Casey Chaney, Associate Professor of Physical Therapy Education, 1993. BS, MS, Russell Sage College;
PhD University of Utah, College of Health.
George Charney, Professor of Surgery/Anesthesiology, 1997. BA, Brooklyn College; DO, Philadelphia
College of Osteopathic Medicine.
Jack J. Chen, Assistant Professor of Pharmacy Practice, 2000. BA, University of California, San Diego;
BS, Massachusetts College of Pharmacy and Allied Health Sciences; PharmD, University of Utah.
Eunice P. Chung, Assistant Professor of Pharmacy Practice, 1999. BS, University of California, Berkeley;
PharmD, University of California, San Francisco.
Norman Coakley, Assistant Professor of Family Medicine, 1997. DO, College of Osteopathic Medicine of
the Pacific.
Frank Comunale, Professor of Surgery/Anesthesiology (Emeritus), 1997. BS, Tufts University; MD,
Boston University.
Suellen Crano, Associate Professor of Health Professions Education, 1999. BA, MA, EdS, The George
Washington University; PhD, Michigan State University.
Alan D. Cundari, Associate Professor of Family Medicine, 1987. AS, University of Albuquerque; MS,
College of Osteopathic Medicine of the Pacific; DO, College of Osteopathic Medicine of the Pacific.
J. Vivian Davis III, Associate Professor of Surgery (2000). BA, MA, University of Texas, Austin; DO,
Texas College of Osteopathic Medicine; MA, William Woods University.
Jeffrey Felton, Professor of Microbiology, 1993. BS, Massachusetts Institute of Technology; PhD, Tufts
University.
J. Michael Findley, Associate Professor of Internal Medicine, 2000. BS, Michigan State University; DO,
Chicago College of Osteopathic Medicine.
179
Robert P. Fiorindo, Professor of Physiology, 1980. BS, Albright College; MS, University of Maryland;
PhD, University of California, Berkeley.
Duane H. Foley, Professor of Physiology, 1984. BS, University of California, Davis; PhD, University of
California, Davis.
James Dana Foster, Associate Professor of Anatomy, 2000. BS, MS, Oakland University; PhD, Temple
University.
Viola M. Frymann, Professor of Family Medicine/Osteopathic Principles and Practice, 1978. MB, BS,
University of London; DO, College of Osteopathic Physicians and Surgeons, Los Angeles.
Spencer B. Gilbert, Professor of Pathology, 1995. MD, Chicago Medical School.
Robert A. Graf, Assistant Professor of Pharmaceutical Sciences, 1999. AB, University of California,
Berkeley; PhD, University of Hawaii.
Lee R. Grunden, Professor of Pharmacology (Emeritus), 1980. BS Oregon State University; PhD,
University of California, San Francisco Medical Center.
Vitalita Genove Grunden, Professor of Pathology (Emerita), 1980. AA, Sillman University; MD,
University of Santa Tomas.
Gary M. Gugelchuk, Associate Professor of Health Professions Education, 1986. BA, MA, PhD, The Ohio
State University.
Beverly Guidry, Instructor of Health Professions Education, 1997. BA, MS, EdD, University of LaVerne.
Roy A. Guizado, Assistant Professor of Physician Assistant Education, 1995. PA-C, College of
Osteopathic Medicine of the Pacific; MS, Western University of Health Sciences.
Karen J. Hanford, Professor of Nursing, 1997. BSN, San Francisco State University; MSN, California
State University, Chico; FNP, PA, University of North Dakota.
Rick M. Hirsh, Assistant Professor of Family Medicine, 2000. AS, Fullerton College; BS, Loma Linda
University; DO; Western University of Health Sciences.
Raymond J. Hruby, Professor of Family Medicine/Osteopathic Manipulative Medicine, 1999. BA, St.
Vincent College; DO, College of Osteopathic Medicine and Surgery; MS, West Coast University.
Carol J. Huston, Adjunct Professor of Nursing, 1998. BS, University of Iowa; MSN, California State
University, Chico; MPA, DPA, University of Southern California.
Mahtab Jafari-Fesharaki, Assistant Professor of Pharmacy Practice, 1996. PharmD, University of
California, San Francisco.
Kevin Jenkins, Professor of Internal Medicine, 1981. BS, Capital University; DO, College of Osteopathic
Medicine & Surgery.
Gary R. Johnston, Professor of Veterinary Medicine, 1999. BA, University of Washington; DVM,
Washington State University; MS, University of Minnesota.
Shirley D. Johnston, Professor of Veterinary Medicine, 1998. BS, University of Washington; DVM,
Washington State University; MS, PhD, University of Minnesota.
180
H. James Jones, Assistant Professor of Osteopathic Manipulative Medicine, 1997. BS, California State
University, Long Beach; DO, College of Osteopathic Medicine of the Pacific.
Anita Kay Kalousek, Assistant Professor of Family Medicine, 2000. BA, Loma Linda University; DO,
MS, College of Osteopathic Medicine of the Pacific.
Sylvia Kamath, Professor of Anatomy, 1995. MS, Bangalore University; MBBS, Madras University.
Nancy Edman Kawahara, Assistant Professor of Pharmacy Practice, 2000. PharmD, MSEd, University of
Southern California.
Jerry Kellogg, Adjunct Assistant Professor of Nursing, 1998. BA, University of California, Riverside; MA,
California State University, Los Angeles.
Nadir Khan, Professor of Microbiology, 1978. BS, DJ, Government Science College; MS, University of
Karachi; PhD, University of Missouri.
Dennis M. Kiick, Associate Professor of Biochemistry, 1995. BS, San Diego State University; PhD,
University of North Texas.
Katherine K. Knapp, Professor of Social and Administrative Sciences, 2001. BA, MA, MS, University of
Michigan; PhD, University of California, Davis.
Donald J. Krpan, Professor of Family Medicine, 1987. BS, University of Nevada; DO, University of
Health Sciences, College of Osteopathic Medicine, Kansas City.
Craig S. Kuehn, Professor of Anatomy, 1985. BS, California State Polytechnic University, Pomona; PhD,
University of Southern California.
Maria Lambros, Assistant Professor of Pharmaceutical Science, 1999. BS, University of Athens; MS,
University of Cincinnati; PhD, University of Minnesota.
Anandi V. Law, Assistant Professor of Social and Administrative Sciences. 1999. BPharm, University of
Bombay; MS, PhD, The Ohio State University.
Craig L. Lenz, Associate Professor of Family Medicine, 1999. BSE, Princeton University; MEd,
University of Pennsylvania; DO, Philadelphia College of Osteopathic Medicine.
Jonathan Leo, Associate Professor of Anatomy, 1995. BA, MacAlister College; PhD, University of Iowa.
Diane Lithgow, Professor of Nursing, 1997. BS, University of California, Irvine; BSN, MSN, California
State University, Long Beach.
Susan E. Lominska, Assistant Professor of Nursing, 2000. ASN, Chaffey College; BA, University of
Kansas; BSN, California State University, Los Angeles; MN, University of California, Los Angeles.
Rebecca Maldonado, Instructor of Physician Assistant Education (2000). BS, California State University,
Long Beach; PA, College of Osteopathic Medicine of the Pacific.
James T. Martin, Professor of Physiology and Behavioral Science, 1986. BA, West Virginia University;
MS, University of Connecticut; Dr. re. Nat., University of Munich and Max Planck Institute, Seewiesen,
Germany.
181
James F. May, Professor of Anatomy, 1981. BS, California State College, Los Angeles; MS, Occidental
College; PhD, University of Southern California.
Miguel A. Medina, Instructor of Physician Assistant Education, 1992. AA, East Los Angeles Junior
College; PA-C, University of Southern California.
Kenneth Mengel, Instructor of Physical Therapy Education, 2000. BA, Whittier College; MPT, University
of Southern California.
Christian G. Merkel, Professor of Biochemistry, 1979. BA, University of Cincinnati; MA, University of
California, Santa Barbara; PhD, University of Cincinnati.
Mary Anne Morelli, Assistant Professor of Osteopathic Manipulative Medicine/Family Medicine, 1992.
BA, California State University; DO, College of Osteopathic Medicine of the Pacific.
Tony Mosconi, Assistant Professor of Anatomy, 1997. BS, Allegheny College; MS, PhD, Albany Medical
College.
Wallace J. Murray, Associate Professor of Pharmaceutical Sciences, 1999. BS, San Diego State
University; PhD, University of California, San Francisco.
Amelia Naccarto-Coleman, Assistant Professor of Physician Assistant Education, 1995. BA, West Virginia
University; BS, MAS, Johns Hopkins University.
Gayle H. Nelson, Professor of Anatomy (Emeritus), 1980. BA, Walla Walla College; MS, University of
Maryland; PhD, University of Michigan.
Nancy Nielsen-Brown, Instructor of Physician Assistant Education, 1995. BTh, University of La Verne;
AS, Cypress College; PA, University of Southern California.
Stephen A. O'Barr, Assistant Professor of Pharmaceutical Sciences, 1999. BS, University of California,
San Diego; PhD, Arizona State University.
Christopher Oberg, Associate Professor of Health Professions Education, 1998. BA, University of
California, San Diego; PhD, The Claremont Graduate School.
Alice Shoemaker Oglesby, Professor of Microbiology (Emerita), 1979. BS, University of Oklahoma; MA,
University of Kansas; PhD, University of California, Berkeley.
Mark P. Okamoto, Associate Professor of Social and Administrative Sciences & Pharmacy Practice, 2000.
BS, University of California, Los Angeles; PharmD, University of Southern California.
Cyrus Parsa, Professor of Pathology, 1992. BS, California State University, Northridge; DO, University of
Health Sciences, Kansas City.
Sunil Prabhu, Assistant Professor of Pharmaceutical Sciences, 1996. PhD, School of Pharmacy, Western
Virginia University; BPharm, Birla Institute of Technology.
Brenda Premo, Associate Professor of Health Professions Education, 1999. BA, California State
University, Long Beach; MBA, Pepperdine University.
Lara M. Rasmussen, Assistant Professor of Veterinary Medicine, 1999. BS, DVM, University of
California, Davis; MS, University of Minnesota.
182
Max D. Ray, Professor of Pharmacy Practice, 1996. BS, University of South Carolina, MS, PharmD,
University of Tennessee.
David Redding, Assistant Professor of Osteopathic Manipulative Medicine, 1996. BS, PT, California State
University, Long Beach; DO, College of Osteopathic Medicine of the Pacific.
Donna Redman-Bentley, Professor of Physical Therapy Education, 1998. BS, Pennsylvania State
University; MS, The Ohio State University; PhD, University of Southern California.
Elizabeth A. Rega, Assistant Professor of Anatomy, 2000. BA, Valparaiso University; MA, PhD,
University of Chicago.
R. Ashley Robinson, Professor of Veterinary Medicine, 1998. BVSc, University of Sydney; Dip.
Microbiol, Otago University; MPH, PhD, University of Minnesota.
Burton N. Routman, Professor of Family Medicine, 1995. BA, Johns Hopkins University; DO, University
of Osteopathic Medicine and Health Sciences.
Margaret J. Rowberg, Assistant Professor of Nursing, 2000. BSN, MSN, California State University, Long
Beach.
Stanley Saul, Professor of Surgery/Urology, 1985. BS, Albright College; DO, Philadelphia College of
Osteopathic Medicine.
Clifton S. Schermerhorn, Associate Professor of Family Medicine, 1999. AA, Orange Coast College; BA,
California State University, Fullerton; MD, American University of the Caribbean.
James D. Scott, Assistant Professor of Pharmacy Practice, 2000. BS, MEd, PharmD, University of Florida.
Michael A. Seffinger, Assistant Professor of Family Medicine/Osteopathic Manipulative Medicine, 1999.
BA, University of California, Santa Cruz; DO, Michigan State University.
David M. Selkowitz, Associate Professor of Physical Therapy Education, 2000. BS, State University of
New York, Buffalo; MS, Boston University.
Natalie Semaan, Assistant Professor of Pharmacy Practice, 2000. BS, Portland State University; PharmD,
University of the Pacific.
Karen Shapiro, Assistant Professor of Pharmacy Practice, 2000. BA, Boston University, PharmD,
University of Southern California.
Sam Shimomura, Professor of Pharmacy Practice, 1997. PharmD, University of California, San Francisco.
Gail L. Singer-Chang, Assistant Professor of Family Medicine, 1999. BA, San Diego State University,
MA, PsyD, California School of Professional Psychology, Los Angeles.
Quentin W. Smith, Associate Professor of Health Professions Education, 1999. AAS, Hudson Valley
Community College; BS, State University of New York, Downstate Medical Center; MS, State University
of New York, Stony Brook.
Edward E. Soltis, Professor of Pharmaceutical Sciences, 1998. BS, Butler University; PhD, University of
Florida.
Sandra Stuckey, Assistant Professor of Physical Therapy Education, 1991. BS, Michigan State University;
MA, California State University, Los Angeles; PT, Stanford University.
183
Ruth Ann Subach, Assistant Professor of Pharmacy Practice, 1999. BS, St. John's University; PharmD,
University of Utah.
Richard A. Sugerman, Professor of Anatomy, 1980. BA, California State University, San Diego; MS, PhD,
University of New Mexico.
Reza Taheri, Assistant Professor of Pharmacy Practice, 2000. BA, PharmD, University of Minnesota.
Brett P. Thomas, Assistant Professor of Osteopathic Manipulative Medicine/Family Medicine, 1996. BS,
University of Florida; DO, Southeastern University of Health Sciences.
M. Elizabeth Towner, Adjunct Professor of Nursing, 2000. BS, Duquesne University; MSN, University of
California, San Francisco; FNP, Indiana University; PhD, University of Texas.
Carl E. Trinca, Professor of Social and Administrative Sciences, 1995. BS, MS, PhD, University of
Arizona.
Ehab Tuppo, Assistant Professor of Geriatrics/Internal Medicine, 2000. BS, MS, MA, Wayne State
University; DO Michigan State University.
Guillermo Valenzuela, Associate Professor of Obstetrics/Gynecology, 1995. MD, Catholic University
Medical School.
Karen Van Leuven, Adjunct Associate Professor of Nursing, 1997. BSN, University of Delaware; MS,
University of San Francisco; PhD, University of California, San Francisco; FNP, Western University of
Health Sciences.
Georgeanne Vlad, Assistant Professor of Physical Therapy Education, 1991. BS, California State
Polytechnic University, Pomona; MA, University of California, Santa Barbara; PT, Children's Hospital,
Los Angeles.
Edward J. Wagner, Assistant Professor of Physiology, 2001. BS, University of California, Los Angeles;
PhD, Michigan State University.
Donald E. Walters, Associate Professor of Pharmacology, 2001. BS, St. Louis College of Pharmacy; PhD,
University of Louisville.
Sompon Wanwimolruk, Associate Professor of Pharmaceutical Sciences, 2001. BSc, MSc, Mahidol
University; PhD, Flinders University of South Australia.
Michael Weiss, Assistant Professor of Family Medicine/Pediatrics, 1994. BS, University of Michigan; DO,
College of Osteopathic Medicine of the Pacific.
Stanley K. Wong, Professor of Pharmacology, 1981. BS, MS, PhD, University of Wisconsin.
Siu-Fun Wong, Associate Professor of Pharmacy Practice, 1997. BS, University of California, Los
Angeles; PharmD, University of California, San Francisco.
Annie Wong-Beringer, Associate Professor of Pharmacy Practice, 1997. PharmD, University of Southern
California, Los Angeles.
Frances Yang, Assistant Professor of Pediatrics, 1999. BS, California State Polytechnic University,
Pomona; DO, Western University of Health Sciences.
184
Joanne Yasuda, Assistant Professor of Pharmacy Practice, 1996. BA, University of California, Los
Angeles; PharmD, University of Southern California, San Francisco.
Bartley Yee, Assistant Professor of Family Medicine, 1999. BS, University of California, Los Angeles;
DO, Michigan State University.
LaTanya J. Young, Assistant Professor of Physician Assistant Education, 2000. BS, Xavier University of
Louisiana; MMS, Emory University; MPH, University of California, Los Angeles.
Rafi Younoszai, Professor of Anatomy, 1979. BS, University of California, Berkeley; PhD, University of
Minnesota.
185
CLINICAL AND ADJUNCT FACULTY
Mary L. Adair, PA-C
Instructor of Physician Assistant Education
Ross Mitchell Adams, DO
Assistant Professor of Pediatrics
Cyrus Afrasiabi, MD
Associate Professor of Internal Medicine
Afshin Afrookhteh, JD
Assistant Professor of Physician Assistant
Education
Chandrahas Agarwal, MD
Assistant Professor of Internal Medicine/
Cardiology
Vandana Agarwal, MD
Assistant Professor of Internal Medicine/
Oncology & Hematology
Luz del Carmen Aguirre, MD
Assistant Professor of Physician Assistant
Education
Joseph Aiello, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Laye Akinloye, PA-C
Associate Professor of Physician Assistant
Education
Murtadha Al-Marashi, MD
Associate Professor of Internal
Medicine/Neurology
Steven Alder, MD
Assistant Professor of Internal Medicine/
Pathology
John G. Alevizos, DO
Assistant Professor of Family Medicine
Brent R. Allan, MPH, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Ethan R. Allen, DO
Professor of Family Medicine
Larkin Allen, DO
Assistant Professor of Surgery/Ophthalmology
Robert F. Altamura, DO
Associate Professor of Internal Medicine
Louis R. Alvarez, MD, MPH
Assistant Professor of Family Medicine/
Psychiatry
M. Mark Alwan, MD
Assistant Professor of Obstetrics/Gynecology
Deepak Anand, Ph.D.
Assistant Professor of Pharmacy Practice
Kenneth Anderson III, DO
Assistant Professor of Family Medicine
Ray E. Anderson, DO
Assistant Professor of Family Medicine
Wayne E. Anderson, DO
Assistant Professor of Internal Medicine/
Neurology
William G. Anderson, DO, FACOS
Professor of Surgery
Soran Andrei, MS
Assistant Professor of Health Professions
Education
Elias I. Anoub, MD
Assistant Professor of
Surgery/Otorhinolaryngology
Jeffrey P. Anthony, DO
Assistant Professor of Family Medicine/
Sports Medicine
Michael D. Antos, MD
Assistant Professor of Internal Medicine/
Pediatrics
Y. Paul Aoyagi, MD
Associate Professor of Physician Assistant
Education
Rubina Aqueel, MD
Assistant Professor of Internal Medicine/
Endocrinology
186
Neal S. Archer, DO
Associate Professor of Family Medicine
John J. Aryanpur, MD
Assistant Professor of Surgery
Allison Atkinson, PA-C
Assistant Professor of Physician Assistant
Education
Gary K. Augter, MS, DO
Assistant Professor of Family Medicine/
Dermatology
Gino Aveni, PA-C
Instructor of Physician Assistant Education
Paul A. Aversano, DO
Associate Professor of Internal Medicine/
Neurology
Aziz F. Awad, DO
Assistant Professor of Family Medicine
Mg San Aye, MD
Assistant Professor of Surgery/Ophthalmology
Muhammad A. Azam, MD
Assistant Professor of Physician Assistant
Education
Richard M. Bachrach, DO
Assistant Professor of Family Medicine
Peter A. Badua, PA-C
Assistant Professor of Physician Assistant
Education
Rana A. Bahl, MD
Associate Professor of Internal Medicine/
Cardiology
O.J. (Jerry) Bailes, DO
Professor of Family Medicine
Farhan Bakir, MD, MS
Professor of Internal Medicine
Bradley A. Baldwin, DO
Assistant Professor of Surgery
Vijaya Bansal, MD
Assistant Professor of Obstetrics/Gynecology
Steven H. Barag, DO, MS
Assistant Professor of Family Medicine
Rebecca Barnett, PA-C
Assistant Professor of Physician Assistant
Education
Rodolfo Cantu Barrera, DO
Assistant Professor of Pediatrics
Connie P. Bartlett, DO
Assistant Professor of Pediatrics
Geoffrey Baum, DO
Assistant Professor of Surgery
Daniel J. Beavers, DO
Associate Professor of Family Medicine/
Psychiatry
Robert D. Belanger, DO
Professor of Family Medicine
Joseph W. Bell Jr., DO
Assistant Professor of Obstetrics/Gynecology
Robert B. Bell, DO
Professor of Family Medicine
Linda Beth Benaderet, DO
Professor of Internal Medicine/Oncology
Michael Benavidez, DO
Assistant Professor of Family Medicine
Paul Benchwick, DO
Professor of Internal Medicine
Irvin S. Benowitz, DO
Associate Professor of Family Medicine
Mark P. Berland, DO
Assistant Professor of Obstetrics/Gynecology
Yoopin Bernbrock, PharmD
Assistant Professor of Pharmacy Practice
Steven M. Beutler, MD
Assistant Professor of Internal Medicine/
Infectious Diseases
A. Raja Bhupathy, DO
Assistant Professor of Family Medicine/
Dermatology
187
Vellore R. Bhupathy, MD, FACOG
Associate Professor of Obstetrics/Gynecology
Henry B. Bikhazi, MD, FACS
Assistant Professor of Surgery/
Otorhinolaryngology
Lori B. Birndorf, DO
Assistant Professor of Surgery/Ophthalmology
Murray L. Black, DO
Adjunct Assistant Professor of Family Medicine
Eliot S. Blackman, DO
Assistant Professor of Family Medicine
Andre V. Blaylock, MD
Assistant Professor of Family Medicine
William A. Blee, MD
Assistant Professor of Internal Medicine
Russell C. Bloom, DO
Assistant Professor of Family Medicine
Robert J. Bohr, MD
Assistant Professor of Surgery/Orthopedics
Richard A. Bond, DO
Associate Professor of Family Medicine
Gregory R. Bonomo, MD
Assistant Professor of Internal Medicine/
Neurology
Timothy R. Borman, DO
Assistant Professor of Surgery/Orthopedics
Allen D. Bott, MD
Assistant Professor of Internal
Medicine/Neurology
James B. Boyd, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Cory D. Boyles, MD
Assistant Professor of Physician Assistant
Education
John D. Branch, DO
Assistant Professor of Family Medicine
Michael Brand, MD
Assistant Professor of Internal Medicine/
Radiology
Rodney D. Brandt, MD
Assistant Professor of Surgery/Orthopedics
David A. Brauner, DO
Associate Professor of Pediatrics
Marc D. Braunstein, DO
Assistant Professor of Family Medicine
Randy J. Brazie, MD
Assistant Professor of Family Medicine/
Psychiatry
Mary Lou Breslin, MS
Adjunct Assistant Professor of Health
Professions Education
Sister Anne E. Brooks, DO
Associate Professor of Family Medicine
Thomas C. Brown, PhD
Associate Professor of Family Medicine/
Behavioral Sciences
Karen E. Brungardt, DO
Assistant Professor of Family Medicine
Bernard Buchanan, MD
Assistant Professor of Family Medicine/
Psychiatry
Timothy W. Burke, DO
Associate Professor of Internal Medicine/
Gastroenterology
Patrick J. Burns, DO
Assistant Professor of Internal Medicine/
Neurology
Michael S. Burton, MD
Assistant Professor of Family Medicine
Robert D. Bush, MD
Assistant Professor of Family Medicine
Jay M. Butterman, DO
Assistant Professor of Family Medicine/
Psychiatry
Grethel A. Cabison, MD
Assistant Professor of Surgery/Anesthesiology
188
Carol T. Cahill, DO
Assistant Professor of Pediatrics
William J. Cairney, PhD
Adjunct Professor of Family Medicine
Paul H. Caldron, DO
Assistant Professor of Internal Medicine/
Rheumatology
John B. Campbell, MD
Assistant Professor of Internal Medicine/
Pathology
Dennis M. Carden, DO
Associate Professor of Obstetrics/Gynecology
Samuel A. Carlis, DO
Assistant Professor of Family Medicine
Sherie Carnegie, DO
Assistant Professor of Family Medicine
Michael A. Carnevale, DO
Assistant Professor of Internal Medicine
Dale M. Carrison, DO
Assistant Professor of Family
Medicine/Emergency Medicine
John Joseph Cassani, DO
Assistant Professor of Family Medicine
Angela Jo Castro, PA-C
Instructor of Physician Assistant Education
Mary Caizza Cerni, DO
Assistant Professor of Family Medicine
Ramon M. Cestero, MD
Associate Professor of Obstetrics/Gynecology
Mikyung Chai, BS
Assistant Professor of Pharmacy Practice
Sammy C. Chan, MD
Assistant Professor of Physician Assistant
Education
Jonathan L. Chang, MD
Assistant Professor of Surgery/Orthopedics
Laura Chang-Strauss, MD
Assistant Professor of Pediatrics
Janet Cheetham, PharmD
Assistant Professor of Pharmacy Practice
Kenneth S. Cheng, DO
Assistant Professor of Physician Assistant
Education
Stuart B. Chesky, DO
Professor of Obstetrics/Gynecology
Gary Lee Child, DO
Assistant Professor of Family Medicine
William L. Chin, DO
Assistant Professor of Internal Medicine
William T. Choctaw, MD
Associate Professor of Surgery
Michael S. Choi, MD
Assistant Professor of Surgery/Anesthesiology
Serina Chong, PharmD
Assistant Professor of Pharmacy Practice
Don L. Christensen, MD, FACS
Professor of Surgery
Lance W. Christiansen, DO
Assistant Professor of Family Medicine
Philip S. Cifarelli, MD, JD
Professor of Internal Medicine/Gastroenterology
Robin D. Clark, MD
Professor of Pediatrics/Medical Genetics
Susan J. Clark, MD
Associate Professor of Pediatrics/Endocrinology
Therese Sage Clark, PharmD
Assistant Professor of Pharmacy Practice
Trence Clark, MD
Assistant Professor of Family Medicine/
Emergency Medicine
John O. Clune, MD
Assistant Professor of Internal Medicine/
Hematology &Oncology
Ellen Clymer, EdD
Adjunct Associate Professor of Health
Professions Education
189
Alan L. Cohen, DO
Assistant Professor of Family Medicine
Donald A. Cohen, DO
Adjunct Assistant Professor of Physician
Assistant Education
Murray H. Cohen, DO
Professor of Internal Medicine
Robert S. Cohen, DO
Associate Professor of Internal Medicine/
Nephrology
Samantha Cohen, PA-C
Instructor of Physician Assistant Education
Steven W. Cohen, DO
Assistant Professor of Family Medicine
William C. Cohen, DO
Assistant Professor of Surgery/
Otorhinolaryngology
Wilbur Cole III, DO
Assistant Professor of Family Medicine
Stacey L. Coleman, DO
Assistant Professor of Family Medicine
Randy E. Collins, DO
Assistant Professor of Obstetrics/Gynecology
Francis L. Comunale, MD
Professor of Surgery/Anesthesiology
Ralph E. Conner, DO
Assistant Professor of Family Medicine/
Emergency Medicine
David A. Connett, DO
Associate Professor of Family Medicine
Eugene T. Conte, DO
Assistant Professor of Family Medicine/
Dermatology
Milissa A. Cooper, DO
Assistant Professor of Family Medicine
Joel B. Cooperman, DO
Associate Professor of Family Medicine
Marshall Cooperson, DO
Assistant Professor of Internal Medicine
M. Larry Copeland, DO
Assistant Professor of Surgery/Orthopedics
Joe Corless, MD
Associate Professor of Pediatrics
Michael Coronado, PharmD
Assistant Professor of Pharmacy Practice
Conrad A. Cox, MD
Assistant Professor of Internal Medicine
Gary W. Crawford, MD
Assistant Professor of Internal Medicine
Linda L. Crawford, DO
Assistant Professor of Family Medicine
Gary M. Critser, DO
Assistant Professor of Family Medicine
James A. Crosby, DO
Assistant Professor of Internal
Medicine/Neurology
Michael P. Curley, MD
Assistant Professor of Physician Assistant
Education
Jack Dabbert, MS, PT
Adjunct Assistant Professor of Physical Therapy
Education
Himmet Dajee, MD
Assistant Professor of Surgery
Maria F. Daly, DO
Assistant Professor of Family Medicine
Joseph Damiani, DO
Assistant Professor of Surgery/Plastic Surgery
Kathleen Damiani, MD
Assistant Professor of Surgery/
Otorhinolaryngology
Stephen Damiani, DO
Assistant Professor of Internal Medicine/
Endocrinology
Sid Danesh, MD
Assistant Professor of Family Medicine
190
Nghiem Duc Dang, MD
Assistant Professor of Surgery
Sarah G. Daum, EdD
Adjunct Associate Professor of Health
Professions Education
Bert J. (Hans) Davidson, MD, PhD
Assistant Professor of Obstetrics/Gynecology
Richard C. Davies, DO
Assistant Professor of Family Medicine
Steven E. Davis, DO, MS
Assistant Professor of Family Medicine
Anil Daya, MD
Assistant Professor of Internal Medicine
James J. Dearing, DO
Assistant Professor of Family Medicine
Lori de Bold, MD
Associate Professor of Physician Assistant
Education
Lino J. de Guzman, MD
Assistant Professor of Internal Medicine/
Gastroenterology
Ricardo E. de Napoli, DO
Assistant Professor of Family Medicine
Harry W. Depew, MD
Assistant Professor of Family Medicine
Nilesh Desai, MD
Assistant Professor of Internal Medicine
Steven M. Deterville, MD
Assistant Professor of Family Medicine
Joel Dickerman, DO
Professor of Family Medicine
Dinh V. Dinh, DO
Assistant Professor of Family Medicine
Lew B. Disney, MD, PhD
Assistant Professor of Surgery
Stephen D. Docherty, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Neil E. Doherty III, MD
Assistant Professor of Internal Medicine/
Cardiology
Eric J. Dolgin, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
William C. Domb, DMD
Associate Professor of Family Medicine/
Dentistry
Thomas K. Donaldson, MD
Associate Professor of Surgery
Tennison S. Dong, MD
Assistant Professor of Surgery
Gregory J. Downs, MD
Assistant Professor of Surgery/Anesthesiology
Roger D. Duber, DO
Professor of Internal Medicine/Cardiology
Patrick Duke, PA-C
Instructor of Physician Assistant Education
Ian R. Duncan, DO
Assistant Professor of Family Medicine
Sheila K. Dunlop, DO
Assistant Professor of Family Medicine
Virginia (Ginny) D. Dunn, MS, PT
Adjunct Assistant Professor of Physical Therapy
Education
Nguyen (Andy) D. Duy, MD
Assistant Professor of Surgery/Vascular Surgery
Emily A. Ebert, MD
Associate Professor of Family Medicine
Richard E. Eby, DO
Professor of Obstetrics/Gynecology
Joel B. Edelstein, DO
Assistant Professor of Internal Medicine
Roy Egari, MD
Assistant Professor of Surgery/Urology
Hisham El-Bayer, MD
Assistant Professor of Surgery
191
Mohamad Eletreby, PharmD
Assistant Professor of Pharmacy Practice
Dale A. Elleson, DO
Assistant Professor of Surgery/
Otorhinolaryngology
Bernard T. Elpedes, DO
Assistant Professor of Family Medicine
Larry I. Emdur, DO, PhD
Assistant Professor of Internal Medicine/
Pulmonary Medicine
Richard J. Emerson, DO
Professor of Surgery/Orthopedics
Paul E. Emmans Jr., DO
Assistant Professor of Family Medicine
Jack D. England, DO
Professor of Family Medicine/Emergency
Medicine
Scott Engwall, MD
Assistant Professor of Surgery
Carl M. Erikson, DO
Assistant Professor of Family Medicine
J. Yusuf Erskine, DO
Assistant Professor of Family Medicine
Brenda Espe, DO
Assistant Professor of Family Medicine
James T. Evans, MD
Assistant Professor of Family Medicine
Thomas W. Eyler, DO
Assistant Professor of Family Medicine
Wade Faerber, DO
Associate Professor of Surgery/Orthopedics
Robert R. Fajardo, PA-C
Instructor of Physician Assistant Education
Rachel Farrell, PA-C
Instructor of Physician Assistant Education
John R. Feeney, DO
Assistant Professor of Family Medicine
Gary M. Feinberg, MD
Assistant Professor of Surgery/
Otorhinolaryngology
Michael J. Feinstein, DO
Professor of Family Medicine
Rodney J. Felber, DO
Assistant Professor of Internal Medicine
Edward M. Feldman, DO
Assistant Professor of Obstetrics/Gynecology
George Ferenczi, MD
Assistant Professor of Internal Medicine/
Gastroenterology
Carl E. Ferguson, DO
Assistant Professor of Family Medicine
Ronald B. Ferris, MD
Associate Professor of Family Medicine
Henie A. Fialkoff, MD
Assistant Professor of Pediatrics
George Fields, DO
Associate Professor of Family Medicine
Elizabeth Finebaum, PA-C
Instructor of Physician Assistant Education
David E. Fisher, MD
Associate Professor of Physician Assistant
Education
Katherine L. Fisher, DO
Assistant Professor of Internal Medicine
Steven M. Fitzmorris, MD
Assistant Professor of Internal Medicine/
Cardiology
Bruce D. Flagg, DO
Assistant Professor of Family Medicine
Paul M. Fleiss, MD, MPH
Professor of Pediatrics
Stanley L.K. Flemming, DO
Associate Professor of Family Medicine
Jon W. Fong, DO
Assistant Professor of Family Medicine
192
Nicole Foster, PA-C, MS
Assistant Professor of Physician Assistant
Education
Ali Fouladi, MD
Assistant Professor of Surgery
Paul A. Fredrick, MD
Associate Professor of Internal Medicine
John B. Freitas, DO
Assistant Professor of Family Medicine
Richard Frelinger, DO
Assistant Professor of Family Medicine
Gerald Stanley Friedman, MD
Associate Professor of Family Medicine
Theodore A. Friedman, MD
Associate Professor of Internal Medicine/
Pathology
Leonard M. Fromer, MD
Assistant Professor of Family Medicine
Byron Fujimoto, MD
Assistant Professor of Internal Medicine/
Radiology
Ronald Y. Fujimoto, DO
Assistant Professor of Family Medicine
Michele Fujiokon, PharmD
Assistant Professor of Pharmacy Practice
Geoffrey Furman, MD
Assistant Professor of Family Medicine
Balu Gadhe, MD
Assistant Professor of Internal Medicine
Karen L. Gaio, MD
Assistant Professor of Obstetrics/Gynecology
Anil K. Gandhi, MB/BS
Assistant Professor of Family Medicine
James E. Garmon Jr., PA-C
Assistant Professor of Physician Assistant
Education
Ronny G. Ghazal, MD
Associate Professor of Surgery/Orthopedics
Bharati Ghosh, MD
Associate Professor of Pediatrics
Mark Gibson, PA-C
Instructor of Physician Assistant Education
Ulric Gilkes, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Lawrence S. Glass, DO
Assistant Professor of Family Medicine
Jeffrey W. Glassheim, DO
Assistant Professor of Pediatrics
Justin R. Glodowski, DO
Assistant Professor of Family Medicine
Appanagari (Dev) Gnanadev, MD
Associate Professor of Surgery
Sergio Y. Go Jr, MD
Assistant Professor of Internal Medicine
Edward Goering, DO, MS
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Stanley A. Golanty, MD
Professor of Internal Medicine
Allan P. Goldman, DO
Associate Professor of Family Medicine
Frank C. Gomez, DrPH.
Assistant Professor of Physician Assistant
Education
Myron J. Gomez, MD
Assistant Professor of Surgery/Vascular Surgery
Allen E. Gorenberg, MD
Assistant Professor of Internal Medicine/Allergy
Daniel Gorenberg, MD
Assistant Professor of Internal Medicine/Allergy
Dale J. Gorski, DO
Assistant Professor of Family Medicine
David C. Gorsulowsky, MD
Assistant Professor of Family Medicine/
Dermatology
193
Lawrence F. Gosenfeld, DO
Assistant Professor of Family Medicine/
Psychiatry
Galal S. Gough, MD
Associate Professor of Obstetrics/Gynecology
David S. Goya, DO
Assistant Professor of Internal Medicine/
Pulmonary Diseases
William M. Graham, DO
Associate Professor of Surgery
Howard Graitzer, DO
Associate Professor of Internal Medicine
Barry S. Grames, MD
Assistant Professor of Surgery
Gary A. Gramm, DO
Assistant Professor of Family Medicine
Bradley C. Grant, DO
Associate Professor of Family Medicine
David Greenberg, PA-C
Instructor of Physician Assistant Education
Gerald R. Greene, MD
Professor of Pediatrics/Infectious Diseases
Roger Greenham, PharmD
Assistant Professor of Pharmacy Practice
Lindy S. Griffin, DO
Assistant Professor of Family Medicine
Peter D. Grimm, DO
Associate Professor of Internal Medicine/
Oncology
James W. Groff, DO
Assistant Professor of Family Medicine/
Dermatology
Debra L. Gromacki-Blyth, PA-C
Instructor of Physician Assistant Education
Joel S. Grubbs, DO
Assistant Professor of Family Medicine
David Gu, DO
Assistant Professor of Internal Medicine
Gary W. Gulizia, DO
Assistant Professor of Family Medicine
Mahesh C. Gupta, MD
Assistant Professor of Internal Medicine
Suresh Gurbani, MD, PhD
Assistant Professor of Pediatrics
Thomas C. Gustafson, DO
Assistant Professor of Family Medicine
Angeline Hadiwidhaha, MD
Assistant Professor of Pediatrics
Thomas A. Haffey, DO
Professor of Internal Medicine/Cardiology
David B. Hagie, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Stefan L.J. Hagopian, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Roger Hall, DO
Assistant Professor of Family Medicine
Issa Y. Hallaq, DO
Associate Professor of Internal Medicine
Norman Hamada, PharmD
Assistant Professor of Pharmacy Practice
Robert C. Hamilton, MD
Assistant Professor of Pediatrics
Curtis R. Handler, MD
Assistant Professor of Internal Medicine/
Radiology
Lofty R. Hanna, MD
Assistant Professor of Internal Medicine
Charles E. Hansing, MD
Assistant Professor of Internal Medicine/
Cardiology
Ben Hara, DPM
Professor of Family Medicine/Podiatry
W. Benson Harer, MD
Professor of Obstetrics/Gynecology
194
Pamela J. Harford, DO
Assistant Professor of Family Medicine
Jon Frederic Harrell, DO, FACS
Assistant Professor of Surgery
Clyde O. Harris III, MD
Assistant Professor of Surgery
Elliot A. Harris, MD
Professor of Family Medicine/Psychiatry
Imran Hasnain, MD
Assistant Professor of Internal Medicine
John R. Hawes Jr., DO
Associate Professor of Family Medicine
Todd Hee, MD
Associate Professor of Internal Medicine
Ole A. Heggeness, DO
Assistant Professor of Family Medicine
Joseph J. Helak, DO
Professor of Surgery
Helge S. Helgesen, PA-C
Instructor of Physician Assistant Education
William W. Henning, DO
Assistant Professor of Family Medicine
Joseph J. Herbert, MD
Assistant Professor of Pediatrics
Guillermo Hernandez, DO
Assistant Professor of Family Medicine
Raul Hernandez, MD
Assistant Professor of Physician Assistant
Education
Stanley S. Herr, DO
Assistant Professor of Family Medicine
Edward A. Heusch, DO
Associate Professor of Surgery
Michael L. Hicks, BA, PA-C
Assistant Professor of Physician Assistant
Education
Cynthia A. Hill, DO
Assistant Professor of Family Medicine
Ronald H. Hino, MD
Assistant Professor of Physician Assistant
Education
Jerry W. Hizon, MD
Assistant Professor of Physician Assistant
Education
Timothy P. Hodges, DO
Assistant Professor of Family Medicine
Joseph O. Hoffman, DO
Associate Professor of Family Medicine
Marc A. Hoffman, DO
Assistant Professor of Family Medicine
David P. Hofheins, DO
Assistant Professor of Family Medicine
E. Carlisle Holland, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Philip Holman, PharmD
Assistant Professor of Pharmacy Practice
Lorin G. Holst, MD
Assistant Professor of Internal Medicine
Charles Holzner, MD
Professor of Internal Medicine
Theresa A. Hong, DO
Assistant Professor of Family Medicine
William K. Hooks III, MD
Assistant Professor of Internal Medicine/
Radiology
Franklin Horowitz, MD
Professor of Surgery (Emeritus)
Mark Horowitz, DO
Assistant Professor of Family Medicine/
Dermatology
Joseph Hourany, MD
Assistant Professor of Internal Medicine/
Pulmonology
Bruce R. Hoyle, MD
Assistant Professor of Physician Assistant
Education
195
David W. P. Huang, MD
Assistant Professor of Surgery/Orthopedics
Kuo-Liang Huang, MD
Assistant Professor of Internal Medicine/
Infectious Diseases
W. Luke Huang, MD
Assistant Professor of Pediatrics
Catherine Ann Hunter, DO
Assistant Professor of Obstetrics/Gynecology
Paul V.B. Hyde, MD
Assistant Professor of Surgery
John Hyun, PharmD
Assistant Professor of Pharmacy Practice
Robert A. Innocenzi, DO
Assistant Professor of Surgery/Ophthalmology
Anthony L. Jackson, MD
Assistant Professor of Physician Assistant
Education
Marianne B. Jacobs, DO
Assistant Professor of Internal Medicine/
Neurology
Arthur J. Jaffee, JD
Professor of Medical Jurisprudence
David S. James, DO
Assistant Professor of Family Medicine
Wen-Feng Jan, MD
Assistant Professor of Pediatrics/Endocrinology
Carl Jansen, MD
Professor of Internal Medicine/Radiology
Kedy Ying Jao, DO
Assistant Professor of Family Medicine
Mahmood J. Jazayeri, MD
Assistant Professor of Surgery/Orthopedics
Richard R. Jeffries, DO
Associate Professor of Family Medicine
Kraig K. Jenson, MD
Assistant Professor of Family Medicine/
Dermatology
Debra L. Johnson, RN, NP, PA-C
Assistant Professor of Physician Assistant
Education
Eric G. Johnson, MPT
Adjunct Assistant Professor of Physical Therapy
Education
Gary R. Johnson, DO, DVM
Assistant Professor of Family Medicine
Jacqueline A. Johnson, MD
Assistant Professor of Family Medicine
Robert C. Jones, MD
Assistant Professor of Internal Medicine
Christopher Jordan, MD
Associate Professor of Surgery/ Orthopedics
Layne S. Jorgensen, DO
Assistant Professor of Family Medicine
Randal Carl Juengel, MD
Assistant Professor of Internal Medicine/
Pathology
Anthony A Juguilon, MD
Assistant Professor of Internal Medicine/
Pathology
Nami Jun, PharmD
Assistant Professor of Pharmacy Practice
Nancy R. Kahaner, DO
Assistant Professor of Obstetrics/Gynecology
June Isaacson Kailes, MSW
Adjunct Associate Professor of Health
Professions Education
Stanley A. Kaller, DO
Assistant Professor of Family Medicine
Charles L. Kaluza, DO
Associate Professor of Surgery/
Otorhinolaryngology
Steven D. Kamajian, DO
Associate Professor of Family Medicine
Frank G. Karneges, DO
Assistant Professor of Internal Medicine
196
Thomas J. Karras, MD
Associate Professor of Internal Medicine/
Cardiology
Andre M. Kasko, DO
Assistant Professor of Physician Assistant
Education
Hooshang Kasravi, MD
Assistant Professor of Surgery
Michael D. Kasseles, DO
Assistant Professor of Internal Medicine
Louis B. Kasunic, DO
Assistant Professor of Family Medicine
Lionel B. Katchem, DO
Associate Professor of Family Medicine
Lia Katz, MD
Assistant Professor of Family Medicine
Martin H. Kay, MD, PhD
Assistant Professor of Family Medicine/
Dermatology
Christopher Keenan, MD
Assistant Professor of Family Medicine
Lori A. Kemper, DO
Associate Professor of Family Medicine
Darlina M. Keseg-Manthei, DO
Assistant Professor of Family Medicine
Stephen E. Kessler, DO
Assistant Professor of Family Medicine/
Dermatology
Ahmed Khosrowshahi, MD
Assistant Professor of Physician Assistant
Education
Karen S. Kiefer, DO
Assistant Professor of Family Medicine/
Psychiatry
Peter V. Kilburn, DO
Professor of Surgery
Karine Kim, PharmD
Assistant Professor of Pharmacy Practice
Lauren Kim, PharmD
Assistant Professor of Pharmacy Practice
Hwa-Kou King, MD
Professor of Internal Medicine/Anesthesiology
Neil E. Klein, MD
Assistant Professor of Surgery/Plastic &
Reconstructive
Calvin N. Kobluk, DVM, DVSc
Professor of Veterinary Medicine
Johannes Koch, MD
Assistant Professor of Internal Medicine
Shahrokh Kohanim, DO
Assistant Professor of Family Medicine
Benjamin L. Konell, DO
Assistant Professor of Family Medicine
Choon Won Koo, MD
Assistant Professor of Obstetrics/Gynecology
Mark S. Kosins, MD
Professor of Family Medicine/Psychiatry
Dana Kosmala, DO
Assistant Professor of Pediatrics
Richard T. Kotomori, Jr., MD
Assistant Professor of Family Medicine
Thomas Koumas, MD
Associate Professor of Family Medicine
Alan P. Kratz, MD
Assistant Professor of Surgery/Ophthalmology
David E. Kreshek, MD
Assistant Professor of Surgery
Divakar R. Krishnareddy, MD
Assistant Professor of Surgery/Orthopedics
Pamela C. Krochalk, DrPH.
Professor of Physician Assistant Education
Ellen B. Kruusmagi, MD
Assistant Professor of Family Medicine
Donald J. Kurth, MD
Assistant Professor of Family Medicine/
Emergency Medicine
197
Michael Z. Kurtz, DO
Assistant Professor of Family Medicine
Veronika R. Kurucz, MD
Assistant Professor of Internal Medicine
Mary Jo Kutler, DO
Assistant Professor of Pediatrics
Eugene L. Kwong, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Grant Lackey, PharmD
Assistant Professor of Pharmacy Practice
Jennifer Lackey, PharmD
Assistant Professor of Pharmacy Practice
Linda D. Lafferty, DO, MS
Associate Professor of Family Medicine
Elizabeth M. Laine, PA-C
Instructor of Physician Assistant Education
James M. Lally, DO, MS
Assistant Professor of Family Medicine
Richard E. Land, DO
Associate Professor of Family Medicine/
Psychiatry
Carol L. Lang, DO
Assistant Professor of Family Medicine
Elizabeth C. Laqui, MD
Assistant Professor of Physician Assistant
Education
Lawrence A. Larson, DO
Assistant Professor of Pediatrics
Laurence J. Kasky, MD
Assistant Professor of Family Medicine
Ronald E. Lazar, MD
Assistant Professor of Internal Medicine/
Anesthesiology
Arthur J. Lazik, MD, PhD
Assistant Professor of Internal Medicine/
Cardiology
Ha M. Le, MD
Assistant Professor of Internal Medicine/
Radiology
Scott C. Lederhaus, MD
Assistant Professor of Surgery
Carol Hyeun Lee, MD
Assistant Professor of Family Medicine/
Emergency Medicine
James T. Lee, DO
Associate Professor of Family Medicine
Thomas T. Lee, MD, FACOG
Assistant Professor of Obstetrics/Gynecology
William Y.W. Lee, DO
Assistant Professor of Family Medicine
David P. Leibel, DO
Assistant Professor of Surgery/Urology
Steven Leifheit, DO
Assistant Professor of Family Medicine
John F. Lennox, DO
Associate Professor of Obstetrics/Gynecology
Peter C. LePort, MD
Assistant Professor of Surgery
Catherine Jones Lesnick, MS, PT
Adjunct Assistant Professor of Physical Therapy
Education
David Z. Levine, DO
Assistant Professor of Family Medicine
M. Richard Levinson, DO
Assistant Professor of Pediatrics
Gwen A. Levitt, DO
Assistant Professor of Family Medicine/
Psychiatry
Elaine Levy, BS
Assistant Professor of Pharmacy Practice
David O. Lewis, MD
Assistant Professor of Family Medicine
Judith L. Lewis, DO
Assistant Professor of Family Medicine
198
Sherman N. Lewis, DO
Assistant Professor of Surgery/Plastic &
Reconstructive
Lawrence Leyba, DO
Professor of Surgery/Anesthesiology
David Y. Li, DO
Assistant Professor of Internal
Medicine/Radiology
Robert Ligorsky, DO
Associate Professor of Internal Medicine/
Hematology and Oncology
Joseph L. Lillo, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Alice Lim, PharmD
Assistant Professor of Pharmacy Practice
Howard B. Limmer, DO
Associate Professor of Family Medicine
Augustin Lin, DO
Assistant Professor of Family Medicine
Matthew Y.C. Lin, MD
Assistant Professor of Surgery/Orthopedics
Leonard M. Linde, MD
Professor of Pediatrics
Cathleen Lindsay, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Ronald Liskanich, DO
Assistant Professor of Family Medicine/
Dermatology
Sol Lizerbram, DO
Professor of Family Medicine
Hedy C. Loa, MD
Assistant Professor of Internal Medicine/
Geriatrics
William T. Long, MD
Assistant Professor of Physician Assistant
Education
Paul K. Longmore, PhD
Adjunct Professor of Health Professions
Education
Christopher Lopatosky, PA-C
Assistant Professor of Physician Assistant
Education
Felice L. Loverso, Ph.D.
Assistant Professor of Health Professions
Education
Nelman C. Low, MD
Assistant Professor of Surgery/
Otorhinolaryngology
Kenneth Luck, PharmD
Assistant Professor of Pharmacy Practice
Grant Lum, PharmD
Assistant Professor of Pharmacy Practice
Lisa M. Lupo, MD
Assistant Professor of Obstetrics/Gynecology
Hector F. Luque, DO
Assistant Professor of Internal Medicine
Pamela Renee Archer Lux, DO
Assistant Professor of Family Practice/
Emergency Medicine
Marc E. Lynch, DO
Assistant Professor of Surgery/Anesthesiology
Alfred C. Ma, MD, PhD, MBA
Professor of Internal Medicine/Anesthesiology
Richard H. Mabie, MD
Assistant Professor of Pediatrics
Daryl K. MacCarter, MD
Assistant Professor of Internal Medicine/
Rheumatology
F. Roy MacKintosh, MD, PhD
Professor of Internal Medicine
Gregory R. Maddex, DO
Assistant Professor of Family Medicine
Julie Madorsky, MD
Professor of Family Medicine/Physical Medicine
and Rehabilitation
199
Lon Madsen, DO
Assistant Professor of Family Medicine
Harold I. Magoun Jr., DO
Professor of Family Medicine/Osteopathic
Manipulative Medicine
Michael J. Mahon, DO
Associate Professor of Family Medicine/
Dermatology
Mark B. Maine, MSHSA
Instructor of Health Professions Education
Lisa L. Majer, DO
Assistant Professor of Family Medicine/Sports
Medicine
Samuel A. Malayan, MD, PhD
Assistant Professor of Internal Medicine
Barry D. Malina, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
John F. Manfredonia, DO
Assistant Professor of Family Medicine
Andrew J. Manos, DO
Associate Professor of Family Medicine
Rudy R. Manthei, DO
Assistant Professor of Surgery/Ophthalmology
Scott E. Manthei, DO
Assistant Professor of Surgery/
Otorhinolaryngology
Krishna N. Manvi, MD
Associate Professor of Internal Medicine/
Cardiology
Charles M. Maples, DO
Assistant Professor of Family Medicine
Shoaib U. Maqvi, MD
Assistant Professor of Internal Medicine
Calvin Marantz, MD
Associate Professor of Internal Medicine/
Pathology
Rod Marchiando, PharmD
Assistant Professor of Pharmacy Practice
Dante E. Marinelli, MD
Associate Professor of Surgery/Urology
Steven Marks, DO
Assistant Professor of Internal Medicine
David E. Marshburn, DO
Assistant Professor of Surgery/Ophthalmology
Michael J. Martelli, DO
Associate Professor of Family Medicine
Katherine A. Martin, DO
Assistant Professor of Family Medicine
Timothy B. Martin, DO
Assistant Professor of Family Medicine
Kathryn Martinazzi, PharmD
Assistant Professor of Pharmacy Practice
Robert V. Mason, DVM, MS
Associate Professor of Veterinary Medicine
James D. Matiko, MD
Associate Professor of Surgery/Orthopedics
H. Preston Matthews, DO
Assistant Professor of Family Medicine
Robert J. Maurer, DO
Associate Professor of Pediatrics
C. L. McArthur III, MD, MBA
Associate Professor of Family Medicine/
Emergency Medicine
Edward P. McDermott, DO
Assistant Professor of Surgery/Orthopedics
Sharon S. McGarrity, DO
Assistant Professor of Family Medicine
Maj. Thomas A. McGerty, DO
Assistant Professor of Pediatrics
William H. McGhee, MD
Professor of Family Medicine/Psychiatry
Paul McHugh, DO
Assistant Professor of Family Medicine
Kelly L. McKerahan, DO
Assistant Professor of Family Medicine
200
Matthew J. McMahon, DO
Assistant Professor of Internal Medicine/
Cardiology
John M. Medeiros, PhD, PT
Assistant Professor of Surgery/Orthopedics
James J. Mendola, DO
Professor of Surgery/Otorhinolaryngology
Max Mener, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Norman S. Merchant, MD
Associate Professor of Obstetrics/Gynecology
Clifford D. Merkel, MD
Associate Professor of Surgery/Orthopedics
Frank J. Metzger, DO
Professor of Internal Medicine
Barry S. Meyer, DO
Assistant Professor of Internal Medicine
Wafa F. Michael, MD
Assistant Professor of Internal Medicine/
Pathology
Constantine A. Michas, MD, MPH
Assistant Professor of Surgery
Alexander Miller, MD
Assistant Professor of Family Medicine/
Dermatology
Howard G. Milstein, MD
Assistant Professor of Family Practice/
Dermatology
John S. Missanelli, DO
Professor of Obstetrics/Gynecology
Gary S. Mono, DO
Assistant Professor of Surgery
Louis H. Monty, MD
Assistant Professor of Family Medicine/
Psychiatry
Robert L. Moody, DO
Assistant Professor of Family Medicine
Cheryl L. Morell, MD
Assistant Professor of Pediatrics
James A. Morrow, DO
Assistant Professor of Family Medicine
Glynnis M. Morton, MD
Assistant Professor of Obstetrics/Gynecology
Bassam Mouazzen, MD
Assistant Professor of Internal Medicine
Angela K. Moultrie-Lizana, DO
Assistant Professor of Family Medicine
M. Kenneth Mudge, MB, ChB
Professor of Surgery/Orthopedics
Sharon K. Muenchow, MD
Assistant Professor of Surgery/Pediatrics
Moses T. Mukai Jr., DO
Assistant Professor of Obstetrics/Gynecology
Pramod Multani, MD
Assistant Professor of Internal Medicine/
Cardiology
Debra Foreman Munsell, PA-C
Associate Professor of Physician Assistant
Education
Wadsworth H. Murad, DO
Assistant Professor of Family Medicine/
Psychiatry
Vellore G. Muraligopal, MD
Associate Professor of Pediatrics
John Lamont Murdoch, MD
Professor of Internal Medicine
Mohan S. Nair, MD
Associate Professor of Family Medicine/
Psychiatry
G. Nalinajith Nanayakkara, MD
Assistant Professor of Obstetrics/Gynecology
J. Michael Nelson, DO
Assistant Professor of Family Medicine/
Emergency Medicine
201
Robert G. Nelson, MD
Assistant Professor of Physician Assistant
Education
William E. Newsome, MD
Associate Professor of Internal Medicine
Anh Ngoc Nguyen, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Dana Huong Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Lan-Phuong Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Phong K. Nguyen, MD
Assistant Professor of Physician Assistant
Education
Phuong Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Tuyen Ngoc Nguyen, PharmD
Assistant Professor of Pharmacy Practice
Karen J. Nichols, DO
Associate Professor of Internal Medicine
Peter J. Niciforos, MD
Assistant Professor of Family Medicine
Andre M. Noe, MD
Assistant Professor of Physician Assistant
Education
James W. Norcross, DO
Assistant Professor of Family Medicine
Robert E. Norcross, MD
Associate Professor of Surgery
Jeffrey C. Northup, DO
Associate Professor of Obstetrics/Gynecology
William H. Nuesse, MD
Assistant Professor of Family Medicine
Chinyere N. Obasi, MD
Instructor of Surgery/Neurosurgery
Udoh O. Obioha, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Cynthia Odegard, PharmD
Assistant Professor of Pharmacy Practice
So-Jeong Oh, PharmD
Assistant Professor of Pharmacy Practice
Ikechukwu Ohiaeri, MD
Assistant Professor of Family Medicine/
Psychiatry
Joseph L. Olivarez, PA-C
Instructor of Physician Assistant Education
Daniel Olson, DO
Assistant Professor of Family Medicine
Robert W. Olson, DO
Assistant Professor of Internal Medicine/
Cardiology
Edward Onuma, MD
Assistant Professor of Internal Medicine/
Gastroenterology
Stephen Eric Osburn, MD
Assistant Professor of Pediatrics
Mark P. Owens, MD
Associate Professor of Surgery
Edward E. Packer, DO
Associate Professor of Pediatrics
Jeffrey Packer, DO
Assistant Professor of Internal Medicine/
Nephrology
James A. Padova, MD
Assistant Professor of Internal Medicine
Joseph T. Palermo Jr., DO
Associate Professor of Internal Medicine
George C. Parides, DO
Assistant Professor of Internal Medicine/
Pulmonary Diseases
Heran Angela Park, MD
Assistant Professor of Pediatrics
Samuel Kyung Uk Park, MD
Assistant Professor of Family Medicine
202
Dennis R. Parker, DO
Assistant Professor of Family Medicine
Richard A. Parker, DO
Assistant Professor of Family Medicine/Sports
Medicine
David M. Parrack, DO
Assistant Professor of Surgery/Urology
Daniel D. Pearce, DO
Assistant Professor of Family Medicine
David J. Peck, DO
Assistant Professor of Family Medicine
Luis Jesus Mejia Perez, MD
Assistant Professor of Physician Assistant
Education
Robert G. Peterson, MD
Assistant Professor of Family Medicine
Warren A. Peterson, DO
Assistant Professor of Family Medicine/
Dermatology
Sara D. Petry, MD
Assistant Professor of Family Medicine/
Psychiatry
John Pettit, MD
Assistant Professor of Surgery
William J. Pevsner, DO
Assistant Professor of Family Medicine
Anthony Pham, MD
Assistant Professor of Physician Assistant
Education
Thang Pham, MD
Assistant Professor of Physician Assistant
Education
Hai Phan, MD
Assistant Professor of Internal Medicine/
Nephrology
Craig M. Phelps, DO
Associate Professor of Family Medicine/Sports
Medicine
Mitchel E. Phillips, DO, MS
Assistant Professor of Family Medicine
Wendell B. Phillips, DO
Assistant Professor of Family Medicine
John R. Piconi, MD
Assistant Professor of Surgery/Urology
Allyn M. Pierce, DO
Associate Professor of Obstetrics/Gynecology
Harry A. Pierce, DO
Associate Professor of Internal Medicine
Remy A. Piibe, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Ronald E. Pinkerton, MD
Professor of Family Medicine
Lynne B. Pirie, DO
Assistant Professor of Family Medicine/Sports
Medicine
Richard T. Pitts, DO
Associate Professor of Family Medicine/
Emergency Medicine
M. Jay Porcelli, DO, MS
Professor of Family Medicine
Gregson J. Porteous, DO
Assistant Professor of Surgery/Anesthesiology
Stuart Brent Porter, DO
Assistant Professor of Family Medicine
Larry Potts, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Michael A. Pousti, MD
Assistant Professor of Surgery/Plastic and
Reconstructive
Michael J. Powell, DO
Assistant Professor of Internal Medicine/
Rheumatology
Vance M. Powell, DO
Assistant Professor of Obstetrics/Gynecology
Na’Imah D. Powell-Williams, MD
Assistant Professor of Physician Assistant
Education
203
Arudi L. Prabhakar, MD
Assistant Professor of Surgery
Venu Prabaker, MD
Associate Professor of Internal Medicine
William J. Previte, DO
Assistant Professor of Surgery/
Orthopedics/Sports Medicine
Todd O. Primack, DO
Assistant Professor of Surgery/Anesthesiology
Charles Edward Pritchard Jr., DO
Assistant Professor of Pediatrics
Andrew S. Pumerantz, DO
Assistant Professor of Internal Medicine
Mark Purnell, MD
Assistant Professor of Surgery/Orthopedics
Paul A. Pyka, DO
Associate Professor of Obstetrics/Gynecology
John F. Quinn, MD
Assistant Professor of Family Medicine
David C. Rabinowitz, DO
Professor of Internal Medicine/Pulmonary
Medicine
Richard L. Ragle, DO
Assistant Professor of Family Medicine
Stephen R. Rakower, MD
Associate Professor of Surgery
Laura T. Rampil, DO
Assistant Professor of Family Medicine
John F. Randolph, MD
Associate Professor of Family Medicine
Lawrence D. Raphael, MD
Associate Professor of Internal Medicine
Hugo F. Rauld, MD
Assistant Professor of Physician Assistant
Education
Niren A. Raval, DO
Assistant Professor of Family Medicine
Carl A. Recine, MD
Assistant Professor of Internal Medicine/
Radiology
Joe W. Redd, DO
Assistant Professor of Family Medicine
David E. Rhodes, MD
Assistant Professor of Family Medicine
Terence P. Rhone, DO
Assistant Professor of Internal Medicine
E. Lee Rice, DO
Professor of Family Medicine/Sports Medicine
Robin (Rob) L. Richardson, DO
Assistant Professor of Family Medicine
Joel S. Richmon, MD
Assistant Professor of Internal Medicine/
Neurology
Ronald D. Richmond, MD
Assistant Professor of Physician Assistant
Education
Jerome B. Riebman, MD
Associate Professor of Surgery
Jeffrey D. Ries, DO
Associate Professor of Internal Medicine/
Neurology
Donna Rios, BS, PA-C, RN
Instructor of Physician Assistant Education
Andrea A. Roberson, DO
Assistant Professor of Family Medicine
Natalie Roberts, DO
Assistant Professor of Internal Medicine
Ward A. Robidart, PA-C
Instructor of Physician Assistant Education
Mark I. Robinson, MD
Assistant Professor of Internal Medicine/
Pulmonology
Zenia Robinson, PA-C
Assistant Professor of Physician Assistant
Education
204
Tari L. Roche, DO
Assistant Professor of Family Medicine
Arturo Rodrigues, PA-C
Instructor of Physician Assistant Education
Jose L. Rodriguez, MD
Professor of Surgery
Michael J. Rodriguez, MD
Professor of Surgery
Michael L. Rohrenback, DO
Assistant Professor of Family Medicine
Lorenzo Romney, DO
Assistant Professor of Family Medicine
Andrew J. Rooks, MD
Professor of Family Medicine/Psychiatry
Marc R. Rose, MD
Assistant Professor of Surgery/Ophthalmology
Michael R. Rose, MD
Assistant Professor of Surgery/Ophthalmology
Mark E. Rosen, DO
Assistant Professor of Family
Medicine/Osteopathic Manipulative Medicine
Alan S. Rosenthal, DO
Professor of Internal Medicine
Phyllis M. Ross, PA-C
Instructor of Physician Assistant Education
Timothy J. Roth, DO
Assistant Professor of Family Medicine
Horst R. Rudrich, DO
Assistant Professor of Family Medicine
Michael Rudolph, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Michael N. Rutman, DO
Assistant Professor of Internal Medicine
David M. Ryan, DO
Assistant Professor of Family Medicine
Thomas K. Ryu, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Shida Saam, DO
Assistant Professor of Family Medicine
Lovina Sabnani, DO
Assistant Professor of Surgery/Ophthalmology
Suresh Sabnani, DO
Assistant Professor of Family Medicine
Mazin Q. Sabri, MD
Assistant Professor of Surgery/Orthopedics
Michael Sachs, DO
Assistant Professor of Internal Medicine
Steven Sackrin, MD
Assistant Professor of Internal Medicine
Gurbinder S. Sadana, MD
Assistant Professor of Internal Medicine
Conrad Salinas, MD
Associate Professor of Family Medicine/
Emergency Medicine
David Saperia, MD
Assistant Professor of Physician Assistant
Education
David J. Saperstein, DO
Professor of Internal Medicine/Radiology
Phisit Saphyakhajon, MD
Assistant Professor of Pediatrics
Jan O. Sarkin, MD
Associate Professor of Surgery
Sampat S. Saste, MD
Assistant Professor of Internal Medicine
John D. Schaeffer, DO
Assistant Professor of Internal Medicine/
Neurology
Irving Schaffner, MD
Assistant Professor of Family Medicine
Ivan B. Schatz, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Kenneth Schell, PharmD
Assistant Professor of Pharmacy Practice
205
Kenneth C.J. Scherbarth, DO
Assistant Professor of Family Medicine
Clifton S. Schermerhorn, MD
Associate Professor of Family Medicine/
Psychiatry
Mark D. Schneider, DO
Associate Professor of Family Medicine
Robert B. Schorr, DO
Assistant Professor of Pediatrics/Psychiatry
Andrew O. Schreiber, MD
Assistant Professor of Internal Medicine/
Neurology
Saul E. Schreiber, DO
Associate Professor of Family Medicine/
Dermatology
Robert C. Schreiman, MD
Assistant Professor of Family Medicine
Lawrence Schuyler, DO
Assistant Professor of Family Medicine
Ernest R. Schwab, PhD
Adjunct Associate Professor of Physical
Therapy Education
Paul E. Schwartz, MD
Associate Professor of Physician Assistant
Education
Charles Schwengel, DO
Assistant Professor of Family Medicine
James H. Scott, DO
Assistant Professor of Family Medicine
Kendall G. Scott, MD
Associate Professor of Physician Assistant
Education
Martin T. Sechrist, DO
Associate Professor of Family Medicine
David Sellen, DMin
Associate Professor of Health Professions
Education
Avedik Semergian, MD
Assistant Professor of Internal Medicine/
Nephrology
Manohar R. Senra, MD
Assistant Professor of Internal Medicine
Michael A. Sequeira, MD
Assistant Professor of Physician Assistant
Education
Stephen R. Severance, MD
Associate Professor of Internal Medicine/
Gastroenterology
Conrado C. Sevilla III, MD
Assistant Professor of Family Medicine/
Psychiatry
Stewart Shankel, MD
Professor of Internal Medicine/Nephrology
Baljit K. Sharma, MD
Assistant Professor of Surgery/Cardiothoracic
Robert C. Sharp, MD
Professor of Pediatrics
Frank P. Sheridan, MD
Assistant Professor of Internal Medicine/
Pathology
Julie Ann Sherman, DO, MS
Assistant Professor of Family Medicine
Christan T. Shimoda, DO
Associate Professor of Family Medicine
Kathleen Jane Shimoda, RN
Assistant Professor of Family Medicine
Dong-Soo Shin, MD
Assistant Professor of Surgery
William L. Shoemaker, DO
Assistant Professor of Surgery/Orthopedics
Henrietta (Hennie) B. Sholars, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Randall G. Shue, DO
Assistant Professor of Family Medicine
206
Annie Shugarman, PA-C
Assistant Professor of Physician Assistant
Education
Javed Siddiqi, MD
Assistant Professor of Surgery/Neurosurgery
Antonio R. Silva, MD
Assistant Professor of Surgery/Oncology
Arnold Sin, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Ravinder P. Singh, MD
Assistant Professor of Family
Medicine/Psychiatry
Tejinder Singh, MD
Assistant Professor of Internal Medicine
Prem Singla, MD
Associate Professor of Family Medicine
C. Paul Sinkhorn, MD
Assistant Professor of Obstetrics/Gynecology
Harry B. Skinner, MD, PhD
Professor of Physician Assistant Education
Daniel M. Skotte Sr., DO
Assistant Professor of Family Medicine
Carl M. Smith, MD
Professor of Internal Medicine/Radiology
Carl W. Smith, MD
Assistant Professor of Surgery/Orthopedics
David E. Smith, MD
Professor of Family Medicine/Addiction
Medicine
Keith U. Smith, DO
Assistant Professor of Internal Medicine/
Anesthesiology
Kenneth R. Smith, DO
Assistant Professor of Family Medicine
Larry D. Smith, DO
Assistant Professor of Internal Medicine
Wyatt S. Smith, DO
Assistant Professor of Internal Medicine/
Hematology & Oncology
Dorian D. Snyder, MD
Assistant Professor of Family
Medicine/Emergency Medicine
Mehrzad M. Soleimani, DO
Assistant Professor of Family Medicine
Hamilton M. Solomon, PhD
Adjunct Assistant Professor of Physical Therapy
Education
Joseph K. Song, MD
Assistant Professor of Internal
Medicine/Cardiology
Willes Wolfe Sonnefield, MA, PT
Adjunct Assistant Professor of Physical Therapy
Education
Andrei Soran
Assistant Professor of Health Professions
Education
Michelle Spencer, PharmD
Assistant Professor of Pharmacy Practice
Richard Spini, PharmD
Assistant Professor of Pharmacy Practice
Yemelyan L. Spivak, MD
Assistant Professor of Surgery
Ruth Stanhiser, MD
Assistant Professor of Family Medicine
Robert A. Steedman, MD
Associate Professor of Surgery
Lisa M. Steffensen-Gambrath, DO
Assistant Professor of Family Medicine
Paul J. Steier, DO
Assistant Professor of Family Medicine
Michael A. Steingard, DO
Assistant Professor of Surgery/ Orthopedics
Paul M. Steingard, DO
Professor of Family Medicine/Sports Medicine
207
Scott A. Steingard, DO
Assistant Professor of Family Medicine
John C. Steinmann, DO
Associate Professor of Surgery/Orthopedics
Gloria J. Stevens, MD
Assistant Professor of Family
Medicine/Dermatology
William C. Stonecipher, DO
Associate Professor of Family Medicine
John Strathakis, DO
Assistant Professor of Family Medicine/
Dermatology
Howard N. Straub, DO
Professor of Surgery/Ophthalmology
Josef Strazynski, DO
Associate Professor of Family Medicine
Gregory D. Strebel, DO
Assistant Professor of Family Medicine
Michael W. Sue, MD
Associate Professor of Physician Assistant
Education
Jocelyn L. Sumcad, MD
Assistant Professor of Physician Assistant
Education
Gretchen Swanson, DPT
Adjunct Associate Professor of Physical
Therapy Education
Jamie L. Switzer, DO
Assistant Professor of Family Medicine
Brian M. Swope, DO
Assistant Professor of Pediatrics
Khanh Ta-Le, PharmD
Assistant Professor of Pharmacy Practice
Parvis Taherpour, MD
Assistant Professor of Family Medicine
Benjamin C. Tam, MD
Assistant Professor of Surgery/Orthopedics
Bruce L.M. Tannenbaum, MD
Professor of Family Medicine/Psychiatry
Mark A. Tapscott, DO
Assistant Professor of Surgery/Proctology
Collin Teguh, DO
Assistant Professor of Family Medicine
Edward Tessier, BA
Adjunct Instructor of Health Professions
Education
Stephen W. Thacker, DO
Associate Professor of Family Medicine
Jack (John) L. Thomas, DO
Assistant Professor of Family Medicine
Larry L. Thomas, MD
Assistant Professor of Family Medicine/
Emergency Medicine
Julie G. Thompson-Dobkin, DO
Assistant Professor of Internal Medicine/
Neurology
Nguyen Thong, MD
Assistant Professor of Internal Medicine
Rama K.P. Thumati, MD
Assistant Professor of Internal Medicine/
Cardiology
Brian L. Tiep, MD
Assistant Professor of Family Medicine/
Pulmonary Rehabilitation
Jeffrey Tipton, DO, MPH
Assistant Professor of Family Medicine/Public
Health
Eric M. Toder, DO
Assistant Professor of Family Medicine
Gilbert J. Toffol, DO
Assistant Professor of Internal
Medicine/Neurology
Helen Tonnu, PharmD
Assistant Professor of Pharmacy Practice
Bao Cong Tran, MD
Assistant Professor of Internal Medicine
208
Doug Dung Anh Tran, MD
Associate Professor of Surgery/
Otorhinolaryngology
Tanya Tuyen Tran, PharmD
Assistant Professor of Pharmacy Practice
Ingrid E. Trenkle, MD
Assistant Professor of Family Medicine/
Dermatology
Vincent M. Tristan, PA-C
Instructor of Physician Assistant Education
Lawrence Troxell, PharmD
Assistant Professor of Pharmacy Practice
William Tsai, DO
Assistant Professor of Family Medicine
Jonathan C. Tsao, DO
Assistant Professor of Family Medicine
Stephen W. Turay, MD
Assistant Professor of Family Medicine
Alfred L. Turner, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
Sheri R. Tysch, DO
Assistant Professor of Pediatrics
Paul M. Umof, MD
Assistant Professor of Family Medicine/
Emergency Medicine & Occupational Medicine
Khushro B. Unwalla, MD
Assistant Professor of Family Medicine/
Psychiatry
Sukhdev Uppal, MD
Assistant Professor of Pediatrics
Geraldine N. Urse, DO
Assistant Professor of Family Medicine
Daryoosh Valamanesh, MD
Assistant Professor of Internal Medicine
Guillermo J. Valenzuela, MD
Professor of Obstetrics/Gynecology
James P. Veen, DO
Assistant Professor of Physician Assistant
Education
Roger Vielbig, MD
Assistant Professor of Internal Medicine/
Cardiology
Rafael Villarosa, MD
Assistant Professor of Internal Medicine
Norman E. Vinn, DO
Associate Professor of Family Medicine
Michael P. Vitullo, DO
Assistant Professor of Family Medicine/
Emergency Medicine
Monique Ngoc Vo, PharmD
Assistant Professor of Pharmacy Practice
Lee E. Vranna, MD
Assistant Professor of Family Medicine/Physical
Medicine and Rehabilitation
Barton H. Wachs, MD
Assistant Professor of Surgery/Urology
Ralph D. Wade, DO
Assistant Professor of Family Medicine
Paul E. Wakim, DO
Assistant Professor of Surgery/
Orthopedics/Sports Medicine
Wendy Waldman, RPh
Assistant Professor of Pharmacy Practice
Bryan D. Walls, DO
Assistant Professor of Family Medicine/
Osteopathic Manipulative Medicine
James P. Warren, MD
Assistant Professor of Internal Medicine/
Radiology
Harry C. Watters, DO
Assistant Professor of Obstetrics/Gynecology
Gerald Weingarden, DO
Assistant Professor of Family Medicine/
Dermatology
Elliot Weinstein, MD
Assistant Professor of Pediatrics
209
Frederick R. Weiss, MD
Assistant Professor of Internal Medicine
Michael Weiss, DO
Associate Professor of Pediatrics
Jill Weissman, PharmD
Assistant Professor of Pharmacy Practice
Erna L. Wells, MPA, RN, CCM
Professor of Physician Assistant Education
Randall M. West, DO
Assistant Professor of Family Medicine
H. Eric Westman, DO
Associate Professor of Surgery/
Otorhinolaryngology
Frederick E. White, DO
Assistant Professor of Internal Medicine/
Radiology
Peter J. White, MD
Assistant Professor of Surgery/Anesthesiology
Rosamond C. White, PhD, RN, NP
Assistant Professor of Physician Assistant
Education
Janette M. Wilcox, DO
Assistant Professor of Family Medicine
Imani S. Williams, PA-C
Assistant Professor of Physician Assistant
Education
Kenneth L. Williams Jr., DO
Assistant Professor of Family Medicine
Paul W. Willis, DO
Assistant Professor of Family Medicine
Brian C. Wilson, MD
Assistant Professor of Internal Medicine/
Radiology
Rochelle L. Wilson, DO
Assistant Professor of Family Medicine
Deborah Kay Winberry, PA-C
Instructor of Physician Assistant Education
Heidi A. Winkler, MD
Assistant Professor of Pediatrics
Barry R. Wiss, DO
Assistant Professor of Internal Medicine/
Gastroenterology
Albert A. Witte, DO
Professor of Internal Medicine/Cardiology
Sandy Witzling, MD
Associate Professor of Surgery
Laurie M. Woll, DO
Associate Professor of Family Medicine/
Dermatology
Donna Wong, DO
Assistant Professor of Family Medicine
Thomas A. Woodbury, DO
Assistant Professor of Family Medicine
Clarence Woods Jr., MD
Associate Professor of Physician Assistant
Education
Sandor J. Woren, DO
Associate Professor of Family Medicine/
Emergency Medicine
R. Bruce Worth, MD
Assistant Professor of Family Medicine
George D. Wright, MD
Assistant Professor of Family Medicine
Craig J. Wronski, DO
Assistant Professor of Family Medicine/
Psychiatry
Brett Wyrick, DO
Associate Professor of Surgery
Anthony P. Yang, MD
Assistant Professor of Surgery/Orthopedics
Cecile Yared, PharmD
Assistant Professor of Pharmacy Practice
Ralph A. Yates, DO
Assistant Professor of Family Medicine
Florence Yee, PharmD
Assistant Professor of Pharmacy Practice
210
Jeffrey C. Young, DO
Assistant Professor of Family Medicine
John Yuen, PharmD
Assistant Professor of Pharmacy Practice
Joseph A. Zammuto, DO
Assistant Professor of Family Medicine
Stephen W. Zecher, MPT
Adjunct Assistant Professor of Physical Therapy
Education
Robert Zelman, DO
Assistant Professor of Internal Medicine/
Cardiology
Nicole Zimmerman, PhD
Instructor of Health Professions Education
Sheldon S. Zinberg, MD
Professor of Internal Medicine
Phillip C. Zinni III, DO
Assistant Professor of Family Medicine
Robert D. Zipser, MD
Associate Professor of Internal Medicine/
Gastroenterology
John P. Zopfi, DO
Assistant Professor of Surgery/Trauma Surgery
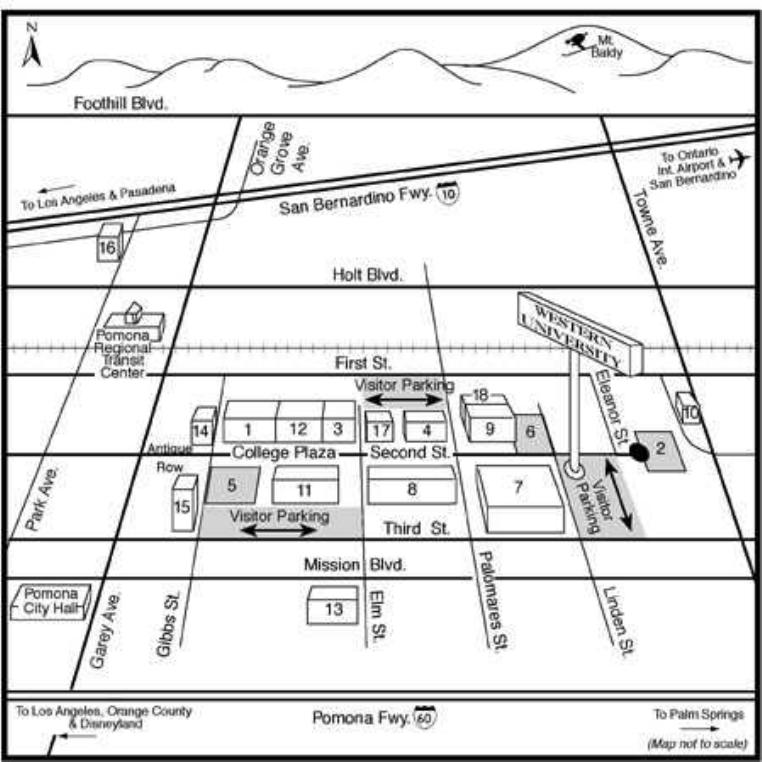
211
1. ALUMNI CENTER
2. UNIVERSITY PARK
3. BOOTH CENTER
4. BUSINESS CENTER
5. CENTENNIAL PARK
6. FOUNDERS PARK
7. HEALTH PROFESSIONS CENTER
8. HEALTH SCIENCES CENTER
9. VETERINARY SCIENCES CENTER
(future site)
10. MAINTENANCE/AUXILIARY SERVICES
FACILITY
11. STUDENT SERVICES CENTER
12. UNIVERSITY ADMINISTRATION
CENTER
13. WESTERN UNIVERSITY MEDICAL
CENTER
14. WESTERN UNIVERSITY CAMPUS
GOURMET/STUDENT LOUNGE
15. HEALTH SCIENCES LIBRARY AND
LEARNING RESOURCES CENTER
16. WESTERN UNIVERSITY VETERINARY
MEDICAL CENTER (future site)
17. INLAND EMPIRE CREDIT UNION
18. VETERINARY SCIENCES (future site)
How to Reach Western University
The University's main campus is located about 35 miles east of Los Angeles, in the City of Pomona. Ontario
International Airport is six miles east of the University and Los Angeles International Airport is located 60
miles west.

Catalogue Supplement: Doctor of Osteopathic Medicine Program
Page 46, Transfer Policy. Replace the entire transfer policy section with the following:
WesternU/COMP offers a transfer program for persons who have completed one or more years of medical studies at a medical school
accredited by the American Osteopathic Association (AOA) or Liaison Committee on Medical Education (LCME) and whose
curriculum is academically compatible with that of WesternU/COMP.
Candidates seeking transfer must be in good academic standing at the school where they are enrolled and be eligible for continuation
there. Candidates are expected to meet the minimum entrance requirements that are required of our entering first-year students. Please
refer to the Admissions Policies and Procedures section for specific information regarding these requirements.
Transfers from an LCME accredited medical school or college to a College of Osteopathic Medicine (COM) shall require that no less
than the last fifty percent (50%) of instruction be completed within the COM. In the case of such transfers, the COM requirement for
osteopathic manipulative medicine must be completed prior to graduation.
Transfer applications are available from the Admissions Office after September 1. Application deadline for students wishing to
transfer into the second year is March 1. Application deadline for students wishing to transfer into the third year is January 1. We do
not accept applications for transfer into the fourth year.
Candidates must provide:
1. Official transcripts from all colleges and universities attended.
Official transcripts showing the successful completion of studies at the medical school where currently enrolled.
2. Official MCAT scores.
3. Letters of recommendation from three science professors at your college of medicine and a letter from an osteopathic
physician.
4. A fully completed transfer application accompanied by a non-refundable application fee of $100.00.
5. Upon request, candidates must submit a letter of good academic standing from the Academic Dean of the medical school
where they are currently enrolled. If an interview is granted, candidates are invited to the campus at their own expense.
Candidates should plan to spend a half-day on campus for orientation and interview. Approximately three weeks after the
interview, candidates will receive a letter stating the decision of the Admissions Committee. Acceptance of a transfer student
will be dependent upon the student’s current academic good standing, qualifications, academic compatibility and available
space. Confirmation of available seats in the MSII class does not occur until mid-June.
Decisions of the Admissions Committee regarding the admissions of applicants to the Doctor of Osteopathic Medicine program are
final.
Applications are to be returned directly to: WesternU/COMP, Admissions Office
309 E. Second Street
Pomona, CA 91766-1854
Page 55: Insert the following paragraph at the end of the section entitled Attendance and Absences:
National Board Review Policies
The following policies are to be followed for any D.O. class wishing to have a National Board Review course.
• No
organized National Board Review course will be permitted on campus during the academic year (when classes are being
conducted).
• The COMP faculty (by discipline) will be available at the end of the MS-2 Spring semester for scheduling discipline reviews.
• No outside vendor or review organization can be invited to campus for a discussion without the approval of the Director of COMP
Student Services.
• Any outside vendor or review organization to be considered for conducting a review course shall negotiate the contract with the
Director of COMP Student Services and the COMP Assistant Dean of Academic Affairs.

• Final approval for any Review course will be by the Dean of the College of Osteopathic Medicine of the Pacific.
Page 56-57: Phase I: First Year-First Semester (CORE courses)
Replace the listed courses with the following listing containing revised credit hours:
DO 5010 Biochemistry (4.5 credit hours)
DO 5020 Embryology (1 credit hour)
DO 5025 Medical Genetics (1 credit hour)
DO 5030 Gross Anatomy (12.5 credit hours)
DO 5040 Histology (2 credit hours)
DO 5050 Microbiology (5 credit hours)
DO 5060 Pathology (2.5 credit hours)
DO 5070 Pharmacology (2.5 credit hours)
DO 5080 Physiology (1.5 credit hours)
DO 5090 Osteopathic Principles and
Practice I (2 credit hours)
Page 57: Phase II: Second semester-first year through Second semester-second year
Replace the listed courses with the following listing containing revised credit hours:
First Year-Second Semester
DO 5110 Dermal System (3.5 credit hours, 4 weeks)
DO 5120 Neurosensory System (15.5 credit hours, 10 weeks)
DO 5130 Musculoskeletal System (6.5 credit hours, 4 weeks)
DO 5140 Medical Ethics (Cr/NCr)
DO 5150 Introduction to Clinical Medicine I (ICM I) (2 credit hours, 1 week)
DO 5160 Behavioral Science & Substance Abuse (4 credit hours)
DO 5190 Osteopathic Principles and
Practice II (2.5 credit hours)
Second Year-First Semester
DO 6010 Blood & Recticuloendothelial System (6.5 credit hours, 3 weeks)
DO 6020 Cardiovascular System (9.5 credit hours, 9 weeks)
DO 6030 Public Health (1.5 credit hours, 1 week)
DO 6040 Respiratory System (9 credit hours, 7 weeks)
DO 6050 Psychiatry (2 credit hours)
DO 6090 Osteopathic Principles & Practice III (2.5 credit hours)
Second Year-Second Semester
DO 6110 Renal System (5 credit hours, 3 weeks)
DO 6120 Endocrine System (5.5 credit hours, 3 weeks)
DO 6130 Reproductive System (7 credit hours, 4 weeks)
DO 6140 Gastrointestinal System (11 credit hours, 7 weeks)
DO 6150 Introduction to Clinical Medicine II (ICMII) (Cr/NCr)
DO 6160 Medical Jurisprudence (1.5 credit hours)
DO 6190 Osteopathic Principles & Practice IV (2.5 credit hours)
Page 58, Clinical Curriculum: Replace the third year clinical rotations requirements with the following:
Third Year
1 Family Practice
3 Internal Medicine (2 General; 3
rd
General, GI, CARD, or PULM)
1 Surgery (General)
2 Pediatrics, or 1 Pediatrics and 1 additional Family Practice
1 Obstetrics/Gynecology
1 Osteopathic Manipulative Medicine
1 Psychiatry
1 Geriatrics, or 1 additional Family Practice, or 1 additional Internal Medicine
1 Vacation
Page 60:
DO 5030 Gross Anatomy: Change credit hours from 14.5 to 12.5
DO 5050 Microbiology: Change credit hours from 5.5 to 5
DO 5070 Pharmacology: Change credit hours from 3.5 to 2.5
Page 61:
DO 5110 Dermal System: Change credit hours from 4 to 3.5
DO 5120 Neurosensory System: Change credit hours from 17.5 to 15.5
DO 5130 Musculoskeletal System: Change credit hours from 7.5 to 6.5
DO 5160 Behavioral Science and Substance Abuse: Change credit hours from 2.5 to 4
Page 62:
DO 6010 Blood and Reticuloendothelial System: Change credit hours from 7.5 to 6.5
DO 6020 Cardiovascular System: Change credit hours from 14.5 to 9.5
DO 6030 Public Health: Change credit hours from 1 to 1.5
DO 6040 Respiratory System: Change credit hours from 9.5 to 9
DO 6110 Renal System: Change credit hours from 5.5 to 5
Page 63:
DO 6130 Reproductive System: Change credit hours from 8 to 7
DO 6140 Gastrointestinal System: Change credit hours from 13 to 11
DO 6160 Medical Jurisprudence: Change credit hours from 1 to 1.5
Page 64:
DO 6190 Osteopathic Principles and Practice IV: change credit hours from 5 to 2.5
Page 25: Insert the following at the end of the University Registrar section:
STUDENT LOAN DEFERMENT PROCESSING
Western University of Health Sciences participates in the National Student Clearinghouse, located in Herndon,
Virginia. Three times a semester, the University submits a report of students' enrollment status to the Clearinghouse,
which in turn supplies verification of enrollment to lending agencies.
A number of lenders and loan servicing organizations that are members of the Clearinghouse participate in a
Paperless Deferment Process. With this process, no paper forms need to be completed by either students or schools -
the student simply calls his or her servicer to request a deferment. The servicer then posts a deferment to the
student's account after the student's verbal order is matched against the Clearinghouse electronic data verifying in-
school status.
If a lender needs a deferment form processed, bring it to the Registrar’s Office. The Registrar’s Office will then
forward all deferment forms to the Clearinghouse, which will verify the student’s enrollment to the lender. Western
University of Health Sciences does not supply this information directly to lending agencies that participate in the
National Student Clearinghouse.
If a student has registered late, this information may not be reported until the submission of the next tape. The
Clearinghouse requests the student take the following steps if a collection letter has been received:
1. Call the lending agency to see if a deferment form was received between the time the Clearinghouse
supplied the information and the lending agency sent the collection letter.
2. If, after calling the servicer, it still appears that the deferment has not been processed, the student may
call the Clearinghouse at (703) 742-7791 and ask for a Student Service Representative. The representative
will verify the date on which the deferment form was received by the Clearinghouse, the date the deferment
was certified and mailed, the enrollment status that was certified, and where the forms were sent.
3. If an emergency exists -- for example, the student is 150 days delinquent and being threatened with
default -- the Clearinghouse will intervene on the student's behalf by faxing another enrollment certification
to the servicer. Further, it will work with the servicer to ensure that the form is processed on a high-priority
basis.
The Registrar’s Office will continue to process deferment requests to lending agencies that do not participate in
the Clearinghouse, however.
Catalogue Supplement: Master of Physical Therapy
Page 112: PT 5200 Foundations of Musculoskeletal Intervention has increased from 4 to 5 credit
hours, effective with the class entering in January 2001.
Page 112: PT 5210 Evaluation and Treatment of Upper Quarter Musculoskeletal Problems has
decreased from 6 to 5 credit hours, effective with the class entering in January 2001.
Page 115: PT 5200 has increased from 4 to 5 credit hours.
Page 115: PT 5210 has decreased from 6 to 5 credit hours.
Page 117: The following courses have been added to the offerings of the Department of Physical
Therapy Education:
PT 8100 Pharmacology for the Physical Therapist (3 credit hours)
Prerequisite: Bachelor’s or Master’s degree in Physical Therapy. This course addresses basic
and applied pharmacology for the practicing physical therapist. The content includes the effects
of pharmacotherapy on the health and well being of physical therapy patients.
PT 8120 Medical Screening and Systems Review (3 credit hours)
Prerequisite: Graduate of an accredited Physical Therapy program and current licensure as a
physical therapist. This course familiarizes the physical therapist with patient history and systems
review from the medical and physical therapy perspectives. Lecture notes, internet discussions,
and case discussions are used to prepare the PT for the appropriate medical screening and
physical examination skills required to practice in a direct access environment. A systems
approach is used to discuss common medical conditions, their epidemiology, etiology, clinical
manifestations, medical management and issues related to PT screening, examination,
interventions, and red flags.
Catalogue Supplement: Master of Science in Physician Assistant Studies
Page 139: PA 5000 CPR has been removed from the curriculum of the first semester of the MSPA
program. The total number of credit hours required for the first semester is thereby reduced to 27 units.
Page 140: Delete the course title and course description for PA 5000 CPR
Page 140: The course description for PA5005 Medical Terminology should read as follows:
This course is designed to provide a framework for building a comprehensive medical vocabulary. The
basic techniques of medical word building will be used to enhance appropriate use and spelling of medical
terms in oral and written presentations.
Page 143: Replace the decimal place numbering system for PA 7500 Extended Core Selectives with the
following:
PA 7500A Orthopedics
PA 7500B Oncology
PA 7500C Family Practice III
PA 7500D Infectious Disease
PA 7500E Cardiology
PA 7500F Cardiothoracic Surgery
PA 7500G Geriatrics
PA 7500H General Surgery II
PA 7500J Rheumatology
PA 7500K Endocrinology
PA 7500L Dermatology
PA 7500M Occupational Medicine
PA 7500N Trauma Surgery
PA 7500P Psychiatry
PA 7500Q Otolaryngology
PA 7500Y Directed Research/Independent Study
PA 7500Z Other
